

Introduction to qualitative nursing research
This type of research can reveal important information that quantitative research can’t.
- Qualitative research is valuable because it approaches a phenomenon, such as a clinical problem, about which little is known by trying to understand its many facets.
- Most qualitative research is emergent, holistic, detailed, and uses many strategies to collect data.
- Qualitative research generates evidence and helps nurses determine patient preferences.
Research 101: Descriptive statistics
Differentiating research, evidence-based practice, and quality improvement
How to appraise quantitative research articles
All nurses are expected to understand and apply evidence to their professional practice. Some of the evidence should be in the form of research, which fills gaps in knowledge, developing and expanding on current understanding. Both quantitative and qualitative research methods inform nursing practice, but quantitative research tends to be more emphasized. In addition, many nurses don’t feel comfortable conducting or evaluating qualitative research. But once you understand qualitative research, you can more easily apply it to your nursing practice.
What is qualitative research?
Defining qualitative research can be challenging. In fact, some authors suggest that providing a simple definition is contrary to the method’s philosophy. Qualitative research approaches a phenomenon, such as a clinical problem, from a place of unknowing and attempts to understand its many facets. This makes qualitative research particularly useful when little is known about a phenomenon because the research helps identify key concepts and constructs. Qualitative research sets the foundation for future quantitative or qualitative research. Qualitative research also can stand alone without quantitative research.
Although qualitative research is diverse, certain characteristics—holism, subjectivity, intersubjectivity, and situated contexts—guide its methodology. This type of research stresses the importance of studying each individual as a holistic system (holism) influenced by surroundings (situated contexts); each person develops his or her own subjective world (subjectivity) that’s influenced by interactions with others (intersubjectivity) and surroundings (situated contexts). Think of it this way: Each person experiences and interprets the world differently based on many factors, including his or her history and interactions. The truth is a composite of realities.
Qualitative research designs
Because qualitative research explores diverse topics and examines phenomena where little is known, designs and methodologies vary. Despite this variation, most qualitative research designs are emergent and holistic. In addition, they require merging data collection strategies and an intensely involved researcher. (See Research design characteristics .)
Although qualitative research designs are emergent, advanced planning and careful consideration should include identifying a phenomenon of interest, selecting a research design, indicating broad data collection strategies and opportunities to enhance study quality, and considering and/or setting aside (bracketing) personal biases, views, and assumptions.
Many qualitative research designs are used in nursing. Most originated in other disciplines, while some claim no link to a particular disciplinary tradition. Designs that aren’t linked to a discipline, such as descriptive designs, may borrow techniques from other methodologies; some authors don’t consider them to be rigorous (high-quality and trustworthy). (See Common qualitative research designs .)
Sampling approaches
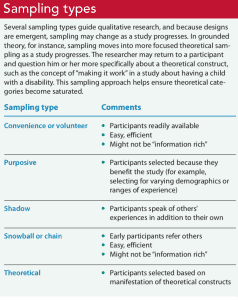
Sampling approaches depend on the qualitative research design selected. However, in general, qualitative samples are small, nonrandom, emergently selected, and intensely studied. Qualitative research sampling is concerned with accurately representing and discovering meaning in experience, rather than generalizability. For this reason, researchers tend to look for participants or informants who are considered “information rich” because they maximize understanding by representing varying demographics and/or ranges of experiences. As a study progresses, researchers look for participants who confirm, challenge, modify, or enrich understanding of the phenomenon of interest. Many authors argue that the concepts and constructs discovered in qualitative research transcend a particular study, however, and find applicability to others. For example, consider a qualitative study about the lived experience of minority nursing faculty and the incivility they endure. The concepts learned in this study may transcend nursing or minority faculty members and also apply to other populations, such as foreign-born students, nurses, or faculty.
Qualitative nursing research can take many forms. The design you choose will depend on the question you’re trying to answer.
| Action research | Education | Conducted by and for those taking action to improve or refine actions | What happens to the quality of nursing practice when we implement a peer-mentoring system? |
| Case study | Many | In-depth analysis of an entity or group of entities (case) | How is patient autonomy promoted by a unit? |
| Descriptive | N/A | Content analysis of data | |
| Discourse analysis | Many | In-depth analysis of written, vocal, or sign language | What discourses are used in nursing practice and how do they shape practice? |
| Ethnography | Anthropology | In-depth analysis of a culture | How does Filipino culture influence childbirth experiences? |
| Ethology | Psychology | Biology of human behavior and events | What are the immediate underlying psychological and environmental causes of incivility in nursing? |
| Grounded theory | Sociology | Social processes within a social setting | How does the basic social process of role transition happen within the context of advanced practice nursing transitions? |
| Historical research | History | Past behaviors, events, conditions | When did nurses become researchers? |
| Narrative inquiry | Many | Story as the object of inquiry | How does one live with a diagnosis of scleroderma? |
| Phenomenology | Philosophy Psychology | Lived experiences | What is the lived experience of nurses who were admitted as patients on their home practice unit? |
A sample size is estimated before a qualitative study begins, but the final sample size depends on the study scope, data quality, sensitivity of the research topic or phenomenon of interest, and researchers’ skills. For example, a study with a narrow scope, skilled researchers, and a nonsensitive topic likely will require a smaller sample. Data saturation frequently is a key consideration in final sample size. When no new insights or information are obtained, data saturation is attained and sampling stops, although researchers may analyze one or two more cases to be certain. (See Sampling types .)
Some controversy exists around the concept of saturation in qualitative nursing research. Thorne argues that saturation is a concept appropriate for grounded theory studies and not other study types. She suggests that “information power” is perhaps more appropriate terminology for qualitative nursing research sampling and sample size.
Data collection and analysis
Researchers are guided by their study design when choosing data collection and analysis methods. Common types of data collection include interviews (unstructured, semistructured, focus groups); observations of people, environments, or contexts; documents; records; artifacts; photographs; or journals. When collecting data, researchers must be mindful of gaining participant trust while also guarding against too much emotional involvement, ensuring comprehensive data collection and analysis, conducting appropriate data management, and engaging in reflexivity.
Data usually are recorded in detailed notes, memos, and audio or visual recordings, which frequently are transcribed verbatim and analyzed manually or using software programs, such as ATLAS.ti, HyperRESEARCH, MAXQDA, or NVivo. Analyzing qualitative data is complex work. Researchers act as reductionists, distilling enormous amounts of data into concise yet rich and valuable knowledge. They code or identify themes, translating abstract ideas into meaningful information. The good news is that qualitative research typically is easy to understand because it’s reported in stories told in everyday language.
Evaluating a qualitative study
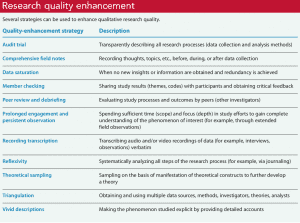
Evaluating qualitative research studies can be challenging. Many terms—rigor, validity, integrity, and trustworthiness—can describe study quality, but in the end you want to know whether the study’s findings accurately and comprehensively represent the phenomenon of interest. Many researchers identify a quality framework when discussing quality-enhancement strategies. Example frameworks include:
- Trustworthiness criteria framework, which enhances credibility, dependability, confirmability, transferability, and authenticity
- Validity in qualitative research framework, which enhances credibility, authenticity, criticality, integrity, explicitness, vividness, creativity, thoroughness, congruence, and sensitivity.
With all frameworks, many strategies can be used to help meet identified criteria and enhance quality. (See Research quality enhancement ). And considering the study as a whole is important to evaluating its quality and rigor. For example, when looking for evidence of rigor, look for a clear and concise report title that describes the research topic and design and an abstract that summarizes key points (background, purpose, methods, results, conclusions).
Application to nursing practice
Qualitative research not only generates evidence but also can help nurses determine patient preferences. Without qualitative research, we can’t truly understand others, including their interpretations, meanings, needs, and wants. Qualitative research isn’t generalizable in the traditional sense, but it helps nurses open their minds to others’ experiences. For example, nurses can protect patient autonomy by understanding them and not reducing them to universal protocols or plans. As Munhall states, “Each person we encounter help[s] us discover what is best for [him or her]. The other person, not us, is truly the expert knower of [him- or herself].” Qualitative nursing research helps us understand the complexity and many facets of a problem and gives us insights as we encourage others’ voices and searches for meaning.
When paired with clinical judgment and other evidence, qualitative research helps us implement evidence-based practice successfully. For example, a phenomenological inquiry into the lived experience of disaster workers might help expose strengths and weaknesses of individuals, populations, and systems, providing areas of focused intervention. Or a phenomenological study of the lived experience of critical-care patients might expose factors (such dark rooms or no visible clocks) that contribute to delirium.
Successful implementation
Qualitative nursing research guides understanding in practice and sets the foundation for future quantitative and qualitative research. Knowing how to conduct and evaluate qualitative research can help nurses implement evidence-based practice successfully.
When evaluating a qualitative study, you should consider it as a whole. The following questions to consider when examining study quality and evidence of rigor are adapted from the Standards for Reporting Qualitative Research.
| o What is the report title and composition of the abstract? o What is the problem and/or phenomenon of interest and study significance? o What is the purpose of the study and/or research question? | → Clear and concise report title describes the research topic and design (e.g., grounded theory) or data collection methods (e.g., interviews) → Abstract summarizes key points including background, purpose, methods, results, and conclusions → Problem and/or phenomenon of interest and significance is identified and well described, with a thorough review of relevant theories and/or other research → Study purpose and/or research question is identified and appropriate to the problem and/or phenomenon of interest and significance |
| o What design and/or research paradigm was used? o Is there evidence of researcher reflexivity? o What is the setting and context for the study? o What is the sampling approach? How and why were data selected? Why was sampling stopped? o Was institutional review board (IRB) approval obtained and were other issues relating to protection of human subjects outlined? | → Design (e.g., phenomenology, ethnography), research paradigm (e.g., constructivist), and guiding theory or model, as appropriate, are identified, along with well-described rationales → Design is appropriate to research problem and/or phenomenon of interest → Researcher characteristics that may influence the study are identified and well described, as well as methods to protect against these influences (e.g., journaling, bracketing) → Settings, sites, and contexts are identified and well described, along with well-described rationales |
| o What data collection and analysis instruments and/or technologies were used? o What is the method for data processing and analysis? o What is the composition of the data? o What strategies were used to enhance quality and trustworthiness? | → Sampling approach and how and why data were selected are identified and well described, along with well-described rationales; participant inclusion and exclusion criteria are outlined and appropriate → Criteria for deciding when sampling stops is outlined (e.g., saturation) and rationale is provided and appropriate → Documentation of IRB approval or explanation of lack thereof provided; consent, confidentiality, data security, and other protection of human subject issues are well described and thorough → Description of instruments (e.g., interview scripts, observation logs) and technologies (e.g., audio-recorders) used is provided, including how instruments were developed; description of if and how these changed during the study is given, along with well-described rationales → Types of data collected, details of data collection, analysis, and other processing procedures are well described and thorough, along with well-described rationales → Number and characteristics of participants and/or other data are described and appropriate → Strategies to enhance quality and trustworthiness (e.g., member checking) are identified, comprehensive, and appropriate, along with well-described rationales; trustworthiness framework, if identified, is established from experts (e.g., Lincoln and Guba, Whittemore et al.) and strategies are appropriate to this framework |
| o Were main study results synthesized and interpreted? If applicable, were they developed into a theory or integrated with prior research? o Were results linked to empirical data? | → Main results (e.g., themes) are presented and well described and a theory or model is developed and described, if applicable; results are integrated with prior research → Adequate evidence (e.g., direct quotes from interviews, field notes) is provided to support main study results |
| o Are study results described in relation to prior work? o Are study implications, applicability, and contributions to nursing identified? o Are study limitations outlined? | → Concise summary of main results are provided and thorough, including relation to prior works (e.g., connection, support, elaboration, challenging prior conclusions) → Thorough discussion of study implications, applicability, and unique contributions to nursing is provided → Study limitations are described thoroughly and future improvements and/or research topics are suggested |
| o Are potential or perceived conflicts of interest identified and how were these managed? o If applicable, what sources of funding or other support did the study receive? | → All potential or perceived conflicts of interest are identified and well described; methods to manage potential or perceived conflicts of interest are identified and appear to protect study integrity → All sources of funding and other support are identified and well described, along with the roles the funders and support played in study efforts; they do not appear to interfere with study integrity |
Jennifer Chicca is a PhD candidate at the Indiana University of Pennsylvania in Indiana, Pennsylvania, and a part-time faculty member at the University of North Carolina Wilmington.
Amankwaa L. Creating protocols for trustworthiness in qualitative research. J Cult Divers. 2016;23(3):121-7.
Cuthbert CA, Moules N. The application of qualitative research findings to oncology nursing practice. Oncol Nurs Forum . 2014;41(6):683-5.
Guba E, Lincoln Y. Competing paradigms in qualitative research . In: Denzin NK, Lincoln YS, eds. Handbook of Qualitative Research. Thousand Oaks, CA: SAGE Publications, Inc.;1994: 105-17.
Lincoln YS, Guba EG. Naturalistic Inquiry . Thousand Oaks, CA: SAGE Publications, Inc.; 1985.
Munhall PL. Nursing Research: A Qualitative Perspective . 5th ed. Sudbury, MA: Jones & Bartlett Learning; 2012.
Nicholls D. Qualitative research. Part 1: Philosophies. Int J Ther Rehabil . 2017;24(1):26-33.
Nicholls D. Qualitative research. Part 2: Methodology. Int J Ther Rehabil . 2017;24(2):71-7.
Nicholls D. Qualitative research. Part 3: Methods. Int J Ther Rehabil . 2017;24(3):114-21.
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: A synthesis of recommendations. Acad Med . 2014;89(9):1245-51.
Polit DF, Beck CT. Nursing Research: Generating and Assessing Evidence for Nursing Practice . 10th ed. Philadelphia, PA: Wolters Kluwer; 2017.
Thorne S. Saturation in qualitative nursing studies: Untangling the misleading message around saturation in qualitative nursing studies. Nurse Auth Ed. 2020;30(1):5. naepub.com/reporting-research/2020-30-1-5
Whittemore R, Chase SK, Mandle CL. Validity in qualitative research. Qual Health Res . 2001;11(4):522-37.
Williams B. Understanding qualitative research. Am Nurse Today . 2015;10(7):40-2.

NurseLine Newsletter
- First Name *
- Last Name *
- Hidden Referrer
*By submitting your e-mail, you are opting in to receiving information from Healthcom Media and Affiliates. The details, including your email address/mobile number, may be used to keep you informed about future products and services.
Test Your Knowledge
Recent posts.

Emotional intelligence: A neglected nursing competency

Hypnosis and pain

Measuring nurses’ health

From Retirement to Preferment: Crafting Your Next Chapter

Leadership in changing times
Promoting health literacy

Mentorship: A strategy for nursing retention

States Set Minimum Staffing Levels for Nursing Homes. Residents Suffer When Rules Are Ignored or Waived
Anatomy of Writing for Publication for Nurses: The writing guide you’ve been looking for

Nurse leadership: Pitfalls and solutions

Home health nursing

Navigating the crossroads of nursing faculty practice

Does money matter?

It’s time embrace AI in nursing
CMS establishes minimum LTC staffing standards
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals
You are here
- Volume 15, Issue 1
- Qualitative data analysis
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Correspondence to Kate Seers RCN Research Institute, School of Health & Social Studies, University of Warwick, Coventry, CV4 7AL, Warwick, UK; kate.seers{at}warwick.ac.uk
https://doi.org/10.1136/ebnurs.2011.100352
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Good qualitative research uses a systematic and rigorous approach that aims to answer questions concerned with what something is like (such as a patient experience), what people think or feel about something that has happened, and it may address why something has happened as it has. Qualitative data often takes the form of words or text and can include images.
Qualitative research covers a very broad range of philosophical underpinnings and methodological approaches. Each has its own particular way of approaching all stages of the research process, including analysis, and has its own terms and techniques, but there are some common threads that run across most of these approaches. This Research Made Simple piece will focus on some of these common threads in the analysis of qualitative research.
So you have collected all your qualitative data – you may have a pile of interview transcripts, field-notes, documents and notes from observation. The process of analysis is described by Richards and Morse 1 as one of transformation and interpretation.
It is easy to be overwhelmed by the volume of data – novice qualitative researchers are sometimes told not to worry and the themes will emerge from the data. This suggests some sort of epiphany, (which is how it happens sometimes!) but generally it comes from detailed work and reflection on the data and what it is telling you. There is sometimes a fine line between being immersed in the data and drowning in it!
A first step is to sort and organise the data, by coding it in some way. For example, you could read through a transcript, and identify that in one paragraph a patient is talking about two things; first is fear of surgery and second is fear of unrelieved pain. The codes for this paragraph could be ‘fear of surgery’ and ‘fear of pain’. In other areas of the transcript fear may arise again, and perhaps these codes will be merged into a category titled ‘fear’. Other concerns may emerge in this and other transcripts and perhaps best be represented by the theme ‘lack of control’. Themes are thus more abstract concepts, reflecting your interpretation of patterns across your data. So from codes, categories can be formed, and from categories, more encompassing themes are developed to describe the data in a form which summarises it, yet retains the richness, depth and context of the original data. Using quotations to illustrate categories and themes helps keep the analysis firmly grounded in the data. You need to constantly ask yourself ‘what is happening here?’ as you code and move from codes, to categories and themes, making sure you have data to support your decisions. Analysis inevitably involves subjective choices, and it is important to document what you have done and why, so a clear audit trail is provided. The coding example above describes codes inductively coming from the data. Some researchers may use a coding framework derived from, for example, the literature, their research questions or interview prompts, (Ritchie and Spencer 2 ) or a combination of both approaches.
Qualitative data, such as transcripts from an interview, are often routed in the interaction between the participant and the researcher. Reflecting on how you, as a researcher, may have influenced both the data collected and the analysis is an important part of the analysis.
As well as keeping your brain very much in gear, you need to be really organised. You may use highlighting pens and paper to keep track of your analysis, or use qualitative software to manage your data (such as NVivio or Atlas Ti). These programmes help you organise your data – you still have to do all the hard work to analyse it! Whatever you choose, it is important that you can trace your data back from themes to categories to codes. There is nothing more frustrating than looking for that illustrative patient quote, and not being able to find it.
If your qualitative data are part of a mixed methods study, (has both quantitative and qualitative data) careful thought has to be given to how you will analyse and present findings. Refer to O’Caithain et al 3 for more details.
There are many books and papers on qualitative analysis, a very few of which are listed below. 4 , – , 6 Working with someone with qualitative expertise is also invaluable, as you can read about it, but doing it really brings it alive.
- Richards L ,
- Ritchie J ,
- O'Cathain ,
- Bradley EH ,
- Huberman AM
Competing interests None.
Read the full text or download the PDF:

Nursing Research Guide
- General Search Strategies
- Searching by Author & Theory
- Searching for Qualitative Studies
- Searching for Systematic Reviews & Controlled Trials
- Health Data & Statistics
- Tutorials & Help
- SoN and APA (7th Ed.)
- NSC 890: PICOT Searches
What is qualitative research?
Qualitative research in Nursing approaches a clinical question from a place of unknowing in an attempt to understand the complexity, depth, and richness of a particular situation from the perspective of the person or persons impacted by the situation (i.e., the subjects of the study).
Study subjects may include the patient(s), the patient's caregivers, the patient's family members, etc. Qualitative research may also include information gleaned from the investigator's or researcher's observations.
While typically more subjective than quantitative research (which focuses on measurements and numbers), qualitative research still employs a systematic approach.
Qualitative research is generally preferred over quantitative research (which on measurements and numbers) when the clinical question centers around life experiences or meaning.
Adapted from:
- Wilson, B., Austria, M.J., & Casucci, T. (2021 March 21). Understanding Quantitative and Qualitative Approaches
- Chicca, J. (2020 June 5). Introduction to qualitative nursing research. American Nurse Journal.
Where can I find qualitative research?
Qualitative research can be found in numerous databases. Some good starting options are:
- CINAHL Ultimate Journal articles and eBooks in nursing and allied health.
- MEDLINE (EBSCOhost Web) Journal articles in medicine, life sciences, health care, and biomedical research.
- APA PsycINFO Articles from journals, newspapers, and magazines, along with eBooks in nearly every social science subject area.
- PubMed Citation search of journal articles and books in health and life sciences.
How can I find qualitative research?
Cinahl and/or medline.
- Start at the Advanced Search screen.
- Add a search term that represents the topic you are interested in into one (or more) of the search boxes.
- Scroll down until you see the Limit your results section.
- Qualitative - High Sensitivity (broadest category/broad search)
- Qualitative - High Specificity (narrowest category/specific search)
- Qualitative - Best Balance (somewhere in between)
- Select or click the search button.

APA PsycINFO
- Start at the Advanced Search screen.
- Use the Methodology menu to select Qualitative .

- Use the drop-down menu next the Enter search term box to set the search to MeSH Terms
- Qualitative Research
- Nursing Methodology Research

How can I use keywords to search for qualitative research?
Try adding adding a keyword that might specifically identify qualitative research. You could add the term qualitative to your search and/or your could add different types of qualitative research according to your specific needs and/or research assignment.
For example, consider the following types of qualitative research in light of the types of questions a researcher might be trying to answer with each qualitative research type:
- Clinical question: What happens to the quality of nursing practice when we implement a peer-mentoring system?
- Clinical question: How is patient autonomy promoted by a unit?
- Clinical question: What is the nursing role in end-of-life decisions?
- Clinical question: What discourses are used in nursing practice and how do they shape practice?
- Clinical question: How does Filipino culture influence childbirth experiences?
- Clinical question: What are the immediate underlying psychological and environmental causes of incivility in nursing?
- Clinical question: How does the basic social process of role transition happen within the context of advanced practice nursing transitions?
- Clinical question: When and why did nurses become researchers?
- Clinical question: How does one live with a diagnosis of scleroderma?
- Clinical question: What is the lived experience of nurses who were admitted as patients on their home practice units?
Adapted from: Chicca, J. (2020 June 5). Introduction to qualitative nursing research . American Nurse Journal.
Need more help?
Finding relevant qualitative research can be both difficult and time consuming. Once you conduct a search, you will need to review your search results and look at individual articles, their subject terms, and abstracts to determine if they are truly qualitative research articles. And that's a determination that only you can make.
If you still need help after trying the search strategies and tips suggested on this research guide, we encourage you to schedule an in-person or Zoom research appointment . Health Services librarian Rachel Riffe-Albright is a great bet, but any librarian would be happy to help!
Additonal resources on qualitative research
The following are research guides created by other academic libraries. While you likely will not have access to any of their linked resources, the tips and tricks shared may be useful to you as you search for qualitative research:
- What is Qualitative Research? from UTA Libraries at University of Texas Arlington
- Finding Qualitative Research Articles from Ashland University Library
- Finding Qualitative Research Articles from the Health Sciences Library at University of Washington
- Advanced Search Guide: Qualitative and Quantitative Studies from Southern Connecticut State University Library
- Finding Qualitative and Quantitative Studies in CINAHL from Southern Connecticut State University Library
- << Previous: Searching by Author & Theory
- Next: Searching for Systematic Reviews & Controlled Trials >>
- Last Updated: Apr 22, 2024 2:39 PM
- URL: https://libguides.eku.edu/nursing
EO/AA Statement | Privacy Statement | 103 Libraries Complex Crabbe Library Richmond, KY 40475 | (859) 622-1790 ©
- Research article
- Open access
- Published: 09 November 2005
A qualitative study of nursing student experiences of clinical practice
- Farkhondeh Sharif 1 &
- Sara Masoumi 2
BMC Nursing volume 4 , Article number: 6 ( 2005 ) Cite this article
362k Accesses
169 Citations
9 Altmetric
Metrics details
Nursing student's experiences of their clinical practice provide greater insight to develop an effective clinical teaching strategy in nursing education. The main objective of this study was to investigate student nurses' experience about their clinical practice.
Focus groups were used to obtain students' opinion and experiences about their clinical practice. 90 baccalaureate nursing students at Shiraz University of Medical Sciences (Faculty of Nursing and Midwifery) were selected randomly from two hundred students and were arranged in 9 groups of ten students. To analyze the data the method used to code and categories focus group data were adapted from approaches to qualitative data analysis.
Four themes emerged from the focus group data. From the students' point of view," initial clinical anxiety", "theory-practice gap"," clinical supervision", professional role", were considered as important factors in clinical experience.
The result of this study showed that nursing students were not satisfied with the clinical component of their education. They experienced anxiety as a result of feeling incompetent and lack of professional nursing skills and knowledge to take care of various patients in the clinical setting.
Peer Review reports
Clinical experience has been always an integral part of nursing education. It prepares student nurses to be able of "doing" as well as "knowing" the clinical principles in practice. The clinical practice stimulates students to use their critical thinking skills for problem solving [ 1 ]
Awareness of the existence of stress in nursing students by nurse educators and responding to it will help to diminish student nurses experience of stress. [ 2 ]
Clinical experience is one of the most anxiety producing components of the nursing program which has been identified by nursing students. In a descriptive correlational study by Beck and Srivastava 94 second, third and fourth year nursing students reported that clinical experience was the most stressful part of the nursing program[ 3 ]. Lack of clinical experience, unfamiliar areas, difficult patients, fear of making mistakes and being evaluated by faculty members were expressed by the students as anxiety-producing situations in their initial clinical experience. In study done by Hart and Rotem stressful events for nursing students during clinical practice have been studied. They found that the initial clinical experience was the most anxiety producing part of their clinical experience [ 4 ]. The sources of stress during clinical practice have been studied by many researchers [ 5 – 10 ] and [ 11 ].
The researcher came to realize that nursing students have a great deal of anxiety when they begin their clinical practice in the second year. It is hoped that an investigation of the student's view on their clinical experience can help to develop an effective clinical teaching strategy in nursing education.
A focus group design was used to investigate the nursing student's view about the clinical practice. Focus group involves organized discussion with a selected group of individuals to gain information about their views and experiences of a topic and is particularly suited for obtaining several perspectives about the same topic. Focus groups are widely used as a data collection technique. The purpose of using focus group is to obtain information of a qualitative nature from a predetermined and limited number of people [ 12 , 13 ].
Using focus group in qualitative research concentrates on words and observations to express reality and attempts to describe people in natural situations [ 14 ].
The group interview is essentially a qualitative data gathering technique [ 13 ]. It can be used at any point in a research program and one of the common uses of it is to obtain general background information about a topic of interest [ 14 ].
Focus groups interviews are essential in the evaluation process as part of a need assessment, during a program, at the end of the program or months after the completion of a program to gather perceptions on the outcome of that program [ 15 , 16 ]. Kruegger (1988) stated focus group data can be used before, during and after programs in order to provide valuable data for decision making [ 12 ].
The participants from which the sample was drawn consisted of 90 baccalaureate nursing students from two hundred nursing students (30 students from the second year and 30 from the third and 30 from the fourth year) at Shiraz University of Medical Sciences (Faculty of Nursing and Midwifery). The second year nursing students already started their clinical experience. They were arranged in nine groups of ten students. Initially, the topics developed included 9 open-ended questions that were related to their nursing clinical experience. The topics were used to stimulate discussion.
The following topics were used to stimulate discussion regarding clinical experience in the focus groups.
How do you feel about being a student in nursing education?
How do you feel about nursing in general?
Is there any thing about the clinical field that might cause you to feel anxious about it?
Would you like to talk about those clinical experiences which you found most anxiety producing?
Which clinical experiences did you find enjoyable?
What are the best and worst things do you think can happen during the clinical experience?
What do nursing students worry about regarding clinical experiences?
How do you think clinical experiences can be improved?
What is your expectation of clinical experiences?
The first two questions were general questions which were used as ice breakers to stimulate discussion and put participants at ease encouraging them to interact in a normal manner with the facilitator.
Data analysis
The following steps were undertaken in the focus group data analysis.
Immediate debriefing after each focus group with the observer and debriefing notes were made. Debriefing notes included comments about the focus group process and the significance of data
Listening to the tape and transcribing the content of the tape
Checking the content of the tape with the observer noting and considering any non-verbal behavior. The benefit of transcription and checking the contents with the observer was in picking up the following:
Parts of words
Non-verbal communication, gestures and behavior...
The researcher facilitated the groups. The observer was a public health graduate who attended all focus groups and helped the researcher by taking notes and observing students' on non-verbal behavior during the focus group sessions. Observer was not known to students and researcher
The methods used to code and categorise focus group data were adapted from approaches to qualitative content analysis discussed by Graneheim and Lundman [ 17 ] and focus group data analysis by Stewart and Shamdasani [ 14 ] For coding the transcript it was necessary to go through the transcripts line by line and paragraph by paragraph, looking for significant statements and codes according to the topics addressed. The researcher compared the various codes based on differences and similarities and sorted into categories and finally the categories was formulated into a 4 themes.
The researcher was guided to use and three levels of coding [ 17 , 18 ]. Three levels of coding selected as appropriate for coding the data.
Level 1 coding examined the data line by line and making codes which were taken from the language of the subjects who attended the focus groups.
Level 2 coding which is a comparing of coded data with other data and the creation of categories. Categories are simply coded data that seem to cluster together and may result from condensing of level 1 code [ 17 , 19 ].
Level 3 coding which describes the Basic Social Psychological Process which is the title given to the central themes that emerge from the categories.
Table 1 shows the three level codes for one of the theme
The documents were submitted to two assessors for validation. This action provides an opportunity to determine the reliability of the coding [ 14 , 15 ]. Following a review of the codes and categories there was agreement on the classification.
Ethical considerations
The study was conducted after approval has been obtained from Shiraz university vice-chancellor for research and in addition permission to conduct the study was obtained from Dean of the Faculty of Nursing and Midwifery. All participants were informed of the objective and design of the study and a written consent received from the participants for interviews and they were free to leave focus group if they wish.
Most of the students were females (%94) and single (% 86) with age between 18–25.
The qualitative analysis led to the emergence of the four themes from the focus group data. From the students' point of view," initial clinical anxiety", "theory-practice gap", clinical supervision"," professional role", was considered as important factors in clinical experience.
Initial clinical anxiety
This theme emerged from all focus group discussion where students described the difficulties experienced at the beginning of placement. Almost all of the students had identified feeling anxious in their initial clinical placement. Worrying about giving the wrong information to the patient was one of the issues brought up by students.
One of the students said:
On the first day I was so anxious about giving the wrong information to the patient. I remember one of the patients asked me what my diagnosis is. ' I said 'I do not know', she said 'you do not know? How can you look after me if you do not know what my diagnosis is?'
From all the focus group sessions, the students stated that the first month of their training in clinical placement was anxiety producing for them.
One of the students expressed:
The most stressful situation is when we make the next step. I mean ... clinical placement and we don't have enough clinical experience to accomplish the task, and do our nursing duties .
Almost all of the fourth year students in the focus group sessions felt that their stress reduced as their training and experience progressed.
Another cause of student's anxiety in initial clinical experience was the students' concern about the possibility of harming a patient through their lack of knowledge in the second year.
One of the students reported:
In the first day of clinical placement two patients were assigned to me. One of them had IV fluid. When I introduced myself to her, I noticed her IV was running out. I was really scared and I did not know what to do and I called my instructor .
Fear of failure and making mistakes concerning nursing procedures was expressed by another student. She said:
I was so anxious when I had to change the colostomy dressing of my 24 years old patient. It took me 45 minutes to change the dressing. I went ten times to the clinic to bring the stuff. My heart rate was increasing and my hand was shaking. I was very embarrassed in front of my patient and instructor. I will never forget that day .
Sellek researched anxiety-creating incidents for nursing students. He suggested that the ward is the best place to learn but very few of the learner's needs are met in this setting. Incidents such as evaluation by others on initial clinical experience and total patient care, as well as interpersonal relations with staff, quality of care and procedures are anxiety producing [ 11 ].
Theory-practice gap
The category theory-practice gap emerged from all focus discussion where almost every student in the focus group sessions described in some way the lack of integration of theory into clinical practice.
I have learnt so many things in the class, but there is not much more chance to do them in actual settings .
Another student mentioned:
When I just learned theory for example about a disease such as diabetic mellitus and then I go on the ward and see the real patient with diabetic mellitus, I relate it back to what I learned in class and that way it will remain in my mind. It is not happen sometimes .
The literature suggests that there is a gap between theory and practice. It has been identified by Allmark and Tolly [ 20 , 21 ]. The development of practice theory, theory which is developed from practice, for practice, is one way of reducing the theory-practice gap [ 21 ]. Rolfe suggests that by reconsidering the relationship between theory and practise the gap can be closed. He suggests facilitating reflection on the realities of clinical life by nursing theorists will reduce the theory-practice gap. The theory- practice gap is felt most acutely by student nurses. They find themselves torn between the demands of their tutor and practising nurses in real clinical situations. They were faced with different real clinical situations and are unable to generalise from what they learnt in theory [ 22 ].
Clinical supervision
Clinical supervision is recognised as a developmental opportunity to develop clinical leadership. Working with the practitioners through the milieu of clinical supervision is a powerful way of enabling them to realize desirable practice [ 23 ]. Clinical nursing supervision is an ongoing systematic process that encourages and supports improved professional practice. According to Berggren and Severinsson the clinical nurse supervisors' ethical value system is involved in her/his process of decision making. [ 24 , 25 ]
Clinical Supervision by Head Nurse (Nursing Unit Manager) and Staff Nurses was another issue discussed by the students in the focus group sessions. One of the students said:
Sometimes we are taught mostly by the Head Nurse or other Nursing staff. The ward staff are not concerned about what students learn, they are busy with their duties and they are unable to have both an educational and a service role
Another student added:
Some of the nursing staff have good interaction with nursing students and they are interested in helping students in the clinical placement but they are not aware of the skills and strategies which are necessary in clinical education and are not prepared for their role to act as an instructor in the clinical placement
The students mostly mentioned their instructor's role as an evaluative person. The majority of students had the perception that their instructors have a more evaluative role than a teaching role.
The literature suggests that the clinical nurse supervisors should expressed their existence as a role model for the supervisees [ 24 ]
Professional role
One view that was frequently expressed by student nurses in the focus group sessions was that students often thought that their work was 'not really professional nursing' they were confused by what they had learned in the faculty and what in reality was expected of them in practice.
We just do basic nursing care, very basic . ... You know ... giving bed baths, keeping patients clean and making their beds. Anyone can do it. We spend four years studying nursing but we do not feel we are doing a professional job .
The role of the professional nurse and nursing auxiliaries was another issue discussed by one of the students:
The role of auxiliaries such as registered practical nurse and Nurses Aids are the same as the role of the professional nurse. We spend four years and we have learned that nursing is a professional job and it requires training and skills and knowledge, but when we see that Nurses Aids are doing the same things, it can not be considered a professional job .
The result of student's views toward clinical experience showed that they were not satisfied with the clinical component of their education. Four themes of concern for students were 'initial clinical anxiety', 'theory-practice gap', 'clinical supervision', and 'professional role'.
The nursing students clearly identified that the initial clinical experience is very stressful for them. Students in the second year experienced more anxiety compared with third and fourth year students. This was similar to the finding of Bell and Ruth who found that nursing students have a higher level of anxiety in second year [ 26 , 27 ]. Neary identified three main categories of concern for students which are the fear of doing harm to patients, the sense of not belonging to the nursing team and of not being fully competent on registration [ 28 ] which are similar to what our students mentioned in the focus group discussions. Jinks and Patmon also found that students felt they had an insufficiency in clinical skills upon completion of pre-registration program [ 29 ].
Initial clinical experience was the most anxiety producing part of student clinical experience. In this study fear of making mistake (fear of failure) and being evaluated by faculty members were expressed by the students as anxiety-producing situations in their initial clinical experience. This finding is supported by Hart and Rotem [ 4 ] and Stephens [ 30 ]. Developing confidence is an important component of clinical nursing practice [ 31 ]. Development of confidence should be facilitated by the process of nursing education; as a result students become competent and confident. Differences between actual and expected behaviour in the clinical placement creates conflicts in nursing students. Nursing students receive instructions which are different to what they have been taught in the classroom. Students feel anxious and this anxiety has effect on their performance [ 32 ]. The existence of theory-practice gap in nursing has been an issue of concern for many years as it has been shown to delay student learning. All the students in this study clearly demonstrated that there is a gap between theory and practice. This finding is supported by other studies such as Ferguson and Jinks [ 33 ] and Hewison and Wildman [ 34 ] and Bjork [ 35 ]. Discrepancy between theory and practice has long been a source of concern to teachers, practitioners and learners. It deeply rooted in the history of nurse education. Theory-practice gap has been recognised for over 50 years in nursing. This issue is said to have caused the movement of nurse education into higher education sector [ 34 ].
Clinical supervision was one of the main themes in this study. According to participant, instructor role in assisting student nurses to reach professional excellence is very important. In this study, the majority of students had the perception that their instructors have a more evaluative role than a teaching role. About half of the students mentioned that some of the head Nurse (Nursing Unit Manager) and Staff Nurses are very good in supervising us in the clinical area. The clinical instructor or mentors can play an important role in student nurses' self-confidence, promote role socialization, and encourage independence which leads to clinical competency [ 36 ]. A supportive and socialising role was identified by the students as the mentor's function. This finding is similar to the finding of Earnshaw [ 37 ]. According to Begat and Severinsson supporting nurses by clinical nurse specialist reported that they may have a positive effect on their perceptions of well-being and less anxiety and physical symptoms [ 25 ].
The students identified factors that influence their professional socialisation. Professional role and hierarchy of occupation were factors which were frequently expressed by the students. Self-evaluation of professional knowledge, values and skills contribute to the professional's self-concept [ 38 ]. The professional role encompasses skills, knowledge and behaviour learned through professional socialisation [ 39 ]. The acquisition of career attitudes, values and motives which are held by society are important stages in the socialisation process [ 40 ]. According to Corwin autonomy, independence, decision-making and innovation are achieved through professional self-concept 41 . Lengacher (1994) discussed the importance of faculty staff in the socialisation process of students and in preparing them for reality in practice. Maintenance and/or nurturance of the student's self-esteem play an important role for facilitation of socialisation process 42 .
One view that was expressed by second and third year student nurses in the focus group sessions was that students often thought that their work was 'not really professional nursing' they were confused by what they had learned in the faculty and what in reality was expected of them in practice.
The finding of this study and the literature support the need to rethink about the clinical skills training in nursing education. It is clear that all themes mentioned by the students play an important role in student learning and nursing education in general. There were some similarities between the results of this study with other reported studies and confirmed that some of the factors are universal in nursing education. Nursing students expressed their views and mentioned their worry about the initial clinical anxiety, theory-practice gap, professional role and clinical supervision. They mentioned that integration of both theory and practice with good clinical supervision enabling them to feel that they are enough competent to take care of the patients. The result of this study would help us as educators to design strategies for more effective clinical teaching. The results of this study should be considered by nursing education and nursing practice professionals. Faculties of nursing need to be concerned about solving student problems in education and clinical practice. The findings support the need for Faculty of Nursing to plan nursing curriculum in a way that nursing students be involved actively in their education.
Dunn SV, Burnett P: The development of a clinical learning environment scale. Journal of Advanced Nursing. 1995, 22: 1166-1173.
Article CAS PubMed Google Scholar
Lindop E: Factors associated with student and pupil nurse wastage. Journal of Advanced Nursing. 1987, 12 (6): 751-756.
Beck D, Srivastava R: Perceived level and source of stress in baccalaureate nursing students. Journal of Nursing Education. 1991, 30 (3): 127-132.
CAS PubMed Google Scholar
Hart G, Rotem A: The best and the worst: Students' experience of clinical education. The Australian Journal of Advanced Nursing. 1994, 11 (3): 26-33.
Sheila Sh, Huey-Shyon L, Shiowli H: Perceived stress and physio-psycho-social status of nursing students during their initial period of clinical practice. International Journal of Nursing Studies. 2002, 39: 165-175. 10.1016/S0020-7489(01)00016-5.
Article Google Scholar
Johnson J: Reducing distress in first level and student nurses. Journal of Advanced Nursing. 2000, 32 (1): 66-74. 10.1046/j.1365-2648.2000.01421.x.
Admi H: Nursing students' stress during the initial clinical experience. Journal of Nursing Education. 1997, 36: 323-327.
Blainey GC: Anxiety in the undergraduate medical-surgical clinical student. Journal of Nursing Education. 1980, 19 (8): 33-36.
Wong J, Wong S: Towards effective clinical teaching in nursing. Journal of Advanced Nursing. 1987, 12 (4): 505-513.
Windsor A: Nursing students' perceptions of clinical experience. Journal of Nursing Education. 1987, 26 (4): 150-154.
Sellek T: Satisfying and anxiety creating incidents for nursing students. Nursing Times. 1982, 78 (35): 137-140.
PubMed Google Scholar
Krueger RA: Focus Groups: A Practical Guide for Applied Research. Sage Publications: California. 1988
Google Scholar
Denzin NK: The Research Act. 1989, Prentice Hall: Englewood Cliffs, New Jersey, 3
Stewart DW, Shamdasani PN: Analysing focus group data. Focus Groups: Theory and Practice. Edited by: Shamdasani PN. 1990, Sage Publications: Newbury Park
Barbour RS, Kitzinger J: Developing focus group research : politics, theory and practice. Sage. 1999
Patton MQ: Qualitative Evaluation and Research Methods. 1990, Sage publications, 2
Graneheim UH, Lundman B: Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2004, 24: 105-112. 10.1016/j.nedt.2003.10.001.
Streubert HJ, Carpenter DR: Qualitative Research in Nursing. Advancing the Humanistic Imperative. 1995, J.B. Lippincott Company: Philadelphia
Polit DF, Hungler BP: Nursing research: Principles and Methods. Philadelphia newyork. 1999
Allmark PA: classical view of the theory-practice gap in nursing. Journal of Advanced Nursing. 1995, 22 (1): 18-23. 10.1046/j.1365-2648.1995.22010018.x.
Tolley KA: Theory from practice for practice: Is this a reality?. Journal of Advanced Nursing. 1995, 21 (1): 184-190. 10.1046/j.1365-2648.1995.21010184.x.
Rolfe G: Listening to students: Course evaluation as action research. Nurse Education Today. 1994, 14 (3): 223-227. 10.1016/0260-6917(94)90085-X.
Johns Ch: clinical supervision as a model for clinical leadership. Journal of Nursing Management. 2003, 11: 25-34. 10.1046/j.1365-2834.2002.00288.x.
Article PubMed Google Scholar
Berggren I, Severinsson E: Nurses supervisors'action in relation to their decision-making style and ethical approach to clinical supervision. Journal of Advanced Nursing. 2003, 41 (6): 615-622. 10.1046/j.1365-2648.2003.02573.x.
Begat I, Severinsson E: Nurses' satisfaction with their work environment and the outcomes of clinical nursing supervision on nurses' experiences of well-being. Journal of Nursing Management. 2005, 13: 221-230. 10.1111/j.1365-2834.2004.00527.x.
Bell P: Anxiety in mature age and higher school certificate entry student nurses – A comparison of effects on performance. Journal of Australian Congress of Mental Health Nurses. 1984, 4/5: 13-21.
Ruth L: Experiencing before and throughout the nursing career. Journal of Advanced Nursing. 2002, 39: 119-10.1046/j.1365-2648.2000.02251.x.
Neary M: Project 2000 students' survival kit: a return to the practical room. Nurse Education Today. 1997, 17 (1): 46-52. 10.1016/S0260-6917(97)80078-0.
Jinks A, Pateman B: Nither this nor that: The stigma of being an undergraduate nurse. Nursing Times. 1998, 2 (2): 12-13.
CAS Google Scholar
Stephen RL: Imagery: A treatment for nursing student anxiety. Journal of Nursing Education. 1992, 31 (7): 314-319.
Grundy SE: The confidence scale. Nurse Educator. 1993, 18 (1): 6-9.
Copeland L: Developing student confidence. Nurse Educator. 1990, 15 (1): 7-
Ferguson K, Jinks A: Integrating what is taught with what is practised in the nursing curriculum: A multi-dimensional model. Journal of Advanced Nursing. 1994, 20 (4): 687-695. 10.1046/j.1365-2648.1994.20040687.x.
Hewison A, Wildman S: The theory-practice gap in nursing: A new dimension. Journal of Advanced Nursing. 1996, 24 (4): 754-761. 10.1046/j.1365-2648.1996.25214.x.
Bjork T: Neglected conflicts in the discipline of nursing: Perceptions of the importance and value of practical skill. Journal of Advanced Nursing. 1995, 22 (1): 6-12. 10.1046/j.1365-2648.1995.22010006.x.
Busen N: Mentoring in advanced practice nursing. Journal of Advanced Nursing Practice. 1999, 2: 2-
Earnshaw GP: Mentorship: The students' view. Nurse Education Today. 1995, 15 (4): 274-279. 10.1016/S0260-6917(95)80130-8.
Kelly B: The professional self-concepts of nursing undergraduates and their perceptions of influential forces. Journal of Nursing Education. 1992, 31 (3): 121-125.
Lynn MR, McCain NL, Boss BJ: Socialization of R.N. to B.S.N Image:. Journal of Nursing Scholarship. 1989, 21 (4): 232-237.
Article CAS Google Scholar
Klein SM, Ritti RR: Understanding Organisational Behaviour. 1980, Kent: Boston
Corwin RG: The professional employee: A study of conflict in nursing roles. The American Journal of Sociology. 1961, 66: 604-615. 10.1086/223010.
Lengacher CA: Effects of professional development seminars on role conception, role deprivation, and self-esteem of generic baccalaureate students. Nursing Connections. 1994, 7 (1): 21-34.
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1472-6955/4/6/prepub
Download references
Acknowledgements
The author would like to thank the student nurses who participated in this study for their valuable contribution
Author information
Authors and affiliations.
Psychiatric Nursing Department, Fatemeh (P.B.U.H) College of Nursing and Midwifery Shiraz University of Medical Sciences, Zand BlvD, Shiraz, Iran
Farkhondeh Sharif
English Department, Shiraz University, Shiraz, Iran
Sara Masoumi
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Farkhondeh Sharif .
Additional information
Competing interests.
The author(s) declare that they no competing interests.
Authors' contributions
FSH: Initiation and design of the research, focus groups conduction, data collection, analysis and writing the paper, SM: Editorial revision of paper
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Sharif, F., Masoumi, S. A qualitative study of nursing student experiences of clinical practice. BMC Nurs 4 , 6 (2005). https://doi.org/10.1186/1472-6955-4-6
Download citation
Received : 10 June 2005
Accepted : 09 November 2005
Published : 09 November 2005
DOI : https://doi.org/10.1186/1472-6955-4-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Focus Group
- Nursing Student
- Professional Role
- Nursing Education
- Focus Group Session
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Quantitative and Qualitative Research
You can find evidence for clinical decision making in quantitative and qualitative research studies . Quantitative research refers to any research based on something that can be accurately and precisely measured and will include studies that have numerical data . Quantitative data are expressed numerically and analyzed statistically. The data are collected from experiments and tests, metrics, databases, and surveys. In healthcare research they often include studies of intervention effectiveness, satisfaction with care, the incidence, prevalence, and etiology of diseases, and the properties of measurement tools (Kolaski, 2023).
Findings in qualitative studies are not based on measurable statistics. Qualitative data are descriptive rather than numerical. Qualitative research derives data from observation, interviews, verbal interactions, or textual analyses and focuses on the meanings and interpretations of the participants. Qualitative research studies in healthcare investigate the impact of illnesses and interventions. The research explores experiences, attitudes, beliefs, and perspectives of patients, caregivers, and clinicians (Kolaski, 2023). The analysis of qualitative research is interpretative, subjective, and impressionistic.
Kolaski, K., Logan, L. R., & Ioannidis, J. P. A. (2023). Guidance to best tools and practices for systematic reviews. Systematic Reviews , 12 (1), 96. https://doi.org/10.1186/s13643-023-02255-9
Quantitative vs Qualitative Study Types:

For more information on qualitative research:
Curtis, A. & Keeler, C. (2022). An introduction to qualitative methods for the nurse researcher. American Journal of Nursing, 122 (8), 52-56. https://doi: 10.1097/01.NAJ.0000854992.17329.51.
Noyes, J., Booth, A., Cargo, M., Flemming, K., Harden, A., Harris, J., Garside, R., Hannes, K., Pantoja, T., & Thomas, J. (2023). Chapter 21: Qualitative evidence. In Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A. (Eds.). Cochrane handbook for systematic reviews of interventions version 6.4. Cochrane. www.training.cochrane.org/handbook
Video: UniversityNow: Quantitative vs. Qualitative Research
Appraising Quantitative and Qualitative Research
The articles below provide a step-by-step appraisal on how to critique quantitative and qualitative research articles:
- Ryan, F., Coughlan, M. & Cronin, P. (2007). Step-by-step guide to critiquing research. Part 1: quantitative research. British Journal of Nursing, 16 (11), 658-663 .
- Ryan, F., Coughlan, M. & Cronin, P. (2007). Step-by-step guide to critiquing research. Part 2: qualitative research. British Journal of Nursing, 16 (2), 738-744 .
- << Previous: Study Types & Terminology
- Next: Critical Appraisal: Evaluating Studies >>
- Evidence-Based Medicine/Evidence-Based Practice
- Evidence-Based Practice in Nursing
- Question Types
- Levels of Evidence
- Systematic Reviews and Meta Analyses
- Study Types & Terminology
- Critical Appraisal: Evaluating Studies
- Conducting a Systematic Review
- Research Study Design
- Selected Books for EBP Research
- Find a Book by Call Number
- Find EBP Articles in the Databases
- Selected EBP Journals
- Finding the Full Text of an Article from a Citation
- Nursing Databases
- Databases for EBP
- More EBP Resources
- Intro to Nursing Resources
- Citation Management Programs
- Annotated Bibliography
- Last Updated: Aug 26, 2024 10:56 AM
- URL: https://libguides.adelphi.edu/evidence-based-practice
Library Research Guides - University of Wisconsin Ebling Library
Uw-madison libraries research guides.
- Course Guides
- Subject Guides
- University of Wisconsin-Madison
- Research Guides
- Nursing Resources
- Qualitative vs Quantitative
Nursing Resources : Qualitative vs Quantitative
- Definitions of
- Professional Organizations
- Nursing Informatics
- Nursing Related Apps
- EBP Resources
- PICO-Clinical Question
- Types of PICO Question (D, T, P, E)
- Secondary & Guidelines
- Bedside--Point of Care
- Pre-processed Evidence
- Measurement Tools, Surveys, Scales
- Types of Studies
- Table of Evidence
- Types of Research within Qualitative and Quantitative
- Cohort vs Case studies
- Independent Variable VS Dependent Variable
- Sampling Methods and Statistics
- Systematic Reviews
- Review vs Systematic Review vs ETC...
- Standard, Guideline, Protocol, Policy
- Additional Guidelines Sources
- Peer Reviewed Articles
- Conducting a Literature Review
- Systematic Reviews and Meta-Analysis
- Writing a Research Paper or Poster
- Annotated Bibliographies
- Levels of Evidence (I-VII)
- Reliability
- Validity Threats
- Threats to Validity of Research Designs
- Nursing Theory
- Nursing Models
- PRISMA, RevMan, & GRADEPro
- ORCiD & NIH Submission System
- Understanding Predatory Journals
- Nursing Scope & Standards of Practice, 4th Ed
- Distance Ed & Scholarships
- Assess A Quantitative Study?
- Assess A Qualitative Study?
- Find Health Statistics?
- Choose A Citation Manager?
- Find Instruments, Measurements, and Tools
- Write a CV for a DNP or PhD?
- Find information about graduate programs?
- Learn more about Predatory Journals
- Get writing help?
- Choose a Citation Manager?
- Other questions you may have
- Search the Databases?
- Get Grad School information?
Differences between Qualitative & Quantitative Research
" Quantitative research ," also called " empirical research ," refers to any research based on something that can be accurately and precisely measured. For example, it is possible to discover exactly how many times per second a hummingbird's wings beat and measure the corresponding effects on its physiology (heart rate, temperature, etc.).
" Qualitative research " refers to any research based on something that is impossible to accurately and precisely measure. For example, although you certainly can conduct a survey on job satisfaction and afterwards say that such-and-such percent of your respondents were very satisfied with their jobs, it is not possible to come up with an accurate, standard numerical scale to measure the level of job satisfaction precisely.
It is so easy to confuse the words "quantitative" and "qualitative," it's best to use "empirical" and "qualitative" instead.
Hint: An excellent clue that a scholarly journal article contains empirical research is the presence of some sort of statistical analysis
See "Examples of Qualitative and Quantitative" page under "Nursing Research" for more information.
|
|
|
|
|
|
|
|
| Considered hard science |
| Considered soft science |
| Objective |
| Subjective |
| Deductive reasoning used to synthesize data |
| Inductive reasoning used to synthesize data |
| Focus—concise and narrow |
| Focus—complex and broad |
| Tests theory |
| Develops theory |
| Basis of knowing—cause and effect relationships |
| Basis of knowing—meaning, discovery |
| Basic element of analysis—numbers and statistical analysis |
| Basic element of analysis—words, narrative |
| Single reality that can be measured and generalized |
| Multiple realities that are continually changing with individual interpretation |
- John M. Pfau Library
Examples of Qualitative vs Quantitiative
|
|
|
|
|
|
|
|
|
|
| What is the impact of a learner-centered hand washing program on a group of 2 graders? | Paper and pencil test resulting in hand washing scores | Yes | Quantitative |
| What is the effect of crossing legs on blood pressure measurement? | Blood pressure measurements before and after crossing legs resulting in numbers | Yes | Quantitative |
| What are the experiences of fathers concerning support for their wives/partners during labor? | Unstructured interviews with fathers (5 supportive, 5 non-supportive): results left in narrative form describing themes based on nursing for the whole person theory | No | Qualitative |
| What is the experience of hope in women with advances ovarian cancer? | Semi-structures interviews with women with advances ovarian cancer (N-20). Identified codes and categories with narrative examples | No | Qualitative |
- << Previous: Table of Evidence
- Next: Types of Research within Qualitative and Quantitative >>
- Last Updated: Aug 29, 2024 10:13 AM
- URL: https://researchguides.library.wisc.edu/nursing
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
[Importance of qualitative research for nursing and nursing science]
Affiliation.
- 1 Universität Utrecht.
- PMID: 9370721
Qualitative research has an important place in nursing science and is becoming increasingly recognized. Qualitative research in nursing mainly deals with the lived experiences of patients and nurses. In the field of chronic illness, qualitative research has brought to the open some of the processes chronically ill patients undergo and what it means living with chronic illness. In addition, new insights were gained about the processes involved in receiving and in giving care. Qualitative research about chronic illness provided nurses with understanding of the lived experience of patients. This understanding is essential for good nursing care. However, qualitative research is not the only method and for some aspects of nursing not the adequate one. Qualitative and quantitative research are complementary.
PubMed Disclaimer
Similar articles
- Two decades of insider research: what we know and don't know about chronic illness experience. Thorne SE, Paterson BL. Thorne SE, et al. Annu Rev Nurs Res. 2000;18:3-25. Annu Rev Nurs Res. 2000. PMID: 10918930 Review.
- Capturing day-to-day aspects of living with chronic illness: the need for longitudinal designs. Russell CK, Gregory DM. Russell CK, et al. Can J Nurs Res. 2000 Dec;32(3):99-102. Can J Nurs Res. 2000. PMID: 11928137 Review. No abstract available.
- Ricoeur's hermeneutic phenomenology: an implication for nursing research. Charalambous A, Papadopoulos IR, Beadsmoore A. Charalambous A, et al. Scand J Caring Sci. 2008 Dec;22(4):637-42. doi: 10.1111/j.1471-6712.2007.00566.x. Epub 2008 Oct 16. Scand J Caring Sci. 2008. PMID: 19000085
- The nature of hope in hospitalized chronically ill patients. Kim DS, Kim HS, Schwartz-Barcott D, Zucker D. Kim DS, et al. Int J Nurs Stud. 2006 Jul;43(5):547-56. doi: 10.1016/j.ijnurstu.2005.07.010. Epub 2005 Sep 6. Int J Nurs Stud. 2006. PMID: 16140301
- Clients with chronic and complex conditions: their experiences of community nursing services. Wilkes L, Cioffi J, Warne B, Harrison K, Vonu-Boriceanu O. Wilkes L, et al. J Clin Nurs. 2008 Apr;17(7B):160-8. doi: 10.1111/j.1365-2702.2008.02454.x. J Clin Nurs. 2008. PMID: 18578792
Publication types
- Search in MeSH
LinkOut - more resources
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

Evidence Based Nursing
- Electronic Resources
- Step 1: Ask
- Step 2: Aquire
- Step 3: Appraise
- Peer-Reviewed Articles
- Systematic Reviews
- Qualitative vs. Quantitative Research
- Searching Tips
- APA Citations
- Useful Websites
Difference between Qualitative vs. Quantitative Research
Qualitative research allows you to discover the why and how of people and activities. The abstract from this dissertation shows the study:
- Asks open-ended questions
- Examines people's activities
- Gives a narrative conclusion
- Observations and Interviews
- Understanding and interpreting social interactions and behaviors
- Uses a small group of subjects
- Uses words
Quantitative research is based on things that can be accurately and precisely measured. The abstract shows that this dissertation:
- Describes with statistics
- Gives a statistical result
- Makes predictions
- Objective
- Studies a randomly selected group
- Tests a theory
- Uses numbers
- Uses a survey
Identifying Quantitative Research- Example
This abstract has several indications that this is a quantitative study:
- the goal of the study was examining relationships between several variables
- the researchers used statistical methods (logistic regression models)
- subjects completed questionnaires
- the study included a large number of subjects
Based on Eastern Michigan University Library Libguide Quantitative and Qualitative Research
Identifying Qualitative Research-Example
This abstract has several indications that this is a qualitative study:
- the goal of the study was to explore the subjects' experiences.
- the researchers conducted open-ended interviews.
- the researchers used thematic analysis when reviewing the interviews.
Based on Eastern Michigan University Library Libguide Quantitative and Qualitative Research
- << Previous: Systematic Reviews
- Next: Searching Tips >>
- Last Updated: May 8, 2024 10:17 AM
- URL: https://libguide.umary.edu/evidencebasednursing

Nursing: Quantitative vs. Qualitative?
- Reading Scholarly Articles
- Searching for Empirical Articles
- Clinical Practice Guidelines
- Systematic Reviews
- Grey Literature
- Writing a Literature Review
- Annotated Bibliography vs. Literature Review
- Quantitative vs. Qualitative?
- Writing Help
Qualitative vs Quantitative worksheet
- Methodology Decision Tree This diagram should help you to determine whether the research you are looking at is qualitative or quantitative. NOTE: This is a brief guide and might not be correct in every instance

- << Previous: Annotated Bibliography vs. Literature Review
- Next: EndNote >>
- Last Updated: Aug 28, 2024 10:22 AM
- URL: https://libraryguides.fullerton.edu/nursing
This site is maintained by Pollak Library .
To report problems or comments with this site, please contact [email protected] . © California State University, Fullerton. All Rights Reserved.
Web Accessibility
CSUF is committed to ensuring equal accessibility to our users. Let us know about any accessibility problems you encounter using this website. We'll do our best to improve things and get you the information you need.
- Adobe Reader
- Microsoft Viewers
- Report An ATI Issue
- Accessible @ CSUF
- Open access
- Published: 28 August 2024
The design, implementation, and evaluation of a blended (in-person and virtual) Clinical Competency Examination for final-year nursing students
- Rita Mojtahedzadeh 1 ,
- Tahereh Toulabi 2 , 3 &
- Aeen Mohammadi 1
BMC Medical Education volume 24 , Article number: 936 ( 2024 ) Cite this article
7 Altmetric
Metrics details
Introduction
Studies have reported different results of evaluation methods of clinical competency tests. Therefore, this study aimed to design, implement, and evaluate a blended (in-person and virtual) Competency Examination for final-year Nursing Students.
This interventional study was conducted in two semesters of 2020–2021 using an educational action research method in the nursing and midwifery faculty. Thirteen faculty members and 84 final-year nursing students were included in the study using a census method. Eight programs and related activities were designed and conducted during the examination process. Students completed the Spielberger Anxiety Inventory before the examination, and both faculty members and students completed the Acceptance and Satisfaction questionnaire.
The results of the analysis of focused group discussions and reflections indicated that the virtual CCE was not capable of adequately assessing clinical skills. Therefore, it was decided that the CCE for final-year nursing students would be conducted using a blended method. The activities required for performing the examination were designed and implemented based on action plans. Anxiety and satisfaction were also evaluated as outcomes of the study. There was no statistically significant difference in overt, covert, and overall anxiety scores between the in-person and virtual sections of the examination ( p > 0.05). The mean (SD) acceptance and satisfaction scores for students in virtual, in-person, and blended sections were 25.49 (4.73), 27.60 (4.70), and 25.57 (4.97), respectively, out of 30 points, in which there was a significant increase in the in-person section compared to the other sections. ( p = 0.008). The mean acceptance and satisfaction scores for faculty members were 30.31 (4.47) in the virtual, 29.86 (3.94) in the in-person, and 30.00 (4.16) out of 33 in the blended, and there was no significant difference between the three sections ( p = 0.864).
Evaluating nursing students’ clinical competency using a blended method was implemented and solved the problem of students’ graduation. Therefore, it is suggested that the blended method be used instead of traditional in-person or entirely virtual exams in epidemics or based on conditions, facilities, and human resources. Also, the use of patient simulation, virtual reality, and the development of necessary virtual and in-person training infrastructure for students is recommended for future research. Furthermore, considering that the acceptance of traditional in-person exams among students is higher, it is necessary to develop virtual teaching strategies.
Peer Review reports
The primary mission of the nursing profession is to educate competent, capable, and qualified nurses with the necessary knowledge and skills to provide quality nursing care to preserve and improve the community’s health [ 1 ]. Clinical education is one of the most essential and fundamental components of nursing education, in which students gain clinical experience by interacting with actual patients and addressing real problems. Therefore, assessing clinical skills is very challenging. The main goal of educational evaluation is to improve, ensure, and enhance the quality of the academic program. In this regard, evaluating learners’ performance is one of the critical and sensitive aspects of the teaching and learning process. It is considered one of the fundamental elements of the educational program [ 2 ]. The study area is educational evaluation.
Various methods are used to evaluate nursing students. The Objective Structured Clinical Examination (OSCE) is a valid and reliable method for assessing clinical competence [ 1 , 2 ]. In the last twenty years, the use of OSCE has increased significantly in evaluating medical and paramedical students to overcome the limitations of traditional practical evaluation systems [ 3 , 4 ]. The advantages of this method include providing rapid feedback, uniformity for all examinees, and providing conditions close to reality. However, the time-consuming nature and the need for a lot of personnel and equipment are some disadvantages of OSCE [ 5 , 6 ]. Additionally, some studies have shown that this method is anxiety-provoking for some students and, due to time constraints, being observed by the evaluator and other factors can cause dissatisfaction among students [ 7 , 8 ].
However, some studies have also reported that this method is not only not associated with high levels of stress among students [ 9 ] but also has higher satisfaction than traditional evaluation methods [ 4 ]. In addition, during the COVID-19 pandemic, problems such as overcrowding and student quarantine during the exam have arisen. Therefore, reducing time and costs, eliminating or reducing the tiring quarantine time, optimizing the exam, utilizing all facilities for simulating the clinical environment, using innovative methods for conducting the exam, reducing stress, increasing satisfaction, and ultimately preventing the transmission of COVID-19 are significant problems that need to be further investigated.
Studies show that using virtual space as an alternative solution is strongly felt [ 10 , 11 , 12 ]. In the fall of 2009, following the outbreak of H1N1, educational classes in the United States were held virtually [ 13 ]. Also, in 2005, during Hurricane Katrina, 27 universities in the Gulf of Texas used emergency virtual education and evaluation [ 14 ].
One of the challenges faced by healthcare providers in Iran, like most countries in the world, especially during the COVID-19 outbreak, was the shortage of nursing staff [ 15 , 16 ]. Also, in evaluating and conducting CCE for final-year students and subsequent job seekers in the Clinical Skills Center, problems such as student overcrowding and the need for quarantine during the implementation of OSCE existed. This problem has been reported not only for us but also in other countries [ 17 ]. The intelligent use of technology can solve many of these problems. Therefore, almost all educational institutions have quickly started changing their policies’ paradigms to introduce online teaching and evaluation methods [ 18 , 19 ].
During the COVID-19 pandemic, for the first time, this exam was held virtually in our school. However, feedback from professors and students and the experiences of researchers have shown that the virtual exam can only partially evaluate clinical and practical skills in some stations, such as basic skills, resuscitation, and pediatrics [ 20 ].
Additionally, using OSCE in skills assessment facilitates the evaluation of psychological-motor knowledge and attitudes and helps identify strengths and weaknesses [ 21 ]. Clinical competency is a combination of theoretical knowledge and clinical skills. Therefore, using an effective blended method focusing on the quality and safety of healthcare that measures students’ clinical skills and theoretical expertise more accurately in both in-person and virtual environments is essential. The participation of students, professors, managers, education and training staff, and the Clinical Skills Center was necessary to achieve this important and inevitable goal. Therefore, the Clinical Competency Examination (CCE) for nursing students in our nursing and midwifery school was held in the form of an educational action research process to design, implement, and evaluate a blended method. Implementing this process during the COVID-19 pandemic, when it was impossible to hold an utterly in-person exam, helped improve the quality of the exam and address its limitations and weaknesses while providing the necessary evaluation for students.
The innovation of this research lies in evaluating the clinical competency of final-year nursing students using a blended method that focuses on clinical and practical aspects. In the searches conducted, only a few studies have been done on virtual exams and simulations, and a similar study using a blended method was not found.
The research investigates the scientific and clinical abilities of nursing students through the clinical competency exam. This exam, traditionally administered in person, is a crucial milestone for final-year nursing students, marking their readiness for graduation. However, the unforeseen circumstances of the COVID-19 pandemic and the resulting restrictions rendered in-person exams impractical in 2020. This necessitated a swift and significant transition to an online format, a decision that has profound implications for the future of nursing education. While the adoption of online assessment was a necessary step to ensure student graduation and address the nursing workforce shortage during the pandemic, it was not without its challenges. The accurate assessment of clinical skills, such as dressing and CPR, proved to be a significant hurdle. This underscored the urgent need for a change in the exam format, prompting a deeper exploration of innovative solutions.
To address these problems, the research was conducted collaboratively with stakeholders, considering the context and necessity for change in exam administration. Employing an Action Research (AR) approach, a blend of online and in-person exam modalities was adopted. Necessary changes were implemented through a cyclic process involving problem identification, program design, implementation, reflection, and continuous evaluation.
The research began by posing the following questions:
What are the problems of conducting the CCE for final-year nursing students during COVID-19?
How can these problems be addressed?
What are the solutions and suggestions from the involved stakeholders?
How can the CCE be designed, implemented, and evaluated?
What is the impact of exam type on student anxiety and satisfaction?
These questions guided the research in exploring the complexities of administering the CCE amidst the COVID-19 pandemic and in devising practical solutions to ensure the validity and reliability of the assessment while meeting stakeholders’ needs.
Materials and methods
Research setting, expert panel members, job analysis, and role delineation.
This action research was conducted at the Nursing and Midwifery School of Lorestan University of Medical Sciences, with a history of approximately 40 years. The school accommodates 500 undergraduate and graduate nursing students across six specialized fields, with 84 students enrolled in their final year of undergraduate studies. Additionally, the school employs 26 full-time faculty members in nursing education departments.
An expert panel was assembled, consisting of faculty members specializing in various areas, including medical-surgical nursing, psychiatric nursing, community health nursing, pediatric nursing, and intensive care nursing. The panel also included educational department managers and the examination department supervisor. Through focused group discussions, the panel identified and examined issues regarding the exam format, and members proposed various solutions. Subsequently, after analyzing the proposed solutions and drawing upon the panel members’ experiences, specific roles for each member were delineated.
Sampling and participant selection
Given the nature of the research, purposive sampling was employed, ensuring that all individuals involved in the design, implementation, and evaluation of the exam participated in this study.
The participants in this study included final-year nursing students, faculty members, clinical skills center experts, the dean of the school, the educational deputy, group managers, and the exam department head. However, in the outcome evaluation phase, 13 faculty members participated in-person and virtually (26 times), and 84 final-year nursing students enrolled in the study using a census method in two semesters of 2020–2021 completed the questionnaires, including 37 females and 47 males. In addition, three male and ten female faculty members participated in this study; of this number, 2 were instructors, and 11 were assistant professors.
Data collection tools
In order to enhance the validity and credibility of the study and thoroughly examine the results, this study utilized a triangulation method consisting of demographic information, focus group discussions, the Spielberger Anxiety Scale questionnaire, and an Acceptance and Satisfaction Questionnaire.
Demographic information
A questionnaire was used to gather demographic information from both students and faculty members. For students, this included age, gender, and place of residence, while for faculty members, it included age, gender, field of study, and employment status.
Focus group discussion
Multiple focused group discussions were conducted with the participation of professors, administrators, experts, and students. These discussions were held through various platforms such as WhatsApp Skype, and in-person meetings while adhering to health protocols. The researcher guided the talks toward the research objectives and raised fundamental questions, such as describing the strengths and weaknesses of the previous exam, determining how to conduct the CCE considering the COVID-19 situation, deciding on virtual and in-person stations, specifying the evaluation checklists for stations, and explaining the weighting and scoring of each station.
Spielberger anxiety scale questionnaire
This study used the Spielberger Anxiety Questionnaire to measure students’ overt and covert anxiety levels. This questionnaire is an internationally standardized tool known as the STAI questionnaire that measures both overt (state) and covert (trait) anxiety [ 22 ]. The state anxiety scale (Form Y-1 of STAI) comprises twenty statements that assess the individual’s feelings at the moment of responding. The trait anxiety scale (Form Y-2 of STAI) also includes twenty statements that measure individuals’ general and typical feelings. The scores of each of the two scales ranged from 20 to 80 in the current study. The reliability coefficient of the test for the apparent and hidden anxiety scales, based on Cronbach’s alpha, was confirmed to be 0.9084 and 0.9025, respectively [ 23 , 24 ]. Furthermore, in the present study, Cronbach’s alpha value for the total anxiety questionnaire, overt anxiety, and covert anxiety scales were 0.935, 0.921, and 0.760, respectively.
Acceptance and satisfaction questionnaire
The Acceptability and Satisfaction Questionnaire for Clinical Competency Test was developed by Farajpour et al. (2012). The student questionnaire consists of ten questions, and the professor questionnaire consists of eleven questions, using a four-point Likert scale. Experts have confirmed the validity of these questionnaires, and their Cronbach’s alpha coefficients have been determined to be 0.85 and 0.87 for the professor and student questionnaires, respectively [ 6 ]. In the current study, ten medical education experts also confirmed the validity of the questionnaires. Regarding internal reliability, Cronbach’s alpha coefficients for the student satisfaction questionnaire for both virtual and in-person sections were 0.76 and 0.87, respectively. The professor satisfaction questionnaires were 0.84 and 0.87, respectively. An online platform was used to collect data for the virtual exam.
Data analysis and rigor of study
Qualitative data analysis was conducted using the method proposed by Graneheim and Lundman. Additionally, the criteria established by Lincoln and Guba (1985) were employed to confirm the rigor and validity of the data, including credibility, transferability, dependability, and confirmability [ 26 ].
In this research, data synthesis was performed by combining the collected data with various tools and methods. The findings of this study were reviewed and confirmed by participants, supervisors, mentors, and experts in qualitative research, reflecting their opinions on the alignment of findings with their experiences and perspectives on clinical competence examinations. Therefore, the member check method was used to validate credibility.
Moreover, efforts were made in this study to provide a comprehensive description of the research steps, create a suitable context for implementation, assess the views of others, and ensure the transferability of the results.
Furthermore, researchers’ interest in identifying and describing problems, reflecting, designing, implementing, and evaluating clinical competence examinations, along with the engagement of stakeholders in these examinations, was ensured by the researchers’ long-term engagement of over 25 years with the environment and stakeholders, seeking their opinions and considering their ideas and views. These factors contributed to ensuring confirmability.
In this research, by reflecting the results to the participants and making revisions by the researchers, problem clarification and solution presentation, design, implementation, and evaluation of operational programs with stakeholder participation and continuous presence were attempted to prevent biases, assumptions, and research hypotheses, and to confirm dependability.
Data analysis was performed using SPSS version 21, and descriptive statistical tests (absolute and relative frequency, mean, and standard deviation) and inferential tests (paired t-test, independent t-test, and analysis of variance) were used. The significance level was set at 0.05. Parametric tests were used based on the normality of the data according to the Kolmogorov-Smirnov statistical test.
Given that conducting the CCE for final-year nursing students required the active participation of managers, faculty members, staff, and students, and to answer the research question “How can the CCE for final-year nursing students be conducted?” and achieve the research objective of “designing, implementing, and evaluating the clinical competency exam,” the action research method was employed.
The present study was conducted based on the Dickens & Watkins model. There are four primary stages (Fig. 1 ) in the cyclical action research process: reflect, plan, act, observe, and then reflect to continue through the cycle [ 27 ].

The cyclical process of action research [ 27 ]
Stage 1: Reflection
Identification of the problem.
According to the educational regulations, final semester nursing students must complete the clinical competency exam. However, due to the COVID-19 pandemic and the critical situation in most provinces, inter-city travel restrictions, and insufficient dormitory space, conducting the CCE in-person was not feasible.
This exam was conducted virtually at our institution. However, based on the reflections from experts, researchers have found that virtual exams can only partially assess clinical and practical skills in certain stations, such as basic skills, resuscitation, and pediatrics. Furthermore, utilizing Objective Structured Clinical Examination (OSCE) in skills assessment facilitates the evaluation of psychomotor skills, knowledge, and attitudes, aiding in identifying strengths and weaknesses.
P3, “Due to the COVID-19 pandemic and the critical situation in most provinces, inter-city travel restrictions, and insufficient dormitory space, conducting the CCE in-person is not feasible.”
Stage 2: Planning
Based on the reflections gathered from the participants, the exam was designed using a blended approach (combining in-person and virtual components) as per the schedule outlined in Fig. 2 . All planned activities for the blended CCE for final-year nursing students were executed over two semesters.
P5, “Taking the exam virtually might seem easier for us and the students, but in my opinion, it’s not realistic. For instance, performing wound dressing or airway management is very practical, and it’s not possible to assess students with a virtual scenario. We need to see them in person.”
P6"I believe it’s better to conduct those activities that are highly practical in person, but for those involving communication skills like report writing, professional ethics, etc., we can opt for virtual assessment.”

Design and implementation of the blended CCE
Stage 3: Act
Cce implementation steps.
The CCE was conducted based on the flowchart in Fig. 3 and the following steps:

Steps for conducting the CCE for final-year nursing students using a blended method
Step 1: Designing the framework for conducting the blended Clinical Competency Examination
The panelists were guided to design the blended exam in focused group sessions and virtual panels based on the ADDIE (Analysis, Design, Development, Implementation, Evaluation) model [ 28 ]. Initially, needs assessment and opinion polling were conducted, followed by the operational planning of the exam, including the design of the blueprint table (Table 1 ), determination of station types (in-person or virtual), designing question stems in the form of scenarios, creating checklists and station procedure guides by expert panel groups based on participant analysis, and the development of exam implementation guidelines with participant input [ 27 ]. The design, execution, and evaluation were as follows:
In-person and virtual meetings with professors were held to determine the exam schedule, deadlines for submitting checklists, decision-making regarding the virtual or in-person nature of stations based on the type of skill (practical, communication), and presenting problems and solutions. Based on the decisions, primary skill stations, as well as cardiac and pediatric resuscitation stations, were held in person. In contrast, virtual stations for health, nursing ethics, nursing reports, nursing diagnosis, physical examinations, and psychiatric nursing were held.
News about the exam was communicated to students through the college website and text messages. Then, an online orientation session was held on Skype with students regarding the need assessment of pre-exam educational workshops, virtual and in-person exam standards, how to use exam software, how to conduct virtual exams, explaining the necessary infrastructure for participating in the exam by students, completing anxiety and satisfaction questionnaires, rules and regulations, how to deal with rejected individuals, and exam testing and Q&A. Additionally, a pre-exam in-person orientation session was held.
To inform students about the entire educational process, the resources and educational content recommended by the professors, including PDF files, photos and videos, instructions, and links, were shared through a virtual group on the social media messenger, and scientific information was also, questions were asked and answered through this platform.
Correspondence and necessary coordination were made with the university clinical skills center to conduct in-person workshops and exams.
Following the Test-centered approach, the Angoff Modified method [ 29 , 30 ] was used to determine the scoring criteria for each station by panelists tasked with assigning scores.
Additionally, in establishing standards for this blended CCE for fourth-year nursing students, for whom graduation was a prerequisite, the panelists, as experienced clinical educators familiar with the performance and future roles of these students and the assessment method of the blended exam, were involved [ 29 , 30 ](Table 1 ).
Step 2: Preparing the necessary infrastructure for conducting the exam
Software infrastructure.
The pre- and post-virtual exam questions, scenarios, and questionnaires were uploaded using online software.
The exam was conducted on a trial basis in multiple sessions with the participation of several faculty members, and any issues were addressed. Students were authenticated to enter the exam environment via email and personal information verification. The questions for each station were designed and entered into the software by the respective station instructors and the examination coordinator, who facilitated the exam. The questions were formatted as clinical scenarios, images, descriptive questions, and multiple-choice questions, emphasizing the clinical and practical aspects. This software had various features for administering different types of exams and various question formats, including multiple-choice, descriptive, scenario-based, image-based, video-based, matching, Excel output, and graphical and descriptive statistical analyses. It also had automatic questionnaire completion, notification emails, score addition to questionnaires, prevention of multiple answer submissions, and the ability to upload files up to 4 gigabytes. Student authentication was based on national identification numbers and student IDs, serving as user IDs and passwords. Students could enter the exam environment using their email and multi-level personal information verification. If the information did not match, individuals could not access the exam environment.
Checklists and questionnaires
A student list was prepared, and checklists for the in-person exam and anxiety and satisfaction questionnaires were reproduced.
Empowerment workshops for professors and education staff
Educational needs of faculty members and academic staff include conducting clinical competency exams using the OSCE method; simulating and evaluating OSCE exams; designing standardized questions, checklists, and scenarios; innovative approaches in clinical evaluations; designing physical spaces and setting up stations; and assessing ethics and professional commitment in clinical competency exams.
Student empowerment programs
According to the students’ needs assessment results, in-person workshops on cardiopulmonary resuscitation and airway management and online workshops were held on health, pediatrics, cardiopulmonary resuscitation, ethics, nursing diagnosis, and report writing through Skype messenger. In addition, vaccination notes, psychiatric nursing, and educational files on clinical examinations and basic skills were recorded by instructors and made available to students via virtual groups.
Step 3: CCE implementation
The CCE was held in two parts, in-person and virtual.
In-person exam
The OSCE method was used for this section of the exam. The basic skills station exam included dressing and injections, and the CPR and pediatrics stations were conducted in person. The students were divided into two groups of 21 each semester, and the exam was held in two shifts. While adhering to quarantine protocols, the students performed the procedures for seven minutes at each station, and instructors evaluated them using a checklist. An additional minute was allotted for transitioning to the next station.
Virtual exam
The professional ethics, nursing diagnosis, nursing report, health, psychiatric nursing, and physical examination stations were conducted virtually after the in-person exam. This exam was made available to students via a primary and a secondary link in a virtual space at the scheduled time. Students were first verified, and after the specified time elapsed, the ability to respond to inactive questions and submitted answers was sent. During the exam, full support was provided by the examination center.
The examination coordinator conducted the entire virtual exam process. The exam results were announced 48 h after the exam. A passing grade was considered to be a score higher than 60% in all stations. Students who failed in various stations were given the opportunity for remediation based on faculty feedback, either through additional study or participation in educational workshops. Subsequent exams were held one week apart from the initial exam. It was stipulated that students who failed in more than half of the stations would be evaluated in the following semester. If they failed in more than three sessions at a station, a decision would be made by the faculty’s educational council. However, no students met these situations.
Step 4: Evaluation
The evaluation of the exam was conducted by examiners using a checklist, and the results were announced as pass or fail.
Stage 4: Observation / evaluation
In this study, both process and outcome evaluations were conducted:
Process evaluation
All programs and activities implemented during the test design and administration process were evaluated in the process evaluation. This evaluation was based on operational program control and reflections received from participants through group discussion sessions and virtual groups.
Sample reflections received from faculty members, managers, experts, and students through group discussions and social messaging platforms after the changes:
P7: “The implementation of the blended virtual exam, in the conditions of the COVID-19 crisis where the possibility of holding in-person exams was not fully available, in my opinion, was able to improve the quality of exam administration and address the limitations and weaknesses of the exam entirely virtually.”
P5: “In my opinion, this blended method was able to better evaluate students in terms of clinical readiness for entering clinical practice.”
Outcomes evaluation
The study outcomes were student anxiety, student acceptance and satisfaction, and faculty acceptance and satisfaction. Before the start of the in-person and virtual exams, the Spielberger Anxiety Questionnaire was provided to students. Additionally, immediately after the exam, students and instructors completed the acceptance and satisfaction questionnaire for the relevant section. After the exam, students and instructors completed the acceptance and satisfaction questionnaire again for the entire exam process, including feasibility, satisfaction with its implementation, and educational impact.

Design framework and implementation for the blended Clinical Competency Examination
The exam was planned using a blended method (part in-person, part virtual) according to the Fig. 2 schedule, and all planned programs for the blended CCE for final-year nursing students were implemented in two semesters.
Evaluation results
In this study, 84 final-year nursing students participated, including 37 females (44.05%) and 47 males (55.95%). Among them, 28 (33.3%) were dormitory residents, and 56 (66.7%) were non-dormitory residents.
In this study, both process and outcome evaluations were conducted.
All programs and activities implemented during the test design and administration process were evaluated in the process evaluation (Table 2 ). This evaluation was based on operational program control and reflections received from participants through group discussion sessions and virtual groups on social media.
Anxiety and satisfaction were examined and evaluated as study outcomes, and the results are presented below.
The paired t-test results in Table 3 showed no statistically significant difference in overt anxiety ( p = 0.56), covert anxiety ( p = 0.13), and total anxiety scores ( p = 0.167) between the in-person and virtual sections before the blended Clinical Competency Examination.
However, the mean (SD) of overt anxiety in persons in males and females was 49.27 (11.16) and 43.63 (13.60), respectively, and this difference was statistically significant ( p = 0.03). Also, the mean (SD) of overt virtual anxiety in males and females was 45.70 (11.88) and 51.00 (9.51), respectively, and this difference was statistically significant ( p = 0.03). However, there was no significant difference between males and females regarding covert anxiety in the person ( p = 0.94) and virtual ( p = 0.60) sections. In addition, the highest percentage of overt anxiety was apparent in the virtual section among women (15.40%) and the in-person section among men (21.28%) and was prevalent at a moderate to high level.
According to Table 4 , One-way analysis of variance showed a significant difference between the virtual, in-person, and blended sections in terms of acceptance and satisfaction scores.
The results of the One-way analysis of variance showed that the mean (SD) acceptance and satisfaction scores of nursing students of the CCE in virtual, in-person, and blended sections were 25.49 (4.73), 27.60 (4.70), and 25.57 (4.97) out of 30, respectively. There was a significant difference between the three sections ( p = 0.008).
In addition, 3 (7.23%) male and 10 (76.3%) female faculty members participated in this study; of this number, 2 (15.38%) were instructors, and 11 (84.62%) were assistant professors. Moreover, they were between 29 and 50 years old, with a mean (SD) of 41.37 (6.27). Furthermore, they had 4 to 20 years of work experience with a mean and standard deviation of 13.22(4.43).
The results of the analysis of variance showed that the mean (SD) acceptance and satisfaction scores of faculty members of the CCE in virtual, in-person, and blended sections were 30.31 (4.47), 29.86 (3.94), and 30.00 (4.16) out of 33, respectively. There was no significant difference between the three sections ( p = 0.864).
This action research study showed that the blended CCE for nursing students is feasible and, depending on the conditions and objectives, evaluation stations can be designed and implemented virtually or in person.
The blended exam, combining in-person and virtual elements, managed to address some of the weaknesses of entirely virtual exams conducted in previous terms due to the COVID-19 pandemic. Given the pandemic conditions, the possibility of performing all in-person stations was not feasible due to the risk of students and evaluators contracting the virus, as well as the need for prolonged quarantine. Additionally, to meet the staffing needs of hospitals, nursing students needed to graduate. By implementing the blended exam idea and conducting in-person evaluations at clinical stations, the assessment of nursing students’ clinical competence was brought closer to reality compared to the entirely virtual method.
Furthermore, the need for human resources, station setup costs, and time spent was less than the entirely in-person method. Therefore, in pandemics or conditions where sufficient financial resources and human resources are not available, the blended approach can be utilized.
Additionally, the evaluation results showed that students’ total and overt anxiety in both virtual and in-person sections of the blended CCE did not differ significantly. However, the overt anxiety of female students in the virtual section and male students in the in-person section was considerably higher. Nevertheless, students’ covert anxiety related to personal characteristics did not differ in virtual and in-person exam sections. However, students’ acceptance and satisfaction in the in-person section were higher than in the virtual and blended sections, with a significant difference. The acceptance and satisfaction of faculty members from the CCE in in-person, virtual, and blended sections were the same and relatively high.
A blended CCE nursing competency exam was not found in the literature review. However, recent studies, especially during the COVID-19 pandemic, have designed and implemented this exam using virtual OSCE. Previously, the CCE was held in-person or through traditional OSCE methods.
During the COVID-19 pandemic, nursing schools worldwide faced difficulties administering clinical competency exams for students. The virtual simulation was used to evaluate clinical competency and develop nursing students’ clinical skills in the United States, including standard videos, home videos, and clinical scenarios. Additionally, an online virtual simulation program was designed to assess the clinical competency of senior nursing students in Hong Kong as a potential alternative to traditional clinical training [ 31 ].
A traditional in-person OSCE was also redesigned and developed through a virtual conferencing platform for nursing students at the University of Texas Medical Branch in Galveston. Survey findings showed that most professors and students considered virtual OSCE a highly effective tool for evaluating communication skills, obtaining a medical history, making differential diagnoses, and managing patients. However, professors noted that evaluating examination techniques in a virtual environment is challenging [ 32 ].
However, Biranvand reported that less than half of the nursing students believed the in-person OSCE was stressful [ 33 ]. At the same time, the results of another study showed that 96.2% of nursing students perceived the exam as anxiety-provoking [ 1 ]. Students believe that the stress of this exam is primarily related to exam time, complexity, and the execution of techniques, as well as confusion about exam methods [ 7 ]. In contrast to previous research results, in a study conducted in Egypt, 75% of students reported that the OSCE method has less stress than other examination methods [ 9 ]. However, there has yet to be a consensus across studies on the causes and extent of anxiety-provoking in the OSCE exam. In a study, the researchers found that in addition to the factors mentioned above, the evaluator’s presence could also be a cause of stress [ 34 ]. Another survey study showed that students perceived the OSCE method as more stressful than the traditional method, mainly due to the large number of stations, exam items, and time constraints [ 7 ]. Another study in Egypt, which designed two stages of the OSCE exam for 75 nursing students, found that 65.6% of students reported that the second stage exam was stressful due to the problem-solving station. In contrast, only 38.9% of participants considered the first-stage exam stressful [ 35 ]. Given that various studies have reported anxiety as one of the disadvantages of the OSCE exam, in this study, one of the outcomes evaluated was the anxiety of final-year nursing students. There was no significant difference in total anxiety and overt anxiety between students in the in-person and virtual sections of the blended Clinical Competency Examination. The overt anxiety was higher in male students in the in-person part and female students in the virtual section, which may be due to their personality traits, but further research is needed to confirm this. Moreover, since students’ total and overt anxiety in the in-person and virtual sections of the exam are the same in resource and workforce shortages or pandemics, the blended CCE is suggested as a suitable alternative to the traditional OSCE test. However, for generalization of the results, it is recommended that future studies consider three intervention groups, where all OSCE stations are conducted virtually in the first group, in-person in the second group, and a blend of in-person and virtual in the third group. Furthermore, the results of the study by Rafati et al. showed that the use of the OSCE clinical competency exam using the OSCE method is acceptable, valid, and reliable for assessing nursing skills, as 50% of the students were delighted, and 34.6% were relatively satisfied with the OSCE clinical competency exam. Additionally, 57.7% of the students believed the exam revealed learning weaknesses [ 1 ]. Another survey study showed that despite higher anxiety about the OSCE exam, students thought that this exam provides equal opportunities for everyone, is less complicated than the traditional method, and encourages the active participation of students [ 7 ]. In another study on maternal and infant care, 95% of the students believed the traditional exam only evaluates memory or practical skills. In contrast, the OSCE exam assesses knowledge, understanding, cognitive and analytical skills, communication, and emotional skills. They believed that explicit evaluation goals, appropriate implementation guidelines, appropriate scheduling, wearing uniforms, equipping the workroom, evaluating many skills, and providing fast feedback are among the advantages of this exam [ 36 ]. Moreover, in a survey study, most students were satisfied with the clinical environment offered by the OSCE CCE using the OSCE method, which is close to reality and involves a hypothetical patient in necessary situations that increase work safety. On the other hand, factors such as the scheduling of stations and time constraints have led to dissatisfaction among students [ 37 ].
Furthermore, another study showed that virtual simulations effectively improve students’ skills in tracheostomy suctioning, triage concepts, evaluation, life-saving interventions, clinical reasoning skills, clinical judgment skills, intravenous catheterization skills, role-based nursing care, individual readiness, critical thinking, reducing anxiety levels, and increasing confidence in the laboratory, clinical nursing education, interactive communication, and health evaluation skills. In addition to knowledge and skills, new findings indicate that virtual simulations can increase confidence, change attitudes and behaviors, and be an innovative, flexible, and hopeful approach for new nurses and nursing students [ 38 ].
Various studies have evaluated the satisfaction of students and faculty members with the OSCE Clinical Competency Examination. In this study, one of the evaluated outcomes was the acceptability and satisfaction of students and faculty members with implementing the CCE in blended, virtual, and in-person sections, which was relatively high and consistent with other studies. One crucial factor that influenced the satisfaction of this study was the provision of virtual justification sessions for students and coordination sessions with faculty members. Social messaging groups were formed through virtual and in-person communication, instructions were explained, expectations and tasks were clarified, and questions were answered. Students and faculty members could access the required information with minimal presence in medical education centers and time and cost constraints. Moreover, with the blended evaluation, the researcher’s communication with participants was more accessible. The written guidelines and uploaded educational content of the workshops enabled students to save the desired topics and review them later if needed. Students had easy access to scientific and up-to-date information, and the application of social messengers and Skype allowed for sending photos and videos, conducting workshops, and questions and answering questions. However, the clinical workshops and examinations were held in-person to ensure accuracy. The virtual part of the examination was conducted through online software, and questions focused on each station’s clinical and practical aspects. Students answered various questions, including multiple-choice, descriptive, scenario, picture, and puzzle questions, within a specified time. The blended examination evaluated clinical competency and did not delay these individuals’ entry into the job market. Moreover, during the severe human resource shortage faced by the healthcare system, the examination allowed several nurses to enter the country’s healthcare system. The blended examination can substitute in-person examination in pandemic and non-pandemic situations, saving facilities, equipment, and human resources. The results of this study can also serve as a model to guide other nursing departments that require appropriate planning and arrangements for Conducting Clinical Competency Examinations in blended formats. This examination can also be developed to evaluate students’ clinical performance.
One of the practical limitations of the study was the possibility that participants might need to complete the questionnaires accurately or be concerned about losing marks. Therefore, in a virtual session before the in-person exam, the objectives and importance of the study were explained. Participants were assured that it would not affect their evaluation and that they should not worry about losing marks. Additionally, active participation from all nursing students, faculty members, and staff was necessary for implementing this plan, achieved through prior coordination, virtual meetings, virtual group formation, and continuous reflection of results, creating the motivation for continued collaboration and participation.
Among other limitations of this study included the use of the Spielberger Anxiety Questionnaire to measure students’ anxiety. It is suggested that future studies use a dedicated anxiety questionnaire designed explicitly for pre-exam anxiety measurement. Another limitation of the current research was its implementation in nursing and midwifery faculty. Therefore, it is recommended that similar studies be conducted in nursing and midwifery faculties of other universities, as well as in related fields, and over multiple consecutive semesters. Additionally, for more precise effectiveness assessment, intervention studies in three separate virtual, in-person, and hybrid groups using electronic checklists are proposed. Furthermore, it is recommended that students be evaluated in terms of other dimensions and variables such as awareness, clinical skill acquisition, self-confidence, and self-efficacy.
Conducting in-person Clinical Competency Examination (CCE) during critical situations, such as the COVID-19 pandemic, is challenging. Instead of virtual exams, blended evaluation is a feasible approach to overcome the shortages of virtual ones and closely mimic in-person scenarios. Using a blended method in pandemics or resource shortages, it is possible to design, implement, and evaluate stations that evaluate basic and advanced clinical skills in in-person section, as well as stations that focus on communication, reporting, nursing diagnosis, professional ethics, mental health, and community health based on scenarios in a virtual section, and replace traditional OSCE exams. Furthermore, the use of patient simulators, virtual reality, virtual practice, and the development of virtual and in-person training infrastructure to improve the quality of clinical education and evaluation and obtain the necessary clinical competencies for students is recommended. Also, since few studies have been conducted using the blended method, it is suggested that future research be conducted in three intervention groups, over longer semesters, based on clinical evaluation models and influential on other outcomes such as awareness and clinical skill acquisition self-efficacy, confidence, obtained grades, and estimation of material and human resources costs. This approach reduced the need for physical space for in-person exams, ensuring participant quarantine and health safety with higher quality. Additionally, a more accurate assessment of nursing students’ practical abilities was achieved compared to a solely virtual exam.
Data availability
The datasets generated and analyzed during the current study are available on request from the corresponding author.
Rafati F, Pilevarzade M, Kiani A. Designing, implementing and evaluating once to assess nursing students’ clinical competence in Jiroft faculty of nursing and midwifery. Nurs Midwifery J. 2020;18(2):118–28.
Google Scholar
Sadeghi T, Ravari A, Shahabinejad M, Hallakoei M, Shafiee M, Khodadadi H. Performing of OSCE method in nursing students of Rafsanjan University of Medical science before entering the clinical field in the year 2010: a process for quality improvement. Community Health J. 2012;6(1):1–8.
Ali GA, Mehdi AY, Ali HA. Objective structured clinical examination (OSCE) as an assessment tool for clinical skills in Sohag University: nursing students’ perspective. J Environ Stud. 2012;8(1):59–69.
Article Google Scholar
Bolourchifard F, Neishabouri M, Ashktorab T, Nasrollahzadeh S. Satisfaction of nursing students with two clinical evaluation methods: objective structured clinical examination (OSCE) and practical examination of clinical competence. Adv Nurs Midwifery. 2010;19(66):38–42.
Noohi E, Motesadi M, Haghdoost A. Clinical teachers’ viewpoints towards Objective Structured Clinical examination in Kerman University of Medical Science. Iran J Med Educ. 2008;8(1):113–20.
Reza Masouleh S, Zare A, Chehrzad M, Atrkarruoshan Z. Comparing two methods of evaluation, objective structured practical examination and traditional examination, on the satisfaction of students in Shahid Beheshti faculty of nursing and midwifery. J Holist Nurs Midwifery. 2008;18(1):22–30.
Bagheri M, Sadeghineajad Forotagheh M, Shaghayee Fallah M. The comparison of stressors in the assessment of basic clinical skills with traditional method and OSCE in nursing students. Life Sci J. 2012;9(4):1748–52.
Eldarir SH, El Sebaae HA, El Feky HA, Hussein HA, El Fadil NA, El Shaeer IH. An introduction of OSCE versus the traditional method in nursing education: Faculty capacity building and students’ perspectives. J Am Sci. 2010;6(12):1002–14.
Al-Zeftawy AM, Khaton SE. Student evaluation of an OSCE in Community Health nursing clinical course at Faculty of nursing, Tanta University. J Nurs Health Sci. 2016;5(4):68–76.
Hayter M, Jackson D. Pre-registration undergraduate nurses and the COVID-19 pandemic: students or workers? J Clin Nurs. 2020;29(17–18):3115–6.
Bayham J, Fenichel EP. Impact of school closures for COVID-19 on the US health-care workforce and net mortality: a modeling study. Lancet Public Health. 2020;5(5):e271–8.
Murphy MPA. COVID-19 and emergency eLearning: consequences of the securitization of higher education for post-pandemic pedagogy. Contemp Secur Policy. 2020;41(3):492–505.
Allen IE, Seaman J. Learning on demand: Online education in the United States, 2009.
Meyer KA, Wilson JL. The role of Online Learning in the emergency plans of Flagship Institutions. Online J Distance Learn Adm. 2011;14(1):110–8.
Kursumovic E, Lennane S, Cook TM. Deaths in healthcare workers due to COVID-19: the need for robust data and analysis. Anaesthesia. 2020;75(8):989–92.
Malekshahi Beiranvand F, Hatami Varzaneh A. Health care workers challenges during coronavirus outbreak: the qualitative study. J Res Behav Sci. 2020;18(2):180–90.
Boursicot K, Kemp S, Ong TH, Wijaya L, Goh SH, Freeman K, Curran I. Conducting a high-stakes OSCE in a COVID-19 environment. MedEdPublish. 2020;9:285–89.
Atwa H, Shehata MH, Al-Ansari A, Kumar A, Jaradat A, Ahmed J, Deifalla A, Online. Face-to-Face, or blended learning? Faculty and Medical Students’ perceptions during the COVID-19 pandemic: a mixed-method study. Front Med. 2022;9:791352.
Chan MMK, Yu DS, Lam VS, Wong JY. Online clinical training in the COVID-19 pandemic. Clin Teach. 2020;17(4):445–6.
Toulabi T, Yarahmadi S. Conducting a clinical competency test for nursing students in a virtual method during the Covid-19 pandemic: a case study. J Nurs Educ. 2021;9(5):33–42.
Meskell P, Burke E, Kropmans TJB, Byrne E, Setyonugroho W, Kennedy KM. Back to the future: an online OSCE Management Information System for nursing OSCEs. Nurse Educ Today. 2015;35(11):1091–6.
Lichtenberg PA. (2010). Handbook of Assessment in Clinical Gerontology, 2nd Ed. Academic Press, https://doi.org/10.1016/B978-0-12-374961-1.10030-2
Gholami Booreng F, Mahram B, Kareshki H. Construction and validation of a scale of research anxiety for students. IJPCP. 2017;23(1):78–93.
Esmaili M. A survey of the influence of Murita therapy on reducing the rate of anxiety in clients of counseling centers. Res Clin Psychol Couns. 2011;1(1):15–30.
Farajpour A, Amini M, Pishbin E, Arshadi H, Sanjarmusavi N, Yousefi J, Sarafrazyazdi M. Teachers’ and students’ satisfaction with DOPS Examination in Islamic Azad University of Mashhad, a study in Year 2012. Iran J Med Educ. 2014;14(2):165–73.
StraussAC, Corbin JM. Basics of qualitative research: grounded theory procedures and technique. 2nd ed. London: Sage, Newbury Park; 1998.
Dickens L, Watkins K. Action research: rethinking Lewin. Manage Learn. 1999;30(2):127–40.
Rezaeerad M, Nadri Kh, Mohammadi Etergoleh R. The effect of ADDIE (analysis, design, development, implementation, evaluation) designing method with emphasizing on mobile learning on students’ self-conception, development motivation and academic development in English course. Educational Adm Res Q. 2013;4(15):15–32.
Ben-David MF. AMEE Guide 18: standard setting in student assessment. Med Teach. 2000;22(2):120–30.
McKinley DW, Norcini JJ. How to set standards on performance-based examinations: AMEE Guide 85. Med Teach. 2014;36(2):97–110.
Fung JTC, Zhang W, Yeung MN, Pang MTH, Lam VSF, Chan BKY, Wong JYH. Evaluation of students perceived clinical competence and learning needs following an online virtual simulation education programmed with debriefing during the COVID-19 pandemic. Nurs Open. 2021;8(6):3045–54.
Luke S, Petitt E, Tombrella J, McGoff E. Virtual evaluation of clinical competence in nurse practitioner students. Med Sci Educ. 2021;31:1267–71.
Beiranvand SH, Hosseinabadi R, Ghasemi F, Anbari KH. An Assessment of nursing and Midwifery Student Veiwwpoin, Performance, and feedback with an objective structured clinical examination. J Nurs Educ. 2017;6(1):63–7.
Sheikh Abumasoudi R, Moghimian M, Hashemi M, Kashani F, Karimi T, Atashi V. Comparison of the Effect of Objective Structured Clinical evaluation (OSCE) with Direct and Indirect Supervision on nursing student’s test anxiety. J Nurs Educ. 2015;4(2):1–8.
Zahran EM, Taha EE. Students’ feedback on Objective Structured Clinical examinations (OSCEs) experience in emergency nursing. J High Inst Public Health. 2009;39(2):370–87.
Na A-G. Assessment of Students’ knowledge, clinical performance and satisfaction with objective structured clinical exam. Med J Cairo Univ. 2009;77(4):287–93.
Adib-Hajbaghery M, Yazdani M. Effects of OSCE on learning, satisfaction and test anxiety of nursing students: a review study. Iran J Med Educ. 2018;18:70–83.
Purwanti LE, Sukartini T, Kurniawati ND, Nursalam N, Susilowati T. Virtual Simulation in clinical nursing education to improve knowledge and clinical skills: Literature Review. Open Access Maced J Med Sci. 2022;10(F):396–404.
Download references
Acknowledgements
We want to thank the Research and Technology deputy of Smart University of Medical Sciences, Tehran, Iran, the faculty members, staff, and officials of the School of Nursing and Midwifery, Lorestan University of Medical Sciences, Khorramabad, Iran, and all individuals who participated in this study.
All steps of the study, including study design and data collection, analysis, interpretation, and manuscript drafting, were supported by the Deputy of Research of Smart University of Medical Sciences.
Author information
Authors and affiliations.
Department of E-Learning in Medical Education, Center of Excellence for E-learning in Medical Education, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran
Rita Mojtahedzadeh & Aeen Mohammadi
Department of Medical Education, Smart University of Medical Sciences, Tehran, Iran
Tahereh Toulabi
Cardiovascular Research Center, School of Nursing and Midwifery, Lorestan University of Medical Sciences, Khorramabad, Iran
You can also search for this author in PubMed Google Scholar
Contributions
RM. Participating in study design, accrual of study participants, review of the manuscript, and critical revisions for important intellectual content. TT : The investigator; participated in study design, data collection, accrual of study participants, and writing and reviewing the manuscript. AM: Participating in study design, data analysis, accrual of study participants, and reviewing the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Tahereh Toulabi .
Ethics declarations
Ethics approval and consent to participate.
This action research was conducted following the participatory method. All methods were performed according to the relevant guidelines and regulations in the Declaration of Helsinki (ethics approval and consent to participate). The study’s aims and procedures were explained to all participants, and necessary assurance was given to them for the anonymity and confidentiality of their information. The results were continuously provided as feedback to the participants. Informed consent (explaining the goals and methods of the study) was obtained from participants. The Smart University of Medical Sciences Ethics Committee approved the study protocol (IR.VUMS.REC.1400.011).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Mojtahedzadeh, R., Toulabi, T. & Mohammadi, A. The design, implementation, and evaluation of a blended (in-person and virtual) Clinical Competency Examination for final-year nursing students. BMC Med Educ 24 , 936 (2024). https://doi.org/10.1186/s12909-024-05935-9
Download citation
Received : 21 July 2023
Accepted : 20 August 2024
Published : 28 August 2024
DOI : https://doi.org/10.1186/s12909-024-05935-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Clinical Competency Examination (CCE)
- Objective Structural Clinical Examination (OSCE)
- Blended method
- Satisfaction
BMC Medical Education
ISSN: 1472-6920
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
A qualitative study of stressors faced by older stroke patients in a convalescent rehabilitation hospital
Roles Formal analysis, Investigation, Methodology, Writing – original draft
* E-mail: [email protected]
Affiliation Department of Occupational Therapy, Tokyo Bay Rehabilitation Hospital, Narashino, Chiba, Japan
Roles Writing – review & editing
Affiliation Department of Occupational Therapy, Teikyo Heisei University, Toshima, Tokyo, Japan
Affiliation Department of Occupational Therapy, Saitama Medical Center, Kawagoe, Saitama, Japan
Affiliation Faculty of Human Sciences, Graduate School of Comprehensive Human Sciences, University of Tsukuba, Ibaraki, Japan
- Yuta Asada,
- Kaori Nishio,
- Kohei Iitsuka,

- Published: August 26, 2024
- https://doi.org/10.1371/journal.pone.0309457
- Peer Review
- Reader Comments
This study aimed to explore the stressors experienced by older patients with stroke in convalescent rehabilitation wards in Japan. Semi-structured interviews were conducted with four stroke patients aged > 65 years who experienced a stroke for the first time in their lives. The interviews were analyzed using the Steps for Coding and Theorization method for qualitative data analysis. The results of the qualitative analysis demonstrated that patients experienced specific stressors, such as, difficulty in movement of the paralyzed hand, fear of stroke recurrence, and dietary problems. Some stressors were manageable through healthcare professionals’ active and sensitive communication strategies. These stressors were derived from the theoretical framework of “stressors related to hospitalization” and “stressors related to the illness”. Additional stressors emerged from the interaction between these two types within the theoretical framework. The results of this study contribute to a deeper understanding of the specific stressors experienced by older stroke patients during the recovery process.
Citation: Asada Y, Nishio K, Iitsuka K, Yaeda J (2024) A qualitative study of stressors faced by older stroke patients in a convalescent rehabilitation hospital. PLoS ONE 19(8): e0309457. https://doi.org/10.1371/journal.pone.0309457
Editor: Chinh Quoc Luong, Bach Mai Hospital, VIET NAM
Received: February 24, 2024; Accepted: August 13, 2024; Published: August 26, 2024
Copyright: © 2024 Asada et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting Information files.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Stress is a nonspecific response of the body to external stimuli [ 1 ]. Stress varies as the stressors faced by individuals differ depending on their age, sex, and social role [ 2 ]. Stressors include physical, biological, chemical, psychological, and social factors. The accumulation of these stressors causes stress, which, if not adequately addressed, can lead to physical or mental health problems, such as cardiovascular disease and depression, respectively [ 3 ]. To prevent these stress-related diseases, it is imperative to identify and address the stressors.
Patients often face various stressors in inpatient settings as their physical and human environments differ significantly from those of their regular home settings [ 4 ]. As the length of the hospital stay increases, patients may become particularly vulnerable to stressors such as “concern for family” and “anxiety about financial situation” [ 4 ]. The severity of a stroke, the age of the patient, and the presence of underlying medical conditions are factors that tend to extend the duration of hospitalization [ 5 ]. The incidence of stroke increases with age and is more common among older adults [ 6 ]. Moreover, patients present with a variety of symptoms, such as motor paralysis and higher brain dysfunction, and their ability to perform activities of daily living (ADL) becomes more limited. In particular, convalescent rehabilitation hospitals have a prolonged hospital stay [ 7 ] as one of their goals is to help patients return to the community and their homes.
Much of what is known about stressors related to stroke involves the risk of stroke onset [ 8 , 9 ], and there are insufficient studies on the stressors faced by older stroke patients in hospitals. Clarifying these unspoken stressors can contribute to reducing the stress of hospitalization for older stroke patients during convalescent rehabilitation, meeting their true needs, and enriching their lives after discharge. Few studies have elicited patients’ true feelings regarding stressors in convalescent rehabilitation wards. The purpose of this study is to provide a deeper understanding of the specific stressors experienced by older stroke patients in convalescent rehabilitation wards during their hospital stay.
Materials and methods
We conducted a qualitative study and interviewed each participant separately. The interview transcripts were analyzed according to the “Steps for Coding and Theorization” method (SCAT), a sequential and thematic qualitative data analysis technique [ 10 – 12 ].
This study was conducted in accordance with the Consolidated Criteria for Reporting Qualitative Research (COREQ), a checklist designed to improve the transparency and reliability of qualitative research [ 13 ] (S1 Table in S1 File ).
Preparation for the study
The first author (hereafter, “the author”) is a M.S. student in comprehensive human sciences and male occupational therapist with six years of clinical experience in recovery rehabilitation. Before this study was conducted, the author reviewed the literature on SCAT, conducted an analysis, and attended a workshop for SCAT developers to deepen his understanding of the analysis methods to ensure the accuracy of the analysis [ 10 – 12 ].
Participants
Patients aged 65 years or older, experiencing stroke for the first time, and hospitalized in a recovery center were included in the study. Patients who had difficulty answering the interview questions owing to the effects of aphasia, hospitalized patients in the charge of an interviewer, patients diagnosed with dementia or psychiatric disorders, and patients who were hospitalized for a short period of approximately one month were excluded.
Patients were asked to cooperate in the study and fully informed about the purpose and significance of the study, research methods, voluntary nature of research cooperation and freedom to withdraw, and handling of personal information. Signing a consent form indicated patients’ willingness to cooperate in the study.
Interview procedure
Three interviews were conducted between June and November, 2022. The interviewer asked questions according to an interview guide. Semi-structured in-person interviews were conducted in a private room in the hospital that the author is affiliated with, involving the patients and interviewer only. The first interview was conducted at the time of hospital admission, and subsequent interviews were conducted several times, with a gap of approximately one month. The interviews were recorded with the participants’ consent using the voice recorder function of an iPad and transcribed afterwards. The interview transcripts were not returned to participants for comments or correction. The interviewer recited the patients’ statements to them and made efforts to confirm the content of the statements to ensure data accuracy.
The interview guide was developed based on a preliminary survey of two stroke patients to determine ease of response. The content of the interview guide was first explained to the participants through specific examples to help them fully understand the difference between “stress” and “stressors.” The guide began by explaining, through specific examples, what the stressors in this study were. To investigate the stressors faced by older stroke patients in recovery, we asked, “What comes to mind when you hear the term ‘stressors in hospitalization’?”
Data analysis
We predicted that the outcome of the interviews would be strongly influenced by the participants’ individual characteristics. Therefore, to obtain objective results, we used the SCAT technique that specializes in coding and theorization and can be applied to a small amount of data. The SCAT method consists of the following steps [ 10 – 12 ]:
Step 1: Focus words from within the interview texts.
Step 2: Words outside the text that can replace the words from Step 1.
Step 3: Words that explain the words in Step 1 and Step 2.
Step 4: Themes and constructs, including the process of writing a story and offering theories that weave the themes and constructs together.
As this study was designed to create multiple storylines from a single participant, we integrated those multiple storylines into a single storyline and wrote a theoretical description, ensuring no loss of chronological contextuality and individuality of the storylines. The data analysis and confirmation process were conducted by the author and three other authors who were not involved in the interview process.
Ethical considerations
This study was approved by the Ethical Review Committee (Approval No. 289–2) of Tokyo Bay Rehabilitation Hospital.
Basic attributes of the participants
Five participants who met the inclusion criteria were recruited for the study. One participant (female) was excluded owing to early discharge from the hospital on short notice. Thus, four patients (two male and two female) were included in the study. The participants’ average age was 79.3 years (range: 71–88 years). Their disabilities included cerebral hemorrhage (one patient) and cerebral infarctions (three patients).
The average duration of the series of 12 interviews was 20.3 minutes, ranging from 7.5 to 32.7 minutes.
Storyline and theoretical descriptions
In the sections below, the storylines and theoretical descriptions as well as quotes from each participant, are described.
Case 1: Mr. A, facing an inconvenient situation.
At the time of the first interview, Mr. A experienced stress owing to an inconvenient situation during hospitalization. He was unable to perform the activities he did before the onset of the disease, especially owing to the psychological burden caused by the inability to eat and drink according to his preferences. He also expressed dissatisfaction with the current situation, limitations in leisure-time activities, inconvenience of activities, and a sense of shame caused by assistance with bathing. Limited leisure-time activities resulted from challenges in moving his paralyzed hands. He specifically encountered difficulties in willingly engaging them to act. Furthermore, he was separated from his family as a result of hospitalization. Thus, he faced restrictions in eating and drinking luxury foods, lack of freedom in daily life, and lack of family time.
“ Not being able to do things freely is the biggest stressor. All in all, there’s nothing better than that. I can’t eat what I like, or drink a lot. Even if I have a computer, I can’t use my right hand. I can’t even do my own hobbies. And, it is still significant whether or not you have a wife nearby.”
At the time of the second interview, Mr. A experienced stress regarding eating and drinking, including dissatisfaction with the variety of meals compared to before the disease onset, and the psychological burden owing to meals not being replaced on a daily basis. This was also the minimum element that Mr. A looked for during hospitalization. Other stress factors included a feeling of disappointment owing to limited leisure-time activities, and feelings of activity limitation and resignation owing to the inability to walk independently.
“ The most important thing is the food. Anyway, there’s nothing to do, so at least a meal, you’d think, wouldn’t you? The food is different from when we’re at home. It doesn’t help that I can’t walk. And, I think it’s a bit hard not to have hobbies.”
At the time of the third interview, Mr. A expressed that his biggest stress factor was difficulty moving his paralyzed dominant hand. This significantly impacted his daily self-care, including toileting and grooming. He also encountered limitations in various leisure activities, such as reading books. Eating and drinking induced a significant psychological burden. He felt dissatisfied with the lack of variety in meals as he could not manage to eat as well as previously.
“ Whatever I do, my hands don’t work. For example, when you brush your teeth. It’s the same when you go to the toilet and wipe your bottom. I can’t use my right hand. Also, I like books and I want to read, but I can’t turn the pages. And, unlike in the past, I eat rice and side dishes every day. My eating habits have changed drastically.”
Case 2: Ms. B, facing stressors caused by communal living.
At the time of the first interview, Ms. B faced stressors related to basic lifestyle habits, such as falling asleep and toileting, in the hospital. Variations in individual lifestyles and environmental factors, like noise and room brightness, contributed to sleep deprivation in shared living arrangements. Furthermore, inadequate management of the paralyzed side during sleep led to anxiety and sleep deprivation. Problems related to toileting needs arose owing to overlap in toilet timings with roommates and assisted by staff of the opposite sex.
“ I sometimes have trouble sleeping well at night because of noises or brightness. Everyone is trying to go to the toilet before rehabilitation, so the timing is… And with male nurses, there was a bit of resistance to using the toilet. After all, in shared living arrangements, everyone has a different rhythm of life.”
During the second interview, Ms. B continued to face stress owing to communal living. Stressors included abnormal breathing noises caused by roommates when falling asleep, noise problems during roommates’ movements, and nocturnal awakenings caused by physical environmental factors such as differences in depth of sleep. Additionally, there were case of sleep problems caused by the staff’s response to a roommate’s problematic behavior, and case of nocturnal awakenings caused by noise from staff responses. Other issues included self-perceived persistent distress over defecation problems and dealing with defecation needs in a time-constrained environment, with a roommate.
“ Like last time, in shared living arrangements, everyone has a different rhythm of life, but it can’t be helped. Sleep, you know, because some people go to the toilet at night or early in the morning, so it’s quite noisy and you can’t sleep well. And the nurse puts the patient next to me to sleep, and there are all sorts of noises when she does that. We all have the same desire to go to the toilet before rehabilitation, so we don’t make it in time. Toilets are a perpetual problem.”
At the time of the third interview, Ms. B had problems with how he interacted with his roommates and stressors related to falling asleep at night. Ms. B was dissatisfied with differences in personal characteristics in communal living, and concerned about the deterioration of his relationship with his roommates over defecation. Furthermore, stress was caused by differences in lifestyle in communal living affecting sleep and awakening during the night owing to physical environmental factors such as noises made by roommates. Sudden changes in training hours also caused dissatisfaction.
“ Like how to communicate with people in the room. Like sleeping. Because of the lights and noise when my roommate goes to the toilet at night. Roommates have different living patterns. In rehabilitation, though, there were some questionable things like time changes.”
Case 3: Ms. C, facing an excrement problem and anxiety about stroke recurrence.
At the time of the first interview, Ms. C faced the problem of excrement in communal living. Dissatisfaction was caused by the suppression of excretory behavior and rejection of excretion in communal living, leading to anxiety. There were also conflicts and a psychological burden caused by the staff’s lack of information sharing, which led to restraining from defecating after unpleasant experiences.
“ I don’t like the situation of one toilet for four people. I and others are suffering. I thought it was hard. I didn’t know that you have to press the nurse call. Then I wished they had told me from the beginning. That was a bit of a shock.”
At the time of the second interview, Ms. C expressed dissatisfaction with their lack of independence in elimination. This led to a sense of aversion caused by dealing with the need to defecate frequently during the night and self-consciousness about requests for nighttime defecation assistance, which, in turn, led to resisting the need to defecate, a distressing experience unique to the patient.
“ I feel bad because I have to go to the toilet in the middle of the night. But I try to be patient. If it was during the day, I would ask the nurse to help me, but at night I would still feel sorry. It’s painful. You have to be experienced to understand.”
At the time of the third interview, Ms. C was anxious about the gap between their life at home after discharge and their life in the hospital and about the gradual decline of their brain functions. They also experienced anxiety owing to the fear of stroke recurrence and an undecided medical support system for the prevention of recurrence. These stressors were related to worry caused by a lack of information sharing by the staff and delays in sharing information about discharge from the hospital.
“ I have a little bit of anxiety about my future and my life. Because I’ve got comfortable here. And I don’t know what I would do if I fell ill again. No one is going to talk to me about it. I’m a bit worried about that. That’s what I’m most worried about.”
Case 4: Mr. D, facing a meal problem.
At the time of the first interview, Mr. D expressed their stress that they had to hold their toileting until the hospital staff arrived when they needed to defecate. This occurred as the hospital staff were extremely busy, and they experienced failure in excretory management. However, at the time of the interview, they were able to use the toilet independently.
“ I’ve had a leak before the nurse came. She can’t come right away, she’s too busy. It’s gone now.”
At the time of the second interview, Mr. D had a low appetite owing to low-temperature meals and refused to eat as a result of inappropriate meal temperature. Additionally, there were difficulties with grooming movements around the use of the wash basin and dealing with the need to defecate in communal living.
“ The rice and side dishes are cold. So I feel sorry to leave it. I can eat it beautifully when it’s warm. But when it’s cold, I just can’t. After the meal, I can’t wash my hands because some people wash their hands in their rooms first. When I want to go into the toilet, there are people ahead of me. It can’t be helped.”
In the third interview, Mr. D felt stress when the meal was not hot enough to eat and lost their appetite. He also felt stress when his mealtime was delayed as it that cause would take time for them to do their personal grooming after returning to their room where their roommate occupied t the wash basin.
“ Side dish is cold. Wish it was room temperature. I eat my meals late, so I’m the last one to go back to my room. So, I can’t wash my hands first.”
In this study, semi-structured interviews were conducted to identify the stressors faced by older patients with stroke during convalescent rehabilitation, throughout hospitalization; data analysis was conducted using SCAT.
Based on the storylines and theoretical descriptions, the stressors experienced by stroke patients were categorized into “stressors related to hospitalization” and “stressors related to the illness” [ 4 ].
Stressors related to hospitalization
The results of this study revealed that older stroke patients in convalescent rehabilitation face stressors related to ADLs, such as eating, sleeping, grooming, and toileting; leisure activities; problems with roommates in communal living; and inability to be with their family members. In this study, the first interview was conducted at the time of admission, and stressors were reported by all participants. Stress during hospitalization is caused by the fact that patients are forced to live a life with less freedom than before [ 4 ].
The psychological burden is particularly high for older adults as they have a reduced ability to adapt to changes in the external environment compared with younger patients [ 14 ]. In light of the above, older stroke patients may face a variety of stressors from the early stages of hospitalization compared with younger patients; therefore, intervention against these stressors is necessary from the early stages of hospitalization.
Factors such as relationships with roommates may lead patients to experience discomfort [ 15 ], and the way patients relate to their roommates is considered important. In this study, physical environmental factors caused by differences in lifestyle and the timing of toilet and wash basin use with roommates emerged as stressors. Additionally, these factors affected the participants’ ADL, such as grooming, toileting, and sleeping. Considering these findings, it is important for patients living together to consider each other’s needs. Therefore, it is necessary for patients to communicate with each other to deepen their understanding, and healthcare professionals are expected to play a role in building such relationships.
Furthermore, stressors such as meal variations and meal temperature emerged rather than stressors such as taste and preference. Older people tend to experience a decline in dietary variety owing to a decline in physical and oral functions and appetite [ 16 ]. Moreover, older patients undergoing treatment for cerebrovascular disease are more likely to experience changes in food preferences than younger patients [ 17 ], which is not consistent with the results of the present study. Given that the amount of food intake in a hospital setting is linked to the quality of food, including taste and the dining environment [ 18 , 19 ], there is a need for further research on qualitative aspects of meal preparation, such as food variations and appropriate temperatures. However, studies on meal variations and temperature are limited. In the future, these should be investigated in detail as characteristic stressors faced by older stroke patients during convalescent rehabilitation.
Stressors related to the disease
The results revealed that older stroke patients in rehabilitation face stressors such as difficulty moving the hand affected by motor paralysis, recurrent strokes, lack of information given by healthcare providers, and inappropriate actions or words of healthcare providers. Approximately 50% of stroke survivors experience unilateral motor paralysis [ 20 ]. Improvement in motor paralysis of the upper limbs and fingers contributes to greater independence in ADL [ 21 , 22 ]. It not only affects ADL but a wide range of activities, such as housework and leisure activities [ 23 , 24 ].
In this study, there were patients whose hobbies were limited by difficulty in moving the paralyzed hand. Additionally, based on the interviews at the time of admission, activity limitation caused by paralysis was a stressor faced from the time of admission itself. Therefore, early interventions and psychological support are needed for patients with paralysis.
A lack of information about the disease may also increase patient anxiety and cause dissatisfaction among healthcare providers [ 4 ]. Stroke recurs at a rate of 2.2% to25.4% within one year of disease onset, 12.9% within two years, and approximately 16% within five years [ 25 ]. Therefore, it is important to support stroke patients to prevent recurrence [ 26 ]. The participants were interviewed before discharge from the hospital about stressors such as recurrent stroke and lack of information provided by healthcare providers. This suggests that providing information to older patients with stroke undergoing convalescent rehabilitation to prevent recurrence is very important, especially for patients who are about to be discharged from the hospital, and that a lack of information can cause stress. Furthermore, communication between stroke patients and healthcare professionals does not always match [ 27 ]. Efforts should be made to prevent a lack of information, considering the patient’s cognitive function and the degree of higher brain dysfunction.
Additionally, stressors such as the personal care of patients by healthcare professionals of the opposite sex, and behaviors and words caused by misunderstandings on the part of healthcare professionals emerged. Patients may experience discomfort and high psychological distress owing to factors such as the attitudes and actions of healthcare workers [ 16 , 28 ]. An inadequate explanation or lack of consideration of shame may also arouse anger in patients [ 29 ]. Stroke patients are placed in a situation where they are prone to feelings of shame owing to assistance with ADL such as bathing and toileting. Therefore, healthcare professionals must be sensitive to patients when providing daily care. Stress can be prevented through appropriate attitude and information sharing.
Various symptoms, such as motor paralysis, sensory disturbance, higher brain dysfunction, and cognitive decline, appear as post-effects of stroke. The complex interplay between these symptoms causes a decline in the ability to perform ADL [ 30 – 32 ]. In this study, there were patients for whom difficulty in achieving independence in ADL was a stressor. Patients with higher levels of ADL independence had higher self-efficacy, and successful experiences were effective in forming self-efficacy [ 33 ]. This principle should be applicable to older stroke patients in convalescent rehabilitation hospitals. The positive outcomes of their hospital experience may be partially attributed to reduced stress.
Additionally, some patients faced limitations in self-care, stressors related to hospitalization owing to the aftereffects of stroke, and stressors related to illness. Given these findings, it was suggested that stroke patients may have been stressed by the interaction of “stressors related to the disease” and “stressors related to hospitalization.” However, if one of these stressors can be adequately addressed, it is likely that related stressors can be reduced.
Limitations
In conclusion, we clarified the stressors faced by older stroke patients in convalescent for rehabilitation. However, this study has some limitations. First, the study was severely limited by the small number of patients, which prevents us from drawing some important conclusions. The SCAT method can be used to analyze data from a small number of people because it provides a theoretical description from the participants’ storylines; however, the number of participants in this study was not sufficient to generalize the findings. Second, this study did not fully consider the participants’ individual characteristics, such as personality and background, nor did it analyze the patients in terms of their pathology and sequelae. Therefore, the results obtained should be interpreted carefully, as individual bias was not sufficiently eliminated. In future, it is necessary to select other participants and data analysis methods that consider participants’ individual characteristics and the aftereffects of stroke and recruit more participants to elucidate the stressors faced by older stroke patients in convalescent rehabilitation.
Stressors specific to older stroke patients were identified, including difficulty moving the paralyzed hand, recurrent stroke, and diet-related stressors. Stressors identified in this study can be broadly classified into “stressors related to hospitalization” and “stressors related to the disease,” consistent with previous studies [ 4 ]. However, it was found that stress is also caused by the interaction between “stressors related to hospitalization” and “stressors related to the disease.” To the best of our knowledge, thus far, no reports have identified the specific stressors faced by older stroke patients. Therefore, this study provides valuable information from a first-hand perspective that will lead to a deeper understanding of the specific stressors experienced by older stroke patients during recovery. Future studies should explore how various stressors lead to stress in older stroke patients at various types of rehabilitation hospitals.
Supporting information
S1 file. consolidated criteria for reporting qualitative studies (coreq): a 32-item checklist..
https://doi.org/10.1371/journal.pone.0309457.s001
Acknowledgments
We thank all the participants who agreed to be interviewed for this study. We also thank the members of the Rehabilitation Science Degree Program, Graduate School of Comprehensive Human Sciences, University of Tsukuba, for their guidance and encouragement during this study.
- View Article
- PubMed/NCBI
- Google Scholar
- Open access
- Published: 28 August 2024
A qualitative study identifying implementation strategies using the i-PARIHS framework to increase access to pre-exposure prophylaxis at federally qualified health centers in Mississippi
- Trisha Arnold ORCID: orcid.org/0000-0003-3556-5717 1 , 2 ,
- Laura Whiteley 2 ,
- Kayla K. Giorlando 1 ,
- Andrew P. Barnett 1 , 2 ,
- Ariana M. Albanese 2 ,
- Avery Leigland 1 ,
- Courtney Sims-Gomillia 3 ,
- A. Rani Elwy 2 , 5 ,
- Precious Patrick Edet 3 ,
- Demetra M. Lewis 4 ,
- James B. Brock 4 &
- Larry K. Brown 1 , 2
Implementation Science Communications volume 5 , Article number: 92 ( 2024 ) Cite this article
3 Altmetric
Metrics details
Mississippi (MS) experiences disproportionally high rates of new HIV infections and limited availability of pre-exposure prophylaxis (PrEP). Federally Qualified Health Centers (FQHCs) are poised to increase access to PrEP. However, little is known about the implementation strategies needed to successfully integrate PrEP services into FQHCs in MS.
The study had two objectives: identify barriers and facilitators to PrEP use and to develop tailored implementation strategies for FQHCs.
Semi-structured interviews were conducted with 19 staff and 17 PrEP-eligible patients in MS FQHCs between April 2021 and March 2022. The interview was guided by the integrated-Promoting Action on Research Implementation in Health Services (i-PARIHS) framework which covered PrEP facilitators and barriers. Interviews were coded according to the i-PARIHS domains of context, innovation, and recipients, followed by thematic analysis of these codes. Identified implementation strategies were presented to 9 FQHC staff for feedback.
Data suggested that PrEP use at FQHCs is influenced by patient and clinic staff knowledge with higher levels of knowledge reflecting more PrEP use. Perceived side effects are the most significant barrier to PrEP use for patients, but participants also identified several other barriers including low HIV risk perception and untrained providers. Despite these barriers, patients also expressed a strong motivation to protect themselves, their partners, and their communities from HIV. Implementation strategies included education and provider training which were perceived as acceptable and appropriate.
Conclusions
Though patients are motivated to increase protection against HIV, multiple barriers threaten uptake of PrEP within FQHCs in MS. Educating patients and providers, as well as training providers, are promising implementation strategies to overcome these barriers.
Peer Review reports
Contributions to the literature
We propose utilizing Federally Qualified Health Centers (FQHCs) to increase pre-exposure prophylaxis (PrEP) use among people living in Mississippi.
Little is currently known about how to distribute PrEP at FQHCs.
We comprehensively describe the barriers and facilitators to implementing PrEP at FQHCs.
Utilizing effective implementation strategies of PrEP, such as education and provider training at FQHCs, may increase PrEP use and decrease new HIV infections.
Introduction
The HIV outbreak in Mississippi (MS) is among the most critical in the United States (U.S.). It is distinguished by significant inequalities, a considerable prevalence of HIV in remote areas, and low levels of HIV medical care participation and virologic suppression [ 1 ]. MS has consistently ranked among the states with the highest HIV rates in the U.S. This includes being the 6th highest in new HIV diagnoses [ 2 ] and 2nd highest in HIV diagnoses among men who have sex with men (MSM) compared to other states [ 2 , 3 , 4 ]. Throughout MS, the HIV epidemic disproportionately affects racial and ethnic minority groups, particularly among Black individuals. A spatial epidemiology and statistical modeling study completed in MS identified HIV hot spots in the MS Delta region, Southern MS, and in greater Jackson, including surrounding rural counties [ 5 ]. Black race and urban location were positively associated with HIV clusters. This disparity is often driven by the complex interplay of social, economic, and structural factors, including poverty, limited access to healthcare, and stigma [ 5 ].
Pre-exposure prophylaxis (PrEP) has gained significant recognition due to its safety and effectiveness in preventing HIV transmission when taken as prescribed [ 6 , 7 , 8 , 9 ]. However, despite the progression in PrEP and its accessibility, its uptake has been slow among individuals at high risk of contracting HIV, particularly in Southern states such as MS [ 10 , 11 , 12 , 13 , 14 ]. According to the CDC [ 5 ], “4,530 Mississippians at high risk for HIV could potentially benefit from PrEP, but only 927 were prescribed PrEP.” Several barriers hinder PrEP use in MS including limited access to healthcare, cost, stigma, and medical mistrust [ 15 , 16 , 17 ].
Federally qualified health centers (FQHCs) are primary healthcare organizations that are community-based and patient-directed, serve geographically and demographically diverse patients with limited access to medical care, and provide care regardless of a patient’s ability to pay [ 18 ]. FQHCs in these areas exhibit reluctance in prescribing or counseling patients regarding PrEP, primarily because they lack the required training and expertise [ 19 , 20 , 21 ]. Physicians in academic medical centers are more likely to prescribe PrEP compared to those in community settings [ 22 ]. Furthermore, providers at FQHCs may exhibit less familiarity with conducting HIV risk assessments, express concerns regarding potential side effects of PrEP, and have mixed feelings about prescribing it [ 23 , 24 ]. Task shifting might also be needed as some FQHCs may lack sufficient physician support to manage all aspects of PrEP care. Tailored strategies and approaches are necessary for FQHCs to effectively navigate the many challenges that threaten their patients’ access to and utilization of PrEP.
The main objectives of this study were to identify the barriers and facilitators to PrEP use and to develop tailored implementation strategies for FQHCs providing PrEP. To service these objectives, this study had three specific aims. Aim 1 involved conducting a qualitative formative evaluation guided by the integrated-Promoting Action on Research Implementation in Health Services (i-PARIHS) framework- with FQHC staff and PrEP-eligible patients across three FQHCs in MS [ 25 ]. Interviews covered each of the three i-PARIHS domains: context, innovation, and recipients. These interviews sought to identify barriers and facilitators to implementing PrEP. Aim 2 involved using interview data to select and tailor implementation strategies from the Expert Recommendations for Implementing Change (ERIC) project [ 26 ] (e.g., provider training) and methods (e.g., telemedicine, PrEP navigators) for the FQHCs. Aim 3 was to member-check the selected implementation strategies and further refine these if necessary. Data from all three aims are presented below. The standards for reporting qualitative research (SRQR) checklist was used to improve the transparency of reporting this qualitative study [ 27 ].
Formative evaluation interviews
Interviews were conducted with 19 staff and 17 PrEP-eligible patients from three FQHCs in Jackson, Canton, and Clarksdale, Mississippi. Staff were eligible to participate if they were English-speaking and employed by their organization for at least a year. Eligibility criteria for patients included: 1) English speaking, 2) aged 18 years or older, 3) a present or prior patient at the FQHC, 4) HIV negative, and 5) currently taking PrEP or reported any one of the following factors that may indicate an increased risk for HIV: in the past year, having unprotected sex with more than one person with unknown (or positive) HIV status, testing positive for a sexually transmitted infection (STI) (syphilis, gonorrhea, or chlamydia), or using injection drugs.
Data collection
The institutional review boards of the affiliated hospitals approved this study prior to data collection. An employee at each FQHC acted as a study contact and assisted with recruitment. The contacts advertised the study through word-of-mouth to coworkers and relayed the contact information of those interested to research staff. Patients were informed about the study from FQHC employees and flyers while visiting the FQHC for HIV testing. Those interested filled out consent-to-contact forms, which were securely and electronically sent to research staff. Potential participants were then contacted by a research assistant, screened for eligibility, electronically consented via DocuSign (a HIPAA-compliant signature capturing program), then scheduled for an interview. Interviews occurred remotely over Zoom, a HIPAA-compliant, video conferencing platform. Interviews were conducted until data saturation was reached. In addition to the interview, all participants were asked to complete a short demographics survey via REDCap, a HIPAA-compliant, online, data collection tool. Each participant received a $100 gift card for their time.
The i-PARIHS framework guided interview content and was used to create a semi-structured interview guide [ 28 ]. Within the i-PARIHS framework’s elements, the interview guide content included facilitators and barriers to PrEP use at the FQHC: 1) the innovation, (PrEP), such as its degree of fit with existing practices and values at FQHCs; 2) the recipients (individuals presenting to FQHCs), such as their PrEP awareness, barriers to receiving PrEP such as motivation, resources, support, and personal PrEP experiences; and 3) the context of the setting (FQHCs), such as clinic staff PrEP awareness, barriers providing PrEP services, and recommendations regarding PrEP care. Interviews specifically asked about the use of telemedicine, various methods for expanding PrEP knowledge for both patients and providers (e.g., social media, advertisements, community events/seminars), and location of services (e.g., mobile clinics, gyms, annual health checkups, health fairs). Staff and patients were asked the same interview questions. Data were reviewed and analyzed iteratively throughout data collection, and interview guides were adapted as needed.
Data analysis
Interviews were all audio-recorded, then transcribed by an outside, HIPAA-certified transcription company. Transcriptions were reviewed for accuracy by the research staff who conducted the interviews.
Seven members of the research team (TA, LW, KKG, AB, CSG, AL, LKB) independently coded the transcripts using an a priori coding schedule that was developed using the i-PARIHS and previous studies [ 15 , 16 , 17 ]. All research team members were trained in qualitative methods prior to beginning the coding process. The coding scheme covered: patient PrEP awareness, clinic staff PrEP awareness, barriers to receiving PrEP services, barriers to providing PrEP services, and motivation to take PrEP. Each coder read each line of text and identified if any of the codes from the a priori coding framework were potentially at play in each piece of text. Double coding was permitted when applicable. New codes were created and defined when a piece of text from transcripts represented a new important idea. Codes were categorized according to alignment with i-PARIHS constructs. To ensure intercoder reliability, the first 50% of the interviews were coded by two researchers. Team meetings were regularly held to discuss coding discrepancies (to reach a consensus). Coded data were organized using NVivo software (Version 12). Data were deductively analyzed using reflexive thematic analysis, a six-step process for analyzing and reporting qualitative data, to determine themes relevant to selecting appropriate implementation strategies to increase PrEP use at FQHCs in MS [ 29 ]. The resulting thematic categories were used to select ERIC implementation strategies [ 26 ]. Elements for each strategy were then operationalized and the mechanism of change for each strategy was hypothesized [ 30 , 31 ]. Mechanisms define how an implementation strategy will have an effect [ 30 , 31 ]. We used the identified determinants to hypothesize the mechanism of change for each strategy.
Member checking focus groups
Member checking is when the data or results are presented back to the participants, who provide feedback [ 32 ] to check for accuracy [ 33 ] and improve the validity of the data [ 34 ]. This process helps reduce the possibility of misrepresentation of the data [ 35 ]. Member checking was completed with clinic staff rather than patients because the focus was on identifying strategies to implement PrEP in the FQHCs.
Two focus groups were conducted with nine staff from the three FQHCs in MS. Eligibility criteria were the same as above. A combination of previously interviewed staff and non-interviewed staff were recruited. Staff members were a mix of medical (e.g., nurses, patient navigators, social workers) and non-medical (e.g., administrative assistant, branding officer) personnel. Focus group one had six participants and focus group two had three participants. The goal was for focus group participants to comprise half of staff members who had previously been interviewed and half of non-interviewed staff.
Participants were recruited and compensated via the same methods as above. All participants electronically consented via DocuSign, and then were scheduled for a focus group. Focus groups occurred remotely over Zoom. Focus groups were conducted until data saturation was reached and no new information surfaced. The goal of the focus groups was to member-check results from the interviews and assess the feasibility and acceptability of selected implementation strategies. PowerPoint slides with the results and implementation strategies written in lay terms were shared with the participants, which is a suggested technique to use in member checking [ 33 ]. Participants were asked to provide feedback on each slide.
Focus groups were all audio-recorded, then transcribed. Transcriptions were reviewed for accuracy by the research staff who completed focus groups. Findings from the focus groups were synthesized using rapid qualitative analyses [ 36 , 37 ]. Facilitators (TA, PPE) both took notes during the focus groups of the primary findings. Notes were then compared during team meetings and results were finalized. Results obtained from previous findings of the interviews and i-PARIHS framework were presented. To ensure the reliability of results, an additional team member (KKG) read the transcripts to verify the primary findings and selected supportive quotes for each theme. Team meetings were regularly held to discuss the results.
Thirty-six semi-structured interviews in HIV hot spots were completed between April 2021 and March 2022. Among the 19 FQHC staff, most staff members had several years of experience working with those at risk for HIV. Staff members were a mix of medical (e.g., doctors, nurses, CNAs, social workers) and non-medical (e.g., receptionists, case managers) personnel. Table 1 provides the demographic characteristics for the 19 FQHC clinic staff and 17 FQHC patients.
Table 2 provides a detailed description of the findings within each category: PrEP knowledge, PrEP barriers, and PrEP motivation. Themes are described in detail, with representative quotes, below. Implementation determinants are specific factors that influence implementation outcomes and can be barriers or facilitators. Table 3 highlights which implementation determinants can increase ( +) or decrease (-) the implementation of PrEP at FQHCs in MS. Each determinant, mapped to its corresponding i-PARIHS construct, is discussed in more detail below. There were no significant differences in responses across the three FQHCs.
PrEP knowledge
Patient prep awareness (i-parihs: recipients).
Most patients had heard of PrEP and were somewhat familiar with the medication. One patient described her knowledge of PrEP as follows, “I know that PrEP is I guess a program that helps people who are high-risk with sexual behaviors and that doesn't have HIV, but they're at high-risk.”- Patient, Age 32, Female, Not on PrEP. However, many lacked knowledge of who may benefit from PrEP, where to receive a prescription, the different medications used for PrEP, and the efficacy of PrEP. Below is a comment made by a patient listing what she would need to know to consider taking PrEP. “I would need to know the price. I would need to know the side effects. I need to know the percentage, like, is it 100 or 90 percent effective.”— Patient, Age Unknown, Female, Not on PrEP. Patients reported learning about PrEP via television and social media commercials, medical providers, and their social networks. One patient reported learning about PrEP from her cousin. “The only person I heard it [PrEP] from was my cousin, and she talks about it all the time, givin’ us advice and lettin’ us know that it’s a good thing.”— Patient, Age Unknown, Female, Not on PrEP.
Clinic Staff PrEP Awareness (i-PARIHS: Context)
Training in who may benefit from PrEP and how to prescribe PrEP varied among clinic staff at different FQHCs. Not all clinics offered formal PrEP education for employees; however, most knew that PrEP is a tool used for HIV prevention. Staff reported learning about PrEP via different speakers and meetings. A clinic staff member reported learning about PrEP during quarterly meetings. “Well, sometimes when we have different staff meetings, we have them quarterly, and we discuss PrEP. Throughout those meetings, they tell us a little bit of information about it, so that's how I know about PrEP.” – Staff, Dental Assistant, Female. Some FQHC staff members reported having very little knowledge of PrEP. One staff member shared that she knew only the “bare minimum” about PrEP, stating,
“I probably know the bare minimum about PrEP. I know a little about it [PrEP] as far as if taken the correct way, it can prevent you from gettin’ HIV. I know it [PrEP] doesn’t prevent against STDs but I know it’s a prevention method for HIV and just a healthier lifestyle.” –Staff, Accountant, Female
A few of the organizations had PrEP navigators to which providers refer patients. These providers were well informed on who to screen for PrEP eligibility and the process for helping the patient obtain a PrEP prescription. One clinic staff member highlighted how providers must be willing to be trained in the process of prescribing PrEP and make time for patients who may benefit. Specifically, she said,
“I have been trained [for PrEP/HIV care]. It just depends on if that’s something that you’re willing to do, they can train on what labs and stuff to order ’cause it’s a whole lot of labs. But usually, I try to do it. At least for everybody that’s high-risk.” – Staff, OB/GYN Nurse Practitioner, Female
Another clinic staff member reported learning about PrEP while observing another staff member being training in PrEP procedures.
“Well, they kinda explained to me what it [PrEP] is, but I was in training with the actual PrEP person, so it was kinda more so for his training. I know what PrEP is. I know the medications and I know he does a patient assistance program. If my patients have partners who are not HIV positive and wanna continue to be HIV negative, I can refer 'em.” – Staff, Administrative Assistant, Female
PrEP barriers
Barriers receiving prep services (i-parihs: recipients, innovation).
Several barriers to receiving PrEP services were identified in both patient and clinic staff interviews. There was a strong concern for the side effects of PrEP. One patient heard that PrEP could cause weight gain and nightmares, “I’m afraid of gaining weight. I’ve heard that actual HIV medication, a lotta people have nightmares or bad dreams.” - Patient, Age 30, Female, Not on PrEP. Another patient was concerned about perceived general side effects that many medications have. “Probably just the [potential] side effects. You know, most of the pills have allergic reactions and side effects, dizziness, seizures, you know.” - Patient, Age 30, Female, Not on PrEP.
The burden of remembering to take a daily pill was also mentioned as a barrier to PrEP use. One female patient explained how PrEP is something she is interested in taking; however, she would be unable to take a daily medication.
“I’m in school now and not used to takin’ a medication every day. I was takin’ a birth control pill, but now take a shot. That was one of the main reasons that I didn’t start PrEP cause they did tell me I could get it that day. So like I wanna be in the mind state to where I’m able to mentally, in my head, take a pill every day. PrEP is somethin’ that I wanna do.” - Patient, Age Unknown, Female, Not on PrEP
Stigma and confidentiality were also barriers to PrEP use at FQHCs. One staff member highlighted how in small communities it is difficult to go to a clinic where employees know you personally. Saying,
“If somebody knows you’re going to talk to this specific person, they know what you’re goin’ back there for, and that could cause you to be a little hesitant in coming. So there’s always gonna be a little hesitancy or mistrust, especially in a small community. Everybody knows everybody. The people that you’re gonna see goes to church with you.” – Staff, Accountant, Female
Some patients had a low perceived risk of HIV and felt PrEP may be an unnecessary addition to their routine. One patient shared that if she perceived she was at risk for HIV, then she would be more interested in taking PrEP, “If it ever came up to the point where I would need it [PrEP], then yes, I would want to know more about it [PrEP].”— Patient, Age Unknown, Female, Not on PrEP.
Some participants expressed difficulty initiating or staying on PrEP because of associated costs, transportation and/or scheduling barriers. A staff member explained how transportation may be available in the city but not available in more rural areas,
“I guess it all depends on the person and where they are. In a city it might take a while, but at least they have the transportation compared to someone that lives in a rural area where transportation might be an issue.” - Staff, Director of Nurses, Female
Childcare during appointments was also mentioned as a barrier, “It looks like here a lot of people don't have transportation or reliable transportation and another thing I don't have anybody to watch my kids right now. —Staff, Patient Navigator, Female.
Barriers Providing PrEP Services (i-PARIHS: Context)
Barriers to providing PrEP services were also identified. Many providers are still not trained in PrEP procedures nor feel comfortable discussing or prescribing PrEP to their patients. One patient shared an experience of going to a provider who was PrEP-uninformed and assumed his medication was to treat HIV,
“Once I told her about it [PrEP], she [clinic provider] literally right in front of me, Googled it [PrEP], and then she was Googlin’ the medication, Descovy. I went to get a lab work, and she came back and was like, “Is this for treatment?” I was like, “Why would you automatically think it’s for treatment?” I literally told her and the nurse, “I would never come here if I lived here.” - Patient, Age 50, Male, Taking PrEP
Also, it was reported that there is not enough variety in the kind of providers who offer PrEP (e.g., OB/GYN, primary care). Many providers such as OB/GYNs could serve as a great way to reach individuals who may benefit from PrEP; however, patients reported a lack of PrEP being discussed in annual visits. “My previous ones (OB/GYN), they’ve talked about birth control and every other method and they asked me if I wanted to get tested for HIV and any STIs, but the conversation never came up about PrEP.” -Patient, Age Unknown, Female, Not on PrEP.
PrEP motivation
Motivation to take prep (i-parihs: recipients).
Participants mentioned several motivators that enhanced patient willingness to use PrEP. Many patients reported being motivated to use PrEP to protect themselves and their partners from HIV. Additionally, participants reported wanting to take PrEP to help their community. One patient reported being motivated by both his sexuality and the rates of HIV in his area, saying, “I mean, I'm bisexual. So, you know, anyway I can protect myself. You know, it's just bein' that the HIV number has risen. You know, that's scary. So just being, in, an area with higher incidents of cases.”— Patient, Age Unknown, Male, Not on PrEP . Some participants reported that experiencing an HIV scare also motivated them to consider using PrEP. One patient acknowledged his behaviors that put him at risk and indicated that this increased his willingness to take PrEP, “I was havin' a problem with, you know, uh, bein' promiscuous. You know? So it [PrEP] was, uh, something that I would think, would help me, if I wasn't gonna change the way I was, uh, actin' sexually.”— Patient, Age Unknown, Male, Taking PrEP .
Table 3 outlines the implementation strategies identified from themes from the interview and focus group data. Below we recognize the barriers and determinants to PrEP uptake for patients attending FQHCs in MS by each i-PARIHS construct (innovation, recipient, context) [ 28 ]. Based on the data, we mapped the determinants to specific strategies from the ERIC project [ 26 ] and hypothesized the mechanism of change for each strategy [ 30 , 31 ].
Two focus groups were conducted with nine staff from threeFQHCs in MS. There were six participants in the 1st focus group and three in the 2nd. Staff members were a mix of medical (e.g., nurses, patient navigators, social workers) and non-medical (e.g., administrative assistant, branding officer) personnel. Table 4 provides the demographic characteristics for the FQHC focus group participants.
Staff participating in the focus groups generally agreed that the strategies identified via the interviews were appropriate and acceptable. Focus group content helped to further clarify some of the selected strategies. Below we highlight findings by each strategy domain.
PrEP information dissemination
Participants specified that awareness of HIV is lower, and stigma related to PrEP is higher in rural areas. One participant specifically said,
“There is some awareness but needs to be more awareness, especially to rural areas here in Mississippi. If you live in the major metropolitan areas there is a lot of information but when we start looking at the rural communities, there is not a lot.” – Staff, Branding Officer, Male
Participants strongly agreed that many patients don’t realize they may benefit from PrEP and that more inclusive advertisements are needed. A nurse specifically stated,
“ When we have new clients that come in that we are trying to inform them about PrEP and I have asked them if they may have seen the commercial, especially the younger population. They will say exactly what you said, that “Oh, I thought that was for homosexuals or whatever,” and I am saying “No, it is for anyone that is at risk.” – Staff, Nurse, Female
Further, staff agreed that younger populations should be included in PrEP efforts to alleviate stigma. Participants added that including PrEP information with other prevention methods (i.e., birth control, vaccines) is a good place to include parents and adolescents:
“Just trying to educate them about Hepatitis and things of that nature, Herpes. I think we should also, as they are approaching 15, the same way we educate them about their cycle coming on and what to expect, it’s almost like we need to start incorporating this (PrEP education), even with different forms of birth control methods with our young ladies.” – Staff, Nurse, Female
Participants agreed that PrEP testimonials would be helpful, specifically from people who started PrEP, stopped, and then were diagnosed with HIV. Participants indicated that this may improve PrEP uptake and persistence. One nurse stated:
“I have seen where a patient has been on PrEP a time or two and at some point, early in the year or later part of the year, and we have seen where they’ve missed those appointments and were not consistent with their medication regimen. And we have seen those who’ve tested positive for HIV. So, if there is a way we could get one of those patients who will be willing to share their testimony, I think they can really be impactful because it’s showing that taking up preventive measures was good and then kind of being inconsistent, this is what the outcome is, unfortunately.” – Staff, Nurse, Female
Increase variety and number of PrEP providers
Participants agreed that a “PrEP champion” (someone to promote PrEP and answer PrEP related questions) would be helpful, especially for providers who need more education about PrEP to feel comfortable prescribing. A patient navigator said,
“I definitely think that a provider PrEP champion is needed in every clinic or organization that is offering PrEP. And it goes back to what we were saying about the providers not being knowledgeable on it [PrEP]. If you have a PrEP champion that already knows this information, it is gonna benefit everybody, patients, patient advocates, the provider, everyone all around. Everyone needs a champion." – Staff, Patient Navigator, Female
Staff noted that they have walk-in appointments for PrEP available; however, they often have too many walk-in appointments to see everyone. They noted that having more resources and providers may alleviate this barrier for some patients:
“We still have challenges with people walking in versus scheduling an appointment, but we do have same day appointments. It is just hard sometimes because the volume that we have at our clinic and the number of patients that we have that walk in on a daily basis.” – Staff, Social Worker, Female
Enhance PrEP provider alliance and trust
Participants agreed that educational meetings would be beneficial and highlighted that meetings should happen regularly and emphasized a preference for in-person meetings. This is emphasized by the statement below,
“They should be in-person with handouts. You have to kind of meet people where they are as far as learning. Giving the knowledge, obtaining the knowledge, and using it, and so you have to find a place. I definitely think that yearly in-person training to update guidelines, medication doses, different things like that." – Staff, Patient Navigator, Female
Staff also suggested hosting one very large collaborative event to bring together all organizations that offer PrEP and HIV testing to meet and discuss additional efforts:
“What I would like to see happen here in the state of Mississippi, because we are so high on the list for new HIV infections, I would like to see a big collaborative event. As far as PrEP goes, those that are not on PrEP, one big collaborative event with different community health centers. You do testing, we do PrEP, and the referral get split. Everyone coming together for one main purpose.” – Staff, Patient Navigator, Female
Increase access to PrEP
Participants highlighted that most of the clinics they worked for already offer a variety of service sites (pharmacy, mobile clinic) but that more clinics should offer these alternative options for patients to receive PrEP. One patient navigator outlined the services they offer,
“We have a mobile unit. We do not have a home health travel nurse. We do telephone visits. We offer primary care, OB/GYN. We have our own pharmacy. We also have samples in our pharmacy available to patients that can’t get their medicine on the same day cos we like to implement same day PrEP. It has worked for us. More people should utilize those services.” – Staff, Patient Navigator, Female
Other staff suggested utilizing minute clinics and pharmacies at grocery stores. Highlighting, that offering PrEP at these locations may increase PrEP uptake.
There has been great scientific expansion of HIV prevention research and priorities must now pivot to addressing how to best implement effective interventions like PrEP [ 38 ]. PrEP remains underutilized among individuals who may benefit, particularly in Southern states such as MS [ 10 , 11 , 12 , 13 , 14 ]. Implementation science could help ameliorate this by identifying barriers and facilitators to PrEP rollout and uptake. We selected and defined several strategies from the ERIC project [ 26 ] to increase PrEP use utilizing FQHCs. Our results, as shown in Table 3 , highlight the four domains of strategies selected: 1) PrEP Information Dissemination, 2) Increase Variety and Number of PrEP Providers, 3) Enhance PrEP Provider Alliance and Trust, and 4) Increase Access to PrEP.
Firstly, individuals cannot utilize PrEP if they are not aware of its presence and utility. In Mississippi, advertising PrEP services is integral to implementation efforts given the existing stigma and lack of health literacy in this region [ 39 ]. Potential avenues for expanding PrEP awareness are integrating it into educational curriculums, adolescents’ routine preventative healthcare, and health fairs. This study compliments prior research that people should be offered sexual health and PrEP education at a younger age to increase awareness of risk, foster change in social norms and enhance willingness to seek out prevention services [ 40 , 41 ]. To meet the resulting growing need for PrEP educators, healthcare professionals should receive up-to-date PrEP information and training, so that they can confidently relay information to their patients. Similar to existing research, increasing provider education could accelerate PrEP expansion [ 42 , 43 , 44 ]. Training programs aimed at increasing provider PrEP knowledge may increase PrEP prescriptions provided [ 43 ] by addressing one of the most frequently listed barriers to PrEP prescription among providers [ 45 , 46 ].
Many patients prefer to receive PrEP at the healthcare locations they already attend and report a barrier to PrEP being limited healthcare settings that offer PrEP [ 39 , 47 , 48 , 49 ]. The aforementioned PrEP training could increase the number of healthcare workers willing to provide PrEP services. It is also imperative that providers in a diverse range of healthcare settings (e.g., primary care, OB/GYN, pediatricians and adolescent medicine providers) join the list of those offering PrEP to reduce stigma and enhance patient comfort.
These results mirrored other studies in the South that have shown that using relatable healthcare providers and trusted members of the community may serve to facilitate PrEP uptake [ 41 , 50 , 51 ]. If patients have a larger number of PrEP providers to choose from, they can select one that best fits their needs (e.g., location, in-network) and preferences (e.g., familiarity, cultural similarities). Enhanced comfort facilitates a strong patient-provider alliance and can lead to more open/honest communication regarding HIV risk behavior.
The lack of conveniently located PrEP providers is consistently reported as a structural barrier in the South [ 44 , 52 ]. This creates an increase in the demand on patients to attend regular follow-up appointments. The three strategies above all play a vital role in increasing access to PrEP. If more individuals are trained to provide PrEP care, there will be more PrEP providers, and patients can choose the best option for them. A sizeable influx of new PrEP providers could help staff new care facilities and service options in the community (e.g., mobile health units, home care, community-based clinics, telemedicine). Offering PrEP via telemedicine and mobile clinics to patients has been largely supported in the literature [ 44 , 53 , 54 ]. Intra- and inter-organizational collaborations could similarly increase PrEP access by sharing information and resources to ensure patients get timely, reliable care.
Our results largely supported previous findings by two systematic reviews on the barriers to PrEP uptake and implementation strategies to overcome it [ 39 , 47 ]. Sullivan et.al.’s review focused on the Southern U.S. [ 38 ], while Bonacci et. al. explored steps to improve PrEP equity for Black and Hispanic/Latino communities [ 47 ]. Both agreed that barriers to PrEP access are complex. Thus, cooperation from policymakers and the expansion of state Medicaid or targeted Medicaid waivers is vital to make PrEP attainable for those living in the coverage gap. Further, many FQHCs receive Ryan White funding for HIV care and treatment, contracting flexibility in the utility of these other sources of support may aid in eliminating the cost of PrEP as a barrier. They also stressed the need for educating community members and healthcare personnel about PrEP, increasing and diversifying PrEP service sites, normalizing PrEP campaigns and screening to alleviate stigma, and streamlining clinical procedures to facilitate the option for same-day PrEP. However, they also noted that these strategies are easier said than done. This further highlights the need for prioritizing research efforts towards implementation studies for effectiveness and practicality of overcoming the complex and systemic needs around HIV prevention/treatment.
The present study was able to build on past findings by providing a more holistic view of the barriers to PrEP use and possible strategies to address them through querying PrEP-eligible patients, medical providers, and non-medical staff. By interviewing a diverse range of stakeholders, it was possible to identify unmet patient needs, current PrEP care procedures and infrastructure, and attitudes and needed resources among those who could potentially be trained to provide PrEP in the future.
Limitations
Our results are limited to participants and clinic staff who were willing to engage in a research interview to discuss PrEP and FQHCs. Results are only generalizable to Mississippi and may be less relevant for other geographic areas. However, this is a strength given these strategies are meant to be tailored specifically to FQHCs in MS. Due to COVID-19 restrictions, interviews were conducted via Zoom. This allowed us to reach participants unable to come in physically for an interview and may have increased their comfort responding to questions [ 55 ]. However, some participants may have been less comfortable discussing via Zoom, which may have limited their willingness to respond.
This study highlighted the need for implementing PrEP strategies to combat HIV in Mississippi. PrEP knowledge, barriers, and motivation were identified as key factors influencing PrEP utilization, and four domains of strategies were identified for improving PrEP accessibility and uptake. Future research should further refine and assess the feasibility and acceptability of selected and defined implementation strategies and test strategies.
Availability of data and materials
De-identified data from this study are not available in a public archive due to sensitive nature of the data. De-identified data from this study will be made available (as allowable according to institutional IRB standards) by emailing the corresponding author.
Abbreviations
Mississippi
Pre-Exposure Prophylaxis
Federally Qualified Health Centers
Integrated-Promoting Action on Research Implementation in Health Services
Expert Recommendations for Implementing Change
Men Who Have Sex With Men
Health MSDo. Mississippi’s Ending the HIV Epidemic Plan: MSDH; 2021. Available from: http://healthyms.com/msdhsite/_static/resources/5116.pdf .
Digre P, Avoundjian T, Johnson K, Peyton D, Lewis C, Barnabas RV, et al. Barriers, facilitators, and cost of integrating HIV-related activities into sexually transmitted disease partner services in Jackson, Mississippi. Sexually Transmit Dis. 2021;48(3):145–51.
Article Google Scholar
Rosenberg ES, Grey JA, Sanchez TH, Sullivan PS. Rates of prevalent HIV infection, prevalent diagnoses, and new diagnoses among men who have sex with men in US states, metropolitan statistical areas, and counties, 2012–2013. JMIR Public Health Surveill. 2016;2(1):e5684.
Khosropour CM, Backus KV, Means AR, Beauchamps L, Johnson K, Golden MR, et al. A pharmacist-led, same-day, HIV pre-exposure prophylaxis initiation program to increase PrEP uptake and decrease time to PrEP initiation. AIDS Patient Care STDS. 2020;34(1):1–6.
Article PubMed PubMed Central Google Scholar
Stopka TJ, Brinkley-Rubinstein L, Johnson K, Chan PA, Hutcheson M, Crosby R, et al. HIV Clustering in Mississippi: spatial epidemiological study to inform implementation science in the deep south. JMIR Publ Health Surveil. 2018;4(2):e35-e.
Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. The Lancet. 2013;381(9883):2083–90.
Molina J-M, Capitant C, Spire B, Pialoux G, Cotte L, Charreau I, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373:2237–46.
Article CAS PubMed Google Scholar
Molina J, Charreau I, Spire B, Cotte L, Chas J, Capitant C, et al. ANRS IPERGAY Study Group Efficacy, safety, and effect on sexual behaviour of on-demand pre-exposure prophylaxis for HIV in men who have sex with men: an observational cohort study. Lancet HIV. 2017;4(9):e402–10.
Article PubMed Google Scholar
Centers for Disease Control and Prevention. How effective is PrEP? : CDC; 2022. Available from: https://www.cdc.gov/hiv/basics/prep/prep-effectiveness.html .
Kirby T, Thornber-Dunwell M. Uptake of PrEP for HIV slow among MSM. Lancet. 2014;383(9915):399–400.
Elopre L, Kudroff K, Westfall AO, Overton ET, Mugavero MJ. The right people, right places, and right practices: disparities in PrEP access among African American men, women and MSM in the Deep South. J Acquired Immune Deficiency Syndr (1999). 2017;74(1):56.
Article PubMed Central Google Scholar
Brantley ML, Rebeiro PF, Pettit AC, Sanders A, Cooper L, McGoy S, et al. Temporal trends and sociodemographic correlates of PrEP uptake in Tennessee, 2017. AIDS Behav. 2019;23:304–12.
Hollcroft MR, Gipson J, Barnes A, Mena L, Dombrowski JC, Ward LM, et al. PrEP acceptance among eligible patients attending the largest PrEP Clinic in Jackson, Mississippi. J Int Assoc Providers AIDS Care (JIAPAC). 2023;22:23259582231167960.
PubMed Google Scholar
Chase E, Mena L, Johnson KL, Prather M, Khosropour CM. Patterns of Pre-exposure Prophylaxis (PrEP) Use in a Population Accessing PrEP in Jackson, Mississippi. AIDS Behav. 2023;27(4):1082–90. https://doi.org/10.1007/s10461-022-03845-9 .
Arnold T, Brinkley-Rubinstein L, Chan PA, Perez-Brumer A, Bologna ES, Beauchamps L, et al. Social, structural, behavioral and clinical factors influencing retention in Pre-Exposure Prophylaxis (PrEP) care in Mississippi. PLoS ONE. 2017;12(2):e0172354.
Cahill S, Taylor SW, Elsesser SA, Mena L, Hickson D, Mayer KH. Stigma, medical mistrust, and perceived racism may affect PrEP awareness and uptake in black compared to white gay and bisexual men in Jackson, Mississippi and Boston, Massachusetts. AIDS care. 2017;29(11):1351–8.
Arnold T, Gaudiano BA, Barnett AP, Elwy AR, Whiteley L, Giorlando KK, et al. Development of an acceptance based PrEP intervention (ACTPrEP) to engage young black MSM in the South utilizing the Adaptome Model of intervention adaptation. J Contextual Behav Sci. 2023;28:60–70.
Administration HRS. What is a Health Center? 2023. Available from: https://bphc.hrsa.gov/about-health-centers/what-health-center .
Oster AM, Dorell CG, Mena LA, Thomas PE, Toledo CA, Heffelfinger JD. HIV risk among young African American men who have sex with men: A case–control study in Mississippi. Am J Public Health. 2011;101(1):137–43.
Hall HI, Li J, McKenna MT. HIV in predominantly rural areas of the United States. J Rural Health. 2005;21(3):245–53.
Williams PB, Sallar AM. HIV/AIDS and African American men: Urban-rural differentials in sexual behavior, HIV knowledge, and attitude towards condoms use. J Natl Med Assoc. 2010;102(12):1139–49.
Krakower D, Mayer KH. Engaging healthcare providers to implement HIV pre-exposure prophylaxis. Curr Opin HIV AIDS. 2012;7(6):593.
Krakower D, Ware N, Mitty JA, Maloney K, Mayer KH. HIV providers’ perceived barriers and facilitators to implementing pre-exposure prophylaxis in care settings: a qualitative study. AIDS Behav. 2014;18:1712–21.
Hakre S, Blaylock JM, Dawson P, Beckett C, Garges EC, Michael NL, Danaher PJ, Scott PT, Okulicz JF. Knowledge, attitudes, and beliefs about HIV pre-exposure prophylaxis among US Air Force Health Care Providers. Medicine (Baltimore). 2016;95(32):e4511. https://doi.org/10.1097/MD.0000000000004511 .
Yakovchenko V, Bolton RE, Drainoni ML, Gifford AL. Primary care provider perceptions and experiences of implementing hepatitis C virus birth cohort testing: a qualitative formative evaluation. BMC Health Serv Res. 2019;19(1):236.
Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10(1):21.
O'Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–51. https://doi.org/10.1097/ACM.0000000000000388 .
Harvey G, Kitson A. PARIHS revisited: from heuristic to integrated framework for the successful implementation of knowledge into practice. Implement Sci. 2016;11(1):33.
Braun V, Clarke V, Hayfield N, Terry G. Thematic Analysis. In: Liamputtong P, editor. Handbook of research methods in health social sciences. Singapore: Springer Singapore; 2019. p. 843–60.
Chapter Google Scholar
Lewis CC, Klasnja P, Powell BJ, Lyon AR, Tuzzio L, Jones S, Walsh-Bailey C, Weiner B. From Classification to Causality: Advancing Understanding of Mechanisms of Change in Implementation Science. Front Public Health. 2018;6:136. https://doi.org/10.3389/fpubh.2018.00136 .
Lewis CC, Powell BJ, Brewer SK, Nguyen AM, Schriger SH, Vejnoska SF, et al. Advancing mechanisms of implementation to accelerate sustainable evidence-based practice integration: protocol for generating a research agenda. BMJ Open. 2021;11(10):e053474.
Varpio L, Ajjawi R, Monrouxe LV, O’Brien BC, Rees CE. Shedding the cobra effect: problematising thematic emergence, triangulation, saturation and member checking. Med Educ. 2017;51(1):40–50.
McKim C. Meaningful member-checking: a structured approach to member-checking. Am J Qual Res. 2023;7(2):41–52.
Google Scholar
Elo S, Kääriäinen M, Kanste O, Pölkki T, Utriainen K, Kyngäs H. Qualitative content analysis: A focus on trustworthiness. SAGE Open. 2014;4(1):2158244014522633.
Candela AG. Exploring the function of member checking. The qualitative report. 2019;24(3):619–28.
Vindrola-Padros C, Johnson GA. Rapid techniques in qualitative research: a critical review of the literature. Qual Health Res. 2020;30(10):1596–604.
Neal JW, Neal ZP, VanDyke E, Kornbluh M. Expediting the analysis of qualitative data in evaluation: a procedure for the Rapid Identification of Themes from Audio recordings (RITA). Am J Eval. 2015;36(1):118–32.
Theobald S, Brandes N, Gyapong M, El-Saharty S, Proctor E, Diaz T, et al. Implementation research: new imperatives and opportunities in global health. The Lancet. 2018;392(10160):2214–28.
Sullivan PS, Mena L, Elopre L, Siegler AJ. Implementation strategies to increase PrEP Uptake in the South. Curr HIV/AIDS Rep. 2019;16(4):259–69.
Elopre L, Ott C, Lambert CC, Amico KR, Sullivan PS, Marrazzo J, et al. Missed prevention opportunities: why young, black MSM with recent HIV diagnosis did not access HIV pre-exposure prophylaxis services. AIDS Behav. 2021;25(5):1464–73.
Arnold T, Giorlando KK, Barnett AP, Gaudiano BA, Rogers BG, Whiteley L, et al. Social, structural, behavioral, and clinical barriers influencing Pre-exposure Prophylaxis (PrEP) use among young black men who have sex with men in the south: a qualitative update to a 2016 study. Arch Sex Behav. 2024;53(2):785–97.
Edelman EJ, Moore BA, Calabrese SK, Berkenblit G, Cunningham CO, Ogbuagu O, et al. Preferences for implementation of HIV pre-exposure prophylaxis (PrEP): Results from a survey of primary care providers. Prev Med Rep. 2020;17: 101012.
Petroll AE, Walsh JL, Owczarzak JL, McAuliffe TL, Bogart LM, Kelly JA. PrEP awareness, familiarity, comfort, and prescribing experience among US primary care providers and HIV specialists. AIDS Behav. 2017;21(5):1256–67.
Barnett AP, Arnold T, Elwy AR, Brock JB, Giorlando KK, Sims-Gomillia C, et al. Considerations for PrEP implementation at federally qualified health centers in Mississippi: perspectives from staff and patients. AIDS Educ Prev. 2023;35(4):309–19.
Seidman D, Carlson K, Weber S, Witt J, Kelly PJ. United States family planning providers’ knowledge of and attitudes towards preexposure prophylaxis for HIV prevention: a national survey. Contraception. 2016;93(5):463–9.
Clement ME, Seidelman J, Wu J, Alexis K, McGee K, Okeke NL, et al. An educational initiative in response to identified PrEP prescribing needs among PCPs in the Southern U.S. AIDS Care. 2018;30(5):650–5.
Bonacci RA, Smith DK, Ojikutu BO. Toward greater pre-exposure prophylaxis equity: increasing provision and uptake for black and Hispanic/Latino individuals in the US. Am J Prev Med. 2021;61(5 Suppl 1):S60-s72.
Arnold T, Whiteley L, Elwy RA, Ward LM, Konkle-Parker DJ, Brock JB, et al. Mapping Implementation Science with Expert Recommendations for Implementing Change (MIS-ERIC): strategies to improve PrEP use among black cisgender women living in Mississippi. J Racial Ethn Health Disparities. 2023;10(6):2744–61.
Hirschhorn LR, Brown RN, Friedman EE, Greene GJ, Bender A, Christeller C, Bouris A, Johnson AK, Pickett J, Modali L, Ridgway JP. Black Cisgender Women's PrEP Knowledge, Attitudes, Preferences, and Experience in Chicago. J Acquir Immune Defic Syndr. 2020;84(5):497–507. https://doi.org/10.1097/QAI.0000000000002377 .
Pichon LC, Teti M, McGoy S, Murry VM, Juarez PD. Engaging black men who have sex with men (MSM) in the South in identifying strategies to increase PrEP uptake. BMC Health Serv Res. 2022;22(1):1491.
Auerbach JD, Kinsky S, Brown G, Charles V. Knowledge, attitudes, and likelihood of pre-exposure prophylaxis (PrEP) use among US women at risk of acquiring HIV. AIDS Patient Care STDS. 2015;29(2):102–10.
Siegler AJ, Bratcher A, Weiss KM. Geographic access to preexposure prophylaxis clinics among men who have sex with men in the United States. Am J Public Health. 2019;109(9):1216–23.
Rousseau E, Julies RF, Madubela N, Kassim S. Novel platforms for biomedical HIV prevention delivery to key populations — community mobile clinics, peer-supported, pharmacy-Led PrEP delivery, and the use of telemedicine. Curr HIV/AIDS Rep. 2021;18(6):500–7.
Article CAS PubMed PubMed Central Google Scholar
Player MS, Cooper NA, Perkins S, Diaz VA. Evaluation of a telemedicine pilot program for the provision of HIV pre-exposure prophylaxis in the Southeastern United States. AIDS Care. 2022;34(12):1499–505.
Gray LM, Wong-Wylie G, Rempel GR, Cook K. Expanding qualitative research interviewing strategies: Zoom video communications. Qual Rep. 2020;25(5):1292–301.
Download references
Acknowledgements
Authors would like to acknowledge and thank Sarah Bailey for reviewing the manuscript and assisting for formatting.
This study was funded by the National Institute of Health (R34MH115744) and was facilitated by the Providence/Boston Center for AIDS Research (P30AI042853). Additionally, work by Dr. Trisha Arnold was supported by the National Institute of Mental Health Grant (K23MH124539-01A1) and work by Dr. Andrew Barnett was supported by the National Institute of Mental Health Grant (T32MH078788). Dr. Elwy is supported by a Department of Veterans Affairs Research Career Scientist Award (RCS 23–018).
Author information
Authors and affiliations.
Department of Psychiatry, Rhode Island Hospital, One Hoppin Street, Coro West, 204, Providence, RI, 02903, USA
Trisha Arnold, Kayla K. Giorlando, Andrew P. Barnett, Avery Leigland & Larry K. Brown
Department of Psychiatry and Human Behavior, Warren Alpert Medical School of Brown University, Providence, RI, USA
Trisha Arnold, Laura Whiteley, Andrew P. Barnett, Ariana M. Albanese, A. Rani Elwy & Larry K. Brown
Department of Population Health Science, University of Mississippi Medical Center, Jackson, MS, USA
Courtney Sims-Gomillia & Precious Patrick Edet
Department of Medicine, University of Mississippi Medical Center, Jackson, MS, USA
Demetra M. Lewis & James B. Brock
Center for Healthcare Organization and Implementation Research, VA Bedford Healthcare System, Bedford, MA, USA
A. Rani Elwy
You can also search for this author in PubMed Google Scholar
Contributions
TA and ARE led the conceptualization of this paper. TA, LW, LKB, DML, and JBB completed the literature search and study design. TA, LW, LKB, KKG, PPE, AB, AL, and CSG assisted with analyzing and interpreting the data. TA, ARE, and AMA finalized the results and implementation concepts of the study. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Trisha Arnold .
Ethics declarations
Ethics approval and consent to participate.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by both the Rhode Island Hospital Institutional Review Board and the University of Mississippi Medical Center Institutional Review Board. Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no conflicts of interest or competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Arnold, T., Whiteley, L., Giorlando, K.K. et al. A qualitative study identifying implementation strategies using the i-PARIHS framework to increase access to pre-exposure prophylaxis at federally qualified health centers in Mississippi. Implement Sci Commun 5 , 92 (2024). https://doi.org/10.1186/s43058-024-00632-6
Download citation
Received : 22 May 2024
Accepted : 21 August 2024
Published : 28 August 2024
DOI : https://doi.org/10.1186/s43058-024-00632-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- HIV Prevention
- Implementation Science
- Pre-exposure prophylaxis (PrEP)
- Telemedicine
Implementation Science Communications
ISSN: 2662-2211
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Media Center
- Not yet translated
Qualitative Research
What is qualitative research.
Qualitative research is a methodology focused on collecting and analyzing descriptive, non-numerical data to understand complex human behavior, experiences, and social phenomena. This approach utilizes techniques such as interviews, focus groups, and observations to explore the underlying reasons, motivations, and meanings behind actions and decisions. Unlike quantitative research, which focuses on measuring and quantifying data, qualitative research delves into the 'why' and 'how' of human behavior, providing rich, contextual insights that reveal deeper patterns and relationships.
The Basic Idea
Theory, meet practice.
TDL is an applied research consultancy. In our work, we leverage the insights of diverse fields—from psychology and economics to machine learning and behavioral data science—to sculpt targeted solutions to nuanced problems.
Ever heard of the saying “quality over quantity”? Well, some researchers feel the same way!
Imagine you are conducting a study looking at consumer behavior for buying potato chips. You’re interested in seeing which factors influence a customer’s choice between purchasing Doritos and Pringles. While you could conduct quantitative research and measure the number of bags purchased, this data alone wouldn’t explain why consumers choose one chip brand over the other; it would just tell you what they are purchasing. To gather more meaningful data, you may conduct interviews or surveys, asking people about their chip preferences and what draws them to one brand over another. Is it the taste of the chips? The font or color of the bag? This qualitative approach dives deeper to uncover why one potato chip is more popular than the other and can help companies make the adjustments that count.
Qualitative research, as seen in the example above, can provide greater insight into behavior, going beyond numbers to understand people’s experiences, attitudes, and perceptions. It helps us to grasp the meaning behind decisions, rather than just describing them. As human behavior is often difficult to qualify, qualitative research is a useful tool for solving complex problems or as a starting point to generate new ideas for research. Qualitative methods are used across all types of research—from consumer behavior to education, healthcare, behavioral science, and everywhere in between!
At its core, qualitative research is exploratory—rather than coming up with a hypothesis and gathering numerical data to support it, qualitative research begins with open-ended questions. Instead of asking “Which chip brand do consumers buy more frequently?”, qualitative research asks “Why do consumers choose one chip brand over another?”. Common methods to obtain qualitative data include focus groups, unstructured interviews, and surveys. From the data gathered, researchers then can make hypotheses and move on to investigating them.
It’s important to note that qualitative and quantitative research are not two opposing methods, but rather two halves of a whole. Most of the best studies leverage both kinds of research by collecting objective, quantitative data, and using qualitative research to gain greater insight into what the numbers reveal.
You may have heard the world is made up of atoms and molecules, but it’s really made up of stories. When you sit with an individual that’s been here, you can give quantitative data a qualitative overlay. – William Turner, 16th century British scientist 1
Quantitative Research: A research method that involves collecting and analyzing numerical data to test hypotheses, identify patterns, and predict outcomes.
Exploratory Research: An initial study used to investigate a problem that is not clearly defined, helping to clarify concepts and improve research design.
Positivism: A scientific approach that emphasizes empirical evidence and objectivity, often involving the testing of hypotheses based on observable data. 2
Phenomenology: A research approach that emphasizes the first-person point of view, placing importance on how people perceive, experience, and interpret the world around them. 3
Social Interaction Theory: A theoretical perspective that people make sense of their social worlds by the exchange of meaning through language and symbols. 4
Critical Theory: A worldview that there is no unitary or objective “truth” about people that can be discovered, as human experience is shaped by social, cultural, and historical contexts that influences reality and society. 5
Empirical research: A method of gaining knowledge through direct observation and experimentation, relying on real-world data to test theories.
Paradigm shift: A fundamental change in the basic assumptions and methodologies of a scientific discipline, leading to the adoption of a new framework. 2
Interpretive/descriptive approach: A methodology that focuses on understanding the meanings people assign to their experiences, often using qualitative methods.
Unstructured interviews: A free-flowing conversation between researcher and participant without predetermined questions that must be asked to all participants. Instead, the researcher poses questions depending on the flow of the interview. 6
Focus Group: Group interviews where a researcher asks questions to guide a conversation between participants who are encouraged to share their ideas and information, leading to detailed insights and diverse perspectives on a specific topic.
Grounded theory : A qualitative methodology that generates a theory directly from data collected through iterative analysis.
When social sciences started to emerge in the 17th and 18th centuries, researchers wanted to apply the same quantitative approach that was used in the natural sciences. At this time, there was a predominant belief that human behavior could be numerically analyzed to find objective patterns and would be generalizable to similar people and situations. Using scientific means to understand society is known as a positivist approach. However, in the early 20th century, both natural and social scientists started to criticize this traditional view of research as being too reductive. 2
In his book, The Structure of Scientific Revolutions, American philosopher Thomas Kuhn identified that a major paradigm shift was starting to occur. Earlier methods of science were being questioned and replaced with new ways of approaching research which suggested that true objectivity was not possible when studying human behavior. Rather, the importance of context meant research on one group could not be generalized to all groups. 2 Numbers alone were deemed insufficient for understanding the environment surrounding human behavior which was now seen as a crucial piece of the puzzle. Along with this paradigm shift, Western scholars began to take an interest in ethnography , wanting to understand the customs, practices, and behaviors of other cultures.
Qualitative research became more prominent throughout the 20th century, expanding beyond anthropology and ethnography to being applied across all forms of research; in science, psychology, marketing—the list goes on. Paul Felix Lazarsfield, Austrian-American sociologist and mathematician often known as the father of qualitative research, popularized new methods such as unstructured interviews and group discussions. 7 During the 1940s, Lazarfield brought attention to the fact that humans are not always rational decision-makers, making them difficult to understand through numerical data alone.
The 1920s saw the invention of symbolic interaction theory, developed by George Herbert Mead. Symbolic interaction theory posits society as the product of shared symbols such as language. People attach meanings to these symbols which impacts the way they understand and communicate with the world around them, helping to create and maintain a society. 4 Critical theory was also developed in the 1920s at the University of Frankfurt Institute for Social Research. Following the challenge of positivism, critical theory is a worldview that there is no unitary or objective “truth” about people that can be discovered, as human experience is shaped by social, cultural, and historical contexts. By shedding light on the human experience, it hopes to highlight the role of power, ideology, and social structures in shaping humans, and using this knowledge to create change. 5
Other formalized theories were proposed during the 20th century, such as grounded theory , where researchers started gathering data to form a hypothesis, rather than the other way around. This represented a stark contrast to positivist approaches that had dominated the 17th and 18th centuries.
The 1950s marked a shift toward a more interpretive and descriptive approach which factored in how people make sense of their subjective reality and attach meaning to it. 2 Researchers began to recognize that the why of human behavior was just as important as the what . Max Weber, a German sociologist, laid the foundation of the interpretive approach through the concept of Verstehen (which in English translates to understanding), emphasizing the importance of interpreting the significance people attach to their behavior. 8 With the shift to an interpretive and descriptive approach came the rise of phenomenology, which emphasizes first-person experiences by studying how individuals perceive, experience, and interpret the world around them.
Today, in the age of big data, qualitative research has boomed, as advancements in digital tools allow researchers to gather vast amounts of data (both qualitative and quantitative), helping us better understand complex social phenomena. Social media patterns can be analyzed to understand public sentiment, consumer behavior, and cultural trends to grasp how people attach subjective meaning to their reality. There is even an emerging field of digital ethnography which is entirely focused on how humans interact and communicate in virtual environments!
Thomas Kuhn
American philosopher who suggested that science does not evolve through merely an addition of knowledge by compiling new learnings onto existing theories, but instead undergoes paradigm shifts where new theories and methodologies replace old ones. In this way, Kuhn suggested that science is a reflection of a community at a particular point in time. 9
Paul Felix Lazarsfeld
Often referred to as the father of qualitative research, Austrian-American sociologist and mathematician Paul Lazarsfield helped to develop modern empirical methods of conducting research in the social sciences such as surveys, opinion polling, and panel studies. Lazarsfeld was best known for combining qualitative and quantitative research to explore America's voting habits and behaviors related to mass communication, such as newspapers, magazines, and radios. 10
German sociologist and political economist known for his sociological approach of “Verstehen” which emphasized the need to understand individuals or groups by exploring the meanings that people attach to their decisions. While previously, qualitative researchers in ethnography acted like an outside observer to explain behavior from their point of view, Weber believed that an empathetic understanding of behavior, that explored both intent and context, was crucial to truly understanding behavior. 11
George Herbert Mead
Widely recognized as the father of symbolic interaction theory, Mead was an American philosopher and sociologist who took an interest in how spoken language and symbols contribute to one’s idea of self, and to society at large. 4
Consequences
Humans are incredibly complex beings, whose behaviors cannot always be reduced to mere numbers and statistics. Qualitative research acknowledges this inherent complexity and can be used to better capture the diversity of human and social realities.
Qualitative research is also more flexible—it allows researchers to pivot as they uncover new insights. Instead of approaching the study with predetermined hypotheses, oftentimes, researchers let the data speak for itself and are not limited by a set of predefined questions. It can highlight new areas that a researcher hadn’t even thought of exploring.
By providing a deeper explanation of not only what we do, but why we do it, qualitative research can be used to inform policy-making, educational practices, healthcare approaches, and marketing tactics. For instance, while quantitative research tells us how many people are smokers, qualitative research explores what, exactly, is driving them to smoke in the first place. If the research reveals that it is because they are unaware of the gravity of the consequences, efforts can be made to emphasize the risks, such as by placing warnings on cigarette cartons.
Finally, qualitative research helps to amplify the voices of marginalized or underrepresented groups. Researchers who embrace a true “Verstehen” mentality resist applying their own worldview to the subjects they study, but instead seek to understand the meaning people attach to their own behaviors. In bringing forward other worldviews, qualitative research can help to shift perceptions and increase awareness of social issues. For example, while quantitative research may show that mental health conditions are more prevalent for a certain group, along with the access they have to mental health resources, qualitative research is able to explain the lived experiences of these individuals and uncover what barriers they are facing to getting help. This qualitative approach can support governments and health organizations to better design mental health services tailored to the communities they exist in.
Controversies
Qualitative research aims to understand an individual’s lived experience, which although provides deeper insights, can make it hard to generalize to a larger population. While someone in a focus group could say they pick Doritos over Pringles because they prefer the packaging, it’s difficult for a researcher to know if this is universally applicable, or just one person’s preference. 12 This challenge makes it difficult to replicate qualitative research because it involves context-specific findings and subjective interpretation.
Moreover, there can be bias in sample selection when conducting qualitative research. Individuals who put themselves forward to be part of a focus group or interview may hold strong opinions they want to share, making the insights gathered from their answers not necessarily reflective of the general population.13 People may also give answers that they think researchers are looking for leading to skewed results, which is a common example of the observer expectancy effect .
However, the bias in this interaction can go both ways. While researchers are encouraged to embrace “Verstehen,” there is a possibility that they project their own views onto their participants. For example, if an American researcher is studying eating habits in China and observes someone burping, they may attribute this behavior to rudeness—when in fact, burping can be a sign that you have enjoyed your meal and it is a compliment to the chef. One way to mitigate this risk is through thick description , noting a great amount of contextual detail in their observations. Another way to minimize the researcher’s bias on their observations is through member checking , returning results to participants to check if they feel they accurately capture their experience.
Another drawback of qualitative research is that it is time-consuming. Focus groups and unstructured interviews take longer and are more difficult to logistically arrange, and the data gathered is harder to analyze as it goes beyond numerical data. While advances in technology alleviate some of these labor-intensive processes, they still require more resources.
Many of these drawbacks can be mitigated through a mixed-method approach, combining both qualitative and quantitative research. Qualitative research can be a good starting point, giving depth and contextual understanding to a behavior, before turning to quantitative data to see if the results are generalizable. Or, the opposite direction can be used—quantitative research can show us the “what,” identifying patterns and correlations, and researchers can then better understand the “why” behind behavior by leveraging qualitative methods. Triangulation —using multiple datasets, methods, or theories—is another way to help researchers avoid bias.
Linking Adult Behaviors to Childhood Experiences
In the mid-1980s, an obesity program at the KP San Diego Department of Preventive Medicine had a high dropout rate. What was interesting is that a majority of the dropouts were successfully losing weight, posing the question of why they were leaving the program in the first place. In this instance, greater investigation was required to understand the why behind their behaviors.
Researchers conducted in-depth interviews with almost 200 dropouts, finding that many of them had experienced childhood abuse that had led to obesity. In this unfortunate scenario, obesity was a consequence of another problem, rather than the root problem itself. This led Dr. Vincent J. Felitti, who was working for the department, to launch the Adverse Childhood Experiences (ACE) Study, aimed at exploring how childhood experiences impact adult health status.
Felitti and the Department of Preventive Medicine studied over 17,000 adults with health plans that revealed a strong relationship between emotional experiences as children and negative health behaviors as adults, such as obesity, smoking, and intravenous drug use. This study demonstrates the importance of qualitative research to uncover correlations that would not be discovered by merely looking at numerical data. 14
Understanding Voter Turnout
Voting is usually considered an important part of political participation in a democracy. However, voter turnout is an issue in many countries, including the US. While quantitative research can tell us how many people vote, it does not provide insights into why people choose to vote or not.
With this in mind, Dawn Merdelin Johnson, a PhD student in philosophy at Walden University, explored how public corruption has impacted voter turnout in Cook County, Illinois. Johnson conducted semi-structured telephone interviews to understand factors that contribute to low voter turnout and the impact of public corruption on voting behaviors. Johnson found that public corruption leads to voters believing public officials prioritize their own well-being over the good of the people, leading to distrust in candidates and the overall political system, and thus making people less likely to vote. Other themes revealed that to increase voter turnout, voting should be more convenient and supply more information about the candidates to help people make more informed decisions.
From these findings, Johnson suggested that the County could experience greater voter turnout through the development of an anti-corruption agency, improved voter registration and maintenance, and enhanced voting accessibility. These initiatives would boost voting engagement and positively impact democratic participation. 15
Related TDL Content
Applying behavioral science in an organization.
At its core, behavioral science is about uncovering the reasons behind why people do what they do. That means that the role of a behavioral scientist can be quite broad, but has many important applications. In this article, Preeti Kotamarthi explains how behavioral science supports different facets of the organization, providing valuable insights for user design, data science, and product marketing.
Increasing HPV Vaccination in Rural Kenya
While HPV vaccines are an effective method of preventing cervical cancer, there is low intake in low and middle-income countries worldwide. Qualitative research can uncover the social and behavioral barriers to increasing HPV vaccination, revealing that misinformation, skepticism, and fear prevent people from getting the vaccine. In this article, our writer Annika Steele explores how qualitative insights can inform a two-part intervention strategy to increase HPV vaccination rates.
- Versta Research. (n.d.). Bridging the quantitative-qualitative gap . Versta Research. Retrieved August 17, 2024, from https://verstaresearch.com/newsletters/bridging-the-quantitative-qualitative-gap/
- Merriam, S. B., & Tisdell, E. J. (2015). Qualitative research: A guide to design and implementation (4th ed.). Jossey-Bass.
- Smith, D. W. (2018). Phenomenology. In E. N. Zalta (Ed.), Stanford Encyclopedia of Philosophy . Retrieved from https://plato.stanford.edu/entries/phenomenology/#HistVariPhen
- Nickerson, C. (2023, October 16). Symbolic interaction theory . Simply Psychology. https://www.simplypsychology.org/symbolic-interaction-theory.html
- DePoy, E., & Gitlin, L. N. (2016). Introduction to research (5th ed.). Elsevier.
- ATLAS.ti. (n.d.). Unstructured interviews . ATLAS.ti. Retrieved August 17, 2024, from https://atlasti.com/research-hub/unstructured-interviews
- O'Connor, O. (2020, August 14). The history of qualitative research . Medium. https://oliconner.medium.com/the-history-of-qualitative-research-f6e07c58e439
- Sociology Institute. (n.d.). Max Weber: Interpretive sociology & legacy . Sociology Institute. Retrieved August 18, 2024, from https://sociology.institute/introduction-to-sociology/max-weber-interpretive-sociology-legacy
- Kuhn, T. S. (2012). The structure of scientific revolutions (4th ed.). University of Chicago Press.
- Encyclopaedia Britannica. (n.d.). Paul Felix Lazarsfeld . Encyclopaedia Britannica. Retrieved August 17, 2024, from https://www.britannica.com/biography/Paul-Felix-Lazarsfeld
- Nickerson, C. (2019). Verstehen in Sociology: Empathetic Understanding . Simply Psychology. Retrieved August 18, 2024, from: https://www.simplypsychology.org/verstehen.html
- Omniconvert. (2021, October 4). Qualitative research: Definition, methodology, limitations, and examples . Omniconvert. https://www.omniconvert.com/blog/qualitative-research-definition-methodology-limitation-examples/
- Vaughan, T. (2021, August 5). 10 advantages and disadvantages of qualitative research . Poppulo. https://www.poppulo.com/blog/10-advantages-and-disadvantages-of-qualitative-research
- Felitti, V. J. (2002). The relation between adverse childhood experiences and adult health: Turning gold into lead. The Permanente Journal, 6 (1), 44–47. https://www.thepermanentejournal.org/doi/10.7812/TPP/02.994
- Johnson, D. M. (2024). Voters' perception of public corruption and low voter turnout: A qualitative case study of Cook County (Doctoral dissertation). Walden University.
About the Author

Emilie Rose Jones
Emilie currently works in Marketing & Communications for a non-profit organization based in Toronto, Ontario. She completed her Masters of English Literature at UBC in 2021, where she focused on Indigenous and Canadian Literature. Emilie has a passion for writing and behavioural psychology and is always looking for opportunities to make knowledge more accessible.
We are the leading applied research & innovation consultancy
Our insights are leveraged by the most ambitious organizations.

I was blown away with their application and translation of behavioral science into practice. They took a very complex ecosystem and created a series of interventions using an innovative mix of the latest research and creative client co-creation. I was so impressed at the final product they created, which was hugely comprehensive despite the large scope of the client being of the world's most far-reaching and best known consumer brands. I'm excited to see what we can create together in the future.
Heather McKee
BEHAVIORAL SCIENTIST
GLOBAL COFFEEHOUSE CHAIN PROJECT
OUR CLIENT SUCCESS
Annual revenue increase.
By launching a behavioral science practice at the core of the organization, we helped one of the largest insurers in North America realize $30M increase in annual revenue .
Increase in Monthly Users
By redesigning North America's first national digital platform for mental health, we achieved a 52% lift in monthly users and an 83% improvement on clinical assessment.
Reduction In Design Time
By designing a new process and getting buy-in from the C-Suite team, we helped one of the largest smartphone manufacturers in the world reduce software design time by 75% .
Reduction in Client Drop-Off
By implementing targeted nudges based on proactive interventions, we reduced drop-off rates for 450,000 clients belonging to USA's oldest debt consolidation organizations by 46%
Randomized Controlled Trial
Psychological theories.

Automatic Thinking

Eager to learn about how behavioral science can help your organization?
Get new behavioral science insights in your inbox every month..
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.60(1); 2021 Mar

Language: English | Slovene
A Cross-sectional Multicentre Qualitative Study Exploring Attitudes and Burnout Knowledge in Intensive Care Nurses with Burnout
Presečna multicentrična kvalitativna raziskava o znanju in stališčih, ki jih imajo medicinske sestre na intenzivni negi o izgorelosti, adriano friganović.
1 University Hospital Centre Zagreb, Department of Anaesthesiology and Intensive Medicine, Kispaticeva 12, 10000 Zagreb, Croatia
2 University of Applied Health Sciences, Department of Nursing, Mlinarska 38, 10000 Zagreb, Croatia
Biljana Kurtović
Polona selič.
3 University of Ljubljana, Faculty of Medicine, Department of Family Medicine, Poljanski nasip 58, 1000 Ljubljana, Slovenia
Although nurses in intensive care units (ICUs) are exposed to prolonged stress, no burnout prevention policy has yet been established. This study aims to determine the attitudes and “sense” of knowledge of burnout in nurses with burnout.
The study, which has a qualitative exploratory phenomenological design, was carried out in several Croatian ICUs in 2017. ICU nurses suffering from burnout according to their score on the Maslach Burnout Inventory were chosen randomly from five hospitals. Their participation was voluntary. Of the 28 participants, 86% were women (n=24) and 14% men (n=4). They were aged mainly between 36 and 45 (n=11 (40%)) and between 26 and 35 (n=10 (36%)). Semi-structured interviews were conducted up to the saturation point. The conversations were audio-recorded and transcribed verbatim. The text was analysed using inductive thematic analysis, with codes derived and grouped into clusters by similarities in meaning, and interpretation as the final stage.
Emergent themes, compromised private life, stressful work demands, stress reduction options, protective workplace measures and sense of knowledge reflected a variety of experiences, attitudes and knowledge of burnout.
Nurses with burnout provided an insight into their experience and attitudes, and the problems created by burnout. Given the poor sense of knowledge about this syndrome, there is a need to implement education on burnout in nursing school curricula, and clear strategies in the ICU environment, i.e. information, awareness-raising, and specific guidelines on coping, burnout detection and prevention. Approaching burnout prevention through attitudes/social learning may be a novel and feasible model of addressing this issue.
Izvleček
Izhodišča.
Medicinske sestre na oddelkih za intenzivno nego (ICU) so izpostavljene dolgotrajnemu stresu, ob tem pa sistem ukrepov za preprečevanje izgorelosti ni vzpostavljen. Cilj študije je bil raziskati odnos do izgorelosti in znanja o tej okvari zdravja pri medicinskih sestrah, ki so že izgorele.
Študija, ki ima kvalitativno raziskovalno fenomenološko zasnovo, je bila izvedena v več hrvaških univerzitetnih kliničnih bolnišnicah, na oddelkih za intenzivno nego, v letu 2017. Medicinske sestre z izgorelostjo glede na z oceno MBItot na vprašalniku izgorelosti Maslach so bile izbrane naključno iz vsake bolnišnice in so sodelovale prostovoljno. Od 28 udeležencev je bilo 86 % žensk (n = 24) in 14 % moških (n = 4), starih 36–45 (n = 11, 40 %) in 26–35 let (n = 10, 36 %). Raziskovalna vprašanja o stališčih do izgorelosti in znanju o izgorelosti, ki prevladujejo pri medicinskih sestrah na intenzivni negi, pri katerih se je že razvil ta sindrom, so ciljala na različna področja izkušenj intervjuvancev. Polstrukturirani intervjuji so potekali, dokler ni bila dosežena nasičenost. Pogovori so bili zvočno posneti in dobesedno prepisani. Besedilo je bilo analizirano z uporabo induktivne tematske analize, pri čemer so bile kode izpeljane in razvrščene v skupine po podobnostih v pomenu; temu je sledila interpretacija kot zadnja faza analize. Odgovori na vsako vprašanje so bili organizirani v eno ali dve glavni temi, vse teme so imele podteme, te so bile izvedene iz več kod, število kod na podtemo se je gibalo med dve in pet.
Pet glavnih tem, ki odražajo izkušnje in vedenje o izgorelosti, je: (i) okrnjeno zasebno življenje s podtemami pomanjkanje prostega časa, zaostreni odnosi, projiciranje nezadovoljstva v družino, neustrezno spoprijemanje in učinki; (ii) stresne delovne zahteve (podteme: objektivni delovni pogoji, psihološke obremenitve, medosebni odnosi) in možnosti za zmanjšanje stresa z dvema podtemama (spontano uporabljene in povezane z upravljanjem); (iii) zaščitni ukrepi na delovnem mestu s štirimi podtemami (vodenje, preventiva in psihosocialna podpora, organizacijski ukrepi ter nadzor kakovosti in nagrade) in občutek znanja o izgorelosti s petimi podtemami (prepoznavanje, poznavanje in razumevanje izgorelosti, ideje o lajšanju izgorelosti in možni viri informacij (o sindromu izgorelosti)).
Razprava in zaključki
Izpovedi izgorelih medicinskih sester so omogočile uvid v izkušnje, stališča in težave, ki jih povzroča izgorelost. Glede na slabo znanje o tem sindromu bi bilo treba v učne programe zdravstvenih šol na vseh ravneh študija vključiti izobraževanje o izgorelosti in spoprijemanju s stresom. V oddelkih intenzivne nege pa so potrebne jasne strategije in protokoli, tj. informacije, ozaveščanje in posebne smernice za prepoznavanje, blaženje in preprečevanje izgorelosti. Pristop k preprečevanju izgorelosti preko spreminjanja stališč oziroma z uporabo socialnega učenja je lahko nov in izvedljiv model reševanja tega vprašanja, ki zadeva blagostanje in učinkovitost zdravstvenih delavcev povsod po svetu.
1. Introduction
Burnout is a response to long-term emotional and interpersonal stressors, usually in the context of the workplace, and is largely determined by work environment and workload ( 1 , 2 ). ICUs are a specific environment characterised by high-tech devices, high levels of responsibility, rapid patient turnover, and stress ( 3 ). Nurses employed in ICUs are exposed to work-related stress ( 4 ) and burdened with high levels of burnout ( 5 , 6 , 7 , 8 ), which can lead to frequent physical illness, reduced well-being (e.g. insomnia and irritability), eating problems and depression, and increased turnover, absenteeism and sick leave ( 6 , 9 ). Moreover, burnout in nurses can affect the quality of patient care they are able to offer ( 10 ). Several factors have been found to be associated with the development of burnout syndrome: personal characteristics, working conditions (prolonged overload), conflicts with patients, families or other staff members, lack of support, and a feeling that the work is not useful ( 11 , 12 , 13 ).
Numerous studies have determined the prevalence and assessment of burnout in ICU healthcare providers, the risk factors, and the organisational impact, yet burnout therapies have been relatively unexplored ( 13 , 14 ). There have been several studies conducted on nurses diagnosed with burnout aimed at identifying measures to strengthen workplace well-being ( 15 ), interventions for reducing burnout symptoms, and the application of coping strategies ( 16 ). ICU nurses’ well-being was shown to be better when they re-focused on their own resources using yoga and mindfulness, together with organisational support (e.g. peer supervision, official conversation, and teamwork ( 16 )).
This study was conducted to fill the gap in information on the attitudes and experience of burnout in participants previously assessed as burnt out. The approach also targeted the sense of knowledge among ICU nurses, e.g. describing their own knowledge as sufficient, superficial, non-existent etc. The findings could be of the utmost importance when planning burnout prevention, and could provide a better understanding of the phenomenon, which has been clearly recognised as a current problem in all healthcare systems. They might, therefore, be of international relevance.
The study had a qualitative phenomenological design with semi-structured interviews, and is reported in accordance with the Consolidated Criteria for Reporting Qualitative Research checklist. The inductive approach enabled the researchers to develop a thematic framework emerging from the data (“from the ground up”), while a semantic approach was needed to explore the participants’ experiences, beliefs and views ( 17 ).
2.1. Participants and procedure
This study was carried out as part of a larger cross-sectional study conducted in Croatia from April to September 2017. The participants included 620 ICU nurses working in cardiac surgery, neurosurgery, paediatric and neonatal ICUs, medical ICUs, general surgery, coronary ICUs and neurology ICUs at five Zagreb university hospitals. A convenience sampling method was used, and the target population was intensive care nurses employed at intensive care units (ICUs) at five Croatian university hospitals. Participation was voluntary, and the inclusion criterion for this study was more than six months of work experience.
A systematic review found that the most commonly used instrument in ICU burnout studies was the Maslach Burnout Inventory (MBI) ( 2 , 13 ). This was therefore used for the assessment. The MBI scores were collapsed into low, moderate and high according to Maslach et al. ( 2 ). A score of 57 out of a possible 132 points on the MBI scale was considered as high burnout, according to the definition of the sub-scales ( 18 ). High burnout was reported by 72 (12%) of the 620 participants. Of this number, nurses with burnout were chosen randomly from each participating ICU to ensure diversity of experience. Randomisation was carried out using the statistical programme MedCalc for Windows, Version 15.1 ( 19 ).
The principal investigator, who did not have any bias towards the participants, either in terms of their age, profession or sexual orientation, contacted the head nurse of each participating ICU to arrange a meeting to share the background and aims of the study, and present the semi-structured interviews that would be used. In the cross-sectional study that preceded this one, several demographic characteristics were already collected, i.e. age, gender, education, time working in the ICU and type of ICU. After informed consent had been obtained, a time and place for the interviews was agreed. A series of 28 interviews with ICU nurses was eventually carried out. The principal investigator conducted the interviews, and the participants were informed about the reasons for the study. Only the interviewer and the participant were present.
Each interview lasted 30–60 minutes and was audio-recorded. Saturation was reached when a rapid decrease in new codes was noted. This occurred after the 26th participant. All the interviewees were informed about the study and gave written consent to participation. They had the possibility of withdrawing or interrupting their participation at any time.
2.2. Data analysis
A detailed transcript of the conversations (verbatim) was made, followed by an inductive thematic content analysis. According to Guest et al. ( 20 ), this is an “organic approach” to coding and theme-generation, allowing for the in-depth exploration of experiences, beliefs and views, and providing a comprehensive understanding of the knowledge that participants had about burnout ( 21 ). The analysis was performed as follows: after becoming familiar with the data while reading the transcripts, the initial codes were generated in the first stage of open coding. Themes based on the codes were subsequently constructed by organising the data into meaningful groups. A review of the initial codes and their (re)combination into previous/new themes took place before the names of the themes were developed and defined. A theme captures something important about the data in relation to the research question, and represents some level of patterned response or meaning within the data set. This process corresponds to the axial coding procedure. Finally, the number of themes was reduced to a more manageable set of important themes (main themes ( 21 )). The data from each stage was treated collaboratively and corroboratively. All the researchers coded the data and confirmed the thematic analysis to ensure that one person’s perspective did not bias interpretation of the date. This made the working methods trustworthy and valid (investigator triangulation) ( 22 ).
There were 4 (14%) male and 24 (86%) female nurses aged between 18 and 25 (n=6 (21%)), 26 and 36 (n=10 (36%)), and 36 and 45 (n=11 years (40%)), with one person over 45 years of age. They were mostly single (n=18 (64%)), with one divorced person, and had secondary levels of education (n=12 (43%)) or higher. Of the total number, 11 (40%) had less than five years’ work experience, while the others reported between five and ten years (n=5 (18%)), 11 to 15 years (n=3 (11%)), 16 to 20 years (n=6 (21%)) or 21 or more years of professional experience (n=3 (11%)). They were employed at Zagreb university hospitals (n=17 (61%)), Sestre Milosrdnice (n=4 (14%)), Sveti Duh (n=3 (11%)), Merkur (n=3 (11%)) and Dubrava (n=1 (3%)).
For each question, the analysis displayed the main themes that recurred throughout the conversation. An inventory of the themes, including the codes, is presented in Tables 1 – 4 .
How does your work influence your home and your private life?
| PRIVATE LIFE COMPROMISED | ||||
|---|---|---|---|---|
| LACK OF LEISURE TIME (N=12) | STRAINED RELATIONSHIPS (N=7) | PROJECTING DISSATISFACTION ONTO FAMILY (N=5) | INADEQUATE COPING (N=12) | EFFECTS (N=14) |
| Time-consuming | Stress impacts family relationships | Emotional strain causing dissatisfaction at home | Mentally and physically tired | No negative effects |
| Unfinished work carried home | Frustration | Avoidance | Performing duties outside my line of work | Some positive influence |
| Assignments given outside working hours | Thinking about stressful events after work | Personal changes/harm | Working overtime | Occasional negative effects |
| Work schedule more important than family time | Overwhelming work-related strain | Unrealistic demands | ||
Please can you tell me what you know about burnout syndrome?
| SENSE OF KNOWLEDGE | ||||
|---|---|---|---|---|
| RECOGNISING BURNOUT (N=15) | BEING ACQUAINTED WITH IT (N=10) | BEING ABLE TO DESCRIBE IT (N=14) | BURNOUT RELIEF (N=9) | SOURCES OF INFORMATION (N=5) |
| No/never | Superficial knowledge | Something that happens after several years on the job | Specialist help (psychology/ counselling) | Not mentioned at school |
| Not enough knowledge | Being able to describe what it is | Irritated, depressed, not able to sleep because of work | Awareness-raising workshops | Heard about it at school |
| Experiencing burnout by myself | Knowledgeable | Tired/concerned about becoming physically ill | The team leader as a problem-solving facilitator | Lectures at work/knew about it at work |
| Definitions/notions about burnout | Leaving for an easier workplace | Information from various sources, various sources of knowledge | ||
| Do not know what to do | ||||
There were four research questions. These covered different areas of the interviewees’ experience. The data collected was organised into three sub-levels: code(s), sub-theme(s) and main theme(s). The answers to each question were organised into one or two main themes. All the themes had sub-themes based on several codes, with the number of codes per sub-theme varying from two to five.
There was one main theme identified in the answers to this question ( Table 1 ), Private life compromised , with five sub-themes (lack of leisure time, strained relationships, projecting dissatisfaction onto family, inadequate coping and the effects). With regard to the main theme Private life compromised , the participants most often mentioned two sub-themes, namely a lack of leisure time, and strained family relationships (“ I rarely see my family ” or “ Sometimes I get calls late in the afternoon outside working hours and I have to do something for work before I go there the next time ”). On the one hand, work-related stress manifests itself in a limited amount of leisure time (due to the long working hours and sometimes also due to work assignments/telephone calls outside working hours); on the other hand, work affects nurses’ mood and mental state in such a way that they seclude themselves from family members or they pass their stress on to their families (“ I bring home the things that happen at work and I mull over them and cannot devote myself to my family as normal ”).
The participants tried to alleviate the negative effects on their families as much as possible, yet most of them stated that they did not have an efficient method of achieving that goal. The two sub-themes were therefore labelled Inadequate coping and Projecting dissatisfaction onto family , due to the participants’ lack of constructive coping strategies, so they ended up projecting dissatisfaction at home and felt mentally and physically tired. The participants felt that stress in their private lives stemmed from a lack of sleep (primarily because of night shifts) and long shifts (“ I am privately strained because of fatigue, chronic stress, insufficient rest between shifts and so on ”) and also from the difficulty of the job itself. The fifth sub-theme covered the Effects , derived from the codes “no” and/or “occasional negative effects” and “some positive influence”, for the participants who said they experienced them. Very few participants (three in all) said they did not feel any negative consequences from work stress, or even had positive impacts (resisting stress) on their private lives.
The participants’ answers were grouped around two main themes: Stressful work demands (sub-themes: objective working conditions, psychological strain, interpersonal relationships) and Stress-reduction options with two sub-themes, i.e. spontaneously applied and management-related ( Table 2 ). All agreed that their work was extremely stressful and demanding. Besides its objectively demanding characteristics, such as unpredictability, great responsibility and extreme workload, the participants also reported objective stressors, such as responsibility and rapid decision-making about human lives (“ Too much to do, not enough staff, you try to do everything you need ”). Being surrounded by human suffering, death and dying also makes the job emotionally demanding/tiring. The third cause of workplace stress is poor workplace environment and poor interpersonal relationships (“ It’s not fair ” or “ I think some people work a lot more and a lot better than others do, and for practically the same amount of money ”).
Intensive care is said to be a very stressful environment. What is your view?
| STRESSFUL WORK DEMANDS | STRESS REDUCTION OPTIONS | |||
|---|---|---|---|---|
| OBJECTIVE WORKING CONDITIONS (N=14) | PSYCHOLOGICAL STRAIN (N=13) | INTERPERSONAL RELATIONSHIPS (N=14) | SPONTANEOUSLY APPLIED (N=8) | MANAGEMENT-RELATED (N=8) |
| Stressful, demanding, high pressure | Human suffering | Poor interpersonal relationships | Socialising outside work | Mediating interpersonal relationships |
| Unpredictability | Emotionally overwhelming | Unfairness | Smaller teams | Efficient work organisation |
| Workload | Psychological toll | General dissatisfaction | Improving work conditions | |
| Constant changes in technology | Increasing competencies | |||
Besides talking about the presence of stress at work, some participants spontaneously mentioned certain techniques to reduce stress (second theme, Stress reduction options ). They suggested means of stress relief and work environment improvements that were already in place on their wards, e.g. socialising outside work, or creating smaller work groups on the ward that encourage teamwork and cooperation (“ I think it is important to foster a good team spirit in various ways ”). Unfortunately, there was just a handful of examples of these successful strategies. Most proposals made by the nurses were wishes and unfulfilled needs, but they included very specific guidelines on stress relief in the workplace: “ The only thing that comes to my mind is to increase the medical staff. I think everyone here gives the best that they can, but sometimes they can’t do what’s best because they simply don’t have enough time ” or “ For example, they could provide us with the supplies needed for work that we often don’t have... Providing enough equipment and supplies, providing enough staff, all of that relieves stress ”. These are all management-related.
When asked directly about the role of the employer, the nurses gave suggestions that fall into one major theme called Protective workplace measures , and four sub-themes ( Table 3 ). The first sub-theme was leadership: “ Creating a positive work environment, having teams that work well together, whose members work well together, because if the environment is positive, if people communicate well, then it’s easier to bear it all ”. The second sub-theme was creating preventive and psychosocial support. The employer needs to provide education/training on stress prevention for employees, as well as a support system when the negative impacts of stress appear: “ In the sense of support for various programmes and training in stress prevention, it doesn’t exist here, so you’re left to yourown devices when it comes to coping ”. As the third sub-theme, Organisational measures, states, prerequisites for stress reduction are better working conditions in the sense of improved staff education (“ The better the staff are educated, the less insecurity at work ”), and better-equipped wards. Finally, the fourth sub-theme recognises that rewards and quality control are also important – it seems that the existing system of rewards is not satisfying because of a lack of unified criteria for quality assessment. Nurses are aware of the differences in work quality, and feel it is both necessary and encouraging to reward better nurses and give them some privileges.
Thinking about stress in your workplace, what do you think the employer’s role is?
| PROTECTIVE WORKPLACE MEASURES | |||
|---|---|---|---|
| LEADERSHIP (N=8) | PREVENTION AND PSYCHOSOCIAL SUPPORT (N=9) | ORGANISATIONAL MEASURES (N=12) | QUALITY CONTROL AND REWARDS (N=13) |
| Relaxed approach | A defined system for help provision | Increased staff numbers | Regular recuperation/days off |
| Supervisors creating a better climate | Team building | Maintenance of equipment and supplies | Participation in the shift schedule |
| Questionnaire/problems list | Education focused on job- related technical demands | Unified rules and assessment of work quality | |
| Stress prevention programmes | Better communication within the team | Rewards for better work | |
| Protocols/system of reporting | Improved working conditions | ||
The main theme is one of the recurring themes on burnout ( Table 4 ), Sense of knowledge of burnout , with five sub-themes (recognising and being acquainted with burnout, being able to describe it, ideas about burnout relief, and possible sources of information). The participants’ personal experience varies: most stated that they had some notion about what burnout might be, but insufficient knowledge, while a lower number stated that they were already feeling the symptoms of burnout (“ I think I have felt the full scope of burnout and that it struck because I thought it could not happen to me and that I could control it. I did not have support, but it wasn’t until I realised that I couldn’t function, that I couldn’t sleep, that I couldn’t function privately, that I realised I had a problem ”). This is an indicative finding, since the interviews were carried out only with those with burnout (MBI TOT ) and those who had stated a higher level of negative stress influence.
In line with this, it was generally acknowledged in the second sub-theme that other nurses also did not know enough about burnout syndrome, but that they could only say what it was on purely a superficial level: “ I think knowledge is insufficient and most do not understand what it means at all ”. Only a few individual participants felt that nurses were sufficiently well-informed.
How nurses feel about burnout syndrome and what they know about it is best seen through their own words: “ For me, it represents a state where I no longer have the willpower to go to work after a while when a lot of these things have accumulated ”.
The two additional sub-themes were burnout relief and sources of information, which vary (although it seems that they are primarily found at work). Some nurses had heard about the syndrome at college/school, but most had reportedly heard of it for the first time at work (from coworkers, through organised courses). There is definitely a need for certain strategies, i.e. information, awareness-raising and specific guidelines about who to turn to for help and how to proceed. An important role is attributed to the team leader/head nurse (“ The head nurse knows best what interpersonal relations are like and what kind of a work place this is, so I think she should take up a bigger role here, since she knows everything, and she should encourage people to talk to each other, to get frustrations out in a civilised manner, to just talk ”).
4. Discussion
The aim of this study was to explore intensive care nurses’ experience of and attitudes towards burnout, and to identify their sense of knowledge about this syndrome. Five main themes were generated from a rich amount of data, including, inevitably, a reflection of the authors’ perspective: Compromised private life with five sub-themes (lack of leisure time, strained relationships, projecting dissatisfaction onto family, inadequate coping and the effects); Stressful work demands (sub-themes: objective working conditions, psychological strain, interpersonal relationships) and Stress reduction options with two sub-themes (spontaneously applied and management-related); Protective workplace measures with four sub-themes (leadership, prevention and psychosocial support, organisational measures, and quality control and rewards) and Sense of knowledge of burnout with five sub-themes (recognising and being acquainted with burnout, being able to describe it, ideas about burnout relief and possible sources of information).
The study tried to present what a group of ICU nurses felt, experienced and knew about burnout. Their perceptions and perspectives were all analysed, and then used to create an understanding of this part of their professional experience in a broader sense. The nurses’ expectations and proposals for protective workplace measures, e.g. leadership, prevention and psychosocial support, organisational measures, and quality control and rewards are among the very illustrative findings of this study ( Table 3 ). In addition, the results also showed that participants had a poor sense of knowledge about burnout ( Table 4 ).
High dependency departments are very stressful environments and can lead to a greater incidence of burnout, especially by way of emotional exhaustion and poor personal accomplishment. Nurse education has been increasing in the past decade, but it has not been followed by more competencies and greater autonomy ( 23 ). This study aimed to provide an insight into the attitudes towards and knowledge of burnout among ICU nurses with burnout. A poor sense of knowledge of burnout was identified in the participants ( Table 4 ). The participants tried to alleviate the adverse effects on their families as much as possible, yet most of them stated that they did not have an efficient method of achieving that goal ( Table 1 ). This accords with Shanafelt et al. ( 10 ), who reported poor communication with families, with the effects of work spilling over into personal life in healthcare providers who came home upset and unhappy.
The participants felt that the causes of the adverse effects (Theme 3, Table 1 ) and stress in their private lives stemmed not only from a lack of sleep (primarily because of night shifts) and long shifts, but also from the difficulty of the job itself ( Table 2 ). Research has shown that high stress contributes to the development of lethargy, which can worsen further due to difficulty sleeping ( 24 , 25 ). The participants reported an array of difficulties, and the study’s findings confirmed that ICU nurses considered their work to be extremely stressful and emotionally demanding ( Table 3 ). The interviewees reported objective stress sources, such as responsibility and rapid decision-making about human lives ( Table 3 ), similarly to Donchin ( 26 ), who described the ICU as an extremely stressful environment, and other authors who focused on workload as an independent factor in the development of burnout ( 5 ). Research exploring a reduction in burnout levels has shown promising results for burnout recovery when combined with individually and professionally focused activities ( 27 , 28 ). An improvement in work organisation has been shown to be the most important factor for reducing stress ( 29 ), and the need for a balanced interaction between job demands and resources in order to prevent burnout in hospital nurses has been confirmed among Croatian hospital nurses in previous research ( 30 ).
In this study, one frequently mentioned cause of workplace stress was an unpleasant or poor work environment and poor interpersonal relationships ( Table 3 ). Others have also confirmed that the work environment and interpersonal relationships are linked to burnout ( 1 , 9 , 31 ). This study participants suggested some solutions to address occupational stress, including changes in organisational and working conditions, refining interpersonal communication, and obliging supervisors/superiors/head nurses to implement them ( Table 4 ), which accords with research findings that stress in hospital nurses is related to the organisation of work ( 32 , 33 ). In their cross-sectional survey conducted in 2006-2007, Golubić et al. identified several major groups of occupational stressors in hospital nurses: organisation of work and financial issues; public criticism; hazards and interpersonal conflicts in the workplace; shift work; and professional and intellectual demands. They advised hospital managers to develop strategies to address and improve the quality of working conditions for nurses in Croatian hospitals ( 34 ). Other authors have also proposed that head nurses be encouraged to accept suggestions from staff, given how employees feel about their work and how personal relationships in the workplace affect their well-being ( 35 ). This is similar to this study participants’ expectations and proposals ( Tables 3 , ,4). 4 ). Providing specialist help and awareness-raising workshops ( Table 4 ) could help to reduce nurses’ occupational stress levels and staff turnover ( Table 4 , “Leaving for an easier workplace”), and enable nurses to maintain their capacity to work.
This study showed that there was an insufficient sense of knowledge of burnout syndrome, with information coming from a variety of sources ( Table 4 ). This makes it difficult to diagnose burnout early, and to prevent and possibly treat it. However, the ICU environment should primarily target the prevention of burnout ( 36 ). This could be accomplished by developing capacity-building to help staff become more aware of the issue, and encouraging them to talk about it ( 37 ). It has already been suggested in Croatia that developing prevention plans and including psychological education as an intervention would greatly reduce both the incidence and the adverse effects on the health system ( 38 ). Given that differences in job satisfaction and psychological and subjective well-being have been found to be conditioned by level of education, i.e. nurses with a higher level of education are more satisfied with their jobs ( 35 ), continuing education could affect both burnout and job satisfaction. Within continuous education, lectures should provide information about coping skills ( 39 ). There is definitely a need for certain strategies for ICU nurses, i.e. information, awareness-raising and specific guidelines about who to turn to for help and how to proceed ( Table 4 ).
To produce more conclusive findings with an international impact, it is of the utmost importance that research using a mixed (quantitative and qualitative) methodology is carried out again in the region, in hospitals with similar organisational set-ups and conditions. Aside from this, absenteeism and career changes related to working conditions and demands in ICU nurses should be taken into account when planning further research.
4.1. Strengths and limitations of the study
This study was focused on how ICU nurses perceived and experienced burnout. The results have provided us with a profound and detailed understanding of this phenomenon. This study’s findings should also help hospital management and other decision-makers to better understand nurses’ concerns. The results based on phenomenological analysis can be recognised as natural rather than artificial findings. Although data collected by interview offer insights on the relationship between a stressful working environment and burnout, and on the consequences on ICU nurses’ well-being and family life, the qualitative nature of the data limits generalisation of the conclusions to the entire population of ICU nurses and technicians with burnout. Considering the fact that this form of research generally works with small groups, it can be dubious to claim the results are typical of all ICU nurses. The reliability and validity of this approach is a primary limitation of this study. Although data-gathering took up a great deal of time and resources, and the results are valuable because they provide us with a better understanding of nurses’ perceptions and feelings with regard to stressful working conditions and burnout, they lack objective measures and specific behaviours that manifest these thoughts and feelings. This was partly overcome by means of the semistructured approach (vs. completely unstructured), which made it possible to compare information and organise it into meaningful patterns and themes. However, potential bias should be taken into account. Researcher-induced bias might have influenced the outcome of the analysis, since this type of research is based more on opinion and judgement than on results, meaning that this qualitative study, as in all qualitative research, would be difficult to replicate. Given that qualitative research is open-ended, it is safe to conclude that the participants had more control over the content of the data collected.
Qualitative phenomenological research is not the proper means of knowledge assessment, so it is only feasible to discuss the participants’ sense of their own knowledge. The suggestion would be first to provide knowledge about burnout in nurses’ education, then to follow up the effects and possibly provide some ongoing skill-development programmes for this professional group as a general preventive measure.
Quantitative data is required for circumstances that need statistical representation. That is not part of the qualitative research process.
In the near future, it will be very important to cross-reference the data obtained in this study with quantitative data.
5. Conclusions
In order to prevent or reduce burnout syndrome levels, compromised private life and stressful work demands, the various levels of the nursing education system should address stress reduction options, protective workplace measures and the poor sense of knowledge among ICU nurses. These should also be addressed within administrative and institutional settings. The information provided can help ICU nurses, and nurses in general, to understand how burnout affects their professional and family lives, and offers a variety of methods aimed at mitigating these harmful effects. Finally, the findings can motivate healthcare professionals with limited skills and/ or knowledge of burnout to at least accept the necessity to modify their coping strategies so that they are more problem-oriented and constructive.
Acknowledgements
The authors are grateful to the study participants and would like to thank Justi Carey for her language editing.
Funding Statement
The author, Polona Selič, acknowledges the financial support of the Slovenian Research Agency, research core funding Research in the Field of Public Health No P3–0339.
Conflicts of interest
The authors declare that no conflicts of interest exist.
Ethical approval
The study procedures were conducted in accordance with the Declaration of Helsinki, and the study was approved by all the ethics committees at the university hospitals at which the study was conducted (Zagreb University Hospital, 8.1-16/179-2, 21 November 2016; Sestre Milosrdnice University Hospital, EP-18818/16-2, 28 November 2016; Merkur University Hospital, 0311-12251, 8 December 2016; Sveti Duh University Hospital, 01-1916, 1 June 2017; Dubrava University Hospital, EP 17-05-2017, 17 May 2017).

IMAGES
VIDEO
COMMENTS
Qualitative Research Questions and Purpose Statements. Qualitative questions are exploratory and are open-ended. A well-formulated study question forms the basis for developing a protocol, guides the selection of design, and data collection methods. Qualitative research questions generally involve two parts, a central question and related ...
A sample size is estimated before a qualitative study begins, but the final sample size depends on the study scope, data quality, sensitivity of the research topic or phenomenon of interest, and researchers' skills. ... Nursing Research: A Qualitative Perspective. 5th ed. Sudbury, MA: Jones & Bartlett Learning; 2012. Nicholls D. Qualitative ...
This adds credibility to both the study and qualitative descriptive research. Methods in qualitative descriptive research ... Doody O. (2017) Employing a qualitative description approach in health care research. Global Qualitative Nursing Research 4: 1-8. [PMC free article] [Google Scholar] Braun V, Clarke V. (2006) Using thematic analysis in ...
Useful terms. Some of the qualitative approaches used in nursing research include grounded theory, phenomenology, ethnography, case study (can lend itself to mixed methods) and narrative analysis. The data collection methods used in qualitative research include in depth interviews, focus groups, observations and stories in the form of diaries ...
The main strength of this study is the use of a validated and scientifically robust qualitative method to explore nursing care for patients with pressure ulcers in a geriatric ward. This could not have been achieved using a quantitative study. A limitation is the relative small number of interviewed participants.
Global Qualitative Nursing Research (GQNR) is an open access, peer-reviewed journal focusing on qualitative research in fields relevant to nursing and other health professionals world-wide. Please see the Aims and Scope tab for further information. View full journal description. This journal is a member of the Committee on Publication Ethics ...
Background Transitions in healthcare delivery, such as the rapidly growing numbers of older people and increasing social and healthcare needs, combined with nursing shortages has sparked renewed interest in differentiations in nursing staff and skill mix. Policy attempts to implement new competency frameworks and job profiles often fails for not serving existing nursing practices. This study ...
In crit-ically appraising qualitative research, steps need to be taken to ensure its rigour, credibility and trustworthiness. (table 1). Some of the qualitative approaches used in nursing research include grounded theory, phenomenology, ethnography, case study (can lend itself to mixed methods) and narrative analysis.
Good qualitative research uses a systematic and rigorous approach that aims to answer questions concerned with what something is like (such as a patient experience), what people think or feel about something that has happened, and it may address why something has happened as it has. Qualitative data often takes the form of words or text and can include images. Qualitative research covers a ...
Qualitative Research in Nursing and Healthcare Discover how to conduct qualitative nursing research with confidence Co-authored by experienced researchers, Qualitative Research in Nursing and Healthcare offers practical and applied examples for those who carry out qualitative research in the healthcare arena. With clear explanations of abstract ideas and practical procedures, this updated ...
Qualitative research in Nursing approaches a clinical question from a place of unknowing in an attempt to understand the complexity, depth, and richness of a particular situation from the perspective of the person or persons impacted by the situation (i.e., the subjects of the study).. Study subjects may include the patient(s), the patient's caregivers, the patient's family members, etc ...
Aim: This paper is a report of an integrative review conducted to critically analyse the contemporary use of qualitative case study methodology in nursing research. Background: Increasing complexity in health care and increasing use of case study in nursing research support the need for current examination of this methodology. Data sources: In 2007, a search for case study research (published ...
While many books and articles guide various qualitative research methods and analyses, there is currently no concise resource that explains and differentiates among the most common qualitative approaches. We believe novice qualitative researchers, students planning the design of a qualitative study or taking an introductory qualitative research course, and faculty teaching such courses can ...
Qualitative research is critical for studies about regulatory issues in nursing and across all health professions. When in-depth stakeholder perspectives are needed, qualitative approaches are often the best methodological choice to ensure their viewpoints and experiences are captured when evaluating the consequences of policy implementation or when informing regulation design.
In study done by Hart and Rotem stressful events for nursing students during clinical practice have been studied. They found that the initial clinical experience was the most anxiety producing part of their clinical experience [ 4 ]. The sources of stress during clinical practice have been studied by many researchers [ 5 - 10] and [ 11 ].
Appraising Quantitative and Qualitative Research. The articles below provide a step-by-step appraisal on how to critique quantitative and qualitative research articles: Ryan, F., Coughlan, M. & Cronin, P. (2007). Step-by-step guide to critiquing research. Part 1: quantitative research. British Journal of Nursing, 16(11), 658-663.
1.1. Background. Research indicates that there is a potential for patients to improve safety (Davis, Jacklin, Sevdalis, & Vincent, 2007; Vincent & Coulter, 2002) and that patients are willing and able to be involved in safety‐related work (Waterman et al., 2006 Wright et al., 2016).However, several barriers to involving patients in improving patient safety has been identified and organized ...
It is so easy to confuse the words "quantitative" and "qualitative," it's best to use "empirical" and "qualitative" instead. Hint: An excellent clue that a scholarly journal article contains empirical research is the presence of some sort of statistical analysis. See "Examples of Qualitative and Quantitative" page under "Nursing Research" for ...
Qualitative research has an important place in nursing science and is becoming increasingly recognized. Qualitative research in nursing mainly deals with the lived experiences of patients and nurses. In the field of chronic illness, qualitative research has brought to the open some of the processes chronically ill patients undergo and what it ...
Women's power in hospital-based nursing: A critical qualitative study. Journal of Advanced Nursing, 79 (2023), pp. 798-810, 10.1111/jan.15550. View in Scopus Google Scholar. Glaser and Strauss, 1967. ... Qualitative research: The essential guide to theory and practice. Routledge, London (2013) Google Scholar.
This abstract has several indications that this is a qualitative study: the goal of the study was to explore the subjects' experiences. the researchers conducted open-ended interviews. the researchers used thematic analysis when reviewing the interviews. Based on Eastern Michigan University Library Libguide Quantitative and Qualitative Research
Therefore, in this study, this approach was selected to gain a comprehensive understanding of hospice nurses' perceptions regarding occupational stressors. This study was reported following the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist. 2.2. Settings, Recruitment, and Sampling
Nursing: Quantitative vs. Qualitative? A guide for students in the CSUF Nursing program. Home; Articles Toggle Dropdown. ... This diagram should help you to determine whether the research you are looking at is qualitative or quantitative. NOTE: This is a brief guide and might not be correct in every instance
Introduction Studies have reported different results of evaluation methods of clinical competency tests. Therefore, this study aimed to design, implement, and evaluate a blended (in-person and virtual) Competency Examination for final-year Nursing Students. Methods This interventional study was conducted in two semesters of 2020-2021 using an educational action research method in the nursing ...
Clinical research nursing and factors influencing success: a qualitative study describing the interplay between individual and organisational leadership influences and their impact on the delivery of clinical research in healthcare ... (2018) Professional identity and the Clinical Research Nurse: A qualitative study exploring issues impacting ...
This study aimed to explore the stressors experienced by older patients with stroke in convalescent rehabilitation wards in Japan. Semi-structured interviews were conducted with four stroke patients aged > 65 years who experienced a stroke for the first time in their lives. The interviews were analyzed using the Steps for Coding and Theorization method for qualitative data analysis. The ...
A qualitative research design was employed using semi-structured interviews to understand experiences of occupational therapists and their involvement in social prescribing. The study has been reported following Consolidated criteria for reporting qualitative research (COREQ; Tong et al., 2007). The core research team consisted of three ...
This study compliments prior research that people should be offered sexual health and PrEP education at a younger age to increase awareness of risk, foster change in social norms and enhance willingness to seek out prevention services [40, 41]. To meet the resulting growing need for PrEP educators, healthcare professionals should receive up-to ...
Quantitative Research: A research method that involves collecting and analyzing numerical data to test hypotheses, identify patterns, and predict outcomes. Exploratory Research: An initial study used to investigate a problem that is not clearly defined, helping to clarify concepts and improve research design. Positivism: A scientific approach that emphasizes empirical evidence and objectivity ...
Discussion. Nurses with burnout provided an insight into their experience and attitudes, and the problems created by burnout. Given the poor sense of knowledge about this syndrome, there is a need to implement education on burnout in nursing school curricula, and clear strategies in the ICU environment, i.e. information, awareness-raising, and specific guidelines on coping, burnout detection ...