An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Sage Choice


The Fallacy of Sham-Controlled Neurofeedback Trials: A Reply to Thibault and Colleagues (2018)
H. edmund pigott.
1 NeuroThrive, LLC, Lutherville, MD, USA
2 Private Practice, Juno Beach, FL, USA
3 Knoxville Neurofeedback Group, TN, USA
Mark Trullinger
Background: Sham-controlled neurofeedback (NFB) trials consistently find no separation on ADHD outcome measures leading many to conclude that NFB’s beneficial effects are due to placebo. Method: We deconstruct the NFB training methodology and findings of six sham-controlled trials that assessed for evidence of learning. Results: All six studies found no evidence NFB subjects learned to self-modulate the targeted electroencephalogram (EEG). Careful analyses revealed these studies’ training methodologies were antithetical to the established science of operant conditioning thereby preventing subjects from learning to self-modulate. These findings are in marked contrast to NFB studies whose methodology mirror the best practices of operant conditioning. Conclusion: The premise that NFB’s beneficial effects are due to placebo phenomenon is unproven as these studies compared two forms of false-feedback, not operant conditioning of the EEG. Because these studies are highly cited and considered the gold standard in scientific rigor, a reappraisal of the evidence is urgently needed.
This is now Thibault, Veissière, Olson, and Raz’s (2018) eighth publication making the same argument based on the consistent finding of no separation on any outcome measure when comparing so-called “genuine” neurofeedback (NFB) and sham feedback in sham-controlled trials (e.g., Thibault & Raz, 2017 ). The authors therefore assert that NFB operates as a placebo, all be it a powerful one, with effects commonly equivalent to optimized versions of established ADHD treatments (e.g., Pigott, 2017 ). In their current effort, the authors provide guidance how clinicians can ethically prescribe NFB “as a form of neurosuggestion therapy” ( Thibault et al., 2018 , p. 2). Our Guest Editorial deconstructs these sham-controlled studies demonstrating the fallacies of the authors’ argument. We also examine the evidence supporting neurosuggestion as a therapeutic intervention as well as that supporting NFB’s specificity, sustainability, and effectiveness when compared with stimulant medication (SM). Finally, we question why prescribe NFB as a placebo when with proper training clinicians can provide operant conditioning of the electroencephalogram (EEG) with proven sustained effects.
Learning Methodology Matters
Table 1 summarizes the methodology and findings from six sham-controlled trials treating ADHD. Although each study acknowledged NFB is based on operant learning, their methodology violated established learning science by using either automated or manually adjusted EEG reward thresholds to maintain an “about 80%” level of reward across sessions and subjects. This procedure is contrary to basic learning principles. First, operant conditioning targets a response followed by a stimulus-event to make the desired response occur more or less frequently and then plots the target response’s occurrence over time to document whether or not learning has occurred. In these studies, the target response was not consistently calculated, monitored, plotted, and presented to NFB subjects. Therefore, it is not known what response (if any) was conditioned. Second, the studies do not reference the effects of practice in the experimental process. Subjects in both groups engaged in the same set of behaviors during sessions (e.g., maintaining stillness and focus, reducing muscle and eye-movement artifacts, relaxation, posture, and breathing). If subjects did not engage in these practiced behaviors, their EEG data were riddled with artifact and worthless. Third, operant conditioning of the EEG requires that these core concepts are strictly adhered to demonstrating the operant behavior has been learned and such documentation of learning should occur before examining outcome measures of interest ( Cannon, 2015 ).
Sham-Controlled NFB Studies.
| Study citation | NFB training methodology | Key findings |
|---|---|---|
| “Feedback thresholds were automatically and dynamically adjusted every 30 s to keep power 80% of time above or below threshold (depending on whether feedback consisted of up or down training)” (p. 51). | 1. Study terminated when there was no trend of an NFB effect in the interim analysis. 2. Found “NFB treatment did not seem to affect EEG” (p. 51). 3. Found “most participants thought they were in the sham group. For the treatment group, 10 out of 14 (71%) participants thought they received sham feedback. 10 out of 12 participants in the sham group thought they were in the sham group” (p. 51). | |
| “Reward threshold levels were automatically adjusted every 30 s so that the child was rewarded about 80% of the time (i.e., received positive feedback)” (p. 279). | 1. Found “analyses revealed significant improvements of ADHD symptoms over time, but changes were similar for both Groups” (p. 275). 2. Found “75% of children and their parent(s) in the active neurofeedback group and 50% of children and their parent(s) in the placebo feedback group thought they received placebo feedback” (p. 275). 3. Based on these pilot results, the authors changed their NFB training methodology to have trainers adjust “manually the feedback parameters” for new subjects (p. 283). | |
| | “Reinforcement was provided for EEG theta–beta power ratio below a threshold that was set minute-to-minute by fuzzy logic based on the immediately preceding EEG” (p. 412). Auto-thresholding ensured subjects played videogames with full-control approximately 80% of the time. | 1. Both groups showed significant improvement in ADHD symptoms but there was no NFB specific effect. 2. In a subsequent publication ( ), authors report, “the sham group (as well as active group) showed no obvious EEG changes in a simple pre–post measure of theta/beta ratio” (p. 5). |
| | This is a continuation of . For newly enrolled subjects ( = 27) “reward threshold levels were manually adjusted so that the child was rewarded about 80% of the time (ie, received positive feedback), consequently the amount of reward remained at about the same level across sessions and across groups” (p. 823). | 1. Authors combined subjects from Lansbergen et al. ( = 14) with 27 new subjects who had “trainers” manually readjust thresholds to maintain the same “about 80%” level of reward. 2. Found “while total ADHD symptoms improved over time for both groups, there was no significant treatment effect” (p. 821). 3. Although authors report that “guessing assignment was no better than chance level” (p. 821), in a subsequent article ( ), the authors note, “most participants of NFB placebo-controlled RCTs conducted until now seem to experience the treatment as a placebo condition” (p. 2). |
| Same subjects/method as . | 1. Found “no significant treatment effect on any of the neurocognitive variables” (p. 460). 2. Pre–post EEG data were reported for only 10 of the 22 NFB subjects. Found more evidence of negative shaping of the EEG away from the reward targets than positive shaping. | |
| “Reward thresholds were automatically adjusted every 15 s to provide positive feedback about 80% of the time” (p. 677). | 1. Found “self-reported ADHD symptoms decreased substantially for all treatment groups between pretreatment and the end of 6 month follow-up, independent of treatment condition” (p. 673). 2. Found “no significant effect of time or treatment-by-time interaction was observed” (p. 678) for the targeted EEG confirming there was no evidence NFB subjects learned to self-modulate. |
Note. NFB = neurofeedback; EEG = electroencephalogram; RCT = randomized controlled trials.
In these studies, every reset of the EEG reward threshold delivered operant consequences to subjects’ brains antithetical to the goal of training. As Pigott and colleagues (2017) note
if the targeted EEG was strengthening, reinforcement was withdrawn and reset down to 80% thereby punishing participants for learning to self-modulate. Conversely, if the targeted EEG was decreasing, participants were reinforced up to 80% thereby rewarding them for decreasing its strength. (p. 897)
At every reset of the reward threshold, NFB subjects therefore were either rewarded for not learning to self-modulate the targeted EEG or administered a Type 2 punishment for the beginnings of success.
Given their flawed methodology, it is not surprising that all six studies found:
- No evidence NFB subjects learned to self-modulate the targeted EEG;
- No separation between NFB and sham feedback on any outcome measure; and
- When assessed, the vast majority (71% to 75%) of NFB subjects thought they received sham-feedback—correctly determining the NFB they received was often false.
Intriguingly, four of the studies also found significant improvement in both groups, leading Thibault and colleagues among many others to argue that these beneficial effects are due to placebo phenomena versus any specific effects from NFB. Two points in response below:
First, flawed methodology prevented NFB subjects from learning to self-modulate the targeted EEG and therefore no specific effects should be expected since each study compared two forms of false-feedback. Second, both groups participated in an active intervention. Ninaus and colleagues (2013) found multiple cortical regions of the brain are activated when blinded subjects were told to focus and try to control randomly moving bars during five 20-s rounds. In contrast, no such changes occurred when subjects were instructed to merely watch the moving bars. Subjects in sham-controlled trials are commonly instructed to sit still, focus, and use their brains to increase positive feedback. Similar cortical regions therefore likely underwent a vigorous workout during subjects’ 30+ sessions sitting still and trying to control that which was uncontrollable. This is hardly a “placebo” intervention as traditionally understood and likely only had positive effects because subjects were deceived into believing they had a 50% chance of receiving accurate EEG feedback. Transparency eliminated the brain activation found by Ninaus et al. as it likely would in all false-feedback trials.
Thibault and colleagues’ (2018) claim that NFB is a placebo is not supported by the referenced data. Their referenced studies compared two forms of false-feedback— not operant conditioning of the EEG . NFB has a 75+ year history of scientific inquiry documenting operant conditioning of the EEG in cats (e.g., Wyrwicka & Sterman, 1968 ), primates (e.g., Schafer & Moore, 2011 ), and people (e.g., Jasper & Shagass, 1941 ), including a 40-year history of research treating ADHD children ( Lubar & Shouse, 1976 ; Shouse & Lubar, 1979 ). The authors though dismiss this extensive research history asserting that “Following the results from recent double-blind studies, we can now add EEG-nf for ADHD to this list of placebo therapies that masquerade under other biomedical labels” (p. 2). In contrast, it is our assessment that it is these double-blind studies themselves that are the masquerade since they did not compare operant conditioning of the EEG with a sham-control but rather two forms of false-feedback.
Bad Science Begets More Bad Science
In their introductions, each of these sham-controlled studies states something similar to “neurofeedback is based on the assumption that deviant brain activity patterns can be voluntarily modulated by operant learning strategies” ( Schönenberg et al., 2017a , p. 674) and yet then used a methodology antithetical to operant learning. When we challenged Schönenberg and colleagues to either “acknowledge that their neurofeedback methodology violates the very essence of operant conditioning or explain the errors in our analysis” ( Pigott et al., 2017 , p. 897), these authors stated that they used a “previously established protocol” ( Schönenberg et al., 2017b , p. 897) and then made additional points unrelated to our analysis.
This is the problem. Bad science begets more bad science until it is corrected. Each of these studies cited one or more of their predecessors and appears more focused on single/double/triple blinding and empirical rigor than ensuring competence in administering the independent variable, in this case operant conditioning of the EEG. True scientific rigor demands a higher level of adherence to learning principles when evaluating treatments based on operant conditioning.
Unfortunately, the impact factors of the journals publishing these six studies ranged from 2.5 to 11.6 placing them in the mid-to-top tier of behavioral health journals. These studies therefore have had a nefarious impact on the scientific literature as they are highly cited in research and review articles, meta-analyses, editorials, and authoritative practice guidelines (e.g., AACAP, 2011 ) as well as by insurance companies when denying coverage since these studies are presumed to demonstrate that NFB has no specific effects when rigorously evaluated and therefore does not meet evidence-based treatment standards. This contaminated scientific literature has harmed the public by limiting access to a treatment with a long history of using operant conditioning to improve lives by teaching children and adults how to self-modulate targeted neuronal activity.
Neurosuggestion, Specificity, and Comparative Effectiveness
Thibault and colleagues (2018) argue it is the efficacy of suggestion and the placebo effect that drives behavioral change from NFB— nothing specific to NFB itself —and if transparent, clinicians can ethically prescribe NFB as a placebo treatment “with an eye for amplifying the psychosocial mechanisms of suggestion rather than grasping at the elusive neural signatures many practitioners speciously assign as the cause of ADHD” (p. 709). To buttress their argument, the authors cite an unpublished, uncontrolled, open-label feasibility study they presented at a hypnosis conference ( Veissière, Olson, & Raz, 2017 ). In this study, the authors used a decommissioned magnetic resonance imaging (MRI) machine as a prop with nine ADHD children. They told the children it was an inactive “brain machine” and the authors would “use it as a suggestion” to “help their brain heal itself.” While in the MRI, the authors “gave the children positive verbal suggestions to promote relaxation, focus, and confidence.” They report that in follow-up interviews, parents of two children “reported near complete remission of symptoms, and six reported improvements in areas such as confidence, self-control, and social skills” (p. 709) The authors then claim that “In essence, this study provided neurofeedback-like treatment, but instead of focusing on a specific physiological mechanism, we emphasized suggestion-based healing” ( Thibault et al., 2018 , p. 708, 709). Four points in response below:
First, besides the inherent potential for multiple biases in an unpublished, uncontrolled, open-label hypnosis study, we have no evidence of functional deficits or improvements in ADHD symptoms using standardized measures for such deficits in the children themselves. Instead, just post-treatment “qualitative” interviews conducted by the authors with the children’s parents of domains unrelated to ADHD’s core symptoms (e.g., “confidence, self-control, and social skills”). Furthermore, we have no data indicating the diagnoses were correct. One would assume an accurate differential diagnosis was conducted at some point in these children’s evaluation procedures; however, this is not clear given the lack of information available. Finally, this is a hypnosis feasibility study using an MRI machine as a prop, not “neurofeedback-like treatment.” It is hard to see how this study provides anything more than anecdotal support for a new experimental treatment.
Second, Thibault and colleagues ignore the evidence suggestive of NFB’s specificity and effectiveness in treating the “neural signatures” of ADHD. For example, in their double-blinded within-subject reversal design studies, Lubar and Shouse ( Lubar & Shouse, 1976 ; Shouse & Lubar, 1979 ) demonstrated both (a) the functional relationship between the sensory motor rhythm (SMR) and manifestation of hyperkinetic behaviors and (b) that through real-time SMR feedback paired with operant conditioning, ADHD children could learn to self-regulate SMR with the resulting improvements or worsening in their hyperkinetic behaviors based on whether they were reinforced to increase or decrease SMR. In their clinical utility of EEG article, Loo and Barkley (2005) state, “To demonstrate that EEG changes are responsible for treatment effects, reporting of actual EEG changes and correlation with treatment outcome must be shown” (p. 72). Four studies have met this challenge by correlating the extent of NFB subjects’ learning to self-modulate the targeted EEG with treatment outcome and found that those subjects demonstrating the greatest learning experience the most improvement on ADHD outcome measures ( Drechsler et al., 2007 ; Gevensleben et al., 2009 ; Janssen et al., 2016 ; Lubar, Swartwood, Swartwood, & O’Donnell, 1995 ). These findings provide further evidence that enhancing EEG self-regulation is the mechanism of change from NFB treatment versus “neurosuggestion” or other placebo effects. Furthermore, two randomized controlled trials (RCT) have compared electromyographic (EMG) biofeedback with NFB to control for both nonspecific effects and the effects of self-regulation training ( Bakhshayesh, Hansch, Wyschkon, Rezai, & Esser, 2011 ; Strehl et al., 2017 ). Both of these studies found that subjects learned to self-modulate the targeted physiological mechanism (either EMG or EEG) with NFB demonstrating significant superiority over EMG in reducing ADHD symptoms and this despite the fact that EMG subjects demonstrated more pronounced learning to self-regulate. Finally, in one RCT SM combined with NFB was found superior in multiple outcome domains at the end of treatment and 6-month follow-up to SM combined with attention training that used the identical instructions and game sequences as NFB except that the feedback was not based on subjects’ EEG thereby suggesting a specific effect for NFB as an augmentation to SM ( Li, Yang, Zhuo, & Wang, 2013 ). Lia and colleagues also found that the combined SM/NFB subjects used significantly lower doses of SM during follow-up and reported fewer adverse side effects.
Third, the authors fail to acknowledge that in eight head-to-head comparisons with SM (see Table 2 ), NFB resulted in essentially equivalent improvement in treating ADHD’s core symptoms ( Duric, Assmus, Gundersen, & Elegen, 2012 ; Flisiak-Antonijczuk, Adamowska, Chładzińska-Kiejna, Kalinowski, & Adamowski, 2015 ; Fuchs, Birbaumer, Lutzenberger, Gruzelier, & Kaiser, 2003 ; Gelade et al., 2017 ; Meisel, Servera, Garcia-Banda, Cardo, & Moreno, 2013 ; Moreno-García, Meneres-Sancho, Camacho-Vara de Rey, & Servera, 2019 ; Rossiter, 2004 ; Rossiter & La Vaque, 1995 ). These eight studies comprised 581 subjects and in only one head-to-head comparison ( n = 32) has SM been found superior to NFB ( Ogrim & Hestad, 2013 ). These comparative effectiveness studies provide strong evidence that NFB is an evidence-based treatment for ADHD.
Studies Comparing NFB With SM in Treating ADHD’s Core Symptoms.
| Study | Subjects/design | Key findings |
|---|---|---|
| 46 ADHD children and adults matched by age ( = 12.8 years), IQ, gender, and ADHD subtype to receive either 20 NFB sessions based on standardized EEG protocols ( = 23) or SM ( = 23) based on patient or parent preference. Outcome measure was the TOVA. | 1. Both the NFB and SM groups improved ( < .05) on measures of inattention, impulsivity, information processing, and variability, but did not differ ( > .3) on TOVA change scores. 2. The authors concluded, “The EEG biofeedback program is an effective alternative to stimulants and may be the treatment of choice when medication is ineffective, has side effects, or compliance is a problem” (p. 48). | |
| 34 ADHD children ages 8 to 12 years were assigned based on parental preference to NFB ( = 22) or SM ( = 12). NFB consisted of 30 60-min sessions with sessions administered 3 times per week. The NFB protocol was either theta/beta or SMR training dependent the child’s subtype of ADHD. The doses for the SM group were adjusted during study based on need and ranged between 10 and 60 mg/day. Outcome measures were the TOVA, Attention Endurance Test, and parent- and teacher-rated CBRS. | 1. Both groups showed significant improvement in each of the outcome measures with no significant differences between groups. 2. The authors concluded, “These findings suggest that neurofeedback was efficient in improving some of the behavioral concomitants of ADHD in children whose parents favored a nonpharmacological treatment” (p. 1). | |
| 62 ADHD children and adults ages 7-55 were matched to NFB ( = 31) or SM ( = 31) based on patient or parent preference. Patients were matched by (in order) age, sum of 4 baseline TOVA scores, IQ, gender, and ADHD subtype. The SM patients were titrated based on TOVA results and maintained on the dose that maximized TOVA scores. The NFB patients received either 40 sessions in office or 60 at home over 3 to 3.5 months based on standard protocols. Outcome measures were the TOVA for both groups and for the NFB group only the BASC and BADDS. | 1. Both the NFB and SM groups had similar significant improvements in attention, impulsivity, and processing speed on the TOVA with no significant differences between groups. 2. The NFB group demonstrated statistically and clinically significant improvement on behavioral measures (BASC, ES = 1.16, and BADDS, ES = 1.59). 3. The author concluded that “confidence interval and nonequivalence null hypothesis testing confirmed that the neurofeedback program produced patient outcomes equivalent to those obtained with stimulant drugs” (p. 233). | |
| 130 ADHD children and adolescents, ages 6 to 18 years, were randomly assigned to receive either (a) NFB, (b) SM, or (c) combined NFB/SM. After randomization, 39 dropped out (36 immediately after randomization), 13 from the NFB group, 15 from the SM group, 11 from the combined group resulting in 91 completing the study; NFB ( = 30), SM ( = 31), and combined ( = 30). The NFB group received 30 40-minute theta/beta sessions 3 times per week for 10 weeks. Outcome measures were the Inattention and Hyperactivity subscales of the parent-rated CMADBD-P. | 1. The parents reported highly significant effects of the treatments in reducing the core symptoms of ADHD, but no significant differences between the treatment groups were observed. 2. Although not significant, the NFB group showed twice the level of pre–post change in attention compared with the other two treatments (3.1 vs. 1.1 and 1.5 for the means) and NFB’s effect size was larger than the other two treatments on both the Inattention and Hyperactivity subscales and total score measures. 3. The authors concluded, “NFB produced a significant improvement in the core symptoms of ADHD, which was equivalent to the effects produced by methylphenidate, based on parental reports. This supports the use of NFB as an alternative therapy for children and adolescents with ADHD” (p. 1). | |
| 23 ADHD children, ages 7 to 14 years, were randomly assigned to receive either 40 theta/beta NFB ( = 12) or SM ( = 11). Outcome measures were behavioral rating scales completed by fathers, mothers, and teachers (ADHD RS-IV and ODDRS-IV) at baseline and post-treatment as well as 2- and 6-month follow-up of academic performance. | 1. In both groups, there were similar significant reductions in ADHD functional impairment as rated by parents and in primary ADHD symptoms by parents and teachers. 2. Significant academic performance improvements were only detected in the NFB group. 3. NFB gains were maintained in both the 2- and 6-month follow-up assessment. 4. The authors concluded, “Our findings provide new evidence for the efficacy of Neurofeedback, and contribute to enlarge the range of non-pharmacological ADHD intervention choices” (p. 12). | |
| 32 ADHD children, ages 7 to 16 years, were randomly assigned to receive either 30 sessions of QEEG-guided NFB ( = 16) or SM ( = 16). The 30 NFB sessions took place over 6 to 9 months. Outcome measures were parent and teacher Conners’ Rating Scales, BRIEF, CPT, QEEG and ERP. | 1. SM was superior to NFB with a large effect size on the Conners’ Rating Scales and confirmed by other outcome measures. 2. The QEEG spectral power in the theta and beta bands did not change in either group. 3. In ERP, the P3 no-go component increased significantly in eight of 12 SM responder patients, but did not increase in nonresponders or the NF group. 3. The authors concluded, “Our study supports effects for stimulants, but not for NFB. Effects of NFB may require thorough patient selection, frequent training sessions, a system for excluding nonresponders, and active transfer training” (p. 448). | |
| 115 ADHD children, ages 6 to 14 years, meeting similar criteria regarding the nature of ADHD were assigned to receive either 20 NFB sessions ( = 85) or MPH adjusted to their age ( = 30). Outcome measure was a structured interview of ADHD symptoms based on criteria. | 1. Both treatments significantly reduced ( < .01) the number of attention deficit, hyperactivity and impulsiveness symptoms in subgroups with attention deficit prevalence and mixed type ADHD. 2. There were only four children with hyperactivity and impulsiveness prevalence and none in the MPH group so a comparison between treatments could not be made for this subtype of ADHD. 3. The authors concluded, “The NF method proved similarly effective to methylphenidate in reducing the number of symptoms in two types of ADHD: ADHD with the prevalence of attention deficit and in mixed type ADHD” (p. 31). | |
| (6-month follow-up findings) | 112 ADHD children, ages 7 to 13 years, were randomly assigned to receive either 30 sessions of theta/beta NFB ( = 39), 30 sessions of moderate to vigorous PA ( = 37), or optimally titrated SM ( = 36) over the course of 10 weeks. Optimal SM was determined via the same procedures as the MTA (i.e., double-blind placebo-controlled titration in which subjects received in random order 1-week each of 5 mg, 10 mg, 15 mg, and 20 mg SM along with 1-week of placebo). At the end of each week, parents and teachers completed rating scales of inattention and hyperactivity-impulsivity along with a side effects questionnaire. This information was used to determine optimal SM dosing for 4 weeks prior to administering the post treatment outcome measures. There was no similar involvement of parents and teachers in NFB and PA treatments. Outcome measures were parent and teacher ratings on the SDQ and SWAN. | 1. All three treatments evidenced significant improvement on the parent-rated SDQ and SWAN Hyperactivity/Impulsivity scales ( < .001). 2. SM was superior to NFB and PA on the parent-rated SWAN Inattention scale ( < .001) and on all teacher-rated scales ( < .001). 3. concluded, “optimally titrated methylphenidate is superior to neurofeedback and physical activity in decreasing ADHD symptoms in children with ADHD” (p. 1) 4. At 6-month follow-up, reported, “Interestingly, teacher reports showed less inattention and hyperactivity/impulsivity at follow-up for NFB than PA (p = .004–.010), even after controlling for medication use (p = .013–.036). Our findings indicate that the superior results previously found for parent reports and neurocognitive outcome measures obtained with MPH compared to NFB and PA post intervention became smaller or non-significant at follow-up. Teacher reports suggested superior effects of NFB over PA” (p. 1). COMMENT: As the authors note, they followed a similar strategy as the MTA Cooperative study to determine optimal SM dosing. As analysis of the MTA study demonstrates, making parents and teachers integral to delivering SM and BT treatments biased the use of their ratings when compared to outcomes of treatments they were not involved with. Similarly in this study, it was the parent and teacher ratings that both identified the optimal SM dose and their subsequent ratings were then compared with parent/teacher ratings of NFB and PA subjects even though there is strong evidence that using parent/teacher ratings biases the report of outcomes favoring those treatments the parents and teachers were most involved in delivering. This is consistent with 6-month results that showed “outcome measures obtained with MPH compared to NFB and PA post intervention became smaller or non-significant at follow-up” as parents and teachers were “less proximal” in their follow-up assessments to their prior role of providing these assessments weekly for 5 weeks to determine optimal SM dosing. |
| ; | 59 ADHD children, ages 7 to 14 years, were randomly assigned to receive either 40 sessions of theta/beta NFB that was tailored based on learning curves ( = 21), BT that combined parent and teacher training along with 15 individualized cognitive therapy sessions for the child ( = 19) and protocol-driven pharmacology (PH; = 19). Outcomes measures were parent and teacher ADHD RS-IV ratings, parent ADDES ratings, and IVA/CPT. | 1. All three treatments evidenced a significant impact in reducing ADHD symptoms based on parent and teacher ratings as well as on IVA measures of attention and response control. 2. While the authors concluded that “From a global perspective, BT had the most extensive results, but PH had the greatest capacity to improve overall attention. NF was able to improve both control response and inattention” ( , p. 1), documents how this conclusion for BT was based on the biased ratings of parents and teachers who were integral to delivering the package of BT treatments, but not the NFB and PH treatments. 3. Furthermore, as reported by , “Treatment differences observed in attentional variables in post-treatment are not maintained in follow-up phase” (p. 222) thereby indicating that the report that “PH had the greatest capacity to improve overall attention” was not maintained in the follow-up IVA/CPT assessment. |
| (NFB/SM combination RCT) | 40 ADHD children, ages 7 to 16, were randomly assigned to combined NFB and SM or SM combined with attention training that used the identical instructions and game sequences as NFB except the feedback was not based on subjects’ EEG. Subjects were assessed using multiple parameters at baseline, after 20 treatment sessions, after 40 treatment sessions, and at 6-month follow-up. | 1. The study found that “compared to the control group, patients in the combination NFB/SM group had reduced ADHD symptoms and improved in related behavioural and brain function” (p. 1). 2. The combined SM/NFB subjects used significantly lower doses of SM during 6-month follow-up and reported fewer adverse side effects. 3. The authors concluded, “The combination of EEG feedback and methylphenidate treatment is more effective than methylphenidate alone. The combined therapy is especially suitable for children and adolescents with ADHD who insufficiently respond to single drug treatment or experience drug side effects” (p. 1). |
Note. IQ = intelligence quotient; NFB = neurofeedback; EEG = electroencephalogram; SM = stimulant medication; TOVA = Test of Variables of Attention; SMR = sensory motor rhythm; CBRS = Conners’ Behavior Rating Scale; BASC = Behavior Assessment System for Children; BADDS = Brown Attention Deficit Disorder Scales; ES = effect size; CMADBD-P = Clinician’s Manual for the Assessment of Disruptive Behavior Disorders–Rating Scale for Parents; ADHD-RS-IV = ADHD Rating Scale-IV; ODDRS-IV = Oppositional defiant disorder rating scale based on DSM-IV ; BRIEF = Behavior Rating Inventory for Executive Function; CPT = Continuous Performance Test; DSM = Diagnostic and statistical manual of mental disorders ; PA = physical activity; SDQ = Strength and Difficulty Questionnaire; SWAN = Strengths and Weaknesses of ADHD symptoms and Normal Behavior Scale; MPH = methylphenidate; BT = behavior therapy; ADDES = Attention Deficit Disorder Evaluation Scale; IVA = Integrated Visual and Auditory; CPT = Continuous Performance Task; RCT = randomized controlled trials; QEEG = quantitative EEG; ERP = evoked response potential; MTA = multimodal treatment study of children with ADHD; PH = pharmacology.
Fourth, Thibault and colleagues fail to acknowledge the extensive evidence from NFB studies whose training methodology mirror the best practices of operant conditioning. These studies consistently find NFB subjects learn to self-modulate the targeted EEG, this learning is associated with improvements on a wide variety of ADHD outcome measures of interest, and both are sustained at follow-up (e.g., Leins et al., 2007 ; Strehl et al., 2017 ; Strehl et al., 2006 ) even up to 2 years later ( Gani, Birbaumer, & Strehl, 2008 ). These findings demonstrating the sustained ability to self-modulate the targeted EEG during follow-up with ongoing symptomatic improvement are unlike anything in the placebo literature. Findings further buttressed by Doren et al.’s (2018) recent meta-analysis documenting the sustained effects on ADHD outcomes for NFB subjects in RCTs.
The NFB Field Shares the Blame
Although NFB’s origins are based in the science of learning, the field has been negligent at ensuring that clinicians, researchers, and device manufactures adhere to this science. Examples include the following:
- Monitoring within-session learning curves is not standard practice for NFB clinicians, and in fact it is our observation that most clinicians do not assess for evidence of learning.
- The vast majority of NFB studies do not assess for evidence of learning even though this is the presumed mechanism of change. It is only recently that this is required for publication in the industry-sponsored journal NeuroRegulation when authors claim to provide operant conditioning of the EEG.
- Virtually all device manufacturers include an auto-thresholding option despite Sherlin and colleagues (2011) clarion call that such systems violate learning science and “could effectively train in the opposite direction and result in an increase in aberrant and negative (EEG) behaviors” (p. 299). Unfortunately, this option is used by many, if not most, clinicians, particularly those who oversee multiple “NFB” sessions at a time.
As with any form of operant conditioning, there are learners and nonlearners. The same is true with NFB and it is learners who experience the most improvement on ADHD outcome measures. Given this fact, it is an indictment of the field that there are no studies comparing strategies to identify those practices that best promote subjects’ learning to self-modulate the targeted EEG. Consequently, there is no empirical guidance to determine which operant training methodologies are most effective in maximizing learning— and this in a field with a 75+ year history of basic and applied research .
Finally, the NFB field and its detractors continue to conduct research that violates behavioral principles, and both sides cite such substandard research when it supports their viewpoint. This practice must stop. Evidence of learning trumps all, and if there is no evidence of learning, operant conditioning of the EEG did not occur.
There is plenty of blame to go around, yet if the field is to evolve and progress, we must demand training methodologies that follow learning principles and proof that learning occurred from all who claim to perform NFB. Hence, our critique of Thibault and colleagues, and the sham-controlled studies on which their argument is based, is also a plea to NFB researchers and clinicians to demonstrate that their methods are consistent with the best practices in behavioral learning. If both sides can agree to this rigor, it will promote clarity and consistency in the NFB literature that is not present today and provide guidance to necessary steps for advancing it forward.
Most importantly, we hope our Guest Editorial conveys the truth that learning methodology matters. With this caveat, we strongly recommend operant conditioning of the EEG for the treatment of ADHD, either as a standalone treatment or augmentation to other evidence-based treatments. As for prescribing “neurosuggestion therapy” for the treatment of ADHD, more research is required since its underlying premise is unproven and evidentiary base anecdotal.
Author Biographies
H. Edmund Pigott is a licensed psychologist trained as a scientist-practitioner. He enjoys deconstructing and documenting errors in published research.
Rex Cannon is a neuroscientist and an accomplished author, researcher, and Editor-in-Chief for Neuroregulation. He is a staunch supporter of non-pharmaceutical, evidence-based practices to aid individuals to improve performance. He currently directs science and operations for Knoxville Neurofeedback Group and the development of treatment models for Intrauterine Drug Exposure (IUDE) and addictions.
Mark Trullinger is a PhD Candidate in the International Psychology Department of The Chicago School of Professional Psychology, Washington, D.C. He studies the barriers to the acceptance of innovative medical devices and technologies in mental healthcare. He is a Registered Psychology Associate in Maryland and the Managing Director of NeuroThrive, LLC.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: H.E.P. is board certified in neurofeedback and has consulted for Amen Clinics, Brain Resources, CNS Response, and the International Society of Neurofeedback and Research. He is also on the scientific advisory board of Narbis, a neurofeedback technology company. R.C. is board certified in neurofeedback and Editor-in-Chief of the journal NeuroRegulation . M.T. is board certified in neurofeedback.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The International Society of Neurofeedback and Research, Biofeedback Certification International Alliance, and Association of Applied Psychophysiology and Biofeedback contributed equally to the open access publication fees with our deep gratitude.

Helping the brain help us.
Type to Search
Board members and staff.

Estate Sokhadze, PhD President
Estate (Tato) Sokhadze received a Ph.D. in Human Physiology in 1988 in Novosibirsk, Russia. He completed a post-doctoral fellowship in Psychopharmacology at Wake Forest University in 2001-2003, and post-doctoral training in Cognitive Neuroscience at Rice University in 2004. His research interests include application of dense-array EEG/ERP brain mapping, neurofeedback, TMS, and other applied psychophysiological techniques in psychiatric research.

Valerie DeLar, MA CCC-SLP Secretary
Valerie DeLar, MA CCC-SLP, completed a BA in Psychology at Franklin and Marshall College in Lancaster, PA, and then went on to work as a computer programmer and systems analyst in the banking and insurance industries. Subsequently, she earned a master’s degree in Speech and Hearing Science from the University of Maryland, College Park, MD. She served as a Speech-Language Pathologist and research associate at Kernan Hospital (part of the University of Maryland Medical System in Baltimore, MD), where she participated in grants and publications related to language rehabilitation for stroke patients. She has been utilizing neurofeedback and neuromodulation techniques in private practice and in clinical settings since 2008. She worked with speech-language therapy clients utilizing neurofeedback at Upstate Pediatric Speech Therapy Services in Mauldin, SC for three years and now is owner/principal in her private practice Path to Vibrant Living located in Burke, VA where she focuses primarily on helping to improve academic performance.

Mark Zinn, PhD Treasurer
Mark Zinn obtained his Ph.D. in Psychology at DePaul University, working with Dr. Leonard Jason. He has a diversified background in quantitative EEG, psychology, computer science, graphic arts, piano performance, and applied psychophysiology. Between 2012 and 2014, Mark was a research consultant for the ME/CFS Initiative team headed Dr. Jose Montoya at Stanford University School of Medicine. During that time, he was involved in two major studies utilizing techniques in EEG to yield objective measurements for evaluating cognitive impairment in patients with ME/CFS, linking the patients’ symptoms to brain regions. Currently, Mark is a director and investigator at the NeuroCognitive Research Institute in Chicago, IL, where he conducts studies which model brain connectivity in patients using 3-D neuroimaging EEG techniques.

Jon Frederick, PhD Sergeant-At-Arms
Jon Frederick, PhD earned his degree in psychology in Dr. Joel Lubar’s lab at the University of Tennessee. He has worked as a postdoctoral fellow at the UT Health Sciences Center-Houston and the University of Minnesota, researching topics such as MRI in Autism, evoked potentials in ADHD and the efficacy of neurofeedback for dementia. His research focuses on mechanisms of learning in physiological self-regulation and interactions between EEG state discrimination and standard neurofeedback training. Dr. Frederick has authored or co-authored 53 scientific publications and conference presentations. He is currently in clinical practice in Lafayette, CO.

Mary Blair Dellinger, LPC, BCN
Mary Blair Dellinger is a Licensed Professional Counselor in the state of South Carolina. She completed her Masters in Professional Counseling at Liberty University. A graduate of Psychology and Neuroscience from the University of South Carolina in Columbia, Dellinger is BCIA Board Certified in neurofeedback. She has eight years experience working at a private practice in Greenville, SC conducting neurofeedback with adults and children. She has specialized training in use of advanced procedures such as LORETA neurofeedback, neurostimulation techniques, and BCIA certification in Heart Rate Variability (HRV) biofeedback. She was an editor for the recent publication Neurofeedback: The First Fifty Years .

Tom Collura
Thomas Collura is the Founder and President of BrainMaster Technologies, Inc., and Clinical Director of the Brain Enrichment Center, Bedford, Ohio, and is an Instructor with Stress Therapy Solutions, Beachwood, Ohio. He holds degrees in philosophy, biology, biomedical engineering, and mental health counseling, from Brown University, Case Western Reserve University, and Walden University. He has held staff and clinical positions with AT&T Bell Laboratories, the Cleveland Clinic Department of Neurology, and Siemens Medical Systems. He is a Diplomate of the Quantitative EEG Board, and Board Certified in Neurofeedback with the BCIA. He has received the Hans Berger Award of Merit from the AAPB, and is a fellow of the ISNR, and has received the ISNR Lifetime Achievement Award. He is a Past President of the ISNR and the AAPB. He is the author of “Technical Foundations of Neurofeedback” and co-editor of the “Handbook of QEEG and Neurotherapy,” both published by Taylor Francis. He holds numerous patents and has published in the areas of EEG, evoked potentials, and neurofeedback systems. His continuing interests are in EEG and QEEG in clinical and research applications, evoked potentials, and mental health and personal optimization applications. Certified as trainer by Biofeedback Certification Institute of America (BCIA)

Mark Trullinger
Mark Trullinger, MSc., BCN completed his masters in Psychology: Clinical Neuroscience from Wales, United Kingdom on International Scholarship and is currently a PhD Candidate in Washington D.C. His dissertation is on medical innovation in international healthcare. Mark is actively engaged in providing scientific and technical support to management of research projects and private enterprises within many settings. He is currently the Managing Director of NeuroThrive, LLC in Maryland and a consultant to various academic researchers, clinicians, and non-profits in the region. Mark’s expertise and experience are multidisciplinary and includes 5 peer-reviewed original research publications, numerous mental health grants, and designing and implementing clinician trainings in coordination with major universities. He has proven expertise in the healthcare industry: including over 8 years of clinical practice and 4 years BCIA certified, assistant behavioral director of one of the largest community mental health centers in the country, assistant program director and team lead for NeurExpand Brain Center, and chief operating officer of a neurology practice. He has served as a representative to the AMA CPT Editorial Panel meetings on behalf of multiple stakeholders and is a board member-at-large Foundation for Neurofeedback and Neuromodulation Research (FNNR). Mark has a history of passionate and high energy leadership across various organizations and settings. In his various roles, he always strives to advance value-driven business and practice. His leadership crosses a wide spectrum of professional settings and is directed toward achieving his goals of implementing healthcare practices that are culturally sensitive, purposeful, and innovative. Mark has lead multidisciplinary teams in clinical settings for achieving goals and elevating spirits and inspiration in team members while acting as a mentor and source of thought leadership. He has a record of being involved in co-curricular events such as, but not limited, to fundraising, participating and assisting in planning events, conferences, trainings, etc. Mark has always strived to continually learn and improve himself, while giving back through mentoring of junior members. Fun Fact: Mark enjoys learning to fly and international travel.

Thomas Feiner
Thomas Feiner QEEG-D, BCIA, Naturopath, is the founder and director of the Institute for EEG-Neurofeedback (IFEN). He studied Occupational Therapist, and was one of the first Neurofeedback providers in Germany. Located in Munich, he runs a center for neurofeedback, where he utilizes modern brain-based assessments and offers treatments with innovative technologies, such as Photobiomodulation and Hyperbaric Oxygen Therapy for the treatment of brain disorders. Feiner is an internationally sought-after instructor and speaker for Neurofeedback, Peak Performance and health and lifestyle related topics. The Institute for EEG-Neurofeedback offers certification programs for Neurofeedback worldwide and organizes workshops and international conferences. He is a founding member of the Global Neurofeedback Initiative (GNI). Furthermore, he founded the QEEG Research Unit to study the brainwave changes that occur during certain meditation states. Meanwhile, he has studied and analyzed over 5000 EEGs from meditators. Thomas Feiner published many articles and book chapters on neurofeedback, stress, and optimization and maintenance of human performance and brain health in general. As head of the IFEN-Neuroscience laboratory, one of the largest private neuroscience research institutes in Germany, he has develops innovative tools for research and neurofeedback practitioners. Among them is the program “CAPITO” which he developed to measure and to monitor cognitive functions. Some features of this program are stimulus presentation and the evaluation of the results thanks to the sLORETA projection. This method leads to new insights into emotional decision-making processes through the so-called Gamma-Asymmetry. Another achievement of him and his team is a system that helps to administer and analyze cognitive evoked Brain Potentials. With their ERP-Analyzer it is also possible to measure Event-Related Potentials in a short amount of time. He also participates with international researchers in the study of so-called Heart beat evoked potentials (HEPs), a new field of research that provides valuable insights into heart-brain interaction with potential of showing mental disturbances from a very different perspective. In addition to running his center and institute, Thomas Feiner is also an inventor who, for example, invented the Free-Cap. This salt water cap he developed is already being used with great success in hundreds of practices around the world. He also developed a new method of Z-Score training, in which individual components can be trained in a protocol that precisely targets deviant Z-scores. Other neurofeedback protocols, such as the SCP training protocol for the Brain-Avatar platform, are also used by many practitioners. Since his interest has always been in optimizing the training process and breaking new ground, he has also become the father of a number of new neurofeedback games for virtual reality. Thomas Feiner furthermore maintains a highly regarded neurofeedback blog, where he documents the latest developments in neurofeedback and brain training. He also sees it as his mission to raise awareness of brain health and optimal performance among the public, especially for children. He has also created numerous materials to help children with learning disabilities overcome their problems with writing and math.

Rebecca Bassham
Rebecca Bassham is a health educator who after working as a medical imaging specialist studying the brain from the inside out, has committed her life to helping people to become healthier through facilitation of mind-body awareness. She is board certified in Neurofeedback (BCN), Quantitative EEG technologist (QEEG-T), and HRV, a licensed Radiologic Technologist (ARRT), has a BS degree in Exercise Science with a minor in Health promotions from CSUF, completed a fellowship in Special Imaging (CT and MRI) at Loma Linda University and studied Applied Psychophysiology at Saybrook University. Rebecca has worked in the field of health and wellness for over 30 years with experience to include employee health, facilitating lifestyle change programs, and promoting community health education and outreach through radio, television, and email news campaigns. After discovering the power and healing of neurofeedback within her own family, she embarked on her studies of applied neuroscience in 2010. Rebecca has worked in private practice, peak performance, and as a Psychophysiology Specialist at Pure Sports Recovery where her focus was with multi-traumatized recently retired NFL players. These clients present simultaneously with traumatic brain injury, PTSD, mood disorders, addictions, and/or chronic pain. Her multi-modality approach includes a wide variety of tools beginning with qEEG Brain Mapping, a psychophysiological stress profile, live 3D sLORETA Imaging, Neurofeedback, peripheral Biofeedback, and several neuromodulation technologies to foster optimal brain states. She is a BCIA-approved mentor for aspiring neurofeedback practitioners. Rebecca facilitates groups with life and wellness coaching to include brain fitness strategies, nutrition, exercise, goal setting, mindfulness, stress management, and time management for a holistic, alternative approach to improve cognitive function. She is also experienced with and certified in equine-assisted learning. Rebecca has mentored since 2015 with EEG authority Jay Gunkelman and has a sophisticated approach to qEEG data analysis, reporting, and treatment planning. At the heart of her rapid stabilization approach for the multiply traumatized is her bottom-up approach that emphasizes regaining brain cellular health and capacity via tight integration of brain stimulation and feedback-driven approaches.
Advisory Board

Former FNNR (ISNR Research Foundation) Board of Directors members
Marcie Zinn
Efthymios Angelakis
Martijn Arns
Ivette Bledsoe
Genie Bodenhamer-Davis
Helen Budzynski
Richard Davis
Jay Gunkelman
Ali Hashemian
Cynthia Kerson
Barry Sterman
Robert Thatcher
You must be logged in to post a comment.
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Perspectives on Type III Statistical Errors: Exaggerating the Effects of Placebo in Neurofeedback

NeuroRegulation
Related Papers
Frontiers in Human Neuroscience
Pierre Philip , Pierre Alexis Geoffroy
Journal of Attention Disorders
Xueliang Pan
Cynthia Kerson
Objective: Additional treatments with persisting benefit are needed for ADHD. Because ADHD often shows excessive theta electroencephalogram (EEG) power, low beta, and excessive theta-beta ratio (TBR), a promising treatment is neurofeedback (NF) downtraining TBR. Although several nonblind randomized clinical trials (RCTs) show a mediumlarge benefit for NF, a well-blinded, sham-controlled RCT is needed to differentiate specific from nonspecific effects. Method: Experts in NF, ADHD, clinical trials, and statistics collaborated to design a double-blind multisite RCT. Results/ Conclusion: At four sites, 180 children aged 7 to 10 years with rigorously diagnosed ADHD and TBR ≥ 5 will be randomized to active TBR-NF versus sham NF of equal duration, intensity, and appearance. Sham, utilizing prerecorded EEGs with participant artifacts superimposed, will keep participants and staff blind. Treatment fidelity will be trained/ monitored by acknowledged NF leaders. Multidomain assessments before,...
Objective: Additional treatments with persisting benefit are needed for ADHD. Because ADHD often shows excessive theta electroencephalogram (EEG) power, low beta, and excessive theta-beta ratio (TBR), a promising treatment is neurofeedback (NF) downtraining TBR. Although several nonblind randomized clinical trials (RCTs) show a medium-large benefit for NF, a well-blinded, sham-controlled RCT is needed to differentiate specific from nonspecific effects. Method: Experts in NF, ADHD, clinical trials, and statistics collaborated to design a double-blind multisite RCT. Results/Conclusion: At four sites, 180 children aged 7 to 10 years with rigorously diagnosed ADHD and TBR ≥ 5 will be randomized to active TBR-NF versus sham NF of equal duration, intensity, and appearance. Sham, utilizing prerecorded EEGs with participant artifacts superimposed, will keep participants and staff blind. Treatment fidelity will be trained/monitored by acknowledged NF leaders. Multidomain assessments before, ...
Samuel Veissiere
Recent critical publications on neurofeedback raise a conundrum: Does EEG-neurofeedback (EEG-nf) work, and if so, how? In a series of papers, we reported that EEG-nf seems to help the symptoms of ADHD, but for different reasons than most advocates would expect—i.e., due to a placebo response (Thibault, Lifshitz, Birbaumer, & Raz, 2015; Thibault & Raz, 2017). In this Guest Editorial, we address ethical considerations concerning prescribing placebos and highlight how we can leverage prevailing brain-based beliefs about behavioral disorders to better treat patients. We conclude that clinicians can apply EEG-nf to ADHD as a form of clinical suggestion for patients with the time, finances, and inclination to pursue such a treatment.
Sarah N Wyckoff
Clinical EEG and Neuroscience
Anton Coenen , Ute Strehl
European Child & Adolescent Psychiatry
Günter Esser
Journal of the American Academy of Child and Adolescent Psychiatry
Paramala Santosh
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Practice in Clinical Psycholoy (JPCP) , Elnaz Ensafi
International Journal of …
Birgit Holl
Journal of Neurotherapy
E. Sokhadze
Tristan Sguigna
Robert Brennan
European child & adolescent psychiatry
CATHLYN NIRANJANA BENNETT
Applied Psychophysiology and Biofeedback
Clinical Neurophysiology
Bjoern Albrecht
Tato Sokhadze
javier garcia campayo
Neurofeedback as an Integrative Approach to Health
Roxana Sasu
Neuropsychiatric Disease and Treatment
Irene Elgen
Dove Medical Press
Siegfried Othmer
Biological Psychology
Steven Lynn
Shahrokh Amiri , Arash Mohaggheghi
International Journal of Environmental Research and Public Health
LAURA M CAÑAMERO
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024

to your new world of serenity and brain power

We, at NeuroThrive, provide comprehensive and individualized services for people from all walks of life. Our services are designed to improve brain health and function. During the course of the day our brain helps us perform every single action and function; yet it does not occur to most of us how important it is to take care of our brain and it's well-being. At NeuroThrive, our team provides science based treatments personalized to each individual to optimize brain functioning. We use cutting edge technology for Neurofeedback, customized cognitive-skills training, lifestyle behavioral change, and other neurotherapeutics in order to change and optimize specific brain areas for best overall brain functioning through neuroplasticity. We also serve those who have acquired or experience biological based brain disorders to reach their life goals and maximize their quality of life and cognitive functions. We are a full psychological practice and provide services for clinical and non clinical goals. It is essential to keep in mind that therapy is not a magic pill or a quick fix: therapy is a healing process that necessitates participation and investment from the patient and caretaker alike. But in the end, making small changes to self-defeating behavior and coping with feelings of sadness, fear, and pain can bring life-altering results.
We look forward to riding this wave with you!
Our Services
How we, can help you., neurofeedback, stress reduce & meditation, brain mapping, counseling and brain coaching, cognitive skills, academic excellence, neuro-cognitive evaluation, executive coaching, meet the team.

Deepti Pradhan

Mark Trullinger
Managing Director

3505 Ellicott Mills Dr, B-1
Ellicott City, MD 21043
BUSINESS HOURS
Monday - Friday
11 a.m. - 6 p.m.
Phone : (443) 810- 9483
Fax: (410) 828- 4269
Email: [email protected]
Success! Message received.
The Interational Society of Neurofeedback & Research

Mark Trullinger, BCN
Mark has his BCN certification from BCIA and his QEEG-D certification from the QEEG Certification Board, with 8+ years of clinical practice. He has attended AMA CPT Editorial Panel meetings as a volunteer to represent the interests of ISNR for the past few years. Starting initiatives to modernize Neurofeedback coding and petition for inclusion as an AMA recognized organization in their CPT/RUC efforts going forward. He is also the managing director of NeuroThrive in Maryland, a private psychology practice with a strong track record of insurance reimbursement from many public and private payers and has numerous Neurofeedback publications. He is also a student of International Psychology, completing his dissertation this year. It is titled "Paradigm Shifting and Healthcare Professionals Impact on the Adoption of Innovative Medical Devices for Treating Mental Disorders: Neurofeedback for ADHD in the U.S. and The Netherlands."

Topic: CPT Billing
Presentation Title: Update on the Work Towards CPT Codes and Third-Party Reimbursement
Friday, October 19 at 11:30 AM
ISNR, in partnership with AAPB and BCIA, have taken significant strides in the past few years toward pushing for insurance reimbursement. This presentation will provide a macro-level progress report on the CPT coding workgroup trying to modernize our codes, petitions for inclusion as a recognized organization for AMA activities for CPT coding and Relative-Value Unit (RVU) determinations, and national level efforts for insurance reimbursement.

- Find a Mentor
- Find a Provider
- Find a Member
Meet the ISNR Committees
The ISNR does a lot, but it takes a lot of people to make it happen! Chairpersons of each committee are listed below. If you would like to get in touch with them, please click on the chairperson’s name to communicate by e-mail or reach out to Susan Alvarez, Executive Director, at [email protected] .
Standing Committees

Executive Committee
Chaired by the current President of the Board, Tanya Morosoli, MSc
Personnel Committee

Ethics Committee
Chaired by Robert Longo, LPC
ISNR values the credibility of our field and for this reason, the Ethics Committee’s role is to help improve the professionalism and ethical conduct of professionals and organizations utilizing neuroregulation techniques, including internationally.
It is important to mention that ISNR is not a legal entity nor a professional board that has authority to penalize or admonish clinicians or organizations. This committee can only make recommendations in order to help those providers and organizations more clearly align their work with the ISNR Code of Ethics .
Any individual may file an ethics inquiry about an ISNR member to the ISNR Ethics Committee.
If you are concerned about the practice of a provider, please first address it with the provider. If there is no resolution or the event is suspected to be illegal, please report it to the licensing board and/or other related agency.
The Ethics Committee is committed to maintaining a welcoming and safe environment for all our members. Please click here to file a complaint.

Conference Committee
Chaired by Noel Larson Ford , the Conference Committee is responsible for planning and organizing the annual conference.
Nominations Committee
Chaired by Robert Longo, LPC , the Nominations Committee is responsible for seeking out and announcing nominations.
Structure Committee
Chaired by Robert Longo, LPC

Finance Committee
Chaired by the current Treasurer of the Board, Dr. Nicholas Colosi , the Finance Committee is responsible for keeping track of the financial well-being of ISNR.
Public Relations Committee
Ad-hoc committees.

Membership Committee
Chaired by Tanya Morosoli , MSc, BCN , the Membership Committee is responsible for keeping track of current members and reaching out to new members.

Student Advocacy Committee
J. Claire Gregory, PhD chairs the Student Advocacy Committee (SACom) of ISNR. The SACom acts as a liaison between students and the Society as a whole by sponsoring special meetings and activities and maintaining a student forum. The SACom works to increase both domestic and international student affiliate membership and to foster a lifetime affiliation with ISNR. The mission of the SACom is to attract and retain student members and to serve as a major resource promoting access to the benefits of the student membership in ISNR. Finally, the SACom is an advocate for the issues and concerns of the student affiliate members of ISNR.

Neuroregulation Guidelines Committee
The Neuroregulation Guidelines Committee is Chaired by Dr. Michael Trayford .

Website Committee

Public Education Committee
Chaired by Cynthia Wilson , the Education Committee is responsible for planning and implementing a continuing education program called ISNR University as well as running ISNR webinars.

Vetting Committee
Chaired by Alissa Paramo, MS, BCN , the Vetting Committee is committed to high standards that assure each vendor and each item being displayed at ISNR conference will meet ISNR criteria for quality, honesty, and reliability. For the list of the criteria, please click here .
Vendors – Please click here to fill out the vetting form.
Members – We welcome your feedback about any products being displayed at the ISNR conference. Please click here to submit your feedback.


Neuroregulation Journal
Rex Cannon, PhD is the editor of the NeuroRegulation Journal. If you are interested in submitting research articles to this publication, please contact Rex Cannon, PhD.

CPT Committee
The CPT Committee is chaired by Mark Trullinger, PhD .
We’ve Moved…
To accommodate the organization’s growing needs, we have decided to move our office to a new location.
2146 Roswell Road
Suite 108, PMB 736
Marietta, GA 30062
Start typing and press enter to search
Are you having problems clicking next on the membership form, internet explorer 7 on windows.
- Click the “Tools” menu
- Click “Internet Options”
- Select the “Privacy” tab
- Option 1: To enable third-party cookies for all sites
- Click “Advanced”
- Select “Override automatic cookie handling”
- Select the “Accept” button under “Third-party Cookies” and click “OK”
Firefox 3 on Windows
- Click “Options…”
- Select the “Privacy” menu
- Make sure “Keep until” is set to “they expire”
- Option 1: To enable third party cookies for ALL sites: Make sure “Accept third-party cookies” is checked
Safari on Apple OS X:
- Click the “Safari” menu
- Click “Preferences…”
- Click the “Security” menu
- For “Cookies and website data” unselect “Block all cookies”
- For “Website tracking”, unselect “Prevent cross-site tracking”

Firefox 3 on Apple OS X:
- Click the “Firefox” menu
- Click Preferences…
- Click the Privacy menu
- Option 1: To enable third-party cookies for ALL sites: Make sure “Accept third-party cookies” is checked
Google Chrome on Windows
- Select the Wrench (spanner) icon at the top right
- Select “Options”
- Select the “Under the Hood” tab
- Select “Allow all cookies” under “Cookie Settings” and click “Close”
Internet Explorer 6 on Windows
- Move the settings slider to “Low” or “Accept all cookies”
Opera 9 on Windows
- Click the “Advanced” tab
- Select “Cookies” on the left list
- Make sure “Accept cookies” is selected and uncheck “Delete new cookies when exiting Opera”
- Who is BCIA?
- Board of Directors
- What is Certification and Who Recognizes It?
- BCIA Professional Standards/Ethical Principles
- Modalities Comparison Chart
- BF Entry Level
- BF Technician
- BF Technician CPE
- NF Entry Level
- NF Technician
- NF Technician CPE
- HRV Certification/Certificate Comparison
- HRV Certification Entry Level
- HRV Certification CPE
- HRV Certificate
- PMDB Entry Level
- PMDB Technician
- International Fee Structure
- International Training & Seminars
- BCIA Australia
- BCIA Hispanoamerica
- International BF/NF Associations
- Consumers - Find a Practitioner
- Certificants - Find a Mentor
- Biofeedback
- Neurofeedback
- Lapsed Recertification
- Mentoring Application
- Didactic Accreditation Training Fees
 -->
--> | |
|
Friday, December 16, 2022 11am Pacific, Noon Mountain, 1pm Central, 2pm Eastern 90 minutes $40 for those in Group I (US, Canada, etc.) with a reduced fee structure with possible savings for international attendees. For more information on the international fee structure, . Mark Trullinger, PhD, BCN Clinical Update/Ethics webinar will provide 1.5 CE's towards the requirement for recertification. Purchase a seat for the live event as we will record this webinar. You'll be among the first to receive a link which will enable you to view the entire presentation and earn your CE. The training program will address common billing and coding mistakes in biofeedback and neurofeedback. It will include the proper ways to bill and code biofeedback and neurofeedback, including when the requirements for using the CPT code are met or not met. In doing so, it will cover the importance of scope of practice. It will provide a foundation understand some of the complexities around telehealth, remote training, and home training with biofeedback and neurofeedback with CPT coding. It will address the role of the FDA in regulating biofeedback and neurofeedback, including the presence of and ability to obtain “on label” uses for specific diagnoses under current categories. It will also address how a provider can advertise for their services and how that varies from a device manufacturer. The goal is to empower the licensed providers offering biofeedback and neurofeedback services, through education about what is proper and removing the ruthless myths that continue to perpetuate in the field, to feel confident in their practice and how they represent themselves to the public.
1. Be able to correctly identify the CPT coding for biofeedback and neurofeedback, whether in office, telehealth, home training, or remote training.
|







IMAGES
VIDEO
COMMENTS
Mark Trullinger, PhD has a history of passionate and high energy leadership across a wide spectrum of professional settings with a focus on value-driven, culturally-sensitive, purposeful and innovative health care practice. He is currently the Managing Director of NeuroThrive, LLC in Maryland and a consultant to various academic researchers ...
Mark Trullinger, PhD, BCN, QEEG-D Managing Director, NeuroThrive BrainFutures Advisor brainfutures.org 2 Neurofeedback | Acknowledgements. Neurofeedback 3 BrainFutures. Executive Summary A CHALLENGING TIME. BRAIN-BASED DISORDERS ON THE RISE The incidence of attention-deficit hyperactivity disorder
Mark Trullinger is a PhD Candidate in the International Psychology Department of The Chicago School of Professional Psychology, Washington, D.C. He studies the barriers to the acceptance of innovative medical devices and technologies in mental healthcare. He is a Registered Psychology Associate in Maryland and the Managing Director of ...
Mark Trullinger. Background: Sham-controlled neurofeedback (NFB) trials consistently find no separation on ADHD outcome measures leading many to conclude that NFB's beneficial effects are due to ...
Mark Trullinger. Mark Trullinger, MSc., BCN completed his masters in Psychology: Clinical Neuroscience from Wales, United Kingdom on International Scholarship and is currently a PhD Candidate in Washington D.C. His dissertation is on medical innovation in international healthcare.
John Sullivan, PhD CEO Clinical and Sports Consulting Services Tara Thiagarajan, PhD Founder and Chief Scientist Sapien Labs Mark Trullinger, MSC, BCN Managing Director NeuroThrive Bruce Wexler, MD Professor Emeritus of Psychiatry Yale University School of Medicine Brain Fitness and Executive Function 3.
Vol. 6(1):38-41 2019 doi:10.15540/nr.6.1.38 Trullinger et al. NeuroRegulation Author Disclosure Mark Trullinger receives grant funding as a primary investigator from BrainFutures, is a board member of the Foundation for Neurofeedback and Neuromodulation Research, and is the managing director of NeuroThrive, LLC.
Instructor: Mark Trullinger, PhD, BCN, QEEG-D, Registered Psychology Associate (Maryland) Office: Virtual Office Hours: Monday, Wednesday, and Friday 8am-9am and by appointment. All office hours are distance only. I will either call or set up a Microsoft Teams meeting with you. Office Phone: 443-810-9483(Cell) Email:[email protected]
Mark Trullinger . Managing Director. Contact Us. CONTACT US. 3505 Ellicott Mills Dr, B-1. Ellicott City, MD 21043 ...
Mark Trullinger, BCN. Mark has his BCN certification from BCIA and his QEEG-D certification from the QEEG Certification Board, with 8+ years of clinical practice. He has attended AMA CPT Editorial Panel meetings as a volunteer to represent the interests of ISNR for the past few years. Starting initiatives to modernize Neurofeedback coding and ...
Rex Cannon, PhD is the editor of the NeuroRegulation Journal. If you are interested in submitting research articles to this publication, please contact Rex Cannon, PhD. Contact CPT Committee The CPT Committee is chaired by Mark Trullinger, PhD.
Infraslow Neurofeedback, the Latest Research. August 2020. Conference: International Society for Neuroregulation and Research 28th Annual Conference. Authors: Mark Llewellyn Smith. Neurofeedback ...
Mark Trullinger, MSc, BCN, Ana Maiques, Nicholas J. Dogris, PhD, BCN, QEEG-D. 9/7/2017. Neuroelectrics' pioneering work in advancing the science and application of tDCS (transcranial direct current stimulation) to address a wide range of health conditions, including ADHD, autism and depression, will be shared.
Presented by: Mark Trullinger, PhD, BCN. Type of Webinar: Clinical Update/Ethics webinar will provide 1.5 CE's towards the requirement for recertification. What if I can't attend the live presentation? Purchase a seat for the live event as we will record this webinar.
Mark Stephen Trullinger is a Lutherville, Maryland based psychologist who is specialized in Clinical Psychology. His current practice location is 1205 York Rd ... 443-777-8742 Gerard J Hunt, PHD Cognitive & Behavioral Psychologist 1300 York Rd Ste C300, Lutherville, MD Phone: 410-853-7691 Fax: 443-519-5167 Lisa Jane Hoffmeyer, PH.D. LICENSED ...
Mark Trullinger. Professor in the Counseling department at Marshall University. 0%. Would take again. 4. Level of Difficulty. Rate Compare. I'm Professor Trullinger. Check out Similar Professors in the . Counseling Department 5.00 Jonathan Lent; 5.00 Michelle Biggs; 5.00 Morgan Conley; 1; Student Ratings. All courses. COUN609. Apr 12th, 2021 ...
Trullinger et al. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (CC-BY). Edited by: Nancy L. Wigton, PhD, Grand Canyon University, Phoenix, Arizona, USA Reviewed by: John Davis, PhD, McMaster University, Hamilton, Ontario, Canada
Ostrogozhsk population. Ostrogozhsk (Russian: Острого́жск) is a town and the administrative center of Ostrogozhsky District in Voronezh Oblast, Russia, located on the Tikhaya Sosna River (a tributary of the Don), 142 kilometers (88 mi) south of Voronezh, the administrative center of the oblast. As of the 2021 Census, its population ...
Voronezh (Russian: Воро́неж, IPA: [vɐˈronʲɪʂ] ⓘ) is a city and the administrative centre of Voronezh Oblast in southwestern Russia straddling the Voronezh River, located 12 kilometers (7.5 mi) from where it flows into the Don River.The city sits on the Southeastern Railway, which connects western Russia with the Urals and Siberia, the Caucasus and Ukraine, and the M4 highway ...
Mark McGovern, Ph.D., is a health economist and associate professor in the Department of Health Behavior, Society, and Policy at the Rutgers School of Public Health. Prior to joining Rutgers, he was an assistant professor at Queen's University Belfast and the Centre of Excellence for Public Health (Northern Ireland). Dr.
Mark Purdue, Ph.D., senior investigator in the Occupational and Environmental Epidemiology Branch (OEEB), has been appointed Branch Director September 2024.Dr. Purdue is an internationally recognized expert in the study of cancer associations with occupational and environmental exposures to chlorinated solvents, per- and polyfluoroalkyl substances (PFAS) and other agents and the etiology of ...
At-Home Executive. sources Educators Guide Function forB rainFutures is a national nonprofit dedicated to improving human outcomes by assessing and advancing the practical applications of new s. ientific understanding of the brain. As a citizen advocacy organization, we enlist specialists to ofer rigorous assessment of—and education about ...
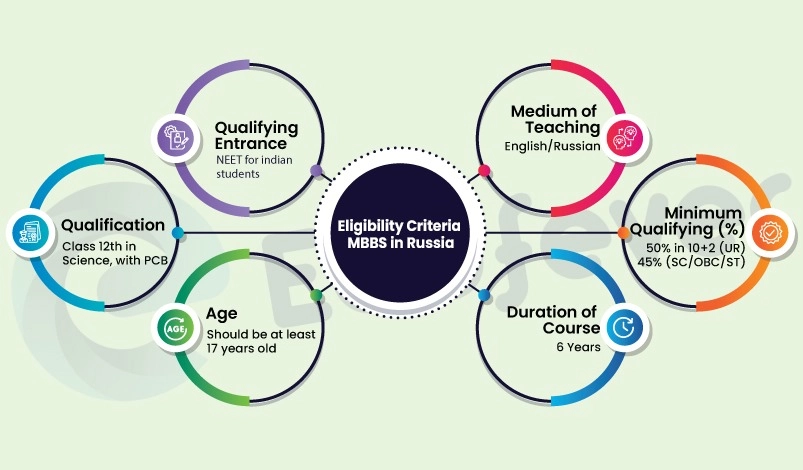
Class 12th in Science, with PCB and English subjects from a board recognized by the authorities in India. Minimum Qualifying (%) 60% in 10+2 (UR) 50% (SC/OBC/ST) Qualifying Entrance. NEET (For Indian Students) Graphical Representation of Eligibility Criteria. Voronezh State Medical University Eligibility Criteria.
Mark Trullinger, MSc, BCN, NeuroThrive William A. Richards, PhD, Johns Hopkins School of Medicine Scott Cousino, George Carpenter IV, MYND Analytics Dror Ben-Zeev, PhD, University of Washington Holistic Life Foundation General Peter W. Chiarelli, US Army (Retired), One Mind BIOGRAPHIES ARE AVAILABLE ONLINE
Voronezh Oblast. Voronezh Oblast is in Russia's Chernozemye region, bordering Ukraine to the southwest, Belgorod Oblast to the west, Kursk Oblast to the northwest, Lipetsk Oblast to the north, Tambov Oblast to the northeast, Ulyanovsk Oblast to the northeast, Volgograd Oblast to the east, and Rostov Oblast to the south. Overview. Map. Directions.