- प्रेगनेंसी में जामुन खा सकते हैं क्या | Eating Jamun During Pregnancy
- Maharaj NETFLIX Movie Review : Junaid Khan Debut Film
- महाराज: Netflix पर एक विवादित ऐतिहासिक ड्रामा | Maharaj Netflix Review
- Is it safe to eat litchi during pregnancy or not
- प्रेगनेंसी में लीची खाना सुरक्षित या नहीं – कब खाएं और कितनी


गर्भ में लड़का है या लड़की – प्लेसेंटा की पोजीशन से जाने | Anterior or Posterior Placenta and Baby Gender Prediction
Read this article in english.
Highlights of Article
प्लेसेंटा की पोजीशन
गर्भ में प्लेसेंटा की दो मुख्य स्थितियां होती हैं। पहला एंटीरियर प्लेसेंटा और दूसरा पोस्टीरियर प्लेसेंटा। यह एक सामान्य सोच और विश्वास है कि इनके द्वारा आप जान सकते हैं कि आपके गर्भ में लड़का है या लड़की ।
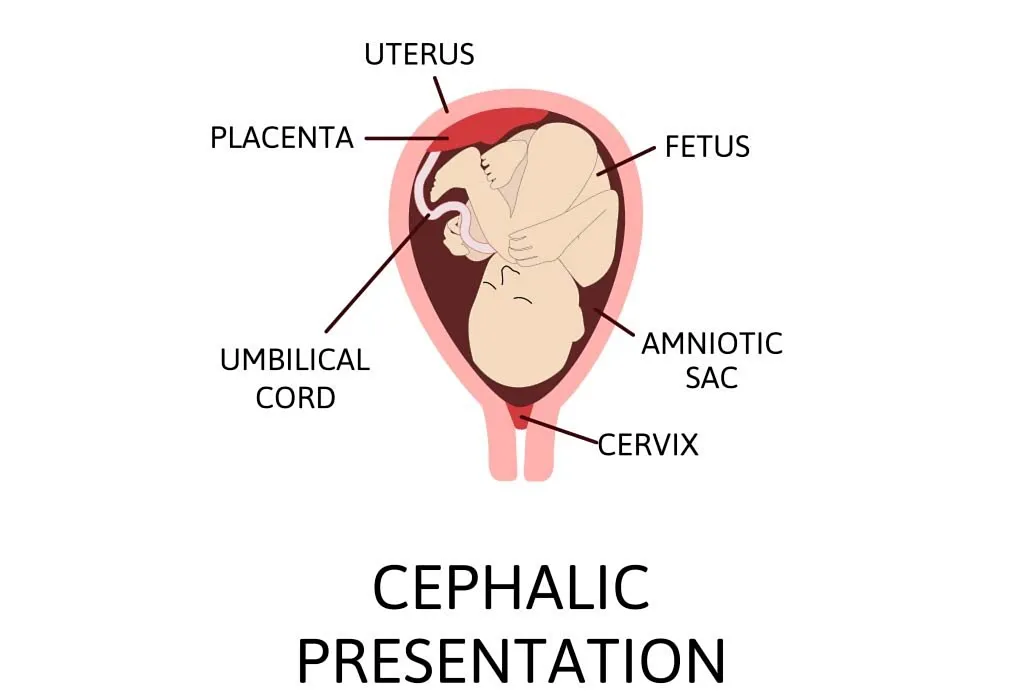
प्लेसेंटा क्या है
प्लेसेंटा गर्भ में बच्चे को ऑक्सीजन और आवश्यक पोषक तत्व प्रदान करता है। एंटीरियर प्लेसेंटा, प्लेसेंटा की एक स्थिति है जिसमें यह गर्भाशय के सामने की ओर स्थित होता है, जो मां की पेट की दीवार के करीब होता है।
Play Pregnancy Games (Super Mario Bros)
पोस्टीरियर प्लेसेंटा क्या है.
पोस्टीरियर प्लेसेंटा, प्लेसेंटा की एक स्थिति है जिसमें यह गर्भाशय के पीछे की ओर स्थित होता है, जो मां की रीढ़ के करीब होता है। ये दोनों स्थितियां सामान्य हैं और बच्चे के स्वास्थ्य या विकास में कोई महत्वपूर्ण अंतर नहीं है चाहे प्लेसेंटा आगे हो या पीछे हो।
प्लेसेंटा और शिशु के लिंग
माना जाता है कि अगर प्लेसेंटा एंटीरियर स्थिति में है तो यह गर्भ में पल रहे शिशु के लड़की होने का संकेत देता है। दूसरी ओर, यदि प्लेसेंटा गर्भाशय के पीछे की ओर स्थित है, तो इसे पोस्टीरियर पोजीशन कहा जाता है। ऐसे में माना जाता है कि गर्भ में पल रहा बच्चा लड़का है ।
प्लेसेंटा कैसे स्थित होता है
महिला का अंडा जब यह निषेचित हो जाता है, तो यह गर्भाशय की दीवार में खुद को प्रत्यारोपित कर लेता है। यह दीवार में कहीं भी, बायीं ओर, दायीं ओर, आगे, पीछे, ऊपर या नीचे कहीं भी प्रत्यारोपित किया जा सकता है। जैसे-जैसे बच्चा गर्भ में बढ़ता है, गर्भाशय भी फैलता है। जब बच्चा हिलना शुरू करता है, तो प्लेसेंटा की स्थिति में बदलाव संभव है।
प्रेगनेंसी में महिलाओं के पेट पर काली रेखा – गर्भ में लड़का है या लड़की
जैसा कि पहले उल्लेख किया गया है, नाल की स्थिति स्थिर नहीं है और गर्भावस्था के दौरान बदल सकती है। इसलिए, बच्चे के लिंग का निर्धारण करने के लिए प्लेसेंटा की स्थिति का उपयोग करना सटीक या विश्वसनीय नहीं है।
एक स्वस्थ गर्भावस्था को बनाए रखने पर ध्यान देना और अंधविश्वास या ओल्ड वाइव्स टेल्स के आधार पर बच्चे के लिंग की भविष्यवाणी करने की कोशिश करने की चिंता न करना महत्वपूर्ण है।
बच्चे के लिंग का सटीक निर्धारण करने का एकमात्र तरीका आनुवंशिक परीक्षण या अल्ट्रासाउंड के दौरान बच्चे की शारीरिक विशेषताओं की पहचान करना है। परिणाम जो भी हो उसके लिए खुश और आभारी होना और माँ और बच्चे दोनों के स्वास्थ्य और भलाई पर ध्यान देना महत्वपूर्ण है।
अगर आपको यह लेख अच्छा लगा हो तो कृपया इसे शेयर करें। garbhgyan.com को सब्सक्राइब करें। पढ़ने के लिए धन्यवाद।
Anterior and posterior placenta
Baby gender prediction in womb
Baby Boy Symptoms During Pregnancy
पोस्टीरियर प्लेसेंटा क्या है, placenta anterior meaning in hindi, placenta posterior meaning in hindi, anterior placenta meaning in hindi, posterior placenta baby gender in hindi, placenta anterior means boy or girl in hindi, पोस्टीरियर प्लेसेंटा मीन्स बॉय
- Diwali 2023 Date, Time and Pregnancy Do’s and Don’ts
- पेट में बच्चा ठहरते ही आपको इन 4 जगह सबसे ज्यादा दर्द होगा | These Body Parts Pain Soon You Get Pregnant
You May Also Like

गर्भ में बच्चे को गोरा बनाने के लिए ये करें प्रेगनेंसी में | Fair Baby Tips During Pregnancy

प्रेगनेंसी के 9वें महीने में नार्मल डिलीवरी के लिए इन बातों का ध्यान रखें

प्रेगनेंसी के पहले तिमाही में शिशु कैसे विकसित होता है
Leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

- Learn /
Why Is Cephalic Presentation Ideal For Childbirth?

5 Dec 2017 | 8 min Read
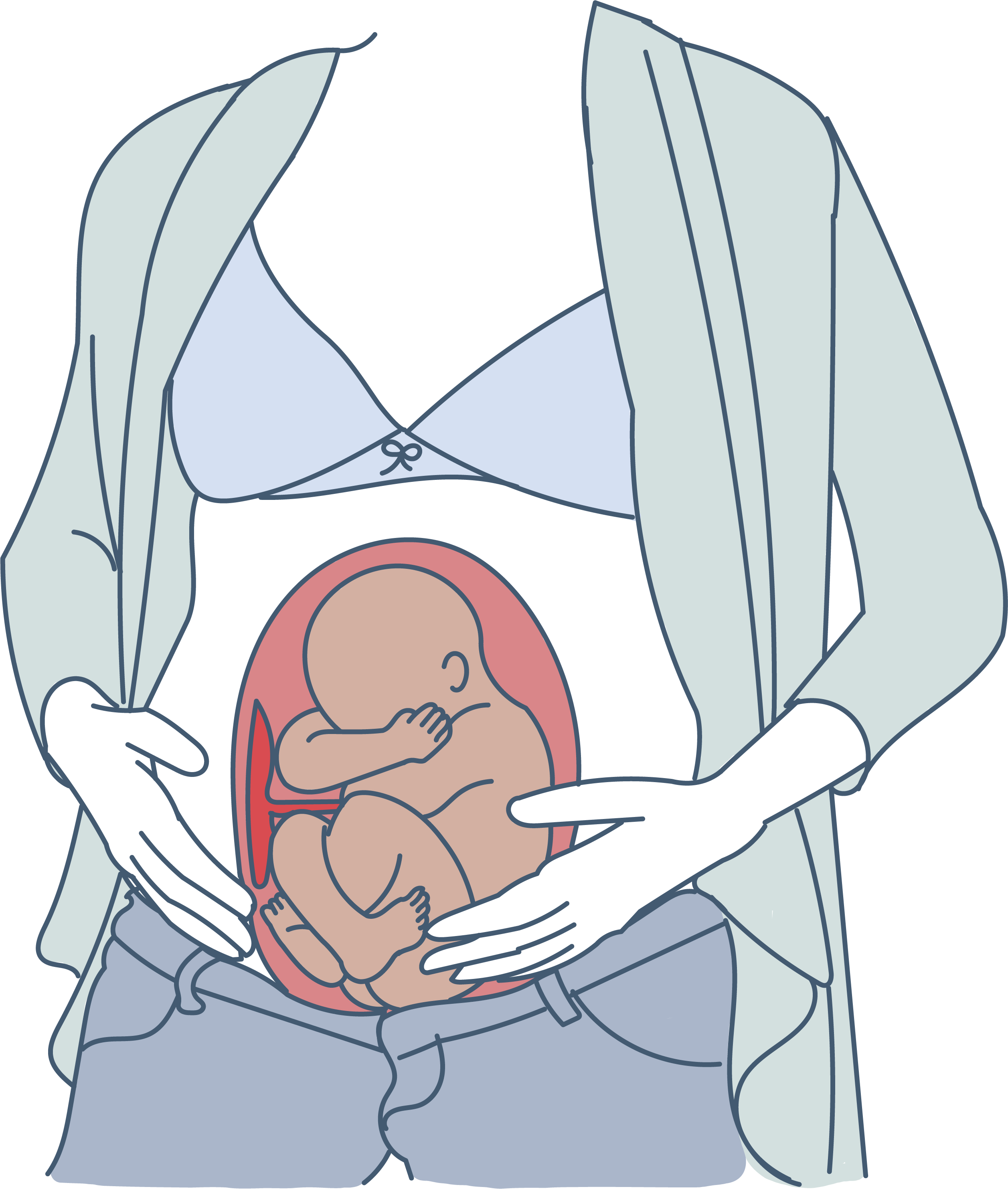
During labour, contractions stretch your birth canal so that your baby has adequate room to come through during birth. The cephalic presentation is the safest and easiest way for your baby to pass through the birth canal.
If your baby is in a non-cephalic position, delivery can become more challenging. Different fetal positions pose a range of difficulties and varying risks and may not be considered ideal birthing positions.
Two Kinds of Cephalic Positions
There are two kinds of cephalic positions:
- Cephalic occiput anterior , where your baby’s head is down and is facing toward your back.
- Cephalic occiput posterior , where your baby is positioned head down, but they are facing your abdomen instead of your back. This position is also nicknamed ‘sunny-side-up’ and can increase the chances of prolonged and painful delivery.
How to Know if Your Baby is In a Cephalic Position?
You can feel your baby’s position by rubbing your hand on your belly. If you feel your little one’s stomach in the upper stomach, then your baby is in a cephalic position. But if you feel their kicks in the lower stomach, then it could mean that your baby is in a breech position.
You can also determine whether your baby is in the anterior or posterior cephalic position. If your baby is in the anterior position, you may feel their movement underneath your ribs and your belly button could also pop out. If your baby is in the posterior position, then you may feel their kicks in their abdomen, and your stomach may appear rounded up instead of flat.
You can also determine your baby’s position through an ultrasound scan or a physical examination at your healthcare provider’s office.
Benefits of Cephalic Presentation in Pregnancy
Cephalic presentation is one of the most ideal birth positions, and has the following benefits:
- It is the safest way to give birth as your baby’s position is head-down and prevents the risk of any injuries.
- It can help your baby move through the delivery canal as safely and easily as possible.
- It increases the chances of smooth labour and delivery.
Are There Any Risks Involved in Cephalic Position?
Conditions like a cephalic posterior position in addition to a narrow pelvis of the mother can increase the risk of pregnancy complications during delivery. Some babies in the head-first cephalic presentation might have their heads tilted backward. This may, in some rare cases, cause preterm delivery.
What are the Risks Associated with Other Birth Positions?
A small percentage of babies may settle into a non-cephalic position before their birth. This can pose risks to both your and your baby’s health, and also influence the way in which you deliver.
In the next section, we have discussed a few positions that your baby can settle in throughout pregnancy, as they move around the uterus. But as they grow old, there will be less space for them to tumble around, and they will settle into their final position. This is when non-cephalic positions can pose a risk.
Breech Position
There are three types of breech fetal positioning:
- Frank breech : Your baby’s legs stick straight up along with their feet near their head.
- Footling breech: One or both of your baby’s legs are lowered over your cervix.
- Complete breech: Your baby is positioned bottom-first with their knees bent.
If your baby is in a breech position , vaginal delivery is considered complicated. When a baby is born in breech position, the largest part of their body, that is, their head is delivered last. This can lead to injury or even fetal distress. Moreover, the umbilical cord may also get damaged or get wrapped around your baby’s neck, cutting off their oxygen supply.
If your baby is in a breech position, your healthcare provider may recommend a c-section, or they may try ways to flip your baby’s position in a cephalic presentation.
Transverse Lie
In this position, your baby settles in sideways across the uterus rather than being in a vertical position. They may be:
- Head-down, with their back facing the birth canal
- One shoulder pointing toward the birth canal
- Up with their hands and feet facing the birth canal
If your baby settles in this position, then your healthcare provider may suggest a c-section to reduce the risk of distress in your baby and other pregnancy complications.
Turning Your Baby Into A Cephalic Position
External cephalic version (ECV) is a common, and non-invasive procedure that helps turn your baby into a cephalic position while they are in the womb. However, your healthcare provider may only consider this procedure if they consider you have a stable health condition in the last trimester, and if your baby hasn’t changed their position by the 36th week.
You can also try some natural remedies to change your baby’s position, such as:
- Lying in a bridge position: Movements like bridge position can sometimes help move your baby into a more suitable position. Lie on your back with your feet flat on the ground and your legs bent. Raise your pelvis and hips into a bridge position and hold for 5-10 minutes. Repeat several times daily.
- Chiropractic care: A chiropractor can help with the adjustment of your baby’s position and also reduce stress in them.
- Acupuncture: After your doctor’s go-ahead, you can also consider acupuncture to get your baby to settle into an ideal birthing position.
While most babies settle in a cephalic presentation by the 36th week of pregnancy, some may lie in a breech or transverse position before birth. Since the cephalic position is considered the safest, your doctor may recommend certain procedures to flip your baby’s position to make your labour and delivery smooth. You may also try the natural methods that we discussed above to get your baby into a safe birthing position and prevent risks or other pregnancy complications.
When Should A Baby Be In A Cephalic Position?
Your baby would likely naturally drop into a cephalic position between weeks 37 to 40 of your pregnancy .
Is Cephalic Position Safe?
Research shows that 95% of babies take the cephalic position a few weeks or days before their due date. It is considered to be the safest position. It ensures a smooth birthing process.
While most of the babies are in cephalic position at delivery, this is not always the case. If you have a breech baby, you can discuss the available options for delivery with your doctor.
Does cephalic presentation mean labour is near?
Head-down is the ideal position for your baby within your uterus during birth. This is known as the cephalic position. This posture allows your baby to pass through the delivery canal more easily and safely.
Can babies change from cephalic to breech?
The external cephalic version (ECV) is the most frequent procedure used for turning a breech infant.
How can I keep my baby in a cephalic position?
While your baby naturally gets into this position, you can try some exercises to ensure that they settle in cephalic presentation. Exercises such as breech tilt, forward-leaning position (spinning babies program), cat and camel pose can help.
Stitches after a normal delivery : How many stitches do you need after a vaginal delivery? Tap this post to know.
Vaginal birth after caesarean delivery : Learn all about the precautions to consider before having a vaginal delivery after a c-section procedure.
How many c-sections can you have : Tap this post to know the total number of c-sections that you can safely have.
Cover Image Credit: Freepik.com

Related Topics for you
babychakraenglish
cephalicposition
cephalicpresentation
fetaldevelopment
fetalmovement
preganancycare
Suggestions offered by doctors on BabyChakra are of advisory nature i.e., for educational and informational purposes only. Content posted on, created for, or compiled by BabyChakra is not intended or designed to replace your doctor's independent judgment about any symptom, condition, or the appropriateness or risks of a procedure or treatment for a given person.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Cephalic Position?
The ideal fetal position for labor and delivery
- Why It's Best
Risks of Other Positions
- Determining Position
- Turning a Fetus
The cephalic position is when a fetus is head down when it is ready to enter the birth canal. This is one of a few variations of how a fetus can rest in the womb and is considered the ideal one for labor and delivery.
About 96% of babies are born in the cephalic position. Most settle into it between the 32nd and 36th weeks of pregnancy . Your healthcare provider will monitor the fetus's position during the last weeks of gestation to ensure this has happened by week 36.
If the fetus is not in the cephalic position at that point, the provider may try to turn it. If this doesn't work, some—but not all—practitioners will attempt to deliver vaginally, while others will recommend a Cesarean (C-section).
Getty Images
Why Is the Cephalic Position Best?
During labor, contractions dilate the cervix so the fetus has adequate room to come through the birth canal. The cephalic position is the easiest and safest way for the baby to pass through the birth canal.
If the fetus is in a noncephalic position, delivery becomes more challenging. Different fetal positions have a range of difficulties and varying risks.
A small percentage of babies present in noncephalic positions. This can pose risks both to the fetus and the mother, and make labor and delivery more challenging. It can also influence the way in which someone can deliver.
A fetus may actually find itself in any of these positions throughout pregnancy, as the move about the uterus. But as they grow, there will be less room to tumble around and they will settle into a final position.
It is at this point that noncephalic positions can pose significant risks.
Cephalic Posterior
A fetus may also present in an occiput or cephalic posterior position. This means they are positioned head down, but they are facing the abdomen instead of the back.
This position is also nicknamed "sunny-side up."
Presenting this way increases the chance of a painful and prolonged delivery.
There are three different types of breech fetal positioning:
- Frank breech: The legs are up with the feet near the head.
- Footling breech: One or both legs is lowered over the cervix.
- Complete breech: The fetus is bottom-first with knees bent.
A vaginal delivery is most times a safe way to deliver. But with breech positions, a vaginal delivery can be complicated.
When a baby is born in the breech position, the largest part—its head—is delivered last. This can result in them getting stuck in the birth canal (entrapped). This can cause injury or death.
The umbilical cord may also be damaged or slide down into the mouth of the womb, which can reduce or cut off the baby's oxygen supply.
Some providers are still comfortable performing a vaginal birth as long as the fetus is doing well. But breech is always a riskier delivery position compared with the cephalic position, and most cases require a C-section.
Likelihood of a Breech Baby
You are more likely to have a breech baby if you:
- Go into early labor before you're full term
- Have an abnormally shaped uterus, fibroids , or too much amniotic fluid
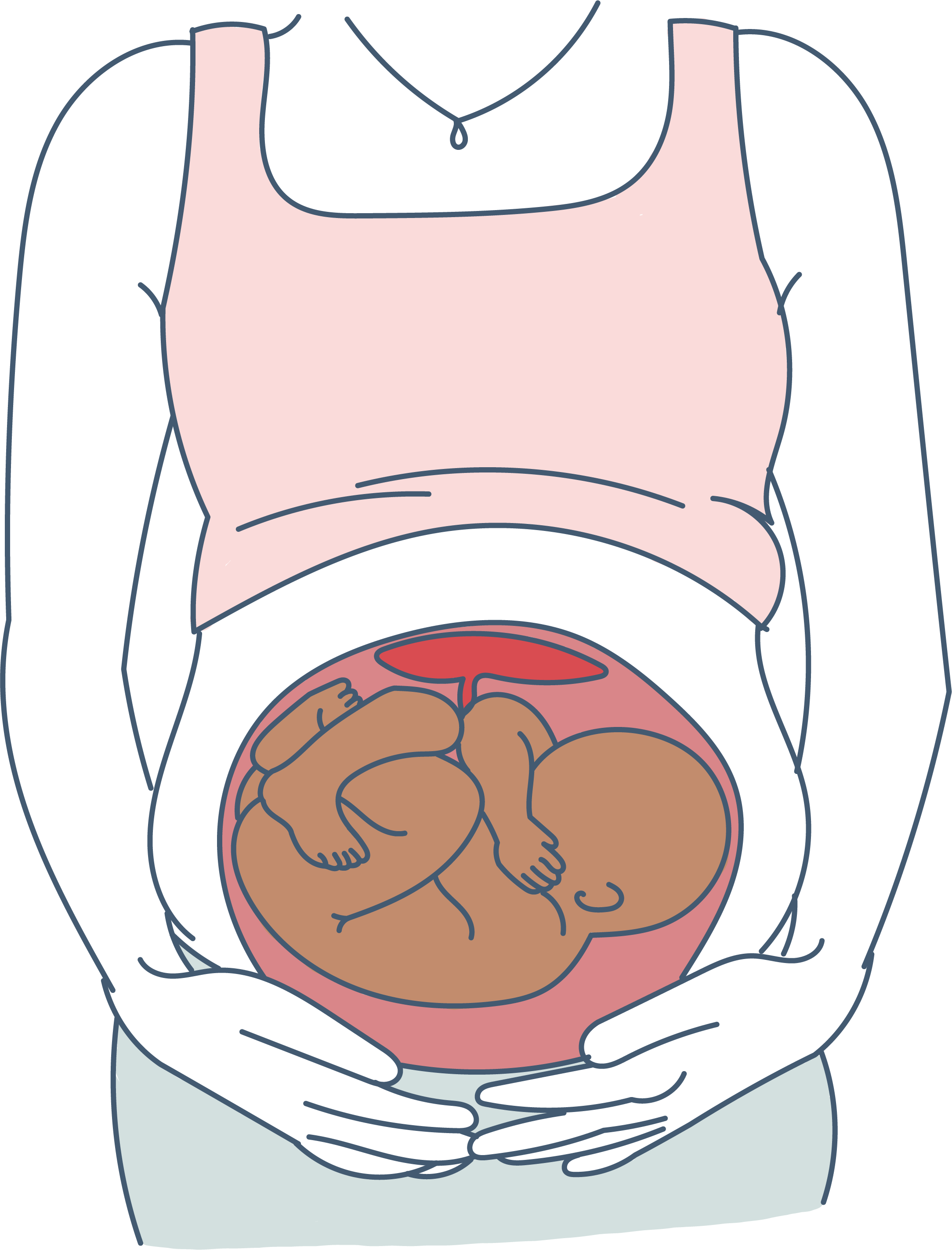
- Are pregnant with multiples
- Have placenta previa (when the placenta covers the cervix)
Transverse Lie
In transverse lie position, the fetus is presenting sideways across the uterus rather than vertically. They may be:
- Down, with the back facing the birth canal
- With one shoulder pointing toward the birth canal
- Up, with the hands and feet facing the birth canal
If a transverse lie is not corrected before labor, a C-section will be required. This is typically the case.
Determining Fetal Position
Your healthcare provider can determine if your baby is in cephalic presentation by performing a physical exam and ultrasound.
In the final weeks of pregnancy, your healthcare provider will feel your lower abdomen with their hands to assess the positioning of the baby. This includes where the head, back, and buttocks lie
If your healthcare provider senses that the fetus is in a breech position, they can use ultrasound to confirm their suspicion.
Turning a Fetus So They Are in Cephalic Position
External cephalic version (ECV) is a common, noninvasive procedure to turn a breech baby into cephalic position while it's still in the uterus.
This is only considered if a healthcare provider monitors presentation progress in the last trimester and notices that a fetus is maintaining a noncephalic position as your delivery date approaches.
External Cephalic Version (ECV)
ECV involves the healthcare provider applying pressure to your stomach to turn the fetus from the outside. They will attempt to rotate the head forward or backward and lift the buttocks in an upward position. Sometimes, they use ultrasound to help guide the process.
The best time to perform ECV is about 37 weeks of pregnancy. Afterward, the fetal heart rate will be monitored to make sure it’s within normal levels. You should be able to go home after having ECV done.
ECV has a 50% to 60% success rate. However, even if it does work, there is still a chance the fetus will return to the breech position before birth.
Natural Methods For Turning a Fetus
There are also natural methods that can help turn a fetus into cephalic position. There is no medical research that confirms their efficacy, however.
- Changing your position: Sometimes a fetus will move when you get into certain positions. Two specific movements that your provider may recommend include: Getting on your hands and knees and gently rocking back and forth. Another you could try is pushing your hips up in the air while laying on your back with your knees bent and feet flat on the floor (bridge pose).
- Playing stimulating sounds: Fetuses gravitate to sound. You may be successful at luring a fetus out of breech position by playing music or a recording of your voice near your lower abdomen.
- Chiropractic care: A chiropractor can try the Webster technique. This is a specific chiropractic analysis and adjustment which enables chiropractors to establish balance in the pregnant person's pelvis and reduce undue stress to the uterus and supporting ligaments.
- Acupuncture: This is a considerably safe way someone can try to turn a fetus. Some practitioners incorporate moxibustion—the burning of dried mugwort on certain areas of the body—because they believe it will enhance the chances of success.
A Word From Verywell
While most babies are born in cephalic position at delivery, this is not always the case. And while some fetuses can be turned, others may be more stubborn.
This may affect your labor and delivery wishes. Try to remember that having a healthy baby, and staying well yourself, are your ultimate priorities. That may mean diverting from your best laid plans.
Speaking to your healthcare provider about turning options and the safest route of delivery may help you adjust to this twist and feel better about how you will move ahead.
Glezerman M. Planned vaginal breech delivery: current status and the need to reconsider . Expert Rev Obstet Gynecol. 2012;7(2):159-166. doi:10.1586/eog.12.2
Cleveland Clinic. Fetal positions for birth .
MedlinePlus. Breech birth .
UT Southwestern Medical Center. Can you turn a breech baby around?
The American College of Obstetricians and Gynecologists. If your baby is breech .
Roecker CB. Breech repositioning unresponsive to Webster technique: coexistence of oligohydramnios . Journal of Chiropractic Medicine . 2013;12(2):74-78. doi:10.1016/j.jcm.2013.06.003
By Cherie Berkley, MS Berkley is a journalist with a certification in global health from Johns Hopkins University and a master's degree in journalism.

- Vishal's account
- Prenatal Care
Fetal Cephalic Presentation During Pregnancy

What Is Cephalic Position?
Types of cephalic position, benefits of cephalic presentation, risks of cephalic position, what are some other positions and their associated risks, when does a foetus get into the cephalic position, how do you know if baby is in cephalic position, how to turn a breech baby into cephalic position, natural ways to turn a baby into cephalic position.
If your baby is moving around in the womb, it’s a good sign as it tells you that your baby is developing just fine. A baby starts moving around in the belly at around 14 weeks. And their first movements are usually called ‘ quickening’ or ‘fluttering’.
A baby can settle into many different positions throughout the pregnancy, and it’s alright. But it is only when you have reached your third and final trimester that the position of your baby in your womb will matter the most. The position that your baby takes at the end of the gestation period will most likely be how your baby will make its appearance in the world. Out of all the different positions that your baby can settle into, the cephalic position at 36 weeks is considered the best position. Read on to learn more about fetal cephalic presentation.
When it comes to cephalic presentation meaning, the following can be considered. A baby is in the cephalic position when he is in a head-down position. This is the best position for them to come out in. In case of a ‘cephalic presentation’, the chances of a smooth delivery are higher. This position is where your baby’s head has positioned itself close to the birth canal, and the feet and bottom are up. This is the best position for your baby to be in for safe and healthy delivery.
Your doctor will begin to keep an eye on the position of your baby at around 34 weeks to 36 weeks . The closer you get to your due date, the more important it is that your baby takes the cephalic position. If your baby is not in this position, your doctor will try gentle nudges to get your baby in the right position.
Though it is pretty straightforward, the cephalic position actually has two types, which are explained below:
1. Cephalic Occiput Anterior
Most babies settle in this position. Out of all the babies who settle in the cephalic position, 95% of them will settle this way. This is when a baby is in the head-down position but is facing the mother’s back. This is the preferred position as the baby is able to slide out more easily than in any other position.
2. Cephalic Occiput Posterior
In this position, the baby is in the head-down position but the baby’s face is turned towards the mother’s belly. This type of cephalic presentation is not the best position for delivery as the baby’s head could get stuck owing to its wide position. Almost 5% of the babies in cephalic presentation settle into this position. Babies who come out in this position are said to come out ‘sunny side up’.
Cephalic presentation, where the baby’s head is positioned down towards the birth canal, is the most common and optimal fetal presentation for childbirth. This positioning facilitates a smoother delivery process for both the mother and the baby. Here are several benefits associated with cephalic presentation:
1. Reduced risk of complications
Cephalic presentation decreases the likelihood of complications during labor and delivery , such as umbilical cord prolapse or shoulder dystocia, which can occur with other presentations.
2. Easier vaginal delivery
With the baby’s head positioned first, vaginal delivery is generally easier and less complicated compared to other presentations, resulting in a smoother labor process for the mother.
3. Lower risk of birth injuries
Cephalic presentation reduces the risk of birth injuries to the baby, such as head trauma or brachial plexus injuries, which may occur with other presentations, particularly breech or transverse positions.
4. Faster progression of labor
Babies in cephalic presentation often help to stimulate labor progression more effectively through their positioning, potentially shortening the duration of labor and reducing the need for medical interventions.
5. Better fetal oxygenation
Cephalic presentation typically allows for optimal positioning of the baby’s head, which facilitates adequate blood flow and oxygenation, contributing to the baby’s well-being during labor and delivery.
Factors such as the cephalic posterior position of the baby and a narrow maternal pelvis can increase the likelihood of complications during childbirth. Occasionally, infants in the cephalic presentation may exhibit a backward tilt of their heads, potentially leading to preterm delivery in rare instances.
In addition to cephalic presentation, there are several other fetal positions that can occur during pregnancy and childbirth, each with its own associated risks. These positions can impact the delivery process and may require different management strategies. Here are two common fetal positions and their associated risks:
1. Breech Presentation
- Babies in breech presentation, where the buttocks or feet are positioned to enter the birth canal first, are at higher risk of birth injuries such as hip dysplasia or brachial plexus injuries.
- Breech presentation can lead to complications during labor and delivery, including umbilical cord prolapse, entrapment of the head, or difficulty delivering the shoulders, necessitating interventions such as cesarean section.
2. Transverse Lie Presentation
- Transverse lie , where the baby is positioned sideways across the uterus, often leads to prolonged labor and increases the likelihood of cesarean section due to difficulties in the baby’s descent through the birth canal.
- The transverse position of the baby may result in compression of the umbilical cord during labor, leading to decreased oxygen supply and potential fetal distress. This situation requires careful monitoring and intervention to ensure the baby’s well-being.
When a foetus is moving into the cephalic position, it is known as ‘head engagement’. The baby stars getting into this position in the third trimester, between the 32nd and the 36th weeks, to be precise. When the head engagement begins, the foetus starts moving down into the pelvic canal. At this stage, very little of the baby is felt in the abdomen, but more is felt moving downward into the pelvic canal in preparation for birth.
You may think that in order to find out if your baby has a cephalic presentation, an ultrasound is your only option. This is not always the case. You can actually find out the position of your baby just by touching and feeling their movements.
By rubbing your hand on your belly, you might be able to feel their position. If your baby is in the cephalic position, you might feel their kicks in the upper stomach. Whereas, if the baby is in the breech position, you might feel their kicks in the lower stomach.
Even in the cephalic position, it may be possible to tell if your baby is in the anterior position or in the posterior position. When your baby is in the anterior position, they may be facing your back. You may be able to feel your baby move underneath your ribs. It is likely that your belly button will also pop out.
When your baby is in the posterior position, you will usually feel your baby start to kick you in your stomach. When your baby has its back pressed up against your back, your stomach may not look rounded out, but flat instead.
Mothers whose placentas have attached in the front, something known as anterior placenta , you may not be able to feel the movements of your baby as well as you might like to.
Breech babies can make things complicated. Both the mother and the baby will face some problems. A breech baby is positioned head-up and bottom down. In order to deliver the baby, the birth canal needs to open a lot wider than it has to in the cephalic position. Besides this, your baby can get an arm or leg entangled while coming out.
If your baby is in the breech position, there are some things that you can do to encourage the baby to get into the cephalic position. There are a few exercises that could help such as pelvic tilts , swimming , spending a bit of time upside down, and belly dancing are a few ways you can try yourself to get your baby into the head-down position .
If this is not working either, your doctor will try an ECV (External Cephalic Version) . Here, your doctor will be hands-on, applying some gentle, but firm pressure to your tummy. In order to reach a cephalic position, the baby will need to be rolled into a bottom’s up position. This technique is successful around 50% of the time. When this happens, you will be able to have a normal vaginal delivery.
Though it sounds simple enough to get the fetal presentation into cephalic, there are some risks involved with ECV. If your doctor notices your baby’s heart rate starts to become problematic, the doctor will stop the procedure right away.
Encouraging a baby to move into the cephalic position, where the head is down towards the birth canal, is often desirable for smoother labor and delivery. While medical interventions may be necessary in some cases, there are natural methods that pregnant individuals can try to help facilitate this positioning. Here are several techniques that may help turn a baby into the cephalic position:
1. Optimal Maternal Positioning
Maintaining positions such as kneeling, hands and knees, or pelvic tilts may encourage the baby to move into the cephalic position by utilizing gravity and reducing pressure on the pelvis.
2. Spinning Babies Techniques
Specific exercises and positions recommended by the Spinning Babies organization, such as Forward-Leaning Inversion or the Sidelying Release, aim to promote optimal fetal positioning and may help encourage the baby to turn cephalic.
3. Chiropractic Care or Acupuncture
Some individuals find that chiropractic adjustments or acupuncture sessions with qualified practitioners can help address pelvic misalignment or relax tight muscles, potentially creating more space for the baby to maneuver into the cephalic position.
4. Prenatal Yoga and Swimming
Engaging in gentle exercises like prenatal yoga or swimming may help promote relaxation, reduce stress on the uterine ligaments, and encourage the baby to move into the cephalic position naturally. These activities also support overall physical and mental well-being during pregnancy.
1. What factors influence whether my baby will be in cephalic presentation?
Several factors can influence your baby’s position during pregnancy, including the shape and size of your uterus, the strength of your abdominal muscles, the amount of amniotic fluid, and the position of the placenta . Additionally, your baby’s own movements and preferences play a role.
2. Is it necessary for my baby to be in cephalic presentation for a vaginal delivery?
While cephalic presentation is considered the optimal position for vaginal delivery, some babies born in non-cephalic presentations can still be safely delivered vaginally with the guidance of a skilled healthcare provider. However, certain non-cephalic presentations may increase the likelihood of needing a cesarean section.
3. What can I do to encourage my baby to stay in the cephalic presentation?
Maintaining good posture, avoiding positions that encourage the baby to settle into a breech or transverse lie, staying active with gentle exercises, and avoiding excessive reclining can all help encourage your baby to remain in the cephalic presentation. Additionally, discussing any concerns with your healthcare provider and following their recommendations can be beneficial.
This was all about fetus with cephalic presentation. Most babies get into the cephalic position on their own. This is the most ideal situation as there will be little to no complications during normal vaginal labour. There are different cephalic positions, but these should not cause a lot of issues. If your baby is in any position other than cephalic in pregnancy, you may need C-Section . Keep yourself updated on the smallest of progress during your pregnancy so that you are aware of everything that is going on. Go for regular check-ups as your doctor will be able to help you if a complication arises during acephalic presentation at 20, 28 and 30 weeks.
References/Resources:
1. Glezerman. M; Planned vaginal breech delivery: current status and the need to reconsider (Expert Review of Obstetrics & Gynecology); Taylor & Francis Online; https://www.tandfonline.com/doi/full/10.1586/eog.12.2 ; January 2014
2. Feeling your baby move during pregnancy; UT Southwestern Medical Center; https://utswmed.org/medblog/fetal-movements/
3. Fetal presentation before birth; Mayo Clinic; https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/fetal-positions/art-20546850
4. Fetal Positions; Cleveland Clinic; https://my.clevelandclinic.org/health/articles/9677-fetal-positions-for-birth
5. FAQs: If Your Baby Is Breech; American College of Obstetricians and Gynecologists; https://www.acog.org/womens-health/faqs/if-your-baby-is-breech
6. Roecker. C; Breech repositioning unresponsive to Webster technique: coexistence of oligohydramnios (Journal of Chiropractic Medicine); Science Direct; https://www.sciencedirect.com/science/article/abs/pii/S1556370713000588 ; June 2013
7. Presentation and position of baby through pregnancy and at birth; Pregnancy, Birth & Baby; https://www.pregnancybirthbaby.org.au/presentation-and-position-of-baby-through-pregnancy-and-at-birth
Belly Mapping Pregnancy Belly Growth Chart Baby in Vertex Position during Labour and Delivery
- RELATED ARTICLES
- MORE FROM AUTHOR

Why Should You Avoid Eating Liquorice Root During Pregnancy?

17 Weeks Pregnant Ultrasound - What to Expect

Black (Dark) Poop While Pregnant: Causes & Prevention


Smoking During Pregnancy: Effects On You And Your Baby

Baby Shower Food Ideas to Impress Your Guests

7 Yoga Poses to Avoid When Pregnant and Why
Popular on parenting.

245 Rare Boy & Girl Names with Meanings

Top 22 Short Moral Stories For Kids

170 Boy & Girl Names That Mean 'Gift from God'

800+ Unique & Cute Nicknames for Boys & Girls
Latest posts.

90 Hilarious Winter Jokes for Kids to Make Holiday More Fun

60 Best Back to School Jokes for Kids to Start the Year With a Smile

100+ Heartfelt Thank You Messages and Quotes for Parents

150+ Step Daughter Quotes to Show Your Love

I want to publish
To find out how to publish or submit your book proposal:
To find a journal or submit your article to a journal:
- Cephalic Presentation
- Medicine and Healthcare
- Obstetrics, Gynecology & Women'S Health
Management of Labour and Delivery – Questions
Rekha Wuntakal, Madhavi Kalidindi, Tony Hollingworth in Get Through , 2014
For each clinical scenario below, choose the single most appropriate stage of labour from the above list of options. Each option may be used once, more than once or not at all. A 30-year-old para 3 woman was admitted at term with regular uterine activity at 5 cm cervical dilatation and 4 hours later she delivered a female neonate with APGARs 9, 10, 10 at 1, 5 and 10 minutes. Syntometrine injection was given immediately after delivery and placenta with membranes was delivered completely 20 minutes after the delivery of the baby by continuous cord traction.A 23-year-old para 3 woman was admitted after spontaneous rupture of membranes at 39 weeks’ gestation. She is contracting 4 in 10 minutes and pushing involuntarily. On vaginal examination the cervix was fully dilated, vertex was 2 cm below the spines in direct occipito-anterior position with minimal caput and moulding.A 30-year-old nulliparous woman was admitted at term with uterine contractions once in every 5 minutes. On examination, the fetus is in cephalic presentation with two fifths palpable per abdomen. The cervix is central, soft, fully effaced and 2 cm dilated with intact membranes.
Biometric Measurements and Normal Growth Parameters in a Child
Nirmal Raj Gopinathan in Clinical Orthopedic Examination of a Child , 2021
In cephalic presentation, the intra-uterine fetal position is of universal flexion, which is carried by the child to the immediate post-partum period. The hips and knees are flexed. The lower legs are internally rotated. The feet are further internally rotated with respect to the lower legs. At times there is an external rotational contracture of the hip that tends to mask the true femoral rotational profile. The anatomy of the lower limbs changes significantly as the child grows. This is primarily in response to the development of motor abilities and the ability of the child to crawl, cruise, stand, walk, and finally run. These changes are seen right from the hip joints, the femoral neck, knees, and tibia to the feet.
DRCOG MCQs for Circuit A Questions
Una F. Coales in DRCOG: Practice MCQs and OSCEs: How to Pass First Time three Complete MCQ Practice Exams (180 MCQs) Three Complete OSCE Practice Papers (60 Questions) Detailed Answers and Tips , 2020
External cephalic version: Used to convert a breech presentation to cephalic presentation.Not contraindicated if there is a prior Caesarean section scar.Can cause premature labour.Contraindicated in hypertension.Can be performed after 33 weeks' gestation in a rhesus-negative mother.
Complex maternal congenital anomalies – a rare presentation and delivery through a supra-umbilical abdominal incision
Published in Journal of Obstetrics and Gynaecology , 2018
Samantha Bonner, Yara Mohammed
She had a spontaneous conception and booked at 9 weeks of gestation under consultant-led care. A scan confirmed the pregnancy was in the right uterus. She had no other significant medical history but did suffer from recurrent urinary tract infections and hence was on low-dose antibiotic prophylaxis. There was no sonographic evidence of hydronephrosis. Her body mass index (BMI) was 18 at the time of booking. Combined screening was low risk and she had a normal 20 week anomaly scan. She had serial growth scans which demonstrated a normal growth trajectory on a customised chart. The baby was consistently a cephalic presentation. She had multidisciplinary antenatal care, including specialist urologists, general surgeons, obstetricians and anaesthetists. An antenatal MRI scan had shown extensive adhesions over the lower segment of the uterus. She was extensively counselled regarding the mode of delivery and this was scheduled at 37 weeks of gestation to avoid the potential of spontaneous labour and an emergency Caesarean section.
Utilization of epidural volume extension technique for external cephalic version
Published in Baylor University Medical Center Proceedings , 2021
Hanna Hussey, James Damron, Mark F. Powell, Michelle Tubinis
Repeat ultrasound demonstrated breech presentation, normal amniotic fluid volume, and fetal head toward the maternal left abdomen. After 0.25 mg of intramuscular terbutaline injection, a forward roll was initiated by applying pressure from behind the fetal head toward the maternal left. Continuous progress was made and bedside ultrasound showed cephalic presentation. Immediately after successful ECV, the fetal heart rate was 70 beats/min but returned to baseline with conservative measures. Motor blockade regressed after approximately 1.5 hours. After 4 hours of fetal heart rate monitoring and tocometry, the patient was deemed stable for discharge. Follow-up discussion with the patient via phone call on postprocedure day 1 confirmed that she was not experiencing pain or concerning symptoms for neuraxial complications. She returned to the labor and delivery unit at 40 weeks’ gestation for elective induction of labor and had a successful vaginal delivery.
Antenatal scoring system in predicting the success of planned vaginal birth following one previous caesarean section
Aida Kalok, Shahril A. Zabil, Muhammad Abdul Jamil, Pei Shan Lim, Mohamad Nasir Shafiee, Nirmala Kampan, Shamsul Azhar Shah, Nor Azlin Mohamed Ismail
The inclusion criteria were pregnant women at 36 weeks of gestation or more with singleton foetus in cephalic presentation, who agreed for trial of vaginal delivery after one lower segment caesarean section. We excluded women with contraindication for vaginal birth, or who declined trial of vaginal delivery from this study. Previous antenatal history was noted and recorded during the 36-week assessment, including year and indication for previous caesarean section. Recurrent indications involved were cephalopelvic disproportion and obstructed labour. While non-recurrent indications were foetal distress and malpresentation. Past operative notes were checked for any operative complications such as extended uterine tear, organ injury and post-partum haemorrhage. Information regarding current pregnancy including pre-existing medical disorder was recorded. Estimated foetal weight based on ultrasound scan at 36 weeks of gestation was used in this study.
Related Knowledge Centers
- Breech Birth
- Occipital Bone
- Pelvic Cavity
- Presentation
- Shoulder Presentation
Current Research
- Clinical Trials (United States)
- Clinical Trials (Europe)
- Clinical Trials (Australia/New Zealand)
- Clinical Trials (India)
Knowledge is an evolving asset. Help us improve this page for a future release.

Which Way Is Up? What Your Baby’s Position Means For Your Delivery
by Physicians & Midwives | Feb 11, 2022 | Pregnancy

“Will I be able to have a vaginal delivery?”, “Will labor pains be more in my pelvis or back?”, and “How long will labor and delivery last?” are all questions that have probably entered your head at some point. The answers to these questions, in large part, depend on the position of your baby within your uterus at the time you go into labor. Medical professionals call this the fetal presentation and position. Let’s break down different fetal presentations and what your baby’s position could mean for your delivery.
Cephalic presentation
Almost all (95-97%) babies are delivered by cephalic presentation, where they are head-down with legs and feet at the top of the uterus. Most babies move into the head-down position by the third trimester. Cephalic presentation is further broken down by the position of the head; in the vast majority of cephalic deliveries, the crown or top of the head (called the vertex), enters the birth canal first and is the first part of the baby to be delivered. This is what we mean when we say a baby is “crowning”.

In most cases of vertex presentation, the back of the baby’s head (called the occiput) is toward the front (anterior) of the mother’s pelvis. This presentation is called occiput anterior and is considered the best position for a vaginal delivery. This position is considered best because this position typically leads to the easiest navigation of the baby through the birth canal.
Around 5% of babies are delivered in the occiput posterior position, where the back of the baby’s head is toward the mother’s backbone and tailbone. This is popularly believed to be the cause of painful “back labor”, although the scientific support for this is somewhat lacking. What is known is that the occiput posterior presentation can significantly prolong labor, and is three times more likely than occiput anterior presentation to result in cesarean section. This comes down to less ease of passage through the birth canal. Occiput posterior presentation is more common in older and first-time mothers, as well as with larger or overdue babies. Surfing the internet will provide you with many different exercises which claim to prevent occiput posterior presentation, but none of these have been scientifically proven to be of benefit.
Rarely (around 1 in every 800 births), the baby will present face-first instead of with the top of the head. Around 70% of these babies can be delivered vaginally, although the labor may be mildly prolonged. The remainder tend to be delivered by cesarean section either because the labor is not progressing or because the doctor or midwife is concerned about the baby’s heart rate. Around 5% of babies are delivered in the occiput posterior position, where the back of the baby’s head is toward the mother’s backbone and tailbone. This is popularly believed to be the cause of painful “back labor”, although the scientific support for this is somewhat lacking. What is known is that the occiput posterior presentation can significantly prolong labor, and is three times more likely than occiput anterior presentation to result in cesarean section. This comes down to less ease of passage through the birth canal. Occiput posterior presentation is more common in older and first-time mothers, as well as with larger or overdue babies. Surfing the internet will provide you with many different exercises which claim to prevent occiput posterior presentation, but none of these have been scientifically proven to be of benefit.
Breech presentation
Shoulder presentation.
- Brand Resource Library
- Marketing Collateral
- Business Cards
- Gmail Signature
- PowerPoint Master Template
- Signage & Wayfinding
- Style Guides
- Submit a Design Request
- 011 4211 1111
- 011 4290 9090 (E)

Posterior Placenta: 5 Myths (and Facts) You Need to Know
By Sitaram Bhartia Team | September 29, 2020 | Maternity | 2020-09-29 05 August 2024
The placenta is an organ that supplies oxygen and nutrients via the umbilical cord to the baby and plays an important role in pregnancy.
“Ultrasound reports sometimes mention a posterior or an anterior placenta but these are not significant findings,” says Dr. Anita Sabherwal Anand , Senior Obstetrician-Gynecologist at Sitaram Bhartia Hospital in South Delhi.
Where is the placenta located?
The placenta can be positioned in any of these ways:
Anterior placenta : This means that the placenta is located toward the front wall of the uterus.
Posterior placenta : The placenta is attached to the back wall of the uterus. The term ‘fundal posterior’ means that the placenta is toward the top and back of the uterine wall as ‘fundal’ means the top of the fundus/uterus.
Low Lying Placenta: The placenta is often positioned in the lower segment of the uterus in the early weeks of pregnancy. After 20 weeks as the uterus grows bigger, the placenta shifts away from the lower segment.
Are there any implications of the placental position?
Most positions of the placenta , whether it is located at the back or the front do not signify anything in particular.
Located in Delhi and looking for an experienced gynaecologist to get advice on the posterior placenta? Book a paid consultation with Dr Anita by clicking the button below.

5 Myths to know about Posterior Placenta
Expecting parents often have queries around placenta position and the baby’s gender, the best position for a normal delivery and so on.
The doctor clarifies these concerns so that expecting couples can be more informed and less stressed about pregnancy.
- Posterior placenta linked to gender of fetus : There is no scientific evidence that proves that a posterior placenta means a boy or a girl . The same holds true for a fundal posterior placenta and an anterior placenta . “A few studies may have indicated a relation between the placental position and gender but there are no references to this theory in medical literature.”
- Posterior placenta heightens fetal movement: “A few anecdotal reports suggest that mothers feel stronger kicks early in pregnancy when the placenta is positioned at the back or subtle kicks due to an anterior placenta as it cushions the kicks, but there is no solid study that validates these claims. “
- Posterior placenta increases risk of preterm labour : None of the national or international obstetrics guidelines substantiate the findings that a posterior placenta increases the risk of preterm delivery and an anterior placenta increases the risk of pregnancy induced hypertension , gestational diabetes or intrauterine growth restriction.
- Posterior placenta is the best position: It is believed that this is the most ideal position as it allows the baby to move into the correct position.
- Posterior placenta impacts chances of normal delivery : “You can have a vaginal birth as long as the placenta does not cover the cervix, as this prevents the baby from descending down the birth canal and causes painless bleeding.”
“In such a situation, a cesarean becomes the best method to deliver the baby safely.”
The position of the placenta can vary from woman to woman and each of her pregnancies.
“It can be exciting to discuss every detail of an ultrasound report with friends and family but you needn’t become unnecessarily anxious about unscientific assertions. Enjoy your pregnancy – eat right , practice breathing exercises and yoga – and believe that all will be well!”
This blog post has been written with editorial inputs from Dr. Anita Sabherwal Anand, who has over 24 years of experience, and is known for the time and attention she gives to pregnant couples.
Please book an appointment with Dr Anita by Clicking the button below.

More Resources:
- 5 Easy Tips You Need to Know for a Normal Delivery
- Ask Your Gynaecologist for her C-Section Rate
- C-Section Delivery: 9 Indications Where It May Be Avoidable
START TYPING AND PRESS ENTER TO SEARCH
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Geburtshilfe Frauenheilkd
- v.76(3); 2016 Mar
Language: English | German
Foetal Gender and Obstetric Outcome
Fetales geschlecht und geburtshilfliches outcome, b. schildberger.
1 FH Gesundheitsberufe OÖ, Linz, Österreich
2 Institut für klinische Epidemiologie der Tirol Kliniken, Innsbruck, Österreich
Associated Data
Introduction: Data on specific characteristics based on the gender of the unborn baby and their significance for obstetrics are limited. The aim of this study is to analyse selected parameters of obstetric relevance in the phases pregnancy, birth and postpartum period in dependence on the gender of the foetus. Materials and Methods: The selected study method comprised a retrospective data acquisition and evaluation from the Austrian birth register of the Department of Clinical Epidemiology of Tyrolean State Hospitals. For the analysis all inpatient singleton deliveries in Austria during the period from 2008 to 2013 were taken into account (live and stillbirths n = 444 685). The gender of the baby was correlated with previously defined, obstetrically relevant parameters. Results: In proportions, significantly more premature births and sub partu medical interventions (vaginal and abdominal surgical deliveries. episiotomies) were observed for male foetuses (p < 0.001). The neonatal outcome (5-min Apgar score, umbilical pH value less than 7.1, transfer to a neonatal special unit) is significantly poorer for boys (p < 0.001). Discussion: In view of the vulnerability of male foetuses and infants, further research is needed in order to be able to react appropriately to the differing gender-specific requirements in obstetrics.
Zusammenfassung
Einleitung: Die Studienlage über die vom Geschlecht des ungeborenen Kindes ausgehenden Spezifika und deren Bedeutung in der Geburtshilfe ist limitiert. Ziel der Arbeit ist, anhand ausgewählter, geburtshilflich relevanter Parameter die Phasen Schwangerschaft, Geburt und Wochenbett in Abhängigkeit zum fetalen Geschlecht zu analysieren. Material und Methoden: Als Methode wurde eine retrospektive Datenerhebung und -auswertung aus dem Geburtenregister Österreich des Instituts für klinische Epidemiologie der Tirol Kliniken gewählt. Zur Analyse wurden alle stationären Einlingsgeburten in Österreich im Zeitraum von 2008–2013 (Lebend- und Totgeburten n = 444 685) herangezogen. Das Geschlecht des Kindes wurde mit vorab definierten, geburtshilflich relevanten Variablen in Beziehung gesetzt. Ergebnisse: Im Verhältnis sind bei männlichen Feten signifikant mehr Frühgeburten und medizinische Interventionen sub partu (vaginal und abdominal operativer Entbindungsmodus, Episiotomie) zu verzeichnen (p < 0,001). Das neonatale Outcome (5-min-Apgar-Wert, Na-pH-Wert unter 7,1, Verlegung auf neonatologische Abteilung) ist bei Knaben signifikant schlechter (p < 0,001). Diskussion: Im Hinblick auf die Vulnerabilität von männlichen Feten und Neugeborenen ist weitere Forschung notwendig, um in der Geburtshilfe den geschlechtsspezifisch unterschiedlichen Bedarfen entsprechend agieren zu können.
Introduction
The available studies on foetal gender as a specific influencing variable during pregnancy and birth are limited. In comparison our knowledge on the progress of infantile growth is relatively certain. In 280 days the unborn baby achieves a length of ca. 50 centimetres, whereby infant boys have on average a body length 1 centimetre and a head circumference of ca. 5 millimetres more than infant girls. At all times during pregnancy female foetuses have larger length-weight and head circumference-weight ratios than males. Already in the second trimester girls exhibit a shorter femur length and a smaller biparietal head diameter. Although girls show a lower intrauterine growth in comparison to boys they exhibit an accelerated maturation of about 4–6 weeks 1 .
Various studies have shown that placental dysfunctions, especially severe pre-eclampsia and intrauterine growth retardation, occur significantly more frequently in pregnancies involving a male foetus. The placentas of male foetuses exhibit significantly higher rates of deciduitis and velamentous navel insertions as well as a significantly lower incidence of placental infarction than the placenta of female foetuses 2 , 3 , 4 , 5 , 6 .
In the mothers of male infants, in comparison to the mothers of female babies, higher incidences of premature rupture of membranes and premature births can be observed 7 . The rates of gestational diabetes mellitus, macrosomia, protracted opening and expulsion phases, umbilical cord prolapses, umbilical cord looping and genuine umbilical cord knots are significantly elevated. Furthermore, male babies are more frequently delivered by Caesarean section than female babies 7 , 8 , 9 .
Also, the rates of vaginal surgical deliveries are higher, and the indication for birth completion is more frequently given with the diagnosis of “threatening intrauterine asphyxia” in the case of male babies. The rate of sonographically diagnosed growth retardation, however, is higher for female infants 10 .
Several studies have recognised male gender as being a risk factor during pregnancy and birth. The biological mechanisms of this gender-specific difference are, however, still virtually unknown even though various theories discuss the influence of hormonal, physiological or genetic factors 8 , 11 , 12 , 13 , 14 .
Although new management strategies have led to better and better therapeutic results for very preterm infants, boys still exhibit higher mortality and morbidity than girls. For boys in the group of very preterm infants significant differences can be seen in the criteria higher birth weight, oxygen dependency, hospital stay, pulmonary bleeding, treatment with steroids, skull anomalies and mortality. These differences also remain significant in the subsequent course. The authors conclude that male gender per se represents a risk factor for the poor general condition of very premature babies as well as for their poorer developmental course 15 , 16 , 17 .
The accelerated maturation for girls is well known and, in the neonatal period and infancy, results in girls having a markedly greater ability to form a primary relationship, being emotional stable, easier to calm down and being less restless. The perception of social and other interactions starts earlier in girls. In boys, on the other hand, the early ability to form relationships and coping strategies, for example, in cases of pain and discomfort are influenced by the greater restlessness, the delayed development of sleep rhythm and the vulnerability. “In unfavourable circumstances this leads to a higher degree of psychophysical stress in the male child” 18 .
The consideration of gender-specific components already in the perinatal phase should, in the sense of the aims of gender medicine, help to optimise the preventative, diagnostic, therapeutic and rehabilitation processes of general and health care from the very beginning “to act as an important step and bridge towards personalised medicine” 19 .
The aim of this study is to consider with the help of selected obstetrically relevant parameters the phases pregnancy, birth and postpartum period in relation to foetal gender. On the basis of the above-mentioned considerations, we posed the following guiding question for our research: what influence does foetal gender have on selected obstetric parameters?
Materials and Methods
For this publication we have obtained a positive vote from the Ethics Commission of Upper Austria and permission for the data analysis from the board of the Austrian birth register at the Department of Clinical Epidemiology of Tyrolean State Hospitals in Innsbruck.
We have decided upon a retrospective data acquisition and evaluation from the Austrian birth register as method for this study. The Austrian birth register contains the results of all births occurring in hospitals in Austria since 2008 in an epidemiological data base.
Samples and variables
For the analysis, all inpatient singleton births in Austria in the period from 2008 to 2013 (n = 444 685 live births) were included. The gender of the baby was correlated with the following, previously defined and obstetrically relevant variables: parity, duration of pregnancy, birth weight, tocolysis, position of the baby at birth, drug-induced labour, micro blood gas analysis sub partu, peridural or spinal anaesthesia, delivery mode, delivery position, duration of delivery, performance of episiotomy, perineal trauma, 5-min Apgar score, umbilical cord pH, disorder of placenta separation, transfer of the infant post partum to neonatal department, perinatal mortality.
The parameters duration of delivery, episiotomy, 5-min Apgar score, umbilical cord pH under 7.1 and transfer of the baby to a neonatal department were additionally analysed with the specific sample “live birth at term” (gestational weeks 36 + 6–42 + 0) (n = 411 380), in order to enable a differentiated presentation of the results.
Statistical evaluation
The χ2 test was used for the statistical evaluation and presentation of the results. As a consequence of the large sample size statistically significant results are possible already for small differences and have to be considered for their clinical relevance.
Among the total number of all inpatient live births from singleton pregnancies in Austria in the period 2008–2013 (n = 444 685) 51.5 % were boys and 48.5 % were girls ( Table 1 ).
Table 1 Representation of the proportions of boys and girls arranged according to the obstetric parameters. The influence of the foetal gender on selected obstetric parameters.
| Obstetric parameter | Gender of the infant | ||
|---|---|---|---|
| male | female | total | |
| 229 014 (51.5 %) | 215 671 (48.5 %) | 444 685 (100.0 %) | |
| 112 365 (51.6 %) | 105 603 (48.4 %) | 217 968 (100.0 %) | |
| 78 316 (51.4 %) | 73 994 (48.6 %) | 152 310 (100.0 %) | |
| 26 793 (51.4 %) | 25 300 (48.6 %) | 52 093 (100.0 %) | |
| 7 766 (51.7 %) | 7 255 (48.3 %) | 15 021 (100.0 %) | |
| 2 422 (51.8 %) | 2 253 (48.2 %) | 4 675 (100.0 %) | |
| 786 (50.1 %) | 782 (49.9 %) | 1 568 (100.0 %) | |
| 311 (56.0 %) | 244 (44.0 %) | 555 (100.0 %) | |
| Pearson χ (6) = 6.8979 Pr = 0.330 | |||
| 789 (55.1 %) | 644 (44.9 %) | 1 433 (100.0 %) | |
| 1 413 (56.3 %) | 1 099 (43.8 %) | 2 512 (100.0 %) | |
| 13 766 (55.2 %) | 11 153 (44.8 %) | 24 919 (100.0 %) | |
| 210 710 (51.2 %) | 200 670 (48.8 %) | 411 380 (100.0 %) | |
| 1 546 (53.4 %) | 1 347 (46.6 %) | 2 893 (100.0 %) | |
| Pearson χ (4) = 186.9733 Pr = 0.000 | |||
| 120 (47.1 %) | 135 (52.9 %) | 255 (100.0 %) | |
| 281 (50.5 %) | 275 (49.5 %) | 556 (100.0 %) | |
| 394 (55.3 %) | 318 (44.7 %) | 712 (100.0 %) | |
| 999 (52.6 %) | 900 (47.4 %) | 1 899 (100.0 %) | |
| 8 789 (46.5 %) | 10 098 (53.5 %) | 18 887 (100.0 %) | |
| 192 315 (50.2 %) | 190 619 (49.8 %) | 382 934 (100.0 %) | |
| 25 822 (66.4 %) | 13 084 (33.6 %) | 38 906 (100.0 %) | |
| Pearson χ (6) = 3.9e + 03 Pr = 0,000 | |||
| 2 550 (55.4 %) | 2 051 (44.6 %) | 4 601 (100.0 %) | |
| Pearson χ (1) = 38.5233 Pr = 0.000 | |||
| 205 194 (51.7 %) | 191 581 (48.3 %) | 396 775 (100.0 %) | |
| 12 697 (52.7 %) | 11 383 (47.3 %) | 24 080 (100.0 %) | |
| 9 389 (45.6 %) | 11 194 (54.4 %) | 20 583 (100.0 %) | |
| 701 (53.8 %) | 603 (46.2 %) | 1 304 (100.0 %) | |
| Pearson χ (3) = 309.9401 Pr = 0.000 | |||
| 27 051 (50.7 %) | 26 269 (49.3 %) | 53 320 (100.0 %) | |
| Pearson χ (1) = 0.5884 Pr = 0.443 | |||
| 3 638 (55.0 %) | 2 972 (45.0 %) | 6 610 (100.0 %) | |
| Pearson χ (1) = 47.4789 Pr = 0.000 | |||
| 51 735 (52.9 %) | 45 981 (47.1 %) | 97 716 (100.0 %) | |
| Pearson χ (1) = 14.6536 Pr = 0.000 | |||
| 147 106 (50.3 %) | 145 490 (49.7 %) | 292 596 (100.0 %) | |
| 16 076 (56.8 %) | 12 215 (43.2 %) | 28 291 (100.0 %) | |
| 352 (62.4 %) | 212 (37.6 %) | 564 (100.0 %) | |
| 283 (38.2 %) | 457 (61.8 %) | 740 (100.0 %) | |
| 2 (40.0 %) | 3 (60.0 %) | 5 (100.0 %) | |
| 31 382 (50.8 %) | 30 387 (49.2 %) | 61 769 (100.0 %) | |
| 33 456 (55.7 %) | 26 614 (44.3 %) | 60 070 (100.0 %) | |
| Pearson χ (6) = 1.0e + 03 Pr = 0.000 | |||
| 140 636 (51.1 %) | 134 551 (48.9 %) | 275 187 (100.0 %) | |
| 6 772 (50.1 %) | 6 747 (49.9 %) | 13 519 (100.0 %) | |
| 5 827 (48.6 %) | 6 153 (51.4 %) | 11 980 (100.0 %) | |
| 6 454 (49.0 %) | 6 729 (51.0 %) | 13 183 (100.0 %) | |
| Pearson χ (3) = 52.5296 Pr = 0.000 | |||
| 142 783 (50.8 %) | 138 441 (49.2 %) | 281 224 (100.0 %) | |
| 12 689 (51.9 %) | 11 748 (48.1 %) | 24 437 (100.0 %) | |
| 1 055 (49.5 %) | 1 078 (50.5 %) | 2 133 (100.0 %) | |
| Pearson χ (2) = 13.6362 Pr = 0.001 | |||
| 134 109 (50.5 %) | 131 658 (49.5 %) | 265 767 (100.0 %) | |
| 12 181 (51.7 %) | 11 372 (48.3 %) | 23 553 (100.0 %) | |
| 983 (48,8 %) | 1 033 (51,2 %) | 2 016 (100,0 %) | |
| Pearson χ (2) = 16.2652 Pr = 0.000 | |||
| 33 037 (54.6 %) | 27 447 (45.4 %) | 60 484 (100.0 %) | |
| Pearson χ (1) = 421.8449 Pr = 0.000 | |||
| 31 128 (54.4 %) | 26 050 (45.6 %) | 57 178 (100.0 %) | |
| Pearson χ (1) = 423.8031 Pr = 0.000 | |||
| 110 497 (50.5 %) | 108 510 (49.5 %) | 219 007 (100.0 %) | |
| 30 344 (50.3 %) | 30 000 (49.7 %) | 60 344 (100.0 %) | |
| 20 081 (53.0 %) | 17 780 (47.0 %) | 37 861 (100.0 %) | |
| 2 764 (58.3 %) | 1 976 (41.7 %) | 4 740 (100.0 %) | |
| 133 (54.5 %) | 111 (45.5 %) | 244 (100.0 %) | |
| Pearson χ (4) = 200.9563 Pr = 0.000 | |||
| 5 719 (47.2 %) | 6 387 (52.8 %) | 12 106 (100.0 %) | |
| Pearson χ (2) = 65.6443 Pr = 0.000 | |||
| 498 (54.1 %) | 422 (45.9 %) | 920 (100.0 %) | |
| 272 (56.5 %) | 209 (43.5 %) | 481 (100.0 %) | |
| 1 311 (59.6 %) | 889 (40.4 %) | 2 200 (100.0 %) | |
| 9 212 (56.8 %) | 7 018 (43.2 %) | 16 230 (100.0 %) | |
| 216 767 (51.2 %) | 206 247 (48.8 %) | 423 014 (100.0 %) | |
| Pearson χ (4) = 255.9797 Pr = 0.000 | |||
| 253 (52.0 %) | 234 (48.0 %) | 487 (100.0 %) | |
| 162 (54.0 %) | 138 (46.0 %) | 300 (100.0 %) | |
| 870 (61.4 %) | 548 (38.6 %) | 1 418 (100.0 %) | |
| 6 633 (56.6 %) | 5 082 (43.4 %) | 11 715 (100.0 %) | |
| 202 051 (51.0 %) | 193 949 (49.0 %) | 396 000 (100.0 %) | |
| Pearson χ (4) = 202.1802 Pr = 0.000 | |||
| 4 865 (53.9 %) | 4 154 (46.1 %) | 9 019 (100.0 %) | |
| Pearson χ (1) = 20.5651 Pr = 0.000 | |||
| 4 458 (53.6 %) | 3 863 (46.4 %) | 8 321 (100.0 %) | |
| Pearson χ (1) = 17.7195 Pr = 0.000 | |||
| 7 888 (57.5 %) | 5 829 (42.5 %) | 13 717 (100.0 %) | |
| 4 500 (56.5 %) | 3 459 (43.5 %) | 7 959 (100.0 %) | |
| 1 071 (57.0 %) | 807 (43.0 %) | 1 878 (100.0 %) | |
| Pearson χ (3) = 322.8287 Pr = 0.000 | |||
| 4 296 (57.8 %) | 3 141 (42.2 %) | 7 437 (100.0 %) | |
| 3 740 (56.4 %) | 2 886 (43.6 %) | 6 626 (100.0 %) | |
| 474 (58.6 %) | 335 (41.4 %) | 809 (100.0 %) | |
| Pearson χ (3) = 227.7274 Pr = 0.000 | |||
| 730 (51.0 %) | 702 (49.0 %) | 1 432 (100.0 %) | |
| 81 (63.3 %) | 47 (36.7 %) | 128 (100.0 %) | |
| 371 (56.7 %) | 283 (43.3 %) | 654 (100.0 %) | |
| Pearson χ (3) = 14.4344 Pr = 0.002 | |||
On analysis of the parity and its relationship to the gender of the baby, at first, no significant differences can be determined. Only after the motherʼs 7th delivery does a difference become visible: the relationship for boys of 56 % is significantly higher than that for girls with 44 %.
Duration of pregnancy and birth weight
The proportion of male infants is markedly higher than that for female infants not only for the extremely preterm births (weeks of gestation < 27 + 6) and the very preterm births (weeks of gestation 28 + 0–31 + 6) but also for the late preterm births (weeks of gestation 32 + 0–36 + 6) (55.1 : 44.9 %; 56.3 : 43.8 %; 55.2 : 44.8 %). For term births, the ratio of girls to boys is balanced. Significantly more boys (53.4 %) than girls (46.6 %) are born after completion of the 42nd week of pregnancy (p < 0.001).
For the birth weights of the babies, it is seen that in the category under 500 g the ratio of male infants with 47.1 % is markedly lower than that of female infants with 52.9 %. In the category between 500 g and 750 g the ratio of boys to girls is balanced. The ratio of male to female infants is significantly higher in the categories 750–999 g (55.3 % boys and 44.7 % girls) and 1000–1499 g (52.6 % boys and 47.4 % girls) (p < 0.001). In the category 1500–2499 g the ratio is reversed (46.5 % boys and 53.5 % girls), in the category 2500–3999 g it is balanced and in the category 4000–6500 g again markedly elevated in favour of boys (66.4 % boys and 33.6 % girls).
The proportion of pregnancies and births in which tocolysis was applied is markedly higher for male foetuses with 55.4 % as compared to females with 44.6 %.
Sub partu interventions and delivery mode
For the parameters position of the baby at delivery, the ratio of boys to girls is relatively balanced for the proper cephalic position. On the other hand, there are marked differences with higher proportions for boys in cases with anomalous cephalic presentation (52.7 % boys, 47.3 % girls) and transverse presentation (53.8 % boys, 46.2 % girls) and there are significantly more girls with breech presentations at birth (45.6 % boys, 54.4 % girls) (p < 0.001).
With regard to drug-induced labour and foetal gender no differences could be found.
Micro blood gas analyses during birth for evaluation of the general condition of the infant were employed significantly more often for boys (55 %) than for girls (45 %) (p < 0.001).
Use of peridural or, respectively, spinal anaesthesia as pain therapy during birth was requested similarly independent of the gender of the unborn baby.
With regard to the mode of delivery, there were no significant differences between the genders of the babies in the categories “spontaneous birth” and “primary Caesarean section”. The proportion of boys is markedly higher than that of girls in the vaginal surgical delivery modes (vacuum: 56.8 % boys, 43.2 % girls; forceps: 62.4 % boys, 37.6 % girls) and also in the category “secondary Caesarean section” (55.7 % boys, 44.3 % girls).
For the parameter position of the baby in vaginal deliveries, the Austrian birth register records the categories “delivery room bed”, “stool delivery”, “water birth” and “others”. In the context of these categories no relevant differences between the foetal genders could be demonstrated.
For the duration of delivery, no relationships with foetal gender could be derived. In the case of duration of delivery in excess of 24 hours, the proportion of girls is slightly elevated as compared to boys, and this is also the case in the sample of term births.
With 54.6 %, episiotomies are performed significantly more frequently in the births of boys than in the births of girls (p < 0.001). If we consider only the sample of term births (weeks of gestation 36 + 6 to 42 + 0), the result is very similar. In this subgroup the ratio is 54.4 % for the boys and 45.6 % for the girls.
Similarly, perineal traumata, especially severe perineal traumata are more frequent in the course of birth of boys than during the birth of girls.
Disorders of placental separation are significantly less frequent with 47.2 % in the placentas of male foetuses than in the placentas of female foetuses with 52.8 %.
Perinatal outcome
In the case of the 5-min Apgar score as instrument to evaluate the clinically identifiable general condition of the new born baby we find a significantly higher proportion especially of low scores for the boys. For all new born infants exhibiting an Apgar score of 9–10 after 5 minutes, the ratio between boys and girls is balanced.
This tendency can also be seen when the reduced sample of live births at term is used in the analysis (weeks of gestation 36 + 6–42 + 0).
The proportion of boys with an umbilical cord pH value of less than 7.1 is 53.9 % which is significantly higher than that for the girls with 46.1 %. Also in the sample of live births at term, boys show a significantly higher proportion of 53.6 % than girls with 46.4 % (p < 0.001).
Transfer of the new born baby to a neonatal department between birth and the 7th day after birth in all categories is significantly more frequently necessary for boys than for girls. The same result is found on evaluating the sample of live births at term.
The obstetric parameter mortality prior to birth (n = 2214) does not exhibit any differences with regard to the gender of the foetus. During delivery the relative proportion of male foetuses with 63.3 % as compared to 36.7 % for the female foetuses is markedly elevated as it is also after birth with 63.3 % for the boys and 36.7 % for the girls.
An analysis of selected, obstetrically relevant parameters in relation to the gender of the foetus provides a contribution to the gender-oriented optimisation of general and health-care management. Our results are, in principle, in accord with the results of studies by Di Renzo et al. (2007), Aibar et al. (2012) and Khalil (2013) and demonstrate that male foetuses have a higher vulnerability in the perinatal phase and a high obstetric risk 7 , 10 , 11 .
The high tendency towards premature births or, respectively, the higher rate of preterm births for boys revealed by these data confirms the results of previous studies 2 , 3 , 6 , 7 . Di Renzo et al. assumed that the higher incidences of premature rupture of membranes and preterm births among boys can be attributed to their relatively higher weights and lower gestational ages 7 . However, this assumption contradicts the results of Challis et al. (2013), who demonstrated in their study that chorionic trophoblast cells from pregnancies with a male foetus possess the potential to generate a pro-inflammatory environment by which the significantly higher rate of male preterm births than female preterm births can be explained 20 . This further substantiates the results of Zeitlin et al. (2004) that the tendency for preterm births among boys is significantly more frequently due to the spontaneous onset of contractions and less often due to a medically indicated and drug-induced completion of the pregnancy 21 . This generally high rate of preterm births requires more research initiatives on the pathophysiological processes. For this there is a need to acquire basic knowledge about the intrinsic and extrinsic triggers of the threatening preterm birth as a complex event under consideration of gender-specific characteristics.
We can also confirm the high rates of interventions among males foetuses sub partu (vaginal surgical conclusion of the birth process, Caesarean section) demonstrated in the studies of Di Renzo et al., Sheiner et al. and Dunn et al. 7 , 8 , 14 . The relatively higher rate of micro blood gas analyses (MBA) employed during the birth of boys allows the conclusion of a higher rate of at least suspected hypoxia in the foetal metabolism. In this context it is still not clear whether the physiological characteristics of boys lead more often to stress phases during birth or if the interpretation of findings (above all of CTG and MBA) require a gender-specific differentiation. In order to more exactly evaluate the foetal condition sub partu, we need a further specialisation of the possible monitoring and diagnostic options as well as their adaptation to gender-specific peculiarities.
The higher birth weight of boys may be a factor to help explain the higher rates of vaginal surgical deliveries and Caesarean sections. However, it has not been possible to confirm a relationship between higher birth weight and longer duration of birth. At duration of birth in excess of 24 hours the proportion of girls is even higher than that of boys.
As can be seen from the parameters 5-min Apgar score, umbilical pH value and transfer of the infant post partum, the higher intervention rate sub partu does not lead to a better neonatal outcome for boys in comparison to girls. Dunn et al. reported similar results where, in spite of a higher rate of interventions, lower Apgar scores, more reanimation procedures and a higher rate of respiratory distress were demonstrated for male babies 14 . Also in this context the question must be posed as to how reliable are the instruments used during birth to monitor the foetus and how valid is the interpretation of the so obtained data.
One limitation of this study is the lacking analysis of multifactorial events. This would have been suitable to more precisely describe indications, interventions and neonatal outcome in relation to foetal gender.
According to these results male foetuses and babies exhibit a vulnerable constitution not only in the prepartal phase but also sub partu and post partum. On the basis of this finding, it is essential to generate further basic knowledge about the physiological and pathophysiological processes during pregnancy and birth in dependence on the gender of the foetus.
Then it would be possible to derive preventative, diagnostic and therapeutic measures according to the foetal gender and to apply them accordingly. This knowledge could contribute to an optimisation of obstetric management, especially with regard to a reduction in the rates of preterm births and preterm interventions.
Conflict of Interest None.
Supporting Information
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 15: Abnormal Cephalic Presentations
Jessica Dy; Darine El-Chaar
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Malpresentations.
- TRANSVERSE POSITIONS OF THE OCCIPUT
- POSTERIOR POSITIONS OF THE OCCIPUT
- BROW PRESENTATIONS
- MEDIAN VERTEX PRESENTATIONS: MILITARY ATTITUDE
- FACE PRESENTATION
- SELECTED READING
- Full Chapter
- Supplementary Content
The fetus enters the pelvis in a cephalic presentation approximately 95 percent to 96 percent of the time. In these cephalic presentations, the occiput may be in the persistent transverse or posterior positions. In about 3 percent to 4 percent of pregnancies, there is a breech-presenting fetus (see Chapter 25 ). In the remaining 1 percent, the fetus may be either in a transverse or oblique lie (see Chapter 26 ), or the head may be extended with the face or brow presenting.
Predisposing Factors
Maternal and uterine factors.
Contracted pelvis: This is the most common and important factor
Pendulous maternal abdomen: If the uterus and fetus are allowed to fall forward, there may be difficulty in engagement
Neoplasms: Uterine fibromyomas or ovarian cysts can block the entry to the pelvis
Uterine anomalies: In a bicornuate uterus, the nonpregnant horn may obstruct labor in the pregnant one
Abnormalities of placental size or location: Conditions such as placenta previa are associated with unfavorable positions of the fetus
High parity
Fetal Factors
Errors in fetal polarity, such as breech presentation and transverse lie
Abnormal internal rotation: The occiput rotates posteriorly or fails to rotate at all
Fetal attitude: Extension in place of normal flexion
Multiple pregnancy
Fetal anomalies, including hydrocephaly and anencephaly
Polyhydramnios: An excessive amount of amniotic fluid allows the baby freedom of activity, and he or she may assume abnormal positions
Prematurity
Placenta and Membranes
Placenta previa
Cornual implantation
Premature rupture of membranes
Effects of Malpresentations
Effects on labor.
The less symmetrical adaptation of the presenting part to the cervix and to the pelvis plays a part in reducing the efficiency of labor.
The incidence of fetopelvic disproportion is higher
Inefficient uterine action is common. The contractions tend to be weak and irregular
Prolonged labor is seen frequently
Pathologic retraction rings can develop, and rupture of the lower uterine segment may be the end result
The cervix often dilates slowly and incompletely
The presenting part stays high
Premature rupture of the membranes occurs often
The need for operative delivery is increased
Effects on the Mother
Because greater uterine and intraabdominal muscular effort is required and because labor is often prolonged, maternal exhaustion is common
There is more stretching of the perineum and soft parts, and there are more lacerations
Tears of the uterus, cervix, and vagina
Uterine atony from prolonged labor
Early rupture of the membranes
Excessive blood loss
Tissue damage
Frequent rectal and vaginal examinations
Prolonged labor
Get Free Access Through Your Institution
Pop-up div successfully displayed.
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
- Getting pregnant
- Life as a parent
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How long will it take to conceive?
- When to take a pregnancy test
- Best positions to conceive
- Top signs of pregnancy
- How to use ovulation kits
- How age affects fertility
- When can I get pregnant after c-section?
- What fertile cervical mucus looks like
- Late period but no pregnancy
- Faint line on pregnancy test
- See all in Getting Pregnant
- How big is my baby?
- Due Date Calculator
- Painful baby movements
- Symptoms you should never ignore
- Hospital bag packing checklist
- How your baby's developing
- Signs of labour
- How to tell baby position by kicks
- Baby movements: boy or girl?
- How to count pregnancy months & weeks
- Nuchal Translucency (NT) scan
- Baby Weight Chart
- See all in Pregnancy
- Baby Name Finder
- Modern Indian Baby Names
- Most Popular Names in India
- Baby Names inspired by the Quran
- Baby Names inspired by Lord Shiva
- Sanskrit Baby Names
- See all in Baby Names
- Your baby week by week
- Baby milestones by month
- Baby Rashes
- Baby skin colour
- Worms in babies and toddlers
- Sleep training methods
- Baby teething remedies
- How to do steaming for a baby
- See all in Baby
- Your toddler month by month
- How much water should toddlers drink?
- When your toddler gets frustrated
- Vegetarian meals for toddlers
- When your toddler won't eat
- Potty training
- Help your toddler sleep
- Bottle to cup
- Games & activities
- What to feed a sick toddler
- See all in Toddler
- गर्भवती होने के लिए संभोग
- प्रेगनेंसी टेस्ट में हल्की रेखा का मतलब
- गर्भावस्था के लक्षण
- गर्भावस्था में खून के धब्बे (ब्लीडिंग)
- गर्भावस्था में शिशु की हलचल
- प्रसव पीड़ा (लेबर पेन) के लक्षण
- शिशु के नक्षत्र पर आधारित नाम
- शिशु को कितनी मात्रा में फॉर्मूला दूध देना है?
- बच्चे के पेट में कीड़े: लक्षण व इलाज
- हिंदी अनुभाग देखें
- Postnatal symptoms to watch out for
- Pain and stitches after delivery
- Postnatal massage
- Postnatal diet
- Post-delivery confinement
- See all in Life as a parent
- Best Maternity Bras
- 9 Breastfeeding Pillows You'll Love!
- Best Strollers for You and Your Baby
- Best Baby Carriers
- 10 Best Baby High Chairs
- Best Baby Walking Toys
- See all in Baby Products
- Astrology names
- Goddess Lakshmi names
- Baby names by date of birth
- Conjunctivitis
- Combination baby names
- Goddess Durga names
- Sikh baby names
- Bengali baby names
- Eclipses and pregnancy
- Name numerology
- Lord Vishnu names
- What to feed baby with a fever
- Traditional Indian names
- Gestational age vs fetal age
- South Indian baby names
- Mythological baby names
- Pregnancy food chart
- Names that rhyme
- Goddess Saraswati names
- Are air conditioners safe for babies?
- Annaprashan rice ceremony
- Nature names
- Godh bharai: baby shower
- Sesame seeds in pregnancy
What does it mean if my baby is in a transverse position?

In a transverse position, also known as a transverse lie, your baby lies horizontally (sideways) across your uterus, rather than the typical head-down position. Your baby's head is on one side of your body, and his feet on the other side.

Your baby may be facing up or down, and may be positioned differently, such as:
- Facing up towards your head, with his back towards the birth canal.
- Facing down towards your feet, with his hands and stomach towards the birth canal.
- One shoulder pointing toward the birth canal.
A transverse lie a common position for your baby to take in early pregnancy. But, most babies will get themselves into a head-down position by the end of the final trimester, if not before.
What causes a transverse lie position in pregnancy?
Your baby is more likely to end up in the transverse lie position in late pregnancy, if:
- you have too much amniotic fluid in your womb (polyhydramnios)
- you’ve had multiple pregnancies
- you have any abnormalities or malformations of the uterus
- you have a low-lying placenta (placenta praevia)
- you have fibroids or ovarian cysts
Sometimes a cause cannot be found, and it's just one of those things. A transverse lie can occasionally be a sign of a problem with the baby. If your baby is transverse, your ultrasound doctor will take a closer look to check that all is well.
When and how is a transverse lie position diagnosed?
Your doctor will check your baby’s position in your final trimester, at around 36 weeks . She may suspect your baby is transverse if she can’t feel his head or bottom in your pelvis when she feels your bump. If this is the case, you'll need an ultrasound scan to check how your baby is lying. The later in your pregnancy that transverse lie is diagnosed, the more likely it is that your baby will stay in this position until birth. This is rare, though, and approximately about one in 300 babies remain in a transverse lie by the time of birth.
Can you get a transverse baby to turn?
After 36 weeks, if your baby is transverse and your condition allows, some doctors may consider carrying out a procedure known as an external cephalic version (ECV). This is when a doctor places firm but gentle pressure on your tummy to encourage your baby to turn. If you decide to go ahead with an ECV, it's important that it's done by an experienced doctor in a hospital. If the ECV is successful, and your baby moves to a head-down position, you can wait for labour to start . A head-down (cephalic presentation), with the back of a baby's head towards the front of your tummy (anterior position), is the most common and best position for a normal delivery .
Is a normal delivery possible if my baby is in a transverse position?
If your baby stays in a transverse lie until the end of your pregnancy, a normal vaginal delivery will not be possible. This is because a baby in the transverse position won't be able to go through the birth canal as his back, shoulders, or arms may be poised to enter first. Attempting a vaginal birth can be dangerous for both the mother and her baby. Your doctor will recommend you have a planned c-section as that would be the safest delivery option. Sometimes your medical team won’t know your baby is transverse until your labour. Your doctor may only find out when she feels the fore waters (part of the amniotic sac) or your baby’s arm or leg, rather than your baby's head, during an internal check-up . If this is the case, your doctor will recommend an emergency cesarean.
Can transverse lie cause an umbilical cord prolapse?
There is a higher chance of umbilical cord prolapse if your baby is in a transverse, although the risk is still very small.
What is the difference between a transverse and oblique position?
Oblique lie position means that your baby is lying diagonally in the uterus, with his rump facing the side of your body at an angle. It happens in rare cases.

Like the transverse lie, this position is more common earlier in pregnancy, and it's likely your doctor will intervene if your baby is still in the oblique lie at the end of your third trimester.
- Fetal development
- Baby movements
- Pregnancy complications
Was this article helpful?
How often should I feel my baby move?

Can I know my baby's position in the womb by their movements?

I'm overweight. Will it take longer for me to feel my baby kick?

How can I encourage my baby to stop kicking my ribs?

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organisations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Ahmad A et al. 2014. Association of fetal position at onset of labor and mode of delivery: A prospective cohort study. Ultrasound in obstetrics & gynecology 43(2):176-182. www.ncbi.nlm.nih.gov Opens a new window Hankins GD. 1990. Transverse lie. American Journal of Perinatology 7(1):66-70. www.ncbi.nlm.nih.gov Opens a new window March of Dimes. 2016. Umbilical cord conditions. www.marchofdimes.org Opens a new window Medline Plus. 2020. Your baby in the birth canal . U.S. National Library of Medicine. www.medlineplus.gov Opens a new window RCOG. 2017. External Cephalic Version and Reducing the Incidence of Term Breech Presentation. Royal College of Obstetricians and Gynaecologists, Green-top guideline, 20a. www.rcog.org.uk Opens a new window

Where to go next


COMMENTS
प्लेसेंटा क्या है. प्लेसेंटा गर्भ में बच्चे को ऑक्सीजन और आवश्यक पोषक तत्व प्रदान करता है। एंटीरियर प्लेसेंटा, प्लेसेंटा की एक स्थिति है जिसमें यह ...
Cephalic Position का क्या मतलब होता है? Cephalic Presentation Of Baby //Cephalic Presentation HindiAbout this video:What is Cephalic Position ?What is its si...
In obstetrics, a cephalic presentation or head presentation or head-first presentation is a situation at childbirth where the fetus is in a longitudinal lie and the head enters the pelvis first; the most common form of cephalic presentation is the vertex presentation, where the occiput is the leading part (the part that first enters the birth canal). All other presentations are abnormal ...
Benefits of Cephalic Presentation in Pregnancy. Cephalic presentation is one of the most ideal birth positions, and has the following benefits: It is the safest way to give birth as your baby's position is head-down and prevents the risk of any injuries. It can help your baby move through the delivery canal as safely and easily as possible.
Cephalic presentation क्या है? Cephalic presentation in ultrasound! Cephalic position means in HindiJoin this channel to get access to perks:https://www ...
The cephalic position is when a fetus is head down when it is ready to enter the birth canal. This is one of a few variations of how a fetus can rest in the womb and is considered the ideal one for labor and delivery. About 96% of babies are born in the cephalic position. Most settle into it between the 32nd and 36th weeks of pregnancy.
Cephalic presentation from initial... a. Ajnan. Posted 27-08-12. Hi all, Iam now 33 weeks preg, my scan report yesterday shows normal fetal development with cephalic presentation, but all my scans taken so far shows baby position cephalic... which means baby has not turned throughout but in same position....however movements i feel are good ...
Cephalic Occiput Posterior. In this position, the baby is in the head-down position but the baby's face is turned towards the mother's belly. This type of cephalic presentation is not the best position for delivery as the baby's head could get stuck owing to its wide position. Almost 5% of the babies in cephalic presentation settle into ...
In cephalic presentation, the intra-uterine fetal position is of universal flexion, which is carried by the child to the immediate post-partum period. The hips and knees are flexed. The lower legs are internally rotated. The feet are further internally rotated with respect to the lower legs. At times there is an external rotational contracture ...
Cephalic presentation. Almost all (95-97%) babies are delivered by cephalic presentation, where they are head-down with legs and feet at the top of the uterus. Most babies move into the head-down position by the third trimester. Cephalic presentation is further broken down by the position of the head; in the vast majority of cephalic deliveries ...
Head Down, Facing Down (Cephalic Presentation) This is the most common position for babies in-utero. In the cephalic presentation, the baby is head down, chin tucked to chest, facing their mother's back. This position typically allows for the smoothest delivery, as baby's head can easily move down the birth canal and under the pubic bone ...
Posterior placenta is the best position: It is believed that this is the most ideal position as it allows the baby to move into the correct position. Posterior placenta impacts chances of normal delivery: "You can have a vaginal birth as long as the placenta does not cover the cervix, as this prevents the baby from descending down the birth ...
On the other hand, there are marked differences with higher proportions for boys in cases with anomalous cephalic presentation (52.7 % boys, 47.3 % girls) and transverse presentation (53.8 % boys, 46.2 % girls) and there are significantly more girls with breech presentations at birth (45.6 % boys, 54.4 % girls) (p < 0.001).
The fetus enters the pelvis in a cephalic presentation approximately 95 percent to 96 percent of the time. In these cephalic presentations, the occiput may be in the persistent transverse or posterior positions. In about 3 percent to 4 percent of pregnancies, there is a breech-presenting fetus (see Chapter 25).
What is cephalic presentation? Flexi Says: Cephalic presentation is the position of the baby's head pointing downwards, facing your back. Discuss further with Flexi. Ask your own question!
An umbilical cord prolapse is when the umbilical cord slips into the vagina ahead of the baby during labour and delivery. Usually the cord delivers after the baby, along with the placenta. If the cord gets pressed on by your baby's weight or your position, it could cut off his oxygen supply. It's considered a medical emergency.
90,000 U.S. doctors in 147 specialties are here to answer your questions or offer you advice, prescriptions, and more. can you tell me about fetus cephalic presentation and placenta anterior low lying will i deliver before my due date?: All normal: Fetus in the cephalic presentation just means the baby is.