

More teens than ever are overdosing. Psychologists are leading new approaches to combat youth substance misuse
“Just Say No” didn’t work , but experts are employing new holistic programs to help steer kids away—or at least keep them from dying—from illicit substances.
Vol. 55 No. 2 Print version: page 48
- Substance Use, Abuse, and Addiction

For years, students in middle and high schools across the country were urged to “just say no” to drugs and alcohol. But it’s no secret that the Drug Abuse Resistance Education (D.A.R.E.) program, which was typically delivered by police officers who urged total abstinence, didn’t work. A meta-analysis found the program largely ineffective and one study even showed that kids who completed D.A.R.E. were more likely than their peers to take drugs ( Ennett, S. T., et al., American Journal of Public Health , Vol. 84, No. 9, 1994 ; Rosenbaum, D. P., & Hanson, G. S., Journal of Research in Crime and Delinquency , Vol. 35, No. 4, 1998 ).
“We know that the ‘Just Say No’ campaign doesn’t work. It’s based in pure risks, and that doesn’t resonate with teens,” said developmental psychologist Bonnie Halpern-Felsher, PhD, a professor of pediatrics and founder and executive director of several substance use prevention and intervention curriculums at Stanford University. “There are real and perceived benefits to using drugs, as well as risks, such as coping with stress or liking the ‘high.’ If we only talk about the negatives, we lose our credibility.”
Partially because of the lessons learned from D.A.R.E., many communities are taking a different approach to addressing youth substance use. They’re also responding to very real changes in the drug landscape. Aside from vaping, adolescent use of illicit substances has dropped substantially over the past few decades, but more teens are overdosing than ever—largely because of contamination of the drug supply with fentanyl, as well as the availability of stronger substances ( Most reported substance use among adolescents held steady in 2022, National Institute on Drug Abuse ).
“The goal is to impress upon youth that far and away the healthiest choice is not to put these substances in your body, while at the same time acknowledging that some kids are still going to try them,” said Aaron Weiner, PhD, ABPP, a licensed clinical psychologist based in Lake Forest, Illinois, and immediate past-president of APA’s Division 50 (Society of Addiction Psychology). “If that’s the case, we want to help them avoid the worst consequences.”
While that approach, which incorporates principles of harm reduction, is not universally accepted, evidence is growing for its ability to protect youth from accidental overdoses and other consequences of substance use, including addiction, justice involvement, and problems at school. Psychologists have been a key part of the effort to create, test, and administer developmentally appropriate, evidence-based programs that approach prevention in a holistic, nonstigmatizing way.
“Drugs cannot be this taboo thing that young people can’t ask about anymore,” said Nina Christie, PhD, a postdoctoral research fellow in the Center on Alcohol, Substance Use, and Addictions at the University of New Mexico. “That’s just a recipe for young people dying, and we can’t continue to allow that.”
Changes in drug use
In 2022, about 1 in 3 high school seniors, 1 in 5 sophomores, and 1 in 10 eighth graders reported using an illicit substance in the past year, according to the National Institute on Drug Abuse’s (NIDA) annual survey ( Monitoring the Future: National Survey Results on Drug Use, 1975–2022: Secondary School Students , NIDA, 2023 [PDF, 7.78MB] ). Those numbers were down significantly from prepandemic levels and essentially at their lowest point in decades.
Substance use during adolescence is particularly dangerous because psychoactive substances, including nicotine, cannabis, and alcohol, can interfere with healthy brain development ( Winters, K. C., & Arria, A., Prevention Research , Vol. 18, No. 2, 2011 ). Young people who use substances early and frequently also face a higher risk of developing a substance use disorder in adulthood ( McCabe, S. E., et al., JAMA Network Open , Vol. 5, No. 4, 2022 ). Kids who avoid regular substance use are more likely to succeed in school and to avoid problems with the juvenile justice system ( Public policy statement on prevention, American Society of Addiction Medicine, 2023 ).
“The longer we can get kids to go without using substances regularly, the better their chances of having an optimal life trajectory,” Weiner said.
The drugs young people are using—and the way they’re using them—have also changed, and psychologists say this needs to inform educational efforts around substance use. Alcohol and cocaine are less popular than they were in the 1990s; use of cannabis and hallucinogens, which are now more salient and easier to obtain, were higher than ever among young adults in 2021 ( Marijuana and hallucinogen use among young adults reached all-time high in 2021, NIDA ).
“Gen Z is drinking less alcohol than previous generations, but they seem to be increasingly interested in psychedelics and cannabis,” Christie said. “Those substances have kind of replaced alcohol as the cool thing to be doing.”
Young people are also seeing and sharing content about substance use on social media, with a rise in posts and influencers promoting vaping on TikTok and other platforms ( Vassey, J., et al., Nicotine & Tobacco Research , 2023 ). Research suggests that adolescents and young adults who see tobacco or nicotine content on social media are more likely to later start using it ( Donaldson, S. I., et al., JAMA Pediatrics , Vol. 176, No. 9, 2022 ).
A more holistic view
Concern for youth well-being is what drove the well-intentioned, but ultimately ineffective, “mad rush for abstinence,” as Robert Schwebel, PhD, calls it. Though that approach has been unsuccessful in many settings, a large number of communities still employ it, said Schwebel, a clinical psychologist who created the Seven Challenges Program for treating substance use in youth.
But increasingly, those working to prevent and treat youth substance use are taking a different approach—one that aligns with principles Schwebel helped popularize through Seven Challenges.
A key tenet of modern prevention and treatment programs is empowering youth to make their own decisions around substance use in a developmentally appropriate way. Adolescents are exploring their identities (including how they personally relate to drugs), learning how to weigh the consequences of their actions, and preparing for adulthood, which involves making choices about their future. The Seven Challenges Program, for example, uses supportive journaling exercises, combined with counseling, to help young people practice informed decision-making around substance use with those processes in mind.
“You can insist until you’re blue in the face, but that’s not going to make people abstinent. They ultimately have to make their own decisions,” Schwebel said.
Today’s prevention efforts also tend to be more holistic than their predecessors, accounting for the ways drug use relates to other addictive behaviors, such as gaming and gambling, or risky choices, such as fighting, drag racing, and having unprotected sex. Risk factors for substance use—which include trauma, adverse childhood experiences, parental history of substance misuse, and personality factors such as impulsivity and sensation seeking—overlap with many of those behaviors, so it often makes sense to address them collectively.
[ Related: Psychologists are innovating to tackle substance use ]
“We’ve become more sophisticated in understanding the biopsychosocial determinants of alcohol and drug use and moving beyond this idea that it’s a disease and the only solution is medication,” said James Murphy, PhD, a professor of psychology at the University of Memphis who studies addictive behaviors and how to intervene.
Modern prevention programs also acknowledge that young people use substances to serve a purpose—typically either social or emotional in nature—and if adults expect them not to use, they should help teens learn to fulfill those needs in a different way, Weiner said.
“Youth are generally using substances to gain friends, avoid losing them, or to cope with emotional problems that they’re having,” he said. “Effective prevention efforts need to offer healthy alternatives for achieving those goals.”
Just say “know”
At times, the tenets of harm reduction and substance use prevention seem inherently misaligned. Harm reduction, born out of a response to the AIDS crisis, prioritizes bodily autonomy and meeting people where they are without judgment. For some harm reductionists, actively encouraging teens against using drugs could violate the principle of respecting autonomy, Weiner said.
On the other hand, traditional prevention advocates may feel that teaching adolescents how to use fentanyl test strips or encouraging them not to use drugs alone undermines the idea that they can choose not to use substances. But Weiner says both approaches can be part of the solution.
“It doesn’t have to be either prevention or harm reduction, and we lose really important tools when we say it has to be one or the other,” he said.
In adults, harm reduction approaches save lives, prevent disease transmission, and help people connect with substance use treatment ( Harm Reduction, NIDA, 2022 ). Early evidence shows similar interventions can help adolescents improve their knowledge and decision-making around drug use ( Fischer, N. R., Substance Abuse Treatment, Prevention, and Policy , Vol. 17, 2022 ). Teens are enthusiastic about these programs, which experts often call “Just Say Know” to contrast them with the traditional “Just Say No” approach. In one pilot study, 94% of students said a “Just Say Know” program provided helpful information and 92% said it might influence their approach to substance use ( Meredith, L. R., et al., The American Journal of Drug and Alcohol Abuse , Vol. 47, No. 1, 2021 ).
“Obviously, it’s the healthiest thing if we remove substance use from kids’ lives while their brains are developing. At the same time, my preference is that we do something that will have a positive impact on these kids’ health and behaviors,” said Nora Charles, PhD, an associate professor and head of the Youth Substance Use and Risky Behavior Lab at the University of Southern Mississippi. “If the way to do that is to encourage more sensible and careful engagement with illicit substances, that is still better than not addressing the problem.”
One thing not to do is to overly normalize drug use or to imply that it is widespread, Weiner said. Data show that it’s not accurate to say that most teens have used drugs in the past year or that drugs are “just a part of high school life.” In fact, students tend to overestimate how many of their peers use substances ( Dumas, T. M., et al., Addictive Behaviors , Vol. 90, 2019 ; Helms, S. W., et al., Developmental Psychology , Vol. 50, No. 12, 2014 ).
A way to incorporate both harm reduction and traditional prevention is to customize solutions to the needs of various communities. For example, in 2022, five Alabama high school students overdosed on a substance laced with fentanyl, suggesting that harm reduction strategies could save lives in that community. Other schools with less reported substance use might benefit more from a primary prevention-style program.
At Stanford, Halpern-Felsher’s Research and Education to Empower Adolescents and Young Adults to Choose Health (REACH) Lab has developed a series of free, evidence-based programs through community-based participatory research that can help populations with different needs. The REACH Lab offers activity-based prevention, intervention, and cessation programs for elementary, middle, and high school students, including curricula on alcohol, vaping, cannabis, fentanyl, and other drugs ( Current Problems in Pediatric and Adolescent Health Care , Vol. 52, No. 6, 2022 ). They’re also working on custom curricula for high-risk groups, including sexual and gender minorities.
The REACH Lab programs, including the comprehensive Safety First curriculum , incorporate honest discussion about the risks and benefits of using substances. For example: Drugs are one way to cope with stress, but exercise, sleep, and eating well can also help. Because many young people care about the environment, one lesson explores how cannabis and tobacco production causes environmental harm.
The programs also dispel myths about how many adolescents are using substances and help them practice skills, such as how to decline an offer to use drugs in a way that resonates with them. They learn about the developing brain in a positive way—whereas teens were long told they can’t make good decisions, Safety First empowers them to choose to protect their brains and bodies by making healthy choices across the board.
“Teens can make good decisions,” Halpern-Felsher said. “The equation is just different because they care more about certain things—peers, relationships—compared to adults.”
Motivating young people
Because substance use and mental health are so intertwined, some programs can do prevention successfully with very little drug-focused content. In one of the PreVenture Program’s workshops for teens, only half a page in a 35-page workbook explicitly mentions substances.
“That’s what’s fascinating about the evidence base for PreVenture,” said clinical psychologist Patricia Conrod, PhD, a professor of psychiatry at the University of Montreal who developed the program. “You can have quite a dramatic effect on young people’s substance use without even talking about it.”
PreVenture offers a series of 90-minute workshops that apply cognitive behavioral insights upstream (addressing the root causes of a potential issue rather than waiting for symptoms to emerge) to help young people explore their personality traits and develop healthy coping strategies to achieve their long-term goals.
Adolescents high in impulsivity, hopelessness, thrill-seeking, or anxiety sensitivity face higher risks of mental health difficulties and substance use, so the personalized material helps them practice healthy coping based on their personality type. For example, the PreVenture workshop that targets anxiety sensitivity helps young people learn to challenge cognitive distortions that can cause stress, then ties that skill back to their own goals.
The intervention can be customized to the needs of a given community (in one trial, drag racing outstripped substance use as the most problematic thrill-seeking behavior). In several randomized controlled trials of PreVenture, adolescents who completed the program started using substances later than peers who did not receive the intervention and faced fewer alcohol-related harms ( Newton, N. C., et al., JAMA Network Open , Vol. 5, No. 11, 2022 ). The program has also been shown to reduce the likelihood that adolescents will experiment with illicit substances, which relates to the current overdose crisis in North America, Conrod said ( Archives of General Psychiatry , Vol. 67, No. 1, 2010 ).
“People shouldn’t shy away from a targeted approach like this,” Conrod said. “Young people report that having the words and skills to manage their traits is actually helpful, and the research shows that at behavioral level, it really does protect them.”
As young people leave secondary school and enter college or adult life, about 30% will binge drink, 8% will engage in heavy alcohol use, and 20% will use illicit drugs ( Alcohol and Young Adults Ages 18 to 24, National Institute on Alcohol Abuse and Alcoholism, 2023 ; SAMHSA announces national survey on drug use and health (NSDUH) results detailing mental illness and substance use levels in 2021 ). But young people are very unlikely to seek help, even if those activities cause them distress, Murphy said. For that reason, brief interventions that leverage motivational interviewing and can be delivered in a school, work, or medical setting can make a big difference.
In an intervention Murphy and his colleagues are testing, young adults complete a questionnaire about how often they drink or use drugs, how much money they spend on substances, and negative things that have happened as a result of those choices (getting into an argument or having a hangover, for example).
In an hour-long counseling session, they then have a nonjudgmental conversation about their substance use, where the counselor gently amplifies any statements the young person makes about negative outcomes or a desire to change their behavior. Participants also see charts that quantify how much money and time they spend on substances, including recovering from being intoxicated, and how that stacks up against other things they value, such as exercise, family time, and hobbies.
“For many young people, when they look at what they allocate to drinking and drug use, relative to these other things that they view as much more important, it’s often very motivating,” Murphy said.
A meta-analysis of brief alcohol interventions shows that they can reduce the average amount participants drink for at least 6 months ( Mun, E.Y., et al., Prevention Science , Vol. 24, No. 8, 2023 ). Even a small reduction in alcohol use can be life-altering, Murphy said. The fourth or fifth drink on a night out, for example, could be the one that leads to negative consequences—so reducing intake to just three drinks may make a big difference for young people.
Conrod and her colleagues have also adapted the PreVenture Program for university students; they are currently testing its efficacy in a randomized trial across multiple institutions.
Christie is also focused on the young adult population. As a policy intern with Students for Sensible Drug Policy, she created a handbook of evidence-based policies that college campuses can use to reduce harm among students but still remain compliant with federal law. For example, the Drug Free Schools and Communities Act mandates that higher education institutions formally state that illegal drug use is not allowed on campus but does not bar universities from taking an educational or harm reduction-based approach if students violate that policy.
“One low-hanging fruit is for universities to implement a Good Samaritan policy, where students can call for help during a medical emergency and won’t get in trouble, even if illegal substance use is underway,” she said.
Ultimately, taking a step back to keep the larger goals in focus—as well as staying dedicated to prevention and intervention approaches backed by science—is what will help keep young people healthy and safe, Weiner said.
“What everyone can agree on is that we want kids to have the best life they can,” he said. “If we can start there, what tools do we have available to help?”
Further reading
Public Policy Statement on Prevention American Society of Addiction Medicine, 2023
Listen to young people: How to implement harm reduction in the collegiate setting Christie, N. C., 2023
Brief alcohol interventions for young adults: Strengthening effects and disentangling mechanisms to build personalized interventions for widespread uptake Special issue of Psychology of Addictive Behaviors , 2022
Addressing adolescent substance use with a public health prevention framework: The case for harm reduction Winer, J. M., et al., Annals of Medicine , 2022
A breath of knowledge: Overview of current adolescent e-cigarette prevention and cessation programs Liu, J., et al., Current Addiction Reports , 2020
Recommended Reading
Six things psychologists are talking about.
The APA Monitor on Psychology ® sister e-newsletter offers fresh articles on psychology trends, new research, and more.
Welcome! Thank you for subscribing.
Speaking of Psychology
Subscribe to APA’s audio podcast series highlighting some of the most important and relevant psychological research being conducted today.
Subscribe to Speaking of Psychology and download via:

Contact APA
You may also like.
Teenage Drug Abuse in the United States Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Social and health issues that take part during the formation of human identity have negative consequences on the individual’s further development. Thus, teenage drug abuse presents a severe danger to an individual’s health in adulthood. The problem of teenage drug abuse inflicts a threat to the future society and health state of the overall population in the United States. This essay will discuss the core reasons and consequences of teenage drug abuse and propose a possible solution based on the collected information.
There are several reasons for teenage drug abuse in the United States. As teenagers are influenced by high concertation of hormones, some of the core reasons for teenage drug abuse are specific to the age category, implying that those reasons are not connected to adult drug abuse. Moreover, teenagers are more influenced by external factors such as social connections and media. One of the core reasons for teenage drug abuse is the willingness to be accepted and validated in a social circle of individuals who already use drugs. In teenagers’ perception, drugs are often used in media as an attribute of cool characters, so they frequently try to fit in with the cool image, unaware of the consequences of drug use. In addition, current teenagers often experience depression and helplessness from being unable to control their lives or social rejection from excessive social media involvement and resort to drug abuse to feel better.
The consequences of teenage drug abuse include development and widespread poor morals, increased danger from sexual activity-related problems, such as STDs and unplanned pregnancy, dangerous driving, and poor performance in school. Even though some minor consequences of episodic drug abuse could be solved, threats like impaired driving present a significant danger to the population. Development and widespread of poor morals will also negatively affect the development of society as poor morals suggest an increased number of crime commitments among adolescents. With the current issues in the prison system, such as difficulties in offenders’ re-entry into the society, the teenagers’ future will be negatively affected in cases of crime commission.
Despite the complex character of the issues imposed by teenage drug abuse, one primary measure could solve the issue or partially improve the current state. The significant difference between teenage drug abuse and drug abuse among adults is parental participation in teenagers’ lives. Increasing the level of parental awareness on the issue of teenage drug abuse and providing them with necessary information could positively influence the situation. Providing parents with helpful information such as red flags in teenager’s behavior, and current state of drug involvement in the local area/school would help the parents establish connection with the teenager. The connection will provide an opportunity for a dialogue on the topic of drug use and its consequences. Moreover, active parental participation in teenagers’ activities would help prevent other issues, such as dangerous and harmful connections or violent tendencies.
In conclusion, this essay explored the issue of teenage drug abuse in the United States through the aspects of core reasons and consequences. Based on the collected information, teenagers are more subjected to drug abuse due to their social interactions and the high risk of depression tendencies. The increased parental participation in teenagers’ lives is the primary solution to the problem. Parents should express concerns about the child’s social circle and activities outside the home. Increasing parental awareness on the problem and providing opportunities for parent-teenager dialogue on the issue of drug abuse will positively influence the current state of teenage drug abuse in the United States.
- Healthy People 2020 and Tobacco Use
- History and Social Side of Drug Addiction
- Teenage Pregnancy in the Modern World
- Drug and Alcohol Abuse Among Teenagers
- Teenage Suicide: Statistics Data, Reasons and Prevention
- Explaining Drug Use: Social Scientific Theories
- Drug and Substance Addiction
- My Personal Beliefs About People With Addictions
- Alcoholics Anonymous Program Evaluation
- Drug-Related Individual Situation and Treatment Method
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, November 25). Teenage Drug Abuse in the United States. https://ivypanda.com/essays/teenage-drug-abuse-in-the-united-states/
"Teenage Drug Abuse in the United States." IvyPanda , 25 Nov. 2022, ivypanda.com/essays/teenage-drug-abuse-in-the-united-states/.
IvyPanda . (2022) 'Teenage Drug Abuse in the United States'. 25 November.
IvyPanda . 2022. "Teenage Drug Abuse in the United States." November 25, 2022. https://ivypanda.com/essays/teenage-drug-abuse-in-the-united-states/.
1. IvyPanda . "Teenage Drug Abuse in the United States." November 25, 2022. https://ivypanda.com/essays/teenage-drug-abuse-in-the-united-states/.
Bibliography
IvyPanda . "Teenage Drug Abuse in the United States." November 25, 2022. https://ivypanda.com/essays/teenage-drug-abuse-in-the-united-states/.
Appointments at Mayo Clinic
- Tween and teen health
Teen drug abuse: Help your teen avoid drugs
Teen drug abuse can have a major impact on your child's life. Find out how to help your teen make healthy choices and avoid using drugs.
The teen brain is in the process of maturing. In general, it's more focused on rewards and taking risks than the adult brain. At the same time, teenagers push parents for greater freedom as teens begin to explore their personality.
That can be a challenging tightrope for parents.
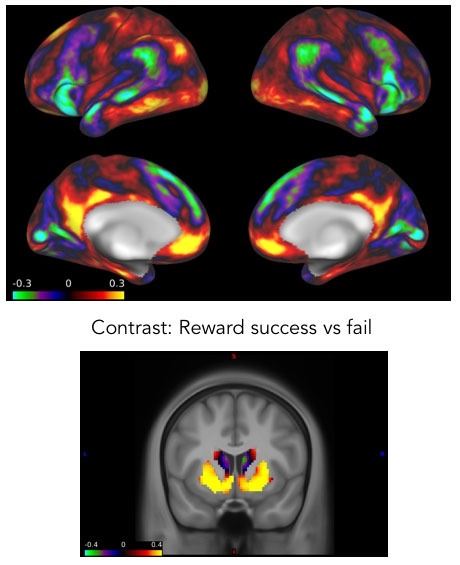
Teens who experiment with drugs and other substances put their health and safety at risk. The teen brain is particularly vulnerable to being rewired by substances that overload the reward circuits in the brain.
Help prevent teen drug abuse by talking to your teen about the consequences of using drugs and the importance of making healthy choices.
Why teens use or misuse drugs
Many factors can feed into teen drug use and misuse. Your teen's personality, your family's interactions and your teen's comfort with peers are some factors linked to teen drug use.
Common risk factors for teen drug abuse include:
- A family history of substance abuse.
- A mental or behavioral health condition, such as depression, anxiety or attention-deficit/hyperactivity disorder (ADHD).
- Impulsive or risk-taking behavior.
- A history of traumatic events, such as seeing or being in a car accident or experiencing abuse.
- Low self-esteem or feelings of social rejection.
Teens may be more likely to try substances for the first time when hanging out in a social setting.
Alcohol and nicotine or tobacco may be some of the first, easier-to-get substances for teens. Because alcohol and nicotine or tobacco are legal for adults, these can seem safer to try even though they aren't safe for teens.
Teens generally want to fit in with peers. So if their friends use substances, your teen might feel like they need to as well. Teens also may also use substances to feel more confident with peers.
If those friends are older, teens can find themselves in situations that are riskier than they're used to. For example, they may not have adults present or younger teens may be relying on peers for transportation.
And if they are lonely or dealing with stress, teens may use substances to distract from these feelings.
Also, teens may try substances because they are curious. They may try a substance as a way to rebel or challenge family rules.
Some teens may feel like nothing bad could happen to them, and may not be able to understand the consequences of their actions.
Consequences of teen drug abuse
Negative consequences of teen drug abuse might include:
- Drug dependence. Some teens who misuse drugs are at increased risk of substance use disorder.
- Poor judgment. Teenage drug use is associated with poor judgment in social and personal interactions.
- Sexual activity. Drug use is associated with high-risk sexual activity, unsafe sex and unplanned pregnancy.
- Mental health disorders. Drug use can complicate or increase the risk of mental health disorders, such as depression and anxiety.
- Impaired driving. Driving under the influence of any drug affects driving skills. It puts the driver, passengers and others on the road at risk.
- Changes in school performance. Substance use can result in worse grades, attendance or experience in school.
Health effects of drugs
Substances that teens may use include those that are legal for adults, such as alcohol or tobacco. They may also use medicines prescribed to other people, such as opioids.
Or teens may order substances online that promise to help in sports competition, or promote weight loss.
In some cases products common in homes and that have certain chemicals are inhaled for intoxication. And teens may also use illicit drugs such as cocaine or methamphetamine.
Drug use can result in drug addiction, serious impairment, illness and death. Health risks of commonly used drugs include the following:
- Cocaine. Risk of heart attack, stroke and seizures.
- Ecstasy. Risk of liver failure and heart failure.
- Inhalants. Risk of damage to the heart, lungs, liver and kidneys from long-term use.
- Marijuana. Risk of impairment in memory, learning, problem-solving and concentration; risk of psychosis, such as schizophrenia, hallucination or paranoia, later in life associated with early and frequent use. For teens who use marijuana and have a psychiatric disorder, there is a risk of depression and a higher risk of suicide.
- Methamphetamine. Risk of psychotic behaviors from long-term use or high doses.
- Opioids. Risk of respiratory distress or death from overdose.
- Electronic cigarettes (vaping). Higher risk of smoking or marijuana use. Exposure to harmful substances similar to cigarette smoking; risk of nicotine dependence. Vaping may allow particles deep into the lungs, or flavorings may include damaging chemicals or heavy metals.
Talking about teen drug use
You'll likely have many talks with your teen about drug and alcohol use. If you are starting a conversation about substance use, choose a place where you and your teen are both comfortable. And choose a time when you're unlikely to be interrupted. That means you both will need to set aside phones.
It's also important to know when not to have a conversation.
When parents are angry or when teens are frustrated, it's best to delay the talk. If you aren't prepared to answer questions, parents might let teens know that you'll talk about the topic at a later time.
And if a teen is intoxicated, wait until the teen is sober.
To talk to your teen about drugs:
- Ask your teen's views. Avoid lectures. Instead, listen to your teen's opinions and questions about drugs. Parents can assure teens that they can be honest and have a discussion without getting in trouble.
- Discuss reasons not to use drugs. Avoid scare tactics. Emphasize how drug use can affect the things that are important to your teen. Some examples might be sports performance, driving, health or appearance.
- Consider media messages. Social media, television programs, movies and songs can make drug use seem normal or glamorous. Talk about what your teen sees and hears.
- Discuss ways to resist peer pressure. Brainstorm with your teen about how to turn down offers of drugs.
- Be ready to discuss your own drug use. Think about how you'll respond if your teen asks about your own drug use, including alcohol. If you chose not to use drugs, explain why. If you did use drugs, share what the experience taught you.
Other preventive strategies
Consider other strategies to prevent teen drug abuse:
- Know your teen's activities. Pay attention to your teen's whereabouts. Find out what adult-supervised activities your teen is interested in and encourage your teen to get involved.
- Establish rules and consequences. Explain your family rules, such as leaving a party where drug use occurs and not riding in a car with a driver who's been using drugs. Work with your teen to figure out a plan to get home safely if the person who drove is using substances. If your teen breaks the rules, consistently enforce consequences.
- Know your teen's friends. If your teen's friends use drugs, your teen might feel pressure to experiment, too.
- Keep track of prescription drugs. Take an inventory of all prescription and over-the-counter medications in your home.
- Provide support. Offer praise and encouragement when your teen succeeds. A strong bond between you and your teen might help prevent your teen from using drugs.
- Set a good example. If you drink, do so in moderation. Use prescription drugs as directed. Don't use illicit drugs.
Recognizing the warning signs of teen drug abuse
Be aware of possible red flags, such as:
- Sudden or extreme change in friends, eating habits, sleeping patterns, physical appearance, requests for money, coordination or school performance.
- Irresponsible behavior, poor judgment and general lack of interest.
- Breaking rules or withdrawing from the family.
- The presence of medicine containers, despite a lack of illness, or drug paraphernalia in your teen's room.
Seeking help for teen drug abuse
If you suspect or know that your teen is experimenting with or misusing drugs:
- Plan your action. Finding out your teen is using drugs or suspecting it can bring up strong emotions. Before talking to your teen, make sure you and anyone who shares caregiving responsibility for the teen is ready. It can help to have a goal for the conversation. It can also help to figure out how you'll respond to the different ways your teen might react.
- Talk to your teen. You can never step in too early. Casual drug use can turn into too much use or addiction. This can lead to accidents, legal trouble and health problems.
- Encourage honesty. Speak calmly and express that you are coming from a place of concern. Share specific details to back up your suspicion. Verify any claims your child makes.
- Focus on the behavior, not the person. Emphasize that drug use is dangerous but that doesn't mean your teen is a bad person.
- Check in regularly. Spend more time with your teen. Know your teen's whereabouts and ask questions about the outing when your teen returns home.
- Get professional help. If you think your teen is involved in drug use, contact a health care provider or counselor for help.
It's never too soon to start talking to your teen about drug abuse. The conversations you have today can help your teen make healthy choices in the future.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Children’s health information and parenting tips to your inbox.
Sign-up to get Mayo Clinic’s trusted health content sent to your email. Receive a bonus guide on ways to manage your child’s health just for subscribing. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing
Our e-newsletter will keep you up-to-date on the latest health information.
Something went wrong with your subscription.
Please try again in a couple of minutes
- Dulcan MK, ed. Substance use disorders and addictions. In: Dulcan's Textbook of Child and Adolescent Psychiatry. 3rd ed. American Psychiatric Association Publishing; 2021. https://psychiatryonline.org. Accessed Jan. 24, 2023.
- 6 parenting practices: Help reduce the chances your child will develop a drug or alcohol problem. Partnership to End Addiction. https://drugfree.org/addiction-education/. Accessed Jan. 24, 2023.
- Why do teens drink and use substances and is it normal? Partnership to End Addiction. https://drugfree.org/article/why-do-teens-drink-and-use-substances/. Accessed Jan. 24, 2023.
- Teens: Alcohol and other drugs. American Academy of Child & Adolescent Psychiatry. https://www.aacap.org/aacap/families_and_youth/facts_for_families/fff-guide/Teens-Alcohol-And-Other-Drugs-003.aspx. Accessed Dec. 27, 2018.
- Drugged driving. National Institute on Drug Abuse. https://www.drugabuse.gov/publications/drugfacts/drugged-driving. Accessed Jan. 24, 2023.
- Marijuana talk kit. Partnership for Drug-Free Kids. https://drugfree.org/drugs/marijuana-what-you-need-to-know/. Accessed Jan. 24, 2023.
- Drug guide for parents: Learn the facts to keep your teen safe. Partnership for Drug-Free Kids. https://www.drugfree.org/resources/. Accessed Dec. 12, 2018.
- Vaping: What you need to know and how to talk with your kids about vaping. Partnership to End Addiction. https://drugfree.org/addiction-education/. Accessed Jan. 24, 2023.
- How to listen. Partnership for Drug-Free Kids. https://www.drugfree.org/resources/. Accessed Dec. 12, 2018.
- Drug abuse prevention starts with parents. American Academy of Pediatrics. https://publications.aap.org/patiented/article/doi/10.1542/peo_document352/81984/Drug-Abuse-Prevention-Starts-With-Parents. Accessed Jan. 24, 2023.
- How to talk to your kids about drugs if you did drugs. Partnership for Drug-Free Kids. https://www.drugfree.org/resources/. Accessed Dec. 12, 2018.
- My child tried drugs, what should I do? Partnership to End Addiction. https://drugfree.org/article/my-child-tried-drugs-what-should-i-do/. Accessed Jan. 24, 2023.
- Gage SH, et al. Association between cannabis and psychosis: Epidemiologic evidence. Biological Psychiatry. 2016;79:549.
- Quick facts on the risks of e-cigarettes for kids, teens and young adults. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/Quick-Facts-on-the-Risks-of-E-cigarettes-for-Kids-Teens-and-Young-Adults.html. Accessed Jan. 30, 2023.
- Distracted Driving
- Piercings: How to prevent complications
- Talking to your teen about sex
- Teen suicide
- Teens and social media use
- Mayo Clinic Minute: Weight loss surgery for kids
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Teen drug abuse Help your teen avoid drugs
Help transform healthcare
Your donation can make a difference in the future of healthcare. Give now to support Mayo Clinic's research.
Home — Essay Samples — Nursing & Health — Substance Abuse — Teenage Drug Abuse In The United States
Teenage Drug Abuse in The United States
- Categories: Drug Addiction Substance Abuse Teenagers
About this sample

Words: 1000 |
Published: Sep 1, 2020
Words: 1000 | Pages: 2 | 5 min read
Table of contents
Introduction, the physiological impact of teenage drug abuse, the psychological toll of teenage drug abuse, societal implications of teenage drug abuse, works cited.
- Center on Addiction. (n.d.). Teen Drug Abuse: Get the Facts. Retrieved from https://www.centeronaddiction.org/addiction-prevention/teenage-addiction/teen-drug-abuse-facts
- Foundation for a Drug-Free World. (n.d.). The Truth About Drugs: Real People, Real Stories.
- Lubman, D. I., & Yücel, M. (2016). Substance use and the adolescent brain: A toxic combination? Journal of Psychopharmacology, 30(2), 118-120.
- National Council on Alcoholism and Drug Dependence. (n.d.). Facts About Alcohol.
- National Institute on Drug Abuse. (2018). Drugs, Brains, and Behavior: The Science of Addiction. Retrieved from https://www.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/drug-use-in-adolescence
- New York Times. (2019). D.A.R.E. Program Teaches the Skills to Say No to Drugs but Not to Use. Retrieved from https://www.nytimes.com/2019/03/25/us/dare-program-lessons.html
- Office of National Drug Control Policy. (2018). Teen Substance Use & Risks.
- Paglia-Boak, A., Adlaf, E. M., & Mann, R. E. (2011). Drug Use Among Ontario Students, 1977–2011: Detailed OSDUHS Findings (CAMH Research Document Series No. 35). Centre for Addiction and Mental Health.
- Slavit, W. I., & Mooney, A. (2017). Adolescent Substance Use. Pediatric Clinics, 64(1), 231-244.
- Yap, M. B. H., Cheong, T. W. K., Zaravinos-Tsakos, F., Lubman, D. I., & Jorm, A. F. (2017). Modifiable parenting factors associated with adolescent alcohol misuse: A systematic review and meta-analysis of longitudinal studies. Addiction, 112(7), 1142-1162.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Prof Ernest (PhD)
Verified writer
- Expert in: Nursing & Health Sociology

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
1 pages / 657 words
2 pages / 1066 words
1 pages / 661 words
1 pages / 435 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Substance Abuse
Substance Abuse and Mental Health Services Administration. (2018). The Importance of Mental Health: Parity for Mental Health and Substance Use.
Drug courts play a pivotal role in the criminal justice system, offering individuals grappling with substance abuse disorders an alternative to incarceration. These programs are structured with distinct phases that participants [...]
The issue of substance abuse presents a pervasive and multifaceted challenge, impacting individuals, families, and communities globally. Its consequences extend far beyond individual suffering, posing significant threats to [...]
Pleasure Unwoven is a documentary film produced by Dr. Kevin McCauley that explores the complex nature of addiction and the underlying neurobiology behind it. The film delves into the concept of pleasure and how it relates to [...]
Motivational interviewing (MI) is a counseling technique which assists the interviewee in identifying the internal motivation to change the client’s behavior by resolving ambivalence and insecurities. The term holds similar [...]
The Beatles’ were no doubt the most influential British band in the 1960’s, with their music bringing and becoming a revolution to the face of rock and roll. Their use of drugs through their music changed the way and the [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free

Essay on Impact of Drugs on Youth
Students are often asked to write an essay on Impact of Drugs on Youth in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Impact of Drugs on Youth
Introduction.
Drugs have a significant impact on youth, affecting their health, education, and social relationships.
Health Consequences
Drugs can damage a young person’s physical and mental health. They can lead to addiction, organ damage, and mental disorders.
Educational Impact
Drugs can impair a youth’s ability to concentrate and learn, leading to poor academic performance.
Social Effects
Drug use can lead to isolation from friends and family, and involvement in illegal activities.
250 Words Essay on Impact of Drugs on Youth
The impact of drugs on youth is a topic of significant concern, affecting individuals, families, and communities worldwide. The youth, being the most vulnerable demographic, are particularly susceptible to the harmful effects of drug use.
The Allure of Drugs
The allure of drugs for young people often stems from a desire to fit in, escape reality, or experiment. Peer pressure, social media influence, and the thrill of rebellion can all contribute to the initiation of drug use. This early exposure can lead to addiction, impacting their physical, mental, and social health.
Physical Impact
Drugs can have devastating physical effects on young bodies. They can hinder growth, affect brain development, and lead to long-term health problems like heart disease and cancer. Moreover, drug use can lead to risky behaviors, increasing the likelihood of accidents, violence, and sexually transmitted diseases.
Mental Impact
On the mental front, drug use can exacerbate or trigger mental health disorders such as depression, anxiety, and psychosis. It can also impair cognitive abilities, memory, and academic performance, limiting a young person’s potential for success.
Social Impact
Socially, drug use can lead to isolation, strained relationships, and a loss of interest in previously enjoyed activities. It can also lead to legal issues, reducing opportunities for future employment and education.
500 Words Essay on Impact of Drugs on Youth
The global landscape of drug abuse and addiction is a complex issue that has significant implications on the youth. The impact of drugs on youth is far-reaching, affecting not just their physical health, but also their mental well-being, academic performance, and future prospects.
The Physical Consequences
The first and most apparent impact of drugs on youth is the physical damage. Substance abuse can lead to a host of health problems, ranging from liver damage, cardiovascular diseases, to neurological issues. Furthermore, drugs can interfere with the normal growth and development processes, particularly during the critical adolescent years when the body undergoes significant changes.
Mental Health Implications
The social implications of drug use among youth are equally significant. Substance abuse can strain relationships with family and friends, leading to isolation and loneliness. It can also lead to delinquency, crime, and a general disregard for societal norms and values. This damage to their social fabric can have long-term consequences, affecting their ability to form meaningful relationships and contribute positively to society.
Educational and Career Impact
Substance abuse can severely impact a young person’s educational attainment and future career prospects. The cognitive impairments caused by drug use can lead to poor academic performance, lower grades, and increased likelihood of dropping out. This, in turn, can limit their career opportunities and earning potential, trapping them in a cycle of poverty and substance abuse.
Prevention and Intervention
In conclusion, the impact of drugs on youth is a multifaceted issue that extends beyond the individual to families, schools, and communities. It is a pressing problem that requires collective effort and commitment to address. By understanding the depth of its impact, we can better equip ourselves to combat this issue and pave the way for a healthier, more productive future for our youth.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
Happy studying!
please help me with problems faced by drugs addicted people essay note
Leave a Reply Cancel reply

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Drugs, Brains, and Behavior: The Science of Addiction Preventing Drug Misuse and Addiction: The Best Strategy
Why is adolescence a critical time for preventing drug addiction.
As noted previously, early use of drugs increases a person's chances of becoming addicted. Remember, drugs change the brain—and this can lead to addiction and other serious problems. So, preventing early use of drugs or alcohol may go a long way in reducing these risks.
Risk of drug use increases greatly during times of transition. For an adult, a divorce or loss of a job may increase the risk of drug use. For a teenager, risky times include moving, family divorce, or changing schools. 35 When children advance from elementary through middle school, they face new and challenging social, family, and academic situations. Often during this period, children are exposed to substances such as cigarettes and alcohol for the first time. When they enter high school, teens may encounter greater availability of drugs, drug use by older teens, and social activities where drugs are used. When individuals leave high school and live more independently, either in college or as an employed adult, they may find themselves exposed to drug use while separated from the protective structure provided by family and school.
A certain amount of risk-taking is a normal part of adolescent development. The desire to try new things and become more independent is healthy, but it may also increase teens’ tendencies to experiment with drugs. The parts of the brain that control judgment and decision-making do not fully develop until people are in their early or mid-20s. This limits a teen’s ability to accurately assess the risks of drug experimentation and makes young people more vulnerable to peer pressure. 36
Because the brain is still developing, using drugs at this age has more potential to disrupt brain function in areas critical to motivation, memory, learning, judgment, and behavior control. 12
Can research-based programs prevent drug addiction in youth?
Yes. The term research-based or evidence-based means that these programs have been designed based on current scientific evidence, thoroughly tested, and shown to produce positive results. Scientists have developed a broad range of programs that positively alter the balance between risk and protective factors for drug use in families, schools, and communities. Studies have shown that research-based programs, such as described in NIDA’s Principles of Substance Abuse Prevention for Early Childhood: A Research-Based Guide and Preventing Drug Use among Children and Adolescents: A Research-Based Guide for Parents, Educators, and Community Leaders , can significantly reduce early use of tobacco, alcohol, and other drugs. 37 Also, while many social and cultural factors affect drug use trends, when young people perceive drug use as harmful, they often reduce their level of use. 38
How do research-based prevention programs work?
These prevention programs work to boost protective factors and eliminate or reduce risk factors for drug use. The programs are designed for various ages and can be used in individual or group settings, such as the school and home. There are three types of programs:
- Universal programs address risk and protective factors common to all children in a given setting, such as a school or community.
- Selective programs are for groups of children and teens who have specific factors that put them at increased risk of drug use.
- Indicated programs are designed for youth who have already started using drugs.
Young Brains Under Study
Using cutting-edge imaging technology, scientists from the NIDA’s Adolescent Brain Cognitive Development (ABCD) Study will look at how childhood experiences, including use of any drugs, interact with each other and with a child’s changing biology to affect brain development and social, behavioral, academic, health, and other outcomes. As the only study of its kind, the ABCD study will yield critical insights into the foundational aspects of adolescence that shape a person’s future.
Economics of Prevention
Evidence-based interventions for substance use can save society money in medical costs and help individuals remain productive members of society. Such programs can return anywhere from very little to $65 per every dollar invested in prevention. 39
Adolescent Drug Abuse
According to Nawi et al. (2021), in 2016, 5.6% of the world’s population of age range fifteen to sixty-five at least utilized drugs. Drugs are supplements for good health if used in reasonable quantities while following qualified doctors’ guidelines. However, there are instances that drug use is bizarre. The bizarre drug use is known as drug abuse and is high among younger generations (Nawi et al., 2021). The effects of drug abuse are threats to socio-economic and collective development. Therefore, it is paramount to identify the cause-root of drug abuse, especially among teenage, to curb such a health problem. Consequently, various literature has been developed to postulate the risk factors leading to teenagers’ drug abuse. Several risk factors are identified across a spectrum of literature; some risk factors overlap. According to Centers for Disease Control and Prevention (2022), the risk factors for drug abuse by adolescents can be effectively managed by prioritizing the most prevalent risk factors as follows: substance abuse history in the family, parental view of the behavior is standard, poor parental guidelines, parent (s) abusing drugs, and absence of support towards teenager gender identity, or sexual orientation.
Drug abuse is a health issue that eminent itself in a person after exposure to various stimuli. In my opinion and from lived experience, I believe drug abuse among youths is triggered by the environment (availability of drugs and peers) and parental neglect. Through such keen observations, I have realized that in my neighborhood, the number of individuals with retarded growth or multiple symptoms of drug abuse is decreasing, especially among youths. The cause of the reduction could be strict government policies, increased social security benefits to needy families, and the use of evidence-based policing in curbing illicit drug businesses. As a child, drug corners and stores were easy to locate, but as I grew, drug outlets were decreasing in number, reducing the availability of drugs to youths. Generally, I have identified trends in the decrease in teenage drug abuse. Through research, I could extract statistical data from two sources that, on analysis, prove my observation to be valid. Statistical data from SAMHSA (2014) indicates that the rate of drug use prevalence among youths in the age bracket of twelve to seventeen was 8.8%. However, recent statistics show that the prevalence is 8.33% (NCDAS, 2023). The two sets of data show that there has been a reduction in drug use prevalence among teenagers in the past decade, concurring with my lived experience.
Nevertheless, drug abuse is still a health issue that needs sound policies, social practices, and strategies to be controlled. Drug abuse is rampant, but the degree varies with drug type. The major contributor to a drug being frequently abused is its ease of acquisition. Therefore, drugs that can easily be acquired, such as illicit drugs, are frequently abused. Considerately, I rank Cocaine and Marijuana as the illicit drugs that are being abused. Prescribed drugs are less abused as their circulations are significantly controlled by the government and medical practitioners.
The fight against drugs will have a positive outcome if the strategies employed are proactive. Prevention mechanisms are of utmost importance in this scenario because drug abuse is accompanied by addictive nature, making it an uphill and resourceful undertaking to cure. As youths’ active hours are primarily spent in schools, prevention measures or programs must be school-based. Therefore, preventing teenage drug abuse includes implementing school-based programs such as Fast Track (RHIhub, 2020), targeted programs, and universal programs (National Crime Prevention Centre, 2022).
Fast Track is an evidence-based approach directed towards children enrolling in kindergarten to protect them from indulging in drug abuse activities through grade ten. The program incorporates various interventions as the child grows through the grades. The major interventions associated with the program are child tutoring, teacher-led sessions, home visits, and parent training groups. The program concept has been used in a particular scenario leading to positive results. Evidence shows that the program reduced the development of substance abuse disorders among youths, binge drinking, and alcohol consumption (RHIhub, 2020).
The targeted program comprises the Schools Using Coordinated Community Efforts to Strengthen Students project and Project Toward No Drug Abuse (TND). Targeted programs are considerately designed for specific youth groups, for instance, youth at high risk of indulging in drug abuse activities or of a particular age range. The programs offer varied interventions, ranging from parent programs, prevention education series, social skill training, and role-playing exercises. Both the programs under the targeted program have been tested to be efficient. For instance, the TND program proved to facilitate a reduction in alcohol use and hard drug use among teenagers (National Crime Prevention Centre, 2022).
Universal programs consist of two categorical programs. The two programs are Project ALERT and project life skills training. About Project ALERT, it is a drug abuse prevention mechanism that is popular among middle-class schools. The program focuses on high-risk youths and curbing three drugs (alcohol, marijuana, and cigarettes) abused. The intervention scheme of the program workout in eleven classroom sessions with three subsequent booster sessions in the following year. The program intervention scheme is designed to aid students in drug abuse awareness and enable them to create sound emotional and social decisions to overcome peer pressure on drug abuse. Generally, the program aims to impart students with the strength of knowledge in resistance behavior to withstand any pressures of drug abuse temptations. Project ALERT program has proven successful in ensuring youths are not engaging in risky drinking. Evidence shows that projects ALERT students’ alcohol consumption reduced by twenty-four percent after an 18-month evaluation (National Crime Prevention Centre, 2022).
Teenagers are a fragile population as they are more impulsive, and any treatment that is not suitable will facilitate their antisocial behavior instead of curing them. Therefore, any means to treat a teenager should consider that they are still developing and can adequately change. Thus, I would propose treatment interventions such as medical therapies and subjection to the criminal justice system. Therapies are the most benign mechanisms in treating a drug abuse effect such as SUD development in youths in that youths have the mental characteristics to continue learning and unlearn the unwanted knowledge through gaining an insight into reality. Therefore, I highly recommend cognitive-behavioral therapy as the primary treatment approach to drug abuse effects in youth. I would recommend subjecting the youth drug abuser to the criminal justice system. Juvenile jails, in most cases, are fitted with rehabs. When a child is exposed to difficulty and solitude plus rehab services, there is evidence that they constantly reshape their behavior more than those who have not been subjected to juvenile rehab. The primary reason I would prefer the approaches in treating juveniles is that both tend to redefine the youth victims’ lives and expose them to a transformation path in the most salient way.
Rural Health Information Hub. (2020). Prevention Programs for Youth and Families. https://www.ruralhealthinfo.org/toolkits/substance-abuse/2/prevention/youth-and-families
National Crime Prevention Centre (Canada). (2022). School-based drug abuse prevention: promising and successful programs . Her Majesty the Queen in Right of Canada. https://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/sclbsd-drgbs/index-en.aspx
Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. (September 4, 2014). The NSDUH Report: Substance Use and Mental Health Estimates from the 2013 National Survey on Drug Use and Health: Overview of Findings . Rockville, MD. https://www.samhsa.gov/data/sites/default/files/NSDUH-SR200-RecoveryMonth-2014/NSDUH-SR200-RecoveryMonth-2014.htm
National Center for Drug Abuse Statistics (NCDAS). (2023). Drug Use Among Youth: Facts & Statistics. https://drugabusestatistics.org/teen-drug-use/
Nawi, A. M., Ismail, R., Ibrahim, F., Hassan, M. R., Manaf, M. R. A., Amit, N., … & Shafurdin, N. S. (2021). Risk and protective factors of drug abuse among adolescents: a systematic review. BMC public health , 21 (1), 1–15.
Centres for Disease Control and Prevention (CDC). (2022). High-Risk Substance Use Among Youth. U.S. Department of Health & Human Services . https://www.cdc.gov/healthyyouth/substance-use/index.htm#:~:text=Risk%20Factors%20for%20High%2DRisk%20Substance%20Use&text=Poor%20parental%20monitoring,delinquent%20or%20substance%20using%20peers
Cite This Work
To export a reference to this article please select a referencing style below:
Related Essays
Black women’s club movement, early childhood education program review, marginalized group career counseling, the first stages of self-expression, abusive wilderness therapy: a violation of human rights, reducing gambling addiction in australia, popular essay topics.
- American Dream
- Artificial Intelligence
- Black Lives Matter
- Bullying Essay
- Career Goals Essay
- Causes of the Civil War
- Child Abusing
- Civil Rights Movement
- Community Service
- Cultural Identity
- Cyber Bullying
- Death Penalty
- Depression Essay
- Domestic Violence
- Freedom of Speech
- Global Warming
- Gun Control
- Human Trafficking
- I Believe Essay
- Immigration
- Importance of Education
- Israel and Palestine Conflict
- Leadership Essay
- Legalizing Marijuanas
- Mental Health
- National Honor Society
- Police Brutality
- Pollution Essay
- Racism Essay
- Romeo and Juliet
- Same Sex Marriages
- Social Media
- The Great Gatsby
- The Yellow Wallpaper
- Time Management
- To Kill a Mockingbird
- Violent Video Games
- What Makes You Unique
- Why I Want to Be a Nurse
- Send us an e-mail
- Open access
- Published: 13 November 2021
Risk and protective factors of drug abuse among adolescents: a systematic review
- Azmawati Mohammed Nawi 1 ,
- Rozmi Ismail 2 ,
- Fauziah Ibrahim 2 ,
- Mohd Rohaizat Hassan 1 ,
- Mohd Rizal Abdul Manaf 1 ,
- Noh Amit 3 ,
- Norhayati Ibrahim 3 &
- Nurul Shafini Shafurdin 2
BMC Public Health volume 21 , Article number: 2088 ( 2021 ) Cite this article
147k Accesses
111 Citations
20 Altmetric
Metrics details
Drug abuse is detrimental, and excessive drug usage is a worldwide problem. Drug usage typically begins during adolescence. Factors for drug abuse include a variety of protective and risk factors. Hence, this systematic review aimed to determine the risk and protective factors of drug abuse among adolescents worldwide.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was adopted for the review which utilized three main journal databases, namely PubMed, EBSCOhost, and Web of Science. Tobacco addiction and alcohol abuse were excluded in this review. Retrieved citations were screened, and the data were extracted based on strict inclusion and exclusion criteria. Inclusion criteria include the article being full text, published from the year 2016 until 2020 and provided via open access resource or subscribed to by the institution. Quality assessment was done using Mixed Methods Appraisal Tools (MMAT) version 2018 to assess the methodological quality of the included studies. Given the heterogeneity of the included studies, a descriptive synthesis of the included studies was undertaken.
Out of 425 articles identified, 22 quantitative articles and one qualitative article were included in the final review. Both the risk and protective factors obtained were categorized into three main domains: individual, family, and community factors. The individual risk factors identified were traits of high impulsivity; rebelliousness; emotional regulation impairment, low religious, pain catastrophic, homework completeness, total screen time and alexithymia; the experience of maltreatment or a negative upbringing; having psychiatric disorders such as conduct problems and major depressive disorder; previous e-cigarette exposure; behavioral addiction; low-perceived risk; high-perceived drug accessibility; and high-attitude to use synthetic drugs. The familial risk factors were prenatal maternal smoking; poor maternal psychological control; low parental education; negligence; poor supervision; uncontrolled pocket money; and the presence of substance-using family members. One community risk factor reported was having peers who abuse drugs. The protective factors determined were individual traits of optimism; a high level of mindfulness; having social phobia; having strong beliefs against substance abuse; the desire to maintain one’s health; high paternal awareness of drug abuse; school connectedness; structured activity and having strong religious beliefs.
The outcomes of this review suggest a complex interaction between a multitude of factors influencing adolescent drug abuse. Therefore, successful adolescent drug abuse prevention programs will require extensive work at all levels of domains.
Peer Review reports
Introduction
Drug abuse is a global problem; 5.6% of the global population aged 15–64 years used drugs at least once during 2016 [ 1 ]. The usage of drugs among younger people has been shown to be higher than that among older people for most drugs. Drug abuse is also on the rise in many ASEAN (Association of Southeast Asian Nations) countries, especially among young males between 15 and 30 years of age. The increased burden due to drug abuse among adolescents and young adults was shown by the Global Burden of Disease (GBD) study in 2013 [ 2 ]. About 14% of the total health burden in young men is caused by alcohol and drug abuse. Younger people are also more likely to die from substance use disorders [ 3 ], and cannabis is the drug of choice among such users [ 4 ].
Adolescents are the group of people most prone to addiction [ 5 ]. The critical age of initiation of drug use begins during the adolescent period, and the maximum usage of drugs occurs among young people aged 18–25 years old [ 1 ]. During this period, adolescents have a strong inclination toward experimentation, curiosity, susceptibility to peer pressure, rebellion against authority, and poor self-worth, which makes such individuals vulnerable to drug abuse [ 2 ]. During adolescence, the basic development process generally involves changing relations between the individual and the multiple levels of the context within which the young person is accustomed. Variation in the substance and timing of these relations promotes diversity in adolescence and represents sources of risk or protective factors across this life period [ 6 ]. All these factors are crucial to helping young people develop their full potential and attain the best health in the transition to adulthood. Abusing drugs impairs the successful transition to adulthood by impairing the development of critical thinking and the learning of crucial cognitive skills [ 7 ]. Adolescents who abuse drugs are also reported to have higher rates of physical and mental illness and reduced overall health and well-being [ 8 ].
The absence of protective factors and the presence of risk factors predispose adolescents to drug abuse. Some of the risk factors are the presence of early mental and behavioral health problems, peer pressure, poorly equipped schools, poverty, poor parental supervision and relationships, a poor family structure, a lack of opportunities, isolation, gender, and accessibility to drugs [ 9 ]. The protective factors include high self-esteem, religiosity, grit, peer factors, self-control, parental monitoring, academic competence, anti-drug use policies, and strong neighborhood attachment [ 10 , 11 , 12 , 13 , 14 , 15 ].
The majority of previous systematic reviews done worldwide on drug usage focused on the mental, psychological, or social consequences of substance abuse [ 16 , 17 , 18 ], while some focused only on risk and protective factors for the non-medical use of prescription drugs among youths [ 19 ]. A few studies focused only on the risk factors of single drug usage among adolescents [ 20 ]. Therefore, the development of the current systematic review is based on the main research question: What is the current risk and protective factors among adolescent on the involvement with drug abuse? To the best of our knowledge, there is limited evidence from systematic reviews that explores the risk and protective factors among the adolescent population involved in drug abuse. Especially among developing countries, such as those in South East Asia, such research on the risk and protective factors for drug abuse is scarce. Furthermore, this review will shed light on the recent trends of risk and protective factors and provide insight into the main focus factors for prevention and control activities program. Additionally, this review will provide information on how these risk and protective factors change throughout various developmental stages. Therefore, the objective of this systematic review was to determine the risk and protective factors of drug abuse among adolescents worldwide. This paper thus fills in the gaps of previous studies and adds to the existing body of knowledge. In addition, this review may benefit certain parties in developing countries like Malaysia, where the national response to drugs is developing in terms of harm reduction, prison sentences, drug treatments, law enforcement responses, and civil society participation.
This systematic review was conducted using three databases, PubMed, EBSCOhost, and Web of Science, considering the easy access and wide coverage of reliable journals, focusing on the risk and protective factors of drug abuse among adolescents from 2016 until December 2020. The search was limited to the last 5 years to focus only on the most recent findings related to risk and protective factors. The search strategy employed was performed in accordance with the Preferred Reporting Items for a Systematic Review and Meta-analysis (PRISMA) checklist.
A preliminary search was conducted to identify appropriate keywords and determine whether this review was feasible. Subsequently, the related keywords were searched using online thesauruses, online dictionaries, and online encyclopedias. These keywords were verified and validated by an academic professor at the National University of Malaysia. The keywords used as shown in Table 1 .
Selection criteria
The systematic review process for searching the articles was carried out via the steps shown in Fig. 1 . Firstly, screening was done to remove duplicate articles from the selected search engines. A total of 240 articles were removed in this stage. Titles and abstracts were screened based on the relevancy of the titles to the inclusion and exclusion criteria and the objectives. The inclusion criteria were full text original articles, open access articles or articles subscribed to by the institution, observation and intervention study design and English language articles. The exclusion criteria in this search were (a) case study articles, (b) systematic and narrative review paper articles, (c) non-adolescent-based analyses, (d) non-English articles, and (e) articles focusing on smoking (nicotine) and alcohol-related issues only. A total of 130 articles were excluded after title and abstract screening, leaving 55 articles to be assessed for eligibility. The full text of each article was obtained, and each full article was checked thoroughly to determine if it would fulfil the inclusion criteria and objectives of this study. Each of the authors compared their list of potentially relevant articles and discussed their selections until a final agreement was obtained. A total of 22 articles were accepted to be included in this review. Most of the excluded articles were excluded because the population was not of the target age range—i.e., featuring subjects with an age > 18 years, a cohort born in 1965–1975, or undergraduate college students; the subject matter was not related to the study objective—i.e., assessing the effects on premature mortality, violent behavior, psychiatric illness, individual traits, and personality; type of article such as narrative review and neuropsychiatry review; and because of our inability to obtain the full article—e.g., forthcoming work in 2021. One qualitative article was added to explain the domain related to risk and the protective factors among the adolescents.
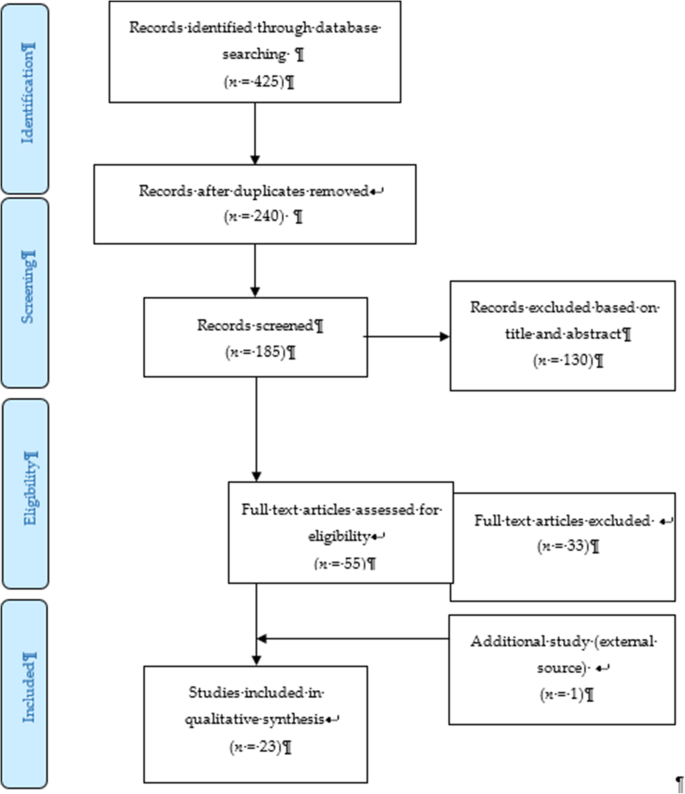
PRISMA flow diagram showing the selection of studies on risk and protective factors for drug abuse among adolescents.2.2. Operational Definition
Drug-related substances in this context refer to narcotics, opioids, psychoactive substances, amphetamines, cannabis, ecstasy, heroin, cocaine, hallucinogens, depressants, and stimulants. Drugs of abuse can be either off-label drugs or drugs that are medically prescribed. The two most commonly abused substances not included in this review are nicotine (tobacco) and alcohol. Accordingly, e-cigarettes and nicotine vape were also not included. Further, “adolescence” in this study refers to members of the population aged between 10 to 18 years [ 21 ].
Data extraction tool
All researchers independently extracted information for each article into an Excel spreadsheet. The data were then customized based on their (a) number; (b) year; (c) author and country; (d) titles; (e) study design; (f) type of substance abuse; (g) results—risks and protective factors; and (h) conclusions. A second reviewer crossed-checked the articles assigned to them and provided comments in the table.
Quality assessment tool
By using the Mixed Method Assessment Tool (MMAT version 2018), all articles were critically appraised for their quality by two independent reviewers. This tool has been shown to be useful in systematic reviews encompassing different study designs [ 22 ]. Articles were only selected if both reviewers agreed upon the articles’ quality. Any disagreement between the assigned reviewers was managed by employing a third independent reviewer. All included studies received a rating of “yes” for the questions in the respective domains of the MMAT checklists. Therefore, none of the articles were removed from this review due to poor quality. The Cohen’s kappa (agreement) between the two reviewers was 0.77, indicating moderate agreement [ 23 ].
The initial search found 425 studies for review, but after removing duplicates and applying the criteria listed above, we narrowed the pool to 22 articles, all of which are quantitative in their study design. The studies include three prospective cohort studies [ 24 , 25 , 26 ], one community trial [ 27 ], one case-control study [ 28 ], and nine cross-sectional studies [ 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ]. After careful discussion, all reviewer panels agreed to add one qualitative study [ 46 ] to help provide reasoning for the quantitative results. The selected qualitative paper was chosen because it discussed almost all domains on the risk and protective factors found in this review.
A summary of all 23 articles is listed in Table 2 . A majority of the studies (13 articles) were from the United States of America (USA) [ 25 , 26 , 27 , 29 , 30 , 31 , 34 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ], three studies were from the Asia region [ 32 , 33 , 38 ], four studies were from Europe [ 24 , 28 , 40 , 44 ], and one study was from Latin America [ 35 ], Africa [ 43 ] and Mediterranean [ 45 ]. The number of sample participants varied widely between the studies, ranging from 70 samples (minimum) to 700,178 samples (maximum), while the qualitative paper utilized a total of 100 interviewees. There were a wide range of drugs assessed in the quantitative articles, with marijuana being mentioned in 11 studies, cannabis in five studies, and opioid (six studies). There was also large heterogeneity in terms of the study design, type of drug abused, measurements of outcomes, and analysis techniques used. Therefore, the data were presented descriptively.
After thorough discussion and evaluation, all the findings (both risk and protective factors) from the review were categorized into three main domains: individual factors, family factors, and community factors. The conceptual framework is summarized in Fig. 2 .
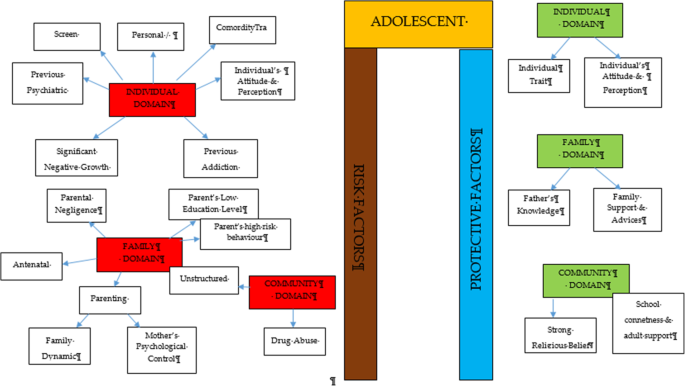
Conceptual framework of risk and protective factors related to adolescent drug abuse
DOMAIN: individual factor
Risk factors.
Almost all the articles highlighted significant findings of individual risk factors for adolescent drug abuse. Therefore, our findings for this domain were further broken down into five more sub-domains consisting of personal/individual traits, significant negative growth exposure, personal psychiatric diagnosis, previous substance history, comorbidity and an individual’s attitude and perception.
Personal/individual traits
Chuang et al. [ 29 ] found that adolescents with high impulsivity traits had a significant positive association with drug addiction. This study also showed that the impulsivity trait alone was an independent risk factor that increased the odds between two to four times for using any drug compared to the non-impulsive group. Another longitudinal study by Guttmannova et al. showed that rebellious traits are positively associated with marijuana drug abuse [ 27 ]. The authors argued that measures of rebelliousness are a good proxy for a youth’s propensity to engage in risky behavior. Nevertheless, Wilson et al. [ 37 ], in a study involving 112 youths undergoing detoxification treatment for opioid abuse, found that a majority of the affected respondents had difficulty in regulating their emotions. The authors found that those with emotional regulation impairment traits became opioid dependent at an earlier age. Apart from that, a case-control study among outpatient youths found that adolescents involved in cannabis abuse had significant alexithymia traits compared to the control population [ 28 ]. Those adolescents scored high in the dimension of Difficulty in Identifying Emotion (DIF), which is one of the key definitions of diagnosing alexithymia. Overall, the adjusted Odds Ratio for DIF in cannabis abuse was 1.11 (95% CI, 1.03–1.20).
Significant negative growth exposure
A history of maltreatment in the past was also shown to have a positive association with adolescent drug abuse. A study found that a history of physical abuse in the past is associated with adolescent drug abuse through a Path Analysis, despite evidence being limited to the female gender [ 25 ]. However, evidence from another study focusing at foster care concluded that any type of maltreatment might result in a prevalence as high as 85.7% for the lifetime use of cannabis and as high as 31.7% for the prevalence of cannabis use within the last 3-months [ 30 ]. The study also found significant latent variables that accounted for drug abuse outcomes, which were chronic physical maltreatment (factor loading of 0.858) and chronic psychological maltreatment (factor loading of 0.825), with an r 2 of 73.6 and 68.1%, respectively. Another study shed light on those living in child welfare service (CWS) [ 35 ]. It was observed through longitudinal measurements that proportions of marijuana usage increased from 9 to 18% after 36 months in CWS. Hence, there is evidence of the possibility of a negative upbringing at such shelters.
Personal psychiatric diagnosis
The robust studies conducted in the USA have deduced that adolescents diagnosed with a conduct problem (CP) have a positive association with marijuana abuse (OR = 1.75 [1.56, 1.96], p < 0.0001). Furthermore, those with a diagnosis of Major Depressive Disorder (MDD) showed a significant positive association with marijuana abuse.
Previous substance and addiction history
Another study found that exposure to e-cigarettes within the past 30 days is related to an increase in the prevalence of marijuana use and prescription drug use by at least four times in the 8th and 10th grades and by at least three times in the 12th grade [ 34 ]. An association between other behavioral addictions and the development of drug abuse was also studied [ 29 ]. Using a 12-item index to assess potential addictive behaviors [ 39 ], significant associations between drug abuse and the groups with two behavioral addictions (OR = 3.19, 95% CI 1.25,9.77) and three behavioral addictions (OR = 3.46, 95% CI 1.25,9.58) were reported.
Comorbidity
The paper by Dash et al. (2020) highlight adolescent with a disease who needs routine medical pain treatment have higher risk of opioid misuse [ 38 ]. The adolescents who have disorder symptoms may have a risk for opioid misuse despite for the pain intensity.
Individual’s attitudes and perceptions
In a study conducted in three Latin America countries (Argentina, Chile, and Uruguay), it was shown that adolescents with low or no perceived risk of taking marijuana had a higher risk of abuse (OR = 8.22 times, 95% CI 7.56, 10.30) [ 35 ]. This finding is in line with another study that investigated 2002 adolescents and concluded that perceiving the drug as harmless was an independent risk factor that could prospectively predict future marijuana abuse [ 27 ]. Moreover, some youth interviewed perceived that they gained benefits from substance use [ 38 ]. The focus group discussion summarized that the youth felt positive personal motivation and could escape from a negative state by taking drugs. Apart from that, adolescents who had high-perceived availability of drugs in their neighborhoods were more likely to increase their usage of marijuana over time (OR = 11.00, 95% CI 9.11, 13.27) [ 35 ]. A cheap price of the substance and the availability of drug dealers around schools were factors for youth accessibility [ 38 ]. Perceived drug accessibility has also been linked with the authorities’ enforcement programs. The youth perception of a lax community enforcement of laws regarding drug use at all-time points predicted an increase in marijuana use in the subsequent assessment period [ 27 ]. Besides perception, a study examining the attitudes towards synthetic drugs based on 8076 probabilistic samples of Macau students found that the odds of the lifetime use of marijuana was almost three times higher among those with a strong attitude towards the use of synthetic drugs [ 32 ]. In addition, total screen time among the adolescent increase the likelihood of frequent cannabis use. Those who reported daily cannabis use have a mean of 12.56 h of total screen time, compared to a mean of 6.93 h among those who reported no cannabis use. Adolescent with more time on internet use, messaging, playing video games and watching TV/movies were significantly associated with more frequent cannabis use [ 44 ].

Protective factors
Individual traits.
Some individual traits have been determined to protect adolescents from developing drug abuse habits. A study by Marin et al. found that youth with an optimistic trait were less likely to become drug dependent [ 33 ]. In this study involving 1104 Iranian students, it was concluded that a higher optimism score (measured using the Children Attributional Style Questionnaire, CASQ) was a protective factor against illicit drug use (OR = 0.90, 95% CI: 0.85–0.95). Another study found that high levels of mindfulness, measured using the 25-item Child Acceptance and Mindfulness Measure, CAMM, lead to a slower progression toward injectable drug abuse among youth with opioid addiction (1.67 years, p = .041) [ 37 ]. In addition, the social phobia trait was found to have a negative association with marijuana use (OR = 0.87, 95% CI 0.77–0.97), as suggested [ 31 ].
According to El Kazdouh et al., individuals with a strong belief against substance use and those with a strong desire to maintain their health were more likely to be protected from involvement in drug abuse [ 46 ].
DOMAIN: family factors
The biological factors underlying drug abuse in adolescents have been reported in several studies. Epigenetic studies are considered important, as they can provide a good outline of the potential pre-natal factors that can be targeted at an earlier stage. Expecting mothers who smoke tobacco and alcohol have an indirect link with adolescent substance abuse in later life [ 24 , 39 ]. Moreover, the dynamic relationship between parents and their children may have some profound effects on the child’s growth. Luk et al. examined the mediator effects between parenting style and substance abuse and found the maternal psychological control dimension to be a significant variable [ 26 ]. The mother’s psychological control was two times higher in influencing her children to be involved in substance abuse compared to the other dimension. Conversely, an indirect risk factor towards youth drug abuse was elaborated in a study in which low parental educational level predicted a greater risk of future drug abuse by reducing the youth’s perception of harm [ 27 , 43 ]. Negligence from a parental perspective could also contribute to this problem. According to El Kazdouh et al. [ 46 ], a lack of parental supervision, uncontrolled pocket money spending among children, and the presence of substance-using family members were the most common negligence factors.
While the maternal factors above were shown to be risk factors, the opposite effect was seen when the paternal figure equipped himself with sufficient knowledge. A study found that fathers with good information and awareness were more likely to protect their adolescent children from drug abuse [ 26 ]. El Kazdouh et al. noted that support and advice could be some of the protective factors in this area [ 46 ].
DOMAIN: community factors
- Risk factor
A study in 2017 showed a positive association between adolescent drug abuse and peers who abuse drugs [ 32 , 39 ]. It was estimated that the odds of becoming a lifetime marijuana user was significantly increased by a factor of 2.5 ( p < 0.001) among peer groups who were taking synthetic drugs. This factor served as peer pressure for youth, who subconsciously had desire to be like the others [ 38 ]. The impact of availability and engagement in structured and unstructured activities also play a role in marijuana use. The findings from Spillane (2000) found that the availability of unstructured activities was associated with increased likelihood of marijuana use [ 42 ].
- Protective factor
Strong religious beliefs integrated into society serve as a crucial protective factor that can prevent adolescents from engaging in drug abuse [ 38 , 45 ]. In addition, the school connectedness and adult support also play a major contribution in the drug use [ 40 ].
The goal of this review was to identify and classify the risks and protective factors that lead adolescents to drug abuse across the three important domains of the individual, family, and community. No findings conflicted with each other, as each of them had their own arguments and justifications. The findings from our review showed that individual factors were the most commonly highlighted. These factors include individual traits, significant negative growth exposure, personal psychiatric diagnosis, previous substance and addiction history, and an individual’s attitude and perception as risk factors.
Within the individual factor domain, nine articles were found to contribute to the subdomain of personal/ individual traits [ 27 , 28 , 29 , 37 , 38 , 39 , 40 , 43 , 44 ]. Despite the heterogeneity of the study designs and the substances under investigation, all of the papers found statistically significant results for the possible risk factors of adolescent drug abuse. The traits of high impulsivity, rebelliousness, difficulty in regulating emotions, and alexithymia can be considered negative characteristic traits. These adolescents suffer from the inability to self-regulate their emotions, so they tend to externalize their behaviors as a way to avoid or suppress the negative feelings that they are experiencing [ 41 , 47 , 48 ]. On the other hand, engaging in such behaviors could plausibly provide a greater sense of positive emotions and make them feel good [ 49 ]. Apart from that, evidence from a neurophysiological point of view also suggests that the compulsive drive toward drug use is complemented by deficits in impulse control and decision making (impulsive trait) [ 50 ]. A person’s ability in self-control will seriously impaired with continuous drug use and will lead to the hallmark of addiction [ 51 ].
On the other hand, there are articles that reported some individual traits to be protective for adolescents from engaging in drug abuse. Youth with the optimistic trait, a high level of mindfulness, and social phobia were less likely to become drug dependent [ 31 , 33 , 37 ]. All of these articles used different psychometric instruments to classify each individual trait and were mutually exclusive. Therefore, each trait measured the chance of engaging in drug abuse on its own and did not reflect the chance at the end of the spectrum. These findings show that individual traits can be either protective or risk factors for the drugs used among adolescents. Therefore, any adolescent with negative personality traits should be monitored closely by providing health education, motivation, counselling, and emotional support since it can be concluded that negative personality traits are correlated with high risk behaviours such as drug abuse [ 52 ].
Our study also found that a history of maltreatment has a positive association with adolescent drug abuse. Those adolescents with episodes of maltreatment were considered to have negative growth exposure, as their childhoods were negatively affected by traumatic events. Some significant associations were found between maltreatment and adolescent drug abuse, although the former factor was limited to the female gender [ 25 , 30 , 36 ]. One possible reason for the contrasting results between genders is the different sample populations, which only covered child welfare centers [ 36 ] and foster care [ 30 ]. Regardless of the place, maltreatment can happen anywhere depending on the presence of the perpetrators. To date, evidence that concretely links maltreatment and substance abuse remains limited. However, a plausible explanation for this link could be the indirect effects of posttraumatic stress (i.e., a history of maltreatment) leading to substance use [ 53 , 54 ]. These findings highlight the importance of continuous monitoring and follow-ups with adolescents who have a history of maltreatment and who have ever attended a welfare center.
Addiction sometimes leads to another addiction, as described by the findings of several studies [ 29 , 34 ]. An initial study focused on the effects of e-cigarettes in the development of other substance abuse disorders, particularly those related to marijuana, alcohol, and commonly prescribed medications [ 34 ]. The authors found that the use of e-cigarettes can lead to more severe substance addiction [ 55 ], possibly through normalization of the behavior. On the other hand, Chuang et al.’s extensive study in 2017 analyzed the combined effects of either multiple addictions alone or a combination of multiple addictions together with the impulsivity trait [ 29 ]. The outcomes reported were intriguing and provide the opportunity for targeted intervention. The synergistic effects of impulsiveness and three other substance addictions (marijuana, tobacco, and alcohol) substantially increased the likelihood for drug abuse from 3.46 (95%CI 1.25, 9.58) to 10.13 (95% CI 3.95, 25.95). Therefore, proper rehabilitation is an important strategy to ensure that one addiction will not lead to another addiction.
The likelihood for drug abuse increases as the population perceives little or no harmful risks associated with the drugs. On the opposite side of the coin, a greater perceived risk remains a protective factor for marijuana abuse [ 56 ]. However, another study noted that a stronger determinant for adolescent drug abuse was the perceived availability of the drug [ 35 , 57 ]. Looking at the bigger picture, both perceptions corroborate each other and may inform drug use. Another study, on the other hand, reported that there was a decreasing trend of perceived drug risk in conjunction with the increasing usage of drugs [ 58 ]. As more people do drugs, youth may inevitably perceive those drugs as an acceptable norm without any harmful consequences [ 59 ].
In addition, the total spent for screen time also contribute to drug abuse among adolescent [ 43 ]. This scenario has been proven by many researchers on the effect of screen time on the mental health [ 60 ] that leads to the substance use among the adolescent due to the ubiquity of pro-substance use content on the internet. Adolescent with comorbidity who needs medical pain management by opioids also tend to misuse in future. A qualitative exploration on the perspectives among general practitioners concerning the risk of opioid misuse in people with pain, showed pain management by opioids is a default treatment and misuse is not a main problem for the them [ 61 ]. A careful decision on the use of opioids as a pain management should be consider among the adolescents and their understanding is needed.
Within the family factor domain, family structures were found to have both positive and negative associations with drug abuse among adolescents. As described in one study, paternal knowledge was consistently found to be a protective factor against substance abuse [ 26 ]. With sufficient knowledge, the father can serve as the guardian of his family to monitor and protect his children from negative influences [ 62 ]. The work by Luk et al. also reported a positive association of maternal psychological association towards drug abuse (IRR 2.41, p < 0.05) [ 26 ]. The authors also observed the same effect of paternal psychological control, although it was statistically insignificant. This construct relates to parenting style, and the authors argued that parenting style might have a profound effect on the outcomes under study. While an earlier literature review [ 63 ] also reported such a relationship, a recent study showed a lesser impact [ 64 ] with regards to neglectful parenting styles leading to poorer substance abuse outcomes. Nevertheless, it was highlighted in another study that the adolescents’ perception of a neglectful parenting style increased their odds (OR 2.14, p = 0.012) of developing alcohol abuse, not the parenting style itself [ 65 ]. Altogether, families play vital roles in adolescents’ risk for engaging in substance abuse [ 66 ]. Therefore, any intervention to impede the initiation of substance use or curb existing substance use among adolescents needs to include parents—especially improving parent–child communication and ensuring that parents monitor their children’s activities.
Finally, the community also contributes to drug abuse among adolescents. As shown by Li et al. [ 32 ] and El Kazdouh et al. [ 46 ], peers exert a certain influence on other teenagers by making them subconsciously want to fit into the group. Peer selection and peer socialization processes might explain why peer pressure serves as a risk factor for drug-abuse among adolescents [ 67 ]. Another study reported that strong religious beliefs integrated into society play a crucial role in preventing adolescents from engaging in drug abuse [ 46 ]. Most religions devalue any actions that can cause harmful health effects, such as substance abuse [ 68 ]. Hence, spiritual beliefs may help protect adolescents. This theme has been well established in many studies [ 60 , 69 , 70 , 71 , 72 ] and, therefore, could be implemented by religious societies as part of interventions to curb the issue of adolescent drug abuse. The connection with school and structured activity did reduce the risk as a study in USA found exposure to media anti-drug messages had an indirect negative effect on substances abuse through school-related activity and social activity [ 73 ]. The school activity should highlight on the importance of developmental perspective when designing and offering school-based prevention programs [75].
Limitations
We adopted a review approach that synthesized existing evidence on the risk and protective factors of adolescents engaging in drug abuse. Although this systematic review builds on the conclusion of a rigorous review of studies in different settings, there are some potential limitations to this work. We may have missed some other important factors, as we only included English articles, and article extraction was only done from the three search engines mentioned. Nonetheless, this review focused on worldwide drug abuse studies, rather than the broader context of substance abuse including alcohol and cigarettes, thereby making this paper more focused.
Conclusions
This review has addressed some recent knowledge related to the individual, familial, and community risk and preventive factors for adolescent drug use. We suggest that more attention should be given to individual factors since most findings were discussed in relation to such factors. With the increasing trend of drug abuse, it will be critical to focus research specifically on this area. Localized studies, especially those related to demographic factors, may be more effective in generating results that are specific to particular areas and thus may be more useful in generating and assessing local control and prevention efforts. Interventions using different theory-based psychotherapies and a recognition of the unique developmental milestones specific to adolescents are among examples that can be used. Relevant holistic approaches should be strengthened not only by relevant government agencies but also by the private sector and non-governmental organizations by promoting protective factors while reducing risk factors in programs involving adolescents from primary school up to adulthood to prevent and control drug abuse. Finally, legal legislation and enforcement against drug abuse should be engaged with regularly as part of our commitment to combat this public health burden.
Data availability and materials
All data generated or analysed during this study are included in this published article.
Nation, U. World Drug Report 2018 (United Nations publication, Sales No. E.18X.XI.9. United Nation publication). 2018. Retrieved from https://www.unodc.org/wdr2018
Google Scholar
Degenhardt L, Stockings E, Patton G, Hall WD, Lynskey M. The increasing global health priority of substance use in young people. Lancet Psychiatry. 2016;3(3):251–64. https://doi.org/10.1016/S2215-0366(15)00508-8 Elsevier Ltd.
Article PubMed Google Scholar
Ritchie H, Roser M. Drug Use - Our World in Data: Global Change Data Lab; 2019. https://ourworldindata.org/drug-use [10 June 2020]
Holm S, Sandberg S, Kolind T, Hesse M. The importance of cannabis culture in young adult cannabis use. J Subst Abus. 2014;19(3):251–6.
Luikinga SJ, Kim JH, Perry CJ. Developmental perspectives on methamphetamine abuse: exploring adolescent vulnerabilities on brain and behavior. Progress Neuro Psychopharmacol Biol Psychiatry. 2018;87(Pt A):78–84. https://doi.org/10.1016/j.pnpbp.2017.11.010 Elsevier Inc.
Article CAS Google Scholar
Ismail R, Ghazalli MN, Ibrahim N. Not all developmental assets can predict negative mental health outcomes of disadvantaged youth: a case of suburban Kuala Lumpur. Mediterr J Soc Sci. 2015;6(1):452–9. https://doi.org/10.5901/mjss.2015.v6n5s1p452 .
Article Google Scholar
Crews F, He J, Hodge C. Adolescent cortical development: a critical period of vulnerability for addiction. Pharmacol Biochem Behav. 2007;86(2):189–99. https://doi.org/10.1016/j.pbb.2006.12.001 .
Article CAS PubMed Google Scholar
Schulte MT, Hser YI. Substance use and associated health conditions throughout the lifespan. Public Health Rev. 2013;35(2). https://doi.org/10.1007/bf03391702 Technosdar Ltd.
Somani, S.; Meghani S. Substance Abuse among Youth: A Harsh Reality 2016. doi: https://doi.org/10.4172/2165-7548.1000330 , 6, 4.
Book Google Scholar
Drabble L, Trocki KF, Klinger JL. Religiosity as a protective factor for hazardous drinking and drug use among sexual minority and heterosexual women: findings from the National Alcohol Survey. Drug Alcohol Depend. 2016;161:127–34. https://doi.org/10.1016/j.drugalcdep.2016.01.022 .
Article PubMed PubMed Central Google Scholar
Goliath V, Pretorius B. Peer risk and protective factors in adolescence: Implications for drug use prevention. Soc Work. 2016;52(1):113–29. https://doi.org/10.15270/52-1-482 .
Guerrero LR, Dudovitz R, Chung PJ, Dosanjh KK, Wong MD. Grit: a potential protective factor against substance use and other risk behaviors among Latino adolescents. Acad Pediatr. 2016;16(3):275–81. https://doi.org/10.1016/j.acap.2015.12.016 .
National Institutes on Drug Abuse. What are risk factors and protective factors? National Institute on Drug Abuse (NIDA); 2003. Retrieved from https://www.drugabuse.gov/publications/preventing-drug-use-among-children-adolescents/chapter-1-risk-factors-protective-factors/what-are-risk-factors
Nguyen NN, Newhill CE. The role of religiosity as a protective factor against marijuana use among African American, White, Asian, and Hispanic adolescents. J Subst Abus. 2016;21(5):547–52. https://doi.org/10.3109/14659891.2015.1093558 .
Schinke S, Schwinn T, Hopkins J, Wahlstrom L. Drug abuse risk and protective factors among Hispanic adolescents. Prev Med Rep. 2016;3:185–8. https://doi.org/10.1016/j.pmedr.2016.01.012 .
Macleod J, Oakes R, Copello A, Crome PI, Egger PM, Hickman M, et al. Psychological and social sequelae of cannabis and other illicit drug use by young people: a systematic review of longitudinal, general population studies. Lancet. 2004;363(9421):1579–88. https://doi.org/10.1016/S0140-6736(04)16200-4 .
Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319–28. https://doi.org/10.1016/S0140-6736(07)61162-3 .
Semple DM, McIntosh AM, Lawrie SM. Cannabis as a risk factor for psychosis: systematic review. J Psychopharmacol. 2005;19(2):187–94. https://doi.org/10.1177/0269881105049040 .
Nargiso JE, Ballard EL, Skeer MR. A systematic review of risk and protective factors associated with nonmedical use of prescription drugs among youth in the united states: A social ecological perspective. J Stud Alcohol Drugs. 2015;76(1):5–20. https://doi.org/10.15288/jsad.2015.76.5 .
Guxensa M, Nebot M, Ariza C, Ochoa D. Factors associated with the onset of cannabis use: a systematic review of cohort studies. Gac Sanit. 2007;21(3):252–60. https://doi.org/10.1157/13106811 .
Susan MS, Peter SA, Dakshitha W, George CP. The age of adolescence. Lancet Child Adolesc Health. 2018;2(Issue 3):223–8. https://doi.org/10.1016/S2352-4642(18)30022-1 .
Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34(4):285–91. https://doi.org/10.3233/EFI-180221 .
McHugh ML. Interrater reliability: The kappa statistic. Biochem Med. 2012;22(3):276–82. https://doi.org/10.11613/bm.2012.031 .
Cecil CAM, Walton E, Smith RG, Viding E, McCrory EJ, Relton CL, et al. DNA methylation and substance-use risk: a prospective, genome-wide study spanning gestation to adolescence. Transl Psychiatry. 2016;6(12):e976. https://doi.org/10.1038/tp.2016.247 Nature Publishing Group.
Article CAS PubMed PubMed Central Google Scholar
Kobulsky JM. Gender differences in pathways from physical and sexual abuse to early substance use. Child Youth Serv Rev. 2017;83:25–32. https://doi.org/10.1016/j.childyouth.2017.10.027 .
Luk JW, King KM, McCarty CA, McCauley E, Stoep A. Prospective effects of parenting on substance use and problems across Asian/Pacific islander and European American youth: Tests of moderated mediation. J Stud Alcohol Drugs. 2017;78(4):521–30. https://doi.org/10.15288/jsad.2017.78.521 .
Guttmannova K, Skinner ML, Oesterle S, White HR, Catalano RF, Hawkins JD. The interplay between marijuana-specific risk factors and marijuana use over the course of adolescence. Prev Sci. 2019;20(2):235–45. https://doi.org/10.1007/s11121-018-0882-9 .
Dorard G, Bungener C, Phan O, Edel Y, Corcos M, Berthoz S. Is alexithymia related to cannabis use disorder? Results from a case-control study in outpatient adolescent cannabis abusers. J Psychosom Res. 2017;95:74–80. https://doi.org/10.1016/j.jpsychores.2017.02.012 .
Chuang CWI, Sussman S, Stone MD, Pang RD, Chou CP, Leventhal AM, et al. Impulsivity and history of behavioral addictions are associated with drug use in adolescents. Addict Behav. 2017;74:41–7. https://doi.org/10.1016/j.addbeh.2017.05.021 .
Gabrielli J, Jackson Y, Brown S. Associations between maltreatment history and severity of substance use behavior in youth in Foster Care. Child Maltreat. 2016;21(4):298–307. https://doi.org/10.1177/1077559516669443 .
Khoddam R, Jackson NJ, Leventhal AM. Internalizing symptoms and conduct problems: redundant, incremental, or interactive risk factors for adolescent substance use during the first year of high school? Drug Alcohol Depend. 2016;169:48–55. https://doi.org/10.1016/j.drugalcdep.2016.10.007 .
Li SD, Zhang X, Tang W, Xia Y. Predictors and implications of synthetic drug use among adolescents in the gambling Capital of China. SAGE Open. 2017;7(4):215824401773303. https://doi.org/10.1177/2158244017733031 .
Marin S, Heshmatian E, Nadrian H, Fakhari A, Mohammadpoorasl A. Associations between optimism, tobacco smoking and substance abuse among Iranian high school students. Health Promot Perspect. 2019;9(4):279–84. https://doi.org/10.15171/hpp.2019.38 .
Miech RA, O’Malley PM, Johnston LD, Patrick ME. E-cigarettes and the drug use patterns of adolescents. Nicotine Tob Res. 2015;18(5):654–9. https://doi.org/10.1093/ntr/ntv217 .
Schleimer JP, Rivera-Aguirre AE, Castillo-Carniglia A, Laqueur HS, Rudolph KE, Suárez H, et al. Investigating how perceived risk and availability of marijuana relate to marijuana use among adolescents in Argentina, Chile, and Uruguay over time. Drug Alcohol Depend. 2019;201:115–26. https://doi.org/10.1016/j.drugalcdep.2019.03.029 .
Traube DE, Yarnell LM, Schrager SM. Differences in polysubstance use among youth in the child welfare system: toward a better understanding of the highest-risk teens. Child Abuse Negl. 2016;52:146–57. https://doi.org/10.1016/j.chiabu.2015.11.020 .
Wilson JD, Vo H, Matson P, Adger H, Barnett G, Fishman M. Trait mindfulness and progression to injection use in youth with opioid addiction. Subst Use Misuse. 2017;52(11):1486–93. https://doi.org/10.1080/10826084.2017.1289225 .
Dash GF, Feldstein Ewing SW, Murphy C, Hudson KA, Wilson AC. Contextual risk among adolescents receiving opioid prescriptions for acute pain in pediatric ambulatory care settings. Addict Behav. 2020;104:106314. https://doi.org/10.1016/j.addbeh.2020.106314 Epub 2020 Jan 11. PMID: 31962289; PMCID: PMC7024039.
Osborne V, Serdarevic M, Striley CW, Nixon SJ, Winterstein AG, Cottler LB. Age of first use of prescription opioids and prescription opioid non-medical use among older adolescents. Substance Use Misuse. 2020;55(14):2420–7. https://doi.org/10.1080/10826084.2020.1823420 .
Zuckermann AME, Qian W, Battista K, Jiang Y, de Groh M, Leatherdale ST. Factors influencing the non-medical use of prescription opioids among youth: results from the COMPASS study. J Subst Abus. 2020;25(5):507–14. https://doi.org/10.1080/14659891.2020.1736669 .
De Pedro KT, Esqueda MC, Gilreath TD. School protective factors and substance use among lesbian, gay, and bisexual adolescents in California public schools. LGBT Health. 2017;4(3):210–6. https://doi.org/10.1089/lgbt.2016.0132 .
Spillane NS, Schick MR, Kirk-Provencher KT, Hill DC, Wyatt J, Jackson KM. Structured and unstructured activities and alcohol and marijuana use in middle school: the role of availability and engagement. Substance Use Misuse. 2020;55(11):1765–73. https://doi.org/10.1080/10826084.2020.1762652 .
Ogunsola OO, Fatusi AO. Risk and protective factors for adolescent substance use: a comparative study of secondary school students in rural and urban areas of Osun state, Nigeria. Int J Adolesc Med Health. 2016;29(3). https://doi.org/10.1515/ijamh-2015-0096 .
Doggett A, Qian W, Godin K, De Groh M, Leatherdale ST. Examining the association between exposure to various screen time sedentary behaviours and cannabis use among youth in the COMPASS study. SSM Population Health. 2019;9:100487. https://doi.org/10.1016/j.ssmph.2019.100487 .
Afifi RA, El Asmar K, Bteddini D, Assi M, Yassin N, Bitar S, et al. Bullying victimization and use of substances in high school: does religiosity moderate the association? J Relig Health. 2020;59(1):334–50. https://doi.org/10.1007/s10943-019-00789-8 .
El Kazdouh H, El-Ammari A, Bouftini S, El Fakir S, El Achhab Y. Adolescents, parents and teachers’ perceptions of risk and protective factors of substance use in Moroccan adolescents: a qualitative study. Substance Abuse Treat Prevent Policy. 2018;13(1):–31. https://doi.org/10.1186/s13011-018-0169-y .
Sussman S, Lisha N, Griffiths M. Prevalence of the addictions: a problem of the majority or the minority? Eval Health Prof. 2011;34(1):3–56. https://doi.org/10.1177/0163278710380124 .
Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev. 2010;30(2):217–37. https://doi.org/10.1016/j.cpr.2009.11.004 .
Ricketts T, Macaskill A. Gambling as emotion management: developing a grounded theory of problem gambling. Addict Res Theory. 2003;11(6):383–400. https://doi.org/10.1080/1606635031000062074 .
Williams AD, Grisham JR. Impulsivity, emotion regulation, and mindful attentional focus in compulsive buying. Cogn Ther Res. 2012;36(5):451–7. https://doi.org/10.1007/s10608-011-9384-9 .
National Institutes on Drug Abuse. Drugs, brains, and behavior the science of addiction national institute on drug abuse (nida). 2014. Retrieved from https://www.drugabuse.gov/sites/default/files/soa_2014.pdf
Hokm Abadi ME, Bakhti M, Nazemi M, Sedighi S, Mirzadeh Toroghi E. The relationship between personality traits and drug type among substance abuse. J Res Health. 2018;8(6):531–40.
Longman-Mills S, Haye W, Hamilton H, Brands B, Wright MGM, Cumsille F, et al. Psychological maltreatment and its relationship with substance abuse among university students in Kingston, Jamaica, vol. 24. Florianopolis: Texto Contexto Enferm; 2015. p. 63–8.
Rosenkranz SE, Muller RT, Henderson JL. The role of complex PTSD in mediating childhood maltreatment and substance abuse severity among youth seeking substance abuse treatment. Psychol Trauma Theory Res Pract Policy. 2014;6(1):25–33. https://doi.org/10.1037/a0031920 .
Krishnan-Sarin S, Morean M, Kong G, et al. E-Cigarettes and “dripping” among high-school youth. Pediatrics. 2017;139(3). https://doi.org/10.1542/peds.2016-3224 .
Adinoff B. Neurobiologic processes in drug reward and addiction. Harvard review of psychiatry. NIH Public Access. 2004;12(6):305–20. https://doi.org/10.1080/10673220490910844 .
Kandel D, Kandel E. The gateway hypothesis of substance abuse: developmental, biological and societal perspectives. Acta Paediatrica. 2014;104(2):130–7.
Dempsey RC, McAlaney J, Helmer SM, Pischke CR, Akvardar Y, Bewick BM, et al. Normative perceptions of Cannabis use among European University students: associations of perceived peer use and peer attitudes with personal use and attitudes. J Stud Alcohol Drugs. 2016;77(5):740–8.
Cioffredi L, Kamon J, Turner W. Effects of depression, anxiety and screen use on adolescent substance use. Prevent Med Rep. 2021;22:101362. https://doi.org/10.1016/j.pmedr.2021.101362 .
Luckett T, NewtonJohn T, Phillips J, et al. Risk of opioid misuse in people with cancer and pain and related clinical considerations:a qualitative study of the perspectives of Australian general practitioners. BMJ Open. 2020;10(2):e034363. https://doi.org/10.1136/bmjopen-2019-034363 .
Lipari RN. Trends in Adolescent Substance Use and Perception of Risk from Substance Use. The CBHSQ Report. Substance Abuse Mental Health Serv Admin. 2013; Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/27656743 .
Muchiri BW, dos Santos MML. Family management risk and protective factors for adolescent substance use in South Africa. Substance Abuse. 2018;13(1):24. https://doi.org/10.1186/s13011-018-0163-4 .
Becoña E, Martínez Ú, Calafat A, Juan M, Fernández-Hermida JR, Secades-Villa R. Parental styles and drug use: a review. In: Drugs: Education, Prevention and Policy: Taylor & Francis; 2012. https://doi.org/10.3109/09687637.2011.631060 .
Berge J, Sundel K, Ojehagen A, Hakansson A. Role of parenting styles in adolescent substance use: results from a Swedish longitudinal cohort study. BMJ Open. 2016;6(1):e008979. https://doi.org/10.1136/bmjopen-2015-008979 .
Opara I, Lardier DT, Reid RJ, Garcia-Reid P. “It all starts with the parents”: a qualitative study on protective factors for drug-use prevention among black and Hispanic girls. Affilia J Women Soc Work. 2019;34(2):199–218. https://doi.org/10.1177/0886109918822543 .
Martínez-Loredo V, Fernández-Artamendi S, Weidberg S, Pericot I, López-Núñez C, Fernández-Hermida J, et al. Parenting styles and alcohol use among adolescents: a longitudinal study. Eur J Invest Health Psychol Educ. 2016;6(1):27–36. https://doi.org/10.1989/ejihpe.v6i1.146 .
Baharudin MN, Mohamad M, Karim F. Drug-abuse inmates maqasid shariah quality of lifw: a conceotual paper. Hum Soc Sci Rev. 2020;8(3):1285–94. https://doi.org/10.18510/hssr.2020.83131 .
Henneberger AK, Mushonga DR, Preston AM. Peer influence and adolescent substance use: a systematic review of dynamic social network research. Adolesc Res Rev. 2020;6(1):57–73. https://doi.org/10.1007/s40894-019-00130-0 Springer.
Gomes FC, de Andrade AG, Izbicki R, Almeida AM, de Oliveira LG. Religion as a protective factor against drug use among Brazilian university students: a national survey. Rev Bras Psiquiatr. 2013;35(1):29–37. https://doi.org/10.1016/j.rbp.2012.05.010 .
Kulis S, Hodge DR, Ayers SL, Brown EF, Marsiglia FF. Spirituality and religion: intertwined protective factors for substance use among urban American Indian youth. Am J Drug Alcohol Abuse. 2012;38(5):444–9. https://doi.org/10.3109/00952990.2012.670338 .
Miller L, Davies M, Greenwald S. Religiosity and substance use and abuse among adolescents in the national comorbidity survey. J Am Acad Child Adolesc Psychiatry. 2000;39(9):1190–7. https://doi.org/10.1097/00004583-200009000-00020 .
Moon SS, Rao U. Social activity, school-related activity, and anti-substance use media messages on adolescent tobacco and alcohol use. J Hum Behav Soc Environ. 2011;21(5):475–89. https://doi.org/10.1080/10911359.2011.566456 .
Simone A. Onrust, Roy Otten, Jeroen Lammers, Filip smit, school-based programmes to reduce and prevent substance use in different age groups: what works for whom? Systematic review and meta-regression analysis. Clin Psychol Rev. 2016;44:45–59. https://doi.org/10.1016/j.cpr.2015.11.002 .
Download references
Acknowledgements
The authors acknowledge The Ministry of Higher Education Malaysia and The Universiti Kebangsaan Malaysia, (UKM) for funding this study under the Long-Term Research Grant Scheme-(LGRS/1/2019/UKM-UKM/2/1). We also thank the team for their commitment and tireless efforts in ensuring that manuscript was well executed.
Financial support for this study was obtained from the Ministry of Higher Education, Malaysia through the Long-Term Research Grant Scheme-(LGRS/1/2019/UKM-UKM/2/1). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and affiliations.
Department of Community Health, Universiti Kebangsaan Malaysia, Cheras, 56000, Kuala Lumpur, Malaysia
Azmawati Mohammed Nawi, Mohd Rohaizat Hassan & Mohd Rizal Abdul Manaf
Centre for Research in Psychology and Human Well-Being (PSiTra), Faculty of Social Sciences and Humanities, Universiti Kebangsaan Malaysia, 43600, Bangi, Selangor, Malaysia
Rozmi Ismail, Fauziah Ibrahim & Nurul Shafini Shafurdin
Clinical Psychology and Behavioural Health Program, Faculty of Health Sciences, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
Noh Amit & Norhayati Ibrahim
You can also search for this author in PubMed Google Scholar
Contributions
Manuscript concept, and drafting AMN and RI; model development, FI, NI and NA.; Editing manuscript MRH, MRAN, NSS,; Critical revision of manuscript for important intellectual content, all authors. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Rozmi Ismail .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Ethics Committee of the Secretariat of Research Ethics, Universiti Kebangsaan Malaysia, Faculty of Medicine, Cheras, Kuala Lumpur (Reference no. UKMPPI/111/8/JEP-2020.174(2). Dated 27 Mac 2020.
Consent for publication
Not applicable.
Competing interests
The authors AMN, RI, FI, MRM, MRAM, NA, NI NSS declare that they have no conflict of interest relevant to this work.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Nawi, A.M., Ismail, R., Ibrahim, F. et al. Risk and protective factors of drug abuse among adolescents: a systematic review. BMC Public Health 21 , 2088 (2021). https://doi.org/10.1186/s12889-021-11906-2
Download citation
Received : 10 June 2021
Accepted : 22 September 2021
Published : 13 November 2021
DOI : https://doi.org/10.1186/s12889-021-11906-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Drug abuse, substance, adolescent
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
HEALTH AND SCIENCE MADE SIMPLE
Understanding Adolescent Substance Abuse
Published June 17, 2024 by coopero

Written by Minowa Gonzalez | Edited by Danica Kwan
Photo by MART PRODUCTION
Every year, 15% of high school students take their first steps into a realm that promises escape but often delivers extreme consequences: the world of illicit drug use. The developing adolescent brain is especially vulnerable to addiction and the damaging effects of substance abuse. According to the National Institute on Drug Abuse in 2023, “10.9% of eighth graders, 19.8% of 10th graders, and 31.2% of 12th graders report any illicit drug use in the past year” [1] . This statistic only represents the reported cases, without accounting for unreported instances due to legal repercussions, such as jail time and potential impact on future opportunities. A government foundation called Get Smart About Drugs reports that the need to relieve boredom, forget their troubles, and the pressure of belonging to a certain group drive adolescents (aged 13-18) to experiment with drugs [2] . Moreover, the combination of easy access to drugs and limited awareness about the risks drives adolescents to engage in illicit drug use.
Substance use affects groups differently. The likelihood of developing a substance use disorder increases significantly when individuals initiate alcohol and drug use during adolescence [4] . The 2009-2019 Youth Risk Behavior report from the Centers for Disease Control (CDC) highlights a concern regarding youth high-risk substance abuse: among high school students who had ever used illicit drugs (such as cocaine, inhalants, methamphetamines, hallucinogens, etc.) there was a higher prevalence of drug use among male students than female students [3] . Additionally, youth with lower socioeconomic status are at higher risk for engaging in substance use [5] . Being high-risk is categorized as involving the misuse of prescription drugs, illicit drug use, and/or injection drug use, all of which can lead to consequences such as injury, criminal involvement, and school dropout.
Education plays a pivotal role in preventing teen illicit drug use by providing adolescents with the knowledge and skills necessary to make informed decisions about substance use. Organizations such as the CDC Division of Adolescent and School Health (DASH) and the National Institute on Drug Abuse (NIDA) promote education on drug abuse. Through initiatives like the School Health Policies and Practices Study (SHPPS), DASH works to implement effective health education programs about teen drug abuse [6] [7] . Similarly, NIDA conducts research, develops education materials, and funds prevention programs [8] . Through education, teens can better understand the implications of their choices and develop the tools necessary to resist the allure of illicit drugs, ultimately leading to healthier and more fulfilling lives.
As we move forward, it is necessary to address the consequences of adolescent substance abuse in our changing world. Every day another adolescent falls prey to the hidden consequences of drug use. Effective education given to our youth can create a supportive environment that promotes healthy choices and reduces the prevalence of high-risk substance abuse among adolescents. Collective efforts from families, schools, communities, and policymakers are crucial in protecting our youth against substance abuse.
References:
1. Reported drug use among adolescents continued to hold below pre-pandemic levels in 2023 | National Institute on Drug Abuse . (2024, March 27). National Institute on Drug Abuse. https://nida.nih.gov/news-events/news-releases/2023/12/reported-drug-use-among-adolescents-continued-to-hold-below-pre-pandemic-levels-in-2023
2. Why do teens use drugs? | Get smart about drugs . (n.d.). https://www.getsmartaboutdrugs.gov/family/why-do-teens-use-drugs
3. Youth Risk Behavior Surveillance Data Summary & Trends Report: 2009-2019 | 2020 | Dear Colleague Letters | NCHHSTP | CDC . (n.d.). https://www.cdc.gov/nchhstp/dear_colleague/2020/dcl-102320-YRBS-2009-2019-report.html
4. Gray, K. M., & Squeglia, L. M. (2017). Research Review: What have we learned about adolescent substance use? Journal of Child Psychology and Psychiatry and Allied Disciplines , 59 (6), 618–627. https://doi.org/10.1111/jcpp.12783
5. Frobel, W., Grafe, N., Meigen, C., Vogel, M., Hiemisch, A., Kiess, W., & Poulain, T. (2022). Substance use in childhood and adolescence and its associations with quality of life and behavioral strengths and difficulties. BMC Public Health , 22 (1). https://doi.org/10.1186/s12889-022-12586-2
6. Adolescent and School Health (DASH) | CDC . (n.d.). https://www.cdc.gov/healthyyouth/index.htm
7. School Health Policies and Practices Study (SHPPS) . (n.d.). https://www.cdc.gov/healthyyouth/data/shpps/index.htm
8. National Institute on Drug Abuse (NIDA) . (2024, March 6). National Institutes of Health (NIH). https://www.nih.gov/about-nih/what-we-do/nih-almanac/national-institute-drug-abuse-nida
9. Hsiung, H., Patel, K., Hundal, H., Baccouche, B. M., & Tsao, K. W. (2022). Preventing Substance Abuse in Adolescents: A Review of High-Impact Strategies. Curēus . https://doi.org/10.7759/cureus.27361
Share this post:
Published in Pharmacy
- Adolescents
- Danica Kwan
- Minowa Gonzalez
- Substance abuse
Teenage Drug Abuse
This essay will address the issue of teenage drug abuse. It will explore its causes, effects on health and development, preventive measures, and the role of education and support in addressing this societal concern. PapersOwl showcases more free essays that are examples of Addiction.
How it works
There is a major concern about the teenage drug use today. Within the ages 15 through 24, fifty percent of deaths (from homicides, accidents, suicides) involve drugs. The two common reasons why teens use drugs are anxiety and depression. Factors like peer pressure, desire to escape, curiosity, emotional struggles, and stress may also lead to the consumption of drugs or alcohol. Teens are more likely to abuse drugs than adults because the part of their brain used for judgment and decision making is yet to fully develop.
Therefore, they lack the mental capacity to truly understand the consequences of drugs. As a result of this carelessness, teenagers face a series of problems such as brain damage, delayed puberty, addiction, emotional and physical problems. For example, Marijuana is the substance most widely used by adolescents, after alcohol. Studies show that thirty percent of those who use Marijuana have some level of Marijuana use disorder. Drugs have been abused for thousands of years and its effects are that long. The extraction of active ingredients from psychoactive drugs first occurred in the 19th century.
By the early 1900s, about 250,000 were drug addicts. After noticing the addiction epidemic, legislators made it illegal for doctors and pharmacies to prescribe narcotics to addicts. Marijuana was the most commonly used illicit drug in 2013 used by 80.6% of current illicit drug users. The potency of marijuana in today market is nearly triple the strength of what was available 20 years ago. In the previous years’ teenagers were addicted to tobacco and now they are addicted to marijuana. More teenagers have experience with marijuana than nicotine. They believe marijuana is healthier because it is a plant base but in reality, it is unhealthy because of its addictive chemicals.Moreover, various doctors and drug specialists have come up with a solution to not only teenage drug use but alcohol as well. For example, Dr. Amy Schreiner and Dr. Sherry Steward explained how personality traits can lead to future drug and alcohol problems. They came up with four profiles, impulsiveness, anxiety sensitivity, sensation seeking and hopelessness. Impulsiveness may prompt an adolescent to consume cocaine or other stimulants, without considering the consequences. Also, teens who are immune to peer pressure, and are identified as thrill- seekers, are more prone to drug abuse. Stewart expresses that teens with high-risk personalities may be attracted to drugs that meet their short-term needs. Teens with anxiety-sensitive tend to get into trouble because they go for drugs that make them risk takers, to deal with their anxiety.
Results of their Efforts
In response to that, Stewart helped create the Substance Use Risk Profile Scale (SURPS), to identify children at higher risk for future drug and alcohol problems. The self-report questionnaire later known as Preventure?, was developed by Canadian researcher Dr. Patricia Concard who tested it in thousands of adolescents in various countries around the world. The results were encouraging as preventure has reduced the odds of overall drug use. Preventure has also delayed the severity of mental health problems including depression and panic attacks. In addition, the trails showed reduced anxiety and good conduct symptoms.Constantly reminding teenagers about the consequences of drug use might not always be effective for those who do not want to listen. Sometimes teenagers need to be heard and how can we aid teenagers if we do not truly understand them? We can set up support groups where teenagers would not be judged but feel that they belong. For instance, low self-esteem teenagers would be given motivational speeches; perhaps by an adult who has had experience with drugs and understands what they are going through. In addition, they can be offered information about their health issue that can occur when they are in contact with drugs. Furthermore, these group sessions may include fun games that would boost the confidence in teenagers’. Basically, teens will be ensured that they are worth so much more and that there are other alternatives, rather than using drugs. This method would help them realize their mistakes and motivate them to stop consuming drugs.
Cite this page
Teenage Drug Abuse. (2020, Apr 11). Retrieved from https://papersowl.com/examples/teenage-drug-abuse/
"Teenage Drug Abuse." PapersOwl.com , 11 Apr 2020, https://papersowl.com/examples/teenage-drug-abuse/
PapersOwl.com. (2020). Teenage Drug Abuse . [Online]. Available at: https://papersowl.com/examples/teenage-drug-abuse/ [Accessed: 26 Aug. 2024]
"Teenage Drug Abuse." PapersOwl.com, Apr 11, 2020. Accessed August 26, 2024. https://papersowl.com/examples/teenage-drug-abuse/
"Teenage Drug Abuse," PapersOwl.com , 11-Apr-2020. [Online]. Available: https://papersowl.com/examples/teenage-drug-abuse/. [Accessed: 26-Aug-2024]
PapersOwl.com. (2020). Teenage Drug Abuse . [Online]. Available at: https://papersowl.com/examples/teenage-drug-abuse/ [Accessed: 26-Aug-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers

A Front-Row Change Agent of the Drug Epidemic
Dr. robert dupont shifted the paradigm from demonization to treatment of users..
Updated August 19, 2024 | Reviewed by Hara Estroff Marano
- What Is Addiction?
- Find a therapist to overcome addiction
- In the 1970s, people addicted to opioids were demonized, considered hopeless. Some still believe this.
- Setting high standards and following addicted patients for five years helps doctors know what treatments work.
- Prevention is key to success in substance abuse, and it’s important to encourage non-use among teens.

In the United States, people addicted to opioids were once demonized as hopelessly bad, and treatment was virtually nonexistent. No one may have done more to change both matters than psychiatrist Robert DuPont, M.D, who, in 1969, during an unexplained surge in crime in the nation's capital, was working with prisoners in the District of Columbia Department of Corrections. DuPont decided to test incoming inmates for drugs and was shocked to learn that nearly half (45%) were addicted to heroin. Desperate for heroin, they turned to crime for money.
At the behest of the district's mayor, DuPont developed a D.C.-based clinic, the Narcotics Treatment Administration. It treated more than 15,000 heroin addicts over the next three years, and the D.C. crime rate plummeted by 50%, in a direct correlation.
Helping Medical Professionals Do Better
Robert L. “Bob” DuPont, born in 1936, graduated from Emory University and Harvard Medical School and completed his psychiatric training at the National Institutes of Health. He became the first director of the newly-created National Institute on Drug Abuse (NIDA), where he created a first-of-its-kind comprehensive training program for doctors, nurses, and counselors working in addiction treatment programs. Drug overdose deaths began declining, from from 6,413 to 2,492 by 1980.
In 1978, DuPont left government service to create the Institute for Behavior and Health (IBH), a think tank focusing on drug policy. Dupont has published more than 400 journal articles and 15 books, most recently Chemical Slavery: Understanding Addictions and Stopping the Drug Epidemic (2018).
The IBH conducted the first national study of doctors dependent on drugs and alcohol , their treatment, and five-year outcomes. “Physicians are given a comprehensive assessment by a team of professionals and get treatment for comorbidities, but the focus is on their addictions. They typically attend a month or more of residential treatment and, as outpatients, are monitored for five years with random drug and alcohol testing. If they miss a scheduled test or test positive for any drug, including alcohol, they are taken out of their practice again, assessed, and sent back to treatment.”
DuPont points out that many doctors who entered the program were initially resentful because they didn’t think there was anything wrong with them—typical of individuals with substance use disorder from all walks of life. Yet, most physicians greatly value their medical license, and the overwhelming majority cooperated because participation and success meant they could continue to practice medicine.
His study of nearly 1,000 drug-addicted physicians closely monitored for five years showed what is possible for the rest of the population. Seventy-eight percent never tested positive for drugs or alcohol, an excellent record. In addition, of those who did have a positive or missed drug test, nearly two-thirds never had a second positive test.
A follow-up study of physicians who successfully completed treatment and monitoring contracts five or more years ago showed that more than 95% were still in recovery. Physicians rated the treatment they had received as important to their recovery but said the most valued part of their care was involvement in the 12 steps.

Lessons Learned About Substance Abuse
DuPont says many people don’t realize that it’s rarely just one drug abused by most problematic substance users. And that is particularly true of individuals who die from drug overdoses, in whom two or more drugs are often identified post-mortem.
He also notes that many drugs used today are not in their natural forms but instead are ultra-potent synthetics, like fentanyl. In 2022, about 111,000 people died, and in 2023, about 108,300 people died of drug overdose. .
Early diagnosis and treatment is key
The earlier patients are diagnosed and treated, the better their chances of achieving and sustaining recovery, says DuPont. Many people can stop using substances for some period. However, the real problem is not drug withdrawal, as many people believe, but, instead, the repeated relapses . Yet he has known many individuals with seemingly hopeless drug or alcohol issues who emerged sober and productive. He largely credits organizations like Alcoholics Anonymous and Narcotics Anonymous.
Prevention is best
Whenever possible, prevention of drug use is best, particularly among young people. Not only is adolescence a time when most addictions begin, it's also a time when the brain is uniquely vulnerable..
DuPont now focuses on youth substance-use prevention: no alcohol, nicotine, marijuana/THC, or other drugs by those under age 21. He notes that the percentage of 12th graders who report never using in their lifetime has increased from around 26% in 2018 to 32% in 2023. The trend is also evident in younger students. DuPont emphasizes, “This trend is key to reversing decades of pain, suffering, and addictions.“

At age 88, Robert DuPont, M.D., advocates for treatment research, long-term treatment with outcome reporting, mental health treatment parity (as important as physical health), and prevention. Recovery, he insists, is possible.

Levy S, Campbell MD, Shea CL, DuPont R. Trends in Abstaining From Substance Use in Adolescents: 1975-2014. Pediatrics. 2018 Aug;142(2):e20173498. doi: 10.1542/peds.2017-3498. PMID: 30026244.
DuPont RL, McLellan AT, White WL, Merlo LJ, Gold MS. Setting the standard for recovery: Physicians' Health Programs. J Subst Abuse Treat. 2009 Mar;36(2):159-71. doi: 10.1016/j.jsat.2008.01.004. PMID: 19161896.; DuPont RL, Compton WM, McLellan AT. Five-Year Recovery: A New Standard for Assessing Effectiveness of Substance Use Disorder Treatment. J Subst Abuse Treat. 2015 Nov;58:1-5. doi: 10.1016/j.jsat.2015.06.024. Epub 2015 Aug 1. PMID: 26277423.
Compton WM, Valentino RJ, DuPont RL. Polysubstance use in the U.S. opioid crisis. Mol Psychiatry. 2021 Jan;26(1):41-50. doi: 10.1038/s41380-020-00949-3. Epub 2020 Nov 13. PMID: 33188253; PMCID: PMC7815508.
DuPont RL, Lieberman JA. Young brains on drugs. Science. 2014 May 9;344(6184):557. doi: 10.1126/science.1254989. PMID: 24812368

Mark S. Gold, M.D., is a pioneering researcher, professor, and chairman of psychiatry at Yale, the University of Florida, and Washington University in St Louis. His theories have changed the field, stimulated additional research, and led to new understanding and treatments for opioid use disorders, cocaine use disorders, overeating, smoking, and depression.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

Sticking up for yourself is no easy task. But there are concrete skills you can use to hone your assertiveness and advocate for yourself.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier Sponsored Documents
Interventions for Adolescent Substance Abuse: An Overview of Systematic Reviews
a Division of Women and Child Health, Aga Khan University, Karachi, Pakistan
Rehana A. Salam
Ahmed arshad, yaron finkelstein.
b Division of Emergency Medicine, The Hospital for Sick Children, Toronto, Ontario, Canada
c Division of Clinical Pharmacology and Toxicology, The Hospital for Sick Children, Toronto, Ontario, Canada
Zulfiqar A. Bhutta
d Centre for Global Child Health, The Hospital for Sick Children, Toronto, Ontario, Canada
e Center of Excellence in Women and Child Health, The Aga Khan University, Karachi, Pakistan
Many unhealthy behaviors often begin during adolescence and represent major public health challenges. Substance abuse has a major impact on individuals, families, and communities, as its effects are cumulative, contributing to costly social, physical, and mental health problems. We conducted an overview of systematic reviews to evaluate the effectiveness of interventions to prevent substance abuse among adolescents. We report findings from a total of 46 systematic reviews focusing on interventions for smoking/tobacco use, alcohol use, drug use, and combined substance abuse. Our overview findings suggest that among smoking/tobacco interventions, school-based prevention programs and family-based intensive interventions typically addressing family functioning are effective in reducing smoking. Mass media campaigns are also effective given that these were of reasonable intensity over extensive periods of time. Among interventions for alcohol use, school-based alcohol prevention interventions have been associated with reduced frequency of drinking, while family-based interventions have a small but persistent effect on alcohol misuse among adolescents. For drug abuse, school-based interventions based on a combination of social competence and social influence approaches have shown protective effects against drugs and cannabis use. Among the interventions targeting combined substance abuse, school-based primary prevention programs are effective. Evidence from Internet-based interventions, policy initiatives, and incentives appears to be mixed and needs further research. Future research should focus on evaluating the effectiveness of specific interventions components with standardized intervention and outcome measures. Various delivery platforms, including digital platforms and policy initiative, have the potential to improve substance abuse outcomes among adolescents; however, these require further research.
Adolescence is recognized as the period for onset of behaviors and conditions that not only affect health limited to that time but also lead to adulthood disorders. Unhealthy behaviors such as smoking, drinking, and illicit drug use often begin during adolescence; they are closely related to increased morbidity and mortality and represent major public health challenges. Unemployment, poor health, accidents, suicide, mental illness, and decreased life expectancy all have drug misuse as a major common contributing factor [1] , [2] . Substance abuse has a major impact on individuals, families, and communities as its effects are cumulative, contributing to costly social, physical, and mental health problems [3] . Several factors can enhance the risk for initiating or continuing substance abuse including socioeconomic status, quality of parenting, peer group influence, and biological/inherent predisposition toward drug addiction [4] . This culminates in a cycle where these individuals cease to perform as effective members of society and instead are consumed by their addictions [5] .
Globally, tobacco use is the leading preventable cause of premature death and most adult smokers initiate smoking in adolescence [6] , [7] . The prevalence of smoking in girls and boys varies across countries; 1 in every 10 girls aged 13–15 years and 1 in every 5 boys aged 13–15 years use tobacco [2] , [6] . Smoking rates are generally highest in Europe and the Western Pacific regions while cigarette smoking is decreasing among younger adolescents in most high-income countries (HICs) and in some low- and middle-income countries. Approximately 4% of the global burden of disease is attributable to alcohol use [8] . Alcohol consumption among adolescents and young adults is increasing globally; however, it is decreasing in most HICs in Europe and North America [2] , [9] . Currently, the World Health Organization (WHO) European Region and WHO Region of the Americas report the highest proportions of drinkers among adolescents while the WHO South-East Asia Region and WHO Eastern Mediterranean Region have the lowest [9] . In general, men drink more alcohol than women, but the sex difference is smaller at younger age. Cannabis use is associated with a decline in intelligence quotient scores before age 18 years and an increase in the risk of injury among adults. Unlike other substances, in many countries, boys and girls show similar prevalence of ever-using cannabis.
Efforts should be concerted on early identification, awareness and prevention programs, and routine monitoring of adolescent health data. Given the prevailing burden and impact of substance abuse in children and adolescents, it is essential that effective interventions and delivery platforms on enhancing social skills, problem-solving skills, and self-confidence are identified and implemented [10] . Standardized screening tools on identifying adolescents at high risk are available and outlined in the American Academy of Pediatrics and National Institute on Alcohol Abuse and Alcoholism publications [11] , [12] , [13] , [14] . School-based surveys of adolescents monitor a number of these health-related behaviors among adolescents at the country level. The focus should be targeting modifiable risk factors and enhancing protective factors through family, school, and community prevention programs [15] . The various types of prevention programs can be delivered via school, community, and health care systems with general goals of case finding with accompanying referral and treatment or risk factor reduction [16] , [17] , [18] .
This article is part of a series of reviews conducted to evaluate the effectiveness of potential interventions to improve adolescent health and well-being. We developed a conceptual framework based on existing conceptual frameworks [19] , [20] and consultations and deliberations with the global experts in the field of adolescent health, and based on the recommendations, we identified a set of interventions to be incorporated in our review process. The interventions were chosen from the existing work on the basis of proven and potential effectiveness to improve adolescent health outcomes and access to primary health care and commodities for adolescents [20] , [21] , [22] , [23] . Detailed conceptual framework, methodology, and other potential interventions have been discussed in separate articles [24] , [25] , [26] , [27] , [28] , [29] , [30] . Our conceptual framework depicts the individual and general risk factors through the life cycle perspective that can have implications at any stage. However, the focus of this overview is to evaluate potential interventions and delivery platforms targeting adolescent age group only and impact quality of life thereon [25] . We focused on risk factors including risky sexual behaviors, unintended pregnancies, violence, risky driving (including speeding and drunk driving), undernutrition, obesity, infections, and mental health risks. Then we identified a range of potential interventions which could alleviate these risks including sexual and reproductive health interventions, nutrition interventions, infections and immunizations, mental health interventions, substance abuse, and injury prevention interventions. The conceptual framework shows that implementation of these interventions could yield immediate and direct results, including improving access to sexual health, mental health, and substance abuse services; knowledge of sexually transmitted infections, dietary behavior, and physical activity; immunization uptake; and delivery of suicide preventive services. Broadly, the conceptual framework classifies outcomes to individual, community, and societal levels, and it illustrates that the immediate and direct impacts could yield improved health, better adult life, and improved work productivity; these individual impacts could lead to gains at the family and immediate community which collectively could help accelerate economic growth and national progress.
In this article, we conducted a comprehensive overview of systematic reviews for the effectiveness of substance abuse interventions for adolescents and various delivery platforms.
We systematically reviewed literature published up to December 2015 to identify systematic reviews on interventions for substance abuse in adolescent population. For the purpose of this overview, the adolescent population was defined as aged 11–19 years; however, since many reviews targeted youth (aged 15–24 years) along with adolescents, exceptions were made to include reviews targeting adolescents and youth. We did not apply any limitations on the start search date or geographical settings. We considered all available published systematic reviews on interventions for adolescent substance abuse. A broad search strategy was used that included a combination of appropriate keywords, medical subject heading, and free text terms. Search was conducted in the Cochrane Library and PubMed. The abstracts (and the full sources where abstracts are not available) were screened by two abstractors to identify systematic reviews adhering to our objectives. Any disagreements on selection of reviews between these two primary abstractors were resolved by the third reviewer. After retrieval of the full texts of all the reviews that met the inclusion/exclusion criteria, data from each review were extracted independently into a standardized form. Information was extracted on (1) the characteristics of included studies; (2) description of methods, participants, interventions, and outcomes; (3) measurement of treatment effects; (4) methodological issues; and (5) risk of bias tool. We extracted pooled effect size for the outcomes reported by the review authors with 95% confidence intervals (CIs). We assessed and reported the quality of included reviews using the 11-point assessment of the methodological quality of systematic reviews (AMSTAR) criteria [31] . We excluded nonsystematic reviews, nonindexed publications/reports, systematic reviews evaluating the efficacy of pharmacological intervention, systematic reviews focusing on interventions for secondhand smoking, systematic review focusing on multiple health risk factors rather than substance abuse alone, systematic reviews focusing on specific population groups (e.g., European countries) alone, interventions targeting population other than adolescents and youth, and reviews not reporting outcomes related to substance abuse.
Our search identified 614 potentially relevant review titles, of which 110 full texts were reviewed. Finally, 46 reviews were deemed eligible and meeting the inclusion criteria ( Figure 1 ). We classified the included reviews into the following categories for reporting findings:
- 1. Intervention for smoking/tobacco use (n = 20)
- 2. Interventions for alcohol use (n = 8)
- 3. Interventions for drug use (n = 2)
- 4. Interventions targeting combined substance abuse (n = 16)

Search flow diagram. MeSH = Medical Subject Heading.
Table 1 describes the characteristics of the included reviews while Table 2 provides the summary estimates for all the interventions.
Table 1
Characteristics of included reviews
| Intervention | Review | Number of included studies | Setting | Intervention details | AMSTAR rating | Meta-analysis | Outcomes reported |
|---|---|---|---|---|---|---|---|
| Smoking/tobacco | |||||||
| School-based interventions | Thomas et al. | 134 RCTs | Mostly in high-income countries except a few trials in India, Thailand, and Mexico | Information-only curricula, social competence curricula, social influence curricula, multimodal programs | 9 | Yes | Smoking status |
| Isensee and Hanewinkel | 5 RCTs | High-income countries | “Smoke-Free Class competition” (SFC) is a school-based smoking prevention program including commitment not to smoke, contract management, and prizes as rewards broadly implemented in Europe. | 6 | Yes | Current smoking at follow-up | |
| Wiehe et al. | 8 RCTs | High-income countries | School-based smoking prevention trials with follow-up smoking prevalence data through at least 12th grade or age 18 years | 6 | No | Smoking prevalence | |
| Family-/community-based interventions | Thomas et al. | 27 RCTs | All in high-income countries except one in India | Interventions with children and family members intended to deter starting to use tobacco. Those with school- or community-based components were included provided the effect of the family-based intervention could clearly be measured and separated from the wider school- or community-based interventions. Interventions that focused on preventing drug or alcohol use were included if outcomes for tobacco use were reported. The family-based intervention could include any components to change parenting behavior, parental or sibling smoking behavior, or family communication and interaction. | 10 | Yes | New smoking at follow-up, smoking at follow-up |
| Carson et al. | 15 RCTs and 10 CCTs | All in high-income countries except one in India | Interventions were considered which (1) were targeted at entire or parts of entire communities or large areas, (2) had the intention of influencing the smoking behavior of young people, and (3) focused on multicomponent (i.e., more than one) community intervention, which could include but was not limited to: school-based programs, media promotion (e.g., TV, radio, print), public policy, organizational initiatives, health care provider initiatives, sports, retailer and workplace initiatives, antitobacco contests, and youth antismoking clubs. Community interventions were defined as coordinated widespread (multicomponent) programs in a particular geographical area (e.g., school districts) or region or in groupings of people who share common interests or needs, which support nonsmoking behavior. Studies which only included single component interventions, did not have community involvement (e.g., school based only), or had mass media as the sole form of intervention delivery were excluded. | 10 | Yes | Smoking daily, smoking weekly, smoking monthly, ever smoked, smokeless tobacco use | |
| Patnode et al. | 19 RCTs | All in high-income countries | Primary care interventions | 5 | Yes | Smoking initiation, smoking cessation | |
| Digital platforms | Hutton et al. | 21 RCTs | All in high-income countries | Web delivered smoking cessation program and had a minimum of 1-month follow-up after intervention. | 8 | No | Smoking cessation |
| Allen et al. | — | — | Antitobacco media campaign intended to influence youth cognitions or behavior or explore the relative effectiveness of campaign characteristics among youth. | — | No | — | |
| Civljak et al. | 28 RCTs and quasi RCTs | All in high-income countries | Internet-based interactive, personalized and noninteractive interventions, which focused on standard approaches to information delivery. Interactive interventions were not necessarily personalized. | 9 | No | Smoking cessation at 6 months | |
| Brinn et al. | 7 RCTs | All in high-income countries | Mass media is defined here as channels of communication such as television, radio, newspapers, billboards, posters, leaflets, or booklets intended to reach large numbers of people and which are not dependent on person-to-person contact. | 9 | No | Smoking/tobacco use status | |
| Policy interventions | Lovato et al. | 19 longitudinal studies | All in high-income countries | The “intervention” is tobacco mass media advertising by the industry, including tobacco promotion. Mass media channels of communication include advertising delivered through television, radio, newspapers, billboards, posters, and so forth. Tobacco promotion includes giveaways such as T-shirts and other items bearing tobacco industry logos. In practice, the measure of exposure to the intervention may not discriminate between specific types of advertising since adolescents are exposed to many sources. Indices of receptivity to advertising which use measures such as having a favorite advertisement, and ownership of or willingness to own promotional items could be used as indicators of exposure. | 6 | No | Self-reported smoking status (nonsmoker, current smoker, ex-smoker) Self-reported consumption of specific brands |
| Coppo et al. | 1 RCT | China | All written policies that regulate tobacco use inside and/or outside the school property were eligible. We would have classified interventions as partial bans, inside bans, and comprehensive policies. We would have included studies of policies aiming to ban drug or alcohol use in addition to smoking if tobacco use outcomes were reported. We would have considered interventions in which an STP was a component of a smoking prevention program only if it was possible to isolate its effect. Studies that compared stronger and weaker policies were eligible. We would have considered whether the implementation of a policy had an impact on its effect. | 10 | Not applicable | Prevalence of current smokers | |
| Stead and Lancaster | 35 studies | All in high-income countries | The main interventions were education about legal requirements, notification of the results of compliance checks, warning of enforcement, and implementation of enforcement by police or health officials. | 8 | No | ||
| Fichtenberg and Glantz | 9 studies | All in high-income countries | Presence of restrictions on the ability of teens to purchase cigarettes | 7 | Yes | 30-day smoking prevalence, regular smoking prevalence | |
| Incentives | Thomas and Johnston | 7 cRCTs | High-income countries | An incentive was any tangible benefit externally provided with the explicit intention of preventing smoking. This includes contests, competitions, incentive schemes, lotteries, raffles, and contingent payments to reward not starting to smoke. We included rewards to third parties (e.g., to schools, health care providers, or family members), as well as interventions that directly reward children and adolescents. | 9 | Yes | Smoking uptake at longest follow-up |
| Multicomponent interventions | Müller-Riemenschneider et al. | 35 RCTs | All in high-income countries except one in India | A mixture of school-based, community-based and multicomponent interventions | 8 | Yes | Lifetime smoking, 30-day smoking, regular smoking |
| Suls et al. | 14 studies | All in high-income countries | Any smoking cessation interventions | 6 | Yes | Smoking cessation | |
| Stanton and Grimshaw | 28 RCTs | All in high-income countries | Interventions could be specifically designed to meet the needs of young people aged <20 years or could also be applicable to adults. Interventions could range from simple ones such as pharmacotherapy, targeting individual young people, through strategic programs targeting people, or organizations associated with young people (for example, their families or schools), to complex programs targeting the community in which young people study or live. | 9 | Yes | Smoking cessation | |
| Garrison et al. | 6 RCTs | All in high-income countries except one in Singapore | Any intervention targeting adolescent smoking cessation | 7 | No | Smoking cessation | |
| Carson et al. | 2 RCTs | All in high-income countries | Interventions considered in this review aim to prevent tobacco use initiation or progression from experimentation to regular tobacco use in indigenous youth. | 9 | No | Tobacco use | |
| Alcohol use | |||||||
| School-based interventions | Scott-Sheldon et al. | 41 studies | All in high-income countries | Interventions were typically delivered during a single-session lasting less than 1 hour. Most interventions were delivered to individuals, but some were delivered in groups and others used a combination of individual and group sessions. | 8 | Yes | Alcohol consumption and alcohol-related problems |
| Strøm et al. | 28 RCTs | All in high-income countries | Any school-based programs targeting alcohol misuse | 8 | Yes | Alcohol use | |
| Hennessy and Tanner-Smith | 17 RCTs and quasi | All in high-income countries | School-based individual or group-delivered interventions using a range of modalities (motivational enhancement therapy; cognitive behavioral therapy/skills training; cognitive behavioral and motivational enhancement therapy combined; psychoeducational therapy) whereas all the individually delivered interventions used an MET approach. | 7 | Yes | Alcohol use | |
| Foxcroft and Tsertsvadze | 53 RCTs | Mostly in high-income countries except one in India and one in Swaziland | Universal school-based psychosocial or educational prevention program; psychosocial intervention is defined as one that specifically aims to develop psychological and social skills in young people (e.g., peer resistance) so that they are less likely to misuse alcohol; educational intervention is defined as one that specifically aims to raise awareness of the potential dangers of alcohol misuse so that young people are less likely to misuse alcohol; studies that evaluated interventions aiming specifically at preventing and reducing alcohol misuse as well as generic interventions (e.g., drug education programs, healthy school or community initiatives) or other types of interventions (e.g., screening for alcohol consumption) were eligible for inclusion in the review. | 9 | No | Alcohol use | |
| Family-/community-based interventions | Foxcroft and Tsertsvadze | 12 RCTs | Any universal family-based psychosocial or educational prevention program. Psychosocial intervention is defined as one that specifically aims to develop psychological and social attributes and skills in young people (e.g., behavioral norms, peer resistance), via parental socialization and influence, so that young people are less likely to misuse alcohol. Educational intervention is defined as one that specifically aims to raise awareness amongst parents and/or carers of how to positively influence young people or of the potential dangers of alcohol misuse, so that young people are less likely to misuse alcohol. Studies that evaluated interventions aiming specifically at preventing and reducing alcohol misuse as well as generic interventions (e.g., drug education programs) or other types of interventions (e.g., screening for alcohol consumption) were eligible for inclusion in the review. | 9 | No | Alcohol consumption | |
| Digital platforms | Carey et al. | 35 studies | All in high-income countries | The typical intervention was a single-session computerized task delivered via the Internet, intranet, or CD-ROM/DVD lasting a median of 20 minutes. Most CDIs were delivered on-site, whereas some of the students completed the CDI off-site. | 8 | Yes | Alcohol consumption and problems |
| Policy interventions | Siegfried et al. | 2 studies (1 RCT and 3 ITSs) | All in high-income countries | Studies that evaluated the restriction or banning of alcohol advertising via any format including advertising in the press, on the television, radio, or Internet, via billboards, social media, or product placement in films. | 10 | Yes | Alcohol consumption, alcohol sales |
| Multicomponent interventions | Foxcroft and Tsertsvadze | 20 RCTs | All in high-income countries except one in India | Universal multicomponent prevention programs in preventing alcohol misuse in school-aged children up to 18 years. Multicomponent prevention programs are defined as those prevention efforts that deliver interventions in multiple settings, for example, in both school and family settings, typically combining school curricula with a parenting intervention. | 10 | No | Alcohol use |
| Drug use | |||||||
| School-based interventions | Faggiano et al. | 51 RCTs | All in high-income countries | School-based primary prevention interventions, classified in terms of their: | 10 | Yes | Marijuana use, hard drug use, any drug use |
| Porath-Waller et al. | 15 RCTs | All in high-income countries | School-based programs targeting cannabis use among adolescents | 8 | Yes | Cannabis use | |
| Interventions targeting combined substance abuse | |||||||
| School-based interventions | Manoj Sharma et al. | 18 studies | All in high-income countries except one in China | School-based interventions for preventing any substance abuse | 6 | No | Drug use |
| Carney et al. | 6 RCTs | All in high-income countries | Brief interventions (BIs) are targeted, time-limited, low-threshold services that aim to reduce substance use and its associated risks, as well as prevent progression to more severe levels of use and potential negative consequences. | 10 | Yes | Alcohol frequency, alcohol quantity, cannabis dependence, cannabis frequency, other substance abuse related outcomes | |
| Lemstra et al. | 6 RCTs | All in high-income countries | School-based interventions to prevent marijuana and/or alcohol use (defined as at least once per month) in adolescents between the ages of 10 and 15 years old. | 8 | Yes | Knowledge, alcohol use, marijuana use | |
| Fletcher et al. | 4 trials | All in high-income countries | School institutional factors influence young people's use of drugs | 6 | No | ||
| Family-/community-based interventions | Petrie et al. | 20 RCTs | All in high-income countries | “Parenting programs” as any intervention involving parents which was designed to develop parenting skills, improve parent/child communication, or enhance the effects of other interventions, for example, classroom-based programs. We included all types of learning medium, for example, group discussion, distance learning by the Internet or post, video program, individual coaching, and so forth, and any source of delivery, for example, programs provided by health visitors or school nurses, programs run by charities or voluntary organizations, and so forth. Interventions where there was minimal contact with parents (e.g., leaflets only) were not considered to constitute a program and were therefore excluded. | 8 | No | Any substance abuse or intent for substance abuse |
| Digital platforms | Champion et al. | 12 RCTs | All in high-income countries | Seven trials evaluated Internet-based programs and five delivered an intervention via CD-ROM. The interventions targeted alcohol, cannabis, and tobacco. | 8 | No | Alcohol, cannabis, and tobacco use |
| Tait and Christensen | 16 RCTs | All in high-income countries | Web-based interventions | 7 | No | Substance abuse | |
| Haug et al. | 31 studies | All in high-income countries | Internet and mobile phone interventions to decrease alcohol consumption and for smoking cessation in adolescents | 7 | No | Substance abuse | |
| Rodriguez et al. | 8 studies | All in high-income countries | Serious educational games | 7 | No | Knowledge | |
| Individual interventions | Thomas et al. | 4 RCTs | All high-income countries | All mentoring programs whose goal is to deter alcohol and drug use, irrespective of theoretical intervention | 9 | Yes | Alcohol use, substance use, marijuana use |
| Rongione et al. | 20 studies | All high-income countries | The definition of counseling or psychotherapy for substance abuse was any intervention or treatment used to reduce substance use and provided by a mental health professional or professional-in-training. | 7 | No | Substance abuse frequency | |
| Waldron and Turner | 17 studies | All high-income countries | Cognitive behavioral therapy (CBT), family therapy replications, minimal treatment control conditions | 7 | No | Substance abuse frequency | |
| Multicomponent interventions | Skara and Sussman | 25 studies | All high-income countries | Prevention strategies that addressed the issues of social influences to smoke and the development of skills to resist such pressures | 7 | No | Frequency of substance use |
| Vaughn and Howard | 18 studies | All high-income countries | Multidimensional interventions: family-based, psychotherapy, education, behavioral therapy, life skills training | 7 | No | Substance abuse | |
| Carney and Myers | 9 RCTs | All high-income countries | Early interventions that target adolescent substance use as a primary outcome, and criminal or delinquent behaviors as a secondary outcome | 8 | Yes | Aggregate effect estimate | |
| Williams and Chang | 53 studies | Mostly high-income countries | Comprehensive range of treatment (individual counseling, group therapy, medication for comorbid conditions, family therapy, schooling, and recreational programming) | 7 | Yes | Alcohol frequency, binge drinking, marijuana use | |
AMSTAR = assessment of the methodological quality of systematic reviews; CCT = controlled clinical trial; CDI = computer-delivered intervention; cRCT = cluster randomized controlled trial; ITS = interrupted tie series; MD = mean difference; MET = motivational enhancement therapy; RCT = randomized controlled trials; RD = risk difference; STP = school tobacco policies.
Table 2
Summary estimates for substance abuse interventions
| Substance abuse | Interventions | Outcomes and estimates |
|---|---|---|
| Smoking/tobacco use | School-based interventions | |
| Family-/community-based interventions | | |
| Policy interventions | ||
| Incentives | ||
| Multicomponent interventions | | |
| Alcohol use | School-based interventions | |
| Digital platforms | | |
| Policy interventions | | |
| Drug use | School-based interventions | |
| Combined substance abuse | School-based interventions | |
| Mentoring | | |
| Multicomponent intervention | |
Bold indicates significant impact. Italics indicates nonsignificant impact.
CI = confidence interval; RR = relative risk; SMD = standard mean difference.
Interventions for smoking/tobacco use
We report findings from a total of 20 systematic reviews focusing on various interventions for smoking/tobacco use among adolescents. Of these 20 reviews, three reviews focused on school-based interventions; three reviews focused on family-/community-based interventions; four reviews focused on digital platforms; four reviews focused on policy interventions; one review focused on the effect of providing incentives; while five reviews focused on multicomponent interventions for smoking/tobacco use among adolescent age group. The AMSTAR rating for the reviews ranged between 5 and 10 with a median score of 8. Meta-analysis was conducted in nine of the included reviews.
School-based interventions
We report findings from three systematic reviews focusing on school-based interventions for smoking/tobacco use among adolescents [32] , [33] , [34] . A review based on 134 studies evaluated the impact of school smoking interventions for preventing youth from starting smoking [32] and suggested that pure prevention program (where never-smokers at baseline were followed and the number of remaining never-smokers at the various follow-up intervals was ascertained), and combined social competence and social influences curricula have an overall significant effect on reducing smoking initiation (relative risk [RR]: .88; 95% CI: .82–.96 and RR: .49; 95% CI: .28–.87, respectively) while there is no impact of only-information or social influence interventions. Another review evaluated the impact of “Smoke-Free Class Competition” (SFC) [33] . SFC is a school-based smoking prevention program including commitment not to smoke, contract management, and prizes as rewards. Findings from this review suggest that SFC participation is effective in reducing students who are currently smoking (RR: .86; 95% CI: .79–.94). A review specifically focused on long-term follow-up of school-based smoking prevention trials and reported that the interventions varied in intensity, presence of booster sessions, follow-up periods, and attrition rates. This review found very limited evidence on long-term impact of school-based smoking prevention programs [34] .
Family-/community-based interventions
We included three systematic reviews evaluating the impact of family-/community-based interventions for smoking/tobacco use among adolescents [35] , [36] , [37] . Family-based interventions had a positive impact on preventing smoking with a significant reduction in smoking behavior (RR: .76; 95% CI: .68–.84) [35] . Most of these studies used intensive interventions typically addressing family functioning and introduced when children were between 11 and 14 years old. However, these findings should be interpreted cautiously because effect estimates could not include data from all studies. Another review evaluated the impact of coordinated widespread community interventions which support nonsmoking behavior [36] . The interventions included involvement of community leaders for the development and support of community programs, training community workers to form a community coalition of diverse stakeholders to implement and monitor smoking prevention interventions, and involving multiple organizations including the national health service, city councils, social workers, business owners, voluntary organizations, sports organizations, health care providers, community organizations, media, retailers, schools, government, law enforcement, or workplaces. Findings from 25 studies suggest positive impact of community-delivered interventions on reducing smoking rates, intentions to smoke, and increasing knowledge about effects of smoking; however, the evidence is not strong and contains a number of methodological flaws [36] . Evidence from primary care relevant interventions (including coordinated, multicomponent interventions that combine mass media campaigns, price increases, school-based policies and programs, and statewide or community-wide changes in policies and norms) suggests a significant reduction in smoking initiation (RR: .81; 95% CI: .70–.93) among participants in behavior-based prevention interventions with no impact on cessation rates [37] . However, the interventions and measures were reported to be heterogeneous.
Digital platforms
We report findings from four systematic reviews evaluating various digital platforms for smoking/tobacco use among adolescent age group [38] , [39] , [40] , [41] . A review evaluating antitobacco mass media campaigns suggests that these media campaigns can be effective across various racial/ethnic populations for smoking prevention, although the size of the campaign effect may differ by race/ethnicity [39] . Existing evidence supports advertising that includes personal testimonials; surprising narrative; and intense images, sound, and editing while research is insufficient to determine whether advertising with secondhand smoke or social norms theme influences youth tobacco use. Another review evaluated the effectiveness of mass media interventions to prevent smoking in young people in terms of reduced smoking uptake, improved smoking outcomes, attitudes, behaviors, knowledge, self-efficacy, and perception [41] and suggests that mass media can prevent the uptake of smoking in young people; however, the evidence is not strong and contains a number of methodological flaws. The review further suggests that effective media campaigns had a solid theoretical basis, used formative research in designing the campaign messages, and message broadcast was of reasonable intensity over extensive period of time. A review on Web-based smoking cessation interventions among college students suggests mixed results, with insufficient evidence supporting their efficacy [38] . Another review evaluating Internet-based interventions for smoking cessation suggests that Internet-based interventions can assist smoking cessation for a period of 6 months or longer, particularly those which were interactive and tailored to individuals; however, more research is needed to confirm the findings [40] .
Policy level interventions
We found four reviews reporting the impact of smoking/tobacco use policy initiatives [42] , [43] , [44] , [45] . A review evaluating the effect of tobacco advertising and promotion suggests that these policies increase the likelihood of adolescents to start smoking [42] . However, there was variation in the strength of association and the degree to which potential confounders were controlled for. A review evaluated the impact of school policies aiming to prevent smoking initiation [43] and included only one trial. The review suggests no difference in smoking prevalence between intervention and control schools. One review assessed the effect of interventions to reduce underage access to tobacco by deterring shopkeepers from making illegal sales [44] . This review suggests that giving retailer's information is less effective in reducing illegal sales than active enforcement and/or multicomponent educational strategies while there is little effect of intervention on youth perceptions of access to tobacco products or prevalence of youth smoking. Another review evaluated the effectiveness of laws restricting youth access to cigarettes by limiting the ability of teens to purchase cigarette on prevalence of smoking among teens [45] . Findings suggest that there is no detectable relationship between the level of merchant compliance and 30-day or regular smoking prevalence and no significant difference in youth smoking.
We found one review evaluating the impact of incentives (involving any tangible benefit externally provided with the explicit intention of preventing smoking. This includes contests, competitions, incentive schemes, lotteries, raffles, and contingent payments to reward not starting to smoke) to prevent smoking among adolescents [46] . Findings from seven included trials suggest that there is no statistically significant effect of incentives to prevent smoking initiation among children and adolescents (RR: 1.00; 95% CI: .84–1.19). There is lack of robust evidence to suggest that unintended consequences (such as youth making false claims about their smoking status and bullying of smoking students) are consistently associated with such interventions, although this has not been the focus of much research. There was insufficient information to assess the dose–response relationship or costs.
Multicomponent interventions
We found five reviews addressing multicomponent interventions for smoking/tobacco use among adolescents [47] , [48] , [49] , [50] , [51] . One review evaluated the long-term effectiveness of different school-based, community-based, and multisectorial intervention strategies [47] . Although the overall effectiveness of prevention programs showed considerable heterogeneity, the majority of studies report some positive long-term effects for behavioral smoking prevention programs. There was evidence that community-based and multisectoral interventions were effective in reducing smoking rates, while the evidence for school-based programs alone was inconclusive. Another review evaluating any intervention for smoking cessation suggests that any type of intervention is more effective in producing successful smoking cessation compared to no intervention (RR: 1.55; 95% CI: 1.16–2.06) [48] . One review evaluated the effectiveness of strategies that help young people to stop smoking tobacco [49] . Majority of the included studies used some form of motivational enhancement combined with psychological support such as cognitive behavioral therapy (CBT), and some were tailored to stage of change using the transtheoretical model. Transtheoretical model and motivational enhancement interventions have shown moderate long-term success (RR: 1.56; 95% CI: 1.21–2.01) and (RR: 1.60; 95% CI: 1.28–2.01), respectively. However, complex interventions that included CBT did not achieve statistically significant results. A review evaluating interventions targeting smoking cessation among adolescents suggests limited evidence demonstrating efficacy of smoking cessation interventions in adolescents and no evidence on the long-term effectiveness of such interventions [50] . One review specifically evaluated the effectiveness of intervention programs to prevent tobacco use, initiation, or progression to regular smoking amongst young indigenous populations [51] . The review included two studies reporting no difference in weekly smoking at 42-month follow-up.
Interventions for alcohol use
We report findings from a total of eight systematic reviews focusing on various interventions for alcohol use among adolescents. Four reviews focused on school-/college-based interventions while one review each focused on family-/community-based interventions, digital platforms, policy interventions, and multicomponent interventions. The AMSTAR rating ranged between 7 and 10 with a median score of 8.5. Meta-analysis was conducted in five of the included reviews.
We report findings from a total of four reviews focusing on school-/college-based interventions for alcohol use [52] , [53] , [54] , [55] . A review evaluating college-based interventions for alcohol misuse prevention suggests lower quantity and frequency of drinking and fewer problems among the adolescents in the intervention group compared to controls [52] . Findings suggest that college-based interventions that include personalized feedback, moderation strategies, expectancy challenge, identification of risky situations, and goal setting are effective in reducing alcohol-related behavior issues among adolescents. Another review evaluating school-based prevention program showed that, overall, the effects of school-based preventive alcohol interventions on adolescent alcohol use were small but positive among studies reporting the continuous measures, whereas no effect was found among studies reporting the categorical outcomes [53] . School-based brief alcohol interventions (BAIs) among adolescents are associated with significant reduction in alcohol consumption [54] . Subgroup analyses indicated that individually delivered BAIs are effective while there is no evidence that group-delivered BAIs are also associated with reductions in alcohol use. Universal school-based preventive interventions showed some evidence of effectiveness compared to a standard curriculum [55] .
We found one review evaluating the impact of universal family-based prevention programs (including any form of supporting the development of parenting skills including parental support, nurturing behaviors, establishing clear boundaries or rules, and parental monitoring) in preventing alcohol misuse in school-aged adolescents [56] . Most of the trials in the included review have shown some evidence of effectiveness, with persistence of effects over the medium and longer term. The review concluded that the effects of family-based prevention interventions are small but generally consistent and also persistent over the medium to long term.
We found one systematic review reporting the efficacy of computer-delivered interventions (CDIs) to reduce alcohol use among college students [57] . The typical intervention was a single-session computerized task delivered via the Internet, intranet, or CD-ROM/DVD lasting a median of 20 minutes. Most CDIs were delivered on-site, whereas some of students completed the CDI off-site. The effects of CDIs depended on the nature of the comparison condition: CDIs reduced quantity and frequency measures relative to assessment-only controls but rarely differed from comparison conditions that included alcohol-relevant content. Overall, CDIs are found to reduce the quantity and frequency of drinking among college students and are comparable to alternative alcohol-related comparison interventions.
Policy interventions
We found one review that evaluated restriction or banning of alcohol advertising via any format including advertising in the press, on the television, radio, Internet, billboards, social media, or product placement in films [58] . The review found lack of robust evidence for or against recommending the implementation of alcohol advertising restrictions. Advertising restrictions should be implemented within a high-quality, well-monitored research program to ensure the evaluation over time of all relevant outcomes in order to build the evidence base.
We found one review evaluating the effectiveness of universal multicomponent prevention programs in preventing alcohol misuse in school-aged children [59] . Twelve of the 20 trials showed evidence of effectiveness, with persistence of effects ranging from 3 months to 3 years. There is some evidence that multicomponent interventions for alcohol misuse prevention in young people can be effective. However, there is little evidence that interventions with multiple components are more effective than interventions with single component.
Interventions for drug use
We report findings from two systematic reviews focusing on various interventions for drug use among adolescents. Both the reviews focused on school-based interventions. The AMSTAR rating for the reviews ranged between 8 and 10 with a median score of 9. Meta-analysis was conducted in both the included reviews.
We found two reviews evaluating school-based interventions for drug use [60] , [61] . One review evaluated school-based primary prevention interventions including educational approaches (knowledge-focused, social competence–focused, and social norms–focused programs; combined programs; other types of interventions). Findings suggest that both social influence and social competent approach combined favors intervention (RR: .83; 95% CI: .69–.99) for marijuana use at 12+ months with no difference on hard drug use at 12+ months (RR: .86; 95% CI: .39–1.90). Combined interventions are effective in reducing any drug use at <12 months (RR: .76; 95% CI: .64–.89). Overall, school programs based on a combination of social competence and social influence approaches have shown, on average, small but consistent protective effects in preventing drug use. Another review evaluating the impact of school-based programs on cannabis use suggested that school-based programs have a positive impact on reducing students' cannabis use compared to control conditions [61] . Findings revealed that programs incorporating elements of several prevention models were significantly more effective than those were based only on a social influence model. Programs that were longer in duration (≥15 sessions) and facilitated by individuals other than teachers in an interactive manner also yielded stronger effects.
Interventions for combined substance abuse
We report findings from a total of 16 systematic reviews focusing on various interventions for combined substance abuse among adolescents. Of these 16 reviews, four reviews focused on school-based interventions, one review focused on family-/community-based interventions, four reviews focused on digital platforms, three reviews focused on individual-targeted interventions (mentoring and psychotherapy), and four reviews focused on multicomponent interventions. The AMSTAR rating for the reviews ranged between 6 and 10 with a median score of 7. Meta-analysis was conducted in five of the included reviews.
We found four systematic reviews evaluating the impact of school-based interventions targeting substance abuse among adolescents [62] , [63] , [64] , [65] . Interventions that promote a positive school ethos and reduce student disaffection may be an effective complement to drug prevention interventions addressing individual knowledge, skills, and peer norms [65] . One review based on 18 program evaluations suggested mixed and inconclusive evidence to provide any judgment on the effectiveness of school-based programs [62] . Another review evaluating the effectiveness of brief school-based interventions in reducing substance use and other behavioral outcomes among adolescents found moderate quality evidence that, compared to information provision only, brief interventions did not have a significant effect on any of the substance use outcomes at short-, medium-, or long-term follow-up [63] . When compared to assessment-only controls, brief interventions reduced cannabis frequency, alcohol use, alcohol abuse and dependence, and cannabis abuse. Brief interventions also have mixed effects on adolescents' delinquent or problem behaviors, although the effect at long-term follow-up on these outcomes in the assessment-only comparison was significant. School-based marijuana and alcohol prevention programs are found to be effective in preventing marijuana and alcohol use in adolescents between the ages of 10 and 15 years [64] . The most effective primary prevention programs for reducing marijuana and alcohol use among adolescents aged 10–15 years in the long term are comprehensive programs that included antidrug information combined with refusal skills, self-management skills, and social skills training.
We found one review evaluating parenting programs to prevent tobacco, alcohol, or drug abuse in children younger than 18 years [66] . Findings suggest that parenting programs can be effective in reducing or preventing substance use. The most effective intervention appears to be those that shared an emphasis on active parental involvement and on developing skills in social competence, self-regulation, and parenting. However, more work is needed to investigate further the change processes involved in such interventions and their long-term effectiveness.
We report findings from four reviews evaluating digital platforms for substance abuse among adolescents [67] , [68] , [69] , [70] . A review evaluating the impact of Internet-based programs and intervention delivered via CD-ROM targeting alcohol, cannabis, and tobacco suggests that these programs have the potential to reduce alcohol and other drug use as well as intentions to use substances in the future [67] . Web-based interventions for problematic substance use by adolescents and young adults highlighted insufficient data to assess the effectiveness of Web-based interventions for tobacco use by adolescents [68] . For Internet and mobile phone use, one review suggested good empirical evidence concerning the efficacy of Web-based social norms interventions to decrease alcohol consumption in students [69] . Internet interventions for smoking prevention are found to be heterogeneous. Interventions using mobile phone text messaging for smoking cessation are found to be well accepted and promising; however, they are primarily tested within pilot studies, and conclusions about their efficacy are not possible so far. One review evaluated the impact of serious educational games targeting tobacco, alcohol, cannabis, methamphetamine, ecstasy, inhalants, cocaine, and opioids and reported very limited evidence to suggest benefit [70] .
Individual-targeted interventions
We report findings from three systematic reviews evaluating individual-targeted interventions for substance abuse among adolescents; these included mentoring [71] , counseling, or psychotherapy [72] , [73] . Review evaluating mentoring suggested limited evidence to conclude that the intervention was effective [71] . The review evaluating counseling and psychotherapy to treat alcohol and other drug use problems in school-aged youth suggested that the effects of counseling and psychotherapy for drug abuse are consistently significant at termination, but follow-up effects yielded inconsistent results [72] . A review evaluating CBT, family therapy replication, and minimal treatment control conditions suggested the need for more data since none of the treatment approaches appeared to be clearly superior to any others in terms of treatment effectiveness for adolescent substance abuse [73] .
Multicomponent intervention
We report findings from four systematic reviews evaluating multicomponent interventions for substance abuse among adolescents [74] , [75] , [76] , [77] . One review suggested that there is some empirical evidence of the effectiveness of social influences programs in preventing or reducing substance use for up to 15 years after completion of programming. However, this conclusion is prone to great variability in the level of internal and external validity across all studies [74] . Another review suggested that multidimensional family therapy and cognitive behavioral group treatment received the highest level of evidentiary support [75] . Early interventions for adolescent substance use do hold benefits for reducing substance use and associated behavioral outcomes if delivered in an individual format and over multiple sessions [76] . One review found relatively few studies on the adolescent substance abuse treatment and suggested that there is evidence that treatment is superior to no treatment but insufficient evidence to compare the effectiveness of treatment types [77] .
We included 46 systematic reviews focusing on interventions for smoking/tobacco use, alcohol use, drug use, and combined substance abuse. Our overview findings suggest that among smoking/tobacco use interventions, school-based pure prevention programs and SFC are effective in reducing smoking initiation and current smoking. However, there is lack of long-term follow-up for the impact of school-based smoking/tobacco use programs. Family-based intensive interventions typically addressing family functioning are also found to effectively prevent smoking. Coordinated widespread community-based interventions have also shown positive impacts on smoking behaviors. Mass media campaigns involving solid theoretical basis, formative research in designing the campaign messages, and message broadcast have shown positive impacts on uptake of smoking given that these were of reasonable intensity over extensive periods of time. Evidence from Internet-based interventions, policy initiatives, and incentives appears to be mixed and needs further research.
Among interventions for alcohol use, school-based alcohol prevention interventions including personalized feedback, moderation strategies, expectancy challenge, identification of risky situations, goal setting, and BAIs have been associated with reduced frequency of drinking. Family-based interventions have a small but persistent effect on alcohol misuse among adolescents while CDIs for alcohol are found to reduce the quantity and frequency of drinking among college students. There is lack of robust evidence for or against recommending the implementation of alcohol advertising restrictions and multiple component interventions. For drug use, school-based interventions based on a combination of social competence and social influence approaches have shown protective effects in preventing drugs and cannabis use. Among the interventions targeting combined substance abuse, school-based primary prevention programs that include antidrug information combined with refusal skills, self-management skills, and social skills training are effective in reducing marijuana and alcohol use among adolescents. There is very limited evidence on the effectiveness of mass media and mentoring for combined substance abuse.
We adopted an overview of reviews approach for synthesizing existing evidence on adolescent substance abuse. Although an overview of systematic reviews builds on the conclusions of rigorous reviews of studies in different settings and of varying quality, avoids duplication of work and allows for a much faster review, there are some potential limitations. The interventions on which primary data exist, but which have not been covered by a systematic review, will not have been included. Furthermore, an overview of systematic reviews relies on review authors' characterizations of the findings rather than on individual studies and therefore may be affected by selective reporting biases. It also misses upon studies not taken up by included reviews. However, we have quality rated the existing reviews for transparency.
Our review findings highlight that school-based delivery platforms are the most highly evaluated platforms for targeting adolescents for substance abuse. Most of the existing evidence for substance abuse interventions comes from HICs. There is lack of data to determine the differential effects of interventions by gender, socioeconomic status, and population density. Meta-analysis could not be conducted in most of the included reviews since the interventions varied in intensity, follow-up periods, and reported outcomes. Furthermore, in reviews where meta-analysis was conducted, not all the data contributed to the pooled effect estimate. There is lack of rigorous data evaluating the sustainability and long-term effectiveness of substance abuse programs targeting adolescents. Future research should focus on evaluating the effectiveness of specific intervention components with standardized intervention and outcome measures. There is a need to evaluate relative effectiveness and cost-effectiveness of various delivery platforms targeting adolescents for substance abuse interventions. Various delivery platforms, including digital platforms and policy initiative, have the potential to improve substance abuse outcomes among adolescents; however, these require further research. Future trials should focus on reporting separate data for gender and socioeconomic subgroups since the impact of such behavior change interventions might vary among various population subgroups. Lastly, there is a dire need for rigorous, higher quality evidence especially from low- and middle-income countries on effective interventions to prevent and manage substance abuse among adolescents.
Acknowledgments
All authors contributed to finalize the manuscript.
Conflicts of Interest: The authors do not have any financial or nonfinancial competing interests for this review.
Disclaimer: Publication of this article was supported by the Bill and Melinda Gates Foundation. The opinions or views expressed in this supplement are those of the authors and do not necessarily represent the official position of the funder.
Funding Sources
The preparation and publication of these papers was made possible through an unrestricted grant from the Bill & Melinda Gates Foundation (BMGF).
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Marijuana Abuse and Addiction: Know the Signs
- Signs and Symptoms
- Who Is At Risk?
Frequently Asked Questions
Marijuana comes from the Cannabis sativa or Cannabis indica plant. It’s often made from the dried leaves and flowers of the plant and even the seeds and stems. It contains a chemical called THC, which is a psychoactive chemical.
While many people use marijuana (it's the third most commonly used addictive drug, after tobacco and alcohol) most won't become addicted. About 1 in 10 people who use marijuana will become addicted; when they start using before the age of 18, the number increases to 1 in 6.
Verywell / Danie Drankwalter
Research suggests that about 30% of people who use marijuana might have marijuana use disorder, the severity of which can vary.
Cannabis use disorder is widely defined as problematic use of cannabis that results in significant distress or impairment with at least two issues within a 12-month period, like the substance use results in not being able to meet work, social, or familial obligations, or the substance use continues even after it's affected or caused interpersonal issues.
Signs and Symptoms of Marijuana Abuse and Addiction
When someone you love is abusing marijuana or addicted to it, there are often signs and symptoms to look for. Knowing what these are can help you approach your loved one in a caring way.
Marijuana Abuse
Substance abuse occurs when an individual regularly uses drugs or alcohol and experiences negative consequences as a result. This can include missing work or school, getting in trouble with the law or school authorities, or putting oneself in dangerous situations.
Signs of marijuana abuse can include:
- Tolerance, which means using more of the drug to get the desired effects
- Craving the substance
- Abandoning social or occupational activities because of the drug use
- Repeatedly trying to cut back or stop using, to no avail
- Spending a lot of time searching for, using, or recovering from drug use
- Engaging in high-risk behaviors while under the influence
- Withdrawal symptoms when cannabis use is discontinued
These signs, along with any negative consequences from marijuana use, may signal a drug abuse problem.
Marijuana Addiction
Addiction refers to the compulsive use of substances driven by strong physical and psychological urges.
Signs of Addiction
Signs of addiction can include:
- Tolerance to the drug and using more of it
- Withdrawal symptoms occur if less is used or if you stop using it
- Withdraw from social activities
- Continued use despite awareness of all of the problems associated with the drug use
Withdrawal Symptoms
Cannabis withdrawal syndrome is now found in the " Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition" (DSM-5) . It's characterized by the presence of at least three of these symptoms and develops within seven days of reduced marijuana use:
- Irritability, anger, or aggression
- Nervousness or anxiety
- Sleep disruptions
- Changes in appetite or weight
- Restlessness
- Depressed mood
- Somatic symptoms: headache , nausea , sweating
Who Is At Risk for Marijuana Abuse?
Although anyone who uses marijuana has the potential to abuse it, there are risk factors that can make marijuana abuse more likely. Having these risk factors doesn't mean you definitely will develop a substance abuse problem, but you may be more at risk.
Risk Factors for Substance Abuse
There are various risk factors that can increase your risk of developing a substance abuse problem. These can include:
- Family history of addiction
- Family history of mental illness
- Lack of parental involvement
- Personal mental illness, including depression and anxiety
- Learning disorders
Protective factors can help people avoid substance use disorders. Things like extended family support, language-based discipline from parents, and a supportive peer group can help counteract some risk factors.
Marijuana Abuse in Teens
Teens naturally take risks and push the envelope. Many teens will try illicit substances.
The teenage brain is immature and still developing. If marijuana is abused during these years, it can interfere with brain development. Side effects can include:
- Trouble thinking and concentrating
- Memory, learning, and attention problems
- Increased risk of mental health issues
- Increased risk of addiction
What Are Signs My Teen Is Marijuana?
Signs of marijuana use can include:
- Smelling like pot
- Bloodshot eyes
- Mood swings
- Laziness and tiredness
- Marijuana accessories like bongs or pipes
Marijuana Abuse in Pregnancy
Marijuana is the most commonly used illegal drug during pregnancy.
According to the American Academy of Pediatrics, there's no safe amount of marijuana during pregnancy or breastfeeding. In addition to THC, there are almost 500 chemicals in marijuana.
These chemicals can cross the placenta and affect the fetus. Many studies have been done on the effects of marijuana abuse during pregnancy, and results are conflicting, possibly because of other substances used and/or abused during pregnancy, including tobacco.
There are studies of children whose mothers used marijuana when pregnant with them. These children were found to have decreased verbal reasoning skills and more hyperactivity, impulsivity, and decreased attention.
However, there may be other reasons for these findings and more research is necessary.
Treatment for Marijuana Abuse
There's treatment for marijuana abuse. If you think you might have a problem, there's help out there.
Talk Therapy
Cognitive behavioral therapy (CBT) , motivational enhancement therapy (MET), and contingency management (CM) have all been used in treating cannabis use disorder, and it was found that a combination of all three might be most effective.
CBT helps people identify why they use, develop relapse prevention and coping skills, and come up with more effective behaviors.
MET is based on motivational interviewing and helps to increase changes in behavior by giving nonjudgmental feedback and helping people set goals.
CM uses operant conditioning with a target behavior; this means that the desired behavior is rewarded and reinforced to increase the likelihood of it occurring again.
Support Groups
Support groups may be another option for treatment. Finding others who are dealing with the same issues as you can be validating, and you can learn from one another about different ways to cope. Marijuana Anonymous is one such support group based on the principles of Alcoholics Anonymous.
Motivational Incentives
Motivational incentives are part of CM, since it uses operant conditioning on positive behaviors you want to increase. The incentives are most effective when there are plenty of opportunities to get reinforcement. The reinforcement immediately follows the behavior, and the value of the motivator is significant to the person.
Medication for Underlying Conditions
Cannabis use disorder is significantly higher in those with mental illness than in the general population.
Cannabis use disorder is higher in those who have:
- Schizophrenia
- Mood and anxiety disorders
- Personality disorders
- Post-traumatic stress disorder (PTSD)
Accurate diagnosis of mental health disorders and appropriate treatment, including medication, may help to reduce attempts to self-medicate with marijuana.
Coping With Marijuana Abuse
It can be hard when you’re living with marijuana abuse or watching someone you care about deal with it. You don’t have to manage it alone. Talk with your healthcare professional. They can help identify treatment options that are appropriate for your situation and provide resources for family and friends.
Other things you can do to help cope with abuse or addiction include:
- Seek counseling with a licensed counselor.
- Attend a support group.
- Keep your schedule busy with other sober individuals so you're not tempted to use.
- Adopt stress-relieving activities like exercise , yoga, or other things that help relax you.
With the ongoing legalization of marijuana in the United States and around the world, it can be hard to say how this will impact marijuana use and abuse. More research needs to be done on potential treatments for marijuana abuse and how to increase support and accessibility for existing treatments.
Marijuana Use
Many people can use marijuana safely without becoming addicted or abusing it. But like any mind-altering substance, there's always a chance that it can become problematic. This is nothing to be ashamed about. There is effective treatment available for you.
Preventing Marijuana Use and Addiction
Many people think marijuana use is harmless, especially because it’s a natural product. While many people are able to use it without becoming addicted or abusing it, it's not a benign substance. Even though you may not be able to prevent marijuana abuse and addiction, there are things you can do to reduce the risk.
Tips for Reducing Addiction Risk
- Increase family support and supervision.
- Discuss the risks and side effects of drugs, including marijuana.
- Encourage open conversations about substances and risks.
- Model healthy behavior.
- Implement prevention programs in schools and communities.
Although marijuana is becoming legal in more states, there's still the potential for abuse and addiction. Using more to get the same effect, giving up once-loved activities in order to use, and withdrawal symptoms like irritability, mood changes, and disruptions to sleep and/or appetite can all signal that someone might be experiencing marijuana abuse.
There are multiple treatments available, like talk therapy, support groups, and even medication when necessary for underlying issues. Recovery is possible.
A Word From VeryWell
Many people use marijuana at one point or another. However, if the use is becoming a need or you're experiencing negative consequences because of it, it may be a problem. If you or someone you love may be experiencing marijuana abuse or addiction, talk with a trusted healthcare professional. They will work with you to get properly evaluated and the appropriate treatment.
Drug abuse and addiction can be scary and uncertain, but it's treatable, and there's help out there. There are a variety of treatments available, and if one doesn’t work, another one may be better for you.
It can be. Marijuana use can lead to dependence if a person has withdrawal symptoms when they stop using it.
Addiction is when the person has to use it even after it negatively affects their life. It's hard to get accurate numbers because many studies conflate dependence and addiction. Still, those studies report about 9% of marijuana users will become dependent, and 17% if they start as a teenager.
More research needs to be done, but it might be a gateway drug for some people more at risk than others.
National Institutes of Health. What is marijuana?
Substance Abuse and Mental Health Administration. Know the risks of marijuana.
National Institute on Drug Abuse. Is marijuana addictive?
Johns Hopkins Medicine. Substance abuse/chemical dependency.
Bahji A, Stephenson C, Tyo R, et al. Prevalence of cannabis withdrawal symptoms among people with regular or dependent use of cannabinoids. JAMA Netw Open. 2020;3(4):e202370. doi: 10.1001/jamanetworkopen.2020.2370
Youth.Gov. Risk and protective factors.
Centers for Disease Control and Prevention. What you need to know about marijuana use in teens.
American Addiction Centers. Signs of marijuana use in teens: how to tell if your child is high.
Ryan SA, Ammerman SD, O'Connor ME, et al. Marijuana use during pregnancy and breastfeeding: Implications for neonatal and childhood outcomes . Pediatrics . 2018;142(3):e20181889. doi:10.1542/peds.2018-1889
Substance Abuse and Mental Health Services Administration. Marijuana and pregnancy.
Stickrath E. Marijuana use in pregnancy: An updated look at marijuana use and its impact on pregnancy. Clinical Obstetrics and Gynecology . 2019;62(1):185-190. doi:10.1097/GRF.0000000000000415
Sherman BJ, McRae-Clark AL. Treatment of cannabis use disorder: current science and future outlook. Pharmacotherapy. 2016;36(5):511-535. doi:10.1002/phar.1747
Marijuana Anonymous.
Lowe DJE, Sasiadek JD, Coles AS, George TP. Cannabis and mental illness: a review . Eur Arch Psychiatry Clin Neurosci . 2019;269(1):107-120. doi:10.1007/s00406-018-0970-7
Williams AR. Cannabis as a gateway drug for opioid use disorder. J Law Med Ethics. 2020;48(2):268-274. doi:10.1177/1073110520935338
By Jaime R. Herndon, MS, MPH Herndon is a freelance health/medical writer with a graduate certificate in science writing from Johns Hopkins University.

IMAGES
COMMENTS
Drug abuse is detrimental, and excessive drug usage is a worldwide problem. Drug usage typically begins during adolescence. Factors for drug abuse include a variety of protective and risk factors. Hence, this systematic review aimed to determine the risk ...
Teenage drug addiction has prevailed in society, making it a growing problem. The essay presents the issues of substance abuse among adolescents.
Abstract. Adolescence is a crucial time for biological, psychological, and social development. It is also a time when substance addiction and its adverse effects are more likely to occur. Adolescents are particularly susceptible to the negative long-term effects of substance use, including mental health illnesses, sub-par academic performance ...
Adolescent substance-related attitudes and use patterns have evolved over time, informed by adult and peer behaviors, public policy, media messaging, substance availability, and other variables. A number of risk and resiliency factors contribute to individual differences in substance use and related consequences.
This study aimed to describe the adverse effects that adolescent substance abuse has on the levels of care giving and well-being of families. The researchers used a qualitative case study design wh...
Aside from vaping, adolescent use of illicit substances has dropped substantially over the past few decades, but more teens are overdosing than ever—largely because of contamination of the drug supply with fentanyl, as well as the availability of stronger substances ( Most reported substance use among adolescents held steady in 2022, National ...
Substance abuse among adolescents is the problem that requires the joint effort of parents, teachers, and social workers. It can affect families that have various social, racial, or economic characteristics and no one can say that he or she is insured against this risk. This paper is aimed at discussing the factors that contribute to substance ...
Second, family dynamics, parental education, socioeconomic status, parental approval of substance use, and experiences of physical and sexual abuse can influence adolescent substance use.
In conclusion, this essay explored the issue of teenage drug abuse in the United States through the aspects of core reasons and consequences. Based on the collected information, teenagers are more subjected to drug abuse due to their social interactions and the high risk of depression tendencies. The increased parental participation in ...
Drug abuse is defined as the use of mood modifying substance in dosage many times in excess of those used medically and over lengths of time impacting negatively on individuals, society and family.
Adolescent youth experience emotional, social, and psychological changes in their growth and during the ages from 12 to 18 years old it is common to experiment with illicit substances, but most teens do not realize what experimenting with drugs can lead to. Some teens will experiment with drugs and stop, or continue to use occasionally, without ...
Learn how to prevent teen drug abuse and help your teen cope with the challenges of adolescence. Mayo Clinic offers expert advice and resources for parents.
Teenage drug abuse exerts a profound psychological toll, impacting mental health, emotional stability, and overall quality of life. The co-occurrence of substance abuse and mental health disorders is a well-established phenomenon. Adolescents who abuse drugs are at a heightened risk of experiencing mental health challenges such as depression ...
Many teens have a problem with substance abuse, such as alcohol, marijuana, and prescription drugs. Learn the warning signs and what puts teens at risk.
Identifying and understanding the associations between adolescent substance use and changes in cognition, mental health, and future substance use risk may assist our understanding of the consequences of drug exposure during this critical window. Keywords: adolescence, youth, addiction, drug, abuse psychology, special population.
The first and most apparent impact of drugs on youth is the physical damage. Substance abuse can lead to a host of health problems, ranging from liver damage, cardiovascular diseases, to neurological issues. Furthermore, drugs can interfere with the normal growth and development processes, particularly during the critical adolescent years when ...
Why is adolescence a critical time for preventing drug addiction? As noted previously, early use of drugs increases a person's chances of becoming addicted. Remember, drugs change the brain—and this can lead to addiction and other serious problems. So, preventing early use of drugs or alcohol may go a long way in reducing these risks.
Adolescent Drug Abuse According to Nawi et al. (2021), in 2016, 5.6% of the world's population of age range fifteen to sixty-five at least utilized drugs. Drugs are supplements for good health if used in reasonable quantities while following qualified doctors' guidelines. However, there are instances that drug use is bizarre. The bizarre drug use is known as drug abuse and is high among ...
Background Drug abuse is detrimental, and excessive drug usage is a worldwide problem. Drug usage typically begins during adolescence. Factors for drug abuse include a variety of protective and risk factors. Hence, this systematic review aimed to determine the risk and protective factors of drug abuse among adolescents worldwide. Methods Preferred Reporting Items for Systematic Reviews and ...
1613 Words. 7 Pages. 7 Works Cited. Open Document. It has been discovered that most people who struggle with drug addiction began experimenting with drugs in their teens. Teenage drug abuse is one of the largest problems in society today and the problem grows and larger every year. Drugs are a pervasive force in our culture today.
The developing adolescent brain is especially vulnerable to addiction and the damaging effects of substance abuse. According to the National Institute on Drug Abuse in 2023, "10.9% of eighth graders, 19.8% of 10th graders, and 31.2% of 12th graders report any illicit drug use in the past year" [1] .
Adolescents are significant long-term contributors to the crisis due to their susceptibilities to drug abuse and impressionable age. This review examines the particular vulnerabilities of the adolescent brain to drug abuse and the risk and protective factors thereof, especially in light of the Rat Park studies.
Teenage Drug Abuse. There is a major concern about the teenage drug use today. Within the ages 15 through 24, fifty percent of deaths (from homicides, accidents, suicides) involve drugs. The two common reasons why teens use drugs are anxiety and depression. Factors like peer pressure, desire to escape, curiosity, emotional struggles, and stress ...
At the behest of the district's mayor, DuPont developed a D.C.-based clinic, the Narcotics Treatment Administration. It treated more than 15,000 heroin addicts over the next three years, and the D ...
You may also be able to spot a loved one's substance abuse through the new or increased presence of drug paraphernalia. Paper wraps, small pieces of cling film, and tiny plastic bags are used to store drugs. Rolling papers, pipes, bongs, or pierced plastic bottles or cans are often used to smoke drugs.
Risk of drug abuse also increases greatly during times of transition, such as changing schools, moving, or divorce. The challenge for parents is to distinguish between the normal, often volatile, ups and downs of the teen years and the red flags of substance abuse. These include:
We conducted an overview of systematic reviews to evaluate the effectiveness of interventions to prevent substance abuse among adolescents. We report findings from a total of 46 systematic reviews focusing on interventions for smoking/tobacco use, alcohol use, drug use, and combined substance abuse.
Marijuana Abuse in Teens . Teens naturally take risks and push the envelope. Many teens will try illicit substances. The teenage brain is immature and still developing. If marijuana is abused during these years, it can interfere with brain development. ... Substance Abuse and Mental Health Services Administration. Marijuana and pregnancy.