- Get new issue alerts Get alerts
- IARS MEMBER LOGIN

Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Fire in the Operating Room: A Case Report and Laboratory Study
Barker, Steven J. PhD, MD; Polson, J. Scott MD
Department of Anesthesiology, The University of Arizona College of Medicine, Tucson, Arizona
June 15, 2001.
Address correspondence and reprint requests to Steven J. Barker, PhD, MD, Professor and Head, Department of Anesthesiology, The University of Arizona College of Medicine, 1501 North Campbell Avenue, Tucson, AZ 85724-5114. Address e-mail to [email protected] .
In July, 1998 a fire occurred in an operating room (OR) at the University Medical Center in Tucson, AZ. A patient was burned on the face, neck, and shoulders by the fire, which started during cranial burr-hole placement under monitored anesthesia care. This paper describes the actual case in some detail. The incident was simulated as accurately as possible in a laboratory experiment, in an attempt to determine specific risk factors for this event. The experiment found that a specific combination of factors was required to produce a fire similar in appearance to the one in the OR. The risk factors determined in these experiments are discussed in the context of previous reports of OR fires. Although other reports demonstrate some common characteristics of these events, the fire at the University Medical Center appears to be unique within the literature regarding the specific chain of events that led up to it.
Fires in operating rooms (ORs) are rare events, but they usually have serious if not grave consequences. Most OR fires are not reported in the open literature because of liability issues. In this paper we describe a fire that occurred in the OR at University Medical Center in Tucson, AZ, in 1998. A patient was seriously burned on the head and neck, requiring 2 mo in the intensive care unit (ICU) as a result.
After detailed interviews with the operating room team who participated in the case, we performed laboratory experiments in an attempt to recreate the circumstances of the fire. The results of those experiments established some key factors that led to the fire. In the Discussion we examine these factors in the context of the rather sparse existing literature on OR fires. We conclude with tentative recommendations for avoiding the type of event that occurred in our OR.
Case Report
A 73-yr-old Caucasian man was scheduled for bilateral parietal burr-holes to evacuate a subdural hematoma at the University Medical Center in Tucson, AZ—the primary teaching hospital of the University of Arizona College of Medicine. The patient had severe Parkinson’s disease treated with Sinemet® (combination of levodopa and carbidopa) (DuPont Pharma, Wilmington, DE), and postviral cardiomyopathy with a measured ejection fraction of <20%. Because of his risk factors for general anesthesia, and at the patient’s request, the burr-hole procedure was performed under monitored anesthesia care (MAC).
The patient was brought to the OR without premedication, and connected to standard monitors, including electrocardiogram, automated sphygmomanometer, pulse oximeter, and capnograph. A clear plastic mask (Model 1041 Oxygen Mask; Hudson Respiratory Care, Inc., Temecula, CA) was loosely strapped to his face, and oxygen was introduced through the mask at 6 L/min. The head was shaved, and the skin surrounding the right parietal surgical site was prepared with a commercially available surgical solution of Iodofor (0.7% available iodine) in 74% isopropyl alcohol.
After preparing the site and allowing at least 2 min drying time, as recommended in the manufacturer’s instructions, the surgical field was draped. First, the field was “squared off” using a barrier of surgical towels. Next, a layer of Ioban™ Antimicrobial Incise Drape (3M Corporation, St. Paul, MN) was applied to the skin over the field, also covering the edges of the towels. Ioban is a clear plastic adhesive drape through which an incision can be made. Ioban will not adhere to a wet surface. Then a standard paper surgical drape (Baxter, Inc., Irvine, CA) was applied over the Ioban. The paper drape covered the entire head, neck, and chest area, with a roughly 15 cm diameter hole where it adhered to the Ioban.
The burr-hole procedure on the right side of the head was uneventful, the skin was closed, and the surgical drapes and Ioban dressing were removed. The head was turned slightly to the opposite side, and the site preparation was repeated as before, using the alcohol/iodine solution and recommended drying time. Surgical towels and a new Ioban dressing were applied to the left parietal side, followed again by a paper drape. The oxygen mask was left in place with a 6 L/min flow rate. The patient was responsive but sedated when the second draping took place.
A 3-cm skin incision was made using a scalpel, cutting directly through the Ioban dressing in the usual fashion. Then the electrosurgical monopolar pencil (“Force 2” Electrosurgical Generator; Pfizer Valley Labs, Boulder, CO) was used to incise the pericranium, using a setting of 3 for cutting. During the first activation of the electrosurgical unit (ESU), a muffled “pop” was heard. This was followed almost immediately by the appearance of smoke from under the paper drapes. The surgeon acted very quickly and removed the entire drape from the patient’s head. According to the surgical team, the head was fully engulfed in a “ball of flame” as the drapes were removed. The oxygen mask was also observed to be in flames. The paper drapes themselves were not on fire, and the surgeon immediately used these to smother the flames. At the same time, the anesthesiologist turned off the oxygen flow to the mask. Observers reported that the entire fire lasted <15 s from ignition to complete extinction.
The patient appeared stunned, but was still conscious and moving after the fire was extinguished. He had obvious burns and soot on his face, neck, and upper chest. Because of the possibility of airway burns and inhalation injury, general anesthesia was induced and an endotracheal tube was placed after consultation with the patient’s family. The patient was sedated, supported with mechanical ventilation, and then transferred to the ICU.
The burns to the face and neck eventually proved to be second degree, and all areas healed without surgical intervention. However, the patient’s ICU course lasted approximately 2 mo and was complicated by pneumonia, difficulty weaning from mechanical ventilation, and intolerance to enteric feeding. Some of these problems appeared related to his preexisting conditions of Parkinson’s disease and cardiomyopathy. He was eventually transferred from the ICU to a rehabilitation center, and then home.
To determine the causes and mechanisms of this OR fire, we performed multiple laboratory simulations of the event. A full-scale manikin made of a nonflammable plastic was used to simulate the head, neck, and upper torso of the patient ( Fig. 1 ). To provide an electrical current pathway for the ESU, a 3 × 3 cm area of the manikin’s “skin” at the surgical site was covered with a thin layer of aluminum. One corner of this piece was connected to the return pad outlet of the ESU. This aluminum skin was an artifice made necessary by the fact that the manikin’s body has a much lower electrical conductivity than the human body. For the ESU to generate the localized heating responsible for its action, an electrical current must flow from the electrode tip into the patient. This current is normally returned to the ESU through the conductive pad on the patient’s skin. This pad is incorrectly referred to as the “grounding pad.” It is not an electrical ground, and it is properly called a “return pad” or “dispersive electrode.”

All experiments were performed under a fume hood, whose exhaust fan was activated at the end of each experiment to evacuate smoke. The experiments were photographed by a VHS video camera equipped with a continuous timer display, as well as by a 35-mm still camera.
In the first experiment, we attempted to duplicate as closely as possible the circumstances of the OR fire. The manikin was placed on a bed sheet with a small towel under the back of the head in the same manner as in the actual case. The clear plastic oxygen mask (Model 1041; Hudson Respiratory Care, Inc.) was placed over the nose and mouth, and the oxygen flow was set at 6 L/min ( Fig. 1 ).
The head and one side of the face were prepared with the alcohol/iodine solution using the sponge applicator provided with the product. During the preparation process, we noted that a few drops of solution dripped onto the towel and bed sheet, even though we were very cautious in the application. The package insert for the solution provides the following warning: “Do not allow to pool or soak into materials and do not use around ignition sources until dry (2–3 min).” We allowed exactly 2 min for drying.
The surgical site was then covered with the Ioban occlusive drape as was done in the OR. The paper surgical drape was then placed over the Ioban, leaving a 15-cm hole over the surgical site. Oxygen concentration was measured at several locations under the drape (POET II Gas Analyzer; Criticare, Waukesha, WI) and was found to range from 35% to 50% during steady-state conditions. The Valley Labs ESU intensity was set on 3, the same setting that was used in the OR. At the time of ESU activation, both video and still cameras were operating.
The experiment was repeated nine times. Four of these were done using the exact sequence of events that we believe occurred in the OR. Each experiment was filmed from a different angle to determine exactly where the fire began. In the other five simulations, we altered some of the variables that were expected to be important factors in the occurrence of fire: electrocautery setting, oxygen flow rate, amount of preparation solution applied, and the configuration of the surgical drapes.
In the first experiment, the ESU pencil electrode was applied to the surgical site, and sparks were observed at the tip of the electrode, as they typically appear in the OR ( Fig. 2 ). After roughly 3 s of application, a muffled “pop” sound was heard. Five seconds later, smoke began to appear from under the paper drapes ( Fig. 3 ). We did not interrupt the process, although it was apparently at this point in the actual case that the surgeon removed the paper drapes from the patient. After another 8 s, bright yellow flames burst through the paper drapes ( Fig. 4 ). Within 10 s after that, the entire head and surgical drapes were involved in flame ( Fig. 5 ). The plastic oxygen mask produced bright yellow flames and quickly melted onto the manikin’s face. The laboratory was rapidly filling with smoke, and the experiment was terminated at this point. The oxygen supply was turned off, and the fume hood fan was activated. The remaining flames were smothered with towels.

At this point we carefully inspected our manikin. The melted oxygen mask was adherent to the manikin’s face. During the actual fire, events were stopped as soon as smoke came from under the paper drapes, but the oxygen mask was melted nevertheless. The manikin’s face and neck were stained with black soot, but there was no apparent thermal damage to the plastic itself. The manikin was cleansed with soap and water, and reused in the additional experiments.
In the next three experiments, we created the same initial conditions, but filmed the events from various angles to determine precisely where the fire began and how it propagated. In one experiment, we installed a Plexiglas ® sidewall so that we could see into the closed cavity formed by the surgical drape. Through this transparent wall, we observed that when the ESU ignition source was activated, the fire spread almost instantly through the closed space within the drapes. Flames were then seen originating from the towel on which the head rested, in the area whereupon some preparation solution had dripped ( Fig. 6 ). The cup-shaped depression in the lower right of the figure is the manikin’s shoulder socket; it had no arms. The plastic mask itself ignited a few seconds later and appeared to burn with an extremely hot flame.

We tested three of the plastic masks separately from the manikin setup, and found that in the absence of oxygen flow an open flame could melt them, although they did not themselves support combustion. However, when oxygen was flowing through a mask, even at 3 L/min, the mask could be easily ignited and would burn with an intense white flame.
In the remaining experiments, we varied the initial conditions one factor at a time to determine the exact ingredients required to produce a fire of this sort. We found the following consistent results:
- 1) If there was no flow of supplemental oxygen to the plastic mask, there was no fire. The paper drapes could eventually be ignited by aggressive application of the ESU, but the resulting fire was very slow burning and would self-extinguish within seconds.
- 2) If the alcohol-based preparation solution was not used, there was no fire. Furthermore, if we allowed 5 min of drying time after solution application (the manufacturer’s recommendation is 2–3 min), there was no fire.
- 3) If there was no closed space formed by a “tent” of surgical drapes covering the head, there was no fire. The alcohol-based preparation solution, the supplemental oxygen supply, the closed tent of surgical drapes, and the electrocautery ignition source were all required ingredients to produce a fire in our simulation.
Well-established principles of chemistry require three ingredients for the rapid exothermic reaction known as “fire”: fuel, oxidizer, and an ignition source. There are exceptions to this rule called “hypergolic fuels” that, when mixed with the appropriate oxidizer, will immediately begin to burn without an ignition source. Such chemicals are used as rocket fuels, but there are currently none present in the OR setting. Hence we can assume that all three of the ingredients listed above must be present to have an OR fire.
Among the three required ingredients, the ignition source and oxidizer are obvious in our case. Ignition was provided by the ESU, which, by design, generates high local temperatures to either cut or cauterize tissue. The ESU has been implicated as an ignition source in many previous OR fire reports. In our experimental simulation, no fires occurred without the activation of the ESU. The source of oxidizer in our case is equally obvious: 6 L/min of 100% oxygen being piped into a plastic mask in a closed space formed by surgical drapes. As stated above, this created measured oxygen concentrations as large as 50% under the drapes. When supplemental oxygen was not provided, no significant fire occurred in our experiment.
The source of fuel in our OR case was more controversial. The paper surgical drapes, the plastic mask, and “lint” from surgical towels or hair on the patient’s skin were all proposed as possible fuels in this fire. Our experiments showed that both the surgical drapes and the oxygen mask did not burn until late in the process, well after the manikin was engulfed in flames. Lint from towels or sheets seems an unlikely source, because we observed the flames to “flash” almost instantly from the ignition point throughout the surgical tent. Furthermore, when no preparation solution was used in the experiment, there was no fire. The sheets and towels used in the experiment were identical to those used in the OR.
We conclude from our laboratory experiments that the alcohol-based preparation solution (74% isopropanol) did indeed provide the fuel for this fire. Isopropyl alcohol is much more volatile than water: isopropanol vapor pressure is 46 mm Hg at 25°C and isopropanol has a boiling point of 82°C; water vapor pressure is 23.8 mm Hg at 25°C with a boiling point of 100°C. Any residual liquid alcohol, either on the patient or soaked into the linens, will vaporize within a closed space, such as that formed by the surgical drapes. The resulting alcohol vapor and increased oxygen concentrations can create a highly flammable mixture, simply waiting for an ignition source. There is, of course, no guarantee that our laboratory experiment was a completely accurate representation of what happened in the OR, and other experts may disagree regarding the primary fuel in this fire. However, our experiments clearly demonstrate that a very similar fire can be created by the combination of electrocautery, supplemental oxygen, and alcohol.
OR fires are uncommon, but when they occur the results are often disastrous for both patients and OR personnel. Fortunately for our patient, quick recognition and action on the part of the surgical team prevented him from receiving third-degree burns or any permanent disfigurement. Nevertheless, he experienced a prolonged ICU course with considerable morbidity. Other patients have been less fortunate. In October 1988 at Cedars Sinai Medical Center in Los Angeles, a fire occurred during cardiac surgery on a 19-day-old infant (1) . The fire was apparently ignited by an ESU. The flames spread from a gauze sponge to the surgical drapes and were intensified by large oxygen concentrations under the drapes. The child was engulfed by the fire and died as a result.
In 1990, at UCLA Medical Center in Los Angeles, fire occurred during emergency surgery on a 26-year-old trauma victim (2,3) . An ESU pencil electrode that was hanging near the bottom of the surgical drapes apparently ignited the fire. The flames spread rapidly and soon engulfed the patient despite staff attempts to quench them. Dense smoke forced staff members to retreat from the room. By the time the fire department arrived and extinguished the fire, the patient was dead and the body was described as charred.
Many OR fire reports have implicated paper surgical drapes as a fuel. As a result, the government and various standard-setting organizations (AORN, Consumer Product Safety Commission, and the National Fire Protection Agency) have designated flammability standards for all fabric and paper materials used in the operating suite (4) . Nevertheless, paper drapes and other materials meeting current standards can and will burn in an oxygen-enriched atmosphere. We were surprised in our experiments by the intense, hot flames with which a commonly used plastic oxygen mask will burn once ignited during oxygen flow.
Other reported OR fires include seemingly bizarre circumstances, such as the explosion of bowel gas, endotracheal tube fires during laser surgery, patient’s gown on fire, and facial hair fire (5) . Based on anecdotal information, there are at least 20–30 surgical patient fires each year in the US (5) . Most of these events are not reported in the literature. In nearly all reported cases, the classic “triangle” of fuel, oxidizer, and ignition can be identified retrospectively. ECRI (formerly called Emergency Care Research Institute), a nonprofit healthcare safety organization, concludes: “most such fires could be prevented if the surgeon and the anesthesiologist understood the nature of the hazard and how to minimize the risks.” ECRI has provided an excellent summary of the ingredients and risk factors of OR fires, including the most common fuels encountered in the surgical setting, shown in Table 1 (5) .

In the University Medical Center (Tucson, AZ) fire, the three required ingredients of an OR fire came together in an unusual manner. Ignition was provided by an ESU, a common theme in these events. The enriched oxygen environment occurred as a result of oxygen flow to a mask under the surgical drapes during a “MAC” case. The fuel was most likely provided by the vapors of an alcohol-based preparation solution.
In view of what we have learned from this event and the laboratory experiments, how can we avoid similar fires in the future? We make three recommendations.
- 1) As stated in previous reports, before using any electrosurgical device, we must be certain that a fuel-oxidizer combination is not present in or near the surgical field.
- 2) In a head-neck procedure in which the patient’s trachea is not intubated (i.e., MAC or mask anesthesia), we must try to avoid large oxygen concentrations in the closed space within the surgical drapes. In healthy patients, we can flow air into the plastic mask rather than 100% oxygen. If supplemental oxygen is required, we should use only the minimum amount needed to keep Spo 2 within an acceptable range. This usually does not require 6 L/min of 100% oxygen.
- 3) Finally, we must be very cautious with flammable preparation solutions, especially when they are used on the head-neck region during “MAC” cases, wherein large local oxygen concentrations may be unavoidable.
We may never eliminate all risks of OR fires, but we can minimize them by educating OR personnel on this subject; by carefully investigating each incident to determine causes and risk factors; and by reporting fires in the literature when they occur.
- Cited Here |
- View Full Text | PubMed | CrossRef
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Simulation education in anesthesia training: a case report of successful..., successful spinal anesthesia in a patient with huntington’s chorea, cardiac arrest during neuraxial anesthesia: are all databases comparable, systolic anterior motion of the mitral valve with left ventricular outflow..., cardiac arrest during neuraxial anesthesia: frequency and predisposing factors....
- ACS Foundation
- Diversity, Equity, and Inclusion
- ACS Archives
- Careers at ACS
- Federal Legislation
- State Legislation
- Regulatory Issues
- Get Involved
- SurgeonsPAC
- About ACS Quality Programs
- Accreditation & Verification Programs
- Data & Registries
- Standards & Staging
- Membership & Community
- Practice Management
- Professional Growth
- News & Publications
- Information for Patients and Family
- Preparing for Your Surgery
- Recovering from Your Surgery
- Jobs for Surgeons
- Become a Member
- Media Center
Our top priority is providing value to members. Your Member Services team is here to ensure you maximize your ACS member benefits, participate in College activities, and engage with your ACS colleagues. It's all here.
- Membership Benefits
- Find a Surgeon
- Find a Hospital or Facility
- Quality Programs
- Education Programs
- Member Benefits
- QI Resources
- Case Studies
- Reducing Returns to the Op...
Reducing Returns to the Operating Room: A Patient Quality and Safety Initiative
Holston valley medical center, ballad health, general information.
Institution Name: Holston Valley Medical Center, Ballad Health
Primary Author and Title: Elizabeth Jackson, MD, MBA, FACS
Co-Authors and Titles: Alisha Westmoreland, RN, and Sara Shields-Tarwater, MD
Name of Case Study: Reducing Returns to the Operating Room: A Patient Quality and Safety Initiative
What Was Done?
Global problem addressed.
While technology has continued to advance the surgical field toward more minimally invasive, cost-conscious, patient satisfaction driven procedures, the battle to prevent surgical complications has also taken center stage as a means to improve patient outcomes and reduce overall health care costs for both patients and hospitals. Complications and their associated costs after surgical intervention vary widely in both complexity and cost. Wound infections alone can vary from estimated costs of $400 to $30,000 dependent on complexity. 1 Major surgeries with significant complications, including those requiring re-operation, can surge cost by five times, approximating an increase of $159,345 per case. 2 Many guidelines and initiatives have been developed to reduce surgical complications. Initiatives like Enhanced Recovery After Surgery (ERAS) have greatly reduced complications, re-operations, and readmissions all while improving costs and satisfaction. 3 Ideally, developing an overall plan that incorporates a multi-initiative approach to reduce complications and minimize returns to the operating room while decreasing length of stay and improving patient satisfaction is key.
Identification of Local Problem
In 2017, an initiative was started within our facility to increase efficiency, quality of care, and safety within the operating room at Holston Valley Medical Center. During a retrospective review of cases, concern arose regarding patient returns to the operating room. These issues were brought to light when multiple returns labeled as “planned,” consisting often of acute care surgical patients left in discontinuity with wound vacs, were called out as a concern for quality of care. As an example, a single patient experienced more than 30 returns to the operating room by multiple surgeons. While a reasonable number of returns to the operating room are expected, we began our journey reviewing all returns in attempt to identify specific areas of improvement. Review of the nearly 11,000 cases performed yearly in the main operating room at our facility demonstrated that one out of every six patients experienced a return to the operating room, most of which were unplanned. These returns led to decreased patient satisfaction and increased health care cost not only for the hospital, but more importantly the patient. The return cases were clustered between acute care surgery and orthopaedic surgery, many which were emergent/urgent in nature.
Our goal was to focus on improving quality of care by working through a team effort to identify and reduce returns to the operating room while improving overall outcomes. We identified that critical to the success of this project was the cooperative involvement of our quality team, surgeons, and operating room team, combined with overall support of our hospital’s administrative team. Of upmost importance was obtaining surgeon buy-in while maintaining a non-punitive approach in both case review and communication.
How Was the Quality Improvement (QI) Activity Put in Place?
Context of the qi activity.
Holston Valley Medical Center is a not-for-profit, tertiary center located in Kingsport, TN. During the time this initiative was started, Holston Valley served as one of two Level I trauma centers in our region. Since that time, Holston Valley has undergone a merger into a larger system, Ballad Health. In order to minimize duplication and better serve our communities, Holston Valley became a Level III trauma center while remaining a large tertiary care center in our region.
Since 2016, Holston Valley has participated in the American College of Surgeons National Surgical Quality Improvement Project. We are an active member in the Tennessee Surgical Quality Collaborative. Our involvement in both these areas dramatically increased from 2016 forward. As a result, our focus turned to improving areas demonstrated on our ACS NSQIP risk-adjusted score card.
While focusing on overall improvements in surgical site infections, length of stay, and moving forward with starting our ERAS program, reducing returns to the operating room became a priority.
Planning and Development Process
Once our return to the operating room rates were determined to be 16.67 percent, we knew as a facility that we must act swiftly. The process for improvement started by designating that all cases that returned to the operating room within thirty days of the original operation would be reviewed weekly then presented to an overseeing committee, the Incident Review Committee (IRC). Additional review can be provided if necessary at monthly Peer Review or existing Quality Committee meetings. These committees report to the Medical Executive Committee which in turn reports to the Community Board for Holston Valley.
In order to obtain buy-in from the surgeons, establishing their involvement early was critical. The Medical Director of the Operating Room, a surgeon, reviewed all return to the operating room cases. Once presented to the IRC, the attending surgeon was sent a letter either stating that there were no concerns of care identified or asking for further explanation. This letter serves to keep the surgeon in the loop for which cases are being reviewed and allows them active participation in the quality review process. With consensus reached amongst surgeons that reducing returns and therefore improving patient care, our project moved forward rapidly.
Description of the Quality Improvement Activity
Having garnered the support of both surgeons and administration, we began outlining a clear process that incorporated both the involvement of our quality team and our medical staff to facilitate change. The overall process was two-pronged.
First, we established a process to review each return to the operating room. Second, we focused on changes that can be made in the operating room to reduce potential causes for unplanned returns.
In regard to the review process for returns to the operating room, we developed the policy to review all returns to the operating room on a case-by-case basis, regardless of whether the return was planned or unplanned. In addition, any case, for which a concern is identified, whether it involves a return to the operating room or not, can be reported through the incident report system by any staff member. This has allowed all staff members to feel empowered to report quality of care concerns in real-time for evaluation. Each return to the operating room or reported concern is reviewed in detail by the Medical Director of the Operating Room, a fellow surgeon.
Once the case is reviewed, the Medical Director reports the details of the case along with a recommendation to either validate, invalidate, or request further review to the IRC. The IRC consists of the Chief Medical Officer (CMO), Medical Staff Executive committee (President, President-Elect, Past President, and Secretary/Treasurer), Quality Physician Chair, Quality Manager, Risk Management, Chief Nursing Officer (CNO), and Pharmacy Director. At this point, the reviewed case can be deemed invalid with no concerns, valid with concerns, recommended to Peer Review for that specialty for further evaluation, or request explanation from the surgeon. Peer Review recommendations are made to the Quality Committee which forwards information to the Medical Executive Committee. Validated concerns are placed on the surgeons Ongoing Professional Practice Evaluation (OPPE) Scorecard for two years. The surgeon is contacted throughout the course of the review by letter for full transparency and allowed to contribute in dialog throughout.
The second arm of our approach to quality improvement focused on reducing potential risks contributing to returns in the operating room. A considerable portion of the focus in the area utilized a team of Infection Prevention, Quality, and Operating Room Management who drove an initiative of re-education. Emphasis was placed on reinforcing sterilization techniques, re-educating to ensure proper hand scrubbing, and patient optimization as the patient moved through all phases of the operating room. Traffic in and out of the individual operating suites was minimized. Vendors were monitored to ensure scrubs were changed, movement in and out of the operating suite was reduced, and re-education performed to reiterate not violating sterile field.
In conjunction with the implementation of our return to the operating room reduction initiative in late 2018, other initiatives contributed to reduction in returns. In November 2016 a colorectal bundle aimed to reduce colon surgical site infections was started. ERAS protocols were implemented in April 2017. Both these initiatives, as a result of reduction in surgical complications in colorectal patients, assisted with returns to the operating room and improved quality of care.
The orthopedists assisted during the initiative by helping to develop appropriate guidelines governing elective orthopaedic cases. These guidelines established body mass index (BMI) and glucose (A1C) parameters that determine if a patient qualifies for elective orthopaedic surgeries, or if weight loss/improved glucose control is required before a case can be scheduled. Appropriate antibiotic use was also closely monitored. In order to further contribute, Orthopaedics Peer Review specifically requested to review all joint infections that occur on a monthly basis.
Resources Used and Skills Needed
The staffing required for this quality improvement project was filled with existing staff members. Those staff members included: perioperative and surgical nursing staff, Operating Room Manager, Quality nurse, and Risk Management Staff member. Leadership included: CMO, CNO, Medical Director of the Operating Room, Medical Executive Committee Staff, Quality Chair. No additional staffing positions were created for this initiative. All surgeons actively participated on an as needed basis depending on cases reviewed.
No additional costs were created beyond existing costs.
Funding Sources, If Any
Funding in the form of an annual stipend from the Tennessee Surgical Quality Collaborative was utilized in the colorectal bundle and ERAS patient information and signs that contributed to this initiative.
What Were the Results?
Overall results.
When the percentage of returns to the operating room were calculated for 2017 and 2018 prior to our initiative, the data resulted with rates of return at 16.1 percent and 15 percent respectively. The raw numbers were 1,736 of 10,769 cases in 2017 experienced a return to the Operating Room. For 2018, 1,611 of 10,763 cases experienced a return. Clearly these numbers were unacceptable and demonstrate why our initiative became a priority.
After the call to action was made and a plan for a quality initiative focusing on reducing unnecessary set in motion, dramatic results followed. We calculated.
our monthly returns to the operating for all cases, planned and unplanned, from January through August of 2019. It is important to note that starting in September of 2019, Holston Valley Medical Center made the transition from a Level I to Level III trauma center. In order to preserve the integrity of the data, we stopped our data collection for this case study at that transition time. We continue to collect our return to the operating room data, but beyond that time it is not included. The results demonstrated that Holston Valley saw a reduction in returns to the operating room for all cases to 8.2 percent (Table 1).
At times during the initiative, we did experience setbacks, mostly related to lack of communication or unwillingness to participate in re-education opportunities. These experiences reiterated the need for continued open communication and utilizing our available resources to provide data in support of the initiative. For example, when resistance was met regarding guidelines for elective orthopaedic cases regarding body mass index (BMI) or appropriate antibiotic preoperatively, instead of demanding adoption of the recommendations, we relied on the Orthopaedic Service Line meeting to discuss amongst themselves, provide the most current guidelines/recommendations, and vote them into acceptance. Utilizing experts in their respective field facilitates buy-in and lends credibility to the initiative.
Cost Savings
The overall magnitude of cost savings realized by our initiative is very difficult to calculate. As cited earlier, complications range in severity, and therefore their additional health care cost also varies widely from as low as $400 to as much as $159,345. 1,2 Assuming the case volume held stable for 2019 at 10,770 cases, 8.2 percent returns to the operating room translates to approximately 883 fewer cases of varying complexity. The cost savings from this decrease in returns is demonstrated by multiple factors including fewer incurred operating room costs, decreased complications necessitating a return, and reduced length of stays.
Tips for Others
Getting Started
Fortunately, this as well as many other quality initiatives that have a significant impact do not require considerable funding. Identifying those individuals in key roles that have access to the data and collect it appropriately is critical.
Once the plan for data collection is solidified, often the data can be gathered relatively quickly. When the goal of the initiative and the plan for data collection established, early involvement with encouraged input from critical participants (surgeons, mangers, staff) is crucial. These individuals should be motivated and supportive of the task at hand.
How to Sustain the Activity
Once the pathway for data collection, monitoring, and implementation for change has been established, routinely scheduled meetings must be scheduled to allow for constant data analysis and near real-time implementation of change. It is far too easy to allow backward slipping into old habits and soon the progress made is quickly lost.
Other Tips and Considerations
Sharing of outcomes data can be a strong motivator especially to those outliers or late adopters. It is important to always remain supportive and not malignant in all interactions with data sharing. Individuals take data very personally and often will self-motivate once the data is available.
- Urban JA. Surgical Infections. Jan 2006.s19-s22. http://doi.org/10.1089/sur.2006.7.s1-19.
- Vonlanthen R, et al. The Impact of Complications on Costs of Major Surgical Procedures: A Cost Analysis of 1200 Patients. Annals of Surgery. December 2011;Volume 254(Issue 6):907-913.
- Ljungqvist O, Scott M, Fearon KC. Enhanced Recovery After Surgery: A Review. JAMA Surg. 2017;152(3):292-298.
- Research article
- Open access
- Published: 19 May 2020
Managing complexity in the operating room: a group interview study
- Camilla Göras 1 , 2 , 3 ,
- Ulrica Nilsson 4 , 5 ,
- Mirjam Ekstedt 6 , 7 ,
- Maria Unbeck 4 , 8 &
- Anna Ehrenberg 1
BMC Health Services Research volume 20 , Article number: 440 ( 2020 ) Cite this article
19k Accesses
32 Citations
Metrics details
Clinical work in the operating room (OR) is considered challenging as it is complex, dynamic, and often time- and resource-constrained. Important characteristics for successful management of complexity include adaptations and adaptive coordination when managing expected and unexpected events. However, there is a lack of explorative research addressing what makes things go well and how OR staff describe they do when responding to challenges and compensating for constraints. The aim of this study was therefore to explore how complexity is managed as expressed by operating room nurses, registered nurse anesthetists, and surgeons, and how these professionals adapt to create safe care in the OR.
Data for this qualitative explorative study were collected via group interviews with three professional groups of the OR-team, including operating room nurses, registered nurse anesthetists and operating and assisting surgeons in four group interview sessions, one for each profession except for ORNs for which two separate interviews were performed. The audio-taped transcripts were transcribed verbatim and analyzed by inductive qualitative content analysis.
The findings revealed three generic categories covering ways of creating safe care in the OR: preconditions and resources , planning and preparing for the expected and unexpected , and adapting to the unexpected . In each generic category, one sub-category emerged that was common to all three professions: coordinating and reaffirming information , creating a plan for the patient and undergoing mental preparation , and prioritizing and solving upcoming problems , respectively.
Creating safe care in the OR should be understood as a process of planning and preparing in order to manage challenging and complex work processes. OR staff need preconditions and resources such as having experience and coordinating and reaffirming information, to make sense of different situations. This requires a mental model, which is created through planning and preparing in different ways. Some situations are repetitive and easier to plan for but planning for the unexpected requires anticipation from experience. The main results strengthen that abilities described in the theory of resilience are used by OR staff as a strategy to manage complexity in the OR.
Peer Review reports
Clinical work in the operating room (OR) is dynamic, and complex, and often time- and resource-constrained [ 1 ]. Performing surgical procedures requires, specific technical and cognitive skills from OR staff, such as anticipating patients’ needs, managing changes and handling unexpected events [ 1 , 2 ]. Increased co-morbidities of patients [ 3 ], and pressure for efficiency and productivity [ 4 , 5 ] are other challenges that may influence the work in the OR. Teams in the OR interact, communicate, adapt, learn and self-organize over time [ 6 , 7 ] which are common determinants of a complex adaptive system (CAS) [ 7 ]. From the perspective of complexity there are different strategies for improving patient safety, from attempting to control complexity to embracing it by encouraging flexible behaviors [ 8 ]. Complexity requires to wisely balance thoroughness and control with flexibility and adaptations [ 9 ]. The surgical safety checklist [ 10 ] is an example of a procedure that structures safe care processes in the OR that lay ground for patient safety which also can include flexibility in the face of unpredictable events. Complexity means that work processes may be disturbed or interrupted by unpredictable events that the OR staff has to adapt to and handle [ 11 ]. Adaptations contribute to keeping the system’s performance at an acceptably high level under both ordinary and extraordinary conditions, but can also create high-risk situations [ 12 ]. According to the coordination and mobilization of many interdependent processes, support and resources in a CAS are seldom optimal which may produce strain among staff and lead them to develop compensatory strategies [ 13 ].
In the attempts to understand and influence how complex systems such as OR works, traditional ways of thinking in forms of linear causality models are insufficient. A ‘system thinking’ approach that consider the flow of interactive activities (e.g. between people, equipment, procedures) and the continuous adjustments needed to cope with system variability can help to improve safety and performance in the daily practice in an OR [ 12 ]. Patient safety in the OR should be understood by studying “work-as-done”, which reflects the reality that professionals have to deal with in their everyday clinical work, rather than through the ideal picture of “work-as-imagined” which is often presented in policy documents or action plans [ 12 ]. However, a deeper knowledge is needed to understand how “the work is described as being done” in relation to safe care in the OR.
Strategies to cope with and adapt to complexity have been described from the perspective of Resilience engineering, RE [ 14 , 15 ]. Resilience is defined as the ability of the healthcare system to adjust its functioning prior to, during, or following changes or disturbances, so that required operations can be sustained under expected and unexpected conditions [ 16 ]. From a RE perspective, rather than controlling what professionals do, patient safety is strengthened by a systemic capacity which enables professionals to be reflexive, to adapt to changing conditions, and to understand the whole system [ 14 ]. Resilient organizations is often described through four abilities: the ability to respond to events, to monitor ongoing developments, to anticipate future threats and opportunities and to learn from past failures and successes [ 16 ]. Resilience research has shown that ways of managing complexity are also characterized by abilities such as anticipation, sensemaking, trade-offs, and adaptation [ 17 ]. Operationalization of resilience in inpatient healthcare is characterized by professionals anticipating and bridging gaps by proactively monitoring and acting on problems [ 18 ]. Adaptive coordination, the ability of a team to change its coordination activities in response to unexpected events and varying task characteristics [ 19 ], are other cornerstones of effective team performance in complex settings [ 20 ]. Preoperative huddles have shown to contribute to improvements in patient safety, communication, and teamwork. Postoperative debriefings after non-routine and routine cases are other strategies that stimulated learning, and improved work processes and teamwork [ 21 ]. Behaviors to manage non-routine events in the OR are also described to include task- and information management, teaching, and leadership [ 19 ].
To cope with complexity, that is managing expected and unexpected events, resilience has been described to be important. When managing unexpected events in the OR adaptive coordination was described an important skill. However, there is a lack of explorative research addressing what makes things go well and how the OR staff describe they do when responding to challenges and compensating for constraints. This can be understood by describing how health professionals describe that work is done in a clinical setting. Knowing how surgical teams manage complexity will be an important contribution to a deeper understanding of how patient safety is created in a collaborative way in the OR. The aim of this study was therefore to explore how complexity is managed as expressed by operating room nurses (ORNs), registered nurse anesthetists (RNAs), and surgeons, and how these professionals adapt to create safe care in the OR.
Setting and sample
This study employed a qualitative explorative design by using group interviews with OR staff. The interviews were conducted at two central OR departments at one county hospital and one local county hospital in mid-Sweden. Each hospital had one department for day surgery and one central OR department. The central OR department at the local county hospital served both acute and elective surgical and orthopedic patients, whereas the OR department at the county hospital in addition also served gynecological patients. Teams in Swedish ORs commonly comprise six different professionals: ORN, operating surgeon (surgeon), assisting surgeon, circulating nurse (commonly a licensed practical nurse) anesthesiologist and RNA. In Sweden, RNAs are allowed to maintain anaesthesia with direct or indirect supervision of the anesthesiologist [ 22 ]. The sample consisted of three professional groups of the OR-team, including ORNs, RNAs and operating and assisting surgeons in four group interview sessions, one for each profession except for ORNs for which two separate interviews were performed. Two ORNs at the county hospital, who participated in the pilot interview, were included, to achieve large enough group sizes. The four groups comprised a convenience sample of professionals who were available to be released from clinical work and who had been employed at the OR for least 6 months. The interviews were conducted at separate occasions divided in groups by professional specialization. The informants’ characteristics are given in Table 1 .
Data collection
Open questions were asked based on an interview guide which had been developed by the researchers. The interview guide was pilot tested and resulted in a minor rearranging of the themes, but no revisions or changes in content were needed. The interview guide consisted of five questions including “Can you tell me how you plan your day at work?”, “Could you tell me about situations when the work proceeded according to plan?”, “Could you tell me about situations when work did not proceed according to plan?”, “What enables and what hinders you from being able to do the work as planned?”, and "Do you ever have to abandon routines. To get permission to conduct the study, information was provided both verbally and in writing to the medical director of the surgical department and nurse managers at the OR department who invited their staff to participate. Those who volunteered gave their written informed consent after receiving verbal and written information including the voluntary nature of participation and the ability to withdraw at any time without further explanation, and confidential treatment of data.
The data were collected during February and April 2018, via scheduled 1-h interviews in an undisturbed and quiet location at the workplace. At the beginning of each session, the moderator and the assistant (i.e., the first and last authors) gave a brief presentation of the study, including the aim of the study and why the participants were selected. The discussions were led by the same moderator (first author) throughout all four interviews. The interviews were audiotaped, and field notes were taken by the assistant. The interviews lasted between 50 and 59 min and were transcribed verbatim.
Data analysis
The interviews were analyzed by using inductive qualitative content analysis focused on the manifest content [ 23 ]. All the authors are registered nurses or RNAs with experience of healthcare and the OR, and all participated throughout the analytical process to identify codes, sub-categories, and generic categories. Transcripts were read thoroughly several times to obtain a sense of the whole. Content that related to the aim of the study was noted first in the margins of the text and then on a coding sheet. The codes were based on similarities and differences and were sorted into sub-categories which were then interpreted and aggregated into broader generic categories. The different steps were discussed within the research team. To maintain consistency, there was a movement back and forth between the transcripts, codes, sub-categories, and generic categories. To reach consensus, the research group independently categorized the codes and discussed the findings several times. The analysis generated three generic categories. An example of the analytical procedure is presented in Table 2 .
When analyzing the group interviews three generic categories emerged from the sub-categories of each professional group: preconditions and resources, planning and preparing for the expected and unexpected, and adapting to the unexpected. In each generic category, one sub-category was common and shared between the three professions: coordinating and reaffirming information, creating a plan for the patient and undergoing mental preparation, and prioritizing and solving upcoming problems as displayed in Table 3 . Subsequently the generic categories with specific sub-categories representative for each profession follows.
Descriptions of how safe care is created shared by three professional groups
Preconditions and resources, coordinating and reaffirming information.
Coordinating and reaffirming information was a sub-category that emerged as common to all three professions. If critical situations or changes in patient conditions occurred, communication was described as central to creating safe care. Having the same information was also considered essential for a well-functioning surgical teamwork. When a change of plans was called for, the ORNs often used communication with external support services such as coordinators at the OR department to convey information, get support, and obtain new equipment. When issues occurred regarding surgical instruments, the ORNs expressed communication with the surgeon to be important in order to allow prioritization and planning. The surgeons said that they interpreted communication depending on their understanding of the urgency of the situation, which helped them to prioritize. Safe communication was perceived by both ORNs and RNAs to be easier in a small workplace with shorter information paths. The ORNs said that when the team was less integrated, communication within the sub-team (e.g. ORNs and surgeons) was even more important for safe care:
“Communication is more important when the team is not well integrated. That applies to talking to each other, who does what, and what do you need help with, so you don’t get parts of the team taking it for granted that others are doing it.” (ORN)
For the RNAs, an essential precondition was the ability to get access to colleagues quickly by having a telephone nearby. From the surgeon’s perspective, communication was a prerequisite for conveying difficult moments during surgery that required an increased focus from the entire surgical team.
Planning for the expected and unexpected
Creating a plan for the patient and undergoing mental preparation.
An important sub-category common to all three professions emerged as creating a plan for the patient and undergoing mental preparation. In order to be mentally prepared, the professionals created a plan for the patient before the procedure. They read about the patient individually or together to create a mental model and a shared plan. From identified potential patient risks they planned what might be needed for that patient and procedure. The ORNs described how they planned and prepared for equipment adjustments prior and during a surgical procedure, based on the individual needs of both the surgeon and the patient:
“It’s based on what’s best for the patient — to ensure that the surgery will be as good as possible. Don’t hurt the patient. How does it look, what are the things you have to watch out for when you use leg support — we’re thinking about that all the time.” (ORN)
While much of the work was standardized, it was then supplemented after the ORNs had created their mental model or seen the patient. The RNAs anticipated what could happen and adjusted the plan for the patient. The plan was also communicated and structured together with the anesthesiologists, based on the anticipated scenarios. The surgeons said that in most cases they knew the patient, when this was not the case, they created a mental model of the patient and the procedure by consulting the patient record and talking to the patient:
“Often you’ll already know the patient, but if you don’t then you read the patient record and create a mental picture of them.” (Surgeon)
For the RNAs to be mentally and practically prepared clinical experience emerged as a crucial underlying prerequisite. The RNAs described a standardized routine and workflow in which information was obtained from different systems, including reported patient status by the ward nurse. Preoperatively, they also anticipated possible scenarios by inspecting and talking to the patient. Hence, possible scenarios could be identified and anticipated in advance:
“Yes, you’re prepared for it ... You might ‘read’ the patient and understand that this isn’t going to work. Like, I can see that 82-year-old Agda hasn’t had anything to drink since noon yesterday, so she’s already dehydrated…a large surgical intervention, and then when I’m positioning her I find candy under her pillow. I mean, then it’s a completely different scenario.” (RNA).
The RNAs argued, if they planned and prepared carefully in advance this was not a problem:
“Otherwise, once the process has started things just keep rolling. And you’ve, like, created this whole plan for the patient. That’s why we plan — so that won't happen.” (RNA)
Adapting to the unexpected
Prioritizing and solving upcoming problems.
Adapt to the unexpected, by prioritizing and solving upcoming problems was the third sub-category that emerged as common to all three professions. When unexpected issues occurred during a surgical procedure, both RNAs and ORNs said that they assessed the risks against the benefits and adapted to the situation. The ORNs expressed that prioritizing the saving of life over ensuring sterility was an important strategy for safe care:
“Sometimes you can’t scrub the patient — life is more important than ensuring sterility, and you can deal with that later. If an infection occurs, you have to treat it then. For example, we don’t scrub the urgent Cesarean sections, or the ruptured aortas when they arrive directly from the emergency room. Those aren’t the times to argue if someone comes in in white clothes, without a surgical cap and coat.” (ORN)
When problems and issues occurred during surgery, the surgeons and the RNAs expressed that problems had to be solved and it was not an option to allow things to go wrong. Surgeons described that consultation took place with more experienced colleagues or specialized hospital clinics. The problem had to be solved, and inaction was not an option.
The ORNs said that when unexpected equipment-related issues occurred, they checked the equipment, asked for a replacement or handed the problem over to a colleague and continued to focus on the surgery without being affected. The surgeons said they prioritized the interruptions that were perceived as urgent. For the RNAs, intraoperative changes in patient status were anticipated by monitoring trends in the patient’s vital signs, which allowed them to be prepared and hence respond quickly to changes. Being flexible and responsive was one of the RNAs professional skills and perceived as an inherent ability of an RNA. The RNAs explained that when facing changes or challenges they adapted to the new situation and asked for help from their colleagues. To adapt, they used previously created plans B and C, as a part of their mental model when preparing for the procedure:
“It’s the planning ahead, you plan the surgical procedure. As I said, experience from this or that can happen, but then you have a plan B. Perhaps you also have a plan C as well, as it’s like … it’s people, and it can’t go wrong, you have to handle it.” (RNA)
The surgeons perceived that working in the OR meant having to be prepared for changes and variations that sometimes contributed to a lack of focus. Unexpected urgent procedures were taken care of ad-hoc in the work process. Handling this required flexibility, adaptation, prioritization and the ability to relate to variation, interruptions and disturbances. Everyone in the care process, including staff on the wards as well as staff in the OR and recovery, had to be flexible because changes could affect everyone. Some considered variations challenging, but being able to handle a complex workday was also a positive experience which helped make the work enjoyable and stimulating:
“Or is it that they, like most of us, love their work, so it’s more a positive challenge to, like, hit the volley, I think.” (Surgeon)
Preconditions and resources from the perspective of each profession
Orns’ perspectives, team coordination.
The ORNs described team coordination as a precondition for safe care. Familiarity with the team was described as providing security. When assisting surgeons, interaction and detection of the situation ahead were perceived as important. Cooperating with and supporting less-experienced surgeons were described as a significant part of their responsibility.
“After all, there are constantly new surgeons from different specialties who also need support, to make them feel safe and that they are moving forward, which is actually something I would say that is part of our profession. If we just stand there and wait, are grumpy, and turn our backs, the operating time extends. But when you have the flow, “a dream team” as you say, then it's wonderful.” (ORN)
The preconditions were also described as focused on the closest team members (surgeons and circulating nurse), the patient, and the assignment, as well as interacting and having a common goal.
Having experience
The ORNs saw experience as a resource, crucial for maintaining safe care in the OR. Being aware of one’s limitations and increased experience was said to make it easier to get a sense of the whole surgical work process. Different levels of responsibility were given to the other members of the team based on their experience. The less experience the circulating nurse had, the more responsibility was perceived to be placed on the ORN. Decision making seemed, by the ORNs, dependent on experience by making it easier to make decisions, speak up, and follow the plan. The ORNs said that if issues arose, they could always use their experience to find a solution:
“We solve problems; we see them as a challenge. Problems are there to be solved. Do the best thing possible. We now have the advantage of having so much experience that we don’t get stressed about it — we always have a plan B.” (ORN)
The ORNs also described how they gained experience by discussing and reflecting on a situation retrospectively with the other team members and learning from prior situations and decisions.
RNAs’ perspectives
Maintaining focus.
The RNAs said that there were many disturbances during surgical procedures. Staying focused was perceived important. To stay focused, they did not let themselves be disturbed, by conveying when it was not appropriate to interrupt and continuing with the ongoing task:
“When it comes to induction of anesthesia and the awakening, those are the sensitive phases. We can’t have people running in and out of the OR, giving a lot of information, or asking for a change. That’s when there needs to be a little more focus. Those are the situations when we’re in an extra sensitive phase, I think.” (RNA)
Surgeons’ perspectives
Having respect for the team and shared goals.
Respect and cooperation were considered preconditions for a well-functioning team, and the most essential prerequisite for the work in the OR:
“The team is everything. You go there to help and not to counteract each other. It has to do with respect and cooperation and all that.” (Surgeon)
Surgeons considered familiarity within the team and helping each other as a precondition for a smooth surgical workflow. Having a common goal and focusing on the patient were perceived to create the conditions for getting the job done properly. The surgeons also described a small “team within the team” comprising the operating surgeon, the assisting surgeon, and the ORN. With a well-functioning small team, they perceived themselves to be less disturbed by what was happening around them. It was important to respect the function of the team. Understanding and showing respect for one’s colleagues and recognizing that everyone was as important for the team despite having different tasks were described as prerequisites for safe care.
Having experience and competence
The surgeons described how they were trained from day one to handle interruptions and disturbances, which were perceived as expected and normal. They were prepared for unexpected events to occur and knew that they would have to handle the changing situation. When they were interrupted or disturbed during surgery and then continued with the primary task, it took a while to get used to these changes. However, all these abilities were linked to professional experience and would come with time:
“For that reason, I think the longer you work, the less disturbed you get, or you find some strategy for dealing with it.” (Surgeon)
As well as experience, high competence in the organization was described as an important precondition for safe care . Professional competence and training were important preconditions that had to be ensured by the management.
Maintaining focus and creating space for mental rest
Maintaining focus was considered an important ability, and the surgeons described several strategies to achieve this. When there was a high level of disturbance and noise in the OR, they tried to ignore it by staying calm, resisting, and staying in the “bell jar”. If, in spite of this, they were disturbed to the point of losing focus, they would speak up. For them to lose their focus, the interruption had to be of high urgency:
“It’s easy to say, but you have to brace yourself and stay hyper-focused. You don’t leave that state of extreme focus unless it’s something very important and relevant.” (Surgeon)
In order to maintain focus while still being able to adapt to the unexpected events that can occur during surgery, the surgeons described that they took care of unexpected issues ad hoc along the way. The strategy was to avoid cognitive overload that would consume energy. To maintain focus, they took small mental breaks; experienced surgeons said that they could do this without anyone noticing.
Planning and preparing for the expected and the unexpected per profession
Checking and having control to be prepared.
The ORNs considered preoperative control crucial for safety and security. To be able to plan for the expected, they described several operational checks prior to surgery including functional tests and checking of settings, the amount of gas, and availability of other material and equipment. When applicable, the marked operating area on the patient was checked, and paired organs were double-checked with radiographs and verified with the patient . To maintain awareness of the patient’s condition intraoperatively, the ORNs continuously observed the activity within the anesthesia team, such as looking at monitors, or calling on a colleague for support, as this was an indication of the patient’s status. Much of the preoperative preparation was performed by other ORNs or circulating nurses. For responsible ORNs to be prepared they had to check that the instruments, materials, and supplies were adequate. Counting and checking the sterile instruments and surgical tissues continuously during the procedure was another strategy described by the ORNs. To retain control, the surgeons were not allowed to pick up their own sterile instruments from the medical instrument stand. Being prepared and knowing that everything was in order before the surgeon arrived and being one-step ahead of the intraoperative process was important strategies described by ORNs. When working with new employees, the ORNs were more vigilant and prepared, as they did not know what to expect from the new colleague. However, they recognized the person’s capacity and prepared themselves mentally to provide support when needed:
“Interaction — get a sense of who the person is and give them a chance. But don’t retract those sensitive antennae — extra preparedness.” (ORN)
Taking support from roles and routines
When planning for the expected and unexpected, the ORNs described that they used routines and tools when preparing instruments for the procedure that existed in the OR to support their work.
“We have a lot of tools, routines, index cards, positioning guidelines — everyone has their position and knows what to do.” (ORN)
Adhering to policies and procedures, was important to reduce unnecessary interruptions or disturbances. The ORNs also described the importance of the different responsibilities of the professions in the surgical team. For example, when problems with equipment occurred, they often asked the circulating nurse for assistance as they were more skilled in handling the medical technical equipment.
Creating a basic plan for work
The RNAs described that they checked which OR they were placed in and the team members of the day, and then created a tentative plan of what could happen during the day .
“I might start by checking out the daily OR schedule in paper form, the number of procedures at this moment and what kind of procedures. Which team members, which ORN, which circulating nurse and maybe which anesthesiologist I should contact.” (RNA)
By looking at the OR schedule for the day, they could also anticipate potential changes in the schedule.
Checking and restoring
Another way the RNAs planned for the expected and unexpected was to conduct several pre-surgery operational checks including functional tests and checking settings and intended anesthesia equipment.
“Yes, you go through the trolley with all anesthesia equipment, locate what you need, and bring it out so it’s ready — then you can quickly see.” (RNA)
The RNAs also described how the team preoperatively checked the patient’s skin quality to prevent surgical site infections. When restoring the room after surgery, and to be prepared for acute surgery it was important to check and refill all the supplies that had been used.
Creating and re-evaluating a basic plan for work
The surgeons also said they created a basic plan to be prepared and plan for the expected and unexpected.
“There’s also a basic plan, but you sort of figure out the day as it develops, and no day is like another, which is also nice — variable and revitalizing I think, compared to many boring industrial jobs.” (Surgeon)
The preparation phase started the day before, when the surgeons thought about what could be expected and how they would get things done. On the day of surgery, they checked the OR schedule again as it might have been changed. Making a rigid long-term plan was not feasible, as the plan would be verified and re-evaluated several times during the day. This was perceived as an appropriate strategy when working in an unpredictable context such as the OR.
Using guidelines and routines but with certain degrees of freedom
The surgeons explained that following routines and using guidelines was important for being prepared, creating a good workflow, and reducing unnecessary interruptions and disturbances during surgery. However, sometimes a deviation from routine could be necessary:
“Routines are built from standard flows. Then you also have urgent situations, but they also have routines, right? So you can know what’s coming — at a certain interval this or that will happen and we have routines for it. But in every situation, you also have to be able to improvise. It’s like those Russian ice dancers — the more they practice, the more they can improvise.” (Surgeon)
The main results show that to manage complexity and create safe care in the OR, the professionals shared experiences that certain preconditions and resources were crucial, including having work experience and coordinating and reaffirming information. More specifically, resilience was expressed in the professional’s capacity to prepare, respond and adapt to expected and unexpected situations. By creating a common mental model of the patient, the team established readiness to anticipate, prioritize and solve upcoming problem during the surgical procedure.
The challenges, fragility, and unpredictability of working in a CAS have been described as time- and resource constraints in the OR [ 13 ], and gaps in continuity of care, such as lack of information or communication between professionals in handover situations [ 24 ]. Why most things go right, has been proposed to be pertaining to professionals ability to accomplish their tasks by adaptations and work-arounds [ 6 ]. One common precondition for safe care was expressed by the three groups as coordinating and reaffirming information. A previous observational study, that studied how work was done, found that communication was the most common task involved in multitasking [ 25 ]. The results of the present study show that professionals described communication as an important for achieving a safe and smooth care process and may reflect the challenges that comes with working in a CAS. Speaking up may fuel resilience, from a safety culture perspective [ 26 ] members of a surgical team must have the right speak up about a perceived risk or transfer of patient information [ 27 ]. Communication has been described as comprising important transfer of information between professionals, contributing to a safe, seamless, and efficient care process in the OR. In other situations it may cause interruptions resulting in non-completion of tasks [ 28 ] or gaps in continuity of care [ 29 ] that in turn may have a negative impact on patient safety. Good outcomes have been proposed to be related to the systems adaptive capacity, the individuals, teams’ and the managements’ ability to adapt to unexpected events and changing situations, for example by using interaction and communication [ 30 ]. With a focus on how work was done in a context with variable complexity, an ethnographic study explored communication and relationship dynamics in surgical teams. Proactive and intuitive communication, silent and ordinary communication, inattentive and ambiguous communication and contradictory and high dynamic communication were identified. Different types of team collaboration were connected to the level of complexity of performed surgical procedures [ 31 ]. From the perspective of a CAS, communication is crucial for having the right preconditions to create safe care, adapt to unexpected events and creating effective team interactions and coordination. Teamwork and shared mental models are also considered crucial for patient safety in dynamic domains such as the OR [ 32 , 33 ]. Communication allows a greater understanding of potential risks to develop [ 6 ] within the team, as the different professionals share their mental models [ 32 ] of the situation and ways to anticipate and be prepared to respond to system failures. A flat hierarchy seems more likely to manifest a well-functioning team communication [ 34 ].
The professionals also expressed that clinical expertise [ 30 ], experience and competence, were important individual resources to be able to plan and to meet the unexpected. According to surgeons, experience as well as organizational competence was described as an important precondition for safe care. Experienced colleagues were perceived by ORNs, as being more aware of the other team members’ capacity, competence, and need for support which made it easier to make decisions, speak up, and follow the plan. In line with other studies in the OR [ 19 , 35 , 36 ] the RNAs’ work experience was perceived as important for having the cognitive ability to anticipate risks, planning for the expected and unexpected, and be prepared both mentally and practically for the surgical procedure. Participants in this study had quite high mean experience which may predispose for degrees of freedom to be flexible and adapt to situations and opportunities are easier to be seen. From a theoretical perspective, experience seems a crucial component in handling the unexpected. Resilience does not merely emerge in response to specific disturbances, but develops over time from a continuous training in managing and learning from risks, stresses, and strains [ 37 ]. Mental models play a central role in individual’s behavior and sustained learning based on both one’s own experiences and those of other team members [ 38 ]. Sensemaking, retrospective and prospective learning, that is arriving at a common understanding of a situation in order to adapt to and handle it adequately evolves during communication where professionals share their expertise and knowledge [ 39 ].
When planning and preparing for the expected and unexpected, it was during these processes mental models primarily were created. This was described as collecting relevant information, anticipating potential risks, and talking to the patient. This is in line with sensemaking, a social process [ 30 , 40 ], usually triggered when the team is facing an uncertain situation. It is a retrospective skill with focus on achieving plausibility, dependent on previous situational experience [ 41 ]. The same skills involved in using past experiences to find a pattern in a sensemaking process can also be used to proactively anticipate and prepare for situations that may arise. Prospective sensemaking is described as building the capacity for anticipation, which enables smooth collaboration and preparation for coping with undesired but foreseeable situations related to patient safety. Important interactions with technology in the OR have been described as prospective sensemaking, a sociotechnical process central to capturing the dynamic work in the OR supported by social and technological resources. The surgical team were shown to be constantly aware of emerging risks and were thus prepared for a rapid response [ 36 ]. Anticipating, or knowing what to expect, is also a cornerstone of resilience [ 16 ]. To some extent, planning was described differently by the three professions. The ORNs’ primary focus was on the surgical instruments, while the RNAs anticipated risks and adjusted the plan accordingly; this result is comparable to the findings of other studies of surgical teams in the OR [ 35 , 36 ], and confirms the OR as a CAS [ 7 ]. In our study, the surgeons said that usually they knew the patient, but when this was not the case they planned for the patient’s care by reading the record and created a mental model. Similarly, to our results, planning [ 35 ] coordination, behavior and adaptive coordination strategies [ 19 ] have been previously described as important strategies for surgical teams to manage their tasks. The preoperative plan also showed to serve as a shared mental model for the team [ 19 , 32 ] which allowed new situations to be contrasted and evaluated. In general, shared mental models have been described related to positive outcomes by creating effective teamwork [ 33 ] and minimizing preventable uncertain processes and performance [ 42 , 43 ] in ad-hoc constellations of teams [ 42 ]. On an individual level, mental models can also limit professionals by using familiar ways of thinking and acting. Professionals are usually not aware of these models or potential effects on their behavior [ 44 ]. When working in a CAS it can be difficult to get a sense of the whole solely from detailed descriptions such as guidelines. Sensemaking and mental models seems to have the ability to enhance planning for the expected and unexpected. However, in a dynamic CAS such as the OR, mental models need to be shared and discussed within the team [ 19 , 42 ] to avoid misunderstandings.
To be able to adapt to the unexpected, the three professional groups were unanimous in stating that prioritizing and solving upcoming problems was necessary in order to handle the unexpected. From a theoretical perspective when an unexpected event occurs, first it must be noticed, then the surgical team has to make sense of it, and then they have to do something about it [ 45 ]. To be able to adapt to unexpected events, the ORNs and RNAs described that they used previously created plans B and C, which were a part of the mental model when planning and preparing for the procedure. These results are similar to the findings of other studies in the OR context [ 19 , 35 , 36 ]. Having several plans appears to be a common key strategy to handle unexpected events in a CAS. However, the present study also shows the necessity of the planning phase being done carefully, as this appears to be a pre-requisite for a reflexive and quick response when unexpected events occur. From the perspective of resilience, adaptation is a central key factor that is not always about changing the plan, model, or previous approaches, but sometimes involves the readiness to modify plans to suit changing situations. Woods [ 46 ], describes this ability as being able to recognize and to stretch, extend, or change what is being done or had been planned to be done. In our study, prioritizing and solving upcoming issues was a crucial strategy as the problem had to be solved; inaction was not an option. The same strategies were also expressed in other OR studies; in order to respond to unexpected events, adaptability [ 33 ] and adaptive coordination were identified as important for safe performance, and were usually achieved through communication [ 19 , 31 , 32 ].
Patient safety and risk arise through variability and the managements’ ability to provide resources and pre-conditions with different degrees of freedom on which the adaptations from the surgical team are based. However, there is a need for reflection on the extent of the ability to adapt and the degrees of freedom needed in the adaptation. Resilience is often expressed as the extensibility of the system, which may result in pushing the limits for taking risks too far; this is intimately linked to exposure to risk. However, the risk of high adaptive capacity is that adaptations become normalized and signals of organizational weaknesses are masked by individual’s ability to adapt and therefore, despite system deficiencies, more difficult to be perceived by decision makers [ 47 ], balanced considerations must be considered.
Methodological considerations
One strength of this study is the inclusion of three OR core professional groups with varied gender, age, and experience. However, the mean age and experience were both quite high, probably due to that the included OR department had quite low turnover rates among staff. This can be considered as both a strength and a limitation. On one hand, individuals with a lot of experience may contribute with more rich descriptions than those with less experience. On the other hand, perceptions from less experienced could have contributed with more variations in the phenomena of study. Transferability of qualitative results is difficult, as these results are highly dependent on the studied context. To ensure trustworthiness [ 48 ] in terms of confirmability, we have presented a selection of transcripts, codes, sub-categories, and generic categories in Table 2 . To increase the credibility, interactive discussions of codes, sub-categories and generic categories took place among the authors, and quotations are presented in connection to the descriptions. Further, triangulation of sources was made of similar descriptions of the same phenomenon by the three professionals, and analyst triangulation was achieved by the research group through independent categorization. To ensure dependability, open questions were asked using an interview guide during all group interviews. The aim for choosing group interviews, instead of individual interviews was to obtain each professional group’s perceptions and experiences by dynamic group interactions. Since the OR is an unpredictable context, there was uncertainty in how many participants that could attend the planned time and day for the group interviews. The interviews were conducted at two central OR departments at one county hospital and one local county hospital in mid-Sweden by reasons as practical feasibility to obtain access to professional groups. The interviewer was an RNA, which may have affected the interpretation of the results both positively, by making it easier to interpret context-specific nuances, and negatively, by taking things for granted. As described previously, surgical teams in Sweden usually consist of six different professionals. The focus in this study was on the core professionals of the OR, including ORNs, RNAs, and surgeons. This may be considered a limitation, as not all professionals were represented.
Creating safe care in the OR should be understood as a process of anticipating, planning, and preparing in order to manage challenging and complex work processes. OR staff need preconditions and resources such as having experience and coordinating and reaffirming information, to make sense of different situations. This requires a mental model, which is created through planning and preparing in different ways. Some situations are repetitive and easier to plan for but planning for the unexpected requires anticipation from experience and coordination among team members. The main results strengthen that the four abilities in the theory of resilience is used by OR staff as a strategy to manage complexity in the OR. Managing complexity seems dependent on clinical experience. Therefore, future research should focus on how to provide effective learning of effective strategies for safe practice in a complex health care environment for less experienced colleagues.
Clinical implications
Managing complexity in the OR, being able to respond to the expected and unexpected, requires adaptive capacities such as anticipating and monitoring. Before a procedure starts surgical teams should use safety briefings to discuss potential challenges and risks and solve problems. To promote learning and to have the same goals, mental models should be shared and discussed between team members. After the surgical procedure, debriefings about what and why things went right or wrong and what could be improved may support reflective learning [ 34 ].
Availability of data and materials
Data are available on request for any interested researchers to allow replication of results provided all ethical and legal requirements are met according to GDPR, The General Data Protection Regulation for the European Union. Contact person, Center for Clinical Research, Dalarna, Uppsala University ( [email protected] ), Nissers väg 3, SE-79182 Falun, Sweden.
Abbreviations
Complex adaptive system
- Operating room
Operating room nurses
Registered nurse anesthetists
Resilience engineering
Potter P, Wolf L, Boxerman S, Grayson D, Sledge J, Dunagan C, Evanoff B. Understanding the cognitive work of nursing in the acute care environment. J Nurs Adm. 2005;35(7–8):327–35.
PubMed Google Scholar
Skaugset LM, Farrell S, Carney M, Wolff M, Santen SA, Perry M, Cico SJ. Can you multitask? Evidence and limitations of task switching and multitasking in emergency medicine. Ann Emerg Med. 2016;68(2):189–95.
Article PubMed Google Scholar
Pittet V, Perret C, Moret V, Despond O, Burnand B. Evolution of anaesthesia care and related events between 1996 and 2010 in Switzerland. Acta Anaesthesiol Scand. 2013;57(10):1275–86.
Article CAS PubMed Google Scholar
Cima RR, Brown MJ, Hebl JR, Moore R, Rogers JC, Kollengode A, Amstutz GJ, Weisbrod CA, Narr BJ, Deschamps C. Use of lean and six sigma methodology to improve operating room efficiency in a high-volume tertiary-care academic medical center. J Am Coll Surg. 2011;213(1):83–92 discussion 93-84.
Weinger MB, Gaba DM. Human factors engineering in patient safety. Anesthesiology. 2014;120(4):801–6.
Braithwaite J, Churruca K, Ellis LA, Long J, Clay-Williams R, Damen R, et al. Complexity science in healthcare - aspirations , approaches, applications and accomplishments: a white paper. 2017.
Tsai MH, Sanford JA, Black IH, Boggs SD, Urman RD. Operating room management at the edge of order and chaos. J Med Pract Manag. 2017;32(4):250–5.
Google Scholar
Guédon ACP, Spruit SL, Wauben LSGL, van der Elst M, Doorn N, Dankelman J, van den Dobbelsteen J, Klein J. Delicate balance: adaptive support to improve patient safety. BMJ Innov. 2017;3(1):1–6.
Article Google Scholar
Hollnagel E Prologue: the scope of resilience engineering. In Resilience engineering in practice: a guidebook. Hollnagel E, Dédale, J.P., Woods, D., Wreathall, J. Farnham: Ashgate; 2011.
Weiser TG, Haynes AB. Ten years of the surgical safety checklist. Br J Surg. 2018;105(8):927–9.
Article CAS PubMed PubMed Central Google Scholar
Woods D, Dekker S, Cook R, Johannesen L, Sarter N. Behind human error. Farnham: Ashgate; 2010.
Hollnagel E, Wears RL, Braithwaite J. From Safety-I to Safety-II: a white paper. The resilient health care net: published simultaneously by the University of Southern Denmark, University of Florida, USA, and Macquarie University, Australia; 2015.
Dixon-Woods M. Why is patient safety so hard? A selective review of ethnographic studies. J Health Serv Res Policy. 2010;15(Suppl 1):11–6.
Nemeth C, Wears RL, Patel S, Rosen G, Cook R. Resilience is not control: healthcare, crisis management, and ICT. Cogn Tech Work. 2011;13(3):189–202.
Bueno WP, Saurin TA, Wachs P, Kuchenbecker R, Braithwaite J. Coping with complexity in intensive care units: a systematic literature review of improvement interventions. Saf Sci. 2019;118:814–25.
Hollnagel E. Resilience engineering in practice : a guidebook. Farnham: Ashgate; 2010.
Wiig S, Fahlbruch B. Exploring resilience: a scientific journey from practice to theory. Heidelberg: Springer; 2018.
Ross AJ, Anderson JE, Kodate N, Thompson K, Cox A, Malik R. Inpatient diabetes care: complexity, resilience and quality of care. Cogn Tech Work. 2014;16(1):91–102.
Bogdanovic J, Perry J, Guggenheim M, Manser T. Adaptive coordination in surgical teams: an interview study. BMC Health Serv Res. 2015;15:128.
Article PubMed PubMed Central Google Scholar
Manser T, Harrison TK, Gaba DM, Howard SK. Coordination patterns related to high clinical performance in a simulated anesthetic crisis. Anesth Analg. 2009;108(5):1606–15.
McQuaid-Hanson E, Pian-Smith MC. Huddles and debriefings: improving communication on labor and delivery. Anesthesiol Clin. 2017;35(1):59–67.
Meeusen V, van Zundert A, Hoekman J, Kumar C, Rawal N, Knape H. Composition of the anaesthesia team: a European survey. Eur J Anaesthesiol (EJA). 2010;27(9):773–9.
Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–15.
Ekstedt M, Ödegård S. Exploring gaps in cancer care using a systems safety perspective. Cogn Tech Work. 2015;17(1):5–13.
Goras C, Olin K, Unbeck M, Pukk-Harenstam K, Ehrenberg A, Tessma MK, Nilsson U, Ekstedt M. Tasks, multitasking and interruptions among the surgical team in an operating room: a prospective observational study. BMJ Open. 2019;9(5):e026410.
Sammer CE, Lykens K, Singh KP, Mains DA, Lackan NA. What is patient safety culture? A review of the literature. J Nurs Scholarsh. 2010;42(2):156–65.
Berg LM, Kallberg AS, Ehrenberg A, Florin J, Ostergren J, Djarv T, Brixey JJ, Goransson KE. Factors influencing clinicians’ perceptions of interruptions as disturbing or non-disturbing: a qualitative study. Int Emerg Nurs. 2016;27:11–6.
Westbrook JI, Coiera E, Dunsmuir WT, Brown BM, Kelk N, Paoloni R, Tran C. The impact of interruptions on clinical task completion. Qual Saf Health Care. 2010;19(4):284–9.
Cook RI, Render M, Woods DD. Gaps in the continuity of care and progress on patient safety. BMJ (Clin Res ed). 2000;320(7237):791–4.
Article CAS Google Scholar
Wears RL, Hollnagel E, Braithwaite J. Resilient health care volume 2 the resilience of everyday clinical work. Farnham: Ashgate; 2015.
Torring B, Gittell JH, Laursen M, Rasmussen BS, Sorensen EE. Communication and relationship dynamics in surgical teams in the operating room: an ethnographic study. BMC Health Serv Res. 2019;19(1):528.
Manser T. Teamwork and patient safety in dynamic domains of healthcare: a review of the literature. Acta Anaesthesiol Scand. 2009;53(2):143–51.
Salas E, Sims DE, Burke CS. Is there a “big five” in teamwork? Small Group Res. 2005;36(5):555–99.
Nilsson U, Gruen R, Myles PS. Postoperative recovery: the importance of the team. Anaesthesia. 2020;75(S1):e158–64.
Høyland S, Aase K, Hollund JG. Exploring varieties of knowledge in safe work practices-an ethnographic study of surgical teams. Patient Saf Surg. 2011;5(1):21.
Rosness R, Evjemo TE, Haavik T, Wærø I. Prospective sensemaking in the operating theatre. Cogn Tech Work. 2016;18(1):53–69.
Weick KE, Sutcliffe KM. Managing the unexpected: sustained performance in a complex world. Hoboken: John Wiley & Sons, Inc.; 2015.
Book Google Scholar
Senge PM. The fifth discipline: the art and practice of the learning organization. London: Random House Business; 2006.
Battles JB, Dixon NM, Borotkanics RJ, Rabin-Fastmen B, Kaplan HS. Sensemaking of patient safety risks and hazards. Health Serv Res . 2006;41(4p2):1555–75.
Weick KE, Sutcliffe KM, Obstfeld D. Organizing and the process of sensemaking. Organ Sci. 2005;16(4):409–21.
Weick KE. Sensemaking in organizations. Thousand Oaks: Sage; 1995.
Burtscher MJ, Manser T. Team mental models and their potential to improve teamwork and safety: a review and implications for future research in healthcare. Saf Sci. 2012;50(5):1344–54.
Mathieu JE, Heffner TS, Goodwin GF, Salas E, Cannon-Bowers JA. The influence of shared mental models on team process and performance. J Appl Psychol. 2000;85(2):273.
Senge PM. The fifth discipline: the art and practice of the learning organization. New York: Doubleday/Currency; 1990.
Weick K. The reduction of medical errors through mindful interdependence: what do we know, what do we do. San Francisco: Jossey-Bass; 2002.
Woods D. Resilience is a verb. In: Trump BD, Florin M-V, Linkov I, editors. IRGC resource guide on resilience (vol 2): domains of resilience for complex interconnected systems. Lausanne: EPFL International Risk Governance Center; 2018.
Ekstedt M, Flink M. Hemsjukvård : olika perspektiv på trygg och säker vård. Liber: Stockholm; 2019.
Lincoln YS, Guba EG. Naturalistic inquiry. Beverly Hills: Sage; 1985.
Download references
Acknowledgements
We also thank the heads of the participating departments and the surgical teams for their willingness to participate in this study.
The Center for Clinical Research Dalarna and the Department of Anesthesia and Intensive Care Unit Falu Lasarett supported this work but was not involved in the design and running of the study. Open access funding provided by Dalarna University.
Author information
Authors and affiliations.
School of Education, Health and Social Studies, Dalarna University, Falun, Sweden
Camilla Göras & Anna Ehrenberg
Department of Anesthesia and Intensive Care Unit, Falu Hospital, Falun, Sweden
Camilla Göras
Center for Clinical Research, Falun, Dalarna, Sweden
Department of Neurobiology, Care Sciences and Society, Karolinska Institutet, Stockholm, Sweden
Ulrica Nilsson & Maria Unbeck
Perioperative Medicine and Intensive Care, Karolinska University Hospital, Stockholm, Sweden
Ulrica Nilsson
Department of Health and Caring Sciences, Linnaeus University, Kalmar/Växjö, Sweden
Mirjam Ekstedt
Department of Learning, Informatics, Management and Ethics, Karolinska Institutet, Stockholm, Sweden
Acute and Reparative Medicine Theme, Karolinska University Hospital, Stockholm, Sweden
Maria Unbeck
You can also search for this author in PubMed Google Scholar
Contributions
CG, UN, ME, MU and AE contributed to the study design. CG was the project supervisor and performed the group interviews together with AE. CG also undertook the initial interpretation of the data, which was followed by discussions with UN, ME, MU and AE. Drafts of the manuscript were reviewed by UN, ME, MU and AE. All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Camilla Göras .
Ethics declarations
Ethics approval and consent to participate.
This study was conducted according to International research ethics and standards following the Declaration of Helsinki and was approved by the Swedish Ethical Review Authority in Uppsala, Sweden (No. 2016/264). To get permission to conduct the study, information was provided both verbally and in writing to the medical director of the surgical department and nurse managers at the OR department. Those who volunteered gave their written informed consent after receiving verbal and written information from one researcher (CG) including the voluntary nature of participation and the ability to withdraw at any time without further explanation, and confidential treatment of data. The manuscript had followed the reporting criteria for qualitative research according to the COREQ checklist.
Consent for publication
Consent for publication has been obtained from participants.
Competing interests
The authors report no conflict of interest. The authors alone are responsible for the content and the writing of this manuscript.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Göras, C., Nilsson, U., Ekstedt, M. et al. Managing complexity in the operating room: a group interview study. BMC Health Serv Res 20 , 440 (2020). https://doi.org/10.1186/s12913-020-05192-8
Download citation
Received : 29 January 2020
Accepted : 06 April 2020
Published : 19 May 2020
DOI : https://doi.org/10.1186/s12913-020-05192-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Group interviews
- Patient safety and work processes
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Open access
- Published: 07 January 2022
Operating room efficiency in a low resource setting: a pilot study from a large tertiary referral center in Ethiopia
- Samuel Negash ORCID: orcid.org/0000-0001-7660-6912 1 ,
- Endale Anberber 1 ,
- Blen Ayele 2 ,
- Zeweter Ashebir 2 ,
- Ananya Abate 2 ,
- Senait Bitew 3 ,
- Miliard Derbew 1 , 3 ,
- Thomas G. Weiser 3 , 4 , 5 ,
- Nichole Starr 3 , 6 &
- Tihitena Negussie Mammo 1 , 3
Patient Safety in Surgery volume 16 , Article number: 3 ( 2022 ) Cite this article
7930 Accesses
7 Citations
5 Altmetric
Metrics details
The operating room (OR) is one of the most expensive areas of a hospital, requiring large capital and recurring investments, and necessitating efficient throughput to reduce costs per patient encounter. On top of increasing costs, inefficient utilization of operating rooms results in prolonged waiting lists, high rate of cancellation, frustration of OR personnel as well as increased anxiety that negatively impacts the health of patients. This problem is magnified in developing countries, where there is a high unmet surgical need. However, no system currently exists to assess operating room utilization in Ethiopia.
Methodology
A prospective study was conducted over a period of 3 months (May 1 to July 31, 2019) in a tertiary hospital. Surgical case start time, end time, room turnover time, cancellations and reason for cancellation were observed to evaluate the efficiency of eight operating rooms.
A total of 933 elective procedures were observed during the study period. Of these, 246 were cancelled, yielding a cancellation rate of 35.8%. The most common reasons for cancellation were related to lack of OR time and patient preparation (8.7% and 7.7% respectively). Shortage of facilities (instrument, blood, ICU bed) were causes of cancelation in 7.7%. Start time was delayed in 93.4% (mean 8:56 am ± 52 min) of cases. Last case completion time was early in 47.9% and delayed in 20.6% (mean 2:54 pm ± 156 min). Turnover time was prolonged in 34.5% (mean 25 min ± 49 min). Total operating room utilization ranged from 10.5% to 174%. Operating rooms were underutilized in 42.7% while overutilization was found in 14.6%.
We found a high cancellation rate, most attributable to late start times leading to delays for the remainder of cases, and lack of preoperative patient preparation. In a setting with a high unmet burden of surgical disease, OR efficiency must be maximized with improved patient evaluation workflows, adequate OR staffing and commitment to punctual start times. We recommend future quality improvement projects focusing on these areas to increase OR efficiency.
Operating rooms (ORs) are some of the most important areas of hospitals that have significant impact on the overall picture of a hospital’s performance [ 1 , 2 ]. Running an operating room is capital and labor intensive [ 1 , 2 , 3 , 4 ]. When OR utilization is inefficient, it leads to wastage of time and human resources, higher costs and fewer patients treated than planned. This constellation of issues results in financial losses as well as decreased patient satisfaction [ 5 ].
Furthermore, recent publications regarding global surgery have highlighted the high unmet need for safe surgery in developing countries. Lack of personnel and facility are contributors to this problem [ 6 , 7 ]. However, it is also our observation that many existing operating rooms in our country are underutilized. In this case, increasing efficiency can reduce patient wait times without incurring additional cost [ 8 ].
Thus far, there is scant literature assessing OR efficiency in different areas of Ethiopia [ 8 , 9 , 10 , 11 ]. Additionally, all of the studies assessed focused solely on the cancellation rate. Looking into this parameter alone may lead to wrong conclusion and lack of improved outcome after intervention. Other factors affecting performance such as late starts, early finishes, long time between cases and mismatch of scheduled sessions with existing capacity were not considered but have a potentially large impact on the OR efficiency.
The aim of this study was to evaluate all five indicators of OR utilization: start time, finish time turnover time and total daily utilization, together with cancellation rate. This evaluation aimed to provide a comprehensive assessment of the overall OR efficiency and inform the subsequent planning of interventions. In addition, we hope to encourage the culture of continuous monitoring of efficiency in operatinng rooms across Ethiopia.
This study was undertaken at Tikur Anbessa Specialized Hospital (TASH), in Addis Ababa, Ethiopia. TASH is the main teaching hospital of the country and provides many specialized clinical services that are not available in other public or private institutions. TASH is also the largest hospital in the country with a capacity of more than 700 beds. It has 12 operating rooms which is more than any other hospital in the country.
The design was a descriptive observational study. Data was collected from eight operating rooms over a period of three months (May 1 – July 31, 2019). Surgical specialties utilizing these operating rooms included otolaryngology, urology, cardiothoracic surgery, neurosurgery, pediatric surgery, general surgery and obstetrics/gynecology. Emergency operating rooms were excluded because they function without a schedule.
Based on existing literature [ 12 , 13 ] and considering standard working hours to be 8 h per day starting at 8:00 am; we set standards the five indicators in our hospital (Table 1 ).
A data collection tool was designed by the investigators and pretested with a subset of cases for ease of administration and clarity of terminology. Data were collected by trained operating room nurses. Data cleaning and analysis was done using SPSS version 23. Chi-squared tests were used to report outcomes and two-sided significance level was set to be 0.05 (5%). Ethical clearance was obtained from the research committee at the Department of Surgery, Addis Ababa University College of Health Sciences.
A total of 687 operations were performed during the study period. Most of the time, two procedures were performed in a room per day (39.6%), followed by a single procedure per day (36.5%). Additional procedures were sometimes performed with three procedures per day in 16.4% and 4 procedures per day in 7.4% of operating rooms.
Total number of scheduled elective cases were 933 of which 246 were cancelled, yielding a cancellation rate of 35.8%. The most common cause of cancellation was lack of OR time (workday ending before scheduled cases are finished). This was followed by issues related to perioperative patient preparation. Others were institutional factors, of which the lack of an ICU bed was the most common (Table 2 ).
The start time ranged from 7:45 am to 9:30 am. Mean start time was 8:56 am ± 52 min. The start time was delayed past 8:15am in 93.4% of the cases. In addition, the time of start for the first surgery (incision time) ranged from 8:00 am to 10:18 am with mean 9:41 am ± 60 min.
Turnover time ranged from 3 min to 2 h. Mean was 25 min ± 49 min. Turnover time was prolonged in 34.5%. The finish time ranged from 8:45 am to 11:12 pm. Mean finish time was 2:54 pm ± 156 min. The end time was early in 47.9% and delayed in 27.8%.
Mean number of surgeries per day was 1.9 ± 0.9. Mean time spent on surgery per day was 4 h ± 140 min. Remaining time was occupied by anesthesia preparation and intubation (1 h and 23 min ± 132 min), extubating and transfer of patients (42 min ± 34 min), turnovers (40 min ± 38 min). Total operating room utilization ranged from 10.5% to 174%. It was underutilized (< 6 h) in 42.7% of the cases while overutilization (> 8 h) was found in 14.6% (Table 3 ).
An efficient operating room should start early, finish on time, allocate minimal time for preparation between procedures and have a low rate of cancellation. Poor utilization of the operating room leads to wastage and drains resources which is very valuable in low income countries with a high unmet need for surgery [ 14 , 15 ]. Additionally, it results in patient dissatisfaction and staff demoralization [ 14 , 16 ].
In our study, the cancellation rate was 35.8% which is similar to the previous study on elective surgery cancellation in the same hospital (33.9%) [ 10 ]. Studies done in other major teaching hospitals in Ethiopia also had similar findings with the cancelation rate at Gondar University Hospital 33.1% [ 11 ] Hawassa Gondar University Hospital 31.6% [ 9 ], and Jimma University Hospital 23% [ 8 ]. The reasons for cancellation were also similarly related to shortage of time (over scheduling) and inadequate patient preparation. This is in contradiction to the belief that higher rate of cancellation in low income countries is unavoidable (due to resource constraints) [ 17 ].
We found turnover time was 25 min ± 49 min with delay in 34.5%. This is an acceptable figure considering the best performing operating rooms report a turnover time less than 25 min [ 13 ]. Furthermore, we have found the number of procedures done per OR each day is low (76% perform either 1 or 2 procedures per OR per day). Therefore, attempting to decrease turnover time would likely not have significant impact in this setting.
The start time was delayed in 93.4% of the cases. This may be the most important parameter as it decides the day’s surgical activity [ 18 ]. Downstream effect of the late starts can also be the cause for frequent cancellations observed in our study due to lack of OR time. Many institutions have used different strategies to improve starting time [ 18 , 19 , 20 ]. To implement these in our setting we need further data evaluating the reasons for delay of the first case. In addition, we found frequent delays between patient entering operating room and start of surgery (43 min ± 40 min). This needs further evaluation of anesthesia induction and surgical preparation practice.
Assessment of the total OR utilization found a wide range with a majority (57.3%) either underutilized or overutilized. The finish time was very early or late in 75.7%. Early finish times can be improved by decreasing the cancellation rate, especially those related to patient preparation. Overutilization and late finish times also need to be corrected as it leads to staff burnout and overtime costs [ 21 ]. Having a late start time can again be an important factor cascading to delay in the finish time.
Overall, this study found our operating rooms are inefficient, with high cancelation rates that can be attributed to delayed start times, short working days and inadequate patient preparation. This is in contrary to the belief that inefficiency in operating rooms of low-income countries is related to lack of infrastructure. While the physical space may not be a limiting factor, human resources to adequately staff ORs and meet overtime needs, and culture change around earlier start times may ameliorate some of these challenges. In a setting such as Ethiopia where there is a large unmet burden of surgical disease, future interventions to improve the function of our operating rooms should be focused on these two areas.
Availability of data and materials
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- Operating room
Tikur Anbessa Specialized Hospital
Al-Saffar A. Enhancing Operating Theatre Efficiency of Private Hospital in Kuwait; Business Management Approach [Masters dissertation]. Dublin R Coll Surg Irel. 2011;186.
Scotland AC for. Full House- Theatre Utilisation in Scottish Hospitals. 1999.
Google Scholar
Cymru A. Operating Theatres: A Summary of Local Audit Findings | Audit Wales. 2016. ([cited 2021 Oct 4]; Available from: https://www.audit.wales/publication/operating-theatres-summary-local-audit-findings-0 ).
Cardoen B, Demeulemeester E, Beliën J. Operating room planning and scheduling: A literature review. Eur J Oper Res. 2010;201(3):921–32.
Article Google Scholar
Street W. Operation theater efficiency. Off Audit Gen West Aust. 2015;58.
Derbew M. Pediatric surgery in Eastern Africa: The unmet need. J Pediatr Surg. 2019;54(1):21–6.
Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. The Lancet Commissons. 2015 [cited 2021 Oct 4]; Available from: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(15)60160-X/fulltext?dgcid=recommender_referral_trendmd
Haile M, Desalegn N. Prospective study of proportions and causes of cancellation of surgical operations at Jimma University Teaching Hospital, Ethiopia. Int J Anesth Res. 2015;3(2):87–90.
Desta M, Manaye A, Tefera A, Worku A, Wale A, Mebrat A, et al. Incidence and causes of cancellations of elective operation on the intended day of surgery at a tertiary referral academic medical center in Ethiopia. Patient Saf Surg. 2018;12(1):1–6.
Ayele A, Weldeyohannes M, Tekalegn Y. Magnitude and reasons of surgical case cancellation at a specialized Hospital in Ethiopia. J Anesth Clin Res. 2019;10(927):2.
Nigatu YA, Aytolign HA. Cause and incidence of Cancellation of elective surgeries at Gondar University hospital, Ethiopia. 2020.
Book Google Scholar
Fixler T, Wright JG. Identification and use of operating room efficiency indicators: the problem of definition. Can J Surg. 2013;56(4):224–6.
Nuhu SI, Embu HY, Atteh FD, Kokong D, Aliyu HA. Theatre start and turnover times in a developing country. Highl Med Res J. 2020;20(1):51–5.
Schuster M, Neumann C, Neumann K, Braun J, Geldner G, Martin J, et al. The Effect of Hospital Size and Surgical Service on Case Cancellation in Elective Surgery: Results from a Prospective Multicenter Study. Anesth Analg. 2011;113(3):578–85.
Stavrou G, Panidis S, Tsouskas J, Tsaousi G, Kotzampassi K. An audit of operating room time utilization in a teaching hospital: is there a place for improvement? Int Sch Res Not. 2014;2014:431740.
Heslin MJ, Doster BE, Daily SL, Waldrum MR, Boudreaux AM, Smith AB, et al. Durable Improvements in Efficiency, Safety, and Satisfaction in the Operating Room. J Am Coll Surg. 2008;206(5):1083–9.
Prin M, Eaton J, Mtalimanja O, Charles A. High Elective Surgery Cancellation Rate in Malawi Primarily Due to Infrastructural Limitations. World J Surg. 2018;42(6):1597–602.
Pashankar DS, Zhao AM, Bathrick R, Taylor C, Boules H, Cowles RA, et al. A Quality Improvement Project to Improve First Case On-time Starts in the Pediatric Operating Room. Pediatr Qual Saf. 2020;5(4):e305.
Shippert RD. A Study of Time-Dependent Operating Room Fees and How to save $100 000 by Using Time-Saving Products. Am J Cosmet Surg. 2005;22(1):25–34.
Wright JG, Roche A, Khoury AE. Improving on-time surgical starts in an operating room. Can J Surg. 2010;53(3):167–70.
PubMed PubMed Central Google Scholar
Overutilization and underutilization of operating rooms - insights from behavioral health care operations management. Health Care Manag Sci. 2017;20:115–28.
Download references
Acknowledgements
We would like to express our gratitude to all staff working in the operating room at TASH.
This study did not receive funding.
Author information
Authors and affiliations.
Department of Surgery, Addis Ababa University, Addis Ababa, Ethiopia
Samuel Negash, Endale Anberber, Miliard Derbew & Tihitena Negussie Mammo
Department of Anesthesia, Addis Ababa University, Addis Ababa, Ethiopia
Blen Ayele, Zeweter Ashebir & Ananya Abate
Lifebox Foundation, London, UK
Senait Bitew, Miliard Derbew, Thomas G. Weiser, Nichole Starr & Tihitena Negussie Mammo
Department of Surgery, University of Edinburgh, Edinburgh, UK
Thomas G. Weiser
Department of Surgery, Stanford University, Stanford, USA
Department of Surgery, University of California San Francisco, San Francisco, USA
Nichole Starr
You can also search for this author in PubMed Google Scholar
Contributions
EA designed the methodology and coded data. SN performed data analysis and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Samuel Negash .
Ethics declarations
Ethics approval and consent to participate.
Ethical clearance was obtained from the research committee at the Department of Surgery, Addis Ababa University College of Health Sciences.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Negash, S., Anberber, E., Ayele, B. et al. Operating room efficiency in a low resource setting: a pilot study from a large tertiary referral center in Ethiopia. Patient Saf Surg 16 , 3 (2022). https://doi.org/10.1186/s13037-021-00314-5
Download citation
Received : 24 October 2021
Accepted : 13 December 2021
Published : 07 January 2022
DOI : https://doi.org/10.1186/s13037-021-00314-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Utilization
- Cancellation rate
- Turnover time
- Start time delay
Patient Safety in Surgery
ISSN: 1754-9493
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Perioperative Nursing Unfolding Case Study: Bringing the Operating Room Experience to the Classroom
Affiliation.
- 1 Author Affiliation: Professor of Nursing and Director, The College of New Jersey Quality and Safety Innovation Center, The College of New Jersey, Ewing.
- PMID: 32349006
- DOI: 10.1097/NNE.0000000000000844
PubMed Disclaimer
Similar articles
- Academic-Practice Partnerships to Reduce the Shortage of Operating Room Nurses. Plank L. Plank L. Nurse Educ. 2018 Nov/Dec;43(6):326-329. doi: 10.1097/NNE.0000000000000496. Nurse Educ. 2018. PMID: 30339135
- Implementing a baccalaureate perioperative nursing elective. Long MC, George SE, Gulledge HS. Long MC, et al. AORN J. 1995 Feb;61(2):372-6. doi: 10.1016/s0001-2092(06)63889-1. AORN J. 1995. PMID: 7717700
- Future perioperative registered nurses: an insight into a perioperative programme for undergraduate nursing students. Clark-Burg K. Clark-Burg K. J Perioper Pract. 2008 Oct;18(10):432-5. doi: 10.1177/175045890801801001. J Perioper Pract. 2008. PMID: 18983065
- Global interprofessional perioperative education: discussing the reality. Ward PR. Ward PR. Can Oper Room Nurs J. 2008 Sep;26(3):7-8, 10-1, 13 passim. Can Oper Room Nurs J. 2008. PMID: 18980067 Review.
- Perioperative nursing education "down under". Hilbig JI. Hilbig JI. Semin Perioper Nurs. 1996 Oct;5(4):189-94. Semin Perioper Nurs. 1996. PMID: 9025591 Review.
- Glendon K, Ulrich DL. Unfolding cases: an experiential learning model. Nurse Educ. 1997;22(4):15–18.
- Day L. Using unfolding cases in a subject-centered classroom. J Nurs Educ. 2011;50(8):447–452.
- O'Rourke J, Zerwic J. Measure of clinical decision-making abilities of nurse practitioner students. J Nurs Educ. 2016;55(1):18–23.
- Shellenbarger T, Robb M. Technology-based strategies for promoting clinical reasoning skills in nursing education. Nurse Educ. 2015;40(2):79–82.
- Altmiller G. Perioperative nursing: an unfolding case study. Quality and Safety Education for Nurses. 2020. Available at https://qsen.org/perioperative-unfolding-case-study/ .
- Search in MeSH
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- Wolters Kluwer

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Case Study #5: Motor Vehicle Collision (MVC)
Operating Room
Time: 03h30 (5 hours post mvc), place: operating room: charge nurse’s desk.
“Dr. Labinski! On-call again, I see.”
“Yes, Ruth, and I see you are in charge again. I have a patient downstairs with a lacerated spleen. Aaron Knoll. I have classified him as a 1A. Needs to be done soon. Is that possible? ”
“Yeah, we should be finished with the C-section in OR 4,” says Ruth. “I ’ ll ask Lydia to set up a major abdominal set for you. Is there anything special you need?”
“No, that should be good. Let Dr. Lai, the anesthetist, know that he may need the rapid infuser and should have four units up, as I expect a lot of bleeding,” instructs Dr. Labinski. “And make sure there are a lot of suction containers available. Is there an assist around to help me out? I ’ m concerned that this could go sideways quickly.”
“Dr. Bondie is available. She ’ s watching the C-section right now.”
“Excellent. Which OR? ”
“We ’ ll set up OR 7 for you. It ’ ll be ready in about 30 minutes.”
Time: 04h00 (5.5 hours post MVC)
Ruth looks up to see Dr. Bondie and Lydia bringing a patient through the doors.
“Is this Aaron Knoll?” asks Ruth.
“Yes, it is. I have checked the pre-op checklist and checked him against his consent. His mother identified him as well,” confirms Lydia. “So, right patient.”
“Ok, you ’ re already set up. Bassam is scrubbed in and ready. I ’ ll follow you down and help you position.”
“Thanks, Ruth,” says the doctor.
Positioning their masks correctly, both Dr. Bondie and Lydia enter OR 7 to see that Bassam has most of the back table set up and is standing in his sterile gown at the far end of the back table. Dr. Lai is relaxing on his stool by the anaesthetic machine.
“Hey, guys, this is Aaron Knoll. He ’ s still a bit unconscious, most likely from a concussion post-MVC. Let ’ s get him positioned and draped.”
Ruth, Dr. Lai, and Lydia slide Aaron from the stretcher onto the OR table. Dr. Bondie checks the patient’s identity again and assists with positioning him at a 45 degree tilt to the right, with his left arm stretched over his head and supported by the arm board attachment from the OR table.
Dr. Bondie steps back. “That looks good, but before we go ahead and prep and drape, let ’ s check with Dr. Labinski.”
Dr. Lai nods. “Sure. I ’ m going to go ahead and start putting him to sleep and getting myself ready here. Should be about 15 minutes at the most.”
A few minutes later, Dr. Bondie and Dr. Labinski re-enter the OR and assist with prepping and draping the patient.
Dr Lai looks over top of the drape separating him from the operative field. “I’m ready and the patient is fully under.”
“Thanks. Ok, everyone let ’ s just pause before we begin and double check we have everything, and we all know what’s going to happen.”
Ruth and Lydia gather a bit closer but stay a meter away from the surgical field. Bassam, who is scrubbed, and Dr. Bondie lean in close. Dr. Lai adjusts his stool so his head is above the separation drape.
“Ok, let ’ s confirm a couple of things. This is Aaron Knoll, right?” Everyone nods. Ruth and Lydia confirm that his identity is correct.
“Great. Aaron was in an MVC about six hours ago. Appears he fell asleep at the wheel. Pretty messed up crash, which required fire rescue to cut the car into pieces. His girlfriend is still in Emergency; not sure what is happening there. Aaron received a significant laceration to his head and a concussion. The spleen laceration was confirmed on CT. Most likely from the trauma of the seat belt. The bleeding looked a bit loculated, but I expect it is tamponaded due to the swelling of the spleen and the parietal membrane.”
Bassam nods. “I have extra lap sponges and three extra sterile suctions with bottles hooked up.”
“Thanks. I hope we won’t need all of that, but I expect we may. Looking at the CT scan, I had hoped to repair minimally invasively, but there is so much blood and swelling that I ’ m unsure how big the tear may be. My plan is to go in slowly and once I get to the parietal membrane, expose it as much as possible. I ’ ll let Dr. Bondie and Bassam know when I ’ m going to cut in deeper. It will be a smaller incision. Then we will stick the suction in to see if we can relieve some of the pressure and help visualize the area better. Once that ’ s done, we ’ ll fully open him up, find any bleeders, tie those off, and then if we can sew the spleen up or do a partial splenectomy, that is preferable to fully removing it. I can’t decide which until I see what is what in there.”
Ruth speaks up. “Four units of PRCs in the fridge and Dr. Blake has told me he ’ s going to stick around in case Dr. Lai needs any help managing the rapid infuser. PACU is aware that he may be unstable and I have arranged for ICU nurse coverage if necessary.”
“I have extra vascular clamps, retractors, and silk on the back table. I ’ m all counted in and ready.”
“Ok, if there are no more questions, let ’ s get started,” states Dr. Bondie. “Lydia, would you turn on the Michael Bublé mixed tape, please?”
Health Case Studies Copyright © 2017 by BCIT is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License , except where otherwise noted.
Share This Book
- Email Us

- Executive Moves
- Transaction & Valuation
- Patient Flow
- Philanthropy
- Other Channels ►
- Patient Experience
- Care Coordination
- Legal & Regulatory
- Compensation
- Rankings & Ratings
- Becker's Healthcare Websites ►
- Dental + DSO
- Behavioral Health
- Physician Leadership
- E-Newsletters ►
- Sign Up For Our Free E-Newsletters
- Hospital Review
- Hospital CEO Report
- Hospital CFO Report
- Health IT and CIO Report
- Digital & Innovation Report
- Clinical Leadership & Infection Control
- Revenue Cycle
- Supply Chain
- Payer Issues
- Pharmacy Report
- Women's Leadership
- Cardiology Report
- Oncology Report
- Laboratory Review
- HR + Talent Review
- Post Acute Review
- Conferences ►
- Conferences and Events
- Call for Speakers
- Exhibiting & Sponsoring
- Virtual Conferences ►
- Upcoming Virtual Events
- Past Virtual Events
- Featured Sessions OnDemand
- Upcoming Webinars
- OnDemand Webinars
- Past Webinars
- Whitepapers ►
- Current Whitepapers
- Our Podcasts
- Becker's Healthcare Podcast Episodes
- Becker's Women's Leadership Podcast
- Becker's Ambulatory Surgery Centers Podcast
- Becker's Spine and Orthopedics Podcast
- Becker's Dental + DSO Review Podcast
- Becker’s Payer Issues Podcast
- Becker’s Pediatric Leadership Podcast
- Becker's Cardiology + Heart Surgery Podcast
- Becker’s Clinical Leadership Podcast
- Becker’s Digital Health + Health IT Podcast
- Print Issue ►
- Current Issue
- Past Issues
- Current Issue - Becker's Clinical Leadership & Infection Control
- Past Issues - Becker's Clinical Leadership & Infection Control
- Multimedia ►
- Robotics Content Hub
- Featured Content
- Living Like a Leader Series
- 100 of the largest hospitals and health systems in America | 2021
- Nominations
- About Becker's Hospital Review
- Careers at Becker's
- Request Media Kit
- Content Specifications
Optimizing operating room utilization: A case study
Thursday, july 28th, 2022 | 12:00 pm - 1:00 pm ct .
- Inefficient processes
- Deep-rooted cultures and a "scarcity mindset"
- An emphasis on metrics that don’t have a significant impact on OR utilization
- A lack of tools that go beyond the standard capabilities EHRs can provide to increase access, accountability and transparency
Presenters:

Sara Hubbard, MBA, MA, LSSB, CPT, SHRM-SCP
Principal consultant, operational performance improvement, baptist health jacksonville, fl.

Nicole B. Thomas, FACHE
Hospital president, baptist medical center jacksonville.
Becker's Websites
- Career Center
Virtual Learning
- Whitepapers
Conferences
- 9th Annual Health IT + Digital Health + RCM Meeting: The Future of Business and Clinical Technologies
- Becker's ASC 30th Annual Meeting: The Business and Operations of ASCs
- Fall Future of Dentistry Roundtable
- 12th Annual CEO + CFO Roundtable
- Fall Payer Issues Roundtable
- 1.800.417.2035
- [email protected]

- Healthcare Executives and Senior Leaders
- Solutions for Physicians and Clinical Staff
- Non-Healthcare Leaders
- Organizational and Cultural Transformation
- Developing Vision and Alignment
- Assessments
- Immersive Experiences
- Coaching and Facilitation
- Speakers and Inspiration
- Academic Journals
- Our Approach
- Solutions for Non-Healthcare Leaders
Lean Management, Patient Safety, Performance Improvement, Quality and Safety
Case study | surgical setup reduction improves patient outcomes.
To be financially viable, a hospital’s operating rooms (ORs) must keep quality and utilization high and expenses low. It’s critical to plan ahead, be prepared, and set volumes correctly. This means an organization’s OR team should be continuously finding ways to improve turnover time in their ORs, while also sustaining improvements to patient safety, staff engagement and organizational costs.
Surgical instrument processing is critical to safe, high-quality surgical care but has receives little attention. Typical hospitals have inventories in the tens of thousands of surgical instruments organized into thousands of instrument sets. The use of these instruments for multiple procedures per day leads to millions of instrument sets being reprocessed yearly in a single hospital. Errors in the processing of sterile instruments may lead to increased operative times and costs, as well as potentially contributing to surgical infections and perioperative morbidity.
When Virginia Mason’s team examined their inventory of surgical instruments they saw, that at any one time, thousands of instruments were being used and processed during setup, surgery, breakdown or sterilization — about 5.2 million instruments per year — and still large amounts of instruments were left unused in storage. Additionally, there were roughly 3,800 unique instruments sets set to different surgeries and different physician’s preferences. Although they had worked hard to keep the inventory down, 3 they knew innovative thinking could help them make lasting improvements.
A quality monitoring approach was developed to identify and categorize errors in sterile instrument processing through use of a Daily Defect Sheet. Virginia Mason Production System ® (VMPS ® ) improvement methods were used to improve the quality of surgical instrument processing through redefining operator roles, alteration of the workspace, mistake-proofing, quality monitoring, staff training, and continuous feedback.
To study the effectiveness of the quality improvement project, a before and after comparison of prospectively collected sterile processing error rates during a 37-month time frame was performed. After implementing a transformation to their operating rooms’ build-to-order (BTO) process, they removed 58,728 unnecessary instruments, and eliminated all $500,000 worth of unused “sleeping” sets — weighing 29,480 pounds — from processing in the first year. In neurosurgery alone, instrument assembly time decreased by 42 percent, and inventory was reduced by 26 percent.
Instrument Assembly Time
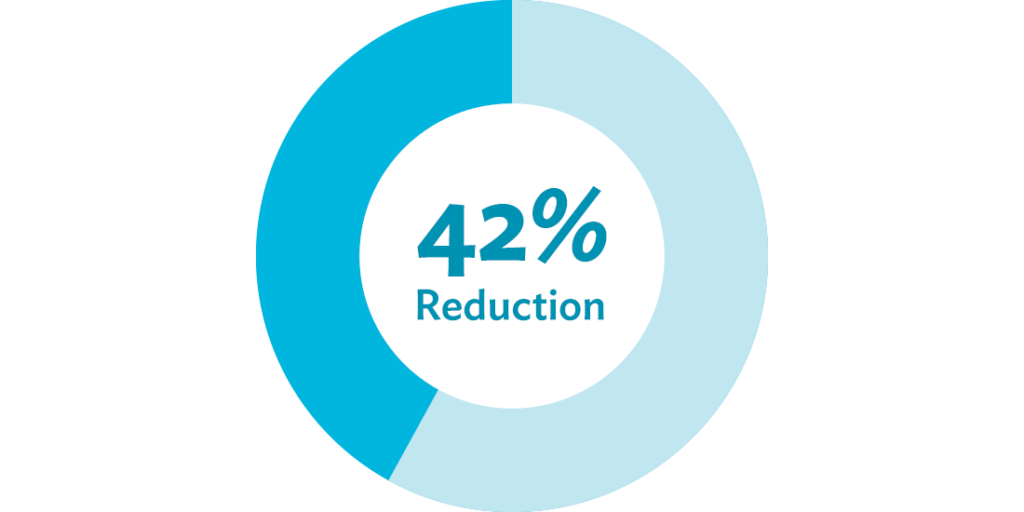
Starting with inventory, progressing with data collection
To answer the question of which instruments surgeons needed most or preferred to use, the team examined and collected surgeons’ preferences based on actual usage. The vision, according to the director of sterile processing at the time, was to create a “better patient experience, with fewer defects, faster setup and better patient throughput.”
Team leaders — after evaluating their employees’ interest and aptitude — trained a nominated group of surgical technicians in VMPS ® improvement tools and methods. Following the training, the group took their clipboards, pens and timers to operating rooms, setup areas, breakdown areas, sterilization rooms and storage rooms. They observed the different work areas to understand physician priorities and track how much time was spent on tasks that made a difference to patients and staff versus time spent on wasteful processes that didn’t benefit patients and overburdened staff.
The improvement team was able to easily step into the operating rooms, introduce themselves and explain what type of data they’d be collecting. The work was transparent from the beginning, and no one felt threatened or worried. The surgeons and staff knew they were all a team and that the improvement team was there to improve work for patients and staff alike. They observed each surgeon and procedure five times, building data so that the team could truly understand the current state and begin planning for a better process to test.
Establishing a structure to guide the work
Armed with data, team members came together for a 3P (Production Preparation Process) 4 workshop to set their vision for a dramatically more efficient process. By the end of the 3P, the participants had created a guiding team to determine next steps, oversee all the work and answer any questions that came up throughout the process. The guiding team included a sterile processing leader, operating room leader, improvement office leader, neurosurgeon, surgical technologist, sterile processing technician, project support staff member and administrative support staff member.
Using improvement methods and tools to get results
Next, the team employed the concept of 5S (sort, simplify, sweep, standardize, self-discipline). They discovered that almost 60 percent of the items in their orthopedic case sets were rarely used. This equates to 700 tons of unnecessary instruments being processed, per year. Using data, they sorted which instruments were being used, and simplified the process by removing non-critical instruments left unused. They swept the area by designing a repeatable inspection of case sets, standardized their tray layout, and established a team agreement to continue monitoring.
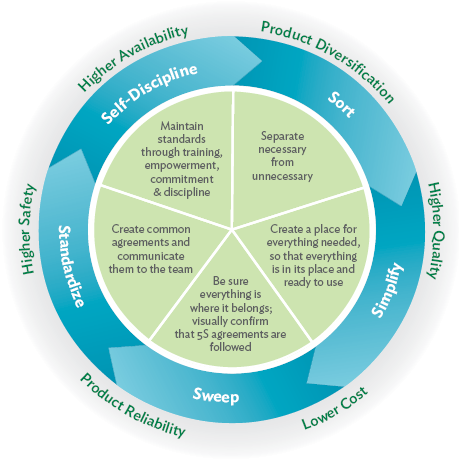
The creation of the build-to-order instrument sets employed the concept of just-in-time inventory — in which just the right surgical instruments would be delivered just when they were needed — and allowed for customization to each surgeon’s needs for a procedure. The new setup technique made the process of tool assembly much easier for surgical technologists. A production board provided team members with a visual reference of the current demand for supplies.
In an additional improvement event, focusing on the setup for craniotomy procedures, participants discovered how to customize each set, reducing the setup time and the OR space needs in the suite. By the end of the event, they were able to combine sets, reducing their setup time from 34 minutes to 2 1/2 minutes, a 92 percent reduction. The team compared times before and after the improvement events and found that the more limited case sets did not increase overall procedure time but greatly increased OR turnover time.
Seeing financial gains
This work also yields significant financial benefits to a health care organization. A reduction in processing yielded an annual cost savings of $65,000 per year. The number of lost, broken and damaged instruments was also reduced.
Getting results for other surgery sets
The team spread the work by helping other specialty teams, including orthopedics, neurosurgery and thoracic surgery produce similar setup reductions. The results for improving the laminectomy surgical setup were very impressive. After implementing the build-to-order sets, the instrument assembly went from 34 minutes to 20 minutes, 15 seconds. The instrument setup in the OR went from 24 minutes, 9 seconds, to 2 minutes, 29 seconds — a 90 percent decrease. The number of instruments used decreased from 152 to 59, and the number of instrument sets decreased from 5 to 2.
Instrument Assembly

Operating Room Instrument Setup
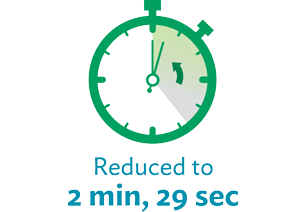
Number of Instruments
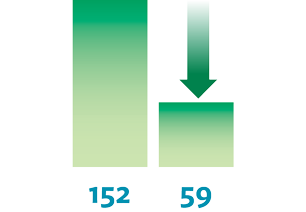
Improving quality and safety
During the assessment of their instrument inventory before the improvement work, the team determined that the large number of unnecessary instruments in storage could have a big impact on safety. Not only was the probability greater for a surgical technologist to select the wrong instrument for a procedure, but the time spent searching for specific instruments and maintaining all these instruments — many of which were processed and sterilized yet never used — could potentially affect patient care.
Before the intervention, instrument processing errors occurred in 3.0 percent of surgical cases, decreasing to 1.5 percent. Improvements were observed in multiple categories of error types, particularly the assembly errors of packaging (from 0.66 to 0.24 errors per hundred cases), and foreign objects (0.17 to 0.02 errors per hundred cases).
Improving patient access and timely care delivery
The lead time for booking orthopedic surgery, for example, went from 65 days down to 21 days. This meant surgeons did not have to wait as long between procedures and could handle an increase in volume of patient cases.
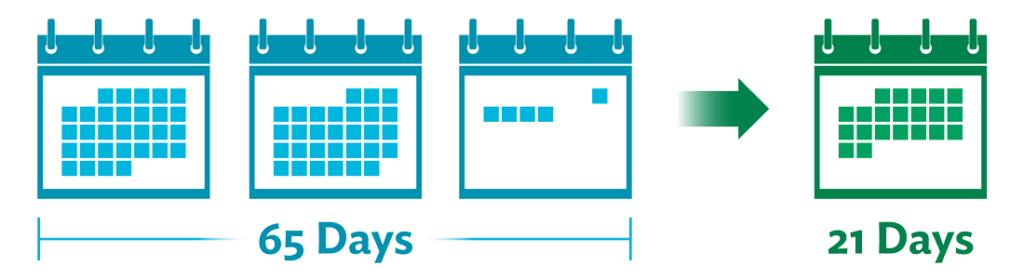
Key takeaway
Surgical instrument processing errors are a barrier to the highest quality and safety in surgical care but are amenable to substantial improvement using improvement techniques.
Originally published May 24 2018, updated July 12 2021
Are you ready to develop advanced process improvement expertise?
Learn more about our virtual intensive certificate program – Advanced Process Improvement Training.
“This course work came in at the perfect time as the topics we covered in class aligned perfectly with a vaccine delivery clinic we created and we used almost every tool taught 100% to deploy something outside of our comfort zone, and it was wildly successful!” – Chuck Hampston, Lean and Process Improvement Coordinator, Memorial Medical Center, Ashland WI
Similar resources
Lean Management, Optimizing Flow, Quality and Safety
Case study | 36-clinic federally qualified health center saves $600k annually improving patient flow.

Case Study | Building a New Outpatient Surgery Center With Patients and Staff in Mind
Leadership Development, Lean Management, Performance Improvement
Podcast | systematizing equity at virginia mason franciscan health, stay connected.
Sign up for our monthly emails to stay up to date with our latest news, resources, case studies, events and more.
Your information will not be shared. Learn more about our privacy policy here .
- Open access
- Published: 23 July 2022
Bringing the patient voice into the operating room: engaging patients in surgical safety research with the Operating Room Black Box ®
- Cole Etherington 1 , 2 ,
- Maxime Lê 3 ,
- Laurie Proulx 3 , 4 &
- Sylvain Boet ORCID: orcid.org/0000-0002-1679-818X 1 , 2 , 5 , 6 , 7 , 8 , 9
Research Involvement and Engagement volume 8 , Article number: 32 ( 2022 ) Cite this article
3437 Accesses
8 Altmetric
Metrics details
Surgery is one of the most common patient experiences in the health care system. Yet, efforts to engage patients in surgical safety research have not matched those of other health care fields. This is a critical issue given the nature of surgery inhibits patients’ abilities to advocate for themselves as they are typically under anesthetic when the procedure is performed. We partnered with patients throughout our research program, which uses the Operating Room Black Box ® to enhance surgical patient safety through transparent and proactive analysis of human factors to detect and prevent avoidable errors.
In this article, we outline the need for, and our approach to, patient engagement in surgical safety research. Our approach included a series of planned activities and skill development opportunities designed to build capacity and bring together patients, clinicians, and researchers to inform research and practice. We also conducted evaluation surveys during the first year of our program, which have indicated a positive experience by both patient partners and the research team.
We believe our approach can serve as an important first step toward building a model for patient engagement in the surgical safety field and could significantly contribute to improved quality of care and outcomes for surgical patients.
Plain English summary
Although surgery is one of the most common patient experiences, patients have not been engaged in surgical safety research. Patients were engaged as patient advisors in the use of the Operating Room Black Box ® at The Ottawa Hospital. The Operating Room Black Box ® is a tool that is used in the operating room (OR) which captures audio, video, patient vital signs and other information that are analyzed for research purposes. The aim of the OR Black Box ® is to learn from experience and improve practice and care. Patient advisors influenced the nature of the activities undertaken, co-developed the communication materials for patients, evaluated patient engagement practices, and disseminated the research results. These patient engagement activities are an important first step in engaging patients in surgical safety research.
Peer Review reports
Introduction
Surgery is one of the most common patient experiences in acute care [ 1 ]. Yet, efforts to engage patients in operative safety research have not matched those of other health care fields [ 2 ]. This is a critical issue for several reasons. First, anesthesia inhibits patients’ abilities to advocate for themselves as they are sedated during surgery. Second, nearly one in ten surgical patients will experience a complication (e.g. infection, injury, bowel obstruction, pulmonary embolism) [ 1 ], which can reduce patients’ quality of life, delay recovery, and sometimes result in mortality [ 3 ]. Third, the rate of preventable errors in surgery remains relatively high (> 50%) [ 3 , 4 , 5 , 6 ], and there has been minimal improvement in recent years despite ongoing proliferation of practice interventions [ 1 , 7 ]. While interventions for the operating (OR) room have typically not been developed in partnership with patients [ 8 , 9 ], both evidence and practice demonstrate this is essential for preventing, responding to and learning from patient safety incidents [ 10 ].
The OR Black Box ® as a unique opportunity for patient engagement
Our research team uses OR Black Box ® technology [ 11 , 12 ] to study and improve OR practice and obtain the best possible patient outcomes. Like black boxes used in aviation, the OR Black Box ® is an innovative tool that records detailed information from the surgical environment (e.g. audio, video, physiological and environmental data). Data can be used for research purposes and to improve practice. Further information about the OR Black Box ® is described elsewhere [ 13 , 14 , 15 ]. The Ottawa Hospital was among the first institutions in the world to adopt the OR Black Box ® , which we successfully implemented in June 2018 [ 14 ]. We are currently using this technology to study teamwork in everyday clinical practice, to identify areas for improvement, and to assess the effectiveness of interventions (manuscripts in preparation and under review). Our initial exploratory studies aim to better understand current practices in the OR, which will inform decision-making regarding areas for improvement, future research, and intervention development. Once identified, we will work with our patient partners to prioritize key areas.
Unlike other OR technologies that may be used to collect data, the OR Black Box ® provides systematic, real-time capture of a wider range of intraoperative data than has previously been possible [ 14 ]. Room cameras, microphones, laparoscopic cameras, along with various devices and sensors capture patient physiology and environmental factors (e.g. decibel level, room temperature) [ 14 ]. High definition (HD) cameras record a 180-degree view of the surgical field and HD unidirectional microphones are strategically placed around OR team members (e.g. surgeon, anesthesiologist, scrub nurse) [ 14 ].
To ensure this innovation could be optimally beneficial to patients, we determined it would be important to engage them at each stage of OR Black Box ® implementation and subsequent research studies. However, there was a lack of examples within the surgical safety literature on how to best engage patient partners. In this commentary, we therefore aim to outline our approach to patient engagement in order to provide an example that may be of use to other research teams in surgery.

Why does patient engagement in surgical safety research matter?
As experienced health system users, patients can bring a unique perspective to research that can increase its accountability, relevance, and transparency [ 16 , 17 , 18 ]. While patient-centered care is a key underlying principle of modern perioperative practice [ 19 ], surgical safety research has often overlooked the role of patients in being active partners and co-designers in the research process rather than solely participants [ 18 ]. This is a missed opportunity to increase the value and impact of surgical safety research, particularly as patients are the ultimate recipients of research findings [ 20 ]. Given there has not been any substantial annual reduction in patient safety events in recent years despite a proliferation of practice interventions and medical advances [ 1 , 7 ], it is time to approach research differently.
Surgical patients have first-hand experience of a variety of services throughout the perioperative pathway, including gaps in the current healthcare system. This type of lived experience can be invaluable for informing surgical safety research priorities, analysis of results, and translation of findings into clinical practice [ 21 ]. For example, including the patient in OR team briefings (e.g. the patient confirms their name and allergies) when possible has been suggested as a patient-centered practice [ 19 ], but its implementation and effects have never been investigated. Involving patient partners could provide key insights as to how patients might prefer to be included in the activities of the OR team while awake (e.g., under regional anesthesia) and reveal specific considerations for when fully anesthetized. By including patient partners, surgical safety research agendas can become more informed and more accountable [ 20 ], ultimately enhancing patient-centered surgical care [ 21 , 22 ].
Our approach to patient engagement
To recruit patient partners, we leveraged the Patient and Family Advisor Council (PFAC) at The Ottawa Hospital (TOH). PFAC maintains an active database of patients and family members who are interested in partnering with hospital researchers, clinicians, or administrators to improve safety and quality of care at TOH. PFAC connected us to potential patient partners. We aimed to recruit two patients rather than one in order to avoid tokenism, help patients to feel more comfortable to participate in team meetings, and ensure a balanced workload. Recruiting two patient partners was also suggested by LP during her interview, based on her vast experience in working with research teams. We also aimed to recruit patients representing different genders and age groups, as experiences of surgery can vary based on these characteristics. We conducted interviews with several candidates. Interviews were approximately 45 to 60 min, and inquired about patients’ previous experiences with both surgery and research, as well as their motivations for and interest in combining the two. We ultimately selected two patient advisors whom we felt had the best fit with our team and who had lived experience of multiple surgeries (ML, LP) to join our team. It was important to us that patients had experience of different types of surgeries given the variation in experiences that may occur across procedures. This would help to inform our implementation of the OR Black Box ® in a more generalizable manner which could be relevant to patients regardless of their procedure type.
We consulted with the Strategy for Patient-Oriented Research (SPOR) Program Facilitator of the Ottawa Methods Centre (OMC) to obtain guidance for working with patient advisors. The OMC is a member of the Ontario SPOR Support Unit housed at the Ottawa Hospital Research Institute. The Unit is funded by the Canadian Institutes of Health Research to provide investigators with methodological guidance on patient-oriented research. The OMC SPOR Program Facilitator provided our team with resources on engaging patients in research, which covered a range of topics such as conducting team meetings and activity planning. Based on this guidance, we planned an initial set of patient engagement activities, which were subsequently refined after the patient advisors joined our team (Table 1 ).
After both patient advisors were recruited, terms of reference were co-designed based on an example template provided by the OMC SPOR Program Facilitator (Additional file 1 ). We elected to collaboratively develop the terms of reference to establish a clear understanding of roles and responsibilities by all team members. The terms of reference were also designed to ensure that the research partnership would be respectful of patient partners’ other commitments, responsibilities, and needs. This included, for example, setting meetings on particular dates based on patient advisors’ availability and providing travel vouchers as needed. Patient advisors were then formally onboarded at our centre through training and orientation provided by TOH to orient all new volunteers to hospital policies and procedures. We also held an initial team meeting to orient the patient advisors to our research program and invited them to various events at our research institution to learn more about the organization and work being done.
Planned patient engagement activities commenced following patient advisor onboarding and evolved as needed based on advisors’ feedback (Table 1 ). Below we provide a chronological account and brief description of each activity.
The first planned activity involved grant review to establish our research program and implement the OR Black Box ® . Feedback obtained at this stage was incorporated into the grant applications and also helped to develop new activities, such as regular evaluation of our patient engagement approach. The second planned activity was co-design of the patient communication campaign as part of the OR Black Box ® implementation at our centre. Based on data from our previously conducted study of patient perceptions regarding this technology [ 23 ], patient advisors created messages and materials to be distributed to patients prior to surgery. The details of the communication campaign are described elsewhere [ 14 ].
In brief, our research question focused on determining what might prevent patients from agreeing to have their surgery captured by the OR Black Box ® and what could make them feel more comfortable with it [ 23 ]. Results indicated that patients unanimously valued the much-needed transparency offered by this tool and were supportive of its use for patient safety research [ 23 ]. From the interviews, we identified key themes regarding important information patients would want to have communicated to them prior to having surgery in the OR Black Box ® room [ 23 ]. For example, patients expressed that they wanted to be informed about the research goals (i.e., what we were using the technology to study) and also wanted to be told about the privacy measures in place [ 23 ]. We incorporated these themes into an evidence-based, hospital-wide communications campaign to inform patients and their families about the OR Black Box ® .
The communications campaign was developed in collaboration with our patient advisors (ML, LP). The advisors helped to identify the most important themes to share with the larger patient population based on their own experiences of surgery. They then took part in a design session alongside members of the research team to pair messages with relatable images and to develop appropriate and accessible wording. From there, we engaged in an iterative review process of informational poster and pamphlet prototypes. We also worked closely with the communications team at our centre. The final poster and pamphlet were agreed upon by everyone involved and are currently available to patients at our centre. Patient partners also suggested the appropriate timing in the care pathway to receive this information; namely, during the preoperative assessment which takes places several weeks before the procedure. This was suggested because it would give patients enough time to learn and ask questions about the OR Black Box ® , without adding to any anxiety experienced on the day of surgery. This important consideration may have been overlooked without the involvement of our patient advisors and has been key to the high number of patients agreeing to be recorded during their surgery at our centre.
As the campaign was launched, the patient advisors participated in numerous dissemination activities. Our initial engagement plan was for the patient partners to attend and present their experience with implementing the OR Black Box ® for surgical safety research at the annual Surgical Safety Network (SSN) meeting. The SSN meeting is an international meeting of surgical safety experts, including clinician-researchers and organizational leaders. Following this event, however, many additional opportunities arose for patient partners to share their experience. This was not anticipated or planned for ahead of time but was fully embraced and supported by our team. In addition, we did not initially plan for patient partners to be interviewed by the media, but this occurred several times over the course of our project as patient partners expressed interest in these opportunities. The patient advisors shared their experience and insights on patient engagement with diverse audiences, including the public, hospital stakeholders, the broader health research community, and other patient-related organizations. This ultimately facilitated positive momentum around the OR Black Box ® initiative, particularly for centres considering implementing the OR Black Box ® in the future. Sharing their lived experiences to these audiences thus laid the groundwork for future international collaborations to advance patient engagement in surgical safety research.
Following successful implementation of the OR Black Box ® at our centre, we began to plan our first series of research studies. Patient advisors assisted with developing additional grant applications and study protocols, and were listed as co-authors/co-applicants as appropriate. Their feedback was consistently incorporated, often helping to identify key research gaps. For example, our patient partners have shared their experiences of considerable variation in how healthcare professionals interact with patients in the pathway leading up to general anesthesia or during the surgery when performed under sedation or regional anesthesia. This has expanded our research program to include a series of studies that focus on how to develop and implement patient-centered teamwork in every OR. This could involve ensuring that team members explain what is going on, what will happen next, and what choices are available at each point in the process where possible. A patient-centered conception of OR teamwork may also shift patient safety culture and further empower patients to play an active role in their surgical care, even in the OR. With the OR Black Box ® , we will be able to study the extent to which these things happen, identify key moments for including patients, and determine intervention effectiveness. As we move forward with this work, we will work with our patient partners to evaluate our data and translate our findings into practice.
Learning from our approach
Throughout the first year of our program development, we conducted three informal evaluation surveys in order to reflect on and improve our approach to patient engagement. Surveys were conducted at months 5, 10 and 15. Patient partners (n = 2) and research team members (n = 4) were surveyed, and results were collated and shared with the full team after each survey. Research Ethics Board approval was not required as the surveys were viewed as internal quality improvement activities. We specifically explored satisfaction with the experience, attitudes toward engagement, feelings of being heard and understood, perceived team effectiveness and trust, resources invested (e.g. time, money), products emerging from our activities, and practice/clinical improvements resulting from our activities. The survey used was recommended by the OMC SPOR Program Facilitator and developed by Patients Canada, a national organization that works to bring the patient voice to healthcare decision-making [ 24 ]. Survey questions capture the research team’s and patient partners’ experiences with the initial engagement and subsequent research processes. This was deemed suitable for our purposes of documenting and learning from our experiences to constructively move our research program forward. Of note, this was not a formal program evaluation but rather an internal assessment for the purposes of our team. As our program expands, there may be opportunities to conduct a formal evaluation.
Overall, the surveys indicated a positive experience by both patient partners and the research team. Both patient partners reported that, in their opinion, their insights and comments impacted the decisions of the team regarding the research project. Research team members rated the feedback given by patient partners as very valuable and indicated that patients should definitely be involved in this type of research. Patient partners indicated that our group’s collaboration helped them to learn more about the research process, the challenges involved, and important information to relay to the patient community. Research team members expressed that patients’ voices were assets to the project and that researchers should “never underestimate how much patients can offer”. Patients also reported that the team accommodated their needs appropriately (e.g. flexibility in meeting times and locations), that they felt comfortable speaking up in meetings, and that they felt equipped to contribute to the project.
From the surveys, we identified resource-related issues as a key area for improvement. Research projects are primarily grant-funded, which can be unpredictable and make long-term planning difficult. Our initial year of patient engagement was funded, meaning we were able to provide our patient partners with compensation (payment) and cover travel costs and other related expenses. However, we recommend that funding agencies and healthcare organizations consider strategies to secure funding for sustainable and long-term patient engagement activities. Alternatively, research teams will need to secure additional funds to account for the extended contributions of patient partners. We also suggest budgeting for team-building activities, networking and training opportunities, and unanticipated expenses that may be incurred by patient partners as a result of engaging with the project (e.g., having to take a day off of work to attend conferences).
Lessons learned
From our experience so far, we have obtained several insights that may be useful to other research teams seeking to engage patient partners in their surgical safety projects. In addition to establishing open communication, respect, and active involvement, which have been emphasized by other authors [ 20 , 25 , 26 ] we identified several key logistical points based on the evaluation survey responses. These lessons are summarized in Table 2 . With regard to engagement in surgical safety research in particular, it may be beneficial to seek patient partners with experience of certain procedures depending on the research area. In our case, a wide range of experiences was suitable to inform OR Black Box ® implementation; however, researchers focusing on a narrower surgical field (e.g., orthopedics, neurology, cardiovascular) may wish to engage patients who have experienced those procedures specifically.
Future directions
Data collection with the OR Black Box ® is currently underway. This data will be used to identify areas for improvement in OR teamwork and interventions will be co-designed with patient partners. We plan to assess the impact of OR teamwork and teamwork interventions on patient-centered outcomes, determined in partnership with patient advisors. It is our hope that patient engagement will ensure a direct link between research objectives and outputs and the lived experiences of surgical patients and real-world healthcare services.
We will continue to explore avenues for building capacity in surgical patient engagement across centres in order to maximize research impact and dissemination. We also plan to work with our centre and others to support patient engagement in surgical safety research long-term. For example, we recognize that patient needs, and experiences may vary by type of surgery. Therefore, it may be valuable to form sub-committees within our network where patient partners can be involved in research across different surgical contexts (e.g., emergency vs. elective procedures, oncological, cardiovascular, procedures for chronic disease management, etc.). Innovation and collaboration are needed in this area to ensure enduring and meaningful patient partnerships in research that will ultimately make surgery safer.
Conclusions
We believe that engaging patient partners in implementation of the OR Black Box ® was a key aspect of successful implementation and provided a strong foundation for patient-centered surgical safety research at our centre. Our approach represents an important first step toward advancing patient engagement in the surgical safety field at a larger scale. Funding agencies and healthcare organizations should consider strategies to support meaningful and long-term collaborations between researchers and patient partners. These partnerships are essential for improving patient safety and outcomes in surgery.
Availability of data and materials
Not applicable.
Abbreviations
Operating room
Canadian Institute for Health Information and Canadian Patient Safety Institute. Measuring Patient Harm in Canadian Hospitals [Internet]. Ottawa, ON; 2016 [cited 2017 Jan 27]. Available from: www.cihi.ca
Prey JE, Woollen J, Wilcox L, Sackeim AD, Hripcsak G, Bakken S, et al. Patient engagement in the inpatient setting: a systematic review. J Am Med Inform Assoc. 2014;21(4):742–50. https://doi.org/10.1136/amiajnl-2013-002141 .
Article PubMed Google Scholar
Zegers M, de Bruijne MC, de Keizer B, Merten H, Groenewegen PP, van der Wal G, et al. The incidence, root-causes, and outcomes of adverse events in surgical units: implication for potential prevention strategies. Patient Saf Surg. 2011;5(1):13. https://doi.org/10.1186/1754-9493-5-13 .
Article PubMed PubMed Central Google Scholar
Baker GR, Norton PG, Flintoft V, Blais R, Brown A, Cox J, et al. The Canadian adverse events study: the incidence of adverse events among hospital patients in Canada. CMAJ. 2004;170(11):1678–86.
Article Google Scholar
Healey MA, Shackford SR, Osler TM, Rogers FB, Burns E. Complications in surgical patients. Arch Surg. 2002;137(5):611–8.
Weiser TG, Regenbogen SE, Thompson KD, Haynes AB, Lipsitz SR, Berry WR, et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet. 2008;372(9633):139–44.
Kapur N, Parand A, Soukup T, Reader T, Sevdalis N. Aviation and healthcare: a comparative review with implications for patient safety. JRSM Open. 2016;7(1):2054270415616548.
Burke CS, Salas E, Wilson-Donnelly K. How to turn a team of experts into an expert medical team: guidance from the aviation and military communities. Qual Saf Heal Care. 2004;13:96–104.
Salas E, Sims DE, Burke CS. Is there a “big five” in teamwork? Small Group Res. 2005;36(5):555–99.
Canadian Patient Safety Institute. Engaging Patients in Patient Safety: A Canadian Guide -Evaluating patient engagement [Internet]. Ottawa, ON; 2017. Available from: https://www.patientsafetyinstitute.ca/en/toolsResources/Patient-Engagement-in-Patient-Safety-Guide/Documents/Engaging%20Patients%20in%20Patient%20Safety.pdf .
Goldenberg MG, Jung J, Grantcharov TP. Using data to enhance performance and improve quality and safety in surgery. JAMA Surg. 2017;369(15):1434–42. https://doi.org/10.1001/jamasurg.2017.2888 .
Jung JJ, Jüni P, Lebovic G, Grantcharov T. First-year Analysis of the Operating Room Black Box Study. Ann Surg. 2018;271(1):122–7. https://doi.org/10.1097/SLA.0000000000002863 .
Etherington N, Usama A, Patey AM, Trudel C, Przybylak-brouillard A, Presseau J, et al. Exploring stakeholder perceptions around implementation of the Operating Room Black Box for patient safety research : a qualitative study using the theoretical domains framework. BMJ Open Qual. 2019. https://doi.org/10.1136/bmjoq-2019-000686 .
Boet S, Etherington N, Lam S, Lê M, Proulx L, Britton M, et al. Implementation of healthcare research technology through patient, clinical, and organizational engagement: a case study of the Operating Room Black Box ® research program at the Ottawa Hospital. JMIR. 2021;23(3):e15443.
PubMed PubMed Central Google Scholar
Jung JJ, Jüni P, Lebovic G, Grantcharov T. First-year analysis of the Operating Room Black Box study. Ann Surg. 2020;271(1):122–7.
McCarron TL, Moffat K, Wilkinson G, Zelinsky S, Boyd JM, White D, et al. Understanding patient engagement in health system decision-making: a co-designed scoping review. Syst Rev. 2019;8(1):1–10.
Liang L, Cako A, Urquhart R, Straus SE, Wodchis WP, Baker GR, et al. Patient engagement in hospital health service planning and improvement: a scoping review. BMJ Open. 2018;8(1):1–8.
Tscherning SC, Bekker HL, Vedelø TW, Finderup J, Rodkjær LØ. How to engage patient partners in health service research: a scoping review protocol. Res Involv Engagem. 2021;7(1):1–7.
Koo K. Patient-centered operating room briefings to improve surgical quality. JAMA Surg. 2015;150(2):183. https://doi.org/10.1001/jamasurg.2014.2917 .
Manafo E, Petermann L, Mason-Lai P, Vandall-Walker V. Patient engagement in Canada: a scoping review of the “how” and “what” of patient engagement in health research. Heal Res Policy Syst. 2018;16(1):1–11.
Domecq JP, Prutsky G, Elraiyah T, Wang Z, Nabhan M, Shippee N, et al. Patient engagement in research: a systematic review. BMC Health Serv Res. 2014;14:1–9.
NEJM Catalyst. What is patient-centered care? NEJM Catal Innov Care Deliv. 2017. https://doi.org/10.1056/CAT.17.0559 .
Etherington N, Usama A, Patey AM, Trudel C, Przybylak-Brouillard A, Presseau J, et al. Exploring stakeholder perceptions around implementation of the Operating Room Black Box for patient safety research: a qualitative study using the theoretical domains framework. BMJ Open Qual. 2019;8(3):e000686.
Patients Canada. Patients as partners in research surveys. 2016.
Witteman HO, Chipenda Dansokho S, Colquhoun H, Fagerlin A, Giguere AMC, Glouberman S, et al. Twelve lessons learned for effective research partnerships between patients, caregivers, clinicians, academic researchers, and other stakeholders. J Gen Intern Med. 2018;33(4):558–62.
Heckert A, Forsythe LP, Carman KL, Frank L, Hemphill R, Elstad EA, et al. Researchers, patients, and other stakeholders’ perspectives on challenges to and strategies for engagement. Res Involv Engagem. 2020;6(1):1–18.
Download references
Acknowledgements
The authors wish to thank Antoine Przybylak-Brouillard and Sandy Lam for their contributions to project coordination, as well as Zarah Monfaredi and Claudia Hampel for their support and guidance with patient engagement resources. The authors also wish to thank Stuart Nicholls for his critical review.
This project was supported by a grant from the Canadian Institutes of Health Research (CIHR) Strategy for Patient-Oriented Research (SPOR) and matching funds from the IBM Center for Advanced Studies. Dr. Boet was supported by The Ottawa Hospital Anesthesia Alternate Funds Association and the Faculty of Medicine, University of Ottawa with a Tier 2 Clinical Research Chair.
Author information
Authors and affiliations.
Clinical Epidemiology Program, Ottawa Hospital Research Institute, Ottawa, Canada
Cole Etherington & Sylvain Boet
Department of Anesthesiology and Pain Medicine, University of Ottawa, Ottawa, Canada
The Ottawa Hospital, Ottawa, Canada
Maxime Lê & Laurie Proulx
Canadian Arthritis Patient Alliance, Ottawa, Canada
Laurie Proulx
Department of Innovation in Medical Education, University of Ottawa, Ottawa, Canada
Sylvain Boet
Francophone Affairs, Faculty of Medicine, University of Ottawa, Ottawa, ON, Canada
Institute du Savoir Monfort, Ottawa, ON, Canada
Faculty of Education, University of Ottawa, Ottawa, ON, Canada
Department of Anesthesiology and Pain Medicine, The Ottawa Hospital, University of Ottawa, 501 Smyth Road, Ottawa, ON, K1H 8L6, Canada
You can also search for this author in PubMed Google Scholar
Contributions
CE conceptualized the article and wrote the initial draft. SB, ML, LP critically reviewed and made additional contributions to the content of the manuscript. All authors reviewed and approved the final version of the submitted manuscript and agree to be accountable for all aspects of the work.
Corresponding author
Correspondence to Sylvain Boet .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
Maxime Lê is the Principal of Lê and Co. Consultants.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
. Terms of Reference.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Etherington, C., Lê, M., Proulx, L. et al. Bringing the patient voice into the operating room: engaging patients in surgical safety research with the Operating Room Black Box ® . Res Involv Engagem 8 , 32 (2022). https://doi.org/10.1186/s40900-022-00367-5
Download citation
Received : 21 September 2021
Accepted : 12 July 2022
Published : 23 July 2022
DOI : https://doi.org/10.1186/s40900-022-00367-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient participation
- Patient safety
- Operating rooms
- Quality improvement
- Healthcare delivery
- Patient engagement
- Surgical safety
Research Involvement and Engagement
ISSN: 2056-7529
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- SAGE Open Nurs
- v.9; Jan-Dec 2023
- PMC10350747
Operating Room Nurses’ Understanding of Their Roles and Responsibilities for Patient Care and Safety Measures in Intraoperative Practice
Bisma chellam singh.
1 Staff Nurse, Head and Neck Operation Theater, Manchester Royal Infirmary Hospital, Manchester, UK
Judie Arulappan
2 Department of Maternal and Child health, College of Nursing, Sultan Qaboos University, Muscat, Sultanate of Oman
Introduction
Surgical care has been a vital part of healthcare services worldwide. Several patient safety measures have been adopted universally in the operating room (OR) before, during, and following surgical procedures. Despite this, errors or near misses still occur. Nurses in the OR have a pivotal role in the identification of factors that may impact patient safety and quality of care. Therefore, exploring the OR nurses’ understanding of their roles and responsibilities for patient care and safety in the intraoperative practice, which could lead to optimal patient safety, is essential.
This study explored the understanding of OR nurses regarding their roles and responsibilities for patient care and safety measures in the intraoperative practice.
The study was conducted in one of the tertiary care hospitals in the United Arab Emirates. Qualitative, descriptive, exploratory research design was utilized. The data were collected using semi-structured face to face interviews. Purposive sampling included eight nurses. Data analysis was performed following Colaizzi's seven-step strategy.
Seven emerging themes were identified. The main themes are: patient safety, preoperative preparation, standardization of practice, time management, staffing appropriateness, staff education and communication, and support to the patient in the OR.
OR nurse leaders may take into consideration the current findings as a reference for quality improvement projects in the hospital, considering the specific characteristics of each local setting. Although the participants consider that the environment is safe and the quality of care is high in the study setting, there is still room for improvement on workflows and processes. OR workflow should be improved especially by addressing the potential patient safety issues.
Introduction/Background
Intraoperative practice is highly complex and challenging considering the vulnerability of the patient ( Peate, 2015 ). The intraoperative period starts when the patient arrives at the operating room (OR) and ends when the patient gets transferred to the postoperative ward (Salazar Maya, 2022 ). The care in the OR involves high use of technology and is different than the care provided in other settings of the hospital. OR nurses play an instrumental role in preventing infection, maintaining asepsis, handling instruments, adopting medical techniques, preventing complications, and handling biological preparations. Additionally, nurses play an essential role in planning care and collaborating with the patient, surgical team, and other healthcare providers ( Flaubert et al., 2021 ; Kelvered et al., 2012 ).
Patient safety during surgery is one of the major alarms for intraoperative teams as adverse events occurring during this period is the major cause of disability and death ( Rodziewicz et al., 2022 ). Patient safety involves decreasing the danger of superfluous harm including anticipation of errors and avoidable adverse events to shield patients from injury ( Ingvarsdottir & Halldorsdottir, 2018 ). Major complications emerge in 3%–22% of surgeries, and the mortality rate is reported as 0.4%–0.8%. As the issue of patient safety takes a major toll, the World Health Organization ( WHO, 2017 ) calls for addressing the issue in the report “Safe Surgery Saves Lives.” These complications might be avoided if patients are taken care of during this period ( Ingvarsdottir & Halldorsdottir, 2018 ).
Review of Literature
Ugur et al. (2016) claim that errors occur more in OR as the staff come from various disciplines with various educational schemes and work as groups, which may cause surgical confusions. Therefore, the preventable mistakes can be lessened when OR staff are qualified in patient safety, clear systems are pursued step by step, and control structures are created and utilized. Likewise, effective communication among the OR staff reduces the surgical errors ( Ingvarsdottir & Halldorsdottir, 2018 ) and effective communication between the patient and medical and nursing staff enhances patient satisfaction ( Allison & George, 2014 ).
Ensuring patient safety in the OR includes prevention of all avoidable medical and surgical errors including preventing wrong person, site, procedure, and retained foreign objects. These errors can be prevented by structured communication with the patient, surgeon, and other healthcare team members ( American College of Obstetricians and Gynecologists, 2010 ; Rodziewicz et al., 2018 ). Additionally, correct identification of patients who are at risk of high blood loss, anesthesia or airway issues, history of allergies, and prevention of surgical site infection is essential ( Mcdowell & Mccomb, 2014 ; Woodman & Walker, 2016 ). In addition, the errors could be prevented during the preparation of surgical environment, instrumentation, sutures, and drugs ( Taaffe et al., 2018 ; Williams & Hopper, 2015 ). Likewise, patient safety can be enhanced through proper scheduling of procedures, communicating with other colleagues, helping to ensure consistency with the surgical safety checklist, and screening the progress in the surgeries and reporting to the board ( Rothrock, 2018 ).
Despite all safety checks, there is a risk for errors, which could cause adverse events to surgical patients ( Rodziewicz et al., 2018 ). Hence, it is imperative that the nurses are knowledgeable about patient safety and do corrective actions as patient advocates. Considering the surgical risk for the patients, McGarry et al. (2018) and Brown-Brumfield and Deleon (2010) emphasize the role of nurses in intraoperative patient safety and Kelvered et al. (2012) and Blomberg et al. (2018) point out the vulnerability of patients undergoing surgery and the risks associated with the intraoperative environment. Moreover, Gutierres et al. (2018) recommend various measures to improve patient safety during intraoperative period. Furthermore, the International Council for Nurses (2013) asserts that each registered nurse has a moral and ethical duty to speak-up for the patient's best interest, show quietude, regard, secure patient autonomy, and self-esteem ( Blomberg et al., 2018 ). Besides, accountability of nurses is essential for professional nursing practice and patient safety ( Battié & Steelman, 2014 ).
At the author's department, there were few incidences, such as specimen rejection, hand hygiene issues, errors in needles, sponge counting, and skin tearing in 2017 and 2018. Similarly, there was one incidence of skin injury during this period. This urged the authors to conduct the study to explore the understanding of OR nurses’ roles and responsibilities for patient care and safety in the intraoperative practice, which could lead to optimal patient safety using evidence-based practice.
Research Aim
The study explored the understanding of OR nurses regarding their roles and responsibilities for patient care and safety measures in the intraoperative practice.
We adopted a qualitative, descriptive, exploratory research design. Nurse researchers who conduct qualitative studies are contributing important information to the nursing body of knowledge that cannot be obtained by any other research design (Burns & Grove, 2005 , p. 52). The qualitative researchers have a preference for understanding events, actions, and processes within a specific context ( Babbie & Mouton, 2001 , p. 272). In addition, explorative research examines a phenomenon of interest, rather than simply observing and recording incidents of the phenomenon ( Lobelo, 2004 , p. 20). Likewise, qualitative descriptive approaches to nursing and healthcare research provide a broad insight into particular phenomena ( Doyle et al., 2020 ). Similar research design has been utilized in a previous research ( Sehularo et al., 2012 ). This design is utilized in the current study to explore and describe the understanding of OR nurses regarding their roles and responsibilities for patient care and safety measures in the intraoperative practice.
The study was conducted in one of the tertiary hospitals in the city of Abu Dhabi in the United Arab Emirates. All Interviews were taken place in a private room within the General Surgery OR department, which was quiet, private and calm that helped the participants to feel relaxed and ready to open and share their views.
Population comprised general surgery OR nurses.
Sample and Sampling Method
The sample comprised eight general surgery OR nurses working at a tertiary hospital. Purposive sampling was adopted.
Criteria for Sample Selection
Inclusion criteria.
The study included nurses with more than 2 years of experience in OR as they had extensive experience and in-depth knowledge to share their roles and responsibilities for patient care and safety measures in intraoperative practice.
Exclusion Criteria
Nurses in management positions were excluded in this study as they are not performing direct patient care in the OR.
Ethical Considerations
The study was approved by the Royal College of Surgeons in Ireland (RCSI) - Medical University of Bahrain (MUB) - Research Ethical Committee (REC). Further approval was granted from the organization involved in accessing and recruiting participants. All audio recordings were coded, password-protected, and stored in a double-locked cabinet in the primary investigator's office. Names, address, phone number, e-mail, and staff ID were not collected. Moreover, any information that may lead to the identification of the interviewees was deleted from the interview scripts. Likewise, the findings from the study were presented in ways that ensured that individuals cannot be identified.
Data Collection Method
The data were collected through a direct face-to-face individual interview with the participants using semi-structured probing questions. The data were collected in June 2019. The questionnaire comprised six central questions ( Table 1 ). All interviews were done in English language and audio-recorded after obtaining consent and agreement from the study participants. Eight interviews were conducted individually. Each interview lasted approximately 27–55 min. The interviewer asked follow-up inquiries to clear up individual reactions and to support elaboration as deemed appropriate.
Interview Questions.
| Interview questions guide |
Positions and Roles in the Study
The research team had four members: the lead investigator, one researcher, one research team member with managerial responsibilities of supervision of nurses, and one research supervisor directly tied to the study organization. The research team members used online meetings to track the study's progress and conclusions. All members have experience in nursing research. No repeated interviews were conducted in this study, and it is noted that no relationship between researchers and participants might influence the responses.
Pilot of Interview
Two pilot interviews were conducted before commencing the actual interviews. The pilot interview helped the researcher to get familiar with the aptitudes in interviewing and the progression of conversation.
Statistical Analysis
The collected data were transcribed and analyzed using Colaizzi's ( 1978 ) seven-step framework. The steps are (i) transcribing all the subjects’ descriptions, (ii) extracting significant statements, (iii) creating formulated meanings, (iv) aggregating formulated meanings into theme clusters, (v) developing an exhaustive description, (vi) identifying the fundamental structure of the phenomenon, and (vii) returning to participants for validation ( Edward & Welch, 2011 ). The principal investigator performed the analysis. The supervisor and the corresponding author verified the coding and themes and cross-checked for the consistency of the information.
Credibility, Dependability, Transferability, Rigor, and Trustworthiness
To ensure credibility of the data, the researcher strongly engaged with the interviews by means of observation, documentation, and taking notes. Dependability was achieved through reviews and comments on coding accuracy given by the supervisor who has full knowledge of the study design and methodology. To establish transferability, data collected from participants and the findings could be applicable to other contexts, situations, times, and populations and the study setting. The researcher adhered to rigor by carefully collecting data via audio recordings and by taking field notes. Each interview was transcribed immediately after the interview by the Principal investigator. The transcripts were given to the participants for cross-checking and approval ( Forero et al., 2018 ; Lincoln & Guba, 1986 ). As described by Stahl and King ( 2020 ), trustworthiness was established by using an unbiased approach in selecting the participants and by participant's being honest, clearly recorded and accurately presented inputs. The samples were selected purely on the basis of inclusion and exclusion criteria. No selection bias was applicable in the study.
Sample Characteristics
The demographic variables of the study participants are presented in Table 2 . There were eight study participants. Six of them were females and two were males. Age ranged from 28 to 52 years. Nurses’ OR experience varied between 8 and 23 years. All the participants had previous OR experience. The participants either had Higher Diploma in Nursing or BSN degree.
Participants’ Demographic Characteristics ( N = 8).
| Participant no. | Age | Gender | Years of experience in OR | Previous clinical experience | Highest educational level |
|---|---|---|---|---|---|
| P1 | 45 | Female | 22 | OR | BSN |
| P2 | 28 | Female | 8 | OR | BSN |
| P3 | 49 | Female | 22 | OR | Higher Diploma in Nursing |
| P4 | 33 | Male | 10 | OR | BSN |
| P5 | 31 | Female | 9 | OR | BSN, CNOR (Certified Nurse Operating Room) |
| P6 | 46 | Male | 22 | OR | BSN |
| P7 | 41 | Female | 12 | OR | BSN, CNOR, RNFA (Registered Nurse First Assistant) |
| P8 | 52 | Female | 23 | OR | BSN, CNOR, RNFA |
OR = operating room.
Research Question Results
There were a total of seven emergent themes developed from 20 theme clusters. The themes include patient safety, preoperative preparation, standardization of practice, time management, staffing appropriateness, staff education and communication, and support to the patient in the OR ( Table 3 ).
The List of the Final Theme Clusters and Emergent Themes.
| Themes cluster | Emergent themes |
|---|---|
| Patient safety | |
| Preoperative preparation | |
| Standardization of practice | |
| Time management | |
| Staffing appropriateness | |
| Staff education | |
| Communication with and support to the patients in the OR |
Theme 1: Patient Safety
After comparing the statements from all the participants, patient safety was identified as the major role of all the OR nurses. Institute of Medicine defines patient safety as “the prevention of harm to patients.” Emphasis is placed on the system of care delivery that (1) prevents errors, (2) learns from the errors that do occur, and (3) is built on a culture of safety that involves healthcare professionals, organizations, and patients ( Aspden et al., 2004 ; Clancy et al., 2005 ).
Theme Cluster: Safety Checks, Pressure Over Staff, and Nursing Responsibility for Patient Safety
The participants mentioned that the nurses should check if the patient is adequately padded to prevent contact with metal surfaces and improper positioning that causes nerve damage. Also, patients should be identified correctly.
The main thing is the skin of the patient, the skin integrity. When she wakes up, I don’t want her to get blisters because of her positioning, so nurses should make sure to check from top to toe that they are properly padded, their skin is not attached to any metal especially if they are going to use diathermy, it will cause burn if any metal is attached
rushing can lead specimen being labeled incorrectly (Participant 1)
…if you are in a rush or if you are distracted, you miss out on vital information. That could have safety implication (Participant 3)
The participants suggested that patient safety should be the main goal for nurses and nurses are responsible for promoting safety and preventing injuries.
It's very important for the patient to have someone that is paying attention to them, then you can do your other works afterward, once they have gone to sleep. You must spend that time with the patient, it's only a short period before they go off to sleep, then you can proceed with the rest of your duties (Participant 3)
Another three participants also pointed out the nursing responsibilities for patient safety especially in protecting their confidentiality and prevention of falls.
Theme Cluster: Total Time Patient Spent Under Anesthesia and Appropriate Instrument Handling
The participants pointed out that if the patient spends more time under anesthesia, it can affect the safety of patient. Staff members have to prepare everything in advance so as to avoid waiting for equipment and instruments once the patient is under anesthesia.
The more prolong the patient is under anesthesia more complication it is. So, it is also reflecting the patient safety during the intraoperative period (Participant 5)
Theme Cluster: Adherence to Universal Protocol
Majority of the participants talked about the importance of universal protocol in patient safety.
The World Health Organization created the Sign-in, the Timeout, and the Sign-out, these are separate little checklists, but all for one procedure, including various aspects of care. So you pause when you do a little checklist, then you pause again before skin incision to ensure it is the right patient for the right surgery, check any allergies again and make sure the antibiotics have been given and then at the very end we do the Sign-out. This is what we do, was there any specimens, any blood loss, any issue to report, so it is checked, check all along the way. (Participant 3)
Theme Cluster: Appropriate OR Environment
The participants highlighted the importance of appropriate OR environment in patient safety. They mentioned that the OR should be illuminated adequately and the noise should be kept minimum in order to attend to the needs of the patient.
in our laparoscopic case, it is dark inside in the OR. So, it is hard to move around to help
If the music is playing, the surgeons are also teaching some of the interns, the residents, and another surgeon, so if they are talking all at the same time with the music, you wouldn’t hear what they want at first. So, they have to repeat it again until they get mad and they will shout again so it can lead to one after the other because it is very noisy in the room (Participant 7)
Theme Cluster: Staff Familiarization With Holistic Care of Patient
Two of the participants discussed the staff familiarity with the holistic care of the patient. They described that the surgeons should not operate on patients whose health status is not familiar to them, even though it is a simple surgery.
All the staff in the room, is to be aware of the patient's status (intraoperatively) at all times, for example, hemodynamic, looking at the anesthesia monitors, ECG, pulse oximeter, etc, so the second set of eyes is always a safe practice (Participant 8)
According to the participants, the same surgeon who is operating on the patient must be the one to provide care preoperatively, intraoperatively, and postoperatively to render continuity of care.
Theme Cluster: Patient Advocacy
The participants claimed that nurses are the patient's advocates and they must speak up for the patients.
When the patient is inside the OR, we are their only advocate and we should look after them very well. Because they trusted their life to us, so have to do our best
The patients are trusting us, and we have to do the best for the patient. Nurses must advocate for the patients as they cannot speak for themselves while under anesthesia and also, they are very anxious in the OR. (Participant 1)
Theme Cluster: Hand Hygiene
Most of the participants acknowledged that hand hygiene is the fundamental concept in the prevention of infection and in promoting patient safety.
So if you don’t have proper hygiene, the patient is getting infection or the disease that he didn’t have when he came to the hospital. That means, he is getting his condition worsening if you don’t have proper hand hygiene (Participant 5)
It is like disciplining yourself to do hand hygiene because we have everything around us. We have the water, we have the sink all over, we have the solution, to do the hand hygiene. So, I think it is more on the discipline of the person on how to do it. (Participant 7)
Theme 2: Preoperative Preparation
The participants argued that the preoperative readiness of instruments, equipment, and supplies prior to wheeling the patient into OR can enhance patient safety in many ways. Preoperative preparation includes the psychologic and physiologic preparation of a patient before an operation. The preoperative period may be extremely short, as with an emergency operation, or it may encompass several weeks during which diagnostic tests, specific medications and treatments, and measures to improve the patient's general wellbeing are employed in preparation for surgery ( Turner, 2006 ).
Theme Cluster: Materials and Equipment Readiness
Almost all the participants declared the importance of materials and equipment readiness prior to wheeling the patient into OR.
Everything should be set up, the equipment in the room available, because we don’t want to delay things when the patient is already on sleep, the surgeon needs this kind of equipment, as daily task, check that all the equipment available. I don’t want to put the patient asleep without having the proper equipment. (Participant 1)
The equipment-wise, make sure that it is working well, it is not malfunctioning, and then instrument wise, make sure that our instruments are not defective, working well (Participant 7)
Theme Cluster: Preoperative Preparation Prior to Intraoperative Phase
One participant mentioned about the thorough preparation of the patient in the preoperative department prior to wheeling inside OR. The assessment should be done thoroughly to prevent complications during intraoperative period.
I don’t know how the pre-op nurses do the assessment. I think the assessment should be more thorough like sometimes they miss the patient still goes to the OR with hair clips, still with jewelry. (Participant 7)
Theme 3: Standardization of Practice
Majority of the participants highlighted that the practices should be based on the policy and protocol of the hospital. In addition, it is crucial for the safety of patients and staff. Standardization of practice refers to the creation of standard clinical processes using process management in conjunction with robust, targeted measurement, and team-based care, in which measurement informs practice and practice informs evidence and further improvement ( McGinnis et al., 2013 ).
Theme Cluster: Uniformity of Practice Within the Hospital
The participants said that everyone should practice patient care with proper understanding of the policies and procedure. The staff from different backgrounds should be trained to provide uniform care. Non-uniformity can lead to delayed treatments.
We want to be safe; we want the patient to be safe, we want to provide the best care possible, that we can give, and we want to adhere to our standards and protocols. (Participant 3)
We had a different understanding of the consent and then the consent in preparation they have different understanding too… So that will just delay the treatment, utility, and flow of services. (Participant 6)
The participants mentioned the importance of uniform practice to be legally safe and also in handling instruments and sharps.
Theme Cluster: Appropriate Workflow for Specimen Handling
One of the participants mentioned that the specimen workflow of lymphoma is confusing as it has many tests under one specimen.
I think the practices are quite safe from our side except for technical issues like may be a lot of confusion regarding the lymphoma protocol, which the system can solve it for you. The Information technology (IT) can try and solve it. People are confused because the number of tests under the lymphoma protocol keeps on changing as per the surgeon and there is no lymphoma protocol built-in epic yet here. (Participant 5)
Theme 4: Time Management
The participants enumerated the importance of time management in the OR. They emphasized that time management should be done without compromising patient safety and staff injury. Time management involves the effective planning and balancing of activities in order to promote satisfaction and health ( Turner, 2006 ).
Theme Cluster: Turnaround Time
Five out of eight participants talked about various aspects of turnaround time between two surgeries.
We are after the turnaround time. We are missing something like connection between the nurses and the patients. That could affect the safety of the patient inside OR. (Participant 7)
Another thing is time management because there are only 3 people in the OR we should be able to manage our time when to go for a break. When is a good time and it should not compromise the patient safety? (Participant 1)
Theme Cluster: Teamwork
According to the participants, teamwork is greatly encouraged as it plays a pivotal role in patient care.
I think that everyone is willing to step out of their immediate role to help someone else. For instance, the circulator is willing to help the anesthesia team if needed and vice versa. (Participant 8)
It would be helpful if the preparation nurse would bring the first patient to the room, then at least we can save time. We have more time to prepare the room instead of one person going out of the room getting this patient (Participant 6)
Theme Cluster: Instrument Reprocessing
The staff pointed the reprocessing of instruments, especially during busy days. This can prevent delays. The instruments should be fast-tracked during busy schedules.
If your institution has a lot of volume of cases and all are laparoscopy imagine if you have three rooms running and all of this have just 10 cameras, how can you deal with it? You need to fast track it every now and then. So that it is one of the responsibilities of theatre nurse to make sure to fast track it (Participant 4)
Theme 5: Staffing Appropriateness
Majority of the participants mentioned about the staffing appropriateness. They affirmed that understaffing and rushing to accomplish tasks with the available staff can place the staff at risk of injuries. Staffing appropriateness is ensuring the effective match between patient needs and nurse competencies. Appropriate staffing is clearly linked to the health of the work environment. It affects everything in the unit, including nurse performance and retention, quality of care, patient outcomes, and hospital costs ( Mitchell et al., 1989 ).
Theme Cluster: Adequacy of Staffing
The participants described, when the OR is understaffed, it can affect the overall care of patients such as it reduces the chance of nurses staying with the patient. When there are more things to accomplish, there should be additional staff provided for that OR.
I think if we have more staff at night, it won’t be a problem. We could have a thorough assessment of the patient, and we won’t be in a hurry to finish the cases. We won’t mind that case would extend little bit because there are staff doing that case at night. (Participant 7)
The policy is 2.5 nurses in the room. That should be the nursing care. Not to do computer work or some other care. But, in our practice, ideally, we must be 3 nurses in the room as we don’t have a technician to help the scrub nurse to open the stuff (Participant 5)
Although six out of eight participants talked about understaffing, just one nurse talked about organizing of booking of surgeries to save staff.
Theme Cluster: Surgeon Availability
One of the participants highlighted the presence of surgeon during preparation especially while positioning. He emphasized that they should take part in positioning the patient.
For patient safety, the surgeon should also be there in positioning the patient because they are the one who knows what position will be needed for the case. So, I think they should be really part of the positioning of the patient. (Participant 7)
Theme Cluster: Health Status of Staff
The participants felt that nurses should be fit enough to carry outpatient care. They should get adequate rest and breaks so as to function well.
First of all, I prepare myself. I go to work in good condition. So, if I am not feeling well, I will not go to work. Because I know that I can’t compromise the safety of the patient. So, I make sure that I am well. I am in a condition to go then study the procedure, analyze it and give my 100%. (Participant 4)
Research has proven that fatigue can impact patient safety, it can impact our reaction time or our concentration level. (Participant 3)
Half of the participants stressed the importance of staff fitness and rest. They said these two can affect patient safety in large proportion.
Theme 6: Staff Education
The participants urged that staff training and education can make the nurses more knowledgeable and enhance their performance. Staff education involves training to improve the performance or knowledge of the employees or workforce or a company ( Turner, 2006 ).
Theme Cluster: Staff Training
Although the majority of them pointed the staff training, one participant talked about robotic training, which should be improved to avoid chaotic situations.
I feel the Robotics area needs to be improved upon. We have some good robotically trained nurses here already, but I think the flow needs to be better, more consistent. Set up of the room should be more consistent and less chaotic (cords and equipment mismatched, etc) (Participant 8)
We do the in-service every Thursday that gives us updates with the new technologies; at the same time updated in the practice of what we should do, what should not do (Participant 6)
Among the participants who mentioned about the staff training, one of them stressed the importance of training anesthesia technicians in patient handling and another one emphasized that staff should be rotated in all specialties in order for them to be familiar in all surgeries.
Theme 7: Communication With and Support to Patient in the OR
The participants talked about the patient's overall experience during the intraoperative period as it can impact patient safety. This has two subthemes: establish a better rapport and empathy with the patient, and proper communication with the patient. Communication involves imparting or exchanging of information by speaking, writing, or using some other medium ( Merriam-Webster, 2018 ). Empathy is the action of understanding, being aware of, being sensitive to, and vicariously experiencing the feelings, thoughts, and experience of another ( Merriam-Webster, 2018 ).
Theme Cluster: Establish a Better Rapport and Empathy With the Patient
The participants affirmed the importance of establishing a better rapport with the patient during intraoperative period.
Try not to leave the patient unattended as much as possible (Participant 2)
Make sure that the patient is well padded, comfortable, putting a blanket, making sure, not exposing the patient and putting the gel pad is very important. Just think that the patient is your own relative (Participant 7)
Four out of eight participants talked about rapport and empathetic care. They urged to stay with the patients as the environment itself is scary and they do not know what to expect.
Theme Cluster: Proper Communication With the Patient
The participants explained the importance of verbal and non-verbal communication as it relieves stress and anxiety.
Try to talk to them and ask them how they are feeling, how the day is going. I think it can alleviate the anxiousness (Participant 2)
You should be making the patient relaxed, make them feel at ease. Even if there is a language barrier, use your non-verbal skills, you can touch them, or you can even just look at them, eye contact. There are always ways, you can smile, you can smile through your eyes, even though you are wearing a mask (Participant 3)
Communication with the patient was emphasized by three of the participants. They said communication has the ability to alleviate the anxiety of the patient.
Patient safety was the major theme that emerged from this study, and it showed that OR nurses play a pivotal role in intraoperative patient safety. The OR nurses consider that the intraoperative safety of patients depend on the overall intraoperative nursing care as nurses are in close proximity to patients. Also, nurses can act as advocates when the patients cannot do for themselves. These findings coincide with the result of a previous study, which points out that intraoperative nursing care creates confidence-based relationship and event-related wellbeing. It ensures persistent wellbeing and safety by keeping a watchful eye. Thus, strategies should be designed to make a safe environment that enhances wound healing, recovery, and wellbeing ( Kelvered et al., 2012 ). Moreover, frontline employees including nurses are in best position to watch and distinguish concealed preconditions that inadvertently advance from anticipated behaviors ( Graling & Sanchez, 2017 ; Gutierres et al., 2018 ).
The findings of the present study also emphasize that in all aspects of intraoperative practice, nurses have to make sure that the patient safety is the main goal and nurses are responsible for preventing injuries and promoting patient safety. Likewise, Cole et al. (2013) concluded that recognizing and correcting an inaccurate count is a basic segment of OR nurse's duty. The present study also affirmed that adherence to universal protocol is a crucial component of patient safety. Similarly, Collins et al. (2014) also declared that checklists alone cannot counteract all errors. In addition, effective comprehension of the nature of gaffes, perception of the intricate dynamic between frameworks and people, and making a just culture support a common vision of patient safety. Furthermore, the Association of periOperative Registered Nurses (AORN) recommends to articulate commitment to safety at all levels of the organization. Safety must be valued as the top priority in every healthcare organization and incentives and rewards must be provided to promote patient safety culture. In addition, AORN recognizes that the patient safety initiatives will fail in the absence of viable safety culture ( Association of periOperative Registered Nurses, 2006 ).
In the current study, the participants mentioned that everything should be set up for the surgeries including the materials and equipment in order not to delay things. These study results are in line with previous study conducted by Rose (2010) , which concluded that preoperative planning can improve surgical results and counteract unexpected issues; it improves correspondence with different individuals from the surgical team. Moreover, with insightful planning, suspensions and misperception can be effectively evaded. Additionally, Boggs et al. (2019) warrant that the hospitals are intricate frameworks and OR administration is centered on cost reduction to create efficiencies that offers value-based care, forms value control actions that support efficiencies, and improve patient access to core services. Likewise, the AORN emphasize the need for ongoing education about disinfection and sterilization techniques to improve the understanding of the improper instrument handling ( Goss, 2012 ).
The participants in our study mentioned that the instruments and equipment should be available and ready according to the specified surgery before wheeling the patient to avoid harm. Weerakkody et al. (2013) confirm that there is clear advantage in the utilization of preoperative checklist-based frameworks, by which an enormous extent of equipment-related errors can be decreased. Our study highlights that the preoperative assessment prior to intraoperative phase is vital. Consistently, Malley et al. (2015) affirm that OR nurses continually watch out for the patient and the nurses assumes a significant role in distinguishing patients’ needs and hazard factors that may influence the surgical outcome.
In the current study, almost all the participants said that the staff from different backgrounds of practice must be trained to provide uniform care to the patient. The practices must be based on policy and protocol of the hospital, and it is vital for patient and staff safety. Having an institutionalized policy that speaks the best practices is an initial move towards accomplishing patient safety ( Norton et al., 2012 ). Moreover, if the staff grasp and follow institutionalized and proficient procedures, they can counteract potential negative incidences and lead to clinical enhancements ( Shirey & Perrego, 2015 ). Standardized care at the minimum in the healthcare facility can lessen or eradicate workarounds by reaching consensus among care providers ( Gurses et al., 2012 ).
The current study suggested that uniform standards and protocol be followed by all the staff. Consistently, Brown-Brumfield and Deleon (2010) concluded that the surgical team members are in charge of utilizing every single sensible measure to secure the patient. Established guidelines, best practice proposals, and protocols are accessible and ought to be constantly pursued to diminish the probability of medication labeling mistakes and harm to the patients who depend on care provided by the nurses. Benze et al. (2021) very recently published 18 perioperative nursing scope and standards of practice that can be utilized by the nurses to follow the uniform standards of perioperative nursing practice.
The participants of the present study proclaimed that the appropriate workflow of specimen is essential and communication between surgical and laboratory team is vital for proper specimen handling. This finding is in line with the study conducted by Tracey Lee Rn (2015), which concluded that the specimen collection process depends on a human capacity, which makes it susceptible against human components and administrative impacts like time pressures. Institutionalizing a procedure, for instance, takes consistency into consideration and sets a standard by which desires for training are set.
The OR nurses in this study reported that nurses should manage their time in the workplace without compromising patient safety. They also mentioned, rushing to have quick turnaround can be injurious to staff and patients. Those findings are corroborating with findings from the literature, which concluded that the perioperative environment is one of the most challenging environment for nurses because of patient acuity, high-stress environment, production pressures, and risk of physical harm ( Morath et al., 2014 ). The participants in the study declared that complex cases cannot have 30 min of turnaround time. These findings were in line with previously described findings of Morgenegg et al. (2017) , which concluded that OR turnaround times were essentially influenced by the time of the surgical procedure, age of the patient, staffing changes, length of the surgery, and the utilization of equipment and materials requiring additional preparation time.
This study is consistent with the reviewed studies conducted on the surgical technologist's perception of teamwork and the culture of safety in the OR in Trident University International. The discoveries of the study demonstrated that teamwork had a noteworthy constructive outcome on the culture of safety. Teams with learning, specialized and non-specialized aptitudes, and safety attitudes are significant for the result of the culture of safety ( Murphy, 2018 ).
The qualitative analysis in this current study suggested that during busy schedules, fast tracking of the instruments has to be made sure to avoid any delays. This coincides with the study conducted by Weart (2014) , which concluded that the management of surgical instruments reduces the incidence of Immediate Use Steam Sterilization that is critical in the success of OR, which can positively impact patient safety goals. Improved communication and coordination between the OR and sterile processing unit must occur to bring the process under control. Understanding, managing, and improving the instrument reprocessing can have a positive impact on the safety of patients and prevents delays.
Prolonged work periods without adequate rest may contribute to diminished performance by perioperative personnel, placing both patients and workers at risk. AORN guidance statement of safe on-call practices in perioperative practice settings may assist managers and clinicians in developing policies and procedures for safe call practices ( Association of Perioperative Registered Nurses, 2005a , 2005b ).
In the current study, the participants debated that adequacy of staffing is crucial. When the OR is understaffed and there is rushing, it can affect patient safety. These findings are in line with the findings of Tørring et al. ( 2019 ) who reported that, in surgical teams, healthcare experts are exceptionally reliant and work under time pressure. It is of specific significance that collaboration is well-working so as to accomplish quality treatment and patient safety. One study also affirmed that Extreme workloads may expand patient safety dangers, and patients are adversely influenced ( Yu et al., 2019 ). The findings of Weart (2014) also affirmed that inadequate staffing can cause personnel to rush, make errors, and possibly curtail established hospital procedures. Therefore, AORN guidance statement on perioperative staffing warrants the perioperative nursing leaders to develop effective staffing plan relative to surgical patient's needs ( Association of periOperative Registered Nurses, 2005a , 2005b ).
Nurses involved in the research conveyed that the health status of the staff is vital. Nurses should be fit to work, and staff fatigue can harm the patient. This is similar to the findings of the study conducted by Seyman and Ayaz (2016) . It states that the OR can cause numerous dangers to patient and staff safety. It is suggested that in-service training on patient and staff safety issues ought to be expanded, measures ought to be taken against dangers in the OR, and the quantity of OR nurses and assistants ought to be expanded. This study agrees with the findings of Pashley (2012) who highlighted that burnout can negatively affect an individual's relationships, health, and job. If registered nurses experience burnout, incidents of sentinel events or medical errors could occur and affect patient care.
Throughout the interviews, staff training was defined clearly by most of the participants. They agreed that nurses must have adequate training related to the nursing profession, which can enhance their performance and make them more knowledgeable. These findings are in coherence with the findings of Ugur et al. (2016) , which depicts that surgical complexities on account of medical errors can be diminished when OR staff individuals are trained in patient safety. A previous quasi-experimental study conducted by Sousa et al. (2015) portray that it is the nurse's responsibility to be continuously up-to-date with scientific knowledge, and to disseminate this knowledge among their staff in order to upgrade the skills of the professionals, so that in this way, the patients can be assisted with excellence.
Theme 7: Communication With and Support to the Patient in the OR
The participants of this study explained that nurses have to communicate and establish better rapport and empathy with the patient. A study conducted by Norman et al. (2016) on “Creating healing environments through the theory of caring” declared that making a trusting association with patients enables nurses to better care for them when they are at their most susceptible condition. Building up a believing relationship can be troublesome in the perioperative care as the patient's emotional condition and nervousness levels before and after surgery vary.
Nevertheless, another study conducted on the Responsibility for patient care in perioperative practice by Blomberg et al. (2018) also declared that a typical duty in the surgical team is to take good care of and not relinquish the patient. In circumstances where patients show vulnerability about the sickness and have a need to talk before the operation, the members recounted a longing to make themselves accessible ( Kelvered et al., 2012 ). More recently, the new AORN “Guideline for team communication” provides guidance on using standardized processes and tools to improve the quality of team communication: the key points address hand overs between phases of perioperative care; a briefing to share the surgical plan; a time out to verify the correct patient, procedure, site, and side; and a debriefing to discuss what was learned and how to improve ( Link, 2018 ).
Strengths of the Study
This is the only study conducted in the United Arab Emirates to explore the understanding of the OR nurses regarding their role and responsibilities for patient care and safety in the intraoperative practice. A qualitative descriptive exploratory approach was identified as more suitable to gain insight into the participant's understanding rather than testing research idea.
Semi-structured, exhaustive interviews helped the researcher to explore the OR nurses’ understanding of their role and responsibilities for patient care and safety in intraoperative practice. The information obtained by the researcher from each nurse was of great value in terms of intraoperative patient safety. The author used several strategies to ensure methodological rigor and minimize bias such as pilot interviews, data saturation, and member checks. One of the biggest strengths of this study is the consistency of findings identified by the participants. The themes identified were mentioned by most of the participants. This gives a strong meaning to the findings.
Limitations of the Study
Being a small-scale qualitative study, this research has some limitations. The findings in the General Surgery OR may not be applicable to other OR such as Cardiology, Neurology, and Ophthalmology where the workflow varies slightly from the general surgery OR. The present study did not include surgeon, anesthesiologist, or anesthesia technicians as the aim was to explore the understanding of OR nurses regarding their role and responsibilities for intraoperative patient safety. However, these professionals could be included in studies in the future. As a novice qualitative researcher, the principal investigator had initial difficulty in the in-depth interviewing process and coding, which was guided and supported by the supervisor.
Implications for Practice
Based on these findings, as well a growing body of related literature, the nursing leadership should consider that in the study setting, despite the environment being safe and the quality of care is high, there is always room for improvement and processes. They should work on improving these aspects of care with more adaptive methods of patient safety. These study findings highlight the quality of speak-up culture of nurses when patient safety concerns arise. Speak-up culture could strengthen patient safety by guarding against mistakes and identifying and solving errors. It is imperative that nurses know and implement the most current evidence to prevent harm to patients and promote the best possible outcomes. The present study findings affirm various nursing skills for patient safety in intraoperative practice. Nurses have to possess the ability to be efficient in knowledge and skills to render safe patient care. Also, they have to work in harmony with the other members of the surgical team to deliver optimal patient safety. The findings of this study described some of the hurdles in intraoperative patient safety such as staff shortage and time pressure. If the nursing management reviews the finding, it could help to reduce the work overload and improve patient safety and quality of care.
Recommendations
The findings of this study could influence the clinical education, practice, and future research. The nursing leadership should encourage a safe environment for the patients and caregivers by establishing standardized, consistent, and measurable tools and processes to anticipate and prevent patient harm. The OR nurses should report any errors and near misses so that the OR department together with other team members could work on the aftermath of the unsafe incidences, near misses, and improve patient safety by identifying and preventing errors. Trust is the cornerstone for patient safety and quality care. Creating a culture of safety by encouraging raising concerns and being transparent is vital in intraoperative nursing care. For future research, it is recommended to apply and assess the great practices offered in this research through an intervention to improve a safe environment in the OR. Also, it is hoped that this study will provide a catalyst for future investigations and interventions that will maximize patient safety.
The issues identified by the participants in the study are directly linked to patient safety but not all are under nurse's responsibility. Also, some of the identified themes reflect the OR nurses’ understanding over other issues mainly connected to patient experience. Therefore, the aim of this study is achieved as all the themes identified as nurses were able to express their thoughts on their roles and responsibilities towards patient safety in their practice. There are opportunities for improvement based on the study findings even in a safe and high quality of care OR department. As nurses are the ones with more proximity to patients, they are in a privileged position to identify issues related to patient safety and quality of care.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Judie Arulappan https://orcid.org/0000-0003-2788-2755
- Allison J., George M. (2014). Using preoperative assessment and patient instruction to improve patient safety . AORN Journal , 99 (3), 364–375. 10.1016/j.aorn.2013.10.021 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- American College of Obstetricians and Gynecologists. (2010). Patient safety in the surgical environment. Committee opinion No. 464. American College of Obstetricians and Gynecologists . Obstetrics & Gynecology , 116 , 786–790. ISSN: 1074-861X. [ PubMed ] [ Google Scholar ]
- Aspden P., Corrigan J. M., Wolcott J., Erickson S. M. (2004). Patient safety reporting systems and applications. In Patient safety: Achieving a new standard for care . National Academies Press (US). [ PubMed ] [ Google Scholar ]
- Association of Perioperative Registered Nurses. (2006). AORN guidance statement: Creating a patient safety culture . AORN Journal , 83 ( 4 ), 936–942. 10.1016/s0001-2092(06)60012-4 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Association of Perioperative Registered Nurses. (2005b). AORN guidance statement: Perioperative staffing. Association of periOperative Registered Nurses . AORN Journal , 81 ( 5 ), 1059–1066. 10.1016/s0001-2092(06)60474-2 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Association of Perioperative Registered Nurses. (2005a). AORN guidance statement: Safe on-call practices in perioperative practice settings. Association of periOperative Registered Nurses . AORN Journal , 81 ( 5 ), 1054–1057. 10.1016/s0001-2092(06)60473-0 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Babbie E., Mouton J. (2001). The practice of social research: South African edition . Oxford University Press Southern Africa. [ Google Scholar ]
- Battié R., Steelman V. M. (2014). Accountability in nursing practice: Why it is important for patient safety . AORN Journal , 100 (5), 537--541. https://doi.org/10.1016/j.aorn.2014.08.008 [ PubMed ] [ Google Scholar ]
- Benze C., Spruce L., Groah L. (2021). Perioperative nursing: Scope and standards of practice .
- Blomberg A. C., Bisholt B., Lindwall L. (2018). Responsibility for patient care in perioperative practice . Nursing Open , 5 ( 3 ), 414–421. 10.1002/nop2.153 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Boggs S. D., Tan D. W., Watkins C. L., Tsai M. H. (2019). OR management and metrics: How it all fits together for the healthcare system . Journal of Medical Systems , 43 , 1–8. 10.1007/s10916-019-1272-y [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brown-Brumfield D., Deleon A. (2010). Adherence to a medication safety protocol: Current practice for labeling medications and solutions on the sterile field . AORN Journal , 91 ( 5 ), 610–617. 10.1016/j.aorn.2010.03.002 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Burns N., Grove S. K. (2005). Selecting a quantitative research design. The Practice of Nursing Research: Conduct, Critique, and Utilization (5th ed.). St Louis, MO: Elsevier Saunders. [ Google Scholar ]
- Clancy C. M., Farquhar M. B., Sharp B. A. C. (2005). Patient safety in nursing practice . Journal of Nursing Care Quality , 20 ( 3 ), 193–197. 10.1097/00001786-200507000-00001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Colaizzi P. F. (1978). Psychological research as the phenomenologist views it. In Vaile R., King M. (Eds.), Existential phenomenological alternatives for psychology (pp. 48–71). New York, NY: Oxford University Press. [ Google Scholar ]
- Cole K. M., Viscofsky N. A., Ebrahimi M. (2013). Finding a needle in the dark . AORN Journal , 98 ( 5 ), 532–537. 10.1016/j.aorn.2013.08.010 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Collins S. J., Newhouse R., Porter J., Talsma A. (2014). Effectiveness of the surgical safety checklist in correcting errors: A literature review applying reason’s Swiss cheese model . AORN Journal , 100 ( 1 ), 65–79. e5 [ PubMed ] [ Google Scholar ]
- Doyle L., McCabe C., Keogh B., Brady A., McCann M. (2020). An overview of the qualitative descriptive design within nursing research . Journal of Research in Nursing , 25 ( 5 ), 443–455. 10.1177/1744987119880234 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Edward K. L., Welch T. (2011). The extension of Colaizzi’s method of phenomenological enquiry . Contemporary Nurse , 39 ( 2 ), 163–171. 10.5172/conu.2011.163 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Flaubert, J. L., Le Menestrel, S., Williams, D. R., Wakefield, M. K. & National Academies of Sciences, Engineering, and Medicine. (2021). The role of nurses in improving health care access and quality. In The future of nursing 2020–2030: Charting a path to achieve health equity . National Academies Press (US). [ PubMed ] [ Google Scholar ]
- Forero R., Nahidi S., De Costa J., Mohsin M., Fitzgerald G., Gibson N.,…& Aboagye-Sarfo P. (2018). Application of four-dimension criteria to assess rigour of qualitative research in emergency medicine . BMC Health Services Research , 18 ( 1 ), 1–11. 10.1186/s12913-018-2915-2 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Goss L. K. (2012). Staying up to date on disinfection and sterilization techniques: Brush up on AORN’s recommendations for perioperative practice . Plastic and Aesthetic Nursing , 32 ( 3 ), 112–116. 10.1097/01.ORN.0000403418.74883.f8 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Graling P. R., Sanchez J. A. (2017). Learning and mindfulness: Improving perioperative patient safety . AORN Journal , 105 (3), 317–321. 10.1016/j.aorn.2017.01.006. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gurses A. P., Kim G., Martinez E. A., Marsteller J., Bauer L., Lubomski L. H., Pronovost P. J., Thompson D. (2012). Identifying and categorising patient safety hazards in cardiovascular operating rooms using an interdisciplinary approach: a multisite study . BMJ Quality & Safety , 21 ( 10 ) 810–818. 10.1136/bmjqs-2011-000625 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gutierres L. D. S., Santos J. L. G. D., Peiter C. C., Menegon F. H. A., Sebold L. F., Erdmann A. L. (2018). Good practices for patient safety in the operating room: Nurses’ recommendations . Revista brasileira de enfermagem , 71 , 2775–2782. 10.1590/0034-7167-2018-0449 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ingvarsdottir E., Halldorsdottir S. (2018). Enhancing patient safety in the operating theatre: From the perspective of experienced operating theatre nurses . Scandinavian Journal of Caring Sciences , 32 ( 2 ), 951–960. https://doi.org/10.1111/scs.12532 [ PubMed ] [ Google Scholar ]
- Kelvered M., Öhlén J., Gustafsson B. Å. (2012). Operating theatre nurses’ experience of patient-related, intraoperative nursing care . Scandinavian Journal of Caring Sciences , 26 (3), 449–457. 10.1111/j.1471-6712.2011.00947.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lee, T. (2016). Specimen labelling errors just don't cut it in the operating room/Les erreurs d'etiquetage des prelevements sont tout simplement inacceptables en salle d'operation. ORNAC Journal , 34 (3), 14–29. [ Google Scholar ]
- Lincoln Y. S., Guba E. G. (1986). But is it rigorous? Trustworthiness and authenticity in naturalistic evaluation . New Directions for Program Evaluation , 1986 ( 30 ), 73–84. 10.1002/ev.1427 [ CrossRef ] [ Google Scholar ]
- Link T. (2018). Guideline implementation: Team communication: 1.8 www.aornjournal.org/content/cme . AORN Journal , 108 ( 2 ), 165–177. 10.1002/aorn.12300 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lobelo M. I. (2004). Experiences of relapsed psychiatric patients in Mafikeng in the North-West Province . Doctoral dissertation , University of Johannesburg. [ Google Scholar ]
- Malley A., Kenner C., Kim T., Blakeney B. (2015). The role of the nurse and the preoperative assessment in patient transitions . AORN Journal , 102 ( 2 ), 181–e1. 10.1016/j.aorn.2015.06.004 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McDowell D. S., McComb S. A. (2014). Safety checklist briefings: A systematic review of the literature . AORN Journal , 99 ( 1 ), 125–137. 10.1016/j.aorn.2013.11.015 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McGarry J. R., Pope C., Green S. M. (2018). Perioperative nursing: Maintaining momentum and staying safe . Journal of Research in Nursing , 23 ( 8 ), 727–739. 10.1177/1744987118808835 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McGinnis J. M., Stuckhardt L., Saunders R., Smith M. (Eds.). (2013). Best care at lower cost: the path to continuously learning health care in America . National Academies Press (US). [ PubMed ] [ Google Scholar ]
- Merriam-Webster D. (2018). America’s Most-Trusted Online Dictionary; 2019. Available at: www. merriam-webster.com/. Accessed October, 15.
- Mitchell P. H., Armstrong S., Simpson T. F., Lentz M. (1989). American association of critical-care nurses demonstration project: Profile of excellence in critical care nursing . Heart & Lung: The Journal of Critical Care , 18 ( 3 ), 219–237 PMID: 2722533. [ PubMed ] [ Google Scholar ]
- Morath J., Filipp R., Cull M. (2014). Strategies for enhancing perioperative safety: promoting joy and meaning in the workforce . AORN Journal , 100 ( 4 ), 376–389. 10.1016/j.aorn.2014.01.027 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Morgenegg R., Heinze F., Wieferich K., Schiffer R., Stueber F., Luedi M. M., Doll D. (2017). Discrepancies between planned and actual operating room turnaround times at a large rural hospital in Germany . Sultan Qaboos University Medical Journal , 17 ( 4 ), e418. 10.18295/squmj.2017.17.04.007 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Murphy V. A. (2018). The surgical technologist’s perception of teamwork and the culture of safety in the operating room . Trident University International. [ Google Scholar ]
- Norman V., Rossillo K., Skelton K. (2016). Creating healing environments through the theory of caring . AORN Journal , 104 ( 5 ), 401–409. 10.1016/j.aorn.2016.09.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Norton E. K., Micheli A. J., Gedney J., Felkerson T. M. (2012). A nurse-led approach to developing and implementing a collaborative count policy . AORN Journal , 95 ( 2 ), 222–227. 10.1016/j.aorn.2011.11.009 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pashley H. S. (2012). Improving sharps safety and other workplace safety concerns .
- Peate I. (2015). The principles of surgical care: Intraoperative care . British Journal of Healthcare Assistants , 9 ( 11 ), 534–537. 10.12968/bjha.2015.9.11.534 [ CrossRef ] [ Google Scholar ]
- Rodziewicz T. L., Houseman B., Hipskind J. E. (2018). Medical error reduction and prevention . [ PubMed ]
- Rodziewicz T. L., Houseman B., Hipskind J. E. (2022). Medical error reduction and prevention . StatPearls; [Internet]. [ PubMed ] [ Google Scholar ]
- Rose J. (2010). Preoperative planning in orthopedic trauma: benefits and contemporary uses . Orthopedics , 33 ( 8 ) , 581–584. 10.3928/01477447-20100625-21 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rothrock J. C. (2018) Alexander’s care of the patient in surgery-E-book . Elsevier Health Sciences. [ Google Scholar ]
- Salazar Maya Á. M. (2022). Nursing care during the perioperative within the surgical context . Investigación y Educación en Enfermería , 40 ( 2 ). [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sehularo L. A., Du Plessis E., Scrooby B. (2012). Exploring the perceptions of psychiatric patients regarding marijuana use . Health SA Gesondheid , 17 ( 1 ). 10.4102/hsag.v17i1.608 [ CrossRef ] [ Google Scholar ]
- Seyman Ç., Ayaz S. (2016). Opinions of operating room nurses regarding patient and staff safety in operating room . Dicle Tıp Dergisi , 43 ( 1 ), 12–17. 10.5798/diclemedj.0921.2016.01.0630 [ CrossRef ] [ Google Scholar ]
- Shirey C., Perrego K. (2015). Standardizing the handling of surgical specimens . AORN Journal , 102 (5), 516–e1. 10.1016/j.aorn.2015.09.012 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sousa C. S., Bispo D. M., Cunha A. L. M. D., Siqueira I. L. C. P. D. (2015). Educational intervention on malignant hyperthermia with nursing professionals of the operating room . Revista da Escola de Enfermagem da USP , 49 , 0292–0297. 10.1590/S0080-623420150000200015 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stahl N. A., King J. R. (2020). Expanding approaches for research: Understanding and using trustworthiness in qualitative research . Journal of Developmental Education , 44 ( 1 ), 26–28. [ Google Scholar ]
- Taaffe, K., Lee, B., Ferrand, Y., Fredendall, L., San, D., Salgado, C.,…& S. Reeves (2018). The influence of traffic, area location, and other factors on operating room microbial load . Infection Control & Hospital Epidemiology , 39 ( 4 ), 391–397. 10.1017/ice.2017.323 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tørring B., Gittell J. H., Laursen M., Rasmussen B. S., Sørensen E. E. (2019). Communication and relationship dynamics in surgical teams in the operating room: An ethnographic study . BMC Health Services Research , 19 , 1–16. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Turner R. (2006). Collins English Dictionary . New Library World , 107 ( 1/2 ), 81–83. [ Google Scholar ]
- Ugur E., Kara S., Yildirim S., Akbal E. (2016). Medical errors and patient safety in the operating room . Age , 33 ( 6.53 ), 19–50. PMID: 27183943. [ PubMed ] [ Google Scholar ]
- Weart G. (2014). Surgical instrument reprocessing in a hospital setting analyzed with . Arizona State University. [ Google Scholar ]
- Weerakkody R. A., Cheshire N. J., Riga C., Lear R., Hamady M. S., Moorthy K., Darzi A. W., Vincent C., Bicknell C. D. (2013). Surgical technology and operating-room safety failures: A systematic review of quantitative studies . BMJ Quality & Safety , 22 ( 9 ), 710–718. 10.1136/bmjqs-2012-001778 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Williams L. S., Hopper P. D. (2015). Understanding medical surgical nursing . FA Davis. [ Google Scholar ]
- Woodman N., Walker I. (2016). World Health Organization surgical safety checklist. World Federation of Societies of Anesthesiologists . ATOTW , 325 . [ Google Scholar ]
- World Health Organization. (2017). Patient safety: making health care safer (No. WHO/HIS/SDS/2017.11). World Health Organization. [ Google Scholar ]
- Yu M. H., Lee T. T., Mills M. E. (2019). The effect of barcode technology use on pathology specimen labeling errors . AORN Journal , 109 ( 2 ) , 183–191. 10.1002/aorn.12585 [ PubMed ] [ CrossRef ] [ Google Scholar ]
An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel
Patient falls in the operating room setting: an analysis of reported safety events.
Tan J, Krishnan S, Vacanti JC, et al. Patient falls in the operating room setting: an analysis of reported safety events. J Healthc Risk Manag. 2022;42(1):9-14. doi:10.1002/jhrm.21503.
Inpatient falls are a common patient safety event and can have serious consequences . This study used hospital safety reporting system data to characterize falls in perioperative settings. Falls represented 1% of all safety reports between 2014 and 2020 and most commonly involved falls from a bed or stretcher. The author suggests strategies to identify patients at high risk for falls, improve fall-related training for healthcare personnel, and optimize equipment design in perioperative areas to prevent falls.
The nature of reported safety events related to care coordination in the operating room setting in a tertiary academic center. November 17, 2021
A contemporary analysis of closed claims related to wrong site surgery. March 29, 2023
Safety culture in the operating room: variability among perioperative healthcare workers. September 13, 2017
Optimizing Pediatric Patient Safety in the Emergency Care Setting. October 19, 2022
Qualitative content analysis: a framework for the substantive review of hospital incident reports. March 23, 2022
Implementation of the I-PASS handoff program in diverse clinical environments: a multicenter prospective effectiveness implementation study. November 16, 2022
Social risk, health inequity, and patient safety. October 5, 2022
Improving transfusion safety in the operating room with a barcode scanning system designed specifically for the surgical environment and existing electronic medical record systems: an interrupted time series analysis. September 9, 2020
Long-term effects of teamwork training on communication and teamwork climate in ambulatory reproductive health care. October 28, 2020
A failure in the medication delivery system-how disclosure and systems investigation improve patient safety. January 11, 2023
An examination of Leapfrog safety measures and Magnet designation. April 5, 2023
A description of medical malpractice claims involving advanced practice providers. July 15, 2020
The necessary leadership skillsets for the high-reliability organization framework adoption within acute healthcare organizations. March 16, 2022
Association of diagnostic stewardship for blood cultures in critically ill children with culture rates, antibiotic use, and patient outcomes: results of the Bright STAR Collaborative. May 18, 2022
The patient's "story": an examination of patient-reported safety incidents in general practice. May 4, 2022
Harnessing the power of medical malpractice data to improve patient care. January 8, 2020
New graduate registered nurses: Risk mitigation strategies to ensure safety and successful transition to practice. August 3, 2022
What can we learn from in-depth analysis of human errors resulting in diagnostic errors in the emergency department: an analysis of serious adverse event reports. May 18, 2022
Are operating room distractions, interruptions, and disruptions associated with performance and patient safety? A systematic review and meta-analysis. May 19, 2021
Electronic approaches to making sense of the text in the adverse event reporting system. September 7, 2016
National improvements in resident physician-reported patient safety after limiting first-year resident physicians' extended duration work shifts: a pooled analysis of prospective cohort studies. May 25, 2022
Leadership behaviors, attitudes and characteristics to support a culture of safety. September 28, 2022
Comparison of a voluntary safety reporting system to a global trigger tool for identifying adverse events in an oncology population. August 3, 2022
"It's a big part of being good surgeons": surgical trainees' perceptions of error recovery in the operating room. July 28, 2021
Implementing a human factors approach to RCA(2) : tools, processes and strategies. March 10, 2021
Correlation between the number of patient-reported adverse events, adverse drug events, and quality of life in older patients: an observational study. November 2, 2022
Development and usability testing of the Agency for Healthcare Research and Quality Common Formats to capture diagnostic safety events. May 25, 2022
Hemodialysis bleeding events and deaths: an 18-year retrospective analysis of patient safety and root cause analysis reports in the Veterans Health Administration. November 24, 2021
Analysis of risk factors for patient safety events occurring in the emergency department. October 7, 2020
How gender shapes interprofessional teamwork in the operating room: a qualitative secondary analysis. January 26, 2022
The challenge of competency assessment of the late-career practitioner. February 9, 2022
Do my feelings fit the diagnosis? Avoiding misdiagnoses in psychosomatic consultation services. November 3, 2021
Where should patient safety be installed? November 29, 2017
The association of acute COVID-19 infection with Patient Safety Indicator-12 events in a multisite healthcare system. May 25, 2022
Allergy safety events in healthcare: development and application of a classification schema based on retrospective review. June 15, 2022
The association of nursing home characteristics and quality with adverse events after a hospitalization. April 28, 2021
Patient-related factors associated with an increased risk of being a reported case of preventable harm in first-line health care: a case-control study March 11, 2020
Identifying boundary spanning reporter roles in patient safety events. August 24, 2022
Review of reported adverse events occurring among the homeless veteran population in the Veterans Health Administration. November 17, 2021
An analysis of the structure and content of dashboards used to monitor patient safety in the inpatient setting. December 8, 2021
Root cause analyses of reported adverse events occurring during gastrointestinal scope and tube placement procedures in the Veterans Health Association. March 25, 2020
Association of patient and family reports of hospital safety climate with language proficiency in the US. June 29, 2022
An e-Delphi study to obtain expert consensus on the level of risk associated with preventable e-prescribing events. April 13, 2022
What safety events are reported for ambulatory care? Analysis of incident reports from a patient safety organization. October 21, 2020
Filling a gap in safety metrics: development of a patient-centred framework to identify and categorise patient-reported breakdowns related to the diagnostic process in ambulatory care. October 27, 2021
Nursing implications of an early warning system implemented to reduce adverse events: a qualitative study. May 11, 2022
The presence and potential impact of psychological safety in the healthcare setting: an evidence synthesis. August 25, 2021
The effect of a system-level tiered huddle system on reporting patient safety events: an interrupted time series analysis. October 12, 2022
Anesthesia-related closed claims in free-standing ambulatory surgery centers. June 19, 2024
Analysis of patient safety risk management call data during the COVID‐19 pandemic. January 27, 2021
Implementing root cause analysis and action: integrating human factors to create strong interventions and reduce risk of patient harm. July 20, 2022
Systematic review and meta-analysis of interventions for operating room to intensive care unit handoffs. March 10, 2021
We asked the experts: the WHO Surgical Safety Checklist and the COVID-19 pandemic: recommendations for content and implementation adaptations. March 17, 2021
Effect on diagnostic accuracy of cognitive reasoning tools for the workplace setting: systematic review and meta-analysis. September 14, 2022
Nurse-reported bullying and documented adverse patient events: an exploratory study in a US Hospital. June 24, 2020
Advanced medication reconciliation: a systematic review of the impact on medication errors and adverse drug events associated with transitions of care. June 16, 2021
The burden of opioid-related adverse drug events on hospitalized previously opioid-free surgical patients. March 10, 2021
Rate of sepsis hospitalizations after misdiagnosis in adult emergency department patients: a look-forward analysis with administrative claims data using Symptom-Disease Pair Analysis of Diagnostic Error methodology in an integrated health system. May 12, 2021
Medication safety in mental health hospitals: a mixed-methods analysis of incidents reported to the National Reporting and Learning System. August 4, 2021
Distraction in the operating room: a narrative review of environmental and self-initiated distractions and their effect on anesthesia providers. December 16, 2020
Risk factors for clinically relevant deviations in patients' medication lists reported by patients in personal health records: a prospective cohort study in a hospital setting. March 2, 2022
Non-technical skills in surgery during the COVID-19 pandemic: an observational study. March 9, 2022
A handoff protocol from the cardiovascular operating room to cardiac ICU is associated with improvements in care beyond the immediate postoperative period. July 17, 2013
Reducing failure to rescue rates in a paediatric in-patient setting: a 9-year quality improvement study. November 24, 2021
Support for healthcare professionals after surgical patient safety incidents: a qualitative descriptive study in 5 teaching hospitals. May 26, 2021
Family safety reporting in hospitalized children with medical complexity. July 20, 2022
Analysis of hospital-level readmission rates and variation in adverse events among patients with pneumonia in the United States. June 22, 2022
Adverse events in infants less than 6 months of age after ambulatory surgery and diagnostic imaging requiring anesthesia. August 10, 2022
Perioperative safety determinants in ethnic patient groups. April 5, 2023
System factors affecting patient safety in the OR: an analysis of safety threats and resiliency. August 25, 2021
From fable to reality at Parkland Hospital: the impact of evidence-based design strategies on patient safety, healing, and satisfaction in an adult inpatient environment. February 10, 2021
Cybersecurity in health is an urgent patient safety concern: we can learn from existing patient safety improvement strategies to address it. April 7, 2021
Defining diagnostic error: a scoping review to assess the impact of the National Academies' report Improving Diagnosis in Health Care. May 25, 2022
The impact of the built environment on patient falls in hospital rooms: an integrative review. June 16, 2021
Teamwork before and during COVID-19: the good, the same, and the ugly…. August 24, 2022
Evolving factors in hospital safety: a systematic review and meta-analysis of hospital adverse events. September 29, 2021
Safety gaps in medical team communication: closing the loop on quality improvement efforts in the cardiac catheterization lab. June 8, 2022
Exploring changes in patient safety incidents during the COVID-19 pandemic in a Canadian regional hospital system: a retrospective time series analysis. February 23, 2022
Room of hazards: a comparison of differences in safety hazard recognition among various hospital-based healthcare professionals and trainees in a simulated patient room. July 27, 2022
Association of implementation and social network factors with patient safety culture in medical homes: a coincidence analysis. September 2, 2020
The randomized AMBORA trial: impact of pharmacological/pharmaceutical care on medication safety and patient-reported outcomes during treatment with new oral anticancer agents. April 21, 2021
Cost of inpatient falls and cost-benefit analysis of implementation of an evidence-based fall prevention program. February 1, 2023
Implementing the clinical occurrence reporting and learning system: a double-loop learning incident reporting system in long-term care. March 24, 2021
Patient perspectives on the usefulness of an artificial intelligence-assisted symptom checker: cross-sectional survey study. March 11, 2020
Root cause analysis of adverse events involving opioid overdoses in the Veterans Health Administration. June 23, 2021
Medication adverse events in the ambulatory setting: a mixed-methods analysis. October 26, 2022
Burnout and its relationship to self-reported quality of patient care and adverse events during COVID-19: a cross-sectional online survey among nurses. June 9, 2021
Rates of adverse events in hospitalized patients after summer-time resident changeover in the United States: is there a July effect? August 25, 2021
Clarifying radiology's role in safety events: a 5-year retrospective common cause analysis of safety events at a pediatric hospital. September 2, 2020
Analysis of suicides reported as adverse events in psychiatry resulted in nine quality improvement initiatives. July 21, 2021
Factors associated with workplace violence among healthcare workers in an academic medical center. April 27, 2022
Associations of workflow disruptions in the operating room with surgical outcomes: a systematic review and narrative synthesis. June 17, 2020
The physiology of failure: identifying risk factors for mortality in emergency general surgery patients using a regional health system integrated electronic medical record. September 7, 2022
Coping with errors in the operating room: intraoperative strategies, postoperative strategies, and sex differences. September 22, 2021
Peer support by interprofessional health care providers in aftermath of patient safety incidents: a cross-sectional study. June 9, 2021
Interprofessional team collaboration and work environment health in 68 US intensive care units. November 30, 2022
The costs associated with adverse drug events among older adults in the ambulatory setting. December 7, 2005
Patient safety trends in 2021: an analysis of 288,882 serious events and incidents from the nation’s largest event reporting database. July 6, 2022
Impact of a nationwide prospective drug utilization review program to improve prescribing safety of potentially inappropriate medications in older adults: an interrupted time series with segmented regression analysis. November 4, 2020
Performance variability in perioperative sentinel events: report on a nationwide data set. April 20, 2022
Patient falls in the operating room: why is this still a problem in 2024? July 24, 2024
Grading recommendations for enhanced patient safety in sentinel event analysis: the recommendation improvement matrix. June 12, 2024
WebM&M Cases
Reducing retained foreign objects in the operating room: a quality improvement initiative. December 20, 2023
Perceptions of use of names, recognition of roles, and teamwork after labeling surgical caps. December 6, 2023
Anesthesia workspaces for safe medication practices: design guidelines. November 15, 2023
Facilitators and barriers to the implementation of surgical safety checklist (SSC): an integrative review. November 15, 2023
Beyond the surgical safety checklist: using intraoperative handoff to facilitate team situation awareness in the OR. October 25, 2023
CheckPOINT: a simple tool to measure Surgical Safety Checklist implementation fidelity. October 18, 2023
Surgeons' leadership style and team behavior in the hybrid operating room: prospective cohort study. October 4, 2023
Standardization and visualization of the surgical time-out. October 4, 2023
Fire safety in the operating room. October 1, 2023
International perspectives on modifications to the surgical safety checklist. June 21, 2023
Evaluation of detected medication errors within the operating room at an academic medical center. June 21, 2023
The good, the bad, and the ugly: operative staff perspectives of surgeon coping with intraoperative errors. June 14, 2023
Use of technology to improve the adherence to surgical safety checklists in the operating room. May 31, 2023
Proactive patient safety: focusing on what goes right in the perioperative environment. May 24, 2023
Clinicians' perspectives on proactive patient safety behaviors in the perioperative environment. April 26, 2023
Normalization of deviance is contrary to the principles of high reliability. April 12, 2023
Distractions in the operating room: a survey of the healthcare team. April 5, 2023
Surgical fire in the United States: 2000-2020. March 15, 2023
Compliance with and barriers to implementing the surgical safety checklist: a mixed-methods study. March 8, 2023
Human factors in anaesthesia: a narrative review. February 15, 2023
Persisting high rates of omissions during anesthesia induction are decreased by utilization of a pre- & post-induction checklist. February 1, 2023

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.
- Open access
- Published: 09 August 2024
Virus and viral components transmitted through surgical smoke; a silent danger in operating room: a systematic review
- Bahareh Mahdood ORCID: orcid.org/0000-0002-7774-2294 1 ,
- Amirmohammad Merajikhah ORCID: orcid.org/0000-0003-0249-4975 2 ,
- Mina Mirzaiee ORCID: orcid.org/0000-0003-1296-6040 3 ,
- Maryam Bastami ORCID: orcid.org/0000-0001-5163-217X 4 &
- Sara Banoueizadeh ORCID: orcid.org/0000-0002-0898-0010 3
BMC Surgery volume 24 , Article number: 227 ( 2024 ) Cite this article
Metrics details
During surgical procedures, heat-generating devices are widely used producing surgical smoke (SS). Since the SS can transmit infectious viruses, this systematic review was designed to investigate the potential viruses transmitted through SS.
PubMed, Scopus, Web of Science, ProQuest, and Embase databases, along with Cochran Library, and Google Scholar search engine were searched systematically (by April 21, 2024). No language, place, and time restrictions were considered. All studies evaluating the SS and virus transmission, and whole investigations regarding the viral infections transmitted through SS were totally considered inclusion criteria. Besides, non-original, qualitative, case reports, case series, letters to the editor, editorial, and review studies were excluded from the analysis. This study was conducted in accordance with the PRISMA 2020 statement.
Twenty-six eligible studies were selected and reviewed for data extraction. The results showed that the SS contains virus and associated components. Six types of viruses or viral components were identified in SS including papillomavirus (HPV, BPV), Human Immunodeficiency Virus (HIV), varicella zoster, Hepatitis B (HBV), SARS-CoV-2, and Oral poliovirus (OPV), which are spread to surgical team through smoke-producing devices.
Conclusions
Since the studies confirm the presence of viruses, and viral components in SS, the potential risk to the healthcare workers, especially in operating room (OR), seems possible. Thus, the adoption of protective strategies against SS is critical. Despite the use of personal protective equipment (PPE), these viruses could affect OR personnel in surgical procedures.
Peer Review reports
Introduction
Following the progress of surgical procedures, several energy-generated devices are utilized in ORs [ 1 , 2 ]. Electrocautery is the most common heat-generating device that hires high-frequency electric current to cut or coagulate tissues [ 3 ]. Todays, electrocautery, laser, and ultrasonic scalpel are widely recognized as important advances in surgical procedures. It is increasingly used for tissue cutting, hemostasis [ 4 , 5 , 6 ], surgical cutting, and tissue separation. Also, laser, ultrasonic scalpel, and electrocautery are used for coagulation of small blood vessels. The main feature of these techniques is the induction of high temperatures causing the burn and rupture of cell membranes and other structures of tissue [ 7 ]. SS is a byproduct of bioaerosols produced by energy devices during cutting or coagulation which contains a lot of dangerous components [ 1 , 8 ]. SS is comprised of 95% of water vapor and 5% of particulate matter active viruses [ 9 ] identified as potential hazards for surgical room staff [ 10 , 11 ]. Inhalation of surgical fumes could be dangerous for the patient and all members of the surgical team, OR nurses, physicians, and surgical technologists [ 12 ]. Small inhalable components are discovered in SS. SS also includes several gaseous particulates with the potential of cancer induction. Evidences show that daily inhaled SS particles is equivalent to smoking ten cigarettes [ 13 ]. The smoke of the particles is not visible and the smell is unpleasant [ 12 ]. Many types of viruses have been detected in SS which are produced in different surgical procedures [ 13 ]. Some studies confirmed the transmission of various viruses through SS [ 14 , 15 , 16 ]. SS is created with or without during a heating procedure, including bioaerosols with living and non-living cellular materials, which subsequently induce the risk of infection with the virus, and lung irritation, leading to acute and chronic inflammatory changes. [ 17 , 18 ].
Garden et al. showed that HPV can be identified from SS in dioxide lasers during gynecological procedures [ 19 ]. Also, Zhou et al. (2019) approved the presence of DNA of human papilloma available in SS which can be transferred from patients to the members of surgical team [ 20 ]. Also, Parker et al. reported that a gynecological surgeon was infected with HPV through SS. [ 21 ] Surgical personnel are exposed to these chemicals for an average of 7 h per day, 5 days per week, and throughout the period of several years [ 22 ] and smoke production during surgical procedures is unavoidable [ 23 ]. Although SS can induce unavoidable side effects for the surgical team as well as the patients, these side effects are not fully discovered. One of these complications is the transmission of viruses through SS. Since the surgical team members may not be aware of this risk, they are more vulnerable. In the meantime, it should be noted that the utilization of PPE supply is not sufficient safety against SS [ 17 ]. Also, the personnel widely use surgical masks, which are ineffective in protecting against the effects of SS [ 24 ]. As a result, it is necessary to be aware of viruses transmitted through SS and to adopt methods preventing the transmission of infection in this regard.
Materials and methods
Data collection.
The PRISMA flowchart and the associated checklist were utilized to assess and identify the types of viruses transmitted through SS [ 25 ].
Search strategy
The related studies were searched using PubMed, Scopus, Web of Science, ProQuest, Embase, Cochran Library and Google Scholar search engine. The studies were compiled by April 21, 2024, with no language, place and time limitation. The search was applied using the keywords of (surgical smoke) OR (surgical plume) OR (aerosol) AND (electrocautery) OR (diathermy) OR (laser) OR (scalpel harmonic) AND (viral infection) OR (Virus) AND (Complications) AND (DNA) OR (DNA transmission) OR (RNA) OR (RNA transmission).
To conduct the search protocol, two authors initially reviewed the sources of qualified article reports and subsequently evaluated the Abstracts and Titles of the identified articles. 1126 duplicate articles were found and merged. Unrelated and non-original articles were excluded from the study. The related data, device, type of article, surgical procedure, and viral type were identified using separate authors.
Inclusion and exclusion criteria
Inclusion criteria were the studies regarding the expression of SS and virus transmission and the investigations about viral infections transmitted through SS. Non-original, qualitative, case report, case series, letters to the editor, editorial and review studies were excluded from the analysis. Also, the studies with no report of the presence of any viral components in SS were excluded.
Data extraction
Article selection process was conducted by two researchers (BM, MM), independently. In case of disagreement, the third author (AM) was responsible for final agreement. For the data extraction process, an electronic datasheet including the year of publication, first author`s name, study design, device, and viral component was used.
Quality assessment
Based on the guidelines provided by the Newcastle and Ottawa declarations, the methodological quality of the articles was evaluated [ 26 ]. In this guideline, a confirmed framework for quality assessment of the articles is used. In this guideline, criteria were considered for the selection of study subjects, comparison, exposure, and their results, and a maximum of 9 stars were assigned to each study. Studies > 7 stars were classified as high quality and studies < 6 stars had low quality. In order to avoid probable bias, the results of the study were independently checked by two researchers. In case of disagreement, the authors resolved it with negotiation. This approach provided a complete assessment of possible bias in the results.
SS is frequently inhaled by surgical team members in OR. The particles in this smoke can be dangerous for healthcare workers and may contain pathogenic microorganisms. Thus, the present study examined the viruses transmitted through SS. In the initial search, 4341 articles were found in PubMed, Scopus, Web of Science, ProQuest, Embase, Cochran Library, and Google Scholar. These studies were compiled by April 21, 2024. Following the paper checking by Endnote software (v.8x), 1126 duplicate articles were detected. By examination of the Titles and Abstracts, 3001 records were removed and 214 articles remained for full-text study. In the next step, 188 full-text articles were removed and 26 full-text articles were reviewed, based on the inclusion/exclusion criteria. The remaining 26 articles included 5 clinical trials, 4 prospective studies, 15 in vitro-in vivo-ex vivo, and 2 descriptive studies (Fig. 1 and Table 1 ).

Flow diagram of the study selection for the review process
The results showed that the SS contains the virus and associated components. Finally, 26 eligible studies were reviewed. Six types of viruses and the associated components were identified including Human papillomavirus (HPV), Human Immunodeficiency Virus (HIV), Hepatitis B (HBV), SARS-CoV-2, Oral poliovirus (OPV), and varicella-zoster which are spread through smoke-producing devices (Table 1 ).
Eleven studies approved the presence of papillomavirus in SS. Also, 7 investigations of SARS-CoV-2, 3 studies of HBV, 2 studies of HIV, and 1 study for OPV and varicella-zoster were identified. Also, 1 study reported no identified virus. The use of heat-generating devices in surgeries causes SS, and according to the analyses, some types of viruses were found in SS.
The results of this systematic review verified the viruses and viral components transmitted through SS. Since electrosurgical devices are commonly used in operations globally, the SS is considered a health risk. Smoke-generating devices include Electrocautery and Electrosurgery, Ultrasonic Ablation, High-speed Burs, Drills, Saws, Lasers, and Harmonic scalpels. Among these devices, electrocautery is the most common tool used in OR, which is considered an essential tool in modern surgeries in all ORs [ 24 , 43 , 44 ]. Approximately, 500,000 healthcare providers (such as surgeons, nurses, anesthesiologists, and technicians) are exposed to SS in ORs per year [ 45 ]. Several studies reported the presence of viral genomes in SS [ 30 , 31 , 46 ]. Also, some articles showed the existence of virus DNA in SS [ 19 , 32 ].
Our study revealed 6 types of viruses and viral components in SS.
Papillomavirus
HPV and bovine papillomavirus (BPV) can be spread in the air through SS leading to human diseases. However, according to several papers, HPV is not found in SS and the SS infection threat is low levels or impossible [ 47 , 48 ]. Also, recent studies approved the presence of HPV in SS [ 20 , 39 ]. On the other hand, Xiaoli Hu et al. indicated that gynecologists using electrosurgery such as LEEP are at risk of HPV infection [ 39 ]. According to a case report, a 66-year-old gynecologist with the experience in approximately 500 electrosurgical procedures was reported for HPV-related cervical dysplasia and vulvar lesions over a 40-year period. [ 21 ].
Surgical face masks, particularly the N95, reduce the hazard of HPV transmission. On the other hand, gynecologists and surgical technologists are at risk of this disease. Stefano Palma et al.'s study also confirmed the spread of this virus following the application of LEEP and CO2 laser. Also, this study reported the cases of upper airway neoplasms due to HPV transmission through SS [ 49 ]. DNA of papillomavirus has been identified from laser plumes from papilloma lesions, and nasal papilloma is detected to develop in the noses of OR staff and physicians exposed to laser smoke [ 19 ].
Since this virus is very contagious and prevalent leading to benign dermatological and anogenital warts, oropharyngeal and laryngobronchial lesions, cervical cancer, mouth, and laryngeal cancer, depending on the genotype of the virus. Although the transmission of this virus is applied mainly through intercourse, recent studies confirmed the SS as a transmission route [ 39 , 50 ].
William S. Sawchuk et al. reported the spread of papillomavirus DNA from carbon dioxide laser smoke and tissue coagulation in leg biopsy resection surgery [ 32 ]. Because this virus has different genotypes, the dangerous genotypes in SS can increase the risk of developing malignant cancers in healthcare workers. Transmission of this virus with SS is more common in gynecological procedures than in other surgeries.
The utilization of electrocautery and laser by gynecologists is a prominent step in cervical and ovarian cancer surgeries; especially, the LEEP which is used for treatment of precancerous lesions due to the HPV infection causing a critical issue due to the SS produced by these devices. This smoke has many potential risks to gynecologists. Linzhi Yan's study showed that the SS produced during cervical cancer surgery contains HPV with cytotoxicity and infectivity in laboratory conditions [ 34 ]. Another case was a 64-year-old gynecologist who was infected by HPV. He performed 250 electrosurgical surgeries for HPV-associated cervical dysplasia and vulvar lesions over a 27-year [ 21 ].
Based on the transmission of this type of virus through SS, it is necessary to prevent smoke inhalation and contracting this disease for all healthcare workers exposed to SS. The use of masks, especially N95 and Gardasil vaccination for prevention of this disease seems essential for surgical staff.
SARS-CoV-2 virus
In early December 2019, a case of pneumonia with unknown origin was identified in Wuhan, China [ 51 , 52 ]. The causative pathogen was a novel beta-coronavirus with capsular RNA, named Coronavirus 2, which is phylogenetically similar to SARS-CoV [ 52 , 53 ]. SARS-CoV-2 is highly contagious which affects the respiratory system, causing fever, sore throat, cough, chest and muscle pain, Dyspnea, anosmia, headache, confusion, and ageusia [ 54 , 55 , 56 ]. These complications cause life-threatening respiratory failure, as well as affect the heart, kidneys, liver, and nervous system. In addition to the involvement of respiratory system, this virus affects the gastrointestinal system from the mouth to the rectum, blood, saliva, urine, and probably the liver in infected individuals [ 57 , 58 , 59 , 60 ]. Although this virus spreads through the aerosols in air, our findings showed that it is also transmitted by SS.
Bogani et al. confirmed that this virus could be transmitted through SS and aerosolized fluid from the abdominal cavity through the SS from monopolar electrosurgical units in women's laparoscopic procedures [ 28 ]. On the other hand, evidence showed that SS could transfer this virus [ 29 , 50 ].
In his study, Takuya Yokoe collected SS with a vacuum pump and analyzed it for the presence of SARS-CoV-2 virus RNA. The results of this study showed that human coronavirus RNA is present in SS generated by cutting infectious tissue using an ultrasonic scalpel [ 14 ]. Also, Andrade et al. approved the risk of COVID-19 infection for surgical teams in the OR due to long-term exposure to SS [ 27 ].
Weissleder et al. showed that sputum and feces from patients infected with SARS-CoV-2 individuals include viral RNA [ 61 ]. Thus, incisions made on the intestinal and upper respiratory tract can generate SS containing viral components. Evidence also showed that the risk of active virus transmission through SS is higher in laparoscopic surgeries [ 62 ]. Coccolini et al. stated that peritoneal fluid can contain SARS-CoV-2 [ 63 ]. Other studies confirmed the presence of this virus in SS aerosols from laparoscopic surgeries [ 28 , 42 ]. Following the presentation of COVID-19 vaccines, this disease was controlled, however, it is observed in different parts of the world. Thus, more preventive strategies should be adopted in ORs despite vaccination [ 64 ].
HBV infection is an international health threat, and 2.57 billion people worldwide are affected by HBV. The estimated annual mortality of hepatitis B is more than 780,000 [ 65 , 66 , 67 , 68 ]. Hepatitis B virus is transmitted through direct contact with infected blood and aerosol form. Our study confirms the existence of the hepatitis B virus in SS.
Han Deok Kwak et al. identified the HBV in SS from electrosurgery in robotic or laparoscopic colorectal resection, laparoscopic gastrectomy, and laparoscopic hepatic wedge resections [ 31 ]. This dangerous virus leads to a comprehensive range of hepatic pathologies from acute diseases (including severe liver failure) to chronic hepatitis, cirrhosis, and hepatocellular carcinoma. Although vaccination of healthcare workers with hepatitis B vaccine can effectively prevent this disease, the reduction of antibody titer below the required level of immunogenicity can threaten them. Thus, it is recommended to periodically check the antibody titer in all at risk personnel.
Vourtzoumis et al. reported that HBV exists in SS during laparoscopic procedures in patients [ 57 ]. However, these types of studies reporting the presence of HBV are rare. Acute HBV infection can be asymptomatic or with symptomatic acute hepatitis [ 69 , 70 ]. Thus, some strategies must be adopted to reduce the risk of the virus in health workers.
Our study confirms the existence of HIV in SS. Human immunodeficiency virus, the cause of AIDS (Acquired immunodeficiency syndrome), is responsible for the most common epidemic in humans [ 71 , 72 ]. HIV attacks the immunological system and suppresses the potential activity. This virus is transmitted through intercourse, exposure to infected blood or tissue, and from mother to fetus during pregnancy, childbirth, or breastfeeding. However, the transmission of this virus through SS is discussed.
Although there are a few studies regarding the dangerous condition, the evidence show that HIV is present in the SS from electrocautery causing associated infection [ 30 ]. Also, in a laboratory study, Baggish et al. showed that HIV proviral DNA was found in SS produced by CO2 laser [ 73 ]. Although epidemiological data regarding the prevalence of HIV infection in different populations show that transmission through aerosols is not common [ 74 , 75 , 76 ], the risk of transmission through SS remains a threat to the health of medical personnel. The incubation period of this disease is long-term which can increase the risk of transmission of this type of virus. Because the patient represents no signs during the incubation period, the patient is unaware of the existence of the disease.
HIV virus diagnostic test is not performed prior to all surgical procedures. Thus, the healthcare workers must be aware of this dangerous condition. Other evidence also found the existence of HIV DNA and RNA in SS. Since this virus leads to immunodeficiency as a life-threatening agent, the recognition of the routes of virus transmission is crucial.
Poliomyelitis is caused by the poliovirus. Polio is a gastrointestinal disease, mostly with an oral-fecal transmission route. Besides, pharyngeal droplet secretion is also considered another route of virus transmission. Polio virus enters the body through the mouth, then passes through the digestive system tract, and is finally eliminated by feces and oral secretions in several weeks. Viremia occurs following initial multiplication. In the absence of proper immunity and neutralization, the virus may reach the secondary organs, including the central nervous system. In these organs, the multiplication can lead to the destruction of motor neurons and paralysis [ 77 ].
Taravella et al. observed the existence of poliovirus in SS created by excimer laser tissue ablation. Oral poliovirus as an RNA-based virus has no lipid envelope. This characteristic in comparison with other viruses (such as herpes) makes it safe from the heat generated by the excimer laser [ 35 ]. Since the OPV is mostly rare due to the existence of a vaccine and the awareness of the associated problems, the potential risks are prevented.
Varicella zoster
Varicella zoster virus (VZV) causes primary infection (varicella or chicken pox) followed by delayed onset of sensory ganglia. The virus can reactivate and cause herpes zoster (HZ, shingles) leading to considerable complications such as death, in rare cases [ 78 ]. Following the ablation of human fetal lung fibroblasts infected with attenuated varicella-zoster virus by an excimer laser, Taravella et al. concluded that varicella-zoster DNA is found in laser smoke [ 41 ]. Since there are a few studies investigating the presence of this virus or its genetic material in SS, more studies are needed to confirm this issue.
Since the identification of viral DNA in SS is a challenging process, further researches regarding the number of viruses present and their transmissibility are needed.
In the present study, all aspects of transmission of viruses, DNA, and its viral contents were systematically exhibited. Potentially, the risk of transmission seems probable, but there are a few diagnosed cases of HPV infection. This systematic review showed that only HPV infections among healthcare workers are recorded so far; however, the risk of contraction of other viruses cannot be ignored. Many in-vitro/vivo studies identified the associated risk. According to the fact that there is a strict need for more clinical research on other viruses, preventive measures should be applied in ORs.
How to protect yourself against SS?
Safety is an important content in health procedures [ 79 ]. Although general room ventilation (GRV) with positive pressure can reduce the concentration of SS, it is not enough to absorb the pollutants produced by SS. In order to protect the OR staff, surgeons, and other treatment staff from possible dangers of SS, the local exhaust ventilation (LEV) can be used in addition to the GRV in the OR. Two main methods of LEV which can reduce the smoke for surgical team members are portable SS extraction devices and OR suction systems. The SS vacuum should contain the speed of 100–150 feet/minute and the filter should be HEPA (high-efficiency particulate air) or more powerful. These filters must be changed regularly and destroyed along with infectious waste [ 24 ]. Surgical room suction systems exhaust smoke at a slower rate. However the use of a smoke-evacuator pencil cautery or an attentive assistant with handheld suction can reduce SS to a greater extent [ 80 ].
In addition, the use of highly protective masks (such as N95, N99, N100, P95, P99, P100, R95, R99, and R100) is recommended [ 81 , 82 ]. Also, one of the most important solutions to control SS is the continuous training of all members of the surgical team regarding the risks and ways to reduce and eliminate SS [ 83 ]. Safety and quality are considerable matters while providing healthcare services.
Utilization of SS-generating devices in surgical procedures is unavoidable. This smoke can threaten the surgical and anesthesia team and even the patients. OR staff are always exposed to SS. This is a chemical and biological hazard. Our research showed that this smoke can contain viruses and non-disease viral components. Some of these viruses can even be considered a threat to a person's life. Educational strategies are crucial to prevent the transmission of infection to healthcare workers through SS. The application of suitable and sufficient PPE can effectively avoid transmission of the virus through SS.
Availability of data and materials
This published article includes all data generated or analyzed during the study.
Zhou YZ, Wang CQ, Zhou MH, Li ZY, Chen D, Lian AL, et al. Surgical smoke: A hidden killer in the operating room. Asian J Surg. 2023;46(9):3447–54.
Article PubMed Google Scholar
Sinha UK, Gallagher LA. Effects of steel scalpel, ultrasonic scalpel, CO2 laser, and monopolar and bipolar electrosurgery on wound healing in guinea pig oral mucosa. Laryngoscope. 2003;113(2):228–36.
Ulmer B. Report of OSHA’s draft: information for health care workers exposed to laser and electrosurgery smoke. Todays Surg Nurse. 1999;21(2):18–9.
CAS PubMed Google Scholar
Bigony L. Risks associated with exposure to surgical smoke plume: a review of the literature. AORN J. 2007;86(6):1013–24.
Massarweh NN, Cosgriff N, Slakey DP. Electrosurgery: history, principles, and current and future uses. J Am Coll Surg. 2006;202(3):520–30.
Bolliger CT, Sutedja TG, Strausz J, Freitag L. Therapeutic bronchoscopy with immediate effect: laser, electrocautery, argon plasma coagulation and stents. Eur Respir J. 2006;27(6):1258–71.
Article CAS PubMed Google Scholar
Ragde SF, Jørgensen RB, Føreland S. Characterisation of exposure to ultrafine particles from surgical smoke by use of a fast mobility particle sizer. Ann Occup Hyg. 2016;60(7):860–74.
Zakka K, Erridge S, Chidambaram S, Beatty JW, Kynoch M, Kinross J, et al. Electrocautery, Diathermy, and Surgical Energy Devices: Are Surgical Teams at Risk During the COVID-19 Pandemic? Ann Surg. 2020;272(3):e257–62.
Lewin JM, Brauer JA, Ostad A. Surgical smoke and the dermatologist. J Am Acad Dermatol. 2011;65(3):636–41.
Steege AL, Boiano JM, Sweeney MH. Secondhand smoke in the operating room? Precautionary practices lacking for surgical smoke. Am J Ind Med. 2016;59(11):1020–31.
Article PubMed PubMed Central Google Scholar
Garbey M, Joerger G, Furr S. A Systems Approach to Assess Transport and Diffusion of Hazardous Airborne Particles in a Large Surgical Suite: Potential Impacts on Viral Airborne Transmission. Int J Environ Res Public Health. 2020;17(15):5404.
CDC. Strategies for Optimizing the Supply of N95 Respirators: CDC; 2020 [Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/index.html ].
Limchantra IV, Fong Y, Melstrom KA. Surgical Smoke Exposure in Operating Room Personnel: A Review. JAMA Surg. 2019;154(10):960–7.
Yokoe T, Kita M, Odaka T, Fujisawa J, Hisamatsu Y, Okada H. Detection of human coronavirus RNA in surgical smoke generated by surgical devices. J Hosp Infect. 2021;117:89–95.
Article CAS PubMed PubMed Central Google Scholar
Chapman LW, Korta DZ, Lee PK, Linden KG. Awareness of surgical smoke risks and assessment of safety practices during electrosurgery among us dermatology residents. JAMA Dermatol. 2017;153(5):467–8.
Neumann K, Cavalar M, Rody A, Friemert L, Beyer DA. Is surgical plume developing during routine LEEPs contaminated with high-risk HPV? A pilot series of experiments. Arch Gynecol Obstet. 2018;297(2):421–4.
Alp E, Bijl D, Bleichrodt RP, Hansson B, Voss A. Surgical smoke and infection control. J Hosp Infect. 2006;62(1):1–5.
Gollakota AR, Gautam S, Santosh M, Sudan HA, Gandhi R, Jebadurai VS, et al. Bioaerosols: characterization, pathways, sampling strategies, and challenges to geo-environment and health. Gondwana Res. 2021;99:178–203.
Article Google Scholar
Garden JM, O’Banion MK, Shelnitz LS, Pinski KS, Bakus AD, Reichmann ME, et al. Papillomavirus in the Vapor of Carbon Dioxide Laser-Treated Verrucae. JAMA. 1988;259(8):1199–202.
Zhou Q, Hu X, Zhou J, Zhao M, Zhu X, Zhu X. Human papillomavirus DNA in surgical smoke during cervical loop electrosurgical excision procedures and its impact on the surgeon. Cancer Manag and Res. 2019;11:3643–54.
Article CAS Google Scholar
Parker J, Clark J. HPV positive oropharyngeal cancer in two gynaecologists exposed to electrosurgical smoke plume. Obstet Gynecol Cases Rev. 2021;8:205.
Google Scholar
Dobrogowski M, Wesolowski W, Kucharska M, Paduszynska K, Dworzynska A, Szymczak W, et al. Health risk to medical personnel of surgical smoke produced during laparoscopic surgery. Int J Occup Med Environ Health. 2015;28(5):831–40.
Choi SH, Choi DH, Kang DH, Ha YS, Lee JN, Kim BS, et al. Activated carbon fiber filters could reduce the risk of surgical smoke exposure during laparoscopic surgery: application of volatile organic compounds. Surg Endosc. 2018;32(10):4290–8.
Ilce A, Yuzden GE, Yavuzvan Giersbergen M. The examination of problems experienced by nurses and doctors associated with exposure to surgical smoke and the necessary precautions. J Clin Nurs. 2017;26(11–12):1555–61.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000.
Andrade WP, Gonçalves GG, Medeiros LC, Araujo DCM, Pereira GTG, Moraes DMP, Spencer RMSSB. Low-cost, safe, and effective smoke evacuation device for surgical procedures in the COVID-19 age. J Surg Oncol. 2020;122(5):844-7. https://doi.org/10.1002/jso.26133 .
Bogani G, Ditto A, De Cecco L, Lopez S, Guerrisi R, Piccioni F, Micali A, Daidone MG, Raspagliesi F. Transmission of SARS-CoV-2 in Surgical Smoke during Laparoscopy: A Prospective, Proof-of-concept Study. J Minim Invasive Gynecol. 2021;28(8):1519-25. https://doi.org/10.1016/j.jmig.2020.12.026 .
Garbey M, Joerger G, Furr S. A systems approach to assess transport and diffusion of hazardous airborne particles in a large surgical suite: potential impacts on viral airborne transmission. Int J Environ Res Public Health. 2020;17(15):5404.
Johnson GK, Robinson WS. Human immunodeficiency virus-1 (HIV-1) in the vapors of surgical power instruments. J Med Virol. 1991;33(1):47–50.
Kwak HD, Kim SH, Seo YS, Song KJ. Detecting hepatitis B virus in surgical smoke emitted during laparoscopic surgery. Occup Environ Med. 2016;73(12):857–63.
PubMed Google Scholar
Sawchuk WS, Weber PJ, Lowy DR, Dzubow LM. Infectious papillomavirus in the vapor of warts treated with carbon dioxide laser or electrocoagulation: detection and protection. J Am Acad Dermatol. 1989;21(1):41–9.
Wisniewski PM, Warhol MJ, Rando RF, Sedlacek TV, Kemp JE, Fisher JC. Studies on the transmission of viral disease via the CO2 laser plume and ejecta. J Reprod Med. 1990;35(12):1117–23.
Yan L, Liu Y, Zhang J, Chen X, Li J, Zhu X. In vivo and in vitro study of the potential hazards of surgical smoke during cervical cancer treatment with an ultrasonic scalpel. Gynecol Oncol. 2022;164(3):587–95.
Taravella MJ, Weinberg A, May M, Stepp P. Live virus survives excimer laser ablation. Ophthalmology. 1999;106(8):1498–9.
Garden JM, O’Banion MK, Bakus AD, Olson C. Viral disease transmitted by laser-generated plume (aerosol). Arch Dermatol. 2002;138(10):1303–7.
Cizmic A, Eichel VM, Weidner NM, Wise PA, Müller F, Rompen IF, et al. Viral load of SARS-CoV-2 in surgical smoke in minimally invasive and open surgery: a single-center prospective clinical trial. Sci Rep. 2023;13(1):20299.
Hirota M, Takahashi H, Miyazaki Y, Takahashi T, Kurokawa Y, Yamasaki M, et al. Surgical plume from tissue infected with human hepatitis B virus can contain viral substances. Minim Invasive Ther Allied Technol. 2022;31(5):728–36.
Hu X, Zhou Q, Yu J, Wang J, Tu Q, Zhu X. Prevalence of HPV infections in surgical smoke exposed gynecologists. Int Arch Occup Environ Health. 2021;94(1):107–15.
Hughes PS, Hughes AP. Absence of human papillomavirus DNA in the plume of erbium: YAG laser–treated warts. J Am Acad Dermatol. 1998;38(3):426–8.
Taravella MJ, Weinberg A, Blackburn P, May M. Do intact viral particles survive excimer laser ablation? Arch Ophthalmol. 1997;115(8):1028–30.
Llueca A, Barneo-Muñoz M, Escrig J, Rosa de L, Wang W. SARS-CoV-2 Prevalence in Laparoscopic Surgery Filters. Analysis in Patients with Negative Oropharyngeal RT-qPCR in a Pandemic Context: A Cross-Sectional Study †. J Personal Med. 2021;11(11):1052.
Hurst RD, Stewart CL. Hazards of surgical smoke from electrocautery: A critical review of the data. The American Journal of Surgery. 2024.
Benson SM, Maskrey JR, Nembhard MD, Unice KM, Shirley MA, Panko JM. Evaluation of Personal Exposure to Surgical Smoke Generated from Electrocautery Instruments: A Pilot Study. Ann Work Expo Health. 2019;63(9):990-1003. https://doi.org/10.1093/annweh/wxz070 .
Choi SH, Kwon TG, Chung SK, Kim TH. Surgical smoke may be a biohazard to surgeons performing laparoscopic surgery. Surg Endosc. 2014;28(8):2374–80.
Rioux M, Garland A, Webster D, Reardon E. HPV positive tonsillar cancer in two laser surgeons: case reports. J Otolaryngol Head Neck Surg. 2013;42(1):54.
Manson LT, Damrose EJ. Does exposure to laser plume place the surgeon at high risk for acquiring clinical human papillomavirus infection? Laryngoscope. 2013;123(6):1319–20.
Weyandt GH, Tollmann F, Kristen P, Weissbrich B. Low risk of contamination with human papilloma virus during treatment of condylomata acuminata with multilayer argon plasma coagulation and CO 2 laser ablation. Arch Dermatol Res. 2011;303:141–4.
Palma S, Gnambs T, Crevenna R, Jordakieva G. Airborne human papillomavirus (HPV) transmission risk during ablation procedures: A systematic review and meta-analysis. Environ Res. 2021;192:110437. https://doi.org/10.1016/j.envres.2020.110437 .
Imani B, Merajikhah A, Khazaei S, Bouraghi H. Surgical smoke and transmission of coronavirus to surgical team members; a letter to editor. Surgical Innovation. 2021:1553350620977999.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China The lancet. 2020;395(10223):497–506.
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–33.
Liu C-Y, Yang Y-z, Zhang X-M, Xu X, Dou Q-L, Zhang W-W, et al. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiology & Infection. 2020;148.
Kevadiya BD, Machhi J, Herskovitz J, Oleynikov MD, Blomberg WR, Bajwa N, et al. Diagnostics for SARS-CoV-2 infections. Nat Mater. 2021;20(5):593–605.
Dutta D, Naiyer S, Mansuri S, Soni N, Singh V, Bhat KH, et al. COVID-19 diagnosis: a comprehensive review of the RT-qPCR method for detection of SARS-CoV-2. Diagnostics. 2022;12(6):1503.
Mika J, Tobiasz J, Zyla J, Papiez A, Bach M, Werner A, et al. Symptom-based early-stage differentiation between SARS-CoV-2 versus other respiratory tract infections-Upper Silesia pilot study. Sci Rep. 2021;11(1):13580.
Vourtzoumis P, Alkhamesi N, Elnahas A, Hawel JE, Schlachta C. Operating during COVID-19: Is there a risk of viral transmission from surgical smoke during surgery? Can J Surg. 2020;63(3):E299-e301.
COVID R. Review team and UKISCRS. Cataract surgery guidelines for post COVID-19 pandemic: recommendations. 2020.
Morris SN, Fader AN, Milad MP, Dionisi HJ. Understanding the “scope” of the problem: why laparoscopy is considered safe during the COVID-19 pandemic. J Minim Invasive Gynecol. 2020;27(4):789–91.
Chang L, Yan Y, Wang L. Coronavirus disease 2019: coronaviruses and blood safety. Transfus Med Rev. 2020;34(2):75–80.
Weissleder R, Lee H, Ko J, Pittet MJ. COVID-19 diagnostics in context. Sci Transl Med. 2020;12(546):eabc1931.
Pavan N, Crestani A, Abrate A, De Nunzio C, Esperto F, Giannarini G, et al. Risk of Virus Contamination Through Surgical Smoke During Minimally Invasive Surgery: A Systematic Review of the Literature on a Neglected Issue Revived in the COVID-19 Pandemic Era. Eur Urol Focus. 2020;6(5):1058–69.
Coccolini F, Tartaglia D, Puglisi A, Giordano C, Pistello M, Lodato M, et al. SARS-CoV-2 is present in peritoneal fluid in COVID-19 patients. Ann Surg. 2020;272(3):e240–2.
Merajikhah A, Beigi-Khoozani A, Soleimani M. Risk of spreading delta coronavirus to operating room personnel after COVID-19 vaccination. Disaster Emerge Med J. 2021;6(4):206–7.
Wang H, Men P, Xiao Y, Gao P, Lv M, Yuan Q, et al. Hepatitis B infection in the general population of China: a systematic review and meta-analysis. BMC Infect Dis. 2019;19(1):811.
Chuo C-Y. The impact of chronic hepatitis B infection, antiviral treatment and HIV coinfection on the occurrence of cancer outcomes among US veterans: A retrospective cohort study: The University of Texas School of Public Health; 2016.
Roade L, Riveiro-Barciela M, Esteban R, Buti M. Long-term efficacy and safety of nucleos(t)ides analogues in patients with chronic hepatitis B. Ther Adv Infect Dis. 2021;8:2049936120985954. https://doi.org/10.1177/2049936120985954 .
Madukaji L, Ossamulu I, Mambulla G, Galadimma M, Kuta F. Prevalence and Risk Factors of Hepatitis B among Pregnant women attending antenatal clinics in Abuja Nigeria. 2019.
Liang TJ. Hepatitis B: the virus and disease. Hepatology. 2009;49(5 Suppl):S13-21. https://doi.org/10.1002/hep.22881 .
Gerlich WH, Uy A, Lambrecht F, Thomssen R. Cutoff levels of immunoglobulin M antibody against viral core antigen for differentiation of acute, chronic, and past hepatitis B virus infections. J Clin Microbiol. 1986;24(2):288–93.
Timeline A-J. HIV Cell. 2020;183(2):550.
Sliwa K, Carrington MJ, Becker A, Thienemann F, Ntsekhe M, Stewart S. Contribution of the human immunodeficiency virus/acquired immunodeficiency syndrome epidemic to de novo presentations of heart disease in the Heart of Soweto Study cohort. Eur Heart J. 2012;33(7):866–74.
Baggish MS, Poiesz BJ, Joret D, Williamson P, Refai A. Presence of human immunodeficiency virus DNA in laser smoke. Lasers Surg Med. 1991;11(3):197–203.
Melbye M. The natural history of human T lymphotropic virus-III infection: the cause of AIDS. Br Med J (Clin Res Ed). 1986;292(6512):5–12.
Henderson DK, Saah AJ, Zak BJ, Kaslow RA, Lane HC, Folks T, et al. Risk of nosocomial infection with human T-cell lymphotropic virus type III/lymphadenopathy-associated virus in a large cohort of intensively exposed health care workers. Ann Intern Med. 1986;104(5):644–7.
Friedland GH, Klein RS. Transmission of the human immunodeficiency virus. N Engl J Med. 1987;317(18):1125–35.
Williams G. Paralysed with fear: the story of polio: Springer. 2013.
Book Google Scholar
Andrei G, Snoeck R. Advances and perspectives in the management of varicella-zoster virus infections. Molecules. 2021;26(4):1132.
Mirzaiee M, Soleimani M, Banoueizadeh S, Mahdood B, Bastami M, Merajikhah A. Ability to predict surgical outcomes by surgical Apgar score: a systematic review. BMC Surg. 2023;23(1):282.
O’Brien DC, Lee EG, Soo J-C, Friend S, Callaham S, Carr MM. Surgical team exposure to cautery smoke and its mitigation during tonsillectomy. Otolaryngology-Head and Neck Surgery. 2020;163(3):508–16.
Gallo O, Locatello LG. Laser-assisted head and neck surgery in the COVID-19 pandemic: Controversial evidence and precautions. Head Neck. 2020;42(7):1533-4. https://doi.org/10.1002/hed.26271 .
Foster M, Sharma S, Biss L, Pennock J, Ogg MJ. Surgical Smoke Inhalation: Dangerous Consequences for the Surgical Team Posted on June 18, 2020 by Mary J. Ogg, MSN, RN, CNOR.
Ball K. Controlling surgical smoke: A team approach. Information Booklet. 2004.
Download references
Acknowledgements
The authors received no funding from any organization for this research.
Author information
Authors and affiliations.
Department of Operating Room, Faculty Member of Paramedical School, Jahrom University of Medical Sciences, Jahrom, Iran
Bahareh Mahdood
Department of Operating Room, Sabzevar University of Medical Sciences, Sabzevar, Iran
Amirmohammad Merajikhah
Department of Operating Room, School of Paramedical Science, Hamadan University of Medical Sciences, Hamadan, Iran
Mina Mirzaiee & Sara Banoueizadeh
Department of Operating Room, School of Allied Medical Sciences, Ilam University of Medical Sciences, Ilam, Iran
Maryam Bastami
You can also search for this author in PubMed Google Scholar
Contributions
BM: Writing content, data screening, data analysis. AM: Writing content, data analysis, final scientific review, Search, arranging content, and data screening and supervisor. MM: Set the tables, Writing content, data screening. MB: Writing content, data screening. SB: Set the tables, Writing content, and data screening
Corresponding author
Correspondence to Amirmohammad Merajikhah .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Mahdood, B., Merajikhah, A., Mirzaiee, M. et al. Virus and viral components transmitted through surgical smoke; a silent danger in operating room: a systematic review. BMC Surg 24 , 227 (2024). https://doi.org/10.1186/s12893-024-02514-z
Download citation
Received : 05 December 2023
Accepted : 29 July 2024
Published : 09 August 2024
DOI : https://doi.org/10.1186/s12893-024-02514-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Surgical smoke
- Smoke-generating device
- Viral components
BMC Surgery
ISSN: 1471-2482
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
COMMENTS
A 65-year-old woman was admitted to the day-surgery unit of this hospital for release of a trigger finger of the left ring finger. A carpal-tunnel release was performed. After the procedure, the su...
In this paper we describe a fire that occurred in the OR at University Medical Center in Tucson, AZ, in 1998. A patient was seriously burned on the head and neck, requiring 2 mo in the intensive care unit (ICU) as a result. After detailed interviews with the operating room team who participated in the case, we performed laboratory experiments ...
The raw numbers were 1,736 of 10,769 cases in 2017 experienced a return to the Operating Room. For 2018, 1,611 of 10,763 cases experienced a return. Clearly these numbers were unacceptable and demonstrate why our initiative became a priority. After the call to action was made and a plan for a quality initiative focusing on reducing unnecessary ...
Ramos P, Bonfá E, Goulart P, Medeiros M, Cruz N, Puceh-leão P, et al. Perioperative Care and Operating Room Management First-case tardiness reduction in a tertiary academic medical center operating room : A lean six sigma perspective. Perioperative Care and Operating Room Management. 2016; 5 (December):7-12. doi: 10.1016/j.pcorm.2016.12.001.
Operating Room. Day: 0. Time: 10h55. Place: Operating Room. Fred enters the operating room and quickly notes he is the only one not wearing a mask. He looks around to see a horrendous amount of gleaming silver utensils laying on a dark green table. He is then asked to shift over to an even more uncomfortable bed.
Clinical work in the operating room (OR) is considered challenging as it is complex, dynamic, and often time- and resource-constrained. Important characteristics for successful management of complexity include adaptations and adaptive coordination when managing expected and unexpected events. However, there is a lack of explorative research addressing what makes things go well and how OR staff ...
The operating room is the single most important place in the hospital for surgeons. Despite enormous innovation in surgical practice, relatively fewer advances have been made to the actual operating room itself. New technology and devices have been introduced to crowd the space, but changes to the actual lay out and how to organize the room ...
The risk of an operating room (OR) fire should be assessed in the holding area, as well as early in the time out checklist ... Case Study. A nurse gave the wrong medication to a pneumonia patient, causing a fatal heart issue. Failure to Order Medical Imaging Leads to Permanent Vision Loss Case Study . A young adult suffered retinal detachment ...
Organizational factors may influence surgical outcomes, regardless of extensively studied factors such as patient preoperative risk and surgical complexity. This study was designed to explore how operating room organization determines surgical performance and to identify gaps in the literature that necessitate further investigation. We conducted a systematic review according to PRISMA ...
A prospective study was conducted over a period of 3 months (May 1 to July 31, 2019) in a tertiary hospital. Surgical case start time, end time, room turnover time, cancellations and reason for cancellation were observed to evaluate the efficiency of eight operating rooms. A total of 933 elective procedures were observed during the study period.
A keystone of operating room (OR) management is proper OR allocation to optimize access, safety, efficiency, and throughput. ... Overlapping Surgery: A Case Study in Operating Room Throughput and Efficiency Anesthesiol Clin. 2018 Jun;36(2):161-176. doi: 10.1016/j.anclin.2018.01.002.
This research examines current waste management within an operating room at a large United Kingdom National Health Service (NHS) hospital. The study measured the volume and type of waste produced for primary hip operations (PHOs) and estimated the total waste produced across the United Kingdom by the procedure.
The present study therefore aimed to analyze all elective surgery cases of a university hospital within 1 year in search of visible patterns. A total of 14,014 cases scheduled on 254 regular working days at a university hospital between September 2015 and August 2016 underwent screening. ... and surgical times for current procedural terminology ...
Perioperative Nursing Unfolding Case Study: Bringing the Operating Room Experience to the Classroom. Nurse Educ. 2020 Sep/Oct;45 (5):231-232. doi: 10.1097/NNE.0000000000000844.
Dr. Lai is relaxing on his stool by the anaesthetic machine. "Hey, guys, this is Aaron Knoll. He ' s still a bit unconscious, most likely from a concussion post-MVC. Let ' s get him positioned and draped.". Ruth, Dr. Lai, and Lydia slide Aaron from the stretcher onto the OR table. Dr. Bondie checks the patient's identity again and ...
Optimizing operating room utilization: A case study. Thursday, July 28th, 2022 | 12:00 PM - 1:00 PM CT. For most hospitals and health systems, operating rooms are their economic engine. However, OR utilization is often constrained by: Inefficient processes.
Air quality in the microenvironment of operating rooms (ORs) has attracted much attention as surgical smoke may pose health risks. We investigated air pollution in the operating room with a laminar flow system by examining the number and size distribution of airborne particles, the chemical composition and morphology of single particles, and polycyclic aromatic hydrocarbons (PAHs).
The results for improving the laminectomy surgical setup were very impressive. After implementing the build-to-order sets, the instrument assembly went from 34 minutes to 20 minutes, 15 seconds. The instrument setup in the OR went from 24 minutes, 9 seconds, to 2 minutes, 29 seconds — a 90 percent decrease.
In our case, a wide range of ... First-year analysis of the Operating Room Black Box study. Ann Surg. 2020;271(1):122-7. Article Google Scholar McCarron TL, Moffat K, Wilkinson G, Zelinsky S, Boyd JM, White D, et al. Understanding patient engagement in health system decision-making: a co-designed scoping review. Syst Rev. 2019;8(1):1-10.
Of 5,598 cases examined, 88% were delayed. Patients arrived late to the hospital (<2 hours before scheduled surgery) in 65% of first cases. Mean time from arrival to scheduled surgery and in-room placement was 104.6 and 127.4 minutes, respectively. Mean delay time was 28.2 minutes.
We won't mind that case would extend little bit because there are staff doing that case at night. (Participant 7) The policy is 2.5 nurses in the room. ... Communication and relationship dynamics in surgical teams in the operating room: An ethnographic study. BMC Health Services Research, 19, 1-16. [PMC free article] [Google Scholar] Turner ...
Case Study- Operating Room. Case Study- Operating Room. Course. Nursing (234321) 999+ Documents. Students shared 1077 documents in this course. University Western Mindanao State University. Academic year: 2019/2020. Uploaded by: Anonymous Student. This document has been uploaded by a student, just like you, who decided to remain anonymous.
Both of the case series reported data from patients treated within a single centre. One study 14 involved 17 pregnant women who tested positive for COVID-19 and had a caesarean section in Renmin University Hospital, Wuhan, China. Recommendations for the physical OR specified the use of a negative-pressure OR, alongside strict separation of ...
Inpatient falls are a common patient safety event and can have serious consequences. This study used hospital safety reporting system data to characterize falls in perioperative settings. Falls represented 1% of all safety reports between 2014 and 2020 and most commonly involved falls from a bed or stretcher. The author suggests strategies to identify patients at high risk for falls, improve ...
Background During surgical procedures, heat-generating devices are widely used producing surgical smoke (SS). Since the SS can transmit infectious viruses, this systematic review was designed to investigate the potential viruses transmitted through SS. Methods PubMed, Scopus, Web of Science, ProQuest, and Embase databases, along with Cochran Library, and Google Scholar search engine were ...