Essay on Diabetes for Students and Children
500+ words essay on diabetes.
Diabetes is a very common disease in the world. But people may never realize, how did they get diabetes and what will happen to them and what will they go through. It may not be your problem but you have to show respect and care for the one who has diabetes. It can help them and also benefited you to know more about it and have a better understanding of it. Diabetes is a metabolic disorder which is identified by the high blood sugar level. Increased blood glucose level damages the vital organs as well as other organs of the human’s body causing other potential health ailments.


Types of Diabetes
Diabetes Mellitus can be described in two types:
Description of two types of Diabetes Mellitus are as follows
1) Type 1 Diabetes Mellitus is classified by a deficiency of insulin in the blood. The deficiency is caused by the loss of insulin-producing beta cells in the pancreas. This type of diabetes is found more commonly in children. An abnormally high or low blood sugar level is a characteristic of this type of Diabetes.
Most patients of type 1 diabetes require regular administration of insulin. Type 1 diabetes is also hereditary from your parents. You are most likely to have type 1 diabetes if any of your parents had it. Frequent urination, thirst, weight loss, and constant hunger are common symptoms of this.
2) Type 2 Diabetes Mellitus is characterized by the inefficiency of body tissues to effectively respond to insulin because of this it may be combined by insulin deficiency. Type 2 diabetes mellitus is the most common type of diabetes in people.
People with type 2 diabetes mellitus take medicines to improve the body’s responsiveness to insulin or to reduce the glucose produced by the liver. This type of diabetes mellitus is generally attributed to lifestyle factors like – obesity, low physical activity, irregular and unhealthy diet, excess consumption of sugar in the form of sweets, drinks, etc.
Get the huge list of more than 500 Essay Topics and Ideas
Causes of Diabetes
By the process of digestion, food that we eat is broken down into useful compounds. One of these compounds is glucose, usually referred to as blood sugar. The blood performs the job of carrying glucose to the cells of the body. But mere carrying the glucose to the cells by blood isn’t enough for the cells to absorb glucose.
This is the job of the Insulin hormone. Pancreas supply insulin in the human body. Insulin acts as a bridge for glucose to transit from blood to the body cells. The problem arises when the pancreas fails to produce enough insulin or the body cells for some reason do not receive the glucose. Both the cases result in the excess of glucose in the blood, which is referred to as Diabetes or Diabetes Mellitus.
Symptoms of Diabetes
Most common symptoms of diabetes are fatigue, irritation, stress, tiredness, frequent urination and headache including loss of strength and stamina, weight loss, increase in appetite, etc.
Levels of Diabetes
There are two types of blood sugar levels – fasting blood sugar level and postprandial blood sugar level. The fasting sugar level is the sugar level that we measure after fasting for at least eight hours generally after an overnight fast. Blood sugar level below 100 mg/dL before eating food is considered normal. Postprandial glucose level or PP level is the sugar level which we measure after two hours of eating.
The PP blood sugar level should be below 140 mg/dL, two hours after the meals. Though the maximum limit in both the cases is defined, the permissible levels may vary among individuals. The range of the sugar level varies with people. Different people have different sugar level such as some people may have normal fasting sugar level of 60 mg/dL while some may have a normal value of 90 mg/dL.
Effects of Diabetes
Diabetes causes severe health consequences and it also affects vital body organs. Excessive glucose in blood damages kidneys, blood vessels, skin resulting in various cardiovascular and skin diseases and other ailments. Diabetes damages the kidneys, resulting in the accumulation of impurities in the body.
It also damages the heart’s blood vessels increasing the possibility of a heart attack. Apart from damaging vital organs, diabetes may also cause various skin infections and the infection in other parts of the body. The prime cause of all type of infections is the decreased immunity of body cells due to their inability to absorb glucose.
Diabetes is a serious life-threatening disease and must be constantly monitored and effectively subdued with proper medication and by adapting to a healthy lifestyle. By following a healthy lifestyle, regular checkups, and proper medication we can observe a healthy and long life.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Entire Site
- Research & Funding
- Health Information
- About NIDDK
- Diabetes Overview
What Is Diabetes?
- Español
Diabetes is a disease that occurs when your blood glucose, also called blood sugar, is too high. Glucose is your body’s main source of energy. Your body can make glucose, but glucose also comes from the food you eat.
Insulin is a hormone made by the pancreas that helps glucose get into your cells to be used for energy. If you have diabetes, your body doesn’t make enough—or any—insulin, or doesn’t use insulin properly. Glucose then stays in your blood and doesn’t reach your cells.
Diabetes raises the risk for damage to the eyes, kidneys, nerves, and heart. Diabetes is also linked to some types of cancer. Taking steps to prevent or manage diabetes may lower your risk of developing diabetes health problems.

What are the different types of diabetes?
The most common types of diabetes are type 1, type 2, and gestational diabetes.
Type 1 diabetes
If you have type 1 diabetes , your body makes little or no insulin. Your immune system attacks and destroys the cells in your pancreas that make insulin. Type 1 diabetes is usually diagnosed in children and young adults, although it can appear at any age. People with type 1 diabetes need to take insulin every day to stay alive.
Type 2 diabetes
If you have type 2 diabetes , the cells in your body don’t use insulin properly. The pancreas may be making insulin but is not making enough insulin to keep your blood glucose level in the normal range. Type 2 diabetes is the most common type of diabetes. You are more likely to develop type 2 diabetes if you have risk factors , such as overweight or obesity , and a family history of the disease. You can develop type 2 diabetes at any age, even during childhood.
You can help delay or prevent type 2 diabetes by knowing the risk factors and taking steps toward a healthier lifestyle, such as losing weight or preventing weight gain.
Gestational diabetes
Gestational diabetes is a type of diabetes that develops during pregnancy. Most of the time, this type of diabetes goes away after the baby is born. However, if you’ve had gestational diabetes, you have a higher chance of developing type 2 diabetes later in life. Sometimes diabetes diagnosed during pregnancy is type 2 diabetes.
Prediabetes
People with prediabetes have blood glucose levels that are higher than normal but not high enough to be diagnosed with type 2 diabetes. If you have prediabetes, you have a higher risk of developing type 2 diabetes in the future. You also have a higher risk for heart disease than people with normal glucose levels.
Other types of diabetes
A less common type of diabetes, called monogenic diabetes , is caused by a change in a single gene . Diabetes can also come from having surgery to remove the pancreas, or from damage to the pancreas due to conditions such as cystic fibrosis or pancreatitis .
How common are diabetes and prediabetes?
More than 133 million Americans have diabetes or prediabetes. 1
As of 2019, 37.3 million people—or 11.3% of the U.S. population—had diabetes. 1 More than 1 in 4 people over the age of 65 had diabetes. Nearly 1 in 4 adults with diabetes didn’t know they had the disease. 2
About 90% to 95% of diabetes cases are type 2 diabetes. 3
In 2019, 96 million adults—38% of U.S. adults—had prediabetes. 4
What other health problems can people with diabetes develop?
Over time, high blood glucose can damage your heart , kidneys , feet , and eyes . If you have diabetes, you can take steps to lower your chances of developing diabetes health problems by taking steps to improve your health and learning how to manage the disease . Managing your blood glucose, blood pressure, and cholesterol levels can help prevent future health problems.

This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
NIDDK would like to thank: Daniel Bessesen, M.D., University of Colorado; Domenico Accili, M.D., Columbia University
Home — Essay Samples — Nursing & Health — Other Diseases & Conditions — Diabetes
Essays About Diabetes
The burden of diabetes, the dangers of diabetes and the proper management of the disease, made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
Diabetes: Type 1 and Type 2
Overview of diabetes mellitus, research on diabetes and its effects on people, a research on the management of type 2 diabetes mellitus, let us write you an essay from scratch.
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Types, Causes and Treatment of Diabetes
Diabetes mellitus: definition, types, effects and causes, results of diabetes mellitus type 2 progressing, the types of diabetes, get a personalized essay in under 3 hours.
Expert-written essays crafted with your exact needs in mind
The Type 1 and Type 2 Diabetes
Overview of diabetes mellitus: symptoms, types and treatment, what is gestational diabetes, critically analyse the effect of physical activity on type 2 diabetes, home remedies for diabetes, a study on diabetes, the risks of amputation, and life after amputation, the need for special diabetes program in america, insulin therapy in type 2 diabetes mellitus, medications for blood glucose and pressure control during diabetes, diabetes in children: definition of diabetes burnout and how peer pressure contributes to diabetes, recommendations to delay the onset of diabetes and control of diabetes, the np influence and diabetes, the types of diabetes mellitus, review of the consequences of diabetes mellitus, current methods of treating diabetic foot ulcer, the role and responsibilities of a registered nurse when treating diabetic patients, methods of improvement in the awareness & treatment of insulin abuse, diabetes: how to eat healthy and maintain good levels, behavioral interventions to improve glycemic control in african americans with t2dm, diabetes mellitus: analysis of the types, strategies and treatments.
Diabetes mellitus, commonly known as diabetes, is a group of metabolic disorders characterized by a high blood sugar level (hyperglycemia) over a prolonged period of time.
Symptoms often include frequent urination, increased thirst and increased appetite.
There are three main types of diabetes mellitus: Type 1 diabetes, Type 2 diabetes, and Gestational diabetes.
Family history, obesity, lack of exercise, genetics, air pollution, etc.
More than 37 million people in the United States have diabetes, and 1 in 5 of them don’t know they have it. Diabetes is the 7th leading cause of death in the United States. In the last 20 years, the number of adults diagnosed with diabetes has more than doubled as the American population has aged and become more overweight or obese.
Relevant topics
- Drug Addiction
- Healthy Food
- Teenage Pregnancy
- Stress Management
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
The Paradox of How We Treat Diabetes

Understanding diabetes today requires holding two conflicting realities in your head simultaneously.
First, diabetes therapy has been revolutionized by a world of new drugs that have become available since the turn of the century—most notably, drugs of the same class as Wegovy and Ozempic that began their existence as diabetes medications and are now hailed as wonder drugs for treating obesity. These drugs do the best job yet of controlling blood sugar and, of course, body weight, which is critical for those Type 2 diabetes, the common form of the disease that constitutes over 90 percent of cases and is associated with age and obesity. For type 1 diabetes, the acute condition that typically strikes in childhood and adolescence, new devices—continuous blood sugar monitors and automated insulin delivery systems—make blood sugar control easier than ever. Still more advanced devices and better drugs are in the pipeline.
But then there’s the flip-side. It’s why the pharmaceutical industry has invested so heavily in new therapies: Once a relatively rare condition, diabetes is now so common that drugstores dedicate entire aisles to it and television commercials for diabetic medications are common fare. In 1960, when the first concerted federal surveys were quantifying prevalence, two million Americans were living with a diabetes diagnosis. Today that number is 30 million; almost nine million more have diabetes but don’t yet know it. Each year, 1.4 million new cases are diagnosed and at ever younger ages.
Diabetes puts all of these individuals at increased risk of heart disease, strokes, cancer, blindness, kidney failure, nerve damage, gangrene, and lower limb amputation. It increases cognitive impairment and dementia risk as patients age. Living with diabetes still comes with a decrease in life expectancy of six years .
For those with Type 1 diabetes, despite the remarkable new drugs and devices, blood sugar control is seemingly getting worse, on average, not better. As of 2018, fewer than one in five individuals diagnosed with Type 1 diabetes were achieving even the relatively generous blood-sugar goals set by the American Diabetes Association (ADA); this was a smaller proportion than a decade earlier.
More From TIME
Despite the remarkable advances in therapy, both Type 1 and Type 2 diabetes are still considered progressive chronic diseases, meaning the patient’s condition is expected inevitably to deteriorate as they live with the disease. The greatest challenge to better therapy, as one recent analysis suggested , is the hesitation of physicians to continue prescribing more or newer drugs and increasing dosages as the diseases progress.
All of this comes with a staggering financial burden. In November, the ADA estimated that the total annual cost of diabetes in the U.S. is over $400 billion; over $300 billion is direct medical costs. This was up $80 billion from 2017 when an editorial commenting on a similar accounting characterized these costs as the “elephant in the room” of the diabetes epidemic. Patients with diabetes are likely to spend over $12,000 a year just for medical care, almost three times that of healthy individuals of equivalent age. It does not help that the drugs themselves—whether insulin or Ozempic and its ilk —are expensive, costing many thousands of dollars a year. One in every four health care dollars spent in America goes to treating diabetic patients.
And the U.S. is by no means unique. The World Health Organization estimates that diabetes prevalence worldwide increased four-fold between 1980 and 2014, from 108 million to over 400 million, with the greatest rise coming, paradoxically, in the poorest countries. In 2016, Margaret Chan, then WHO director general, described the situation as a “ slow-motion disaster” and predicted with near absolute certainty that these numbers would only get worse. They have.
So how do we reconcile these conflicting realities: Unprecedented advances in medical therapies for an out-of-control disease epidemic in which patients, at least in general, are doing poorly and can expect to do worse as time goes on? Confronted with such a dismal state of affairs shouldn’t we be asking how we got to this point? Were mistakes made in how we think about this disease? Were questionable assumptions treated as facts, and could those assumptions be wrong?
Asking the Right Questions
These are the kinds of questions you would hope health organizations worldwide would be asking, but surprisingly they have no mechanisms or protocols to do so. Diabetes associations like the ADA will regularly convene expert panels to address revisions in the latest standard of care guidelines to accommodate the latest research, but not whether the guiding principles underlying those guidelines should be rethought entirely. Independent investigators are not recruited to analyze and to provide an unbiased assessment of where progress might have gone off the rails. That job instead has been left to physicians in their clinics, those confronted with ever more diabetic patients and willing to take the risk of thinking independently, and to investigative journalists like myself, whose obligation when confronted with such conflicting realities is to ask just these kinds of questions.
Among the revolutions that changed medical practice over the past half century, one in particular is very relevant here. Beginning in the 1970s, health-care analysts began to confront quite how little physicians really knew about the risks and benefits of what they were doing for their patients. Not only had clinical trials demonstrated that some standard medical practices resulted in far more harm than good—the surgical procedure known as a radical mastectomy, most infamously, for breast cancer—but researchers were documenting wide variations in medical practices from physician to physician, hospital to hospital and state to state. This, in turn, resulted in a wide variation of benefits, harms and costs to the patients, depending on which physicians they might visit, and so which treatments they might get.
Read More: Should We End Obesity?
The revolution that followed became known as the Evidence-Based Medicine (EBM) movement, founded on the principle that medical interventions should be rigorously tested in clinical trials— double-blind, randomized, placebo-controlled—before they be used or prescribed. This would be necessary whenever physicians were faced with a choice between multiple options, and whenever the harms of an intervention might outweigh the benefits. David Sackett of McMaster University, a founder of the movement, would describe the EBM process as beginning with the fact that half of what aspiring doctors learn in medical school is “dead wrong,” and then trying to establish thoughtfully and critically which half that is. David Eddy of Duke University, another EBM pioneer, later described his motivation and that of his colleagues as the revelation that “medical decision making was not built on a bedrock of evidence or formal analysis, but was standing on Jell-O.”
It would be nice to think that this situation has been widely resolved by evidence-based guidelines, but that’s not the case. Journalists or physicians looking for the evidence base in decision making about diabetes therapies, will likely find themselves, as I did, with the same revelation. Clearly it, too, was standing on Jello-O in the 1970s, but the problem neither began nor ended there. A remarkable history emerges, with three clear observations.
First, we’ve been here before. We have had miracle drugs for diabetes. Most notably, the hormone insulin itself, when University of Toronto researchers led by Frederick Banting and Charles Best purified it and put it to use in 1922 treating patients with severe cases of diabetes. We then had better insulins, slower-acting and longer-lasting, and then, in the post-World War 2 years, drugs (oral hypoglycemic agents) that could lower blood sugar without having to be injected, as insulin did. We have had revolutionary advances in diabetes technology, beginning in the 1970s with devices that allowed patients to monitor their own blood sugar, and then insulin pumps that automated the process of insulin therapy. All contributed to easing the day-to-day burden of diabetes. None had any influence in controlling the epidemic, nor did they eradicate or meaningfully reduce the long-term complications of the disease. Put simply: diabetes plus drug therapy and devices, even the best drug therapy and devices, does not equate to health.
Secondly, diabetes researchers have not been averse to testing their fundamental assumptions. They‘ve done so in ever more ambitious clinical trials. But a disconcerting proportion of those trials failed to confirm the assumptions, despite the fact that it was these assumptions that constituted the rationale for therapeutic approaches. The $200 million Look AHEAD Trial, for example, tested a foundational belief in the field: that weight loss in those with Type 2 diabetes would lengthen lives. The trial was ended for “futility” in 2012 . ”We have to have an adult conversation about this,” as David Nathan, a Harvard diabetes specialist, said to The New York Times . The 10,000-patient ACCORD trial had also been ended prematurely just four years earlier. “Halted After Deaths,” in the words of The New York Times headline. “Medical experts were stunned,” the 2008 article said. ACCORD was one of three trials testing the assumption that intensive blood sugar control by medications would reduce the macrovascular complications of Type 2 diabetes—particularly heart disease—and premature death. All three trials failed to confirm it.
Third, the remarkable aspect of all these trials is that they all assumed an approach to dietary therapy that itself had never been tested. This is the “standing on Jell-O” problem. For well over a century, diabetes textbooks and chapters in medical texts invariably included some variation on the statement that diet is the cornerstone of treatment. The most recent guidelines from the ADA refer to dieting as “medical nutrition therapy” (MNT) and say MNT is “integral” to therapy.
But what constitutes MNT—the dietary advice given—has been determined not by any meaningful research comparing different dietary approaches. Rather it has been assumed that individuals with diabetes should eat the same “healthful eating pattern” that health organizations recommend for all of us—“non-starchy vegetables, fruits, legumes, dairy, lean sources of protein… nuts, seeds, and whole grains”—albeit with the expectation, if weight control is necessary, that they should eat fewer calories.
Read More: Are Weight Loss Drugs From Compounding Pharmacies Safe?
Controlling the symptoms and complications of the disease is left to insulin and the pharmacopeia of drugs that work to maintain blood sugar levels near enough normal that the specter of diabetic complications may be reduced as well. Diabetes associations have assumed that this approach is easiest on the patients, allowing them to balance the burden of insulin injections or multi-drug therapy, against the joy of eating as their non-diabetic friends and family do. But this assumption has never been tested to see if it is true, nor whether a better approach exists that might truly minimize the disease burden of diabetes, extend lives and make the trade-off of restrictive eating vs. health worthwhile.
History of Diet and Diabetes
This is where understanding the history of the diet-diabetes relationship can be vitally important. What has been known for certain about diabetes since the 19 th century is that it is characterized by the inability to safely metabolize the carbohydrates in our diet. This observation led to two divergent approaches/philosophies to dietary therapy. Beginning in 1797, when a British physician named John Rollo wrote about curing a diabetic patient using a diet of fatty (rancid) meat and green vegetables, through the early 1900s, diabetes therapy was based on the assumption that since individuals with diabetes could not safely metabolize the sugary and starchy foods in their diet, they should abstain from eating them. In this pre-insulin era, the only meaningful advice physicians could give their patients was dietary, variations on Rollo’s approach: sugars, grains, starches, even legumes were prohibited because they are carbohydrate-rich: meats, ideally as fatty as possible, butter and eggs, along with green leafy vegetables (boiled three times to remove the digestible carbohydrates) could be eaten to satiety.
Throughout Europe and America, this was known was “the animal diet,” endorsed by virtually every major diabetes specialist of the 19th Century. Physicians believed that the more calories their diabetic patients consumed, and ideally the more fat (because protein is composed of amino acids, some of which the liver converts to carbohydrates), the healthier they would be. “Patients were always urged to take more fat,” is how this was described in 1930 by the Harvard physician Elliot Joslin, who was then, far and away, the most influential diabetes authority worldwide. “At one time my patients put fat in their soup, their coffee and matched their eggs with portions of fat of equal size. The carbohydrate was kept extraordinarily low….”
This thinking only changed in the years before World War I, when Joslin embraced and disseminated the idea promoted by a Harvard colleague, Frederick Allen, that diabetic patients, still without insulin, were best served if they were semi-starved—avoiding carbohydrates and fat. In short, patients suffering from a disease in which one characteristic symptom is ravenous hunger would be treated by making them go even hungrier than otherwise. The approach was unsurprisingly controversial. Joslin and others, though, came to believe they could keep their young Type 1 patients alive longer with Allen’s starvation therapy, even while the high fat, animal-based diet seemed more than adequate for their older Type 2 patients. Allen’s starvation therapy was in turn challenged between 1920 and 1923, when University of Michigan physicians Louis Newburgh and Robert Marsh reported in a series of articles that it was simply unnecessary, that even young patients with severe diabetes could thrive on the high-fat, carbohydrate-abstention approach if properly administered. By then, though, it was too late.
Insulin therapy had arrived in the winter of 1922. It launched what medical historians would call a “therapeutic revolution,” as close as medicine had ever come, and maybe ever has, to a miracle. Patients, often children, on the brink of death, horribly emaciated by the disease and the starvation therapy, would recover their health in weeks, if not days on insulin therapy. They were resurrected, to use the biblical terminology, which physicians of the era often did.
Diabetes specialists realized that insulin therapy was not a cure of the disease, but it allowed their patients to metabolize carbohydrates and held the promise of allowing them to eat whatever and however they wanted. “Were I a diabetic patient,” wrote Frederick Banting in 1930, by then a Nobel Laureate. “I would go to the doctor and tell him what I was going to eat and relieve myself of the worry by demanding of him a proper dose of insulin.”
That thinking, for better or worse, has governed diabetes therapy ever since.
While diabetes specialists still had no conception of the long-term complications of living with diabetes—the damage to large and small blood vessels that results in heart disease, strokes, kidney disease, neuropathy, amputations, blindness, dementia—they would advocate for ever more liberal carbohydrate diets and ever higher insulin doses to cover them. Patients would be taught to count the carbohydrate content of each meal, but only so they could properly dose their insulin. Diets would be prescribed, and still are, to allow for the drugs to be used freely, not to minimize their use. Patients, in turn, were allowed to eat anything, which physicians assumed they would do anyway.

Whether the patients lived longer, healthier lives because of it, would never be tested. As diabetes specialists began to understand the burden of the disease they were treating, the wave of microvascular and macrovascular complications that set in after 10 or 20 years, they would rarely, if ever, ask the question, whether these complications were mitigated by their dietary approach or perhaps exacerbated by it. They would only test drug therapy.
In 1971, the American Diabetes Association institutionalized this philosophy with dietary guidelines that would commit the organization to this approach ever after: diabetic patients would be told to restrict dietary fat—by then thought to cause heart disease—rather than carbohydrates, the one macronutrient they could not metabolize safely without pharmaceutical help. “Medical Group, in a Major Change, Urges a Normal Carbohydrate Diet for Diabetics,” was the headline in The New York Times . By taking the ADA’s advice, diabetic patients would trade off blood sugar control for cholesterol, assuming this would prevent heart disease and lengthen their lives. While the guidelines explicitly acknowledged that the ADA authorities had no idea if this was the right thing to do, the advice would be given anyway.
Read More: Why You're Not Losing Weight
By 1986, the ADA was recommending diabetic patients get “ideally up to 55-60% of total calories” from carbohydrates, while researchers led by the Stanford endocrinologist Gerald Reaven had established that such a diet was almost assuredly doing more harm than good. That same year, the NIH held a “consensus conference” on diet and exercise in Type 2 diabetes. The assembled authorities concluded that, at best, the nature of a healthy diet for diabetes remained unknown. The conference chairman, Robert Silverman of the NIH, summed the state of affairs up this way: “High protein levels can be bad for the kidneys. High fat is bad for your heart. Now Reaven is saying not to eat high carbohydrates. We have to eat something.” And then he added, “Sometimes we wish it would go away, because nobody knows how to deal with it.”
The modern era of the diabetes-diet relationship began 25 years ago, with the awareness that the nation was in the midst of an obesity epidemic. Physicians, confronted with ever more obese and diabetic patients and the apparent failure of conventional advice—eat less, exercise more—suggested instead the only obvious options, the approaches suggested by popular diet books. Many of these— Dr. Atkins’ Diet Revolution, Protein Power, Sugar Busters —were touting modern incarnations of Rollo’s animal diet.
The Diet Trials
The result was a series of small, independent clinical trials, comparing, for the first time, the conflicting dietary philosophies of a century before. Is it better for patients with Type 2 diabetes, specifically, to avoid dietary fat and, if they’re gaining weight, restrict total calories (both carbohydrates and fat), or will they do better by avoiding carbohydrate-rich foods alone and perhaps entirely? The earliest trials focused on treating obesity, but many of the participants also struggled with Type 2 diabetes. In 2003, physicians at the Philadelphia VA Medical Center published the results from the first of such trials in the New England Journal of Medicine : patients with both obesity and diabetes counseled to eat as much food as they desired but to avoid carbohydrates, became both leaner and healthier than patients counseled to eat the low-fat, carbohydrate-rich, calorie-restricted diet prescribed by both the American Heart Association and ADA. The numerous trials since then have concluded much the same.
Among the profound assumptions about Type 2 diabetes that these trials have now challenged is that it is, indeed, a progressive, degenerative disorder. This may only be true in the context of the carbohydrate-rich diets that the ADA has recommended. In 2019, researchers led by the late Sarah Hallberg of the University of Indiana, working with a healthcare start-up called Virta Health, reported that more than half of the participants in their clinical trial were able to reverse their type 2 diabetes by eating what amounts to a 21 st century version of Rollo’s animal diet or the Newburgh and Marsh approach. They were able to discontinue their insulin therapy and all but the most benign of their diabetes medications (known as metformin) while achieving healthy blood sugar control. A third of these patients remained in remission, with no sign of their disease, for the five years , so far, that their progress has been tracked.
As for Type 1 diabetes, in 2018, a collaboration led by the Harvard endocrinologists Belinda Lennerz and David Ludwig reported on a survey of members of a Facebook Group called TypeOneGrit dedicated to using the dietary therapy promoted by Dr. Richard Bernstein in his book Dr. Bernstein’s Diabetes Solution . Bernstein’s approach requires patients to self-experiment until they find the diet that provides stable healthy levels of blood sugar with the smallest doses of insulin. Such a diet, invariably, is very low in carbohydrates with more fat than either the ADA or AHA would deem healthy. Both youth and adults in the Harvard survey maintained near-normal blood sugar with surprisingly few signs of the kind of complications—including very low blood sugar, known as hypoglycemia—that make the life of a patient with Type 1 diabetes so burdensome. The TypeOneGrit survey, Lennerz said , revealed “a finding that was thought to not exist. No one thought it possible that people with type one diabetes could have [blood sugar levels] in the healthy range.” This does not mean that such diets are benign. They may still have the potential to cause significant harm, as Lennerz and Ludwig and their colleagues made clear. That, again, has never been tested.
One consequence of the diabetes associations embracing and prescribing a dietary philosophy in 1971 that has only recently been tested is that we’re back to the kind of situation that led to the evidence based medicine movement to begin with: enormous variation in therapeutic options from physician to physician and clinic to clinic with potentially enormous variations in benefits, harms and costs.
Even the ADA advice itself varies from document to document and expert panel to expert panel. In 2019, for instance, the ADA published two consensus reports on lifestyle therapy for diabetes. The first was the association’s consensus report on the standard of car e for patients with diabetes. The authors were physicians; their report repeated the conventional dietary wisdom about eating “vegetables, fruits, legumes, whole grains….” It emphasized “healthful eating patterns”, with “less focus on specific nutrients,” and singled out Mediterranean diets, Dietary Approaches to Stop Hypertension (known as the DASH diet) and plant-based diets as examples that could be offered to patients. This ADA report still argued for the benefits of low-fat and so carbohydrate-rich diets, while suggesting that the “challenges with long-term sustainability” of carbohydrate-restricted eating plans made them of limited use.
Three months later, the ADA released a five-year update on nutrition therapy . This was authored by a 14-member committee of physicians, dietitians and nutritionists. Among the conclusions was that the diets recommended as examples of healthful eating patterns in the lifestyle management report—low-fat diets, Mediterranean diets, plant-based diets and the DASH diet—were supported by surprisingly little evidence. In the few short-term clinical trials that had been done, the results had been inconsistent. As for carbohydrate-restricted high fat eating patterns, they were now “among the most studied eating patterns for Type 2 diabetes,” and the only diets for which the results had been consistent. “Reducing overall carbohydrate intake for individuals with diabetes,” this ADA report stated, “has demonstrated the most evidence for improving glycemia [high blood sugar] and may be applied in a variety of eating patterns that meet individual needs and preferences.”
Physician awarenessof the potential benefits of carbohydrate-restriction for Type 2 diabetes, meanwhile, still often comes from their patients, not their professional organizations. In the United Kingdom, for instance, David Unwin, a senior partner in a medium-sized practice began suggesting carbohydrate-restricted high fat diets to his patients in 2011, after seeing the results in one such patient who chose to do it on her own and lost 50 pounds. When results of her blood tests came back, says Unwin, they both realized that she was no longer suffering from diabetes. Both the weight loss and the reversal of diabetes were unique in Unwin’s experience. After reading up on the burgeoning literature on carbohydrate restriction, Unwin began counseling his diabetic patients to follow a very-low-carbohydrate, high-fat eating pattern. In 2017, the UK’s National Health Service awarded Unwin its “innovator of the year” award for applying a 200-year-old approach to diabetes therapy, as Unwin says, that “was routine until 1923.” Unwin has now published two papers documenting the experience in his medical practice. As of last year, 20 percent of the clinic’s diabetic patients— 94 in total —had chosen to follow this restricted dietary approach and put their Type 2 diabetes into remission.
If the diabetes community is to solve the formidable problems confronting it, even as drug therapies get ever more sophisticated, it will have to accept that some of its fundamental preconceptions about diabetes and diet may indeed be wrong. As it does so, it will have to provide support for those living with diabetes who decide that what theyhave been doing is not working. Some patients, when confronted with the choice between following a restricted eating pattern that seemingly maximizes their health and wellbeing or eating whatever they want and treating the symptoms and complications with drug therapy, will prefer the former. For those who do, the informed guidance of their physicians and diabetes educators will be invaluable.
When I interviewed individuals living with Type 1 diabetes, among the most poignant comments I heard was from a nutrition consultant diagnosed in 1977 when she was eight years old. She told me that she finally had faith she could manage her blood sugar and live with her disease when she met a physician who said to her “What can I do to help you?” That’s what changed her life, as much as any technology or medical intervention. In the context of the dietary therapies we’re discussing, that requires practitioners who are themselves open-minded and willing to spend the necessary time and effort to truly understand an approach to controlling diabetes that is, by definition, unconventional and, in Type 1 diabetes, still lacking clinical trials that test (or testify to) its safety and efficacy. Easy as it is for physicians to continue believing that what they should be doing is what they have been doing, they do not serve their patients best by doing so.
Adapted from Gary Taubes' new book Rethinking Diabetes: What Science Reveals About Diet, Insulin and Successful Treatments
More Must-Reads from TIME
- The 100 Most Influential People in AI 2024
- Inside the Rise of Bitcoin-Powered Pools and Bathhouses
- How Nayib Bukele’s ‘Iron Fist’ Has Transformed El Salvador
- What Makes a Friendship Last Forever?
- Long COVID Looks Different in Kids
- Your Questions About Early Voting , Answered
- Column: Your Cynicism Isn’t Helping Anybody
- The 32 Most Anticipated Books of Fall 2024
Contact us at [email protected]
Diabetes - Free Essay Samples And Topic Ideas
Diabetes is a chronic disease characterized by high levels of sugar in the blood due to insulin production issues or the body’s response to insulin. Essays on diabetes could delve into the types of diabetes, its prevalence, management strategies, and the impact on individuals and communities. Discussions might also explore ongoing research and advancements in diabetes care. A substantial compilation of free essay instances related to Diabetes you can find in Papersowl database. You can use our samples for inspiration to write your own essay, research paper, or just to explore a new topic for yourself.
A Problem of Hispanics with Diabetes
Introduction The health care industry changes each and every year. Making America a very diverse nation and with diversity many issues present itself in today's society. One of the main issues that is affecting society is the prevalence of Type 2 Diabetes in Hispanics. The purpose of this paper is to provide cultural information and awareness of this issue with ways to assist in the prevention of Diabetes. Knowledge about diabetes is very important and sometimes there is not enough […]
Clinical Problem of Diabetes Type i and II
Abstract This capstone paper integrates the current clinical problem of diabetes type I and II in the hospitalized adult and youth patients with the associated QSEN nursing competency of patient centered care by addressing and exploring the following question: Among patients with Diabetes, how does diabetes self-management education programs (DSME) compared with no diabetes self-management education programs affect diabetic self-care/self-management? After an introduction of the problem and its significance to patient centered care, a review of current research literature that […]
King’s Theory and Nursing Process
My institution, Overlake Hospital has a multidisciplinary diabetes inpatient team that include, endocrinologists, diabetes specialist podiatrist, nurses, wound care specialist, dietitian and social workers. Often patients expressed their concern and fear over not being able to self-manage their condition. Lack of knowledge on how to treat, lack of understanding of proper food choices, exercise regimen and overwhelming burden of this chronic disease causes depression. Our interdisciplinary team focuses on care for each and every individual's complex need and educate, train […]
We will write an essay sample crafted to your needs.
General Characteristic of Type II Diabetes
Type 2 Diabetes Background about the disease- Type 2 Diabetes is a disorder caused by an imbalance of insulin. It is the more common form of diabetes, mostly seen in adults but now increasingly observed in young adults as well. Also known as non-insulin-dependent diabetes, this lifelong disease causes your blood glucose level to rise above the normal range. Pathophysiology and causes- Type 2 diabetes stems from several factors. It can develop when your body becomes resistant to insulin or […]
Keto Diet and Type Diabetes
Some people experience autoimmune diseases while others do not. Maybe you have tried to understand how changes in your diet might help an autoimmune disease. Or maybe you are worried that what you are eating is contributing to it? Perhaps you are someone that is suffering from type 1 diabetes and wonder how the ketogenic (referred to as “keto”) diet might help to ease some of the symptoms. We want to assist you in choosing fuel for your body that […]
Importance of Nursing Theories
Nursing theories are important tools for the designing, understanding, and application of diabetes patient education (Anderson, Funnell, & Hernandez, 2005). Imogene King is one of the nursing theorists who has made significant contributions to nursing. King's Conceptual Framework and Theory of Goal Attainment (TGA) is valuable in the care of diabetes patients and adherence to treatment. In my unit most commonly-used nursing theories include, King's theory of goal attainment to the care of the adult with diabetes mellitus. TGA theory […]
History and Types of Diabetes
The first sign of diabetes was discovered in 1500 B.C.E by the Egyptians. According to one study, ancient Indians were familiar with the condition and had even determined two types of the condition. They called it "honey urine" and tested for it by determining if the ants were drawn to the urine. The first mention of the word diabetes was by the Greeks. It means "to go through", it was named this because of its main symptom: the excessive passing […]
The Basic Problem of Diabetes
Uncontrolled levels of blood glucose are the basic problem in patients admitted to our unit. Many are related to lack of knowledge and self-care in diabetes management, sedentary lifestyle, and food habits. This reveals that when assessing a patient in the hospital, a nurse must consider all factors and design a care plan accordingly. Nurses need to be non-judgmental and assess what factors may limit patients' abilities to follow lifestyle recommendations. According to the American Diabetes Association (ADA), uncontrolled blood […]
My Work as a Nurse
I work at Overlake Hospital Medical Center on a Medical Surgical and Oncology Unit. As a bedside nurse, my job and responsibility not only centered around vigilant monitoring for physiological changes and immediate needs of patients but also centered around an emotional aspect of caring and advocating. Our 37-bed unit provides care for various medical-surgical conditions, chemotherapy infusion, blood transfusion, dialysis, oncology with hospice, and end of life care patients on a day to day basis. As a bedside nurse, […]
Diabetes and its Main Types
Diabetes is a disorder of the endocrine system, which messes with the metabolism of carbohydrates, fats, and proteins. The metabolism is compromised because of a lack of insulin, either from destruction of the beta cells, which secrete insulin, or because of insulin resistance. Insulin is secreted by beta cells and it is what enables the cells to use glucose. Type 1 diabetes was formerly called juvenile diabetes because mostly kids were diagnosed with it. It is now changed to be […]
Adverse Health Effect of Environmental Heavy Metals on Diabetes
ABSTRACT Type 2 diabetes (T2D) and its complications constitute a major public health problem for both developed and developing countries due to the high rate of morbidity and mortality associated with the disease. New evidence from both experimental and human studies has resulted in increased interest in analyzing the relationship between T2D and heavy metal exposures that are ubiquitous in the environment. Vellore district is a major leather- processing centre in Tamil Nadu, with an estimated 60,000 tannery workers. Tannery […]
Becoming an Endocrinology Nurse Practitioner
Since the introduction and continued implementation of the Affordable Care Act, millions of individuals now have access to health care who did not before. With this influx of patients in the health care system, there has been an increased demand for primary care providers in a health care environment already dealing with shortage, (Buppert, 2015)A large amount of this population includes patients battling diabetes and hypertension. These patients would benefit from a nurse practitioner specializing in these diseases such as […]
An Issue of Nutrition and Diabetes
The article I've reviewed is called, "Nutrition Therapy Recommendations for the Management of Adults with Diabetes". My decision to review this article is based upon interest in links with nutrition and chronic disease. A National Center for Health Statistics study (Table 18) identified eight of the top ten killers in America as chronic diseases. I've read multiple books that link the two and this article conducted a systematic review of 228 articles or studies. The article goes fairly in depth […]
How is Low Carbohydrate Diet Beneficial to Diabetes
Abstract: This essay is about the global status of diabetes, what is diabetes, how insulin works, why people easy to have diabetes, what is carbohydrate and why low carbohydrate diet beneficial to the diabetes. With the development of society, people's living standards have gradually improved. The choice of food is gradually becoming more and more, also it has brought us many diseases. Diabetes, as one of the top ten death diseases in the world, has attracted the attention of people […]
What should you Know about Diabetes
What is diabetes? Diabetes is when your blood sugars, or blood glucose, is to high. Your main source of energy is blood glucose, which comes from the food you eat. Your pancreas creates a hormone called insulin. Insulin helps all the glucose from the food you eat get into your body's cells and use it for energy. But in some cases, the body doesn't create enough insulin, sometimes the body doesn't make any insulin at all. If this is the […]
Diabetes: One of the Hardest Illness
Diabetes is a standout amongst the most widely recognized maladies that can prompt passing if not treated right. In any case there are particular sorts of this ailment which is Type 1,Type 2, and Gestational diabetes. Diabetes is an illness that happens when your blood glucose, additionally called glucose, is too high. Blood glucose is your fundamental wellspring of significance and begins from the sustenance you eat. Diabetes is the sort of ailment that goes with conspicuous signs with in […]
IDDM: Pathophysiology and Pre-hospital Management
Introduction Diabetes mellitus is a global problem facing various populations. As such, many victims tend to appreciate the underlying treatment prescribed by doctors to reduce its effects. There exist two categories of diabetes that includes types 1 and type 2 covered in film. The movie shows that type 1 diabetes is insulin-related and when the body cells are unable to absorb glucose in the presence of insulin to produce energy. Type 2 diabetes is non-dependent on insulin and can develop […]
Connection between Genetics and Diabetes
Each single person has a specific set of genes; however, these genetics are greatly influenced by their families. Genetics can also be affected via one's environmental surroundings, as well. These genetics are associated with most diseases, such as cancer, kidney diseases, and psychologic diseases. Diabetes is no different. Genetics are not the only causative factor in diabetes, but it can alert healthcare members to look for this disease due to predisposition. According to the American Diabetes Association (2018), "Type 1 […]
Diabetes Type One in the Pediatric Patient
Diabetes is a very complex disease that effects all the system of the body. Often people only think about blood sugar when the think of diabetes, nut this disease is so much more complicated than just controlling blood sugar. This is especially true in the pediatric population. These youngsters are not old enough or mature enough to understand this complex disease and rely on the parents to help them manage this disease (Perry, 2010). The pathophysiology of diabetes type one […]
Insulin-Dependent Diabetes Mellitus
Diabetes Mellitus 1, more specifically known as IDDM is a disorder concerning glucose homeostasis, which needs insulin therapy is generally seen in children. Diabetes is generally classified into 2 types IDDM (Insulin dependent diabetes mellitus) and the other NIDDM (Non-insulin dependent diabetes mellitus). Diabetes simply means an increase of glucose levels in the body as a result of the improper or no production of insulin from ones pancreatic ??-cells. The standard auto-immune response of type 1 diabetes is specific destruction […]
An Evolution of Diabetes
EVOLUTION Diabetes is a major public health problem with a rapid increase in prevalence globally. Twelve percent of all health care spending is related to diabetes. The diagnosis and treatment of diabetes has evolved extensively over the last century. Although there is still no cure for the disorder, diabetes is much more manageable due to advancement in medicine and technology. In the beginning of the 20th century, Edward Schafer concluded that the pancreas of diabetics was unable to produce insulin […]
Problem: Childhood Obesity in America
As you've probably heard, more children are becoming overweight today in America than ever before. Experts are calling this an "obesity epidemic." To first understand childhood obesity we must ask ourselves what is obesity? Obesity is a diet-related chronic disease involving excessive body fat that increases the risk of health problems. Many doctors have expressed obesity has an increasing problem in today's youth as obesity can lead to many health issues such as type 2 diabetes, high blood pressure, heart […]
Treatment of Diabetes in Adolescents
Abstract Background: Diabetes is a significant public health challenge facing the US and several other countries around the world. It is mostly perceived as a lifestyle disease, although type 1 diabetes can be viewed as a congenital autoimmune disorder. Diabetes is increasingly becoming a problem among young adolescents in America, with high prevalence and incidence rates. This study sought to establish the impact of treatment of adolescents for diabetes on their maturity process, demand for independence, parent-adolescent conflict, and their […]
What are the Main Causes and Treatments of Diabetes
Diabetes is a chronic disease that can cause complications and death if left untreated. It is one of the most common chronic diseases in the world and affects nearly half of the global population. According to Koye et al. (2018), it is also a leading cause of disability worldwide, affecting more than 300 million people globally. Diabetes is one of the most common diseases in the United States, with more than 100 million adults affected by type 2 diabetes and over 6.3 […]
Diabetes a Matter of the Heart
Diabetes. Cardiovascular disease (CVD). What do these two diagnoses have in common? Well, diabetes does impact the cardiovascular system, according to the 2018 research (REF). There is research showing that diabetes does impact existing CVD risk factors for example high-density lipoproteins. Research is demonstrating that by following a few rules to improve insulin-resistance, that in return it will reduce the cardiovascular risk factors (REF). Diabetes, a chronic disease that is managed today with oral anti hyperglycemic agents, exercise, and diet. […]
Importance of Speech about Diabetes
On 14th November this year on World Diabetes Day we witnessed an amazing talk by the keynote speaker Dr. Ronny Bell at the University of Florida. The title of the talk was 'Challenges and Opportunities in achieving diabetes health equity.' He spoke about important issues that often get lost and not given too much importance when we talk about diabetes. He mentioned that we all know about the complications, we all know about the emergencies, but what we often don't […]
The Stigma Surrounding Medical Cannabis
My understanding of diabetes.
For this essay I'll be covering the topic of diabetes. I've always found diabetes as an interesting topic; maybe because it's a huge problem for most people in the United States. you might be wonder what diabetes is, Diabetes is a disease in which the body response to the hormone insulin is impaired or not fully functional, resluting in complications with the metabolism. Having high glucose is also one of the main reasons people get diabetes. Having high glucose in […]
A Process of Teaching Diabetes Self-Management
Introduction You’ve been diagnosed with Type 2 Diabetes, now what? The idea and topic of diabetes can be overwhelming for anyone, from patient to provider. The content outlined in this paper reflects the need for a plan to implement and educate patients newly diagnosed with Type 2 Diabetes to help them be successful in managing their diabetes and not letting diabetes take control of their lives. If you think about the idea of diabetes singularly as a diagnosis you have […]
Celiac Disease in Type Diabetes Mellitus
Introduction Celiac disease and Type 1 Diabetes Mellitus are both chronic autoimmune diseases exhibiting a steadily increasing prevalence, both in co-occurrence and individually, in the population. The purpose of this review is to outline the literature and studies conducted on Celiac disease in Type 1 diabetes mellitus and the risk factors associated with autoimmune comorbidity. Dietary control is significant to both diseases and plays an essential role in the management of short- and long-term complications. This review will discuss the […]
Related topic
Additional example essays.
- A Research Paper on Alzheimer's Disease
- Tuberculosis research
- Benefits of Swimming
- Alzheimer's Disease Still Alice
- The Mental Health Stigma
- Psychiatric Nurse Practitioner
- Substance Abuse and Mental Illnesses
- Homeschooling vs Public School
- Socioautobiography Choices and Experiences Growing up
- Is Sexual Orientation Determined At Birth?
- Love for Childhood Innocence in The Catcher in the Rye
- What are ACEs (Adverse Childhood Experiences)?
Were you assigned an essay on diabetes that requires extensive research? Do you have to distinguish between Type 1 and Type 2 and the affected age groups? Perhaps, you need to elaborate on the reasons for this disease and its health implications.
If any of these scenarios seem familiar, stop worrying because we have the solution to all your writing concerns. PapersOwl abounds with free argumentative essays about diabetes written by experts in the medical field. Moreover, the platform offers help with framing your thesis statement for diabetes and the overall outline of your paper. Other tools available on the website include a plagiarism checker, conclusion and citation generators, and a title page maker.
Diabetes mellitus is a lifelong condition prevalent in children and adults. It is the sixth leading cause of death in the US, claiming over 178,000 lives annually. The disease is complex because the glucose level in the blood is abnormally high and endangers the functioning of other organs. Improper treatment and lack of insulin can lead to life-threatening outcomes; otherwise, diabetics can have a typical life.
Engaging essay topics can include the effects of uncontrolled diabetes, proper diet, ideal body mass, reducing the risk factors, and avoiding a sedentary lifestyle. However, ensure you check at least several free essay examples on diabetes before you write the introduction. You can also consult titles by eminent experts with years of experience to get inspired for your sample research paper on diabetes.
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers

Essay on Diabetes
Students are often asked to write an essay on Diabetes in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Diabetes
What is diabetes.
Diabetes is a chronic disease where the body can’t control blood sugar levels. This happens because the body either doesn’t make enough insulin or can’t use it properly.
Types of Diabetes
There are two main types: Type 1 and Type 2. Type 1 is when the body doesn’t produce insulin. Type 2 is when the body doesn’t use insulin well.
Managing Diabetes
Diabetes can be managed through a healthy diet, regular exercise, and medication. Regular check-ups are also important to monitor blood sugar levels.
The Impact of Diabetes
If not managed, diabetes can lead to serious health problems like heart disease, kidney disease, and vision loss.
250 Words Essay on Diabetes
Introduction.
Diabetes, a chronic metabolic disorder, is characterized by an increased level of glucose in the blood. It arises due to the body’s inability to produce or effectively utilize insulin, a hormone responsible for glucose regulation.
Etiology of Diabetes
Diabetes is classified into two major types: Type 1 and Type 2. Type 1 diabetes, an autoimmune disorder, is a result of the body’s immune system attacking insulin-producing cells in the pancreas. On the other hand, Type 2 diabetes, the more prevalent form, is primarily associated with insulin resistance and often linked to obesity and sedentary lifestyle.
Impact and Management
Diabetes can lead to severe complications like heart disease, kidney failure, and blindness if left unmanaged. Management involves lifestyle modifications, including a healthy diet, regular physical activity, and medication or insulin therapy as needed.
Prevention and Future Research
Prevention strategies for Type 2 diabetes involve promoting healthier lifestyles and early detection. For Type 1 diabetes, research is still ongoing to understand its triggers. Advances in technology and medicine, such as artificial pancreas systems and islet cell transplantation, show promise for future diabetes management.
Diabetes, a global health crisis, requires comprehensive understanding and management strategies. With ongoing research and advancements, the future holds potential for improved diabetes care and prevention.
500 Words Essay on Diabetes
Introduction to diabetes.
There are primarily two types of diabetes: Type 1 and Type 2. Type 1 diabetes is an autoimmune condition where the body’s immune system attacks the insulin-producing cells in the pancreas. This type is less common and usually develops early in life. Type 2 diabetes, on the other hand, is more prevalent and typically develops in adulthood. It occurs when the body becomes resistant to insulin or doesn’t produce enough to maintain a normal glucose level.
Risk Factors and Symptoms
Several factors increase the risk of developing diabetes, including genetics, obesity, lack of physical activity, and poor diet. Additionally, certain ethnic groups are at a higher risk.
Management and Treatment
While there is currently no cure for diabetes, it can be effectively managed with a combination of lifestyle changes and medication. Regular exercise, a balanced diet, and maintaining a healthy weight are crucial for managing both types of diabetes.
For Type 1 diabetes, insulin injections or use of an insulin pump are necessary. Type 2 diabetes can often be managed with lifestyle changes and oral medication, but insulin may be required as the disease progresses.
Complications and Prevention
Prevention strategies for Type 2 diabetes include regular physical activity, a healthy diet, maintaining a normal body weight, and avoiding tobacco use. Early detection through regular health screenings is also critical, as early treatment can prevent or delay the onset of complications.
Diabetes is a significant global health concern that requires concerted efforts for effective management and prevention. Understanding the disease, its risk factors, and the importance of early detection can go a long way in reducing the impact of this chronic condition. Through lifestyle changes and medical intervention, individuals with diabetes can lead healthy and fulfilling lives.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Diabetes Essays
Case study report: diabetes, development and analysis of an argument that seeks to solve a real-world problem, indigenous health: indigenous people are disproportionately affected by diabetes, prevalence and solutions of diabetes among african americans, economic implications on diabetes, a small pharmaceutical, diabetes in west virginia, diabetes: a comparative analysis of management strategies in the uk and india, diabetes-free maryland: empowering communities for optimal health, patient, family, or population health problem solution, final diabetic care coordination plan, relevance of the glycemic index and glycemic load for body weight, diabetes, and cardiovascular disease, social ecological model of health, diabetes: a review of literature and implications for nutrition practice, type 2 diabetes formative case study, essays on diabetes.
Diabetes is a significant issue, but communicating it is not always easy. The way you approach your essay on diabetes will have a direct effect on the way readers receive it — especially those who have diabetes. So, we encourage you to tackle the subject sensibly and take the opportunity to do something positive, such as spreading understanding or even speaking up about the ineptitudes of the healthcare system when it comes to supporting patients with diabetes.
Exploring diabetes in broad strokes can limit your analysis and perspective, which can affect your essay’s impact. Since diabetes is such a huge issue, you should strive to make a positive impact. So, choosing the focus of your essay is key. For example, you could provide a complete breakdown of diabetes and how it affects people’s lives.
On another note, consider delving into its influence on people’s way of life. Diabetes care presents an intriguing avenue for exploration, encompassing a wide array of facets such as treatment choices, affordability, accessibility, and beyond. The challenges faced by individuals living with diabetes are undeniably significant and warrant thoughtful discussion. One of the biggest struggles is access to affordable healthcare and treatment, which is a very important topic you could explore.
When writing an essay on diabetes, you should have a clear purpose. Whether promoting understanding, raising awareness, presenting prevention strategies, etc., make sure you add something valuable to the conversation and use relevant sources as a foundation. You can engage readers and make a difference by inspiring action. At the very least, you can help readers understand diabetes and have more empathy for people who live with it.
Diabetes is a very important topic because over 500 million people worldwide live with it. It affects every aspect of their lives but doesn’t keep them from fulfillment, success, and happiness. So, you should definitely consider including real stories from people with diabetes to offer more insight into the good and the bad, thus making a greater impact on readers.
If you need help in creating an outline for your paper, use essay examples on this page that may push you in the right direction and help you complete your assignment with excellence.
Popular Essay Topics
- American Dream
- Artificial Intelligence
- Black Lives Matter
- Bullying Essay
- Career Goals Essay
- Causes of the Civil War
- Child Abusing
- Civil Rights Movement
- Community Service
- Cultural Identity
- Cyber Bullying
- Death Penalty
- Depression Essay
- Domestic Violence
- Freedom of Speech
- Global Warming
- Gun Control
- Human Trafficking
- I Believe Essay
- Immigration
- Importance of Education
- Israel and Palestine Conflict
- Leadership Essay
- Legalizing Marijuanas
- Mental Health
- National Honor Society
- Police Brutality
- Pollution Essay
- Racism Essay
- Romeo and Juliet
- Same Sex Marriages
- Social Media
- The Great Gatsby
- The Yellow Wallpaper
- Time Management
- To Kill a Mockingbird
- Violent Video Games
- What Makes You Unique
- Why I Want to Be a Nurse
- Send us an e-mail
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Mol Sci

Pathophysiology of Type 2 Diabetes Mellitus
Unai galicia-garcia.
1 Fundación Biofisika Bizkaia, Barrio Sarriena s/n., 48940 Leioa (Bizkaia), Spain; [email protected] (U.G.-G.); se.oohay@aerralreisa (A.L.-S.)
2 Biofisika Institute (UPV/EHU, CSIC), Barrio Sarriena s/n., 48940 Leioa (Bizkaia), Spain; [email protected] (A.B.-V.); sue.uhe.elsaki@100irabejs (S.J.); se.uhe@clpambfo (H.O.)
Asier Benito-Vicente
3 Department of Biochemistry and Molecular Biology, Universidad del País Vasco UPV/EHU, Apdo. 644, 48080 Bilbao, Spain
Shifa Jebari
Asier larrea-sebal, haziq siddiqi.
4 Havard Medical School, 25 Shattuck St, Boston, MA 02115, USA; [email protected]
Kepa B. Uribe
5 Center for Cooperative Research in Biomaterials (CIC biomaGUNE), Basque Research and Technology Alliance (BRTA), Paseo de Miramon 182, 20014 Donostia San Sebastián, Spain; se.enugamoibcic@osollebk
Helena Ostolaza
César martín.
Type 2 Diabetes Mellitus (T2DM), one of the most common metabolic disorders, is caused by a combination of two primary factors: defective insulin secretion by pancreatic β-cells and the inability of insulin-sensitive tissues to respond appropriately to insulin. Because insulin release and activity are essential processes for glucose homeostasis, the molecular mechanisms involved in the synthesis and release of insulin, as well as in its detection are tightly regulated. Defects in any of the mechanisms involved in these processes can lead to a metabolic imbalance responsible for the development of the disease. This review analyzes the key aspects of T2DM, as well as the molecular mechanisms and pathways implicated in insulin metabolism leading to T2DM and insulin resistance. For that purpose, we summarize the data gathered up until now, focusing especially on insulin synthesis, insulin release, insulin sensing and on the downstream effects on individual insulin-sensitive organs. The review also covers the pathological conditions perpetuating T2DM such as nutritional factors, physical activity, gut dysbiosis and metabolic memory. Additionally, because T2DM is associated with accelerated atherosclerosis development, we review here some of the molecular mechanisms that link T2DM and insulin resistance (IR) as well as cardiovascular risk as one of the most important complications in T2DM.
1. Introduction
Type 2 Diabetes Mellitus (T2DM) is one of the most common metabolic disorders worldwide and its development is primarily caused by a combination of two main factors: defective insulin secretion by pancreatic β-cells and the inability of insulin-sensitive tissues to respond to insulin [ 1 ]. Insulin release and action have to precisely meet the metabolic demand; hence, the molecular mechanisms involved in the synthesis and release of insulin, as well as the insulin response in tissues must be tightly regulated. Therefore, defects in any of the mechanisms involved can lead to a metabolic imbalance that leads to the pathogenesis of T2DM.
This review analyses the key aspects of T2DM, as well as the molecular mechanisms and pathways implicated in insulin metabolism and associations between T2DM and cardiovascular pathophysiology. In this review, we describe the global trends of T2DM, the roles of major risk factors, in particular, obesity, lifestyle factors, genetic predispositions, gut dysbiosis, epigenetics and mitochondrial deregulation. We highlight physiological and molecular mechanisms leading to T2DM and its complications.

2. Type 2 Diabetes Mellitus: Background and Epidemiology
According to the World Health Organization (WHO) diabetes mellitus is a chronic, metabolic disease characterized by elevated levels of blood glucose, which leads over time to damage to the heart, vasculature, eyes, kidneys and nerves. Over 90% of diabetes mellitus cases are T2DM, a condition marked by deficient insulin secretion by pancreatic islet β-cells, tissue insulin resistance (IR) and an inadequate compensatory insulin secretory response [ 2 , 3 ]. Progression of the disease makes insulin secretion unable to maintain glucose homeostasis, producing hyperglycaemia. Patients with T2DM are mostly characterized by being obese or having a higher body fat percentage, distributed predominantly in the abdominal region. In this condition, adipose tissue promotes IR through various inflammatory mechanisms, including increased free fatty acid (FFA) release and adipokine deregulation. The main drivers of the T2DM epidemic are the global rise in obesity, sedentary lifestyles, high caloric diets and population aging, which have quadrupled the incidence and prevalence of T2DM [ 4 , 5 ].
The organs involved in T2DM development include the pancreas (β-cells and α-cells), liver, skeletal muscle, kidneys, brain, small intestine, and adipose tissue [ 6 ]. Evolving data suggest a role for adipokine dysregulation, inflammation, and abnormalities in gut microbiota, immune dysregulation, and inflammation have emerged as important pathophysiological factors [ 7 ].
Epidemiological data show alarming values that predict a worrisome projected future for T2DM. According to the International Diabetes Federation (IDF), in 2019, diabetes caused 4.2 million deaths; and 463 million adults aged between 20 and 79 years old were living with diabetes, a number that will likely rise up to 700 million by 2045. Diabetes was the underlying cause of at least 720 billion USD in health expenditure in 2019. Additionally, the true disease burden of T2DM is likely an underrepresentation as 1 in 3 diabetic people were underdiagnosed, equivalent to 232 million people. The greatest number of people suffering from diabetes are aged between 40 and 59 years old. Incidence and prevalence of T2DM vary according to geographical region, with more than 80% of patients living in low-to-middle-income countries, which poses additional challenges in effective treatment. Patients with T2DM have a 15% increased risk of all-cause mortality compared with people without diabetes with cardiovascular disease (CVD) as the greatest cause of morbidity and mortality associated with T2DM [ 8 ]. The association of diabetes with increased risk of coronary heart disease (hazard ratio [HR] 2.00; 95% CI 1.83–2.19), ischaemic stroke (HR 2.27; 1.95–2.65), and other vascular disease-related deaths (HR 1.73; 1.51–1.98) has been shown in a meta-analysis [ 9 ].
Epidemiology of T2DM is affected both by genetics and the environment. Genetic factors exert their effect following exposure to an environment characterized by sedentary behavior and high-calorie intake. Common glycaemic genetic variants for T2DM have been identified by genome-wide association studies, but these only account for 10% of total trait variance, suggesting that rare variants are important [ 10 ]. People of different ethnic origins may have different specific phenotypes that increase predisposition to clusters of CVD risk factors, including hypertension, insulin resistance, and dyslipidemia [ 11 ].
3. Risk Factors and Pathophysiology
T2DM risk factors include a complex combination of genetic, metabolic and environmental factors that interact with one another contributing to its prevalence. Although individual predisposition to T2DM due to non-modifiable risk factors (ethnicity and family history/genetic predisposition) has a strong genetic basis, evidence from epidemiological studies suggests that many cases of T2DM can be prevented by improving the main modifiable risk factors (obesity, low physical activity and an unhealthy diet) [ 12 , 13 ].
3.1. Ethnicity and Family History/Genetic Predisposition
Globally, the incidence and prevalence of T2DM are found to vary widely depending on ethnicity and geographical region with Japanese, Hispanics and Native Americans having the highest risks [ 14 , 15 , 16 ]. It has been shown higher incidence rates in Asians compared with a White American population [ 17 , 18 ], and white population in the UK, [ 19 ], where the highest risk is among the black population [ 20 ]. Whilst no clear reasons have been found, contributing factors such as modern lifestyle factors (which promote obesity), socioeconomic and direct genetic propensity or gene environmental interactions have been postulated.
Genetic predisposition plays an important part in the risk of developing T2DM. Over the past decade, several T2DM genome-wide association studies have shown the complex polygenic nature of T2DM in which most of these loci increase T2DM risk through primary effects on insulin secretion, and a minority act through reducing insulin action [ 21 , 22 ]. Dimas et al. grouped these variants on the basis of their potential intermediate mechanisms in T2DM pathophysiology, with four variants fitting a clear IR pattern; two reducing insulin secretion with fasting hyperglycemia; nine lowering insulin secretion with normal fasting glycemia; and one altering insulin processing [ 23 ]. According to these data, the genetic architecture of T2DM is highly polygenic, and additional association studies are needed to identify most T2DM loci [ 24 ]. Interactions between susceptibility loci and environmental factors could underlie the missing heritability of T2DM thus the impact of a given genetic variant can be modulated by the environmental factors (and vice versa) as evidenced by both observational studies and clinical trials [ 25 ].
3.2. Obesity, Low Physical Activity and Unhealthy Diet
Obesity (body-mass index [BMI]≥30 kg/m 2 ) is the strongest risk factor for T2DM [ 26 , 27 ] and is associated with metabolic abnormalities resulting in IR [ 28 ]. There exist an inverse linear relationship between BMI and the age at diagnosis of T2DM [ 29 ]. The exact mechanisms by which obesity induces T2DM and IR remain to be elucidated; however, numerous factors have shown a significant role in the development of this pathological process, which involves both cell-autonomous mechanisms and inter-organ communications.
A sedentary lifestyle is another risk factor for T2DM as shown by the Women’s Health Study and in the Kuipio Ischemic Heart Disease Risk Factor Study, which showed a reduction of 34% and 56% reduction of developing T2DM in participants walking 2–3 h a week or at least 40 min a week, respectively [ 30 , 31 ]. There are three primary benefits of physical activity on the delay of T2DM onset. First, the contraction of skeletal muscle cells induces an increase in blood flow into the muscle, enhancing glucose uptake from plasma [ 32 ]. Second, physical activity reduces the notorious intra-abdominal fat, which is a known risk factor that promotes IR [ 33 ]. Finally, moderate-intensity exercise has been shown to improve glucose uptake by 40% [ 34 ]. Physical activity improves glucose uptake and insulin sensitivity but it can also improve or even reverse inflammation and oxidative stress, which are T2DM predisposing factors [ 32 ].
3.3. Pathophysiology
Regarding the pathophysiology of the disease, a malfunctioning of the feedback loops between insulin action and insulin secretion results in abnormally high glucose levels in blood [ 2 ]. In the case of β-cell dysfunction, insulin secretion is reduced, limiting the body’s capacity to maintain physiological glucose levels. On the other hand, IR contributes to increased glucose production in the liver and decreased glucose uptake both in the muscle, liver and adipose tissue. Even if both processes take place early in the pathogenesis and contribute to the development of the disease, β-cell dysfunction is usually more severe than IR. However, when both β-cell dysfunction and IR are present, hyperglycaemia is amplified leading to the progression of T2DM [ 35 , 36 ].
4. Mechanisms Leading to T2DM and Pathophysiology
4.1. insulin secretion: physiological and dysfunctional mechanisms leading to t2dm, 4.1.1. β-cell physiology.
To safeguard proper β-cell function, cellular integrity must be ensured and the mechanisms and pathways implicated in the physiology of β-cell must be tightly regulated [ 35 ].
β-cells are responsible for insulin production, which is synthesized as pre-proinsulin. In the maturation process, pre-proinsulin undergoes a conformational modification carried out with the help of several proteins in the endoplasmic reticulum (ER) to yield proinsulin [ 37 ]. Afterwards, proinsulin is translocated from the ER to the Golgi apparatus (GA), entering into immature secretory vesicles and being cleaved into C-peptide and insulin [ 38 , 39 ].
Once matured, insulin is stored in granules until insulin release is triggered. Insulin release is primarily triggered by a response to high glucose concentrations. It is worth noting that some other factors can also induce insulin release such as amino acids, fatty acids and hormones [ 40 ]. When circulating glucose levels increase, β-cells take in glucose mainly through the glucose transporter 2 (GLUT2), a solute carrier protein that also works as a glucose sensor for β-cells. Once glucose enters, glucose catabolism is activated, increasing the intracellular ATP/ADP ratio, which induces the closing of ATP-dependant potassium channels in the plasma membrane. This leads to membrane depolarization and opening of the voltage dependant Ca 2+ channels, enabling Ca 2+ to enter the cell. The rise in the intracellular Ca 2+ concentration triggers the priming and fusion of the secretory insulin-containing granules to the plasma membrane, resulting in insulin exocytosis [ 38 , 40 , 41 , 42 ] ( Figure 1 A).

Signaling pathways involved in insulin secretion in β-cells in physiological conditions ( A ) and mechanisms leading to dysfunction ( B ). ( A ) Insulin release is primarily triggered by a response to high glucose concentrations and glucose in mainly internalized mainly through GLUT2 transporter. Glucose catabolism increases ATP/ADP ratio, ATP-dependant potassium channels are closed leading to membrane depolarization and opening of the voltage dependant Ca 2+ channels. The latter enables Ca 2+ influx triggering insulin exocytosis. Additional Ca 2+ channels as P2X, P2Y, SERCA and RYR contribute to Ca 2+ mobilization and insulin secretion. ( B ) hyperglycemia and hyperlipidemia promote oxidative stress leading to ROS generation that inhibits Ca 2+ mobilization and activates proapoptotic signals. Additionally, an excess of FFAs and hyperglycemia lead to the activation of the apoptotic unfolded protein response (UPR) pathways and generation of ER stress. Sustained high glucose levels increase proinsulin and IAAP biosynthesis, which generate ROS. GLUT2: glucose transporter 2, P2X: purinergic receptor X; P2Y: purinergic receptor Y; IP2: inositol 1,3-bisphosphate; IP3: inositol 1,4,5-trisphosphate; RYR: ryanodine receptor channel; SERCA: sarco-endoplasmic reticulum Ca 2+ -ATPase; FFA: free fatty acid, ROS: reactive oxygen species; UPR: unfolded protein response.
Additionally, Ca 2+ signals can be amplified by the RY receptors (RYR) and may play important roles in stimulus- insulin secretion coupling by virtue of their strategic locations within the cell and their ability to mediate Ca 2+ induced Ca 2+ release (CICR). RYR amplifies Ca 2+ signals when the channel is sensitized by messenger molecules generated from the nutrient metabolism or ligand-binding and are involved in the amplification of insulin secretion [ 43 ] ( Figure 1 A).
Nevertheless, other cell signals can also assist or enhance insulin release from β-cells. Among them, cAMP might be the most important messenger potentiating insulin release. Accumulated evidence suggests that cAMP induces insulin-containing secretory vesicle mobilization by depleting intracellular Ca 2+ reservoirs, thereby increasing intracellular Ca 2+ concentrations [ 44 ]. There is also compelling evidence that extracellular ATP is another important regulator of β-cell function. It is well-documented that β-cells release ATP through exocytosis of insulin granules upon glucose stimulation. Purinergic signaling via P2Y and P2X purinergic receptors stimulates Ca 2+ mobilization and regulates insulin exocytosis also independently of glucose. P2Y purinoreceptors have been reported to be coupled to G-proteins [ 45 , 46 ] whereas P2X-type receptors are ATP-activated ligand-gated ion channels non-selective for cations [ 47 ]. In the case of P2Y receptors, it has been proposed that insulin release could be mediated by intracellular Ca 2+ mobilization in response to inositol-1,4,5-trisphosphate (IP3) formation that triggers the release of Ca 2+ from ER stores, which amplifies the exocytosis-triggering Ca 2+ signal [ 48 , 49 ] ( Figure 1 A).
4.1.2. Mechanisms Leading to β-Cell Dysfunction
β-cell dysfunction has been traditionally associated with β-cell death [ 50 ]. However, recent evidence suggests that the dysfunction of β-cells in T2DM might be due to a more complex network of interactions between the environment and different molecular pathways implicated in cell biology [ 51 ]. In an excessive nutritional state, similar to that found in obesity, hyperglycemia and hyperlipidemia are often present, favoring IR and chronic inflammation. Under these circumstances, β-cells, due to differences in their genetic susceptibility, are subject to toxic pressures including inflammation, inflammatory stress, ER stress, metabolic/oxidative stress, amyloid stress, with the potential of ultimately leading to a loss of islet integrity [ 50 ].
An excess of FFAs and hyperglycemia lead to β-cell dysfunction by inducing ER stress through the activation of the apoptotic unfolded protein response (UPR) pathways [ 52 ]. In fact, lipotoxicity, glucotoxicity and glucolipotoxicity occurring in obesity, induce metabolic and oxidative stress that leads to β-cell damage [ 51 ]. Stress derived from high levels of saturated FFAs can activate the UPR pathway by several mechanisms including inhibition of the sarco/endoplasmic reticulum Ca 2+ ATPase (SERCA) responsible for ER Ca 2+ mobilization; activation of IP3 receptors or direct impairment of ER homeostasis. In addition, sustained high glucose levels increase proinsulin biosynthesis and islet amyloid polypeptides (IAAP) in β-cells, leading to the accumulation of misfolded insulin and IAAP and increasing the production of oxidative protein folding-mediated reactive oxygen species (ROS) [ 52 ]. These effects alter physiological ER Ca 2+ mobilization and favor proapoptotic signals, proinsulin mRNA degradation and induce interleukin (IL)-1 β release that recruits macrophages and enhances local islet inflammation [ 51 ] ( Figure 1 B).
As previously mentioned, insulin secretion has to be finely regulated to precisely meet metabolic demand. For that reason, proper islet integrity must be conserved in order to allow β-cells to respond to metabolic needs. Under pathogenic conditions, the mechanism described above can ultimately lead to disruption of islet integrity/organization, impairing optimal cell-to-cell communication within pancreatic islets, contributing to poor regulation of insulin and glucagon release and ultimately exacerbating the hyperglycemia. Defects in the synthesis of any insulin precursors, or insulin itself, as well as disruption of the secretion mechanism, can lead to insulin secretory dysfunction, the primary driver of β-cell failure, and a foundation of T2DM. For instance, reduced expression in the GLUT2 glucose transporter would affect the downstream signaling pathway [ 53 ], while failure in the folding of proinsulin is another finding commonly linked to deficient insulin production and diabetes [ 54 ].
4.1.3. Pathological Conditions Perpetuating T2DM
Nutritional factors.
High-caloric Western diet contains large amounts of fats and carbohydrates that elevate blood glucose and circulating very-low-density lipoproteins (VLDLs), chylomicrons (CMs) and their remnants (CMRs) that are rich in triglycerides (TG). This induces a spike in reactive oxygen species (ROS) concentrations, which in turn leads to an abnormal generation of inflammatory molecules. Given that inflammation is a recognized inducer of oxidative stress, a synergistic interaction occurs between the two processes after a heavy meal, with consequent amplification of harmful postprandial effects. The sustained and marked increase in steady-state levels of ROS contributes significantly to the pathogenesis of T2DM and IR. Therefore, a pro-oxidant environment leads to mitochondrial dysfunction, ER stress, activation of NADPH oxidase (NOX) and superoxide (O 2 − ) production. The increase in O 2 − production activates the five major pathways involved in the pathogenesis of diabetes complications: enhancement of the polyol pathway, increased formation of advanced glycation end products (AGEs), increased expression of AGEs receptor and its activating ligands, activation of protein kinase C (PKC) isoforms, and overactivity of the hexosamine pathway [ 55 , 56 , 57 ]. Through these pathways, increased intracellular ROS causes defective angiogenesis in response to ischemia, activates a number of proinflammatory pathways, and cause long-lasting epigenetic changes which drive persistent expression of proinflammatory genes even after glycemia is normalized [ 58 ]. Additionally, increased blood levels of FFAs also lead to mitochondrial dysfunction through two different mechanisms: (1) FFA metabolism by-products disturb the electron flow throughout the mitochondrial respiratory chain and (2) through the incorporation of FFAs into the mitochondrial membranes, thus likely favoring electron leakage [ 59 ].
Physical Activity
Reduced physical activity and exercise training, and increased sedentary behaviors constitute a link between obesity and T2DM and are associated with increased markers of chronic low-grade systemic inflammation [ 60 , 61 ]. In this condition, proinflammatory molecules are released into the bloodstream and within specific tissues such as interleukin 6 (IL-6), C-Reactive Protein (CRP), tumor necrosis factor-alpha (TNF-α) or IL-1 induces an inflammatory state known as metabolic inflammation [ 37 ]. Indeed, IL-1 is involved in the autoimmune response to β-cells in the pancreas, inhibition of β-cell function and activation of the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) transcription factor, thus inhibiting β-cell function and promoting apoptosis [ 32 ]. Preclinical data suggest that inflammation resolution could prevent the development of T2DM in obesity and prediabetes, which was substantiated by preclinical animal data showing that deletion of the macromolecular complex NLRP3 inflammasome, responsible for the production of IL-1β and IL-18, resulted in improved insulin sensitivity [ 62 ].
Intentional weight loss remains the cornerstone therapy to improve insulin sensitivity and in some circumstances to prevent the incidence of T2DM in individuals with obesity and prediabetes [ 63 ]. Regular exercise and increased physical activity enhance the production of anti-inflammatory cytokines such as IL-1 Receptor antagonist (IL-1Ra) and soluble TNF receptor (s-TNF-R) that are antagonists of IL-1 and TNF-α, respectively. Individuals with increased physical activity also show reduced circulating levels of IL-6, IL-18 and CRP, together with lower levels of leptin, a molecule associated with CRP [ 64 ]. Physical exercise can improve T2DM-inducing oxidative stress by inducing the synthesis of antioxidants such as glutathione (GSH), a major non-enzymatic antioxidant [ 65 ] and other antioxidant enzymes which lead to a long-term reduction in free radical levels [ 32 ].
Finally, irisin is an exercise-regulated myokine, which improves glucose tolerance [ 66 ] secreted by skeletal muscle [ 67 ] and adipose tissue [ 57 ] in response to exercise [ 68 ]. T2DM patients have been found to have lower circulating levels of irisin compared to control subjects. Additionally, diabetic patients with CVD had significantly lower serum irisin than non-CVD patients [ 69 ]. Low levels of serum irisin have been associated with 1.6 times increased risk of CVD incidence in T2DM patients [ 70 ].
Gut Dysbiosis
Gut microbiota is composed of many microbial species that impact human physiology and participate in different biological processes [ 71 ]. They can modulate the immune system and inflammatory response, regulate gut barrier integrity and human metabolism, take part in the synthesis of metabolites. Gut resident microorganisms produce many metabolites that contribute to physiology in healthy individuals. However, changes due to both inherited and acquired factors such as age, nutrition, lifestyle, genetic predisposition, or underlying diseases can affect the gut microbiota produced metabolite proportion leading to metabolic disturbances that can culminate in disease [ 72 , 73 , 74 ]. The better understating of gut microbiota has evidenced its important role in the development of diabetes and recent studies indicate that changes in dysbiosis can promote IR and T2DM [ 75 ]. A high-fat diet can induce up to threefold lipopolysaccharide (from Gram-negative bacteria) production in mice models, thereby contributing to low-grade inflammation and insulin resistance [ 76 , 77 ]. Furthermore, intestinal dysbiosis can reduce short-chain fatty acid synthesis that promotes gut barrier integrity, pancreatic β-cell proliferation and insulin biosynthesis [ 78 , 79 ]. Dysbiosis can also compromise the production of other metabolites such as branched aminoacids and trimethylamine thus disrupting glucose homeostasis and triggering T2DM development [ 80 , 81 ]. Understanding the clinical implications of the gut microbiome is a relatively new field, and requires further research to better elucidate the connection between gut microbiota and T2DM.
Metabolic Memory
Metabolic memory refers to the persistence of diabetic complications even after maintained glycemic control. This concept arose from the results of multiple large-scale clinical trials, which showed that after diabetes onset, diabetes complications persist and progress even when glycemic control is restored through pharmaceutical intervention [ 82 , 83 , 84 ]. Among them, the UKPDS post-trial study and Steno-2 trial showed that specifically early glycemic interventions prevent diabetic complication and has a marked decrease in CVD endpoints in patients that received either standard or intensive treatment following their diagnosis [ 84 ]. Later on, animal models of diabetes and in vitro cell cultures demonstrated that the initial hyperglycemic period results in permanent abnormalities (including aberrant gene expression) of target organs/cells [ 85 , 86 , 87 , 88 ]. Metabolic memory involves four mechanisms: epigenetics, oxidative stress, non-enzymatic glycation of proteins and chronic inflammation.
Epigenetics involves genetic modulation by factors other than individuals’ DNA sequence, and can regulate gene expression and determine which proteins are transcribed [ 89 ]. There are different epigenetic regulation mechanisms: direct methylation of cytosine or adenine residues, covalent modifications of histone proteins, higher-order chromatin structure and non-coding RNAs. Disruptions or imbalances in epigenetic mechanisms can lead to the development of diabetic pathophysiology [ 90 ].
MicroRNAs (miRNAs) are small non-coding RNA sequences synthesized as non-mature molecules that undergo several processing steps both in the nucleus and in the cytoplasm to become fully matured miRNAs. Once matured, miRNAs bind to their target gene’s mRNA, leading to mRNA silencing or degradation [ 91 ]. Increasing evidence highlights the importance of miRNA mediated post-transcriptional regulation in different aspects of β-cell biology such as cell differentiation, cytokine and growth factor-mediated signaling, glucose metabolism and insulin synthesis and secretion [ 92 ]. Deregulation of miRNA expression can directly impair β-cell function leading to the development of T2DM [ 93 ]. To date, more than 2600 miRNAs have been described within the human genome (miRBase, v.22.1), and multiple miRNAs have been shown to be involved in the pathogenesis of T2DM, including miR-200, miR-7, miR-184, miR-212/miR132 and miR-130a/b/miR-152 [ 94 ]. For instance, overexpression of miR-7 results in reduced insulin secretion via inhibition of genes involved in vesicle fusion and SNARE activity such as Snca, Cspa and Cplx1 [ 95 ]. In the case of miR-375, over-expression results in impaired exocytosis and thereby reduced insulin secretion. Conversely, it is the downregulation of miR-375 expression that causes a reduction in β-cell mass [ 93 , 96 , 97 ].
Several studies have evidenced that deregulation of the microRNA (miRNA) profile (post-translational histone methylation and non-canonical histone variant inclusion in octomers) may persist even after normoglycemia restoration [ 98 , 99 , 100 , 101 ]. MiRNAs participate in metabolic memory by targeting the mRNA of genes encoding enzymes involved in DNA methylation and those tightly regulated at the level of promoter methylation, transcription, and processing [ 102 ]. It has been shown that high glucose levels can alter post-translational histone modifications (PTHMs) and the activity of DNA methyltransferases generating irreversible changes that explain the long-term harmful effects of metabolic memory [ 103 , 104 , 105 , 106 ].
Hyperglycaemia induces an excess of ROS generation by mitochondria, which gives rise to diabetes complications [ 107 ] that may persist even when hyperglycemia is controlled. The damage following hyperglycemia-induced oxidative stress can be prevented when good glycemic control is initiated very early, but is not easily reversed if poor control is maintained for a longer duration [ 108 , 109 ]. At the early stages of T2DM, there is a relationship between hyperglycemia, increased oxidative stress, and excessive AGE formation. As the disease progresses, there is persistent protein glycation of the components of the respiratory chain that together with mitochondrial DNA damage can generate a hyperglycemia-independent concatenation of events leading to a synergy between oxidative stress and AGEs [ 86 ]. The effects of this metabolic imbalance activate inflammatory processes through receptor binding of AGEs or ROS which can modify the composition and structure of the extracellular matrix [ 98 ]. These structural changes may cause endothelial dysfunction and then atherosclerosis [ 98 ].
Finally, low-grade inflammation, which is involved in T2DM development and its vascular complications, has been shown to mediate metabolic memory. Many environmental factors (age, obesity, sedentarism and diet) that promote T2DM development trigger an inflammatory response leading to IR and endothelial dysfunction [ 105 , 110 , 111 ]. Obesity leads to NF-κB activation, which mediates the expression of inflammatory genes, which enhances monocyte binding to endothelial and vascular smooth muscle cells, subsequently promoting monocyte-to-macrophage differentiation [ 105 ]. In addition, NF-κB activation induces expression of inflammatory cytokines that are involved in vascular inflammation, with subsequent generation of endothelial adhesion molecules, proteases, and other mediators [ 111 ]. Another important factor that links inflammation and oxidative stress in obesity condition is the Toll-like receptor, which contributes to hypertension, insulin resistance, and obesity [ 105 ].
In summary, T2DM is a heterogeneous and progressive disorder that represents a series of metabolic conditions associated with hyperglycemia and caused by defects in insulin secretion and/or insulin action due to a complex network of pathological conditions. There are many different paths, driven by various genetic and environmental factors, that interact and mutually reinforce each other leading to an increased risk of other diseases including heart, peripheral arterial and cerebrovascular disease, obesity and nonalcoholic fatty liver disease, among others. The complex network of pathological conditions leading to T2DM development are summarized in Figure 2 .

Type 2 Diabetes Mellitus (T2DM) risk factors and the pathological changes leading to the perpetuation of insulin dysfunction. Complex combinations of genetic, metabolic and environmental factors that interact with one another constitute both non-modifiable (ethnicity and family history/genetic predisposition) and modifiable risk factors (obesity, low physical activity and an unhealthy diet). These states affect cell function resulting in a complex network of pathological changes that influence mutually and lead to the perpetuation of insulin dysfunction. ROS: reactive oxygen species; ER: endoplasmic reticulum; AGEs: advanced glycation end products; PKC: protein kinase C; LPS: lipopolysaccharide; miRNA: microRNA.
Mitochondrial Dysfunction
There is increasing evidence associating mitochondrial dysfunction with T2DM development, age-related IR and T2DM complications [ 112 ]. Indeed, oxidative stress, defective mitochondrial biogenesis, genetic mutations affecting mitochondrial integrity and aging promote mitochondrial dysfunction and are closely associated with T2DM development ( Figure 3 ) [ 113 , 114 ].

Mitochondrial dysfunction and contribution to T2DM development. Oxidative stress, defective mitochondrial biogenesis and impaired mitophagy promote mitochondrial dysfunction. Generation of ROS links mitochondrial dysfunction and IR. As a consequence of nutrient overload, electron supply to the mitochondrial ETC increases and the electron excess is transferred to oxygen generating O 2 − and H 2 O 2 . ROS oxidize proteins, damage DNA and membrane lipids. Mitofusin-2 and PGC 1α are downregulated leading to reduced mitochondrial biogenesis. Cellular stress and ROS production contribute to higher mitochondrial fission and impaired mitophagy. PCG 1α: Peroxisome proliferator-activated receptor-gamma coactivator-1.
The main function of mitochondria is ATP synthesis through oxidative phosphorylation in response to metabolic demand [ 115 ]. Mitochondria also participate in the production of different metabolites used as precursors of several macromolecules (lipids, proteins, and DNA). In addition, mitochondria play an important role in maintaining ion homeostasis, ROS clearance, the stress response, and serve to integrate multiple signaling pathways [ 116 , 117 ]. An imbalance between energy intake and expenditure in the mitochondria generates mitochondrial dysfunction, a state characterized by a reduced ratio of energy production to respiration [ 112 ]. Under these circumstances, nutrient oxidation efficiency is reduced leading to a decreased ratio of ATP synthesis/oxygen consumption, which increases O 2 − production [ 118 ]. In fact, the accumulation of ROS in the mitochondria is one proposed mechanism linking mitochondrial dysfunction to IR [ 119 ]. This relationship was corroborated in studies showing decreased mitochondria oxidative capacity in skeletal muscle and impaired lipid metabolism in obese and insulin-resistant individuals compared to healthy controls [ 120 , 121 , 122 ]. In addition, patients with T2DM have been found to have downregulation of genes involved in oxidative metabolism that are regulated by the peroxisome proliferator-activated receptor γ co-activator 1α (PGC 1α) [ 123 , 124 ] and a diminished phosphocreatine re-synthesis rate, both indicative of impaired mitochondrial function [ 125 ] ( Figure 3 ). Moreover, some relatives of T2DM patients have been found to have decreased mitochondrial respiration suggesting that mitochondrial dysfunction may precede T2DM development. It has also been proposed that T2DM development may be a direct consequence of defects in the oxidative phosphorylation system and the electron transport chain (ETC) rather than a decrease in mitochondrial content [ 126 ].
The generation of ROS is highly implicated in the relationship between mitochondrial dysfunction and insulin resistance. ROS production takes place mainly at complex I and complex III of the ETC and increases when ETC is not able to handle excessive electron input. In these circumstances, as a consequence of nutrient overload, electron supply to the mitochondrial ETC increases and the electron excess is transferred to oxygen generating O 2 − and subsequent hydrogen peroxide [ 127 ]. ROS generated in mitochondria oxidize the Cys and Met residues in proteins, damaging protein structure, impairing their function and eventually causing cell death. ROS species also damage DNA and membrane lipids, thus promoting mitochondrial dysfunction [ 128 ]. In addition, ROS overproduction activates the polyol pathway, the formation of AGEs, and the expression of the AGEs receptor and its activating ligands. It also activates PKC isoforms and upregulates the hexosamine pathway contributing to T2DM worsening [ 129 , 130 ]. In sum, excessive ROS generation by mitochondria contributes to accelerated T2DM progression ( Figure 3 ).
Mitochondrial dysfunction includes a reduction in mitochondrial biogenesis, along with a decrease in the expression of mitochondrial oxidative proteins, such as ETC complexes, which leads to decreased substrate oxidation. The damage produced by high oxidative stress in the mitochondria activates mitophagic processes in order to eliminate dysfunctional mitochondria or in case of excessive cellular stress to apoptosis [ 131 ]. These two processes reduce substrate utilization and enhance the accumulation of lipid intermediates such as diacylglycerols (DAG) and ceramide (CER) that disrupt the insulin signaling pathway [ 132 ]. DAG induces an increment of the serine/threonine phosphorylation of IRS-1, reducing its insulin-stimulated tyrosine phosphorylation and downstream propagation of the insulin signaling pathway [ 133 ] while CER inhibits protein kinase AKT [ 133 ]. The accumulation of DAG and CER contributes to the mitochondrial dysfunction seen in IR ( Figure 3 ).
Defects in mitochondrial biogenesis may be mediated by the downregulation of PGC 1α that has also been detected in T2DM patients [ 123 , 124 ]. PGC 1α is a transcription coactivator that regulates the expression of key genes involved in mitochondrial biogenesis, adaptive thermogenesis and metabolic substrate metabolism [ 134 ]. Furthermore, some of the genes involved in oxidative metabolism that are downregulated in individuals with T2DM are under the control of PGC 1α [ 124 ]. Mitofusin-2 , a key driver in mitochondria biogenesis is also downregulated in humans with T2DM [ 135 ]. Interestingly, mitofusin-2 levels increase upon weight loss indicating that nutrient and energy oversupply leads to mitochondrial dynamics defects [ 135 ].
Mitochondrial homeostasis is maintained via mitochondrial biogenesis and the selective clearance of damaged organelles. Mitochondrial dynamics are crucial to maintaining healthy mitochondria and control their quantity. Mitochondria fission promotes the removal of damaged mitochondria in a process known as mitophagy, which has to be efficiently and tightly regulated in order to preserve cell homeostasis [ 136 ]. Thus, mitophagy is considered to be one of the core mechanisms controlling the mitochondrial quantity and quality [ 137 ]. The process of removing damaged mitochondria consists of two steps: the induction of general autophagy and the priming of damaged mitochondria for selective autophagy recognition [ 138 ]. Once the degradation process is completed, the products are released back into the cytosol where macromolecular constituents are recycled. This process generates energy to maintain cell viability under unfavorable conditions and protects the cell during stress conditions [ 136 , 139 ]. When mitophagy is impaired, cellular stress and ROS production increase contributing to reduced hepatic insulin sensitivity and glucose homeostasis, two of the major pathological branches of T2DM development [ 112 , 140 ]. Deregulation of mitochondria dynamics with a shift towards fission promotes metabolic dysfunction as demonstrated by the onset of obesity and IR following the ablation of fusion protein in mice [ 141 , 142 ]. Furthermore, increased mitochondrial fission and mitochondrial fragmentation have been associated with mitochondrial depolarization, impaired ATP production and decreased insulin-dependent glucose uptake as well as increased mitochondrial ROS and impaired insulin signalling in C2C12 murine cell line and cybrids, respectively [ 143 , 144 ]. These studies highlight that the deleterious effect of unbalanced mitochondrial dynamics on metabolic health. Enhanced mitochondria fission also negatively impacts fatty acid β-oxidation, which is a pivotal metabolic defect in obesity and IR [ 120 , 121 ] contributing to the accumulation of lipotoxic lipid species. Fusion-shifted mitochondria dynamics has been also associated with an increase in fatty acid utilization putatively preventing lipotoxicity [ 145 ].
The role of mitochondrial genetics in the risk of T2DM has been clearly established. Indeed, several mtDNA variants (homoplasmic or heteroplasmic) have been associated with T2DM development. To date, the group of heteroplasmic variants associated with a higher risk of T2DM development includes A3243G, T14577C and A5178C [ 146 , 147 , 148 , 149 ]. The group of homoplasmic variants associated with T2DM risk includes C1310T, G1438A, A12026G, T16189C and A14693G [ 150 , 151 , 152 ]. It is important to note that additional studies are necessary to determine whether more metabolically active tissues that generate more mitochondrial ROS have increased rates of mtDNA heteroplasmy in T2DM.
To summarize, there is a highly nuanced and bi-directional relationship between mitochondrial dysfunction and T2DM. On one hand, aspects of T2DM such as insulin resistance can lead to mitochondrial dysfunction, such as through nutrient overload leading to ROS accumulation. On the other hand, mitochondrial dysfunction may predispose patients to subsequently developing T2DM, as evidenced by the presence of mtDNA variants associated with T2DM. Additional research is needed to better characterize the relationship between mitochondrial health and diabetes.
5. Insulin Resistance
IR refers to a decrease in the metabolic response of insulin-responsive cells to insulin or, at a systemic level, an impaired/lower response to circulating insulin by blood glucose levels [ 153 ]. There are three broad categories of IR or insulin-deficient conditions: (1) diminished insulin secretion by β-cells; (2) insulin antagonists in the plasma, due either to counter-regulatory hormones or non-hormonal bodies that impair insulin receptors or signaling; and (3) impaired insulin response in target tissues [ 154 ]. The action of insulin is influenced by the interplay of additional molecules including growth hormone and IGF-1 in the fed state. While fasting, the insulin response is mitigated by glucagon, glucocorticoids and catecholamines in order to prevent insulin-induced hypoglycemia. The ratio of insulin/glucagon plays a major role in this regulation, since it determines the relative degree of phosphorylation of downstream enzymes in the regulatory signaling pathways. While catecholamines promote lipolysis and glycogenolysis, glucocorticoids promote muscle catabolism, gluconeogenesis and lipolysis. Hence, excessive secretion of these hormones may be responsible for inducing IR [ 155 , 156 ]. Regarding the last category, there are three main extra-pancreatic insulin-sensitive organs that play major roles in the aforementioned processes: skeletal muscle, adipose tissue and liver. A defective action of insulin in these tissues often precedes the development of systemic IR, thus progressively leading T2DM.
5.1. Skeletal Muscle
Skeletal muscle IR is considered to be the most important extra-pancreatic factor in the development of T2DM [ 157 ]. Under physiological conditions, insulin stimulates muscle glycogen synthesis by enhancing glucose uptake from plasma. There are three primary rate-limiting factors implicated in glucose uptake and glycogen synthesis: glycogen synthase, hexokinase and the glucose transporter GLUT4 [ 158 ]. Upon insulin binding to insulin receptor (INSR) in muscle cells, GLUT4 translocates from intracellular compartments (early endosomes (EE), endosomal recycling compartment (ERC) and trans-Golgi network (TGN)) to the plasma membrane. This process allows glucose uptake and reduces circulating glucose levels [ 159 ].
Mutations that reduce the expression of insulin receptor or GLUT4, as well as any defect in either upstream or downstream signaling pathway would reduce glucose intake into the muscle resulting in a hyperglycaemic state [ 153 , 160 ]. The activation of INSR tyrosine kinase activity is essential for the action of insulin on glucose metabolism. Insulin binding to the α-subunit of the INSR causes phosphorylation of the β-subunit on multiple tyrosine residues and allows insulin-mediated signaling. Thus, mutations in any of the main phosphorylation sites can impair INSR tyrosine kinase activity, thereby impairing insulin action on skeletal muscle [ 161 ]. As mentioned above, mutations in key proteins of the downstream signaling pathway such as IRS-1 and IRS-2 or phosphoinositide 3-kinase (PI3K) also impair insulin action on the muscle. Apart from mutations or defective epigenetic regulation, environmental factors can also play an important role in glucose uptake by muscle. Physical activity increases blood flow into skeletal muscle cells and thereby enhances glucose utilization [ 32 ]. Obesity, which is associated with chronic inflammation, contributes to IR and T2DM. Increasing evidence suggests that as a consequence of obesity, increased immune cell infiltration and secretion of proinflammatory molecules in intermyocellular and perimuscular adipose tissue leads to skeletal muscle inflammation. This ultimately leads to myocyte inflammation, impaired myocyte metabolism, and contributes to IR via paracrine effects [ 162 ].
5.2. Adipose Tissue
Adipose tissue is a metabolically dynamic tissue capable of synthesizing a wide range of biologically active compounds that regulate metabolic homeostasis at a systemic level [ 163 ]. Indeed, adipose tissue participates in a broad range of biological processes involving, among others, immunity, coagulation, angiogenesis, fibrinolysis, reproduction, vascular tone control, appetite regulation, body weight homeostasis and glucose and lipid metabolism [ 164 ].
Insulin acts on adipose tissue in two different ways: (1) stimulating glucose uptake and triglyceride synthesis; and (2) suppressing triglyceride hydrolysis and inducing the uptake of FFA and glycerol from circulation [ 165 ]. In the fed state, GLUT4 allows uptake of glucose from the bloodstream into adipocytes, activating glycolysis in which glycerol-3-phospate (glycerol-3-P) is produced and incorporated into lipogenic pathways. Glycerol-3-P, along with the fatty acids coming from VLDLs, are esterified, forming triacylglycerol (TGA) that is stored in lipid droplets. During metabolic stress, TGA droplets the adipocyte are depleted, in order to provide FFA to be used as an energy source in other tissues.
An impaired response to insulin stimulation by adipose tissue is known as adipose IR (Adipose-IR). Adipose-IR can lead to impaired suppression of lipolysis, impaired glucose uptake, and enhanced FFA release into plasma even in the presence of high insulin levels [ 166 ]. Among the signaling elements affected by adipose-IR, we found that defective AKT activation impairs GLUT4 translocation to the membrane and promotes the activation of lipolytic enzymes that aggravate hyperglycemia [ 153 ]. Adipose-IR, as mentioned before, is associated with glucose intolerance and elevated release of FFA into a plasma that accumulates in other tissues such as muscle or liver. In the case of the liver, FFA accumulation results in impaired insulin signaling that promotes hepatic gluconeogenesis and impairs the glucose-stimulated insulin response, inducing T2DM development.
It has been shown that abnormally increased adipose tissue mass and adipocyte size correlate with pathologic vascularisation, hypoxia, fibrosis and macrophage-mediated inflammation [ 167 ]. A high-fat diet and obesity can activate saturated FFA-stimulated adenine nucleotide translocase 2 (ANT2), an inner mitochondrial protein that results in adipocyte hypoxia and triggers the transcription factor hypoxia-inducible factor-1α (HIF-1α). This culminates in adipose tissue dysfunction and inflammation [ 1 ]. Hypertrophied adipocytes as well as adipose tissue-resident immune cells contribute to increased circulating levels of proinflammatory cytokines. This increase in circulating proinflammatory molecules, together with an increase in local cytokine releases such as TNF and IL-1β and IL-6 facilitates the emergence of a chronic state of low-grade systemic inflammation, also known as metabolic inflammation [ 1 ]. This chronic inflammatory state is considered to be a key part in the pathogenesis of IR and T2DM [ 168 ]. The insulin stimulation effects on healthy and hypertrophic adipose tissue are shown in Figure 4 .

Insulin stimulation effects on healthy and hypertrophic adipose tissue. In healthy adipose tissue insulin stimulates glucose uptake and TG synthesis, induces FFA uptake and diminishes macrophage-mediated inflammation. Hypertrophic adipose tissue leads to diminished glucose uptake, TG synthesis and enhances FFA release, hypoxia and macrophage-mediated inflammation. FFA: free fatty acid.
In the liver, insulin does not only regulate glucose production/utilization but also affects lipid metabolism more broadly. When circulating glucose levels increase and insulin is secreted by pancreatic β-cells, insulin binding to liver INSR induces autophosphorylation of the receptor. Consequently, insulin receptor substrates (IRSs) are recruited and phosphorylated. In turn, IRSs activate PI3K, which phosphorylates phosphatidylinositol (4,5)-bisphosphate (PIP2), generating phosphatidylinositol (3,4,5)-triphosphate (PIP3). PIP3 then activates PDK1, which phosphorylates AKT. In addition, AKT is phosphorylated by mTORC2. Once AKT is fully activated, it participates in several downstream pathways that regulate multiple metabolic processes including glycogen synthesis, gluconeogenesis, glycolysis and lipid synthesis [ 169 ].
In physiological states, the combined action of glucagon and insulin allows the precise regulation of hepatic glucose output. While glucagon induces hepatic glucose production, insulin acts as a potent inhibitor of glucose production when its concentration in the blood is elevated [ 170 ]. The effect of insulin on hepatic glucose production is due to both direct and indirect mechanisms. However, the relative importance of each of these mechanisms remains unclear [ 171 ].
In addition to inducing glycogen synthesis, insulin also inhibits hepatic glucose production by activating FOXO1, resulting in a reduction of hepatic glucose release. FOXO1 is a transcription factor that belongs to a subclass of the forkhead family of transcription factors that possess a forkhead box-type DNA binding domain. FOXO1 recognizes a specific regulatory element termed the insulin response element (IRE) on the promoters of glucose-6-phosphatase (G6Pase) and phosphoenolpyruvate carboxykinase (PEPCK) genes, both of which play important roles in maintaining glucose level in states of starvation [ 172 , 173 , 174 ]. Thus, through inhibition of FOXO1, insulin promotes glucose storage as glycogen and inhibits glucose synthesis and hepatic glucose output [ 175 ] ( Figure 5 ).

Signaling pathways involved in insulin signaling in hepatocytes. Binding of insulin to INSR induces IRSs recruitment and phosphorylation. Phosphorylated IRSs activate PI3K, generating PIP3 which activates PDK resulting in AKT phosphorylation. AKT is fully activated by further mTORC2 phosphorylation and participates in several downstream pathways that regulate multiple metabolic processes including glycogen synthesis, gluconeogenesis, glycolysis and lipid synthesis. INSR: insulin receptor; PIP2: inositol 1,3-bisphosphate; PIP3: inositol 1,4,5-trisphosphate; IRS1: insulin receptor substrate 1; PI3K: phosphoinositide 3 kinase; mTORC2: mammalian target of rapamycin complex 2; PDK1: Phosphoinositide-dependent kinase-1; AKT: protein kinase B; AS160: Akt substrate of 160 kDa; GLUT4: glucose transporter 4; GSk3β: Glycogen Synthase Kinase 3 Beta; GS: Glycogen synthase; FOXO1: Forkhead box protein O1; G6pc:Glucose 6 phosphate; Pck1: Phosphoenolpyruvate Carboxykinase 1.
Similar to the case in insulin-sensitive tissues, in states of IR, physiologic levels of circulating insulin are insufficient to elicit the appropriate insulin response in hepatic cells [ 176 ]. In the liver, IR impairs glycogen synthesis, fails to suppress glucose production, enhances lipogenesis, and increases the synthesis of proteins such as the proinflammatory CRP. In fact, the abnormal production of proinflammatory proteins such as adipocytokines and cytokines, combined with conditions such as oxidative stress, can lead to an inflammatory state responsible for altered insulin response by the liver [ 175 ].
6. T2DM Outcomes/Complications: Cardiovascular Risk
As described in the previous sections, T2DM is a multisystem disease with a strong correlation with CVD development [ 177 ]. T2DM leads to a two- to four-fold increase in the mortality rate of adults from heart disease and stroke and is associated with both micro- and macro-vascular complications, the latter consisting of accelerated atherosclerosis leading to severe peripheral vascular disease, premature coronary artery disease (CAD) and increased risk of cerebrovascular diseases [ 178 , 179 , 180 ]. These factors lead to T2DM being considered a significant risk factor for CVD [ 181 ], likely through the involvement of several molecular mechanisms and pathological pathways. These include the role of IR in atherosclerosis, vascular function, oxidative stress, hypertension, macrophage accumulation and inflammation [ 182 , 183 , 184 , 185 ]. The following sections describe in detail the main factors implicated in cardiovascular risk outcomes from T2DM and the interactions between them ( Figure 6 ).

Factors implicated in cardiovascular risk outcomes from T2DM and the interactions between them. T2DM derived hyperglycemia, hyperinsulinemia and IR causes endothelial dysfunction, diabetic dyslipidemia and inflammation leading to CVD. The flowchart illustrates the multiple interactions among the implicated factors.
6.1. Diabetic Dyslipidaemia and Atherosclerosis Development
Dyslipidaemia is a common feature of T2DM, and increases the incidence of atherosclerosis and mortality of diabetic patients [ 186 ]. The hallmark of diabetic dyslipidemia is a characteristic dyslipidaemic profile consisting of elevated TG, TG-rich lipoproteins (TRLs), small dense LDLs (sdLDL), and reduced HDL levels [ 187 , 188 , 189 ]. Although the pathophysiology of dyslipidemia in T2DM is not completely characterized, several factors such as hyperglycemia, insulin resistance, hyperinsulinemia, abnormalities in adipokines and adipocytokines have been implicated [ 190 ]. Epidemiological studies indicate that TG-rich lipoproteins and their remnants contribute to atherogenesis and CVD risk [ 191 , 192 , 193 , 194 , 195 ] and experimental studies indicated a connection between cholesterol deposition and inflammation as a result of TRLs entry into the artery wall [ 196 , 197 ]. TRLs consist of a great variety of nascent and metabolically modified lipoprotein particles including intestine-derived apoB48 (chylomicrons and chylomicron remnants) and liver-derived apoB100 (VLDL and its remnants). TRLs are highly heterogeneous in size, density, and apolipoprotein composition [ 198 ].
Under physiological conditions, chylomicrons deliver dietary lipids and lipid-biliary sources to the liver, which upon entering central circulation acquire apoE, apo-CI, apo-CII and apo-CIII from circulating HDL ( Figure 7 ). Apo-CII, an activator of lipoprotein lipase (LPL), hydrolyzes TG within the chylomicron core, thereby releasing free fatty acids (FFAs). The progressive removal of TGs leads to the formation of chylomicron remnants (CR), which upon apoE incorporation, are cleared by hepatocytes ( Figure 7 ). This, together with the uptake of FFA generated by lipolysis in adipose tissue provides the major source of hepatic VLDL assembly and secretion. Once in the circulation, VLDL particles incorporate apo-CII and apoE from HDL allowing VLDL to be progressively lipolyzed leading to the generation of smaller VLDL particles (VLDL1, VLDL2 and VLDL3), IDL, and finally LDL ( Figure 7 ). Lipoprotein production, metabolism, and clearance are efficient processes. However, T2DM and IR are among the most important metabolic derangements in these process and they give rise to impaired metabolism and clearance of chylomicrons and VLDLs [ 199 , 200 ].

Diabetic dyslipidemia: mechanisms leading to T2DM dyslipidemia and lipoprotein clearance in physiological an IR conditions. ( A ) IR leads to an impaired adipose tissue fat storage, resulting in constitutive FFA release from the intracellular TG stores of adipocytes. The released FFAs are taken up by hepatocytes, where they can be directed to the mitochondria and undergo β-oxidation; be re-assimilated into TG to assemble new VLDL particles; shifted to gluconeogenesis resulting in a worsening of hyperglycemia; or stored as TG leading to hepatic steatosis. ( B ) Under physiological conditions, VLDL particles incorporate apo-CII and apoE from HDL allowing VLDL to be progressively lipolyzed leading to the generation of smaller VLDL particles (upper panel). T2DM and IR impair metabolism and clearance of chylomicrons and VLDLs. Activation of CETP promotes an exchange of TG out of RLPs and incorporates CE from HDL and LDL particles leading to reduced levels of circulating HDL-C and an increase in the more atherogenic sdLDL particles (lower panel). TG: triglyceride; FFA: free fatty acid, LPL: lipoprotein Lipase; CR: chylomicron remnants; HL: hepatic lipase; CETP: Cholesteryl Ester Transfer Protein; ApoE: apolopoprotein E; ApoC-II: apolipoprotein CII; apoC-III: apolipoprotein CIII; VLDL: very low-density lipoprotein; sdLDL: small dense lipoprotein.
Mechanisms Leading to T2DM Dyslipidemia and Atherosclerosis
Increased hepatic TG content present in T2DM patients leads to elevated hepatic production of VLDL and normal or slightly elevated LDL-C levels, most commonly sdLDLs enriched in TG [ 189 , 201 ]. One of the primary abnormalities in IR is impaired adipose tissue fat storage, resulting from insulin’s inability to inhibit hormone-sensitive lipase (HSL). This results in constitutive FFA release from the intracellular TG stores of adipocytes. The released FFAs are taken up by hepatocytes, where they can be directed to the mitochondria and undergo β-oxidation; be re-assimilated into TG to assemble new VLDL particles; shifted to gluconeogenesis resulting in a worsening of hyperglycemia; or stored as TG leading to hepatic steatosis.
The dominant feature of diabetic dyslipidemia is the increased production rate of VLDL-apoB100 by the liver, mainly VLDL1, which is related to insulin sensitivity indices [ 202 ]. This highlights the role of insulin on VLDL assembly and secretion by hepatocytes [ 203 ]. Insulin plays a role in almost all the steps of VLDL assembly and secretion. It is known that insulin inhibits the transcription of Mttp, the gene coding for the microsomal transfer protein (MTP), the protein responsible for assembling TG with apoB100 [ 204 ]. MTP facilitates concerted lipid transfer and apoB100 folding as it enters the ER lumen and lipidation determines the amount of the active pool of apoB100 [ 205 ]. Lipidation of apoB100 is a co-translational event and a rate-limiting step of apoB100 mRNA stability thus low availability of TG leads to apoB100 degradation. The addition of TG to apoB100 generates nascent VLDL particles that are transported to the GA by Sar2/COPII-containing vesicles. Within the GA, VLDL maturation occurs in a process promoted by the phospholipase D1 (PLD1) [ 203 ]. Therefore, in insulin-resistant condition, MTP expression and activity is increased thus contributing to raising apoB100 lipidation and to its rescue from degradation. Indeed, IR leads to a loss of the acute insulin-mediated inhibition of apoB100 secretion [ 205 ].
Availability of TGs within hepatocytes is important for VLDL synthesis [ 206 ] and the liver uses both de novo synthesized FAs and extra-hepatic FFAs as a substrate for TG synthesis [ 207 ]. De novo lipogenesis occurs primarily in the fed state in which the expression of lipogenic genes is regulated by the sterol regulatory element-binding protein (SREBP). The SREBP-1c isoform up-regulates almost all the enzymes involved in FA synthesis as well as enzymes that supply acetyl-CoA units and reducing equivalents to the pathway [ 208 ]. Insulin regulates SREBP-1c, which explains the lipogenic effect of chronic hyperinsulinemia [ 208 ]. FFAs derived from adipose tissue is also a major source of liver TGs and VLDL production. As mentioned above, T2DM is characterized by increased production of FFAs by adipose tissue [ 207 ]. Therefore, in IR, an increase in TG lipolysis in adipose tissue and FFA influx serves as another source of lipid to the liver [ 207 ].
As mentioned above, in the IR milieu, insulin has reduced capacity to inhibit VLDL secretion in the fed state, the availability of apo-CII is lower and apo-CIII production is increased [ 209 ]. These events result in the accumulation of VLDL remnants and IDL due to diminished clearance of TRLs by hepatocytes [ 210 ]. Additionally, hepatic IR also impairs LRP1 translocation from intracellular vesicles to the hepatocyte plasma membrane, which contributes to impaired clearance of TRLs [ 211 , 212 ] ( Figure 7 ).
In an effort to offload TG from remnant lipoproteins (VLDL 2+3 and IDL; RLPs), CETP is activated and promotes an exchange of TG out of RLPs and incorporates CE from HDL and LDL particles [ 213 ]. The TG-enriched HDL and LDL particles are better substrates for lipolysis by hepatic lipase leading to reduced levels of circulating HDL-C and an increase in sdLDL particles, which are more atherogenic [ 214 ]. The increased movement of CE into circulating TRLs mediated by enhanced activity of CETP [ 215 ] plays a key role in generating small dense HDL and LDL particles, the former being less atheroprotective and the latter more atherogenic [ 216 ]. TG enrichment of HDL enhances circulating HDL clearance [ 217 ].
The lower HDL concentration and modified composition of HDL have an important impact in diminishing the particle capacity of inducing cholesterol efflux from the cells, which is the first step in reverse cholesterol transport (RCT) [ 218 ]. The impaired RCT activity has been associated with increased risk of CAD [ 219 ] and with flow-mediated vasodilation in T2DM patients [ 220 ].
Atherosclerosis is accelerated by the increased permeability of sdLDL into the subendothelial space ( Figure 7 ) [ 221 , 222 ]. SdLDL particles are characterized by a lower affinity for LDLR due to conformational rearrangements occurring in apoB100 as the particle decreases in volume and size [ 223 ]. Furthermore, sdLDL particles are more susceptible to oxidation and thus avidly scavenged by activated macrophages in the subendothelial space, giving rise to foam cells [ 224 ]. In addition, sdLDL particles show increased proteoglycan binding and facilitated entry into the arterial wall, increased arterial retention, and a longer half-life [ 225 ]. sdLDL particles are also more likely to be glycated, more resistant to breakdown, and more susceptible to oxidation by free radicals [ 226 ].
There is an insulin response element in the gene for apoA-I, the primary apolipoprotein constituent of HDL particles [ 227 , 228 ]. As the liver becomes more insulin resistant, less apoA-I is produced and there is less HDL biogenesis. Adipocytes express the ATP-binding membrane cassette transport protein A1 (ABCA1). IR downregulates the expression of ABCA1 on the surface of adipocytes and reduces HDL formation by these cells [ 229 , 230 , 231 ]. Chylomicrons are enriched with apoA-I. IR reduces the release of this apoA-I into the serum by inhibiting LPL. In addition, within the milieu of IR of diabetes, HDL particle concentrations are not only quantitatively reduced, but also tend to be dysfunctional and unable to perform their primary functions, including reversal of cholesterol transport and inhibition of oxidative and inflammatory phenomena [ 232 ].
This highly atherogenic lipid profile is a pivotal contributor to atherogenic dyslipidemia, which is causally linked to the development and progression of atherosclerotic CV disease (ASCVD) [ 233 , 234 ]. The relationship between atherogenic dyslipidemia and ASCVD is supported by prospective longitudinal cohorts, clinical evidence and genetic linkage studies. As an example, the best predictor of risk of myocardial infarction at the population level in the INTERHEART study was the apolipoprotein (apo) B100/apoA-I ratio, reflecting the correlation between all apoB (atherogenic lipoproteins) and HDL (representing classically anti-atherogenic particles) [ 235 ]. The relationship between atherogenic dyslipidemia and ASCVD has also been demonstrated in prospective randomized clinical trials using statins. Even when treated with statins, patients with the atherogenic dyslipidemia phenotype have a higher risk of CV events than those without AD [ 236 , 237 ].
Diabetic dyslipidemia acts in concert with other metabolic and vascular abnormalities to further compound vascular risk. Chronic hyperglycemia induces endothelial dysfunction through a variety of mechanisms such as by reducing vasodilation, increasing vasoconstriction, increasing exposure to free radicals and impairing endothelial cell function, with a net effect of facilitating pro-atherogenic conditions [ 238 ]. Increased activity of the renin-angiotensin axis has also been found to further increase oxidative stress [ 239 ].
6.2. Impaired Endothelial Function and Atherosclerosis Development
Endothelium plays an important role in the regulation of vascular tone and structure through a balanced release of endothelial-derived relaxing and contracting factors. This balance is altered in T2DM leading to alteration of the physicochemical properties of the vascular wall via endothelial dysfunction, oxidative stress, platelet hyperreactivity, and inflammation [ 240 , 241 ]. These abnormalities lead to enhanced vasoconstriction, development of atherosclerosis, and favored thrombus formation [ 179 , 180 ].
6.2.1. Mechanisms Leading to Endothelial Dysfunction in T2DM
Vascular endothelial cells are particularly susceptible to developing intracellular hyperglycemia because glucose diffuses passively through their plasma membrane. In T2DM, the excess of glucose can be metabolized in the sorbitol pathway to sorbitol and fructose by aldose reductase, which activates the aldose reductase secondary metabolic pathway, with concomitant oxidation of NADPH to NADP + and reduction of NAD + to NADH. NADPH depletion and an increased NADH/NAD + cytosolic ratio leads to a change in redox potential that accelerates glycolysis and increases de novo synthesis of DAG [ 242 ]. As a result, protein kinase C (PKC) is activated, nitric oxide (NO) is reduced. These effects cause vascular permeability and increase contractility. Simultaneously, the increased NADH/NAD + ratio also results in higher production of O 2 − , LDL oxidation, cytotoxic effects on endothelial cells and reduced NO availability, leading to endothelial dysfunction [ 241 , 242 ].
The overproduction of aldoses by the sorbitol pathway promotes protein glycosylation that yields the formation of the stable Amadori products (such as glycosylated hemoglobin) and AGEs. AGEs are associated with several molecules that augment oxidant activity and consequently the production of ROS, which increases oxidative stress and prevents the release of NO, resulting in vascular lesions. AGEs may also reduce endothelium-derived NO bioavailability and activity, further compromising vascular activity [ 243 ]. In addition, AGEs can trigger an inflammatory and pro-coagulant state and can cause endothelial activation through the induction of receptor-mediated gene transcription. AGE binding to the RAGE-receptor, nuclear transcription factor NF-κB [ 242 , 243 ] is activated leading to transcription of endothelin-1, VCAM-1, ICAM-1, E-selectin, thrombomodulin, TF, vascular endothelial growth factor (VEGF), IL-1, IL-6, and TNF-α [ 242 , 244 ]. Increased expression of inflammatory and adhesion molecules amplifies the inflammatory response and aggravates diabetic vascular complications. These pro-inflammatory cytokines stimulate the expression and release of pro-coagulant molecules and inhibit the expression of anti-coagulant molecules by endothelial cells [ 245 ]. This leads to a pro-coagulant state in the surface of the endothelium and increases growth factor production resulting in a thickening of the basement membrane, thus favoring protein and lipid deposition and impairing vasodilation [ 242 , 246 ].
6.2.2. Endothelial Dysfunction in T2DM and Atherosclerosis Development
Hyperglycemia-associated vascular injury, oxidative stress, inflammation and altered hemodynamic balance may initiate atherosclerosis development and formation of arterial thrombus [ 247 ]. At early stages of atherosclerosis, circulating LDL binds to matrix proteoglycans where their oxidation is favored, giving rise to highly pro-inflammatory particles that stimulate the expression of several adhesion molecules by endothelial cells [ 242 , 248 ]. This promotes selective binding of leukocytes and their transmigration into the vascular wall along with recruitment and activation of circulating monocytes that differentiate into macrophages. The excess of oxidized LDL is removed by macrophages by a non-regulated mechanism that leads to the formation of foam cells and the onset of fatty streaks. Mononuclear cells release inflammatory cytokines, including IL-1 and IL-6, promoting the recruitment of additional inflammatory cells. As a result, smooth muscle cells proliferate and migrate into the intima where they synthesize and secrete extracellular matrix facilitating fibroatheroma formation [ 242 ]. As the process progresses, if a fissure or ulceration of the plaque occurs, highly thrombogenic substances are exposed leading to adhesion and aggregation of platelets, which promotes thrombus formation [ 249 ]. In addition, platelets can also release pro-inflammatory cytokines and growth factors promoting monocyte recruitment to atherosclerotic plaques, which stimulates fibroblasts and smooth muscle cell proliferation thus accelerating the atherosclerotic process.
6.3. Diabetes-Associated Chronic Inflammation and Atherosclerosis Progression
A critical component of T2DM is a chronic low-grade inflammatory state, referred to as “metaflammation” [ 250 ]. This chronic condition involves the same cellular and molecular players of acute inflammatory responses and has been suggested as an underlying cause of the progression of atherosclerosis in T2DM. Hyperglycaemia can increase circulating cytokines that can lead to chronic inflammation in T2DM [ 250 ]. Among them, patients with T2DM have higher levels of IL-1b, IL-6, IL-8, MCP-1, and other major cytokines in both monocytes and macrophages [ 130 ]. The underlying mechanisms involved in this process are ROS-mediated activation of p38 and other proinflammatory kinases, upregulation of NF-kB induction, oxidative stress, and activation of the AGE-RAGE pathway [ 129 , 130 ]. In addition, exposure to high glucose levels impairs the phagocytic activity of macrophages, which partially explains the increased incidence of chronic infection among T2DM patients [ 251 ]. Indeed, T2DM is associated with increased activity of the inflammasome, upregulation of the nucleotide-binding oligomerization domain-like receptor 3 (NLRP3), increased levels of IL-1β and IL-18 [ 252 , 253 , 254 ]. These events trigger neutrophil extracellular trap activation, or NETosis, a characteristic cell death of macrophages causing chronic inflammation [ 255 ]. High levels of these markers have been found in T2DM patients [ 256 ], which are enhanced in hyperglycaemic conditions [ 257 ].
6.4. Adipokine Balance and CVD Risk
Adipose tissue dysfunction as a result of T2DM can result in an imbalance between pro-inflammatory and anti-inflammatory adipokines, and is one of the mechanisms of T2DM complications. Several studies indicate that adipokines are related to IR, and can result in endothelial dysfunction, and pro-inflammatory and pro-atherogenic states [ 258 , 259 ].
Adiponectin is a well-described insulin-sensitizing hormone and its expression and circulating levels are inversely proportional to the extent of adiposity. Adiponectin has insulin-sensitizing properties [ 260 , 261 ]. Adiponectin acts through ADIPOR1 and ADIPOR2 receptors [ 262 ] and the peroxisome proliferator-activated receptor α (PPARα) pathway, leading to decreased hepatic gluconeogenesis, increased liver and skeletal muscle fatty acid oxidation, increased glucose uptake in skeletal muscle and white adipose tissue, and decreased white adipose tissue inflammation [ 263 ]. In addition, adiponectin ameliorates β-cell death by neutralizing inflammatory and lipotoxic ceramides and DAGs [ 264 ] and shows strong anti-inflammatory effects on other cell types such as macrophages and fibrogenic cells [ 263 , 265 , 266 ]. Low concentrations of adiponectin have been found in T2DM patients and are correlated with increased risk of developing premature arteriosclerosis, and are thus considered an additional CVD risk factor [ 267 ]. Notably, adiponectin deficiency is associated with coronary artery disease, hypertension, endothelial dysfunction and greater carotid intima-media thickness [ 268 , 269 , 270 , 271 ]. Low concentrations of adiponectin lead to an increased expression of intercellular adhesion molecule-1 (ICAM-1), vascular cell adhesion molecule-1 (VCAM-1) and E-selectin, promotes differentiation of macrophages into foam cells and enhances the proliferation and migration of smooth muscle cells [ 272 ].
Omentin is an adipokine secreted from white adipose tissue and is involved in glucose homeostasis [ 273 , 274 ]. Omentin circulates in the blood [ 275 , 276 ], and is associated with reduced levels in T2DM patients [ 277 , 278 ]. In vitro studies have shown that omentin enhances insulin-stimulated glucose uptake in human adipocytes by AKT signaling pathway activation [ 273 ]. In humans, an inverse correlation between omentin levels and IR is seen, both at the protein and mRNA levels [ 277 , 279 , 280 ]. Additional studies show that omentin has anti-inflammatory properties, diminishes cytokine expression [ 281 , 282 ], and is negatively associated with systemic inflammatory markers such as TNF and IL-6 [ 283 ].
Vaspin (visceral adipose tissue-derived serine protease inhibitor) is an adipokine that inhibits proteases responsible for IR and protects against atherosclerosis and plaque development [ 284 , 285 ]. It has been shown that T2DM patients have higher serum vaspin levels than healthy controls. Higher vaspin levels are associated with a 1.7-fold increased risk of CVD [ 70 ]. High vaspin is also associated with increased severity of coronary artery disease [ 286 ].
7. Conclusions
The importance of research in the fields of glucose homeostasis, insulin and diabetes has not faded. In fact, due to rapid globalization and the normalization of a sedentary lifestyle, along with increased obesity, diabetes and their consequent co-morbidities, research in this topic must continue to grow. Understanding the mechanisms implicated in every step in the development and complications of T2DM is crucial in order to prevent, control, treat or revert the pathophysiology of T2DM its complications. Although quality outcomes for patients are optimized by early detection of T2DM through screening and intensive patient-centered management, research efforts are needed to define causative factors accounting for correlations among different demographic subsets and the corresponding variable risks for T2DM as well as the drivers of increased risk in individuals of low socioeconomic status. Being the pathophysiology and underlying mechanisms of T2DM increasingly understood, precision medicine should be implemented and treatments individualized and targeted appropriately with the help of molecular genetic tools by identifying specific variants contributing to disease development as well as by searching biomarkers to assess progression and response to therapeutic interventions. Additional research is needed to determine a direct causal role of the intestinal microbiota in pathogenesis of T2DM and response to therapies needs to be determined.
Taking everything in this review into consideration, it is clear that there is still a long way until we fully understand each of the many stakeholders in glucose homeostasis.
Author Contributions
U.G.-C., A.B.-V., S.J., A.L.-S., H.S., K.B.U., H.O. and C.M. have contributed to the writing of the manuscript. U.G.-G. and C.M. conceptualized the review. A.B.-V. and C.M. drawn the images. H.S. edited language. All authors have read and agreed to the published version of the manuscript.
This work was supported by the Basque Government (Grupos Consolidados IT-1264-19). U.G-G. was supported by Fundación Biofísica Bizkaia. A.B.-V. was supported by Programa de especializaci.n de Personal Investigador Doctor en la UPV/EHU (2019) 2019–2020. S.J. and A.L-S. were supported by a grant PIF (2017–2018) and (2019–2020), Gobierno Vasco, respectively. A.L.-S. was partially supported by Fundación Biofísica Bizkaia.
Conflicts of Interest
The authors declare no conflict of interest.
From Research to Reflection: A Step-by-Step Guide to Writing an Essay on Diabetes

Diabetes is a chronic disease that affects millions of people worldwide. It is characterized by high blood glucose levels, which can lead to various complications if left untreated. One of the most significant complications of diabetes is its impact on cardiovascular health.
The link between diabetes and cardiovascular disease is well-established. People with diabetes are two to four times more likely to develop cardiovascular disease than those without the disease.
The reasons for this are complex, but they include that diabetes can damage blood vessels and nerves throughout the body, including those that supply the heart and brain. This can lead to a range of cardiovascular problems, such as heart attacks, strokes, and peripheral artery disease .
We can guarantee you that most people are not even aware of this much information on diabetes. This is why writing an essay on diabetes makes sense.
What’s more, while writing an essay on diabetes, you make yourself aware of this disease and work towards reflecting on it.
Influence Of Diabetes On The Society
Diabetes can have a significant impact on society in a number of ways.
Here are some examples:
- Healthcare costs: Diabetes is a chronic disease that requires ongoing medical care, including regular check-ups, medications, and in some cases, hospitalization. The cost of treating diabetes can be substantial, both for individuals and for society as a whole. In 2017, the total cost of diabetes in the US was estimated to be $327 billion, including direct medical costs and lost productivity.
- Public health: Diabetes is a major public health issue , with an estimated 463 million adults worldwide living with the disease. Diabetes can lead to various health complications, including heart disease, stroke, kidney disease, and blindness. As a result, diabetes is a leading cause of death and disability worldwide.
- Lifestyle changes: Diabetes is closely linked to lifestyle factors such as diet and physical activity. As a result, efforts to prevent or manage diabetes often involve promoting healthy lifestyle habits such as regular exercise and a balanced diet. These lifestyle changes can have a broader impact on society by promoting overall health and well-being.
- Stigma: Diabetes can be stigmatized, with some people blaming individuals with diabetes for their disease. This can lead to discrimination and social isolation, which can have a negative impact on mental health and well-being.
- Education and awareness: Diabetes education and awareness campaigns can play an important role in reducing the impact of diabetes on society. By promoting an understanding of the disease and its risk factors and encouraging early diagnosis and treatment, these campaigns can help to improve health outcomes and reduce healthcare costs.
Diabetes can significantly impact society, both in terms of healthcare costs and public health outcomes. By promoting education and awareness and encouraging healthy lifestyle habits, we can work to reduce the impact of diabetes on individuals and society as a whole.
Why Such A Subject?
While there are many subjects to write essays on, why write an essay on such a difficult subject? Well, when an educational institution asks you to write an essay, they look at your writing skills and try to figure out your personality along with it.
If you are writing about something that can bring change in society, it can impress them. Writing an essay on diabetes will allow you to stand out from all the other students who have submitted essays on almost the same topic.
Below are a few reasons why writing an essay on diabetes is a good idea.
- To Raise Awareness: Diabetes is a chronic disease that affects millions of people worldwide, yet many people are still unaware of its causes, symptoms, and complications. Writing an essay on diabetes can help raise awareness about the disease, its impact on individuals and communities, and the importance of prevention and management.
- To Educate: Diabetes is a complex disease that requires careful management and monitoring. Writing an essay on diabetes can help educate individuals about the different types of diabetes, risk factors, signs and symptoms, and treatment options.
- To Promote Research: There is ongoing research on diabetes, including new treatments and management strategies. Writing an essay on diabetes can help promote research by highlighting the importance of funding and supporting research efforts.
- To Advocate For Change: Writing an essay on diabetes can help advocate for policy changes that improve access to diabetes care, support for those with diabetes, and prevention efforts.
- To Demonstrate Understanding: Writing an essay on diabetes can be an opportunity to demonstrate an understanding of the disease and its impact on individuals and communities. It can also showcase critical thinking skills and research abilities.
Writing an essay on diabetes can help raise awareness, educate, promote research, advocate for change, and demonstrate an understanding of the disease. It can be an important way to promote public health and improve the lives of individuals with diabetes.
A Step-by-Step Guide To Writing An Essay On Diabetes
Writing an essay on diabetes requires thorough research and reflection. You can’t just proceed with a diabetes essay like any normal essay topic. When writing an essay on diabetes, you can’t get wrong with your facts and information. One mistake in your information can affect your whole efforts.
When you are doing research for your essay, ensure that you are picking information from credible resources.
Follow the steps below to write a high-quality essay.
Step 1: Choose A Specific Topic
The topic of diabetes is vast, so it is essential to narrow it down to a specific area you can thoroughly explore in your essay. Consider the audience, the essay’s purpose, and the assignment’s scope. For instance, you could focus on the causes of diabetes, the different types of diabetes, the impact of diabetes on a particular population, or the latest treatment options for diabetes.
Step 2: Conduct Research
Once you have a specific topic, conduct thorough research to gather relevant information from credible sources such as academic journals, government publications, and reputable websites. Take notes on key points, statistics, and quotes that you can use to support your arguments.
Step 3: Develop A Thesis Statement
Based on your research, develop a clear and concise thesis statement that summarizes the main argument of your essay. Your thesis statement should be debatable and provide a roadmap for the rest of your essay.
Step 4: Create An Outline
Use your research and thesis statement to create an outline for your essay. Organize your ideas into logical sections and subsections, and ensure each point supports your thesis statement.
Step 5: Write The Essay
Using your outline as a guide, write your essay. Start with an introduction that provides background information and a clear thesis statement. Use the body paragraphs to present your arguments and support them with evidence from your research. End with a conclusion that restates your thesis and summarizes your main points.
Step 6: Edit And Proofread
After you have written your essay, edit and proofread it carefully to ensure it is clear, concise, and error-free. Check for spelling and grammatical errors, and ensure your ideas flow logically.
Step 7: Reflect On Your Essay
Finally, take some time to reflect on your essay. Consider the strengths and weaknesses of your argument, and think about what you could have done differently. This reflection can help you improve your writing skills and prepare for future assignments.
By following this step-by-step guide, you can write a well-researched and thoughtful essay on diabetes. Remember to choose a specific topic, conduct thorough research, develop a clear thesis statement, create an outline, write the essay, edit and proofread, and reflect on your work.
However, if you find it difficult to write an essay on diabetes, but the opportunity is too good to miss, ask a professional to ‘ write my essay for me ’.
Things To Consider!
Define your purpose.
Before you start writing, it’s important to clarify why you’re writing about diabetes.
Are you trying to educate readers about the disease? Discuss a specific aspect of diabetes research or treatment. Argue for a particular approach to diabetes prevention or management.
Defining your purpose can help guide your writing and ensure that you stay focused on your main goals.
Know Your Audience
Who will be reading your essay? Are they experts in diabetes, or are they general readers who may not be familiar with the disease? Understanding your audience can help you tailor your writing style and language to make your essay as accessible and engaging as possible.
Research Thoroughly
Diabetes is a complex and multi-faceted disease, so it’s important to do your research to ensure you comprehensively understand the topic. Find reputable sources, such as peer-reviewed journals, government websites, or expert organizations like the American Diabetes Association.
Consider Multiple Perspectives
There are many different viewpoints on diabetes, from healthcare providers to patients to public health advocates. When writing your essay, consider different perspectives and present a balanced view of the topic.
Use Clear, Concise Language
Diabetes is a technical topic with many medical terms and concepts that may be unfamiliar to some readers. To make your essay as accessible as possible, try to use clear, concise language that is easy to understand. Use layman’s terms when appropriate, and define any technical terms you use.
Use Examples And Anecdotes
Diabetes can be a dry and technical topic, so using examples and anecdotes can help to bring your writing to life and make it more engaging for readers. Consider including real-life stories of people with diabetes or describing specific research studies or medical interventions in detail.
Edit And Proofread Carefully
Finally, edit and proofread your essay carefully before submitting it. Look for spelling and grammar errors and any unclear or confusing language. Consider having someone else read your essay to get a fresh perspective and catch any mistakes you may have missed.
Related posts

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Diabetes articles from across Nature Portfolio
Diabetes describes a group of metabolic diseases characterized by high blood sugar levels. Diabetes can be caused by the pancreas not producing insulin (type 1 diabetes) or by insulin resistance (cells do not respond to insulin; type 2 diabetes).
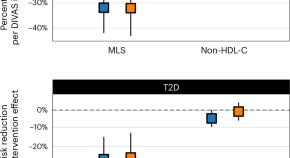
Blood lipid profiling indicates that dietary fat quality is associated with cardiometabolic risk
Dietary guidelines advise substituting saturated fats with unsaturated fats. We used detailed blood fat composition profiling in diet trials and population studies to confirm that a moderate high-fat diet from plant oils is better for metabolism and heart health than a diet with similar fat levels from animal sources.
New insights into the regulation of GIPR signalling
Two recent studies have unravelled novel modes of glucose-dependent insulinotropic polypeptide receptor (GIPR) signalling regulation. Kizilkaya et al. characterized the effect of changes in β-arrestin 2 coupling with naturally occurring GIPR coding variants, whereas Regmi et al. investigated GIPR expression profiles and functional regulation in adipocytes.
- Yusman Manchanda
- Alejandra Tomas

Insights into optimal BMI from the GlasVEGAS study
A human experiment confirms the higher susceptibility of South Asians to adverse metabolic consequences with weight gain compared with white Europeans, which is attributed to underlying differences in muscle and adipose biology.
- Chun-Kwan O
- Juliana C. N. Chan
Related Subjects
- Diabetes complications
- Diabetes insipidus
- Gestational diabetes
- Type 1 diabetes
- Type 2 diabetes
Latest Research and Reviews
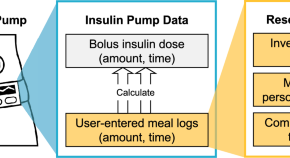
Mealtime prediction using wearable insulin pump data to support diabetes management
- Temiloluwa Prioleau

Transcutaneous vagus nerve stimulation has no anti-inflammatory effect in diabetes
- Tina Okdahl
- Huda Kufaishi
- Christina Brock

Plasma proteomics in children with new-onset type 1 diabetes identifies new potential biomarkers of partial remission
- Olivier G. Pollé
- Sébastien Pyr dit Ruys
- Philippe A. Lysy
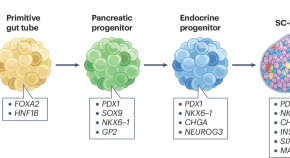
Harnessing cellular therapeutics for type 1 diabetes mellitus: progress, challenges, and the road ahead
Type 1 diabetes mellitus affects 8.5 million people globally and is characterized by autoimmune destruction of pancreatic β cells. This Review discusses cell replacement therapies for T1DM and outlines the challenges and future directions
- Alessandro Grattoni
- Gregory Korbutt
- Paul de Vos
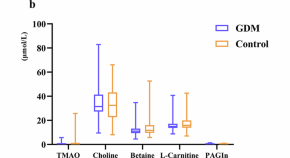
Association of maternal gut microbial metabolites with gestational diabetes mellitus: evidence from an original case-control study, meta-analysis, and Mendelian randomization
- Mengxin Yao
- Xiaoyan Zhu
Finerenone in Heart Failure and Chronic Kidney Disease with Type 2 Diabetes: the FINE-HEART pooled analysis of cardiovascular, kidney, and mortality outcomes
This participant-level pooled analysis of the three phase III trials that have tested the non-steroidal mineralocorticoid receptor antagonist finerenone in patients with heart failure and chronic kidney disease with type 2 diabetes provides an integrated view of the mortality, cardiovascular and renal effects of this treatment. Editor recognition statement: Primary Handling editor: Michael Basson, in collaboration with the Nature Medicine team.
- Muthiah Vaduganathan
- Gerasimos Filippatos
- Scott D. Solomon
News and Comment

Prenatal exposure to famine affects lifelong health
Analysis of data related to the Ukraine famine of 1932–1933 shows that in utero exposure to famine increases the risk of adult type 2 diabetes by more than twofold.
- Karen O’Leary
GLP1 agonists: current and future landscape of clinical trials for patients with metabolic dysfunction
Guidelines currently recommend organ-specific management of obesity-related complications. Agents that agonize glucagon-like peptide 1 receptors, including those that co-agonize other anorexigenic hormone receptors, lead to substantial weight loss and benefits in people with varying obesity-related complications, with further trials underway. These medications enable cause-specific management of obesity complications.
- Jonathan Goldney
- Melanie J. Davies

How rival weight-loss drugs fare at treating obesity, diabetes and more
Wegovy, Zepbound and similar medications all lead to metabolic improvements, but scientists are starting to unpick the differences between them.
- Mariana Lenharo
The promising potential of gene therapy for diabetes mellitus
Gene therapy holds tremendous promise for treating a wide range of hereditary and acquired diseases by delivering exogenous therapeutic nucleotide sequences into specific cells or tissues. Recent advances support the notion that gene therapy could offer a long-term cure for diabetes mellitus, something that current conventional pharmacotherapies cannot achieve.
- Stefan R. Bornstein
- J. Fraser Wright
- Charlotte Steenblock
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Home / Essay Samples / Health / Illness / Diabetes
Diabetes Essay Examples
Personalized prevention and management of diabetes.
Diabetes is a rising global burden. This noncommunicable disease is a major global public health priority that is placing untenable demands on individuals, their careers, society, and their health system as a whole. This is informative speech outline diabetes disease in which the topic is...
Diabetes: Medical Definition of Disease
Out of the most common diseases in the world that affects people of all ages is diabetes. Many factors can contribute to different people suffering from diabetes, some of them include the lifestyles people to adapt, genetic inheritance, and ethnicity among other reasons. It is...
The Effects of Vitamin D on Type One Diabetes
Type One Diabetes is a disease that affects people of all ages all across the world. Type One Diabetes is a disease that makes one’s pancreas stop working permanently. I have seen it first hand, my younger brother was diagnosed around 6 years ago on...
The Link Between Vitamin a Deficiency and Diabetes Mellitus
Vitamin A is a complex alcohol and is represented by retinol. Its oxidative products retinaldehyde (also called retinal as well as retinene) is also a biologically active compound. Vitamin A is quite heat stable, but it is destroyed at high temperatures in the presence of...
Diabetes Melitus and Its Prevalence in the Philippines
Diabetes is a disease that has reached epidemic proportions over the years. It is caused by the increase of sugar in the bloodstream (hyperglycaemia) due to the pancreas’ failure to produce enough insulin to level it out. It can be classified into three (3) main...
The Connection Between Type 2 Diabetes and Parasitic Infections
Parasitosis affects a huge number of the world population. Both urogenital and IPIs are linked to increasing morbidity, mortality, and serious outcomes. Intestinal parasitosis greatly affects body metabolism, nutrition absorption and gut ecosystem. A complex relationship exists between parasitosis and T2DM. The mechanisms of both...
Type 2 Diabetes Mellitus and the Patient Journey: Case Analysis
Mr Joe Bloggs (The patient will be referred to as ‘Joe Bloggs’ throughout this essay, this is a pseudonym. The clinical area will also not be identified in order to respect confidentiality) is a 56-year-old man with poorly controlled type 2 diabetes mellitus. He presented...
Salt Increases the Risk of Diabetes
Salt isn't just a risk factor for diabetes. It can also weaken the heart and irritate the kidneys, favor high blood pressure and promote obesity. Salt is a kind of flavor enhancer. Without salt, many people would not eat half as much. Today hardly anyone...
Nanobots for Glucose Level Monitoring
Diabetes is one of the deadliest disease of the century. Diabetes is a major cause of blindness, kidney failure, heart attacks, stroke and lower limb amputation. The number of people with diabetes has risen from 108 million in 1980 to 422 million in 2014. Tedious...
A Report on Glucose Sensors Devices
Glucose monitoring is a technology that has been used to monitor diabetes for the last thirty years. There has been evolution of glucose, started with glucose measuring methods that used enzymes to determine the content. Nowadays there is plenty of glucose monitoring devices that give...
Trying to find an excellent essay sample but no results?
Don’t waste your time and get a professional writer to help!
You may also like
- Gambling Addiction
- Underage Drinking
- Assisted Suicide
- Physical Exercise
- Neuroplasticity
- Cystic Fibrosis Essays
- Allergy Essays
- Obesity Essays
- Polio Essays
- Hypertension Essays
- Diabetes Mellitus Essays
- Childhood Obesity Essays
- Drunk Driving Essays
- Abortion Essays
About Diabetes
Diabetes is a chronic, metabolic disease characterized by elevated levels of blood glucose (or blood sugar), which leads over time to serious damage to the heart, blood vessels, eyes, kidneys and nerves.
Symptoms the need to urinate often, thirst, constant hunger, weight loss, vision changes and fatigue. These symptoms may occur suddenly.
Type 1 diabetes, Type 2 diabetes, and Gestational diabetes.
Family history, race or ethnicity, obesity, lack of exercise,high blood pressure, genetics, air pollution,polycystic ovary syndrome etc.
About 90-95 percent of people with diabetes have Type 2, while about 5 percent have Type 1, and the remainder have gestational diabetes. It is the number 7 cause of death in the United States. More than 37 million people in the United States have diabetes, and 1 in 5 of them don’t know they have it. In the last 20 years, the number of adults diagnosed with diabetes has more than doubled.
samplius.com uses cookies to offer you the best service possible.By continuing we’ll assume you board with our cookie policy .--> -->