- Search Menu
- Sign in through your institution
- Author Guidelines
- Submission Site
- Open Access
- About Alcohol and Alcoholism
- About the Medical Council on Alcohol
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Contact the MCA
- Journals on Oxford Academic
- Books on Oxford Academic


Article Contents
Conclusion and limitations, acknowledgements, conflict of interest statement, declarations of interest.
- < Previous
Treatment of Alcohol-Induced Psychotic Disorder (Alcoholic Hallucinosis)—A Systematic Review
- Article contents
- Figures & tables
- Supplementary Data
Barkat Masood, Peter Lepping, Dmitry Romanov, Rob Poole, Treatment of Alcohol-Induced Psychotic Disorder (Alcoholic Hallucinosis)—A Systematic Review, Alcohol and Alcoholism , Volume 53, Issue 3, May 2018, Pages 259–267, https://doi.org/10.1093/alcalc/agx090
- Permissions Icon Permissions
To evaluate the effectiveness of evidence based treatments for alcohol-induced psychotic disorder (AIPD) as described by ICD-10 and DSM-5, a condition that is distinct from schizophrenia and has a close relationship with alcohol withdrawal states.
Systematic review using PRISMA guidelines.
Of 6205 abstracts found, fifteen studies and ten case reports met criteria and were examined. Larger studies examined the use of first-generation antipsychotic drugs, reporting full or partial remission in most patients. Newer case reports report similar results using second generation antipsychotic drugs. Novel treatments, such as those acting on GABA receptors reported low numbers of patients in remission. Some large studies report the successful use of standard alcohol withdrawal treatments.
The findings of our systematic review are inconclusive. There was significant heterogeneity between and within studies. Significant publication bias is likely. Randomized control trials of more carefully delineated samples would produce evidence of greater clinical utility, for example, on differential effectiveness of antipsychotics and optimal length of standard alcohol withdrawal treatments. AIPD patients who show poor treatment responses should be studied in greater depth.
This systematic review of alcohol-induced psychotic disorder treatment found 15 studies and 10 case reports of relevance. Older studies of first-generation antipsychotics reported full or partial remission in most patients, as did newer studies with second-generation antipsychotics. Novel drugs reported low remission rates. Standard alcohol withdrawal treatments were successful.
Excess alcohol consumption results in medical and social problems around the world. It accounts for 3% of global deaths ( Rehm et al. , 2009 ). Neuropsychiatric consequences to alcohol dependence syndrome include delirium tremens, alcohol-related brain damage, Korsakoff’s syndrome and alcoholic hallucinosis. The terms ‘alcoholic hallucinosis’ and ‘alcohol-induced psychotic’ disorder (AIPD) are often used interchangeably, although they may be better regarded as over-lapping categories. In this review we follow ICD-10 ( WHO, 1992 ) in using the rubric AIPD to include both syndromes (ICD-10 code F10.5, corresponding to DSM-5 code 292.1).
According to ICD-10 (WHO 2016 version), AIPD is a condition where mental and behavioural symptoms manifest within 2 weeks of alcohol use and must persist for more than 48 h. Symptoms should not arise as part of alcohol intoxication or an alcohol withdrawal state. Clouding of consciousness should not be present to more than to a minor degree. An episode can persist for up to six months. A wide variety of symptoms can occur, including schizophreniform delusions, hallucinations, depression and mania. DSM-5 ( American Psychiatric Association, 2013 ) specifies that the substance should be capable of causing symptoms and that the condition should not be better explained by another psychotic disorder.
There are a number of assertions made within the AIPD literature. In a Finnish study, AIPD was found to have a general population lifetime prevalence of 0.41%, or 4% for people with alcohol dependence syndrome. It was most common amongst men of working age ( Perälä et al. , 2010 ). AIPD is said to manifest immediately after the consumption of large amounts of alcohol. It may not be related to duration of alcohol dependence syndrome ( George and Chin, 1998 ; Perälä et al. , 2010 ). Symptoms may develop during alcohol intoxication or withdrawal or soon thereafter. The diagnosis cannot be made until clear consciousness is restored. AIPD is said to usually resolve within 18–35 days with antipsychotic and/or benzodiazepine treatment ( Vicente et al. , 1990 ). A minority of patients may have persistent symptoms for 6 months or more ( Benedetti, 1952 ; Burton-Bradley, 1958 ). AIPD may end through alcohol abstinence alone and return soon after reinstatement of drinking ( Glass, 1989b ). The assertion that antipsychotic drugs are the treatment of choice ( Soyka et al. , 1988 ; Jordaan and Emsley, 2014 ) is not supported by published randomized controlled trials (RCTs). A number of factors affecting people with AIPD make it difficult to recruit and retain participants in RCTs ( Perälä et al. , 2010 ).
There are few rigorous published studies of treatments for AIPD. This systematic review was conducted in order to evaluate the available evidence on treatment.
PRISMA Guidelines were used to carry out a systematic review. Medline, EMBASE, PsychINFO, Cochrane and CINAHL databases were searched for studies that had been published between 1 January 1900 and 18 August 2016. Subject search terms were: hallucinations/or alcoholism/or psychoses/or alcoholic psychoses/or chemically induced, drug therapy, prevention and control, rehabilitation, therapy/or alcohol intoxication/or delusions/or delirium/or dissociative disorders. (Search strategy available on request.)
had been published in any language,
investigated alcohol with or without polysubstance misuse,
investigated hallucinations,
investigated hallucinations attributed to alcohol and polysubstance misuse,
investigated hallucinations that persisted beyond one week of alcohol/drug withdrawal state,
investigated any treatment of symptoms,
investigated any outcome measures,
investigated patients of any age,
were RCTs and
were case reports or series.
papers that did not have abstracts (Criterion 1),
non-human studies (Criterion 2),
examined acute confusional states/delirium, symptoms that occurred during alcohol/drug withdrawal states of <1 week duration, delirium tremens, drug intoxication states and organic psychoses (Criterion 3),
did not examine hallucinations or psychoses (Criterion 4),
examined schizophrenia, bipolar disorder, mood disorder or delusional disorder (Criterion 5),
did not examine alcohol-related hallucinosis or examined hallucinations due to polysubstance misuse (Criterion 6),
single case studies (Criterion 7) and
did not examine treatment or include outcome measures (Criterion 8).
The minimum standard for outcome measures was classification into no remission, partial remission or full remission.
Overall, 7347 articles were identified and 6205 remained after duplicates were removed. Abstracts for the 6205 articles were screened and the 8 exclusion criteria applied. Twenty-six full text articles were requested to assess eligibility. (See PRISMA flow chart Fig. 1 .)

PRISMA flow diagram of treatment of AIPD.
In December 2016, a search on the ClinicalTrials.gov ( www.clinicaltrials.gov ), the ISRCTN Registry ( www.ISRCTN.com ), the EU Clinical Trials ( www.clinicaltrialsregister.eu ) and the UK Clinical Trials Gateway ( www.ukctg.nihr.ac.uk ) websites did not find any completed or ongoing RCTs of treatment of AIPD.
Treatments and Outcomes in AIPD studies
| Author . | Study type . | Treatment and outcome measurement . | Duration (days) . | , age range . | Outcome: no remission, partial remission and full remission . |
|---|---|---|---|---|---|
| Case series | Electroconvulsive therapy wavelength 7.5 m; 15 min per treatment. Self structured scale of improvement or no improvement. | 5, 6 and 14 treatments. Maximum 28 days | Males 3; aged 28–40 | Full remission: 3 (100%) | |
| Case series (observational study) | Chlorpromazine, antidepressants, psychotherapy. | Unknown | 100 patients | No remission: 100 (100%) | |
| (1968) | Case series | 56–252 | Males 6 | No remission: 6 (100%) | |
| Case series | 28–168 | 73 patients | |||
| Case series (Open label. observational study) | Antipsychotics, vitamin B1 (100–200 mg) and Biyohinol/ Bioochinolum preparation (quinine bismuth iodide) up to 40–50 ml. | 28 | 46 patients | No remission: 46 (100%) | |
| (1980) | Case series (Prospective observational comparison study) | Self constructed outcome scale of full remission, partial remission and no remission. | Initial period-42 days. Then 546 days. | 30 patients with alcoholic hallucinosis (ICD-9 criteria) compared with 30 patients with paranoid schizophrenia | Alcoholic hallucinosis: |
| Paranoid schizophrenia: | |||||
| Double blind randomized placebo controlled. Crossover trial | 6 | 24 male patients (16 withdrawal states and 8 alcohol hallucinosis) | |||
| (1985) | Case series | 2–3 | 35 patients (21 delirium tremens and 14 alcoholic hallucinosis) | Alcoholic hallucinosis: Full remission: 8 (57%). No remission: 6(43%) following parenteral treatment. | |
| (1990) | Case series | 18–35 | 25 (23 males and 2 females) | ||
| Case series | Diazepam 30–40 mg/day. Vitamin B1 (1 ampoule/day) for 3 days, then 200 mg/ day. Haloperidol 30–40 mg/day. | Mean duration: 7 days | 34 patients (32 males and 2 females) | ||
| Self constructed scale of full recovery or no recovery. | |||||
| Double blind randomized placebo controlled trial. | 7 | 40 male patients. 20 to drug and 20 to placebo | Sublingual glycine: partial remission: 20 (100%) | ||
| Placebo: no remission: 20 (100%) | |||||
| Double blind randomized placebo controlled trial. | Sodium valproate. | Initial dose titration 3. Total period 10. | 40 male patients | ||
| Starting dose of 100 mg/day, increased to 300 mg. | |||||
| Clinical Global Impression improvement scale. | |||||
| (2011) | Double blind, randomized placebo controlled trial. | 10 | Lamotrigine: partial remission: 20 (100%) | ||
| Placebo: no remission: 20 (100%) | |||||
| Case series (Observational study) | Unknown. | 26 males | Full remission: 24 (92%), Partial remission: 2(8%). | ||
| (2012) | Case series. (Prospective open label non-comparative study) | 42 | 20 patients (16 males and 4 females) | Full remission: 18 (90%), partial remission: 2 (20%). |
| Author . | Study type . | Treatment and outcome measurement . | Duration (days) . | , age range . | Outcome: no remission, partial remission and full remission . |
|---|---|---|---|---|---|
| Case series | Electroconvulsive therapy wavelength 7.5 m; 15 min per treatment. Self structured scale of improvement or no improvement. | 5, 6 and 14 treatments. Maximum 28 days | Males 3; aged 28–40 | Full remission: 3 (100%) | |
| Case series (observational study) | Chlorpromazine, antidepressants, psychotherapy. | Unknown | 100 patients | No remission: 100 (100%) | |
| (1968) | Case series | 56–252 | Males 6 | No remission: 6 (100%) | |
| Case series | 28–168 | 73 patients | |||
| Case series (Open label. observational study) | Antipsychotics, vitamin B1 (100–200 mg) and Biyohinol/ Bioochinolum preparation (quinine bismuth iodide) up to 40–50 ml. | 28 | 46 patients | No remission: 46 (100%) | |
| (1980) | Case series (Prospective observational comparison study) | Self constructed outcome scale of full remission, partial remission and no remission. | Initial period-42 days. Then 546 days. | 30 patients with alcoholic hallucinosis (ICD-9 criteria) compared with 30 patients with paranoid schizophrenia | Alcoholic hallucinosis: |
| Paranoid schizophrenia: | |||||
| Double blind randomized placebo controlled. Crossover trial | 6 | 24 male patients (16 withdrawal states and 8 alcohol hallucinosis) | |||
| (1985) | Case series | 2–3 | 35 patients (21 delirium tremens and 14 alcoholic hallucinosis) | Alcoholic hallucinosis: Full remission: 8 (57%). No remission: 6(43%) following parenteral treatment. | |
| (1990) | Case series | 18–35 | 25 (23 males and 2 females) | ||
| Case series | Diazepam 30–40 mg/day. Vitamin B1 (1 ampoule/day) for 3 days, then 200 mg/ day. Haloperidol 30–40 mg/day. | Mean duration: 7 days | 34 patients (32 males and 2 females) | ||
| Self constructed scale of full recovery or no recovery. | |||||
| Double blind randomized placebo controlled trial. | 7 | 40 male patients. 20 to drug and 20 to placebo | Sublingual glycine: partial remission: 20 (100%) | ||
| Placebo: no remission: 20 (100%) | |||||
| Double blind randomized placebo controlled trial. | Sodium valproate. | Initial dose titration 3. Total period 10. | 40 male patients | ||
| Starting dose of 100 mg/day, increased to 300 mg. | |||||
| Clinical Global Impression improvement scale. | |||||
| (2011) | Double blind, randomized placebo controlled trial. | 10 | Lamotrigine: partial remission: 20 (100%) | ||
| Placebo: no remission: 20 (100%) | |||||
| Case series (Observational study) | Unknown. | 26 males | Full remission: 24 (92%), Partial remission: 2(8%). | ||
| (2012) | Case series. (Prospective open label non-comparative study) | 42 | 20 patients (16 males and 4 females) | Full remission: 18 (90%), partial remission: 2 (20%). |
a Assuming maximum of two treatments per 7 days. Although 2 or more treatments could occur in a day.
b Unknown regimen. Original sample n = 204. Mixture of delirium tremens, organic brain syndromes and AIPD. Relevant AIPD cases examined.
c Assuming that three participants withdrawn due to severity of withdrawal state and subsequently requiring antipsychotics.
d 29 patients had full remission. It is assumed that all 21 patients with delirium tremens had full remission.
e 28 of 33 patients had complete remission. However, the adjustment of removing one patient is because this patient had delirium tremens and is assumed to have had full remission.
f Original mixed study (clearly defined cases of delirium tremens, AIPD, Korsakov’s syndrome and other psychiatric disorder due to alcohol and psychostimulants) of n = 125.
Treatment and outcomes in AIPD case reports
| Authors . | . | Age (y) . | Sex . | Treatment . | Dosage per day (mg) . | Duration (days) . | Outcome . |
|---|---|---|---|---|---|---|---|
| 2 | 50 | M | Chlorpromazine | Unknown | Unknown | No remission | |
| Electroconvulsive treatment | 1 session | Full remission | |||||
| 55 | M | Electroconvulsive therapy | Unknown | 1 session | Full remission | ||
| 1 | 35 | M | Haloperidol | Unknown | 6 | No remission | |
| 2 | 40 | M | Antipsychotics, vitamins, psychotherapy, supportive measures | Unknown | 56 | Full remission | |
| 47 | M | Unknown | 168 | Full remission | |||
| (1997) | 1 | 33 | M | Haloperidol decanoate | 10 | 2190 | No remission |
| Perazine | 200 | ||||||
| Risperidone | 6 | 56 | Full remission | ||||
| 1 | 58 | M | Risperidone | 2 | 5 | Full remission | |
| Alcohol abstinence | 4 | 56 | Full remission | ||||
| 1 | 40 | M | Olanzapine | 20 | 10 | Full remission | |
| Citalopram | 40 | ||||||
| Risperidone | 6 | 10 | Full remission | ||||
| 2 | 23 | M | Risperidone, benzodiazepines and vitamin B1 | 4 | 42 | Full remission | |
| 43 | M | 4 | 42 | Full remission | |||
| (2014) | 1 | 58 | M | Diazepam | 60 | Unknown | Full remission |
| Olanzapine | 10 | 19 | |||||
| Folic acid and vitamin B complex | Unknown | Unknown | |||||
| 1 | 38 | M | Quetiapine | 900 | 56 | No remission | |
| Flupenthixol | 18 | 56 | No remission | ||||
| Haloperidol | Unknown | Unknown | Partial remission | ||||
| (2016) | 1 | 59 | M | Trifluoperazine | 10 | 56 | No remission |
| Risperidone | 6 | 56 | No remission | ||||
| Clozapine | 200 | 56 | No remission | ||||
| Transcranial direct current stimulation (tDCS) | 2 sessions per day, 2 mA intensity | 5 | Full remission |
| Authors . | . | Age (y) . | Sex . | Treatment . | Dosage per day (mg) . | Duration (days) . | Outcome . |
|---|---|---|---|---|---|---|---|
| 2 | 50 | M | Chlorpromazine | Unknown | Unknown | No remission | |
| Electroconvulsive treatment | 1 session | Full remission | |||||
| 55 | M | Electroconvulsive therapy | Unknown | 1 session | Full remission | ||
| 1 | 35 | M | Haloperidol | Unknown | 6 | No remission | |
| 2 | 40 | M | Antipsychotics, vitamins, psychotherapy, supportive measures | Unknown | 56 | Full remission | |
| 47 | M | Unknown | 168 | Full remission | |||
| (1997) | 1 | 33 | M | Haloperidol decanoate | 10 | 2190 | No remission |
| Perazine | 200 | ||||||
| Risperidone | 6 | 56 | Full remission | ||||
| 1 | 58 | M | Risperidone | 2 | 5 | Full remission | |
| Alcohol abstinence | 4 | 56 | Full remission | ||||
| 1 | 40 | M | Olanzapine | 20 | 10 | Full remission | |
| Citalopram | 40 | ||||||
| Risperidone | 6 | 10 | Full remission | ||||
| 2 | 23 | M | Risperidone, benzodiazepines and vitamin B1 | 4 | 42 | Full remission | |
| 43 | M | 4 | 42 | Full remission | |||
| (2014) | 1 | 58 | M | Diazepam | 60 | Unknown | Full remission |
| Olanzapine | 10 | 19 | |||||
| Folic acid and vitamin B complex | Unknown | Unknown | |||||
| 1 | 38 | M | Quetiapine | 900 | 56 | No remission | |
| Flupenthixol | 18 | 56 | No remission | ||||
| Haloperidol | Unknown | Unknown | Partial remission | ||||
| (2016) | 1 | 59 | M | Trifluoperazine | 10 | 56 | No remission |
| Risperidone | 6 | 56 | No remission | ||||
| Clozapine | 200 | 56 | No remission | ||||
| Transcranial direct current stimulation (tDCS) | 2 sessions per day, 2 mA intensity | 5 | Full remission |
Please note: Outcomes dictate that an individual treatment episode occurred. Some patients received more than one treatment. Whenever more than one treatment is listed for a patient, the treatments listed were given consecutively.
a Full remission after 56 and 168 days. Time of response suggested to be immediate.
b Full remission occurred after a few days.
c Dose of risperidone not specified. Assumed to be maximum doses, as per Joint Formulary Committee. (2015) .
d Four milligrams refers to dose of risperidone. Unknown type, dose and duration of benzodiazepine. Confirmed by email correspondence from B. Masood to A. Farcas.
e Doses and duration not specified for quetiapine and flupenthixol. Assumed to be adequate therapeutic trial at maximum doses, as per Joint Formulary Committee. (2015) .
f Auditory Hallucinations Rating Scale used.
Trial studies
Four studies retrieved were double blind RCTs, of which one was a crossover study. One study included comparison with a group of participants with a diagnosis of paranoid schizophrenia. Ten studies were open label, non-comparative case series of treatment and outcome of AIPD.
Five of the included studies examined cases of AIPD arising in the context of alcohol withdrawal (psychotic symptoms started during the withdrawal state but persisted after other withdrawal symptoms had resolved). The trials are summarized in Table 1 .
Types of treatment
Antipsychotics: No trials examined the use of second-generation antipsychotics. Six trials examined the use of single or multiple first-generation antipsychotics, including haloperidol, chlorpromazine, trifluoperazine, reserpine, thiotixene and levopromazine. Three trials examined the use of antipsychotics, benzodiazepines, vitamin B1 with treatment outcomes, but did not specify which antipsychotic drug was used.
Anticonvulsants: Anticonvulsants were used in three trials (lamotrigine, sodium valproate and phenobarbitone). Hypnotics such as barbamyl and chloral hydrate were used in one trial.
Others: Two trials examined other compounds that act on GABA receptors (piracetam and clorazepate).
One trial examined the primary use of an unusual treatment (glycine). One trial examined the use of electroconvulsive therapy (ECT).
Treatment results
There was marked heterogeneity of results, even with the same drug. For example, full remission rates for chlorpromazine varied from 0 to 68%, and partial remission rates from 0 to 32%. Better results with haloperidol included full remission rates of 68–90%, and partial remission rates of 0–30%. However, there were few trials of antipsychotic monotherapy, so findings are hard to fully interpret.
Heterogeneous outcomes were also evident in trials of non-antipsychotic treatments, apart from one trial of three patients treated with ECT, all of whom experienced full remission.
Treatment duration ranged from 3 to 546 days, but most trials were brief. Longer duration was not associated with more favourable outcomes. In three trials, duration was not stated.
Participants were predominantly male, as noted by Szefal and Zaleski (1983) , who studied women with AIPD. Cohort sizes ranged from 3 to 100. Ten trials involved between 24 and 40 participants.
Case reports
The ten case report papers reported 13 separate patients who were exposed to 21 different treatments or treatment combinations. All patients were treated with first- or second-generation antipsychotics. Three patients were treated with adjunctive benzodiazepines and vitamin B1.
Treatments and outcomes are set out in Table 2 . Outcomes were highly variable. Five patients experienced full remission with risperidone and two with olanzapine. No remission occurred in patients treated with chlorpromazine, perazine, flupenthixol, trifluoperazine or quetiapine. Of three treatment episodes with haloperidol, only one led to (partial) remission. There were two ECT treatment episodes, both of which were associated with full remission. However, it should be noted that the most recent report of ECT for AIPD was published in 1956.
Full remission was reported in one patient treated with transcranial direct current stimulation following failure of three different first- or second-generation antipsychotic drugs
Previous reviews of AIPD have focussed on aetiology, symptoms, prognosis and the relationship with schizophrenia ( Soyka, 1994 ; Engelhard et al. , 2015 ; Jordaan and Emsley, 2014 ). This is the first systematic review to examine treatment of AIPD. We included part of the non-English language literature, papers written in Dutch, French, German, Polish, Russian and Spanish. All papers were translated by P.L. or D.R. who are fully fluent in the respective languages, with the exception of Polish and Spanish where a translation service and Google translate were used respectively.
Main Findings
The findings of our systematic review are inconclusive. Studies generally had relatively low numbers of participants. There were few RCTs. Treatments were sometimes idiosyncratic, although these were usually supported by a rationale. For example, Aliyev et al . ( Aliyev and Aliyev, 2005 , 2008 ; Aliyev et al. , 2011 ) justified their treatment with glycine, lamotrigine and sodium valproate by reference to Branchey et al. (1985) , who suggest that amino acid abnormalities affect cerebral serotonin and dopamine levels and thus cause hallucinations. Their results do not support the use of these treatments. They reported high partial remission rates in RCTs but the trials were brief (10 days) with no indication of longer-term outcomes. High doses of medication were used. These may have caused sedative side effects, confounding findings of partial remission.
Overall, larger studies tended to report at least partial remission on antipsychotic medications, whether in combination with other treatments or as monotherapy. Some case reports concerned treatment with second-generation antipsychotics. Insofar as it is possible to tell, these appear to be no better or worse than older drugs.
Problems in studying treatments for AIPD
The sparseness of the literature is surprising, as alcohol dependence syndrome is common and AIPD is a serious complication of the condition. However, there are several problems in studying treatments for AIPD:
Firstly, it may be difficult to recruit and retain participants who are both alcohol dependent and suffering from psychotic symptoms. Prolonged abstinence can be difficult to achieve. Participants are likely to live in difficult social situations due to alcohol excess ( Ali and McBride, 1997 ). These factors make compliance and retention in rigorous trials difficult.
Secondly, poor treatment outcomes in longer studies may lead to participants dropping out of trials. Underpowered trials generate inconclusive results.
Heterogeneous samples
The literature on AIPD and alcoholic hallucinosis has been dominated by attempts to ascertain whether there is a single syndrome, distinct from schizophrenia and delirium tremens, or whether there are several alcohol-related psychotic syndromes, either discrete or overlapping.
We found that all studies and case reports matched ICD-10 and DSM-5 criteria. All studies and case reports excluded clouding of consciousness as a key diagnostic criterion, which is congruous with DSM-5 and ICD-10 criteria. All case reports and studies described auditory hallucinations as a key feature in AIPD but some authors reported hallucinations in other modalities. Auditory hallucinations were second and third person, commentary, derogatory and command types. Delusions of persecution and of jealousy were reported in some participants. Boriskov (1977) described delusions of grandeur in AIPD, while Jordaan et al. (2012) found no evidence of significant delusions of grandeur. Interestingly, a few studies reported schizophreniform thought disorder ( George and Chin, 1998 ; Vicent-Muelas et al ., 1990). All authors reported that the onset of auditory hallucinations could occur during excess alcohol consumption or on alcohol withdrawal. No auditory hallucinations commenced during periods of extended alcohol abstinence.
The diagnosis of AIPD appears to have been stable in all studies. No changes of diagnosis to schizophrenia were observed. However, some participants experienced alcohol withdrawal symptoms, there was a wide range of psychopathology in different participants, and the timing of onset of AIPD was not always reported.
Attempts have been made to distinguish between AIPD and schizophrenia complicated (or precipitated) by alcohol misuse. In the 1950s, three large-scale studies followed patients with AIPD for 5–23 years in order to examine prognosis and diagnosis ( Benedetti, 1952 ; Burton-Bradley, 1958 ; Victor and Hope, 1958 ). The conclusion was broadly similar: the majority of patients studied did not have schizophrenia. Cutting (1978) concluded from a study of 46 patients that AIPD could be regarded as an organic psychosis, and if there was any resemblance to schizophrenia this was due to an emphasis on Schneider’s first rank symptoms in earlier editions of ICD and DSM. He suggested that people with AIPD do not show features of schizophrenia as propounded by Bleuler (1911) —such as blunting of affect, autism, thought disorder and ambivalence—and by Kraepelin (1913) .
A two part review by Glass (1989a , 1989b ) emphasized that schizophrenia and AIPD have different onsets, different symptoms and different outcomes. This view was shared by Soyka (1994) , who had reported that patients with AIPD were more likely to have a family history of alcohol misuse than psychosis, and vice versa for patients with schizophrenia ( Soyka, 1990 ). A number of family studies support a genetic distinction between AIPD and schizophrenia ( Schukit and Winokur, 1971 ; Rimmer and Jacobsen, 1977 ; Kendler, 1985 ).
These did not add significantly to our understanding of treatment strategies for AIPD. We found only ten case reports (Table 2 ). Treatment periods were usually around 56 days duration ( Chaudhury and Augustine, 1991 ; Soyka et al. , 1997 ; De Millas and Haasen, 2007 ; Bouritius et al. , 2015 ; Goyal et al. , 2016 ). Full or partial remissions occurred within a matter of days or not at all.
Remission on treatment with first-generation antipsychotics was common, but some reported success with subsequent use of second-generation antipsychotics, strengthening the suspicion of publication bias. Only one case report reported no treatment remission ( Hytinnen, 1987 ). Case studies are well recognized to be potentially misleading, and we do not believe that any reliance should be placed upon them.
Non-pharmacological treatment strategies
In a very small number of cases, ECT and transcranial direct current stimulation appeared to be effective treatments ( Gruenberg, 1940 ; Bourdon, 1956 ; Goyal et al. , 2016 ). These findings are interesting but require replication in large studies.
There is a widely held clinical dictum that alcoholic hallucinosis does not resolve without complete abstinence from alcohol and that relapse of drinking tends to cause a return of hallucinations soon thereafter. Abstinence on its own was not an effective treatment for AIPD in one case report ( De Millas and Haasen, 2007 ). Nonetheless, this is a safe treatment strategy, and it is surprising that there are no studies reported anywhere in the literature of alcohol withdrawal followed by complete abstinence with no drug treatment. This is a major gap in the evidence base.
Recommendations for future research
Did psychotic symptoms first arise during alcohol intoxication or, conversely, during acute alcohol withdrawal?
Are symptoms predominately hallucinations, delusions or both?
Is symptom duration one month, more than 1 month or more than 6 months?
Do symptoms persist during abstinence?
Is schizophreniform thought disorder present?
Greater clarity and homogeneity would distinguish, for example, participants who meet criteria for both schizophreniform psychosis and alcohol dependence syndrome from participants displaying a core ‘alcohol hallucinosis’ as described by Lishman (1998) , with persistent vivid auditory hallucinations that arise with a quality of insight, but few or no other psychotic symptoms.
Clinical implications
Our systematic review suggests that there is adequate evidence that some patients with AIPD show a favourable response to antipsychotic medication. There is nothing to indicate the superiority of any particular drug. Both first- and second-generation drugs appear to be effective. However, it seems highly likely that many patients show little or no response to antipsychotics and that persistence when they fail to produce remission (whether partial or full) cannot be justified. There is no evidence to guide the duration of treatment. First principles would dictate that this should be as brief as possible, given the wide range of side effects associated with these medications.
As complete abstinence from alcohol, when it can be achieved, slows or stops other alcohol-related disease processes, there is good reason to strongly recommend it. There is sufficient weight of clinical opinion to caution patients that even controlled drinking may lead to the return of psychotic symptoms.
There is insufficient evidence for other treatments reviewed here to recommend their routine use in the treatment of AIPD
Given the relative dearth of data we chose a wide timeframe for our search. However, earlier papers may have included patients who may have been excluded if modern diagnostic techniques had been available. Furthermore, standard treatments such as antipsychotics were not available for a proportion of the early studies. Much of the evidence for treatment of AIPD is weak and is only level IV evidence ( Agency for Health Care Policy and Research, 1992 ). The lack of research on AIPD may be due to a belief that it is easy to treat ( Soyka et al. , 1988 ; Jordaan and Emsley, 2014 ). However, this is mistaken as hospital readmission rates are high ( Soyka et al. , 2013 ). There is little clarity on how best to treat patients with persistent symptoms.
Heterogeneity is a problem in the studies found. We suggest that distinguishing between key variables of AIPD would help to understand the findings of future treatment trials. The evidence for the effectiveness of first- and second-generation antipsychotic drugs is based upon case reports and underpowered trials. Positive publication bias is likely. A funnel plot was not feasible due to the size and nature of the literature. There is supportive evidence to use this treatment, but better evidence is needed. Similar considerations affect studies using novel treatments such as GABA receptor compounds, but the lack of positive findings means that they cannot be recommended in the treatment of AIPD. Although some larger studies report the successful use of standard alcohol withdrawal treatments, longer-term management remains unexamined. There is an important gap in the literature on the management of patients whose symptoms fail to remit in response to antipsychotic medication.
We would like to thank Nia Morris and Pauline Goodland from the John Spalding Library at the Wrexham Maelor Hospital for their valuable contribution.
There was no external funding provided for this project.
None declared.
All authors have no declarations of interest.
Agency for Health Care Policy and Research . AHCPR Publication 92-0032 . AHPCPR ( 1992 ).
Aleksin DS , Egorov A . ( 2011 ) Current peculiarities of alcoholic psychosis . Zh Nevrol Psikhiatr Im S S Korsakova 111 : 20 – 7 .
Google Scholar
Ali IM , McBride AJ . ( 1997 ) Attendance rate in an alcohol problem clinic . Psychiatrist 21 : 343 – 5 .
Aliyev N , Aliyev AA , Aliyev ZN , et al. . ( 2011 ) FC03-04-Lamotrigine treatment of acute alcohol hallucinosis comorbid depersonalizations disorders: a randomimized double-blind, placebo-controlled study . Eur Psychiatry. 26 : 1825 .
Aliyev NA , Aliyev ZN . ( 2005 ) Application of glycine in acute alcohol hallucinosis . Hum Psychopharm: Clin Exp 20 : 591 – 4 .
Aliyev ZN , Aliyev NA . ( 2008 ) Valproate treatment of acute alcohol hallucinosis: a double-blind, placebo-controlled study . Alcohol Alcohol 43 : 456 – 9 .
American Psychiatric Association . ( 2013 ) Statistical Manual of Mental Disorders: DSM-5 (ed.) . Washington, DC : American Psychiatric Association .
Google Preview
Benedetti G . ( 1952 ) Die Alkoholhalluzinosen . Stuttgart : Thieme .
Bleuler E . ( 1911 ) Dementia Praecox or the Group of Schizophrenias . New York : International University Press: New York , (translated J. Zinkin, 1950).
Bobrov AS . ( 1966 ) On the nature of acute delusional psychoses in the clinical evolution of alcoholism . Zh Nevropatol Psikhiatr Im S S Korsakova 66 : 731 – 8 .
Bokun P . ( 1975 ) [Alcoholic psychoses in Split.] . Socijalna Psihijatr 3 : 215 – 22 .
Boriskov VP . ( 1977 ) Nosologic independence and features of the treatment of alcoholic paraphrenia . Zh Nevropatol Psikhiatr Im S S Korsakova 77 : 739 – 43 .
Bourdon J . ( 1956 ) [Concerning the treatment of alcoholic hallucinosis.] . Acta Neurol Psychiatr Belg 56 : 507 – 12 .
Bouritius EM , Neven A , Blom JD . ( 2015 ) Alcoholhallucinose . Ned Tijdschr Geneeskd 159 : A7901 .
Branchey L , Branchey M , Worner TM , et al. . ( 1985 ) Association between amino acid alterations and hallucinations in alcoholic patients . Biol Psychiatry. 20 : 1167 – 73 .
Burton-Bradley BG . ( 1958 ) Aspects of alcoholic hallucinosis . Med J Aust 45 : 8 – 11 .
Cade JF . ( 1972 ) Massive thiamine dosage in the treatment of acute alcoholic psychoses . Aust N Z J Psychiatry 6 : 225 – 30 .
Chaudhury S , Augustine M . ( 1991 ) Alcoholic hallucinosis: case reports . J Personality Clin Stud 7 : 119 – 22 .
Cutting J . ( 1978 ) A reappraisal of alcoholic psychoses . Psychol Med. 8 : 285 – 95 .
De Millas W , Haasen C . ( 2007 ) Treatment of alcohol hallucinosis with risperidone . Am J Addict 16 : 249 – 50 .
Dvirskiĭ AA . ( 2000 ) Clinical symptoms of schizophrenia in combination with delirium tremens . Zh Nevrol Psikhiatr Im S S Korsakova 101 : 18 – 20 .
Engelhard CP , Touquet G , Tansens A , et al. . ( 2015 ) [Alcohol-induced psychotic disorder: a systematic literature review.] . Tijdschr Psychiatr 57 : 192 – 201 .
Entin GM . ( 1970 ) Clinical picture and therapy of alcoholic psychoses in later years . Zh Nevropatol Psikhiatr Im S S Korsakova 70 : 743 – 50 .
Farcas A . ( 2012 ) Alcoholic hallucinosis: report of two cases . Eur Psychiatry. 27 : 1 . P25.
George S , Chin CN . ( 1998 ) A 3 year case study of alcohol related psychotic disorders at Hospital Seremban . Med J Malaysia 53 : 223 – 6 .
Glass IB . ( 1989 a) Alcoholic hallucinosis: a psychiatric enigma—1. The development of an idea . Addiction 84 : 29 – 41 .
Glass IB . ( 1989 b) Alcoholic Hallucinosis: a psychiatric enigma—2. Follow‐up studies . BJAddiction 84 : 151 – 64 .
Goyal P , Kataria L , Andrade C . ( 2016 ) Transcranial direct current stimulation for chronic continuous antipsychotic-refractory auditory hallucinations in alcoholic hallucinosis . Brain Stimul Basic Transl Clin Res Neuromod 9 : 159 – 60 .
Gruenberg KY . ( 1940 ) High frequency electric current in the treatment of alcoholic hallucinosis . Am Rev Soviet Med 1 : 544 – 52 .
Hyttinen R . ( 1987 ) Management of alcoholic psychosis in a psychiatric hospital . Nord Psykiatr Tidsskr 41 : 197 – 201 .
Imamov A . ( 1986 ) Patterns in the recurrence and transformation of alcoholic psychoses developing against a pathologic background (clinico-statistical study) . Zh Nevropatol Psikhiatr Im S S Korsakova 87 : 608 – 11 .
Joint Formulary Committee . ( 2015 ) British National Formulary 70 . London : BMJ Group and Pharmaceutical Press .
Jordaan GP , Emsley R . ( 2014 ) Alcohol-induced psychotic disorder: a review . Metab Brain Dis 29 : 231 – 43 .
Jordaan GP , Warwick JM , Nel DG , et al. . ( 2012 ) Alcohol-induced psychotic disorder: brain perfusion and psychopathology—before and after anti-psychotic treatment . Metab Brain Dis 27 : 67 – 77 .
Kabeš J , Skondia V , Marholdová K , et al. . ( 1985 ) Piracetam effectivity in alcoholic psychosis: double blind cross-over placebo controlled comparison . Activitas Nervosa Superior 27 : 66 – 7 .
Kendler KS . ( 1985 ) A twin study of individuals with both schizophrenia and alcoholism . B J Psychiatry 147 : 48 – 53 .
Kraepelin E . ( 1913 ) Lectures on Clinical Psychiatry . London : Bailliere, Tindall and Cox , (translated T. Johnstone).
Kumar S , Bankole A . ( 2010 ) A 40-year-old man with acute psychosis . Psychiatr Ann 40 : 600 – 3 .
Levitin LV , Ezarielev GI , Levitin AN . ( 1971 ) [Concerning questions of the epidemiology and structure of alcoholic psychoses.] . Zh Nevropatol Psikhiatr Im S S Korsakova 71 : 583 – 8 .
Lishman WA (ed) . ( 1998 ) Organic Psychiatry: The Psychological Causes of Cerebral Disorder , 3rd edn. London : Blackwell Scientific .
Moefes SM . ( 1970 ) On alcoholic paraphrenia . Zh Nevropatol Psikhiatr Im S S Korsakova 70 : 740 – 3 .
Morales-Belda FJ , de Haro de la Cruz T . ( 1968 ) [Clinical evaluation of the action of thiothixene (P-4657 B) in the treatment of alcoholic psychosis.] . Actas Luso-Espan Neurol Psiquiatr 27 : 537 – 43 .
Ogut DB , Suner O , Citak S . ( 2014 ) Alcoholic hallucinosis . Klin Psikofarmakol Bul 24 : S194 .
Perälä J , Kuoppasalmi K , Pirkola S , et al. . ( 2010 ) Alcohol-induced psychotic disorder and delirium in the general population . Br J Psychiatry 197 : 200 – 6 .
Rehm J , Mathers C , Popova S , et al. . ( 2009 ) Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders . Lancet 373 : 2223 – 33 .
Rimmer J , Jacobsen B . ( 1977 ) Alcoholism in schizophrenics and their relatives . J Stud Alcohol 38 : 1781 – 4 .
Sampath G , Kumar YV , Channabasavanna SM , et al. . ( 1980 ) Alcoholic hallucinosis and paranoid schizophrenia—a comparative (clinical and follow up) study . Indian J Psychiatry 22 : 338 .
Schuckit MA , Winokur G . ( 1971 ) Alcoholic hallucinosis and schizophrenia: a negative study . B J Psychiatry 119 : 549 – 50 .
Sluchevskiĭ FI , Tikhomirov SM , Bakharev VD . ( 1986 ) Neuropeptides in the treatment of alcoholism and alcoholic psychoses . Zh Nevropatol Psikhiatr Im S S Korsakova 86 : 244 – 7 .
Soyka M , Helten B , Cleves M , et al. . ( 2013 ) High rehospitalization rate in alcohol-induced psychotic disorder . Eur Arch Psychiatry Clin Neurosci 263 : 309 – 13 .
Soyka M , Raith L , Steinberg R . ( 1988 ) Mean age, sex ratio and psychopathology in alcohol psychoses . Psychopathology 21 : 19 – 25 .
Soyka M , Wegner U , Moeller HJ . ( 1997 ) Risperidone in treatment-refractory chronic alcohol hallucinosis . Pharmacopsychiatry 30 : 135 – 6 .
Soyka M . ( 1990 ) Psychopathological characteristics in alcohol hallucinosis and paranoid schizophrenia . Acta Psychiatr Scand 81 : 255 – 9 .
Soyka M . ( 1994 ) Sucht und Schizophrenie-Nosologische, klinische und therapeutische Fragestellungen . Fortschr Neurol Psychiatr 62 : 71 – 87 .
Surawica FG . ( 1980 ) Alcoholic hallucinosis—a missed diagnosis: differential diagnosis and management . Can J Psychiatry 25 : 57 – 63 .
Szefel ZR . ( 1983 ) [Acute alcohol hallucinosis in women.] . Psychiatr Pol 17 : 137 – 40 .
Vencovsky E , Kolomaznik M , Vyletal J , et al. . ( 1985 ) Injectable clorazepate in alcoholic psychoses . Socijalna Psihijatr 13 : 31 – 5 .
Vicente MN , Ríos RB , Ochoa ME . ( 1990 ) Alcoholic hallucinosis: response to treatment . Arch Neurobiol 53 : 192 – 5 .
Victor M , Hope JM . ( 1958 ) The phenomenon of auditory hallucinations in chronic alcoholism: a critical evaluation of the status of alcoholic hallucinosis . J Nerv Ment Dis 126 : 451 – 81 .
Wendland K-L , Danzer G . ( 1987 ) [Situational and clinical findings in patients with hallucinosis during or after alcohol abuse.] . Schweiz Archiv Neurol Psychiatr 138 : 69 – 83 .
World Health Organization . ( 1992 ) The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines . Geneva : World Health Organization .
- alcohol withdrawal syndrome
- heterogeneity
- antipsychotic agents
- psychotic disorders
- publication bias
- gaba receptors
- schizophrenia
- alcohol withdrawal hallucinosis
- diagnostic and statistical manual
- atypical antipsychotic
- international classification of diseases
- disease remission
- partial response
- first-generation antipsychotics
| Month: | Total Views: |
|---|---|
| November 2017 | 63 |
| December 2017 | 21 |
| January 2018 | 22 |
| February 2018 | 20 |
| March 2018 | 20 |
| April 2018 | 35 |
| May 2018 | 50 |
| June 2018 | 46 |
| July 2018 | 24 |
| August 2018 | 31 |
| September 2018 | 53 |
| October 2018 | 53 |
| November 2018 | 53 |
| December 2018 | 47 |
| January 2019 | 46 |
| February 2019 | 29 |
| March 2019 | 97 |
| April 2019 | 302 |
| May 2019 | 124 |
| June 2019 | 179 |
| July 2019 | 184 |
| August 2019 | 218 |
| September 2019 | 345 |
| October 2019 | 411 |
| November 2019 | 473 |
| December 2019 | 369 |
| January 2020 | 487 |
| February 2020 | 490 |
| March 2020 | 418 |
| April 2020 | 403 |
| May 2020 | 303 |
| June 2020 | 487 |
| July 2020 | 490 |
| August 2020 | 514 |
| September 2020 | 517 |
| October 2020 | 626 |
| November 2020 | 697 |
| December 2020 | 515 |
| January 2021 | 581 |
| February 2021 | 531 |
| March 2021 | 624 |
| April 2021 | 601 |
| May 2021 | 664 |
| June 2021 | 720 |
| July 2021 | 616 |
| August 2021 | 656 |
| September 2021 | 690 |
| October 2021 | 742 |
| November 2021 | 760 |
| December 2021 | 589 |
| January 2022 | 597 |
| February 2022 | 612 |
| March 2022 | 711 |
| April 2022 | 596 |
| May 2022 | 664 |
| June 2022 | 540 |
| July 2022 | 589 |
| August 2022 | 558 |
| September 2022 | 602 |
| October 2022 | 642 |
| November 2022 | 649 |
| December 2022 | 542 |
| January 2023 | 485 |
| February 2023 | 595 |
| March 2023 | 616 |
| April 2023 | 538 |
| May 2023 | 470 |
| June 2023 | 372 |
| July 2023 | 442 |
| August 2023 | 415 |
| September 2023 | 338 |
| October 2023 | 381 |
| November 2023 | 407 |
| December 2023 | 337 |
| January 2024 | 419 |
| February 2024 | 393 |
| March 2024 | 404 |
| April 2024 | 392 |
| May 2024 | 410 |
| June 2024 | 297 |
| July 2024 | 327 |
| August 2024 | 302 |
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1464-3502
- Copyright © 2024 Medical Council on Alcohol and Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Open access
- Published: 13 November 2019
Evidence-based models of care for the treatment of alcohol use disorder in primary health care settings: protocol for systematic review
- Susan A. Rombouts 1 ,
- James Conigrave 2 ,
- Eva Louie 1 ,
- Paul Haber 1 , 3 &
- Kirsten C. Morley ORCID: orcid.org/0000-0002-0868-9928 1
Systematic Reviews volume 8 , Article number: 275 ( 2019 ) Cite this article
7857 Accesses
3 Citations
Metrics details
Alcohol use disorder (AUD) is highly prevalent and accounts globally for 1.6% of disability-adjusted life years (DALYs) among females and 6.0% of DALYs among males. Effective treatments for AUDs are available but are not commonly practiced in primary health care. Furthermore, referral to specialized care is often not successful and patients that do seek treatment are likely to have developed more severe dependence. A more cost-efficient health care model is to treat less severe AUD in a primary care setting before the onset of greater dependence severity. Few models of care for the management of AUD in primary health care have been developed and with limited implementation. This proposed systematic review will synthesize and evaluate differential models of care for the management of AUD in primary health care settings.
We will conduct a systematic review to synthesize studies that evaluate the effectiveness of models of care in the treatment of AUD in primary health care. A comprehensive search approach will be conducted using the following databases; MEDLINE (1946 to present), PsycINFO (1806 to present), Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials (CENTRAL) (1991 to present), and Embase (1947 to present).
Reference searches of relevant reviews and articles will be conducted. Similarly, a gray literature search will be done with the help of Google and the gray matter tool which is a checklist of health-related sites organized by topic. Two researchers will independently review all titles and abstracts followed by full-text review for inclusion. The planned method of extracting data from articles and the critical appraisal will also be done in duplicate. For the critical appraisal, the Cochrane risk of bias tool 2.0 will be used.
This systematic review and meta-analysis aims to guide improvement of design and implementation of evidence-based models of care for the treatment of alcohol use disorder in primary health care settings. The evidence will define which models are most promising and will guide further research.
Protocol registration number
PROSPERO CRD42019120293.
Peer Review reports
It is well recognized that alcohol use disorders (AUD) have a damaging impact on the health of the population. According to the World Health Organization (WHO), 5.3% of all global deaths were attributable to alcohol consumption in 2016 [ 1 ]. The 2016 Global Burden of Disease Study reported that alcohol use led to 1.6% (95% uncertainty interval [UI] 1.4–2.0) of total DALYs globally among females and 6.0% (5.4–6.7) among males, resulting in alcohol use being the seventh leading risk factor for both premature death and disability-adjusted life years (DALYs) [ 2 ]. Among people aged 15–49 years, alcohol use was the leading risk factor for mortality and disability with 8.9% (95% UI 7.8–9.9) of all attributable DALYs for men and 2.3% (2.0–2.6) for women [ 2 ]. AUD has been linked to many physical and mental health complications, such as coronary heart disease, liver cirrhosis, a variety of cancers, depression, anxiety, and dementia [ 2 , 3 ]. Despite the high morbidity and mortality rate associated with hazardous alcohol use, the global prevalence of alcohol use disorders among persons aged above 15 years in 2016 was stated to be 5.1% (2.5% considered as harmful use and 2.6% as severe AUD), with the highest prevalence in the European and American region (8.8% and 8.2%, respectively) [ 1 ].
Effective and safe treatment for AUD is available through psychosocial and/or pharmacological interventions yet is not often received and is not commonly practiced in primary health care. While a recent European study reported 8.7% prevalence of alcohol dependence in primary health care populations [ 4 ], the vast majority of patients do not receive the professional treatment needed, with only 1 in 5 patients with alcohol dependence receiving any formal treatment [ 4 ]. In Australia, it is estimated that only 3% of individuals with AUD receive approved pharmacotherapy for the disorder [ 5 , 6 ]. Recognition of AUD in general practice uncommonly leads to treatment before severe medical and social disintegration [ 7 ]. Referral to specialized care is often not successful, and those patients that do seek treatment are likely to have more severe dependence with higher levels of alcohol use and concurrent mental and physical comorbidity [ 4 ].
Identifying and treating early stage AUDs in primary care settings can prevent condition worsening. This may reduce the need for more complex and more expensive specialized care. The high prevalence of AUD in primary health care and the chronic relapsing character of AUD make primary care a suitable and important location for implementing evidence-based interventions. Successful implementation of treatment models requires overcoming multiple barriers. Qualitative studies have identified several of those barriers such as limited time, limited organizational capacity, fear of losing patients, and physicians feeling incompetent in treating AUD [ 8 , 9 , 10 ]. Additionally, a recent systematic review revealed that diagnostic sensitivity of primary care physicians in the identification of AUD was 41.7% and that only in 27.3% alcohol problems were recorded correctly in primary care records [ 11 ].
Several models for primary care have been created to increase identification and treatment of patients with AUD. Of those, the model, screening, brief interventions, and referral to specialized treatment for people with severe AUD (SBIRT [ 12 ]) is most well-known. Multiple systematic reviews exist, confirming its effectiveness [ 13 , 14 , 15 ], although implementation in primary care has been inadequate. Moreover, most studies have looked primarily at SBIRT for the treatment of less severe AUD [ 16 ]. In the treatment of severe AUD, efficacy of SBIRT is limited [ 16 ]. Additionally, many patient referred to specialized care often do not attend as they encounter numerous difficulties in health care systems including stigmatization, costs, lack of information about existing treatments, and lack of non-abstinence-treatment goals [ 7 ]. An effective model of care for improved management of AUD that can be efficiently implemented in primary care settings is required.
Review objective
This proposed systematic review will synthesize and evaluate differential models of care for the management of AUD in primary health care settings. We aim to evaluate the effectiveness of the models of care in increasing engagement and reducing alcohol consumption.
By providing this overview, we aim to guide improvement of design and implementation of evidence-based models of care for the treatment of alcohol use disorder in primary health care settings.
The systematic review is registered in PROSPERO international prospective register of systematic reviews (CRD42019120293) and the current protocol has been written according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) recommended for systematic reviews [ 17 ]. A PRISMA-P checklist is included as Additional file 1 .
Eligibility criteria
Criteria for considering studies for this review are classified by the following:
Study design
Both individualized and cluster randomized trials will be included. Masking of patients and/or physicians is not an inclusion criterion as it is often hard to accomplish in these types of studies.
Patients in primary health care who are identified (using screening tools or by primary health care physician) as suffering from AUD (from mild to severe) or hazardous alcohol drinking habits (e.g., comorbidity, concurrent medication use). Eligible patients need to have had formal assessment of AUD with diagnostic tools such as Diagnostic and Statistical Manual of Mental Disorders (DSM-IV/V) or the International Statistical Classification of Diseases and Related Health Problems (ICD-10) and/or formal assessment of hazardous alcohol use assessed by the Comorbidity Alcohol Risk Evaluation Tool (CARET) or the Alcohol Use Disorders Identification test (AUDIT) and/or alcohol use exceeding guideline recommendations to reduce health risks (e.g., US dietary guideline (2015–2020) specifies excessive drinking for women as ≥ 4 standard drinks (SD) on any day and/or ≥ 8 SD per week and for men ≥ 5 SD on any day and/or ≥ 15 SD per week).
Studies evaluating models of care for additional diseases (e.g., other dependencies/mental health) other than AUD are included when they have conducted data analysis on the alcohol use disorder patient data separately or when 80% or more of the included patients have AUD.
Intervention
The intervention should consist of a model of care; therefore, it should include multiple components and cover different stages of the care pathway (e.g., identification of patients, training of staff, modifying access to resources, and treatment). An example is the Chronic Care Model (CCM) which is a primary health care model designed for chronic (relapsing) conditions and involves six elements: linkage to community resources, redesign of health care organization, self-management support, delivery system redesign (e.g., use of non-physician personnel), decision support, and the use of clinical information systems [ 18 , 19 ].
As numerous articles have already assessed the treatment model SBIRT, this model of care will be excluded from our review unless the particular model adds a specific new aspect. Also, the article has to assess the effectiveness of the model rather than assessing the effectiveness of the particular treatment used. Because identification of patients is vital to including them in the trial, a care model that only evaluates either patient identification or treatment without including both will be excluded from this review.
Model effectiveness may be in comparison with the usual care or a different treatment model.
Included studies need to include at least one of the following outcome measures: alcohol consumption, treatment engagement, uptake of pharmacological agents, and/or quality of life.
Solely quantitative research will be included in this systematic review (e.g., randomized controlled trials (RCTs) and cluster RCTs). We will only include peer-reviewed articles.
Restrictions (language/time period)
Studies published in English after 1 January 1998 will be included in this systematic review.
Studies have to be conducted in primary health care settings as such treatment facilities need to be physically in or attached to the primary care clinic. Examples are co-located clinics, veteran health primary care clinic, hospital-based primary care clinic, and community primary health clinics. Specialized primary health care clinics such as human immunodeficiency virus (HIV) clinics are excluded from this systematic review. All studies were included, irrespective of country of origin.
Search strategy and information sources
A comprehensive search will be conducted. The following databases will be consulted: MEDLINE (1946 to present), PsycINFO (1806 to present), Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials (CENTRAL) (1991 to present), and Embase (1947 to present). Initially, the search terms will be kept broad including alcohol use disorder (+synonyms), primary health care, and treatment to minimize the risk of missing any potentially relevant articles. Depending on the number of references attained by this preliminary search, we will add search terms referring to models such as models of care, integrated models, and stepped-care models, to limit the number of articles. Additionally, we will conduct reference searches of relevant reviews and articles. Similarly, a gray literature search will be done with the help of Google and the Gray Matters tool which is a checklist of health-related sites organized by topic. The tool is produced by the Canadian Agency for Drugs and Technologies in Health (CADTH) [ 20 ].
See Additional file 2 for a draft of our search strategy in MEDLINE.
Data collection
The selection of relevant articles is based on several consecutive steps. All references will be managed using EndNote (EndNote version X9 Clarivate Analytics). Initially, duplicates will be removed from the database after which all the titles will be screened with the purpose of discarding clearly irrelevant articles. The remaining records will be included in an abstract and full-text screen. All steps will be done independently by two researchers. Disagreement will lead to consultation of a third researcher.
Data extraction and synthesis
Two researchers will extract data from included records. At the conclusion of data extraction, these two researchers will meet with the lead author to resolve any discrepancies.
In order to follow a structured approach, an extraction form will be used. Key elements of the extraction form are information about design of the study (randomized, blinded, control), type of participants (alcohol use, screening tool used, socio-economic status, severity of alcohol use, age, sex, number of participants), study setting (primary health care setting, VA centers, co-located), type of intervention/model of care (separate elements of the models), type of health care worker (primary, secondary (co-located)), duration of follow-up, outcome measures used in the study, and funding sources. We do not anticipate having sufficient studies for a meta-analysis. As such, we plan to perform a narrative synthesis. We will synthesize the findings from the included articles by cohort characteristics, differential aspects of the intervention, controls, and type of outcome measures.
Sensitivity analyses will be conducted when issues suitable for sensitivity analysis are identified during the review process (e.g., major differences in quality of the included articles).
Potential meta-analysis
In the event that sufficient numbers of effect sizes can be extracted, a meta-analytic synthesis will be performed. We will extract effect sizes from each study accordingly. Two effect sizes will be extracted (and transformed where appropriate). Categorical outcomes will be given in log odds ratios and continuous measures will be converted into standardized mean differences. Variation in effect sizes attributable to real differences (heterogeneity) will be estimated using the inconsistency index ( I 2 ) [ 21 , 22 ]. We anticipate high degrees of variation among effect sizes, as a result moderation and subgroup-analyses will be employed as appropriate. In particular, moderation analysis will focus on the degree of heterogeneity attributable to differences in cohort population (pre-intervention drinking severity, age, etc.), type of model/intervention, and study quality. We anticipate that each model of care will require a sub-group analysis, in which case a separate meta-analysis will be performed for each type of model. Small study effect will be assessed with funnel plots and Egger’s symmetry tests [ 23 ]. When we cannot obtain enough effect sizes for synthesis or when the included studies are too diverse, we will aim to illustrate patterns in the data by graphical display (e.g., bubble plot) [ 24 ].
Critical appraisal of studies
All studies will be critically assessed by two researchers independently using the Revised Cochrane risk-of-bias tool (RoB 2) [ 25 ]. This tool facilitates systematic assessment of the quality of the article per outcome according to the five domains: bias due to (1) the randomization process, (2) deviations from intended interventions, (3) missing outcome data, (4) measurement of the outcome, and (5) selection of the reported results. An additional domain 1b must be used when assessing the randomization process for cluster-randomized studies.
Meta-biases such as outcome reporting bias will be evaluated by determining whether the protocol was published before recruitment of patients. Additionally, trial registries will be checked to determine whether the reported outcome measures and statistical methods are similar to the ones described in the registry. The gray literature search will be of assistance when checking for publication bias; however, completely eliminating the presence of publication bias is impossible.
Similar to article selection, any disagreement between the researchers will lead to discussion and consultation of a third researcher. The strength of the evidence will be graded according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach [ 26 ].
The primary outcome measure of this proposed systematic review is the consumption of alcohol at follow-up. Consumption of alcohol is often quantified in drinking quantity (e.g., number of drinks per week), drinking frequency (e.g., percentage of days abstinent), binge frequency (e.g., number of heavy drinking days), and drinking intensity (e.g., number of drinks per drinking day). Additionally, outcomes such as percentage/proportion included patients that are abstinent or considered heavy/risky drinkers at follow-up. We aim to report all these outcomes. The consumption of alcohol is often self-reported by patients. When studies report outcomes at multiple time points, we will consider the longest follow-up of individual studies as a primary outcome measure.
Depending on the included studies, we will also consider secondary outcome measures such as treatment engagement (e.g., number of visits or pharmacotherapy uptake), economic outcome measures, health care utilization, quality of life assessment (physical/mental), alcohol-related problems/harm, and mental health score for depression or anxiety.
This proposed systematic review will synthesize and evaluate differential models of care for the management of AUD in primary health care settings.
Given the complexities of researching models of care in primary care and the paucity of a focus on AUD treatment, there are likely to be only a few studies that sufficiently address the research question. Therefore, we will do a preliminary search without the search terms for model of care. Additionally, the search for online non-academic studies presents a challenge. However, the Gray Matters tool will be of guidance and will limit the possibility of missing useful studies. Further, due to diversity of treatment models, outcome measures, and limitations in research design, it is possible that a meta-analysis for comparative effectiveness may not be appropriate. Moreover, in the absence of large, cluster randomized controlled trials, it will be difficult to distinguish between the effectiveness of the treatment given and that of the model of care and/or implementation procedure. Nonetheless, we will synthesize the literature and provide a critical evaluation of the quality of the evidence.
This review will assist the design and implementation of models of care for the management of AUD in primary care settings. This review will thus improve the management of AUD in primary health care and potentially increase the uptake of evidence-based interventions for AUD.
Availability of data and materials
Not applicable.
Abbreviations
Alcohol use disorder
Alcohol Use Disorders Identification test
Canadian Agency for Drugs and Technologies in Health
The Comorbidity Alcohol Risk Evaluation
Cochrane Central Register of Controlled Trials
Diagnostic and Statistical Manual of Mental Disorders
Human immunodeficiency virus
10 - International Statistical Classification of Diseases and Related Health Problems
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols
Screening, brief intervention, referral to specialized treatment
Standard drinks
World Health Organization
WHO. Global status report on alcohol and health: World health organization; 2018.
The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990–2016. a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5(12):987–1012.
Article Google Scholar
WHO. Global strategy to reduce the harmful use of alcohol: World health organization; 2010.
Rehm J, Allamani A, Elekes Z, Jakubczyk A, Manthey J, Probst C, et al. Alcohol dependence and treatment utilization in Europe - a representative cross-sectional study in primary care. BMC Fam Pract. 2015;16:90.
Morley KC, Logge W, Pearson SA, Baillie A, Haber PS. National trends in alcohol pharmacotherapy: findings from an Australian claims database. Drug Alcohol Depend. 2016;166:254–7.
Article CAS Google Scholar
Morley KC, Logge W, Pearson SA, Baillie A, Haber PS. Socioeconomic and geographic disparities in access to pharmacotherapy for alcohol dependence. J Subst Abus Treat. 2017;74:23–5.
Rehm J, Anderson P, Manthey J, Shield KD, Struzzo P, Wojnar M, et al. Alcohol use disorders in primary health care: what do we know and where do we go? Alcohol Alcohol. 2016;51(4):422–7.
Le KB, Johnson JA, Seale JP, Woodall H, Clark DC, Parish DC, et al. Primary care residents lack comfort and experience with alcohol screening and brief intervention: a multi-site survey. J Gen Intern Med. 2015;30(6):790–6.
McLellan AT, Starrels JL, Tai B, Gordon AJ, Brown R, Ghitza U, et al. Can substance use disorders be managed using the chronic care model? review and recommendations from a NIDA consensus group. Public Health Rev. 2014;35(2).
Storholm ED, Ober AJ, Hunter SB, Becker KM, Iyiewuare PO, Pham C, et al. Barriers to integrating the continuum of care for opioid and alcohol use disorders in primary care: a qualitative longitudinal study. J Subst Abus Treat. 2017;83:45–54.
Mitchell AJ, Meader N, Bird V, Rizzo M. Clinical recognition and recording of alcohol disorders by clinicians in primary and secondary care: meta-analysis. Br J Psychiatry. 2012;201:93–100.
Babor TF, Ritson EB, Hodgson RJ. Alcohol-related problems in the primary health care setting: a review of early intervention strategies. Br J Addict. 1986;81(1):23–46.
Kaner EF, Beyer F, Dickinson HO, Pienaar E, Campbell F, Schlesinger C, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev. 2007;(2):Cd004148.
O'Donnell A, Anderson P, Newbury-Birch D, Schulte B, Schmidt C, Reimer J, et al. The impact of brief alcohol interventions in primary healthcare: a systematic review of reviews. Alcohol Alcohol. 2014;49(1):66–78.
Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. 2005;165(9):986–95.
Saitz R. ‘SBIRT’ is the answer? Probably not. Addiction. 2015;110(9):1416–7.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Bmj. 2015;350:g7647.
Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. Jama. 2002;288(14):1775–9.
Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, part 2. Jama. 2002;288(15):1909–14.
CADTH. Grey Matters: a practical tool for searching health-related grey literature Internet. 2018 (cited 2019 Feb 22).
Higgins JPT. Thompson SG. Quantifying heterogeneity in a meta-analysis. 2002;21(11):1539–58.
Google Scholar
Higgins JPT, Thompson SG, Deeks JJ. Altman DG. Measuring inconsistency in meta-analyses. 2003;327(7414):557–60.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical research ed). 1997;315(7109):629–34.
Higgins JPT, López-López JA, Becker BJ, Davies SR, Dawson S, Grimshaw JM, et al. Synthesising quantitative evidence in systematic reviews of complex health interventions. BMJ Glob Health. 2019;4(Suppl 1):e000858–e.
Higgins, J.P.T., Sterne, J.A.C., Savović, J., Page, M.J., Hróbjartsson, A., Boutron, I., Reeves, B., Eldridge, S. (2016). A revised tool for assessing risk of bias in randomized trials. In: Chandler, J., McKenzie, J., Boutron, I., Welch, V. (editors). Cochrane methods. Cochrane database of systematic reviews, 10 (Suppl 1). https://doi.org/10.1002/14651858.CD201601 .
Schünemann H, Brożek J, Guyatt G, Oxman A, editor(s). Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach (updated October 2013). GRADE Working Group, 2013. Available from gdt.guidelinedevelopment.org/app/handbook/handbook.html ).
Download references
Acknowledgements
There is no dedicated funding.
Author information
Authors and affiliations.
Discipline of Addiction Medicine, Central Clinical School, Faculty of Medicine and Health, University of Sydney, Sydney, NSW, Australia
Susan A. Rombouts, Eva Louie, Paul Haber & Kirsten C. Morley
NHMRC Centre of Research Excellence in Indigenous Health and Alcohol, Central Clinical School, Faculty of Medicine and Health, University of Sydney, Sydney, NSW, Australia
James Conigrave
Drug Health Services, Royal Prince Alfred Hospital, Camperdown, NSW, Australia
You can also search for this author in PubMed Google Scholar
Contributions
KM and PH conceived the presented idea of a systematic review and meta-analysis and helped with the scope of the literature. KM is the senior researcher providing overall guidance and the guarantor of this review. SR developed the background, search strategy, and data extraction form. SR and EL will both be working on the data extraction and risk of bias assessment. SR and JC will conduct the data analysis and synthesize the results. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Kirsten C. Morley .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
PRISMA-P 2015 Checklist.
Additional file 2.
Draft search strategy MEDLINE. Search strategy.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Rombouts, S.A., Conigrave, J., Louie, E. et al. Evidence-based models of care for the treatment of alcohol use disorder in primary health care settings: protocol for systematic review. Syst Rev 8 , 275 (2019). https://doi.org/10.1186/s13643-019-1157-7
Download citation
Received : 25 March 2019
Accepted : 13 September 2019
Published : 13 November 2019
DOI : https://doi.org/10.1186/s13643-019-1157-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Model of care
- Primary health care
- Systematic review
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

Alcohol's Effects on Health
Research-based information on drinking and its impact.
National Institute on Alcohol Abuse and Alcoholism (NIAAA)
Understanding alcohol use disorder.
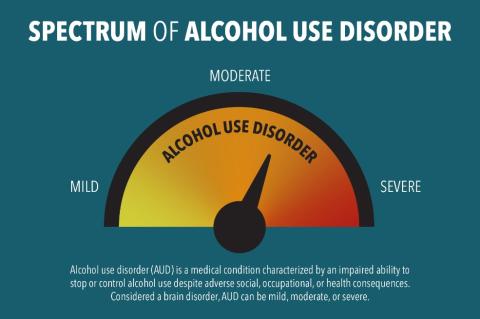
Alcohol use disorder (AUD) is a medical condition characterized by an impaired ability to stop or control alcohol use despite adverse social, occupational, or health consequences. It encompasses the conditions that some people refer to as alcohol abuse, alcohol dependence, alcohol addiction, and the colloquial term, alcoholism. Considered a brain disorder, AUD can be mild, moderate, or severe. Lasting changes in the brain caused by alcohol misuse perpetuate AUD and make individuals vulnerable to relapse. The good news is that no matter how severe the problem may seem, evidence-based treatment with behavioral therapies, mutual-support groups, and/or medications can help people with AUD achieve and maintain recovery. According to the 2022 National Survey on Drug Use and Health, 28.8 million adults ages 18 and older (11.2% in this age group) had AUD in 2021. 1,2 Among youth, an estimated 753,000 adolescents ages 12 to 17 (2.9% of this age group) had AUD during this time frame. 1,2
What Increases the Risk for Alcohol Use Disorder?
A person’s risk for developing AUD depends in part on how much, how often, and how quickly they consume alcohol. Alcohol misuse—defined as drinking in a manner, situation, amount, or frequency that could cause harm to the person who drinks or to those around them—over time increases the risk of AUD. Alcohol misuse includes binge drinking and heavy alcohol use . Other factors also increase the risk of AUD, such as:
- Drinking at an early age. A recent national survey found that among people ages 26 and older, those who began drinking before age 15 were more than three times as likely to report having AUD in the past year as those who waited until age 21 or later to begin drinking. 3 The risk for females in this group is higher than that of males.
- Genetics and family history of alcohol problems. Genetics play a role, with hereditability accounting for approximately 60%; however, like other chronic health conditions, AUD risk is influenced by the interplay between a person’s genes and their environment. Parents’ drinking patterns may also influence the likelihood that a child will one day develop AUD.
- Mental health conditions and a history of trauma. A wide range of psychiatric conditions—including depression, post-traumatic stress disorder, and attention deficit hyperactivity disorder—are comorbid with AUD and are associated with an increased risk of AUD. People with a history of childhood trauma are also vulnerable to AUD.
What Are the Symptoms of Alcohol Use Disorder?
Health care professionals use criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), to assess whether a person has AUD and to determine the severity, if the disorder is present. Severity is based on the number of criteria a person meets based on their symptoms—mild (2–3 criteria), moderate (4–5 criteria), or severe (6 or more criteria).
A health care provider might ask the following questions to assess a person’s symptoms.
In the past year, have you:
- Had times when you ended up drinking more, or longer, than you intended?
- More than once wanted to cut down or stop drinking, or tried to, but couldn’t?
- Spent a lot of time drinking, being sick from drinking, or getting over other aftereffects?
- Wanted a drink so badly you couldn’t think of anything else?
- Found that drinking—or being sick from drinking—often interfered with taking care of your home or family? Or caused job troubles? Or school problems?
- Continued to drink even though it was causing trouble with your family or friends?
- Given up or cut back on activities you found important, interesting, or pleasurable so you could drink?
- More than once gotten into situations while or after drinking that increased your chances of getting hurt (such as driving, swimming, using machinery, walking in a dangerous area, or unsafe sexual behavior)?
- Continued to drink even though it was making you feel depressed or anxious or adding to another health problem? Or after having had an alcohol-related memory blackout?
- Had to drink much more than you once did to get the effect you want? Or found that your usual number of drinks had much less effect than before?
- Found that when the effects of alcohol were wearing off, you had withdrawal symptoms, such as trouble sleeping, shakiness, restlessness, nausea, sweating, a racing heart, dysphoria (feeling uneasy or unhappy), malaise (general sense of being unwell), feeling low, or a seizure? Or sensed things that were not there?
Any of these symptoms may be cause for concern. The more symptoms, the more urgent the need for change.
What Are the Types of Treatment for Alcohol Use Disorder?
Several evidence-based treatment approaches are available for AUD. One size does not fit all and a treatment approach that may work for one person may not work for another. Treatment can be outpatient and/or inpatient and be provided by specialty programs, therapists, and health care providers.
Medications
Three medications are currently approved by the U.S. Food and Drug Administration to help people stop or reduce their drinking and prevent a return to drinking: naltrexone (oral and long-acting injectable), acamprosate, and disulfiram. All these medications are nonaddictive, and they may be used alone or combined with behavioral treatments or mutual-support groups.
Behavioral Treatments
Behavioral treatments—also known as alcohol counseling, or talk therapy, and provided by licensed therapists—are aimed at changing drinking behavior. Examples of behavioral treatments are brief interventions and reinforcement approaches, treatments that build motivation and teach skills for coping and preventing a return to drinking, and mindfulness-based therapies.
Mutual-Support Groups
Mutual-support groups provide peer support for stopping or reducing drinking. Group meetings are available in most communities at low or no cost, and at convenient times and locations—including an increasing presence online. This means they can be especially helpful to individuals at risk for relapse to drinking. Combined with medications and behavioral treatment provided by health care professionals, mutual-support groups can offer a valuable added layer of support.
Please note: People with severe AUD may need medical help to avoid alcohol withdrawal if they decide to stop drinking. Alcohol withdrawal is a potentially life-threatening process that can occur when someone who has been drinking heavily for a prolonged period of time suddenly stops drinking. Doctors can prescribe medications to address these symptoms and make the process safer and less distressing.
Can People With Alcohol Use Disorder Recover?
Many people with AUD do recover, but setbacks are common among people in treatment. Seeking professional help early can prevent a return to drinking. Behavioral therapies can help people develop skills to avoid and overcome triggers, such as stress, that might lead to drinking. Medications also can help deter drinking during times when individuals may be at greater risk of a return to drinking (e.g., divorce, death of a family member).
If you are concerned about your alcohol use and would like to explore whether you might have AUD, please visit the Rethinking Drinking website .
To learn more about alcohol treatment options and search for quality care near you, please visit the NIAAA Alcohol Treatment Navigator .
For more information about alcohol and your health, please visit: niaaa.nih.gov
1 SAMHSA, Center for Behavioral Health Statistics and Quality. 2022 National Survey on Drug Use and Health. Table 5.1A—Substance use disorder for specific substances in past year: among people aged 12 or older; by age group, numbers in thousands, 2021 and 2022 [cited 2023 Dec 29]. Available from: https://www.samhsa.gov/data/sites/default/files/reports/rpt42728/NSDUHDetailedTabs2022/NSDUHDetailedTabs2022/NSDUHDetTabsSect5pe2022.htm#tab5.1a
2 SAMHSA, Center for Behavioral Health Statistics and Quality. 2022 National Survey on Drug Use and Health. Table 5.1B—Substance use disorder for specific substances in past year: among people aged 12 or older; by age group, percentages, 2021 and 2022 [cited 2023 Dec 29]. Available from: https://www.samhsa.gov/data/sites/default/files/reports/rpt42728/NSDUHDetailedTabs2022/NSDUHDetailedTabs2022/NSDUHDetTabsSect5pe2022.htm#tab5.1b
3 Age at drinking onset: age when first drank a beverage containing alcohol (a can or bottle of beer, a glass of wine or a wine cooler, a shot of distilled spirits, or a mixed drink with distilled spirits in it), not counting a sip or two from a drink. AUD: having met two or more of the 11 AUD diagnostic criteria in the past-year according to the American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) AUD risk across different ages at drinking onset is compared using the prevalence ratio weighted by the person-level analysis weight. Derived from the Center for Behavioral Health Statistics and Quality 2022 National Survey on Drug Use and Health (NSDUH-2022-DS0001) public-use file. [cited 2024 Jan 12]. Available from: https://www.datafiles.samhsa.gov/dataset/national-survey-drug-use-and-health-2022-nsduh-2022-ds0001
niaaa.nih.gov
An official website of the National Institutes of Health and the National Institute on Alcohol Abuse and Alcoholism
Cookies on the NHS England website
We’ve put some small files called cookies on your device to make our site work.
We’d also like to use analytics cookies. These send information about how our site is used to a service called Google Analytics. We use this information to improve our site.
Let us know if this is OK. We’ll use a cookie to save your choice. You can read more about our cookies before you choose.
Change my preferences I'm OK with analytics cookies
Robert’s story
Robert was living with an alcohol addiction and was homeless for over 25 years. He was well known in the local community and was identified as one of the top 100 A&E attendees at the Local General Hospital.
He drank all day every day until he would pass out and this was either in the town centre or just by the roadside. In addition, Robert was also incontinent and really struggled with any meaningful communication or positive decision making due to his alcohol usage. This often resulted in local services such as police, ambulance being called in to help. He had no independent living skills and was unable to function without alcohol.
In addition, and due to his lifestyle and presenting behaviours, Robert had a hostile relationship with his family and had become estranged from them for a long period of time.
Robert needed ongoing support and it was identified at the General Hospital that if he was to carry on “living” the way he currently was, then he wouldn’t survive another winter.
On the back of this, Robert was referred to Calico who organised a multi-disciplinary support package for him, which included support with housing as part of the Making Every Adult Matter programme.
After some initial challenges, Robert soon started to make some positive changes.
The intensive, multidisciplinary support package taught him new skills to support him to live independently, sustain his tenancy and make some positive lifestyle changes which in turn would improve his health and wellbeing.
This included providing daily visits in the morning to see Robert and to support him with some basic activities on a daily/weekly basis. This included getting up and dressed; support with shopping and taking to appointments; guidance to help make positive decisions around his associates; support about his benefits and managing his money. In addition, he was given critical support via accessing local groups such as RAMP (reduction and motivational programme) and Acorn (drugs and alcohol service), as well as 1 to 1 sessions with drugs workers and counsellors to address his alcohol addiction.
After six months Robert continued to do well and was leading a more positive lifestyle where he had greatly reduced his A&E attendance. He had significantly reduced his alcohol intake with long periods of abstinence and was now able to communicate and make positive decisions around his lifestyle.
Critically he had maintained his tenancy and continued to regularly attend local groups and other support for his alcohol addiction and had reconnected with some of his family members.
By being able to access these community resources and reduce his isolation he is now engaged in meaningful activities throughout the day and has been able to address some of his critical issues. A small but significant example is that Robert is now wearing his hearing aids which means that he can now interact and communicate more effectively.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Alcohol effects on family relations: a case study
Affiliation.
- 1 Minas Gerais Federal University, School of Nursing. [email protected]
- PMID: 18709271
- DOI: 10.1590/s0104-11692008000700005
Problems related to alcohol abuse have been associated to different factors, regardless of the causes attributed to this phenomenon. Alcohol consumption and dependence is considered a public health problem and deserve attention because of the social, work, family, physical, legal and violence-related risks it represents. This study aimed to identify the effects of alcoholism on family relations and, by means of case management, to encourage the recovery of these relationships. The results show that the problems caused by alcohol abuse impose profound suffering to family members, which contributes to high levels of interpersonal conflict, domestic violence, parental inadequacy, child abuse and negligence, financial and legal difficulties, in addition to clinical problems associated to it.
PubMed Disclaimer
Similar articles
- Nursing students' personal experiences involving alcohol problems. Murphy-Parker D, Martinez RJ. Murphy-Parker D, et al. Arch Psychiatr Nurs. 2005 Jun;19(3):150-8. doi: 10.1016/j.apnu.2005.04.007. Arch Psychiatr Nurs. 2005. PMID: 15991149
- The association of parental alcohol abuse and depression with severe emotional and behavioural problems in adolescents: a clinical study. Peiponen S, Laukkanen E, Korhonen V, Hintikka U, Lehtonen J. Peiponen S, et al. Int J Soc Psychiatry. 2006 Sep;52(5):395-407. doi: 10.1177/0020764006065134. Int J Soc Psychiatry. 2006. PMID: 17278341
- [Out of addictions: Alcohol, or alcohol to alcohol]. Simmat-Durand L, Vellut N, Lejeune C, Jauffret-Roustide M, Mougel S, Michel L, Planche M. Simmat-Durand L, et al. Encephale. 2017 Aug;43(4):326-333. doi: 10.1016/j.encep.2016.02.016. Epub 2016 Jun 29. Encephale. 2017. PMID: 27372354 French.
- Psychosocial difficulties in alcohol dependence: a systematic review of activity limitations and participation restrictions. Levola J, Kaskela T, Holopainen A, Sabariego C, Tourunen J, Cieza A, Pitkänen T. Levola J, et al. Disabil Rehabil. 2014;36(15):1227-39. doi: 10.3109/09638288.2013.837104. Epub 2013 Sep 30. Disabil Rehabil. 2014. PMID: 24079366 Review.
- Marital and family processes in the context of alcohol use and alcohol disorders. Leonard KE, Eiden RD. Leonard KE, et al. Annu Rev Clin Psychol. 2007;3:285-310. doi: 10.1146/annurev.clinpsy.3.022806.091424. Annu Rev Clin Psychol. 2007. PMID: 17716057 Free PMC article. Review.
- Intravenous ketamine for severe alcohol use disorder at Moi Teaching & Referral Hospital, Kenya: a case report. Jaguga F, Kirwa P, Gakinya B, Manji I, Andale T, Kinyanjui D, Kwobah EK, Mwangi F, Werunga K, Kerema J, Kwobah C, Temet E, Songok J, Aruasa WK. Jaguga F, et al. Subst Abuse Treat Prev Policy. 2023 Feb 17;18(1):11. doi: 10.1186/s13011-023-00519-0. Subst Abuse Treat Prev Policy. 2023. PMID: 36803380 Free PMC article.
- Binge-drinking and household role's associations with prevalence of domestic violence: findings from the Thailand smoking and drinking behaviour survey 2017. Wichaidit W, Assanangkornchai S. Wichaidit W, et al. Subst Abuse Treat Prev Policy. 2020 May 20;15(1):34. doi: 10.1186/s13011-020-00278-2. Subst Abuse Treat Prev Policy. 2020. PMID: 32434531 Free PMC article.
- Social competence among children of alcoholic and nonalcoholic parents. Omkarappa DB, Rentala S, Nattala P. Omkarappa DB, et al. J Educ Health Promot. 2019 Apr 24;8:69. doi: 10.4103/jehp.jehp_320_18. eCollection 2019. J Educ Health Promot. 2019. PMID: 31143786 Free PMC article.
- Alcoholic patients' response to their disease: perspective of patients and family. Lima-Rodríguez JS, Guerra-Martín MD, Domínguez-Sánchez I, Lima-Serrano M. Lima-Rodríguez JS, et al. Rev Lat Am Enfermagem. 2015 Nov-Dec;23(6):1165-72. doi: 10.1590/0104-1169.0516.2662. Rev Lat Am Enfermagem. 2015. PMID: 26626009 Free PMC article.
- Problems associated with alcohol consumption by university students. Castaño-Perez GA, Calderon-Vallejo GA. Castaño-Perez GA, et al. Rev Lat Am Enfermagem. 2014 Oct;22(5):739-46. doi: 10.1590/0104-1169.3579.2475. Rev Lat Am Enfermagem. 2014. PMID: 25493668 Free PMC article.
Publication types
- Search in MeSH
Related information
- PubChem Compound
- PubChem Substance
LinkOut - more resources
Full text sources.
- Scientific Electronic Library Online
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram

Alcoholics Anonymous most effective path to alcohol abstinence
A Stanford researcher and two collaborators conducted an extensive review of Alcoholics Anonymous studies and found that the fellowship helps more people achieve sobriety than therapy does.
March 11, 2020 - By Mandy Erickson

The Alcoholics Anonymous model — open to all and free — has spread around the globe, and AA now boasts over 2 million members in 180 nations and more than 118,000 groups. Africa Studio
Alcoholics Anonymous, the worldwide fellowship of sobriety seekers, is the most effective path to abstinence, according to a comprehensive analysis conducted by a Stanford School of Medicine researcher and his collaborators.
After evaluating 35 studies — involving the work of 145 scientists and the outcomes of 10,080 participants — Keith Humphreys , PhD, professor of psychiatry and behavioral sciences, and his fellow investigators determined that AA was nearly always found to be more effective than psychotherapy in achieving abstinence. In addition, most studies showed that AA participation lowered health care costs.
AA works because it’s based on social interaction, Humphreys said, noting that members give one another emotional support as well as practical tips to refrain from drinking. “If you want to change your behavior, find some other people who are trying to make the same change,” he said.
The review was published March 11 in Cochrane Database of Systematic Review . Cochrane requires its authors to undertake a rigorous process that ensures the studies represented in its summaries are high-quality and the review of evidence is unbiased.
“ Cochrane Reviews are the gold standard in medicine for integration of all the research about a particular intervention,” Humphreys said. “We wanted to do this work through Cochrane because of its rigor and reputation.”
The other co-authors are a researcher from Harvard Medical School and a researcher from the European Monitoring Center for Drugs and Drug Addiction.
Though well-known, AA faces skepticism
Although AA is well-known and used by millions around the world, mental health professionals are sometimes skeptical of its effectiveness, Humphreys said. Psychologists and psychiatrists, trained to provide cognitive behavioral therapy and motivational enhancement therapy to treat patients with alcohol-use disorder, can have a hard time admitting that the lay people who run AA groups do a better job of keeping people on the wagon.
Early in his career, Humphreys said, he dismissed AA, thinking, “How dare these people do things that I have all these degrees to do?”
Humphreys noted that counseling can be designed to facilitate engagement with AA — what he described as “an extended, warm handoff into the fellowship.” For the review article, Humphreys and his colleagues evaluated both AA and 12-step facilitation counseling.

Keith Humphreys, a co-author of the review, said that although AA is well-known and used by millions around the world, mental health professionals are sometimes skeptical of its effectiveness. Paul Sakuma
AA began in 1935 when two men in Akron, Ohio, were searching for a way to stay sober; they found it by forming a support group. They later developed the 12 steps, the first being accepting one’s inability to control drinking; the last, helping others sustain sobriety by becoming a sponsor of a new member. The AA model — open to all and free — has spread around the globe, and AA now boasts over 2 million members in 180 nations and more than 118,000 groups.
Though the fellowship has been around for more than eight decades, researchers have only recently developed good methods to measure its effectiveness, Humphreys said.
For the Cochrane review, the researchers found 57 studies on AA; of those, 35 passed their rigorous criteria for quality. The studies used various methods to measure AA’s effectiveness on alcohol use disorder: the length of time participants abstained from alcohol; the amount they reduced their drinking, if they continued drinking; the consequences of their drinking; and health care costs.
Most of the studies that measured abstinence found AA was significantly better than other interventions or no intervention. In one study, it was found to be 60% more effective. None of the studies found AA to be less effective.
In the studies that measured outcomes other than complete abstinence, AA was found to be at least as effective. For the studies that considered costs, most showed significant savings associated with AA participation: One found that AA and 12-step facilitation counseling reduced mental health costs by $10,000 per person.
The researchers looked only at studies of AA; they excluded Narcotics Anonymous and organizations focused on addiction to other substances. While it was beyond the scope of their study, Humphreys said the AA review is “certainly suggestive that these methods work for people who use heroin or cocaine.”
Humphreys noted that the findings were consistent whether the study participants were young, elderly, male, female, veterans or civilians; the studies in the review were also conducted in five different countries. “It absolutely does work,” he said of AA’s method.
He added that he feels validated in giving advice to so many patients to try AA: “That was really good advice, and that continues to be good advice,” he said.
Humphreys is a member of the Wu Tsai Neurosciences Institute at Stanford.
The research was not funded.
Stanford’s Department of Psychiatry and Behavioral Sciences supported the work.
Hear Humphreys discuss the research in a 1:2:1 podcast hosted by Paul Costello, senior communications strategist and adviser for Stanford Health Care and the School of Medicine.
- Mandy Erickson Mandy Erickson is a science writer in the Office of Communications. Email her at [email protected].
About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
The majestic cell
How the smallest units of life determine our health

Quick Links
Get in touch.

Unlock the Latest Knowledge that Can You Help You Achieve More in Life with More Confidence
Print and Digital Options Available
My True Story of Alcoholism, Addiction and the Choice to Live

At 8 years old, I stared out the second-floor window of our apartment. Children my age played on the playground. The windowpane was warm. The sky was clear. I remember this day now as sharp as the edge of a knife because in that moment, I wanted to die.
By this time in my life, I had been abused by my family—sexually and emotionally—for as long as I could remember. I hadn’t even lived a decade, and I hurt so much I wished it were over already.
Twenty years later, I was an alcoholic and a meth addict.
Related: ‘I Was an Everything Addict’: The Bizarre Transformation of Andrew Zimmern
When SUCCESS asked me if I would write about my personal story of getting sober and staying sober, I agreed because I know that my rich life today—as blessed and real and challenging and joyful as it is —wouldn’t be possible without the horror and sadness and hurt that came before it. Today my life is so remarkably blessed, I probably make people sick. I’m happy. I’m loved. I’m what a lot of people would consider successful. But none of it would be what it is without the suffering—the pain caused by others and the pain I brought on myself. That kind of pain isn’t unique to me. I’ve heard stories that make my life sound like Disneyland. Some pain is soul-deep. It’s life-altering. But so is our response to that pain.
I know that my life today—as blessed and real and challenging and joyful as it is—wouldn’t be possible without the horror and sadness and hurt that came before it.
This is a story that I’ve only told in recovery meetings, a story some people who have known me for years don’t even know. I’m sharing it because I want others to see their own stories in the same way: as a starting point not as an ending.
Into the Abyss
I had my first real drink when I was 10 years old. More than just a sip out of someone’s glass, the cold beer with a lime that my new stepdad handed me was all mine. I remember lying down, getting a little woozy, and later, eating some crackers to settle my stomach. One beer was plenty for a 45-pound girl.
I grimaced as it went down, but I reveled in the layer of padding the alcohol put between me and the real world, as if someone had wrapped the block of ice constantly pressed against my soul in a fluffy towel. The pain wasn’t as acute. The constant sense of danger wasn’t as imminent.
Soon I was smuggling airline-sized bottles of booze to school and hiding them in my locker so I could sneak a sip before lunch or gym or any other point in the day when one of my two best friends, depression and anxiety, crippled me socially.
At times, I’m told, I appeared self-assured . I walked with my head up and shoulders back (thanks to years in ballet). I spoke with confidence (thanks to a love of words and theater). From the outside, I probably appeared condescendingly cool at times. But the view looking out was very different.
I was hyper-aware of other people, on constant high-alert thanks to my home life. I had a persistent belief that everyone was talking about me, plotting against me or wishing me harm. I might have looked like a turtle sunning itself on a rock, but I felt like a frog in a frying pan.
By high school, I was drinking every weekend. In my world, drinking was as normal as ordering pizza. When adults sipped iced tea with dinner at a restaurant, I was dumbfounded. How could someone over the legal drinking age not be drinking? I had no idea that most people were living a very different life from mine, a life in which alcohol did not have a daily, starring role. I had been raised to believe that adults drank just like they worked jobs, drove cars and complained about taxes. It was part of being an adult .
I now know that, for the most part, the adults in my life weren’t trying to hurt me. They were living under the same delusion that their life was normal, their insane reasoning sound, and their self-centered choices rational. They, too, endured abuse and trauma that drove them to deaden their pain. The best numbing agent they found was alcohol, so they handed it down to me.
Despite my drinking and emotional instability, I earned a full scholarship to college. I carried a flask of whiskey to treat the searing depression that gripped me as soon as I put some distance between myself and my family. I was happy when I was drunk, but I was in a crying fit at least once a week and found myself in a rage over the smallest offenses. I alternated between giving people the cold shoulder and flooding them with emotional drama. As I look back, I realize that sharing daily life with my roommate—a normal, well-loved, faith-filled human being—contrasted completely with my identity. I couldn’t help acknowledge the truth I constantly tried to run from: I was damaged and hopeless.

So I drank more. I smoked a pack of cigarettes a day. I experimented with drugs. I broke hearts and had mine broken. And I lost my scholarship.
Filling the Void
For the next five years, I did everything I could to blame my deep woundedness on something other than a withering soul caused by abuse, neglect and my own increasing self-centeredness. I switched jobs, apartments and boyfriends at regular six-month intervals. I tried turning to God. I prayed. I joined a couple of churches. I was confirmed one year, then dunked the next. I did Bible studies and learned to meditate . I prayed and yelled and pleaded with God to fix me, heal me, forgive me, do anything with me that would make me feel like a normal human being.
I tried therapy. It was during these five years that I began having panic attacks. Gradually they became more intense and more frequent. Ten times a day, fear poured over my being in a way that convinced me I was about to die. I got help. I got medication. And thankfully I got out of agoraphobia and back into the world. But I didn’t stop drinking.
Related: What Agoraphobia Taught Me About Fear Versus Facts
Drinking wasn’t the problem, as far as I could see. It was the solution. It was the cleansing release that never seemed to come from on high. I drank whiskey at the bar and gulped wine in front of the TV. I started popping tiny speed pills to keep me going after an all-day bender. I ate less and slept more. I flirted with an ulcer, fought headaches, and developed chronic pain that gripped every area of my body and gave me a reason to take pain pills.
Then at 26, I decided enough was enough and I got married. Fearing my own recklessness and lack of control, I clung to the idea that settling down would slow my drinking and having a partner would ease my emotional turmoil. But of course, a person can’t fix another person. A human can’t be a higher power. One partner can’t carry the weight meant for two. So I moved out after a year, and we divorced.
I lived in an efficiency apartment for a few months after we separated. The bleak emptiness that set in during this time was unspeakable. I felt like an utter failure. No life stretched out before me as it always had. I would be no one’s wife, no one’s mother, no one’s anything. I would have no degree, no career, no purpose. I felt like one of the corn husk dolls my grandmother gave me when I was a child: faceless and meaningless, folded over and over and over on myself.
That’s when I chose to use drugs. The moment when I knew I would kill myself if I had to wake up one more day, I made the call to a friend and asked her to give me some meth.
Most people look at addiction or alcoholism from the outside and wonder, How could they sink so low? What these well-meaning people don’t understand is that sometimes addiction and alcoholism feel like a step up from someplace worse.
The first time I used meth, I thought, Wow, I’m an addict. I didn’t fight it. I didn’t care that I couldn’t control my mind and body. It was a relief, all of it, from the lightness that took over my limbs and the smile that spread across my face to the knowledge that I was, officially and forever, an addict. Because an addict has a purpose, a reason for living, a mission in life: to use drugs. Being an addict was far and away better than being a husk.
Arrival of Grace
The day I walked into my first recovery meeting, I hadn’t worked in nearly two years. I hadn’t bathed in a month. I had no running water, phone or heat in my duplex for almost a year. I didn’t brush my teeth anymore. I had sores on my head from not washing my hair and sores on my face from a relentless obsession that meth gives you for picking at anything close by. I weighed 78 pounds and experienced frequent kidney infections, seizures and voices calling my name in the darkness. I nearly died more than once. I stayed awake for three or four days at a time, getting high and drinking myself into alcohol poisoning. I blacked out often and am still missing large chunks of my timeline.
But I remember one moment as vividly as wanting to kill myself that day when I was 8 years old: I remember the second I knew I was done.
Some say that our lives change in a moment, but really, if we think about it, the actual change happened in a heartbeat.
Some say that our lives change in a moment. We might believe it took us 10 years to quit a job or fix a marriage, but really, if we think about it, the actual change happened in a heartbeat. We might think about changing for 10 years, we might tell ourselves we should make the change for 10 years, but the real change , that decision we make like a snap, occurs within us in a fraction of an instant.
For me it happened one gray morning while sitting in a room with another addict and watching what happened as alcohol and drugs shrank this larger-than-life person into a confused, quivering ball of shame. I looked at him and saw myself clearly, starkly, suddenly. I felt the strangling denial deep down inside me switch off and a light flicker on.
I’m done , I thought.
I made a life-altering decision in the thinnest slice of eternity, as if in that messy room just before the sun came up, the divine reached out to the present moment like a crack of light under the door. I was struck hard with truth so profound and so filled with grace that I couldn’t look away. And I knew: I’m worth living for.
Silently, I asked, Now what?
Looking back, this is the first proof that I’d really changed. Unlike countless times before when I had gritted my teeth, determined to solve all of my problems myself, this time I asked for help. In my most shameful moment, rather than hiding or posturing or denying, I let people see me.
I asked, “Now what? Where do I go? What do I do? Tell me, and I’ll do it.” First the someone I asked was God. Then it was someone with a list of recovery meetings.
In the early 1800s, Johann Wolfgang von Goethe published Faust , a play about a man who makes a deal with the devil for earthly satisfaction in exchange for his soul. In it, the main character says, “Whatever you can do or believe you can do, begin it. Action has magic, grace and power in it.”
That’s the only difference between me now and me on that gray morning. Grace arrived, and I didn’t just let it in. I’ve gotten up every day since and left the door wide open.
Surviving the Flood
Living sober isn’t all rainbows and butterflies. The first years of sobriety were filled with terrible realizations, paralyzing fear and daily confusion. All of the pain I’d been trying to deny, all of the wounds I’d been trying to ignore, and all of the memories I’d been trying to repress came slithering out of the darkness. Quitting drinking and using was one thing. Staying quit was another.
It reminds me of that story about the little Dutch boy who put his finger in the dam to stop up the hole. He stayed out all night, waiting for someone to come and fix it, whistling to himself to keep up his spirits. But eventually, if no one had come, he would have taken his finger out and the water would have broken through in a torrent.
For the first few weeks in sobriety, I was a whistling Dutch boy. Then the flood came. Grief, shame, sorrow, anger, bewilderment, self-hatred and random bursts of unbridled joy. I distanced myself from my family as the truth of our codependence and their own sickness dawned on me like an unwelcome hangover. Eventually, my stepdad, who was always supportive of my sobriety, died of cancer caused by his drinking. In his final year, we were closer than ever, and I asked his forgiveness and gave it in return.
Related: How to Forgive
As I tried to ride the waves of realization that arose in my now-clear head, I threw myself into a spiritual program of recovery that sustains me even today. This means, essentially, that I follow a path carved out by countless other sober people who have braved the same floods. I pray to a God that I now know loves me beyond measure, read books written by people who understand what it’s like to live in my skin, and write spirals full of self-reflection and stark unveiling only to share all that mess with another person. I’m guided along the way by women and men who are a few steps ahead of me on the path. And I have the privilege to guide others who come behind me.
Since getting sober, I’ve learned to love myself, forgive myself , and live as the person I was created to be. I’ve earned my college degree, married an incredible man, bought a house, become a mother, created a family of choice, won an Emmy, served on the editorial staffs of seven magazines and started a thriving business I love. My chronic pain is healed, the anxiety and depression are gone, and that feeling of shame has been lifted because I’ve also gotten more therapy, ended my relationships with toxic people no matter how we’re related, and been willing to feel the worst pain in order to find the most freedom. A life like this takes a lot of work for someone like me. Maybe for all of us.
That’s the thing about asking, Now what? I actually have to listen to the answer and be willing to act. Even if it scares me or confuses me or makes me mad. Today the next right action is to share my journey with you, even though it means I cringe as I hit send to file this story; bite my nails while I wait for it to be published; and ignore the fear in my head that tells me I’ll be judged, criticized, or even unduly praised for what I’ve done, seen, and lived.
In the end, I am who I am, and I live this life instead of that old, painful one because I was desperate enough to have enough faith in someone else’s solution for my problems. I can’t really take credit for my sobriety. I believe God keeps me sober one day at a time, but I believe my connection with this higher power depends utterly on my honest and sincere and consistent action—no matter how inconvenient or uncomfortable.
This is what I want you to know: Your suffering is just a starting point. It’s up to you to move, to act and to receive the grace that accompanies even the smallest effort. I know firsthand that if you don’t know you have a choice, then you don’t have one.
Today you have a choice. You can keep asking why and allow your suffering to be the name tag on your life. Or you can start asking, Now what? You can leave the door open for grace and see what it lets in.
Related: Face Your Demons
This article originally appeared in the February 2017 issue of SUCCESS magazine .
Amy Anderson
Amy Anderson is the former senior editor of SUCCESS magazine, an Emmy Award-winning writer and founder of Anderson Content Consulting. She helps experts, coaches, consultants and entrepreneurs to discover their truth, write with confidence, and share their stories so they can transform their past into hope for others. Learn more at AmyKAnderson.com and on Facebook.
5473 Blair Road, Suite 100 PMB 30053 Dallas, TX 75231
Copyright © 2024 SUCCESS Magazine. All rights reserved.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Global health
- BMJ Journals
You are here
- Volume 2013, Issue
- Alcoholic cardiomyopathy
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-3932-3803 Antonio Mirijello ,
- Gabriele Vassallo ,
- Raffaele Landolfi ,
- Giovanni Addolorato
- Department of Internal Medicine , Catholic University of Rome, Rome , Italy
- Correspondence to Dr Antonio Mirijello, antonio.mirijello{at}gmail.com
https://doi.org/10.1136/bcr-2013-201449
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Description
A 42-year-old man was admitted to our internal medicine unit because of exertional dyspnoea and peripheral oedema. The patient was also experiencing fatigue and reduction in effort tolerance. He denied palpitations or chest pain. Medical history was unremarkable for cardiovascular events; he did not smoke and denied family history of heart disease. However, the patient was found to have a history of alcohol dependence lasting 20 years, with a mean alcohol consumption of 15–20 drinks/day (1 drink=12.5 g ethanol).
The patient started a multidisciplinary programme, including counselling and baclofen 10 mg three time a day, to achieve and maintain total alcohol abstinence at our Alcohol Addiction Unit. 1
A chest X-ray performed 1 month after ICD implantation shows typical signs of alcoholic cardiomyopathy ( figure 1 ). The patient has been totally abstinent from alcohol since 3 months.
- Download figure
- Open in new tab
- Download powerpoint
Chest X-ray showing signs of alcoholic cardiomyopathy (cardiomegaly, venous vessels enlargement, pulmonary oedema).
Learning points
Alcohol misuse is one of the causes of dilated cardiomyopathy.
The exact pathogenesis of alcoholic cardiomyopathy is still unclear.
Treatment must include complete alcohol abstinence together with the treatment of heart failure.
- Addolorato G ,
- Mirijello A ,
- d'Angelo C ,
Contributors All the authors managed the patient during hospitalisation. AM, GV and GA are currently managing the patient in the Alcohol Addiction Unit. All the authors wrote and revised the manuscript.
Competing interests None.
Patient consent Obtained.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:

Drinking alcohol before conceiving a child could accelerate their aging – new research in mice
Professor of Physiology, Texas A&M University
Disclosure statement
Michael Golding receives funding through a Medical Research Grant from the W. M. Keck Foundation and a research grant from the NIH through the National Institute on Alcohol Abuse and Alcoholism (NIAAA).
Texas A&M University provides funding as a founding partner of The Conversation US.
View all partners
The conditions within a person’s home, family and community affect their ability to stay healthy. Scientists studying these social determinants of health are trying to understand whether nature or nurture has a stronger effect on a person’s ability to fight disease.
I am a developmental physiologist studying the ways that drinking affects fetal development and lifelong health. Although researchers have long recognized that a father’s alcohol abuse negatively affects his children’s mental health and social development , it hasn’t been clear if paternal drinking has any lasting biological effects on his offspring’s physical health.
My lab’s recently published research shows that chronic alcohol use from both parents has an enduring effect on the next generation by causing their offspring to age faster and become more susceptible to disease.
Fetal alcohol spectrum disorders
According to the National Institutes of Health, nearly 11% of adults in the U.S. have an alcohol use disorder. Heavy drinking causes multiple health issues , including liver disease, heart problems, declining cognitive function and accelerated aging .
Parents may pass these health problems on to their children. Fetal alcohol spectrum disorders refer to a wide range of alcohol-related physical, developmental and behavioral deficits that affect as many as 1 in 20 U.S. schoolchildren .

Children with fetal alcohol spectrum disorders experience an early onset of adult diseases , including type 2 diabetes and heart disease. Cardiovascular disease first appears during adolescence for people with these disorders, while the rest of the population is affected typically in their 40s and 50s. Children with fetal alcohol spectrum disorders are also more likely to be hospitalized and have lifespans that are 40% shorter than children without these conditions.
However, it has been unclear whether these health problems are because of life circumstances – people with fetal alcohol spectrum disorders have high rates of psychiatric disorders , which cause stress that makes them more susceptible to aging and disease – or if their parents’ substance use directly causes lasting negative effects to their health. In other words, can a parent’s alcohol abuse before conception directly influence their offspring’s physical health and lifespan?
Mom and dad drinking
In our study, my colleagues and I used a mouse model to measure the effects that alcohol use by mom, dad or both parents around the time of conception have on their offspring aging and chronic disease. The mice chose when and how much alcohol to drink.
We found that paternal and maternal drinking both cause harmful changes to their offspring’s mitochondria . Mitochondria – often called the battery of the cell – control many aspects of aging and health . Like a cellphone battery, mitochondria deteriorate over time and cause cells to lose their ability to repair damage and control metabolism.
Our experiments in mice show that dad’s drinking causes a defect in mitochondrial function that first emerges during fetal development and persists into adult life , causing the offspring to age faster. For example, paternal alcohol exposure caused a twofold increase in age-related liver disease, suggesting that parental alcohol use – particularly by the father – could have significant implications on aging and age-related diseases.
Importantly, we found that when both parents drank, the effects on their offspring were worse than when only one parent consumed alcohol. For example, we observed a threefold increase in age-related liver scarring when both parents consumed alcohol.
Treating fetal alcohol syndrome
People with fetal alcohol syndrome face lifelong challenges , including problems with hand-eye coordination and difficulties with memory and attention.
Early educational interventions for children with fetal alcohol spectrum disorders, like using visual and auditory materials instead of print, can provide additional structure to help facilitate learning.
Although my team and I examined chronic alcohol exposure, we do not know if moderate alcohol use also causes mitochondrial problems. We also don’t know if these same effects emerge in people who haven’t been diagnosed with fetal alcohol spectrum disorders but whose parents drank heavily. Whether paternal drinking influences human embryonic development is still unclear, although emerging studies are beginning to suggest it does.
The next step is to explore if interventions that focus on mitochondrial health, such as exercise and specific diets , can improve health outcomes for people with fetal alcohol spectrum disorders.
- Fetal development
- Alcohol abuse
- Fetal Alcohol Spectrum Disorder
- Fetal Alcohol Syndrome
- New research
- STEEHM new research

Director of STEM

Community member - Training Delivery and Development Committee (Volunteer part-time)

Chief Executive Officer

Finance Business Partner

Head of Evidence to Action
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Alcohol-induced blackouts: A review of recent clinical research with practical implications and recommendations for future studies
Reagan r. wetherill.
1 Center for Studies of Addiction, Department of Psychiatry, Perelman School of Medicine of the University of Pennsylvania, Philadelphia, PA 19104
2 Department of Psychology, University of Texas at Austin, Austin, TX 78712
Alcohol-induced blackouts, or memory loss for all or portions of events that occurred during a drinking episode, are reported by approximately 50% of drinkers and are associated with a wide range of negative consequences, including injury and death. As such, identifying the factors that contribute to and result from alcohol-induced blackouts is critical in developing effective prevention programs. Here, we provide an updated review (2010–2015) of clinical research focused on alcohol-induced blackouts, outline practical and clinical implications, and provide recommendations for future research.
A comprehensive, systematic literature review was conducted to examine all articles published between January 2010 through August 2015 that focused on examined vulnerabilities, consequences, and possible mechanisms for alcohol-induced blackouts.
Twenty-six studies reported on alcohol-induced blackouts. Fifteen studies examined prevalence and/or predictors of alcohol-induced blackouts. Six publications described consequences of alcohol-induced blackouts, and five studies explored potential cognitive and neurobiological mechanisms underlying alcohol-induced blackouts.
Conclusions
Recent research on alcohol-induced blackouts suggests that individual differences, not just alcohol consumption, increase the likelihood of experiencing an alcohol-induced blackout, and the consequences of alcohol-induced blackouts extend beyond the consequences related to the drinking episode to include psychiatric symptoms and neurobiological abnormalities. Prospective studies and a standardized assessment of alcohol-induced blackouts are needed to fully characterize factors associated with alcohol-induced blackouts and to improve prevention strategies.
Introduction
Alcohol use is a pervasive problem with well-known deleterious effects on memory. Alcohol-induced memory impairments vary in severity, ranging from mild deficits to alcohol-induced blackouts ( Heffernan, 2008 ; White, 2003 ). Alcohol-induced blackouts are defined as amnesia, or memory loss, for all or part of a drinking episode. During a blackout, a person is able to actively engage and respond to their environment; however, the brain is not creating memories for the events. Alcohol-induced blackouts are often confused with passing out from alcohol, but blacking out and passing out are very different states of consciousness. A person experiencing a blackout is conscious and interacting with his or her environment; whereas, a person who has passed out from alcohol has lost consciousness and capacity to engage in voluntary behavior. Memory deficits during a blackout are primarily anterograde, meaning memory loss for events that occurred after alcohol consumption ( White, 2003 ). It is important to note that short-term memory remains intact during an alcohol-induced blackout, and as such, an intoxicated person is able to engage in a variety of behaviors, including having detailed conversations and other more complex behaviors like driving a vehicle, but information about these behaviors is not transferred from short-term to long-term memory, which leads to memory deficits and memory loss for these events ( White, 2003 ). There is no objective evidence that a person is in an alcohol-induced blackout ( Pressman and Caudill, 2013 ), thus it can be difficult or impossible to know whether or not a drinker is experiencing a blackout ( Goodwin, 1995 ). This is similar to the fact that one cannot know whether another person has a headache; the experience is happening inside that person’s brain, with no clear observable indices.
Based on the duration and extent of alcohol-induced memory loss, researchers have described two qualitatively distinct types of blackouts: en bloc and fragmentary ( Goodwin et al., 1969a ; Goodwin et al., 1969b ). En bloc blackouts typically occur at higher blood alcohol concentrations (BAC), have a distinct onset, and involve complete memory loss for a specific period of the drinking event. Fragmentary blackouts (also known as “brown outs” or “gray outs”), however, involve partial amnesia during a drinking episode, but one may be able to recall events of the episode with relevant cues ( Jennison and Johnson, 1994 ). Fragmentary blackouts occur more frequently than en bloc blackouts ( Goodwin et al., 1969b ; Hartzler and Fromme, 2003 ; White et al., 2004 ), but neither type appear to occur until breath alcohol concentrations (BrACs) are 0.06 g/dl or greater ( Hartzler and Fromme, 2003 ). Estimates of BrACs indicated that most blackouts occurred around 0.20 g/dl, but as low as 0.14 g/dl ( Ryback, 1970 ). According to a study of amnesia in people arrested for alcohol-related offenses ( Perry et al., 2006 ), the probability of a fragmentary or an en bloc blackout was 50/50 at a BrAC of 0.22 g/dl and the probability of an en bloc blackout was 50/50 at a BrAC of 0.31 g/dl. As such, blackouts typically occur during binge or excessive drinking episodes. Further, gulping drinks and drinking on an empty stomach ( Goodwin, 1995 ; Perry et al., 2006 ), which cause a rapid rise and high peak BAC, can also increase the likelihood of experiencing an alcohol-induced blackout.
Although alcohol-induced blackouts were previously thought to occur only in individuals who were alcohol dependent ( Jellinek, 1946 ), we now know that blackouts are quite common among healthy young adults. In fact, approximately 50% of college students who consume alcohol report having experienced an alcohol-induced blackout ( Barnett et al., 2014 ; White et al., 2002 ). Consequently, there has been increased media and research interest in alcohol-induced blackouts over the past two decades with at least three reviews describing the phenomenon ( Lee et al., 2009 ; Rose and Grant, 2010 ; White, 2003 ) a brief, descriptive section in a review on excessive alcohol use ( White and Hingson, 2013 ) and a recently published memoir that poignantly describes the phenomenology of blackouts ( Hepola, 2015 ) ( Figure 1 ). Therefore, this systematic review provides an update (2010–2015) on the clinical research focused on alcohol-induced blackouts, outlines practical and clinical implications, and provides recommendations for future research.

Number of published journal articles or reviews that evaluate alcohol-induced blackouts per year (1985 to 2015). The graph represents published articles and reviews published in English and includes both animal and human studies with the terms “blackout” and “alcohol” in the title, abstract, and/or keyword.
Materials and Methods
A Medline search was conducted in September 2015 to identify publications that included either “alcohol” or “ethanol” as one search term and at least one blackout-related search term (e.g., “blackouts”, “blacked out”). The wildcard character “*” was used to include all forms of the root word. The most recent review of blackouts was published in 2010 ( Rose and Grant, 2010 ) and there has since been extensive new research; therefore we limited our review to articles published between January 2010 and August 2015. After removing duplicates, case studies, articles that were not published in English, and studies not conducted in humans, the remaining publications were reviewed to determine whether they met inclusion criteria, namely that the study examined vulnerabilities, consequences, and possible mechanisms for alcohol-induced blackouts.
Study Characteristics
A total of 26 publications met the criteria to be included in the review (see Table 1 for study details). Fifteen studies examined prevalence and/or predictors of alcohol-induced blackouts. Six publications described consequences of alcohol-induced blackouts, and five studies explored potential cognitive and neurobiological mechanisms underlying alcohol-induced blackouts.
Characteristics of Published Studies Examining Alcohol-Induced Blackouts between 2010 and 2015
| Study reference | Design | Sample | Methods | Blackout-related findings |
|---|---|---|---|---|
| Multisite, multicohort, prospective | 1,053 first-year college students, Ages: 16–21 (M=18.4), 58% female | Blackouts and getting physically sick were most common negative consequences 54.2% of subjects endorsed a blackouts during first year of college Almost 1 in 5 drinking weeks resulted in a blackout | ||
| Cross-sectional | 307 incoming freshman college students, 59% female | Freshman who Drink to Get Drunk (DTGD) were more likely to have consumed alcohol prior to going out, participated in a drinking game, drank heavily on a non-school night, used liquor/beer, combined alcohol and drugs, experienced a hangover, vomited, passed out, and/or blacked out 50% of those who DTGD endorsed a blackout during past 30 days | ||
| Cross-sectional | 150 21-year-olds, 50% female | birthday celebration | 40% reported experiencing a blackout during their 21 birthday celebration Physical (e.g., blackout and hangover) and behavioral risks were predicted by higher estimated BACs | |
| Prospective | 166 subjects from the community who consume alcohol, Ages: 23–29 (M=25.9), 60% female | Drinking in hazardous situations, blackouts, and tolerance were most common alcohol problem Blackouts were more prevalent in whites and males Age of onset for blackouts occurred at ~19 years of age | ||
| Cross-sectional | 272 college students, Ages: 18–25 (M=19.9), 52% male | Binge drinkers were more likely to define binge drinking in an extreme manner such that the drinking results in vomiting or blacking out | ||
| Cross-sectional | 942 Australian university students participating in an Internet-based intervention trial and scored ≥8 on AUDIT, Ages: 17–24 (M=19.4), 53% male | Blackouts were one of the most frequently reported non-academic problem (44.8%) Several negative consequences, including blackouts, were rated as positive by a large proportion of the sample | ||
| Multisite, cross-sectional | 2,546 college students, 59% female | 25% of students reported blacking out during at least one occasion in which prepartying occurred in the past 30 days Greek affiliation, family history of alcohol abuse, frequency of prepartying, and both playing drinking games and consuming shots of liquor while prepartying increased the likelihood of blacking out | ||
| Prospective | 1,154 young adults, Mean age 23.8 years, 65% female | 66% of sample reported experiencing an alcohol-induced blackout Women were more likely to report blackouts than men Compared with women with a maternal family history of problematic alcohol use, men with a maternal family history of problematic alcohol use were more than twice as likely to report blackouts | ||
| Cross-sectional | 192 regularly drinking college students, Ages: 18–24 (M=19.1), 52% male | SEM analyses revealed a direct association between enhancement motives and blackouts | ||
| Prospective | 552 college students, Ages: 18–24, 57% age 21, 62% female | SEM analyses revealed an indirect association between enhancement motives at Time 1 and blackouts at Time 2 through increased levels of alcohol use at Time 2 | ||
| Prospective | 336 first-year student drinkers, Ages: 18–20 (M=18.2), 53% male | Students who reported higher levels of alcohol quantity across events were more likely to report experiencing blackout Controlling for individual differences in typical drinking, those who played drinking games more frequently were more likely to experience a blackout When women, compared to men, consumed 1 more drink than their usual amount, odds of experiencing a blackout increased by 13% | ||
| Field study | 1,222 nightclub patrons in Sao Paulo, Brazil, Ages: 51% ≤ 24, 57% male | Blackouts were more prevalent in those who engaged in binge drinking while at the nightclub | ||
| Prospective | 1,402 drinking adolescents, Ages: 15–19 (M=15.5), 60% female | In the 2 years prior to age 15, almost 30% of youth reported experiencing an alcohol-induced blackout At age 19, 74% of youth reported experiencing an alcohol-induced blackout Four latent trajectory classes were identified: Class 2 was used as a reference and predictors included female sex, higher drinking, smoking, externalizing characteristics, and estimated peer substance involvement | ||
| Multisite, cross-sectional | 757 9 and 10 grade students in Germany Ages: 15–16 (M=15.6) 50% female | Predrinking is associated with experiencing alcohol-induced blackouts | ||
| Prospective | 829 college students Mean age of 21.8 years 66% female | Alcohol dependence symptoms in Year 4 predicted increased frequency of blackouts and social/emotional consequences during the following year Blackouts during Year 4 predicted increased alcohol-related social and emotional consequences, but not alcohol dependence symptoms in Year 5 | ||
| Cross-sectional | 42,347 subjects, 54% female | Blackouts were associated with suicidal ideation and suicidal attempts in males, and suicidal ideation in females | ||
| Multisite, prospective | 954 undergraduate and graduate students, Ages: 18–41, 44% between the ages 18–20, 51% female | At baseline, 52% of males and 50% of females had experienced an alcohol-induced blackout in the past year One in eight emergency department visits over a two-year period were associated with blackouts Estimates indicated that blackout-associated emergency department visit costs ranged from $469,000–$546,000/year | ||
| Multisite, prospective | 954 undergraduate and graduate students, Ages: 18–41, 44% ages 18–20, 51% female | Approximately 7% of the sample reported experiencing 6 or more blackouts in the past year Alcohol-induced blackouts at baseline exhibited a dose-response on odds of alcohol-related injury during follow-up increasing from 1.57 among those who reported 1–2 blackouts to 2.64 for those reporting six or more blackouts | ||
| Multisite, cross-sectional | 188 AUD patients in residential alcohol treatment, Ages: 14–64, median=35, 89% male | History of alcohol-induced blackouts was predictive of comorbid MD diagnosis | ||
| Prospective | 997 incoming first year college students, Ages: 18–24 (M=18.1), 65% female | Blackout experience during the first year predicted later increases in drinking among males Blackout experience during the first year predicted decreased drinking the following year among females | ||
| Prospective | 23 heavy episodic drinking youth and 23 demographically-matched non-drinking youth, Ages: 16–18 (M=17.7), 50% female | Heavy episodic drinking youth responded with greater emotional response to the PASAT-C, but emotional responses decreased with sustained abstinence Among heavy episodic drinking youth, greater lifetime and recent alcohol consumption, alcohol-induced blackouts, and withdrawal symptoms were associated with increased negative affect with PASAT-C exposure | ||
| Cross-sectional | 64 patients with bipolar disorder and 49 controls, Ages: 18–30 (M=23), 66% female | H-MRS | In both patients and controls, reduced hippocampal-GSH was associated with blackout presence/severity | |
| Cross-sectional | 48 young adults were included in analyses (21 binge drinkers and 27 light drinkers) Ages: 18–24 ~50% female | H-MRS | Overall, binge drinkers had lower gamma amino-butyric acid and N-acetyl-aspartate in the anterior cingulate cortex than light drinkers When stratified by blackout history, binge drinkers with a history of blackouts had lower anterior cingulate cortex glutamate than light drinkers | |
| Multicohort, prospective | 60 substance-naïve youth who later transition into heavy drinking and experienced a blackout ( =20) or not ( =20) or youth who remain abstinent ( =20) Ages: 12–14 at baseline 55% male | Prior to initiating substance use, youth who later transitioned into heavy drinking and experienced blackouts showed greater activation during inhibitory processing than nondrinkers and youth who transitioned into heavy drinking but did not experience blackouts Mean activation during correct inhibitory processing in the left and right middle frontal brain regions at baseline predicted future blackout experience, after controlling for follow-up externalizing behaviors and lifetime alcohol consumption | ||
| Cross-sectional | 88 college students who consume alcohol (44 with a history of fragmentary blackouts; 44 without a history of blackouts) Ages: 21–22 (M=21.6) 50% female | Individuals with and without a history of blackouts showed similar memory performance when sober Individuals who consumed alcohol and had a positive history of fragmentary blackouts showed greater contextual memory impairments than those who had not previously experienced a blackout | ||
| Cross-sectional | 24 college students who consume alcohol (12 with a history of fragmentary blackouts and 12 without a history of fragmentary blackouts) Ages: 21–23 (M=21.3) 50% female | Groups did not show significant differences when sober Individuals with a history of fragmentary blackouts showed attenuated neural responses to contextual memory recollection in the right posterior parietal cortex and bilateral dorsolateral PFC | ||
AEQ-A, Alcohol Expectancy Questionnaire – Adolescent; BPRS, APS, Alcohol Problems Scale; AREAS, Academic Role Expectations and Alcohol Scale; AUD, alcohol use disorder; AUDIT, Alcohol Use Disorders Identification Test; BDI-II, Beck Depression Inventory-II; BIS-11, Barratt Impulsiveness Scale; BPRS, Brief Psychiatric Rating Scale; BrAC, breathe alcohol concentration; BSSS, Brief Sensation-Seeking Scale; CBCL, Child Behavior Checklist; CDDR, Customary Drinking and Drug Use Record; CIDI, Composite International Diagnostic Interview; DASS, Depression Anxiety Stress Scale; DDQ, Daily Drinking Questionnaire; ESYTC, Edinburgh Study of Youth Transitions and Crime; FHAM, Family History Assessment Module; FTQ, Family Tree Questionnaire; GNG, go-nogo; GSH, glutathione; HDRS, Hamilton Depression Rating Scale; 1 H-MRS, Proton magnetic resonance imaging spectroscopy; HSS, Health Screening Survey; IPAS, Important People and Activities Scale; IPIP-NEO, International Personality Inventory Pool form of the NEO 5-factor Personality Inventory; MD, major depression, MEPS, Medical Expenditure Panel Survey; MRI, magnetic resonance imaging; PANAS, Positive and Negative Affect Scale; PASAT-C, Paced Auditory Serial Addition Test-Computerized Version; PDS, Pubertal Development Scale; POMS, Profile of Mood States; RAPI, Rutgers Alcohol Problem Index; SCID, Structured Clinical Interview for DSM Disorders; SDQ, Strengths and Difficulties Questionnaire; SEM, Structural equation modeling; SRE, Self-ratings of the effects of alcohol; SSAGA-I, Semi-Structured Assessment for the Genetics of Alcoholism-I; STAI, State-Trait Anxiety Inventory; TLFB, Timeline Followback; TMT, Trail Making Test, WAIS-III, Wechsler Adult Intelligence Scale – 3 rd edition; WASI, Wechsler Abbreviated Scale of Intelligence; WHO-ASSIST, World Health Organization’s Alcohol, Smoking and Substance Involvement Screening Test; WMS-III, Wechsler Memory Scale – 3 rd edition; WRAT, Wide Range Achievement Test; YAACQ, Young Adult Alcohol Consequences Questionnaire; YAAPST, Youth Adult Alcohol Problems Screening Test; YMRS, Young Mania Rating Scale; YSR/ASR, Youth Self-Report/Adult Self-Report.
Prevalence and Predictors of Alcohol-Induced Blackouts
The majority of the publications identified for this review examined binge drinking and alcohol-related consequences, including blackouts, among young adults and college students and reported prevalence rates ranging from approximately 20–55% ( Barnett et al., 2014 ; Boekeloo et al., 2011 ; Brister et al., 2011 ; Chartier et al., 2011 ; Clinkinbeard and Johnson, 2013 ; Hallett et al., 2013 ; Sanchez et al., 2015 ; Wilhite and Fromme, 2015 ). Although prevalence rates were typically around 50%, one study reported a prevalence rate of only about 20%; however, this was a qualitative study examining how university students define binge drinking ( Clinkinbeard and Johnson, 2013 ). As such, participants were not directly asked whether they had experienced an alcohol-induced blackout, but rather participants were asked to describe binge drinking and then researchers categorized whether the responses described alcohol-induced blackouts. In addition to their prevalence rate of 54%, Barnett and colleagues (2014) found that college students reported experiencing an alcohol-induced blackout nearly once every five drinking weeks during the first year of college. Thus, alcohol-induced blackouts are not only common among those who consume alcohol, but also recur over time.
Using longitudinal methods, Schuckit and colleagues (2015) and Wilhite and Fromme (2015) focused specifically on prospective analyses of alcohol-induced blackouts. Schuckit and colleagues (2015) used latent class growth analysis to evaluate the pattern of occurrence of alcohol-induced blackouts across 4 time points in 1,402 drinking adolescents between the ages of 15–19. Surprisingly, 30% of the adolescents reported experiencing an alcohol-induced blackout at the age of 15, which increased to 74% at age 19. Analyses revealed 4 classes in the patterns of the occurrence for blackouts (i.e., no blackouts, blackouts rapidly increasing with age, blackouts slowly increasing, and blackouts consistently reported), with female sex, higher drinking quantities, smoking, externalizing characteristics, and estimated peer substance use predicting class membership ( Schuckit et al., 2015 ). In general, these findings are consistent with previous research ( Rose and Grant, 2010 ; White et al., 2002 ) and indicate that alcohol-induced blackouts are common even among early adolescents, which is particularly concerning given that the adolescent brain is undergoing significant developmental changes.
Wilhite and Fromme (2015) examined the associations between alcohol-induced blackouts, alcohol dependence symptoms ((as measured by the Rutgers Alcohol Problem Index ( White and Labouvie, 1989 )), and social and emotional negative consequences across 2 years among 829 young adults who were transitioning out of college. They found that alcohol dependence symptoms predicted an increased frequency of blackouts and consequences the following year. Alcohol-induced blackouts during the past three months prospectively predicted increased social and emotional negative consequences, but not alcohol dependence symptoms the following year. These findings contradict Jellinek’s theory of alcoholism, which posits that alcohol-induced blackouts are a precursor of alcoholism ( Jellinek, 1952 ).
Potential genetic influences
Behavioral genetic research suggests that there is a heritable component to experiencing alcohol-induced blackouts ( Luczak et al., 2006 ; Nelson et al., 2004 ; Slutske et al., 1999 ). Two recent studies explored genetic influences by examining the potential effects of family history of alcohol problems on blackout occurrence ( LaBrie et al., 2011 ; Marino and Fromme, 2015 ). In a study of 2,546 college students, LaBrie and colleagues (2011) found that a family history of alcohol problems increased the likelihood of blacking out. Using data from a longitudinal study of college students, Marino and Fromme (2015) explored whether maternal or paternal family history of problematic alcohol use were better predictors than a general measure of overall family history on the likelihood of experiencing an alcohol-induced blackout. They further tested whether gender moderated the association in a sample of 1,164 college students. Although prenatal alcohol exposure was not assessed and could influence findings, the researchers found that compared to women with a maternal history of problematic alcohol use, men with a maternal history of problematic alcohol use were more than twice as likely to report experiencing an alcohol-induced blackout.
Based on the Marino and Fromme (2015) findings, one could speculate that a genetic vulnerability to alcohol-induced blackouts is expressed only under certain environmental conditions, representing a possible gene by environment interaction. For example, a mother with problematic drinking habits might contribute to an environment that is characterized by lower parental monitoring and increased alcohol availability. These environmental factors, in turn, could create stress and contribute to early initiation of alcohol use and maladaptive drinking behaviors in her offspring, especially sons, who are genetically predisposed to alcohol misuse and alcohol-induced blackouts. Given the potential impact of these findings on prevention and intervention programs, additional research examining genetic and environmental factors contributing to alcohol-induced blackouts is needed.
Prepartying and drinking games
Three studies examined high-risk drinking behaviors common among young adults known as “prepartying,” “pregaming,” and “drinking games” ( LaBrie et al., 2011 ; Ray et al., 2014 ; Wahl et al., 2013 ). Typically, these drinking behaviors involve fast-paced drinking over a short period of time and can cause a rapid rise and high peak BAC, which increases the likelihood of experiencing an alcohol-induced blackout ( Goodwin, 1995 ; Perry et al., 2006 ). LaBrie and colleagues (2011) examined risk factors for blackouts among 2,546 college students who reported past month prepartying. Of these students, 25% reported blacking out during at least one occasion over the past month when prepartying had occurred. Similarly, Wahl and colleagues (2013) examined predrinking and associated behaviors among 757 German high school students and found that those who reported engaging in predrinking were more likely to experience alcohol-induced blackouts. Using an event-level approach, Ray and colleagues (2014) found that students consumed more alcohol during drinking game events compared to non-drinking game events, and all students were more likely to experience an alcohol-induced blackout during events when drinking games occurred. This provides additional support for the importance of drinking style (e.g., pace and type of alcohol), as well as amount of alcohol consumed, in the occurrence of alcohol-induced blackouts.
Drinking motives
Because drinking motives are predictors of alcohol use and consequences, recent research has also examined the association between drinking motives and alcohol-induced blackouts ( Boekeloo et al., 2011 ; Merrill and Read, 2010 ; Merrill et al., 2014 ). Merrill and Read (2010) examined whether affect-relevant motivations for alcohol use (i.e., coping: drinking to alleviate negative affect; enhancement: drinking to increase positive affect) were associated with specific types of consequences, including alcohol-induced blackouts, in 192 regularly drinking college students. Using structural equation modeling (SEM), the authors reported a direct path between enhancement motives and blackouts, suggesting that individuals who drink to increase positive affect might consume alcohol in a manner that results in a rapid increase in BAC and alcohol-induced blackouts, such as taking shots of liquor or drinking rapidly. Merrill and colleagues (2014) conducted a follow-up, longitudinal study examining whether coping and enhancement motives predicted alcohol consequences, including alcohol-induced blackouts, over the course of one year in 552 college students and reported that enhancement motives indirectly predicted blackouts the following year. Although enhancement motives did not directly predict alcohol-induced blackouts in the longitudinal study, drinking to increase positive affect seems to involve a style of drinking that increases the likelihood of blackouts.
Boekeloo and colleauges (2011) examined a different type of drinking motive -“drinking to get drunk,” which the authors defined as “pre-meditated, controlled, and intentional consumption of alcohol to reach a state of inebriation” (p. 89). They explored the prevalence and correlates of this type of drinking behavior in 307 incoming freshman who reported consuming alcohol over the past 30 days. Nearly 77% of the incoming freshmen reported drinking alcohol in a pre-meditated, intentional manner with the goal of becoming intoxicated. Compared to those who did not drink to get drunk, individuals who reported drinking to get drunk were more likely to experience an alcohol-induced blackout. Further, consistent with the prepartying and drinking games studies described previously ( LaBrie et al., 2011 ; Ray et al., 2014 ; Wahl et al., 2013 ), individuals who reported drinking to get drunk were also more likely to have prepartied and participated in drinking games.
Consequences of Alcohol-Induced Blackouts
As indicated by the research described above, alcohol-induced blackouts typically occur following a rapid rise and high peak level of alcohol intoxication, and as such, alcohol-induced blackouts are associated with and predictive of other consequences and behaviors. Using SEM, Read and colleagues (2013) examined whether alcohol-related consequences, including alcohol-induced blackouts, predicted college students’ alcohol consumption one year later and whether these associations differed between men and women. Findings revealed that alcohol-induced blackouts during the first year of college predicted alcohol use the following year, with blackouts predicting later drinking increases in men and decreases in women ( Read et al., 2013 ). Further, using data from a randomized controlled trial of screening and brief physician intervention for problem alcohol use among 954 undergraduate and graduate students, Mundt and colleagues (2012) examined whether baseline alcohol-induced blackouts prospectively identified individuals with alcohol-related injury over the subsequent 2 years after controlling for heavy drinking days ( Mundt and Zakletskaia, 2012 ; Mundt et al., 2012 ). Findings indicated that alcohol-induced blackouts at baseline predicted alcohol-related injury over time with individuals who reported experiencing 1–2 blackouts at baseline being 1.5 times more likely to experience an alcohol-related injury, and those who reported 6 or more blackouts being over 2.5 times more likely to experience an alcohol-related injury. Mundt and Zakletskaia (2012) conducted a follow-up analysis on the same sample and found that one in eight emergency department visits for alcohol-related injuries involved an alcohol-induced blackout. Thus, among young adults, experiencing a blackout increases the likelihood of having an alcohol-related injury over time, even after controlling for heavy drinking.
Recent research has also investigated the associations between alcohol-induced blackouts and psychiatric symptomatology ( Bae et al., 2015 ; Neupane and Bramness, 2013 ; Winward et al., 2014 ). Using data provided by the Korea National Health and Nutritional Examination Survey from 2007–2011, Bae and colleagues (2015) examined associations between alcohol consumption and suicidal behavior in 42,347 Korean subjects and reported that alcohol-induced blackouts were associated with suicidal ideation and suicide attempts in males and suicidal ideation in females. Further, in a sample of 188 Nepalese patients in treatment for alcohol use disorder, a history of alcohol-induced blackouts was predictive of having comorbid major depression ( Neupane and Bramness, 2013 ).
Winward and colleagues (2014) used the Paced Auditory Serial Attention Test (PASAT-C) Computer Version to examine affective reactivity, cognitive performance, and distress tolerance in relation to blackouts, during early abstinence among 23 heavy episodic drinking adolescents (ages 16–18) compared to 23 matched, non-drinking controls. Findings revealed that heavy episodic drinking adolescents responded with greater emotional response to the PASAT-C compared to controls, and among heavy episodic drinking adolescents, greater frequency of alcohol-induced blackouts during the past three months was correlated with greater increases in frustration and irritability during the PASAT-C. Overall, these findings suggest that alcohol-induced blackouts can have profound effects on an individual’s overall health and well-being, above and beyond the effects of heavy alcohol consumption.
Potential Neurobiological Mechanisms of Alcohol-Induced Blackouts
Although early theories posited that alcohol’s effects on cognition and behavior were due to alcohol’s general disruption of brain function and depression of the central nervous system, preclinical and clinical research now indicates that alcohol-induced cognitive and memory deficits are caused by alcohol’s effects on the hippocampus and related neural structures ( Figure 2 ) ( White et al., 2000 ). Briefly, the hippocampus is a brain structure involved in memory formation for events and has been found to be particularly sensitive to alcohol. Indeed, animal research published prior to the period of the current review revealed that blackouts are caused by alcohol disrupting the transfer of information from short-term to long-term memory by interfering with hippocampal, medial septal, and frontal lobe functioning ( White, 2003 ; White et al., 2000 ). Although the mechanism of alcohol-induced blackouts is now known, our understanding of the specific neurobiological vulnerability and why some individuals are more likely to experience alcohol-induced blackouts while others are not has been an area of growing interest.

General overview of alcohol’s effects on memory and alcohol-induced blackouts. Top panel: Sagittal representation of the human brain and the primary structures and associations involved in episodic memory. Bottom panel: A general model of memory formation, storage, and retrieval reproduced with permission from the National Institute on Alcohol Abuse and Alcoholism publication ( White, 2003 ). Alcohol interferes with all stages of the memory process, but the alcohol’s primary effect appears to be on the transfer of information from short-term to long-term storage. Intoxicated individuals are typically able to recall information immediately after it is presented and can keep the information active in short-term memory for one minute or more if they are not distracted. Individuals may also be able to recall long-term memories formed before they became intoxicated; however, after just one or two drinks, individuals show memory impairments. Alcohol can interfere with these memory processes so severely that once sober, the individual is not able to recall all or portions of the events that occurred during the drinking episode.
Contextual memory (often described more broadly as source memory) refers to memory for details associated with a specific event (e.g., where a person was for the event, who was at the event). These memory details facilitate recall by enabling a person to consciously re-experience past events ( Tulving, 2002 ). As such, Wetherill and Fromme (2011) examined the effects of acute alcohol consumption on contextual memory and recall among individuals with and without a history of fragmentary blackouts in an attempt to better understand why some individuals experience alcohol-induced memory impairments whereas other do not, even when these individuals have similar drinking histories and are at comparable BrACs ( Wetherill and Fromme, 2011 ). Using longitudinal data to identify 88 young adults (mean age: 21.6 years ± 0.5; alcohol consumed 3 times a week, 3 standard drinks per occasion over the past 3 months) with ( n= 44) and without ( n= 44) a history of alcohol-induced blackouts who reported comparable drinking histories, denied other illicit drug use, and were demographically matched, Wetherill and Fromme conducted an alcohol administration (target BrAC of .08 g/dl versus no alcohol) with memory assessments and found that while sober, individuals with and without a history of alcohol-induced blackouts did not differ in memory performance; however, after alcohol consumption, individuals with a history of blackouts exhibited contextual memory impairments, while those without a history of blackouts did not.
Wetherill and colleagues (2012) conducted a follow-up study that used a within subject alcohol challenge followed by two functional magnetic resonance imaging (fMRI) sessions under no alcohol and alcohol (target BrAC of .08 g/dl) conditions. During fMRI scanning, participants completed a contextual memory task. Findings again revealed that individuals with and without a history of fragmentary blackouts did not differ in contextual memory performance or neural activity while sober, yet after alcohol consumption, individuals with a history of fragmentary blackouts showed less neural activation during encoding and recollection of contextual details in prefrontal and parietal regions, suggesting that alcohol had differential effects on frontoparietal brain activity ( Wetherill et al., 2012 ).
Subsequently, Wetherill and colleagues (2013) explored whether frontoparietal abnormalities exist among substance-naïve youth who later transition into heavy drinking and experience alcohol-induced blackouts. Specifically, 60 substance-naïve youth completed fMRI scanning during a go/no-go response inhibition task shown to engage frontal and posterior parietal brain regions ( Tapert et al., 2007 ) at baseline and were followed annually. After approximately five years, youth had either remained substance-naïve ( n =20) or had transitioned into heavy drinking and were classified as either alcohol-induced blackout positive ( n =20) or alcohol-induced blackout negative ( n =20). Groups were demographically matched and youth who experienced alcohol-induced blackouts were matched on follow-up substance use. Although groups did not differ in inhibitory processing performance, prior to initiating substance use, youth who later transitioned into heavy drinking and experienced an alcohol-induced blackout showed greater neural activation during inhibitory processing in frontal and cerebellar regions compared to controls and those who did not experience alcohol-induced blackouts. Further, activation during correct inhibitory processing compared to go responses in the left and right middle frontal gyri at baseline predicted future blackout experience, after controlling for alcohol consumption and externalizing behaviors ( Wetherill et al., 2013 ). Findings from this study suggest that some individuals have inherent vulnerabilities to inhibitory processing difficulties that likely contribute to alcohol-induced memory impairments. Overall, these neuroimaging findings provide strong evidence for neurobiological vulnerabilities to alcohol-induced memory impairments and alcohol-induced blackouts that exist prior to the onset of alcohol use but become more evident after alcohol consumption.
Silveri and colleagues (2014) and Chitty and colleagues (2014) used magnetic resonance spectroscopy (MRS) to examine potential neurochemical differences among individuals who experience blackouts and those who do not. Using MRS in a sample of 23 young adults who were binge drinkers and 31 young adult light drinkers, researchers found in vivo evidence of lower frontal lobe (i.e. anterior cingulate cortex, ACC) gamma amino-butyric acid (GABA) and N-acetyl-apartate (NAA) in binge drinkers than light drinkers, with post hoc analyses revealing that these lower neurochemical profiles were driven by binge drinkers who reported a history of alcohol-induced blackouts ( Silveri et al., 2014 ). Further, in a sample of 113 18–30 year olds (64 individuals with bipolar disorder and 49 healthy comparison controls), reduced hippocampal glutathione, the brain’s most potent antioxidant, concentration was associated with blackout occurrence and severity ( Chitty et al., 2014 ). Chitty and colleagues (2014) interpreted these findings as support for the role of the hippocampus in alcohol-induced memory impairments. Together, these MRS findings indicate that binge drinking and riskier alcohol use affect the neurochemistry of some individuals more than others, which may contribute to the recurrence of and vulnerability to alcohol-induced memory impairments.
Practical and Clinical Implications of Alcohol-induced Blackouts
From a review of 26 empirical studies, Pressman and Caudill (2013) concluded that only short-term memory is impaired during a blackout and that other cognitive functions, such as planning, attention, and social skills, were not affected. Because cognitive functions other than memory are not necessarily impaired during a blackout ( Pressman and Caudill, 2013 ), a critical question is whether or not people are responsible for their behavior while in a blackout. This is often a key factor in alcohol-related crimes, when the perpetrator or victim claim to have no memory for their actions ( van Oorsouw et al., 2004 ). For example, Pressman and Caudill (2013) reference a quadruple murder in which the defendant claimed he had no memory of committing the murders because he was in an alcohol-induced blackout at the time. Applying Daubert legal standards to this case (( Daubert v. Merrell Dow Pharmaceuticals , 509 U.S. 579 (1993)), the authors concluded that the accused’s blackout could not be used as a viable defense. Equally important, however, may be the memory of a potential victim of a crime. For example, alleged victims of sexual assault may claim they have no memory for events that led up to the sexual activities (( United States v. Pease , Navy-Marine Corps Court of Criminal Appeals 201400165, (2015)). Whereas there is legal precedent to prevent voluntary intoxication and blackouts from being viable defenses against committing a crime ( Cunnien, 1986 ; Marlowe et al., 1999 ), a remaining question is the extent to which alleged victims in a blackout should be held accountable for their actions, despite their lack of memories. Unquestionably, when a victim is incapacitated from alcohol and unable to provide consent, there are grounds for a conviction of sexual assault. However, as reviewed above, blackouts can occur at BrACs well below the level of incapacitation. If people maintain their ability to make conscious decisions and execute voluntary behaviors while in a blackout, questions remain about whether or not they are responsible for their actions.
It is important to remember that when examining the impact of blackouts, the accused, victim, patient, or research subject is typically being asked to remember not remembering. This is a critical challenge to understanding and studying blackouts, and also raises questions about the accuracy of memories that are reported following a blackout. In an effort to fill in gaps in their memory because of alcohol-induced blackouts, people use a variety of strategies to reconstruct their experiences ( Nash and Takarangi, 2011 ). The most common reconstruction strategy is to ask friends who were present, and who may or may not have also been intoxicated. Consequently, in their quest to learn about their actions while in a blackout, people may be given misinformation from their friends, leading to inaccurate reconstructions of the events. People may also look for photos/videos or other types of physical evidence to help fill gaps in their memories due to blackouts. Regardless of how many different approaches a person takes in order to help reconstruct their memory of what occurred during a blackout, there is rarely a way to validate the memories as accurate because the process of memory reconstruction is inherently fallible.
The fallibility of memory, even in the absence of alcohol or blackouts, has been documented through decades of rigorous experimental and field research. Leading this research, Elizabeth Loftus has authored over 200 books and thousands of peer-reviewed articles which demonstrate the many ways in which memory for events can be distorted or contaminated during the process of recall ( Loftus and Davis, 2006 ; Morgan et al., 2013 ; Patihis et al., 2013 ). Provision of misinformation, the passage of time, and being asked or interviewed about prior events can all lead to memory distortions as the individual strives to reconstruct prior events ( Loftus and Davis, 2006 ; Nash and Takarangi, 2011 ). Consequently, the reliability or accuracy of memories that are recalled following a period of alcohol-induced amnesia are likely to be suspect.
There are also important clinical implications of blackouts, as alcohol-induced blackouts have been associated with psychiatric symptomatology ( Bae et al., 2015 ; Neupane and Bramness, 2013 ; Winward et al., 2014 ), as well as feeling embarrassed or distressed when learning about their behavior during a blackout ( White et al., 2004 ). Efforts to reconcile their intoxicated behavior with their personal values may further contribute to significant emotional angst ( Wilhite and Fromme, 2015 ). As such, educating people about the nature and consequences of alcohol-induced blackouts is needed. Although heavy episodic drinking, a common correlate of alcohol-induced blackouts, is often a focus of alcohol prevention programs, rarely are blackouts considered as a target for intervention. For example, a recent study on the effects of a motivational invention on alcohol consumption and blackouts found that the intervention decreased both alcohol consumption and the number of blackouts experienced ( Kazemi et al., 2013 ). Thus, educating people about the factors that contribute to (e.g., predrinking/prepartying; family history of alcohol problems) and consequences of blackouts may help reduce the likelihood of experiencing blackouts and related negative emotional consequences ( Wilhite and Fromme, 2015 ).
Challenges and Future Research
There are several challenges that hinder research on blackouts. First, alcohol-induced blackouts are amnestic periods, and as such, researchers are relying on self-report of alcohol consumption for a period of time that the individual cannot recall. Further, individuals who experienced a blackout often rely on other individuals to help reconstruct the events that occurred during the blackout, but the information from these other individuals is likely unreliable because they may also be consuming alcohol ( Nash and Takarangi, 2011 ). As such, future research should use alternative methodologies to better understand the phenomenology of alcohol-induced blackouts. For example, information might be obtained from a research observer, posing as a confederate, who is not drinking but is present at the drinking event. Also, because short-term memory remains intact, use of ecological momentary assessment with smart phones might also be useful for gathering information about the drinker’s experiences while he or she is in a blackout state. Subsequent interviews could then determine what aspects of those events were remembered and whether they were remembered in the same way that they were reported during the drinking event.
Another complicating factor for research on blackouts is the potential use of other drugs (illicit or prescription) that might also contribute to memory loss. Although several research studies statistically control for or exclude individuals who report co-occurring illicit drug use, research clearly indicates that some individuals who report blackouts also report other drug use ( Baldwin et al., 2011 ; Haas et al., 2015 ). Thus, researchers must be cautious and account for factors other than alcohol that might contribute to blackouts.
Perhaps the greatest impediment to rigorous tests of alcohol-induced blackouts and behavior is that researchers are not ethically permitted to provide alcohol in sufficient doses to cause a blackout to occur. BrACs of 20 g/dl and above are typically required to induce a blackout, thereby limiting the ability to safely dose research participants to the point of blackout. As such, researchers may consider conducting field studies in order to better characterize and understand alcohol-induced blackouts, as it is quite likely that the events and consequences that occur during a blackout are underestimated given the limits of laboratory research and self-report of events. Finally, given the growing literature on alcohol-induced memory impairments and blackouts, a standardized assessment for alcohol-induced blackouts is sorely needed. Most of the existing research on alcohol-induced blackouts either uses a single item from the Rutgers Alcohol Problem Index or the investigator’s own description/definition of an alcohol-induced blackout. Moreover the frequency of occurrence for blackouts is currently measured in widely different ways, including dichotomous measures (e.g., Yes/No blackouts) and proportion of times drinking that blackouts were experienced (e.g., always, sometimes, never). In an effort to better characterize blackouts, researchers should collect detailed information about past and current alcohol consumption patterns, as well as other illicit drug use. It will be important for future studies to conduct a thorough assessment of the alcohol consumption that occurred during the drinking event in which the blackout occurred (i.e., duration of drinking, type of alcohol consumed, pace of consumption), as well as gender and weight, in order to calculate more accurate estimations of BACs. Optimally, actual BrACs or blood draws could be collected to back-extrapolate peak BACs to the time of blackout. This information will enable researchers to statistically control for the direct effects of alcohol consumption and examine factors that influence alcohol-induced blackouts over and beyond the amount of alcohol consumed.
Despite the increase in research on and our understanding of alcohol-induced blackouts, additional rigorous research is still needed. Studies examining potential genetic and environmental influences, as well as their interactions, are clearly warranted given recent research findings of Marino and Fromme (2015) . Sex differences in alcohol-induced blackouts are another area in need of study. Although previous research indicates that women are more vulnerable to alcohol-induced blackouts due to the effect of sex differences in pharmacokinetics and body composition on alcohol bioavailability ( Rose and Grant, 2010 ), the influence of biological sex on alcohol-induced blackouts are inconsistent. Specifically, several studies either did not assess sex differences ( Clinkinbeard and Johnson, 2013 ; Sanchez et al., 2015 ; Wetherill and Fromme, 2011 ; Wetherill et al., 2013 ), reported no sex differences ( Barnett et al., 2014 ; Boekeloo et al., 2011 ; Brister et al., 2011 , Wilhite and Fromme, 2015 ), reported that males reported higher rates of alcohol-induced blackouts ( Chartier et al., 2011 ) or reported that being a female contributed to the likelihood of experiencing an alcohol-induced blackout ( Hallett et al., 2013 ; Schuckit et al., 2015 ). These inconsistent findings could be due in part to methodological differences across research studies and assessment of alcohol-induced blackouts, and future studies should address this issue. Additional areas for future study include interventions targeting alcohol-induced blackouts, whether the risk for alcohol-induced blackouts increases as individuals age and become more susceptible to memory deficits, and whether there is a “window of vulnerability” such that experiencing an alcohol-induced blackout increases the risk of experiencing another alcohol-induced blackout within a short time frame (akin to second impact syndrome for concussions).
The literature on alcohol-induced blackouts continues to grow, and the recent research reviewed here suggests that there are individual factors that contribute to the occurrence of alcohol-induced memory impairments beyond the amount of alcohol consumed and that alcohol-induced blackouts have consequences beyond memory loss for a drinking episode. Although our understanding of alcohol-induced blackouts has improved dramatically, additional research is clearly necessary. By fine-tuning our approach to studying blackouts, we will improve our understanding of alcohol-induced blackouts, and consequently, be better situated to improve prevention strategies.
Acknowledgments
This material is based upon work supported by the National Institutes of Health/National Institute on Alcohol Abuse and Alcoholism under grants K23 AA023894 awarded to Reagan Wetherill and R01 AA020637 awarded to Kim Fromme.
This work was supported by National Institutes of Health grants K23AA023894 (PI: Wetherill) and R01AA020637 (PI: Fromme) from the National Institute on Alcohol Abuse and Alcoholism. The authors would like to thank Diantha LaVine for her assistance with the artwork.
Conflicts of Interest
The authors have not been involved in financial relationships that pose a conflict of interest for this work. The authors are in agreement regarding the content of this manuscript.
- Bae HC, Hong S, Jang SI, Lee KS, Park EC. Patterns of Alcohol Consumption and Suicidal Behavior: Findings From the Fourth and Fifth Korea National Health and Nutritional Examination Survey (2007–2011) J Prev Med Public Health. 2015; 48 :142–150. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Baldwin K, Barrowman NJ, Farion KJ, Shaw A. Attitudes and practice of Children’s Hospital of Eastern Ontario (Ottawa, Ontario) paediatricians and residents toward literacy promotion in Canada. Paediatr Child Health. 2011; 16 :e38–42. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Barnett NP, Clerkin EM, Wood M, Monti PM, O’Leary Tevyaw T, Corriveau D, Fingeret A, Kahler CW. Description and predictors of positive and negative alcohol-related consequences in the first year of college. J Stud Alcohol Drugs. 2014; 75 :103–114. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Boekeloo BO, Novik MG, Bush E. Drinking to Get Drunk among Incoming Freshmen College Students. Am J Health Educ. 2011; 42 :88–95. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brister HA, Sher KJ, Fromme K. 21st birthday drinking and associated physical consequences and behavioral risks. Psychol Addict Behav. 2011; 25 :573–582. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chartier KG, Hesselbrock MN, Hesselbrock VM. Alcohol problems in young adults transitioning from adolescence to adulthood: The association with race and gender. Addict Behav. 2011; 36 :167–174. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chitty KM, Lagopoulos J, Hickie IB, Hermens DF. The impact of alcohol and tobacco use on in vivo glutathione in youth with bipolar disorder: an exploratory study. J Psychiatr Res. 2014; 55 :59–67. [ PubMed ] [ Google Scholar ]
- Clinkinbeard SS, Johnson MA. Perceptions and practices of student binge drinking: an observational study of residential college students. J Drug Educ. 2013; 43 :301–319. [ PubMed ] [ Google Scholar ]
- Cunnien AJ. Alcoholic blackouts: phenomenology and legal relevance. Behav Sci Law. 1986; 4 :364–370. [ Google Scholar ]
- Goodwin DW. Alcohol amnesia. Addiction. 1995; 90 :315–317. [ PubMed ] [ Google Scholar ]
- Goodwin DW, Crane JB, Guze SB. Alcoholic “blackouts”: a review and clinical study of 100 alcoholics. Am J Psychiatry. 1969a; 126 :191–198. [ PubMed ] [ Google Scholar ]
- Goodwin DW, Crane JB, Guze SB. Phenomenological aspects of the alcoholic “blackout” Br J Psychiatry. 1969b; 115 :1033–1038. [ PubMed ] [ Google Scholar ]
- Haas AL, Wickham R, Macia K, Shields M, Macher R, Schulte T. Identifying Classes of Conjoint Alcohol and Marijuana Use in Entering Freshmen. Psychol Addict Behav 2015 [ PubMed ] [ Google Scholar ]
- Hallett J, Howat P, McManus A, Meng R, Maycock B, Kypri K. Academic and personal problems among Australian university students who drink at hazardous levels: web-based survey. Health Promot J Austr. 2013; 24 :170–177. [ PubMed ] [ Google Scholar ]
- Hartzler B, Fromme K. Fragmentary and en bloc blackouts: similarity and distinction among episodes of alcohol-induced memory loss. J Stud Alcohol. 2003; 64 :547–550. [ PubMed ] [ Google Scholar ]
- Heffernan TM. The impact of excessive alcohol use on prospective memory: a brief review. Curr Drug Abuse Rev. 2008; 1 :36–41. [ PubMed ] [ Google Scholar ]
- Hepola S. Blackout: Remembering the things I drank to forget. Grand Central Publishing; New York, NY: 2015. [ Google Scholar ]
- Jellinek EM. Phases in the drinking history of alcoholics: analysis of a survey conducted by the official organ of Alcoholics Anonymous. Quarterly Journal of Studies on Alcohol. 1946; 7 :1–88. [ PubMed ] [ Google Scholar ]
- Jellinek EM. Phases of alcohol addiction. Q J Stud Alcohol. 1952; 13 :673–684. [ PubMed ] [ Google Scholar ]
- Jennison KM, Johnson KA. Drinking-induced blackouts among young adults: results from a national longitudinal study. Int J Addict. 1994; 29 :23–51. [ PubMed ] [ Google Scholar ]
- Kazemi DM, Levine MJ, Dmochowski J, Nies MA, Sun L. Effects of motivational interviewing intervention on blackouts among college freshmen. J Nurs Scholarsh. 2013; 45 :221–229. [ PubMed ] [ Google Scholar ]
- LaBrie JW, Hummer J, Kenney S, Lac A, Pedersen E. Identifying factors that increase the likelihood for alcohol-induced blackouts in the prepartying context. Subst Use Misuse. 2011; 46 :992–1002. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lee H, Roh S, Kim DJ. Alcohol-induced blackout. Int J Environ Res Public Health. 2009; 6 :2783–2792. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Loftus EF, Davis D. Recovered memories. Annu Rev Clin Psychol. 2006; 2 :469–498. [ PubMed ] [ Google Scholar ]
- Luczak SE, Shea SH, Hsueh AC, Chang J, Carr LG, Wall TL. ALDH2*2 is associated with a decreased likelihood of alcohol-induced blackouts in Asian American college students. J Stud Alcohol. 2006; 67 :349–353. [ PubMed ] [ Google Scholar ]
- Marino EN, Fromme K. Alcohol-induced blackouts and maternal family history of problematic alcohol use. Addict Behav. 2015; 45 :201–206. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Marlowe DB, Lambert JB, Thompson RG. Voluntary intoxication and criminal responsibility. Behav Sci Law. 1999; 17 :195–217. [ PubMed ] [ Google Scholar ]
- Merrill JE, Read JP. Motivational pathways to unique types of alcohol consequences. Psychol Addict Behav. 2010; 24 :705–711. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Merrill JE, Wardell JD, Read JP. Drinking motives in the prospective prediction of unique alcohol-related consequences in college students. J Stud Alcohol Drugs. 2014; 75 :93–102. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Morgan CA, 3rd, Southwick S, Steffian G, Hazlett GA, Loftus EF. Misinformation can influence memory for recently experienced, highly stressful events. Int J Law Psychiatry. 2013; 36 :11–17. [ PubMed ] [ Google Scholar ]
- Mundt MP, Zakletskaia LI. Prevention for college students who suffer alcohol-induced blackouts could deter high-cost emergency department visits. Health Aff (Millwood) 2012; 31 :863–870. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mundt MP, Zakletskaia LI, Brown DD, Fleming MF. Alcohol-induced memory blackouts as an indicator of injury risk among college drinkers. Inj Prev. 2012; 18 :44–49. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nash RA, Takarangi MK. Reconstructing alcohol-induced memory blackouts. Memory. 2011; 19 :566–573. [ PubMed ] [ Google Scholar ]
- Nelson EC, Heath AC, Bucholz KK, Madden PA, Fu Q, Knopik V, Lynskey MT, Lynskey MT, Whitfield JB, Statham DJ, Martin NG. Genetic epidemiology of alcohol-induced blackouts. Arch Gen Psychiatry. 2004; 61 :257–263. [ PubMed ] [ Google Scholar ]
- Neupane SP, Bramness JG. Prevalence and correlates of major depression among Nepalese patients in treatment for alcohol-use disorders. Drug Alcohol Rev. 2013; 32 :170–177. [ PubMed ] [ Google Scholar ]
- Patihis L, Frenda SJ, LePort AK, Petersen N, Nichols RM, Stark CE, McGaugh JL, Loftus EF. False memories in highly superior autobiographical memory individuals. Proc Natl Acad Sci U S A. 2013; 110 :20947–20952. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Perry PJ, Argo TR, Barnett MJ, Liesveld JL, Liskow B, Hernan JM, Trnka MG, Brabson MA. The association of alcohol-induced blackouts and grayouts to blood alcohol concentrations. J Forensic Sci. 2006; 51 :896–899. [ PubMed ] [ Google Scholar ]
- Pressman MR, Caudill DS. Alcohol-induced blackout as a criminal defense or mitigating factor: an evidence-based review and admissibility as scientific evidence. J Forensic Sci. 2013; 58 :932–940. [ PubMed ] [ Google Scholar ]
- Ray AE, Stapleton JL, Turrisi R, Mun EY. Drinking game play among first-year college student drinkers: an event-specific analysis of the risk for alcohol use and problems. Am J Drug Alcohol Abuse. 2014; 40 :353–358. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Read JP, Wardell JD, Bachrach RL. Drinking consequence types in the first college semester differentially predict drinking the following year. Addict Behav. 2013; 38 :1464–1471. [ PubMed ] [ Google Scholar ]
- Rose ME, Grant JE. Alcohol-induced blackout. Phenomenology, biological basis, and gender differences. J Addict Med. 2010; 4 :61–73. [ PubMed ] [ Google Scholar ]
- Ryback RS. Alcohol amnesia. Observations in seven drinking inpatient alcoholics. Q J Stud Alcohol. 1970; 31 :616–632. [ PubMed ] [ Google Scholar ]
- Sanchez ZM, Ribeiro KJ, Wagner GA. Binge Drinking Associations with Patrons’ Risk Behaviors and Alcohol Effects after Leaving a Nightclub: Sex Differences in the “Balada com Ciencia” Portal Survey Study in Brazil. PLoS One. 2015; 10 :e0133646. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schuckit MA, Smith TL, Heron J, Hickman M, Macleod J, Munafo MR, Kendler KS, Dick DM, Davey-Smith G. Latent trajectory classes for alcohol-related blackouts from age 15 to 19 in ALSPAC. Alcohol Clin Exp Res. 2015; 39 :108–116. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Silveri MM, Cohen-Gilbert J, Crowley DJ, Rosso IM, Jensen JE, Sneider JT. Altered anterior cingulate neurochemistry in emerging adult binge drinkers with a history of alcohol-induced blackouts. Alcohol Clin Exp Res. 2014; 38 :969–979. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Slutske WS, True WR, Scherrer JF, Heath AC, Bucholz KK, Eisen SA, Goldberg J, Lyons MJ, Tsuang MT. The heritability of alcoholism symptoms: “indicators of genetic and environmental influence in alcohol-dependent individuals” revisited. Alcohol Clin Exp Res. 1999; 23 :759–769. [ PubMed ] [ Google Scholar ]
- Tapert SF, Schweinsburg AD, Drummond SP, Paulus MP, Brown SA, Yang TT, Frank LR. Functional MRI of inhibitory processing in abstinent adolescent marijuana users. Psychopharmacology (Berl) 2007; 194 :173–183. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tulving E. Episodic memory: from mind to brain. Annu Rev Psychol. 2002; 53 :1–25. [ PubMed ] [ Google Scholar ]
- van Oorsouw K, Merckelbach H, Ravelli D, Nijman H, Mekking-Pompen I. Alcoholic blackout for criminally relevant behavior. J Am Acad Psychiatry Law. 2004; 32 :364–370. [ PubMed ] [ Google Scholar ]
- Wahl S, Sonntag T, Roehrig J, Kriston L, Berner MM. Characteristics of predrinking and associated risks: a survey in a sample of German high school students. Int J Public Health. 2013; 58 :197–205. [ PubMed ] [ Google Scholar ]
- Wetherill RR, Castro N, Squeglia LM, Tapert SF. Atypical neural activity during inhibitory processing in substance-naive youth who later experience alcohol-induced blackouts. Drug Alcohol Depend. 2013; 128 :243–249. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wetherill RR, Fromme K. Acute alcohol effects on narrative recall and contextual memory: an examination of fragmentary blackouts. Addict Behav. 2011; 36 :886–889. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wetherill RR, Schnyer DM, Fromme K. Acute alcohol effects on contextual memory BOLD response: differences based on fragmentary blackout history. Alcohol Clin Exp Res. 2012; 36 :1108–1115. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- White A, Hingson R. The burden of alcohol use: excessive alcohol consumption and related consequences among college students. Alcohol Res. 2013; 35 :201–218. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. J Stud Alcohol. 1989; 50 :30–37. [ PubMed ] [ Google Scholar ]
- White AM. What happened? Alcohol, memory blackouts, and the brain. Alcohol Res Health. 2003; 27 :186–196. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- White AM, Jamieson-Drake DW, Swartzwelder HS. Prevalence and correlates of alcohol-induced blackouts among college students: results of an e-mail survey. J Am Coll Health. 2002; 51 :117–119. 122–131. [ PubMed ] [ Google Scholar ]
- White AM, Matthews DB, Best PJ. Ethanol, memory, and hippocampal function: a review of recent findings. Hippocampus. 2000; 10 :88–93. [ PubMed ] [ Google Scholar ]
- White AM, Signer ML, Kraus CL, Swartzwelder HS. Experiential aspects of alcohol-induced blackouts among college students. Am J Drug Alcohol Abuse. 2004; 30 :205–224. [ PubMed ] [ Google Scholar ]
- Wilhite ER, Fromme K. Alcohol-Induced Blackouts and Other Negative Outcomes During the Transition Out of College. J Stud Alcohol Drugs. 2015; 76 :516–524. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Winward JL, Bekman NM, Hanson KL, Lejuez CW, Brown SA. Changes in emotional reactivity and distress tolerance among heavy drinking adolescents during sustained abstinence. Alcohol Clin Exp Res. 2014; 38 :1761–1769. [ PMC free article ] [ PubMed ] [ Google Scholar ]

- Nutrition counsellor
- Food Allergy
- gastroenterology
- Heptologist In Delhi
- Liver transplant
- Alcoholic Liver Cirrhosis
Alcoholic liver cirrhosis is a late stage of fibrosis of the liver caused by many forms of liver diseases and conditions, such as chronic alcoholism. A person diagnosed with an alcoholic liver case may start from having fatty liver disease, then alcoholic hepatitis, and ultimately develop alcoholic cirrhosis. Hence, alcoholic liver cirrhosis stages in three levels. The diagnosed liver cirrhosis can be of two types :
- Compensated cirrhosis – when symptoms are not noticeable
- Uncompensated cirrhosis- when the symptoms can be noticed
The most common alcoholic liver causes are:
- Chronic alcohol consumption
- Chronic hepatitis
- Fatty liver disease
- Iron buildup in the body or hemochromatosis
- Copper accumulated in the liver (Wilson’s disease)
- Cystic fibrosis
- Biliary Atresia
- Inherited sugar metabolism or digestive disorders
- Infection like syphilis
Many other factors like the destruction of bile ducts(Primary Biliary Cirrhosis) or leaky gut also called, increased intestinal permeability are cofactors for the development of alcoholic liver cirrhosis.
Now, let us have a look at alcoholic liver cirrhosis symptoms:
- Food pipe problems
- Portal hypertension
- Swelling in legs (oedema) and abdomen (ascites)
- Bleeding in mouth
- Confusion, poor memory, loss of appetite
- Patchy red skin on palms (erythema)
Food pipe problem is also known as esophageal varices. Kidney failure and hypersplenism are other complications that happen due to this medical condition. If the symptoms are not taken seriously, then this deficient liver may arise a life-threatening situation. Hence, a person needs to keep a track of these indicators as if these signs are caught early and treated, it may slow down the progression of the disease.
How to treat alcoholic liver cirrhosis:
The first and foremost step in treatments is to help the patient to cease alcohol consumption. Medications like corticosteroids, calcium channel blockers, insulin can also be prescribed by the doctor as per the alcoholic liver care plan. Hepatologists may advise the patient to follow an alcoholic liver disease diet inclusive of fiber and protein. If the condition of the patient gets worsened, then the hepatologist may have to suggest a liver transplant surgery.
Dr. Nivedita Pandey is one of the best liver specialist doctors in Patna, Bihar. She is a well-renowned liver specialist doctor in Delhi, the best stomach doctor in Patna, the best gastroenterologist in Jammu, and a notable stomach doctor in Faridabad. Now, you can sway off all your gastroenterological worries online by booking an online gastroenterologist consultation with one of the best hepatologists in India. She is a liver specialist in Delhi NCR, one of the finest gastroenterologists in Jhansi and Jammu, and an acidity specialist doctor in Patna. Dr. Pandey’s gastroenterologist live chat has also helped people in several ways.
Case Review
This alcoholic liver case study presents a patient with liver cirrhosis. A 43-year-old man was brought into the hospital with a complaints of loss of appetite, abdominal distention, and arrhythmia. He also experienced itchy skin and blood in the stool. The patient’s family rushed him into the hospital, and he was in a half-conscious state. The patient was taken to the emergency room for evaluation. As told by the family, he had a past medical history and was a heavy alcohol consumer. This alcoholic liver case history consisted of various medical ailments like fatty liver, asthma, tuberculosis, malnutrition, hypertension, and hepatitis C. The patient had a heart attack three years back and stented for the same. Due to his health conditions, he was on several medications. In the emergency room, when the patient was under observation by a stomach specialist doctor in Patna and her team, they were able to diagnose from his symptoms that it was alcoholic liver cirrhosis. The patient went for a few scans including, a liver function test, liver ultrasound, and endoscopy along with CT, blood test, and urine tests.
Case Discussion
Though most of the liver cirrhosis causes remain unknown, with the help of her team, the best liver doctor and specialist in Patna was able to find out the reason for this one. The liver cirrhosis caused in this case was due to the medical history of the patient. His scans came out to be reasonably sound, and a liver biopsy was conducted to confirm the severity and type of liver disease. There were problems in his blood and urine culture, and they were taken care of by the team. His liver appeared swollen in the reports. There were certain other problems seen in his ultrasound and endoscopy. The crew decided to start with the treatment while keeping him under observation for the next 72 hours.
Clinical Symptoms
He was initially confused and was not able to respond or hear properly. According to the condition reported by his family i.e.- appetite loss, memory loss, and confusion were some other clinical symptoms of alcoholic liver cirrhosis. When the doctor talked to the family of the patient, she was able to get a clearer picture. The patient complained about acute abdominal pain. When Dr. Pandey, one of the best doctors in Patna for the stomach, observed the patient and talked to him, she noticed bleeding in his mouth. This further helped doctors to eliminate all doubts, and after looking at the lab results, they made out it was alcoholic liver cirrhosis.
The first and foremost management required when treating the alcoholic liver cirrhosis case is calming the patient down. The liver specialist with the help of her fellow doctors was able to counsel the patient and explain his medical condition to the family. After a complete diagnosis, the patient was taken to the ICU as he was under observation. The doctor prescribed him antioxidant drugs and insulin to control any future problems while treating the present one. The doctor is the best gastroenterologist in Faridabad, Delhi, and Patna, and she handled the situation well before any further complications. The patient got his discharge in due time and was sent back home in a healthy and sound condition.
1. Which Group of People are More Likely to get diagnosed with alcoholic liver cirrhosis?
A person who has drunk heavily for a long time is more prone to acquire this disease. Women are also at risk for this medical disease due to the absence of many enzymes which break down alcohol particles.
Consider consulting the best gastroenterologist in India , Dr. Nivedita Pandey who is also well known for her nutritional counselling services and teleconsultation services. She is also famous for her care from afar service. You can also find her as the best liver specialist doctor in Patna, Bihar or hepatologist in Patna or the best doctor for hepatitis b in Patna , a gastroenterologist in Faridabad , the best gastro doctor in Delhi, NCR , a gastroenterologist In Uttarakhand , a liver specialist in Jhansi , best gastroenterologist in Jammu take advantage of the online gastroenterology consultation to gastroenterologist live chat and receive the best treatment that your body deserves!
2. Is liver cirrhosis cancer?
No, liver cirrhosis is not a type of cancer. If a person has alcoholic liver cirrhosis, he/she has an increased risk of liver cancer.
3. Is liver cirrhosis a hereditary disease?
Negative, alcoholic liver cirrhosis is not a hereditary disease, rather it is a type of an acquired disease.
Privacy Preference Center
Privacy preferences.
- DOI: 10.3389/fsufs.2024.1449964
- Corpus ID: 271990975
Food risk assessment based on NSGA-II algorithm: a case study of alcoholic beverages
- Cen Song , Hanwen Shen , +1 author Jun Zhuang
- Published in Frontiers in Sustainable Food… 23 August 2024
- Agricultural and Food Sciences
27 References
Designing a new multi-objective model for the vehicle routing scheduling at a cross-docking center in mitigating co2 emissions at green supply chain under uncertainty, product safety assessment in a dairy dual-channel supply chain using game theory, comprehensive evaluation of the effect of five sterilization methods on the quality of black carrot juice based on pca, topsis and gra models, risk profiling of food security impediments using decision maker’s behavioural preference towards operational risk management, quantitative analysis of food safety policy—based on text mining methods, using accounting dataset for agricultural sustainability assessment through a multi-criteria approach: an italian case study, forecasting transitions in the state of food security with machine learning using transferable features., deep learning and machine vision for food processing: a survey, emerging applications of machine learning in food safety., an analysis of public opinions regarding take-away food safety: a 2015–2018 case study on sina weibo, related papers.
Showing 1 through 3 of 0 Related Papers
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Vaccinium spp. berries in the prevention and treatment of non-alcoholic fatty liver disease: a comprehensive update of preclinical and clinical research.

1. Introduction
2. materials and methods, 2.1. search strategy, 2.2. selection criteria, 2.3. methodological quality assessment, 2.4. study selection, 3.1. overview of vaccinium spp., 3.2. study selection and characteristics, 3.3. clinical study.
| Study | Study Design | Study Population | Type of Intervention | Dose (mg/day) | Trial Duration | ALT Levels (U/L) | AST Levels (U/L) | Insulin (µ/mL) | HOMA IR | Jadad Scale |
|---|---|---|---|---|---|---|---|---|---|---|
| Hormoznejad et al. 2020 [ ] | Randomized double-blind, placebo-controlled clinical trial | Age ≥ 18 years; BMI 25 ± 5 kg/m , N = 41 (groups: cranberry n = 20, placebo n = 21) | The placebo and cranberry groups received either placebo or cranberry tablets (two tablets; one tablet after lunch and another one after dinner) | 288 | 12 weeks | Before: in the cranberry group: 58.35 ± 18.03; in the placebo group: 55.33 ± 26.10; after: in the cranberry group: 36.90 ± 9.00; in the placebo group: 45.42 ± 15.59 | Before: in the cranberry group: 26.85 ± 10.30; in the placebo group: 29.95 ± 15.02; after: in the cranberry group: 22.60 ± 7.68; in the placebo group: 24.90 ± 15.79 | Before: in the cranberry group: 10.55 ± 1.43; in the placebo group: 10.66 ± 1.55; after: in the cranberry group: 8.20 ± 0.61; in the placebo group: 9.80 ± 1.36 | Before: in the cranberry group: 2.59 ± 0.86; in the placebo group: 2.38 ± 0.71; after: in the cranberry group: 1.88 ± 0.20; in the placebo group: 2.20 ± 0.45 | 5 |
| Shirazi et al. 2021 [ ] | Randomized double-blind, placebo-controlled clinical trial (parallel) | Age ≥ 18 years, N = 110 (groups: cranberry n = 46, placebo n = 48) | The cranberry capsule includes 144 mg Vaccinium macrocarpon (equal to 13 g dried cranberry fruit) | 144 | 6 months | Before: in the cranberry group: 42.74 ± 15.04; in the placebo group: 47.48 ± 18.35; after: in the cranberry group: 39.54 ± 16.95; in the placebo group: 38.69 ± 14.20 | Before: in the cranberry group: 37.22 ± 13.51; in the placebo group: 41.17 ± 16.69; after: in the cranberry group: 32.98 ± 14.33; in the placebo group: 31.98 ± 12.48 | Before: in the cranberry group: 10.38 ± 3.09; in the placebo group: 10.65 ± 3.02; after: in the cranberry group: 5.62 ± 2.04; in the placebo group: 10.06 ± 2.94 | Before: in the cranberry group: 2.78 ± 0.99; in the placebo group: 2.84 ± 0.98; after: in the cranberry group: 1.39 ± 0.62; in the placebo group: 2.51 ± 0.85 | 5 |
3.4. Preclinical Study
3.4.1. vaccinium and the alleviation of liver steatosis and hepatocellular damage, 3.4.2. vaccinium and the alleviation of hepatic fibrosis, 3.4.3. anti-inflammatory effects of vaccinium, 3.4.4. antioxidant effects of vaccinium, 3.4.5. vaccinium , lipid metabolism, and nafld, impact of vaccinium on peroxisome proliferator-activated receptors (ppars), impact of vaccinium on sterol regulatory element-binding proteins (srebps), influence of vaccinium on amp-activated protein kinase (ampk), 3.4.6. the effect of vaccinium on glucose metabolism.
| Study | Study Types | Type of Intervention | Effects | STAIR | |
|---|---|---|---|---|---|
| Animal Model | Dosage and Duration | Metabolism/Molecular | |||
| Ren, Huang, and Cheng 2014 [ ] | Male Sprague Dawley rats (200 to 250 g) | Blueberry juice (15 g/kg, once a day) / 8 weeks | Rats were divided into 2 groups: (1) HFD—50 rats; (2) control group—8 rats | ↓ The degrees of NAFLD and degenerated hepatocytes; ↓ Serum activities of AST and ALT; ↓The ratio of TG/HDL-c; ↑ The mRNA levels of SIRT1, PPAR-α; ↓ The levels of SREBP-1c. | 5 |
| Morrison et al. 2015 [ ] | Female ApoE 3Leiden mice | 0.1% (w/w) Mirtoselect—standardized Vaccinium myrtillus L. extract (36% anthocyanins)/20 weeks | Mice were divided into 3 treatment groups: (1) HCD; (2) HCD and 0.1% (w/w) Mirtoselect; and (3) Western-type diet without cholesterol supplementation | ↓ The development of hepatic steatosis; ↓ Microvesicular steatosis; ↓ An accumulation of lipids esterified to cholesterol (cholesteryl esters); ↓ The hepatic free cholesterol; ↓ p65-NF-κB activity; Expression of Emr1 or Ccl2—not significant; ↓ Neutrophil infiltration and the expression of two neutrophil chemoattractants—Cxcl1 and Cxcl2; ↓ The pronounced increase in collagen and significantly reduced Col1a1 expression. | 4 |
| Glisan et al. 2016 [ ] | Male C57BL/6J mice (4 weeks old) | 0.8% CBE—4 g per day (CBE, D13051702) (CBE—macerated sulfite-free dried cranberries)/21 weeks | Mice were divided into 2 treatment groups: (1) HFD (n = 24) and (2) CBE diet (n = 24) for 10 weeks | Blood glucose levels, plasma insulin levels, and HOMA-IR—not significant; ↓ The plasma levels of free fatty acids; ↓ The plasma levels of IL-1β; ↓ The serum levels of ALT levels; ↓ The total lipid droplet area in the liver and the total hepatic lipid area; ↓ The hepatic expression of the NF-κB-dependent proinflammatory genes TNF-α (↓47%) and Cox2 (↓46%); ↓ The hepatic mRNA expression of Il1b (55%) and Ucp2 (57%); ↓ The hepatic mRNA levels of C-C chemokine receptor 2 (Ccr2), the CCL2 receptor expressed on recruited monocytes, by 56% and Ccl3 by 55%; ↓ The hepatic expression of Nlrp3 (43%) and Txnip (30%); ↑ The gene expression of hepatic PPAR-α. ↓ The transcription factor responsible for regulating Txnip expression (24%). | 5 |
| Ren et al. 2017 [ ] | Male Sprague Dawley rats (6 to 8 weeks old) | 10 mL/kg blueberry juice (1 kg blueberries were thawed, milled, and pressed)/12 weeks | Rats were divided into 2 groups: (1) blueberry juice group (injected with 50 μL/kg saline solution and orally received 10 mL/kg blueberry juice and 10 mL/kg liquid placebo daily); (2) blueberry juice and PPAR-α inhibitor group (injected with 50 μL/kg PPAR-α in saline solution and orally received 10 mL/kg blueberry juice and 10 mL/kg liquid placebo daily) | Blueberry juice: ↓ The serum levels of ALT and AST; ↑ The levels of SOD and GSH; ↓ The serum levels of MDA, TG, TC, and LDL-C increased HDL-C levels; ↑ the mRNA levels of PPAR-α, which reduced the level of SREBP-1c and PNPLA-3. Blueberry juice and PPAR-α inhibitor: ↓ the mRNA levels of SREBP-1c and PNPLA3-α. | 5 |
| Shimizu et al. 2019 [ ] | Male mice C57BL/6 (6 weeks old) | 1% cranberry powder or 5% cranberry powder (anthocyanin 120 mg/100g and proanthocyanidin 2600 mg/100 g)/8 weeks | Mice were divided into 4 treatment groups: (1) ND, (2) HFD, (3) HFD + 1% cranberry powder, and (4) HFD + 5% cranberry powder | ↓ Body weight and concomitantly triggered hyperphagia; ↓ Oxidative stress and proinflammatory cytokine expression (IL-6); The serum levels of glucose—not significant; ↓ The serum levels of TG; ↓ The serum level of ALT; ↓ The serum level of hepatic mRNA of PPAR-γ and MCP-1. | 4 |
| Haga et al. 2019 [ ] | Male homozygous leptin receptor-deficient (BKS.Cg-+ Leprdb/+ Leprdb/Jcl; db/db) mice (10 weeks old) | 5% and 10% bilberry fruits extracts (≥36% anthocyanin glycosides)/8 weeks | Mice were divided into 4 treatment groups: (1) ND, (2) HFD + HCD, (3) HFD + HCD + 5% bilberry fruit extracts, and (4) HFD + HCD + 10% bilberry fruit extracts | ↓ Fat accumulation and TG contents in mouse liver; Less fibrosis; ↓ The serum levels of ALT and AST; ↓ The plasma levels of GLU and TC; ↓ Proinflammatory cytokine levels (TNF-α, IL-9, IL-1β, and IFN-γ). | 4 |
| Li et al. 2020 [ ] | Male Sprague Dawley rats (8 weeks old) | Freeze-dried leaf extract of Vaccinium corymbosum L. (PBL)/8 weeks | Mice were divided into 4 groups: (1) ND; (2) HFD (3) HFD + high dose PBL (H-PBL); (4) HFD + low dose PBL (L-PBL). Rats received: PBL at a dose of 400 mg kg/day (H-PBL group) or 100 mg/kg/day (L-PBL group) or an equal volume of vehicle (0.9% NaCl, ND, and HFD groups) by gavage for 9 weeks | ↓ The hepatic TC, TC, L-LDL, ALT, and AST levels; ↓ The hepatic steatosis and inflammatory infiltration; ↓ The generation of hepatic malondialdehyde (MDA); ↓ The hepatic ROS levels; Protection against hepatic oxidative stress; ↓ pAMPKα, PGC-1α, and SIRT3 proteins in liver; ↑ ERRα, Nrf-1, and Nrf-2 genes in liver. | 5 |
| Nakano et al. 2020 [ ] | Male mice C57BL/6N (5 weeks old) | 2% bilberry anthocyanin extract powder (Mirtoselect)/18 weeks | Mice were randomly divided into 4 groups: (1) ND group, (2) ND + 2% bilberry anthocyanins, (3) WD group, and (4) WD + 2% bilberry anthocyanins | ↓ Body weight, liver weight, epididymal fat mass, liver-to-body-weight ratio, and hepatic fat mass; ↓ The serum level of AST and ALT; ↓ The serum level of MCP-1; ↓ The serum level of TC; ↓ The serum level of insulin; ↑ Insulin resistance; The serum levels of HDL-c, TG, and glucose—not significantly different; ↑ The level of lactic acid in the gut; ↑ The levels of Nrf-2 and SOD2; ↓ The level of Keap1 and TBARS in the liver. | 5 |
| Faheem et al. 2020 [ ] | Male albino Wistar rats (12 weeks old) | Cranberry nutraceutical (186c1025) diluted in water (40 mg/mL)/8 weeks | Mice were divided into 5 groups: control group: (1) ND for 8 weeks and received 1 mL/kg distilled water orally thrice weekly; HFCD group: (2) HFCD for 8 weeks and received 1 mL/kg distilled water orally three times weekly; 50/HFCD group: (3) HFCD and cranberry (50 mg/kg/day) orally three times weekly; 100/HFCD group: (4) HFCD and cranberry (100 mg/kg/day) orally three times weekly; treated group: (5) ND and cranberry (100 mg/kg/day) orally three times weekly | ↓ Body weight; ↓ The serum levels of ALT and AST; ↓ The serum levels of TG; ↓ HOMA IR; ↑ SOD and GSH; ↑ ADP levels; ↑ Nrf-2; ↓ The serum level of TNF-α, IL-6, NF-κB, ↓ TGF-β and α-SMA tissue levels; ↓ Reduction of collagen deposition; ↑ IRS-2 expression. | 5 |
| Zhao et al. 2021 [ ] | Male mice C57BL/6 (6–8 weeks old) | Blueberry-derived exosome-like nanoparticles (BELNs) at 25, 50, or 100 mg/kg/4 weeks | Mice in the 3 HFD groups received intragastric administration of blueberry-derived exosome-like nanoparticles at doses of 25, 50, or 100 mg/kg, administered once every other day | ↓ The serum level of insulin, fasting glucose; ↑ Insulin resistance; ↓ The accumulation of lipid droplets in the liver and the liver weight; ↓ The contents of TC and TG, the levels of ALT and AST, and LDL-C; ↑ The content of HDL-C; ↑ The activities of SOD and GSH; ↓ The content of MDA in the liver; Accelerated the translocation of Nrf-2 from the cytoplasm to nuclei in the liver; ↓ The mRNA levels of FAS and ACC1 in the liver; ↓ The expression of Bcl-2, Bax, and HO-1 in the liver. | 5 |
| Hewage et al. 2021 [ ] | Male C57BL/6J mice (6 weeks old) | (5% w/w) Manitoba lingonberry Vaccinium vitis-idaea L./freeze-dried berry powder/12 weeks | Mice were divided into 3 groups: (1) control (D12450J) diet, (2) HFD (D12492), or (3) HFD supplemented with (5% w/w) Manitoba lingonberry | ↓ The serum levels of ALT and AST; ↓ The hepatic accumulation of TG and TC; ↓ MDA levels and restored GSH levels; ↓ The hepatic GSSG level and restored GSH/GSSG ratio; ↓ The hepatic ACC-1, SREBP-1c mRNA expression, and the nuclear protein level of SREBP-1c; ↑ The expression of Gclc in the liver; ↓ The serum levels of IL-6, MCP-1, and TNF-α mRNA expression; ↑ pAMPK level and pAMPK/AMPK ratio; ↑ Nuclear Nrf-2 protein level in the liver. | 4 |
| Ryyti et al. 2021 [ ] | Male C57BL/6N mice (8 weeks old) | 20% w/w air-dried lingonberry Vaccinium vitis-idaea L. powder (900 g of fresh lingonberries were used to produce 100 g of berry powder)/6 weeks | Mice were divided into 3 groups: (1) LFD (10 kcal% fat); (2) HFD (46 kcal% fat); (3) HFD with air-dried lingonberry powder (20% w/w) | ↓ The serum levels of ALT; ↓ The expression of the acute phase inflammatory factors Saa1 and Saa2; ↓ The expression of Cyp46a1; ↑ The expression of hydroxysteroid (17-beta) dehydrogenase 6 (Hsd17b6) and insulin-like growth factor binding protein 2 (Igfbp2); ↓ The expression of genes associated with lipid metabolic process (Mogat1, Plin4), inflammatory/immune response or cell migration (Lcn2, Saa1, Saa2, Cxcl14, Gcp1, S100a10), and cell cycle regulation (Cdkn1a, Tubb2a, Tubb6). | 4 |
| Hewage et al. 2022 [ ] | Male C57BL/6J mice (6 weeks old) | 5% w/w Manitoba wild lingonberry/12 weeks | Mice were divided into 3 groups: (1) a control diet (D12450J) containing 11% kcal fat, 18% kcal protein, and 71% kcal carbohydrate, or (2) an HFD (D12492) containing 62% kcal fat, 18% kcal protein, and 20% kcal carbohydrate, or (3) an HFD supplemented with (5% w/w) Manitoba wild lingonberry | ↓ The hepatic accumulation of TG and TC; ↓ Notch1 expression in the liver; ↓ Liver NICD1 protein and HES1 mRNA levels; ↓ The expression of SREBP-1c and ACC1; ↑ The hepatic mRNA levels of ACOX1 and CPTIα; ↓ Gene expressions of CD36, DGAT1 and DGAT2. | 3 |
| Zhu et al. 2022 [ ] | Male C57BL/6 mice (8–10 weeks old) | TEC–blueberry monomers were prepared as 1000 ppb, 800, 600, 400, 200, and 100 ppb with 0.1% formic acid methanol solution/16 weeks | Mice were treated with TEC via gavage at doses of 7.5, 15.0, or 30.0 mg/kg daily for 6 weeks following 10 weeks on a high-fat diet (HFD). To achieve tRF-47 knockdown in vivo, a tRF-47 antagomir (5 μg/mouse in 1.5 mL saline) was injected into the tail vein of NASH mice three times a week for 2 weeks, starting after 9 weeks on the HFD | ↓ The serum levels of ALT, AST and MDA; ↑ The level of autophagy marker LC3B in the liver; ↓ The activation of inflammasomes and TLR4; TEC relies on tRF-47 (tRF-47-58ZZJQJYSWRYVMMV5BO) to promote autophagy and weaken pyroptosis. | 5 |
| Sotelo-González et al. 2023 [ ] | Male Wistar rats | 10% (w/v) blueberry aqueous extracts/18 weeks | Mice were divided into 3 groups: (1) standard-diet-fed group; (2) HFFD (standard diet added with 20% lard and 18% fructose); (3) HFFD with blueberry beverage | ↓ The serum level of TG; ↓ The accumulation of lipid vacuoles; ↓ The accumulation of saturated, monounsaturated, and polyunsaturated fatty acids; ↓ FAS and ACC expression. | 5 |
3.5. Cell Culture Experiments
| Study | Study Types | Effects | |
|---|---|---|---|
| Model | Dosage and Duration | ||
| Liu et al. 2011 [ ] | Human hepatocellular cancer cell line (HepG2) | Anthocyanin-rich and phenolic-acid-rich fractions from fresh blueberries (Vaccinium spp.) | |
| Wang et al. 2016 [ ] | Human hepatocellular cancer cell line (HepG2) | purified ACNs from wild blueberries (Vaccinium spp.); −10, 20, and 40 µg/mL | |
| Haga et al. 2019 [ ] | Alpha mouse liver 12 cells | A 90% ethanolic extract of bilberry fruits (≥36% anthocyanin glycosides) | |
| Li et al. 2020 [ ] | Human hepatocellular cancer cell line (HepG2) | Blueberry (Vaccinium corymbosum L.) leaves (PBL);3 doses of PBL at 10 (high), 5 (medium), and 2.5 (low) μg/mL | |
| Zhao et al. 2021 [ ] | Human hepatocellular cancer cell line (HepG2) | Blueberry-derived exosome-like nanoparticles (BELNs)—100 µg/mL | |
| Wang et al. 2021 [ ] | Human hepatocellular cancer cell line (HepG2) | Blueberry leaves (PBL)—6.25, 12.5, 25 µg/mL for 48 h | |
| Zhu et al. 2022 [ ] | Human hepatoma cell line HepG2 | 25, 50, and 75 μM C3Glu, myricetin, myricetin 3-o-galactoside, delphinidin, and blueberry monomers (TEC) | |
| Hewage et al. 2022 [ ] | Human hepatoma cells (HepG2, cell line: HB-8065) | 5% w/w Manitoba wild lingonberry | |
4. Discussion
5. future research, 6. strength and limitations, 7. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, acknowledgments, conflicts of interest.
- Paik, J.M.; Golabi, P.; Younossi, Y.; Mishra, A.; Younossi, Z.M. Changes in the Global Burden of Chronic Liver Diseases from 2012 to 2017: The Growing Impact of NAFLD. Hepatology 2020 , 72 , 1605–1616. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Estes, C.; Razavi, H.; Loomba, R.; Younossi, Z.; Sanyal, A.J. Modeling the Epidemic of Nonalcoholic Fatty Liver Disease Demonstrates an Exponential Increase in Burden of Disease. Hepatology 2018 , 67 , 123–133. [ Google Scholar ] [ CrossRef ]
- Friedman, S.L.; Neuschwander-Tetri, B.A.; Rinella, M.; Sanyal, A.J. Mechanisms of NAFLD Development and Therapeutic Strategies. Nat. Med. 2018 , 24 , 908–922. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zhou, Y.; Li, Z.; Xu, M.; Zhang, D.; Ling, J.; Yu, P.; Shen, Y. O-GlycNacylation Remission Retards the Progression of Non-Alcoholic Fatty Liver Disease. Cells 2022 , 11 , 3637. [ Google Scholar ] [ CrossRef ]
- Vernon, G.; Baranova, A.; Younossi, Z.M. Systematic Review: The Epidemiology and Natural History of Non-Alcoholic Fatty Liver Disease and Non-Alcoholic Steatohepatitis in Adults. Aliment. Pharmacol. Ther. 2011 , 34 , 274–285. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Loomba, R.; Sanyal, A.J. The Global NAFLD Epidemic. Nat. Rev. Gastroenterol. Hepatol. 2013 , 10 , 686–690. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Teng, M.L.P.; Ng, C.H.; Huang, D.Q.; Chan, K.E.; Tan, D.J.H.; Lim, W.H.; Yang, J.D.; Tan, E.; Muthiah, M.D. Global Incidence and Prevalence of Nonalcoholic Fatty Liver Disease. Clin. Mol. Hepatol. 2023 , 29 , S32. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Charytoniuk, T.; Drygalski, K.; Konstantynowicz-Nowicka, K.; Berk, K.; Chabowski, A. Alternative Treatment Methods Attenuate the Development of NAFLD: A Review of Resveratrol Molecular Mechanisms and Clinical Trials. Nutrition 2017 , 34 , 108–117. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Li, J.; Zou, B.; Yeo, Y.H.; Feng, Y.; Xie, X.; Lee, D.H.; Fujii, H.; Wu, Y.; Kam, L.Y.; Ji, F.; et al. Prevalence, Incidence, and Outcome of Non-Alcoholic Fatty Liver Disease in Asia, 1999–2019: A Systematic Review and Meta-Analysis. Lancet Gastroenterol. Hepatol. 2019 , 4 , 389–398. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ullah, R.; Rauf, N.; Nabi, G.; Ullah, H.; Shen, Y.; Zhou, Y.D.; Fu, J. Role of Nutrition in the Pathogenesis and Prevention of Non-Alcoholic Fatty Liver Disease: Recent Updates. Int. J. Biol. Sci. 2019 , 15 , 265. [ Google Scholar ] [ CrossRef ]
- Zhang, C.; Yang, M.; Vairetti, M.; Ferrigno, A. Current Options and Future Directions for NAFLD and NASH Treatment. Int. J. Mol. Sci. 2021 , 22 , 7571. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sanyal, A.J.; Friedman, S.L.; Mccullough, A.J.; Dimick-Santos, L. Challenges and Opportunities in Drug and Biomarker Development for Nonalcoholic Steatohepatitis: Findings and Recommendations from an American Association for the Study of Liver Diseases-U.S. Food and Drug Administration Joint Workshop. Hepatology 2015 , 61 , 1392–1405. [ Google Scholar ] [ CrossRef ]
- Cobbina, E.; Akhlaghi, F. Non-Alcoholic Fatty Liver Disease (NAFLD)—Pathogenesis, Classification, and Effect on Drug Metabolizing Enzymes and Transporters. Drug Metab. Rev. 2017 , 49 , 197–211. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Golabi, P.; Otgonsuren, M.; Cable, R.; Felix, S.; Koenig, A.; Sayiner, M.; Younossi, Z.M. Non-Alcoholic Fatty Liver Disease (NAFLD) Is Associated with Impairment of Health Related Quality of Life (HRQOL). Health Qual. Life Outcomes 2016 , 14 , 18. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Konyn, P.; Ahmed, A.; Kim, D. Causes and Risk Profiles of Mortality among Individuals with Nonalcoholic Fatty Liver Disease. Clin. Mol. Hepatol. 2023 , 29 , S43. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Konyn, P.; Alshuwaykh, O.; Dennis, B.B.; Cholankeril, G.; Ahmed, A.; Kim, D. Gallstone Disease and Its Association With Nonalcoholic Fatty Liver Disease, All-Cause and Cause-Specific Mortality. Clin. Gastroenterol. Hepatol. 2023 , 21 , 940–948.e2. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mantovani, A.; Dalbeni, A. Treatments for NAFLD: State of Art. Int. J. Mol. Sci. 2021 , 22 , 2350. [ Google Scholar ] [ CrossRef ]
- Domingues, I.; Leclercq, I.A.; Beloqui, A. Nonalcoholic Fatty Liver Disease: Current Therapies and Future Perspectives in Drug Delivery. J. Control. Release 2023 , 363 , 415–434. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ciardullo, S.; Muraca, E.; Vergani, M.; Invernizzi, P.; Perseghin, G. Advancements in Pharmacological Treatment of NAFLD/MASLD: A Focus on Metabolic and Liver-Targeted Interventions. Gastroenterol. Rep. 2023 , 12 , goae029. [ Google Scholar ] [ CrossRef ]
- Shao, Y.; Chen, S.; Han, L.; Liu, J. Pharmacotherapies of NAFLD: Updated Opportunities Based on Metabolic Intervention. Nutr. Metab. 2023 , 20 , 30. [ Google Scholar ] [ CrossRef ]
- Keam, S.J. Resmetirom: First Approval. Drugs 2024 , 84 , 729–735. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kokkorakis, M.; Boutari, C.; Hill, M.A.; Kotsis, V.; Loomba, R.; Sanyal, A.J.; Mantzoros, C.S. Resmetirom, the First Approved Drug for the Management of Metabolic Dysfunction-Associated Steatohepatitis: Trials, Opportunities, and Challenges. Metabolism 2024 , 154 , 155835. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Semmler, G.; Datz, C.; Reiberger, T.; Trauner, M. Diet and Exercise in NAFLD/NASH: Beyond the Obvious. Liver Int. 2021 , 41 , 2249–2268. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mansour, A.; Hekmatdoost, A.; Mirmiran, P. What Are the Main Areas of Focus to Prevent or Treat Non-Alcoholic Fatty Liver Disease? J. Dig. Dis. 2019 , 20 , 271–277. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Glass, O.; Filozof, C.; Noureddin, M.; Berner-Hansen, M.; Schabel, E.; Omokaro, S.O.; Schattenberg, J.M.; Barradas, K.; Miller, V.; Francque, S.; et al. Standardisation of Diet and Exercise in Clinical Trials of NAFLD-NASH: Recommendations from the Liver Forum. J. Hepatol. 2020 , 73 , 680–693. [ Google Scholar ] [ CrossRef ]
- Yan, T.; Yan, N.; Wang, P.; Xia, Y.; Hao, H.; Wang, G.; Gonzalez, F.J. Herbal Drug Discovery for the Treatment of Nonalcoholic Fatty Liver Disease. Acta Pharm. Sin. B 2020 , 10 , 3–18. [ Google Scholar ] [ CrossRef ]
- Koperska, A.; Wesołek, A.; Moszak, M.; Szulińska, M. Berberine in Non-Alcoholic Fatty Liver Disease—A Review. Nutrients 2022 , 14 , 3459. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Wei, X.; Wang, C.; Hao, S.; Song, H.; Yang, L. The Therapeutic Effect of Berberine in the Treatment of Nonalcoholic Fatty Liver Disease: A Meta-Analysis. Evid.-Based Complement. Altern. Med. 2016 , 2016 , 3593951. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mansour-Ghanaei, F.; Hadi, A.; Pourmasoumi, M.; Joukar, F.; Golpour, S.; Najafgholizadeh, A. Green Tea as a Safe Alternative Approach for Nonalcoholic Fatty Liver Treatment: A Systematic Review and Meta-Analysis of Clinical Trials. Phyther. Res. 2018 , 32 , 1876–1884. [ Google Scholar ] [ CrossRef ]
- Li, H.Y.; Gan, R.Y.; Shang, A.; Mao, Q.Q.; Sun, Q.C.; Wu, D.T.; Geng, F.; He, X.Q.; Li, H. Bin Plant-Based Foods and Their Bioactive Compounds on Fatty Liver Disease: Effects, Mechanisms, and Clinical Application. Oxid. Med. Cell. Longev. 2021 , 2021 , 6621644. [ Google Scholar ] [ CrossRef ]
- Madduma Hewage, S.; Au-Yeung, K.K.W.; Prashar, S.; Wijerathne, C.U.B.; Karmin, O.; Siow, Y.L. Lingonberry Improves Hepatic Lipid Metabolism by Targeting Notch1 Signaling. Antioxidants 2022 , 11 , 472. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hewage, S.M.; Prashar, S.; Karmin, O.; Siow, Y.L. Lingonberry Improves Non-Alcoholic Fatty Liver Disease by Reducing Hepatic Lipid Accumulation, Oxidative Stress and Inflammatory Response. Antioxidants 2021 , 10 , 565. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Glisan, S.L.; Ryan, C.; Neilson, A.P.; Lambert, J.D. Cranberry Extract Attenuates Hepatic Inflammation in High-Fat-Fed Obese Mice. J. Nutr. Biochem. 2016 , 37 , 60–66. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hormoznejad, R.; Mohammad Shahi, M.; Rahim, F.; Helli, B.; Alavinejad, P.; Sharhani, A. Combined Cranberry Supplementation and Weight Loss Diet in Non-Alcoholic Fatty Liver Disease: A Double-Blind Placebo-Controlled Randomized Clinical Trial. Int. J. Food Sci. Nutr. 2020 , 71 , 991–1000. [ Google Scholar ] [ CrossRef ]
- Li, Z.; Zhang, H.; Li, Y.; Chen, H.; Wang, C.; Wong, V.K.W.; Jiang, Z.; Zhang, W. Phytotherapy Using Blueberry Leaf Polyphenols to Alleviate Non-Alcoholic Fatty Liver Disease through Improving Mitochondrial Function and Oxidative Defense. Phytomedicine 2020 , 69 , 153209. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gong, P.; Chen, F.; Wang, L.; Wang, J.; Jin, S.; Ma, Y. min Protective Effects of Blueberries ( Vaccinium corymbosum L.) Extract against Cadmium-Induced Hepatotoxicity in Mice. Environ. Toxicol. Pharmacol. 2014 , 37 , 1015–1027. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kianbakht, S.; Hashem-Dabaghian, F. Antihypertensive Efficacy and Safety of Vaccinium Arctostaphylos Berry Extract in Overweight/Obese Hypertensive Patients: A Randomized, Double-Blind and Placebo-Controlled Clinical Trial. Complement. Ther. Med. 2019 , 44 , 296–300. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chehri, A.; Yarani, R.; Yousefi, Z.; Shakouri, S.K.; Ostadrahimi, A.; Mobasseri, M.; Araj-Khodaei, M. Phytochemical and Pharmacological Anti-Diabetic Properties of Bilberries ( Vaccinium myrtillus ), Recommendations for Future Studies. Prim. Care Diabetes 2022 , 16 , 27–33. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021 , 372 , 71. [ Google Scholar ] [ CrossRef ]
- Fisher, M.; Feuerstein, G.; Howells, D.W.; Hurn, P.D.; Kent, T.A.; Savitz, S.I.; Lo, E.H. Update of the Stroke Therapy Academic Industry Roundtable Preclinical Recommendations. Stroke 2009 , 40 , 2244–2250. [ Google Scholar ] [ CrossRef ]
- Halpern, S.H.; Douglas, J.M. Appendix: Jadad Scale for Reporting Randomized Controlled Trials. In Evidence-Based Obstetric Anesthesia ; Blackwell Publishing Ltd.: Oxford, UK, 2005; pp. 237–238. [ Google Scholar ] [ CrossRef ]
- Martău, G.A.; Bernadette-Emőke, T.; Odocheanu, R.; Soporan, D.A.; Bochiș, M.; Simon, E.; Vodnar, D.C. Vaccinium Species (Ericaceae): Phytochemistry and Biological Properties of Medicinal Plants. Molecules 2023 , 28 , 1533. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kowalska, K.; Olejnik, A.; Rychlik, J.; Grajek, W. Cranberries ( Oxycoccus quadripetalus ) Inhibit Lipid Metabolism and Modulate Leptin and Adiponectin Secretion in 3T3-L1 Adipocytes. Food Chem. 2015 , 185 , 383–388. [ Google Scholar ] [ CrossRef ]
- Kolehmainen, M.; Mykkänen, O.; Kirjavainen, P.V.; Leppänen, T.; Moilanen, E.; Adriaens, M.; Laaksonen, D.E.; Hallikainen, M.; Puupponen-Pimiä, R.; Pulkkinen, L.; et al. Bilberries Reduce Low-Grade Inflammation in Individuals with Features of Metabolic Syndrome. Mol. Nutr. Food Res. 2012 , 56 , 1501–1510. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Aiello, L.P.; Avery, R.L.; Arrigg, P.G.; Keyt, B.A.; Jampel, H.D.; Shah, S.T.; Pasquale, L.R.; Thieme, H.; Iwamoto, M.A.; Park, J.E.; et al. Vascular Endothelial Growth Factor in Ocular Fluid of Patients with Diabetic Retinopathy and Other Retinal Disorders. N. Engl. J. Med. 1994 , 331 , 1480–1487. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mauramo, M.; Onali, T.; Wahbi, W.; Vasara, J.; Lampinen, A.; Mauramo, E.; Kivimäki, A.; Martens, S.; Häggman, H.; Sutinen, M.; et al. Bilberry ( Vaccinium myrtillus L.) Powder Has Anticarcinogenic Effects on Oral Carcinoma in Vitro and in Vivo. Antioxidants 2021 , 10 , 1319. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tumbas Šaponjac, V.; Čanadanović-Brunet, J.; Ćetković, G.; Djilas, S.; Četojević-Simin, D. Dried Bilberry ( Vaccinium myrtillus L.) Extract Fractions as Antioxidants and Cancer Cell Growth Inhibitors. LWT-Food Sci. Technol. 2015 , 61 , 615–621. [ Google Scholar ] [ CrossRef ]
- Mykkänen, O.T.; Huotari, A.; Herzig, K.H.; Dunlop, T.W.; Mykkänen, H.; Kirjavainen, P.V. Wild Blueberries ( Vaccinium myrtillus ) Alleviate Inflammation and Hypertension Associated with Developing Obesity in Mice Fed with a High-Fat Diet. PLoS ONE 2014 , 9 , e114790. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ashique, S.; Mukherjee, T.; Mohanty, S.; Garg, A.; Mishra, N.; Kaushik, M.; Bhowmick, M.; Chattaraj, B.; Mohanto, S.; Srivastava, S.; et al. Blueberries in Focus: Exploring the Phytochemical Potentials and Therapeutic Applications. J. Agric. Food Res. 2024 , 18 , 101300. [ Google Scholar ] [ CrossRef ]
- Faheem, S.A.; Saeed, N.M.; El-Naga, R.N.; Saad Azab, S. Non Alcoholic Fatty Liver Disease: Pathogenesis, Role of (TNF-α, IL-6) in Hepatic Inflammation and Future Potential Nutraceutical Treatment. Arch. Pharm. Sci. Ain Shams Univ. 2019 , 3 , 154–169. [ Google Scholar ] [ CrossRef ]
- Tundis, R.; Tenuta, M.C.; Loizzo, M.R.; Bonesi, M.; Finetti, F.; Trabalzini, L.; Deguin, B. Vaccinium Species (Ericaceae): From Chemical Composition to Bio-Functional Activities. Appl. Sci. 2021 , 11 , 5655. [ Google Scholar ] [ CrossRef ]
- Colak, N.; Primetta, A.K.; Riihinen, K.R.; Jaakola, L.; Grúz, J.; Strnad, M.; Torun, H.; Ayaz, F.A. Phenolic Compounds and Antioxidant Capacity in Different-Colored and Non-Pigmented Berries of Bilberry ( Vaccinium myrtillus L.). Food Biosci. 2017 , 20 , 67–78. [ Google Scholar ] [ CrossRef ]
- Zhu, C.W.; Lü, H.; Du, L.L.; Li, J.; Chen, H.; Zhao, H.F.; Wu, W.L.; Chen, J.; Li, W.L. Five Blueberry Anthocyanins and Their Antioxidant, Hypoglycemic, and Hypolipidemic Effects in Vitro. Front. Nutr. 2023 , 10 , 1172982. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Xu, Y.; Ke, H.; Li, Y.; Xie, L.; Su, H.; Xie, J.; Mo, J.; Chen, W. Malvidin-3- O -Glucoside from Blueberry Ameliorates Nonalcoholic Fatty Liver Disease by Regulating Transcription Factor EB-Mediated Lysosomal Function and Activating the Nrf2/ARE Signaling Pathway. J. Agric. Food Chem. 2021 , 69 , 4663–4673. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Herrera-Balandrano, D.D.; Chai, Z.; Hutabarat, R.P.; Beta, T.; Feng, J.; Ma, K.; Li, D.; Huang, W. Hypoglycemic and Hypolipidemic Effects of Blueberry Anthocyanins by AMPK Activation: In Vitro and in Vivo Studies. Redox Biol. 2021 , 46 , 102100. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mandal, B.; Das, R.; Mondal, S. Anthocyanins: Potential Phytochemical Candidates for the Amelioration of Non-Alcoholic Fatty Liver Disease. Ann. Pharm. Françaises 2024 , 82 , 373–391. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Dangles, O.; Fenger, J.A. The Chemical Reactivity of Anthocyanins and Its Consequences in Food Science and Nutrition. Molecules 2018 , 23 , 1970. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Alvarez-Suarez, J.M.; Cuadrado, C.; Redondo, I.B.; Giampieri, F.; González-Paramás, A.M.; Santos-Buelga, C. Novel Approaches in Anthocyanin Research-Plant Fortification and Bioavailability Issues. Trends Food Sci. Technol. 2021 , 117 , 92–105. [ Google Scholar ] [ CrossRef ]
- Czank, C.; Cassidy, A.; Zhang, Q.; Morrison, D.J.; Preston, T.; Kroon, P.A.; Botting, N.P.; Kay, C.D. Human Metabolism and Elimination of the Anthocyanin, Cyanidin-3-Glucoside: A 13C-Tracer Study. Am. J. Clin. Nutr. 2013 , 97 , 995–1003. [ Google Scholar ] [ CrossRef ]
- Wu, H.; Oliveira, G.; Lila, M.A. Protein-Binding Approaches for Improving Bioaccessibility and Bioavailability of Anthocyanins. Compr. Rev. Food Sci. Food Saf. 2023 , 22 , 333–354. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Herrera-Balandrano, D.D.; Chai, Z.; Beta, T.; Feng, J.; Huang, W. Blueberry Anthocyanins: An Updated Review on Approaches to Enhancing Their Bioavailability. Trends Food Sci. Technol. 2021 , 118 , 808–821. [ Google Scholar ] [ CrossRef ]
- Hahm, T.H.; Tanaka, M.; Matsui, T. Current Knowledge on Intestinal Absorption of Anthocyanins. J. Agric. Food Chem. 2022 , 70 , 2501–2509. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Guo, Y.; Kitts, D.D.; Dolati, D.; Pratap-Singh, A.; Singh, A. Enhancing Resveratrol Bioavailability and Intestinal Uptake Using an Oil-Based Blueberry Extract Formulated with Chitosan/PEG Containing Nanoparticles. Food Hydrocoll. 2024 , 156 , 110373. [ Google Scholar ] [ CrossRef ]
- Lang, Y.; Gao, H.; Tian, J.; Shu, C.; Sun, R.; Li, B.; Meng, X. Protective Effects of α-Casein or β-Casein on the Stability and Antioxidant Capacity of Blueberry Anthocyanins and Their Interaction Mechanism. LWT 2019 , 115 , 108434. [ Google Scholar ] [ CrossRef ]
- Lang, Y.; Li, B.; Gong, E.; Shu, C.; Si, X.; Gao, N.; Zhang, W.; Cui, H.; Meng, X. Effects of α-Casein and β-Casein on the Stability, Antioxidant Activity and Bioaccessibility of Blueberry Anthocyanins with an in Vitro Simulated Digestion. Food Chem. 2021 , 334 , 127526. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ge, J.; Yue, P.; Chi, J.; Liang, J.; Gao, X. Formation and Stability of Anthocyanins-Loaded Nanocomplexes Prepared with Chitosan Hydrochloride and Carboxymethyl Chitosan. Food Hydrocoll. 2018 , 74 , 23–31. [ Google Scholar ] [ CrossRef ]
- Ge, J.; Yue, X.; Wang, S.; Chi, J.; Liang, J.; Sun, Y.; Gao, X.; Yue, P. Nanocomplexes Composed of Chitosan Derivatives and β-Lactoglobulin as a Carrier for Anthocyanins: Preparation, Stability and Bioavailability in Vitro. Food Res. Int. 2019 , 116 , 336–345. [ Google Scholar ] [ CrossRef ]
- Zhao, L.; Temelli, F.; Chen, L. Encapsulation of Anthocyanin in Liposomes Using Supercritical Carbon Dioxide: Effects of Anthocyanin and Sterol Concentrations. J. Funct. Foods 2017 , 34 , 159–167. [ Google Scholar ] [ CrossRef ]
- Cheng, Y.; Liu, J.; Li, L.; Ren, J.; Lu, J.; Luo, F. Advances in Embedding Techniques of Anthocyanins: Improving Stability, Bioactivity and Bioavailability. Food Chem. X 2023 , 20 , 100983. [ Google Scholar ] [ CrossRef ]
- Cai, X.; Du, X.; Cui, D.; Wang, X.; Yang, Z.; Zhu, G. Improvement of Stability of Blueberry Anthocyanins by Carboxymethyl Starch/Xanthan Gum Combinations Microencapsulation. Food Hydrocoll. 2019 , 91 , 238–245. [ Google Scholar ] [ CrossRef ]
- Faheem, S.A.; Saeed, N.M.; El-Naga, R.N.; Ayoub, I.M.; Azab, S.S. Hepatoprotective Effect of Cranberry Nutraceutical Extract in Non-Alcoholic Fatty Liver Model in Rats: Impact on Insulin Resistance and Nrf-2 Expression. Front. Pharmacol. 2020 , 11 , 511975. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Morrison, M.C.; Liang, W.; Mulder, P.; Verschuren, L.; Pieterman, E.; Toet, K.; Heeringa, P.; Wielinga, P.Y.; Kooistra, T.; Kleemann, R. Mirtoselect, an Anthocyanin-Rich Bilberry Extract, Attenuates Non-Alcoholic Steatohepatitis and Associated Fibrosis in ApoE∗3Leiden Mice. J. Hepatol. 2015 , 62 , 1180–1186. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tang, X.; Shen, T.; Jiang, X.; Xia, M.; Sun, X.; Guo, H.; Ling, W. Purified Anthocyanins from Bilberry and Black Currant Attenuate Hepatic Mitochondrial Dysfunction and Steatohepatitis in Mice with Methionine and Choline Deficiency. J. Agric. Food Chem. 2015 , 63 , 552–561. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Haga, S.; YiMin; Yamaki, H.; Jin, S.; Sogon, T.; Morita, N.; Ozaki, M. Extracts of Bilberry ( Vaccinium myrtillus L.) Fruits Improve Liver Steatosis and Injury in Mice by Preventing Lipid Accumulation and Cell Death. Biosci. Biotechnol. Biochem. 2019 , 83 , 2110–2120. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ren, T.; Huang, C.; Cheng, M. Dietary Blueberry and Bifidobacteria Attenuate Nonalcoholic Fatty Liver Disease in Rats by Affecting SIRT1-Mediated Signaling Pathway. Oxid. Med. Cell. Longev. 2014 , 2014 , 469059. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ren, T.; Zhu, J.; Zhu, L.; Cheng, M. The Combination of Blueberry Juice and Probiotics Ameliorate Non-Alcoholic Steatohepatitis (NASH) by Affecting SREBP-1c/PNPLA-3 Pathway via PPAR-α. Nutrients 2017 , 9 , 198. [ Google Scholar ] [ CrossRef ]
- Zhu, J.; Wen, Y.; Zhang, Q.; Nie, F.; Cheng, M.; Zhao, X. The Monomer TEC of Blueberry Improves NASH by Augmenting TRF-47-Mediated Autophagy/Pyroptosis Signaling Pathway. J. Transl. Med. 2022 , 20 , 128. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zhao, W.; Bian, Y.; Wang, Q.; Yin, F.; Yin, L.; Zhang, Y.L.; Liu, J.H. Blueberry-Derived Exosomes-like Nanoparticles Ameliorate Nonalcoholic Fatty Liver Disease by Attenuating Mitochondrial Oxidative Stress. Acta Pharmacol. Sin. 2021 , 43 , 645–658. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Liu, Y.; Wang, D.; Zhang, D.; Lv, Y.; Wei, Y.; Wu, W.; Zhou, F.; Tang, M.; Mao, T.; Li, M.; et al. Inhibitory Effect of Blueberry Polyphenolic Compounds on Oleic Acid-Induced Hepatic Steatosis in Vitro. J. Agric. Food Chem. 2011 , 59 , 12254–12263. [ Google Scholar ] [ CrossRef ]
- Ryyti, R.; Pemmari, A.; Peltola, R.; Hämäläinen, M.; Moilanen, E. Effects of Lingonberry ( Vaccinium vitis-idaea L.) Supplementation on Hepatic Gene Expression in High-Fat Diet Fed Mice. Nutrients 2021 , 13 , 3693. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nakano, H.; Wu, S.; Sakao, K.; Hara, T.; He, J.; Garcia, S.; Shetty, K.; Hou, D.X. Bilberry Anthocyanins Ameliorate NAFLD by Improving Dyslipidemia and Gut Microbiome Dysbiosis. Nutrients 2020 , 12 , 3252. [ Google Scholar ] [ CrossRef ]
- Sotelo-González, A.M.; Reynoso-Camacho, R.; Hernández-Calvillo, A.K.; Castañón-Servín, A.P.; García-Gutiérrez, D.G.; Gómez-Velázquez, H.D.d.J.; Martínez-Maldonado, M.Á.; de los Ríos, E.A.; Pérez-Ramírez, I.F. Strawberry, Blueberry, and Strawberry-Blueberry Blend Beverages Prevent Hepatic Steatosis in Obese Rats by Modulating Key Genes Involved in Lipid Metabolism. Int. J. Environ. Res. Public Health 2023 , 20 , 4418. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Wang, Y.; Cheng, M.; Zhang, B.; Nie, F.; Jiang, H. Dietary Supplementation of Blueberry Juice Enhances Hepatic Expression of Metallothionein and Attenuates Liver Fibrosis in Rats. PLoS ONE 2013 , 8 , e58659. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Shimizu, K.; Ono, M.; Imoto, A.; Nagayama, H.; Tetsumura, N.; Terada, T.; Tomita, K.; Nishinaka, T. Cranberry Attenuates Progression of Non-Alcoholic Fatty Liver Disease Induced by High-Fat Diet in Mice. Biol. Pharm. Bull. 2019 , 42 , 1295–1302. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Masnadi Shirazi, K.; Shirinpour, E.; Masnadi Shirazi, A.; Nikniaz, Z. Effect of Cranberry Supplementation on Liver Enzymes and Cardiometabolic Risk Factors in Patients with NAFLD: A Randomized Clinical Trial. BMC Complement. Med. Ther. 2021 , 21 , 283. [ Google Scholar ] [ CrossRef ]
- Käräjämäki, A.J.; Bloigu, R.; Kauma, H.; Kesäniemi, Y.A.; Koivurova, O.P.; Perkiömäki, J.; Huikuri, H.; Ukkola, O. Non-Alcoholic Fatty Liver Disease with and without Metabolic Syndrome: Different Long-Term Outcomes. Metabolism 2017 , 66 , 55–63. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kleemann, R.; Verschuren, L.; Van Erk, M.J.; Nikolsky, Y.; Cnubben, N.H.P.; Verheij, E.R.; Smilde, A.K.; Hendriks, H.F.J.; Zadelaar, S.; Smith, G.J.; et al. Atherosclerosis and Liver Inflammation Induced by Increased Dietary Cholesterol Intake: A Combined Transcriptomics and Metabolomics Analysis. Genome Biol. 2007 , 8 , R200. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Francque, S.; Szabo, G.; Abdelmalek, M.F.; Byrne, C.D.; Cusi, K.; Dufour, J.F.; Roden, M.; Sacks, F.; Tacke, F. Nonalcoholic Steatohepatitis: The Role of Peroxisome Proliferator-Activated Receptors. Nat. Rev. Gastroenterol. Hepatol. 2020 , 18 , 24–39. [ Google Scholar ] [ CrossRef ]
- Rinella, M.E.; Sanyal, A.J. Management of NAFLD: A Stage-Based Approach. Nat. Rev. Gastroenterol. Hepatol. 2016 , 13 , 196–205. [ Google Scholar ] [ CrossRef ]
- Lindenmeyer, C.C.; McCullough, A.J. The Natural History of Nonalcoholic Fatty Liver Disease—An Evolving View. Clin. Liver Dis. 2018 , 22 , 11–21. [ Google Scholar ] [ CrossRef ]
- Suzuki, M.; Takeuchi, H.; Kakita, T.; Unno, M.; Katayose, Y.; Matsuno, S. The Involvement of the Intracellular Superoxide Production System in Hepatic Ischemia-Reperfusion Injury: In Vivo and in Vitro Experiments Using Transgenic Mice Manifesting Excessive CuZn-SOD Activity. Free Radic. Biol. Med. 2000 , 29 , 756–763. [ Google Scholar ] [ CrossRef ]
- Sayed, A.A.R. Ferulsinaic Acid Modulates SOD, GSH, and Antioxidant Enzymes in Diabetic Kidney. Evid. Based. Complement. Alternat. Med. 2012 , 2012 , 580104. [ Google Scholar ] [ CrossRef ]
- Wang, B.; Zhao, S.; Tan, F.; Li, H.; Chu, R.; Wang, X.; Sun, H.; Zhang, M. A Novel Green Production Process of Citric Acid on the Pilot Scale by Directly Recycling Its Extraction Effluent. J. Clean. Prod. 2020 , 277 , 124068. [ Google Scholar ] [ CrossRef ]
- Qiu, Y.Y.; Zhang, J.; Zeng, F.Y.; Zhu, Y.Z. Roles of the Peroxisome Proliferator-Activated Receptors (PPARs) in the Pathogenesis of Nonalcoholic Fatty Liver Disease (NAFLD). Pharmacol. Res. 2023 , 192 , 106786. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Fougerat, A.; Montagner, A.; Loiseau, N.; Guillou, H.; Wahli, W. Peroxisome Proliferator-Activated Receptors and Their Novel Ligands as Candidates for the Treatment of Non-Alcoholic Fatty Liver Disease. Cells 2020 , 9 , 1638. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hebbachi, A.M.; Knight, B.L.; Wiggins, D.; Patel, D.D.; Gibbons, G.F. Peroxisome Proliferator-Activated Receptor α Deficiency Abolishes the Response of Lipogenic Gene Expression to Re-Feeding: Restoration of the Normal Response by Activation of Liver x Receptor α. J. Biol. Chem. 2008 , 283 , 4866–4876. [ Google Scholar ] [ CrossRef ]
- Christofides, A.; Konstantinidou, E.; Jani, C.; Boussiotis, V.A. The Role of Peroxisome Proliferator-Activated Receptors (PPAR) in Immune Responses. Metabolism 2021 , 114 , 154338. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Han, X.; Wu, Y.L.; Yang, Q.; Cao, G. Peroxisome Proliferator-Activated Receptors in the Pathogenesis and Therapies of Liver Fibrosis. Pharmacol. Ther. 2021 , 222 , 107791. [ Google Scholar ] [ CrossRef ]
- Su, F.; Koeberle, A. Regulation and Targeting of SREBP-1 in Hepatocellular Carcinoma. Cancer Metastasis Rev. 2023 , 43 , 673–708. [ Google Scholar ] [ CrossRef ]
- Kawamura, S.; Matsushita, Y.; Kurosaki, S.; Tange, M.; Fujiwara, N.; Hayata, Y.; Hayakawa, Y.; Suzuki, N.; Hata, M.; Tsuboi, M.; et al. Inhibiting SCAP/SREBP Exacerbates Liver Injury and Carcinogenesis in Murine Nonalcoholic Steatohepatitis. J. Clin. Investig. 2022 , 132 , 1–18. [ Google Scholar ] [ CrossRef ]
- Chandrasekaran, P.; Weiskirchen, R. The Role of SCAP/SREBP as Central Regulators of Lipid Metabolism in Hepatic Steatosis. Int. J. Mol. Sci. 2024 , 25 , 1109. [ Google Scholar ] [ CrossRef ]
- Bayram, H.M.; Majoo, F.M.; Ozturkcan, A. Polyphenols in the Prevention and Treatment of Non-Alcoholic Fatty Liver Disease: An Update of Preclinical and Clinical Studies. Clin. Nutr. ESPEN 2021 , 44 , 1–14. [ Google Scholar ] [ CrossRef ]
- Lin, S.; Wang, Z.; Lin, Y.; Ge, S.; Hamzah, S.S.; Hu, J. Bound Phenolics from Fresh Lotus Seeds Exert Anti-Obesity Effects in 3T3-L1 Adipocytes and High-Fat Diet-Fed Mice by Activation of AMPK. J. Funct. Foods 2019 , 58 , 74–84. [ Google Scholar ] [ CrossRef ]
- Green, C.L.; Lamming, D.W.; Fontana, L. Molecular Mechanisms of Dietary Restriction Promoting Health and Longevity. Nat. Rev. Mol. Cell Biol. 2022 , 23 , 56–73. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Li, L.; Yao, Y.; Zhao, J.; Cao, J.; Ma, H. Dehydroepiandrosterone Protects against Hepatic Glycolipid Metabolic Disorder and Insulin Resistance Induced by High Fat via Activation of AMPK-PGC-1α-NRF-1 and IRS1-AKT-GLUT2 Signaling Pathways. Int. J. Obes. 2020 , 44 , 1075–1086. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Fang, C.; Pan, J.; Qu, N.; Lei, Y.; Han, J.; Zhang, J.; Han, D. The AMPK Pathway in Fatty Liver Disease. Front. Physiol. 2022 , 13 , 970292. [ Google Scholar ] [ CrossRef ]
- Zhao, P.; Saltiel, A.R. From Overnutrition to Liver Injury: AMP-Activated Protein Kinase in Nonalcoholic Fatty Liver Diseases. J. Biol. Chem. 2020 , 295 , 12279–12289. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mehmood, A.; Zhao, L.; Wang, Y.; Pan, F.; Hao, S.; Zhang, H.; Iftikhar, A.; Usman, M. Dietary Anthocyanins as Potential Natural Modulators for the Prevention and Treatment of Non-Alcoholic Fatty Liver Disease: A Comprehensive Review. Food Res. Int. 2021 , 142 , 110180. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Wang, Y.; Zhao, L.; Wang, D.; Huo, Y.; Ji, B. Anthocyanin-Rich Extracts from Blackberry, Wild Blueberry, Strawberry, and Chokeberry: Antioxidant Activity and Inhibitory Effect on Oleic Acid-Induced Hepatic Steatosis in Vitro. J. Sci. Food Agric. 2016 , 96 , 2494–2503. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Wang, C.R.; Chen, H.W.; Li, Y.; Zhou, M.Y.; Wong, V.K.W.; Jiang, Z.H.; Zhang, W. Network Pharmacology Exploration Reveals Anti-Apoptosis as a Common Therapeutic Mechanism for Non-Alcoholic Fatty Liver Disease Treated with Blueberry Leaf Polyphenols. Nutrients 2021 , 13 , 4060. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Pafili, K.; Roden, M. Nonalcoholic Fatty Liver Disease (NAFLD) from Pathogenesis to Treatment Concepts in Humans. Mol. Metab. 2021 , 50 , 101122. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rada, P.; González-Rodríguez, Á.; García-Monzón, C.; Valverde, Á.M. Understanding Lipotoxicity in NAFLD Pathogenesis: Is CD36 a Key Driver? Cell Death Dis. 2020 , 11 , 802. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Maleki, M.; Ariaii, P.; Fallah, H. Effects of Celery Extracts on the Oxidative Stability of Canola Oil Under Thermal Condition. J. Food Process. Preserv. 2016 , 40 , 531–540. [ Google Scholar ] [ CrossRef ]
- Buzzetti, E.; Pinzani, M.; Tsochatzis, E.A. The Multiple-Hit Pathogenesis of Non-Alcoholic Fatty Liver Disease (NAFLD). Metabolism 2016 , 65 , 1038–1048. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Dorairaj, V.; Sulaiman, S.A.; Abu, N.; Murad, N.A.A. Nonalcoholic Fatty Liver Disease (NAFLD): Pathogenesis and Noninvasive Diagnosis. Biomedicines 2021 , 10 , 15. [ Google Scholar ] [ CrossRef ]
- Li, L.; Fu, J.; Sun, J.; Liu, D.; Chen, C.; Wang, H.; Hou, Y.; Xu, Y.; Pi, J. Is Nrf2-ARE a Potential Target in NAFLD Mitigation? Curr. Opin. Toxicol. 2019 , 13 , 35–44. [ Google Scholar ] [ CrossRef ]
- Bhatt-Wessel, B.; Jordan, T.W.; Miller, J.H.; Peng, L. Role of DGAT Enzymes in Triacylglycerol Metabolism. Arch. Biochem. Biophys. 2018 , 655 , 1–11. [ Google Scholar ] [ CrossRef ]
- Sergazy, S.; Shulgau, Z.; Kamyshanskiy, Y.; Zhumadilov, Z.; Krivyh, E.; Gulyayev, A.; Aljofan, M. Blueberry and Cranberry Extracts Mitigate CCL4-Induced Liver Damage, Suppressing Liver Fibrosis, Inflammation and Oxidative Stress. Heliyon 2023 , 9 , e15370. [ Google Scholar ] [ CrossRef ]
- Sun, J.; Wu, Y.; Long, C.; He, P.; Gu, J.; Yang, L.; Liang, Y.; Wang, Y. Anthocyanins Isolated from Blueberry Ameliorates CCl4 Induced Liver Fibrosis by Modulation of Oxidative Stress, Inflammation and Stellate Cell Activation in Mice. Food Chem. Toxicol. 2018 , 120 , 491–499. [ Google Scholar ] [ CrossRef ]
Click here to enlarge figure
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Książek, E.; Goluch, Z.; Bochniak, M. Vaccinium spp. Berries in the Prevention and Treatment of Non-Alcoholic Fatty Liver Disease: A Comprehensive Update of Preclinical and Clinical Research. Nutrients 2024 , 16 , 2940. https://doi.org/10.3390/nu16172940
Książek E, Goluch Z, Bochniak M. Vaccinium spp. Berries in the Prevention and Treatment of Non-Alcoholic Fatty Liver Disease: A Comprehensive Update of Preclinical and Clinical Research. Nutrients . 2024; 16(17):2940. https://doi.org/10.3390/nu16172940
Książek, Ewelina, Zuzanna Goluch, and Marta Bochniak. 2024. " Vaccinium spp. Berries in the Prevention and Treatment of Non-Alcoholic Fatty Liver Disease: A Comprehensive Update of Preclinical and Clinical Research" Nutrients 16, no. 17: 2940. https://doi.org/10.3390/nu16172940
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals

IMAGES
VIDEO
COMMENTS
Dr. Andrew Z. Fenves: This 54-year-old man with a history of alcohol use disorder was admitted to the hospital with concerns about alcohol withdrawal symptoms. He had recent binges in which he ...
This case is first of the kind depicting clinical features as well as withdrawal of combined volatile and moderate alcohol abuse. The feature of combined intoxication of the two abused substances makes it difficult for the clinician to reach a diagnosis. Our case report thus puts forward the scenario of increasing combined alcohol and volatile ...
A Case of Alcohol Abuse. The patient is a 65-year-old white woman, married for 35 years to an accountant. They have 5 grown children and 12 grandchildren. She taught elementary school for 28 years and has not worked since retiring 15 years ago.
Case Study Details. Jeff is a 66-year-old Caucasian man whose wife has encouraged him to seek treatment. He has never been in therapy before, and has no history of depression or anxiety. However, his alcohol use has recently been getting in the way of his marriage, and interfering with his newly-retired life.
How would you diagnose and treat a 54-year-old man with alcohol withdrawal and altered mental status? Read this case challenge and test your knowledge.
An alcoholic patient who continues to drink: case presentation. Stuart McPherson, specialist registrar1 and Colin John Rees, consultant gastroenterologist1. Mr Bond is a 42 year old man with alcoholic cirrhosis who was admitted to our unit with haematemesis. He had had three previous admissions with alcohol related problems and had twice bled ...
This case study presents the diagnosis and treatment of a male patient with an alcohol use disorder (AUD). Although medications are helpful in AUD, nurse practitioners must be cognizant when combining them with other approaches, such as therapy. Some clinicians prefer to control AUD use before treating other issues, under the theory that alcohol can obscure and aggravate underlying physical ...
This case report discusses a 60-year-old male with severe alcohol use disorder who presented with a newly diagnosed AF with RVR, DCM, and cirrhosis. Our case demonstrates the consequential health risks of chronic alcoholism and highlights the significance of timely screening and early intervention for at-risk alcohol use.
Globally, alcohol use is the seventh leading risk factor for both deaths and DALYs (disability-adjusted life years). 1 In India, per-capita consumption of alcohol has increased over time, along with the risk of its public health impact. 2 Besides, the treatment gap for alcohol use disorders (AUDs) is 86%. 3 The relapse rates among untreated patients with AUDs are high. 4 Although the relapse ...
This systematic review of alcohol-induced psychotic disorder treatment found 15 studies and 10 case reports of relevance. Older studies of first-generation antipsychotics reported full or partial remission in most patients, as did newer studies with second-generation antipsychotics.
It is well recognized that alcohol use disorders (AUD) have a damaging impact on the health of the population. According to the World Health Organization (WHO), 5.3% of all global deaths were attributable to alcohol consumption in 2016 [].The 2016 Global Burden of Disease Study reported that alcohol use led to 1.6% (95% uncertainty interval [UI] 1.4-2.0) of total DALYs globally among females ...
Alcohol use disorder (AUD) is a medical condition characterized by an impaired ability to stop or control alcohol use despite adverse social, occupational, or health consequences. It encompasses the conditions that some people refer to as alcohol abuse, alcohol dependence, alcohol addiction, and the colloquial term, alcoholism.
Case studies; Robert's story; Robert's story. Robert was living with an alcohol addiction and was homeless for over 25 years. He was well known in the local community and was identified as one of the top 100 A&E attendees at the Local General Hospital. ... He had significantly reduced his alcohol intake with long periods of abstinence and was ...
This work attempts to address this using a case study and relevant literature review. Case presentation: A 40-year-old male with alcohol dependence (for 20 years) reported new-onset terrifying nightmares and violent behaviours in his sleep precipitated by alcohol withdrawal states for the last 18 months. The polysomnographic finding of REM ...
Alcohol consumption and dependence is considered a public health problem and deserve attention because of the social, work, family, physical, legal and violence-related risks it represents. This study aimed to identify the effects of alcoholism on family relations and, by means of case management, to encourage the recovery of these relationships.
Alcoholics Anonymous, the worldwide fellowship of sobriety seekers, is the most effective path to abstinence, according to a comprehensive analysis conducted by a Stanford School of Medicine researcher and his collaborators.. After evaluating 35 studies — involving the work of 145 scientists and the outcomes of 10,080 participants — Keith Humphreys, PhD, professor of psychiatry and ...
I remember this day now as sharp as the edge of a knife because in that moment, I wanted to die. By this time in my life, I had been abused by my family—sexually and emotionally—for as long as ...
In another study, Payne, explored the role of social support in recovery among Alcoholics Anonymous (AA) members. The study reported on the role of attachment characteristics that influence recovery capital. These findings highlight the importance of fostering self-esteem and addressing attachment issues in the recovery process, particularly ...
Chest X-ray showing signs of alcoholic cardiomyopathy (cardiomegaly, venous vessels enlargement, pulmonary oedema). Alcohol induces several changes in the myocardial structure (myocyte loss, intracellular organelle dysfunction and contractile protein alterations). However, the exact pathogenesis of alcoholic cardiomyopathy is still unclear.
In our study, my colleagues and I used a mouse model to measure the effects that alcohol use by mom, dad or both parents around the time of conception have on their offspring aging and chronic ...
HESI- Alcoholism Case Study. Nick Davis, a 42-year-old, is accompanied to the emergency room by the police who found him standing on a bridge and threatening to jump. He planned to jump off the bridge because his girlfriend moved out on him and he lost his job as a cook several days ago. Vital signs upon admission are BP 146/94, P 92, R 20, and ...
After removing duplicates, case studies, articles that were not published in English, and studies not conducted in humans, the remaining publications were reviewed to determine whether they met inclusion criteria, namely that the study examined vulnerabilities, consequences, and possible mechanisms for alcohol-induced blackouts ...
This alcoholic liver case study presents a patient with liver cirrhosis. A 43-year-old man was brought into the hospital with a complaints of loss of appetite, abdominal distention, and arrhythmia. He also experienced itchy skin and blood in the stool. The patient's family rushed him into the hospital, and he was in a half-conscious state.
Alcoholic beverages have been a significant industry. However, they present food safety risks, necessitating heightened regulation and monitoring. The safety risk assessment of alcoholic beverages encompasses a variety of factors, including microorganisms, excessive methanol content, chemical adulteration, and food additives. The data used in this paper is sourced from the National Food Safety ...
Case Study on Alcoholism - Free download as Word Doc (.doc / .docx), PDF File (.pdf), Text File (.txt) or read online for free. Tandy U., a 49-year-old man with a history of alcoholism, was admitted to the ICU for an upper GI bleed and alcohol intoxication. His lab results indicate chronic heavy drinking and withdrawal risk. He experiences alcohol withdrawal delirium for 36 hours.
Study with Quizlet and memorize flashcards containing terms like Meet the client:, One of the simplest tools that a nurse can use to screen for alcoholism is the CAGE questionnaire. CAGE is an acronym that represents the four questions it contains. What is the first question that the nurse should ask Nick?, Nick answers "yes" to two of the four questions on the CAGE questionnaire.
The document provides a case study of Mr. Johnson Babu, a 24-year-old man admitted to a de-addiction center for alcohol dependence. It details his personal history, including a 6-year history of daily alcohol and tobacco use. A mental status examination found him oriented with normal mood, affect, and cognition. A physical examination showed he was in overall healthy condition. The goal of his ...
Exclusion criteria included reviews, research notes, book chapters, case studies, and grants. The review included 20 studies: 2 clinical trials and 18 studies on animals and cell lines. ... Non-alcoholic fatty liver disease (NAFLD) is a common chronic liver disorder marked by the buildup of triacylglycerols (TGs) in the liver. It includes a ...