- Research article
- Open access
- Published: 16 May 2013

The integration of occupational therapy into primary care: a multiple case study design
- Catherine Donnelly 1 , 2 ,
- Christie Brenchley 3 ,
- Candace Crawford 4 &
- Lori Letts 5
BMC Family Practice volume 14 , Article number: 60 ( 2013 ) Cite this article
30k Accesses
45 Citations
1 Altmetric
Metrics details
For over two decades occupational therapists have been encouraged to enhance their roles within primary care and focus on health promotion and prevention activities. While there is a clear fit between occupational therapy and primary care, there have been few practice examples, despite a growing body of evidence to support the role. In 2010, the province of Ontario, Canada provided funding to include occupational therapists as members of Family Health Teams, an interprofessional model of primary care. The integration of occupational therapists into this model of primary care is one of the first large scale initiatives of its kind in North America. The objective of the study was to examine how occupational therapy services are being integrated into primary care teams and understand the structures supporting the integration.
A multiple case study design was used to provide an in-depth description of the integration of occupational therapy. Four Family Health Teams with occupational therapists as part of the team were identified. Data collection included in-depth interviews, document analyses, and questionnaires.
Each Family Health Team had a unique organizational structure that contributed to the integration of occupational therapy. Communication, trust and understanding of occupational therapy were key elements in the integration of occupational therapy into Family Health Teams, and were supported by a number of strategies including co-location, electronic medical records and team meetings. An understanding of occupational therapy was critical for integration into the team and physicians were less likely to understand the occupational therapy role than other health providers.
With an increased emphasis on interprofessional primary care, new professions will be integrated into primary healthcare teams. The study found that explicit strategies and structures are required to facilitate the integration of a new professional group. An understanding of professional roles, trust and communication are foundations for interprofessional collaborative practice.
Peer Review reports
There is a clear fit between occupational therapy (OT) and primary care. Both view health in a holistic manner and seek to support individuals and communities in achieving and maintaining a healthy lifestyle [ 1 , 2 ]. While there is evidence to support the role of occupational therapy in health promotion and prevention, there have been few practice examples of occupational therapy within primary care settings [ 3 , 4 ].
The lack of an occupational therapy presence in primary care can be attributed to a number of factors [ 5 ]. First and foremost, there has not been funding for occupational therapy in primary care, both in Canada and internationally [ 5 ]. Second, primary care has traditionally been delivered in solo practitioner models [ 6 ]. Finally, the occupational therapy profession has traditionally focused on the rehabilitation or remediation of function versus health promotion [ 7 ].
In 2003, the First Ministers of Canada committed to ensuring that half of Canadians would have access to multidisciplinary primary care teams by 2011 [ 8 ]. While this has not yet been achieved, the province of Ontario’s commitment to health reform has resulted in the establishment of Family Health Teams, an innovative model of interprofessional primary care [ 9 ]. There are currently 200 teams that serve approximately 25% of the province’s population.
Each Family Health Team is interprofessional in nature; however there is considerable variability in structure, size and organizational dimensions. A Family Health Team may consist of a single site or may be comprised of multiple offices that have common programs or structures such as an electronic medical record (EMR), programs and management. The complement of interdisciplinary health professionals also varies according to the specific needs of the community.
While the initial list of funded interdisciplinary health providers did not include occupational therapists, in March 2009 the Ontario government committed funds to include occupational therapy services in Family Health Teams [ 10 ]. At the initiation of the study, 20 teams had occupational therapists within their team complement. Ontario’s initiative is one of the first examples of large-scale integration of occupational therapy into primary care teams in North America.
A growing number of national and international studies have documented the structures and processes to support interprofessional primary care teams [ 11 , 12 ]. However, few of these studies have included occupational therapy within the team complement and no study has exclusively examined the implementation of occupational therapy into a new or existing primary care team.
A handful of articles have examined the integration of other professionals into primary care teams [ 13 – 15 ]. While these findings might provide insights for occupational therapy, each profession entering primary care will have unique features and support the team through unique roles. Occupational therapists have a long history in working in team- based environments and therefore the implementation of occupational therapy services may be experienced differently than professions that have been primarily consultative.
Interprofessional teams are poised to play a greater role in the delivery of primary care in Canada and abroad [ 16 , 17 ]. It is anticipated that more disciplines will continue to enter primary care, making it critical to understand how professionals are being introduced into primary care teams. The purpose of the paper is to examine how occupational therapy is being integrated into primary care teams and understand the structures and processes supporting the integration.
The study aimed to explore the primary guiding question: What structures and processes support the integration of occupational therapy in Family Health Teams? A multiple case study design [ 18 ] was conducted that included four Family Health Team sites within the province of Ontario, Canada. Case study research seeks to investigate real life experiences within the context in which it occurs and involves the collection of detailed information using a variety of data collection methods [ 18 – 20 ]. As there are few documented examples of occupational therapists in primary care, a case study design enabled an in-depth exploration of how occupational therapy was being integrated into interprofessional primary care teams. As per case study methodology as outlined by Yin [ 18 ], each case provided an opportunity for the replication of the outlined questions and methods.
Site identification
Four cases (Family Health Teams) were identified from the approximately 20 that employed occupational therapists at the time of the study. The sites were chosen to reflect different dimensions of service provision that may influence the role and integration of occupational therapy. The literature on interprofessional collaborative practice has identified certain elements that support interprofessional collaborative care, including: (1) EMR, (2) team size, and (3) co-location of health professionals [ 6 , 13 ]. Each dimension was considered in the identification of the cases. Two further dimensions were considered in the case selection; academic versus community and rural versus urban. While there is little evidence examining the role of occupational therapist in primary care, the literature has described occupational therapy working with a wide range of client populations and conditions [ 4 ]. Therefore the nature and duration of clinical experience of occupational therapist as well as the full-time equivalency (FTE) were also thought to be important elements to consider in the identification of cases. Purposeful sampling of sites was used with the intent to sample breadth of communities, teams, and occupational therapists.
Participants
Information letters were sent to the Executive Director at each site describing the study and seeking approval for participation. All occupational therapists working at the Family Health Teams were asked to participate. The Executive Director and the lead physician were also invited due to their leadership and decision making roles on the team. In addition, any member of the team that provided collaborative patient care with the occupational therapist was also considered to be eligible for the study. The occupational therapist(s) at each Family Health Team acted as the main contact for liaising and coordinating interviews with the staff.
Ethics approval was provided by Queen’s University Health Sciences Research Ethics Board.
Data collection
Data collection drew on multiple forms of evidence including semi-structured interviews, document analyses and questionnaires. The principal investigator (CD) visited each Family Health Team to retrieve documents for analyses, distribute questionnaires and conduct interviews with key informants. See Table 1 for list of disciplines interviewed at each site. All interviews were conducted between the February-May 2012 using a semi-structured interview guide. Questions were developed by the research team and were informed by the literature on interprofessional collaborative primary care [ 11 , 12 ]. Questions fell under five broad categories including; roles (how would you describe your role, how did you establish your role), physical space (i.e. location of team members and primary care sites), community collaborations, collaborative practice (i.e. nature, processes and structures to support collaborative practice) and processes (i.e. nature and use of electronic medical record). Additional questions regarding funding for occupational therapy were included in the interview guide for the Executive Director and questions related to clinical practice were removed.
Program documents included job descriptions, occupational therapy assessments, team mission and vision. The web pages of each Family Health Team were viewed to obtain further information about team collaboration, and sites were contacted if further questions about the nature of occupational therapy services were identified. Two sites were contacted to clarify demographic information (number of sites and number of physicians) and the occupational therapist(s) at each site was contacted to provide further details on the referral process to occupational therapy. A Family Health Team Profile was completed by each Executive Director to obtain descriptive information about the Family Health Team demographics, including the type of electronic medical record system, number of rostered patients and health professional make-up. An Occupational Therapy Profile was completed by each occupational therapist to obtain information about their educational background and work experiences.
Data analyses
Both within-case and cross-case analyses were conducted [ 18 , 19 ]. Pattern matching was then used as the overall analytic strategy. This approach “compares an empirically based pattern with a predicted one” [18, p 106], where propositions are developed prior to data collection in order to identify a predicted pattern of variables. Propositions for this study were derived from the literature on interprofessional collaborative practice. A number of factors have been found to support interprofesional practice. One of these is the extent to which there is a shared understanding of team members’ roles and scopes of practice [ 12 ]. This was felt to be particularly relevant for the study as occupational therapists were new professionals within the teams. Studies have also identified the nature of team processes and organizational structures to be important influences on collaboration, and the nature of team processes was anticipated to influence the integration of occupational therapy [ 21 ]. The use of electronic medical records (EMR) have become standard in Family Health Teams in Ontario, Canada [ 22 ] and have already been found to support internal communication. Occupational therapists’ access and use of EMRs thus become an important element to consider [ 13 ]. Therefore, the two study propositions were:
Integration of occupational therapy into the Family Health Team will depend on the understanding of the occupational therapy role by team members, and structures to support interprofessional collaborative practice.
The EMR will be pivotal in supporting the integration of occupational therapy.
Each case was first analyzed individually, followed by cross-site analyses to determine common themes [ 19 ]. Data obtained from documents were extracted using apriori document analysis forms. Tables and matrixes were used to visually examine the data for each case and across cases. Qualitative interview data were digitally recorded and transcribed verbatim by a research assistant. Atlas ti, a qualitative data analysis and research software program, was used to code data and identify themes both within and across cases. All transcripts were read and re-read by the primary author and preliminary codes were established. A number of strategies were used to establish trustworthiness [ 23 , 24 ]. Four transcripts were read and independently coded by a second investigator (LL) using the preliminary coding structure. Transcripts were selected from four different health professions to ensure the coding structure could be applied across transcripts. Any discrepancies in coding were noted and discussed until consensus was reached. Two revisions to the coding structure were made; the first involved collapsing two codes into one code, the second revision involved renaming a code to better reflect the essence of the statements being captured.
A second strategy to establish trustworthiness involved member checking. Occupational therapists were provided with a preliminary summary of their site and asked to contact the primary author if any errors were noted, or if additional information should be included. None of the participants reported any errors or provided further information.
A third strategy involved triangulation of data methods, sources and investigators. The study included a number of data methods including interviews, questionnaires and document analyses. Each contributed to the understanding of how occupational therapists are integrated into primary care and structures to support the integration. Participants included members from a range of disciplines across four sites in order to provide different perspectives and experiences on the integration of occupational therapists. Finally, the investigation team was made up four occupational therapists; two academics (CD, LL), one administrative (CB) and one clinician working in primary care (CC). The diversity of the team brought unique perspectives to the design, implementation and analyses and grounded the study in both research and practice.
Table 2 provides a description of the four sites. Patient rosters ranged from 7,200 to 42,000 patients and sites were located in both rural and urban centres. Three sites were community sites and one was an academic site. The academic site had a dual mandate to provide both primary care services, and to educate medical students/residents and other health disciplines. Occupational therapists were all relatively new to their positions with a range of 3 to 18 months. Occupational therapists in two sites had less than five years experience, while two sites had occupational therapists with 15 and more years of experience. Each site had a unique complement of health providers, which included: chiropodists, psychologists, social workers, dieticians, physician assistants, pharmacists, patient educators, mental health workers, health promoters, respiratory therapists, case managers, nurses, nurse practitioners, and physicians.
Case 1: Very large rural community family health team
In case one the occupational therapists along with the interdisciplinary health providers and administrative staff were located in two buildings in the largest regional town, while the physicians worked in distributed clinics across the region. Despite the lack of co-location each key informant reported a strong sense of collaboration and connection. The EMR was the key structure for collaboration and integration of occupational therapy into the Family Health Team; face-to-face interaction with physicians is limited.
Case 2: Small urban community family health team
Case two was a small Family Health Team with four separate sites located in a large urban setting with a culturally diverse patient population. The occupational therapist was located with nursing and other interdisciplinary health providers across the street from one of the main physician sites.
Lack of co-location was described as a key barrier in the integration of occupational therapy. The Family Health Team was planning a new building to house all team members.
Case 3: Large rural family health team, one occupational therapist
Case three was a large rural Family Health Team providing primary care to approximately 45% of the local population. Having only been recently approved as a Family Health Team, the team was largely in the development phase. The Family Health Team had four separate sites. The occupational therapists and other interdisciplinary health providers were located at one site along with the administrative staff. Each site had its own EMR that could not communicate between sites. At the time of the study the occupational therapist did not have access to the EMR. The long-term goal was to move to one accessible EMR system.
Case 4: Urban academic family health team
Case four was an urban academic Family Health Team with two sites; each with a full interprofessional complement of professions. Services were organized by interprofessional care teams, where patients were designated to a team of clinicians. Two full-time occupational therapists worked between the two sites. The Family Health Team was part of the university Department of Family Medicine and therefore had a dual objective of providing primary care services and training family medicine residents, along with an expectation of research.
Cross case analysis
Three main themes and eight subthemes were identified that influenced integration of occupational therapists into the Family Health Teams: understanding of occupational therapy, collaboration, communication and trust. See Figure 1 for visual outline of the themes and subthemes.
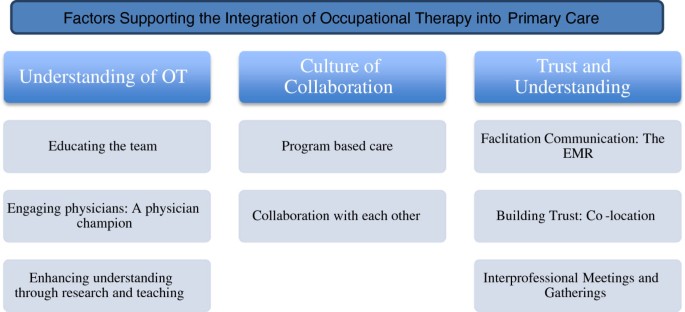
Themes and Subthemes.
1. Understanding occupational therapy
Fundamentally, an understanding of occupational therapy was critical and the tipping point for integration into the team. As referrals originated from team members, a basic understanding of the role of occupational therapy and patients who could benefit were required. Interdisciplinary health care providers and nurses described previous and current working relationships with occupational therapists, which in turn led to an understanding of the occupational therapy role within Family Health Teams.
The other integrated health professionals have been amazing. So I think they have a good idea of what OT is and I think a lot of them have worked with OT in the past (Occupational Therapist) 2P11:33:82
An understanding of and experience with occupational therapy in turn created a level of respect and natural integration into the team.
There’s a very healthy respect among our IHPs [interdisciplinary health providers] for the skill sets that they have and there’s a desire to include one another in the initiatives that they take on (Executive Director) 2P1:14:23
However, physicians had less direct day-to-day contact with occupational therapists, and less familiarity with the role of occupational therapy.
I feel that most family doctors didn’t and still don’t have a great understanding of the OT role (Physician) 4P4:1:6
Ultimately respondents felt that when team members had a good understanding of occupational therapy, referrals were made to the service.
That was the basis of our success here… that people really get what we do (Occupational Therapist). 1P1:93:220
Conversely, less familiarity with the role of occupational therapy was felt to result in an underutilization of services.
It’s underused, because I don’t think everyone knows what the OT can do (Nurse Practitioner) 2P5:5:13
Educating the team
Occupational therapists across all sites used a number of strategies to educate physicians and team members about occupational therapy including formal presentations, educational rounds, ‘meet and greets’, information booths, brochures and information letters. Occupational therapists provided information about the profession, particularly, the services they currently offered within the Family Health Team along with examples of potential services that could be provided. All opportunities were seen as positive and contributing to an increased understanding of occupational therapy.
I’m working on trying to educate the team in what OTs can do (Occupational Therapist) 2P5:5:13
Promoting the role of occupational therapy was a particularly important element during the early integration into the team and a role that needed to be consciously adopted by occupational therapists.
Engaging physicians: a physician champion
Physicians were seen as critical to the integration of occupational therapists as they were a key source of referrals. The identification of a physician lead, or physician liaison for occupational therapy was seen as an important strategy to enhance physician understanding and champion the occupational therapy discipline within the Family Health Team. Information from physician to physician was felt to have greater authority and credibility.
The communication was coming from a physician that they trust and he was saying ‘Use these services’ (Occupational Therapist) 1P1:94:221
A lack of physician engagement regarding the occupational therapy role was seen to significantly influence the integration of the role.
My regret about the occupational therapy program is that we haven’t done a good enough job of engaging the physician group in establishing that program … we’re definitely not utilizing her to the fullest extent that we could in her occupational specialization (Executive Director) 2P1:6:11
Enhancing understanding through research and teaching
Team members at the academic Family Health Team had additional requirements to engage in both research and teaching activities. As a result, site four had a number of unique strategies that served to increase the understanding of occupational therapy and support a deeper integration into the team.
There are two absolutely primary mandates of clinical care and education and then obviously scholarly work … you can’t really separate clinical cases from education in this [Family Health Team]. So our nurses are doing so much of the clinical care and we are reviewing our teaching and the allied health group, including the OT’s, are absolutely woven into that. From co-bookings, to horizontal electives, to the more structured learning opportunities with the rounds, to working with different groups of the learners so family medicine residents and allied health workers sharing the case together. Some of the family residents teach the more junior learner and then going to an allied health person for some input. (Physician) 4P4:26:38
Training was a reciprocal and iterative activity; building an understanding of occupational therapy and supporting collaborative patient care.
Occupational therapists were expected to participate in interprofessional teaching rounds, one-on-one resident training, education clinics and occupational therapy student mentorship. Each activity offered an opportunity for the team to be exposed to the role of occupational therapy and work with the discipline.
One of the really helpful things that [the occupational therapists] did is to take some time at our interprofessional rounds and walk us through their vision in 6 months. Here are the types of cases that are getting referred, and here are success stories of why it was helpful to be involved. Here are some priority areas for us to think about. And that was again, a really nice diplomatic way of increasing our understanding. (Physician) 4P4:11:14
None of the other sites had formal structures in which to provide physician education, nor were they involved in any residency training.
A number of team members were involved in research with occupational therapists at the affiliated University and had been previously exposed to the role of occupational therapy in primary care. This research experience was felt to support the integration of the occupational therapist by offering a deeper understanding of the role.
I think we were better positioned already for a level, a deeper level of understanding of the role of OT and PT in primary care. (Physician) 4P4:3:8
Enhancing understanding through research cultivated opportunities to integrate occupational therapy into clinic programs.
I didn’t know much about chronic pain and [the OT] has been working in chronic pain for over 20 years so I was interested in being part of the research project and she has been mentoring me in that role so we have now created a new [pain] group (Social Worker) 4P2:25:43
2. A culture of collaboration
While an understanding of occupational therapy facilitated referrals to occupational therapists, collaboration was seen as a benchmark of occupational therapy’s integration into Family Health Teams. Each site agreed that building team collaboration was a deliberate and intentional process.
We very deliberately, pretty much, do everything as a team with clinical work. (Physician) 4P4:22:36
Strong collaboration among interdisciplinary health providers was seen across all sites. In some cases assessments and interventions were conducted together with other interdisciplinary health providers.
[Occupational therapist] and I have gone to a couple of home visits together; because the person was appropriate for my services and her services . (Social Worker) 3P9:20:74
As many interdisciplinary health providers were also new to primary care they collaborated to support each other in their mutual integration into the team.
[the interdisciplinary health providers] … that’s my biggest source of support … so a lot of my referrals are actually coming from other allied health (Occupational Therapist) 3P11:33:82
Opportunities to collaborate at the point of care supported the integration of occupational therapy. However across sites there was notably less collaboration between the interdisciplinary health providers and physicians.
The physician group is not engaged strongly enough with the other health providers (Executive Director) 2P1:16:23
Less collaboration with physicians was attributed to a number of factors. First and foremost primary care has traditionally been practiced as a solo enterprise.
[The physicians] have always been the general practitioner that has done everything for their patients (Executive Director) 3P7:41:104
There was a sense that interprofessional collaboration may diminish the physicians’ sense of control.
I am sure there are a lot of physicians that do not like the ball being taken from them (Physician) 1P5:16:53
As physicians could see the benefit of occupational therapy services, opportunities for collaboration would be enhanced.
As physicians refer to the occupational therapist and have comfort level in what they’re getting back, that [occupational therapy] will improve [patient care]. More referrals will come and there will be more of an interaction. (Physician) 3P10:55:22
As the shift to interprofessional teams was relatively new, it was also felt that physicians were not used to having access to so many resources and needed to gain comfort with a team based approach
They’re not used to having this type of resources available to them on a daily basis in their clinics (Executive Director) 3P7:49:118
Program based care
Each site offered a number of health promotion and chronic disease management and prevention programs ranging from mental health, falls prevention, chronic pain and diabetes management. Aligning occupational therapy services within current programs of care provided an opportunity to integrate into the team.
There’s a COPD group that’s held here and I provide some consultation to that group and I’m slowly tying to integrate myself into some other groups we’re going to be starting (Occupational Therapist) 1P1:4:9
Integration into programs occurred in a number of ways. In some cases occupational therapists noted a gap in program offerings, which led to the development of a new program. More frequently, occupational therapists or other team members identified programs that had high volume or wait lists that would benefit from an occupational therapy perspective.
Our program is really busy .. it’s great to have that opportunity to put that person with [the occupational therapist] that specializes and might be able to have the time to do it (Social Worker) 3P9:38:86
The program focus also provided new opportunities to collaborate and engage in program development.
One of our ideas is to have a caregiver stress program … that was going to be a collaboration between [occupational therapist] and myself and the mental health therapist (Social Worker) 3P9:31:76
At two of the sites physicians were aligned with specific programs, which provided a formal opportunity to connect with physicians.
Collaborating with each other
As essential as interprofessional collaboration was in supporting the integration of occupational therapy, the ability to collaborate with occupational therapy colleagues both within and outside of the Family Health Team was also important. Occupational therapists shared resources, engaged in clinical consultations, and provided strategies to each other to support integration into the team.
This whole group of occupational therapists [working in FHT’s] are pioneers in the OT role. So any way we can support one another (Occupational Therapist) 1P3:62:225
Having two occupational therapists at one Family Health Team was seen to facilitate the integration of the role in number of ways. Most importantly it provided professional support and confidence to try new roles and share ideas. Simply having two individuals increased exposure to occupational therapy within the Family Health Team and enhanced the professional profile.
To have each other … I can’t imagine doing this role … as one person (Occupational Therapist) 1P1:27:54
3. Communication and trust
Communication and trust were essential components of collaboration and the integration of occupational therapy, and were supported by a number of strategies including co-location, EMR and formal and informal meetings and gatherings.
Facilitating communication: the electronic medical record
A single and accessible EMR was a critical feature in supporting the integration of occupational therapy into Family Health Teams. The EMR enabled both formal and informal communication with physicians and other team members through the messaging system and patient records. The instant messaging function served as an internal communication system.
I think the EMR allows us to communicate effectively. We can instant message and that piece provides opportunity (Social Worker) 1P2:24:65
The EMR provided a means to collaborate when co-location of team members was not possible, supporting virtual interprofessional teams.
The EMR is fabulous because not only can you communicate back and forth, but everyone can see everyone’s charts. It is like one big family medicine chart. (Physician) 1P5:12:41
The EMR was also seen to support efficient and informed clinical practice.
The OT gets a snapshot of that patient and they’re better equipped to do what they need to do. And to get to the point a lot quicker (Physician) 1P3:40:127
Building trust: co-location
While an integrated EMR provided a foundation for communication, the opportunity for team members to connect face-to-face was pivotal in developing relationships and supporting the integration of occupational therapy. The importance of occupational therapy being located with the entire team cannot be underestimated. Only one of the four cases had a full interprofessional team located in the same building, however two of the other cases had plans to consolidate their clinics. Co-location offered opportunities for occupational therapists to engage in informal communication, have ‘hallway consults’ and be visually present; all of which contributed to understanding the OT role and building of trust.
There are other times where you are not sure if [occupational therapy] would be helpful or not. It is much more relevant to have an [informal] case conversation first and then whatever you end up writing in [the EMR] references the conversation, which is obviously much richer. (Physician ) 3P4:15:22
One site created team rooms where all team members worked in a common desk area, along with common lunch rooms and meeting spaces. When co-location occurred only with other interdisciplinary health providers and nurses, the benefits of communication and understanding were also identified; however as physicians were a key source of referrals their physical presence was viewed as a critical.
Physically we don’t see the [physicians] very often. I think that can spark some reminders, or spark some ideas, as well as is great for relationship building. (Social Worker) 4P9:45:110
Interprofessional meetings and gatherings
Formal meetings provided opportunities for team members to interact, most notably in cases where occupational therapists were off-site from physicians.
Just going to the meeting is an opportunity to talk, see what everyone does (Occupational Therapist) 1P1:66:143
Just as important as meetings, social gatherings supported team building and enabled the team to get to know each other as individuals.
We’ve spent some good networking sessions … you get to know that person and all of a sudden “OK, I’ll trust you with my patient” (Executive Director) 1P3:19:73
Ultimately, the integration of occupational therapy into the primary care teams was grounded in three key factors: trust, understanding, and communication. Meetings and gatherings provided opportunities to facilitate connections and team building.
Integration has been described as one end of the continuum that extends from complete autonomy and independence at one extreme to complete integration of professional services at the other [ 25 ]. In this study, the integration of occupational therapists was observed to range along this continuum and varying both between and within the Family Health Teams. In these cases, occupational therapists were more integrated with the other interdisciplinary health providers such as social workers and pharmacists, than with either nurses or physicians. Vertical and horizontal integration have been used to describe the integration of health services. Horizontal integration refers to the grouping of similar organizations or services, while vertical integration “services a network of organizations that provides or arranges to provide a coordinated continuum of services to a defined community” [ 26 ]. Within the Family Health Teams occupational therapists tended to work closely and collaborate with other allied health professionals in the delivery of health services. Allied health professionals had a common goal of supporting the physicians in the delivery of primary care. While each had different disciplinary perspectives, occupational therapists could be described as being horizontally integrated with their allied health counterparts. Each was remunerated in a similar fashion, worked in close physical proximity, had informal communication structures and provided some degree of collaborative patient care.
In contrast, occupational therapists had relatively little direct contact and few interactions with physicians. The occupational therapy role was seen as supporting the continuum of health services within the Family Health Team and integration could be envisioned as being vertical relative to the physicians. This is congruent with the literature reporting that a key barrier in the implementation of interprofessional teams has been the hierarchical structures within primary care [ 27 – 29 ]. Of note, however is a recent study suggesting that younger cohorts of male physicians are more likely to collaborate with occupational therapists, and other health professionals than older counterparts or younger female physicians [ 30 ]. Occupational therapists at the academic site experienced a high level of integration into the team, including with physicians, nurses and other interdisciplinary health providers. Given the focus on collaboration and teamwork in the training of family medicine practitioners, it makes sense that younger physicians who have had experience with interprofessional collaboration enact this as practicing physicians.
This study also found that the extent of occupational therapists integration into Family Health Teams was influenced by the nature of services provided. Integration was more fully realized within chronic and complex disease programs of care, such as a diabetes or seniors program, than one- time referrals to occupational therapy. This study suggests a plausible explanation for this phenomenon. The more structured programs served to identify and formalize a team of providers and offered an opportunity to develop common patient goals and a shared vision of service delivery. This in turn facilitated communication and the implementation of processes to support the programs, such as meetings and common program outcomes. Russell and colleagues [ 31 ] examined chronic disease management programs and found that organizational features had the greatest influence on patient outcomes. In particular, those clinics with the presence of a nurse practitioner had better outcomes and high-quality chronic disease management care was found most commonly in clinics with an interprofessional team. The success of chronic disease management programs in part contributed to the collaborative nature of the care, highlighting the importance and benefit of integrating professionals within programs of care.
At the same time it is recognized that not all care provided by occupational therapists within primary care teams will be program based. Leutz [ 32 ] described five laws for integration, one of which was “you can integrate all of the services for some of the people, some of the services for all of the people, but you can’t integrate all of the services for all of the people” (p. 83). This may hold true for occupational therapists in the sense that certain elements of their work within the teams may be more individual and consultative in nature.
The literature has described a number of factors that support interprofessional teamwork in primary care [ 21 , 28 , 29 ]. Xyrichis and Lowton [ 21 ] identified both team structures and team processes that support collaboration. As was seen in this study, Family Health Teams with a greater number of structures to support teamwork had occupational therapists that were more fully integrated. Processes that were seen to support the integration of occupational therapist included co-location, a common EMR, formal and informal communication structures and team meetings. Each of these processes naturally facilitated the integration of occupational therapy into the team by building trust, understanding and familiarity. It was the processes and structures, more than the personal characteristics of the occupational therapist that appeared to influence integration. However, the two sites with the greatest supports also had occupational therapists with substantial work experience. Further research is required to explore the relationship between personal characteristics and the integration process. A recent study [ 22 ] examined teamwork within twenty-one Family Health Teams in Ontario, Canada. A survey was used to identify organizational factors contributing to the functioning of an interprofessional primary care team. The study found that culture, leadership and EMR functionality predicted team climate. Each of these elements was also seen to support the integration of occupational therapy in this study.
Studies examining the integration of pharmacists reported some lack of understanding of the role of the pharmacist, but not to the extent found in this current study [ 13 – 15 ]. It is not surprising that the lack of understanding about a profession’s role impedes their integration into the team. The current siloed approach to the training of health care practitioners and practice of health care may be a contributor [ 33 ]. For disciplines new to primary care, there will be a natural learning curve about both the roles of other professionals as well as their own role in a new practice setting. Kolodziejak and colleagues [ 15 ] outlined a step-by-step process to support the integration of pharmacists into established primary care teams. Part of the process of integration included defining the role prior to joining a team and determining early credibility. The current study found a number of intentional strategies were used to integrate occupational therapy within the team, however more formal guidelines to Family Health Teams who have new professionals could further support integration.
The study also found that informal and formal support by occupational therapy colleagues was also helpful in supporting integration. Communities of practice have been shown to support knowledge translation [ 34 , 35 ] and this could be another intentional strategy that is enacted.
Interprofessional education occurs “when two or more professions learn with, from and about each other to improve collaboration and the quality of care ” [ 36 ]. In the case of the academic Family Health Team, the educational processes designed to support physician learning provided a natural opportunity and environment to educate team members of their roles. Without such structures, the occupational therapists at the other sites did not have a forum to provide formal physician education. A growing amount of literature on interprofessional education suggests that experiential based learning is an effective strategy to teach health professionals the competencies of collaborative practice [ 37 , 38 ]. While there are only a small number of academic Family Health Teams, there is much to be learned about the research and teaching activities that can support the integration of new team members.
It must be remembered that this study was limited to four sites. Given the influence of structures and processes on collaboration and integration, it is anticipated that additional sites might have provided further insights into the variety of other assets or constraints to interprofessional integration. Occupational therapy is a new profession within Family Health Teams and the paper focuses on the early integration in the team. Therefore the integration of occupational therapy will continue to evolve and be shaped by individual, team and organizational development. The study was exploratory in nature and while it provides insights into the emerging role of occupational therapy within a primary care context, the results cannot be broadly generalized.
This study builds the foundation for further research. A longitudinal study would provide insights into how health professionals are integrated into teams over time. It would also be of value to understand how integration influences health outcomes and more specifically to use a framework of systems integration in which to understand interprofessional primary care teams. Finally, it would be important to explore how professionals within Family Health Teams were integrated into the broader community services.
Conclusions
With an increased emphasis on interprofessional primary care, new professions will continue to be integrated into primary care teams. Based on the current study the following strategies and structures should be considered to support occupational therapists entering primary care teams.
Occupational therapists entering primary care need to formally include the education of team members in their professional role. Education on the role of occupational therapy and services provided needs to be directed to all team members, with specific focus on physicians.
Occupational therapists need to ensure they gain full access to the EMR to support both informal communication, through the internal messaging features, as well as formal patient documentation and referrals.
Occupational therapy fieldwork placements can provide a mechanism to engage the team in learning about other professions. Student occupational therapists should also be involved in the education of team members.
When possible, occupational therapists should actively participate in educating students from other health disciplines, including offering shadowing opportunities, providing handouts, arranging co-bookings or developing inservices.
Occupational therapists need to actively develop their role in existing interprofessional groups and programs offered within the primary care setting. Working within a structured program provides an opportunity to work closely with team members and can facilitate a deeper understanding of the occupational therapy.
Occupational therapists need to attend networking events, meetings, inservices and social functions to build relationships with team members.
The study adds to the growing body of literature that has identified structures and processes to support interprofessional collaboration in primary healthcare. Exploring the integration of an emerging discipline in primary care underscores the necessity of ensuring team members have an understanding of the roles and scope of each team member. The study also highlights the critical role that communication structures, such as formalized meetings and EMR’s, have in supporting the integration of new professions.
Letts LJ: Optimal positioning of occupational therapy. Can J Occup Ther. 2011, 78: 209-219. 10.2182/cjot.2011.78.4.2.
Article PubMed Google Scholar
Howey M, Angelucci T, Johnston D, Townsend E: Occupation-based program development in primary health care. OT Now. 2003, 11 (3): 4-7.
Google Scholar
Clark F, Azen SP, Zemke R, Jackson J, Carlson M, Mandel D: Occupational therapy for independent-living older adults: A randomized controlled trial. JAMA. 1997, 278: 1321-1326. 10.1001/jama.1997.03550160041036.
Article CAS PubMed Google Scholar
Richardson J, Letts L, Chan D, Stratford P, Hand C, Price D, Hilts L, Coman L, Edwards M, Baptiste S, Law M: Rehabilitation in a primary care setting for persons with chronic illness: A randomized controlled trial. Prim Care Res Devo. 2010, 11: 382-395. 10.1017/S1463423610000113.
Article Google Scholar
Klaiman D: Increasing access to occupational therapy in primary health care. OT Now. 2004, 6 (1): 14-1.
McColl MA, Shortt S, Godwin M, Smith K, Rowe K, O’Brien P, Donnelly C: Models for integrating rehabilitation and primary care: A scoping study. Arch Phys Med Rehab. 2009, 90: 523-531.
Tse S, Penman M, Simms F: Literature review: Occupational therapy and primary health care. NZ J Occup Ther. 2003, 50: 17-23.
Health Canada: First Minister’s Meeting on the Future of Health Care 2004: A 10-year plan to strengthen health care. 2004, http://www.hc-sc.gc.ca/hcs-sss/delivery-prestation/fptcollab/2004-fmm-rpm/index-eng.php ,
Hutchinson B, Levesque JF, Strumpe E, Coyle N: Primary health care in Canada: Systems in motion. MilBank Q. 2011, 89: 256-288. 10.1111/j.1468-0009.2011.00628.x.
Ontario Society of Occupational Therapists: Occupational therapy and Family Health Teams. http://www.osot.on.ca/eng/otinont/familyHealthTeams.asp ,
Belle Brown J, Lewis L, Ellis K, Beckhoff C, Stewart M, Freeman T, Kasperski MJ: Sustaining primary health care teams: What is needed. J Interprof Care. 2010, 24: 463-465. 10.3109/13561820903417608.
Sargeant J, Loney E, Murphy G: Effective interprofessional teams: Contact is not enough to build a team. J Contin Educ Health Prof. 2008, 28: 228-234. 10.1002/chp.189.
Bradley F, Elvey R, Ashcroft DM, Hassell K, Kendall J, Sibbald B, Noyce P: The challenge of integrating community pharmacists into the primary health care team: A case study of local pharmaceutical services (LPS) pilots and interprofessional collaboration. J Interprof Care. 2008, 22: 387-398. 10.1080/13561820802137005.
Dolovich L, Pottie K, Kaczorowski J, Farrell B, Austin Z, Rodriguez C, Gaebel K, Sellors C: Integrating family medicine and pharmacy to advance primay care therapeutics. Clin Pharmacol Ther. 2008, 83: 913-917. 10.1038/clpt.2008.29.
Kolodziejak L, Remillard A, Neubauer S: Integration of a primary healthcare pharmacist. J Interprof Care. 2010, 24: 274-284. 10.3109/13561820903130149.
Drummond D: Commission on the Reform of Ontario’s Public Services: Public Service for Ontarians: A Path to sustainability and excellence. 2012, Toronto, ON: Queen’s Printer for Ontario
Standing Senate Committee on Social Affairs, Science and Technology: Time for Transformative Change: A review of the 2004 Health Accord. 2012
Yin RK: Case Study Research: Design and Methods. 2009, Thousand Oaks California: SAGE Publications Inc, 3
Stake R: The Art of Case Study Research. 1995, Thousand Oaks, California: SAGE Publications Inc
Salminen AL, Harra T, Lautama T: Conducting case study research in occupational therapy. Aus Occup Ther J. 2006, 53: 3-8.
Xyrichis A, Lowton K: What fosters or prevents interprofessional teamworking in primary and community care? A literature review. Int J Nurs Stud. 2008, 45: 140-153. 10.1016/j.ijnurstu.2007.01.015.
Howard M, Brazil K, Akhtar-Danesh N, Agarwal G: Self-reported teamwork in family health team practices in Ontario. Can Fam Phys. 2011, 57 (May): e185-e191.
Krefting L: Rigor in qualitative research: The assessment of trusworthiness. Am J Occup Ther. 1991, 43: 214-222.
Golafshani N: Understanding reliability and validity in qualitative research. Qual Report. 2003, 8: 597-607.
Glendinning C: Breaking down barriers: Integrating health and care services for older people in England. Health Policy. 2003, 65: 139-151. 10.1016/S0168-8510(02)00205-1.
Devers KJ, Shortell SM, Gilles RR, Anderson DA, Mitchell , Erickson K: Implementing organized delivery systems: An integration scorecard. Health Care Manage Rev. 1994, 19 (3): 7-30.
CAS PubMed Google Scholar
Craigie FC, Hobbs RF: Exploring the organizational culture of exemplary community health center practices. Fam Med. 2004, 36: 733-738.
PubMed Google Scholar
Poulton BC, West MA: The determinants of effectiveness in primary health care teams. J Interprof Care. 1999, 13: 7-18. 10.3109/13561829909025531.
Shaw A, De Lusignan S, Rowlands G: Do primary care professionals work as a team: A qualitative study. J of Interprof Care. 2005, 19: 396-405. 10.1080/13561820500053454.
Sarma S, Devlin RA, Thind A, Chu MK: Canadian family physicians’ decision to collaborate: Age, period and cohort effects. Soc Sci Med. 2012, 75: 1811-1819. 10.1016/j.socscimed.2012.07.028.
Russell GM, Dabrouge S, Hogg W, Geneau R, Muldoon L, Tuna M: Managing chronic pain in Ontario primary care: The impact of organizational factors. Ann Fam Med. 2009, 7: 309-318. 10.1370/afm.982.
Article PubMed PubMed Central Google Scholar
Leutz WN: Five laws for integrating medical and social services: Lessons from the United States and the United Kingdom. Milbank Q. 1999, 77: 77-110. 10.1111/1468-0009.00125.
Article CAS PubMed PubMed Central Google Scholar
Pecukonis E, Doyle O, Bliss DL: Reducing barriers to interprofessional training: promoting interprofessional cultural competence. J Interprof Care. 2008, 22: 417-428. 10.1080/13561820802190442.
Barwick MA, Peters J, Boydell K: Getting to update: Do communities of practices support the implementation of evidence-based practice?. J Can Acad Child Adolesc Psych. 2009, 18: 16-29.
Li LC, Grimshaw JM, Nielsen C, Judd M, Coyte PC Graham ID: Use of communities of practice in business and health care sectors: A systematic review. Implement Sci. 2009, 4: 27-10.1186/1748-5908-4-27. http://www.implementationscience.com/content/4/1/27 ,
CAIPE: Defining IPE. http://www.caipe.org.uk/resources/defining-ipe/ ,
Payler J, Meyer E, Humphris D: Pedagogy for IP education – what do we know and how can we evaluate it?. Learn Health Soc Care. 2008, 7: 64-78. 10.1111/j.1473-6861.2008.00175.x.
Sargeant J: Theories to aid understanding and implementation of IP education. J Contin Educ Health Prof. 2009, 29: 178-184. 10.1002/chp.20033.
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-2296/14/60/prepub
Download references
Acknowledgements
We wish to acknowledge the Family Health Teams who participated in the study. We would like to thank Dr. Lyn Shulha for her support and insightful comments on the final drafts of the manuscript. We would also like to thank Kristina Sheridan and Tanya Cerovic for their assistance with transcription and data management. The study was funded by the Primary Healthcare Seed Funding.
Author information
Authors and affiliations.
School of Rehabilitation Therapy, Queen’s University, 31 George Street, Kingston, ON, K7L 3N6, Canada
Catherine Donnelly
Faculty of Education, Queen’s University, 31 George Street, Kingston, ON, K7L 3N6, Canada
Ontario Society of Occupational Therapists, 55 Eglinton Ave. E., Suite 210, Toronto, ON, M4P 1G8, Canada
Christie Brenchley
Wise Elephant Family Health Team, 280 Main Street North, Brampton, ON, L6V 1P6, Canada
Candace Crawford
School of Rehabilitation Science, McMaster University, 1400 Main St. W, Hamilton, ON, L8S 1C7, Canada
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Catherine Donnelly .
Additional information
Competing interests.
The authors declare that they have no competing interests
Authors’ contributions
CD, LL, CB, CC contributed to the design of the study. CD participated in the coordination and acquisition of data. CD, LL, CB contributed to the analyses and interpretation of data. CD participated in the draft of the manuscript and LL, CB, CC provided feedback and approval of the final draft. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Donnelly, C., Brenchley, C., Crawford, C. et al. The integration of occupational therapy into primary care: a multiple case study design. BMC Fam Pract 14 , 60 (2013). https://doi.org/10.1186/1471-2296-14-60
Download citation
Received : 06 February 2013
Accepted : 07 May 2013
Published : 16 May 2013
DOI : https://doi.org/10.1186/1471-2296-14-60
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Inteprofessional primary care
- Collaboration
- Family health teams
- Multiple case study design
- Occupational therapy
- Integration
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

The integration of occupational therapy into primary care: a multiple case study design

2013, BMC Family Practice
Related Papers
The Open Journal of Occupational Therapy
Wen-Pin Chang
Primary Health Care Research & Development
Rachelle Ashcroft
Aim: The aim of the study was to describe practices that support collaboration in interprofessional primary health care teams, and identify performance indicators perceived to measure the impact of this collaboration from the perspective of interprofessional health providers. Background: Despite the surge of interprofessional primary health care models implemented across Canada, there is little evidence as to whether or not the intended outcomes of primary health care teams have been achieved. Part of the challenge is determining the most appropriate measures that can demonstrate the value of collaborative care. To date, little remains known about performance measurement from the providers contributing to the collaborative care process in interprofessional primary care teams. Having providers from a range of disciplinary backgrounds assist in the development of performance measures can help identify measures most relevant to demonstrate the value of collaborative care on the intende...
BMC Family Practice
Carola Döpp
Background: Interprofessional primary care (IPC) teams provide comprehensive and coordinated care and are ideally equipped to support those populations most at risk of adverse health outcomes during the COVID-19 pandemic, including older adults, and patients with chronic physical and mental health conditions. There has been little focus on the experiences of healthcare teams and no studies have examined IPC practice during the early phase of the COVID-19 pandemic. The objective of the study was to describe the state of interprofessional health provider practice within IPC teams during the COVID-19 pandemic. Methods: Observational cross-sectional design. A web-based survey was deployed to IPC providers working in team-based primary care clinics in the province of Ontario, Canada. The survey included 26 close-ended and six open-ended questions. Close-ended questions were analyzed using descriptive statistics. Content analysis was used to analyze the open-ended questions.
Deborah Marshall
Renee Misfeldt
Health and Interprofessional Practice
Karen Slonim
Mary Stoykov
Lori Letts , Ainsley Moore
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Revues modernistes, revues engagées
Douglas B McBride
Journal of multidisciplinary healthcare
Victoria Suen
Syed Aljunid
Scott Reeves
Catriona Kennedy
Mathematica Policy Research Reports
Angela Gerolamo
Implementation Science
Carol Cancelliere
Scott Reeves , Kathleen (Kate) Rice
British Journal of Occupational Therapy
Lynette Mackenzie
Karen Schouten
Pauline O'Brien, RP
Family Practice
Valeria Herskovic , Cecilia Saint-Pierre
Sinead Dufour
Joyce Halliday , Rod Sheaff , Stephen Peckham , Sheena Asthana
International Journal of Chronic Obstructive Pulmonary Disease
Marie-pascale Pomey
BMC Health Services Research
Health Informatics Journal
Josephine McMurray
Edel Tierney
Kimberly Poong
BMC Complementary and Alternative Medicine
Stacie Salsbury
Journal of Multidisciplinary Healthcare
dilani nanayakkara
Rural and Remote Health
Helen Brown
Journal of allied health
Mohammed Nadar
Healthcare Quarterly
Siegrid Deutschlander
Joanne Goldman
Marisa Birkmeier
International Journal of Language & Communication Disorders
American Journal of Occupational Therapy
Penelope Cleveland
mukhlis syukur
Maureen Nash
Mona Morsy , Anita Fisher , Tracey Chambers , Laurie Kennedy , Sinead Dufour , Sue Bookey-Bassett , Jenny Ploeg
Occupational Therapy International
Wesam Darawsheh
Proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems - CHI '15
Lee Sanders
Physical & Occupational Therapy In Pediatrics
Atefeh Esfandiari
Yumna Abdelrahman
Ruta Valaitis
International Congress on Applications of Lasers & Electro-Optics
Ehsan Foroozmehr
Kathleen Mathieson
Irma Ruslina Defi
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Case Studies for Contemporary OT Practice
Already purchased? Please sign in to view.
Do you need to re-use or reproduce this work?
current document all documents
Advanced search
Table of Contents
- Table of Contents v 6
Remember login
Enable two-factor authentication codes.
Forgot password
Please log in to view your account information. Don't have any account? You can register for one now.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search

Workplace-based rehabilitation with garment workers: A multiple case study
Affiliation.
- 1 Division of Occupational Therapy, Department of Health and Rehabilitation Sciences, Stellenbosch University, Cape Town, South Africa.
- PMID: 35527606
- DOI: 10.3233/WOR-210540
Background: Garment workers are at risk of developing work-related upper limb disorders (WRULD) due to the highly repetitive nature of their work. Workplace-based rehabilitation (WBR) facilitates improvement in work performance by providing intervention at the worker's place of work.
Objective: This study aims to determine the documented outcomes of workplace-based occupational therapy rehabilitation of garment workers with upper limb conditions.
Methods: A multiple case study design was used through a retrospective record review. All garment workers with upper limb conditions who were treated at a student occupational therapy practice in Cape Town, South Africa, with pre- and post-intervention outcome assessment, were included in the study (n = 7). Data were extracted from occupational therapy and medical files.
Results: 70% of the cases (n = 5) improved after WBR while 30% of cases showed no improvement or deterioration. Participants received 3- 5 individual WBR sessions of approximately 30 minutes each, over a period of 4 to 6 weeks. Interventions included workstation adaptations, job rotation, psychoeducation, work task modification, assistive technology and exercise programmes. Outcome measures most commonly used were the RULA, DASH, Boston Carpal Tunnel Questionnaire and pain intensity using the VAS.
Conclusion: Workplace-based occupational therapy can be effective at improving upper limb function, pain and ergonomic risk amongst garment workers with upper limb conditions.
Keywords: Occupational therapy; return to work; sewing machine operators; textile workers; upper limb.
PubMed Disclaimer
Similar articles
- Differences in ergonomic and workstation factors between computer office workers with and without reported musculoskeletal pain. Rodrigues MS, Leite RDV, Lelis CM, Chaves TC. Rodrigues MS, et al. Work. 2017;57(4):563-572. doi: 10.3233/WOR-172582. Work. 2017. PMID: 28826196
- Workplace management of upper limb disorders: a systematic review. Dick FD, Graveling RA, Munro W, Walker-Bone K; Guideline Development Group. Dick FD, et al. Occup Med (Lond). 2011 Jan;61(1):19-25. doi: 10.1093/occmed/kqq174. Epub 2010 Dec 2. Occup Med (Lond). 2011. PMID: 21127200 Review.
- Presentation and response of patients with upper extremity repetitive use syndrome to a multidisciplinary rehabilitation program: a retrospective review of 24 cases. Barthel HR, Miller LS, Deardorff WW, Portenier R. Barthel HR, et al. J Hand Ther. 1998 Jul-Sep;11(3):191-9. doi: 10.1016/s0894-1130(98)80037-9. J Hand Ther. 1998. PMID: 9730095
- Ergonomics and efficient workplace design for hand-sewn footwear artisans in Kolhapur, India. Jadhav GS, Arunachalam M, Salve UR. Jadhav GS, et al. Work. 2020;66(4):849-860. doi: 10.3233/WOR-203230. Work. 2020. PMID: 32831216
- Prevention of low back pain: basic ergonomics in the workplace and the clinic. Halpern M. Halpern M. Baillieres Clin Rheumatol. 1992 Oct;6(3):705-30. doi: 10.1016/s0950-3579(05)80134-7. Baillieres Clin Rheumatol. 1992. PMID: 1477898 Review.
- Search in MeSH
LinkOut - more resources
Full text sources.
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

Analysis of University Students’ Mental Health from the Perspective of Occupational Harmony
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- ORCID record for Yijun Liu
- ORCID record for Jin Xing
- For correspondence: [email protected]
- Info/History
- Supplementary material
- Preview PDF
Background Mental health problems are common among university students. Based on the Model of Occupational Harmony, we investigated the relationship between occupational engagement and mental health among Chinese university students.
Methods A mixed methods approach was adopted. A total of 734 Chinese university students responded to online questionnaires: a socio-demographic questionnaire, the Depression Anxiety Stress Scale, the WHOQOL-BREF, and a self-designed Occupational Harmony Questionnaire. Individual interviews with 11 university students and a focus group of four students provided qualitative data.
Results Anxiety, depression, and stress were reported by 11.9%, 9.4%, and 2.9% of the participants, respectively. The level of occupational harmony was negatively correlated with depression, anxiety, and stress (p<.001). The DASS-21 score was significantly different among students who spent different amounts of time on the following activities: exercise, sleep, rest, reflective and consulting activities, study, work, and leisure and entertainment (P<.05). In the context of the COVID-19 pandemic, the key occupational factors contributing to university students’ mental health problems included excessive mental engagement and insufficient physical engagement, excessive active engagement and insufficient quiet engagement, insufficient social engagement, excessive or insufficient Gong (productive) engagement, and insufficient De (virtuous) engagement, Zhi (rational) engagement, and Kang (health maintenance) engagement, lack of coherence within the family, school, social systems, as well as inadequate schedule planning and time management.
Conclusions Occupational disharmony is related to university students’ mental health problems. Occupational therapy can promote university students’ mental well-being by enhancing occupational harmony.
Competing Interest Statement
The authors have declared no competing interest.
Funding Statement
National High Level Hospital Clinical Research Funding (Youth Clinical Research Project of Peking University First Hospital)2024YC10
Author Declarations
I confirm all relevant ethical guidelines have been followed, and any necessary IRB and/or ethics committee approvals have been obtained.
The details of the IRB/oversight body that provided approval or exemption for the research described are given below:
Biomedical Research Ethics Committee of Peking University First Hospital
I confirm that all necessary patient/participant consent has been obtained and the appropriate institutional forms have been archived, and that any patient/participant/sample identifiers included were not known to anyone (e.g., hospital staff, patients or participants themselves) outside the research group so cannot be used to identify individuals.
I understand that all clinical trials and any other prospective interventional studies must be registered with an ICMJE-approved registry, such as ClinicalTrials.gov. I confirm that any such study reported in the manuscript has been registered and the trial registration ID is provided (note: if posting a prospective study registered retrospectively, please provide a statement in the trial ID field explaining why the study was not registered in advance).
I have followed all appropriate research reporting guidelines, such as any relevant EQUATOR Network research reporting checklist(s) and other pertinent material, if applicable.
We have no conflicts of interest to disclose. This article is based on the unpublished doctoral dissertation completed by YL. The data used to support the findings of this study are included within the article and supporting information files.
YL thanks Dr. Zhen-Su She for his guidance throughout this work; Dr. Zhen Huang and Dr. Rongli Wang for their mentorship; Dr. Shuna Song, Dr. Rong Li, Dr. Lei Zhang, and her parents for their encouragement and support.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
View the discussion thread.
Supplementary Material
Thank you for your interest in spreading the word about medRxiv.
NOTE: Your email address is requested solely to identify you as the sender of this article.

Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager
- Tweet Widget
- Facebook Like
- Google Plus One
Subject Area
- Psychiatry and Clinical Psychology
- Addiction Medicine (342)
- Allergy and Immunology (665)
- Anesthesia (180)
- Cardiovascular Medicine (2625)
- Dentistry and Oral Medicine (314)
- Dermatology (222)
- Emergency Medicine (397)
- Endocrinology (including Diabetes Mellitus and Metabolic Disease) (930)
- Epidemiology (12175)
- Forensic Medicine (10)
- Gastroenterology (756)
- Genetic and Genomic Medicine (4064)
- Geriatric Medicine (385)
- Health Economics (676)
- Health Informatics (2625)
- Health Policy (997)
- Health Systems and Quality Improvement (979)
- Hematology (360)
- HIV/AIDS (845)
- Infectious Diseases (except HIV/AIDS) (13659)
- Intensive Care and Critical Care Medicine (790)
- Medical Education (398)
- Medical Ethics (109)
- Nephrology (430)
- Neurology (3832)
- Nursing (209)
- Nutrition (570)
- Obstetrics and Gynecology (734)
- Occupational and Environmental Health (690)
- Oncology (2008)
- Ophthalmology (581)
- Orthopedics (238)
- Otolaryngology (304)
- Pain Medicine (250)
- Palliative Medicine (73)
- Pathology (471)
- Pediatrics (1107)
- Pharmacology and Therapeutics (459)
- Primary Care Research (447)
- Psychiatry and Clinical Psychology (3400)
- Public and Global Health (6499)
- Radiology and Imaging (1390)
- Rehabilitation Medicine and Physical Therapy (806)
- Respiratory Medicine (869)
- Rheumatology (400)
- Sexual and Reproductive Health (407)
- Sports Medicine (338)
- Surgery (441)
- Toxicology (52)
- Transplantation (185)
- Urology (165)
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals
You are here
- Online First
- Multiple metal exposures associate with higher amyotrophic lateral sclerosis risk and mortality independent of genetic risk and correlate to self-reported exposures: a case-control study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0009-0009-7966-1322 Dae-Gyu Jang 1 , 2 ,
- John F Dou 3 ,
- http://orcid.org/0000-0001-6952-3326 Emily J Koubek 1 , 2 ,
- Samuel Teener 1 , 2 ,
- Lili Zhou 4 ,
- Kelly M Bakulski 3 ,
- Bhramar Mukherjee 5 ,
- http://orcid.org/0000-0001-9894-5325 Stuart A Batterman 6 ,
- http://orcid.org/0000-0002-9162-2694 Eva L Feldman 1 , 2 ,
- http://orcid.org/0000-0001-8780-6637 Stephen A Goutman 1 , 2
- 1 Department of Neurology , University of Michigan , Ann Arbor , Michigan , USA
- 2 NeuroNetwork for Emerging Therapies , University of Michigan , Ann Arbor , Michigan , USA
- 3 Department of Epidemiology , University of Michigan , Ann Arbor , Michigan , USA
- 4 Department of Biostatistics , Corewell Health , Royal Oak , Michigan , USA
- 5 Department of Biostatistics , University of Michigan , Ann Arbor , Michigan , USA
- 6 Department of Environmental Health Sciences , University of Michigan , Ann Arbor , Michigan , USA
- Correspondence to Dr Stephen A Goutman; sgoutman{at}med.umich.edu
Background The pathogenesis of amyotrophic lateral sclerosis (ALS) involves both genetic and environmental factors. This study investigates associations between metal measures in plasma and urine, ALS risk and survival and exposure sources.
Methods Participants with and without ALS from Michigan provided plasma and urine samples for metal measurement via inductively coupled plasma mass spectrometry. ORs and HRs for each metal were computed using risk and survival models. Environmental risk scores (ERS) were created to evaluate the association between exposure mixtures and ALS risk and survival and exposure source. ALS (ALS-PGS) and metal (metal-PGS) polygenic risk scores were constructed from an independent genome-wide association study and relevant literature-selected single-nucleotide polymorphisms.
Results Plasma and urine samples from 454 ALS and 294 control participants were analysed. Elevated levels of individual metals, including copper, selenium and zinc, significantly associated with ALS risk and survival. ERS representing metal mixtures strongly associated with ALS risk (plasma, OR=2.95, CI=2.38–3.62, p<0.001; urine, OR=3.10, CI=2.43–3.97, p<0.001) and poorer ALS survival (plasma, HR=1.37, CI=1.20–1.58, p<0.001; urine, HR=1.44, CI=1.23–1.67, p<0.001). Addition of the ALS-PGS or metal-PGS did not alter the significance of metals with ALS risk and survival. Occupations with high potential of metal exposure associated with elevated ERS. Additionally, occupational and non-occupational metal exposures were associated with measured plasma and urine metals.
Conclusion Metals in plasma and urine associated with increased ALS risk and reduced survival, independent of genetic risk, and correlated with occupational and non-occupational metal exposures. These data underscore the significance of metal exposure in ALS risk and progression.
- EPIDEMIOLOGY
Data availability statement
Data are available upon reasonable request.
https://doi.org/10.1136/jnnp-2024-333978
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Contributors D-GJ, JFD, LZ, KMB, BM, SB, ELF and SAG conceived and designed the study. ST and SAG contributed to the acquisition of the data. D-GJ, JD and KMB performed the statistical analyses. D-GJ, EK and SAG interpreted the data, drafted the text and prepared the figures. All authors critically reviewed and approved the final version of the manuscript. SAG is the guarantor of the study.
Funding Funding was provided by the National Institute of Neurological Disorders and Stroke (NINDS) (R01NS127188); National Institute of Environmental Health Sciences (NIEHS) (K23ES027221, R01ES030049); Centers for Disease Control and Prevention (R01TS000344); ALS Association (20-IIA-532, 20-PP-661); NeuroNetwork for Emerging Therapies; Peter R. Clark Fund for ALS Research; Robert and Katherine Jacobs Environmental Health Initiative; Richard Stravitz Foundation; Coleman Therapeutic Discovery Fund; Scott L. Pranger ALS Clinic Fund; the Dr. Randall W. Whitcomb Fund for ALS Genetics; University of Michigan. Metals analysis was carried out at the Dartmouth Trace Element Core Facility, which is supported by Dartmouth Cancer Center with NCI Cancer Center Support Grant 5P30 CA023108.
Competing interests ELF: Listed as inventors on a patent, Issue number US10660895, held by University of Michigan titled 'Methods for Treating Amyotrophic Lateral Sclerosis' that targets immune pathways for use in ALS therapeutics. SAG: Listed as inventors on a patent, Issue number US10660895, held by University of Michigan titled 'Methods for Treating Amyotrophic Lateral Sclerosis' that targets immune pathways for use in ALS therapeutics. Scientific consulting for Evidera.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Occupational Therapy Interventions in Adults with Multiple Sclerosis or Amyotrophic Lateral Sclerosis: A Scoping Review
Luis de-bernardi-ojuel.
1 Department of Public Health, History of Medicine and Gynecology, University Miguel Hernández, 03550 Alicante, Spain; moc.liamg@leujoidranrebedsiul (L.D.-B.-O.); se.hmu@ilonam (M.G.-d.-l.-H.)
Laura Torres-Collado
2 Spanish Consortium for Research on Epidemiology and Public Health (CIBERESP), 28029 Madrid, Spain
3 Alicante Institute for Health and Biomedical Research, ISABIAL-UMH, 03010 Alicante, Spain
Manuela García-de-la-Hera
Associated data.
All data is presented in this article. Researchers can contact authors regarding any request about the data.
This scoping review aims to describe occupational therapy interventions carried out with multiple sclerosis (MS) and amyotrophic lateral sclerosis (ALS) patients in occupational therapy. A peer review of the literature was conducted in different databases: Pubmed, Scopus, Web of Science and Embase, and in some occupational therapy journals. A search of the literature published was carried out before December 2019. The inclusion criteria were as follows: (1) articles evaluating the intervention of occupational therapy in MS or ALS including experimental, randomized, nonrandomized and exploratory studies; (2) written in English or Spanish; (3) adult population (over 18 years old). The initial search identified 836 articles of which we included 32 divided into four areas of intervention: fatigue-targeted interventions, cognitive interventions, physical interventions and others. Only 16 studies were carried out exclusively by occupational therapists. Most occupational therapy interventions are aimed at fatigue and physical rehabilitation. The majority of the studies in our review included MS patients, with little representation from the ALS population. These interventions have shown an improvement in perceived fatigue, manual dexterity, falls prevention and improvement in cognitive aspects such as memory, communication, depression and quality of life in the MS and ALS populations.
1. Introduction
Multiple sclerosis (MS) and amyotrophic lateral sclerosis (ALS) are neurodegenerative diseases of the nervous system [ 1 , 2 ]. These diseases have a medium to high prevalence, but recently published epidemiological studies have shown an increasing incidence and prevalence of MS and ALS in different populations worldwide [ 3 , 4 , 5 ]. Globally, in the case of MS, the incidence is 2.5 per 100,000 inhabitants, while in ALS it is between 0.6 and 3.8 per 100,000 inhabitants, although the age of onset is later than in MS [ 3 , 6 ]. Though the origin of the diseases is unknown, previous studies have ruled out risk factors such as geographical latitude or ethnicity [ 7 ], while other studies suggest that having a family member with these diseases can increase the risk of developing them [ 8 ]. However, the mechanisms and causes for their development are not completely understood.
These diseases affect not only quality of life but also physical and cognitive aspects, increasing fatigue and the probability of suffering from depression [ 9 ]. They can include multiple symptoms such as muscle stiffness, paralysis of the lower and upper limbs, sensory dysfunction, visual problems, ataxia, dysarthria or dysphagia [ 10 ] as well as cognitive impairment and psychological problems in the affected persons [ 2 , 11 , 12 ]. These diseases have a multidimensional impact on a person´s life, and their symptoms imply a significant loss of autonomy which greatly affects their occupational performance [ 11 ].
The treatment of these diseases is carried out by multidisciplinary teams [ 11 , 13 ] and it can be pharmacological [ 14 ] and/or nonpharmacological. In nonpharmacological treatment, there are specific interventions aimed at physical rehabilitation such as electro-stimulation or Proprioceptive Neuromuscular Facilitation (PNF) [ 15 ]; there are also interventions to maintain daily life skills and others aimed at psychological or cognitive rehabilitation with the participation of occupational therapist [ 11 , 13 ]. Regarding cognitive intervention, Lincoln et al., carried out a comparative study based on attention and memory which resulted in an improvement in memory and lifestyle in the experimental group compared to the control group [ 16 ].
Some previous occupational therapy studies have proposed psychosocial promotion interventions [ 17 , 18 ] such as the Community Reintegration for Socially Isolated Patients (CRISP) occupation-based intervention, which used education and self-management strategies in MS patients, performing socializing and recreation activities to improve self-efficacy and to reduce perceptions of loneliness [ 18 ]. Other studies have proposed cognitive rehabilitation interventions to maintain everyday tasks [ 19 ], meal preparation and finance management [ 20 ]. Finally, it should be pointed out that the majority of the studies led by occupational therapist in the treatment of MS were based on Packer and colleagues’ fatigue management intervention. These studies were carried out for both inpatients [ 21 ] and outpatients [ 22 ] and they all sought to maintain or improve the patients´ occupational performance and quality of life, and to improve muscle strength, energy levels as well as other more cognitive aspects [ 11 ].
MS and ALS have a significant impact on people´s activity and participation [ 11 , 12 ]. Recent reviews showed that occupational therapy could improve occupational performance and other outcomes in MS and ALS populations [ 23 , 24 ]. Nevertheless, these reviews focused on the effectiveness of occupational therapy intervention and contained little information about the activities performed and the role of occupational therapists in the intervention. In this sense, several key gaps in the literature impair a complete understanding of how all previously published interventions in MS and ALS with the participation of occupational therapists, were carried out. We would like to underline that this scoping review provides occupational therapists with tools to perform evidence-based interventions, due to an updated summary of previous evidence that exists on MS and ALS interventions. Thus, we aim to describe those interventions carried out with MS and ALS patients in occupational therapy. In particular, we want to answer the following question: Which interventions are performed from occupational therapy in adult people with MS or ALS?
2. Materials and Methods
A search of the literature published before December 2019 was undertaken by two independent reviewers following the recommendations of the Cochrane Manual [ 25 ], the Joanna Briggs Institute [ 26 ] and PRISMA Extension for Scoping Reviews (PRISMA-ScR) [ 27 ]. The same strategy and key words were used in the different bases: “occupational therapy” and “intervention” and “sclerosis” ( Table 1 ).
Database and search strategy.
| Database | Strategy |
|---|---|
| Pubmed | “occupational therapy” [All Fields] AND (“methods” [MeSH Terms] OR “methods” [All Fields] OR “intervention” [All Fields]) AND “sclerosis” [All Fields] |
| Scopus | TITLE-ABS-KEY (“occupational therapy” AND intervention AND “sclerosis”) |
| Embase | (‘occupational therapy’/exp OR ‘occupational therapy’) AND (‘intervention’/exp OR intervention) AND (‘sclerosis’/exp OR sclerosis) |
| Web of Science | (“occupational therapy” AND intervention AND sclerosis) |
| Teseo | (“occupational therapy” AND intervention AND sclerosis) |
| Journal of Occupational Rehabilitation | ‘“occupational therapy” AND intervention AND sclerosis’ |
| Physical & Occupational Therapy In Pediatrics | [All: “occupational therapy”] AND [All: intervention] AND [All: sclerosis] AND [in Journal: Physical & Occupational Therapy In Pediatrics] |
| American Journal of Occupational Therapy | “occupational therapy” AND intervention AND sclerosis |
| Occupation, Participation and Health | [All “occupational therapy”] AND [All intervention] AND [All sclerosis] |
We searched the literature in 4 databases: Pubmed, Scopus, Web of Science and Embase, and in first-quartile Occupational Therapy scientific journals according to Scimago journal rank in 2018 (American Journal of Occupational Therapy, Journal of Occupational Rehabilitation, Physical & Occupational Therapy in Pediatrics and OTJR: Occupation, Participation and Health). In addition, we performed a search in the grey literature in TESEO to identify possible unpublished studies.
The inclusion criteria were as follows: (1) articles evaluating the intervention of occupational therapy in MS or ALS including experimental, randomized, nonrandomized and exploratory studies; (2) written in English or Spanish; (3) adult population (over 18 years old). We excluded the following: (1) qualitative studies; (2) studies with no abstract, no full text or not available.
Study selection and data extraction of the information were carried out independently. We migrated the results from the databases to a Microsoft Excel spreadsheet where inclusion and exclusion decisions were recorded. The two reviewers (LB and LT) independently selected articles based on the selection criteria. Any disagreement between them regarding possible inclusion/exclusion criteria was resolved by a third reviewer (MG). LB and LT only had discrepancies regarding the inclusion of one article, and with the intervention of a third reviewer we decided to exclude it.
The search strategies identified a total of 836 articles and, after conducting the peer review, 58 articles were selected for their retrieval and evaluation of the full text. We excluded 26 articles, as they did not fulfil the inclusion criteria, leaving 32 articles for data analysis and extraction. The flow chart is shown in Figure 1 .

Flowchart of the study selection process.
The 32 selected studies were conducted in different countries: in USA ( n = 12), Belgium ( n = 4), Netherlands ( n = 3), Switzerland ( n = 3), Spain ( n = 2), Italy ( n = 2), and the remaining 6 studies were conducted in Cuba, Ireland, United Kingdom, Israel, Iran and Austria. A total of 29 studies were carried out in MS patients and only three studies were carried out in ALS patients. A total of 16 studies were led exclusively by occupational therapists and the remaining studies were carried out by multidisciplinary teams, including neurologists, neuropsychologists, social workers or experts in certain fields such as assisted technology or mathematics.
The main limitations reported by included studies were small sample size, lack of long-term evaluation of the intervention, lack of randomization and low generalizability of the results. Table 2 presents the characteristics and information of the included studies: author, year, country where study was conducted, objective of study, sample, intervention, standardized proof used, main results and conclusions of study following Cochrane Manual recommendations [ 25 ].
Main characteristics of the studies included in the review.
| Authors, Year, Country | Objective | Sample ( ), Disease | Intervention | Results | Conclusions |
|---|---|---|---|---|---|
| Eyssen et al. [ ], 2013, Netherlands | To evaluate the effectiveness of a client-centred occupational therapy. | 269, MS | Client-centred occupational therapy | The IG results were not significant and in the second measuring results were negative. | There was no improvement in disability, participation and autonomy in IG. |
| Eyssen et al. [ ], 2014, Netherlands | To check whether client-centred practice spends more time on assessment than on intervention. | 269, MS | Client-centred occupational therapy | The results showed a significant increase in time dedication on the diagnostic process in the IG. | The client-centred practice devotes too much time to the evaluation process with no improvements. |
| Block et al. [ ], 2009, United States | To evaluate the effectiveness of the development of capacities and the health promotion in self-efficacy and ability to achieve objectives. | 35, MS | Health promotion in self-efficacy and empowerment | The results showed significant improvements in self-efficacy and ability to achieve objectives. | The program could took action in multiple areas of intrapersonal, interpersonal, and behavioral functioning. |
| Raglio et al. [ ], 2016, Italy | To evaluate the effectiveness of a music therapy and its influence on anxiety, depression or QoL. | 30, ALS | Music therapy | There were only improvements in Mc Gill Quality of life Questionnaire. | The music therapy program showed an improvement in the QoL. |
| Reilly y Hynes. [ ], 2018, Ireland | To evaluate the efectiveness of an occupation-based cognitive program in improving daily life and cognitive decline. | 12, MS | Cognitive intervention (CI) for managing employment and daily life. | There were significant improvements in all areas. | CI is considered the most appropriate intervention. It can be more effective in newly diagnosed people. |
| Chiaravalloti et al. [ ], 2018, United States | To examine the efectiveness of a SPT. | 21, MS | Cognitive intervention in SPT. | The group that received SPT obtained better results than the CG in processing speed, learning and memory, and performance. | Results provide support of SPT in treating processing speed deficits in persons with MS. |
| Goverover et al. [ ], 2017, United States | To examine the effectiveness of a self-generated program of memory and learning strategies. | 35, MS | Cognitive intervention to improve memory and learning | The IG improved learning, memory, self-regulation, metacognition, depression, functional status, and QoL. | Results provides evidence that the intervention improves memory and affective symptomatology. |
| Schettini et al. [ ], 2015, Italy | To evaluate the feasibility and usability of an assistive technology prototype for communication. | 8, ALS | Cognitive intervention in usability of an assistive technology prototype for communication and home control | There were no significant differences between the different measures. | The study shows the feasibility and usability of assistive technology prototype. |
| Gentry. [ ], 2008, United States | To evaluate the effectiveness of a PDA training program, as the assistive technology. | 21, MS | Cognitive intervention with de use of PDAs to improve occupational performance. | Functional performance increased significantly with PDA use. | PDA still work as a compensatory measure for their deficit in executive functions, but it does not improve memory. |
| Shevil et al. [ ], 2009, Israel-United States | To increase knowledge of cognitive impairments, increase levels of self-efficacy and increase use of management strategies. | 35, MS | Cognitive intervention with a program (Mind over Matter) for the knowledge and management of the cognitive deficits. | Participants significantly increased knowledge of cognitive impairments and levels of self-efficacy in their ability to manage cognitive difficulties. | The results support benefits of self-management cognitive perspective to improve cognitive symptoms. |
| Gómez-Fernández et al. [ ], 2001, Cuba | To examine the effect of multifactorial treatment in health. | 6, ALS | Multifactorial physical intervention with intensive rehabilitation programme. | People improved significantly on forced vital capacity and Functional Rating Scales. | Multifactorial rehabilitation works well for the health and survival. |
| Yang et al. [ ], 2019, United States | To explore if patients can adapt to imbalances after a program of training in falls on a treadmill. | 13, MS | Physical intervention to improve stability and falls prevention. | There was a significant reduction in falls and significant improvements in stability and position. | With this training, people with MS may be able to improve their postural adjustments to prevent falls. |
| Kamm et al. [ ], 2014, Switzerland | To evaluate the effectiveness of home-based program to improve manual dextery. | 39, MS | Physical intervention with manual dextery training. | People improved significantly manual dextery and no significant differences in strength straining | Home manual dextery training improved fine mobility in relation with activities of daily living. |
| Lamers et al. [ ], 2019, Belgium | To evaluate the effectiveness of a task-oriented upper limb program. | 20, MS | Physycal intervention with task-oriented upper limb training by individualizing the intensity of training. | There were significant improvements of Action research arm test, Manual Ability Measure-36. | All participants performed the task-oriented training at their individualized intensity without any adverse effects. |
| Finlayson et al. [ ], 2009, United States | To evaluate “Safe at Home BAASE” program for the management of falls risk. | 30, MS | Physical intervention with the “Safe at Home BAASE” program. | Significant improvements in knowledge, prevention and manage of falls risk with 5:6 sessions. | The program has potential to improve knowledge, skills and behavior associated with reduced personal fall risk. |
| Ortiz et al. [ ], 2013, Spain | To examine postural control and balance with a virtual reality telerehabilitation program. | 50, MS | Physical intervention with a telerrehabilitation program to improve balance and postural control. | Significant improvement in balance, visual preference, the contribution of vestibular information, mean response time and Tinetti test yielded. | The rehabilitation program with virtual reality could be an alternative to standard rehabilitation programmes. |
| Waliño-Paniagua et al. [ ], 2019, Spain | To compare the conventional occupational therapy treatment by virtual reality in manual dexterity training. | 16, MS | Physical intervention with virtual reality training in manual dexterity. | Program showed no significant differences in manual dexterity. Improvements were found in precision, execution times, and the efficiency of functional tasks. | This therapy with virtual reality can be complementary to conventional intervention. |
| Bovend´Eerdt et al. [ ], 2010, United Kingdom | To evaluate the effectiveness of a motor imagery program compared with OT. | 30, MS | Physical intervention with a motor imagery program. | Compliance with advised treatment was poor in 85% of the therapists and in 72% of the patients. | Therapist and patient compliance was low, restricting the conclusions of the effectiveness of the imagery program |
| Kalron et al. [ ], 2013, Israel | To evaluate the effectiveness of a sensory home-based hand re-education and manual dextery program. | 18, MS | Physical intervention with a sensory hand re-education and manual dextery program. | There were significant improvements in the IG on nine-hole peg test and functional dexterity test. | Sensory re-education training at an early stage of the disease can slow the progression of manual dexterity deterioration. |
| Bansi et al. [ ], 2013, Switzerland | To investigate the impact of endurance training in health-related quality of life and fatigue | 60, MS | Physical intervention with endurance training with cycle-ergometer/aquatic-bike on QoL and fatigue. | Endurance training affects QoL and fatigue. Cardiorespiratory fitness and short-term TH2 were associated with better QoL. | Endurance training impacts on QoL and fatigue independently of the type of training (cycle-ergometer or aquatic-bike). |
| Vanage et al. [ ], 2003, United States | To evaluate the effectiveness of an energy conservation program on fatigue. | 37, MS | Energy conservation program | Fatigue was and physical, cognitive, and psychosocial measures were improved. | The program was effective and reduced levels of fatigue in people with moderate-severe MS. |
| Rietberg et al. [ ], 2014, Netherlands | To evaluate a multidisciplinary rehabilitation program for chronic fatigue compared to a nursing consultation program. | 48, MS | Multidisciplinary fatigue intervention | There were no significant differences in most fatigue measures. | Multidisciplinary rehabilitation was not more effective in reducing self-reported fatigue compared to nurse consultation. |
| Mathiowetz et al. [ ], 2001, United States | To evaluate the efectiveness of an energy conservation program for its impact on fatigue, self-efficacy and quality of life. | 54, MS | Energy conservation program | Participants reported significantly less fatigue impact, increased self-efficacy, and improved quality of life. | The energy conservation program is effective in improving fatigue. |
| Ghahari et al. [ ], 2009, Iran | To evaluate the effectivenes of a fatigue self-management program. | 23, MS | Fatigue intervention with an online self-manegement program | Participants exposed to pilot 3 (forums, activities online and quiz) improved significantly on the fatigue impact scale. | The results show that the online fatigue self-management program is a viable complex intervention. |
| D´hooghe et al. [ ], 2018, Belgium | To evaluate the feasibility of a TeleCoach progam for the improvement of physical activity and fatigue levels. | 75, MS | Fatigue intervention with TeleCoach program through smartphone. | There were significant improvements in Fatigue Scale for Motor and Cognitive Functions. | The TeleCoach program is viable as complementary training to conventional treatment. |
| Kos et al. [ ], 2007, Belgium | To evaluate the effectiveness of a fatigue management program. | 51, MS | Multidisciplinary fatigue intervention. | A reduction of Modified Fatigue Impact Scale was found in 17% of IG compared to 44% after the placebo intervention programme | The multidisciplinary fatigue management programme showed no efficacy in reducing the impact of fatigue compared to a placebo intervention programme |
| Sauter et al. [ ], 2008, Austria | To examine the effectiveness of fatigue management and energy conservation strategies. | 32, MS | Fatigue intervention | Significant improvements were found in people’s physical and cognitive fatigue. There were less fewer signs of depression and the quality of sleep improved | Fatigue cannot be completely eliminated, but there were improvements in fatigue management and energy conservation |
| Mathiowetz et al. [ ], 2005, United States | To evaluate the effectiveness of an energy conservation course. | 169, MS | Energy conservation program | There were significants effects on reducing the physical and social subscales of fatigue and on increasing QoL. | The energy conservation program is effective in improving fatigue, self-efficacy and quality of life in people with moderate-severe MS |
| Finlayson et al. [ ], 2011, United States | To evaluate the effectiveness of a teleconference-delivered program on fatigue management | 181, MS | Fatigue intervention through teleconference | There were significant improvements in fatigue and quality of life. | The results support for the viability of teleconference-delivered fatigue management education. |
| Kos et al. [ ], 2016, Belgium | To evaluate the effectiveness of an individual SMOoTh vs relaxation on the performance of and satisfaction with relevant daily activities. | 31, MS | Fatigue Intervention with the SMOoTh program | There were significant improvements in COPM. | Both interventions showed improvements in the satisfaction and performance of activities. |
| Lamb et al. [ ], 2004, United States | To evaluate the effectiveness of an energy conservation program vs self-study material at home in a missed session | 92, MS | Energy conservation program | There were no significant differences between groups. | The self-study material is just as effective if the person miss a session, but it would not work as the only method of treatment. |
| Hersche et al. [ ], 2019, Switzerland | To evaluate the effectiveness of the inpatient energy management education (IEME) | 47, MS | Fatigue intervention through IEME program | There were significant improvements in fatigue in both groups. The IEME alone resulted in significant improvements in self-efficacy regarding energy conservation strategies. | The IEME program was effective at improving self-efficacy in performance and fatigue management strategies. |
MS: Multiple sclerosis, ALS: Amyotrophic Lateral Sclerosis, IG: Intervention group, CG: Control group, QoL: Quality of life, OT: Occupational therapy, SPT: speed of processing training, vs: versus, SMOoTh: self-management occupational therapy intervention, COPM: Canadian Occupational Performance Measure, IEME: inpatient energy management education.
We observed that intervention studies conducted in MS and ALS patients could be classified into four clearly differentiated areas: fatigue, physical rehabilitation, cognitive interventions and others. The full description of these interventions are presented in Table 3 .
Characteristics of the interventions performed in the studies included in this scoping review.
| Author, Year, Country | Intervention Category | Intervention | CG/IG | Duration (Weeks) | Sessions | Measurment Instruments | Intervention Manager |
|---|---|---|---|---|---|---|---|
| Eyssen et al. [ ], 2013, Netherlands | Other categories | Client-centred OT | CG: Traditional therapy for the patient.The client-centred framework and tools were not available. IG: OTs encouraged participants to choose, organise and perform activities the patients found useful and meaningful in their environment. The client-centred process model was based on the Canadian practice process framework. | 52 | EDSS, DIP, IPA, 9HPT, MFIS, PES, SF36, COPM, ECGP | OT | |
| Eyssen et al. [ ], 2014, Netherlands | Other categories | Client-centred OT | CG: Traditional therapy for the patient. The client-centred framework and tools were not available IG: OTs encouraged participants to choose, organise and perform activities the patients found useful and meaningful in their environment. The client-centred process model was based on the Canadian practice process framework. | 104 | EDSS | OT | |
| Raglio et al. [ ], 2016, Italy | Other categories * | Music therapy * | CG: Participants received physical and speech rehabilitation, OT an psychological support IG: Music therapy sessions. OTs stimulates patients to communicate using instruments and express emotions. | 4 | Three-weekly half-hour sessions | ALSFRS-R, HADS, MQoL-it, MTRS | OT |
| Block et al. [ ], 2009, United States | Other categories | Health-promotion and self-efficacy management | CG: Nontreatment IG: A variety of indoor and outdoor activities for indepent living and health promotion like using public transport or recreational activities included sailing or cycling. | 23 | Ten full day/sessions, twice a month | GSE, PAL | OT, psichologist |
| Reilly y Hynes. [ ], 2018, Ireland | Cognitive intervention | Cognitive Occupation- Based Programe (COB-MS) | IG: Compensatory strategies and new routines and techniques about employment and daily life. There are seven group session and one individual session. Participants increase their knowledge about cognition, sleep, motivation and future goals. Pre-test/post-test were done. | 8 | Once-weekly sixty minutes sessions | GAS, OSA-DLS, CVLT-II, BVMT-R, SDMT, TMT, BRIEF-A, EMQ-R | OT |
| Chiaravalloti et al. [ ], 2018, United States | Cognitive intervention | Speed of Processing Training (SPT) | CG: Nontreatment IG: Three tasks about speed of processing, divided attention and selective attention on a computer. First, participants practice a discrimination task with targets. In task 2, participants have to locate a peripheral target while they are doing task 1. In task 3, they have to do the same at task 2 but with distracters. | 5 | Twice-weekly thirty to forty minutes sessions | WAIS-III, LC, PC, CVLT-II, TIADL | OT, neuropsychologists |
| Goverover et al. [ ], 2017, United States | Cognitive intervention | Self-generation learning program (self-GEN trial) | CG: Memory and learning tasks. Participants have to learn an items list. IG: Memory and learning task with techniques to improve this skills. Participants have to learn the same list but it has pictures, sentences or a word pair. Participants can choose whose the most useful technique to learn words is. | 3 | Twice-weekly sixty minutes sessions | CMT, SRSI, MIST, CVLT-II, MFQ, AQ, FBP, CMDI, FAMS | OT |
| Schettini et al. [ ], 2015, Italy | Cognitive intervention * | Assistive technology prototype for communication and home control * | IG : Participants were asked to control a standalone P300-speller based BCI to test the ability to control a BCI system and to subsequently compare the performance obtained with the BCI with that observed while controlling the assistive technology prototype with the BCI channel. IG : Users, who operated via a conventional or an alternative input device (eg, mouse, buttons) that best matched their residual motor abilities controlling the assistive technology. Two task: Self-managed environmental control task: and Self-managed communication task. IG : Assistive technology. The prototype visual interface consisted of several menus. Stimulation timing and number of stimulus repetitions for each item were the same as in condition Two tasks: Copy environmental control task: and Copy communication task. | 3 | Once-weekly ninety minutes session | BCI online copy accuracy, BCI offline accuracy, AT prototype online accuracy during self managed tasks). BCI offline Writen Symbol Rate, AT prototype time for correct selection). VAS, System Usability Scale. | OT, engineer, neurologist |
| Gentry. [ ], 2008, United States | Cognitive intervention | 0T therapy using PDAs as assistive technology | IG: Participants learn to use PDAs for three weeks (week 10 to 12) and the OT measure eight weeks before and eight weeks later. They learn about calendar reminders, use of contacts, troubleshoot and train in use of additional features. | 21 | Two sixty minutes sessions and two ninety minutes sessions | RBMT-E, COPM, CHART-R | OT |
| Shevil et al. [ ], 2009, Israel-United States | Cognitive intervention | Program: Mind over Matter.knolwedge and management. | IG: OTs teach to participantes about cognitive impairments and how to manage their symptoms. about how increase participant´s self-efficacy and the use of cognitive strategies. | 5 | Once-weekly two hours sessions | Knowledge quizzes, CMSEQ, CSQ | OT |
| Gómez-Fernández et al. [ ], 2001, Cuba | Physical intervention * | Multifactorial intervention * | IG: Participants received a multifactorial treatment with breathing exercises; face, mouth and neck exercises, balance and walk exercises. OTs have to avoid participants fatigue in the treatment. Pre-test/post-test. | 4 | Monday to Friday seven hours’ sessions. Saturday three hours sessions | FVC, ALSFRS | OT, Neurologists, physiotherapists, logopaedits, defectologists, psychologists and physicians |
| Yang et al. [ ], 2019, United States | Physical intervention | ActiveStep treadmill to improve stability and falls risk | IG: Participants walk on the treadmill with a safety harness and they have to adapt to unexpected slips. | Five sessions | Number of falls, COM, quality of steps | OT, kinesiologist, mathematical | |
| Kamm et al. [ ], 2014, Switzerland | Physical intervention | A home-based program to improve manual dexterity in ADL | IG1: Participants are in two randomized groups. The first group practice a dexterity program (finger tapping, turning coins, modeling clay). IG2: The second group practice a theraband program with strength exercises. Pre-test/post-test. | 4 | Five weekly thirty minutes sessions | CRT, NHPT, JAMAR, CAHAI, | OT, neurologist |
| Lamers et al. [ ], 2019, Belgium | Physical intervention | A task-oriented program to upper limb | CG: Conventional occupational therapy IG: Participants train the task-oriented program at individualized intensity. They have to practice unilateral and bilateral tasks in their daily life and the difficulty is increased throughout the program. | 8 | Five weekly sixty minutes sessions | NHPT, ARAT, BBT, TEMPA, MAM-36 | OT |
| Finlayson et al. [ ], 2009, United States | Physical intervention | “Safe at Home BAASE” a fall risk management program. | IG: Participants train the program to increase the knowledge about falls and to learn skills to manage falls. There are 14 fall prevention strategies. In post-intervention, participants report whether they use the strategies. Pre-test/post-test. | 6 | Once weekly two hours sessions | FCS, FMS, FPMQ, FPSS, FES | OT |
| Ortiz et al. [ ], 2013, Spain | Physical intervention | A virtual reality rehabilitation to improve balance and postural control | CG: Participants received physiotherapy treatment with strength exercises, propioception exercises, gait facilitation and muscle-tendon stretching. IG: Participants received telerehabilitation treatment using the Xbox 360 console monitored via videoconference following activities that have a certain difficulty and intensity (hitting object with hands and feet, imitating postures, obstacles). | 10 | Four weekly twenty minutes sessions | CDP, SOT, MCT | Multidisciplinar: physiotherapist/ OT |
| Waliño-Paniagua et al. [ ], 2019, Spain | Physical intervention | OT virtual reality compared to conventional OT | CG: Conventional occupational therapy. IG: Participants received OT and virtual reality include leisure activities (play cards, play hockey, fishing) | 10 | Twice weekly thirty minutes sessions | PPT, JPT, GPT | OT |
| Bovend´Eerdt et al. [ ], 2010, United Kingdom | Physical intervention | An integrated motor imagery program | CG: Participants watch a film with physical practice, Then, They have conventional OT and physiotherapy. IG: Participants watch a different film than CG and then, OTs train with patients with imagery strategies in particular tasks. | 7 | Two to three weekly six hours and a half the total time spent | GAS, BI, RMI, ARAT, NEADLS | OT, Physiotherapy |
| Kalron et al. [ ], 2013, Israel | Physical intervention | A sensory re-education program on hand sensibility and manual dexterity | CG: Participants received OT sessions with non specific exposure via grasping objects. IG: Participants received two tasks. In the first task, participants are blindfolded and they have to recognize the object. In the second task, all objects are on a table and OTs describe the object. They have to discriminate it. | 10 | Five weekly twenty minutes sessions. | NHPT, FDT, TDP, S-W monofilaments | OT |
| Bansi et al. [ ], 2013, Switzerland | Physical intervention | Effects of a endurance training in quality life and fatigue | IG: Participants in two groups performed a 3 weeks endurance exercise training on a cyclo-ergometer or an aquatic bike with different phases. | 3 | Four daily thirty to forty minutes sessions | FSMC, MFIS, SF-36 | OT, physiotherapist, neurophysicologist |
| Vanage et al. [ ], 2003, United States | Fatigue intervention | An energy conservation course | CG: Participants received 8 weeks control treatment and then, they received 8 weeks energy conservation course. IG: Participants received 8 weeks energy conservation course and then, they received 8 weeks control treatment. | 8 | Once weekly sixty minutes sessions | FSS, FIS, MCA | OT |
| Rietberg et al. [ ], 2014, Netherlands | Fatigue intervention | Multidisciplinary rehabilitation on chronic fatigue | CG: Participants received nurse consultation IG: Participants received physiotherapy, OT or social work sessions when they need. Physiotherapy sessions were determinate in 45 min sessions. | 12 | Number of sessions was on an as-needed basis, with a mínimum of 2 sessions | CIS-20R, MFIS FSS, FIM, DIP, IPA, MSIS-29, SF-36 | OT, physiotherapy, social worker |
| Mathiowetz et al. [ ], 2001, United States | Fatigue intervention | An energy conservation course on fatigue impact | CG: Participants received 6 weeks control intervention with support and discussing about MS topics. IG: Participants received the energy conservation course learning about rest, communication, ergonomic principles, activity and balance lifestyle. | 6 | Once weekly two hours sessions | FIS, SEG, SF-36 | OT |
| Ghahari et al. [ ], 2009, Iran | Fatigue intervention | An online fatigue self-management program | IG: Reachers transform the Energy Conservation Course into a online self-management program through sharing stories, information and activities. With an online version, patients can practice the program at home. | 6 | Once weekly two hours sessions | PW-BI, FIS, ACS, FSS, GES, DASS | OT |
| D´hooghe et al. [ ], 2018, Belgium | Fatigue intervention | TeleCoach program by smartphone | IG: Participants received in their smartphones motivational messages focusing on energy management and monitoring the physical activities to improve fatigue levels. | 12 | NS | FSMC, MFIS | OT, neurologist, neuroscientist |
| Kos et al. [ ], 2007, Belgium | Fatigue intervention | Multidisciplinary fatigue management program. | CG: Participants received information about topics that did not concern to fatigue (car adaptation, communication skills or general information abpur MS) IG: Participants received information about pharmacological treatment, diet, rest, strategies to manage fatigue or adaptation to work or home. | 4 | Once weekly two hours sessions | MFIS, FSS | OT, Multidisciplinary team |
| Sauter et al. [ ], 2008, Austria | Fatigue intervention | A course of energy conservation for people with MS | CG: Participants did not receive treatment IG: Participants received information about different topics like rest, self care, communication, work or leisure tasks. | 6 | Once weekly two hours sessions | FSS, MFIS, MS-SFS, EDSS, MSFC, PSQI S-RSD | OT |
| Mathiowetz et al. [ ], 2005, United States | Fatigue intervention | A course of energy conservation for people with MS | CG: Participants received 6 weeks control intervention with support and discussing about MS topics. IG: Participants received the energy conservation course learning about rest, communication, ergonomic principles, activity and balance lifestyle. | 6 | Once weekly two hours sessions | SEG, FIS, SF-36 | OT |
| Finlayson et al. [ ], 2011, United States | Fatigue intervention | A teleconference- delivered fatigue management program for people with MS | IG: Participants were divided in two groups and they received the treatment in different weeks by teleconference. The intervention consist in teaching sessions, discussing and homework about topics like communication, fatigue, rest, ergomonics and balanced life. | 6 | Once weekly seventy minutes sessions | SF-36, FIS, FSS, SECQ | OT |
| Kos et al. [ ], 2016, Belgium | Fatigue intervention | A self-management fatigue program (SMOoTh) | CG: Participants received physiotherapy sessions with relaxing techniques and some information. IG: Participant received information about fatigue, levels of activity, communication, use of wheelchairs, obstacles and facilitators at home and some strategies. | 3 | Once weekly thirty to ninety minutes sessions | SF-36, MFIS, COPM, CIS-20R, | OT |
| Lamb et al. [ ], 2004, United States | Fatigue intervention | Energy conservation. | CG: Conventional OT. Participants did not receive any modules of treatment IG: Participants divided in three groups and they received one module, two modules, or more than two modules. Evaluators tried to check the course efficacy if participants do not receive some sessions. | 6 | Once weekly two hours sessions | SF-36, FIS, SEA, ECSS | OT |
| Hersche et al. [ ], 2019, Switzerland | Fatigue intervention | An energy management education program. | CG: Participant received progressive muscles relaxation or group sessions. IG: Participants discussed and work about topics such as occupational balance, activity, fatigue, energy account, goals or effective communication. | 3 | Once weekly Two hours sessions | MFIS, SF-36, UWSES, SEPECSA | OT |
* ALS intervention; OT: Occupational therapy; OTs: Occupational therapist; NS:Not stated; BCI: Brain computer interface; ACS: Activity Card Sort; ALSFRS: Amyotrophic Lateral Sclerosis Functional Rating Scale; AQ: Awareness Questionnaire; ARAT: Action Research Arm Test; BBT: Box and Block Test; BI: Barthel Index; BRIEF-A: Behavior Rating Inventory of Executive Function; BVMT-R: Brief Visuospatial Memory Test-Revised; CAHAI: Chedoke Arm and Hand Activity Inventory; CDP: Computerized dynamic posturography; CHART-R: Craig Handicap Assessment and RatingTechnique-Revised; CIS-20R: Checklist Individual Strength; CMDI: Chicago Multiscale Depression Inventory; CMSEQ: Cognitive Management Self-Efficacy Questionnaire; CMT: Contextual Memory Test; COM: Center Of Mass; COPM: Canadian Occupational Performance Measure; CRT: Coin Rotation Task; CVLT-II: California Verbal Learning Test–2nd Edition; CSQ: Cognitive Strategies Questionnaire; DASS: Depression Anxiety and Stress Scale; DIP: Disability and Impact profile; ECGP: Evaluation of the Client-Centered Process; ECSS: Energy Conservation Strategies Survey; EDSS: Expanded Disability Status Score; EMQ-R: Everyday Memory Questionnaire-Revised; FAMS: Functional Assessment of Multiple Sclerosis; FBP: Functional behavior profile; FCS: Falls Control Scale; FDT: Functional Dexterity Test; FES: Falls Efficacy Scale; FIM: Functional Independence Measure; FIS: Fatigue Impact Scale; FMS: Falls Management Scale; FPMQ: Falls Prevention and Management Questionnaire; FPSS: Fall Prevention Strategies Survey; FSMC: Fatigue Scale of Motor and Cognitive Functions; FSS: Fatigue Severity Scale; FVC: Forced Vital Capacity; GAS: Goal Attainment Scaling; GES: Generalized Self-Efficacy Scale; GPT: Grooved Pegboard Test; HADS: Hospital Anxiety and Depression Scale; IPA: Impact on Participation and Autonomy; JTT: Jebsen- Taylor Hand Function Test; LC: Letter Comparison; MAM-36: Manual Ability Measure; MCA: Measure Change Assessment; MCT: Motor Control Test; MIST: Memory for Intentions Test; MFIS: Modified Fatigue Impact Scale; MFQ: Memory Functioning Questionnaire; MQoL-it: Italian version of McGill Quality of Life Questionnaire; MSFC: Multiple Sclerosis Functional Composite; MS-SFS: Multiple Sclerosis- Specific Fatigue Scale; NEADLS: Nottingham Extended Activity of Daily Living Scale; NHPT: Nine Hole Peg Test; OSA-DLS: Occupational Self-Assessment-Daily Living Scales; PAL: Personal Activity Log; PC: Pattern Comparison; PES: Pain Effects Scale; PPT: Purdue Pegboard Test; PSQI: Pittsburgh Sleep Quality Index; MSIS-29: Multiple Sclerosis Impact Scale; PW-BI: Personal Well-Being Index; RBMT-E: Rivermead Behavioral Memory Test- Extended; RMI: Rivermead Mobility Index; SDMT: Symbol Digit Modality Test; SEA: Self-Efficacy for Performing Energy Conservation Strategies Assessment; SECQ: Self-efficacy for Energy Conservation Questionnaire; SEG: Self-Efficacy Gauge; SEPECSA: Self-Efficacy for Performing Energy Conservation Strategies Assessment; SOT: Sensory Organization Test; S-RSD: Self- Rating Scale for Depression; SRSI: Self-Regulation Skills Interview; SF-36: Study Short-Form Health Survey; TEMPA: Test d’Évaluation des Membres Supérieurs des Personnes Âgées; TDP: Two Discrimination Points; TMT: Trail Making Test; TIADL: Timed Instrumental Activities of Daily Living Test; UWSES: University of Washington Self-Efficacy Scale; VAS: Visual Analog Scale; WAIS-III: Wechsler Adult Intelligence Scale-III. Session duration is reported where available.
The articles analyzed were classified into four clearly differentiated areas: (1) interventions for fatigue and energy conservation; (2) cognitive interventions; (3) physical interventions; and (4) other interventions. The fully description of OT intervention carried out in MS and ALS is shown in Table 3 .
3.1. Interventions in Fatigue and Energy Conservation
Twelve studies conducted interventions related to energy and impact on fatigue in people with MS. The results of these interventions are described in Table 2 . Seven of these studies were based on the fatigue management program developed by Packer et al. [ 28 ], which consists of a 12 h intervention for people with MS and includes a balanced lifestyle, rest, posture and efficient communication, among other aspects [ 29 , 30 , 31 , 32 , 33 , 34 , 35 ]. Another study modified Packer´s program and evaluated these interventions nonpresentially by monitoring patients either through teleconferences, applications or on the internet [ 36 ].
In addition, several authors examined the effectiveness of physiotherapy and diet interventions aimed at fatigue carried out by a multidisciplinary team, including occupational therapists [ 37 , 38 ]. Other authors proposed different intervention programs [ 39 , 40 ] based on changes in daily occupational performance and proposed strategies related to occupational balance, activity, fatigue, energy account, goals or effective communication.
We did not identify studies carried out in fatigue and energy conservation in ALS patients.
3.2. Cognitive Interventions
Six studies carried out cognitive interventions. A full description intervention appear in Table 3 .
Of these studies, two included the use of technology to facilitate communication and automated control at home [ 19 , 41 ] to evaluated the functional performance which increased significantly with PDA use [ 18 ]. The remaining studies evaluated interventions related to improvement of memory, attention, processing speed and strategies to compensate these cognitive strategies [ 20 , 42 , 43 , 44 ] with different results ( Table 2 )
Only one study was carried out in people with ALS [ 41 ]. This study evaluated the feasibility and usability of an assistive technology prototype in users who have different degrees of muscular impairment to improve interaction with environment.
3.3. Physical Interventions
Of a total of ten articles describing interventions in relation to physical condition, nine focused on MS patients and one on ALS patients, only 2 were led by occupational therapists. The results and the details of interventions are shown in Table 2 and Table 3 .
In the MS focused studies, we identified three categories: upper limb recovery, physical rehabilitation and falls prevention.
In the first category, four of the studies focused on upper limb recovery, both at the level of sensory re-education and at that of improvement in manual dexterity in MS [ 45 , 46 , 47 , 48 ]. Another study assessed an intervention program to improve the physical resistance of MS patients [ 49 ].
In the second category, two other MS focused studies aimed at physical rehabilitation were carried out using new technologies such as virtual reality [ 50 ] or images and videos [ 51 ].
Finally, the third category included two intervention studies which evaluated programs to decrease falls risk in MS patients, by sending them information related to falls and how to avoid them [ 52 ] or by giving them tape training sessions in order to improve balance reactions [ 53 ].
In relation to the ALS focused study, Gómez-Fernández et al., assessed the effectiveness of a multifactorial program by working on different aspects such as breathing, posture control or transfers using a multidisciplinary approach [ 54 ] which showed that ALS patients improved significantly on forced vital capacity.
3.4. Other Interventions
Four articles did not fit into any of the previous categories. Of these, three studies focused on MS patients.
Two of the studies focusing on MS assessed client-centered practice intervention in people with MS patients to evaluate disability, autonomy and participation in daily life with no significant effects in these outcomes [ 55 , 56 ]. Another of these studies, led by Block et al., assessed the effectiveness of health promotion in people with MS which worked on different aspects such as the empowerment of the person [ 57 ]. This study showed significant improvements in self-efficacy and ability to achieve objectives [ 57 ].
The one study focusing in ALS evaluated the impact of music therapy programs on psychological aspects such as depression and anxiety [ 58 ]. In this study, occupational therapists stimulates patients to communicate using instruments and express emotions with positive results in quality of life.
4. Discussion
This scoping review describes different occupational therapy interventions carried out in MS and ALS patients. These interventions were mainly focused on physical rehabilitation, cognitive rehabilitation and reducing fatigue. Although some of the interventions included in this review were not exclusively led by occupational therapists, they can use these interventions to facilitate the occupational therapy evidence-based interventions. This review shows that the majority of occupational therapy interventions are performed on MS patients while there is little information about ALS patients. In fact, few intervention studies led by occupational therapists have been found.
4.1. Fatigue Interventions and Energy Conservation
This study shows that certain occupational therapy interventions for MS and ALS patients could be effective in improving different outcomes. The majority of the studies identified in this scoping review were fatigue interventions carried out in MS patients. In our search we found that studies principally focused on fatigue are based on the Packer et al. program [ 28 ]. This fatigue program is a six-week energy conservation course, which was designed for adults suffering from fatigue as a symptom of chronic disease [ 28 ]. In this program occupational therapists educated participants in the benefits of breaking up high-energy tasks by incorporating rest periods into their daily activities [ 28 ]. In addition, we observed several studies that included the Packer et al. energy conservation course with some adaptations. Lamb et al. found that patients using self-study material in nonpresential sessions, and who had missed some sessions, obtained similar benefits regarding energy and fatigue management to those whose sessions were guided by a professional and who fully completed the intervention [ 31 ]. Similarly, Sauter et al., adapted the fatigue management program to the German population and showed improvements in users´physical and mental fatigue. Subsequent studies [ 33 , 34 ] modified the Packer et al. fatigue management course [ 28 ] so that it could be delivered by teleconference and online for people with MS who had problems accessing treatment, leading to an improvement in fatigue and quality of life [ 33 , 34 ]. The therapy showed significant improvements in fatigue management even when participants were guided via technological devices [ 29 , 30 , 31 , 32 , 33 , 34 , 35 ]. In a similar way, D´hooghe et al., developed a course related to a fatigue management program using a smartphone to provide monitoring, motivational messaging and the establishment of objectives [ 36 ]. The results showed that this type of intervention can be complementary to conventional treatment to reduce fatigue [ 36 ]. Overall, according to the previous evidence, the use of new technologies seems to be a good treatment option.
Conversely, other studies explored fatigue management using different multidisciplinary interventions related to personal care. Rietberg et al. evaluated an intervention carried out by multidisciplinary professions including physical therapy, social work and occupational therapy which applied fatigue management strategies and personal care as compared with only nurse consultation and found that multidisciplinary rehabilitation did not lead to a more effective reduction of self-reported fatigue [ 37 ]. In the same line, Kos et al. evaluated a multidisciplinary fatigue management program intervention comparing it with an intervention program based on sleep advice and relaxation exercises [ 38 ]. It should be pointed out that neither of the two multidisciplinary interventions explored by these authors showed significant results. This could be because chronic fatigue does not improve significantly over time in MS patients only with personal care advice [ 37 ]. All interventions were conducted solely by occupational therapists, except for the multidisciplinary interventions and the D´hooghe et al. program [ 36 ], in which technology experts collaborated with occupational therapists.
Other authors have proposed other intervention programs [ 39 , 40 ] based on changes in daily occupational performance such as rest management and the proposal of strategies in relation to the management of instrumental activities such as childcare or shopping, that suggest significant improvements in performance, perceived fatigue and individual satisfaction [ 39 , 40 ].
It must be emphasized that fatigue is one of the most frequently reported symptoms in MS patients and can affect their occupational performance [ 59 ]. In this sense, a recent review [ 60 ] showed that patient-reported outcomes (PROs) are increasingly used in MS treatment. PROs not only describes symptoms, function and health status in MS patients but also evaluates the impact of this disease and assess the concerns on MS patient´s life [ 60 ].
Fatigue intervention in the included studies was found to be effective in reducing fatigue, managing fatigue symptoms and improving different aspects such as health-related quality of life [ 12 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 39 , 40 ]. Thus, it is essential that occupational therapy interventions should include fatigue intervention in daily practice with MS and ALS patients.
4.2. Cognitive Interventions
With regard to cognitive interventions, we identified six studies in MS and ALS treatment of which three were conducted exclusively by occupational therapists. In MS interventions, Tony Gentry et al., evaluated a program with PDAs that resulted in an improvement of the person´s functional performance and satisfaction using PDA as a compensation for cognitive deficits [ 19 ]. The remaining cognitive interventions [ 20 , 42 , 43 , 44 ] were related to improving memory, attention, processing speed and strategies to compensate this deficit. Among them, Goverover et al., evaluated the effectiveness of a cognitive strategies program, through visual supports when memorizing words, which showed improvements in memory, learning, depressive symptomatology and quality of life [ 20 ]. Only one cognitive intervention was identified for ALS. Schettini et al., evaluated the reliability of an assistive technology device for home automation control and communication, and there were no significant improvements. This could be due to the fact that the sample included only eight people, which may be too small to provide strong evidence [ 41 ].
Overall, although cognitive interventions in MS and ALS have scarcely been analyzed, these studies show that cognitive interventions in this type of population have significant beneficial effects in functional performance, depression and quality of life [ 12 , 19 , 20 , 42 , 43 , 44 ]. However, these results should be interpreted with caution because the samples in most of the studies described were small and there is no evidence regarding their long-term effects on functional performance [ 41 , 42 , 43 ]. In addition, it also should have taken into account that there is a lack of information about the effectiveness of these interventions in the progressive forms of MS [ 61 ], and there is no evidence about therapeutic intervention to enhance cognitive performances in MS patients [ 62 ]. Thus, more studies are needed.
4.3. Physical Interventions
Evidence based on different physical therapeutic modalities suggested that interventions improve different functional outcomes (manual dexterity), reduce fatigue and improve quality of life [ 12 , 23 ]. All the studies focused on upper limb recovery were carried out in MS patients. Lamers et al., evaluated the ideal intensity in an upper limb recovery program, showing a positive result, although no overall intensity was established [ 45 ]. Kamm et al., conducted a program to improve manual dexterity with exercises using fingers, coins, paper and pencil, and clay, showing improvements in fine motor skills in the experimental group [ 46 ]. In the same way Waliño-Paniagua et al., evaluated manual dexterity with virtual reality games in comparison with conventional occupational therapy, showing significant differences. These interventions could also be used as complementary activities in occupational therapy [ 47 ]. Finally, Kalron et al., conducted a sensory re-education with tubes of different textures and thickness, showing an improvement in manual dexterity and, although sensitivity did not improve, this program may help to prevent deterioration in manual dexterity in early stages of rehabilitation [ 48 ]. It should be pointed out that evidence-based rehabilitation for upper limb recovery are essential for improving performance in daily tasks [ 23 ]. Thus, occupational therapists could carry out this evidence-based intervention in MS and ALS patients.
With respect to physical rehabilitation interventions, Bansi et al., evaluated physical rehabilitation with cycle-ergometers or aquatic- bikes in two groups, showing an improvement in quality of life and fatigue [ 49 ]. Another study examined virtual reality rehabilitation with strength and proprioception exercises on unstable surfaces and muscle-tendon stretching, showing significant improvements at the motor level, which suggests that it could be an alternative treatment [ 50 ]. In the same line, Bovend´Eerdt et al., assessed a film and image presentation program with exercise information and guided rehabilitation strategies [ 51 ]. This intervention did not provide valid results because participants did not perform the program in the established time, although there were significant differences after the intervention [ 51 ].
We only identified one study in ALS patients, where Gómez-Fernández et al., examined a multifactorial program in ALS, through postural control exercises, exercises with lips, breathing, walking or psycho-emotional support that showed significant improvements in forced vital capacity [ 54 ]. However, the sample is very small, which could cast doubt on the results [ 54 ].
Regarding the interventions aimed at falls prevention, previous studies carried out programs either by receiving information about falls, strategies and changes in the environment [ 52 ], or by treadmill with caused imbalance [ 53 ]. Both studies showed a decrease in falls in MS patients.
4.4. Other Interventions
Evidence for other interventions was limited. We included four articles in this category because they did not fit into any of the previous categories. In this category, Eyssen et al., explored the effectiveness of client centered practice, comparing it with a control group that received conventional occupational therapy practice [ 55 , 56 ]. The results showed no significant improvements in participants, possibly because more time was spent on evaluation than on intervention, resulting in a less effective recovery. Therefore, this type of practice is not recommended [ 55 , 56 ].
There is currently only limited evidence for the effectiveness of the role of environment in the experience of disability. However, the project Shake-it-up explored the effectiveness of health promotion which works on aspects such as self-efficacy and empowerment among others and found a significant improvement in these aspects [ 57 ]. These results could be useful for occupational therapists in their routine work in order to improve the independence, community access and participation of MS and ALS patients.
Finally, we also found one study which assessed the impact of music therapy in ALS, participants interacted with different instruments to express their emotions and communicate, showing an improvement in their quality of life [ 58 ]. These findings suggest that there is a need for better designed intervention studies which explore the impact of music therapy on other symptoms in ALS and MS patients.
4.5. Study Limitations
This study has a number of limitations. First, regarding inclusion criteria, we only included studies published in English or Spanish and those with full text available. Second, the articles included in this review were experimental studies and might contain biases associated with the experimental study design. Furthermore, the heterogeneity of the included studies meant that they were not comparable in terms of sessions, hours and study objectives. The generally limited study sample size of some included studies means that the results should be interpreted with caution. Third, like other authors in their respective scoping reviews, we did not critically assess the quality of the included studies, because this is not the role of a scoping review [ 63 ]. However, we mentioned the limitations of some of the studies in the discussion section. Finally, it should be pointed out that some studies did not clearly specify which professionals participated in the intervention or what their role in the study was. Thus, more studies are needed that specify the role of the researchers in the interventions, including those which are led by occupational therapists.
However, this review also has several strengths. To the best of our knowledge, it is the first study with the aim of describing the main occupational therapy interventions carried out in MS and ALS. In addition, this scoping review highlights the gaps in our knowledge: (i) there is no evidence regarding occupational therapy interventions carried out in Spain; (ii) most of the studies had small sample sizes and a lack of randomization; (iii) there is little evidence about long-terms interventions; and (iv) there is a need to determine the role of the different professionals in the multidisciplinary teams. These identified gaps of knowledge might be dealt with in future research.
This study provides the professionals with a description of therapies in MS and ALS that can support the use of early therapeutic interventions aimed at optimizing outcomes in this population. The included studies in this review showed that occupational therapists can not only collaborate in the multidisciplinary intervention but can also lead different interventions in MS and ALS. This review suggests that occupational therapy is a relevant discipline for MS and ALS patients’ rehabilitation. The main intervention led by occupational therapists is fatigue management, which showed beneficial effects in MS patients, but occupational therapists could also carry out psychosocial, physical and emotional interventions in this population. In addition, we would like to underline that the updated summary of previous evidence carried out in this scoping review provides knowledge to facilitate occupational therapy evidence-based interventions.
Finally, our findings add new insights about the potentially beneficial role of physical rehabilitation, fatigue and cognitive interventions, and could inform future evidence-based guidelines for ML and ALS patients.
5. Conclusions
In conclusion, most studies were conducted in the MS population, with little representation from the ALS population. The main interventions in occupational therapy were those aimed at fatigue, cognitive interventions and physical rehabilitation. These interventions have shown an improvement in perceived fatigue, manual dexterity, falls prevention and in cognitive aspects such as memory, communication, depression and quality of life in the MS and ALS population. It should be pointed out that some of the interventions included in this review are not exclusive to occupational therapy practice. However, occupational therapy professionals can use these interventions in patients with MS and ALS, and they can help patients to incorporate activities and occupations into their intervention patterns.
Acknowledgments
We would like to acknowledge the English revision made by Jessica Gorlin and María del Mar Freniche Zanari.
Author Contributions
All authors contributed to the conception or design of the review and to the data analysis and interpretation. M.G.-d.-l.-H. coordinated the scoping review. L.T.-C. and L.D.-B.-O. conducted a peer-reviewed search and screening study. L.D.-B.-O. wrote the first draft of the paper and M.G.-d.-l.-H. and L.T.-C. provided critical revision of the article. All authors have read and agreed to the published version of the manuscript.
This research was funded by grants from Alicante Institute for Health and Biomedical Research, ISABIAL (UGT_18_453, UGP-19-490, and UGT_19_252).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Data availability statement, conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Author Biographies
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
An unconventional case study of neoadjuvant oncolytic virotherapy for recurrent breast cancer.

Share and Cite
Forčić, D.; Mršić, K.; Perić-Balja, M.; Kurtović, T.; Ramić, S.; Silovski, T.; Pedišić, I.; Milas, I.; Halassy, B. An Unconventional Case Study of Neoadjuvant Oncolytic Virotherapy for Recurrent Breast Cancer. Vaccines 2024 , 12 , 958. https://doi.org/10.3390/vaccines12090958
Forčić D, Mršić K, Perić-Balja M, Kurtović T, Ramić S, Silovski T, Pedišić I, Milas I, Halassy B. An Unconventional Case Study of Neoadjuvant Oncolytic Virotherapy for Recurrent Breast Cancer. Vaccines . 2024; 12(9):958. https://doi.org/10.3390/vaccines12090958
Forčić, Dubravko, Karmen Mršić, Melita Perić-Balja, Tihana Kurtović, Snježana Ramić, Tajana Silovski, Ivo Pedišić, Ivan Milas, and Beata Halassy. 2024. "An Unconventional Case Study of Neoadjuvant Oncolytic Virotherapy for Recurrent Breast Cancer" Vaccines 12, no. 9: 958. https://doi.org/10.3390/vaccines12090958
Article Metrics
Article access statistics, supplementary material.
ZIP-Document (ZIP, 205 KiB)
Further Information
Mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.

IMAGES
COMMENTS
The objective of the study was to examine how occupational therapy services are being integrated into primary care teams and understand the structures supporting the integration. A multiple case study design was used to provide an in-depth description of the integration of occupational therapy. Four Family Health Teams with occupational ...
Abstract. Qualitative case study methodology (QCSM) is a useful research approach that has grown in popularity within the social sciences; however, it has received less attention in the occupational therapy literature. The current scoping review aims to explore how studies utilizing a QCSM help inform occupational therapy knowledge and practice ...
This observational multiple-case study included video and audio-recordings of three participants (one male, one female, one nonbinary) completing the ACS-Aus (18-64) and semi-structured interviews at 1-week follow-up. Findings The findings for the process included two themes: the interaction (understanding engagement, therapeutic relationship ...
The present multiple case study adds to a growing body of evidence on the role of occupational therapists in a hospital setting as part of the initial rehabilitation of patients with COVID-19, as well as postdischarge. Our data describe extensive difficulties in carrying out ADL for this patient population.
Methods A multiple case study design was used to provide an in-depth description of the integration of occupational therapy. Four Family Health Teams with occupational therapists as part of the ...
Background: Few studies have examined the role of occupational therapy working in a primary care setting. Purpose: The objective of the study was to describe the emerging role of occupational therapy in Family Health Teams, a model of interprofessional primary care. Method: A multiple case study design was used to provide in-depth description of the occupational therapy role.
The integration of occupational therapy into primary care: a multiple case study design . × Close Log In. Log in with Facebook Log in with Google. or. Email. Password. Remember me on this computer. or reset password. Enter the email address you signed up with and we'll email you a reset link. ... The integration of occupational therapy into ...
From this study's findings, long-time concepts in occupational therapy (e.g. building rapport ... As an outcome of a multiple case study research, the scheme is not generalisable to a population, but it can be generalisable to a proposition according to Yin [Citation 34]. Hence, the proposed scheme should be tested further in various practice ...
An integrative literature review was carried out to explore contemporary occupational. therapy application of case study as an approach. The se arch comprised the. publications between 2006 -2016 ...
study, a collective case study design was utilized (Stake, 2000; Yin, 2003) informed by constructivist grounded theory data analysis methods (Charmaz, 2006) to develop a framework of CD from an occupational therapy perspective. Following a description of the research design, we describe the researcher stance of the first author, case recruitment
Explanatory case study methodology has been used to research complex systems in the fields of business, public policy and urban planning, to name a few. While it has been suggested by some that this might be a useful way to progress complex research issues in health science research, to date, there has been little evidence of this happening.
Case studies in the occupational therapy literature have explored phenomena relating to the delivery of intervention, theoretical concepts, clinical reasoning, and education and research methods and were situated in a range of different practice areas and contexts. QCSM is a valuable approach in occupational therapy research that contributes to ...
The chronic clinical condition discussed in this Evidence Connection article is adults with multiple sclerosis (MS). Findings from the systematic reviews on this topic were published in the January/February 2014 issue of the American Journal of Occupational Therapy (AJOT; Yu & Mathiowetz, 2014a, 2014b) and in the American Occupational Therapy Association's (AOTA's) Occupational Therapy ...
Methods: A multiple case study design was used to provide an in-depth description of the integration of occupational therapy. Four Family Health Teams with occupational therapists as part of the team were identified. Data collection included in-depth interviews, document analyses, and questionnaires. Results: Each Family Health Team had a ...
This scoping review explores case study research within occupational therapy in terms of how it is defined, the methodological characteristics adopted, such as data collection and analysis, and the range of practice contexts in which it is applied. We consider the viability of case study research for contributing to our evidence base.
Article Information. Volume: 43 issue: 2, page(s): 303-312 Issue published: April 01 2023
Abstract: Realistic case studies are a critical part of occupational therapy education to strengthen students' clinical reasonings skills, challenge their assumptions and biases, and expose them to the complexities of real clients. Case Studies for Contemporary Occupational Therapy Practice comprises 40 case studies across eight practice settings.
Methods: A multiple case study design was used through a retrospective record review. All garment workers with upper limb conditions who were treated at a student occupational therapy practice in Cape Town, South Africa, with pre- and post-intervention outcome assessment, were included in the study (n = 7).
Methods. A multiple case study design was used to provide an in-depth description of the integration of occupational therapy. Four Family Health Teams with occupational therapists as part of the team were identified. Data collection included in-depth interviews, document analyses, and questionnaires.
Defining the concept of collaboration in occupational therapy in this study can contribute to the improvement of occupational therapy practice and future studies. ... Crawford C., Letts L. The integration of occupational therapy into primary care: A multiple case study design. BMC Fam. Pract. 2013; 14:60. doi: 10.1186/1471-2296-14-60. [PMC free ...
Occupational therapy (OT) makes a unique contribution to chronic pain (CP) management due to its overarching focus on occupation. The aim of this scoping review was to describe current knowledge ...
Background: Mental health problems are common among university students. Based on the Model of Occupational Harmony, we investigated the relationship between occupational engagement and mental health among Chinese university students. Methods: A mixed methods approach was adopted. A total of 734 Chinese university students responded to online questionnaires: a socio-demographic questionnaire ...
Background The pathogenesis of amyotrophic lateral sclerosis (ALS) involves both genetic and environmental factors. This study investigates associations between metal measures in plasma and urine, ALS risk and survival and exposure sources. Methods Participants with and without ALS from Michigan provided plasma and urine samples for metal measurement via inductively coupled plasma mass ...
1. Introduction. Multiple sclerosis (MS) and amyotrophic lateral sclerosis (ALS) are neurodegenerative diseases of the nervous system [1,2].These diseases have a medium to high prevalence, but recently published epidemiological studies have shown an increasing incidence and prevalence of MS and ALS in different populations worldwide [3,4,5].Globally, in the case of MS, the incidence is 2.5 per ...
Intratumoural oncolytic virotherapy may have promise as a means to debulk and downstage inoperable tumours in preparation for successful surgery. Here, we describe the unique case of a 50-year-old self-experimenting female virologist with locally recurrent muscle-invasive breast cancer who was able to proceed to simple, non-invasive tumour resection after receiving multiple intratumoural ...
A multiple case study design was conducted that included four Family Health Team sites within the province of Ontario, Canada. Case study research seeks to investigate real life experiences within the context in which it occurs and involves the collection of detailed information using a variety of data collection methods [18-20]. As there are ...