Advertisement

Trends in insomnia research for the next decade: a narrative review
- Review Article
- Published: 06 April 2020
- Volume 18 , pages 199–207, ( 2020 )
Cite this article

- Daniel Ruivo Marques 1 , 2 ,
- Ana Allen Gomes 2 , 3 ,
- Vanda Clemente 2 , 4 ,
- José Moutinho dos Santos 4 ,
- Joana Serra 4 &
- Maria Helena Pinto de Azevedo 5
707 Accesses
11 Citations
Explore all metrics
Insomnia disorder has known striking developments over the last few years. Partly due to advances in neuroimaging techniques and brain sciences, our understanding of insomnia disorder has become more fine-tuned. Besides, developments within psychological and psychiatric fields have contributed to improve conceptualization, assessment, and treatment of insomnia. In this paper, we present a list of promising 10 key “hot-topics” that we think in the next 10 years will continue to stimulate researchers in insomnia’s domain: increasing of systematic reviews and meta-analyses; improvement of existing self-report measures; increasing of genetic and epigenetic investigation; research on new pharmacological agents; advances in neuroimaging studies and methods; new psychological clinical approaches; effectiveness studies of e-treatments and greater dissemination of evidence-based therapies for insomnia; call for integrative models; network approach using in insomnia; and assessment of insomnia phenotypes. The breadth of all these topics demands the collaboration of researchers from different scientific fields within sleep medicine. In summarizing, in the next decade, it is predictable that insomnia’s research still benefit from different scientific disciplines.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
Pain-Insomnia-Depression Syndrome: Triangular Relationships, Pathobiological Correlations, Current Treatment Modalities, and Future Direction

Genome-wide analysis of insomnia in 1,331,010 individuals identifies new risk loci and functional pathways
American Academy of Sleep Medicine. International classification of sleep disorders: diagnostic and coding manual. 3rd ed. Westchester: American Academy of Sleep Medicine; 2014.
Google Scholar
American Psychiatric Association. Diagnostic and statistical manual of mental disorders-5. 5th ed. Washington, DC: American Psychiatric Association; 2013.
Book Google Scholar
Baglioni C, Regen W, Teghen A, Spiegelhalder K, Feige B, Nissen C, Riemann D. Sleep changes in the disorder of insomnia: a meta-analysis of polysomnographic studies. Sleep Med Rev. 2014;18(3):195–21313. https://doi.org/10.1016/j.smrv.2013.04.001 .
Article PubMed Google Scholar
Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. https://doi.org/10.1016/S1389-9457(00)00065-4 .
Berman M, Jonides J, Nee D. Studying mind and brain with fMRI. Soc Cogn Affect Neurosci. 2006;1(2):158–61. https://doi.org/10.1093/scan/nsl019 .
Article PubMed PubMed Central Google Scholar
Bheemsain T, Kar S. An overview of insomnia management. Delphi Psychiatry J. 2012;15(2):294–301.
Blanken T, Benjamins J, Borsboom D, Vermunt J, Paquola C, Ramautar J, Van Someren E. Insomnia disorder subtypes derived from life history and traits of affect and personality. Lancet Psychiatry. 2019;6(2):151–63. https://doi.org/10.1016/S2215-0366(18)30464-4 .
Borsboom D, Cramer A. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. 2013;9(1):91–121. https://doi.org/10.1146/annurev-clinpsy-050212-185608 .
Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16(1):5–13. https://doi.org/10.1002/wps.20375 .
Bragantini D, Sivertsen B, Gehrman P, Lydersen S, Güzey IC. Genetic polymorphisms associated with sleep-related phenotypes; relationships with individual nocturnal symptoms of insomnia in the HUNT study. BMC Med Genet. 2019;20(1):179. https://doi.org/10.1186/s12881-019-0916 .
Broomfield N, Espie C. Towards a valid, reliable measure of sleep effort. J Sleep Res. 2005;14(4):401–7. https://doi.org/10.1111/j.1365-2869.2005.00481.x .
Busto U, Sykora K, Sellers E. A clinical scale to assess benzodiazepine withdrawal. J Clin Psychopharmacol. 1989;9(6):412–6. https://doi.org/10.1097/00004714-198912000-00005 .
Article CAS PubMed Google Scholar
Buysse D, Ancoli-Israel S, Edinger J, Lichstein K, Morin C. Recommendations for a standard research assessment of insomnia. Sleep. 2006;29(9):1155–73. https://doi.org/10.1093/sleep/29.9.1155 .
Buysse D, Germain A, Hall M, Monk T, Nofzinger E. A neurobiological model of insomnia. Drug Discov Today Dis Models. 2011;8(4):129–37. https://doi.org/10.1016/j.ddmod.2011.07.002 .
Buysse D, Harvey A. Insomnia: recent developments and future directions. In: Kryger M, Roth T, Dement W, editors. Principles and practices of sleep medicine. 6th ed. Philadelphia: Elsevier; 2017. p. 757–760.
Chapter Google Scholar
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–21313. https://doi.org/10.1016/0165-1781(89)90047-4 .
Cassano GB, Petracca A, Cesana BM. A new scale for the evaluation of benzodiazepine withdrawal symptoms: sessb. Curr Therapeutic Res. 1994;55(3):275–89. https://doi.org/10.1016/s0011-393x(05)80171-7 .
Article Google Scholar
Dekker K, Blanken T, Van Someren E. Insomnia and personality: a network approach. Brain Sci. 2017;7(3):28. https://doi.org/10.3390/brainsci7030028 .
Article PubMed Central Google Scholar
Edinger J, Leggett M, Carney C, Manber R. Psychological and behavioral treatments for insomnia II: implementation and specific populations. In: Kryger M, Roth T, Dement W, editors. Principles and practices of sleep medicine. 6th ed. Philadelphia: Elsevier; 2017. p. 814–831.
Eisai Global. U.S. FDA approves Eisai’s Dayvigo TM (Lemborexant) for treatment of insomnia in adult patients. 2019. https://www.eisai.com/news/2019/news201993.html . Accessed 31 Jan 2020.
Espie C, Kyle S, Williams C, Ong J, Douglas N, Hames P, Brown J. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep. 2012;35(6):769–81. https://doi.org/10.5665/sleep.1872 .
Fernandez-Mendoza J. The insomnia with short sleep duration phenotype: an update on it’s importance for health and prevention. Curr Opin Psychiatry. 2017;30(1):56–63. https://doi.org/10.1097/YCO.0000000000000292 .
Field A, Gillett R. How to do a meta-analysis. Br J Math Stat Psychol. 2010;63:665–94. https://doi.org/10.1348/000711010X502733 .
Gehrman P, Pfeiffenberger C, Byrne E. The role of genes in the insomnia phenotype. Sleep Med Clin. 2013;8(3):323–31. https://doi.org/10.1016/j.jsmc.2013.04.005 .
Gilbert P. The origins and nature of compassion focused therapy. Br J Clin Psychol. 2014;53(1):6–41. https://doi.org/10.1111/bjc.12043 .
Gregory AM, Rijsdijk FV, Eley TC, Buysse DJ, Schneider MN, Parsons M, Barclay NL. A longitudinal twin and sibling study of associations between insomnia and depression symptoms in young adults. Sleep. 2016;39(11):1985–92. https://doi.org/10.5665/sleep.6228 .
Hadian S, Jabalameli S. The effectiveness of compassion-focused therapy (CFT) on rumination in students with sleep disorders: a quasi-experimental research, before and after. J Urmia Univ Med Sci. 2019;30(2):86–96.
Hein M, Lanquart J-P, Loas G, Hubain P, Linkowski P. Similar polysomnographic pattern in primary insomnia and major depression with objective insomnia: a sign of common pathophysiology?. BMC Psychiatry. 2017. https://doi.org/10.1186/s12888-017-1438-4
Hertenstein E, Feige B, Gmeiner T, Kienzler C, Spiegelhalder K, Johann A, Baglioni C. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med Rev. 2019;43:96–105. https://doi.org/10.1016/j.smrv.2018.10.006 .
Jansen P, Watanabe K, Stringer S, Skene N, Bryois J, Posthuma D. Genome-wide analysis of insomnia in 1,331,010 individuals identifies new risk loci and functional pathways. Nat Genet. 2019;51:394–403. https://doi.org/10.1038/s41588-018-0333-3 .
Jones S, van Hees V, Mazzotti D, Marques-Vidal P, Sabia S, van der Spek A, Wood A. Genetic studies of accelerometer-based sleep measures in 85,670 individuals yield new insights into human sleep behaviour. Nat Commun. 2018;10(1):1585. https://doi.org/10.1038/s41467-019-09576-1 .
Article CAS Google Scholar
Kobayashi M, Okajima I, Narisawa H, Kikuchi T, Matsui K, Inada K, Inoue Y. Development of a new benzodiazepine hypnotics withdrawal symptom scale. Sleep Biol Rhythm. 2018;16(3):263–71. https://doi.org/10.1007/s41105-018-0151-0 .
Lane J, Jones S, Dashti H, Wood A, Aragam K, Saxena R. Biological and clinical insights from genetics of insomnia symptoms. Nat Genet. 2019;51:387–93. https://doi.org/10.1038/s41588-019-0361-7 .
Article CAS PubMed PubMed Central Google Scholar
Lilenfeld S. What is “evidence” in psychotherapies? World Psychiatry. 2019;18(3):245–6. https://doi.org/10.1002/wps.20654 .
Lind MJ, Gehrman PR. Genetic pathways to insomnia. Brain Sci. 2016;6(4):64. https://doi.org/10.3390/brainsci6040064 .
Article CAS PubMed Central Google Scholar
Ma Z-R, Shi L-J, Deng M-H. Efficacy of cognitive behavioral therapy in children and adolescents with insomnia: a systematic review and meta-analysis. Braz J Med Biol Res. 2018;51(6):e7070. https://doi.org/10.1590/1414-431X20187070 .
Marques D. Do we need neuroimaging to treat insomnia effectively? Sleep Med. 2019;53:205. https://doi.org/10.1016/j.sleep.2017.08.005 .
Marques D. “Time to relax”: considerations on relaxation training for insomnia disorder. Sleep Biol Rhythm. 2019;17(2):263–4. https://doi.org/10.1007/s41105-018-00203-y .
Marques D. Self-report measures as complementary exams in the diagnosis of insomnia. Revista Portuguesa de Investigação Comportamental e Social. 2020. [Accepted for publication] .
Marques D, Azevedo MH. Potentialities of network analysis for sleep medicine. J Psychosom Res. 2018;111:89–90. https://doi.org/10.1016/j.jpsychores.2018.05.019 .
Marques D, Clemente V, Gomes A, Azevedo MH. Profiling insomnia using subjective measures: where are we and where are we going. Sleep Med. 2018;43:103–4. https://doi.org/10.1016/j.sleep.2017.12.006 .
Marques D, Gomes A, Azevedo MH. Utility of studies in community-based populations. 2019. [Manuscript submitted for publication] .
Marques D, Gomes A, Caetano G, Castelo-Branco M. Insomnia disorder and brain’s default-mode network. Curr Neurol Neurosci Rep. 2018;18(8):45. https://doi.org/10.1007/s11910-018-0861-3 .
Marques D, Gomes A, Clemente V, Santos J, Castelo-Branco M. Default-mode network activity and its role in comprehension and management of psychophysiological insomnia: a new perspective. New Ideas Psychol. 2015;36:30–7. https://doi.org/10.1016/j.newideapsych.2014.08.001 .
Marques D, Gomes A, Clemente V, Santos J, Duarte I, Caetano G, Castelo-Branco M. Unbalanced resting-state networks activity in psychophysiological insomnia. Sleep Biol Rhythm. 2017;15(2):167–77. https://doi.org/10.1007/s41105-017-0096-8 .
Marques D, Gomes AA, Clemente V, Moutinho J, Caetano G, Castelo-Branco M. An overview regarding insomnia disorder: conceptualization, assessment and treatment. In: Columbus AM, editor. Advances in psychology research. New York: Nova Science Publishers Inc; 2016. p. 81–116.
Marques D, Gomes A, Clemente V, Santos J, Caetano G, Castelo-Branco M. Neurobiological correlates of psychological treatments for insomnia: a review. Eur Psychol. 2016;21(3):195–205. https://doi.org/10.1027/1016-9040/a000264 .
McNally R. Can network analysis transform psychopathology? Behav Res Ther. 2016;86:95–104. https://doi.org/10.1016/j.brat.2016.06.006 .
Morales-Lara D, De-la-Peña C, Murillo-Rodríguez E. Dad’s snoring may have left molecular scars in your DNA: the emerging role of epigenetics in sleep disorders. Mol Neurobiol. 2018;55(4):2713–24. https://doi.org/10.1007/s12035-017-0409-6 .
Morin C. Contributions of cognitive-behavioral approaches to the clinical management of insomnia. Prim Care Companion J Clin Psychiatry. 2002;4(1):21–6.
Morin C, Vallières A, Ivers H. Dysfunctional Beliefs and Attitudes about Sleep (DBAS): validation of a brief version (DBAS-16). Sleep. 2007;30(11):1547–54. https://doi.org/10.1093/sleep/30.11.1547 .
Ong J, Manber R, Segal Z, Xia Y, Shapiro S, Wyatt J. A randomized controlled trial of mindfulness meditation for chronic insomnia. Sleep. 2014;37(9):1553–63. https://doi.org/10.5665/sleep.4010 .
Owen M, Cardno A, O’Donovan M. Psychiatric genetics: back to the future. Mol Psychiatry. 2000;5(1):22–31. https://doi.org/10.1038/sj.mp.4000702 .
Päivi L, Sitwat L, Harri O-K, Joona M, Raimo L. ACT for sleep—internet-delivered self-help ACT for sub-clinical and clinical insomnia: a randomized controlled trial. J Context Behav Sci. 2019;12:119–27. https://doi.org/10.1016/j.jcbs.2019.04.001 .
Palagini L, Biber K, Riemann D. The genetics of insomnia–evidence for epigenetic mechanisms? Sleep Med Rev. 2014;18(3):225–35. https://doi.org/10.1016/j.smrv.2013.05.002 .
Perlis M, Ellis J, Kloss J, Riemann D. Etiology and pathophysiology of insomnia. In: Kryger M, Roth T, Dement W, editors. Principles and practices of sleep medicine. 6th ed. Philadelphia: Elsevier; 2017. p. 769–784.
Perlis M, Shaw P, Cano G, Espie C. Models of insomnia. In: Kryger M, Roth T, Dement W, editors. Principles and practice of sleep medicine. 5th ed. Missouri: Elsevier Saunders; 2011. p. 850–865.
Qureshi I, Mehler M. Epigenetics of sleep and chronobiology. Curr Neurol Neurosci Rep. 2014;14(3):432. https://doi.org/10.1007/s11910-013-0432-6 .
Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Dolenc Groselj L, Ellis J, Spiegelhalder K. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26(6):675–700. https://doi.org/10.1111/jsr.12594 .
Riemann D, Spiegelhalder K, Feige B, Voderholzer U, Berger M, Perlis M, Nissen C. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. 2010;14(1):19–311. https://doi.org/10.1016/j.smrv.2009.04.002 .
Riemann D, Spiegelhalder K, Nissen C, Hirscher V, Baglioni C, Feige B. REM sleep instability: a new pathway for insomnia? Pharmacopsychiatry. 2012;45(5):167–76. https://doi.org/10.1055/s-0031-1299721 .
Rodriguez M, Maeda Y. Meta-analysis of coefficient alpha. Psychol Methods. 2006;11(3):306–22. https://doi.org/10.1037/1082-989X.11.3.306 .
Schulz H, Salzarulo P. The development of sleep medicine: a historical sketch. J Clin Sleep Med. 2016;12(7):1041–52. https://doi.org/10.5664/jcsm.5946 .
Siddaway A, Wood A, Hedges L. How to do a systematic review: a best practice guide for conducting and reporting narrative reviews, meta-analyses, and meta-syntheses. Annu Rev Psychol. 2019;70:747–70. https://doi.org/10.1146/annurev-psych-010418-102803 .
Sirois F, Nauts S, Molnar D. Self-compassion and bedtime procrastination: an emotion regulation perspective. Mindfulness. 2019;10(3):434–45. https://doi.org/10.1007/s12671-018-0983-3 .
Spiegelhalder K, Regen W, Baglioni C, Nissen C, Riemann D, Kyle S. Neuroimaging insights into insomnia. Curr Neurol Neurosci Rep. 2015;15(3):9. https://doi.org/10.1007/s11910-015-0527-3 .
Stein M, McCarthy M, Chen C, Jain S, Gelernter J, He F, Ursano R. Genome-wide analysis of insomnia disorder. Mol Psychiatry. 2018;23(11):2238–50. https://doi.org/10.1038/s41380-018-0033-5 .
Stepanski E. Behavioral sleep medicine: a historical perspective. Behav Sleep Med. 2003;1(1):4–21. https://doi.org/10.1207/S15402010BSM0101_3 .
Tam V, Patel N, Turcotte M, Bossé Y, Paré G, Meyre D. Benefits and limitations of genome-wide association studies. Nat Rev Genet. 2019;20(8):467–84. https://doi.org/10.1038/s41576-019-0127 .
Tolin D, McKay D, Forman E, Klonsky E, Thombs B. Empirically supported treatment: recommendations for a new model. Clin Psychol Sci Pract. 2015;22(4):317–38. https://doi.org/10.1111/cpsp.12122 .
Trauer J, Qian M, Doyle J, Rajaratnam S, Cunnington D. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Ann Intern Med. 2015;163(3):191–204. https://doi.org/10.7326/M14-2841 .
van Dalfsen J, Markus C. The involvement of sleep in the relationship between the serotonin transporter gene-linked polymorphic region (5-HTTLPR) and depression: a systematic review. J Affect Disord. 2019;256:205–12. https://doi.org/10.1016/j.jad.2019.05.047 .
van Straten A, van der Zweerde T, Kleiboer A, Cuijpers P, Morin C, Lancee J. Cognitive and behavioral therapies in the treatment of insomnia: a meta-analysis. Sleep Med Rev. 2018;38:3–16. https://doi.org/10.1016/j.smrv.2017.02.001 .
Walsh J, Roth T. Pharmacologic treatment of insomnia: benzodiazepine receptor agonists. In: Kryger M, Roth T, Dement W, editors. Principles and practices of sleep medicine. 6th ed. Philadelphia: Elsevier; 2017. p. 832–841.
Wang Y, Wang F, Zheng W, Zhang L, Ng C, Unqvari G, Xiang Y. Mindfulness-based interventions for insomnia: A meta-analysis of randomized controlled trials. Behav Sleep Med. 2018. https://doi.org/10.1080/15402002.2018.1518228 [Epub ahead of print] .
Whitfield-Gabrieli S, Ford J. Default mode network activity and connectivity in psychopathology. Annu Rev Clin Psychol. 2012;8:49–76. https://doi.org/10.1146/annurev-clinpsy-032511-143049 .
Wilson B. Cutting edge developments in neuropsychological rehabilitation and possible future directions. Brain Impair. 2011;12(1):33–42. https://doi.org/10.1375/brim.12.1.33 .
Wilson B. Neuropsychological rehabilitation: state of the science. S Afr J Psychol. 2013;43(3):267–77. https://doi.org/10.1177/0081246313494156 .
Winkler A, Rief W. Effect of placebo conditions on polysomnographic parameters in primary insomnia: a meta-analysis. Sleep. 2015;38(6):925–31. https://doi.org/10.5665/sleep.4742 .
Wittchen H, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, Steinhausen H. The size and burden of mental disorders and other disorders of the brain in Europe. Eur Neuropsychopharmacol. 2011;21(9):655–79. https://doi.org/10.1016/j.euroneuro.2011.07.018 .
Download references
Acknowledgements
The authors would like to express their gratitude to the reviewers for their important comments and suggestions.
Author information
Authors and affiliations.
Department of Education and Psychology, University of Aveiro, Campus Universitário de Santiago, 3810-193, Aveiro, Portugal
Daniel Ruivo Marques
Faculty of Psychology and Educational Sciences, CINEICC-Center for Research in Neuropsychology and Cognitive Behavioral Intervention, University of Coimbra, Coimbra, Portugal
Daniel Ruivo Marques, Ana Allen Gomes & Vanda Clemente
Faculty of Psychology and Educational Sciences, University of Coimbra, Rua Do Colégio Novo, 3000-115, Coimbra, Portugal
Ana Allen Gomes
Sleep Medicine Centre, Coimbra University Hospital Centre (CHUC), Coimbra, Portugal
Vanda Clemente, José Moutinho dos Santos & Joana Serra
Faculty of Medicine, University of Coimbra, Rua Larga, 3004-504, Coimbra, Portugal
Maria Helena Pinto de Azevedo
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Daniel Ruivo Marques .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Marques, D.R., Gomes, A.A., Clemente, V. et al. Trends in insomnia research for the next decade: a narrative review. Sleep Biol. Rhythms 18 , 199–207 (2020). https://doi.org/10.1007/s41105-020-00269-7
Download citation
Received : 20 August 2019
Accepted : 28 March 2020
Published : 06 April 2020
Issue Date : July 2020
DOI : https://doi.org/10.1007/s41105-020-00269-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sleep disorder
- Find a journal
- Publish with us
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
A Narrative Review of the Literature on Insufficient Sleep, Insomnia, and Health Correlates in American Indian/Alaska Native Populations
Affiliations.
- 1 University of Alaska Anchorage, Anchorage, AK, USA.
- 2 Waianae Coast Comprehensive Health Center, Waianae, HI, USA.
- 3 University of Montana, Missoula, MT, USA.
- 4 New Mexico VA Health Care System, Albuquerque, NM, USA.
- PMID: 31360174
- PMCID: PMC6644264
- DOI: 10.1155/2019/4306463
Insufficient sleep and insomnia promote chronic disease in the general population and may combine with social and economic factors to increase rates of chronic health conditions among AI/AN people. Given that insufficient sleep and insomnia can be addressed via behavioral interventions, it is critical to understand the prevalence and correlates of these disorders among AI/AN individuals in order to elucidate the mechanisms associated with health disparities and provide guidance for subsequent treatment research and practice. We reviewed the available literature on insufficient sleep and insomnia in the AI/AN population. PubMed, PsycINFO, Google Scholar, and ProQuest were searched between June 12 th and October 28 th of 2018. Prevalence of insufficient sleep ranged from 15% to 40%; insomnia prevalence ranged from 25% to 33%. Insufficient sleep was associated with unhealthy diet, low physical activity levels, higher BMI, worse self-reported health, increased risk for diabetes mellitus, cardiovascular disease, frequent mental distress, smoking, binge drinking, depression, and chronic pain. Insomnia was associated with depression, childhood abuse, PTSD, anxiety, alcohol use, low social support, and low trait-resilience levels. Research on evidence-based treatment and implementation practices targeting insufficient sleep and insomnia was lacking, and only one study described the development/validation of a measure of insufficient sleep among AI/AN people. There is a need for rigorous sleep research including testing and implementation of evidence-based treatment for insufficient sleep and insomnia in this population in an effort to help eliminate health disparities. We present recommendations for research and clinical practice based on the current review.
PubMed Disclaimer
Resource identification and screening process.
Similar articles
- Excess frequent insufficient sleep in American Indians/Alaska natives. Chapman DP, Croft JB, Liu Y, Perry GS, Presley-Cantrell LR, Ford ES. Chapman DP, et al. J Environ Public Health. 2013;2013:259645. doi: 10.1155/2013/259645. Epub 2013 Feb 21. J Environ Public Health. 2013. PMID: 23509471 Free PMC article.
- A Systematic Review of Environmental Health Outcomes in Selected American Indian and Alaska Native Populations. Meltzer GY, Watkins BX, Vieira D, Zelikoff JT, Boden-Albala B. Meltzer GY, et al. J Racial Ethn Health Disparities. 2020 Aug;7(4):698-739. doi: 10.1007/s40615-020-00700-2. Epub 2020 Jan 23. J Racial Ethn Health Disparities. 2020. PMID: 31974734
- Sleep Problems and Health Outcomes Among Urban American Indian and Alaska Native Adolescents. Troxel WM, Klein DJ, Dong L, Mousavi Z, Dickerson DL, Johnson CL, Palimaru AI, Brown RA, Rodriguez A, Parker J, Schweigman K, D'Amico EJ. Troxel WM, et al. JAMA Netw Open. 2024 Jun 3;7(6):e2414735. doi: 10.1001/jamanetworkopen.2024.14735. JAMA Netw Open. 2024. PMID: 38833247 Free PMC article.
- Emotional and Behavioral Aspects of Diabetes in American Indians/Alaska Natives. Scarton LJ, de Groot M. Scarton LJ, et al. Health Educ Behav. 2017 Feb;44(1):70-82. doi: 10.1177/1090198116639289. Epub 2016 Jul 9. Health Educ Behav. 2017. PMID: 27179289 Review.
- Resilience and health in American Indians and Alaska Natives: A scoping review of the literature. John-Henderson NA, White EJ, Crowder TL. John-Henderson NA, et al. Dev Psychopathol. 2023 Dec;35(5):2241-2252. doi: 10.1017/S0954579423000640. Epub 2023 Jun 22. Dev Psychopathol. 2023. PMID: 37345444 Free PMC article. Review.
- Effect of Centella asiatica ethanol extract on zebrafish larvae ( Danio rerio ) insomnia model through inhibition of Orexin, ERK, Akt and p38. Afif Z, Eddy Santoso MI, Nurdiana, Khotimah H, Satriotomo I, Kurniawan SN, Sujuti H, Iskandar DS, Hakimah A. Afif Z, et al. F1000Res. 2024 Jul 18;13:107. doi: 10.12688/f1000research.141064.1. eCollection 2024. F1000Res. 2024. PMID: 38812527 Free PMC article.
- Association between poor sleep and mental health issues in Indigenous communities across the globe: a systematic review. Fernandez DR, Lee R, Tran N, Jabran DS, King S, McDaid L. Fernandez DR, et al. Sleep Adv. 2024 May 2;5(1):zpae028. doi: 10.1093/sleepadvances/zpae028. eCollection 2024. Sleep Adv. 2024. PMID: 38721053 Free PMC article.
- Effect of physical activity on sleep problems in sedentary adults: a scoping systematic review. Rai A, Aldabbas M, Veqar Z. Rai A, et al. Sleep Biol Rhythms. 2023 Oct 28;22(1):13-31. doi: 10.1007/s41105-023-00494-w. eCollection 2024 Jan. Sleep Biol Rhythms. 2023. PMID: 38476845 Review.
- Poor self-reported sleep quality associated with suicide risk in a community sample of American Indian adults. Ehlers CL, Karriker-Jaffe KJ, Bernert R. Ehlers CL, et al. Sleep Adv. 2023 May 19;4(1):zpad024. doi: 10.1093/sleepadvances/zpad024. eCollection 2023. Sleep Adv. 2023. PMID: 37293513 Free PMC article.
- Relationship between sleep duration and quality and glycated hemoglobin, body mass index, and self-reported health in Marshallese adults. McElfish PA, Andersen JA, Felix HC, Purvis RS, Rowland B, Scott AJ, Chatrathi M, Long CR. McElfish PA, et al. Sleep Health. 2021 Jun;7(3):332-338. doi: 10.1016/j.sleh.2021.01.007. Epub 2021 Mar 8. Sleep Health. 2021. PMID: 33707104 Free PMC article.
- Sivertsen B., Krokstad S., Overland S., Mykletun A. The epidemiology of insomnia: associations with physical and mental health: the HUNT-2 study. Journal of Psychosomatic Research. 2009;67(2):103–116. doi: 10.1016/j.jpsychores.2009.05.001. - DOI - PubMed
- Biddle D. J., Kelly P. J., Hermens D. F., Glozier N. The association of insomnia with future mental illness: is it just residual symptoms? Sleep Health. 2018;4(4):352–359. doi: 10.1016/j.sleh.2018.05.008. - DOI - PubMed
- Tang W., Lu Y., Xu J. Post-traumatic stress disorder, anxiety and depression symptoms among adolescent earthquake victims: comorbidity and associated sleep-disturbing factors. Social Psychiatry and Psychiatric Epidemiology. 2018;53(11):1241–1251. doi: 10.1007/s00127-018-1576-0. - DOI - PubMed
- Smith M. T., Haythornthwaite J. A. How do sleep disturbance and chronic pain inter-relate? Insights from the longitudinal and cognitive-behavioral clinical trials literature. Sleep Medicine Reviews. 2004;8(2):119–132. doi: 10.1016/s1087-0792(03)00044-3. - DOI - PubMed
- Roberts M. B., Drummond P. D. Sleep problems are associated with chronic pain over and above mutual associations with depression and catastrophizing. Clinical Journal of Pain. 2016;32(9):792–799. doi: 10.1097/ajp.0000000000000329. - DOI - PubMed
Publication types
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- Europe PubMed Central
- Hindawi Limited
- PubMed Central
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
ORIGINAL RESEARCH article
The different faces of insomnia.

- 1 Department of Internal Medicine and Dermatology, Interdisciplinary Center of Sleep Medicine, Charité - Universitätsmedizin Berlin, Berlin, Germany
- 2 Department of Behavioral Therapy and Psychosomatic Medicine, Rehabilitation Center Seehof, Federal German Pension Agency, Seehof, Germany
- 3 Department of Biology, Saratov State University, Saratov, Russia
Objectives: The identification of clinically relevant subtypes of insomnia is important. Including a comprehensive literature review, this study also introduces new phenotypical relevant parameters by describing a specific insomnia cohort.
Methods: Patients visiting the sleep center and indicating self-reported signs of insomnia were examined by a sleep specialist who confirmed an insomnia diagnosis. A 14-item insomnia questionnaire on symptoms, progression, sleep history and treatment, was part of the clinical routine.
Results: A cohort of 456 insomnia patients was described (56% women, mean age 52 ± 16 years). They had suffered from symptoms for about 12 ± 11 years before seeing a sleep specialist. About 40–50% mentioned a trigger (most frequently psychological triggers), a history of being bad sleepers to begin with, a family history of sleep problems, and a negative progression of insomnia. Over one third were not able to fall asleep during the day. SMI (sleep maintenance insomnia) symptoms were most frequent, but only prevalence of EMA (early morning awakening) symptoms significantly increased from 40 to 45% over time. Alternative non-medical treatments were effective in fewer than 10% of cases.
Conclusion: Our specific cohort displayed a long history of suffering and the sleep specialist is usually not the first point of contact. We aimed to describe specific characteristics of insomnia with a simple questionnaire, containing questions (e.g., ability to fall asleep during the day, effects of non-medical therapy methods, symptom stability) not yet commonly asked and of unknown clinical relevance as yet. We suggest adding them to anamnesis to help differentiate the severity of insomnia and initiate further research, leading to a better understanding of the severity of insomnia and individualized therapy. This study is part of a specific Research Topic introduced by Frontiers on the heterogeneity of insomnia and its comorbidity and will hopefully inspire more research in this area.
Introduction
Insomnia is one of the most frequent sleep disorders with continuously increasing prevalence. About 30–50% of the US adult population exhibit insomnia symptoms, 15–20% display a short-term insomnia of <3 months, and 5–15% display a chronic insomnia of >3 months ( 1 – 3 ). Common diagnostic manuals include the ICSD-3 (International Classification of Sleep Disorders, 3 rd Edition, American Academy of Sleep Medicine 2014) and the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5 th Edition, American Psychiatric Association 2013) ( 4 , 5 ). Main characteristics of insomnia include dissatisfaction with sleep quantity and quality with one or more of the following symptoms: difficulties initiating sleep, difficulties maintaining sleep (frequent or prolonged awakenings with problems returning to sleep again), and early morning awakening (occurring earlier than desired after a total sleep time of only 3–5 h with the inability to return to sleep). The disturbed sleep is associated with stress, psychological strain and suffering, as well as impairment in social, occupational, and other important areas of functioning. Complaints include fatigue, exhaustion, lack of energy, daytime sleepiness, cognitive impairment (e.g., attention, concentration, and memory), mood swings (e.g., irritability, dysphoria), impaired occupational functioning and impaired social functioning. The symptoms occur for at least 3 nights per week for at least 3 months and occur despite an adequate sleep environment.
Previous dichotomization of insomnia in primary and secondary (or comorbid) insomnia has been abandoned with the new editions of the DSM-5 and ICSD-3. Currently, insomnia is mostly characterized by the common phenotypes of sleep onset insomnia (SOI insomnia, difficulty falling asleep), sleep maintenance insomnia (SMI insomnia, difficulty staying asleep), early morning awakenings insomnia (EMA insomnia), and a combination of those. Another categorization follows the timeframe of being an acute (<1 month), subacute (1–3 months), and chronic insomnia (>3 months) ( 4 , 5 ). While other sleep disorders (e.g., sleep apnea) are categorized by severity into mild, moderate, or severe, which has important implications for the choice of therapy, insomnia still lacks such a classification. The Insomnia Severity Index (ISI) is the only instrument currently in use that allows for severity classification: no insomnia (score 0–7), subclinical insomnia (score 8–14), or moderate to severe insomnia (score 15–28) ( 6 ).
The characterization of different phenotypes is important to establish clinically relevant subtypes of insomnia. It may help to reduce the heterogeneity of insomnia and facilitate cause identification and personalized treatments. Yet there are not many standardized instruments of insomnia diagnosis allowing for phenotyping. However, there has been evidence that insomniacs with a total sleep time of <6 h suffer a more severe insomnia than insomniacs with a total sleep time of 6 h or more ( 7 ). They display mental and psychological impairment compared to patients with average or longer than average sleep. However, mortality is increased for insomniacs with longer total sleep time ( 8 ). The sleep duration with the 6-h distinction also influences the therapy outcome, success of cognitive-behavioral therapy (CBT), and the relation to comorbid bipolar disorder ( 9 , 10 ). Recently, a study investigated subtypes of insomnia according to psychological stress ( 11 ). Questioning 2,224 volunteers with an ISI score of at least 10 and a control group of 2,098 volunteers with an ISI score below 10, five insomnia subtypes were identified: highly distressed, moderately distressed but sensitive to positive reinforcement (accepting of positive emotions), moderately distressed insensitive to positive reinforcement, slightly distressed with a high reactivity to their environment and life circumstances, and slightly distressed with low reactivity. The results showed a high stability of the classification over the 5-year investigation. The psychological categorization is clinically relevant as there were clear differences identified between the subtypes regarding development, therapy success, presence of electroencephalogram (EEG) biomarker, and the risk for depression. This was a first approach to subtyping insomnia patients according to psychological health. The exact effect of psychological health, family history, comorbidity, personality, environment and sleep quality on insomnia is still unclear. Similar symptom clusters have been discussed for other disorders including depression ( 12 ).
Our study is part of the specific Research Topic introduced by Frontiers on the heterogeneity of insomnia and its comorbidity. We aim to encourage and further the discussion on insomnia heterogeneity and the need for possible phenotyping, we do not intend to provide a complete list of phenotypes or possible clusters. The study picked up the approach of subtyping insomnia by collecting a short questionnaire during anamnesis on possible related symptoms, onset and course of insomnia. We described phenotypical traits of insomniacs with a cohort of sleep disturbed patients from a specialized outpatient clinic for sleep disorders.
Participants and Recruitment
Since 2018, a specialized 14-item insomnia questionnaire has formed part of the clinical routine at the outpatient clinic of the Interdisciplinary Center of Sleep Medicine, Charité—Universitätsmedizin Berlin ( Figure 1 ). The questionnaire is the result of literature research, clinical experience, and consensus of psychologists, neurologist, psychiatrists, and sleep physicians within the sleep center. Patients who visited the outpatient clinic between 01/2019 and 02/2020 and indicated self-reported symptoms presenting a suspicion of insomnia (e.g., difficulties initiating sleep, maintaining sleep, or early morning awakening) according to ICSD-3 criteria were recruited and completed the questionnaire. In total, 486 patients were examined by a physician specializing in sleep disorders and insomnia who confirmed an insomnia diagnosis. The questionnaire did not contain any identifying information. As the questionnaire is part of the clinical routine and the de-identified data has been analyzed retrospectively, ethical review and approval was not required in accordance with the local legislation and institutional requirements. As part of the clinical routine, patients signed informed consent forms allowing de-identified data of their patient file, including the insomnia questionnaire, to be used for research purposes.
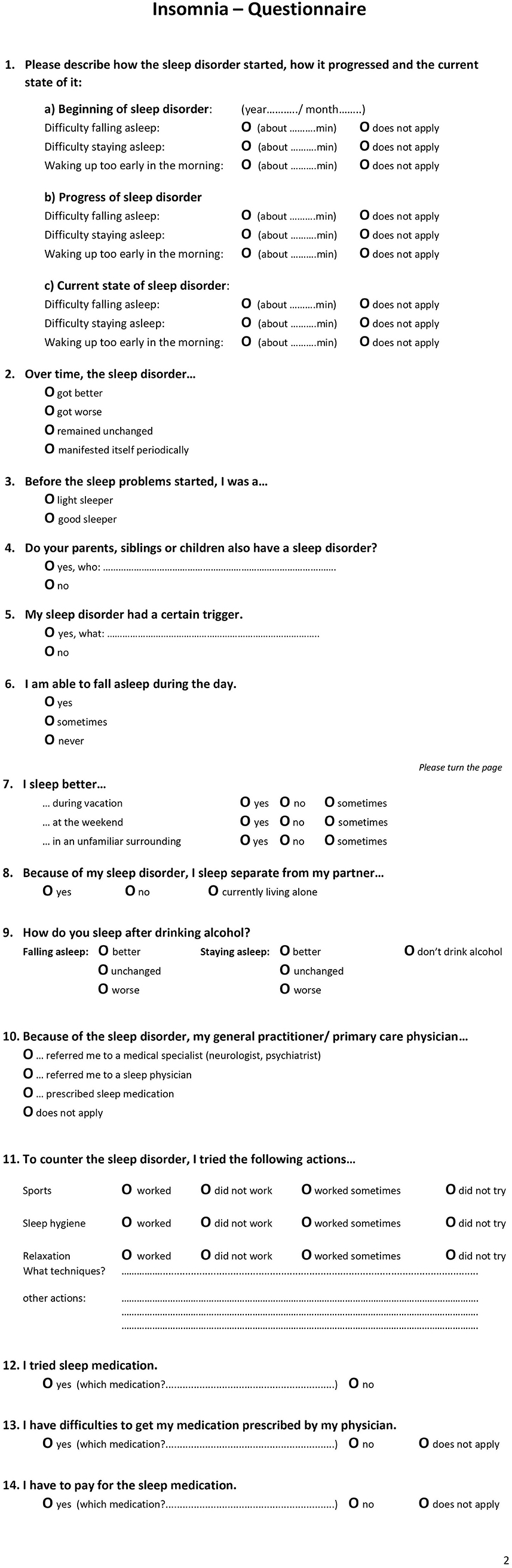
Figure 1 . The English translation of the 14-item Insomnia Questionnaire with page 1 and page 2.
Questionnaire
The insomnia questionnaire consisted of 14 items ( Figure 1 presents an English translation of the questionnaire). These included questions related to (1) type of insomnia (SOI—sleep onset insomnia, SMI—sleep maintenance insomnia, EMA—early awakening insomnia, multiple answers possible) at three points in time (start of disorder, progression, current state), (2) progression of insomnia, (3) sleep history of being a light or good sleeper, (4) relatives with sleep disorder, (5) triggers, (6) daytime sleep, (7) sleeping in different environments, (8) sleeping arrangement with partner, (9) alcohol as a sleep aid, (10) referral/ recommendation of general practitioner (multiple answer options), (11) alternative sleep treatments, and (12–14) sleep medication.
Procedure of the examination was standardized and performed by the same physician: On arrival, patients received several sleep questionnaires including the 14-item insomnia questionnaire. They were asked to complete these questionnaires before seeing the physician. During the following in-person consultation, the physician completed a full anamnesis (a patient-reported medical history) and confirmed a diagnosis of a primary insomnia according to ICSD-3 criteria. Next, the questions of the insomnia questionnaire were evaluated. Certain questions were clarified, and missing information added. For example, for question 3, light sleeper was defined. Light sleeper includes patients with a regular bedtime but whose sleep is sensitive to light, temperature, and noise. They need a specific degree of sleep comfort and sleep worse in an unfamiliar environment. These patients can nap during the day and sleep better during vacation and time off (e.g., weekends). They perceive their sleep as non-restorative. They also do not meet the diagnostic criteria of insomnia. The question refers to the time before the insomnia started, mostly referring to childhood / adolescence. For question 6, it was clarified that daytime napping included a daytime situation that explicitly allows for napping. For question 7, it was explained that “weekend” also included the days off work.
Sample size was calculated based on prevalence data and the estimated number of insomnia patients: ca. 30–50% of 328.2 million people (US population estimate 2019) result in about 98.5–164.1 million patients ( 13 ). With an accepted error rate of maximum 5% and a confidence interval of 95%, the sample size was set to at least 400 questionnaires in order to detect sufficiently powerful effects. Statistical analysis was performed using SPSS (IBM SPSS Statistics, Version 20). The patient cohort was described using a descriptive analysis with numbers and percentages ( Table 1 ). In order to investigate possible insomnia subgroups based on phenotypes/characteristics, we compared items with dichotomous answers. Item 7 (sleeping in different environments), item 9 (alcohol as a sleep aid), and item 11 (alternative sleep treatments) each had several subcategories which were consolidated into one overall category. For the text answer of item 5 (trigger) we performed a qualitative data analysis by subjectively grouping the text data and visually presenting the categories. A t-test was used for group comparisons of continuous variables (e.g., age), the chi-square test for dichotomous variables. Significance level was set at 0.05.
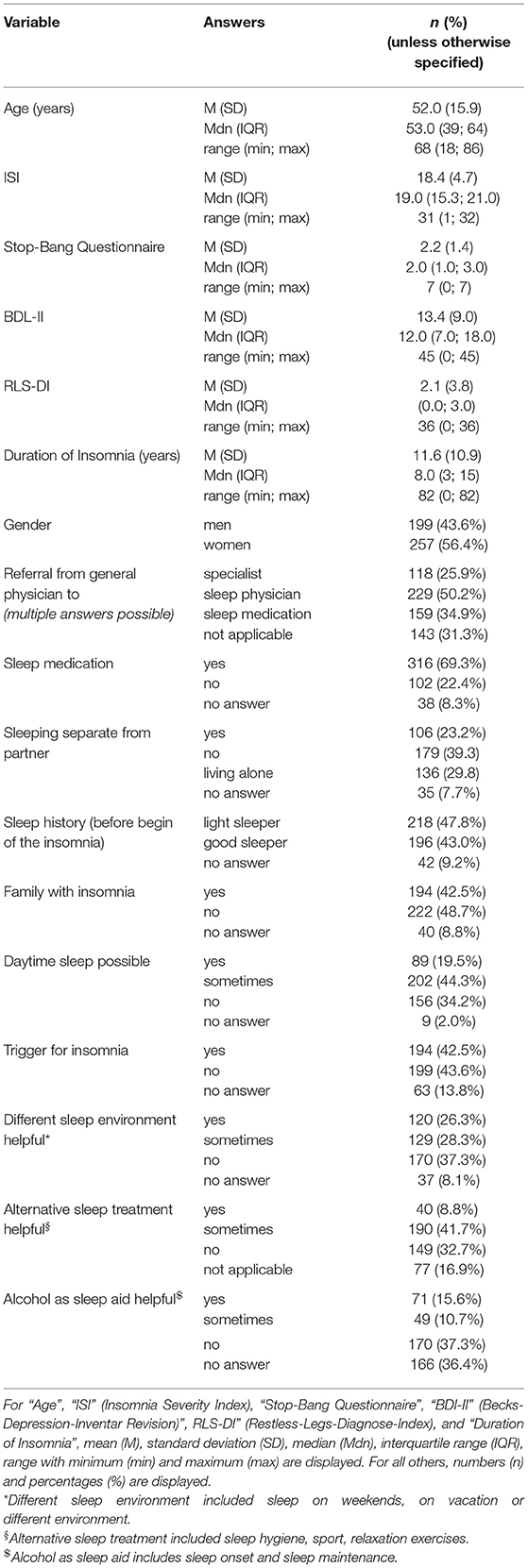
Table 1 . Sample description ( n = 456 patients).
Patient Description
Due to missing information that could also not be completed during the in-person consultation with the physician, 30 questionnaires were removed from analysis. The remaining 456 questionnaires were de-identified and analyzed. The patient cohort ( Table 1 ) reported having sleep problems for an average of 11.6 ± 10.9 years (range: 0–82 years, where 0 means the symptoms just started within the past month). The cohort consisted of slightly more female insomniacs (56%) and had an average age of 52.0 ± 15.9 years (range: 18–86 years). More than half of the patients reported having a partner and not living alone (63%), and of those 37% slept in a separate room due to the sleep disorder. If the patient went to a general physician first, 50% were referred to a sleep specialist and 26% to another specialist (neurologist, psychiatrist etc.). In 35% of those cases, the general physician initiated a therapy with sleep medication. In general, 69% of the patients reported having used sleep medication, 23% indicated that they had not. Only 9% mentioned that it was difficult to get sleep medication. While 26% stated they had to pay for sleep medication, 37% said they did not. In Germany, sleep medication for primary insomnia covered by insurance only includes melatonin (only for patients over 55 years) and z-drugs (only for the acute therapy of 4 weeks).
Sleep Characteristics
About 43% of the patients indicated that they had a history of being good sleepers before the insomnia onset, while 48% mentioned that they have always been light sleepers. Forty-three percent reported having a family member with sleep problems. Despite insomnia symptoms, 20% of patients indicated that they were able to fall asleep during the day and 44% sometimes. While 43% of patients reported a trigger for the sleep problems, 42% reported no trigger ( Table 1 ). Figure 2 presents a categorization of the reported triggers. The most frequent triggers were of psychological nature (22%) including depression, anxiety, post-traumatic stress disorder, death of a family member, trauma, rape, psychotherapy etc. Stress was listed as a separate category but is to be considered as a subcategory of psychological triggers (additional 11%). Work related triggers including change or loss of job, freelance work, work problems, shift work, long work hours, workload, mobbing/ bulling etc. accounted for 15%.
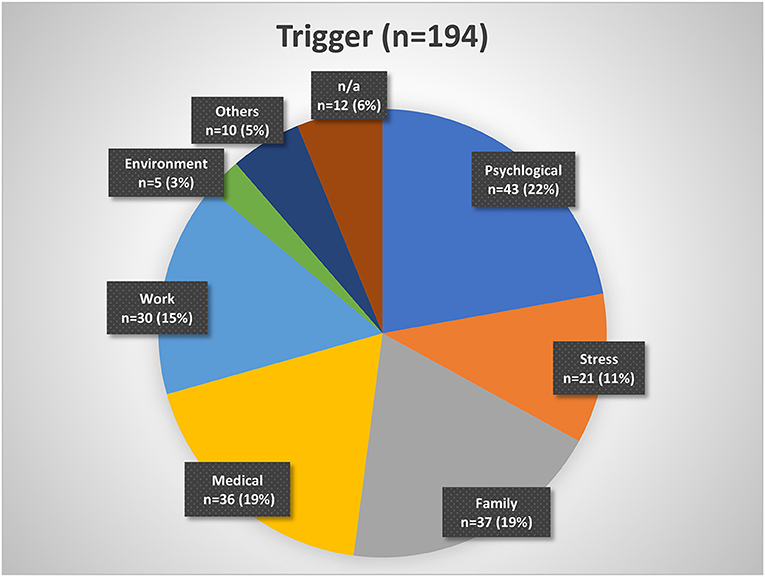
Figure 2 . Insomnia triggers organized by categories. Psychological triggers include depression, fear, trauma, etc. Stress may be considered a subgroup of psychological triggers. Family triggers include birth, children, marriage, divorce, etc. Medical triggers include sickness, operations, etc. Work triggers include mobbing, loss of job, change of job, workload, etc. Environment triggers include noise, lighting, neighborhood, etc. Other triggers include smoking, attitude, etc. n/a, not available.
The question about sleep in a different environment (item 7 of the questionnaire) included three subcategories: sleep during vacation, sleep at weekends, and sleep in unfamiliar surroundings. Sleep during vacation was perceived as better by 21% ( n = 84), sometimes better by 30% ( n = 121), and not at all better by 49% ( n = 198). Sleep at the weekend was perceived as better by 18% ( n = 70), sometimes better by 26% ( n = 103), and not at all better by 56% ( n = 224). Sleep in unfamiliar surroundings was perceived as better by 5% ( n = 19), sometimes better by 17% ( n = 68), and not at all better by 78% ( n = 304). We consolidated the subcategories in one general environment variable. First, sleep in a different environment (in general) was considered better if a patient answered “yes (sleep better)” to at least one of the subgroups. The remaining patients were categorized into the sometimes group if they answered “sometimes” to at least one of the subcategories. Then, the remaining patients were categorized into the “no (do not sleep better)” or “no answer” category. In general, 26% indicated that they sleep better in different environments, 28% sometimes, and 37% not at all ( Table 1 ).
The question for alternative non-medical treatments (item 11) also included three subcategories: sport, sleep hygiene, and relaxation techniques. Sport only helped in 7% ( n = 26), helped sometimes in 32% ( n = 130), and did not help in 46% ( n = 185). Sleep hygiene helped in 5% ( n = 18), helped sometimes in 29% ( n = 103), and did not help in 43% ( n = 154). Relaxation techniques helped in 5% ( n = 19), helped sometimes in 32% ( n = 117), and did not help in 38% ( n = 142). We combined the subcategories into one overall variable of non-medical treatment in the same way as for item 7. In general, 9% of the patients indicated that an alternative treatment helps, 42% mentioned it helped sometimes, and 33% reported it did not help at all ( Table 1 ).
Alcohol as a sleep aid (item 9) included two subcategories: alcohol as a sleep aid for sleep onset and alcohol as a sleep aid for sleep maintenance. While 40% ( n = 112) indicated alcohol helps with SOI symptoms, it did not change sleep onset in 41% ( n = 116) and symptoms got worse in 19% ( n = 54). Alcohol helped with SMI symptoms in 11% ( n = 31), did nothing in 46% ( n = 123), and got worse in 43% ( n = 116). We also consolidated this variable. Alcohol as a sleep aid in general helped, if a patient answered “sleep got better” to at least one of the two subcategories (without a “sleep got worse” for the other category). Alcohol worsened sleep if a patient answered at least once “got worse” (without a “got better” for the other category). We added the answer option “alcohol helps sometimes” for patients that answered “got better” to one of the categories and “got worse” to the other. The remaining patients were categorized as “no change” or “no answer.” In general, alcohol helped in 16%, helped sometimes in 11%, and did not help (or even got worse) in 37% ( Table 1 ).
Table 2 presents a further description of insomnia subtypes based on these sleep characteristics. We dichotomized the answers into yes/no in order to create a more equal group distribution for comparison. Patients with a sleep history of being light sleepers even before insomnia onset, had significantly longer insomnia symptoms than patients with a sleep history of being good sleepers ( p < 0.05). Patients with a family history of sleep problems were significantly more frequently female ( p < 0.05), had suffered from insomnia symptoms significantly longer ( p < 0.01), and presented significantly more EMA symptoms ( p < 0.05) than patients without a family history of sleep problems. Patients who were able to sleep during the day were significantly more frequently male ( p = 0.001) and displayed fewer SOI ( p < 0.001) and fewer EMA symptoms ( p < 0.01) than patients who could not sleep during the day. Patients with no trigger displayed a tendency to having a longer insomnia duration than patients with a trigger ( p = 0.05). Patients who were able to sleep better in different environments were significantly younger ( p < 0.001) and showed a tendency to shorter insomnia duration ( p = 0.05) than patients who did not sleep better in another environment. Patients for whom alcohol helped as a sleep aid were significantly younger ( p < 0.001) and presented significantly more SOI symptoms ( p < 0.001).
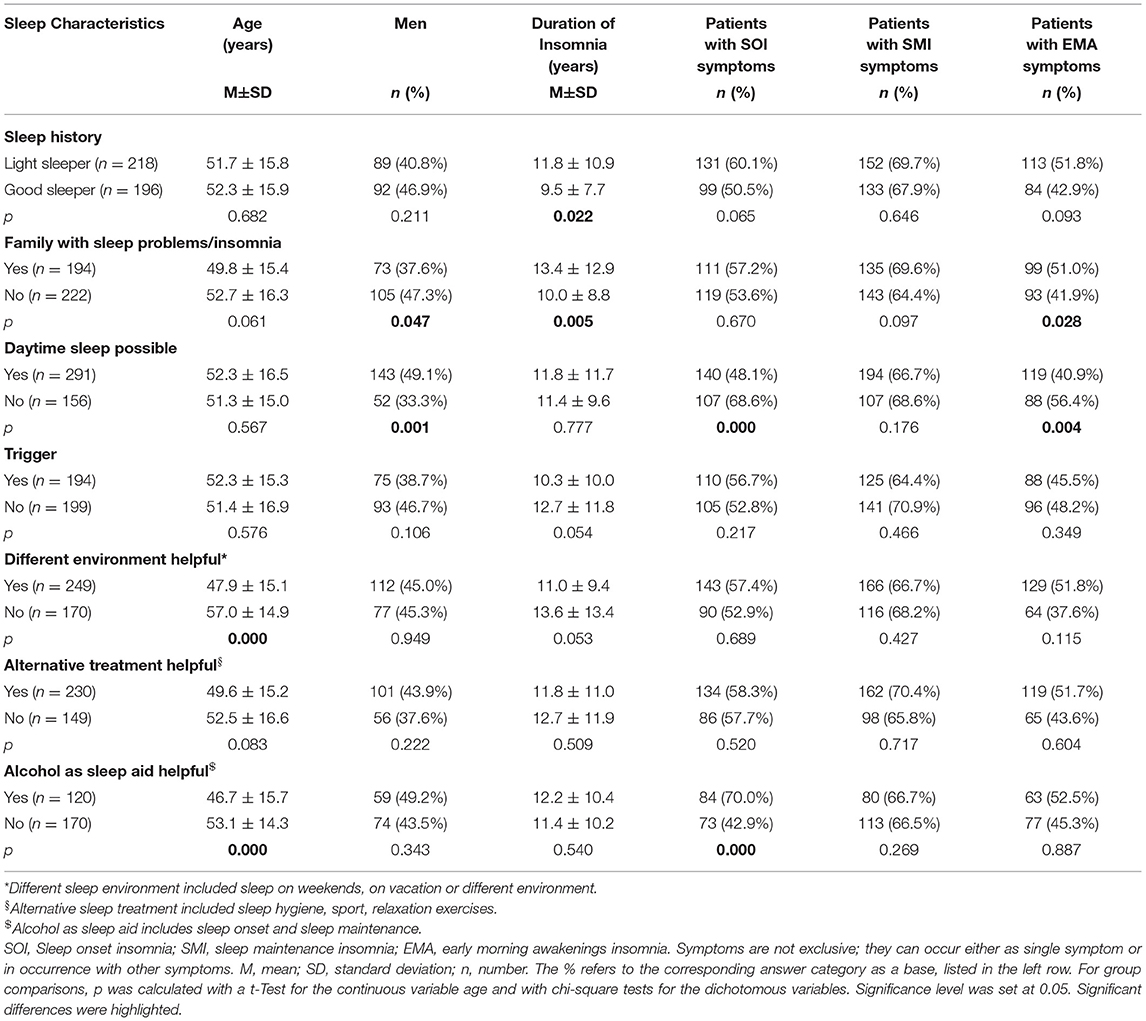
Table 2 . Description of possible insomnia phenotype subgroups based on sleep characteristics.
Insomnia Symptom Subtypes and Progression
At time of visit, 54% of patients presented SOI symptoms, 66% SMI symptoms, and 45% EMA symptoms ( Table 3 ). In 57% of the patients, there was a combination of those symptoms. Patients with SOI symptoms reported on average that they needed 85.6 ± 55.0 min to fall asleep. Patients with SMI symptoms reported waking up for about 79.0 ± 58.2 min after sleep onset. And patients with EMA symptoms reported that they woke up on average 79.0 ± 56.5 min too early in the morning. Patients with EMA symptoms (not exclusively, combination of symptoms possible) had the shortest history of sleep problems (10.2 ± 9.1 years, range: 0–44 years) compared to patients with SOI symptoms (12.0 ± 9.8 years, range: 0–82 years) and patients with SMI symptoms (11.5 ± 10.6 years, range: 0–82 years). Differences were not significant.
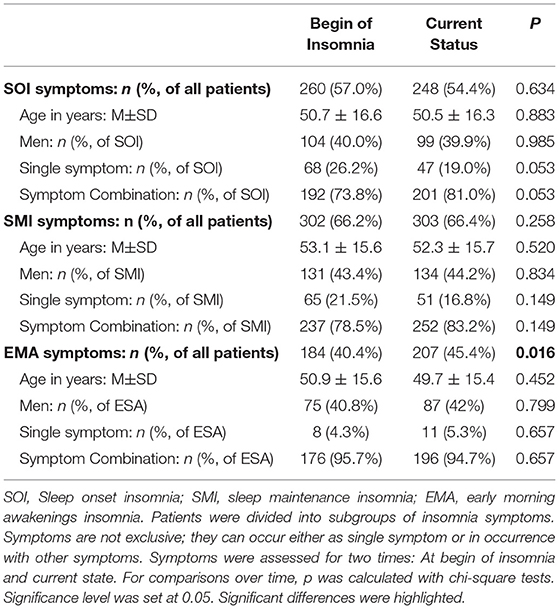
Table 3 . Patient description by insomnia subgroups based on symptoms over time.
Table 3 presents the possible change of sleep symptoms over time by type of sleep symptoms. There was no significant change in SOI or SMI symptoms. Only EMA symptoms significantly increased over time ( p = 0.016). Figure 3 presents the progression in severity of the sleep disorder. Fewer than 10% reported an improvement of symptoms, while in 41% the sleep disorder got worse. In 20% the symptoms showed a periodic pattern. The progression was independent of current symptoms.
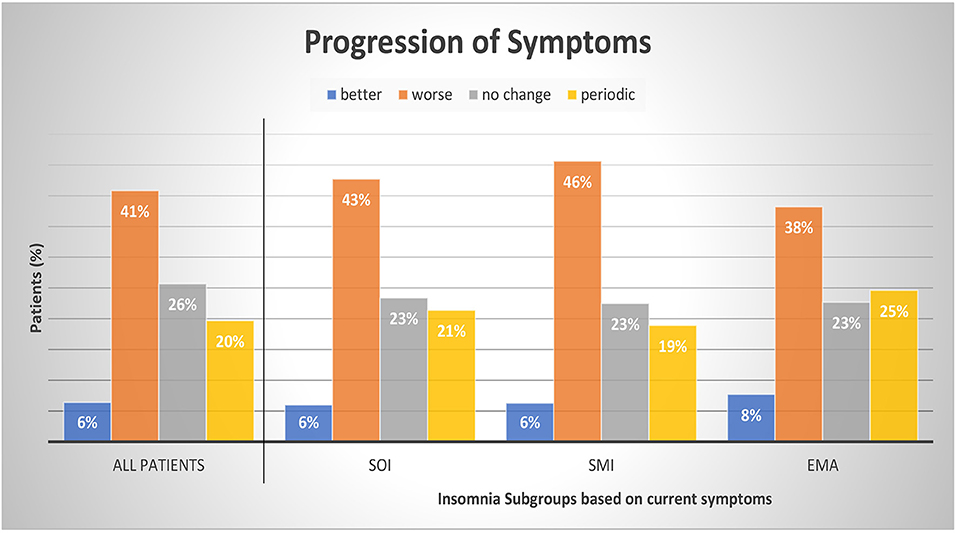
Figure 3 . Progression of symptoms by insomnia subgroups. Patients were divided into subgroups of current insomnia symptom. Symptoms are not exclusive, they can occur either as single symptom or in occurrence with other symptoms. SOI, Sleep onset insomnia; SMI, sleep maintenance insomnia; EMA, early morning awakenings insomnia. A patient with a periodic pattern of insomnia experiences weeks or months long periods with insomnia symptoms alternating with symptom free periods. For comparisons between symptom groups, p was calculated with chi-square tests. Results were not significant at a 0.05 level. The sum of the subcategories does not add up to 100% as we refrained from displaying the category “missing data and multiple answers” (7% All patients, 7% SOI, 6% SMI, and 7% EMA).
A distinct cohort of insomnia patients that reported to a special outpatient clinic for sleep disorders revealed that about 40–50% of the patients mentioned a trigger for the sleep problems, were not good sleepers to begin with (light sleepers), had a family history of sleep problems, and had a progressive course of insomnia. Over one third were not able to fall asleep during the day. Insomnia with SMI symptoms was most frequent, as well as a psychological trigger. Over time, EMA symptoms increased. Alternative non-medical treatments were only lastingly effective in fewer than 10%. Over two thirds of the patients (69%) had tried sleep medication. One of the unique traits of our cohort is the duration of the sleep problem before the visit to a specialist (over 11 years). For most, the sleep specialist/clinic is not the first point of contact. Thus, our patient cohort is not comparable to one from a general physician or population-based cohort.
Our results emphasize the insomnia heterogeneity and the need for phenotyping. Following, we will first discuss the characteristics assessed with our questionnaire starting with some new aspects that are currently not commonly asked (history of being a light sleeper, daytime sleep, effects of alternative treatments, alcohol, temporal stability/change of insomnia symptoms). Then, we will review the current literature for further possible phenotypes. Table 4 presents an overview.
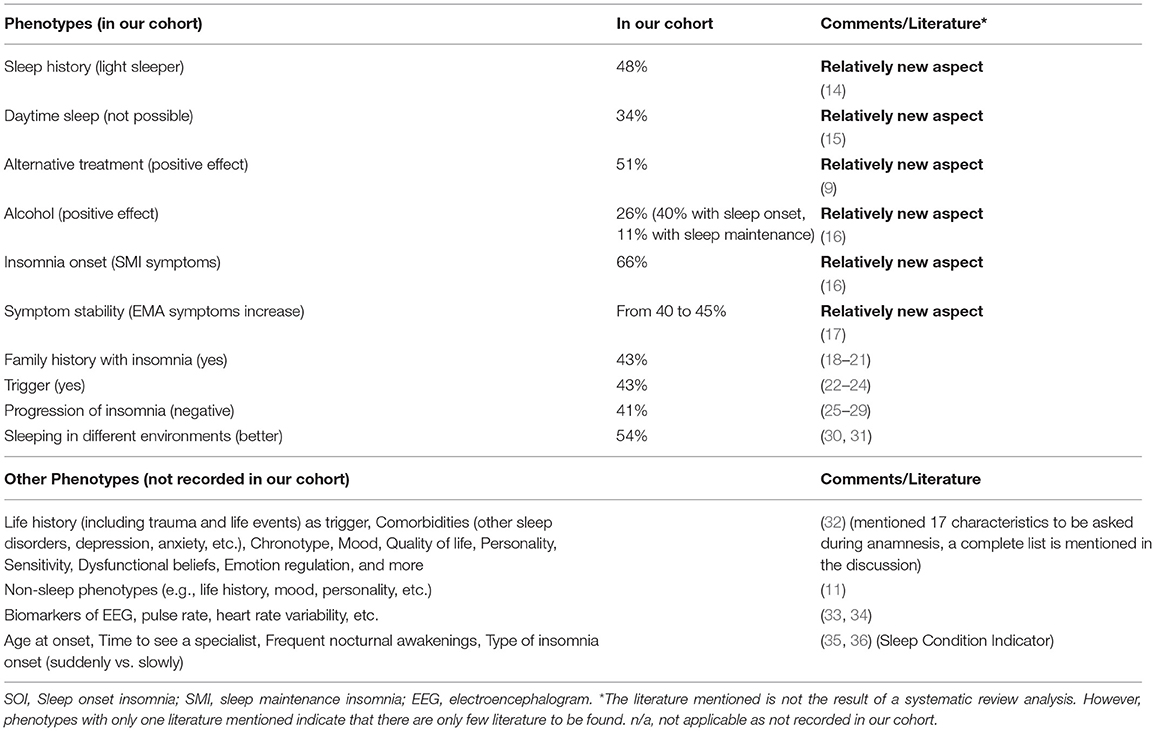
Table 4 . Overview of discussed phenotypes.
Phenotypes—Based on Our Cohort
Sleep history.
Almost half of our cohort (48%) presented a bad sleep history, indicative of an idiopathic insomnia.
There are no clear biomarkers or diagnostic criteria to distinguish between psychophysiological and idiopathic (chronic) insomnia ( 14 ). In order to identify idiopathic insomnia, we ask the patient for their sleep history, specifically before insomnia onset. Did the patient always experience poor (light) sleep, or were they a fairly good sleeper? We assume that light sleep is the pre-stage of insomnia, but not every light sleeper needs to develop insomnia, indicating that these variables are not predictors for differentiating between psychophysiological and idiopathic insomnia. Whether this distinction of good and bad sleep before developing insomnia influences therapy will need to be further investigated. Also, the term “light (bad)” sleep needs to be clearly defined and standardized.
Daytime Sleep
Using our questionnaire, we found in our cohort that 34% of patients reported not being able to take a nap during the daytime despite being tired and despite having the explicit opportunity of taking a nap. Those patients were predominantly women with more SOI and more EMA symptoms compared to patients who were able to fall asleep during the day. They did not differ regarding the duration of their insomnia symptoms.
Currently, it is not common during insomnia diagnosis to ask whether a patient is able to fall asleep during the day or to conduct a Multiple Sleep Latency Test (MSLT) for objective assessment. Our own experience with insomnia patients, however, showed how important this question is. We experienced that patients who sleep poorly at night and are tired during the day, but cannot sleep in the day either, usually have a higher degree of insomnia. They tend to suffer for more nights a week and are more resistant to therapy. In contrast, the possibility of falling asleep during the day, in front of the television, in the car, on public transport, in a meeting, or in other quiet surroundings, seems to be a sign of a lower degree of insomnia.
The ability to nap during the day has also been a criterion for other indications in the literature. The Hyperarousal Scale by Regestein et al. ( 37 ) provides indirectly a reference to the degree of alertness during the day and thus to the inability to fall asleep. Khassawneh et al. ( 38 ) used the scale together with the patient's subjective statement that they cannot nap during the day and found that patients with hyperarousal and short sleep duration have more cognitive deficits in memory tests. Li et al. ( 39 ) used the MSLT with a threshold value of 14 min to define hyperarousal. Drake et al. ( 40 ) also used the MSLT and investigated sleep disturbances due to commonly experienced stressful situations to identify factors representing the construct of “stress-related” vulnerability to sleep disturbance. Subjects with a high Ford Insomnia Response to Stress Test (FIRST) score had poorer sleep quality at night and higher latencies of sleep in the MSLT. Roehrs et al. ( 15 ) performed the MSLT in 95 patients with primary insomnia (32–64 years) and in 55 healthy sleepers and found a higher sleep latency in insomniacs (13.2 ± 4.65 min vs. 11.0 ± 4.93 min). However, the difference is small and the variability among insomniacs is high (between 2 and 20 min). The MSLT is still a questionable method for diagnosing insomnia, but it may be a possible tool for subtyping insomnia with regard to the ability to fall asleep during daytime. Espie et al. ( 41 ) examined daytime symptoms of 11,129 participants with ( n = 5,083) and without insomnia, coming from different backgrounds. Of the analyzed items (energy, concentration, relationships, ability to stay awake, mood, and ability to get through work), the items “energy” and “mood” turned out to be the two most important parameters for insomniacs, but not the item “ability to stay awake.” The importance of the criterion daytime sleepiness and/or ability to stay awake seems therefore recognized, but not yet uniformly defined and requires further research.
Alternative Treatment (Behavioral Therapy)
In our cohort, about 83% of the patients have tried at least one of these alternative non-medical behavioral treatments: sport, sleep hygiene, and/or relaxation techniques. In one third of the patients (33%) these techniques did not help. There were no significant age, gender, or symptom differences between patients with effective alternative treatments and patients where it was not effective. However, we did not investigate the severity of insomnia and it may be possible that patients where the alternative treatments did not show a positive effect may be patients with more severe insomnia.
Therapy recommendations for insomnia include a multi-modal behavioral therapy including psychological elements (e.g., CBT) as the first therapeutic step which many patients do complete, most commonly even before they arrange a visit to a specialist ( 42 ). This is also what we found in our cohort. Most of our patients have tried to educate themselves on their sleep problems, have tried to improve their sleep hygiene, have tried alternative non-medical treatments (e.g., sport, relaxation, etc.), and already went to either a natural health practitioner, homeopath, psychologist or psychotherapist. Currently, CBT is not yet good enough established in Germany as a definite treatment for insomnia. Studies have shown that CBT had less of an effect on insomniacs with short sleep duration ( 9 ). We assume that this also applies to patients with a more severe insomnia. However, severity has yet to been clearly defined. Patients will most likely show a similar reaction to phytopharmacology or alternative “smart” therapy (e.g., acoustic or electrical stimulation). A future quality check and standardization of CBT methods may be helpful in order to use the success of alternative treatment/behavioral therapy as a phenotypical criterion. We hypothesize that successful CBT is mainly linked to mild insomnia. For moderate to severe insomnia, CBT should be a necessary concomitant therapy.
In our cohort, only about 26% mentioned that alcohol helps with sleep problems in general. Patients for whom alcohol helped were significantly younger and presented more SOI symptoms. A more detailed analysis showed that alcohol helped especially with sleep onset (40%), less with sleep maintenance (only 11%). In 43% of our patients, alcohol even worsened sleep maintenance, which other studies confirmed ( 16 ). However, in almost half of our patients, alcohol showed no change.
Alcohol is a widely used sleep aid. Asking for the soporific effect of alcohol should become standard during insomnia anamnesis, as well as asking for the soporific effect of drugs (CBD, cannabis, etc.) which have become more and more a topic of sleep research ( 43 ). It is surprising that in our cohort many patients reported a lack of positive effect of alcohol as a sleep aid. It may be that the alcohol amount consumed was not high enough, as we did not ask for specifics.
Symptoms at Time of Insomnia Onset
In our cohort, 57% had SOI symptoms when the insomnia started (in 74% as a combination with other symptoms), 66% had SMI symptoms at the beginning (in 79% as a combination of symptoms), and 40% started with EMA symptoms (in 96% with other symptoms). The majority had a combination of several symptoms. Hence, in most cases of insomnia the sleep disorder started with SMI symptoms (either as single symptom or in combination). We found that patients with single SOI or single EMA were significantly younger than patients with a SOI combination (single: age 47 ± 17 years, combination: age 52 ± 16 years; p < 0.01) or EMA combination (single: age 39 ± 13 years, combination: age 51 ± 15 years; p < 0.01), respectively.
Bjorøy et al. ( 16 ) also investigated subtypes of insomnia in an extensive web-based survey with 64,503 patients who had displayed insomnia for >6 months. Here, 60% of the younger insomniacs (on average 37 years) showed SOI symptoms, either as a combination with SMI and/or EMA symptoms or as a single symptom. Confirming our own results, Bjorøy et al. ( 44 ) also found that SOI as a single symptom was more frequent in younger insomniacs, a SOI symptom combination more frequent in older insomniacs. They revealed further predictors for a symptom combination including female gender, evening chronotype, less education, and being single. While we do not assess aspects such as chronotype, they are important. Literature has shown that there is a higher insomnia prevalence in general in people with an evening chronotype. Insomniacs with a symptom combination also showed a higher comorbidity with depression, anxiety, and a higher use of alcohol and sleeping pills ( 16 ).
Symptom Stability Over Time
Not just the severity, but also the symptoms can change over time. In our cohort, prevalence of SOI and SMI symptoms did not change; EMA symptoms, however, significantly increased from 40 to 45% from first noticing those symptoms to the present (visit to a sleep specialist). Patients with SOI symptoms showed a tendency of an increase of SOI in symptom combination instead of as a single symptom (from 74 to 81%).
An early study of Hohagen et al. ( 17 ) also investigated the progression of insomnia symptoms and possible temporal stability of different patterns in 328 patients (18–65 years). In only 4 months, they discovered a >50% change in SOI, SMI, and EMA symptoms. Only in rare cases did a specific and single symptom insomnia (either SOI, SMI, or EMA) change from one to another single symptom. However, in many single symptom insomnia cases another symptom occurred over time while the first symptom stayed dominant. This tendency was also seen in our cohort regarding the SOI symptoms.

Family History
Almost half of our patient cohort (43%) reported a family history of disturbed sleep/insomnia. These patients were foremost female and presented more EMA symptoms than patients without a family history present.
A specific gene for insomnia is not known but a genetic predisposition cannot be completely ruled out ( 18 , 19 ). A twin study of children revealed a moderate inheritability of insomnia, and another study reported 35% inheritability ( 20 , 21 ).
In our cohort, almost every second patient (43%) reported a trigger. Patients with or without a trigger in our cohort did not differ regarding age, gender, and insomnia symptoms. However, those patients with no triggers showed a tendency to longer insomnia duration then the ones with a trigger. Here, it may be possible that the start of the trigger (whether sudden or slowly, unconsciously developing) may have an impact on the perception of insomnia as a chronic condition. Within our cohort, most frequently named were psychological triggers (e.g., depression, anxiety, trauma, burnout), family triggers (e.g., birth, divorce, custody battles), and medical/biological triggers including surgery and other illnesses. Work triggers (e.g., mobbing/ bulling, job loss) and stress as a separate psychological trigger came next.
Triggers are part of Spielman's theoretical model (1987) of factors causing chronic insomnia. The 3Ps consist of predisposing factors, precipitating factors which trigger acute insomnia, and perpetuating factors ( 22 , 23 ). Triggers would belong to the precipitating factors and may lead to a chronic insomnia. For a working patient, work related stress and job strain may play a bigger role as a trigger and moderator of the insomnia than for those patients that are not working ( 24 ). However, whether the existence of a trigger influences the progression or therapy of insomnia still needs to be further investigated.
Progression of Insomnia
Our patients reported most frequently a negative progression of insomnia (41%); in 26% there were no changes, and only in 7% was there an improvement. On average, the patients suffered from insomnia symptoms for about 11.6 years (range 0–82 years) before seeing a sleep specialist. Patients with predominantly EMA symptoms showed the shortest sleep problem history with 10.2 years (range 0–44 years) compared to patients with SOI or SMI symptoms. About 20% of our patients reported a periodic pattern of symptom severity.
The periodic pattern may be indicative of a non-24 h disorder ( 25 ). A patient with a periodic pattern of insomnia experiences weeks or months long periods with insomnia symptoms alternating with symptom free periods. Green et al. ( 26 ) also investigated the progression of insomnia for over 20 years in 5-year intervals. Patterns included: healthy pattern, episodic pattern, chronic pattern, and a pattern with the development of symptoms in the follow-up period. Chronic insomnia was linked to older women and the working class. It showed that social factors do affect the progression of a sleep disorder, a fact also indicated by Patel et al. ( 27 ) and Arber et al. ( 28 ). There is another distinction of insomnia subtypes by progression introduced by Wu et al. ( 29 ): persistent insomnia, remission, or relapse.
Sleep in Different Environments
Over half of our patients (54%) reported sleeping better in a different environment, including weekends/days with time off from work (51%), vacation (44%), and unfamiliar surroundings in general (22%). The category “unfamiliar surroundings” received the lowest number. Patients may have included job related hotel stays and therefore increased stress level, which may account for the lower number. Patients stating they slept better in a different environment were predominantly younger members of our cohort.
If patients reported sleeping better at weekends or on vacation, this may be an indication that the sleep disorder was caused by work stress or daily routine. In the literature, this is called behavioral induced insufficient sleep ( 30 , 31 ). As only few insomniacs are able to quit their job or family, this category may represent a specific insomnia phenotype. For those, specific interventions are possible including the end of shift work, change to home office work, change from full-time to part-time work, etc.
Further Discussion of Phenotypes
Studies suggest that insomnia is a heterogenic disorder and the identification of different phenotypes or comorbidities is important for personalized treatments ( 45 ). In our study, we presented some new aspects on what insomniacs should be asked during anamnesis and what should be considered during phenotyping. Benjamin et al. ( 32 ) already proposed the following characteristics: (1) life history including demographics, mental and physical health, trauma and life events. This study showed that more women than men and more older people than younger people suffer from insomnia and life events are usually triggers. Such triggers are mostly to be found at home, in health or at work/school, as could also be confirmed with our patients. But who reacts to such a negative trigger with insomnia and why, when, at what age, is not yet known and may possibly have a genetic reason. Further characteristics included (2) subjective sleep quality, (3) fatigue, sleepiness, hyperarousal in the daytime, (4) other sleep disorders, (5) lifetime sleep history, (6) chronotype, (7) depression, anxiety, mood, (8) quality of life, (9) personality, (10) worry, rumination, self-consciousness, sensitivity, (11) dysfunctional beliefs, (12) self-conscious emotion regulation and coping, (13) nocturnal mentation, (14) wake resting state mentation, (15) lifestyle including physical activity and food intake, (16) body temperature, and (17) hedonic evaluation. Other possible non-sleep phenotypes included: MRI, cognition, mood, traits, history of life events, family history, PSG, sleep microstructure, genetics. Blanken et al. ( 11 ) distinguished insomnia subtypes according to the so-called non-sleep categories of life history, mood perception, and personality. Miller et al. ( 33 ) presented an insomnia cluster analysis based on neurocognitive performance, sleep-onset measures of qualitative EEG, and heart rate variability (HRV). They identified two main clusters, depending on duration of sleep (<6 h vs. >6 h). The HRV changes during falling asleep may also play a role, as may the spectral power of the sleep EEG, and parameters from the sleep hypnogram such as sleep onset latency and wake after sleep onset. In one of our own studies, we were able to demonstrate that the increased nocturnal pulse rate and vascular stiffness in insomniacs with low sleep efficiency (<80%) represented an early sign of elevated cardiovascular risk, and thus presented a useful tool for phenotyping insomnia ( 34 ). In the future, other objective characteristics may include biomarkers or radiological features ( 46 , 47 ).
Further characteristics that may play a role but have not yet been mentioned or investigated are the age of the patient during insomnia onset, frequent nocturnal awakenings, the time it takes to see a specialist, and the kind of insomnia onset, slowly progressing or suddenly unexpected. There is no defined age at which the likelihood of insomnia increases, but we know that menopause is a major trigger for women. Grandner et al. ( 35 ) were able to show that getting older alone is not a predictor of insomnia, it rather includes multifactorial events. The question of how long it takes to see a specialist is also part of the Sleep Condition Indicator (SCI) by Espie et al. ( 36 ). They asked whether the insomnia had lasted longer than a year, 1–2, 3–6, or 7–12 months. We can easily agree with such a classification in terms of content. Many patients who wake up frequently at night consider this an insomnia with SMI symptoms. Frequent nocturnal awakenings, but with the ability to fall asleep again straight away, are according to the definition not considered a SMI insomnia. We did not address this in the present study, which presents a limitation. While it is mentioned in the DSM-5 as an independent sign of insomnia, patients affected by frequent nocturnal but subjectively normal sleep lengths and still restful sleep do not (yet) have insomnia. Whether it is an independent phenotype or a preliminary stage of a SMI insomnia should be further examined and defined. It also needs to be clarified whether devices for sleep registration help us with phenotyping. Polysomnography is certainly a very strong phenotypic feature when sleep time is very short, wake times after sleep onset is high and deep and/or dream sleep and sleep efficiency are not optimal. However, the current status is such that it is not suitable for diagnosis ( 48 ). In the near future, technical advances will help to provide objective, long-term sleep data, which are important for diagnosis, subtyping, and therapy for different types of insomnia.
Currently, questionnaires have been used to assess insomnia. The most known questionnaires include the ISI and the Pittsburgh Sleep Quality Index (PSQI). These are valid instruments ( 6 , 49 ). However, there are a number of other questionnaires used for insomnia such as the Amsterdam Resting-State Questionnaire (ARSQ), Dysfunctional Beliefs and Attitudes About Sleep Scale (DBAS), Sleep-Related Behaviors Questionnaire (SRBQ), Sleep Functional Impact Scale (SFIS), Leeds Sleep Evaluation Questionnaire (LSEQ), Glasgow Sleep Effort Scale (GSES) ( 50 – 55 ). In 2014, Espie et al. ( 36 ) introduced the SCI which presented a good instrument for identifying the presence of insomnia and also allowed for time differentiation. Also, the short version with only 2 questions seems valid, where questions are asked about the number of nights in the past month with poor sleep and about the trouble in general caused by sleep ( 56 ). Kalmbach et al. ( 57 ) presented a differentiation between good and bad sleepers based on the Presleep Arousal Scale—Cognitive (PSAS-C) and—Somatic (PSAS-S). People with a high PSAS-C have higher sleep latency and wake times after sleep onset, as well as higher MSLT latency and lower sleep efficiency and total sleep time. The PSAS-C in particular seems to be a good measure of the hyperarousal state. Research and official expert recommendations will show which questionnaires should be favored in clinical practice.
Limitations
Our study intended to encourage and further the discussion on insomnia heterogeneity and the need for possible phenotyping. While we introduced some new aspects of phenotyping, we neither provided a complete list of possible phenotypes nor defined specific clusters. Limitations of our study include the fact that further important aspects (e.g., comorbidity, employment, having children, chronotype, employment etc.) may need consideration. Also, some aspects of the questionnaire will need a more precise definition (e.g., light sleeper, daytime napping, weekend/vacation, alternative treatment, alcohol use), patients were not differentiated regarding sleep duration (<6 h vs. >6 h), and the progression of insomnia was observed retrospectively and not investigated prospectively. While our study was performed with patients of a sleep center, there is also need for phenotyping and thorough assessment of those phenotype characteristics in patients of a primary care setting.
As part of a specific Research Topic introduced by Frontiers on the heterogeneity of insomnia, our study provides further ideas on the already existing approaches to phenotyping insomnia patients. The aim of our study was not to examine all conceivable phenotypic features of insomnia, but to help document specific characteristics with simple questions about the onset and course of insomnia during anamnesis. While the clinical relevance of some of those possible phenotypes is not yet clear (e.g., sleep history, trigger, daytime sleep, sleep in a different environment, alternative treatment, insomnia progression/symptom stability etc.), they should play a role in future research and medical care of insomnia patients. We would like to give an impulse for further research in this area, in order to better differentiate insomnia, thus leading to more effective individualized therapy.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
IF, TP, and VK had the role of supervision and conceptualized the study. IF was responsible for data collection. NL performed data analysis. All authors were involved in visualization and writing including data interpretation, result discussion, and drafting and reviewing the manuscript.
This was not an industry supported study. The study was initiated and funded by the Charité—Universitätsmedizin Berlin owned funding.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank all the patients that participated, and Hendrik Straße and Sandra Zimmermann involved in data entry and processing.
1. Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. (2002) 6:97–111. doi: 10.1053/smrv.2002.0186
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Morin CM, LeBlanc M, Daley M, Gregoire JP, Merette C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. (2006) 7:123–30. doi: 10.1016/j.sleep.2005.08.008
3. Krystal AD, Prather AA, Ashbrook LH. The assessment and management of insomnia: an update. World Psychiatry. (2019) 18:337–52. doi: 10.1002/wps.20674
CrossRef Full Text | Google Scholar
4. American Academy of Sleep Medicine. International Classification of Sleep Disorders . 3rd ed. Darien, IL: American Academy of Sleep Medicine (2014).
Google Scholar
5. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders – Section II: Diagnostic Criteria and Codes: Sleep-Wake Disorders . 5th ed. Arlingten, VA: American Psychiatric Association (2013).
6. Bastien CH, Vallières A, Morin CM. Validation of the nsomnia Severity Index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/S1389-9457(00)00065-4
7. Vgontzas AN, Fernandez-Mendoza J, Liao D, Bixler EO. Insomnia with objective short sleep duration: the most biologically severe phenotype of the disorder. Sleep Med Rev. (2013) 17:241–54. doi: 10.1016/j.smrv.2012.09.005
8. Wallace ML, Lee S, Hall MH, Stone KL, Langsetmo L, Redline S, et al. Heightened sleep propensity: a novel and high-risk sleep health phenotype in older adults. Sleep Health. (2019) 5:630–8. doi: 10.1016/j.sleh.2019.08.001
9. Bathgate CJ, Edinger JD, Krystal AD. Insomnia patients with objective short sleep duration have a blunted response to cognitive behavioral therapy for insomnia. Sleep. (2017) 40: zsw012. doi: 10.1093/sleepj/zsx050.334
10. Lewis KJS, Richards A, Karlsson R, Leonenko G, Jones SE, Jones HJ, et al. Comparison of genetic liability for sleep traits among individuals with bipolar disorder I or II and control participants. JAMA Psychiatry. (2019) 77:303–10. doi: 10.1001/jamapsychiatry.2019.4079
11. Blanken TF, Benjamins JS, Borsboom D, Vermunt JK, Paquola C, Ramautar J, et al. Insomnia disorder subtypes derived from life history and traits of affect and personality. Lancet Psychiatry. (2019) 6:151–63. doi: 10.1016/S2215-0366(18)30464-4
12. Bondar J, Caye A, Chekroud AM, Kieling C. Symptom clusters in adolescent depression and differential response to treatment: a secondary analysis of the treatment for adolescents with depression study randomised trial. Lancet Psychiatry. (2020) 7:337–43. doi: 10.1016/S2215-0366(20)30060-2
13. United States Census Bureau. Source 2019 Population Estimates . (2020). Available online at: https://data.census.gov/cedsci/all?q=Population%20estimates/ (accessed November 2, 2020).
14. Passarella S, Duong MT. Diagnosis and treatment of insomnia. Am J Health Syst Pharm. (2008) 65:927–34. doi: 10.2146/ajhp060640
15. Roehrs TA, Randall S, Harris E, Maan R, Roth T. MSLT in primary insomnia: stability and relation to nocturnal sleep. Sleep. (2011) 34:1657–52. doi: 10.5665/sleep.1426
16. Bjorøy I, Jørgensen VA, Pallesen S, Bjorvatn B. The prevalence of insomnia subtypes in relation to demographic characteristics, anxiety, depression, alcohol consumption and use of hypnotics. Front Psychol. (2020) 11:527. doi: 10.3389/fpsyg.2020.00527
17. Hohagen F, Käppler C, Schramm E, Riemann D, Weyerer S, Berger M. Sleep onset insomnia, sleep maintaining insomnia and insomnia with early morning awakening–temporal stability of subtypes in a longitudinal study on general practice attenders. Sleep. (1994) 17:551–4.
PubMed Abstract | Google Scholar
18. Jansen PR, Watanabe K, Stringer S, Skene N, Bryois J, Hammerschlag AR, et al. Genome-wide analysis of insomnia in 1,331,010 individuals identifies new risk loci and functional pathways. Nat Genet. (2019) 51:394–403. doi: 10.1038/s41588-018-0333-3
19. Stein MB, McCarthy MJ, Chen CY. Genome-wide analysis of insomnia disorder. Mol Psychiatry. (2018) 23:2238–50. doi: 10.1038/s41380-018-0033-5
20. Barclay NL, Gehrman PR, Gregory AM, Eaves LJ, Silberg JL. The heritability of insomnia progression during childhood/adolescence: results from a longitudinal twin study. Sleep. (2015) 38:109–18. doi: 10.5665/sleep.4334
21. Beaulieu-Bonneau S, LeBlanc M, Mérette C, Dauvilliers Y, Morin CM. Family history of insomnia in a population-based sample. Sleep. (2007) 30:1739– 45. doi: 10.1093/sleep/30.12.1739
22. Spielman AJ, Caruso LS, Glovinsky PB. A behavioral-perspective on insomnia treatment. Psychiatr Clin North Am. (1987) 10:541–53. doi: 10.1016/S0193-953X(18)30532-X
23. Perlis ML, Corbitt CB, Kloss JD. Insomnia research: 3Ps and beyond. Sleep Med Rev. (2014) 18:191–93. doi: 10.1016/j.smrv.2014.01.003
24. Halonen JI, Lallukka T, Pentti J, Stenholm S, Rod NH, Virtanen M, et al. Change in job strain as a predictor of change in insomnia symptoms: analyzing observational data as a non-randomized pseudo-trial. Sleep. (2017) 40:zsw007. doi: 10.1093/sleep/zsw007
25. Solaiman SS, Agrawal R. Non-24-hour sleep-wake circadian rhythm disorder in a sighted male with normal functioning. J Clin Sleep Med. (2018) 14:483–4. doi: 10.5664/jcsm.7008
26. Green MJ, Espie CA, Hunt K, Benzeval M. The longitudinal course of insomnia symptoms: inequalities by sex and occupational class among two different age cohorts followed for 20 years in the west of Scotland. Sleep. (2012) 35:815–23. doi: 10.5665/sleep.1882
27. Patel NP, Grandner MA, Xie D, Branas CC, Gooneratne N. “Sleep disparity” in the population: poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health. (2010) 10:475. doi: 10.1186/1471-2458-10-475
28. Arber S, Bote M, Meadows R. Gender and socio-economic patterning of self-reported sleep problems in Britain. Soc Sci Med. (2009) 68:281–9. doi: 10.1016/j.socscimed.2008.10.016
29. Wu MP, Lin HJ, Weng SF, Ho CH, Wang JJ, Hsu YW. Insomnia subtypes and the subsequent risks of stroke: report from a nationally representative cohort. Stroke. (2014) 45:1349–54. doi: 10.1161/STROKEAHA.113.003675
30. Hublin C, Sallinen M. Behaviorally induced insufficient sleep. Sleep Med Clin. (2012) 7:313–23. doi: 10.1016/j.jsmc.2012.03.008
31. Williams AB, Dzierzewski JM, Griffin SC, Lind MJ, Dick D, Rybarczyk BD. Insomnia disorder and behaviorally induced insufficient sleep syndrome: prevalence and relationship to depression in college students. Behav Sleep Med. (2020) 18:275–86. doi: 10.1080/15402002.2019.1578772
32. Benjamins JS, Migliorati F, Dekker K, Wassing R, Moens S, Blanken TF, et al. Insomnia heterogeneity: characteristics to consider for data-driven multivariate subtyping. Sleep Med Rev. (2017) 36:71–81. doi: 10.1016/j.smrv.2016.10.005
33. Miller CB, Bartlett DJ, Mullins AE, Dodds KL, Gordon CJ, Kyle SD, et al. Clusters of insomnia disorder: an exploratory cluster analysis of objective sleep parameters reveals differences in neurocognitive functioning, quantitative EEG, and heart rate variability. Sleep. (2016) 39:1993–2004. doi: 10.5665/sleep.6230
34. Laharnar N, Grote L, Zou D, Hedner J, Sommermeyer D, Straßenburger C, et al. Overnight pulse wave analysis to assess autonomic changes during sleep in insomnia patients and healthy sleepers. PLoS ONE. (2020) 15:e0232589. doi: 10.1371/journal.pone.0232589
35. Grandner MA. Sleep duration across the lifespan: implications for health. Sleep Med Rev. (2012) 16:199–201. doi: 10.1016/j.smrv.2012.02.001
36. Espie CA, Kyle SD, Hames P, Gardani M, Fleming L, Cape J. The sleep condition indicator: a clinical screening tool to evaluate insomnia disorder. BMJ Open. (2014) 4:e004183. doi: 10.1136/bmjopen-2013-004183
37. Regestein QR, Bambrosia J, Hallett M, Murawski B, Paine M. Daytime alertness in patients with insomnia. Am J Psychiatry. (1993) 150:1529–34. doi: 10.1176/ajp.150.10.1529
38. Khassawneh BY, Bathgate CJ, Tsai SC, Edinger JD. Neurocognitive performance in insomnia disorder: the impact of hyperarousal and short sleep duration. J Sleep Res. (2018) 27:e12747. doi: 10.1111/jsr.12747
39. Li Y, Vgontzas AN, Fernandez-Mendoza J, Bixler EO, Sun Y, Zhou J, et al. Insomnia with physiological hyperarousal is associated with hypertension. Hypertension. (2015) 65:644–50. doi: 10.1161/HYPERTENSIONAHA.114.04604
40. Drake C, Richardson G, Roehrs T, Scofield H, Roth T. Vulnerability to stress-related sleep disturbance and hyperarousal. Sleep. (2004) 27:285–91. doi: 10.1093/sleep/27.2.285
41. Espie CA, Kyle SD, Hames P, Cyhlarova E, Benzeval M. The daytime impact of DSM-5 insomnia disorder: comparative analysis of insomnia subtypes from the Great British Sleep Survey. J Clin Psychiatry. (2012) 73:e1478–84. doi: 10.4088/JCP.12m07954
42. Baglioni C, Altena E, Bjorvatn B, Blom K, Bothelius K, Devoto A, et al. The European academy for cognitive behavioural therapy for insomnia: an initiative of the European insomnia network to promote implementation and dissemination of treatment. J Sleep Res. (2020) 29:e12967. doi: 10.1111/jsr.12967
43. Suraev A, Grunstein RR, Marshall NS, D'Rozario AL, Gordon CJ, Bartlett DJ, et al. Cannabidiol (CBD) and Δ(9)-tetrahydrocannabinol (THC) for chronic insomnia disorder ('CANSLEEP' trial): protocol for a randomised, placebo-controlled, double-blinded, proof-of-concept trial. BMJ Open. (2020) 10:e034421. doi: 10.1136/bmjopen-2019-034421
44. Merikanto I, Kronholm E, Peltonen M, Laatikainen T, Lahti T, Partonen T. Relation of chronotype to sleep complaints in the general Finnish population. Chronobiol Int . (2012) 29:311–7. doi: 10.3109/07420528.2012.655870
45. Bjorvatn B, Jernelöv S, Pallesen S. Insomnia – A heterogenic disorder often comorbid with psychological and somatic disorders and diseases: a narrative review with focus on diagnostic and treatment challenges. Front Psychol. (2021) 12:639198. doi: 10.3389/fpsyg.2021.639198
46. Mikoteit T, Brand S, Eckert A, Holsboer-Trachsler E, Beck J. Brain-derived neurotrophic factor is a biomarker for subjective insomnia but not objectively assessable poor sleep continuity. J Psychiatr Res. (2019) 110:103–9. doi: 10.1016/j.jpsychires.2018.12.020
47. Neumann N, Lotze M, Domin M. Sex-specific association of poor sleep quality with gray matter volume. Sleep. (2020) : zsaa035. doi: 10.1093/sleep/zsaa035
48. Collen J, York CM. Wrist wearables: more questions than answers? J Clin Sleep Med. (2019) 15:1077–78. doi: 10.5664/jcsm.7858
49. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index – a new instrument for psychiatric practice and research. Psychiat Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
50. Espie CA, Inglis SJ, Harvey L, Tessier S. Insomniacs' attributions: psychometric properties of the dysfunctional beliefs and attitudes about sleep scale and the sleep disturbance questionnaire. J Psychosom Res. (2009) 48:141–8. doi: 10.1016/s0022-3999(99)00090-2
51. Palagini L, Cellini N, Mauri M, Mazzei I, Simprage S, dell'Osso L, et al. Multiple phenotypes of resting-state cognition are altered in insomnia disorder. Sleep Health. (2016) 2:239–45. doi: 10.1016/j.sleh.2016.05.003
52. Ree MJ, Harvey AG. Investigating safety behaviours in insomnia: the development of the sleep-related behaviours questionnaire (SRBQ). Behav Change. (2004) 21:26–36. doi: 10.1375/bech.21.1.26.35971
53. Bell C, McLeod LD, Nelson LM, Fehnel SE, Zografos LJ, Bowers B. Development and psychometric evaluation of a new patient-reported outcome instrument measuring the functional impact of insomnia. Qual Life Res. (2011) 20:1457–68. doi: 10.1007/s11136-011-9885-8
54. Tarrasch R1, Laudon M, Zisapel N. Cross-cultural validation of the Leeds Sleep Evaluation Questionnaire (LSEQ) in insomnia patients. Hum Psychopharmacol. (2003) 18:603–10. doi: 10.1002/hup.534
55. Broomfield NM, Espie CA. Towards a valid, reliable measure of sleep effort. J Sleep Res. (2005) 14:401–7. doi: 10.1111/j.1365-2869.2005.00481.x
56. Luik AI, Machado PF, Siriwardena N, Espie CA. Screening for insomnia in primary care: using a two-item version of the Sleep Condition Indicator. Br J Gen Pract. (2019) 69:79–80. doi: 10.3399/bjgp19X701045
57. Kalmbach DA, Cheng P, O'Brien LM, Swanson LM, Sangha R, Sen S, et al. A randomized controlled trial of digital cognitive behavioral therapy for insomnia in pregnant women. Sleep Med. (2020) 72:82–92. doi: 10.1016/j.sleep.2020.03.016
Keywords: insomnia, phenotypes, subtypes, heterogeneity, symptom, progression, questionnaire, screening
Citation: Fietze I, Laharnar N, Koellner V and Penzel T (2021) The Different Faces of Insomnia. Front. Psychiatry 12:683943. doi: 10.3389/fpsyt.2021.683943
Received: 22 March 2021; Accepted: 24 May 2021; Published: 29 June 2021.
Reviewed by:
Copyright © 2021 Fietze, Laharnar, Koellner and Penzel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Naima Laharnar, naima.laharnar@charite.de
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

- Essay Topic Generator
- Essay Grader
- Reference Finder
- AI Outline Generator
- Paragraph Expander
- Essay Expander
- Literature Review Generator
- Thesis Generator
- Text Editing Tools
- AI Rewording Tool
- AI Sentence Rewriter
- AI Article Spinner
- AI Grammar Checker
- Spell Checker
- PDF Spell Check
- Paragraph Checker
- Free AI Essay Writer
- Paraphraser
- Grammar Checker
- Citation Generator
- Plagiarism Checker
- AI Detector
- AI Essay Checker
- Proofreading Service
- Editing Service
- AI Writing Guides
- AI Detection Guides
- Citation Guides
- Grammar Guides
- Paraphrasing Guides
- Plagiarism Guides
- Summary Writing Guides
- STEM Guides
- Humanities Guides
- Language Learning Guides
- Coding Guides
- Top Lists and Recommendations
- AI Detectors
- AI Writing Services
- Coding Homework Help
- Citation Generators
- Editing Websites
- Essay Writing Websites
- Language Learning Websites
- Math Solvers
- Paraphrasers
- Plagiarism Checkers
- Reference Finders
- Spell Checkers
- Summarizers
- Tutoring Websites
- Essay Checkers
- Essay Topic Finders
Most Popular
14 days ago
Works Cited
- Colten, Harvey R. “Extent and Health Consequences of Chronic Sleep Loss and Sleep Disorders—Sleep Disorders and Sleep Deprivation.” National Center for Biotechnology Information . U.S. National Library of Medicine, 01 Jan. 1970. Web. 03 Nov. 2016. .
- “Dangers of Getting Too Little Sleep.” HealthCommunities . N.p., n.d. Web. 03 Nov. 2016. .
- “Chronic Insomnia’s Dangerous Side-Effects.” Newsweek . Newsweek, 23 Aug. 2009. Web. 03 Nov. 2016. .
- “Chronic Insomnia Linked to Increased Risk of Death.” Mercola.com . N.p., n.d. Web. 03 Nov. 2016. .
Follow us on Reddit for more insights and updates.
Comments (0)
Welcome to A*Help comments!
We’re all about debate and discussion at A*Help.
We value the diverse opinions of users, so you may find points of view that you don’t agree with. And that’s cool. However, there are certain things we’re not OK with: attempts to manipulate our data in any way, for example, or the posting of discriminative, offensive, hateful, or disparaging material.
Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
More from Cause and Effect Essay Examples and Samples 2024

Jul 18 2023
How Your Childhood Affects Your Love Style Essay Sample Example
Apr 15 2019
How the Harry Potter Series Became So Popular Essay Sample, Example

Apr 05 2019
Why Our Ancestors Started to Walk on Two Feet Essay Sample, Example
Related writing guides, writing a cause and effect essay.
Remember Me
What is your profession ? Student Teacher Writer Other
Forgotten Password?
Username or Email
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Psychiatry
- v.54(4); Oct-Dec 2012
Behavioral interventions for insomnia: Theory and practice
Mahendra p. sharma.
Department of Clinical Psychology, National Institute of Mental Health and Neurosciences, Bangalore, Karnataka, India
Chittaranjan Andrade
1 Department of Psychopharmacology, National Institute of Mental Health and Neurosciences, Bangalore, Karnataka, India
Insomnia is a general clinical term that refers to a difficulty in initiating or maintaining sleep. Insomnia is widely prevalent in the general population, especially in the elderly and in those with medical and psychiatric disorders. Hypnotic drug treatments of insomnia are effective but are associated with potential disadvantages. This article presents an overview of behavioral interventions for insomnia. Behavioral interventions for insomnia include relaxation training, stimulus control therapy, sleep restriction therapy, sleep hygiene, paradoxical intention therapy, cognitive restructuring, and other approaches. These are briefly explained. Research indicates that behavioral interventions are efficacious, effective, and likely cost-effective treatments for insomnia that yield reliable, robust, and long-term benefits in adults of all ages. Detailed guidance is provided for the practical management of patients with insomnia.
INTRODUCTION
Insomnia is the most common sleep disorder. Insomnia is a general clinical term that refers to the difficulty in initiating or maintaining sleep. It may present as an independent problem (primary insomnia) or as part of a coexisting medical or psychiatric condition (secondary insomnia). According to ICD-10,[ 1 ] nonorganic insomnia (F 51.0) is defined as a problem in initiating and/or maintaining sleep or the complaint of nonrestorative sleep that occurs on at least three nights a week for at least a month, and is associated with daytime distress or impairment. The diagnosis primary insomnia (307.42) in DSM-IV[ 2 ] is used to distinguish insomnia that is considered to be a distinct diagnostic entity from insomnia that is a symptom of an underlying medical and/or psychiatric condition. The DSM lists insomnia related to other Axis I or Axis II disorders as distinct from primary insomnia.
Primary insomnia is referred to as “psychophysiologic insomnia” in the international classification of sleep disorders-revised (ICSD-R) proposed by the American Sleep Disorders Association and endorsed by the American Academy of Sleep Medicine.[ 3 ] The ICSD-R definition is more directly tied to the etiological underpinnings of the disorder and it suggests how insomnia is initiated and maintained. Psychophysiologic insomnia is described as “a disorder of somatized tension and learned sleep preventing associations that results in a complaint of insomnia and associated decreased functioning during wakefulness.”[ 4 ] “Somatized tension” refers to either the patient's subjective sense of, or objective measures of, somatic hyperarousal while attempting to sleep. Somatic hyperarousal is characterized by peripheral nervous system activity which is commonly marked by increased muscle tension, rapid heart rate, sweating, and related symptoms. “Learned sleep-preventing associations” refer to the pattern of pre-sleep arousal that appears to be classically conditioned to the bedroom environment, where intrusive presleep cognitions, racing thoughts, and rumination are often taken as indicators of presleep arousal.[ 4 ]
MAGNITUDE OF THE PROBLEM
Insomnia is widely prevalent and is reported to occur in up to one-third of the adult population.[ 5 ] Persistent sleep problems have been reported by 10-15% of adults.[ 6 , 7 ] The prevalence of sleep problems among women and older adults is even higher.[ 8 , 9 ] Although more than half of primary care patients may experience insomnia, only about one-third report this problem to their physicians[ 10 ] and only 5% seek treatment.[ 6 ] Despite the very high economic cost of insomnia in terms of lost productivity and accidents,[ 11 ] the vast majority of persons with insomnia remain untreated.[ 7 ] Two-thirds of patients with insomnia report a poor understanding of treatment options, and many turn to alcohol (28%) or untested over-the-counter remedies (23%).[ 6 ]
Various psychological, behavioral, and biological factors have been implicated in the development and maintenance of insomnia as a disorder. However, the etiology of insomnia remains under investigation and is still not fully understood. Two types of treatment for insomnia have received adequate empirical support: hypnotic medications and cognitive behavioral interventions.
BEHAVIORAL INTERVENTIONS FOR INSOMNIA: CHRONOLOGY
Early psychological treatments for insomnia focused on primary insomnia. Application of behavioral therapeutic approaches in the treatment of insomnia began with interventions such as systematic desensitization,[ 12 ] relaxation,[ 13 ] hypnosis,[ 14 ] biofeedback,[ 15 ] and paradoxical intention[ 16 ] which targeted hyperarousal associated with insomnia. During the 1970s, stimulus control therapy for insomnia was introduced.[ 17 ] In the late 1980s, a new behavioral intervention, sleep restriction, was introduced.[ 18 ] Around the same time, the application of cognitive restructuring for dysfunctional beliefs related to insomnia was proposed[ 19 ] and subsequently formalized and integrated into several multi-component treatments of insomnia.[ 20 ]
Effective treatment of insomnia must address the cognitive and behavioral mechanisms that maintain insomnia.[ 21 ] Therefore, the best practices of nonpharmacological treatments for insomnia target both dysfunctional attitudes and beliefs about sleep and maladaptive behaviors (increased time in bed) that maintain abnormal sleep patterns.[ 22 ] In recent years, cognitive behavioral therapy for insomnia (CBT-I), which combines different behavioral therapies and cognitive therapy techniques, has emerged as preferred treatment for insomnia.
RELAXATION THERAPY
Relaxation therapy is based on observations that insomnia patients often display high levels of physiologic, cognitive, and/or emotional arousal, both at night and during the daytime.[ 23 ] A number of formal relaxation therapies have been applied to insomnia since such therapies reduce the sleep-related performance anxiety and bedtime arousal common to this condition.[ 24 – 27 ] This type of intervention may be most suitable for patients who characterize their insomnia as an “inability to relax” and/or for patients who present with multiple somatic complaints. Progressive muscle relaxation (PMR), autogenic training, and biofeedback are aimed at reducing somatic arousal (e.g., muscle tension). Biofeedback is a form of relaxation that provides sensory feedback (visual or auditory, either mechanically or with computers and amplifiers) to help patients learn how to control physiological parameters such as galvanic skin response or muscle tension in order to reduce somatic arousal.
Attention-focusing procedures such as imagery training or meditation seek to lower pre-sleep cognitive arousal (e.g., intrusive thoughts, racing mind).[ 28 ] Abdominal breathing is often a component of various relaxation techniques, or it may be used alone. Relaxation therapy is useful for both sleep onset and sleep maintenance insomnia. Regardless of the specific relaxation strategy employed, treatment typically involves conducting specific treatment exercises, teaching relaxation skills, and regular practice with a trained professional over multiple treatment sessions. Most practitioners select the optimal relaxation method based upon which technique is easiest for the patient to learn, and most consistent with how the patient manifests arousal. Some patients, especially those with a history of panic disorder or performance anxiety, might experience a paradoxical response to relaxation techniques. If this occurs with one form of relaxation technique, other suitable techniques may be considered. A detailed discussion of the subject was provided by Perlis et al .[ 29 ]
STIMULUS CONTROL THERAPY
Bootzin[ 17 ] pioneered the use of stimulus control instructions as a behavioral treatment for insomnia. This set of instructions is designed to help the patient with insomnia to establish a consistent sleep-wake rhythm, strengthen the bed and bedroom as cues for sleep, and weaken them as cues for activities that might interfere with sleep. The stimulus control instructions, as described by Bootzin et al .,[ 30 ] address the following points: when to go to sleep; what activities are permitted or disallowed when in bed; what to do if sleep is not attained within a reasonable period of time; when to rise in the morning; and daytime napping.
Stimulus control therapy originated from an operant learning analysis in which falling asleep is conceptualized as an instrumental act intended to produce reinforcement (i.e., sleep). Stimuli associated with sleep become discriminative stimuli for the occurrence of reinforcement. Difficulty in falling asleep, or in returning to sleep after awakening, may be due to inadequate stimulus control.[ 30 , 31 ] The operant conditioning goals of stimulus control are to strengthen sleep-compatible associations with the bed and bedroom environment and to remove sleep incompatible ones; the classical conditioning goals are to break the association between the bedroom and insomnia. The stimulus control instructions decrease the bed and bedroom as cues for arousal and re-establish the bed and bedroom as strong cues for sleep. They additionally promote a more regular circadian sleep–wake cycle.
It is also necessary to caution the patients not to “clock-watch,” an action that reinforces wakefulness. Instead, patients should rise from bed if they think that 15-20 minutes has passed, without sleep, after retiring. One advantage of this instruction is that patients learn to better identify what signs (e.g., yawning, tired eyes, inability to keep eyes open, nodding off) manifest when they are actually sleepy rather than merely fatigued.[ 32 ]
SLEEP RESTRICTION THERAPY
The longer a person stays awake, the less likely it is that he will be able to remain awake, and the more likely he is to start to feel sleepy. This increasing sleepiness is known as the homeostatic sleep drive. Spielman et al .[ 18 ] developed sleep restriction therapy for insomnia based on this biological drive. It is a behavioral technique which is essentially a systematic, controlled, partial form of sleep deprivation designed to consolidate sleep rapidly and then gradually increase the scheduled time allotted for sleep when adequate sleep efficiency has been achieved. The goal of sleep restriction is to regulate the sleep-wake cycle by tailoring the time spent in bed to the patient's true sleep need.[ 18 ] It begins by calculating average total sleep time, which is accomplished by completing sleep logs that record the duration of time in bed and the total duration of time spent sleeping. If a person with insomnia stays in bed for 9 h per night but is only sleeping for 6 h per night, he is advised to limit the time in bed to 6 h, which is his “sleep window.” Therapy seeks to consolidate sleep such that time passed in bed is spent sleeping rather than awake. The sleep efficacy ([total sleep time/total in bed] × 100) goal for a person with insomnia should be around 85%.
Sleep opportunity is never restricted to less than 5 h because, otherwise, the patient may suffer excessive daytime drowsiness. If a person's sleep efficacy is greater than 90% in any week, he or she is given an additional 15-20 min of time each night. Weekly sleep efficacy of less than 80% requires a decrease in sleep window by 15-20 min.
The consistent bedtime and wake time required by this procedure helps re-entrain and strengthen circadian rhythms which are dysregulated with the irregular sleep schedules common to people with insomnia. Sleep restriction therapy is generally combined with stimulus control therapy or other forms of therapy. From a classical conditioning standpoint, sleep restriction increases the establishing operation of sleepiness, which makes the individual more likely to fall asleep when he goes to bed.[ 32 ]
SLEEP HYGIENE EDUCATION
This is another behavioral intervention that is primarily psychoeducational in nature, wherein patients are provided instructions about healthy sleep habits.[ 33 ] Sleep hygiene involves educating the patient about health practices such as diet, exercise, and substance use, and about environmental factors such as light, noise, temperature, and bedding, that is, important personal and environmental factors that can be positive or negative for sleep. Sleep hygiene recommendations have been listed by the National Institute of Health,[ 34 ] Perlis and Youngstead,[ 35 ] Perlis et al .,[ 29 ] and others. Although poor sleep hygiene may not be the sole cause of insomnia, it can perpetuate insomnia. Therefore, sleep hygiene education is a necessary addition to other established known beneficial treatments.[ 36 ]
PARADOXICAL INTENTION THERAPY
Paradox has been part of psychological theory and practice for long. Frankl's[ 16 ] concern that patients took control of their symptoms arose from an existential philosophy. Paradoxical intention is concerned with increasing the frequency of responses that already occur too often. In other words, paradoxical intention involves prescribing the symptom. This intervention is thought to be suitable for insomnia when there is intense preoccupation about sleep, sleep loss, and its consequences.[ 37 ] It is based on the concept that performance anxiety prevents proper sleep. Paradoxical intention reduces performance anxiety about falling asleep by instructing patients to do the opposite - get into bed and stay awake. When the individual with insomnia engages in the most feared behavior, staying awake, performance anxiety related to trying to fall asleep slowly diminishes. Paradoxical intention may be included as an element of multi-component CBT.
COGNITIVE THERAPY
There are several forms of cognitive therapy for insomnia. These can involve didactic focus, paradoxical intention, distraction and imagery techniques, and cognitive restructuring. There is an attempt to alter dysfunctional attitudes and beliefs about sleep, the consequences of which can be insomnia. Cognitive therapy also addresses catastrophization about the consequences of poor sleep. Patients are helped to reconceptualize the realities of their beliefs; this, in turn, helps decrease the sleep-interfering anxiety that generally increases as bedtime approaches.[ 29 ]
COGNITIVE BEHAVIOR THERAPY FOR INSOMNIA
Cognitive behavior therapy for insomnia (CBT-I) refers to combinations of behavioral techniques and conventional cognitive restructuring, and has evolved as a multi-component treatment approach. According to Pigeon,[ 38 ] CBT-I is based on (a) the application of both operant and classical conditioning paradigms in the form of stimulus control instructions[ 39 ] ; (b) the correction of sleep-interfering behaviors through sleep hygiene education[ 40 ] ; (c) the recognition and reduction of hyperarousal precursors of insomnia[ 41 ] ; (d) the improvement of circadian and sleep homeostasis regulation of sleep through sleep scheduling and limited, partial sleep deprivation[ 42 ] ; and (e) the use of cognitive therapy.[ 43 ] The individual components of CBT-I include psychoeducation, behavioral strategies, cognitive therapy, and relaxation training. Whereas these can be delivered separately as monotherapies, multicomponent CBT-I is the preferred approach.[ 38 ]
EVIDENCE FOR THE EFFICACY OF COGNITIVE BEHAVIORAL INTERVENTIONS FOR INSOMNIA
Recently, the American Academy of Sleep Medicine updated practice parameters for the psychological and behavioral treatment of insomnia in adults.[ 44 ] In this document, a treatment was designated as a standard treatment if it had the highest level of empirical validation (e.g., at least two placebo-controlled randomized clinical trials). If the treatment was effective but had a lower level of empirical validation (e.g., only one placebo-controlled randomized clinical trial along with clinical case studies, waitlist control studies, etc.), it was designated as guideline treatment.
Although pharmacotherapy has been found to be useful for acute insomnia, psychological interventions which mainly include cognitive and behavioral interventions are considered better choices for primary insomnia, chronic insomnia, and insomnia comorbid with other psychological disorders and medical conditions.[ 44 – 47 ] CBT-I, which combines different behavioral therapies and cognitive therapy techniques, has emerged as a preferred treatment for insomnia. Hypnotic medications for insomnia carry an advantage in that their benefits are immediate and often ensured. However, hypnotic medications can cause early morning hangover, daytime drowsiness, psychomotor impairment, cognitive impairment, and adverse consequences associated therewith. Hypnotic medications may also be associated with tolerance and dependence. Finally, hypnotics are effective only for as long as they are used, whereas once behavioral interventions are initiated and become a lifestyle practice, their efficacy can be expected to persist. This may be why long-term outcomes of insomnia tend to be better with behavioral interventions than with pharmacological interventions.[ 48 , 49 ]
Relaxation therapy for insomnia includes several relaxation methods. Most research evidence favors PMR as a treatment for insomnia. This treatment has been found to be more effective than placebo, waitlist, and no-treatment controls.[ 20 , 44 , 50 ] Biofeedback as a form of relaxation therapy has been identified as a guideline treatment for insomnia as only one placebo-controlled trial has been performed to date and the findings of two waitlist control studies were mixed. Biofeedback is often paired with some form of relaxation exercise such as PMR. The results are comparable to PMR alone. This makes it difficult to make a case for biofeedback, given that it involves expensive equipment.[ 32 ]
Stimulus control therapy has been found to be the most effective single treatment and is recommended as a standard treatment for chronic insomnia.[ 44 , 51 ] Whereas, sleep restriction therapy is also found to be efficacious[ 20 ] and the AASM lists it as a guideline treatment because fewer RCTs have examined it as a single treatment (most behavioral intervention studies combined stimulus control with sleep restriction, making it impossible to determine the efficacy of sleep restriction, by itself). It is worth noting, however, that sleep restriction has effect sizes equal to that with stimulus control therapy.[ 44 ]
Research on paradoxical intention has produced mixed results, with four studies showing it to be more effective than controls and two studies finding no advantage. Paradoxical intention is rarely recommended over more empirically supported methods or methods included in multimodal therapy, but may be useful when patients do not benefit from other methods.[ 32 , 44 , 50 ]
Sleep hygiene has been found to be ineffective as monotherapy.[ 52 ] Whether sleep hygiene is effective when combined with other approaches cannot be determined from the available data.[ 44 ] Sleep hygiene, therefore, is perhaps best delivered in an interactive and coexperimenter approach where the therapist and patient review each of the sleep hygiene items, discuss how each item is related to sleep, and consider whether any of the items apply to the patient. The simplicity of sleep hygiene may explain why it is the technique with which most nonspecialists are familiar, and why it is often the only treatment offered to patients; and its failure in monotherapy may explain why clinicians advising sleep hygiene often draw an inappropriate conclusion that behavioral treatments are ineffective for insomnia.[ 32 ]
A large number of studies have been conducted to examine whether cognitive behavioral therapy for insomnia (CBT-I) can work under controlled conditions (i.e., efficacy studies) as well as whether CBT-I does work in applied settings (i.e., effectiveness studies). The efficacy and effectiveness research provides strong support for CBT-I.[ 53 ] More than 50 randomized controlled clinical trials have shown that CBI-I results in reliable and robust improvements across different subjective and objective measures of sleep disturbance.[ 54 ] While the individual components of CBT-I (psychoeducation, behavioral strategies, cognitive therapy, and relaxation training) can be delivered as monotherapies, multicomponent CBT-I is the preferred approach.[ 55 ] Additionally, cognitive behavioral interventions are as effective as pharmacological treatments in the short term and more effective in the long term.[ 45 , 48 , 56 , 57 ] Meta-analyses also show that cognitive and behavioral therapies are significantly more effective than placebo in improving sleep in patients with primary insomnia.[ 20 , 50 ] Cognitive and behavioral approaches are also effective in the elderly.[ 58 – 60 ] Whereas research on CBT for insomnia secondary to medical conditions is limited, data suggest that CBT is efficacious for insomnia secondary to both chronic pain and breast cancer.[ 53 ]
Insomnia is widely prevalent in the general population and most patients with insomnia remain untreated. Hypnotic drugs and CBT interventions are both effective intervention with the latter associated with several advantages over the former. CBT-I is a multi-component cognitive-behavioral treatment approach and has received sufficient validation by researchers and clinicians. Available data suggest that CBT-I is an efficacious, and likely cost-effective treatment for insomnia that yields reliable, robust, and long-term benefits among younger as well as older adults. The delivery of formal CBT-I will require professional training on the part of the therapist. However, simple behavioral procedures and techniques can be taught to most patients with insomnia, and these are presented in the Appendix .[ 61 ]
APPENDIX: GUIDELINES FOR SLEEPING BETTER AT NIGHT
The best way to treat insomnia is to identify and remedy the cause: medical, psychiatric, or other. This should be done wherever possible. It is also important, and helpful, to implement behavioral measures; these are described below. None of the suggestions here is an absolute requirement; however, most are based on good scientific evidence and are, therefore, best adhered to. Importantly, the guidelines need to be tailored to individual contexts; what is appropriate for one patient may not be suitable for another.
During the Day
Do not nap during the day unless you have good reason to believe that doing so improves the quality of your life. If you do nap during the day, you must recognize that your nighttime sleep requirement will be correspondingly shortened.
Note . Some persons function with better efficiency if they take a short afternoon nap and one or more short daytime naps may even be desirable in elderly persons.
Exercise moderately during the day so that you are physically “tired out” at night.
Note . Moderate physical fatigue can be relaxing; excessive physical fatigue can be counterproductive because it could result in aches and pains that interfere with sleep. Exercise too late in the evening could result in arousal that persists and prevents sleep at night.
Before bedtime
Taper off your physical activity as you approach your bedtime; otherwise, you will be too alert to sleep. Therefore, you should not exercise vigorously for 4-6 h before you retire; you should not involve yourself in any moderate exertion for 2-4 h before you retire.
Note . Simple stretching or a little walk around the house can be relaxing. The guiding principle is that you should be made more relaxed and not more alert by whatever you do. If whatever you do makes you feel flushed and breathe heavily, or makes your heart beat faster, it will probably keep you awake for longer.
Note . Sexual activity is an exception to the rule because its culmination results in physical and mental relaxation.
Do not consume so much fluid during the late evening that you need to rise in the night to empty your bladder. Avoid alcohol intake and smoking in the late evening; alcohol and nicotine are known to result in disturbed sleep. Avoid eating or drinking much during the hour or two prior to retiring; in particular, avoid stimulating foods (e.g., chocolate, especially dark chocolate) or beverages (e.g., coffee, tea, cocoa, cola drinks). However, do not go to bed hungry.
Note . A glass of warm milk or a carbohydrate snack may, however, help you feel drowsy.
Do not have a cold bath during the hour or two before retiring; this will make you more alert. Likewise, do not have a hot bath during the hour or two before retiring; your body needs to feel cool if you are to fall asleep. Bathing is, itself, a physical activity which may make you more active and alert.
Before bedtime, avoid laughing, joking, speaking on the telephone, or any social activity that gives you a lift or makes you think more. Likewise, avoid any debate, argument, or any social activity that makes you irritable or angry. And do not listen to loud, peppy music because of its activating effects.
Note . Light, desultory conversation with a family member before bedtime can be relaxing.
Avoid mental activity before retiring. Watching an entertaining or engrossing program on television, doing crosswords, playing chess, or concentrating on any other task can make you more alert.
Note . This may not apply to activities that you consider work. For example, attending to your accounts or other paperwork may tire you enough to make you look forward to closing up and going to bed.
Avoid doing anything that may make you alert or annoyed before bedtime. Do not think about emotionally disturbing matters. If you find yourself tense, alert, or irritable, do something that is calming or mentally relaxing in the 5-20 min before you retire. This includes meditating, praying, reading, or pottering around the house, or engaging in a relaxing conversation or any other activity which helps you unwind.
Note . Such relaxing activities are a useful routine but become especially important if you are tense and edgy as a result of the events of the previous hours or the day.
Avoid exposure to bright lights for the 5-10 min or so before you retire. This includes looking at the television. Bright light will tend to make you more alert.
Avoid taking sleeping pills unless you absolutely must. Sleeping pills are habit-forming.
Note . If you slept poorly during the previous night you will tend to sleep poorly during the present night as well. This is because your body can get into a rhythm of sleeping less even though sleeping less leaves you tired and irritable. Furthermore, loss of sleep on a previous night can make you too tense and too tired to be able to relax sufficiently to be able to sleep easily on the present night. In such circumstances, the one-off use of a sleeping pill may sometimes be acceptable. It can break the rhythm of poor sleep to which your body has become accustomed.
Note . Melatonin normalizes biorhythms, cools the body, and promotes normal sleep. Melatonin is not a habit-forming drug. However, melatonin does not work well as a hypnotic for everyone.
Plan your day so that you are able to retire at approximately the same time every night. This will help your body get conditioned to feeling sleepy at that time each night.
Retire only when you are tired; if you go to bed when you feel wide awake, you will toss and turn and find it hard to fall asleep.
If you feel sleepy, go to bed soon. If you postpone retiring, your body will slowly start becoming more alert, and you will find it harder to fall asleep.
Preferably, sleep in the same place every night. This will help your body get conditioned to feeling sleepy when you head for your bed. If you change your sleeping arrangements frequently, your body may take some time to adjust to the change before you begin to feel sleepy.
Reduce environmental stimulation in your sleep zone. Use minimum lighting (or none at all), avoid noise, disconnect your phone, and do whatever else is necessary to ensure that there is no disturbance.
Note . Some persons find it easier to fall asleep if there is soft music playing. Others find that music captures their attention and prevents them from sleeping.
If disturbance due to traffic noise, festival celebration, or any other source is inevitable, it is important that you adopt an accepting attitude much as you would accept the sound of a ceiling fan. Allow the sound to recede into the background. If you resent the sound, you will begin to pay attention to it and you will not be able to sleep. Or, if you resent it, your anger may not allow you to sleep.
Ensure that your pillow and bed are comfortable. Ensure that you have an adequate number of sheets and blankets for cold weather, or that the cooling arrangements are adequate during summer.
Take measures to minimize pests such as mosquitoes.
When in bed, avoid thinking about matters that provoke mental or emotional activity. Thus, do not address an engrossing problem, relive an exciting happening, brood over an unhappy event, think about an irritating or anxiety-provoking issue, etc. Just think about pleasant or peaceful matters, mediate, or pray.
Do not concentrate on trying to fall asleep, worry that you are not falling asleep, or time yourself to falling asleep. Do not periodically check the time. Do not look at the clock if you are awake at night. This will only make you feel alert, frustrated, or annoyed.
Ways in which you can blank out thoughts that keep you awake include the following.
- (1) Direct your attention to restful sounds in your environment, such as distant traffic noise
- (2) Visualize a peaceful scene and imagine yourself in it
- (3) Focus on the air moving in and out of your lungs
- (4) Systematically relax your body, part by part, and imagine your body sinking heavily into the mattress Start with your toes, then your legs, then your thighs, and move upwards, gradually, till you reach your head.
If you sit or stand in the same place for any length of time, you will begin to feel restless. Likewise, if you are unable to fall asleep within a reasonable period of time, you will begin to toss and turn and feel irritable and restless. So if you cannot fall asleep within 15-30 min, the moment you begin to feel restless, get up. Read or listen to soothing music in a dimly lit environment and return to bed only when you feel tired. Repeat this process as many times as it takes you to feel sleepy and fall asleep.
If you awake in the middle of the night and have to get up, avoid bright lights, physical activity, mental activity, or anything that makes you alert.
General suggestions
Rise at the same time every morning, preferably at a reasonable hour, irrespective of the length of time for which you have slept during the night. If you did not sleep well the previous night, the loss of sleep will tend to make it easier for you to fall asleep on the present night. However, if you sleep late into the morning, you will tend to find it difficult to sleep at night.
Do not use your bed for activities other than sex or sleeping; if you do, you may become conditioned to feeling alert in bed.
Adopt stress-management and time-management strategies to reduce the anxiety or other emotional disturbances associated with your lifestyle. Likewise, take up hobbies and recreational pursuits that help you unwind. Make sure that you receive treatment for any medical, psychiatric, or other conditions that may interfere with your sleep. Check with your doctor whether any of the medicines that you are receiving interfere with sleep; if yes, ask whether these can be changed.
Source of Support: Nil
Conflict of Interest: None declared.

IMAGES
VIDEO
COMMENTS
Introduction. The prevalence of insomnia in the general population ranges between 8-40%, depending on the definition used. While 20-30% of the general population has poor sleep (i.e., insomnia symptoms of difficulty initiating or maintaining sleep, early morning awakening, or non-restorative sleep at any given time), another 8-10% of the population suffers from chronic insomnia. 1,2 Also ...
Abstract. In contrast to the association of insomnia with mental health, its association with physical health has remained largely unexplored until recently. Based on findings that insomnia with objective short sleep duration is associated with activation of both limbs of the stress system and other indices of physiological hyperarousal, which ...
Insomnia is a widespread and debilitating condition that can affect anyone, including children [1], adults, and the elderly [2]. It is characterized by difficulties initiating and/or maintaining sleep, and is associated with significant distress or daytime impairments, despite adequate sleep opportunity.
Morin C.M. was the most productive author, ranking first in citations. Sleep had the highest number of manuscripts published in the top 100 ( n = 31), followed by Sleep Medicine Reviews ( n = 9). The most cited manuscript (Bastien et al., Sleep Medicine, 2001; 3,384 citations) reported clinical validation of the Insomnia Severity Index (ISI) as ...
When defined as a sleep disorder, insomnia is characterise d by a. difficulty in falling asleep or remaining asleep, which may represe nt problems with sleep. mainte nance or early morning ...
THESIS FOR DOCTORAL DEGREE (Ph.D.) Room H2, Alfred Nobels allé 23, Karolinska Institutet, Huddinge Friday 23 November 2018, 09:00 By ... insomnia who seek treatment do so in primary health care (PHC). Although the recommended first-line treatment is cognitive behavioral therapy for insomnia (CBT-I), the
Insomnia is the most prevalent sleep disorder and contributes to considerable personal suffering and social cost. Recent advances in conceptual models of insomnia and the ability to investigate ...
Insomnia disorder has known striking developments over the last few years. Partly due to advances in neuroimaging techniques and brain sciences, our understanding of insomnia disorder has become more fine-tuned. Besides, developments within psychological and psychiatric fields have contributed to improve conceptualization, assessment, and treatment of insomnia. In this paper, we present a list ...
Full-text articles of studies exploring the associations of stress with poor sleep quality and/or insomnia in undergraduate students using validated tools and published in peer-reviewed journals were eligible for inclusion. Thirty-four studies, resulting in 37 effect sizes, included and all were suitable for meta-analysis. The weighted pooled ...
Insomnia is defined as sleep continuity disturbance associated with daytime complaints related to sleepiness, fatigue, somatic symptoms (eg, head or body aches), mood disturbance, compromised cognitive or occupational function, concerns about sleep, or dissatisfaction with sleep. Sleep continuity refers to variables that represent sleep ...
Insomnia, whether short-term or chronic, is a common condition. It has a negative impact on vulnerable patient groups, including active military personnel and veterans, patients with coexisting psychiatric and medical disorders, those in life transitions such as menopause, and elderly persons. Although cognitive behavioral therapy for insomnia ...
Pathophysiology of Insomnia. Several models of insomnia etiology and pathophysiology have been proposed, most of which suggest that both external stressors as well as internal psychologic factors have a role. 18 For example, the Spielman model of insomnia, also known as the "Three Factor" or "Three P" model, comprises three factors: predisposing, precipitating, and perpetuating. 43 ...
A novel insomnia theoretical-conceptual framework would enable the drawing of data models for testing mediational relationships between independent variables and outcomes within retrospective studies. Besides, it may also help suggest research strategies and predictions designing prospective studies on insomnia.
We read with interest Kimberly Whitehead and Matthew Beaumont's Perspective1 (June 16, p 2408). As clinicians and researchers working on insomnia over the past three decades, we can only agree that the cultural and historical conditions under which insomnia occurs indeed shape the condition. However, we would like to stress that today's psychological therapies for insomnia2 go far beyond sleep ...
The aims of this thesis were to investigate the need for treatment for sleep difficulties in the general population (study I), evaluate whether a nurse-led group treatment for insomnia is more effective than treatment as usual in improving insomnia in PHC (studies II and III), and to explore patients' experiences of the group treatment (study IV).
Abstract. The present literature review investigated the recent knowledge/ findings on Insomnia, the most prevalent sleep disorder in the general population. Insomnia consequences included mortality risk, physical and mental problems, particularly depression, cognitive impairment, work-related problems such as accidents, injuries, absenteeism ...
Insomnia is defined as a complaint of difficulty falling or staying asleep which is associated with significant distress or impairment in daytime function and occurs despite an adequate opportunity for sleep, . It is a common condition, with an approximate general population point prevalence of 10%, , , . In the vast majority of cases, insomnia ...
INTRODUCTION. Sleep is vital for health and well-being in children, adolescents, and adults. 1-3 Healthy sleep is important for cognitive functioning, mood, mental health, and cardiovascular, cerebrovascular, and metabolic health. 4 Adequate quantity and quality of sleep also play a role in reducing the risk of accidents and injuries caused by sleepiness and fatigue, including workplace ...
Insufficient sleep and insomnia promote chronic disease in the general population and may combine with social and economic factors to increase rates of chronic health conditions among AI/AN people. Given that insufficient sleep and insomnia can be addressed via behavioral interventions, it is critic …
Introduction. Insomnia is one of the most frequent sleep disorders with continuously increasing prevalence. About 30-50% of the US adult population exhibit insomnia symptoms, 15-20% display a short-term insomnia of <3 months, and 5-15% display a chronic insomnia of >3 months (1-3).Common diagnostic manuals include the ICSD-3 (International Classification of Sleep Disorders, 3 rd ...
As it can be seen, insomnia, or sleep deprivation, is a dangerous condition leading to a wide range of health problems. For instance, prolonged periods of sleep deprivation obstructs cognitive and perceptual functions. It also increases the chances of developing diabetes, cardio-vascular problems, and in general, can lead to early death.
MAGNITUDE OF THE PROBLEM. Insomnia is widely prevalent and is reported to occur in up to one-third of the adult population.[] Persistent sleep problems have been reported by 10-15% of adults.[6,7] The prevalence of sleep problems among women and older adults is even higher.[8,9] Although more than half of primary care patients may experience insomnia, only about one-third report this problem ...
1. Introduction. Chronic insomnia is a frequent complaint in Western countries, with reported prevalence ranging from 5.8% to 19% in Europe. In France in 2018, 16.9% of women and 9.1% of men were reported to have chronic insomnia and 13.1% were aged between 18 and 75. 1 Chronic insomnia is associated with long-term health risks including mood disorders, absenteeism, obesity and diabetes ...