- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Sweepstakes
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support

Types of Speech Impediments
Phynart Studio / Getty Images
Articulation Errors
Ankyloglossia, treating speech disorders.
A speech impediment, also known as a speech disorder , is a condition that can affect a person’s ability to form sounds and words, making their speech difficult to understand.
Speech disorders generally become evident in early childhood, as children start speaking and learning language. While many children initially have trouble with certain sounds and words, most are able to speak easily by the time they are five years old. However, some speech disorders persist. Approximately 5% of children aged three to 17 in the United States experience speech disorders.
There are many different types of speech impediments, including:
- Articulation errors
This article explores the causes, symptoms, and treatment of the different types of speech disorders.
Speech impediments that break the flow of speech are known as disfluencies. Stuttering is the most common form of disfluency, however there are other types as well.
Symptoms and Characteristics of Disfluencies
These are some of the characteristics of disfluencies:
- Repeating certain phrases, words, or sounds after the age of 4 (For example: “O…orange,” “I like…like orange juice,” “I want…I want orange juice”)
- Adding in extra sounds or words into sentences (For example: “We…uh…went to buy…um…orange juice”)
- Elongating words (For example: Saying “orange joooose” instead of "orange juice")
- Replacing words (For example: “What…Where is the orange juice?”)
- Hesitating while speaking (For example: A long pause while thinking)
- Pausing mid-speech (For example: Stopping abruptly mid-speech, due to lack of airflow, causing no sounds to come out, leading to a tense pause)
In addition, someone with disfluencies may also experience the following symptoms while speaking:
- Vocal tension and strain
- Head jerking
- Eye blinking
- Lip trembling
Causes of Disfluencies
People with disfluencies tend to have neurological differences in areas of the brain that control language processing and coordinate speech, which may be caused by:
- Genetic factors
- Trauma or infection to the brain
- Environmental stressors that cause anxiety or emotional distress
- Neurodevelopmental conditions like attention-deficit hyperactivity disorder (ADHD)
Articulation disorders occur when a person has trouble placing their tongue in the correct position to form certain speech sounds. Lisping is the most common type of articulation disorder.
Symptoms and Characteristics of Articulation Errors
These are some of the characteristics of articulation disorders:
- Substituting one sound for another . People typically have trouble with ‘r’ and ‘l’ sounds. (For example: Being unable to say “rabbit” and saying “wabbit” instead)
- Lisping , which refers specifically to difficulty with ‘s’ and ‘z’ sounds. (For example: Saying “thugar” instead of “sugar” or producing a whistling sound while trying to pronounce these letters)
- Omitting sounds (For example: Saying “coo” instead of “school”)
- Adding sounds (For example: Saying “pinanio” instead of “piano”)
- Making other speech errors that can make it difficult to decipher what the person is saying. For instance, only family members may be able to understand what they’re trying to say.
Causes of Articulation Errors
Articulation errors may be caused by:
- Genetic factors, as it can run in families
- Hearing loss , as mishearing sounds can affect the person’s ability to reproduce the sound
- Changes in the bones or muscles that are needed for speech, including a cleft palate (a hole in the roof of the mouth) and tooth problems
- Damage to the nerves or parts of the brain that coordinate speech, caused by conditions such as cerebral palsy , for instance
Ankyloglossia, also known as tongue-tie, is a condition where the person’s tongue is attached to the bottom of their mouth. This can restrict the tongue’s movement and make it hard for the person to move their tongue.
Symptoms and Characteristics of Ankyloglossia
Ankyloglossia is characterized by difficulty pronouncing ‘d,’ ‘n,’ ‘s,’ ‘t,’ ‘th,’ and ‘z’ sounds that require the person’s tongue to touch the roof of their mouth or their upper teeth, as their tongue may not be able to reach there.
Apart from speech impediments, people with ankyloglossia may also experience other symptoms as a result of their tongue-tie. These symptoms include:
- Difficulty breastfeeding in newborns
- Trouble swallowing
- Limited ability to move the tongue from side to side or stick it out
- Difficulty with activities like playing wind instruments, licking ice cream, or kissing
- Mouth breathing
Causes of Ankyloglossia
Ankyloglossia is a congenital condition, which means it is present from birth. A tissue known as the lingual frenulum attaches the tongue to the base of the mouth. People with ankyloglossia have a shorter lingual frenulum, or it is attached further along their tongue than most people’s.
Dysarthria is a condition where people slur their words because they cannot control the muscles that are required for speech, due to brain, nerve, or organ damage.
Symptoms and Characteristics of Dysarthria
Dysarthria is characterized by:
- Slurred, choppy, or robotic speech
- Rapid, slow, or soft speech
- Breathy, hoarse, or nasal voice
Additionally, someone with dysarthria may also have other symptoms such as difficulty swallowing and inability to move their tongue, lips, or jaw easily.
Causes of Dysarthria
Dysarthria is caused by paralysis or weakness of the speech muscles. The causes of the weakness can vary depending on the type of dysarthria the person has:
- Central dysarthria is caused by brain damage. It may be the result of neuromuscular diseases, such as cerebral palsy, Huntington’s disease, multiple sclerosis, muscular dystrophy, Huntington’s disease, Parkinson’s disease, or Lou Gehrig’s disease. Central dysarthria may also be caused by injuries or illnesses that damage the brain, such as dementia, stroke, brain tumor, or traumatic brain injury .
- Peripheral dysarthria is caused by damage to the organs involved in speech. It may be caused by congenital structural problems, trauma to the mouth or face, or surgery to the tongue, mouth, head, neck, or voice box.
Apraxia, also known as dyspraxia, verbal apraxia, or apraxia of speech, is a neurological condition that can cause a person to have trouble moving the muscles they need to create sounds or words. The person’s brain knows what they want to say, but is unable to plan and sequence the words accordingly.
Symptoms and Characteristics of Apraxia
These are some of the characteristics of apraxia:
- Distorting sounds: The person may have trouble pronouncing certain sounds, particularly vowels, because they may be unable to move their tongue or jaw in the manner required to produce the right sound. Longer or more complex words may be especially harder to manage.
- Being inconsistent in their speech: For instance, the person may be able to pronounce a word correctly once, but may not be able to repeat it. Or, they may pronounce it correctly today and differently on another day.
- Grasping for words: The person may appear to be searching for the right word or sound, or attempt the pronunciation several times before getting it right.
- Making errors with the rhythm or tone of speech: The person may struggle with using tone and inflection to communicate meaning. For instance, they may not stress any of the words in a sentence, have trouble going from one syllable in a word to another, or pause at an inappropriate part of a sentence.
Causes of Apraxia
Apraxia occurs when nerve pathways in the brain are interrupted, which can make it difficult for the brain to send messages to the organs involved in speaking. The causes of these neurological disturbances can vary depending on the type of apraxia the person has:
- Childhood apraxia of speech (CAS): This condition is present from birth and is often hereditary. A person may be more likely to have it if a biological relative has a learning disability or communication disorder.
- Acquired apraxia of speech (AOS): This condition can occur in adults, due to brain damage as a result of a tumor, head injury , stroke, or other illness that affects the parts of the brain involved in speech.
If you have a speech impediment, or suspect your child might have one, it can be helpful to visit your healthcare provider. Your primary care physician can refer you to a speech-language pathologist, who can evaluate speech, diagnose speech disorders, and recommend treatment options.
The diagnostic process may involve a physical examination as well as psychological, neurological, or hearing tests, in order to confirm the diagnosis and rule out other causes.
Treatment for speech disorders often involves speech therapy, which can help you learn how to move your muscles and position your tongue correctly in order to create specific sounds. It can be quite effective in improving your speech.
Children often grow out of milder speech disorders; however, special education and speech therapy can help with more serious ones.
For ankyloglossia, or tongue-tie, a minor surgery known as a frenectomy can help detach the tongue from the bottom of the mouth.
A Word From Verywell
A speech impediment can make it difficult to pronounce certain sounds, speak clearly, or communicate fluently.
Living with a speech disorder can be frustrating because people may cut you off while you’re speaking, try to finish your sentences, or treat you differently. It can be helpful to talk to your healthcare providers about how to cope with these situations.
You may also benefit from joining a support group, where you can connect with others living with speech disorders.
National Library of Medicine. Speech disorders . Medline Plus.
Centers for Disease Control and Prevention. Language and speech disorders .
Cincinnati Children's Hospital. Stuttering .
National Institute on Deafness and Other Communication Disorders. Quick statistics about voice, speech, and language .
Cleveland Clinic. Speech impediment .
Lee H, Sim H, Lee E, Choi D. Disfluency characteristics of children with attention-deficit/hyperactivity disorder symptoms . J Commun Disord . 2017;65:54-64. doi:10.1016/j.jcomdis.2016.12.001
Nemours Foundation. Speech problems .
Penn Medicine. Speech and language disorders .
Cleveland Clinic. Tongue-tie .
University of Rochester Medical Center. Ankyloglossia .
Cleveland Clinic. Dysarthria .
National Institute on Deafness and Other Communication Disorders. Apraxia of speech .
Cleveland Clinic. Childhood apraxia of speech .
Stanford Children’s Hospital. Speech sound disorders in children .
Abbastabar H, Alizadeh A, Darparesh M, Mohseni S, Roozbeh N. Spatial distribution and the prevalence of speech disorders in the provinces of Iran . J Med Life . 2015;8(Spec Iss 2):99-104.
By Sanjana Gupta Sanjana is a health writer and editor. Her work spans various health-related topics, including mental health, fitness, nutrition, and wellness.

Effects of Limited or Excessive Jaw Mobility during Conversational Speech
- January 6, 2016
- 6 minute read
by Sara Rosenfeld-Johnson
This presentation was made at the 2015 annual ASHA Convention, Session #1080.
Practicing Speech-Language Pathologists report that many clients demonstrate limited or excessive up-and-down jaw movements during communication as compared to their typically developing peers. The results of this retrospective study suggest that atypical jaw skills are related to deficits in speech clarity in clients diagnosed with multiple articulation disorder and dysarthria.
Practicing Speech-Language Pathologists report that many clients, with diagnosed multiple articulation disorders, demonstrate limited or excessive up-and-down jaw movements during communication as compared to their typically developing peers. The focus of this retrospective study was to determine if children and adults, diagnosed with multiple articulation disorders, were using the jaw heights needed to allow the tongue and lips to move independently for consonant and vowel productions on the conversational level. “Individual differences in jaw movement are real and often large; and the jaw is, in a real sense a primary articulator, controlling tongue height for an open vowel (Gay, 1974). Video clips of clients’ jaw mobility during conversational speech, before and after bite block invention, will be shown throughout this presentation.
These same clients were often able to produce the targeted speech sound(s) on the word level in a standardized articulation test but could not produce these same phonemes consistently on the conversational level. The sentence, “As the rate and complexity of the statement increases, the intelligibility decreases,” is found in many SLP’s reports to describe this breakdown in speech clarity.
More than forty years ago Edward Mysak suggested that if articulatory efforts are disrupted by excessive orofacial activities, as observed in many children with cerebral palsy, therapeutic techniques designed to restrain these compounding events must be administered to facilitate speech improvement (Mysak 1968). Ten years later James Dworkin proposed a causal relationship between the articulatory imprecision exhibited by certain school-age children and their co-occuring interruptive, hyperactive or hypoactive mandibular movement patterns” (Dworkin 1978). Clinical focus was then shifted to a treatment method that could measure the degree of jaw activity. Acrylic bite blocks of varying heights were positioned between the upper and lower central incisor teeth. The children were required to bite down gently on a given block, so as to stabilize the mandible. Substantial improvements in speech proficiency and intelligibility were obtained in all of the children studied in a relatively short period of time (Dworkin 1978). Kent and Lybolt (1982), Rosenbek and LaPointe (1985), Netsell (1985), and Dworkin (1991) all discussed the potential diagnostic and therapeutic value of bite block use in the differential diagnosis and treatment of dysarthric patients.
Other studies support the idea that SLPs need to take a closer look at how jaw grading is related to speech production. A 2000 study reported, “precise control of jaw movements precedes lip-control, control over jaw and lip coupling, and independence of upper- and lower-lip movement” and “the present results might be taken to suggest that limited mandibular control in early speech is a negative prognostic factor for later speech motor delays” (Green, 2000). Research into myofunctional disorders identified the relationship between the tongue and jaw dissociation for speech (Meyer, 2000).
In 2003, the following comments were made in a response to the Green, Moore, and Reilly article (Green, 2002) in reference “to the select populations of children and adults with developmental or neurogenic articulation disorders who exhibit mandibular dyscontrol. On the basis of our present work with such patients and a reinforcing clinical literature database, we suggest that the mandible may play a leading role not only in normal articulatory development but also in the origin and persistence of certain abnormal speech behaviors (Dworkin, 2003).
In our present study the charts of several different clinical populations were examined. Subjects were chosen based upon the examiner’s comment that limited or excessive mandibular activity was observed during conversational speech. A video-based movement tracking system had been used to chart the jaw range of motion in connected speech for each of the subjects. In the initial evaluation both the Goldman-Fristoe Test of Articulation (G-FTA-2) and the DCOMT (Dworkin-Culatta Oral Mechanism Examination and Treatment System) had been administered. Based on the results of these inventories, all subjects had been diagnosed with a multiple articulation disorder and dysarthria. Client’s with the diagnosis of motor speech disorders such as Childhood Apraxia of Speech (CAS) or Acquired Apraxia of Speech (AOS) were not included in this study.
Bite blocks representing the following jaw heights were used to assess skills at the high jaw placement (m, b, p, f, v, n, s, z, ∫, t∫, r, vocalic r, I, I, Ʋ, u – teeth almost touching), medium jaw placement (θ, ð, l, t, d,Λ, ɛ, ə, ɔ – teeth slightly more open) and low jaw placement (g, k, h,ɑ, æ – teeth even slightly more open) (Marshalla, 1982).
Prior to data collection, these same bite blocks were used to assess the jaw skills of twenty-five randomly selected children and adults between the ages of 2.5 and 50 years whose speech clarity was considered to be within normal limits as reported by an independent judge. The task was to use the back molars to bite-and-hold the jaw still for fifteen (15) seconds, at each bite block height, while an isometric pull was introduced. Each of these twenty-five individuals was able to perform the bite block task without error. The SRJ Therapies client charts, spanning a period of 12 years, were then examined. The following clients qualified for the study: 1) Down syndrome: 230, 2) Cerebral Palsy: 24, 3) Benign Hypotonia: 180, 4) Other syndromes characterized by hypotonia: 33, and 5) Clients with no medical diagnosis who had been enrolled in speech therapy for a minimum of four years and who had not demonstrated significant improvement: 42. The clients ranged in age from 2.5 years to 47 years.
The results of this retrospective study are remarkable in that only 8% of the 509 client-subjects were able to perform the bite block task without error; 92% could not complete the task. These results suggest that jaw skills are related to deficits in speech clarity in clients with the diagnosis of a muscle-based multiple articulation disorder and dysarthria. Because this was a retrospective study the limitations are clear. The next step would be large sample, double-blind studies that would definitively address the use of bite blocks for diagnosis and treatment of clients with muscle-based speech clarity disorders.
Learner Outcomes:
- Participants will be able to identify client’s with atypical jaw mobility during conversational speech.
- Participants will understand the possible relationship between atypical jaw mobility and dysarthria
- Participants will be able to use bite blocks to assess jaw skills in clients with the diagnosis of dysarthria
References:
Dworkin, J. P. (1978). A therapeutic technique for the improvement of lingua-alveolar valving abilities. Journal of Language, Speech, and Hearing Services in Schools, 9, 162-175.
Dworkin, J. P. (1991). Motor speech disorders: A treatment guide- book. St. Louis: Mosby.
Dworkin, J. P. (1996). Bite block therapy for oromandibular dystonia. Journal of Medical Speech-Language Pathology, 4, 47-56.
Dworkin, J.P, Meleca, R.J., Stachler R.J. (2003) More on the Role of the Mandible in Speech Production: Clinical Correlates for Green, Moore, and Reilly’s (2002) Findings. Journal of Speech, Language, and Hearing Research, 46 (pp. 1020-1021).
Gay, T. J., Ushijima, T., Hirose, H., & Cooper, F. S. (1974). Effect of speaking rate on labial consonant-vowel articulation. Journal of Phonetics, 2, 47-63.
Green, J. R., Moore, C. A., Higashikawa, M., & Steeve, R. W. (2000). The physiologic development of speech motor control: Lip and jaw coordination. Journal of Speech, Language, and Hearing Research, 43, 239-255.
Green, J. R., Moore, C. A., & Reilly, K. J. (2002). The sequential development of jaw and lip control for speech. Journal of Speech, Language, and Hearing Research, 45, 66-79.
Kent, R., & Lybolt, J. (1982). Techniques of therapy based on motor learning theory. In W. H. Perkins (Ed.), Current therapy of communication disorders: General principles of therapy (pp. 13-25). New York: Thieme-Stratton.
Marshalla, (Rosenwinkel), P. (1982) Tactile-proprioceltive stimulation techniques in articulation therapy. Seminar handbook. Champaign: Innovative concepts in Speech and Language.
Meyer, P.G. (2000). Tongue lip and jaw differentiation and its relationship to orofacial myofunctional treatment. Int J Orofacial Myology, 26, 44-52
Mysak, E. D. (1968). Neuroevolutional approach to cerebral palsy and speech. New York: Teachers College Press.
Netsell, R. (1985). Construction and use of a bite-block for the evaluation and treatment of speech disorders. Journal of Speech and Hearing Disorders, 50, 103-106.
Rosenbek, J. C., & LaPointe, L. L. (1985). The dysarthrias: Description, diagnosis, and treatment. In D. F. Johns (Ed.), Clinical management of neurogenic communicative disorders (pp. 97-152). Boston: College Hill Press.
- #IAMTHEHONEYBEAR
- AMERICAN SPEECH-LANGUAGE-HEARING ASSOCIATION
- ASHA CONVENTIONASSESSMENT AND TREATMENT OF THE JAW
- BOTTOM JAW SHIFT
- COMPLETE JAW PROGRAM
- FROM THE EXPERTSHYPOTONIA
- JAW CLOSURE
- JAW CLOSURE TUBES
- JAW DIFFERENTIATION
- JAW GRADING BITE BLOCKS
- JAW INSTABILITYJAW MOBILITY
- JAW STABILITY
- JAW WEAKNESS
- MULTIPLE ARTICULATION DISORDER
- SARA ROSENFELD-JOHNSON
- SPEECH DELAYSPEECH DISORDER
- SPEECH MOTOR DELAY
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
2 YEARS 4&5 MONTHS: MISS INDEPENDENT
Talktools instructor in norway, line avers in media planet, you may also like, aphasia and slps.
- June 3, 2013
Preventing Vocal Burnout in Future Teachers: An Education & Prevention Program
- December 1, 2016
Tongue Ties & Speech Sound Disorders: What Are We Overlooking?
- December 14, 2016
WHAT IS APHASIA?
Brain stem stroke: a case study.
- December 21, 2016
Podcast: A Case for Oral Placement Therapy (OPT)
- July 20, 2015
Previous Story
- Entertainment
Remembering Alan Rickman, the voice of villainy
The die hard and harry potter star was an actor’s character actor.
- By Tasha Robinson
- on January 14, 2016 06:59 pm

There’s a marvelous bit of Alan Rickman business in Harry Potter And The Goblet Of Fire . Harry, Ron, and Hermione are ignoring their classwork and whispering intensely about the upcoming Yule Ball. Alan Rickman, playing formidable professor Severus Snape, repeatedly smacks Ron on the back of the head, reminding him to get back to work. The conversation continues anyway. Mike Newell’s camera finds Rickman, who barely changes expression. Then he raises his chin slightly, and with two precise gestures, he pops back his cuffs to free his hands for another go at the heads of his disobedient young charges. The camera is only on him for a few seconds, but in that brief time, he neatly conveys incredulous disdain, exasperation, and the tiniest hint of smug relish. He’s pleased with himself even as he’s mildly revolted by the frustrating world around him. Rickman makes it hilarious, even though he doesn’t say a word.
"Am I interested, and is it truthful?"
Rickman, whose death from cancer at age 69 was confirmed by his family on Thursday, spent the most visible part of his career on roles that were essentially character-sized embodiments of this gesture. But as useful as his crisp, expressive body language and economy of expression were, his voice was his greatest weapon as a theater and film actor. It was a distinctive sardonic drawl, made for expressing disappointment, judgment, and a feline mixture of malice and pleasure. He was often cast as the big bad — "another in his long line of memorable creeps," a 2011 New York Times piece said of his latest Broadway role — and those roles often lingered longest and most gleefully in his fans’ memories. But he usually expressed a patient weariness when people pigeonholed his characters. "I don’t judge them," he told one fan in 2009, when asked whether he preferred good or evil roles. "I’m not looking for ‘Is it this or is it that?’ Just, ‘Am I interested, and is it truthful?’"

Warner Bros. Entertainment
That intellectual principle likely came from Rickman’s long history in the theater, as a director and actor who learned to analyze as much as perform. Rickman was a London native who grew up in a British council flat, with three siblings and, after age eight, when his father died, a single mother. Rickman first became interested in acting during his adolescent years, but — possibly motivated by early poverty — he began his working life as a graphic designer ( and writer, and copy editor ). At age 26, though, with the design collective he worked with floundering, he gave in to his "impractical" urges and entered the Royal Academy of Dramatic Art, launching the stage career that remained his passion throughout his life.
Rickman was intensely private about his family life — he rarely spoke publicly about his longtime partner and eventual wife Rima Horton until 2015. He didn’t seem to enjoy publicity on many topics, really. A 1992 GQ profile listed his "agenda of no-go topics ranging from his family, his girlfriend, his talent for playing villains, any aspect of acting at all ("too, too hard to articulate") right down to the nether reaches of trivia ("my clothes — not an interesting subject of conversation"). The profile turned out well — but it noticeably went to sources outside Rickman for most of its information.
The one subject Rickman was most often willing to talk about was his passion for live theater, and he tolerated the same questions over and over if they gave him a chance to promote his latest passion project on the stage. He worked primarily as a stage actor for the first part of his career, performing with the Royal Shakespeare Company and breaking into television in 1978 as Tybalt in a BBC production of Romeo & Juliet. Other BBC productions followed, intermittently: in 1982, he drew attention as Obadiah Slope, the slimy curate of the Anthony Trollope TV adaptation of The Barchester Chronicles. And his major breakthrough in theater came in 1987 when the Royal Shakespeare Company production of Les Liaisons Dangereuses he was starring in moved to Broadway. He earned a Tony nomination for his role as the Vicomte de Valmont. He also earned the notice of Die Hard producer Joel Silver and director John McTiernan.
He was 41, and had never acted in cinema, but he was offered the role of terrorist mastermind Hans Gruber in Die Hard within two days of arriving in Los Angeles to meet casting directors and producers. "I didn’t know anything about LA," he says. "I didn’t know anything about the film business." And so he nearly turned down the role on principle: "I read it and I said, ‘What the hell is this? I’m not doing an action movie…’" Agents convinced him otherwise, and Die Hard became his film debut and a memorable launch for a different type of career.
The remarkable thing about Rickman’s work on Die Hard isn’t that his film debut came so late in life, or that it so instantly launched him to stardom. It’s the way he walked in and made the role his own by treating the production like a stage role, where he expected input into his character’s costume, motivations, and behavior. He clashed with Silver and McTiernan, but repeatedly got what he asked for, and the film is better for it. Hans Gruber’s urbane detachment is largely Rickman’s invention. He wanted to wear a suit rather than the "terrorist gear" he was initially given because he felt the character didn’t need a costume when he had flunkies to do the dirty work. Gruber’s unforgettable first meeting with protagonist John McClane was rewritten when Rickman showed off his convincing American accent. According to that 1992 GQ interview, he temporarily shut down production by refusing to knock co-star Bonnie Bedelia to the ground as the script demanded. "My character was very civilized in a strange sort of way and just wouldn’t have behaved like that," he told the interviewer. "Nor would Bonnie’s character, a self-possessed career woman, have allowed him to. It was a stereotype — the woman as eternal victim — that they hadn’t even thought about. Basically, they wanted a reason for her shirt to burst open. We talked our way around it — her shirt still burst open, but at least she stayed upright."
After Die Hard ’s success, Rickman worked steadily in Hollywood, racking up more of those roles he didn’t want to call "villains," but which looked an awful lot like villains to an outside eye. As the jaded, aggressive Sheriff Of Nottingham, he stole the screen from the more staid Kevin Costner in Robin Hood: Prince Of Thieves. In 2001, he first hit the screen as J.K. Rowling’s Severus Snape, the perpetually misjudged, yet deeply hateful potions professor who watches Harry Potter grow up over seven movies. In Tim Burton’s Sweeney Todd , he plays the vile Judge Turpin, who condemns an innocent man in order to isolate and rape his wife, then develops designs on the couple’s teenage daughter.
Looking over his film career, Rickman played more romantic heroes, or at least compromised protagonists, than outright monsters. But the monsters stand out, because of his indelible delivery: his cold, patrician face, ice-chip eyes, and that purring voice, reportedly affected by Rickman’s lack of full facial flexibility. (According to Maureen Paton’s Alan Rickman: The Unauthorised Biography , he was born with a "tight jaw, hence the slightly muffled drawl.") His signature sound could have been interpreted as a speech impediment: it gave him a delivery that often sounded like he was forcing his words out between his teeth.
But he put it to good use. Even his humorous roles — like Marvin the Paranoid Android in The Hitchhiker’s Guide To The Galaxy , the frustrated voice of God in Kevin Smith’s Dogma , or the seething Shakespearean actor stuck in a silly alien role in Galaxy Quest — relied heavily on world-weariness and passive-aggression. Rickman rarely got to play roles without a hint of menace, or a sense of plaintive exhaustion toeing the line toward possible incandescent rage.
Occasionally, though, with films like Truly, Madly, Deeply or Ang Lee’s 1995 Jane Austen adaptation Sense And Sensibility , he was able to express his full versatility, and turn that broody menace into a warmer kind of passion. That unique charisma, that cool, haughty, languid role he played so well, adapted equally to roles meant to seduce the audience as it did to roles meant to repel them. The ambiguity he evoked in people — the appeal of a man who feels dangerous, and the distrust of even the kindest man who seems arrogant — had a great deal to do with his success. He projected complexity, even when he was playing characters without any on the page.
Part of the dignity he brought to his work came from his reserve offstage and offscreen, from the slight air of mystery that made him stand out in a TMI culture. But he was never dubious or mysterious about the stage. When asked what role he felt closest to in an interview with Empire last year, he said, "All of them. It’s me doing them. So what have I got to draw on, really?" To Rickman, acting and actors would always be conduits for the truth. "This is what I have to use," he continued, indicating his body. "Other people can pick up the violin or something. I’ve got this and it’s fallible."
- Brain & Nervous System
What to Know About Speech Impairment

A speech impairment affects people who have problems speaking in a regular tone of voice or tempo. Speech impairments make it hard for people to communicate properly, and they can happen in both children and adults.
These disorders can cause frustration and embarrassment to the person suffering from them.
What is Speech Impairment?
People who have speech impairments have a hard time pronouncing different speech sounds. They might distort the sounds of some words and leave other sounds out completely.
There are three general categories of speech impairment:
- Fluency disorder. This type can be described as continuity, smoothness, rate, and effort in speech production.
- Voice disorder. A voice disorder means you have an atypical tone of voice. It could be an unusual pitch, quality, resonance, or volume.
- Articulation disorder. If you have an articulation disorder, you might distort certain sounds. You could also fully omit sounds.
Stuttering , or stammering, is a common fluency disorder that affects about 3 million Americans. It usually affects young children who are just learning to speak, but it can continue on into adulthood.
Speech and language impairments are two words that are often used interchangeably, but they are two very different types of problems.
Speech means talking. It uses the jaw muscles, tongue, lips, and vocal chords. Language is a set of words and symbols made to communicate a message. Language and speech disorders can affect you separately, or both can happen at the same time.
Types of Speech Impairments
Speech impairments can begin in childhood and carry on through your adult years. Others can happen due to trauma, or after a medical event like a stroke.
The types of speech impairments are:
- Childhood apraxia of speech. This can happen to children when it’s time for them to start talking. The brain’s signals don’t communicate with the mouth, so the child can’t move their lips and tongue in the way they’re mean to.
- Dysarthria. This type of speech impairment happens when the muscles you use to talk are too weak, and can’t form words properly.
- Orofacial myofunctional disorders (OMD). OMDs are characterized by an abnormal pattern of facial muscle use. OMD interferes with how the facial muscles, including the tongue, are used. People who suffer from OMD might also struggle to breathe through their nose.
- Speech sound disorders. It’s normal for children to struggle to pronounce certain sounds as they learn to talk. But after ages four or five, constant mispronunciation might signal a problem. It can continue into adulthood, or some people get it after a stroke.
- Stuttering. Stuttering can mean repeating words or sounds like “uh” and “um” (disfluencies) involuntarily. Stuttering can be intensified by strong emotions or stress.
- Voice. A voice disorder can mean you “lost” your voice because you stressed it too much. It can also mean a chronic cough or paralysis of the vocal cords, among others.
Health Issues That Affect Speech Impairment
Other than childhood speech impairments, there are a range of reasons you could get one in your adult years. They can happen due to a traumatic event, illness, or surgery.
Dysarthria , aphasia, and voice disturbances can happen in adulthood, and are usually due to these medical events.
Aphasia. Aphasia is the loss of ability to understand words, spoken or written. There are many types of aphasia . It can happen after a stroke or if a tumor reaches the part of the brain where language is processed.
Medical issues that can cause aphasia:
- Head trauma
- Transient ischemic attack (TIA)
- Brain tumor
- Alzheimer’s disease
Dysarthria. Dysarthria is usually caused by a nerve problem. The person suffering from it loses the ability to make certain sounds or might have poor pronunciation. It can also affect your ability to control the tongue, larynx, lips, and vocal chords.
Medical issues that can cause dysarthria:
- Facial trauma
- Diseases that affect your nervous system
- Side effects of certain medication
- Alcoholic intoxication
- Dentures that don’t fit properly
- Transient ischemic attack (TIA)
Voice disturbances. Traumatic events or extreme stress placed on the vocal cords can cause you to “lose” your voice or have a vocal disturbance. Disease can also affect the way your voice sounds.
Cancerous or noncancerous growths or nodules on the vocal cords can make your voice sound different.
Understanding Speech Impairments
Having a speech impairment can be a very frustrating and embarrassing experience for the person experiencing it. It’s important to be patient and understanding when communicating.
Try the following tips to improve communication and foster an accepting environment with someone who has a speech impairment:
- Speak slowly and use hand gestures
- Keep a pen and paper handy in case it’s needed to communicate
- Maintain a calm environment free of stimulating sounds
- Use simple phrases when you speak
- Use your normal tone of voice
Consulting with a mental health care provider can help with feelings of anger and depression that can accompany speech impairments.

Top doctors in ,
Find more top doctors on, related links.
- Brain & Nervous System News & Features
- Brain & Nervous System Reference
- Brain & Nervous System Slideshows
- Brain & Nervous System Quizzes
- Brain & Nervous System Videos
- Find a Neurologist
- Living Better With MS
- Alzheimer's Disease
- Creutzfeldt-Jakob Disease
- Guillain-Barré Syndrome
- Lou Gehrig’s Disease (ALS)
- Multiple Sclerosis
- Parkinson's Disease
- Restless Legs Syndrome
- Spinal Muscular Atrophy
- More Related Topics

Temporomandibular joint (TMJ) disorders can impact several aspects of a person's life, including speech function. As Illinois' leading non-surgical TMJ treatment center, we understand the importance of addressing TMJ disorders holistically, considering the spoken language difficulties that may arise as a result of these conditions. By recognizing and addressing the impact TMJ disorders can have on speech, healthcare providers like Dr. Hitesh Patel can help patients achieve optimal well-being and total speech restoration.
Our journey through understanding the relationship between TMJ disorders and speech impairment will provide valuable insights into the treatment options provided by Dr. Hitesh Patel and the comprehensive care his practice offers in addressing both TMJ disorder symptoms and speech concerns. By focusing on this often-overlooked aspect of TMJ disorders, we aspire to equip those affected with the information they need to navigate and overcome this challenge successfully.
The Connection Between TMJ Disorders and Speech Difficulties
The temporomandibular joint plays a crucial role in the mechanics of speech, as it controls the movement of the jaw during the formation of words, pronunciation, and articulation. TMJ disorders can result in joint pain, restricted movement, and muscle tension, all of which can impair speech function. The relationship between TMJ disorders and speech impairments is multi-faceted and can present itself in several ways:
1. Articulation challenges: TMJ disorders can limit jaw movement, making it difficult to enunciate and articulate certain speech sounds accurately.
2. Discomfort while speaking: Pain in the temporomandibular joint may make speaking uncomfortable and cause individuals to alter their speech patterns in an attempt to avoid discomfort.
3. Impaired speech volume: Muscle tension or limited jaw mobility caused by TMJ disorders can hinder one's ability to speak loud enough for others to hear.
4. Slurred speech: Weakness or lack of coordination in the muscles responsible for speech can lead to slurred speech in individuals with TMJ disorders.
Recognizing the Symptoms of Speech Disorders Related to TMJ
To effectively diagnose and treat speech-related TMJ disorder symptoms, it is essential to be aware of how these challenges may present themselves. Symptoms of speech impairments linked to TMJ disorders include:
1. Difficulty pronouncing specific sounds: Pain or restricted jaw movement may make it challenging to produce certain consonants or vowels.
2. Changes in speech rhythm or pace: When experiencing discomfort or pain while speaking, individuals with TMJ disorders may alter their speech rhythm or pace to avoid exacerbating their symptoms.
3. Reduction in speech clarity: Jaw stiffness, muscle tension, and other TMJ-related impairments can lead to decreased speech clarity.
4. Fatigue when speaking: TMJ disorder sufferers may find that their muscles fatigue more quickly during speech, leading to increased difficulty, discomfort, or mumbling.
By recognizing these symptoms, individuals and healthcare providers can better identify the presence of speech disorders related to TMJ and address them accordingly.
Non-Surgical Treatment Options for TMJ-related Speech Disorders
Addressing speech challenges resulting from TMJ disorders requires a multifaceted approach. Dr. Hitesh Patel specializes in non-surgical TMJ treatments that aim to alleviate pain and restore functional jaw mobility, which in turn can help improve speech capabilities. Some non-surgical treatment options include the following:
1. Oral appliance therapy: Custom-made oral appliances, such as bite splints or orthotic devices, can help reposition the jaw and alleviate pressure on the temporomandibular joint, potentially improving speech function.
2. Physical therapy: Exercises targeting the muscles responsible for supporting the temporomandibular joint and facilitating speech can help improve strength, coordination, and overall speech function.
3. Pain management techniques: Reducing TMJ-related pain and inflammation through medication, cold or heat therapy, and relaxation techniques can help create a more comfortable environment for normal speech.
4. Speech therapy: In conjunction with non-surgical TMJ treatment, working with a speech therapist can help address specific speech challenges and re-establish proper speech mechanics.
Developing a personalized treatment plan that addresses both TMJ disorder symptoms and speech impairments is vital for successful outcomes.
The Importance of a Comprehensive Care Approach for TMJ-related Speech Disorders
A comprehensive approach to addressing speech challenges arising from TMJ disorders involves integrating non-surgical treatments for TMJ disorders, focusing on improving jaw mobility and reducing pain, with targeted speech therapy designed to address specific articulation issues. This multifaceted approach ensures that all aspects of the speech impairment are addressed, including the following:
1. Reducing pain and inflammation: Alleviating TMJ-related pain is essential to enable patients to speak comfortably and avoid speech pattern alterations due to discomfort.
2. Restoring functional jaw mobility: Improving jaw movement and mobility provides the foundation for effective speech therapy and addressing articulation challenges.
3. Strengthening and conditioning speech muscles: Building strength and coordination in the muscles controlling speech can lead to improved functionality and speech clarity.
4. Addressing speech-specific concerns: Integrating speech therapy into a comprehensive TMJ treatment plan helps patients practice and refine proper speech mechanics and overcome specific challenges.
A comprehensive care approach led by Dr. Hitesh Patel allows for a personalized treatment plan designed to address all aspects of TMJ-related speech disorders, maximizing the potential for positive outcomes and restored speech function.
Reclaim Your Speech with Non-Surgical TMJ Treatment
Addressing the speech challenges associated with TMJ disorders is an essential aspect of comprehensive care. By understanding the connection between TMJ disorders and speech impairments, it is possible to focus on non-surgical TMJ treatments that target the specific needs of each individual while also incorporating appropriate speech therapy techniques.
If you or a loved one is experiencing speech difficulties due to a TMJ disorder, take the first step towards a better quality of life by scheduling a consultation at Suburban TMJ and Sleep Center, the trusted TMJ clinic in Naperville .

© 2024 All Rights Reserved | Website Designed By: Morningdove - Accessibility Statement

(720) 409-0008
- Meet the Team
- Map & Directions
- Office Policies & Mission
- Financial and Insurance
- Make a Payment
- Family Dentistry
- Cosmetic Dentistry
- CEREC – Same Day Dentistry
- Early Dental Care
- General Treatment
- Teeth Whitening
- Dental Implants
- Emergency Info
- Periodontics
- Root Planing & Scaling
- New Patient Information
- First Visit
- Dental Health
- Brushing & Flossing
How Tooth and Jaw Problems Affect Speech

Crooked Teeth Affect Speech
When the teeth don’t align properly, you have a higher tendency to develop speech problems. Crooked, overlapping, and twisted teeth change the placement of your tongue and may allow excess air to pass between your teeth, creating a whistle when you speak.
The most common way to deal with crooked teeth is to get braces. Invisalign is a popular option to straighten your teeth without metal brackets and wires. A visit with Dr. Evanson will reveal the extent of your problem. Then, we may choose to treat you in our Parker office or refer you to an orthodontist in the Denver area.
Premature Tooth Loss Affects Speech
Getting a tooth knocked out not only leaves a hole in your smile – it also affects your speech. Losing a baby tooth early is especially detrimental since this can negatively affect your child at a critical time of language development. It’s common for a child with a missing tooth to develop a speech impediment that requires help from a therapist later on.
With our restorative dentistry services here at Evanson DDS, you can fill the gaps left by lost teeth in a few ways:
- Space maintainers for children keep the gap open until the permanent tooth erupts.
- Removable partial dentures fill the gap with an artificial tooth attached to a retainer-like appliance.
- Dental implants fill the gap with an artificial tooth anchored to your jaw with a titanium screw.
- Bridges fill the gap with an artificial tooth attached to a crown on the adjacent teeth.
Self-Consciousness About Tooth Appearance Affects Speech
Sometimes, tooth and jaw structure isn’t to blame. Sometimes, discoloration, large front teeth, or even bad breath make you feel self-conscious about your smile, so you refrain from opening your mouth very wide, which causes you to mumble when you talk.
Fortunately, a little cosmetic dentistry is all you need to feel more confident when you smile and talk. At Evanson DDS, we offer:
- In-office and take-home tooth whitening treatments.
- Porcelain veneers to improve the appearance of badly stained teeth.
- Bonding to reinforce cracked or damaged teeth.
Jaw Structure Affects Speech
Sometimes, the jaw is to blame for speech problems. If your jaw bone is too small, your teeth may be crammed together, and your tongue has less room to move around. Upper and lower jaws that are different sizes from one another may also cause you to develop a poor bite pattern . As you can imagine, this has the potential to affect your speech.
If your jaw structure is having a huge impact on your quality of life, visit Evanson DDS for a consultation. Oral surgery is often needed to correct a small jaw. If we determine this is the best course of action for your situation, we’ll either plan to treat you in our office or refer you to a specialist, depending on your case.
Braces Affect Speech
Any dental appliance – from traditional metal braces to clear plastic Invisalign – has the potential to affect speech. Fortunately, the whistling and lisp caused by new braces are usually temporary. After a few days, most people grow accustomed to speaking with braces. Of course, it takes practice, so you might want to talk to yourself when you’re alone to speed up the adjustment process.
Visit Evanson DDS to Correct Tooth and Jaw Problems
We can tackle many tooth and jaw problems at our dentist office in Parker. If you or your child is struggling with a speech impediment, see what we can do before you see a speech pathologist. Simply contact us online or call Dr. Evanson at (720) 409-0008 today to schedule an appointment.
- Angela Evanson
Photostream

- August 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- February 2016
- January 2016
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Tight Jaw Muscles: Causes and Treatment
At-home care, frequently asked questions.
Tight jaw muscles can interfere with the most basic daily tasks, such as talking and chewing your food. Conditions that cause tight jaw muscles can also be quite painful. However, many of these conditions can be treated with medical interventions and home remedies.
This article discusses common causes of tight jaw muscles and how to manage your symptoms.
LaylaBird / Getty Images
Causes of Tight Jaw Muscles
Tight jaw muscles can be caused by a variety of medical conditions and lifestyle habits, such as the following.
Stress and Anxiety
Tight jaw muscles can be a side effect of stress and anxiety . Muscle tension throughout the body increases when you are under a lot of stress or feeling anxious. If you are prone to clenching your jaw, you'll likely experience tension in your jaw muscles as well.
Temporomandibular Joint Disorders
Conditions that affect your jaw joint are called temporomandibular joint disorders (TMJ or TMD). These conditions are very common, affecting over 10 million Americans. There are three main categories of TMD:
- Pain in the muscles that move your jaw
- Joint issues involving the cartilage or bone
- Arthritis in your jaw joint
Regardless of the underlying cause, all types of TMJ can cause tightness in your jaw muscles.
Teeth Grinding
Bruxism is a condition that occurs when you grind or clench your teeth throughout the day or while you sleep. You might not even be aware of this habit until you develop symptoms. In addition to tight jaw muscles, bruxism can cause:
- Chipped teeth
- Sensitive teeth
- Jaw dislocation
- Popping in your jaw
- Flattened teeth
- Grooves in your tongue
- Damage to the inside of your cheeks
Tetanus is a condition caused by a bacterial infection from Clostridium tetani , which is common in the outdoors.
This condition is often called lockjaw because tight jaw muscles are one of the most common symptoms of tetanus. Other symptoms can include:
- Difficulty swallowing
- Muscles spasms
- Blood pressure changes
- Heart rate changes
Tetanus can lead to serious medical conditions, such as pneumonia (an infection of the air sacs in the lungs) or blood clots (collections of blood that form in your veins and arteries).
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is an autoimmune disorder. This means that your immune system attacks your joints as if they were foreign to your body. Inflammation causes pain throughout the joints in your body—which can include your jaw joints. Up to 90% of people with RA also have TMJ.

Osteoarthritis
Osteoarthritis (OA) occurs when padding between the bones in a joint wears down over time. Unlike RA, which tends to attack the same joints on both sides of the body at the same time, OA can affect one or more unrelated joints in your body. This means you could have OA on one side of your jaw, but not the other. In addition to tight jaw muscles, other symptoms of OA in the jaw include:
- Difficulty opening your mouth
- Difficulty moving your jaw to the opposite side
- Pain when chewing with the affected side
- Grinding in the joint
Excessive Chewing
Jaw muscles can become temporarily sore and tight after you've chewed gum or sticky candy or eaten tough or fatty food. However, symptoms typically resolve within a few days.
Diagnosing Jaw Pain
If you have jaw tightness that interferes with your ability to chew or talk, it's time to get it checked out. Tight jaw muscles can be diagnosed by a physical exam performed by your doctor, dentist, or physical therapist. If further TMJ issues are suspected, you might also need an X-ray, CT (computed tomography) scan, or an MRI (magnetic resonance imaging) . Once the underlying cause of your symptoms is clear, treatment can begin.
In many cases, at-home care can relieve symptoms of a tight jaw. Even in cases in which professional help is needed, at-home treatment is often incorporated into a holistic care routine. Types of at-home care include:
- Heat and cold : Hot packs and ice packs can be applied to the side of your face in the area of your TMJ to help reduce your symptoms. Heat increases blood flow to the area, which helps tight muscles relax. Cold reduces blood flow to help decrease inflammation and pain.
- NSAIDs : Over-the-counter (OTC) nonsteroidal anti-inflammatory drugs are frequently used to treat TMJ issues. While these medications won't directly decrease tightness in your jaw muscles, they will decrease inflammation and pain. Common NSAIDs include Aleve (naproxen), Advil or Motrin (ibuprofen), and aspirin.
- Jaw exercises : Movement can help decrease tightness in your jaw muscles. However, the wrong types of exercises can make your symptoms worse, depending on your underlying condition. Talk to your dentist or physical therapist for specific instructions and stop exercising if you experience pain.
Jaw Joint Stretches
- Gently open your jaw and stop when you feel resistance but no pain. Hold this position for a few seconds, then close your jaw. Shift your jaw to the left for a few seconds, then repeat to the right.
- Place your fingertips under your jaw. Apply gentle pressure upward and slowly opening your mouth. Move your fingertips to the front of your jaw. Apply gentle pressure downward as you close your mouth. Repeat several times.
- Mouth guards and splints : Mouth guards and splints are often used to treat tight jaw muscles from teeth grinding and clenching—particularly at night. Basic mouth guards are available over the counter. In some cases, custom-molded mouth guards and/or splints are needed. Consult your dentist for specific recommendations.
- Dietary changes : Avoiding certain foods can help reduce your symptoms if you have tight jaw muscles. Avoid foods that are fatty, chewy, or crunchy, and cut food up into small bites. Cook vegetables until they are soft, rather than eating them raw.
- Massage of facial muscles : Tightness in the chewing muscles in your temples and cheeks can be treated with massage. Given the anatomy of your jaw muscles, this is best performed by a healthcare professional. But you can achieve some relief by applying gentle pressure with a couple of fingertips to your tight muscle and rotating in small circles for several minutes.
Other Treatments for a Tight Jaw
A variety of other treatments are available to reduce tightness in your jaw muscles. These can include:
- Prescription muscle relaxants and pain relievers : In some cases, prescription medications are used to treat TMJ issues. Muscle relaxants can be prescribed, but they don't just target your tight jaw muscles—they affect muscles throughout your body. Prescription pain medications can also be helpful when NSAIDs are not effective. However, they also have potentially serious side effects.
- Physical therapy : Tight jaw muscles and other TMJ disorders are frequently treated with physical therapy. Interventions include manual therapy, exercise, and modalities such as electrical stimulation and ultrasound.
- Injections : Although they aren't the first choice in the treatment of tight jaw muscles, injections are sometimes used when other treatments aren't successful. Injections can include lidocaine to reduce pain, corticosteroids to reduce inflammation, Hyalgan (hyaluronate) to lubricate and reduce friction in the TMJ, and Botox (botulinum toxin) to relieve persistently tight muscles.
Tight jaw muscles can be caused by stress, anxiety, teeth grinding, or other medical conditions such as arthritis. Treatment includes massage, stretching, medications, and physical therapy. Mouth guards can also be helpful to reduce jaw issues from teeth grinding.
A Word From Verywell
Living with tight jaw muscles can be frustrating—especially when you aren't sure what's causing your symptoms. However, treatment can be very effective. Talk to your doctor or dentist about your symptoms, even if they are mild. Early intervention can help prevent more serious jaw issues from developing.
Stress and mouth breathing caused by COVID-19 can lead to jaw pain.
Wear a mouth guard to help your jaw muscles relax while you sleep.
When you clench your jaw, you are working your chewing muscles. Over time, these muscles can get bigger.
National Institute of Dental and Craniofacial Research. TMD (Temporomandibular disorders) .
Johns Hopkins Medicine. Bruxism .
Centers for Disease Control and Prevention. Tetanus symptoms and complications .
Rheumatoid Arthritis Support Network. RA and jaw pain: Can rheumatoid arthritis cause joint pain? .
Global Healthy Living Foundation. Is your jaw pain because of arthritis? Signs your arthritis is affecting your jaw, and what to do about it .
Practical Pain Management. Osteoarthritis of the temporomandibular joint .
Colgate-Palmolive Company. TMJ exercises for pain relief .
Joshua Hong DDS. TMJ diet: What to eat, what not to eat .
River Edge Dental. Muscle relaxants aren't the only way to relax a tense jaw .
University of Michigan Health. Physical therapy for temporomandibular disorders .
Herman Ostrow School of Dentistry of USC. TMJ injection treatments: Lidocaine, steroids, hyaluronate & botox .
By Aubrey Bailey, PT, DPT, CHT Dr, Bailey is a Virginia-based physical therapist and professor of anatomy and physiology with over a decade of experience.

RADA and Genetics Gave Alan Rickman the ‘Perfect Voice’
The sadly missed Alan Rickman was among the most beloved British actors of his generation. From his early roles in theatre to his film breakthrough in Die Hard and later appearances in Love Actually and the Harry Potter series, Rickman was a unique and compelling screen presence – and a huge part of this was his voice.
According to a 2008 scientific study , Alan Rickman literally had the perfect voice, thanks to his immaculate balance of tone, frequency, intonation and speed. Rickman owed his unique voice to a speech impediment – a result of him being born with a tight jaw – and an accent that mixed Irish and Welsh parentage, a working-class London upbringing and training at Britain’s toughest acting school.
From working-class to upper crust
Given his well-spoken, somewhat upper class manner as an actor, it may come as a surprise that Alan Rickman came from thoroughly working-class beginnings. Born in Acton, London on February 21, 1946, Alan was the second oldest among four siblings (with elder brother David, younger brother Michael and younger sister Sheila).
From his early years, Rickman’s voice was unlike that of his siblings. He was born with a condition that left him unable to properly move his lower jaw, as a result of which he grew up with a speech impediment. Despite this, Rickman always had an ear for accents, owing in part to the different accents he was exposed to as a child: Rickman ( who described himself as a “full-blooded Celt”) would remark in 1986 , “My mother was Welsh and my father was Irish and I can speak both accents like a native, yet in my whole career I have never been asked to.”
When Rickman was eight years old, his father (a painter and decorator) died of lung cancer, leaving mother Margaret to raise the four children alone. Young Alan’s fortunes took a turn, however, when his academic prowess at primary school landed him a place at Hammersmith’s prestigious Latymer Upper School. It was here, Rickman explained, that he came to develop a received pronunciation accent.
Training the voice at RADA

Rickman was interested in acting from his teens, though this was a completely alien world from his upbringing, as his parents “didn’t have anything to do with the theatre. I’m some kind of accident.” After completing his secondary education, Rickman attended art college and briefly pursued a career in graphic design. In 1972, a then 26-year-old Rickman pivoted again: he began studying at London’s famed Royal Academy of Dramatic Art (RADA) with a view to pursuing acting for a living.
Here, Rickman’s unusual voice proved a sticking point : “At drama school, it was the subject of a great deal of criticism and a lot of hard work. They said I had a spastic soft palate.” He would later remark of his distinctive tones, “It’s to do with having a high roof of the mouth apparently. I should be a good singer, but a teacher at drama school wasn’t too encouraging.”
This didn’t keep Rickman from later singing on film, in Tim Burton’s Sweeney Todd: The Demon Barber of Fleet Street, but in an interview for that film in 2007 , Rickman recalled one memorably cutting comment on his delivery while at RADA: “Alan, you sound as if your voice is coming under the back end of the drain pipe was one review from my voice teacher.”
After RADA successfully ironed out his delivery and flattened his working-class accent, Rickman joined the Royal Shakespeare Company. There the somewhat aloof, sneering quality of Rickman’s voice made him a natural fit for darker, less clean-cut characters, such as Tybalt in Romeo and Juliet (which became his first televised work in 1978).
Movie debut at 42

The shady role that really launched Rickman was Vicomte de Valmont in Les Liaisons Dangereuses, a 1985 stage adaptation of the Pierre Choderlos de Laclos novel. A Royal Shakespeare Company production, the play proved popular enough in London’s West End to later be sent across the Atlantic to New York’s Broadway, where it garnered even more acclaim, including Tony and Drama Desk Award nominations for Rickman.
Rickman’s performance as Valmont also caught the eye of Joel Silver, a Hollywood producer who was starting work on a new feature, action movie Die Hard. Despite the fact that Rickman had never made a film before, Silver felt he would be ideal for the role of debonair criminal mastermind Hans Gruber, and would provide the perfect counterpoint for leading man Bruce Willis.
Silver’s first choice for Gruber, Sam Neill, turned the part down, and Rickman – who found himself offered the movie almost immediately after coming to Hollywood – also came close to declining: “I read it and I said ‘what the hell is this? I’m not doing an action movie!’ And agents and people said ‘Alan, you don’t understand, this doesn’t happen. You’ve only been in LA two days and you’ve been asked to do this film.'”
Eventually Rickman saw sense and signed on to play Gruber, which proved to be the best start possible to his film career. Die Hard opened in 1988, giving Rickman his movie debut aged 42. A huge success, the film made tremendous use of Rickman’s distinctive voice, as well as his aptitude for accents.

As he plays a German character, Die Hard sees Rickman give the bulk of his performance in a dry German accent; one memorable sequence, though, sees Rickman adopt an LA accent when Gruber meets Bruce Willis’ John McClane face-to-face for the first time, as Gruber attempts to conceal his true identity.
Accounts vary on the genesis of this scene: Rickman claimed to have suggested it himself, but in Netflix series The Movies That Made Us, screenwriter Steven E de Souza claims he had the idea after hearing Rickman put on a stereotypical Californian voice. Either way it proved a key scene in the film, in which Willis’ McClane remarks to Gruber, “you oughta be on f***in’ TV with that accent.”
The critical and commercial success of Die Hard saw Rickman transformed overnight from respected stage actor to fully-fledged movie star. Many more major roles came in the years that followed, including supernatural romance Truly, Madly, Deeply, Jane Austen adaptation Sense and Sensibility and cult sci-fi comedy Galaxy Quest.
A voice for villain roles

However, Rickman’s raspy line delivery and droll manner saw him most closely associated with bad guy roles. Upon his death, the BBC wrote that Rickman’s “sonorous, languid voice” made “even throwaway lines of dialogue sound thought out and authoritative” – a sound that made the actor perfect for playing baddies.
While his villainous turn opposite Tom Selleck in Quigley Down Under is largely forgotten, Rickman memorably played a melodramatic Sheriff of Nottingham opposite Kevin Costner in Robin Hood: Prince of Thieves , a performance which won him his only BAFTA award (one of Rickman’s few major screen acting accolades; he was never Oscar-nominated). Later, he took on the role of complex antagonist Severus Snape in all eight Harry Potter movies.
Still, while the cinema-going public adored Rickman’s villain performances (which could also include his turn as Emma Thompson’s unfaithful husband in Love Actually), this never created a perception of him being a bad guy in reality. Rickman did a good job keeping his private life out of of the spotlight, most likely because there was nothing remotely scandalous to report.
The actor spent the bulk of his life as the partner of politician Rima Horton, the couple having met in their teens. They had no children, and only wed in 2012, four years before Rickman passed away from pancreatic cancer. (This was the second time Rickman battled the disease, having previously suffered prostate cancer in 2005.)
“I don’t hear what anybody else hears”

The 2008 study to find the perfect voice gave some indication of how well thought-of Rickman was. Professor Andrew Linn, the linguist behind the study, remarked of the results: “As humans we instinctively know which voices send shivers down our spine and which make us shudder with disgust… The emotional responses panellists had to the voices were surprising and go some way to explaining how voiceover artists or radio DJs are selected, or why particular celebrity voices appeal.”
The study also found that actors Jeremy Irons and Michael Gambon sport ideal masculine voices, whilst on the female side those most highly regarded included actresses Judi Dench and Honor Blackman and journalist and presenter Mariella Frostrup. Rickman, though, came out on top.
While he spent his career being questioned about his voice, Rickman seemed largely indifferent on the subject. In a 1991 interview with The Telegraph, he rejected suggestions that his voice was cold: “There is a certain warmth, I would have thought… This is me. I have a certain pitch to my voice, a certain way of framing my sentences.” Elsewhere, he shrugged , “I don’t hear what anybody else hears. I’m six-foot-one, I wear size 11 shoes, and I have this voice.”
Common Speech Impediments: Causes, Symptoms, Treatment, And Support
Speech impediments include a variety of both language and speech disorders, some of which can be addressed through online speech therapy with speech-language pathologists. They can arise because of heredity and genetics, developmental delays, or even damage to Broca’s area—the part of the brain that’s involved in language skills and speech skills. They may also be linked to other conditions like autism spectrum disorder, cerebral palsy, dyslexia, or even hearing loss. It depends on the type and the cause, but most speech impediments and speech impairments can be treated through speech therapy.
That said, recognizing when a speech impediment may be present can help you get yourself or your child the treatment and support they may need for improved academic and/or social functioning and self-confidence.

Common symptoms of a speech impediment
There are many different types of speech impediments a person can have, so the symptoms can vary. That said, those listed below are common symptoms that could be initial indicators that you or your child may be experiencing speech problems or challenges:
- Elongating words
- Quiet or muffled speech
- Blinking frequently
- Distorted sounds while talking
- Frequent changes in pitch
- Poor voice quality
- Visible frustration when trying to communicate
- Overall difficulty communicating and expressing thoughts and ideas
- Inability to repeat words
- Inability to pronounce words the same way twice
- A phobia of speaking in public
- Speaking slowly and carefully
- Speech delay
- Frequent pauses when talking
- Limited vocabulary over several years, delayed language development
Some speech and language disorders are consistent with underlying mental health conditions such as autism. You can visit licensed health professionals or speech therapists to receive an accurate diagnosis and find out how to treat a speech impediment or language disorder, and its underlying cause, if applicable.
Key categories of speech impediments
Speech impediments or communication disorders can take many forms, from speech sound disorders to voice-related disorders. While speech sound disorders mostly result from sensory or motor causes, voice-related disorders deal with physical problems regarding speech. Read on for a list of some of the most common categories of speech impediments.
Voice disorders
Voice disorders primarily arise due to issues regarding the health and structure of the larynx or the voice box. They can impact pitch, resonance, volume, and voice quality. Symptoms of a voice disorder may include having a hoarse, quivering, strained, choppy, or weak and whispery voice, which can make it difficult to produce speech sounds.
The root cause of these disorders can be either organic, like alterations to respiratory, laryngeal, or vocal tract mechanisms, or functional, like improper use of the voice. Some risk factors that may contribute to vocal health challenges include allergies, psychological stress, age, excessive alcohol or drug use, screaming, scarring from neck surgery, or even gastroesophageal reflux disease (GERD). Examples of voice disorders include laryngitis, vocal cord paralysis/weakness, polyps or nodes present on the vocal cords, leukoplakia, or muscle tension dysphonia.
Fluency disorders
A person may be diagnosed with a fluency disorder if they have trouble with speech timing and rhythm which makes it difficult to create a normal speech pattern. These disorders are characterized by interruptions in the typical flow of speaking, including abnormal repetitions, hesitation, and prolongations. Their cause is unknown, but it may be genetic. Symptoms can also be exacerbated by stress and anxiety. Stuttering is the most common example of fluency disorders.
Symptoms of a fluency disorder may include dragging out syllables, speaking breathlessly, repetition of words, speaking slowly, and being tense while speaking. Secondary symptoms may include fidgeting, mumbling, saying “um” or “uh” often, not using certain problematic words, rearranging words in sentences, and anxiety around speaking. Treatment options vary depending on the specific disorder. With stuttering, for example, slowing down, practicing, using speech monitors, attending speech therapy, and receiving cognitive behavioral therapy (CBT) are all potential treatment options.
Articulation disorders and phonological disorders
Articulation and phonological disorders are two types of speech disorders classified as speech sound disorders that may impact communication. An articulation disorder includes speech that commonly exhibits errors such as substitution, omission, distortion, and/or addition (SODA). Although the actual causes of articulation disorders aren’t well understood, contributing factors may include brain injuries, a cleft palate/cleft lip, or nerve damage. Phonological disorders typically involve producing sounds correctly but using them in the wrong place and are more predictable than articulation errors. There may also be a genetic factor that contributes to both disorders and other families may be impacted as well. A licensed speech-language pathologist (SLP) can determine if an individual may have an articulation disorder or a phonological disorder. Ongoing speech therapy is typically the recommended treatment method.
Speech impediments versus language impairments
A speech impediment is typically characterized by difficulty creating sound due to factors like fluency disorders or other voice problems. These disorders may arise from underlying mental health issues, neurological problems, or physical factors or conditions impacting speech muscles.
Language impairments, on the other hand, are more about difficulty processing, reading, and writing and can be connected to an issue processing receptive language. They’re common in children, especially when they first start school. Language impairments relate to meaning, whereas speech impediments relate to sound. It’s also very common for a language impairment disorder to present alongside a learning disability like dyslexia.

Examples of speech impediments
Below is a brief overview of a few of the most common speech disorders and speech impediments, along with symptoms and potential treatment options.
Apraxia of speech is a speech sound disorder that affects the pathways of the brain. It’s characterized by a person having difficulty expressing their thoughts accurately and consistently. It involves the brain being able to form the words and knowing exactly what to say, but the person then being unable to properly execute the required speech movements to deliver accurate sounds. In mild cases, a person will only have small limitations in their ability to form speech sounds. In severe cases, alternate communication methods may need to be used.
An SLP is the type of provider who can diagnose apraxia. To diagnose speech disorders, including both childhood apraxia (sometimes called verbal apraxia) and acquired apraxia, they may ask the individual to perform simple speech tasks like repeating a particular word several times or repeating a list of words that increase in length. Apraxia generally needs to be monitored by both parents and an SLP over time for an accurate diagnosis to be possible.
There are various treatment options for apraxia, the most common being one-on-one meetings with a speech pathologist. They’ll likely help you or your child build helpful strategies and skills to help strengthen problem areas and communicate more clearly. Some other treatment methods include improving speech intelligibility or using alternate forms of communication, like electronic speech or manual signs and gestures.
The National Institute on Deafness and Other Communication Disorders describes aphasia as a communication disorder that results in a person’s inability to speak, write, and/or understand language. Like other communication disorders, it may occur because of damage to the portions of the brain that are involved in language, which is common in those who have experienced a stroke. It may also come on gradually in those who have a tumor or a progressive neurological disease like Alzheimer’s. Symptoms may include saying or writing sentences that don’t make sense, a reduction in a person’s ability to understand a conversation, and substituting certain sounds and words for others.
Since this disorder is usually caused by damage to parts of the brain, it will typically first be recognized in an MRI or CT scan that can confirm the presence of a brain injury. The extent and type of aphasia can generally only be determined by observing the affected part of the brain and determining how extensively it has been damaged, which is often done with the help of an SLP.
Treatment options for aphasia can be restorative (aimed at restoring impaired function) or compensatory (aimed at compensating for deficits).
Dysarthria
Dysarthria is usually caused by brain damage or facial paralysis that affects the muscles of the jaw, tongue, or throat, which may result in deficits in a person’s speech. It may also be caused by other conditions like Lou Gehrig’s disease, Parkinson’s, or a stroke. It’s considered a nervous system disorder, subclassified as a motor speech disorder. It’s commonly seen in those who already have other speech disorders, such as aphasia or apraxia. Symptoms of dysarthria include slurred speech, speaking too slowly, speaking too quickly, speaking very softly, being unable to move one’s lips or jaw, and having monotonous speech.
Dysarthria can be diagnosed by an expert in speech-language pathology through an exam and tests like MRI, CT, electromyography, or the Denver articulation screening examination. Treatment depends upon the severity and rate of progression of the disorder. Some potential examples include tactics like slowing down while talking, doing exercises to help strengthen jaw muscles, moving the lips and tongue more, and learning strategies for speaking more loudly. Hand gestures and speech machines may also help.
The importance of treatment
It is important to treat speech disorders; the consequences of an untreated speech or language impediment can vary widely depending on the type, symptoms, and severity, as well as the age and life situation of the individual. In general, it’s usually helpful to seek professional advice on treating speech disorders as soon as you notice or suspect an impediment present in yours or your child’s speech. Especially for moderate to severe cases, some potential effects of leaving these common speech disorders untreated can include:
- Poor academic performance/dropping out of school
- Decrease in quality of life
- Social anxiety and an inability to connect with people
- Damaged relationships
- Social isolation
- Hospitalization

Seeking professional support
Meeting with an SLP is usually the recommended first step for someone who believes they or their child may have a speech impediment. If you have a teenager with dyslexia, there are resources for dyslexic teens that can give supportive information about the condition. Healthcare providers may also provide helpful insights and ask about your family members’ history when it comes to speech and language-related issues as they can be hereditary. While these professionals can help with the physical aspects of a variety of speech and language impediments, you or your child may also benefit from emotional support in relation to the mental health effects of having an impediment. A therapist may be able to provide this type of guidance. If your child is experiencing a speech impediment, a counselor may be able to work with them to process their feelings of frustration and learn healthy coping mechanisms for stress. They can help you manage the same feelings if you receive a speech or language impediment diagnosis, or may be able to support you in your journey of parenting a child with a speech or language impediment diagnosis.
In addition to support at home, teenagers with a diagnosed speech impairment or impediment can receive special education services at school. The Centers for Disease Control notes that under the Individuals with Disabilities Act (IDEA) and Section 504, schools must provide support and accommodations for students with speech disorders. For some children, support groups can provide outlets for social connections and advice for coping.
Meeting with a therapist in person is an option if there are providers in your area. That said, many people find it less intimidating or more comfortable to meet with a therapist virtually. For example, a teen who is experiencing a speech or language impediment may feel better interacting with a counselor through the online chat feature that virtual therapy platforms like TeenCounseling provide. It may allow them to express themselves more clearly than they could face-to-face or over the phone. Parents who need support in caring for a child with a speech or language impediment may find the availability and convenience of meeting with a therapist through an online therapy service like BetterHelp to be most beneficial. Research suggests that online and in-person therapy offer similar benefits for a variety of conditions, so you can choose the format that’s best for you.
Counselor reviews
See below for reviews of TeenCounseling therapists written by parents who sought help for their children through this service.
“Kathleen has been good for my daughter to talk to. I am thankful for her to give my daughter someone else's perspective other than her parents. Thank you.”
“I love Ms. Jones. She doesn’t over-talk or judge you. She gives really good advice and if you're confused she knows how to break it down or explain whatever it is so you can understand. If you need to talk about anything, she’s always an open ear and responds quickly. Not only does she give you points from others' perspectives but she steps into yours so she can understand why certain things are the way they are. In my first session, I was nervous and I think she could tell. She’ll crack a joke every now and then to make me feel more comfortable. She’s just such a bundle of joy and a good counselor to have.”
Speech and language impediments can vary widely in terms of types, causes, symptoms, and severity. These are diagnosed by professionals in the field of speech and language pathology or by a medical doctor. A therapist can provide emotional support for those who are having difficulty coping with their own or their child’s diagnosis or other related challenges.
What are the 3 speech impediments?
Speech impediments can manifest in a variety of ways. Three of the most common are listed below:
- Voice disorders affect the tone, pitch, quality, and volume of a person’s voice. A person with a voice disorder may have difficulty speaking or being heard clearly by others. Voice disorders can be either functional or organic. Functional disorders occur due to improper use of the parts of the throat that produce speech, such as overuse of the voice leading to vocal fatigue. Organic voice disorders result from physical anatomical changes, such as nodules on the vocal cords.
- Fluency disorders affect the rate, rhythm, and cadence of speech. Those with fluency disorders may speak in a disjointed, choppy, or prolonged fashion, making them difficult for others to understand clearly. While many types of fluency disorders exist, stuttering is likely the best-known. Speech often requires precise timing to convey a message accurately, which fluency disorders can disrupt.
- Speech sound disorders are a broad category of disorders that interferes with a person’s ability to produce sounds and words correctly. Speech sound disorders can present very differently from person to person. Sometimes word sounds are omitted or added where not appropriate, and sometimes word sounds are distorted or substituted completely. A typical example of a speech sound disorder is the substitution of “r” for “w” in words like “rabbit” (becoming “wabbit”). Many children experience that substitution, but it does not become a disorder until the child does not outgrow it.
Other types of disorders can cause problems with expressive communication or tongue-tie those experiencing them, such as developmental language disorder. Language disorders also cause concerns related to expressive communication, but the concerns are due to a lack of understanding of one or more components of language, not an inability to produce or use word sounds.
What do you call a speech impediment?
Speech impediments are typically referred to as speech disorders . Speech refers to the ability to form speech sounds using the vocal cords, mouth, lips, and tongue. Speech also requires that a rhythm and cadence be maintained. Speech disorders indicate a problem producing intelligible speech; word sounds may be omitted or misplaced, the rhythm of the speech may be difficult to follow, or a person’s voice might be strangely pitched or too soft to hear clearly.
It is important not to confuse speech disorders with language disorders . Language disorders arise due to difficulty understanding what words mean, how word sounds fit together, or how to use spoken language to communicate. Language problems may affect how a person speaks, but the root cause of the concern is linked to their understanding of language, not their ability to produce intelligible speech.
How do I know if I have a speech impediment?
If you’re experiencing a sudden onset of impaired speech with no apparent cause, seek medical attention immediately. Strokes, traumatic brain injuries, and other serious medical conditions can cause sudden changes in speaking ability. Gradual changes in speaking ability may also indicate an underlying medical problem. If you’re concerned that your speaking ability has been gradually deteriorating, consider making an appointment with a healthcare provider in the near future.
Most people with a speech disorder are diagnosed in childhood. Parents often identify speech-related concerns in early childhood based on their child’s speech patterns. The child’s pediatrician may also refer the child to a speech-language pathologist, a professional specializing in evaluating and treating speech disorders. If problems persist until the child is in school, teachers and other school officials might initiate a referral for an evaluation if they believe speech concerns are present. Children often receive speech and language therapy that resolves or improves their speech problems.
Speech disorders also appear in adulthood, often due to injury or illness. It is also possible, although rare, for speech problems to be misdiagnosed or missed outright during a person’s childhood. In that case, the speech disorder may have been present since childhood and symptoms persisted into adulthood.
If you’re finding it difficult to communicate verbally with others, have an easily identifiable speech problem (like stuttering), or receive feedback that others have trouble understanding you, consider making an appointment with your doctor for an evaluation and referral to the appropriate healthcare providers.
What are 5 causes of speech impairment?
Speech and language disorders can result from conditions that interfere with the development of perceptual, structural, motor, cognitive, or socioemotional functions. The cause of many speech disorders is unknown, but research has indicated several underlying factors that may be responsible:
- Pre-existing genetic conditions, like Down’s syndrome or Fragile X syndrome. Evidence suggests that genes may play a role even if genetic abnormalities do not result in a diagnosable genetic condition.
- Physical abnormalities, such as damage or improper development of the respiratory system, facial muscles, or cranial nerves.
- Hearing problems, which can delay a child’s acquisition of speech.
- Neurodevelopmental disorders, such as autism spectrum disorder, may interfere with speech development. There is also evidence to suggest that those with attention-deficit hyperactivity disorder may have a more challenging time acquiring speech skills.
- Neurological conditions such as cerebral palsy.
Mental health concerns can also cause problems communicating with others. For example, an underlying anxiety disorder may lead to selective mutism , wherein a child speaks only under certain circumstances.
Is speech impediment a disability?
A speech-language disorder is considered a “ communication disability ” under the Americans with Disabilities Act (ADA). The ADA requires government and businesses to establish “effective communication” with people who have communication disabilities. Effective communication can be established in several ways. For those with a speech disorder, accommodation may be as simple as ensuring the person can get hold of writing materials if they need to express themselves quickly. In some cases, organizations may use a transliterator, or person trained to recognize unclear speech and repeat it clearly.
Because speech disorders are known to lead to academic struggles in K-12 and higher education settings, they are categorized as a disability under the Individuals with Disabilities Education Improvement Act (IDEIA) . The IDEIA sets guidelines for all schools in the United States, public or not public, guaranteeing each child a right to accommodations and interventions for their speech disorder.
Can I fix my speech impediment?
Whether or not a speech disorder can be completely eliminated depends heavily on individual factors. The cause of the disorder, its severity, and the type of speech dysfunction all play a role in determining whether a particular disorder can be completely resolved. While it is not possible to guarantee that a speech disorder can be “cured,” nearly all disorders are treatable, and improvement is likely possible.
Can you treat a speech impediment?
Yes, many speech disorders are highly treatable. Most people receive treatment as children when most speech disorders become apparent. For children, speech-language pathologists will identify the specific speech disorder, search for an underlying cause, and design an intervention that targets that child’s speech problem. For example, a child who struggles with articulation errors and producing word sounds consistently may benefit from a contextual utilization approach . Contextual utilization leverages the fact that one sound is easier or more difficult to pronounce depending on which other sounds surround it.
Speech disorders that emerge in adulthood may be more challenging to treat due to underlying factors, such as brain injury. Suppose an adult experiences a traumatic brain injury that affects their speaking ability. In that case, a speech-language pathologist may help them find alternative communication methods, such as using a computer. They may also help them directly restore some of their speaking ability by leading them through exercises that improve nerve function and muscle control.
Is a speech impediment mental?
Speech disorders can be caused by various factors, many of which have nothing to do with the brain. However, there is a relationship between psychiatric mental health concerns and difficulty with spoken communication . Although researchers are still unsure of the exact cause, studies have identified a significant link between speech disorders and mental health disorders like schizophrenia, bipolar disorder, and major depression.
Neurodevelopmental disorders, such as autism spectrum disorder and attention-deficit hyperactivity disorder, are also associated with an increased risk of developing a speech disorder. Although the link between neurodevelopmental disorders and speech disorders is not fully understood, evidence suggests that treating the speech disorder is still possible.
Finally, speech disorders can also be caused by illness or injury in the brain, such as cancer, an infection, or traumatic brain injury. Although these are not considered mental or developmental disorders, they may affect brain function and mental acuity. Speaking is a complex process, and there are many ways it can be affected.
Is autism a speech impediment?
Autism spectrum disorder is not a speech disorder, but it is heavily associated with communication problems. Those on the autism spectrum often use repetitive or rigid language and may not follow communication norms. They may repeat phrases continuously, use a modified tone of voice, or introduce information that has little to do with the conversation at hand.
Those on the autism spectrum are often able to form word sounds properly. The communication deficits of autism spectrum disorder are more closely related to language disorders than speech disorders. Speech disorders are associated with difficulty producing or using word sounds correctly, whereas language disorders are associated with a lack of understanding of one or more language components.
Autism spectrum disorder is also characterized by difficulties using pragmatic communication, or communication that is appropriate to a specific social situation. Although not a disorder of speech, a limited ability to recognize the socioemotional content of speech can significantly impact interpersonal communication and social interactions.
- Recognizing And Navigating Teen Depression Medically reviewed by Elizabeth Erban , LMFT, IMH-E
- ADHD Signs In Women, Men, And Children Medically reviewed by Julie Dodson , MA
- Relationships and Relations
What Causes A Lisp in Adults? Can Speech Therapy Help?
A lisp is when a person cannot pronounce /s/, /z/, /ts/, /dz/ and other sibilants correctly. These misarticulations may result in unclear speech.
Some experts refer to lisps as sigmatism.
Currently, there is no way to predict who will have a lisp growing up. Between 1 and 4% of adults lisp at some point during their lives.
What Causes a Lisp in Adults?
Here are some factors that may cause a lisp –
When a short and tight band of tissue attaches the tip of the tongue to the floor of the mouth not allowing it to move as much as it should, it prevents the person from pronouncing the words correctly. Tongue-tie or ankyloglossia is typically present at birth. This condition may require a small surgery later in life.
Incorrect Jaw Alignment
The correct alignment of the jaw is crucial for its full range of movement. A person with incorrect jaw alignment may face problems articulating sibilant words. Some jaw alignment issues can be treated with early therapy, while others require minor surgical procedures.
Misaligned Teeth
Some children begin to lisp once their permanent teeth come out. If that's the case, you may want to speak to an orthodontist in addition to consulting a speech therapist. An overbite, open bite, or space between the teeth in the upper jaw may contribute to a lisp.
In most cases, children who lisp outgrow it on their own. Only a few continue lisping well into adulthood. Lisp is a speech impediment that makes the speaker difficult to understand. Therefore, many adults look for the treatment of lisps and wonder if speech therapy can help.
Is It Possible To Fix Your Lisp As An Adult?
Well, it absolutely is.
However, let us first tell you that there's nothing wrong with lisping. If you lisp and have no problems with it, that's great. If you do have a problem with the way you speak, that's alright too, because this article is for you!
Lisping does not imply a problem with overall communication. Lisping in adults hardly affects the intelligibility of speech.
Several individuals might perceive lisping in an adult negatively. Although, lisping isn't a representation of one's intelligence or communication skills.
If your lisp has a significant impact on your social life, employment, personal life, and self-esteem, then it may be a wise decision to work towards treating it.
Having a lisp isn’t bad! If you or your loved one(s) have no problems with having a lisp, then that’s perfectly alright too!
One of the primary concerns adult clients have is whether they will be treated like a child when they approach a speech-language pathologist (SLP) for lisp treatment.
The majority of the research on lisp has indeed been conducted on children. There is little published data on the effects and treatment of lisping in adults.
However, every experienced speech therapist should have the resources to treat lisping in adults. If you are looking for speech therapy for your lisp, you should always check if your therapist has the experience or knowledge of dealing with adult clients.
In the case of adult clients, a speech therapist will talk about the mechanism involved in producing speech sounds. They will explain the factors that cause lisping and how each exercise can help you overcome a lisp.
Your speech therapist should give you specific goals depending upon your current challenges and expectations.
At the same time, your therapist should consider how lisping has affected your personal and social life, employment, and self-esteem.
Lisp Treatment for Adults: How Does Speech Therapy Help? Let's find out.
Monitoring and Self-Correction
The speech therapist will show you how each sound is produced. You will learn the relative positions of your tongue, lips, soft palate, and jaws while working with the speech therapist.
Next, you will learn to monitor the pronunciations and self-correct whenever necessary.
Practicing Target Sounds
You will work on isolated sounds, mono-syllables, single words, and sentences with the speech therapist.
These levels aim to give you the highest possible accuracy before moving on to the next stage.
Transition to Everyday Situations
You will gradually learn how to transfer the target sounds to everyday conversations. That is the ultimate goal of lisp therapy! To be able to carry the perfected phonetics over to everyday life effortlessly.
In the case of adults, practice sentences and model conversations are typically based on their interests, hobbies, and employment situations. It is so that you can practice commonly occurring conversations and sentences almost regularly with the speech therapist and by yourself.
Utilization of Technologies
The speech therapist will show you how to utilize speech therapy applications and tools for improving your pronunciations.
Listening to the recording of your own voice and monitoring your progress will give you a fair idea of how far you are from achieving your goals.
How Long Will Lisping Treatment Take?
Speech therapy is not a one-time deal. You need to be patient and regular if you want to see improvement while using speech therapy for lisping treatment.
In most cases, a lisp arises when the individual is a child. So, the muscles in and around their mouth have been trained to move in a certain way while producing sibilant sounds.
Adults have the added advantage of understanding the sound production process. Speech therapy will give you the knowledge and resources to retrain your facial muscles. It will give you the ability to consciously manipulate your tongue, jaws, and lips to produce sounds correctly.
However, it all boils down to home practice. The more you practice, the less time you spend in the therapist's office!
You may also seek speech therapy online via a speech therapy app like Stamurai .
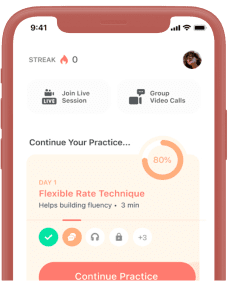
Related Posts
- Therapy Protocol
- Group Video Calls
- Privacy Policy
- Terms of Service
- Cancellation & Refund
Orthodontist Ann Arbor MI Invisalign Braces | McNamara Orthodontics
Orthodontist Ann Arbor MI Invisalign | McNamara Orthodontics
Why Choose An Orthodontist To Correct Speech Problems?
Speech Problems…Did you know that the alignment of your teeth can affect your speech? One of the first things people notice about you is your smile and how we communicate when talking. If you have issues speaking clearly, orthodontics can help!
Lisping, whistling or slurring, and mispronunciation of words with “s” and “t” are the most common offenders. Proper diagnosis and correction during a patient’s developmental years, by an orthodontist makes it much easier to correct the tooth and/or jaw problems associated with poor speech habits. The American Association of Orthodontists recommends that all children be evaluated by age 7.
Common Causes of Many Speech Problems?
An overjet (buck teeth) or openbite, or crossbite are the most common causes of speech impediments. Teeth must come together properly to create an air tight seal for the tongue to swallow properly in the roof of the mouth. If there is an opening which is often found in overjets, and openbites, the tongue creates the seal instead and results in a speech issue when communicating. If there is not enough room for the tongue which is often found with Crossbites or underbites, speech is affected.
Why Choose an Orthodontist to Correct Speech Disorders?
Orthodontics is the treatment of irregularities of the teeth and jaws by a trained dental specialist with 2-3 years additional training after receiving their dental degree. General Dentistry is a broad medical specialty that deals with the teeth, gum, nerves, and jaw, while orthodontics is a specialty within dentistry that focuses on correcting bites, occlusion, jaw development, and the straightness of teeth.
One important difference is that all orthodontists like those at McNamara Orthodontics are dentists, but not all dentists are licensed orthodontists. Understanding the complexities of proper tooth movement and jaw growth allows an orthodontist to drastically improve or eliminate speech problems in patients of all ages.
Children after the ages of 10 are more significantly affected by language impairment resulting in low self-esteem and poor self-image than the children with no speech impediments. If you or your child is suffering from a speech disorder, contact McNamara Orthodontics in Ann Arbor MI today to schedule a Complimentary Evaluation. We will help you determine the cause of the speech problem and offer the best treatment options available to improve the problem at hand.
Copyright © 2024 SpeechPathology.com - All Rights Reserved
- Difficulty with /r/ and Techniques for Dealing with this Phoneme
Julie Hoffmann, M.A.,CCC-SLP
April 21, 2003.
- Ask the Experts
- Articulation, Phonology, and Speech Sound Disorders
The /r/ phoneme is one of the most difficult phonemes to remediate for clients with persistent, long term /r/ problems. Identifying the exact nature of the problem with the /r/ production will allow you to choose appropriate remediation strategies for your client. Typical problems with incorrect /r/ productions include: rounding the lips, incorrect tongue placement, lack of tension with the tongue, tongue is too low in the oral cavity, use of a tense jaw, poor tongue-jaw differentiation, jaw instability, and incorrect productions patterned over time. Here are several therapy facilitation techniques that I have found successful for clients with persistent /r/ problems:
- Teaching general awareness of the articulators (ie. tongue, lips, oral cavity) and their functions with stimulation (flavored tongue depressors, pretzel sticks, small suckers, toothettes) and visual cues (mirror, tongue drawings). Decreasing hyposensitivity by brushing the sides of the tongue and inside of the upper molars with various textures (ie. small toothbrush, toothette, tongue depressor, Popsicles) before and during practice of /r/ targets.
- Eliminate lip rounding by having the client smile during /r/ productions. You could also place a small bite block (ie. coffee stirrer) between the lips while smiling, as the bite block will fall out if the lips are rounded (use a mirror so client can visually monitor lip rounding/retracting).
- Create tongue tension by placing a wet toothette on the back of the tongue and directing the client to close his mouth and push the toothette up with the tongue (squeezing out all the water). Direct the client to complete this task for several trials before sound practice. Also, tongue tension increases by having the client produce the /r/ while pushing against a table/wall or saying the /r/ while lifting the chair he is sitting in.
- Be very picky with your target word choices for /r/ initial words. Choose words with velars in the final position to increase the use of /r/ (ie. rake, rug, rock). Produce a short, quick /r/ (do not prolong), pause for a second, overemphasize the vowel after the /r/, then finish out the word.
- Tongue/jaw differentiation tasks to improve jaw stability, which in turn allows the client to achieve correct tongue placement. Use a mirror and have the client open and close the mouth slowly with no head movement or lateralizing of the jaw. The client could increase jaw stability by opening and closing the mouth in increments for better control as well. Direct the client to open his mouth, leaving it open with a stable jaw, and slowly moving the tongue tip to the alveolar ridge and then behind the lower front teeth. Complete several trials for these tasks. You could also use a bite block (coffee stirrer) placed between the molars on one side to assure jaw stability for the client until he can do this on his own.
- Teach the bunched /r/ (high back) which includes humping up back of tongue for silent /k/; having the sides of the back of the tongue touch the insides of upper back molars and relaxing the jaw).
- Clients with persistent /r/ problems often benefit from the introduction of the retroflex /r/. Teach the retroflex /r/ (curled) which includes placing the tongue tip behind the upper front teeth; curling the tongue tip backward without touching the roof of the mouth; the lateral sides of the tongue should touch the insides of the upper back molars; and the jaw should be slightly lowered. The retroflex /r/ can also be facilitated by producing an /l/ with a slightly lowered jaw and sliding the tongue tip back farther and farther until you hear an /r/ production. If the client has a short frenulum, then the retroflex /r/ will be difficult. Frequently, in time, the retroflex /r/ naturally changes to a high back /r/.
- Shaping / sound modifications: using phonemes /l/, /n/, /d/, /w/, /g/, ''sh', ''y', /i/, /a/ to shape the /r/ sound.
- Use coarticulation if a client is successful with /r/ in the initial or final position of words, use this as a facilitation technique. For example, successful initial /r/ productions could increase the final position /r/ (ie. bear-red, car-read) due to anticipatory behaviors for the upcoming initial /r/. You would gradually work the /r/ initial word during practice as the final position /r/ emerges. Also, you could try the /kr-/ and /gr-/ blends for initial success.
- Drill, drill, drill. Expect accuracy. Once the client is successful with the /r/ production, increase complexity by establishing the /r/ in other contexts and positions. Encourage the client to ''feel' the difference with the /r/ productions.
Related Courses
Treatment approach considerations for school-aged children with speech sound disorders, course: #9472 level: intermediate 1 hour, back to basics: down syndrome, course: #8975 level: introductory 1 hour, 20q: dynamics of school-based speech and language therapy variables, course: #10002 level: advanced 1 hour, sleuthing for /s/ and /r/: facilitating strategies for residual sound errors, course: #9237 level: introductory 2 hours, 20q: a continuum approach for sorting out processing disorders, course: #10008 level: intermediate 1 hour.
Our site uses cookies to improve your experience. By using our site, you agree to our Privacy Policy .

IMAGES
COMMENTS
However, some speech disorders persist. Approximately 5% of children aged three to 17 in the United States experience speech disorders. There are many different types of speech impediments, including: Disfluency. Articulation errors. Ankyloglossia. Dysarthria. Apraxia. This article explores the causes, symptoms, and treatment of the different ...
Abstract: Practicing Speech-Language Pathologists report that many clients demonstrate limited or excessive up-and-down jaw movements during communication as compared to their typically developing peers. The results of this retrospective study suggest that atypical jaw skills are related to deficits in speech clarity in clients diagnosed with ...
Common causes of dysarthria include nervous system disorders and conditions that can cause facial paralysis, tongue or throat muscle weakness. An example of a nervous system disorder that typically causes dysarthria is amyotrophic lateral sclerosis (ALS), also referred to as Lou Gehrig disease. ALS is a progressive neurodegenerative disorder ...
Spasmodic Dysphonia (SD) is a chronic long-term disorder that affects the voice. It is characterized by a spasming of the vocal chords when a person attempts to speak and results in a voice that can be described as shaky, hoarse, groaning, tight, or jittery. It can cause the emphasis of speech to vary considerably.
(According to Maureen Paton's Alan Rickman: The Unauthorised Biography, he was born with a "tight jaw, hence the slightly muffled drawl.") His signature sound could have been interpreted as a ...
Common causes of childhood speech impediments include: Autism spectrum disorder: A neurodevelopmental disorder that affects social and interactive development. Cerebral palsy: A congenital (from birth) disorder that affects learning and control of physical movement. Hearing loss: Can affect the way children hear and imitate speech.
There are three general categories of speech impairment: Fluency disorder. This type can be described as continuity, smoothness, rate, and effort in speech production. Voice disorder. A voice ...
1. Articulation challenges: TMJ disorders can limit jaw movement, making it difficult to enunciate and articulate certain speech sounds accurately. 2. Discomfort while speaking: Pain in the temporomandibular joint may make speaking uncomfortable and cause individuals to alter their speech patterns in an attempt to avoid discomfort. 3.
Children with speech impediments may benefit from seeing an orthodontist before a therapist. Learn how to tell if tooth and jaw problems are to blame. (720) 409-0008. Menu. Phone. Location. ... It could be that bad teeth or a small jaw is causing a speech issue, and by correcting the problem at its source, the impediment may dissipate naturally ...
Summary. Tight jaw muscles can be caused by stress, anxiety, teeth grinding, or other medical conditions such as arthritis. Treatment includes massage, stretching, medications, and physical therapy. Mouth guards can also be helpful to reduce jaw issues from teeth grinding.
According to a 2008 scientific study, Alan Rickman literally had the perfect voice, thanks to his immaculate balance of tone, frequency, intonation and speed. Rickman owed his unique voice to a speech impediment - a result of him being born with a tight jaw - and an accent that mixed Irish and Welsh parentage, a working-class London ...
Overall difficulty communicating and expressing thoughts and ideas. Inability to repeat words. Inability to pronounce words the same way twice. A phobia of speaking in public. Speaking slowly and carefully. Speech delay. Frequent pauses when talking. Limited vocabulary over several years, delayed language development.
If that's the case, you may want to speak to an orthodontist in addition to consulting a speech therapist. An overbite, open bite, or space between the teeth in the upper jaw may contribute to a lisp. In most cases, children who lisp outgrow it on their own. Only a few continue lisping well into adulthood.
A lisp is a functional speech disorder commonly called a speech impediment. A lisp is characterized by difficulty making specific speech sounds, such as /s/ and /z/. Incorrect tongue placement is the primary reason behind a lisp, resulting in difficulty articulating the /s/ and /z/ sounds. are not universally agreed upon.
Understanding the complexities of proper tooth movement and jaw growth allows an orthodontist to drastically improve or eliminate speech problems in patients of all ages. Children after the ages of 10 are more significantly affected by language impairment resulting in low self-esteem and poor self-image than the children with no speech impediments.
The function of the jaw for feeding and speech has long been the discussion of both speechlanguage pathologists and occupational therapists. This article will examine the relationship between jaw movements or jaw skill levels for feeding quality and speech clarity. What has been missing in our discussions concerning jaw function is the role the ...
Produce a short, quick /r/ (do not prolong), pause for a second, overemphasize the vowel after the /r/, then finish out the word. Tongue/jaw differentiation tasks to improve jaw stability, which in turn allows the client to achieve correct tongue placement. Use a mirror and have the client open and close the mouth slowly with no head movement ...