
PhD students’ mental health is poor and the pandemic made it worse – but there are coping strategies that can help
Senior Lecturer in Technology Enhanced Learning, The Open University
Assistant Professor in Strategy and Entrepreneurship, UCL
Disclosure statement
The authors do not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.
University College London and The Open University provide funding as founding partners of The Conversation UK.
View all partners
A pre-pandemic study on PhD students’ mental health showed that they often struggle with such issues. Financial insecurity and feelings of isolation can be among the factors affecting students’ wellbeing.
The pandemic made the situation worse. We carried out research that looked into the impact of the pandemic on PhD students, surveying 1,780 students in summer 2020. We asked them about their mental health, the methods they used to cope and their satisfaction with their progress in their doctoral study.
Unsurprisingly, the lockdown in summer 2020 affected the ability to study for many. We found that 86% of the UK PhD students we surveyed reported a negative impact on their research progress.
But, alarmingly, 75% reported experiencing moderate to severe depression. This is a rate significantly higher than that observed in the general population and pre-pandemic PhD student cohorts .
Risk of depression
Our findings suggested an increased risk of depression among those in the research-heavy stage of their PhD – for example during data collection or laboratory experiments. This was in contrast to those in the initial stages, or who were nearing the end of their PhD and writing up their research. The data collection stage was more likely to have been disrupted by the pandemic.
Our research also showed that PhD students with caring responsibilities faced a greatly increased risk of depression. In our our study , we found that PhD students with childcare responsibilities were 14 times more likely to develop depressive symptoms than PhD students without children.
This does align with findings on people in the general UK population with childcare responsibilities during the pandemic. Adults with childcare responsibilities were 1.4 times more likely to develop depression or anxiety compared to their counterparts without children or childcare duties.
It was also interesting to find that PhD students facing the disruption caused by the pandemic who did not receive an extension – extra financial support and time beyond the expected funding period – or were uncertain about whether they would receive an extension at the time of our study, were 5.4 times more likely to experience significant depression.
Our research also used a questionnaire designed to measure effective and ineffective ways to cope with stressful life events. We used this to look at which coping skills – strategies to deal with challenges and difficult situations — used by PhD students were associated with lower depression levels. These “good” strategies included “getting comfort and understanding from someone” and “taking action to try to make the situation better”.

Interestingly, female PhD students, who were slightly less likely than men to experience significant depression, showed a greater tendency to use good coping approaches compared to their counterparts. Specifically, they favoured the above two coping strategies that are associated with lower levels of depression.
On the other hand, certain coping strategies were associated with higher depression levels. Prominent among these were self-critical tendencies and the use of substances like alcohol or drugs to cope with challenging situations.
A supportive environment
Creating a supportive environment is not solely the responsibility of individual students or academic advisors. Universities and funding bodies must play a proactive role in mitigating the challenges faced by PhD students.
By taking proactive steps, universities could create a more supportive environment for their students and help to ensure their success.
Training in coping skills could be extremely beneficial for PhD students. For instance, the University of Cambridge includes this training as part of its building resilience course .
A focus on good strategies or positive reframing – focusing on positive aspects and potential opportunities – could be crucial. Additionally, encouraging PhD students to seek emotional support may also help reduce the risk of depression.
Another example is the establishment of PhD wellbeing support groups , an intervention funded by the Office for Students and Research England Catalyst Fund .
Groups like this serve as a platform for productive discussions and meaningful interactions among students, facilitated by the presence of a dedicated mental health advisor.
Our research showed how much financial insecurity and caring responsibilities had an effect on mental health. More practical examples of a supportive environment offered by universities could include funded extensions to PhD study and the availability of flexible childcare options.
By creating supportive environments, universities can invest in the success and wellbeing of the next generation of researchers.
- Higher education
- Mental health
- Coping strategies
- PhD students
- Give me perspective

Service Centre Senior Consultant

Director of STEM

Community member - Training Delivery and Development Committee (Volunteer part-time)

Chief Executive Officer

Head of Evidence to Action

Managing While and Post-PhD Depression And Anxiety: PhD Student Survival Guide
Embarking on a PhD journey can be as challenging mentally as it is academically. With rising concerns about depression among PhD students, it’s essential to proactively address this issue. How to you manage, and combat depression during and after your PhD journey?
In this post, we explore the practical strategies to combat depression while pursuing doctoral studies.
From engaging in enriching activities outside academia to finding supportive networks, we describe a variety of approaches to help maintain mental well-being, ensuring that the journey towards academic excellence doesn’t come at the cost of your mental health.
How To Manage While and Post-Phd Depression
| – Participate in sports, arts, or social gatherings. – Temporarily remove the weight of your studies from your mind. | |
| – Find a mentor who is encouraging and positive. – Look for a ‘yes and’ approach to boost morale. | |
| – Regular exercise like walking, swimming, gym combats depression – Improves mood and overall wellbeing. | |
| – Choose a graduate program that fosters community. – Ensure open discussion and support for mental health. – Select a university with the right support system. | |
| – Understand your choices in the PhD journey. – Consider deferment, pause, or quitting if needed. |
Why PhD Students Are More Likely To Experience Depression Than Other Students
The journey of a PhD student is often romanticised as one of intellectual rigour and eventual triumph.
However, beneath this veneer lies a stark reality: PhD students are notably more susceptible to experiencing depression and anxiety.
This can be unfortunately, quite normal in many PhD students’ journey, for several reasons:
Grinding Away, Alone
Imagine being a graduate student, where your day-to-day life is deeply entrenched in research activities. The pressure to consistently produce results and maintain productivity can be overwhelming.
For many, this translates into long hours of isolation, chipping away at one’s sense of wellbeing. The lack of social support, coupled with the solitary nature of research, often leads to feelings of isolation.
Mentors Not Helping Much
The relationship with a mentor can significantly affect depression levels among doctoral researchers. An overly critical mentor or one lacking in supportive guidance can exacerbate feelings of imposter syndrome.
Students often find themselves questioning their capabilities, feeling like they don’t belong in their research areas despite their achievements.
Nature Of Research Itself
Another critical factor is the nature of the research itself. Students in life sciences, for example, may deal with additional stressors unique to their field.
Specific aspects of research, such as the unpredictability of experiments or the ethical dilemmas inherent in some studies, can further contribute to anxiety and depression among PhD students.
Competition Within Grad School
Grad school’s competitive environment also plays a role. PhD students are constantly comparing their progress with peers, which can lead to a mental health crisis if they perceive themselves as falling behind.

This sense of constant competition, coupled with the fear of failure and the stigma around mental health, makes many hesitant to seek help for anxiety or depression.
How To Know If You Are Suffering From Depression While Studying PhD?
If there is one thing about depression, you often do not realise it creeping in. The unique pressures of grad school can subtly transform normal stress into something more insidious.
As a PhD student in academia, you’re often expected to maintain high productivity and engage deeply in your research activities. However, this intense focus can lead to isolation, a key factor contributing to depression and anxiety among doctoral students.
Changes in Emotional And Mental State
You might start noticing changes in your emotional and mental state. Feelings of imposter syndrome, where you constantly doubt your abilities despite evident successes, become frequent.
This is especially true in competitive environments like the Ivy League universities, where the bar is set high. These feelings are often exacerbated by the lack of positive reinforcement from mentors, making you feel like you don’t quite belong, no matter how hard you work.
Lack Of Pleasure From Previously Enjoyable Activities
In doctoral programs, the stressor of overwork is common, but when it leads to a consistent lack of interest or pleasure in activities you once enjoyed, it’s a red flag. This decline in enjoyment extends beyond one’s research and can pervade all aspects of life.
The high rates of depression among PhD students are alarming, yet many continue to suffer in silence, afraid to ask for help or reveal their depression due to the stigma associated with mental health issues in academia.
Losing Social Connections
Another sign is the deterioration of social connections. Graduate student mental health is significantly affected by social support and isolation.

You may find yourself withdrawing from friends and activities, preferring the solitude that ironically feeds into your sense of isolation.
Changes In Appetite And Weight
Changes in appetite and weight can be a significant indicator of depression. As they navigate the demanding PhD study, students might experience fluctuations in their eating habits.
Some may find themselves overeating as a coping mechanism, leading to weight gain. Others might lose their appetite altogether, resulting in noticeable weight loss.
These changes are not just about food; they reflect deeper emotional and mental states.
Such shifts in appetite and weight, especially if sudden or severe, warrant attention as they may signal underlying depression, a common issue in the high-stress environment of PhD studies.
Unhealthy Coping Mechanisms
PhD students grappling with depression often feel immense pressure to excel academically while battling isolation and imposter syndrome. Lacking adequate mental health support, some turn to unhealthy coping mechanisms like substance abuse. These may include:
- Overeating,
- And many more.
These provide temporary relief from overwhelming stress and emotional turmoil. However, such methods can exacerbate their mental health issues, creating a vicious cycle of dependency and further detachment from healthier coping strategies and support systems.
It’s essential for PhD students experiencing depression to recognise these signs and seek professional help. Resources like the National Suicide Prevention Lifeline are very helpful in this regard.
Suicidal Thoughts Or Attempts

Suicidal thoughts or attempts may sound extreme, but they can happen in PhD studies. This is because of the high-pressure environment of PhD studies.
Doctoral students, often grappling with intense academic demands, social isolation, and imposter syndrome, can be susceptible to severe mental health crises.
When the burden becomes unbearable, some may experience thoughts of self-harm or suicide as a way to escape their distress. These thoughts are a stark indicator of deep psychological distress and should never be ignored.
It’s crucial for academic institutions and support networks to provide robust mental health resources and create an environment where students feel safe to seek help and discuss their struggles openly.
How To Prevent From Depression During And After Ph.D?
A PhD student’s experience is often marked by high rates of depression, a concern echoed in studies from universities like the University of California and Arizona State University. If you are embarking on a PhD journey, make sure you are aware of the issue, and develop strategies to cope with the stress, so you do not end up with depression.
Engage With Activities Outside Academia
One effective strategy is engaging in activities outside academia. Diverse interests serve as a lifeline, breaking the monotony and stress of grad school. Some activities you can consider include:
- Social gatherings.
These activities provide a crucial balance. For instance, some students highlighted the positive impact of adopting a pet, which not only offered companionship but also a reason to step outside and engage with the world.
Seek A Supportive Mentor
The role of a supportive mentor cannot be overstated. A mentor who adopts a ‘yes and’ approach rather than being overly critical can significantly boost a doctoral researcher’s morale.
This positive reinforcement fosters a healthier research environment, essential for good mental health.
Stay Active Physically
Physical exercise is another key element. Regular exercise has been shown to help cope with symptoms of moderate to severe depression. It’s a natural stress reliever, improving mood and enhancing overall wellbeing. Any physical workout can work here, including:
- Brisk walking
- Swimming, or
- Gym sessions.
Seek Positive Environment
Importantly, the graduate program environment plays a critical role. Creating a community where students feel comfortable to reveal their depression or seek help is vital.
Whether it’s through formal support groups or informal peer networks, building a sense of belonging and understanding can mitigate feelings of isolation and imposter syndrome.
This may be important, especially in the earlier stage when you look and apply to universities study PhD . When possible, talk to past students and see how are the environment, and how supportive the university is.
Choose the right university with the right support ensures you keep depression at bay, and graduate on time too.
Remember You Have The Power
Lastly, acknowledging the power of choice is empowering. Understanding that continuing with a PhD is a choice, not an obligation. If things become too bad, there is always an option to seek a deferment, pause. You can also quit your studies too.

Work on fixing your mental state, and recover from depression first, before deciding again if you want to take on Ph.D studies again. There is no point continuing to push yourself, only to expose yourself to self-harm, and even suicide.
Wrapping Up: PhD Does Not Need To Ruin You
Combating depression during PhD studies requires a holistic approach. Engaging in diverse activities, seeking supportive mentors, staying physically active, choosing positive environments, and recognising one’s power to make choices are all crucial.
These strategies collectively contribute to a healthier mental state, reducing the risk of depression. Remember, prioritising your mental well-being is just as important as academic success. This helps to ensure you having a more fulfilling and sustainable journey through your PhD studies.

Dr Andrew Stapleton has a Masters and PhD in Chemistry from the UK and Australia. He has many years of research experience and has worked as a Postdoctoral Fellow and Associate at a number of Universities. Although having secured funding for his own research, he left academia to help others with his YouTube channel all about the inner workings of academia and how to make it work for you.
Thank you for visiting Academia Insider.
We are here to help you navigate Academia as painlessly as possible. We are supported by our readers and by visiting you are helping us earn a small amount through ads and affiliate revenue - Thank you!

2024 © Academia Insider

Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Self-reported depression and anxiety among graduate students during the covid-19 pandemic: examining risk and protective factors.

1. Introduction
1.1. the current study, 1.2. theoretical framework, 2. materials and methods, 2.1. recruitment and sampling, 2.2. measures, outcome variables, 2.3. independent variables, 2.4. sociodemographic factors, statistical analysis, 3.1. depression, 3.2. anxiety, 4. discussion, 4.1. implications for higher education research and practice, limitations, 5. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- Mistler, B.J.; Director; Reetz, D.R.; Krylowicz, B.; Barr, V. The AUCCCD Annual Survey and Report Overview. 2013. Available online: http://files.cmcglobal.com/Monograph_2012_AUCCCD_Public.pdf (accessed on 18 January 2022).
- Spring. Reference Group Data Report. 2016. Available online: https://www.acha.org/documents/ncha/NCHA-II%20SPRING%202016%20US%20REFERENCE%20GROUP%20DATA%20REPORT.pdf (accessed on 26 March 2023).
- Feng, B.; Zhang, Y.; Zhang, L.; Xie, X.; Geng, W. Change in the level of depression among Chinese college students from 2000 to 2017: A cross-temporal meta-analysis. Soc. Behav. Personal. 2020 , 48 , 1–16. [ Google Scholar ] [ CrossRef ]
- The Impact of COVID-19 on College Student Well-Being. Available online: https://www.acha.org/documents/ncha/Healthy_Minds_NCHA_COVID_Survey_Report_FINAL.pdf (accessed on 26 March 2023).
- Lipson, S.K.; Zhou, S.; Abelson, S.; Heinze, J.; Jirsa, M.; Morigney, J.; Patterson, A.; Singh, M.; Eisenberg, D. Trends in college student mental health and help-seeking by race/ethnicity: Findings from the national healthy minds study, 2013–2021. J. Affect. Disord. 2022 , 306 , 138–147. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Farrer, L.M.; Gulliver, A.; Bennett, K.; Fassnacht, D.B.; Griffiths, K.M. Demographic and psychosocial predictors of major depression and generalised anxiety disorder in Australian university students. BMC Psychiatry 2016 , 16 , 241. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- National Center for Education Statistics. The NCES Fast Facts Tool Provides Quick Answers to Many Education Questions. Available online: https://nces.ed.gov/fastfacts/display.asp?id=372#Postsecondary-enrollment (accessed on 21 June 2021).
- Eisenberg, D.; Gollust, S.E.; Golberstein, E.; Hefner, J.L. Prevalence and correlates of depression, anxiety, and suicidality among university students. Am. J. Orthopsychiatry 2007 , 77 , 534–542. [ Google Scholar ] [ CrossRef ]
- Lederer, A.M.; Hoban, M.T.; Lipson, S.K.; Zhou, S.; Eisenberg, D. More Than Inconvenienced: The Unique Needs of U.S. College Students During the COVID-19 Pandemic. Health Educ. Behav. 2021 , 48 , 14–19. [ Google Scholar ] [ CrossRef ]
- ACHA. American College Health Association-national college health assessment II: Graduate and professional student executive summary spring 2019 ; American College Health Association: Hanover, MD, USA, 2019; Available online: https://dev.acha.org/documents/ncha/NCHA-II_SPRING_2019_GRADUATE_AND_PROFESSIONAL_REFERENCE_GROUP_EXECUTIVE_SUMMARY.pdf (accessed on 26 March 2023).
- Evans, T.M.; Bira, L.; Gastelum, J.B.; Weiss, L.T.; Vanderford, N.L. Evidence for a mental health crisis in graduate education. Nat. Biotechnol. 2018 , 36 , 282–284. [ Google Scholar ] [ CrossRef ]
- The Chronicle of Higher Education. Available online: https://www.chronicle.com/article/how-has-the-pandemic-affected-graduate-students-this-study-has-answers (accessed on 21 June 2021).
- Alonzi, S.; La Torre, A.; Silverstein, M.W. The psychological impact of preexisting mental health and physical health conditions during the COVID-19 pandemic. Am. Psychol. Assoc. 2020 , 12 , 236–238. [ Google Scholar ] [ CrossRef ]
- Qui, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020 , 33 , e100213. [ Google Scholar ]
- Vahedian-Azimi, A.; Moayed, M.S.; Rahimibashar, F.; Shojaei, S.; Ashtari, S.; Pourhoseingholi, M.A. Comparison of the severity of psychological distress among four groups of an Iranian population regarding COVID-19 pandemic. BMC Psychiatry 2020 , 20 , 402. [ Google Scholar ] [ CrossRef ]
- Women Earned Majority of Doctoral Degrees in 2016 for 8th Straight Year and Outnumber Men in Grad School 135 to 100. American Enterprise Institute—AEI. Available online: https://www.aei.org/carpe-diem/women-earned-majority-of-doctoral-degrees-in-2016-for-8th-straight-year-and-outnumber-men-in-grad-school-135-to-100/#:~:text=13)%2C%20showing%20tht%20there%20is (accessed on 28 March 2023).
- Aloufi, F.; Ibrahim, A.L.; Elsayed, A.M.A.; Wardat, Y.; Ahmed, A.O. Virtual mathematics education during COVID-19: An exploratory study of teaching practices for teachers in simultaneous virtual classes. Int. J. Learn. Teach. Educ. Res. 2021 , 20 , 85–113. [ Google Scholar ] [ CrossRef ]
- Wardat, Y.; Belbase, S.; Tairab, H. Mathematics Teachers’ perceptions of trends in international mathematics and science study (TIMSS)-Related practices in Abu Dhabi Emirate schools. Sustainability 2022 , 14 , 5436. [ Google Scholar ] [ CrossRef ]
- Hamad, S.; Tairab, H.; Wardat, Y.; Rabbani, L.; AlArabi, K.; Yousif, M.; Abu-Al-Aish, A.; Stoica, G. Understanding science teachers’ implementations of integrated STEM: Teacher perceptions and practice. Sustainability 2022 , 14 , 3594. [ Google Scholar ] [ CrossRef ]
- The Chronicle of Higher Education. For Many Graduate Students, Covid-19 Pandemic Highlights Inequities. Available online: https://www.chronicle.com/article/for-many-graduate-students-covid-19-pandemic-highlights-inequities/ (accessed on 21 June 2021).
- The American Associations for the Advancement of Science. As the Pandemic Erodes Grad Student Mental Health, Academics Sounds the Alarm. Available online: https://www.sciencemag.org/careers/2020/09/pandemic-erodes-grad-student-mental-health-academics-sound-alarm (accessed on 21 June 2021).
- Harrison, D.; Rowland, S.; Wood, G.; Bakewell, L.; Petridis, I.; Long, K.; Vasileiou, K.; Barnett, J.; Barreto, M.; Wilson, M.; et al. Designing Technology-Mediated Peer Support for Postgraduate Research Students at Risk of Loneliness and Isolation. ACM Trans. Comput.-Hum. Interact. 2023 , 30 , 1–40. [ Google Scholar ] [ CrossRef ]
- Huang, L.; Wang, Y.; Li, L. Loneliness and depression among Chinese college students during the COVID-19 outbreak: A moderated mediation model. J. Educ. Psychol. 2020 , 112 , 1392–1406. [ Google Scholar ]
- Rahman, R.; Ross, A.; Pinto, R. The critical importance of community health workers as first responders to COVID-19 in USA. Health Promot. Int. 2021 , 36 , 1498–1507. [ Google Scholar ] [ CrossRef ]
- Davies, H.; Cheung, M. COVID-19 and first responder social workers: An unexpected mental health storm. Soc. Work. 2022 , 67 , 114–122. [ Google Scholar ] [ CrossRef ]
- Burns, K.F.; Strickland, C.J.; Horney, J.A. Public health student response to COVID-19. J. Community Health 2021 , 46 , 298–303. [ Google Scholar ] [ CrossRef ]
- Prince, J.P. University student counseling and mental health in the United States: Trends and challenges. Ment. Health Prev. 2015 , 3 , 5–10. [ Google Scholar ] [ CrossRef ]
- Vidourek, R.A.; King, K.A.; Nabors, L.A.; Merianos, A.L. Students’ benefits and barriers to mental health help-seeking. Health Psychol. Behav. Med. Open Access J. 2014 , 2 , 1009–1022. [ Google Scholar ] [ CrossRef ]
- Duffy, A.; Saunders, K.E.; Malhi, G.S.; Patten, S.; Cipriani, A.; McNevin, S.H.; MacDonald, E.; Geddes, J. Mental health care for university students: A way forward? Lancet Psychiatry 2019 , 6 , 885–887. [ Google Scholar ] [ CrossRef ]
- Amendola, S.; Spensieri, V.; Hengartner, M.P.; Cerutti, R. Mental health of Italian adults during COVID-19 pandemic. Br. J. Health Psychol. 2021 , 26 , 644–656. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ren, X.; Huang, W.; Pan, H.; Huang, T.; Wang, X.; Ma, Y. Mental health during the Covid-19 outbreak in China: A meta-analysis. Psychiatr. Q. 2020 , 91 , 1033–1045. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Wang, Y.; Kala, M.P.; Jafar, T.H. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: A systematic review and meta-analysis. PLoS ONE 2020 , 15 , e0244630. [ Google Scholar ] [ CrossRef ]
- Browning, M.H.E.M.; Larson, L.R.; Sharaievska, I.; Rigolon, A.; McAnirlin, O.; Mullenback, L.; Cloutier, S.; Vu, T.M.; Thomsen, H.; Reigner, N.; et al. Psychological impacts from COVID-19 among university students: Risk factors across seven states in the United States. PLoS ONE 2021 , 16 , e0245327. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Yang, D.; Tu, C.; Dai, X. The effect of the 2019 novel coronavirus pandemic on college students in Wuhan. Am. Psychol. Assoc. 2020 , 12 , 6–14. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Posselt, J. Discrimination, Competitiveness, and Support in US Graduate Student Mental Health ; Studies in Graduate and Postdoctoral Education, Rossier School of Education, University of Southern California: Los Angeles, CA, USA, 2021. [ Google Scholar ]
- Braveman, P.; Gottlieb, L. The social determinants of health: It’s time to consider the causes of the causes. Public Health Rep. 2014 , 129 (Suppl. 2), 19–31. [ Google Scholar ] [ CrossRef ]
- Crenshaw, K. Mapping the margins: Intersectionality, identity politics, and violence against women of color. Stanf. Law Rev. 1990 , 43 , 1241. [ Google Scholar ] [ CrossRef ]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001 , 16 , 606–613. [ Google Scholar ] [ CrossRef ]
- American Psychological Association. Patient Health Questionnaire (PHQ-9 & PHQ-2), Construct: Depressive symptoms. Available online: https://www.apa.org/pi/about/publications/caregivers/practice-settings/assessment/tools/patient-health (accessed on 12 February 2023).
- Sun, Y.; Fu, Z.; Bo, Q.; Mao, Z.; Ma, X.; Wang, C. The reliability and validity of PHQ-9 in patients with major depressive disorder in psychiatric hospital. BMC Psychiatry 2020 , 20 , 474. [ Google Scholar ] [ CrossRef ]
- Löwe, B.; Decker, O.; Müller, S.; Brähler, E.; Schellberg, D.; Herzog, W.; Herzberg, P.Y. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med. Care 2008 , 46 , 266–274. [ Google Scholar ] [ CrossRef ]
- Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Cacioppo, J.T. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Res. Aging 2004 , 26 , 655–672. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Russell, D.; Peplau, L.A.; Cutrona, C.E. The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. J. Personal. Soc. Psychol. 1980 , 39 , 472. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hefner, J.; Eisenberg, D. Social support and mental health among college students. Am. J. Orthopsychiatry 2009 , 79 , 491–499. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Taylor, S.E.; Stanton, A.L. Coping resources, coping processes, and mental health. Annu. Rev. Clin. Psychol. 2007 , 3 , 377–401. [ Google Scholar ] [ CrossRef ]
- National Institute of Mental Health. Available online: https://www.nimh.nih.gov/health/topics/college-students-and-mental-health/index.shtml (accessed on 1 June 2021).
- Nochaiwong, S.; Ruengorn, C.; Thavorn, K.; Hutton, B.; Awiphan, R.; Phosuya, C.; Ruanta, Y.; Wongpakaran, N.; Wongpakaran, T. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: A systematic review and meta-analysis. Sci. Rep. 2021 , 11 , 10173. [ Google Scholar ] [ CrossRef ]
- Vahratian, A.; Blumberg, S.J.; Terlizzi, E.P.; Schiller, J.S. Symptoms of Anxiety or Depressive Disorder and Use of Mental Health Care Among Adults During the COVID-19 Pandemic—United States, August 2020–February 2021. MMWR Morb. Mortal. Wkly. Rep. 2021 , 70 , 490–494. [ Google Scholar ] [ CrossRef ]
- Aucejo, E.M.; French, J.; Araya, M.P.U.; Zafar, B. The impact of COVID-19 on student experiences and expectations: Evidence from a survey. J. Public Econ. 2020 , 191 , 104271. [ Google Scholar ] [ CrossRef ]
- Liu, C.H.; Pinder-Amaker, S.; Hahm, H.C.; Chen, J.A. Priorities for addressing the impact of the COVID-19 pandemic on college student mental health. J. Am. Coll. Health 2022 , 70 , 1356–1358. [ Google Scholar ] [ CrossRef ]
- Faura-Martínez, U.; Lafuente-Lechuga, M.; Cifuentes-Faura, J. Sustainability of the Spanish university system during the pandemic caused by COVID-19. Educ. Rev. 2021 , 74 , 645–663. [ Google Scholar ] [ CrossRef ]
- Chakraborty, P.; Mittal, P.; Gupta, M.S.; Yadav, S.; Arora, A. Opinion of students on online education during the COVID-19 pandemic. Hum. Behav. Emerg. Technol. 2021 , 3 , 357–365. [ Google Scholar ] [ CrossRef ]
- Jabbari, J.; Ferris, D.; Frank, T.; Malik, S.; Bessaha, M.L. Intersecting race and gender across hardships and mental health during COVID-19: A moderated-mediation model of graduate students at two universities. Race Soc. Probl. 2022 , 2022 , 1–19. [ Google Scholar ]
- Alismaiel, O.; Cifuentes-Faura, J.; Al-Rahmi, W. Online Learning, Mobile Learning and social media technologies: An Empirical Study on Constructivism Theory during the COVID-19 Pandemic. Sustainability 2022 , 14 , 11134. [ Google Scholar ] [ CrossRef ]
Click here to enlarge figure
| Variable | N | % | Mean (SD) |
|---|---|---|---|
| Age (years) | 31.88 (10.00) | ||
| Gender | |||
| Male | 91 | 26.7 | |
| Female | 233 | 68.3 | |
| Non-binary/third gender | 11 | 3.2 | |
| Not specified | 6 | 1.8 | |
| Race | |||
| White | 216 | 63.3 | |
| Black | 21 | 6.2 | |
| Asian | 66 | 19.4 | |
| Multiracial/biracial | 12 | 3.5 | |
| Other | 11 | 3.2 | |
| Not specified | 15 | 4.4 | |
| Hispanic | |||
| No | 289 | 84.8 | |
| Yes | 44 | 12.9 | |
| Unspecified | 8 | 2.3 | |
| Sexual orientation | |||
| Heterosexual | 248 | 77.3 | |
| Identifies as gay/lesbian/bisexual | 73 | 22.7 | |
| Not specified | 20 | 5.9 | |
| Transgender | |||
| No | 325 | 95.3 | |
| Yes | 10 | 2.9 | |
| Not specified | 6 | 1.8 | |
| Marital status | |||
| Single, never married | 234 | 68.6 | |
| Married/living common-law | 86 | 25.2 | |
| Widowed/divorced/separated | 21 | 6.2 | |
| Children | |||
| No | 266 | 78.0 | |
| Yes | 74 | 21.7 | |
| Not specified | 1 | 0.3 | |
| Country of birth | |||
| United States | 232 | 74.9 | |
| Other | 102 | 29.9 | |
| Not specified | 7 | 2.1 | |
| Household income | |||
| <$20,000 | 52 | 15.2 | |
| $20,000 to $39,999 | 85 | 24.9 | |
| $40,000 to $59,999 | 37 | 10.9 | |
| $60,000 to $79,999 | 43 | 12.6 | |
| $80,000 to $99,999 | 34 | 10.0 | |
| >$100,000 | 84 | 24.6 | |
| Not specified | 6 | 1.8 | |
| Coping, scale of 1–10 (not coping to coping well) | 6.15 (2.17) | ||
| Emotional support, scale of 1–10 (none to a lot) | 7.62 (2.19) | ||
| Physical health, perceived | |||
| Poor | 4 | 1.2 | |
| Fair | 18 | 5.3 | |
| Good | 81 | 23.9 | |
| Very good | 160 | 46.9 | |
| Excellent | 76 | 22.3 | |
| Not specified | 2 | 0.6 | |
| Mental/emotional health, perceived | |||
| Poor | 31 | 9.1 | |
| Fair | 106 | 31.3 | |
| Good | 117 | 34.5 | |
| Very good | 63 | 18.6 | |
| Excellent | 22 | 6.5 | |
| Not specified | 2 | 0.6 | |
| Loneliness | |||
| Never lonely | 63 | 18.5 | |
| Sometimes lonely | 184 | 54.1 | |
| Often or always lonely | 93 | 27.4 | |
| Not specified | 1 | 0.3 | |
| Increased pressure to be productive due to COVID-19 | |||
| Strongly disagree | 20 | 5.9 | |
| Disagree | 26 | 7.6 | |
| Neither agree or disagree | 75 | 22.0 | |
| Agree | 135 | 39.6 | |
| Strongly agree | 78 | 22.9 | |
| Not specified | 7 | 2.1 | |
| Inability to pay full rent/mortgage, previous 3 months | |||
| No | 312 | 91.5 | |
| Yes | 27 | 7.9 | |
| Not specified | 2 | 0.6 | |
| Close family/friend test positive for COVID-19 | |||
| No | 206 | 60.4 | |
| Yes, one person | 44 | 12.9 | |
| Yes, more than 1 | 90 | 26.4 | |
| Not specified | 1 | 0.3 | |
| Close family/friend die from COVID-19 | |||
| No | 309 | 90.6 | |
| Yes, one person | 16 | 4.7 | |
| Yes, more than one | 15 | 4.4 | |
| Not specified | 1 | 0.3 | |
| Time spent searching for COVID-19 information | |||
| Never or almost never | 21 | 6.2 | |
| A few times a month | 49 | 14.4 | |
| A few times a week | 112 | 32.8 | |
| Once a day | 84 | 24.6 | |
| A few times a day | 43 | 12.6 | |
| I try to stay updated all the time | 31 | 9.1 | |
| Not specified | 1 | 0.3 |
| Variable | Unadjusted | Adjusted | ||
|---|---|---|---|---|
| OR | CI | OR | CI | |
| Age | 0.95 *** | 0.93, 0.97 | 1.00 | 0.96, 1.04 |
| Gender | ||||
| Male | ref | ref | ||
| Female | 0.90 | 0.56, 1.46 | 0.57 | 0.28, 1.14 |
| Non-binary | 6.92 | 0.85, 56.20 | 4.41 | 0.24, 81.64 |
| Race | ||||
| White | ref | ref | ||
| Black | 0.69 | 0.29, 1.65 | 0.52 | 0.12, 2.24 |
| Asian | 0.95 | 0.55, 1.64 | 1.02 | 0.40, 2.60 |
| Multi/biracial | 3.26 | 0.70, 15.26 | 2.72 | 0.39, 19.20 |
| Other | 1.21 | 0.35, 4.15 | 0.91 | 0.16, 5.08 |
| Hispanic | 0.98 | 0.52, 1.84 | 0.88 | 0.30, 2.62 |
| Identifies as LGB | 1.92 * | 1.12, 3.30 | 1.60 | 0.73, 3.48 |
| Transgender | 1.23 | 0.36, 4.12 | 0.35 | 0.04, 2.74 |
| Marital Status | ||||
| Single, never married | ref | ref | ||
| Married/common-law | 0.42 *** | 0.26, 0.69 | 1.36 | 0.50, 3.70 |
| Divorced/widowed/separated | 0.43 *** | 0.17, 1.07 | 0.99 | 0.16, 6.00 |
| Has children | 0.32 *** | 0.19, 0.52 | 0.30 * | 0.10, 0.93 |
| Born outside the U.S. | 1.01 | 0.64, 1.61 | 1.50 | 0.66, 3.40 |
| Household income | 0.74 | 0.66, 0.84 | 0.95 | 0.78, 1.15 |
| Loneliness | ||||
| Never lonely | ref | ref | ||
| Sometimes lonely | 5.78 *** | 3.20, 10.44 | 2.83 ** | 1.32, 6.03 |
| Often or always lonely | 23.71 | 10.88, 51.64 | 6.33 *** | 2.17, 18.47 |
| Coping | 0.61 *** | 0.54, 0.69 | 0.84 | 0.70, 1.02 |
| Emotional support | 0.77 *** | 0.69, 0.85 | 0.84 * | 0.72, 0.99 |
| Physical health, perceived | 0.50 *** | 0.38, 0.66 | 0.69 | 0.46, 1.02 |
| Mental/emotional health, perceived | 0.30 *** | 0.23, 0.39 | 0.52 *** | 0.36, 0.76 |
| Someone close test positive COVID | 0.93 | 0.73, 1.18 | 0.89 | 0.61, 1.28 |
| Someone close died from COVID | 1.19 | 0.74, 1.92 | 1.42 | 0.70, 2.88 |
| Time searching for COVID-19 info | 1.37 *** | 1.15, 1.62 | 1.28 * | 1.01, 1.62 |
| Pressure to be productive | 0.58 *** | 0.48, 0.72 | 1.13 | 0.86, 1.49 |
| Inability to pay mortgage/rent | 2.18 | 0.91, 5.26 | 7.98 * | 1.11, 57.36 |
| Variable | Unadjusted | Adjusted | ||
|---|---|---|---|---|
| OR | CI | OR | CI | |
| Age | 0.95 | 0.93, 0.97 | 0.99 | 0.95, 1.03 |
| Gender | ||||
| Male | ref | ref | ||
| Female | 1.03 | 0.66, 1.62 | 0.77 | 0.42, 1.42 |
| Non-binary | 2.88 | 0.82, 10.16 | 3.21 | 0.23, 45.67 |
| Race | ||||
| White | ref | Ref | ||
| Black | 0.80 | 0.35, 1.86 | 1.25 | 0.33, 4.78 |
| Asian | 0.73 | 0.44, 1.21 | 1.25 | 0.53, 2.95 |
| Multi/biracial | 1.86 | 0.59, 5.88 | 1.11 | 0.24, 5.14 |
| Other | 0.79 | 0.26, 2.43 | 1.01 | 0.21, 4.90 |
| Hispanic | 0.96 | 0.52, 1.75 | 1.06 | 0.40, 2.78 |
| Identifies as LGB | 2.44 *** | 1.49, 4.01 | 2.33 * | 1.16, 4.67 |
| Transgender | 1.09 | 0.35, 3.44 | 0.25 | 0.04, 1.73 |
| Marital status | ||||
| Single, never married | ref | ref | ||
| Married/common-law | 0.47 *** | 0.29, 0.75 | 2.24 | 0.88, 5.70 |
| Divorced/widowed/separated | 0.49 | 0.21, 1.15 | 2.97 | 0.58, 15.29 |
| Has children | 0.35 *** | 0.22, 0.58 | 0.33 * | 0.12, 0.94 |
| Born outside the U.S. | 0.68 | 0.44, 1.04 | 0.34 ** | 0.16, 0.72 |
| Household income | 0.77 *** | 0.69, 0.86 | 0.88 | 0.73, 1.04 |
| Loneliness | ||||
| Never lonely | ref | ref | ||
| Sometimes lonely | 3.92 *** | 2.23, 6.87 | 1.77 | 0.84, 3.72 |
| Often or always lonely | 13.45 *** | 6.92, 26.15 | 3.65 ** | 1.43, 9.34 |
| Coping | 0.57 *** | 0.50, 0.64 | 0.78 ** | 0.66, 0.92 |
| Emotional support | 0.81 *** | 0.74, 0.90 | 0.96 | 0.84, 1.10 |
| Physical health, perceived | 0.55 *** | 0.43, 0.71 | 0.94 | 0.67, 1.31 |
| Mental/emotional health, perceived | 0.25 *** | 0.19, 0.32 | 0.41 *** | 0.29, 0.59 |
| Someone close test positive COVID | 1.00 | 0.80, 1.26 | 0.97 | 0.70, 1.36 |
| Someone close died from COVID | 0.96 | 0.63, 1.47 | 0.90 | 0.47, 1.70 |
| Time searching for COVID-19 info | 1.38 *** | 1.18, 1.62 | 1.26 * | 1.02, 1.57 |
| Increased pressure to be productive | 1.85 *** | 1.51, 2.26 | 1.18 | 0.91, 1.52 |
| Inability to pay mortgage/rent | 2.01 | 0.94, 4.31 | 2.17 | 0.60, 7.86 |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Malik, S.; Bessaha, M.; Scarbrough, K.; Younger, J.; Hou, W. Self-Reported Depression and Anxiety among Graduate Students during the COVID-19 Pandemic: Examining Risk and Protective Factors. Sustainability 2023 , 15 , 6817. https://doi.org/10.3390/su15086817
Malik S, Bessaha M, Scarbrough K, Younger J, Hou W. Self-Reported Depression and Anxiety among Graduate Students during the COVID-19 Pandemic: Examining Risk and Protective Factors. Sustainability . 2023; 15(8):6817. https://doi.org/10.3390/su15086817
Malik, Sana, Melissa Bessaha, Kathleen Scarbrough, Jessica Younger, and Wei Hou. 2023. "Self-Reported Depression and Anxiety among Graduate Students during the COVID-19 Pandemic: Examining Risk and Protective Factors" Sustainability 15, no. 8: 6817. https://doi.org/10.3390/su15086817
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Psychol Res Behav Manag
Prevalence and associated factors of depression and anxiety among doctoral students: the mediating effect of mentoring relationships on the association between research self-efficacy and depression/anxiety
1 Department of Clinical Epidemiology, Shengjing Hospital of China Medical University, Shenyang, China, gro.latipsoh-js@hyoahz
2 Department of Library and Medical Information, China Medical University, Shenyang, China
3 Department of Social Medicine, School of Public Health, China Medical University, Shenyang, China
4 Key Laboratory of Immunodermatology, Ministry of Health and Ministry of Education, China Medical University, Shenyang, China
5 Department of Dermatology, First Hospital of China Medical University, Shenyang, China
Weiqiu Wang
Shanshan jia.
6 Key Laboratory of Health Ministry for Congenital Malformation, Shengjing Hospital of China Medical University, Shenyang, China
Deshu Shang
7 Department of Developmental Cell Biology, Key Laboratory of Medical Cell Biology, Ministry of Education, China Medical University, Shenyang, China
8 Department of Developmental Cell Biology, Cell Biology Division, Key Laboratory of Cell Biology, Ministry of Health, China Medical University, Shenyang, China
Yangguang Shao
9 Department of Cell Biology, Key Laboratory of Cell Biology, National Health Commission of the PRC, China Medical University, Shenyang, China
10 Department of Cell Biology, Key Laboratory of Medical Cell Biology, Ministry of Education, China Medical University, Shenyang, China
Xinwang Zhu
11 Department of Nephrology, First Affiliated Hospital of China Medical University, Shenyang, China
Shengnan Yan
12 Graduate Division, School of Public Health, China Medical University, Shenyang, China
Yuhong Zhao
Although the mental health status of doctoral students deserves attention, few scholars have paid attention to factors related to their mental health problems. We aimed to investigate the prevalence of depression and anxiety in doctoral students and examine possible associated factors. We further aimed to assess whether mentoring relationships mediate the association between research self-efficacy and depression/anxiety.
A cross-sectional study was conducted among 325 doctoral students in a medical university. The Patient Health Questionnaire 9 and Generalized Anxiety Disorder 7 scale were used to assess depression and anxiety. The Research Self-Efficacy Scale was used to measure perceived ability to fulfill various research-related activities. The Advisory Working Alliance Inventory-student version was used to assess mentoring relationships. Linear hierarchical regression analyses were performed to determine if any factors were significantly associated with depression and anxiety. Asymptotic and resampling methods were used to examine whether mentoring played a mediating role.
Approximately 23.7% of participants showed signs of depression, and 20.0% showed signs of anxiety. Grade in school was associated with the degree of depression. The frequency of meeting with a mentor, difficulty in doctoral article publication, and difficulty in balancing work–family–doctoral program was associated with both the level of depression and anxiety. Moreover, research self-efficacy and mentoring relationships had negative relationships with levels of depression and anxiety. We also found that mentoring relationships mediated the correlation between research self-efficacy and depression/anxiety.
The findings suggest that educational experts should pay close attention to the mental health of doctoral students. Active strategies and interventions that promote research self-efficacy and mentoring relationships might be beneficial in preventing or reducing depression and anxiety.
Introduction
Recently, the mental health status of students has become a hot topic in public health, higher education, and research policy. 1 – 3 Depression and anxiety are two of the most common psychological disorders. Researchers have reported depression and anxiety among students in several countries and in numerous disciplines, such as counseling, medicine, law, and psychology. 4 – 14 Depression is defined as a mood that includes a feeling of hopelessness, helplessness, or worthlessness. 2 Anxiety is an emotion characterized by unpleasant inner feelings, which is accompanied by caution, complaints, meditation, nervousness, and worry. 5 Depression and anxiety can affect a person’s behavior, academic performance, and general health, as well as quality of sleep, eating habits, and well-being. 8 In addition, it has been confirmed that depression and psychological distress influence suicidal ideation in undergraduate and graduate students. 15 – 18 However, mental health among doctoral students has been relatively ignored by researchers and educational experts. It has only been in the last 2 years that this topic has begun to attract more and more attention.
A doctoral student’s school career is full of hardships and happiness. Doctoral students frequently feel a sense of urgency, worry, and stress as they work toward their doctoral degrees. In addition to financial support and future employment, doctoral students worry about writing a thesis, publishing papers, and handling relationships with advisors. In recent years, a few scholars have explored the prevalence of mental health problems among PhD students. 3 , 12 , 19 – 21 In 2013, Levecquea et al investigated PhD students in Belgium. They concluded that approximately half the PhD students in Flanders had at least two symptoms, and 32% reported at least four symptoms on the 12-item General Health Questionnaire (GHQ12). 3 According to a 2015 survey at the University of California, approximately half the PhD students in science and engineering were depressed. 12 Springer Nature did a survey of PhD students in 2017, and confirmed that 12% reported seeking help for anxiety or depression caused by PhD studies. 20 A 2018 survey of graduate students via social media revealed that 41% of graduate students scored in the moderate–severe range for anxiety and 39% scored in the moderate–severe range for depression. 21 Doctoral students with mental health issues are more likely to drop out of PhD programs. 22 The high attrition rate in PhD programs caused by the dropout of PhD students with psychological illness is damaging to research institutions and the whole research industry. 23 However, there have been few reports on the mental health of doctoral students in medical universities.
Students in medical schools engage in rigorous medical training. 24 , 25 Previous studies have demonstrated that medical students have more pressure, more burnout, and a greater prevalence of mental health disorders than the general population or students in other disciplines. 26 – 31 Medical training varies considerably by discipline, institution, and country. US and Canadian medical students enter medical education systems after they receive a bachelor’s degree. 32 , 33 In China, students can enter medical schools after graduating from high school (similarly to the UK and France). In general, there is an entrance examination required for students with a master’s degree who would like to study for doctoral degrees. Doctoral students need another 3 years to earn a doctoral degree, allowing for an extension of 3 years. Master’s degree candidates in grade two have the choice to apply for a master–doctor combined-training program (a total of 5 years for a doctoral degree, allowing an extension of 3 years). Doctoral students can be either full-time or part-time students. Part-time doctoral students are those who are studying doctoral courses while working in clinical settings or having another job. As such, for clinical doctoral students, some are still fully engaged in clinical work while earning their doctoral degree, whereas others are temporarily away from clinical work to concentrate on the doctoral program research. It is a bit too much to expect clinical doctoral students to do clinical work and research at the same time throughout their doctoral training.
Sociodemographic variables, such as age, sex, and marital status, have been reported to be associated with the mental health of postgraduate students. 8 , 10 However, sex differences in depression among medical students have also yielded mixed results, showing either no difference or high prevalence among female or male medical students. 27 , 29 , 33 Further exploration among doctoral students is still needed. The execution phase during doctoral study has been shown to be prone to mental health problems among doctoral students. 3 Additionally, researchers have suggested that work–life balance is the key factor related to the mental health problems of postgraduate students. 3 , 21 Employed doctoral students work full time or part time while they are studying for their doctoral degree. In this case, conflict concerns not only balancing family and work but also completing the doctoral program itself. Few scholars have focused on the conflicts among family, work, and a doctoral program. Getting married and raising children also puts a strain on doctoral students. Doing experiments, writing a doctoral thesis, and publishing doctoral qualification papers requires considerable time, energy, and financial resources.
Mentorship effectiveness and mentoring functions are thought to be vital to graduate-student programs. 34 , 35 Mentors have a great responsibility to guide their doctoral students through the doctoral program. Advisor mentoring affects student-research self-efficacy, productivity, and development as a scientist. 36 – 38 Recently, a study explored the effect of a supervisor’s leadership style on the mental health of graduate students. 3 Nearly half the doctoral students who withdrew from the doctoral program reported experiencing insufficient supervision, highlighting the fact that good supervision was important for completing the doctoral program. 39 , 40 A survey in 2018 indicated that a weak relationship with a mentor is a common characteristic of most graduate students who experience anxiety and/or depression. 21
Research self-efficacy refers to the individual’s confidence in the successful completion of various aspects of the scientific research process, 41 such as data collection, performing experimental procedures, and writing papers. 42 Studies have evaluated the important role of research self-efficacy in research training. Self-efficacy is a factor that affects how much effort students spend on research tasks and how long they persist when they experience difficulties. 43 Some universities in the US have used research self-efficacy to evaluate the effects of degree programs on graduate research ability. 44 A study has shown that research self-efficacy can predict the research interest and knowledge of doctoral students. 45 Some researchers have reported that high research self-efficacy is correlated with future research involvement and research productivity. 46 , 47 It was suggested that research self-efficacy could play a mediating role between the research-training environment and scientific research output. Furthermore, the relationship between stress and depression has been shown to be mediated by stress management self-efficacy. 48 Interestingly, the length of student–advisor relationships has been reported to be significantly correlated with student research self-efficacy. 36 Moreover, among agricultural students, research self-efficacy has been found to be negatively associated with research anxiety. 49 Therefore, the higher the students’ research self-efficacy, the lower their research anxiety. However, it is not clear whether scientific research self-efficacy is correlated with levels of generalized anxiety.
In this study, we aimed to investigate the prevalence of depression and anxiety among doctoral students in a medical university in China, determine factors that are associated with depression and anxiety, determine whether mentoring relationships and research self-efficacy are associated with depression and anxiety, and test whether mentoring relationships mediate the association between research self-efficacy and depression/anxiety.
Participants
We recruited doctoral students from October to November 2017 using a combination of snowball sampling and stratified sampling from five medical schools and four affiliated clinical hospitals at a medical university in northeast China. This university has the authority to grant doctoral degrees in six major disciplines (basic medicine, clinical medicine, biology, stomatology, public health and preventive medicine, and nursing), including 49 different majors. Our inclusion criteria were still studying at the medical university, had not yet earned a PhD degree, enrollment in a successive postgraduate and doctoral program, and no history of depression or anxiety before entering medical school. A total of 437 doctoral students (218 male, 219 female) were enrolled. This study received approval from the Committee for Human Trials of China Medical University (CMU17/375/R). Written informed consent was obtained from all participants before they entered the experiment. All questionnaires were filled out anonymously and confidentially.
Sociodemographic and doctoral factors
Doctoral students’ sociodemographic status included age, sex, marital status, children, and income. In addition, we selected some doctoral characteristics that might affect the mental health of doctoral students. We asked participants whether they had been employed before doctoral enrollment. Clinical doctoral students refers to students who were doing clinical work while earning their doctoral degree. Grade was measured assigned to one of four categories (1, first year; 2, second year; 3, third year; 4, fourth year or above). Mentors meet with their doctoral students regularly or irregularly. They come together and analyze the latest literature, discuss the research direction or experimental methods, and revise the thesis. Therefore, the frequency of these meetings can reflect the strength of the relationship from a certain quantitative angle. The frequency with which doctoral students met with mentors was measured with one item: “On average, how often do you meet with your advisor? (1, at least once a week; 2, at least once a month; 3, seldom)”. In most medical universities, doctoral students are required to publish at least one academic paper indexed by the Science Citation Index or Social Science Citation Index. Only when this qualification has been reached are doctoral students able to apply for a doctoral degree. The perceived difficulty in publishing a doctoral qualification paper was assessed by one item: “How much effort do you think it takes to publish doctoral qualification papers? (1, a little bit of effort; 2, some effort; 3, a lot of effort). Considering that the total time and energy of doctoral students is limited, we asked the doctoral students, “Do you have difficulty in balancing work, family, and the PhD program? (1, almost no difficulty; 2, some difficulty; 3, great difficulty)”.
Depression questionnaire
We chose the nine-item Patient Health Questionnaire (PHQ-9) 50 to evaluate depression among doctoral students. Each item is measured on a 4-point Likert-like scale (0, not at all; 3, almost every day) based on the frequency of depression symptoms over the last 2 weeks. Total scores range from 0 to 27. A higher PHQ-9 score represents more serious depression (0–4, none–minimal; 5–9, mild; 10–14, moderate; 15–19, moderately severe; 20–27, severe). In general, a diagnosis of depression can only be arrived at after clinical assessment by a mental health professional. With such questionnaires as the PHQ-9, it has been shown that at certain cutoffs there is good correlation with diagnostic interviews. PHQ-9 scores of 10 or above had a sensitivity of 88% and a specificity of 88% for major depressive disorder. 50 The Chinese version of the PHQ-9 has been used in older people and hospital inpatients, with sound reliability. In the current study, Cronbach’s alpha for the PHQ-9 scale was 0.918.
Anxiety questionnaire
We used the seven item Generalized Anxiety Disorder (GAD-7) to indicate the degree of anxiety among doctoral students. 51 The GAD-7 contains seven items that are rated on a 4-point Likert-like scale (0, not at all; 3, almost every day). The total score ranges from 0 to 21. A higher GAD-7 score indicates more serious anxiety (0–4, none–minimal; 5–9, mild; 10–14, moderate; 15–21, severe). Using a threshold score of 10, the GAD-7 has a sensitivity of 89% and a specificity of 82% for major generalized anxiety disorder. 51 The Chinese version of the GAD-7 has been used in outpatients with satisfactory reliability. In the present study, Cronbach’s alpha for the GAD-7 scale was 0.946.
Mentoring-relationship questionnaire
The 30-item Advisory Working Alliance Inventory-student version (AWAI-S) was used to assess the mentoring relationship from the student’s perspective. 36 This scale is a brief, self-reported measure designed on the basis of the Working Alliance model. Its developer, Schlosser, believed that a favorable supervisory alliance was vital to outcomes. 52 The scale has had good reliability in previous studies. 53 The AWAI-S consists of three domains: rapport (11 items), apprenticeship (14 items), and identification-individuation (5 items). Each item is rated on a 5-point Likert scale (1, strongly disagree; 5, strongly agree). The AWAI-S scale contains 16 reverse-scoring questions. High scores (after reverse scoring) suggest that the advisee has a strong mentoring relationship with the advisor. The internal consistency of AWAI-S scores from previous studies ranged from 0.84 to 0.95 36 , 54 and was 0.95 in this study.
Research Self-Efficacy Scale
The Research Self-Efficacy Scale (RSES) was used to measure the doctoral students’ perceived ability to fulfill various research-related tasks. 55 The RSES comprises 50 items with four subscales: conceptualization (18 items), implementation (19 items), early tasks (5 items), and presenting the results (8 items). Individuals were asked to mark the tasks they perceived they could perform. The strength of each item was rated on a 10-point scale ranging from 0 (no confidence) to 10 (complete confidence). A total RSES score was calculated, ranging from 75 to 500. A higher score indicates higher self-efficacy. The internal consistency of RSES scores was 0.98 in the present study.
Data analysis
We used SPSS 17.0 for all statistical analyses. We investigated demographic and doctoral characteristics using ANOVA for continuous variables and chi-squared for categorical data. Correlations among depression, anxiety, mentoring relationships, and research self-efficacy were examined by Pearson correlation. We performed hierarchical linear regression analysis to explore the association of mentoring relationship and research self-efficacy with depression/anxiety. In this study, depression and anxiety were modeled as dependent variables, RSES as an independent variable, AWAI-S as a mediator, and sociodemographic and doctoral variables as controlled variables. In step 1 of the regression, sociodemographic and doctoral variables were entered as controlled variables. Because linear hierarchical regression analysis requires continuous variables, the grade, frequency of meeting with a mentor, difficulty in publishing a doctoral qualification paper, and difficulty in balancing work–family–doctoral program was dummy coded. In step 2 of the regression, research self-efficacy was added. In step 3, the mentoring relationship was added. The asymptotic and resampling method was used to examine mentoring relationship as potential mediator in the association between research self-efficacy and depression/anxiety, based on 5,000 bootstrap samples. 56 A bias-corrected and accelerated (BC a ) 95% CI was used to estimate mediation. If the BC a 95% CI excludes 0, this indicates that the mediation is significant. All statistical tests were two-sided (α=0.05). P <0.05 was considered statistically significant.
Sociodemographic and doctoral characteristics of respondents
After exclusion of 45 doctoral students who refused to fill out questionnaires, the 392 who completed the questionnaires were included. A total of 67 questionnaires with missing values >10% were deemed invalid. As such, we collected 325 valid responses. The effective response rate was 74.37%. The mean age of the participants was 31.1±5.3 (23–47) years. Of the 325 respondents, 60.3% were female, 50.8% married or lived with a partner, and 40% had one or more child. The monthly income for 56.6% of respondents was <CN¥3,000 per month (equivalent of local per capita income), 50.8% had been employed before doctoral enrollment, and 40.6% were clinical doctoral students. Furthermore, 13.8% seldom met with their mentors, 37.2% thought they should try their best to publish a PhD qualification paper, and 31.1% reported that they had difficulty in balancing work–family–PhD ( Table 1 ).
Sociodemographic and doctoral characteristics of respondents (n=325)
| Characteristics | n | % |
|---|---|---|
| 325 | ||
| Age (years) | ||
| ≤25 | 30 | 9.2 |
| 26–30 | 151 | 46.5 |
| ≥31 | 144 | 44.3 |
| Sex | ||
| Male | 129 | 39.7 |
| Female | 196 | 60.3 |
| Marital status | ||
| Married/living with partner | 165 | 50.8 |
| Single/widowed/divorced | 160 | 49.2 |
| Have children | ||
| No | 195 | 60 |
| One or more | 130 | 40 |
| Income (CN¥ per month) | ||
| ≤3,000 | 184 | 56.6 |
| 3,001–5,000 | 30 | 9.2 |
| ≥5,001 | 111 | 34.2 |
| Employment before doctoral enrollment | ||
| No | 160 | 49.2 |
| Yes | 165 | 50.8 |
| Clinical doctoral student | ||
| No | 193 | 59.4 |
| Yes | 132 | 40.6 |
| Grade | ||
| First year | 71 | 21.8 |
| Second year | 121 | 37.2 |
| Third year | 116 | 35.7 |
| Fourth year or above | 17 | 5.23 |
| Frequency of meeting with mentor | ||
| At least once a week | 193 | 59.4 |
| At least once a month | 87 | 26.8 |
| Seldom | 45 | 13.8 |
| Difficulty in publishing doctoral qualification paper | ||
| A little bit of effort | 56 | 17.2 |
| Some effort | 148 | 45.5 |
| A lot of effort | 121 | 37.2 |
| Difficulty in balancing work–family–doctoral program | ||
| Almost no difficulty | 98 | 30.2 |
| Some difficulty | 126 | 38.8 |
| Great difficulty | 101 | 31.1 |
Sociodemographic and doctoral characteristics by depression and anxiety
The prevalence of clinical depression was 23.7% (moderate, moderately severe, and severe) and the prevalence of clinical anxiety was 20.0% (moderate and severe; Tables 2 and and3). 3 ). Factors that were significantly different among respondents at varying levels of depression included age, marital status, having children, employment, grade, frequency of meeting with mentors, difficulty in publishing, and difficulty in balancing work–family–doctoral program. Factors that were significantly different among respondents at varying levels of anxiety included being a clinical doctoral student, frequency of meeting with mentors, difficulty in publishing, and difficulty in balancing work–family–doctoral program.
Sociodemographic and doctoral characteristics by depression (n=325)
| Characteristics | Depression | |||||
|---|---|---|---|---|---|---|
| None–minimal (n=114) | Mild (n=134) | Moderate (n=38) | Moderately severe (n=26) | Severe (n=13) | -value | |
| Age (years), n (%) | 0.023 | |||||
| ≤25 | 15 (50.0) | 11 (36.7) | 3 (10.0) | 1 (3.3) | 0 | |
| 26–30 | 57 (37.7) | 60 (39.7) | 21 (13.9) | 7 (4.6) | 6 (4.0) | |
| ≥31 | 42 (29.2) | 63 (43.8) | 14 (9.7) | 18 (12.5) | 7 (4.9) | |
| Sex, n (%) | 0.475 | |||||
| Male | 45 (34.9) | 51 (39.5) | 20 (15.5) | 9 (7.0) | 4 (3.1) | |
| Female | 69 (35.2) | 83 (42.3) | 18 (9.2) | 17 (8.7) | 9 (4.6) | |
| Marital status, n (%) | 0.016 | |||||
| Married/living with partner | 52 (31.5) | 71 (43.0) | 14 (8.5) | 20 (12.1) | 8 (4.8) | |
| Single/widowed/divorced | 62 (38.8) | 63 (39.4) | 24 (15.0) | 6 (3.8) | 5 (3.1) | |
| Have children, n (%) | 0.002 | |||||
| No | 79 (40.5) | 74 (37.9) | 27 (13.8) | 8 (4.2) | 7 (3.6) | |
| One or more | 35 (26.9) | 60 (46.2) | 11 (8.5) | 18 (13.8) | 6 (4.6) | |
| Income (CN¥ per month), n (%) | 0.982 | |||||
| ≤3,000 | 69 (37.5) | 72 (39.1) | 25 (13.6) | 11 (6.0) | 7 (3.8) | |
| 3,001–5,000 | 13 (43.3) | 10 (33.3) | 2 (6.7) | 2 (6.7) | 3 (10.0) | |
| ≥5,001 | 32 (28.8) | 52 (46.8) | 11 (9.9) | 13 (11.7) | 3 (2.7) | |
| Employment before doctoral enrollment, n (%) | 0.021 | |||||
| No | 68 (42.5) | 57 (35.6) | 21 (13.1) | 8 (5.0) | 6 (3.8) | |
| Yes | 46 (27.9) | 77 (46.7) | 17 (10.3) | 18 (10.9) | 7 (4.2) | |
| Clinical doctoral students, n (%) | 0.221 | |||||
| No | 74 (38.3) | 79 (40.9) | 23 (11.9) | 12 (6.2) | 5 (2.6) | |
| Yes | 40 (30.3) | 55 (41.7) | 15 (11.4) | 14 (10.6) | 8 (6.0) | |
| Grade, n (%) | 0.040 | |||||
| First year | 37 (52.1) | 20 (28.2) | 10 (14.1) | 2 (2.8) | 2 (2.8) | |
| Second year | 42 (34.7) | 54 (44.6) | 11 (9.1) | 9 (7.4) | 5 (4.1) | |
| Third year | 32 (27.6) | 53 (45.7) | 14 (12.1) | 13 (11.2) | 4 (3.4) | |
| Fourth year or above | 3 (17.6) | 7 (41.2) | 3 (17.6) | 2 (11.8) | 2 (11.8) | |
| Frequency of meeting with mentor, n (%) | 0.090 | |||||
| At least once a week | 79 (40.9) | 78 (40.4) | 20 (10.4) | 10 (5.2) | 6 (3.1) | |
| At least once a month | 25 (28.7) | 38 (43.7) | 10 (11.5) | 9 (10.3) | 5 (5.7) | |
| Seldom | 10 (22.2) | 18 (40.0) | 8 (17.8) | 7 (15.6) | 2 (4.4) | |
| Difficulty in publishing doctoral qualification paper, n (%) | <0.001 | |||||
| A little bit of effort | 33 (58.9) | 19 (33.9) | 1 (1.8) | 3 (5.4) | 0 | |
| Some effort | 52 (35.1) | 66 (44.6) | 19 (12.8) | 6 (4.1) | 5 (3.4) | |
| A lot of effort | 29 (24.0) | 49 (40.5) | 18 (14.9) | 17 (14.0) | 8 (6.6) | |
| Difficulty in balancing work–family–doctoral program, n (%) | 0.001 | |||||
| Almost none | 51 (52.0) | 35 (35.7) | 7 (7.1) | 4 (4.1) | 1 (1.0) | |
| Some | 36 (28.6) | 59 (46.8) | 18 (14.3) | 8 (6.3) | 5 (4.0) | |
| Great | 27 (26.7) | 40 (39.6) | 13 (12.9) | 14 (13.9) | 7 (6.9) | |
Sociodemographic and doctoral characteristics by anxiety (n=325)
| Characteristics | Anxiety | ||||
|---|---|---|---|---|---|
| None–minimal (n=151) | Mild (n=109) | Moderate (n=42) | Severe (n=23) | -value | |
| Age (years), n (%) | 0.114 | ||||
| ≤25 | 18 (60.0) | 9 (30.0) | 3 (10.0) | 0 | |
| 26–30 | 68 (45.0) | 55 (36.4) | 19 (12.6) | 9 (6.0) | |
| ≥31 | 65 (45.1) | 45 (31.3) | 20 (13.9) | 14 (9.7) | |
| Sex, n (%) | 0.801 | ||||
| Male | 61 (47.3) | 41 (31.8) | 19 (14.7) | 8 (6.2) | |
| Female | 90 (45.9) | 68 (34.7) | 23 (11.7) | 15 (7.7) | |
| Marital status, n (%) | 0.249 | ||||
| Married/living with partner | 74 (44.8) | 52 (31.5) | 23 (13.9) | 16 (9.7) | |
| Single/widowed/divorced | 77 (48.1) | 57 (35.6) | 19 (11.9) | 7 (4.4) | |
| Have children, n (%) | 0.265 | ||||
| No | 95 (48.7) | 68 (34.9) | 21 (10.8) | 11 (5.6) | |
| One or more | 56 (43.1) | 41 (31.5) | 21 (16.2) | 12 (9.2) | |
| Income (CN¥ per month), n (%) | 0.883 | ||||
| ≤3,000 | 87 (47.3) | 61 (33.2) | 25 (13.6) | 11 (6.0) | |
| 3,001–5,000 | 13 (43.3) | 10 (33.3) | 3 (10.0) | 4 (13.3) | |
| ≥5,001 | 51 (45.9) | 38 (34.2) | 14 (12.6) | 8 (7.2) | |
| Employment before doctoral enrollment, n (%) | 0.429 | ||||
| No | 79 (49.4) | 54 (33.8) | 19 (11.9) | 8 (5.0) | |
| Yes | 72 (43.6) | 55 (33.3) | 23 (13.9) | 15 (9.1) | |
| Clinical doctoral students, n (%) | 0.030 | ||||
| No | 97 (50.3) | 67 (34.7) | 21 (10.9) | 8 (4.1) | |
| Yes | 54 (40.9) | 42 (31.8) | 21 (15.9) | 15 (11.4) | |
| Grade, n (%) | 0.525 | ||||
| First year | 41 (57.7) | 19 (26.7) | 8 (11.3) | 3 (4.2) | |
| Second year | 54 (44.6) | 43 (35.5) | 14 (11.6) | 10 (8.3) | |
| Third year | 49 (42.2) | 43 (37.1) | 16 (13.8) | 8 (6.9) | |
| Fourth year or above | 7 (41.2) | 4 (23.5) | 4 (23.5) | 2 (11.8) | |
| Frequency of meeting with mentor, n (%) | 0.017 | ||||
| At least once a week | 106 (54.9) | 58 (30.1) | 19 (9.8) | 10 (5.2) | |
| At least once a month | 28 (32.2) | 34 (39.1) | 16 (18.4) | 9 (10.3) | |
| Seldom | 17 (37.8) | 17 (37.8) | 7 (15.6) | 4 (8.9) | |
| Difficulty in publishing doctoral qualification paper, n (%) | <0.001 | ||||
| A little bit of effort | 36 (64.3) | 17 (30.4) | 3 (5.4) | 0 | |
| Some effort | 73 (49.3) | 54 (36.5) | 14 (9.5) | 7 (4.7) | |
| A lot of effort | 42 (34.7) | 38 (31.4) | 25 (20.7) | 16 (13.2) | |
| Difficulty in balancing work–family–doctoral program (n,%) | 0.001 | ||||
| Almost none | 58 (59.2) | 30 (30.6) | 9 (9.2) | 1 (1.0) | |
| Some | 58 (46.0) | 45 (35.7) | 16 (12.7) | 7 (5.6) | |
| Great | 35 (34.7) | 34 (33.7) | 17 (16.8) | 15 (14.9) | |
Means and correlations among age and PHQ-9, GAD-7, AWAI-S, and RSES scores
Mean scores for the PHQ-9, GAD-7, and AWAI-S and their correlations with each other and age are presented in Table 4 . Age was positively associated with the PHQ-9. However, there was no significant effect of age on the GAD-7. Both PHQ-9 and GAD-7 scores were negatively associated with AWAI-S and RSES scores.
Correlations among age, AWAI-S, RSES, PHQ-9, and GAD-7 scores
| Continuous variables | Mean | SD | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|---|
| Age (years) | 31.09 | 5.27 | 1 | ||||
| AWAI-S | 113.9 | 18.53 | −0.046 | 1 | |||
| RSES | 329.8 | 68.74 | −0.153 | 0.300 | 1 | ||
| PHQ-9 | 7.32 | 5.92 | 0.110 | −0.328 | −0.293 | 1 | |
| GAD-7 | 5.85 | 5.44 | 0.061 | −0.311 | −0.325 | 0.880 | 1 |
Abbreviations: AWAI-S, Advisory Working Alliance Inventory-student version; GAD, Generalized Anxiety Disorder; PHQ, Patient Health Questionnaire; RSES, Research Self-Efficacy Scale.
Associations of mentoring relationship and research self-efficacy with depression/anxiety
As shown in Tables 5 and and6, 6 , sociodemographic and doctoral variables contributed to 17.7% of the variance in PHQ-9 scores and to 18.3% of the variance in GAD-7 scores. Doctoral students in their fourth year had greater PHQ-9 and GAD-7 scores than first-year doctoral students. Compared with those who met with their mentors at least once a week, doctoral students who met with their mentors only once a month had higher PHQ-9 and GAD-7 scores. Moreover, respondents who reported that they had to try their best to publish doctoral qualification papers had higher PHQ-9 and GAD-7 scores than those who felt they only had to put forth a little effort. Finally, doctoral students who had great difficulty in balancing work–family–doctoral program exhibited a higher level of depression and anxiety than those who had almost no difficulty.
Factors related to depression using hierarchical regression analysis
| Controlled, dependent and mediating variables in the three Step Regression | PHQ-9 scores | ||
|---|---|---|---|
| Step 1 (b) | Step 2 (b) | Step 3 (b) | |
| Age (years) | −0.105 | −0.078 | −0.098 |
| Have children | 0.035 | 0.044 | 0.112 |
| Employment before doctoral enrollment | −0.024 | −0.071 | −0.080 |
| Clinical doctoral students | 0.067 | 0.042 | 0.063 |
| Grade | |||
| Second year vs first year | 0.023 | 0.029 | 0.011 |
| Third year vs first year | 0.044 | 0.042 | 0.008 |
| Fourth year or above vs first year | 0.136 | 0.147 | 0.129 |
| Frequency of meeting with mentor | |||
| At least once a month vs at least once a week | 0.133 | 0.121 | 0.118 |
| Seldom vs at least once a week | 0.119 | 0.093 | 0.049 |
| Difficulty in publishing doctoral qualification paper | |||
| Some effort vs a little bit of effort | 0.141 | 0.130 | 0.084 |
| A lot of effort vs a little bit of effort | 0.325 | 0.276 | 0.265 |
| Difficulty in balancing work–family–doctoral program | |||
| Some vs almost none | 0.161 | 0.141 | 0.118 |
| Great vs almost none | 0.256 | 0.231 | 0.195 |
| RSES | −0.211 | −0.136 | |
| AWAI-S | −0.257 | ||
| 5.054 | 5.958 | 7.419 | |
| Adjusted | 0.142 | 0.179 | 0.232 |
| ∆ | 0.177 | 0.038 | 0.053 |
Abbreviation: PHQ, Patient Health Questionnaire.
Factors related to anxiety using hierarchical regression analysis
| Controlled, dependent and mediating variables in the three Step Regression | GAD-7 scores | ||
|---|---|---|---|
| Step 1 (b) | Step 2 (b) | Step 3 (b) | |
| Age (years) | −0.170 | −0.139 | −0.158 |
| Have children | −0.003 | 0.007 | 0.072 |
| Employment before doctoral enrollment | 0.008 | −0.046 | −0.055 |
| Clinical doctoral students | 0.107 | 0.078 | 0.099 |
| Grade | |||
| Second year vs first year | 0.007 | 0.015 | −0.003 |
| Third year vs first year | 0.011 | 0.009 | −0.024 |
| Fourth year or above vs first year | 0.129 | 0.142 | 0.125 |
| Frequency of meeting mentor | |||
| At least once a month vs at least once a week | 0.163 | 0.150 | 0.147 |
| Seldom vs at least once a week | 0.091 | 0.060 | 0.018 |
| Difficulty in publishing doctoral qualification paper | |||
| Some effort vs a little bit of effort | 0.128 | 0.115 | 0.072 |
| A lot of effort vs a little bit of effort | 0.314 | 0.258 | 0.247 |
| Difficulty in balancing work–family–doctoral program | |||
| Some vs almost none | 0.151 | 0.128 | 0.107 |
| Great vs almost none | 0.288 | 0.260 | 0.225 |
| RSES | −0.242 | −0.170 | |
| AWAI-S | −0.246 | ||
| 5.262 | 6.614 | 7.940 | |
| Adjusted | 0.148 | 0.198 | 0.247 |
| ∆ | 0.183 | 0.050 | 0.049 |
Abbreviation: GAD, Generalized Anxiety Disorder.
After adjustment for controlled variables, the RSES was negatively associated with depression ( b =−0.211, P <0.001) and anxiety ( b =−0.242, P <0.001), and accounted for 3.8% of the variance for depression and 5.0% of the variance for anxiety. In step 3, the AWAI-S was negatively associated with depression ( b =−0.257, P <0.001) and anxiety ( b =−0.246, P <0.001), and accounted for 5.3% of the variance for depression and 4.9% of the variance for anxiety. In step 3, when the AWAI-S was added, the absolute value of RSES b was diminished. Therefore, the AWAI-S might be a mediator in the association between research self-efficacy and depression/anxiety.
Mediating role of mentoring relationship
As shown in Table 7 and Figure 1 , research self-efficacy had a significantly negative correlation with depression/anxiety (c). Research self-efficacy correlated with the mentoring relationship (a). Mentoring relationship correlated with depression/anxiety negatively (b). BC a 95% CI for a×b of the mentoring relationship did not include 0, indicating that mentoring relationship partially mediated the relationship between research self-efficacy and depression/anxiety (c’). Mentoring relationship explained 37.68% of the variance for depression and 29.73% of the variance for anxiety.

Theoretical model through which mentoring relationship mediates association between research self-efficacy and depression/anxiety.
Notes: c, Association between research a elf-efficacy and depression/anxiety; a, association between research self-efficacy and mentoring relationship; b, association between mentoring relationship and depression/anxiety; c’, association between research self-efficacy and depression/anxiety after adding mentoring relationship as a mediator. * P <0.05; ** P <0.01; *** P <0.001.
Bootstrapping test of indirect effect of mentoring relationship acting as mediator on association between research self-efficacy and depression/anxiety
| Model | Y | c | a | b | c′ | a×b (BC 95% CI) |
|---|---|---|---|---|---|---|
| PHQ-9 | −0.2065 | 0.2993 | −0.2598 | −0.1288 | −0.0778 (−0.1315 to −0.0388) | |
| GAD-7 | −0.2439 | 0.2993 | −0.2424 | −0.1713 | −0.0725 (−0.1227 to −0.0353) |
Notes: a×b, indirect effect of research self-efficacy on depression/anxiety via mediator mentoring relationship; c, association between research self-efficacy and depression/anxiety; a, association between research self-efficacy and mentoring relationship; b, association between mentoring relationship and depression/anxiety; c’, association between research self-efficacy and depression/anxiety after adding mentoring relationship as mediator.
Abbreviations: BC a , bias-corrected and accelerated; GAD, Generalized Anxiety Disorder; PHQ, Patient Health Questionnaire.
We found that depression and anxiety symptoms are common among doctoral students in medical universities. Approximately 41.2% of doctoral students showed symptoms of mild depression and 23.7% showed signs of moderate–severe depression. Moreover, 33.5% of the students had mild anxiety symptoms and 20.0% had moderate–severe anxiety symptoms. Researchers worldwide have used the same scales to carry out epidemiological surveys on depression and/or anxiety. An investigation indicated that 53.8% of undergraduate college students at Emory University had moderate–severe depression. 57 In 2017, it was reported that 29.2% of medical students in Nepal had moderate–severe depression. 58 Evans et al conducted a survey that included 90% PhD students and 10% master’s students. Results suggested that 39% of postgraduates had moderate–severe depression and 41% moderate–severe anxiety. 21 Differences in terms of score and positive rate might be related to differing methodologies. Levesque et al found that 33.33% of doctoral students experienced a common psychiatric disorder (GHQ12), such as depression. A PhD candidate was 2.4 times more likely to develop psychiatric health problems than someone in the general population with a bachelor’s degree. 3 Bernstein reported that 42% of PhD students in science and 48% of PhD students in engineering at the University of California were depressed on the Center for Epidemiologic Studies Depression Scale. 12 The psychological stress of medical doctoral students is much higher than that of students with other majors, and students in medical schools have more symptoms of depression than the general population. 26 , 29 However, few reports have focused on the mental health of doctoral students in Chinese medical universities.
Research self-efficacy negatively correlated with depression and anxiety. However, few researchers have reported such an association. Mee found that self-efficacy mediated the relationship between smoking behavior and depression. 59 Pu et al verified that dispositional optimism partially mediated the relationship between self-efficacy and depression. 60 Razavi et al reported a negative relationship between self-efficacy (General Self-Efficacy Questionnaire) and research anxiety among master’s and PhD students at Islamic Azad University. 61 In addition, we found that research self-efficacy (RSES) and mentoring relationship (AWAI-S) correlated significantly. This result was consistent with a previous study. 64 Research self-efficacy has often been studied in relation to research-training environments and research productivity. 47 , 62 Lambie et al found that among PhD students, research self-efficacy was associated with research interest and knowledge. 45
Our study indicated that the association between research self-efficacy and depression/anxiety was partly mediated by the mentoring relationship. As for strategies for promoting research self-efficacy of doctoral students, Overall et al found that high levels of autonomy and strong levels of academic support were associated with higher levels of research self-efficacy. Likewise, students with lower research self-efficacy experienced lower levels of autonomy and lower levels of personal support. 44 Love et al reported that supportive peers or supervisors contributed to positive research experience. Positive team-research experiences were able to predict research self-efficacy. 63 As such, the correlation between mentoring relationship and research self-efficacy might be bidirectional.
Our results also indicated that mentoring relationship correlated with depression and anxiety. Studies suggest that the mentoring relationship is positively correlated with research self-efficacy and negatively correlated with student stress. 53 , 54 , 64 , 65 Peluso et al found that the academic advisor relationship played a role in protecting the mental health of experimental psychology students in Canada. 10 Gottschall also showed a significant association between a harmonious mentoring relationship (RHI-M subscale) and decreased depressive symptoms among Canadian graduate students. 66 In addition, Lunsford suggested that mentoring by doctoral advisors correlated with student outcomes, including satisfaction and academic production. 37
Most importantly, we found that mentoring relationship mediated the correlation between research self-efficacy and depression/anxiety. As far as we know, this issue has not been studied before. The empirical findings in this study have very important applications for general doctoral training strategies and specific interventions for depression and anxiety. The mediating effect suggests that active strategies and interventions that promote research self-efficacy and mentoring relationships might benefit the mental health of doctoral students. Developing courses related to choosing research topics, performing experiments, analyzing data, and writing papers are good strategies for improving research self-efficacy. We should encourage doctoral students to participate in research practices and academic exchange. In addition, we should monitor mentoring relationships, depression, and anxiety by mixed methods at regular intervals, with students’ permission. If we find poor relationships between mentors and their mentees, we must recognize this issue’s importance and adopt flexible methods to deal with it. For example, we should allow the student to change mentors or give them more research support from another faculty.
The percentage of scores that could be categorized as depression and anxiety in the fourth year or above was higher than that in any other grade. Senior students might face more pressure from the institution, the need to graduate, financial burdens, and finding a job than is faced by more junior students. Our findings are in line with a survey in Vietnam, which indicated that major depression and general anxiety rates of medical students were higher in the fifth grade than in the first grade. 67 In contrast, a study of undergraduates in Brazil discovered that 30.8% of first-year students and 9.4% of sixth-year students presented anxiety. 68 Levecque et al observed that mental health problems were more prevalent at the beginning of the PhD program than in the execution phase. This difference with our results could be due to cross-cultural differences in training systems and graduation requirements.
The frequency with which mentees met with their mentors showed a significant relationship with depression and anxiety. This measure is a function of the mentors in terms of quantity. Under great academic pressure, doctoral students who often met with their mentors were less stressed than those who seldom met with their mentors. An ideal situation is that the advisor is accessible at almost all times. Besides weekly group meetings, students should schedule a weekly one-on-one session with an advisor. Students who meet less frequently with their mentor are more likely to be depressed when they encounter difficulties. Moreover, the duration of each meeting and the content of the meeting might also play a vital role in completion of the doctoral program.
Our results also suggest that difficulty in publishing a doctoral qualification paper has a significant effect on depression and anxiety. This has also become one of the main factors preventing students from completing the doctoral degree. Certainly, doctoral students who have greater academic self-efficacy might have less academic pressure and a low risk of mental health problems. In recent years, many policies have been implemented to increase the number of doctoral students enrolled, develop master–doctor combined programs, and expand the requirements for a doctoral degree. However, the cultivation of mentoring ability, availability of funding for doctor training, and assistance for doctoral students in mastering experiments and writing papers are still lacking. Such problems might not only be related to increasing the risk of mental health disorders but might also correlate with deferred graduation, increased dropout rates, and academic misconduct.
Finally, it has been shown that doctoral students who have difficulty in balancing work–family–doctoral program will have a greater risk of depression and anxiety than those who have almost no difficulty. An imbalance among family, work, and doctoral program places great pressure on doctoral students and seriously hampers their progress in doctoral programs, which leads to poorer mental health and even poorer physical health. Although the effect of work–life balance on mental health has been identified in the past, 69 , 70 only in recent years has work–life–doctoral program balance been taken seriously. Sapey, a scientist in the UK, has pointed out that work–life balance in academia is a challenge for her. 71 – 73 She said that she has balanced two vocations (clinical and academic work) and a family (mother of a child), sometimes very badly, sometimes reasonably, and only very, very occasionally has she handled it very well. Is there any successful family–work–doctoral program balance experience from which to learn? Bellucci and Nancy performed a qualitative investigation of PhD nursing students in the US, and suggested that multiple time management and stress management strategies would play a crucial role in balancing the responsibilities of work, family, and a PhD program. 74 Martinez et al interviewed full-time doctoral education students and categorized balancing school–work–life into four themes: purposeful management, well-being, support, and tradeoffs. 75
Limitations
Several limitations of this study should be mentioned. First, we performed only an exploratory survey of doctoral students in a medical university. We will perform a multicenter investigation in multiple cities in the future. Second, it was a cross-sectional study. The results of this study did not reveal causality. We expect to conduct a longitudinal study on associated themes. Further studies should include qualitative measures as well.
Our study has provided insight into the prevalence and factors associated with depression and anxiety among doctoral students in China. Our study revealed that 23.7% of doctoral students showed signs of depression and 20.0% signs of anxiety. Our findings indicated that research self-efficacy and mentoring relationships were protective factors for depression and anxiety. Mentoring relationship mediated the association between research self-efficacy and depression/anxiety. In addition, we revealed that the frequency of meeting with mentors, difficulty in publishing a doctoral qualification paper, and difficulty in balancing work–family–doctoral program were significantly associated with both depression and anxiety. Our findings also indicated that year in school was also associated with depression and anxiety. These findings suggest that policymakers and managers in medical universities should pay close attention to the mental health of doctoral students. Potential interventions might include (but are not limited to) promoting research self-efficacy of doctoral students, monitoring the mentoring relationship, and developing courses that teach how to perform various tasks necessary for obtaining a doctoral degree.
Acknowledgments
This study was funded by the Liaoning Province Education Science 13th Five-Year Plan 2017 of China (No. JG17DB564) and the National Natural Science Foundation of China (No. 71473268). We would like to thank the experts who have offered us constructive suggestions. We would like to acknowledge all the faculty and students for their great help in distributing questionnaires and collecting data.
The authors report no conflicts of interest in this work.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Research disruption during PhD studies and its impact on mental health: Implications for research and university policy
Contributed equally to this work with: Maria Aristeidou, Angela Aristidou
Roles Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Institute for Educational Technology, The Open University, Milton Keynes, Buckinghamshire, United Kingdom
Roles Conceptualization, Investigation, Resources, Writing – original draft, Writing – review & editing
Affiliation UCL School of Management, London, United Kingdom
- Maria Aristeidou,
- Angela Aristidou

- Published: October 18, 2023
- https://doi.org/10.1371/journal.pone.0291555
- Reader Comments
Research policy observers are increasingly concerned about the impact of the disruption caused by the Covid-19 pandemic on university research. Yet we know little about the effect of this disruption, specifically on PhD students, their mental health, and their research progress. This study drew from survey responses of UK PhD students during the Covid-19 pandemic. We explored evidence of depression and coping behaviour (N = 1780) , and assessed factors relating to demographics, PhD characteristics, Covid-19-associated personal circumstances, and significant life events that could explain PhD student depression during the research disruption (N = 1433) . The majority of the study population (86%) reported a negative effect on their research progress during the pandemic. Results based on eight mental health symptoms (PHQ-8) showed that three in four PhD students experienced significant depression. Live-in children and lack of funding were among the most significant factors associated with developing depression. Engaging in approach coping behaviours (i.e., those alleviating the problem directly) related to lower levels of depression. By assessing the impact of research disruption on the UK PhD researcher community, our findings indicate policies to manage short-term risks but also build resilience in academic communities against current and future disruptions.
Citation: Aristeidou M, Aristidou A (2023) Research disruption during PhD studies and its impact on mental health: Implications for research and university policy. PLoS ONE 18(10): e0291555. https://doi.org/10.1371/journal.pone.0291555
Editor: Yadeta Alemayehu, Mettu University, ETHIOPIA
Received: January 23, 2023; Accepted: August 31, 2023; Published: October 18, 2023
Copyright: © 2023 Aristeidou, Aristidou. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: PLOS is discussing with the authors issues pertaining to data availability; in the meantime, requests about underlying data should be sent to the corresponding author.
Funding: This work was supported by the Institute of Educational Technology at The Open University (MA) and the University College London (UCL) School of Management (AA). Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the funders. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Introduction
The abrupt outbreak in January 2020 and the global proliferation of a novel virus (Covid-19) has created a crisis for many sectors, including the international higher education (HE) sector [ 1 ] that continues during the ‘post-pandemic’ period. A point of particular alarm for HE leaders, policy observers, and governments is the disruption to the typical flow and pace of university research activity. While research related to Covid-19 is still in overdrive, other research was slowed or stopped due to worldwide physical distancing measures to contain the virus’ spread (e.g., sudden campus and laboratory closures, mobility restrictions, stay-at-home orders) [ 2 ]. The resulting ‘drop in research work’ is suggested to have a detrimental impact on the HE sector on the ‘research and innovation pipeline’ [ 3 ], and on ‘research capacity, innovation and research impact’ [ 4 ].
As research and university policies internationally are being (re)shaped at a rapid pace in efforts to meet the challenge of university research disruption [ 5 ], we contribute to academic and policy conversations by examining the effect of the research disruption on the mental health of PhD students. A considerable body of research acknowledges the role of PhD students in the innovation process, in knowledge creation and diffusion (e.g., [ 6 ]) and further posits that the period of one’s PhD program is key to early career success and research productivity (e.g., [ 7 ]). These outcomes, which matter to research policy, have been linked to PhD student mental health [ 8 – 10 ]. In those times of relative stability, research had additionally demonstrated the higher prevalence of mental health issues amongst the PhD student population across research disciplines, as compared to other students within academia [ 9 ] and the general population [ 9 , 11 , 12 ]. In the period since Covid-19 disrupted our social and economic lives, depression levels in the general population have been exacerbated globally [ 13 , 14 ]. These trends suggested that the already high prevalence of poor mental health in PhD students is likely to be further exacerbated during the pandemic. Indeed, as reported in early studies on research students’ experience of the Covid-19 pandemic (e.g., [ 15 ]) and the post-pandemic period (e.g., [ 16 ]) the impact on students’ mental wellbeing has been significant, with students suggesting a number of support measures at institutional and national level.
Ignoring, at this critical moment, the increased likelihood of poor mental health in PhD students may jeopardize research capacity and HE competitiveness for years to come. Therefore, there is a pressing need to identify–within the PhD student population–those whose mental health is more affected by the research disruption, so that policies and assistance can be timelier and more targeted. Additionally, by understanding more clearly the factors that may contribute to poor mental health, and their interrelationships (presented in Methods), policymakers and HE leaders may be better placed to tackle, and ultimately overcome, this and future research disruptions.
Motivated by the current lack of an empirical basis for insights into PhD students’ mental health during the pandemic-induced disruption, we collected survey data contemporaneously during July 2020. Our 1780 survey respondents are PhD students in 94 UK Universities, across the natural and social sciences and across PhD stages. Our study has three objectives: first, to explore mental health prevalence (depression) and coping behaviour in a large-scale representative sample of PhD students in the UK (O1); second, to evaluate the relationships among mental health prevalence and coping behaviour (O2); third, to identify factors that increase the likelihood of poor PhD student mental health during the period of research disruption (O3). Our study extends previous research on mental health in the HE sector by considering the dynamics of severe disruption, as opposed to the dynamics of relative stability, on PhD students’ mental health, performance satisfaction, and coping behaviours.
Background and literature review
Uk phd students’ mental health in times of disruption.
In the UK, there are approximately 100,000 postgraduate students completing doctoral research [ 17 ]. Since 2018, significant government funding has been targeted at developing insights into supporting UK PhD students’ mental health [ 18 ]. Still, with the exception of Byrom et al. [ 11 ], published research on PhD students’ mental health in the UK exhibits the same limitations as the international research: It reflects discipline- or institution-related specificity (e.g., [ 19 ]) or utilizes samples of early career researchers in general (e.g., [ 20 ]).
Early findings on postgraduate research students’ wellbeing during the pandemic showed that only a small proportion of them are in good mental health wellbeing (28%) while the rest demonstrate possible or probable depression or anxiety [ 15 ]. Goldstone and Zhang [ 15 ] further highlight the differences among student groups with, for example, students with disabilities or caring responsibilities or female students having lower levels of mental wellbeing. The post-pandemic findings have been more promising, as only about one in four students were at risk of experiencing mental health issues [ 16 ].
In response to the Covid-19 research disruption, substantive actions have been taken by the HE sector and the UK Government to disseminate approaches deployed by UK universities to support student mental health (e.g., [ 18 ]) and to update mental health frameworks for UK universities (e.g., [ 4 ]), but so far, mitigation activities have been targeting mental health for UK university students broadly, not UK PhD students specifically.
Overcoming the paucity of evidence on UK PhD students’ mental health during the pandemic is a crucial first step to drawing strong conclusions on the prevalence and determinants of mental health issues and ways to mitigate them specific to the PhD population. For example, policy recommendations by UK postgraduate respondents during the pandemic [ 15 ] focused mainly on financial support, such as extensions to their funded period of study and tuition and visa fee support (including waivers to fees). To develop an overarching framework specific to the Objectives of our study, we synthesize insights from the international literature on PhD student mental health conducted in the period before the research disruption.
International research on PhD student mental health in times of relative stability
In the international literature examining mental health specifically for PhD students (see the systematic review in [ 21 ], the issue of mental health for PhD students is acknowledged to be multidimensional and complex [ 10 ]. In this growing research area, some address mental health as an aspect of the broader ‘health’ of the PhD students (e.g., [ 22 ]), some focus on psychological distress [ 23 ], while others take depression as a specific manifestation of distress [ 9 , 24 ]. The latter is particularly interesting because depression within the PhD population in these studies is often assessed with standardised questionnaires (e.g., PHQ, see below) that allow for developing comparative insights. It is also the approach adopted by the only global survey of PhD students’ mental health by Evans et al. [ 12 ], showing that 39% of PhD students report moderate-to-severe depression, significantly more than the general population.
Literature on PhD student’s mental health determinants in times of relative stability
Past literature on PhD students’ mental health offers insights into the determinants of PhD students’ mental health in times of stability, which may help understand the relationships we want to examine between PhD mental health, performance satisfaction and coping in times of research disruption.
First, past studies evidence the influence of PhD students’ personal lives on poor mental health. PhD students with children or with partners are less likely to have or develop psychological distress [ 9 ]. The normalcy of family roles is a much-needed antidote to the known pressures of a PhD program [ 25 ] and might even protect against mental health problems [ 22 , 26 ]. Other aspects of PhD students’ personal lives, such as significant life events (e.g., severe problems in personal relationships or severe illness of the student or someone close to them), have been linked to dissatisfaction with their research progress [ 24 ]. Research progress is defined as students’ perception of their progress in the completion of their degree [ 27 ] and is linked to their mental health. Dissatisfaction is tied to negative outcomes, such as attrition and delay [ 28 ], but also to lower productivity and mental health problems, such as worry, anxiety, exhaustion, and stress [ 29 ]. Related to this, Levecque and colleagues [ 9 ] observed that PhD students expressing a high interest in an academic career are in better mental health than those with no or little interest in remaining in academia.
Second, gender was the key personal factor that emerged as a determinant for mental health in past studies: PhD students who self-identify as female report greater clinical [ 9 , 30 ] and non-clinical problems with their mental health [ 23 , 31 ]. This is explained through the additional pressure women report on their professional and personal lives [ 23 ].
Third, past studies argue that each PhD phase presents PhD students with specific sets of challenges and should thus be explored discreetly in relation to mental health [ 32 ]. Still, the evidence on the link between the PhD phase (or the year of study as a proxy for the PhD phase) and mental health is inconclusive. Barry et al.’s [ 33 ] survey reports no connection between the PhD phase and depression levels in an Australian PhD population. However, Levecque et al. [ 9 ] report high degrees of depression in the early PhD stage of students in Belgium, and a global survey of PhD students across countries and disciplines shows that depression likelihood increases as the PhD program progresses [ 32 ].
Fourth, past research offers strong evidence that financial concerns impact PhD students’ mental health negatively. In a study by El-Ghoroury et al. [ 34 ], 63.9% of PhD students cited debt or financial issues as a cause for poor wellbeing and cited financial constraints as the major barrier to improving their wellness (through social interactions, outside-PhD activities, etc). Even uncertainty about funding was shown to predict poor mental health [ 9 ]. To this end, Geven et al. [ 35 ] explored packages of reforms in a pre-pandemic graduate school programme, including an extension of the grant period, and indicated that such policies can increase students’ completion rates to up to 20%.
Finally, age is not shown to be associated with mental health [ 9 ], but numerous studies found that having children, particularly for female PhD students and in Science-Technology-Engineering-Maths (STEM) disciplines [ 36 ], consistently corresponds with heightened stress [ 37 ]. However, a specific examination of the relationship between children and mental health indicates that PhD students with one or more children in the household showed significantly lower odds of having or developing a common psychiatric disorder [ 9 ]. Further, parenting and, in particular, motherhood during doctorate studies contribute to the development of students’ coping mechanisms that allows them to succeed in a balance in both worlds [ 38 ].
Past research insights into PhD mental health and coping
Past research explored how PhD students may “cope” with stressors and thus mitigate poor mental health [ 39 ]. Studies identify the importance of social interactions (e.g., [ 22 ]); balancing life demands (e.g., [ 16 ]), reaching out for social support (e.g., [ 40 ]) sometimes through peer relationships (e.g., [ 10 , 39 ]); and ‘planning’ (e.g., [ 22 ]); As invaluable as these insights are, drawing comparisons between these findings is difficult because often the identification of coping styles or strategies was not the focus of these studies, making it difficult to draw fine-grained conclusions as to their effect on PhD students’ mental health.
There is, however, a long tradition of research on coping for physiological wellbeing that provides standardised measures for individuals’ coping and their link to mental health [ 41 ]. The most widely used measurement instrument in the literature reviewed is the COPE Inventory, which allows researchers to assess how people cope in a variety of stressful situations, including in HE for students [ 42 – 44 ], making it particularly relevant to the context and sample under investigation in our study of PhD students. Additionally, COPE allows for the identification of consistent ways of coping, which provides predictive validity across a range of situations. Predictive validity is desired when examining the role of coping in relation to mental health. Indeed, multiple studies have linked the COPE measurement to mental health outcomes (e.g., [ 45 , 46 ]), including depression [ 43 ], which is a focus of our study.
Data and methods
Participants.
For the current study, we recruited participants that were active PhD students from March to July 2020 at any stage of their research to take part in an online survey. The survey ran between the 31st of July and the 23rd of August 2020, with the aim of capturing the potential impact of the Covid-19 disruption during the first lockdown on their research progress and mental health. The use of online surveys to assess the scope of mental health problems is particularly appropriate during the Covid-19 outbreak [ 47 ]. The current study has been reviewed by, and received a favourable opinion, from The Open University Human Research Ethics Committee (reference number: HREC/3605/Aristeidou), http://www.open.ac.uk/research/ethics/ . For the recruitment of a diverse audience, we followed a snowball sampling method, forwarding our invitation to PhD student groups in a number of UK-based universities, but also exploited the reach of PhD social media channels and online PhD groups, and we invited academics and respondents to recruit other participants. Vouchers were provided as an incentive for participation to the first 300 respondents. Before completing the survey, the respondents were provided with an online information sheet and were asked to provide their written consent through a digital consent form. They reported their email addresses to be identifiable and contactable for validation, consent issues, potential withdrawal, and incentive processing. The dataset was anonymized on the 30th of August 2020, prior to initiating data analysis.
Exclusion criteria included survey respondents who ‘straight-lined’ (chose the same answer option repeatedly), gave inconsistent responses to similar questions, or did not use their institution emails (rendering them unidentifiable). Finally, there were 1790 PhD students in the study from 94 different HE institutions across all four UK nations (England, Scotland, Northern Ireland and Wales). The majority of the study population (86%) reported that their research progress had been impacted in a negative way. The dataset [ 48 ] included 44.4% male and 55.4% female participants, while the doctoral students in the UK consist of 51% male and 49% female students [ 17 ]. Weighting adjustments were made to correct the sample representativeness. The majority of the survey respondents were 25–34 years old (80.4%), with live-in children (71%). Most respondents (86.7%) were conducting their PhDs full-time, and almost two-thirds (64.4%) were funded by a research council or a charitable body in the UK. At the time of the survey, a large proportion of the survey respondents were in the ‘executing’ phase of their research (i.e., data collection/analysis). Finally, a natural science-related PhD was being pursued by slightly over two-thirds of the respondents (68.8%). According to data sourced from HESA [ 17 ], the likelihood of individuals embarking on a research postgraduate degree at a younger age (such as 18–20) appears to be relatively low. This is evident from the fact that only 90–130 students within this age group register for such programs each year. More details on the demographics and characteristics of the sample can be found in Table 1 and below.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0291555.t001
Variables and instruments
Brief cope inventory (bci)..
The BCI [ 49 ] is a 28-item self-report questionnaire designed to measure effective and ineffective ways to cope with a stressful life event, and it is the abbreviated version of the original 60-item COPE inventory developed by [ 42 ]. The BCI has a 4-point Likert scale with options on each item ranging from 0 (I usually do not do this at all) to 3 (I usually do this a lot). Coping in this study is categorised in two overarching coping behaviours, as per Eisenberg et al. [ 50 ]: (a) the approach behaviours that attempt to reduce stress by alleviating the problem directly, which include 12 items related to active coping, positive reframing, planning, acceptance, seeking emotional support, and seeking informational support; and (b) the avoidant coping behaviours that attempt to reduce stress by distancing oneself from the problem, which include 12 items related to denial, substance use, venting, behavioural disengagement, self-distraction, and self-blame. Items that belong to neither overarching behaviour are coping related to humour and religion. These were included in the overall coping score but excluded from the analysis based on the two overarching behaviours. A higher score indicates frequent use of that coping behaviour. Cronbach’s alpha for the BCI was .88. Further, both the approach and avoidant scales have shown very good internal consistency in this sample, with Cronbach’s alpha equal to 0.83 and 0.80, respectively.
Patient health questionnaire eight-item depression scale (PHQ-8).
PHQ-8 [ 57 ] is an eight-item version of the Patient Health Questionnaire (PHQ-9). PHQ is a popular measure for assessing depression and is frequently used for PhD mental health (e.g., [ 12 , 51 ]), making it an ideal choice for our study. PHQ-9 has been validated as both a diagnostic and severity measure [ 52 , 53 ] in population-based settings [ 54 ] and self-administered modes [ 55 , 56 ], and it was recently used in a global survey of PhD students’ depression prevalence [ 12 ]. PHQ-8 omits the ninth question that assesses suicidal or self-injurious thoughts, and it was deemed more appropriate for our research because researchers in web-based interviews/surveys are unable to provide adequate interventions remotely. The PHQ-8 items employ a 4-point Likert scale with options on each item ranging from 0 (not at all) to 3 (nearly every day). Then, the scores are summed to give a total score between 0 and 24 points, where 0–4 represent no significant depressive symptoms, 5–9 mild depressive symptoms, 10–13 moderate, 15–19 moderately severe, and 20–24 severe [ 55 ]. Evidence from a large-scale validation study [ 57 ] indicates that a PHQ-8 score ≥ 10 represents clinically significant depression. In this study, Cronbach’s alpha for the PHQ-8 was 0.71, indicating a good internal consistency.
Performance satisfaction.
Performance satisfaction is an 8-item self-report scale designed to measure the students’ self-perceived progress in their PhD research, their confidence in being able to finish on time, and their satisfaction. The scale was successfully used in a PhD student well-being study at the university of Groningen [ 24 ] prior to the Covid-19 pandemic. The performance satisfaction 5-point Likert scale responses range from 1 (completely disagree) to 5 (completely agree). The score for each respondent equals the mean score of the 8-item responses. A reliability analysis was carried out on the performance satisfaction scale. Cronbach’s alpha showed the scale to reach acceptable reliability, α = 0.86.
Significant life events Significant Life events is a questionnaire designed to capture whether PhD students had experienced any significant life events in the 12 months prior to the survey. This was successfully used in studying PhD students’ mental health at the university of Groningen [ 24 ] prior to the Covid-19 pandemic research disruption. Events include the death of someone close, severe problems in personal relationships, financial problems, severe illness of oneself or someone close, being in the process of buying a house, getting married, expecting a child, none of these events, and prefer not to say. Significant life events were used as an incident control variable in this study.
Statistical analyses
SPSS (Version 25) was used for statistical analysis. In the first phase, descriptive statistics were used to describe the PHQ-8 Depression and coping behaviours of the sample and the distribution of these three variables among demographics, PhD characteristics, and Covid-19-related circumstances (O1). We used a weighting adjustment for gender to correct the survey representativeness for descriptive analysis; females were given a ‘corrective’ weight of 0.88 and males of 1.15.
In relation to O2, Spearman rank correlations were used to examine the degree of association between all of the 28 coping behaviours and PHQ-8 Depression scores. This finding contributed to our understanding of how individual coping behaviours could relate to lower or higher depressive symptoms.
To assess whether the behaviours significant to our study (i.e., those with a negative or the strongest positive PHQ-8 Depression association) were used more frequently by students of a particular demographic group (O2), we used independent-samples t-test and ANOVA. Before assessing the relationship between our variables, outliers, and groups with a sample size smaller than 15 for each group were removed from the tests (e.g., Gender = other; Funding = partially funded; Likelihood in HE = already employed in academia).
In relation to O3, a binary logistic regression analysis was performed to examine whether Covid-19-related circumstances explain significant depression in PhD students, while controlling for demographics, PhD characteristics, and external incidents. Prior to performing the regression analysis, PHQ-8 Depression score outliers, as well as groups with fewer than 10 events per variable (e.g., gender = other; age = 55–64; Impact reason = mental health), were detected and excluded from the dataset. The dichotomous dependent variable was calculated based on PHQ-8 Depression scores smaller than 10 for non-significant depression, and equal or larger than 10 for significant depression. Associations between Depression in PhD students and the independent variables in our dependency model were estimated using odds ratios (ORs) as produced by the logistic regression procedure in SPSS (Version 25). The ORs were used to explain the strength of the presence or absence of significant depression. Wald tests were used to assess the significance of each predictor. A test of the full model against a constant only model was statistically significant, indicating that the predictors as a set reliably distinguished between PhD students who are having or developing significant depression and those who are not ( Χ 2 (25) = 405.258, p < . 001 ). A Nagelkerke R 2 of .798 indicated a good to substantial relationship between prediction and grouping (68% of variance explained by the proposed model in completion rates). Table 2 presents response percentages about the categorical variables entered in the model, including the two dependent variables (significant depression and non-significant depression).
https://doi.org/10.1371/journal.pone.0291555.t002
Exploring depression prevalence and coping behaviours
The average PHQ-8 Depression score was 10.13 ( SD = 3.23) on a scale of 0–24 (weighted cases). Importantly, this highlights that the majority of survey respondents are facing moderate depression symptoms ( Fig 1 ). The PHQ-8 item with the highest score, in a range of 0–4, was ‘having trouble to concentrate on things, such as reading the newspaper or watching television’ ( M = 1.45; SD = 0.84), and the item with the lowest score was ‘moving or speaking so slowly that other people could have noticed; or the opposite–being so fidgety or restless that have been moving around a lot more than usual’ ( M = 1.10; SD = 0.75). Of the study population, 75% self-reported significant depression (moderate, moderately severe, or severe major).
https://doi.org/10.1371/journal.pone.0291555.g001
The coping behaviours that the majority of PhD students used in a medium or large amount to overcome the Covid-19 disruption were “accepting the reality of the fact that it has happened” (84%), followed by “thinking hard about what steps to make” (76%) ( Fig 2 ). Both are approaching coping behaviours. Other coping behaviours used to a great extent were “praying or meditating” (73%) , “blaming myself for things that happened” (avoidant) (71%) , and “expressing my negative feelings” (avoidant) (69%). On the other hand, coping behaviours that were used the least were all avoidant ones: “giving up attempting to cope” ( 13%) , “refusing to believe that it has happened” (15%) , “using alcohol or other drugs to make myself feel better” (17%) , and “giving up trying to deal with it” (17%) . Overall, approach coping behaviours were used to a greater extent ( M = 26.43, SD = 5.15) than avoidant coping behaviours ( M = 23.97, SD = 4.90).
https://doi.org/10.1371/journal.pone.0291555.g002
The Spearman correlations between coping behaviours and PHQ-8 scores ( Table 3 ), which included outliers, suggested that only two items have significant negative (very weak) associations with depression: Item 15, “getting comfort and understanding from someone” ( r s (1780) = -.107, p < .01); and Item 7, “taking action to try to make the situation better” ( r s (1762) = -.077, p < .01). The majority of the coping behaviours had a significant positive relationship with higher scores in depressive symptoms. The coping behaviours with the largest effect and a moderate to strong association were Item 13, “criticizing myself” ( r s (1762) = .452, p < .01), followed by Item 11 “using alcohol or other drugs to help me go through it” ( r s (1762) = .387, p < .01).
https://doi.org/10.1371/journal.pone.0291555.t003
Table 4 shows the relationship among approach and avoidant coping behaviours, and demographics. Our analyses indicated that both approach and avoidant coping behaviours had been significantly used to a greater extent by the female over male PhD students, by students without a live-in partner than those with a live-in partner, and by those without live-in children than those with live-in children. There is no evidence that the students of a particular age group were using avoidant coping more than those of another age group. However, students aged 25–34 were using approach coping behaviours less than other groups, and those aged 45–54 more ( Table 5 ).
https://doi.org/10.1371/journal.pone.0291555.t004
https://doi.org/10.1371/journal.pone.0291555.t005
Our analyses indicated that female PhD students, who had significantly lower PHQ-8 Depression scores, were using Table 3 ‘s Items 15 ( t [1778] = 14.61, p < .001) and Item 7 ( t [480] = 15.11, p < .001) significantly more than male students. Also, those without live-in partners were getting comfort and understanding from someone to a significantly greater extent than those without ( t [702] = 20.09, p < .001). PhD students without live-in children were taking action to try to make the situation better significantly more than those who have them ( t [894] = 25.21, p < .001).

Predictors of depression and relative influence
Covid-19-related circumstances (receiving an extension, impact reasons, and impact results), performance satisfaction, and coping behaviours (approach and avoidant) were entered together as predictors of depression. Demographics (gender, age, live-in partner, and live-in children), PhD characteristics (discipline, PhD phase, PhD mode, funding, interest in HE, and likelihood in HE) and external incidents were used as control variables. Table 6 reports the findings of the analyses.
https://doi.org/10.1371/journal.pone.0291555.t006
Prediction success overall was 95.3% (83.1% for not significant depression and 98.0% for significant depression). The Wald criterion demonstrated that not having an extension ( p = .014), having caring responsibilities ( p < .001), and using approach ( p < .001) or avoidant ( p < .001) coping behaviours made significant contributions to prediction. The OR value indicated that in the case that PhD students were not receiving an extension amid the Covid-19 disruption, or they did not know whether they were receiving one yet, they were 5.4 times more likely to experience significant depression. For the impact reason, our findings showed that–compared to those who experienced personal illness–PhD students who had caring responsibilities (e.g., childcare or other) showed slightly lower depressive symptoms (OR = 0.10). The OR for approach and avoidant coping behaviours were 0.13 and 43.73, respectively. This finding indicates that when approach coping is raised by one unit (e.g., +1 to the score), we see evidence for better mental health, while when avoidant coping is raised by one unit, a PhD student is very likely (44 times) to experience significant depression.
Turning to our control variables, PhD students with children in the household and with live-in partners showed significantly higher odds (about 14 and 7 times more, respectively) of having or developing depressive symptoms than those without. The latter can be explained by the fact that 88% of the participants with live-in partners also reported having live-in children. Also, male students were slightly more likely than female students to experience significant depression (with a borderline p-value), but this might be explained by the significantly increased use of coping approaches by female students. This gender-related finding that shows nearly no difference between the two categories slightly differs from Goldstone and Zhang’s model [ 15 ] which highlights a difference between female and male participants’ mental wellbeing. This difference can be explained by the fact that the research instruments used in the two studies were different, as well as the survey period.
Some PhD characteristics that made significant contributions to prediction were the discipline of PhD studies and the interest of students to remain in academia after finishing their PhD projects. The risk of experiencing significant depression in PhD students in social sciences (OR = 9.68) was lower than in students conducting a PhD in natural sciences. In contrast to findings by Levecque et al. [ 9 ], we observed that PhD students expressing a high interest in an academic career were 3.5 times more likely to develop depressive symptoms than those with no or only little interest in remaining in academia. Further, those considering having a high likelihood of remaining in academia were slightly more depressed (OR = 3.73), as well as those who were in the executing phase of their PhD research (OR = 3.33). No differences between funded and self-funded students were detected. Finally, the OR for the external incident variable was 6.13, indicating that for each incident unit (e.g., one more incident), we see evidence for depressive symptoms that are six times worse.
Our study contributes new empirical data and new insights needed to develop knowledge on the effect of university research disruption on the PhD student population. In turn, new knowledge may provide the evidence base for university and research policy.
Exploring mental health and coping behaviours
Our first contribution is to provide empirical estimates for the performance satisfaction, prevalence of mental health problems, and coping behaviours of PhD students during the pandemic-induced research disruption, on the basis of representative data across disciplines and across universities in the UK.
Our findings show that most UK PhD students across universities and disciplines report that their research progress has been affected negatively (86%). By contrast, in pre-pandemic periods, 79% of UK PhD students across Universities and disciplines had indicated excellent research progress [ 11 ]. This shift within the same population is important to reveal because of its potential implications for PhDs’ careers and university research capacity and innovation, as we know that dissatisfaction about the PhD trajectory is tied to negative outcomes such as attrition and delay [ 24 , 28 ], but also to lower productivity [ 58 ].
We found that during the period of severe research disruption caused by the Covid-19 pandemic, 75% of the UK students surveyed from 94 universities and across disciplines self-reported in the moderate-severe range for depression. This is at least three times more compared to the reported prevalence of depression among the general population internationally during the Covid-19 outbreak (16–28%, [ 59 ]). Our findings are also in line with findings in Goldstone and Zhang’s study [ 15 ] on UK postgraduate students’ mental wellbeing during the pandemic, in which 72% of the surveyed students were found to demonstrate possible or probable depression or anxiety.
By adopting widely used standardised questionnaires, our findings provide an accessible benchmark for the comparison with studies that took place among PhD student populations in periods of HE stability (pre-2020), thereby providing the empirical basis to accurately estimate the issue of poor mental health among PhD students during a period of research disruption. Using the same questionnaire as in our survey (PHQ-9) and drawing on a sample of PhD students from multiple universities and across research disciplines, a pre-pandemic global survey reported that 39% of PhD students scored in the moderate-severe range for depression [ 12 ]. Pre-pandemic national surveys of PhD students across institutions and disciplines report similar rates of depression, between 32% (in Belgium, Levecque et al. [ 9 ] and 38% (in the Netherlands, Van der Weijden et al. [ 60 ]. In a pre-pandemic (2018–2019) survey of UK PhD students across 48 universities and disciplines, only 25% reported levels that would indicate probable depression or anxiety [ 11 ]. These comparisons indicate that the prevalence of depression among the UK PhD student population of our study during the pandemic-induced period of research disruption is two-to-three times more than that which was reported in periods of stability for the UK PhD student population, for PhD student populations of other countries, and the global PhD population.
Our findings on PhD students’ mental health and PhD students’ coping advance past literature [ 22 , 23 , 34 ] in two significant ways. First, by using a highly reliable coping measure (COPE), we are able to demonstrate the relationship between coping styles and mental health outcomes in PhD students in a way that allows for comparisons and to build further research in this area. Second, we identify specific coping behaviours amongst the UK PhD students that are associated with lower depression scores and some that have a negative association with depression (i.e., getting comfort and understanding from someone and taking action to try to make the situation better ). Both are ‘coping approach’ behaviours (i.e., attempts to reduce stress by alleviating the problem directly; [ 50 ]). Studies using COPE in other populations have also linked coping-approach behaviours to fewer symptoms of psychological distress [ 45 ], more physical and psychological well-being at work [ 46 ], and an absence of anxiety and depression [ 61 ].
Factors explaining PhD students’ depression
Our second contribution is to explain–within the UK PhD population–whose mental health is more affected by the pandemic-induced research disruption. We find that several factors have a significant impact on PhD students to have or develop mental health issues during a period of research disruption.
Consistent with past research on PhD students’ mental health, our findings reveal the significant influence of their personal lives on poor mental health. The relationships we observed during a period of research disruption, however, differ from those suggested in studies conducted in periods of stability (e.g., [ 9 , 22 , 25 , 26 , 62 ]). We found that PhD students with live-in children or with a live-in partner and PhDs with caring responsibilities are more likely to have or develop significant depression compared to those without. This difference can be explained by the closure of schools that resulted in parents home-schooling their children, a greater demand for devices and the internet in households, and parents going through emotional hardship [ 63 ]. We additionally find six times worse depressive symptoms for each ‘external life incident’ (e.g., childbirth, moving home) that occurred in the PhD students’ lives. A larger number of external incidents were found to be associated with students with live-in partners and students with live-in children, which may explain these as reinforcing negative effects. These new insights explain that–although most of these realities in PhD students’ personal lives existed besides the research disruption—when combined with the research disruption, their mental health can spiral downward.
Our findings also address the role of structural PhD characteristics (PhD discipline and PhD phase) in predicting whether a student might present mental health issues in times of research disruption. We find that in a period of research disruption, the risk of significant depression is higher in the execution phase of the PhD compared to the beginning or extension phases, contrary to Levecque and colleagues’ findings [ 9 ]. Because there is very limited research on the PhD stage and mental health, our findings contribute insights to a broader community of scholars who advocate for the further study of the challenges in each PhD stage discreetly (e.g., [ 32 ]). Furthermore, we find that the risk of experiencing significant depression in PhD students in social sciences was lower than students conducting a PhD in natural sciences. Our survey respondents offered explanations on the role of PhD discipline in mental health during the pandemic in the open text responses. These converge on the fact that natural sciences often require being physically in a laboratory, which is probably unfeasible when university facilities are closed.
In tune with past research on finances and mental health in PhD students [ 9 , 64 ], we found those without funded extensions are more likely to have or develop significant depression (moderate, moderately severe, and severe) compared to those with them. We reveal the size of this association (about 5.5 times more) and link PhD funding extensions to standardized assessments of depression prevalence, thus uniquely providing new evidence for policy scholars.
Implications for research and higher education policy
Our findings show an alarming increase in self-reported depression levels among the UK PhD student population. The long-term mental health impact of Covid-19 may take years to become fully apparent, and managing this impact requires concerted effort not just from the healthcare system at large [ 59 ] but also from the HE sector specifically. With mental illness a cause for PhD student attrition, loss of research capacity and productivity, data from our survey should prompt consideration of immediate intervention strategies.
For research and education policy scholars, our findings contribute directly to the development of evidence-based research and university policies on support for targeted groups of PhD students in times of disruption. Specifically, our findings show that institutional and funder support should not only be in the form of PhD-funded extensions–which are nevertheless shown in our study and other studies (e.g., [ 15 ]) to be very significant. But also, in the form of providing expedited alternatives to the changes evoked by the pandemic for PhD students, such as new and adjusted policies that explicitly consider those PhDs with caring responsibilities, since 77% of our respondents reported that childcare and other caring responsibilities are the reason for dissatisfaction with their PhD progress. If not, the Covid-19 research disruption could erase decades of progress towards equality in academia [ 65 ].
Our main contribution is that we offer insights into how to mitigate mental health consequences for PhD students in times of research disruption. Individual-driven coping behaviours are suggested to be of equal importance to those promoted by the PhD students’ institutions [ 66 ]. In this study, approach coping behaviours were found to associate with lower depression levels, which may eventually contribute to PhD completion. The importance of developing coping mechanisms has also been highlighted in pre-pandemic studies, with, for instance, mothers finding ways to combine academic work and family responsibilities and succeed in both roles [ 38 ]. Still, institutions may play a crucial role in offering training for PhD students on coping and wellbeing through, for instance, a virtual platform to comply with social distancing policies. Such efforts may include mental health support and coping behaviour guidance, so that students are guided on how to successfully deal with disruptions (for example, to avoid avoidant coping behaviours that may lead them to higher levels of depression). Pre-pandemic reforms have previously shown that a well-structured programme and well-timed financial support can facilitate and uphold PhD completion, alongside student efforts [ 35 ]. As the future generation of academics, PhD students would be better equipped to handle the current and future disruptions and better cope with other disruptions in their academic journeys.
Limitations and implications for further research
Although our study has gone some way towards enhancing our understanding of Covid-19-related effects on UK PhD students’ mental health, it is plausible that a number of limitations could have influenced the results obtained. First, while our research attracted a representative number of students from different age groups, PhD modes, phases and funding, there was a very strong presence of students in natural sciences [ 17 ]. Second, as this was a cross-sectional study, we did not follow the UK PhD population longitudinally, and we may not offer insights into the trajectory of the relationships we articulate in our findings. Nevertheless, our adoption of standardized questionnaires allows for a platform for comparisons with past and future research efforts. Third, findings in this survey are based on self-report and may be subject to unconscious biases (e.g., PhD students assessing themselves or the situation inaccurately). Fifth, the research undertaken employed the PHQ-8 with a specific emphasis on assessing aspects related to depression. It is important to acknowledge that while these questionnaires offer valuable insights into depression, they may not comprehensively encompass the broader spectrum of general mental health. Therefore, the findings of the study should be interpreted within the context of its targeted focus on depression, recognizing the potential existence of other dimensions of mental health that were not directly addressed within this research framework. Finally, despite the high percentage of prediction in our findings (80%), additional factors may likely explain variabilities in our study outcomes, such as leadership factors or supervision styles in the 94 UK Universities whose PhD students participated in our survey.
As our study strongly demonstrates, juxtaposing findings from studies conducted during periods of relative HE stability with those conducted during periods of disruption is a fruitful approach for advancing research and university policy. By identifying which insights that would have been invaluable during periods of stability are less so during a period of disruption, scholars can provide significant advancements to existing research and new insights for policy, research and HE leadership.
Conclusions
Our study extends previous research on mental health in the HE sector by considering the dynamics of a severe disruption as opposed to the dynamics of relative stability in PhD mental health and coping behaviours. Drawing on our insights into these interrelationships, we suggest extensions to the literature on PhD students’ mental health, research and university policy. With our findings, HE leaders and policymakers may be better placed to tackle and ultimately overcome this and future research disruptions.
Acknowledgments
The authors would like to thank all the PhD students who committed time for taking part in this study and their responses informed the writing of this paper.
- View Article
- Google Scholar
- 3. O’Malley B. 180 congressmen support call for US$26bn research support. University World News [Internet]. 2020 [cited 2023 Jan 15]; Available from: https://www.universityworldnews.com/post.php?story=20200502080814674
- PubMed/NCBI
- 39. Drake KL. Psychology Graduate Student Well-being: The Relationship between Stress, Coping, and Health Outcomes. University of Cincinnati; 2010.
- 40. Pychyl T. Personal projects, subjective well-being and the lives of doctoral students. | CURVE [Internet]. Carleton University; 1995 [cited 2023 Jan 15]. Available from: https://curve.carleton.ca/d330c15c-eeaa-459c-afea-4bf841b7daa0
- 48. Aristeidou M, Aristidou A. PhDMentalHealth_UKDataset [Internet]. The Open University; 2023 [cited 2023 May 10]. Available from: https://ordo.open.ac.uk/articles/dataset/PhDMentalHealth_UKDataset/22794203/0 .
- 65. Malisch JL, Harris BN, Sherrer SM, Lewis KA, Shepherd SL, McCarthy PC, et al. Opinion: In the wake of COVID-19, academia needs new solutions to ensure gender equity [Internet]. Vol. 117, Proceedings of the National Academy of Sciences of the United States of America. National Academy of Sciences; 2020 Jul [cited 2023 Jan 15]. Available from: https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2010636117/-/DCSupplemental .

- About the LSE Impact Blog
- Comments Policy
- Popular Posts
- Recent Posts
- Subscribe to the Impact Blog
- Write for us
- LSE comment
Cassie M Hazell
January 12th, 2022, is doing a phd bad for your mental health.
9 comments | 77 shares
Estimated reading time: 6 minutes
Poor mental health amongst PhD researchers is increasingly being recognised as an issue within higher education institutions. However, there continues to be unanswered questions relating to the propensity and causality of poor mental health amongst PhD researchers. Reporting on a new comparative survey of PhD researchers and their peers from different professions, Dr Cassie M Hazell and Dr Clio Berry find that PhD researchers are particularly vulnerable to poor mental health compared to their peers. Arguing against an inherent and individualised link between PhD research and mental health, they suggest institutions have a significant role to play in reviewing cultures and working environments that contribute to the risk of poor mental health.
Evidence has been growing in recent years that mental health difficulties are common amongst PhD students . These studies understandably have caused concern in academic circles about the welfare of our future researchers and the potential toxicity of academia as a whole. Each of these studies has made an important contribution to the field, but there are some key questions that have thus far been left unanswered:
- Is this an issue limited to certain academic communities or countries?
- Do these findings reflect a PhD-specific issue or reflect the mental health consequences of being in a graduate-level occupation?
- Are the mental health difficulties reported amongst PhD students clinically meaningful?
We attempted to answer these questions as part of our Understanding the mental health of DOCtoral researchers (U-DOC) survey. To do this we surveyed more than 3,300 PhD students studying in the UK and a control group of more than 1,200 matched working professionals about their mental health. In our most recent paper , we compared the presence and severity of mental health symptoms between these two groups. Using the same measures as are used in the NHS to assess symptoms of depression and anxiety, we found that PhD students were more likely to meet criteria for a depression and/or anxiety diagnosis and have more severe symptoms overall. We found no difference between these groups in terms of their overall suicidality. However, survey responses corresponding to past suicidal thinking and behaviour, and future suicide intent were generally highly rated in both groups.
42% of PhD students reported that they believed having a mental health problem during your PhD is the norm
We also asked PhD students about their perceptions and lived experience of mental health. Sadly, 42% of PhD students reported that they believed having a mental health problem during your PhD is the norm. We also found similar numbers saying they have considered taking a break from their studies for mental health reasons, with 14% actually taking a mental health-related break. Finally, 35% of PhD students have considered ending their studies altogether because of their mental health.
We were able to challenge the working theory that the reason for our findings is that those with mental health difficulties are more likely to continue their studies at university to the doctoral level. In other words, the idea that doing a PhD doesn’t in any way cause mental health problems and these results are instead the product of pre-existing conditions. Contrary to this notion, we found that PhD students were not more likely than working professionals to report previously diagnosed mental health problems, and if anything, when they had mental health problems, these started later in life than for the working professionals. Additionally, we found that our results regarding current depression and anxiety symptoms remained even after controlling for a history of mental health difficulties.

The findings from this paper and our other work on the U-DOC project has highlighted that PhD students seem to be particularly vulnerable to experiencing mental health problems. We found several factors to be key predictors of this poor mental health ; specifically not having interests and relationships outside of PhD studies, students’ perfectionism, impostor thoughts, their supervisory relationship, isolation, financial insecurity and the impact of stressors outside of the PhD .
the current infrastructure, systems and practices in most academic institutions, and in the wider sector, are increasing PhD students’ risk of mental health problems and undermining the potential joy of pursuing meaningful and exciting research
So, does this mean that doing a PhD is bad for your mental health? Not necessarily. There are several aspects of the PhD process that are conducive to mental health difficulties, but it is absolutely not inevitable. Our research (and our own experiences!) suggests that doing a PhD can be an incredibly positive experience that is intellectually stimulating, personally satisfying, and gives a sense of meaning and purpose. We instead believe a more appropriate conclusion to draw from our work is that the current infrastructure, systems and practices in most academic institutions, and in the wider sector, are increasing PhD students’ risk of mental health problems and undermining the potential joy of pursuing meaningful and exciting research.
Reducing this issue to the common rhetoric that “PhD studies cause mental health problems” is problematic for several reasons: Firstly, it ignores the many interacting moving parts at work here that variably increase and reduce risk of poor mental health across people, time, and place. Secondly, it does not acknowledge the pockets of incredibly good practice in the sector we can learn from and implement more widely. Finally, it reinforces the notion that poor mental health is the norm for PhD students which then becomes a self-fulfilling prophecy- and itself ignores the joy of pursuing a thesis in something potentially so personally meaningful. Nonetheless, a significant paradigm shift is needed in academia to reduce the current environmental toxins so that studying for a PhD can be a truly enjoyable and fulfilling process for all.
Note: This article gives the views of the author, and not the position of the Impact of Social Science blog, nor of the London School of Economics. Please review our Comments Policy if you have any concerns on posting a comment below.
Image Credit: Geralt via Pixabay.

About the author

Dr Cassie M Hazell (she/her) is a lecturer in Social Sciences at the University of Westminster. Her research is on around mental health, with a special interest in implementation science. She is the co-founder of the international Early Career Hallucinations Research (ECHR) group and Early-Mid Career representative on the Research Council at her institution.

Dr Clio Berry is a Senior Lecturer in Healthcare Evaluation and Improvement in the Brighton and Sussex Medical School. She is interested in the application of positive and social psychology approaches to mental health problems and social outcomes for young people and students. Her work spans identification of risk and resilience factors in predicting mental health and social problems and their outcomes, and in the development and evaluation of clinical and non-clinical interventions.
- Pingback: Is doing a PhD bad for your mental health? | Thinking about Digital Publishing
My own experience of doing a PhD (loneliness, the lack of routine, imposter syndrome) has led to my discouraging my daughter, who has a history of mental health issues, from considering it at the moment, despite her having the academic aptitude and even a topic. I would hazard a guess that the problems are worse in the humanities than in the applied sciences, where most PhD students tend to work as part of research teams and be well supported in more structured environments.
- Pingback: What can universities do to support the well-being and mental health of postgraduate researchers? | Impact of Social Sciences
Fascinating research… I had a terrible PhD, but most of the mental health issues arose after the fact. If you ever conducted another survey it would be interesting to include those who had recently finished a PhD.
Looking at your follow up BJPsyche paper, I noticed you haven’t gone into the correlation between subject and mental health. I’d be interested to know how sciences vs humanities compared.
I see that your work is very restrained in discussing the causes of mental health issues, and I’m sure you have plenty of hypothesis. In my experience, a key factor is that there is no mechanism to hold supervisors to account for the quality of their supervision. (Linking to the point above, I believe in the sciences supervisors with poor outcomes do suffer repetitional damage – not so in the humanities.)
I’d also add that the UK’s Viva system, which I believe is unique globally, is a recipe for disaster – years of work evaluated over the course of just a couple of hours by examiners who, again, are not held accountable in any way.
I wrote my experience up here: https://medium.com/the-faculty/i-had-a-brutal-phd-viva-followed-by-two-years-of-corrections-here-is-what-i-learned-about-vivas-5e81175aa5d
- Pingback: The benefits of getting involved with the LSESU as a PhD student | Students@LSE
- Pingback: “Am I ready for a PhD?” - The Undercover Academic
- Pingback: #AcWriMo & online writing communities for off-campus PGRs – UoB PGR Development
- Pingback: Psychische Herausforderungen während der juristischen Promotion › JuWissBlog
- Pingback: What To Expect When You’re PhDing - Völkerrechtsblog
Leave a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Notify me of follow-up comments by email.
What can universities do to support the well-being and mental health of postgraduate researchers? February 1st, 2022
Related posts.

Is peer review bad for your mental health?
April 19th, 2018.

Book Review: Being Well in Academia: Ways to Feel Stronger, Safer and More Connected by Petra Boynton
February 27th, 2021.
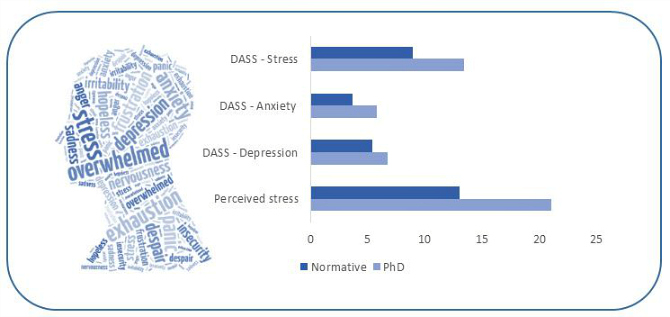
Mental health risks in research training can no longer be ignored
June 25th, 2018.

The neurotic academic: how anxiety fuels casualised academic work
April 17th, 2018.

Visit our sister blog LSE Review of Books
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Signs of depression and anxiety soar among US graduate students during pandemic
- PMID: 32811983
- DOI: 10.1038/d41586-020-02439-6
Keywords: Careers; Lab life; Psychology.
PubMed Disclaimer
Similar articles
- Investigating Mental Health of US College Students During the COVID-19 Pandemic: Cross-Sectional Survey Study. Wang X, Hegde S, Son C, Keller B, Smith A, Sasangohar F. Wang X, et al. J Med Internet Res. 2020 Sep 17;22(9):e22817. doi: 10.2196/22817. J Med Internet Res. 2020. PMID: 32897868 Free PMC article.
- Depression and Anxiety Changes Among Sexual and Gender Minority People Coinciding with Onset of COVID-19 Pandemic. Flentje A, Obedin-Maliver J, Lubensky ME, Dastur Z, Neilands T, Lunn MR. Flentje A, et al. J Gen Intern Med. 2020 Sep;35(9):2788-2790. doi: 10.1007/s11606-020-05970-4. Epub 2020 Jun 17. J Gen Intern Med. 2020. PMID: 32556877 Free PMC article. No abstract available.
- Effects of the COVID-19 Pandemic on Obsessive-Compulsive Symptoms Among University Students: Prospective Cohort Survey Study. Ji G, Wei W, Yue KC, Li H, Shi LJ, Ma JD, He CY, Zhou SS, Zhao Z, Lou T, Cheng J, Yang SC, Hu XZ. Ji G, et al. J Med Internet Res. 2020 Sep 30;22(9):e21915. doi: 10.2196/21915. J Med Internet Res. 2020. PMID: 32931444 Free PMC article.
- Consideraciones sobre la salud mental en la pandemia de COVID-19. Huarcaya-Victoria J. Huarcaya-Victoria J. Rev Peru Med Exp Salud Publica. 2020 Apr-Jun;37(2):327-334. doi: 10.17843/rpmesp.2020.372.5419. Epub 2020 Aug 28. Rev Peru Med Exp Salud Publica. 2020. PMID: 32876225 Review. Spanish.
- The mental health impact of the COVID-19 epidemic on immigrants and racial and ethnic minorities. Rothman S, Gunturu S, Korenis P. Rothman S, et al. QJM. 2020 Nov 1;113(11):779-782. doi: 10.1093/qjmed/hcaa203. QJM. 2020. PMID: 32591836 Free PMC article. Review. No abstract available.
- A narrative review of anxiety regulation in PhD students based on Green model. Ma Y, Yu A, Ma H, Zhao Y, Liu X, Zhai H, Gao Y. Ma Y, et al. Front Psychol. 2024 Jul 9;15:1351386. doi: 10.3389/fpsyg.2024.1351386. eCollection 2024. Front Psychol. 2024. PMID: 39045436 Free PMC article. Review.
- Evaluation of a Pilot Wellness Elective for Master of Public Health Students during the COVID-19 Pandemic. O'Malley BY, Etoundi-Ngono E, Hua J, Nano JP, Pipas CF. O'Malley BY, et al. Int J Environ Res Public Health. 2024 May 3;21(5):590. doi: 10.3390/ijerph21050590. Int J Environ Res Public Health. 2024. PMID: 38791804 Free PMC article.
- The impact of COVID-19 on the mental and sexual health of patients with infertility: a prospective before-and-after study. Qi J, Sun M, Yue X, Hong X, Dong M, Tan J. Qi J, et al. Reprod Biol Endocrinol. 2024 Jan 2;22(1):1. doi: 10.1186/s12958-023-01174-7. Reprod Biol Endocrinol. 2024. PMID: 38167101 Free PMC article.
- Anxiety, Depression, Perceived Stress, and Burnout Among Chinese Researchers: A Cross-Sectional Nationwide Study. Gao L, Wang LL, Yang R, Yang XJ, Zhou SJ. Gao L, et al. Psychol Res Behav Manag. 2023 Oct 17;16:4209-4220. doi: 10.2147/PRBM.S431011. eCollection 2023. Psychol Res Behav Manag. 2023. PMID: 37868653 Free PMC article.
- Overemphasis on publications may disadvantage historically excluded groups in STEM before and during COVID-19: A North American survey-based study. Rowland FE, Prats KA, Alshwairikh YA, Burak MK, Fanton AC, Duguid MC. Rowland FE, et al. PLoS One. 2023 Sep 27;18(9):e0291124. doi: 10.1371/journal.pone.0291124. eCollection 2023. PLoS One. 2023. PMID: 37756261 Free PMC article.
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- Nature Publishing Group
- MedlinePlus Consumer Health Information
- MedlinePlus Health Information
Miscellaneous
- NCI CPTAC Assay Portal

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Find out more about enrolment .
Nearly half of PhD students consider developing a mental health problem ‘normal’
A new study led by the University of Westminster in collaboration with researchers from the University of Sussex and Brighton and Sussex Medical School shows that 42% of PhD students consider developing a mental health problem a ‘normal’ part of the PhD process.

The researchers also found that more than a third (35.8%) of doctoral researchers considered ending or taking a break from their studies due to poor mental health, while just over 14% of doctoral researchers had formally suspended their studies due to mental health problems.
They discovered that compared to working professionals, PhD students are particularly vulnerable to mental health problems, and found initial evidence that PhD studies might be causative of this.
The study, published in Humanities & Social Sciences Communications and funded by Office for Students and Research England, investigated depression and anxiety levels through a nationwide survey of PhD students in the UK to ask them questions about their mental health. Over 3,000 PhD students completed the survey, as well as a matched control group of 1,168 working professionals.
PhD students reported significant anxiety and depression levels, a difference which was not explained by a higher rate of pre-existing mental health problems. The new collaborative research, which is the biggest ever controlled study on PhD student mental health and the first of its kind based in the UK, examined the mental health of PhD students and some factors that might increase their risk or protect against poor mental health. It comes after a recent international survey conducted by Nature, which found that 36% of current doctoral researchers reported seeking help for anxiety and/or depression.
These new findings provide an evidence-based mandate for universities and funders to reflect upon practices related to doctoral researcher training and mental health. Attention should now be directed towards understanding what factors may explain heightened anxiety and depression among PhD students to inform preventative measures and interventions. To help achieve this, the researchers are currently analysing data looking at viable, specific risk factors associated with poor mental health amongst PhD students with the goal of developing policies, strategies and interventions to improve and protect PhD students’ mental health.
Talking about the research, lead author of the study Dr Cassie Hazell , Lecturer in Psychology at the University of Westminster, said: “PhD students are a key part of the university community and are the future of research. Our findings demonstrate that a worrying proportion of PhD students are experiencing clinically significant levels of poor mental health that exceed those seen in other working professionals. It seems clear to us that there is something about the PhD process that is triggering mental health problems, and that a paradigm shift is needed. Without this change, PhD students, academia, and society as a whole will suffer.”
Professor Jeremy E. Niven, Dean of the Doctoral School at the University of Sussex, added: “Doctoral researchers are a key part of universities, they're future thinkers, innovators and leaders that are vital in building and sustaining our economy. Our research shows that they are particularly susceptible to some mental health difficulties that may be linked to the PhD itself. Universities and funding agencies really need to reconsider what is expected of a PhD Thesis or changes in the acceptable length of time over which funding is provided.”
Read the full paper in the Humanities & Social Sciences Communications journal .
- Share on Facebook
- Share on Twitter
- Share on LinkedIn
Related articles
Dame Judith Petts visits Westminster’s Centre for Nutraceuticals

Lecturers behind the scenes - Dr Pooja Basnett: It’s so great to watch my students grow with confidence

Westminster celebrates Sustainability Fund’s successful projects for 2023-24 academic year
Press and media enquiries.
Contact us on:
[email protected]
We use cookies to ensure the best experience on our website.
By accepting you agree to cookies being stored on your device.
Some of these cookies are essential to the running of the site, while others help us to improve your experience.
Functional cookies enable core functionality such as security, network management, and accessibility.
Analytics cookies help us improve our website based on user needs by collecting information, which does not directly identify anyone.
Marketing cookies send information on your visit to third parties so that they can make their advertising more relevant to you when you visit other websites.

Change Password
Your password must have 8 characters or more and contain 3 of the following:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
- Sign in / Register
Request Username
Can't sign in? Forgot your username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
PhDepression: Examining How Graduate Research and Teaching Affect Depression in Life Sciences PhD Students
- Logan E. Gin
- Nicholas J. Wiesenthal
- Isabella Ferreira
- Katelyn M. Cooper
Research for Inclusive STEM Education Center, School of Life Sciences, Arizona State University, Tempe, AZ 85281
Search for more papers by this author
Department of Biology, University of Central Florida, Orlando, FL 32816
*Address correspondence to: Katelyn M. Cooper ( E-mail Address: [email protected] ).
Graduate students are more than six times as likely to experience depression compared with the general population. However, few studies have examined how graduate school specifically affects depression. In this qualitative interview study of 50 life sciences PhD students from 28 institutions, we examined how research and teaching affect depression in PhD students and how depression in turn affects students’ experiences teaching and researching. Using inductive coding, we identified factors that either positively or negatively affected student depression. Graduate students more commonly mentioned factors related to research that negatively affected their depression and factors related to teaching that positively affected their depression. We identified four overarching aspects of graduate school that influenced student depression: the amount of structure in teaching and research, positive and negative reinforcement, success and failure, and social support and isolation. Graduate students reported that depression had an exclusively negative effect on their research, primarily hindering their motivation and self-confidence, but that it helped them to be more compassionate teachers. This work pinpoints specific aspects of graduate school that PhD programs can target to improve mental health among life sciences graduate students.
INTRODUCTION
In 2018, researchers found that graduate students were more than six times as likely to report experiencing depression and anxiety compared with the general population and subsequently declared a “graduate student mental health crisis” ( Evans et al. , 2018 ; Flaherty, 2018 ). Calls to identify which factors exacerbate graduate student mental health problems followed (“The Mental Health of PhD Researchers,” 2019; Woolston, 2019a ). However, few studies have taken an inductive approach to identifying what aspects of graduate school in particular affect student mental health. More commonly, large quantitative studies propose a limited number of factors that may affect student mental health that participants select from, few of which directly relate to graduate research or teaching ( Peluso et al. , 2011 ; Levecque et al. , 2017 ; Evans et al. , 2018 ; Liu et al. , 2019 ). In this interview study, we focus on depression in life sciences PhD students and examine which specific aspects of research and teaching graduate students report as affecting their depression. We also explore how depression affects students’ experiences in graduate school.
The American Psychiatric Association defines depression as a common and serious medical illness that negatively affects how one feels, the way one thinks, and how one acts ( American Psychiatric Association, 2020 ). Depression is characterized by nine symptoms: depressed mood; markedly diminished interest or pleasure in activities; reduced ability to think or concentrate, or indecisiveness; feelings of worthlessness, or excessive or inappropriate guilt; recurrent thoughts of death or suicidal ideation, or suicide attempts or plans; insomnia or hypersomnia; significant change in appetite or weight; psychomotor agitation or retardation; and fatigue or loss of energy ( American Psychiatric Association, 2013 ; Schmidt and Tolentino, 2018 ). For depression to be diagnosed, the presence of at least five of the symptoms is required most of the day, nearly every day, for at least 2 weeks in addition to the occurrence of either depressed mood or diminished interest or pleasure ( American Psychiatric Association, 2013 ). In the general U.S. population, depression affects approximately 6.7% of individuals and is estimated to affect 16.6% of individuals at some point in their lifetime.
Graduate students are far more likely to report experiencing depression compared with the general population ( Evans et al. , 2018 ; Barreira et al. , 2020 ). Specifically, a recent study of master’s and PhD students in programs across the world, spanning a variety of disciplines, found that 39% of graduate students reported having moderate to severe depression ( Evans et al. , 2018 ). Similar studies have demonstrated high rates of depression in graduate students in specific disciplines such as economics ( Barreira et al. , 2020 ), biochemistry ( Helmers et al. , 1997 ), pharmacology ( Helmers et al. , 1997 ), and physiology ( Helmers et al. , 1997 ). Depression rates have surged in recent years among graduate students ( American College Health Association, 2014 , 2019 ). Talking about depression has become more socially acceptable, particularly among younger adults ( Anxiety and Depression Association of America, 2015 ; Lipson et al. , 2019 ), which may have contributed to the number of students willing to reveal that they are struggling with mental health. Additionally, depression is highly related to burnout, defined as a work-related chronic stress syndrome involving emotional exhaustion, depersonalization, and reduced personal accomplishment ( Maslach et al. , 2001 ; Bianchi et al. , 2014 ). Graduate work environments appear to be increasingly characterized as stressful and demanding ( American College Health Association, 2014 , 2019 ; Woolston, 2017 ), which may also be contributing to the increase in graduate depression rates.
Increasingly, scientists, psychologists, and education researchers are recognizing graduate student mental health as a concern and calling for further investigation of graduate student mental health in hopes of identifying interventions to improve graduate student quality of life (“The Mental Health of PhD Researchers,” 2019; Woolston, 2019a , b ). For example, in 2019, Nature added a question to its annual survey of PhD students asking students from around the world whether they had sought help for anxiety or depression, and more than one-third (36%) confirmed they had ( Woolston, 2019b ). Additionally, notable publication outlets such as Nature (“The Mental Health of PhD Researchers,” 2019), Scientific American ( Puri, 2019 ), and Science ( Pain, 2018 ) have published blogs or editorials spotlighting the need to improve graduate student mental health.
Some recent studies have sought to uncover the factors affecting depression in graduate students. Primarily, survey studies with predetermined factors that researchers hypothesized impact student mental health have identified poor mentor–mentee relationships ( Peluso et al. , 2011 ; Evans et al. , 2018 ; Hish et al. , 2019 ; Liu et al. , 2019 ; Charles et al. , 2021 ), financial stress ( Hish et al. , 2019 ; Jones-White et al. , 2020 ; Charles et al. , 2021 ), and lack of work–life balance ( Evans et al. , 2018 ; Liu et al. , 2019 ) to be associated with depression or depressive symptoms among graduate students in various disciplines. Other variables shown to be predictive of depression include low research self-efficacy, defined as low confidence in one’s ability to do research ( Liu et al. , 2019 ), difficulty publishing papers ( Liu et al. , 2019 ), hours worked per week ( Peluso et al. , 2011 ), and perceived institutional discrimination ( Charles et al. , 2021 ). Factors that appear to be protective of depressive symptoms include social support ( Charles et al. , 2021 ), mastery, defined as the extent to which individuals perceive themselves to be in control of the forces that impact their lives ( Hish et al. , 2019 ), positive departmental social climate ( Charles et al. , 2021 ), optimism about career prospects ( Charles et al. , 2021 ), and sense of belonging to one’s graduate program ( Jones-White et al. , 2020 ). While these studies have identified some depression-related factors associated with graduate school broadly and emphasize the importance of positive mentor–mentee relationships, few studies have explored factors specifically associated with research and teaching, the two activities that graduate students engage in most frequently during their time in a program. Additionally, the extant literature has primarily focused on surface causes of graduate student depression, yet understanding the underlying causes may be key to developing meaningful interventions. For example, while it is well established that student perception of poor mentorship is related to student depression ( Evans et al. , 2018 ; Hish et al. , 2019 ; Liu et al. , 2019 ; Charles et al. , 2021 ), it is less well understood what specific behaviors mentors exhibit and how such behaviors negatively affect the cognitive and behavioral underpinnings of graduate student depression. Without this knowledge, it is difficult to develop strategies to help mentors be more inclusive of students.
Theories of depression seek to explain the causes of depression. No theoretical model is widely accepted as an overarching framework for depression within the psychological and psychiatric communities ( Mcleod, 2015 ; Ramnerö et al. , 2016 ); instead, there are a number of models addressing how different aspects of depression are associated with the disorder. Arguably, the three most prominent models are cognitive ( Beck et al. , 1979 ), behavioral ( Martell et al. , 2001 ), and psychodynamic ( Busch et al. , 2016 ). In brief, cognitive theories focus on an individual’s beliefs and propose that changes in thinking precede depressive symptoms; for example, negative views of oneself, the world, and the future are thought to be common for individuals with depression ( Beck et al. , 1979 ; Leahy, 2002 ). Behavioral theories emphasize that depression is a result of one’s interaction with the environment; depressive symptoms are thought to be the result of decreased reward, lack of positive reinforcement, encouragement of depressive or passive behaviors, and discouragement of healthy behaviors ( Lewinsohn, 1974 ; Martell et al. , 2001 ; Carvalho et al. , 2011 ). Psychodynamic theories of depression consider the role of feelings and behaviors in the etiology and persistence of depressive symptoms; these theories often focus on 1) one’s biology and temperamental vulnerabilities, 2) earliest attachment relationships, and 3) childhood experiences associated with frustration, helplessness, loss, guilty, or loneliness ( Busch et al. , 2016 ). While each group of theories has been critiqued and no one theory fully explains one’s experience with depression ( Mcleod, 2015 ; Ramnerö et al. , 2016 ), we propose that each may be helpful in understanding how aspects of graduate school may affect depression among PhD students.
The thoughts and behaviors associated with depression may in turn affect students’ experiences in graduate school, particularly their experiences with research and teaching. While no studies have examined how depression explicitly affects graduate students’ research experiences, studies have identified ways in which depression can affect students’ experiences in undergraduate research ( Cooper et al. , 2020a , b ). Undergraduate researchers report that their depression negatively affected their motivation, ability to concentrate and remember, intellectual engagement, and creativity in research ( Cooper et al. , 2020b ). Undergraduates described that their depression also caused them to be overly self-critical, less social, and ultimately negatively affected their research productivity. Additionally, undergraduates have been reluctant to share their depression with others in the lab, because they fear that they will be judged ( Cooper et al. , 2020b ). While these studies provide some insight into how depression may affect graduate students’ experience in research, there is much less information about how depression may affect graduate teaching.
In this study, we interviewed 50 PhD students in the life sciences who self-identified with having depression with the intent of answering two research questions that address gaps in the literature: 1) What specific aspects of graduate research and teaching affect PhD student depression? 2) How does PhD students’ depression affect their experience in research and teaching?
Student Interviews
This study was done under an approved Arizona State University Institutional Review Board protocol (no. 00011040).
In Fall 2019, we surveyed graduate students by sending an email out to program administrators of all life sciences graduate programs in the United States that are listed in U.S. News & World Report (2019) . Of the 259 graduate programs that we contacted, 75 (29.0%) program administrators agreed to forward our survey to students enrolled in their graduate programs. Of the 840 graduate students who participated in the survey, 459 (54.6%) self-identified as having depression based on general demographic questions on the survey. Of the 459 students who identified as having depression, 327 (71.2%) agreed to be contacted for a follow-up interview. In Summer 2020, we sent a recruitment email out to the 327 students who identified as having depression, asking to interview them about their experiences with depression in a PhD program. We specifically did not require that students be diagnosed with depression in order to participate in the interview study. We did not want to bias our sample, as mental health care is disproportionately unavailable to Black and Latinx individuals, as well as to those who come from low socioeconomic backgrounds ( Howell and McFeeters, 2008 ; Kataoka et al. , 2002 ; Santiago et al. , 2013 ). Of the students who were contacted, 50 PhD students (15.3%) enrolled across 28 life sciences PhD programs completed an interview.
The interview script was based on a previous interview script that we had developed, which successfully elicited what aspects of research affect depression in undergraduates and how depression affects their research ( Cooper et al. , 2020a ). Our previous work has shown that research experiences do not exclusively worsen depression, but that aspects of research can also help students manage their depression ( Cooper et al. , 2020a ). As such, our interview questions explored what aspects of research helped students manage their depression (positively affecting depression), and what aspects worsened students’ depression (negatively affecting depression). Additionally, we hypothesized that other prominent aspects of graduate school, such as teaching, would also affect PhD student depression and revised the interview script to include questions focused on examining the relationship between depression and teaching. We asked students what aspects of graduate research and teaching made their depression worse and what aspects helped them manage their depression. Participants were invited to come up with as many aspects as possible. We also asked how students perceived their depression affected their research and teaching. With the knowledge that we would be conducting interviews during summer of 2020 in the midst of the COVID-19 pandemic, and that the pandemic had likely exacerbated graduate student depression ( Chirikov et al. , 2020 ), we directed students to not reference aspects of research and teaching that were uniquely related to the pandemic (e.g., teaching remotely or halted research) when discussing the relationship between research, teaching, and depression. We were specifically interested in aspects of teaching and research that affected student depression before the pandemic and would presumably affect student depression afterward. We conducted think-aloud interviews with four graduate students who identified as having depression to ensure that our questions would not offend anyone with depression and to establish cognitive validity of the interview script by ensuring that each student understood what each question was asking. The interview script was iteratively revised after each think-aloud interview ( Trenor et al. , 2011 ). A final copy of the interview script can be found in the Supplemental Material.
All interviews were conducted using Zoom by one of two researchers (L.E.G. or K.M.C.). The average interview time was about 45 minutes. After the interview, all participants were sent a short survey to collect their demographics and additional information about their depression (a copy of the survey can be found in the Supplemental Material). Participants were provided a small monetary gift card in exchange for their time. All interviews were deidentified and transcribed before analysis.
Interview Analysis
Three researchers (L.E.G., N.J.W., and K.M.C.) independently reviewed 12 of the same randomly selected interviews to explore each idea that a participant expressed and to identify recurring themes ( Charmaz, 2006 ). Each researcher took detailed analytic notes during the review. After, the three researchers met to discuss their notes and to identify an initial set of recurring themes that occurred throughout the interviews ( Saldaña, 2015 ). The authors created an initial codebook outlining each theme and the related description. Together, the authors then reviewed the same set of five additional interviews to validate the themes outlined in the codebook and to identify any themes that may have been missed during the initial review. The researchers used constant comparison methods to compare quotes from the interviews to each theme and to establish whether any quotes were different enough from a particular theme to warrant an additional code ( Glesne and Peshkin, 1992 ). Together, the three researchers revised the codebook until they were confident that it captured the most common themes and that no new themes were emerging. A final copy of the codebook can be found in the Supplemental Material. Two authors (L.E.G. and N.J.W.) used the final codebook to code five randomly selected interviews (10% of all interviews) and their Cohen’s κ interrater score was at an acceptable level (κ = 0.94; Landis and Koch, 1977 ). Then, one researcher (N.J.W.) coded the remaining 45 interviews. In the text, we present themes mentioned by at least 10% of interviewees and use quotes to highlight themes. Some quotes were lightly edited for clarity.
Author Positionality
Some of the authors identify as having depression and some do not. One author had completed a PhD program (K.M.C.), one author was in the process of completing a PhD program (L.E.G.), and two authors were undergraduates (N.J.W. and I.F.) at the time when the interviews and analyses took place.
Interview Participants
Fifty PhD students agreed to participate in the study. Students were primarily women (58%), white (74%), and continuing-generation college students (78%). Twelve percent of students were international students, and the average age of the participants was 28 years old. While 20% of students were unsure of their career goals, 32% of students planned to pursue a career in academia, and 24% were planning to pursue a career in industry. Students reported how severe they perceived their depression to be, on average, during the time they had spent in their PhD programs. Most students reported their depression as either moderate (50%) or severe (28%). Eighty percent of students reported being diagnosed with depression, and 74% reported receiving treatment for depression. Participants were at different stages in their PhD programs ranging from first year to sixth year or more. Three students had graduated between the time they completed the initial survey and when they participated in the interview in Summer 2020. Students self-reported their main research areas and represented a broad range, with ecology and evolutionary biology (26%), animal science (14%), molecular biology (14%), and neurobiology (10%) being the most common. Eighty-six percent of students had experience teaching undergraduates, primarily as teaching assistants (TAs), at the time of the interviews. All student demographics are summarized in Table 1 .
| Student-level demographics | Interview participants ( = 50) (%) | Research/teaching demographics | Interview participants ( = 50) (%) | Depression demographics | Interview participants ( = 50) (%) |
|---|---|---|---|---|---|
| Woman | 29 (58) | First year | 4 (8) | Mild | 7 (14) |
| Man | 17 (34) | Second year | 13 (26) | Moderate | 25 (50) |
| Nonbinary/gender fluid | 4 (8) | Third year | 12 (24) | Severe | 14 (28) |
| Fourth year | 5 (10) | Extremely severe | 4 (8) | ||
| Asian/Pacific Islander | 4 (8) | Fifth year | 7 (14) | ||
| Black/African American | 1 (2) | Sixth year or more | 6 (12) | Yes | 40 (80) |
| Hispanic/Latinx | 4 (8) | Recently graduated | 3 (6) | No | 8 (16) |
| White/Caucasian | 37 (74) | Decline to state | 2 (4) | ||
| One or more race/ethnicity | 3 (6) | Animal science | 7 (14) | ||
| Decline to state | 1 (2) | Biochemistry | 3 (6) | Yes | 37 (74) |
| Biological anthropology | 1 (2) | No | 11 (22) | ||
| First generation | 11 (22) | Biology education | 1 (2) | Decline to state | 2 (4) |
| Non–first generation | 39 (78) | Ecology/evolutionary biology | 13 (26) | ||
| Environmental and conservation biology | 2 (4) | Medication | 3 (6) | ||
| Yes | 6 (12) | History and philosophy of science | 1 (2) | Therapy/counseling | 12 (24) |
| No | 44 (88) | Immunology | 4 (8) | Both medication and therapy/counseling | 21 (42) |
| Microbiology | 1 (2) | Decline to state | 14 (28) | ||
| Mean (SD) | 28 (3.4) | Molecular biology and genetics | 7 (14) | ||
| Range | 23–40 | Neurobiology | 5 (10) | ||
| Physiology | 2 (4) | ||||
| Academia | 16 (32) | Plant science | 3 (6) | ||
| General research assistant | 8 (16) | ||||
| Industry | 12 (24) | Yes | 43 (86) | ||
| Science policy | 4 (8) | No | 7 (14) | ||
| Undecided | 10 (20) |
The Effect of Research on Graduate Student Depression
Students more commonly identified ways that research negatively affected their depression than ways research positively affected their depression. Considering all factors that students listed and not just those that were most common, students on average listed two ways in which an aspect of research negatively affected their depression and one way in which an aspect of research positively affected their depression.
The most commonly reported aspect of research that worsened students’ depression was experiencing failures, obstacles, or setbacks in research. Specifically, students cited that failed experiments, failed research projects, and the rejection of manuscripts and grants was particularly difficult for their depression. Conversely, students highlighted that their depression was positively affected when they were able to make substantial progress on their research projects; for example, if they wrote part of a manuscript or if an experiment worked. Students also explained that accomplishing smaller or mundane research tasks was helpful for their depression, both because they felt as though they were checking off a box and also because it allowed them to focus on something other than the negative thoughts often associated with depression.
Students also highlighted that the unstructured nature of graduate research worsened their depression. Specifically, students described that, in graduate research, there are often no clear directions, sets of guidelines, or deadlines to help structure their day-to-day activities. Without this structure, students need to rely on their own motivation to outline goals, accomplish tasks, or seek help, which participants described can be difficult when one is experiencing a depressive episode. However, students also felt as though the unstructured nature of research benefited their depression, because it allowed for flexibility. Those who did not have frequent deadlines or strict schedules were able to not conduct research on days when they needed to recover from a depressive episode or schedule research around therapy or other activities that had a positive impact on their depression. Finally, students highlighted that their passion for their research was protective against depression. Their love for the subject of their research or thinking about how their work may have a positive impact on others could positively affect their motivation or mood.
Students described that their relationships with others in the lab also affected their depression. Specifically, if their mentors or others in their lab had unreasonable or overwhelming expectations of them, it could make them feel as though they would never be able to meet such expectations. Research also provides an environment for students to constantly compare themselves with others, both those in supervisory roles as well as peers. Notably, when students mentioned comparing themselves with others, this comparison never made them feel good about themselves, but was exclusively detrimental to their depression; they felt as though they would never be able to accomplish what others had already accomplished. Students’ relationships with their mentors also seemed to have a notable impact on their depression. Having a positive relationship with their mentors or a mentor who provided psychosocial support positively affected their depression, whereas perceiving a negative relationship with their mentors, particularly a mentor who provided consistently harsh or negative feedback, was detrimental. Students who had absent mentors or mentors who provided infrequent technical support and guidance also felt as though this situation worsened their depression, because it prevented or prolonged their success in research. Finally, students highlighted that conducting graduate research can be isolating, because you are often working on something different from those in the lab or because those outside graduate school cannot relate to the stress and struggles associated with research. However, in instances in which students were able to collaborate with others, this could be protective against depression, because it gave students a sense of comradery or validated their feelings about specific aspects of research. The most common research-related factors that students reported negatively and positively affected their depression and example student quotes of each factor are reported in Tables 2 and 3 , respectively.
| Factor | Description | % ( ) ( = 50) | Example quote | Example quote |
|---|---|---|---|---|
| Failures, obstacles, or setbacks during research | Experiencing failure, obstacles, or setbacks in graduate school can negatively affect student depression. This commonly includes experiencing failed experiments or failed research projects, rejections of grant proposals, or rejections of papers. | 48 (24) | Student 20: “Everything just fails and you have zero positive results and nothing you can publish. That was one of the worst things for me. The stress of knowing that you are not succeeding is really bad [for depression].” | Student 5: “I could do everything perfectly and for one reason or another the whole project could just fail. So, I think the breakdown of that link between my actions and the outcome, that was hard.” |
| Unstructured research experiences | Research experiences that are unstructured, that is, they do not have a clear set of directions or deadlines to guide the work, can negatively affect student depression. | 38 (19) | Student 34: “My depression has not enjoyed or been spared by the fact that research is self-directed. Finding the equipment, finding the questions, finding the method rests on me.” | Student 12: “For me, I think the periods of time post-classes were a lot harder in terms of mental health, where there aren’t as many external deadlines. You’re mostly driven by your own goals and ambitions every day. (…) But when [goals and ambitions] are dropped, it’s really easy for depression to kick in.” |
| Negative reinforcement | Negative reinforcement from others in research such as harsh criticism, feedback, comments, or reviews about one’s research or performance can negatively affect student depression. | 34 (17) | Student 26: “[Your mentor] will tell you how poorly you’re doing to inspire you to work harder, and that’s not something that works with me, because I already see everything that I’m doing wrong, and all the problems in a project, so I don’t need a mentor that points out those problems to me again, because I’m like, ‘Yeah, I [expletive] know all the problems! I should just quit, right?’” | Student 7: “You say something stupid and your PI (principal investigator) suddenly says how stupid that is. And then all that just [makes me think] ‘I’m an idiot, I can’t do it.’” |
| Unreasonable or overwhelming expectations | Mentors or others in research who place too high of expectations on students, particularly related to the progress that they are making in research, can negatively affect student depression. | 34 (17) | Student 4: “My [previous] advisor had really high expectations and was really pushy. It really exacerbated my depression a lot, because I felt like I could never live up to the expectations.” | Student 29: “I think when I’m working hard and where my hours are going doesn’t necessarily make sense to my advisor [it affects my depression]. I’m like, ‘No, I’m working, I’m working, I’m working.’ And then they’re like, ‘Well, but maybe work harder.’ That feels pretty bad.” |
| Opportunity to compare self to others | When students compare their success in research to others’ success, it can negatively affect their depression. | 28 (14) | Student 24: “I think that I’m a huge person that compares themselves to others. When I hear others speak about their research or their progress, though it may not be light years away from mine, it feels that way. I get sad. I feel like I’m not where I’m supposed to be or that I don’t deserve to be where I’m at compared to others.” | Student 44: “Sometimes I see my other cohort students succeeding and not even in a jealous way necessarily, but I do measure myself against them. If I haven’t gotten my first author publication yet or whatever, that means I’m behind the curve. I think part of [my depression] is just comparing myself to others.” |
| Lack of technical support or guidance | Not receiving adequate support or guidance in research can negatively affect student depression. | 22 (11) | Student 18: “I’ve experienced my PI being very absent. And so, not having that touchstone of advice like, ‘Stop now, maybe stop while you’re ahead, or maybe you can change this,’ and then wasting all that time or feeling like I’ve wasted all that time can make it harder [on my depression].” | Student 49: “You get thrown in the deep end on projects, and the lab has been so busy that there’s been no support. So, if you fall a little flat, then it’s just all on you where they’re like, ‘Oh man, I wish I could help you out with that or give you this support,’ and I feel like I’ve been set up to fail a lot.” |
| Social isolation | Feeling isolated when doing research, either because others in the lab or others outside graduate school cannot relate to specific stressors and experiences, can negatively affect student depression. | 18 (9) | Student 8: “[Doing research] is very isolating because obviously not many people go for PhDs. I can’t talk to [my friends] about research struggles because they’re like, ‘OK, how do I fix that? You did that to yourself.’ And I’m like, ‘I mean, you’re right, but…’ Nobody understands you.” | Student 20: “I think that’s one thing [that affects my depression], when it comes to research, it’s quite a lonely experience sometimes when you’re working on your own project and everybody else has their own project. They have their own worries to think about and all you are stressing about is your own thing.” |
| Factor | Description | % ( ) ( = 50) | Example quote | Example quote |
|---|---|---|---|---|
| Completing small or concrete research tasks | Completing small or concrete research tasks helps students feel like they have accomplished something or distracts their mind from negative thoughts, which can positively affect student depression. | 26 (13) | Student 24: “When I’m doing wet lab work I’m in the zone, [it is good for my depression]. When I’m in that mode, it doesn’t allow me to be depressed, because I’m too busy to really overthink things.” | Student 35: “I have a very simple goal, which is to collect my data and that’s all I think about for the entire day. I’m hiking, I’m listening to audio books, whatever. And so, there’s literally just no time for me to get caught up in my own mind.” |
| Working with others | Interacting with others can positively affect student depression. | 22 (11) | Student 43: “Working collaboratively with other students and working consistently with faculty helps a lot [with my depression].” | Student 20: “Friends, obviously, colleagues, people who share the same sentiment [help my depression]. It’s amazing to have people right next to you say, ‘Don’t worry about it, this happens to everyone. Try this, try that.’” |
| Passionate about research topic | Feeling passionate about their research topic or caring about the potential impact of research can positively affect student depression. | 18 (9) | Student 10: “I love vaccines, I love immunology, I love recombinant genetic engineering. That in itself actually does help [my depression] a lot because I get to learn more every day. (…) That absolutely helps [my depression] because it drives me.” | Student 25: “I study plants and I really love plants and being around them. And so that’s been the best part is getting to work with plants in the greenhouse, and that feels helpful [for my depression].” |
| Flexibility | Flexibility in research allows students to feel as though they have control over their time and they can prioritize their mental health (e.g., by going to therapy or taking a mental health day) when necessary, which can positively affect student depression. | 18 (9) | Student 12: “I can schedule therapy whenever. I’m not confined to a specific nine-to-five workday. (…) If I wake up one day and I’m really struggling, I can shift my weekends. I can be like, ‘All right. Today I need to take care of me,’ and then maybe I’ll work an extra day of the weekend if I need to catch up or something. So that flexibility can be really supportive.” | Student 47: “Some jobs, you have to be there, whereas with grad school if I’m having a really bad day and I really feel like I can’t handle being in the lab, it’s a little easier for me to not have to be there or for me to rearrange my schedule so I’m doing [tasks] that are a little bit less stressful for me.” |
| Research progress | Making significant progress in research can positively affect student depression. | 16 (8) | Student 46: “I will say [something that helps my depression] is when you are working really hard on the experiment, on the goal, and then finally you get something, when you get good data. This makes all of my effort worth it.” | Student 1: “Making progress helps me feel less [depressed], when I am getting a lot of data. I never feel stressed about my productivity at those points in time.” |
| Emotionally supportive PI | A positive mentor relationship, which often involves psychosocial support, can positively affect student depression. | 12 (6) | Student 23: “Things that help [my depression] are having a supportive PI who you’re able to talk to about your mental illness, and who’s understanding.” | Student 38: “If I didn’t have the advisors that I have now, I don’t know that I would be able to proceed through getting a PhD, because I have been able to be very open with them about my mental health struggles and the reality of how mental illness affects me and affects my life and my productivity. And they haven’t really rigorously pushed me beyond my stated limitations.” |
The Effect of Teaching on Graduate Student Depression
We asked all graduate students who had teaching experience ( n = 43) how teaching affected their depression. Graduate students more commonly identified ways that teaching positively affected their depression than ways teaching negatively affected their depression. On average, considering all factors that graduate students listed and not just those that were most common, participants listed two ways in which teaching positively affected their depression and one way in which teaching negatively affected their depression.
Graduate students most commonly highlighted that teaching provided positive reinforcement from undergraduates, which helped them manage their depression. This positive reinforcement came in multiple forms ranging from formal teaching evaluations to positive verbal comments from undergraduates about how good a graduate student was at teaching to watching undergraduates accomplish academic goals or grasp complex concepts. A subset of graduate students highlighted that teaching was good for their depression, because it was something they were passionate about or that they genuinely enjoyed. As such, it was a source of happiness, as was being able to collaborate and form friendships with other TAs or instructors. Some graduate students also acknowledged that they felt confident teaching, often because they had mastered content that undergraduates had not. However, this was not always the case; some graduate students highlighted that a lack of teaching training and preparation negatively affected their self-efficacy as instructors, which in turn exacerbated their depression. This was further exacerbated by the pressure that graduate students put on themselves to perform well as instructors. The potential to have a negative impact on undergraduates and their learning experiences could worsen students’ depression by increasing the stress surrounding their performance as a teacher. Additionally, some graduate students received negative reinforcement from undergraduates, in the form of negative comments on formal teaching evaluations or disrespectful behavior from undergraduates such as groans or eye rolls, which graduate students explained negatively affected their self-efficacy, further worsening their depression.
Students also highlighted that teaching could negatively affect their depression because it interfered with the time they felt they needed to be spending on research or added to the large number of responsibilities they had as graduate students. However, some students welcomed time away from research; teaching sometimes served as a distraction from research-related stressors. Students also highlighted that teaching is structured, which positively affected their depression. That is, there are concrete tasks, such as grading, that need to be accomplished or places that the graduate student needs to be during a specific time. This structure helped motivate them to accomplish teaching goals, even if they were feeling a lack of motivation because of their depression. The most common teaching-related factors that graduate students reported negatively and positively affected their depression and example student quotes for each factor are reported in Tables 4 and 5 , respectively.
| Factor | Description | % ( ) ( = 43) | Example quote | Example quote |
|---|---|---|---|---|
| Increases number of responsibilities/time away from research | Teaching adds to the total number of responsibilities that graduate students have and can interfere with the time that they feel they need to spend on research, which increases stress and can negatively affect student depression. | 47 (20) | Student 10: “As a PhD student, you’re expected to publish, do all this research, and then also teach. A little while ago, I was both designing a class and teaching two sections at the same time, and I was spending so much time on that class. It was close to 40 hours per week plus research. I definitely was feeling overwhelmed, and I do think that can affect [my depression], because it leads to burnout.” | Student 12: “Teaching often regularly leaves you with less time to focus on research. So, it is time away from research. And if I’m already feeling like I’m not doing enough, having the extra load of teaching can just amp that feeling up.” |
| Negative reinforcement from undergraduates | Negative reinforcement from undergraduates, in the form of being rude, disrespectful, or disengaged, or receiving negative scores and comments on teaching evaluations, can negatively affect student depression. | 28 (12) | Student 29: “It [is hard for my depression] and really bums me out when [the undergraduates] don’t try. I put a lot into [teaching]. (…) The ones that are just like, ‘I don’t want to do this,’ and roll their eyes, it’s just hard. It’s like, I put so much into making [the content] clear and I’m trying. So, when the students are not really trying, it does not feel great.” | Student 19: I’ve had students straight up tell me, ‘This is the least important class that I have to take this semester. I’m not going to put in much effort.’ And it makes me feel kind of crummy, kind of bad. When at the end of the semester, I get the teaching evaluations saying, ‘I just took this class because I need it or I had to. I didn’t think it added anything to my education.’ I feel very low.” |
| Personal pressure to teach well | Feeling an obligation to teach undergraduates well or ensure that they understand the course content can induce stress and negatively affect depression. | 26 (11) | Student 16: “[My depression related to teaching] all comes back to the stress of having to do a good job for my students. I didn’t want to fail them. So that was difficult and I took [being a teacher] very seriously.” | Student 40: “I think feeling like there were these undergrads depending on me [negatively affected by depression]. (…) If I haven’t sufficiently prepared to lead a discussion section or whatever, there are undergrads whose education will suffer. That added pressure was hard [on my depression] and just being afraid of letting them down.” |
| Lack of teaching training or guidance | Not having training or guidance about how to teach made students feel insecure about their teaching abilities, which can negatively affect their depression. | 16 (7) | Student 25: “[My depression worsened] because I was concerned about the lack of supervision and the lack of support for how to teach. (…) I just felt like I was doing a terrible job, which was really discouraging.” | Student 26: “I didn’t feel like I had enough guidance as to what I should be teaching [the undergraduates in my class] and how to control a classroom, so not having the respect of the students and not knowing how to get it was really stressful.” |
a Forty-three out of the 50 students who participated in the study had experience teaching undergraduates either as a TA or as an instructor of record. We only considered the responses from the TAs with teaching experiences when calculating the percent of students who reported each factor.
| Factor | Description | % ( ) ( = 43) | Example quote | Example quote |
|---|---|---|---|---|
| Positive reinforcement from undergraduates | Positive reinforcement from undergraduates, in the form of positive verbal comments, positive comments on formal evaluations, or watching undergraduates grasp a concept or get excited about content, can positively affect student depression. | 58 (25) | Student 15: “What really helped me during those depressive times were that my students would say like, ‘Sulfates in my shampoo, they’re not good for the water. I learned that from you.’” | Student 5: “Interacting with my undergraduates and feeling like I made a difference for them [helps my depression]. Even if it was just something as simple as them saying like, ‘Oh, wow [Student 5], I feel like I actually really get this now,’ or ‘I did better on this exam after we went over material together.’” |
| Teaching as a structured task | The structured nature of teaching, including having concrete tasks to accomplish and specific places to be at specific times, can positively affect student depression. | 33 (14) | Student 27: “Sometimes having concrete tasks does [help my depression]. With research, you never have deadlines or things that get accomplished or finished. Where at least with teaching, you can sit down and you can grade for three hours. You can do things.” | Student 8: “I have to have the test made by the time class starts on an exam day. I have to make sure that I’m there on time and that I don’t go over time, things like that. So just having that kind of strict schedule, I think helped [my depression].” |
| Passion for teaching | Being passionate about teaching and enjoying teaching can positively affect student depression. | 30 (13) | Student 48: “I’ve always enjoyed teaching. One main reason I did a PhD was to teach at the postsecondary level. So, for me, honestly, the experience of interacting with students is energizing, and does rejuvenate me a lot.” | Student 15: “[Teaching] gave me motivation and kind of like a reason to keep going. I love science, but I love the access to science that I can give to other people.” |
| Distraction from research | Teaching can serve as a distraction from stressors related to research, which can positively affect student depression. | 23 (10) | Student 42: “Research is tedious and difficult and honestly I have to admit I never really had fun with it. But teaching is kind of a way away from that. It’s something that you can still do and you can still contribute like you’ve got a good job and you’re doing things. (…) It helped take my mind off of the hardships of what was going on during research.” | Student 4: “[Teaching] is a good respite from my research sometimes. It’s a different side to being in school.” |
| Confidence about teaching | Having confidence about teaching, specifically about being a good teacher or having mastery of the content, can positively affect student depression. | 14 (6) | Student 42: “[Teaching] is helpful for my depression because, like I am sorry if this is cocky sounding, but I’m really good at teaching and when I go in to teach, it’s like, ‘I know that this is right.’” | Student 50: “It’s good to feel like an expert in front of this group of undergrads. When you come from maybe a lab, or field experience where you feel like you don’t know what you’re doing, it can be very positively reinforcing working with undergrads.” |
| Positive relationships with others teaching | Having positive relationships with others involved in teaching, particularly other TAs or a lead instructor, can positively affect student depression. | 12 (5) | Student 16: “[Teaching] was really helpful for my depression, because I made friends with the other TAs, especially during my first year as a TA, and we were all new.” | Student 28: “I had a co-TA giving a lecture with me and he was a very nice person. So, we became friends. Yeah. It helped [my depression] a little bit.” |
The Effect of Depression on Graduate Research
In the interviews, we asked graduate students how their depression affected their graduate research, if at all. They identified three primary ways in which depression could affect research, all of which were negative. The most common way depression affected research was interfering with students’ motivation, which in turn affected their productivity. Students described that their productivity was affected immediately, for example, struggling to execute daily tasks like collecting or analyzing data. However, graduate students described that their lack of motivation ultimately resulted in larger consequences, such as delays in getting papers submitted and published. In fact, some graduate students explicitly stated that they felt as though they would have been able to graduate earlier if they had not had depression. The second way in which depression affected graduate students’ research is that it interfered with their ability to focus or concentrate. Students primarily explained that the lack of focus did not delay their research but caused their research to be less enjoyable or made them frustrated because they had to expend additional mental energy to execute tasks. Depression also caused students to be less confident or overly critical of themselves. Specifically, if an experiment did not go right or they experienced rejection of a manuscript, they tended to internalize it and blame themselves. This lack of confidence often inhibited students’ abilities to make decisions about research or take risks in research. They described frequently second-guessing themselves, which made decisions and taking risks in research more difficult. The most common ways students reported that their depression affected their research and example student quotes are reported in Table 6 .
| Theme | Description | % ( ) ( = 50) | Example quote | Example quote |
|---|---|---|---|---|
| Lack of motivation and productivity | Depression can make students feel less motivated to do research, which can result in a lack of productivity. This lack of productivity can range from not being able to analyze a data set to not being able to write and submit a paper. | 64 (32) | Student 3: “When I’m really depressed and I’m trying to do something that’s pretty positive and challenging, like write a manuscript, it tends to be really difficult. I can go from, when I’m not depressed, banging out some really good work, and then when I become depressed, that definitely tanks.” | Student 35: “[Depression] keeps me from doing the things that I want to do, like every single day and be consistent. Like reading a paper every day or writing for an hour every day and it’s just like, I am so exhausted that I feel like I can’t do that. It increases procrastination.” |
| Low self-esteem or overly self-critical | Depression can cause students to doubt their abilities as a scientist, be self-critical, internalize failure, take unnecessary responsibility for something that did not work, and be hyperaware of any issues they may be having. | 58 (29) | Student 10: “Sometimes I feel I’m an imposter. Internally I know that I have intelligence, but then it’s like I don’t know if I can do it. Everything is harder, and then my research will suffer.” | Student 19: “[My depression] brings on this imposter syndrome. Like, ‘What am I doing in this program?’ So, I’m constantly struggling and battling those thoughts. Never feeling that you fit in, struggling with, ‘Are you good enough? Is what you’re doing good enough? Should I stay in this program?’” |
| Difficulty focusing and concentrating | Depression can cause students to be distracted or unfocused or to struggle to pay attention to detail, which can result in feelings of frustration and exhaustion. | 28 (14) | Student 9: “Because I was going through kind of a mental instability, I was unable to actually focus on what I was actively doing in lab. I was kind of like a zombie going in to work and getting out every day.” | Student 40: “The trouble concentrating just makes everything harder when you just can’t seem to sit down and focus and get things done. I would say it’s made grad school harder, more frustrating, and less enjoyable because I just constantly feel like I’m behind and not doing enough.” |
The Effect of Depression on Teaching
Graduate students described one positive way and two negative ways that depression affected their teaching. Students explained that, because they had experienced depression, they were more compassionate and empathetic toward the undergraduates in their courses. Specifically, they felt they could better understand some of the struggles that undergraduates experience and were sometimes more likely to be flexible or lenient about course requirements and deadlines if an undergraduate was struggling. However, graduate students reported that depression also negatively affected their teaching. Specifically, depression could cause graduate students to feel disconnected or disengaged from undergraduates. It could also cause graduate students to feel as though they had a lack of energy or felt down when teaching. The common self-reported ways that depression affected PhD students’ teaching and example quotes are reported in Table 7 .
| Factor | Description | % ( ) ( = 43) | Example quote | Example quote |
|---|---|---|---|---|
| Negative effects on depression on graduate student teaching | ||||
| Disconnected or disengaged from undergraduates | Depression can cause graduate students to feel disengaged when teaching or to have trouble connecting with undergraduates. | 16 (7) | Student 18: “[When I have depression], I can feel disconnected from the [undergraduates]. I’ll go to my day of teaching, I lead these discussion sections and I’m going through the motions. I don’t really put my full heart into it in terms of going out of my way to connect with the [undergraduates] or being more enthusiastic.” | Student 49: “But there were many days that my depression, through various avenues, caused me to be absentminded [while teaching]. (…) Just less attentive and [less] engaged.” |
| Felt down or lacked energy when teaching | Depression can cause graduate students to be less energetic or to have a low mood when teaching. | 14 (6) | Student 4: “There’s been times where I’ve just been unable to prep for classes, or have prepped very little, just because I’m just struggling with myself and trying to get through things. It upsets me, because I feel like I’m letting the undergrads down.” | Student 13: “I’m sure [my students] have been able to tell when I’ve shown up to classrooms just depressed. And that’s not what they’re paying for, and they’re paying a lot.” |
| Positive effect of depression on graduate student teaching | ||||
| Understanding of student issues | Depression can positively impact graduate students as instructors because they are more understanding or sympathetic to student struggles, including mental health issues. | 23 (10) | Student 16: “[My depression] maybe makes me a little more empathetic with the undergraduates that I teach. And I know that since depression is a big deal for me, it may be as big deal for them. I’m able to empathize better and help people seek out the right resources if necessary, and also give them a leniency that they need if they can’t accomplish something in the time it’s due because of their illness.” | Student 48: “I think it makes me more empathetic to the plights of undergraduate students, because I know that they also experience a lot of these [mental health] problems, and so I think it makes me more sympathetic to their problems.” |
a Forty-three out of the 50 students who participated in the study had experience teaching undergraduates either as a TA or as an instructor of record. We only considered the responses from the TAs with teaching experiences when calculating the percent of students who reported each theme.
Despite the increasing concern about graduate student mental health among those in the scientific community ( Pain, 2018 ; “The Mental Health of PhD Researchers,” 2019; Puri, 2019 ), there is a lack of information about how specific aspects of science PhD programs affect students with depression. This is the first study to explicitly investigate which particular aspects of research and teaching affect depression among life sciences PhD students and how depression, in turn, affects graduate students’ experiences in research and teaching. Overall, graduate students highlighted factors related to teaching and research that both alleviated and exacerbated their symptoms of depression. Graduate students more commonly brought up ways that research negatively affected their depression, than ways that it positively affected their depression. Conversely, graduate students more commonly mentioned ways that teaching had a positive effect on their depression compared with a negative effect. The requirement and opportunity to teach differs among life sciences graduate programs ( Schussler et al. , 2015 ; Shortlidge and Eddy, 2018 ). As such, future research should investigate whether the amount of teaching one engages in during graduate school is related to levels of graduate student depression. Despite differences in how teaching and research affect student depression, this study unveiled factors that protect against or worsen depressive symptoms. Specifically, four overarching factors affecting graduate student depression emerged from the interviews: 1) Structure; 2) Positive and Negative Reinforcement; 3) Failure and Success; 4) Social Support and Isolation. We discuss here how each of these factors may positively and negatively affect graduate student depression.
One stark contrast between research and teaching is the amount of structure in each activity. That is, students expressed that research goals are often amorphous, that there are not concrete instructions for what needs to be accomplished, and that there is often no set schedule for when particular tasks need to be accomplished. Conversely, with teaching, graduate students often knew what the goals were (e.g., to help students learn), exactly what they needed to accomplish each week (e.g., what to grade, what to teach), and when and where they needed to show up to teach (e.g., a class meets at a particular time). Graduate students highlighted that a lack of structure, particularly in research, was detrimental for their depression. Their depression often made it difficult for them to feel motivated when there was not a concrete task to accomplish. Major depression can interfere with executive function and cognition, making goal setting and goal achievement particularly difficult ( Elliott, 1998 ; Watkins and Brown, 2002 ). In fact, research has documented that individuals with depression generate less specific goals and less specific explanations for approaching a goal than individuals who do not have depression ( Dickson and Moberly, 2013 ). As such, it may be particularly helpful for students with depression when an activity is structured, relieving the student from the need to articulate specific goals and steps to achieve goals. Students noted that the lack of structure or the flexibility in research was helpful for their depression in one way: It allowed them to better treat their depression. Specifically, students highlighted that they were able to take time to go to therapy or to not go into the lab or to avoid stressful tasks, which may be important for successful recovery from a depressive episode ( Judd et al. , 2000 ).
Compared with conducting research, many participants reported that the concrete tasks associated with teaching undergraduates were helpful for their depression. This is supported by literature that illustrates that concrete thinking, as opposed to abstract thinking, can reduce difficulty making decisions in individuals with depression ( Dey et al. , 2018 ), presuming that teaching often requires more concrete thinking compared with research, which can be more abstract. Additionally, cognitive-behavioral treatments for depression have demonstrated that developing concrete goals for completing tasks is helpful for individuals with depression ( Detweiler-Bedell and Whisman, 2005 ), which aligns with graduate students’ perceptions that having concrete goals for completing teaching tasks was particularly helpful for their depression.
Positive and Negative Reinforcement
Graduate students reported that the negative reinforcement experienced in research and teaching had a significant negative effect on their depression, while the positive reinforcement students experienced only in teaching had a positive effect. Notably, students did not mention how positive reinforcement affected their depression in the context of research. Based on student interviews, we predict that this is not because they were unaffected by positive reinforcement in research, but because they experienced it so infrequently. Drawing from behavioral theories of depression, the concept of response-contingent positive reinforcement (RCPR; Lewinsohn, 1974 ; Kanter et al. , 2004 ) helps explain this finding. As summarized by Kanter and colleagues (2004) , RCPR describes someone seeking a response and being positively reinforced; for example, graduate students seeking feedback on their research are told that what they have accomplished is impressive. Infrequent RCPR may lead to cognitive symptoms of depression, such as low self-esteem or guilt, resulting in somatic symptoms of depression, such as fatigue and dysphoria ( Lewinsohn, 1974 ; Martell et al. , 2001 ; Manos et al. , 2010 ). RCPR is determined by three factors. 1) How many potential events may be positively reinforcing to an individual. For example, some people may find an undergraduate scoring highly on an exam in a class they are teaching to be reinforcing and others may find that they only feel reinforced when an undergraduate explicitly compliments their teaching. 2) The availability of reinforcing events in the environment. If graduate students’ mentors have the ability to provide them with RCPR but are never able to meet with them, these reinforcing events are unavailable to them. 3) The instrumental behavior of an individual. Does the individual exhibit the behavior required to obtain RCPR? If graduate students do not accomplish their research-related tasks on time, they may not receive RCPR from their mentor. If individuals are not positively reinforced for a particular behavior, they may stop exhibiting it, further exacerbating the depressive cycle ( Manos et al. , 2010 ). Therefore, the lack of positive reinforcement in research may be particularly damaging to graduate students, because it may discourage them from completing tasks, leading to additional depressive symptoms. Conversely, teaching presents many opportunities for positive reinforcement. Every time graduate students teach, they have the opportunity to receive positive reinforcement from their students or to witness a student’s academic accomplishment, such as an undergraduate expressing excitement when they understand a concept. As such, it is not surprising that positive reinforcement was the primary teaching-related factor that graduate students reported helped with their depression. Despite the positive reinforcement of teaching for graduate students with depression, we are not suggesting that graduate students should take on additional teaching loads or that teaching should be viewed as the sole respite for graduate students with depression. Overwhelming students with increased responsibilities may counteract any positive impact that teaching could have on students’ depression.
Failure and Success
Failure and success affected student depression, but only in the context of research; contrary to research, students rarely mentioned concrete metrics for success and failure in teaching. While graduate students highlighted receiving positive or negative reinforcement from undergraduates, they did not relate this to being a “successful” instructor. It is unsurprising that graduate students did not mention failing or succeeding at teaching, given that experts in teaching agree that it is difficult to objectively evaluate quality teaching ( d’Apollonia and Abrami, 1997 ; Kember et al. , 2002 ; Gormally et al. , 2014 ). In fact, the lack of teacher training and knowledge about how to teach effectively negatively affected student depression, because it could cause students to feel unprepared as an instructor. Integrating teacher training into graduate programs has been championed for decades ( Torvi, 1994 ; Tanner and Allen, 2006 ; Schussler et al. , 2015 ); however, the potential for such training to bolster graduate student mental health is new and should be considered in future research. With regard to graduate students’ research, the concept of success and failure was far more concrete; students mentioned failing in terms of failed experiments, research projects, and rejected manuscripts and grant proposals. Successes included accepted manuscripts, funded grant proposals, and concrete progress on significant tasks, such as writing or conducting an experiment that yielded usable data. Failure has been shown to negatively affect depression among undergraduate researchers ( Cooper et al. , 2020a ), who are hypothesized to be inadequately prepared to experience failure in science ( Henry et al. , 2019 ). However, it is less clear how well prepared graduate students are to experience failure ( Simpson and Maltese, 2017 ). Drawing from cognitive theories of depression, depression is associated with dysfunctional cognitive schemas or dysfunctional thinking that can lead individuals with depression to have negative thoughts about the world, themselves, and the future and to interpret information more negatively than is actually the case (called negative information-processing biases; Beck, 1967 ; Beck et al. , 1979 ; Gotlib and Krasnoperova, 1998 ; Maj et al. , 2020 ). Related to failure, individuals with dysfunctional cognitive schemas may harbor beliefs such as if something fails at work (or in graduate research), they are a failure as a person or that a small failure can be as detrimental as a larger failure ( Weissman, 1979 ; Miranda and Persons, 1988 ). As such, setbacks in research may be particularly difficult for PhD students with depression. Graduate students in our study also mentioned how failing in research was often out of their control, particularly failure related to experiments and research projects. The extent to which one feels they can control their environment is important for mental health, and lower estimates of control have been hypothesized to be an important factor for depression ( Grahek et al. , 2019 ). Therefore, this feeling of being unable to control success in research may further exacerbate student depression, but this would need to be tested. Importantly, these findings do not imply that individuals with depression are unable to cope with failure; they only suggest that individuals perceive that failure in science can exacerbate their depression.
Social Support and Isolation
Graduate students reported that feelings of isolation in research could worsen their depression. Specifically, they highlighted that it can be difficult for their mental health when their friends outside graduate school cannot relate to their struggles in research and when others in their research group are not working on similar projects. One study of more than 1400 graduate students at a single university found that feeling isolated from fellow graduate students and faculty positively predicted imposter phenomenon ( Cohen and McConnell, 2019 ), defined as the worry that they were fooling others about their abilities and that their fraudulence would be exposed ( Clance and Imes, 1978 ), which is positively correlated with depression among college students ( McGregor et al. , 2008 ). Developing a positive lab environment, where undergraduates, graduate students, and postgraduates develop positive relationships, has been shown to positively affect undergraduates ( Cooper et al. , 2019 ) and may also positively affect graduate students who experience such feelings of isolation. Graduate students in this study described that both teaching and research had the potential to be a source for relationship development and social support. Students who described positive collaborative relationships in research and teaching felt this had a positive impact on their depression, which aligns with a review of studies in psychiatry concluding that being connected to a large number of people and having individuals who are able to provide emotional support by listening or giving advice is protective against depression ( Santini et al. , 2015 ), as well as a study that found that social support is protective against depression, specifically among the graduate population ( Charles et al. , 2021 ).
These four factors provide clear targets for graduate programs looking to improve the experiences of students with depression. For example, increasing structure in research could be particularly helpful for graduate students with depression. Ensuring that students have concrete plans to accomplish each week may not only positively impact depression by increasing structure, but ultimately by increasing a student’s success in research. Research mentors can also emphasize the role of failure in science, helping students realize that failure is more common than they may perceive. Increasing opportunities for positive reinforcement in teaching and research may be another avenue to improving student mental health. Providing students with appropriate teacher training is a first step to enhancing their teaching skills and potential for positive reinforcement from undergraduate students ( Schussler et al. , 2015 ). Additionally, teaching evaluations, a common form of both positive and negative reinforcement, are known to be biased and disadvantage women, People of Color, and those with non–English speaking backgrounds ( Fan et al. , 2019 ; Chávez and Mitchell, 2020 ) and arguably should not be used to assess teaching. In research, mentors can make an effort to provide positive feedback or praise in meetings in addition to critiques. Finally, to provide social support to graduate students with depression, graduate programs could consider creating specific initiatives that are related to supporting the mental health of graduate students in their departments, such as a support group for students to meet and discuss their experiences in graduate school and how those experience pertain to their mental health.
Limitations and Directions for Future Research
In this study, we chose to only interview students with the identity of interest (depression), as is common with exploratory studies of individuals with underserved, underrepresented, or marginalized identities (e.g. Carlone and Johnson, 2007 ; Cooper and Brownell, 2016 ; Barnes et al. , 2017 , 2021 ; Downing et al. , 2020 ; Gin et al. , 2021 ; Pfeifer et al. , 2021 ). However, in future studies, it would be beneficial to also examine the experiences of individuals who do not have depression. This would provide information about the extent to which specific aspects of graduate research and teaching are disproportionately beneficial or challenging for students with depression. In this study, we did not explicitly examine whether there was a relationship between students’ identities and depression because of the small number of students in particular demographic groups. However, a theme that occurred rather infrequently (but is included in the Supplemental Material) is that discrimination or prejudice in the lab or academia could affect depression, which was reported exclusively by women and People of Color. As such, disaggregating whether gender and race/ethnicity predicts unique factors that exacerbate student depression is an important next step in understanding how to create more equitable and inclusive research and teaching environments for graduate students. Moreover, our sample included a significant number of students from ecology and evolutionary biology PhD programs, which may limit the generalizability of some findings. It is important to acknowledge potential subdisciplinary differences when considering how research may affect depression. Additionally, some of the factors that affect student depression, such as lack of teaching training and confidence in teaching, may be correlated with time spent in a graduate program. Future quantitative studies would benefit from examining whether the factors that affect student depression depend on the student’s subdiscipline and time spent in the graduate program. The primary focus of this study was the relationship between depression and graduate teaching/research. Many of the factors that emerged from the interviews are also associated with burnout ( Bianchi et al. , 2014 ; Maslach et al. , 2001 ). Burnout and depression are known to be highly related and often difficult to disaggregate ( Bianchi et al. , 2014 ). It was beyond the scope and design of this study to disaggregate which factors relate exclusively to the condition of burnout. Additionally, the interviews in this study were collected at a single time point. Thus, we are unable to differentiate between students who had depression before starting graduate school and students who experienced depression after starting graduate school. Future longitudinal studies could explore the effects of students’ experiences in research and teaching on their depression over time as well as on long-term outcomes such as persistence in graduate programs, length of time for degree completion, and career trajectory. This study identified a number of factors that graduate programs can address to benefit graduate student mental health, and we hope that future studies design and test interventions designed to improve the experiences of graduate students in teaching and research.
In this interview study of 50 life sciences PhD students with depression, we examined how graduate research and teaching affect students’ depressive symptoms. We also explored how depression affected graduate students’ teaching and research. We found that graduate students more commonly highlighted ways that research negatively affected their depression and ways that teaching positively affected their depression. Four overarching factors, three of which were related to both teaching and research, were commonly associated with student depression, including the amount of structure provided in research and teaching, failure and success, positive and negative reinforcement, and social connections and isolation. Additionally, graduate students identified depression as having an exclusively negative effect on their research, often hindering motivation, concentration, and self-esteem. However, they did note that depression made them more compassionate teachers, but also could cause them to have low energy or feel disconnected when teaching. This study provides concrete factors that graduate programs can target in hopes of improving the experiences of life sciences PhD students with depression.
Important Note
There are resources available if you or someone you know is experiencing depression and want help. Colleges and universities often have crisis hotlines and counseling services designed to provide students, staff, and faculty with treatment for depression. These can often be found by searching the university website. Additionally, there are free 24/7 services such as Crisis Text Line, which allows you to text a trained live crisis counselor (text “CONNECT” to 741741; Text Depression Hotline, 2019 ), and phone hotlines such as the National Suicide Prevention Lifeline at 1-800-273-8255 (TALK). If you would like to learn more about depression or depression help and resources near you, visit the Anxiety and Depression Association of American website: https://adaa.org ( Anxiety and Depression Association of America, 2019 ) and the Depression and Bipolar Support Alliance: http://dbsalliance.org ( Depression and Bipolar Support Alliance, 2019 ).
ACKNOWLEDGMENTS
We are incredibly grateful to the 50 graduate students who were willing to share their personal experiences with us. We thank Sara Brownell, Tasneem Mohammed, Carly Busch, Maddie Ostwald, Lauren Neel, and Rachel Scott for their helpful feedback on earlier drafts of this work. L.E.G. was supported by an NSF Graduate Fellowship (DGE-1311230). Any opinions, findings, conclusions, or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the NSF.
- American College Health Association . ( 2014 ). Graduate/professional reference group report, Spring 2014 (American College Health Association National College Health Assessment II) . Retrieved March 15, 2021, from www.acha.org/documents/ncha/NCHA-II_WEB-PAPER_SPRING2014_GRADUATE_PROFESSIONAL_REFERENCEGROUP_DATAREPORT.pdf Google Scholar
- American College Health Association . ( 2019 ). Graduate/professional reference group report, Spring 2019 (American College Health Association National College Health Assessment II) . Retrieved March 15, 2021, from www.acha.org/documents/ncha/NCHA-II_SPRING_2019_GRADUATE_AND_PROFESSIONAL_REFERENCE_GROUP_DATA_REPORT.pdf Google Scholar
- American Psychiatric Association . ( 2013 ). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Publishing. Google Scholar
- American Psychiatric Association . ( 2020 ). What is depression? Retrieved March 15, 2021, from www.psychiatry.org/patients-families/depression/what-is-depression Google Scholar
- Anxiety and Depression Association of America . ( 2015 ). A survey about mental health and suicide in the United States . Retrieved March 15, 2021, from https://adaa.org/sites/default/files/College-Aged_Adults_Survey_Summary-1.14.16.pdf Google Scholar
- Anxiety and Depression Association of America . ( 2019 ). Retrieved October 1, 2019, from https://adaa.org Google Scholar
- Barnes, M. E., Truong, J. M., & Brownell, S. E. ( 2017 ). Experiences of Judeo-Christian students in undergraduate biology . CBE—Life Sciences Education , 16 (1), ar15. Link , Google Scholar
- Barnes, M. E., Maas, S. A., Roberts, J. A., & Brownell, S. E. ( 2021 ). Christianity as a concealable stigmatized identity (CSI) among biology graduate students . CBE—Life Sciences Education , 20 (1), ar9. Link , Google Scholar
- Beck, A. T. ( 1967 ). Depression: Clinical, experimental and theoretical aspects . New York: Harper & Row. Google Scholar
- Beck, A. T., Rush, A. J., & Shaw, B. F. ( 1979 ). Cognitive therapy of depression . New York, NY: Guilford. Google Scholar
- Bianchi, R., Schonfeld, I. S., & Laurent, E. ( 2014 ). Is burnout a depressive disorder? A reexamination with special focus on atypical depression . International Journal of Stress Management , 21 (4), 307. Google Scholar
- Barreira, P., Basilico, M., & Bolotnyy, V. ( 2020 ). Graduate student mental health: Lessons from American economics departments . Working Paper. Cambridge, MA: Harvard University. https://scholar.harvard.edu/bolotnyy/publications/graduate-student-mental-health-lessons-american-economics-departments Google Scholar
- Busch, F. N., Rudden, M., & Shapiro, T. ( 2016 ). Psychodynamic treatment of depression . Washington, DC: American Psychiatric Publishing. Google Scholar
- Carlone, H. B., & Johnson, A. ( 2007 ). Understanding the science experiences of successful women of color: Science identity as an analytic lens . Journal of Research in Science Teaching , 44 (8), 1187–1218. Google Scholar
- Carvalho, J., Trent, L. R., & Hopko, D. R. ( 2011 ). The impact of decreased environmental reward in predicting depression severity: Support for behavioral theories of depression . Psychopathology , 44 (4), 242–252. Medline , Google Scholar
- Charmaz, K. ( 2006 ). Constructing grounded theory: A practical guide through qualitative research . Thousand Oaks, CA: Sage. Google Scholar
- Chávez, K., & Mitchell, K. M. ( 2020 ). Exploring bias in student evaluations: Gender, race, and ethnicity . PS: Political Science & Politics , 53 (2), 270–274. Google Scholar
- Chirikov, I., Soria, K. M., Horgos, B., & Jones-White, D. ( 2020 ). Undergraduate and graduate students’ mental health during the COVID-19 pandemic . Oakland, CA: California Digital Library, University of California. Google Scholar
- Clance, P. R., & Imes, S. A. ( 1978 ). The imposter phenomenon in high achieving women: Dynamics and therapeutic intervention . Psychotherapy: Theory, Research & Practice , 15 (3), 241. Google Scholar
- Cohen, E. D., & McConnell, W. R. ( 2019 ). Fear of fraudulence: Graduate school program environments and the impostor phenomenon . Sociological Quarterly , 60 (3), 457–478. Google Scholar
- Cooper, K. M., & Brownell, S. E. ( 2016 ). Coming out in class: Challenges and benefits of active learning in a biology classroom for LGBTQIA students . CBE—Life Sciences Education , 15 (3), ar37. Link , Google Scholar
- Cooper, K. M., Gin, L. E., Barnes, M. E., & Brownell, S. E. ( 2020a ). An exploratory study of students with depression in undergraduate research experiences . CBE—Life Sciences Education , 19 (2), ar19. Link , Google Scholar
- Cooper, K. M., Gin, L. E., & Brownell, S. E. ( 2020b ). Depression as a concealable stigmatized identity: What influences whether students conceal or reveal their depression in undergraduate research experiences? International Journal of STEM Education , 7 , 1–18. Google Scholar
- d’Apollonia, S., & Abrami, P. C. ( 1997 ). Navigating student ratings of instruction . American Psychologist , 52 (11), 1198. Google Scholar
- Depression and Bipolar Support Alliance . ( 2019 ). Retrieved March 15, 2021, from http://dbsalliance.org Google Scholar
- Detweiler-Bedell, J. B., & Whisman, M. A. ( 2005 ). A lesson in assigning homework: Therapist, client, and task characteristics in cognitive therapy for depression . Professional Psychology: Research and Practice , 36 (2), 219. Google Scholar
- Dey, S., Newell, B. R., & Moulds, M. L. ( 2018 ). The relative effects of abstract versus concrete thinking on decision-making in depression . Behaviour Research and Therapy , 110 , 11–21. Medline , Google Scholar
- Dickson, J. M., & Moberly, N. J. ( 2013 ). Reduced specificity of personal goals and explanations for goal attainment in major depression . PLoS ONE , 8 (5), e64512. Medline , Google Scholar
- Downing, V. R., Cooper, K. M., Cala, J. M., Gin, L. E., & Brownell, S. E. ( 2020 ). Fear of negative evaluation and student anxiety in community college active-learning science courses . CBE—Life Sciences Education , 19 (2), ar20. Link , Google Scholar
- Elliott, R. ( 1998 ). The neuropsychological profile in unipolar depression . Trends in Cognitive Sciences , 2 (11), 447–454. Medline , Google Scholar
- Evans, T. M., Bira, L., Gastelum, J. B., Weiss, L. T., & Vanderford, N. L. ( 2018 ). Evidence for a mental health crisis in graduate education . Nature Biotechnology , 36 (3), 282. Medline , Google Scholar
- Fan, Y., Shepherd, L. J., Slavich, E., Waters, D., Stone, M., Abel, R., & Johnston, E. L. ( 2019 ). Gender and cultural bias in student evaluations: Why representation matters . PLoS ONE , 14 (2), e0209749. Medline , Google Scholar
- Flaherty, C. ( 2018 ). New study says graduate students’ mental health is a “crisis.” Inside Higher Ed . Retrieved March 15, 2021, from www.insidehighered.com/news/2018/03/06/new-study-says-graduate-students-mental-health-crisis Google Scholar
- Gin, L. E., Guerrero, F. A., Brownell, S. E., & Cooper, K. M. ( 2021 ). COVID-19 and undergraduates with disabilities: Challenges resulting from the rapid transition to online course delivery for students with disabilities in undergraduate STEM at large-enrollment institutions . CBE—Life Sciences Education , 20 (3), ar36. Link , Google Scholar
- Glesne, C., & Peshkin, A. ( 1992 ). Becoming qualitative researchers: An introduction . London, UK: Longman. Google Scholar
- Gormally, C., Evans, M., & Brickman, P. ( 2014 ). Feedback about teaching in higher ed: Neglected opportunities to promote change . CBE—Life Sciences Education , 13 (2), 187–199. Link , Google Scholar
- Gotlib, I. H., & Krasnoperova, E. ( 1998 ). Biased information processing as a vulnerability factor for depression . Behavior Therapy , 29 (4), 603–617. Google Scholar
- Grahek, I., Shenhav, A., Musslick, S., Krebs, R. M., & Koster, E. H. ( 2019 ). Motivation and cognitive control in depression . Neuroscience & Biobehavioral Reviews , 102 , 371–381. Medline , Google Scholar
- Helmers, K. F., Danoff, D., Steinert, Y., Leyton, M., & Young, S. N. ( 1997 ). Stress and depressed mood in medical students, law students, and graduate students at McGill University . Academic Medicine , 72 (8), 708–714. Medline , Google Scholar
- Henry, M. A., Shorter, S., Charkoudian, L., Heemstra, J. M., & Corwin, L. A. ( 2019 ). FAIL is not a four-letter word: A theoretical framework for exploring undergraduate students’ approaches to academic challenge and responses to failure in STEM learning environments . CBE—Life Sciences Education , 18 (1), ar11. Link , Google Scholar
- Hish, A. J., Nagy, G. A., Fang, C. M., Kelley, L., Nicchitta, C. V., Dzirasa, K., & Rosenthal, M. Z. ( 2019 ). Applying the stress process model to stress–burnout and stress–depression relationships in biomedical doctoral students: A cross-sectional pilot study . CBE—Life Sciences Education , 18 (4), ar51. Link , Google Scholar
- Howell, E., & McFeeters, J. ( 2008 ). Children’s mental health care: Differences by race/ethnicity in urban/rural areas . Journal of Health Care for the Poor and Underserved , 19 (1), 237–247. Medline , Google Scholar
- Judd, L. L., Paulus, M. J., Schettler, P. J., Akiskal, H. S., Endicott, J., Leon, A. C. , ... & Keller, M. B. ( 2000 ). Does incomplete recovery from first lifetime major depressive episode herald a chronic course of illness? American Journal of Psychiatry , 157 (9), 1501–1504. Medline , Google Scholar
- Kanter, J. W., Callaghan, G. M., Landes, S. J., Busch, A. M., & Brown, K. R. ( 2004 ). Behavior analytic conceptualization and treatment of depression: Traditional models and recent advances . Behavior Analyst Today , 5 (3), 255. Google Scholar
- Kataoka, S. H., Zhang, L., & Wells, K. B. ( 2002 ). Unmet need for mental health care among US children: Variation by ethnicity and insurance status . American Journal of Psychiatry , 159 (9), 1548–1555. Medline , Google Scholar
- Kember, D., Leung, D. Y., & Kwan, K. ( 2002 ). Does the use of student feedback questionnaires improve the overall quality of teaching? Assessment & Evaluation in Higher Education , 27 (5), 411–425. Google Scholar
- Landis, J. R., & Koch, G. G. ( 1977 ). “ An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers . Biometrics , 363–374. Medline , Google Scholar
- Leahy, R. ( 2002 ). Clinical advances in cognitive psychotherapy: Theory and application . New York, NY: Springer. Google Scholar
- Levecque, K., Anseel, F., De Beuckelaer, A., Van der Heyden, J., & Gisle, L. ( 2017 ). Work organization and mental health problems in PhD students . Research Policy , 46 (4), 868–879. Google Scholar
- Lewinsohn, P. M. ( 1974 ). The psychology of depression: Contemporary theory and research . Sydney, Australia: Halsted Press. Google Scholar
- Lipson, S. K., Lattie, E. G., & Eisenberg, D. ( 2019 ). Increased rates of mental health service utilization by US college students: 10-year population-level trends (2007–2017) . Psychiatric Services , 70 (1), 60–63. Medline , Google Scholar
- Liu, C., Wang, L., Qi, R., Wang, W., Jia, S., Shang, D. , ... & Yan, S. ( 2019 ). Prevalence and associated factors of depression and anxiety among doctoral students: The mediating effect of mentoring relationships on the association between research self-efficacy and depression/anxiety . Psychology Research and Behavior Management , 12 , 195. Medline , Google Scholar
- Maj, M., Stein, D. J., Parker, G., Zimmerman, M., Fava, G. A., De Hert, M. , ... & Wittchen, H.-U. ( 2020 ). The clinical characterization of the adult patient with depression aimed at personalization of management . World Psychiatry , 19 (3), 269–293. Medline , Google Scholar
- Manos, R. C., Kanter, J. W., & Busch, A. M. ( 2010 ). A critical review of assessment strategies to measure the behavioral activation model of depression . Clinical Psychology Review , 30 (5), 547–561. Medline , Google Scholar
- Martell, C. R., Addis, M. E., & Jacobson, N. S. ( 2001 ). Depression in context: Strategies for guided action . New York: Norton. Google Scholar
- Maslach, C., Schaufeli, W. B., & Leiter, M. P. ( 2001 ). Job burnout . Annual Review of Psychology , 52 (1), 397–422. Medline , Google Scholar
- McGregor, L. N., Gee, D. E., & Posey, K. E. ( 2008 ). I feel like a fraud and it depresses me: The relation between the imposter phenomenon and depression . Social Behavior and Personality: An International Journal , 36 (1), 43–48. Google Scholar
- Mcleod, S. A. ( 2015 ). Psychological Theories of Depression . Simply Psychology , Retrieved March 15, 2021, from https://www.simplypsychology.org/depression.html Google Scholar
- Miranda, J., & Persons, J. B. ( 1988 ). Dysfunctional attitudes are mood-state dependent . Journal of Abnormal Psychology , 97 (1), 76. Medline , Google Scholar
- Pain, E. ( 2018 , March 6). Graduate students need more mental health support, study highlights . Science. Retrieved March 15, 2021, from www.sciencemag.org/careers/2018/03/graduate-students-need-more-mental-health-support-new-study-highlights Google Scholar
- Peluso, D. L., Carleton, R. N., & Asmundson, G. J. ( 2011 ). Depression symptoms in Canadian psychology graduate students: Do research productivity, funding, and the academic advisory relationship play a role? Canadian Journal of Behavioural Science/Revue Canadienne des Sciences du Comportement , 43 (2), 119. Google Scholar
- Pfeifer, M. A., Reiter, E. M., Cordero, J. J., & Stanton, J. D. ( 2021 ). Inside and out: Factors that support and hinder the self-advocacy of undergraduates with ADHD and/or specific learning disabilities in STEM . CBE—Life Sciences Education , 20 (2), ar17. Link , Google Scholar
- Puri, P. ( 2019 ). The emotional toll of graduate school . Scientific American Blog Network . Retrieved March 15, 2021, from https://blogs.scientificamerican.com/observations/the-emotional-toll-of-graduate-school/ Google Scholar
- Ramnerö, J., Folke, F., & Kanter, J. W. ( 2016 ). A learning theory account of depression . Scandinavian Journal of Psychology , 57 (1), 73–82. Medline , Google Scholar
- Saldaña, J. ( 2015 ). The coding manual for qualitative researchers . Thousand Oaks, CA: Sage. Google Scholar
- Santiago, C. D., Kaltman, S., & Miranda, J. ( 2013 ). Poverty and mental health: How do low-income adults and children fare in psychotherapy? Journal of Clinical Psychology , 69 (2), 115–126. Medline , Google Scholar
- Santini, Z. I., Koyanagi, A., Tyrovolas, S., Mason, C., & Haro, J. M. ( 2015 ). The association between social relationships and depression: A systematic review . Journal of Affective Disorders , 175 , 53–65. Medline , Google Scholar
- Schmidt, S. L., & Tolentino, J. C. ( 2018 ). DSM-5 criteria and depression severity: Implications for clinical practice . Frontiers in Psychiatry , 9 , 450. Medline , Google Scholar
- Schussler, E. E., Read, Q., Marbach-Ad, G., Miller, K., & Ferzli, M. ( 2015 ). Preparing biology graduate teaching assistants for their roles as instructors: An assessment of institutional approaches . CBE—Life Sciences Education , 14 (3), ar31. Link , Google Scholar
- Shortlidge, E. E., & Eddy, S. L. ( 2018 ). The trade-off between graduate student research and teaching: A myth? PLoS ONE , 13 (6), e0199576. Medline , Google Scholar
- Simpson, A., & Maltese, A. ( 2017 ). “ Failure is a major component of learning anything”: The role of failure in the development of STEM professionals . Journal of Science Education and Technology , 26 (2), 223–237. Google Scholar
- Tanner, K., & Allen, D. ( 2006 ). Approaches to biology teaching and learning: On integrating pedagogical training into the graduate experiences of future science faculty . CBE—Life Sciences Education , 5 (1), 1–6. Link , Google Scholar
- Text Depression Hotline . ( 2019 ). Crisis text line . Retrieved March 15, 2021, from www.crisistextline.org/depression Google Scholar
- Torvi, D. A. ( 1994 ). Engineering graduate teaching assistant instructional programs: Training tomorrow’s faculty members . Journal of Engineering Education , 83 (4), 376–382. Google Scholar
- Trenor, J. M., Miller, M. K., & Gipson, K. G. ( 2011 ). Utilization of a think-aloud protocol to cognitively validate a survey instrument identifying social capital resources of engineering undergraduates . Vancouver, BC: American Society for Engineering Education. Google Scholar
- U.S. News & World Report: News, Rankings and Analysis on Politics, Education, Healthcare and More . ( 2019 ). Retrieved October 1, 2019, from https://www.usnews.com/best-graduate-schools/top-science-schools/biological-sciences-rankings Google Scholar
- Watkins, E., & Brown, R. G. ( 2002 ). Rumination and executive function in depression: An experimental study . Journal of Neurology, Neurosurgery & Psychiatry , 72 (3), 400–402. Medline , Google Scholar
- Weissman, A. ( 1979 ). Dysfunctional Attitude Scale (DAS) . Acceptance and Commitment Therapy. Measures Package , 54–56. http://www.integrativehealthpartners.org/downloads/ Google Scholar
- Woolston, C. ( 2017 ). Graduate survey: A love–hurt relationship . Nature , 550 (7677), 549–552. Google Scholar
- Tasneem F. Mohammed ,
- Rahmi Q. Aini ,
- M. Elizabeth Barnes , and
- Stephanie Gardner, Monitoring Editor
- Carly A. Busch ,
- Tala Araghi ,
- Jingyi He ,
- Katelyn M. Cooper , and
- Sara E. Brownell
- Colin Harrison, Monitoring Editor
- Carly A. Busch , and
- Derek Braun, Monitoring Editor
- Erika M. Nadile ,
- Madison L. Witt ,
- Cindy Vargas ,
- Missy Tran ,
- Joseph Gazing Wolf ,
- Danielle Brister , and
- Sehoya Cotner, Monitoring Editor
- Katelyn M. Cooper ,
- Sarah L. Eddy , and
- Logan E. Gin ,
- Nicholas J. Wiesenthal , and
- Brian Sato, Monitoring Editor
- Reforming Graduate Student Policies and Resources Starts with Promoting the Ones you Already Have 16 May 2022 | Journal of Science Policy & Governance, Vol. 20, No. 02
- Miranda M. Chen Musgrove ,
- Alyssa Cooley ,
- Olivia Feiten ,
- Kate Petrie , and
- Elisabeth E. Schussler
- Erika Offerdahl, Monitoring Editor
- Danielle Brister ,
- Sara E. Brownell ,
- Chade T. Claiborne ,
- Baylee A. Edwards ,
- Curtis Lunt ,
- Kobe M. Walker ,
- Tamiru D. Warkina ,
- Yi Zheng , and
- Rebecca Price, Monitoring Editor

Submitted: 29 March 2021 Revised: 7 May 2021 Accepted: 14 May 2021
© 2021 L. E. Gin, N. J. Wiesenthal, et al. CBE—Life Sciences Education © 2021 The American Society for Cell Biology. This article is distributed by The American Society for Cell Biology under license from the author(s). It is available to the public under an Attribution–Noncommercial–Share Alike 3.0 Unported Creative Commons License (http://creativecommons.org/licenses/by-nc-sa/3.0).
- A){G=Math.round((C/2)-(A/2))}window.twttr.shareWin=window.open('//twitter.com/share?text=University of Pittsburgh School of Medicine Promotes Nadine Melhem, PhD, to Professor of Psychiatry&hashtags=PittPsychiatry&url=','','left='+H+',top='+G+',width='+D+',height='+A+',personalbar=0,toolbar=0,scrollbars=1,resizable=1');E=F.createElement('script');E.src='//platform.twitter.com/widgets.js';F.getElementsByTagName('head')[0].appendChild(E)}());"> Share on Twitter
- Share on Facebook
- Share via email
University of Pittsburgh School of Medicine Promotes Nadine Melhem, PhD, to Professor of Psychiatry

We are pleased to announce that Nadine Melhem, PhD , has been promoted to Professor of Psychiatry by the University of Pittsburgh School of Medicine.
Dr. Melhem earned her PhD in psychiatric epidemiology from the University of Pittsburgh School of Public Health. She has dedicated her research career to improving our understanding of the risk for psychiatric disorders in children who have experienced trauma or prolonged grief, the familial and genetic contributors to suicide risk, and the contribution of alterations in the hypothalamic-pituitary adrenal axis to suicide risk. She brings new methods to examination of suicidal behavior in youth, including studies of hypothalamic-pituitary adrenal axis dysregulation, neuroinflammation, and of neural mitochondrial function. Her novel findings include showing that suicide attempters had a blunted hypothalamic-pituitary adrenal axis response to stress compared to other high-risk subjects.
Dr. Melhem is principal investigator (PI) or multiple PI on five National Institute of Mental Health (NIMH) R01 grants focused on stress response/suicidality in youth. In addition, she is MPI for the signature R01 of the NIMH Enhancing Triage and Utilization for Depression and Emergent Suicidality (ETUDES) Center of Excellence P50, as well as co-investigator (co-I) on the ETUDES administrative core. Her history of early-career funding includes leading a K01, three R-level grants from the NIMH, a NARSAD Young Investigator Award, and a NARSAD Independent Investigator Award.
Dr. Melhem has disseminated her research through original, peer-reviewed articles in top scientific journals, as well as through presentations at annual meetings in the US and abroad. She has been invited to present her research at the NIMH, the Society of Biological Psychiatry annual meeting, and the Icahn School of Medicine at Mount Sinai, as well as at the American University of Beirut, the International Academy of Suicide Research, and the World Psychiatric Association’s Epidemiology and Public Health Section.
A highly respected scientist with an excellent national and international reputation, Dr. Melhem is a member of the National Institutes of Health Center for Scientific Review’s Child Psychopathology and Developmental Disabilities study section, and serves on the American Foundation for Suicide Prevention Research Grants Committee. She has served on invited review panels for organizations and institutions including the NIMH, Department of Defense Congressionally Directed Medical Research Programs, and the US Army Medical Research and Materiel Command.
As a teacher, Dr. Melhem has made tremendous contributions to the educational mission of the Department of Psychiatry, as well as to schools and departments across the University of Pittsburgh. She has taught School of Public Health master’s and doctoral students on the epidemiology of mental disorders and served as a facilitator for medical students enrolled in Introduction to Psychiatry. She has additionally taught numerous psychiatry residents and postdoctoral scholars. Dr. Melhem is a highly sought after mentor, having worked with medical students, postdoctoral scholars, and early-career faculty. On the national level, she is currently a mentor with the American College of Neuropsychopharmacology.
“Dr. Melhem has a tremendous track record of innovative and influential research. She has employed novel methods in the examination of suicidal behavior in youth, which have yielded critical findings that impact clinical practice,” said David Lewis, MD (Chair, Department of Psychiatry). “She is an outstanding member of the scientific community, as well as an active, engaged, and highly effective teacher and mentor.”
Please join us in congratulating Dr. Melhem!
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 13 July 2021
Systematic review and meta-analysis of depression, anxiety, and suicidal ideation among Ph.D. students
- Emily N. Satinsky 1 ,
- Tomoki Kimura 2 ,
- Mathew V. Kiang 3 , 4 ,
- Rediet Abebe 5 , 6 ,
- Scott Cunningham 7 ,
- Hedwig Lee 8 ,
- Xiaofei Lin 9 ,
- Cindy H. Liu 10 , 11 ,
- Igor Rudan 12 ,
- Srijan Sen 13 ,
- Mark Tomlinson 14 , 15 ,
- Miranda Yaver 16 &
- Alexander C. Tsai 1 , 11 , 17
Scientific Reports volume 11 , Article number: 14370 ( 2021 ) Cite this article
90k Accesses
79 Citations
816 Altmetric
Metrics details
- Epidemiology
- Health policy
- Quality of life
University administrators and mental health clinicians have raised concerns about depression and anxiety among Ph.D. students, yet no study has systematically synthesized the available evidence in this area. After searching the literature for studies reporting on depression, anxiety, and/or suicidal ideation among Ph.D. students, we included 32 articles. Among 16 studies reporting the prevalence of clinically significant symptoms of depression across 23,469 Ph.D. students, the pooled estimate of the proportion of students with depression was 0.24 (95% confidence interval [CI], 0.18–0.31; I 2 = 98.75%). In a meta-analysis of the nine studies reporting the prevalence of clinically significant symptoms of anxiety across 15,626 students, the estimated proportion of students with anxiety was 0.17 (95% CI, 0.12–0.23; I 2 = 98.05%). We conclude that depression and anxiety are highly prevalent among Ph.D. students. Data limitations precluded our ability to obtain a pooled estimate of suicidal ideation prevalence. Programs that systematically monitor and promote the mental health of Ph.D. students are urgently needed.
Similar content being viewed by others

Prevalence of depression among Chinese university students: a systematic review and meta-analysis
A repeated cross-sectional analysis assessing mental health conditions of adults as per student status during key periods of the COVID-19 epidemic in France
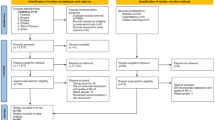
Relationship between depression and quality of life among students: a systematic review and meta-analysis
Introduction.
Mental health problems among graduate students in doctoral degree programs have received increasing attention 1 , 2 , 3 , 4 . Ph.D. students (and students completing equivalent degrees, such as the Sc.D.) face training periods of unpredictable duration, financial insecurity and food insecurity, competitive markets for tenure-track positions, and unsparing publishing and funding models 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 —all of which may have greater adverse impacts on students from marginalized and underrepresented populations 13 , 14 , 15 . Ph.D. students’ mental health problems may negatively affect their physical health 16 , interpersonal relationships 17 , academic output, and work performance 18 , 19 , and may also contribute to program attrition 20 , 21 , 22 . As many as 30 to 50% of Ph.D. students drop out of their programs, depending on the country and discipline 23 , 24 , 25 , 26 , 27 . Further, while mental health problems among Ph.D. students raise concerns for the wellbeing of the individuals themselves and their personal networks, they also have broader repercussions for their institutions and academia as a whole 22 .
Despite the potential public health significance of this problem, most evidence syntheses on student mental health have focused on undergraduate students 28 , 29 or graduate students in professional degree programs (e.g., medical students) 30 . In non-systematic summaries, estimates of the prevalence of clinically significant depressive symptoms among Ph.D. students vary considerably 31 , 32 , 33 . Reliable estimates of depression and other mental health problems among Ph.D. students are needed to inform preventive, screening, or treatment efforts. To address this gap in the literature, we conducted a systematic review and meta-analysis to explore patterns of depression, anxiety, and suicidal ideation among Ph.D. students.
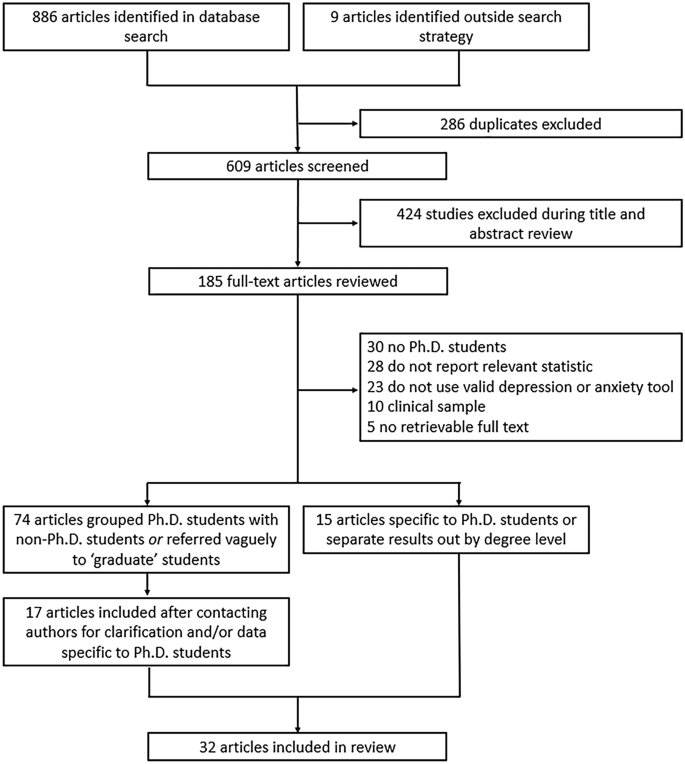
Flowchart of included articles.
The evidence search yielded 886 articles, of which 286 were excluded as duplicates (Fig. 1 ). An additional nine articles were identified through reference lists or grey literature reports published on university websites. Following a title/abstract review and subsequent full-text review, 520 additional articles were excluded.
Of the 89 remaining articles, 74 were unclear about their definition of graduate students or grouped Ph.D. and non-Ph.D. students without disaggregating the estimates by degree level. We obtained contact information for the authors of most of these articles (69 [93%]), requesting additional data. Three authors clarified that their study samples only included Ph.D. students 34 , 35 , 36 . Fourteen authors confirmed that their study samples included both Ph.D. and non-Ph.D. students but provided us with data on the subsample of Ph.D. students 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 . Where authors clarified that the sample was limited to graduate students in non-doctoral degree programs, did not provide additional data on the subsample of Ph.D. students, or did not reply to our information requests, we excluded the studies due to insufficient information (Supplementary Table S1 ).
Ultimately, 32 articles describing the findings of 29 unique studies were identified and included in the review 16 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 (Table 1 ). Overall, 26 studies measured depression, 19 studies measured anxiety, and six studies measured suicidal ideation. Three pairs of articles reported data on the same sample of Ph.D. students 33 , 38 , 45 , 51 , 53 , 56 and were therefore grouped in Table 1 and reported as three studies. Publication dates ranged from 1979 to 2019, but most articles (22/32 [69%]) were published after 2015. Most studies were conducted in the United States (20/29 [69%]), with additional studies conducted in Australia, Belgium, China, Iran, Mexico, and South Korea. Two studies were conducted in cross-national settings representing 48 additional countries. None were conducted in sub-Saharan Africa or South America. Most studies included students completing their degrees in a mix of disciplines (17/29 [59%]), while 12 studies were limited to students in a specific field (e.g., biomedicine, education). The median sample size was 172 students (interquartile range [IQR], 68–654; range, 6–6405). Seven studies focused on mental health outcomes in demographic subgroups, including ethnic or racialized minority students 37 , 41 , 43 , international students 47 , 50 , and sexual and gender minority students 42 , 54 .
In all, 16 studies reported the prevalence of depression among a total of 23,469 Ph.D. students (Fig. 2 ; range, 10–47%). Of these, the most widely used depression scales were the PHQ-9 (9 studies) and variants of the Center for Epidemiologic Studies-Depression scale (CES-D, 4 studies) 63 , and all studies assessed clinically significant symptoms of depression over the past one to two weeks. Three of these studies reported findings based on data from different survey years of the same parent study (the Healthy Minds Study) 40 , 42 , 43 , but due to overlap in the survey years reported across articles, these data were pooled. Most of these studies were based on data collected through online surveys (13/16 [81%]). Ten studies (63%) used random or systematic sampling, four studies (25%) used convenience sampling, and two studies (13%) used multiple sampling techniques.
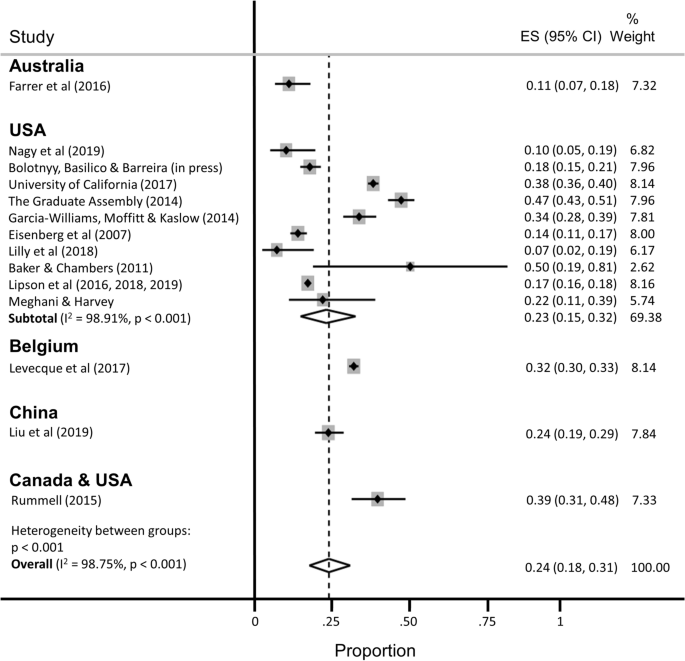
Pooled estimate of the proportion of Ph.D. students with clinically significant symptoms of depression.
The estimated proportion of Ph.D. students assessed as having clinically significant symptoms of depression was 0.24 (95% confidence interval [CI], 0.18–0.31; 95% predictive interval [PI], 0.04–0.54), with significant evidence of between-study heterogeneity (I 2 = 98.75%). A subgroup analysis restricted to the twelve studies conducted in the United States yielded similar findings (pooled estimate [ES] = 0.23; 95% CI, 0.15–0.32; 95% PI, 0.01–0.60), with no appreciable difference in heterogeneity (I 2 = 98.91%). A subgroup analysis restricted to the studies that used the PHQ-9 to assess depression yielded a slightly lower prevalence estimate and a slight reduction in heterogeneity (ES = 0.18; 95% CI, 0.14–0.22; 95% PI, 0.07–0.34; I 2 = 90.59%).
Nine studies reported the prevalence of clinically significant symptoms of anxiety among a total of 15,626 Ph.D. students (Fig. 3 ; range 4–49%). Of these, the most widely used anxiety scale was the 7-item Generalized Anxiety Disorder scale (GAD-7, 5 studies) 64 . Data from three of the Healthy Minds Study articles were pooled into two estimates, because the scale used to measure anxiety changed midway through the parent study (i.e., the Patient Health Questionnaire-Generalized Anxiety Disorder [PHQ-GAD] scale was used from 2007 to 2012 and then switched to the GAD-7 in 2013 40 ). Most studies (8/9 [89%]) assessed clinically significant symptoms of anxiety over the past two to four weeks, with the one remaining study measuring anxiety over the past year. Again, most of these studies were based on data collected through online surveys (7/9 [78%]). Five studies (56%) used random or systematic sampling, two studies (22%) used convenience sampling, and two studies (22%) used multiple sampling techniques.
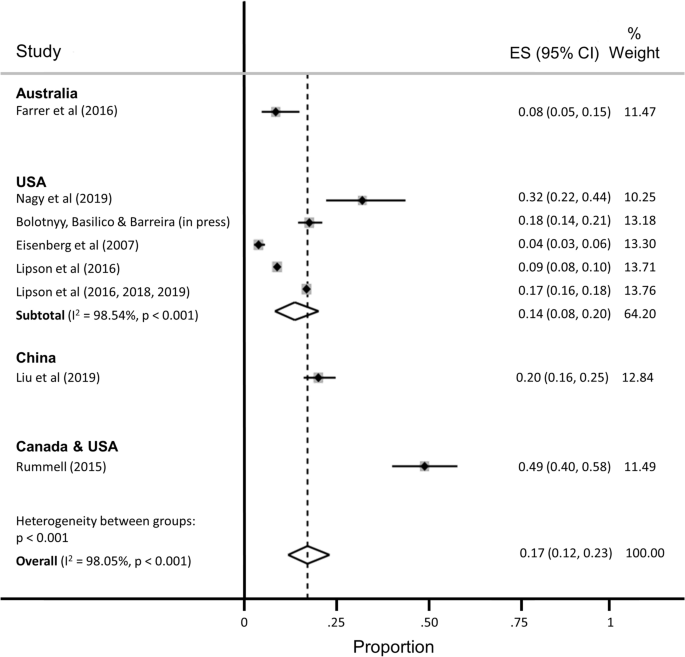
Pooled estimate of the proportion of Ph.D. students with clinically significant symptoms of anxiety.
The estimated proportion of Ph.D. students assessed as having anxiety was 0.17 (95% CI, 0.12–0.23; 95% PI, 0.02–0.41), with significant evidence of between-study heterogeneity (I 2 = 98.05%). The subgroup analysis restricted to the five studies conducted in the United States yielded a slightly lower proportion of students assessed as having anxiety (ES = 0.14; 95% CI, 0.08–0.20; 95% PI, 0.00–0.43), with no appreciable difference in heterogeneity (I 2 = 98.54%).
Six studies reported the prevalence of suicidal ideation (range, 2–12%), but the recall windows varied greatly (e.g., ideation within the past 2 weeks vs. past year), precluding pooled estimation.
Additional stratified pooled estimates could not be obtained. One study of Ph.D. students across 54 countries found that phase of study was a significant moderator of mental health, with students in the comprehensive examination and dissertation phases more likely to experience distress compared with students primarily engaged in coursework 59 . Other studies identified a higher prevalence of mental ill-health among women 54 ; lesbian, gay, bisexual, transgender, and queer (LGBTQ) students 42 , 54 , 60 ; and students with multiple intersecting identities 54 .
Several studies identified correlates of mental health problems including: project- and supervisor-related issues, stress about productivity, and self-doubt 53 , 62 ; uncertain career prospects, poor living conditions, financial stressors, lack of sleep, feeling devalued, social isolation, and advisor relationships 61 ; financial challenges 38 ; difficulties with work-life balance 58 ; and feelings of isolation and loneliness 52 . Despite these challenges, help-seeking appeared to be limited, with only about one-quarter of Ph.D. students reporting mental health problems also reporting that they were receiving treatment 40 , 52 .
Risk of bias
Twenty-one of 32 articles were assessed as having low risk of bias (Supplementary Table S2 ). Five articles received one point for all five categories on the risk of bias assessment (lowest risk of bias), and one article received no points (highest risk). The mean risk of bias score was 3.22 (standard deviation, 1.34; median, 4; IQR, 2–4). Restricting the estimation sample to 12 studies assessed as having low risk of bias, the estimated proportion of Ph.D. students with depression was 0.25 (95% CI, 0.18–0.33; 95% PI, 0.04–0.57; I 2 = 99.11%), nearly identical to the primary estimate, with no reduction in heterogeneity. The estimated proportion of Ph.D. students with anxiety, among the 7 studies assessed as having low risk of bias, was 0.12 (95% CI, 0.07–0.17; 95% PI, 0.01–0.34; I 2 = 98.17%), again with no appreciable reduction in heterogeneity.
In our meta-analysis of 16 studies representing 23,469 Ph.D. students, we estimated that the pooled prevalence of clinically significant symptoms of depression was 24%. This estimate is consistent with estimated prevalence rates in other high-stress biomedical trainee populations, including medical students (27%) 30 , resident physicians (29%) 65 , and postdoctoral research fellows (29%) 66 . In the sample of nine studies representing 15,626 Ph.D. students, we estimated that the pooled prevalence of clinically significant symptoms of anxiety was 17%. While validated screening instruments tend to over-identify cases of depression (relative to structured clinical interviews) by approximately a factor of two 67 , 68 , our findings nonetheless point to a major public health problem among Ph.D. students. Available data suggest that the prevalence of depressive and anxiety disorders in the general population ranges from 5 to 7% worldwide 69 , 70 . In contrast, prevalence estimates of major depressive disorder among young adults have ranged from 13% (for young adults between the ages of 18 and 29 years in the 2012–2013 National Epidemiologic Survey on Alcohol and Related Conditions III 71 ) to 15% (for young adults between the ages of 18 and 25 in the 2019 U.S. National Survey on Drug Use and Health 72 ). Likewise, the prevalence of generalized anxiety disorder was estimated at 4% among young adults between the ages of 18 and 29 in the 2001–03 U.S. National Comorbidity Survey Replication 73 . Thus, even accounting for potential upward bias inherent in these studies’ use of screening instruments, our estimates suggest that the rates of recent clinically significant symptoms of depression and anxiety are greater among Ph.D. students compared with young adults in the general population.
Further underscoring the importance of this public health issue, Ph.D. students face unique stressors and uncertainties that may put them at increased risk for mental health and substance use problems. Students grapple with competing responsibilities, including coursework, teaching, and research, while also managing interpersonal relationships, social isolation, caregiving, and financial insecurity 3 , 10 . Increasing enrollment in doctoral degree programs has not been matched with a commensurate increase in tenure-track academic job opportunities, intensifying competition and pressure to find employment post-graduation 5 . Advisor-student power relations rarely offer options for recourse if and when such relationships become strained, particularly in the setting of sexual harassment, unwanted sexual attention, sexual coercion, and rape 74 , 75 , 76 , 77 , 78 . All of these stressors may be magnified—and compounded by stressors unrelated to graduate school—for subgroups of students who are underrepresented in doctoral degree programs and among whom mental health problems are either more prevalent and/or undertreated compared with the general population, including Black, indigenous, and other people of color 13 , 79 , 80 ; women 81 , 82 ; first-generation students 14 , 15 ; people who identify as LGBTQ 83 , 84 , 85 ; people with disabilities; and people with multiple intersecting identities.
Structural- and individual-level interventions will be needed to reduce the burden of mental ill-health among Ph.D. students worldwide 31 , 86 . Despite the high prevalence of mental health and substance use problems 87 , Ph.D. students demonstrate low rates of help-seeking 40 , 52 , 88 . Common barriers to help-seeking include fears of harming one’s academic career, financial insecurity, lack of time, and lack of awareness 89 , 90 , 91 , as well as health care systems-related barriers, including insufficient numbers of culturally competent counseling staff, limited access to psychological services beyond time-limited psychotherapies, and lack of programs that address the specific needs either of Ph.D. students in general 92 or of Ph.D. students belonging to marginalized groups 93 , 94 . Structural interventions focused solely on enhancing student resilience might include programs aimed at reducing stigma, fostering social cohesion, and reducing social isolation, while changing norms around help-seeking behavior 95 , 96 . However, structural interventions focused on changing stressogenic aspects of the graduate student environment itself are also needed 97 , beyond any enhancements to Ph.D. student resilience, including: undercutting power differentials between graduate students and individual faculty advisors, e.g., by diffusing power among multiple faculty advisors; eliminating racist, sexist, and other discriminatory behaviors by faculty advisors 74 , 75 , 98 ; valuing mentorship and other aspects of “invisible work” that are often disproportionately borne by women faculty and faculty of color 99 , 100 ; and training faculty members to emphasize the dignity of, and adequately prepare Ph.D. students for, non-academic careers 101 , 102 .
Our findings should be interpreted with several limitations in mind. First, the pooled estimates are characterized by a high degree of heterogeneity, similar to meta-analyses of depression prevalence in other populations 30 , 65 , 103 , 104 , 105 . Second, we were only able to aggregate depression prevalence across 16 studies and anxiety prevalence across nine studies (the majority of which were conducted in the U.S.) – far fewer than the 183 studies included in a meta-analysis of depression prevalence among medical students 30 and the 54 studies included in a meta-analysis of resident physicians 65 . These differences underscore the need for more rigorous study in this critical area. Many articles were either excluded from the review or from the meta-analyses for not meeting inclusion criteria or not reporting relevant statistics. Future research in this area should ensure the systematic collection of high-quality, clinically relevant data from a comprehensive set of institutions, across disciplines and countries, and disaggregated by graduate student type. As part of conducting research and addressing student mental health and wellbeing, university deans, provosts, and chancellors should partner with national survey and program institutions (e.g., Graduate Student Experience in the Research University [gradSERU] 106 , the American College Health Association National College Health Assessment [ACHA-NCHA], and HealthyMinds). Furthermore, federal agencies that oversee health and higher education should provide resources for these efforts, and accreditation agencies should require monitoring of mental health and programmatic responses to stressors among Ph.D. students.
Third, heterogeneity in reporting precluded a meta-analysis of the suicidality outcomes among the few studies that reported such data. While reducing the burden of mental health problems among graduate students is an important public health aim in itself, more research into understanding non-suicidal self-injurious behavior, suicide attempts, and completed suicide among Ph.D. students is warranted. Fourth, it is possible that the grey literature reports included in our meta-analysis are more likely to be undertaken at research-intensive institutions 52 , 60 , 61 . However, the direction of bias is unpredictable: mental health problems among Ph.D. students in research-intensive environments may be more prevalent due to detection bias, but such institutions may also have more resources devoted to preventive, screening, or treatment efforts 92 . Fifth, inclusion in this meta-analysis and systematic review was limited to those based on community samples. Inclusion of clinic-based samples, or of studies conducted before or after specific milestones (e.g., the qualifying examination or dissertation prospectus defense), likely would have yielded even higher pooled prevalence estimates of mental health problems. And finally, few studies provided disaggregated data according to sociodemographic factors, stage of training (e.g., first year, pre-prospectus defense, all-but-dissertation), or discipline of study. These factors might be investigated further for differences in mental health outcomes.
Clinically significant symptoms of depression and anxiety are pervasive among graduate students in doctoral degree programs, but these are understudied relative to other trainee populations. Structural and clinical interventions to systematically monitor and promote the mental health and wellbeing of Ph.D. students are urgently needed.
This systematic review and meta-analysis follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) approach (Supplementary Table S3 ) 107 . This study was based on data collected from publicly available bibliometric databases and did not require ethical approval from our institutional review boards.
Eligibility criteria
Studies were included if they provided data on either: (a) the number or proportion of Ph.D. students with clinically significant symptoms of depression or anxiety, ascertained using a validated scale; or (b) the mean depression or anxiety symptom severity score and its standard deviation among Ph.D. students. Suicidal ideation was examined as a secondary outcome.
We excluded studies that focused on graduate students in non-doctoral degree programs (e.g., Master of Public Health) or professional degree programs (e.g., Doctor of Medicine, Juris Doctor) because more is known about mental health problems in these populations 30 , 108 , 109 , 110 and because Ph.D. students face unique uncertainties. To minimize the potential for upward bias in our pooled prevalence estimates, we excluded studies that recruited students from campus counseling centers or other clinic-based settings. Studies that measured affective states, or state anxiety, before or after specific events (e.g., terrorist attacks, qualifying examinations) were also excluded.
If articles described the study sample in general terms (i.e., without clarifying the degree level of the participants), we contacted the authors by email for clarification. Similarly, if articles pooled results across graduate students in doctoral and non-doctoral degree programs (e.g., reporting a single estimate for a mixed sample of graduate students), we contacted the authors by email to request disaggregated data on the subsample of Ph.D. students. If authors did not reply after two contact attempts spaced over 2 months, or were unable to provide these data, we excluded these studies from further consideration.
Search strategy and data extraction
PubMed, Embase, PsycINFO, ERIC, and Business Source Complete were searched from inception of each database to November 5, 2019. The search strategy included terms related to mental health symptoms (e.g., depression, anxiety, suicide), the study population (e.g., graduate, doctoral), and measurement category (e.g., depression, Columbia-Suicide Severity Rating Scale) (Supplementary Table S4 ). In addition, we searched the reference lists and the grey literature.
After duplicates were removed, we screened the remaining titles and abstracts, followed by a full-text review. We excluded articles following the eligibility criteria listed above (i.e., those that were not focused on Ph.D. students; those that did not assess depression and/or anxiety using a validated screening tool; those that did not report relevant statistics of depression and/or anxiety; and those that recruited students from clinic-based settings). Reasons for exclusion were tracked at each stage. Following selection of included articles, two members of the research team extracted data and conducted risk of bias assessments. Discrepancies were discussed with a third member of the research team. Key extraction variables included: study design, geographic region, sample size, response rate, demographic characteristics of the sample, screening instrument(s) used for assessment, mean depression or anxiety symptom severity score (and its standard deviation), and the number (or proportion) of students experiencing clinically significant symptoms of depression or anxiety.
Risk of bias assessment
Following prior work 30 , 65 , the Newcastle–Ottawa Scale 111 was adapted and used to assess risk of bias in the included studies. Each study was assessed across 5 categories: sample representativeness, sample size, non-respondents, ascertainment of outcomes, and quality of descriptive statistics reporting (Supplementary Information S5 ). Studies were judged as having either low risk of bias (≥ 3 points) or high risk of bias (< 3 points).
Analysis and synthesis
Before pooling the estimated prevalence rates across studies, we first transformed the proportions using a variance-stabilizing double arcsine transformation 112 . We then computed pooled estimates of prevalence using a random effects model 113 . Study specific confidence intervals were estimated using the score method 114 , 115 . We estimated between-study heterogeneity using the I 2 statistic 116 . In an attempt to reduce the extent of heterogeneity, we re-estimated pooled prevalence restricting the analysis to studies conducted in the United States and to studies in which depression assessment was based on the 9-item Patient Health Questionnaire (PHQ-9) 117 . All analyses were conducted using Stata (version 16; StataCorp LP, College Station, Tex.). Where heterogeneity limited our ability to summarize the findings using meta-analysis, we synthesized the data using narrative review.
Woolston, C. Why mental health matters. Nature 557 , 129–131 (2018).
Article ADS CAS Google Scholar
Woolston, C. A love-hurt relationship. Nature 550 , 549–552 (2017).
Article Google Scholar
Woolston, C. PhD poll reveals fear and joy, contentment and anguish. Nature 575 , 403–406 (2019).
Article ADS CAS PubMed Google Scholar
Byrom, N. COVID-19 and the research community: The challenges of lockdown for early-career researchers. Elife 9 , e59634 (2020).
Article PubMed PubMed Central Google Scholar
Alberts, B., Kirschner, M. W., Tilghman, S. & Varmus, H. Rescuing US biomedical research from its systemic flaws. Proc. Natl. Acad. Sci. USA 111 , 5773–5777 (2014).
Article ADS CAS PubMed PubMed Central Google Scholar
McDowell, G. S. et al. Shaping the future of research: A perspective from junior scientists. F1000Res 3 , 291 (2014).
Article PubMed Google Scholar
Petersen, A. M., Riccaboni, M., Stanley, H. E. & Pammoli, F. Persistence and uncertainty in the academic career. Proc. Natl. Acad. Sci. USA 109 , 5213–5218 (2012).
Leshner, A. I. Rethinking graduate education. Science 349 , 349 (2015).
National Academies of Sciences Engineering and Medicine. Graduate STEM Education for the 21st Century (National Academies Press, 2018).
Google Scholar
Charles, S. T., Karnaze, M. M. & Leslie, F. M. Positive factors related to graduate student mental health. J. Am. Coll. Health https://doi.org/10.1080/07448481.2020.1841207 (2021).
Riddle, E. S., Niles, M. T. & Nickerson, A. Prevalence and factors associated with food insecurity across an entire campus population. PLoS ONE 15 , e0237637 (2020).
Article CAS PubMed PubMed Central Google Scholar
Soldavini, J., Berner, M. & Da Silva, J. Rates of and characteristics associated with food insecurity differ among undergraduate and graduate students at a large public university in the Southeast United States. Prev. Med. Rep. 14 , 100836 (2019).
Clark, U. S. & Hurd, Y. L. Addressing racism and disparities in the biomedical sciences. Nat. Hum. Behav. 4 , 774–777 (2020).
Gardner, S. K. The challenges of first-generation doctoral students. New Dir. High. Educ. 2013 , 43–54 (2013).
Seay, S. E., Lifton, D. E., Wuensch, K. L., Bradshaw, L. K. & McDowelle, J. O. First-generation graduate students and attrition risks. J. Contin. High. Educ. 56 , 11–25 (2008).
Rummell, C. M. An exploratory study of psychology graduate student workload, health, and program satisfaction. Prof. Psychol. Res. Pract. 46 , 391–399 (2015).
Salzer, M. S. A comparative study of campus experiences of college students with mental illnesses versus a general college sample. J. Am. Coll. Health 60 , 1–7 (2012).
Hysenbegasi, A., Hass, S. & Rowland, C. The impact of depression on the academic productivity of university students. J. Ment. Health Policy Econ. 8 , 145–151 (2005).
PubMed Google Scholar
Harvey, S. et al. Depression and work performance: An ecological study using web-based screening. Occup. Med. (Lond.) 61 , 209–211 (2011).
Article CAS Google Scholar
Eisenberg, D., Golberstein, E. & Hunt, J. B. Mental health and academic success in college. BE J. Econ. Anal. Policy 9 , 40 (2009).
Lovitts, B. E. Who is responsible for graduate student attrition--the individual or the institution? Toward an explanation of the high and persistent rate of attrition. In: Annual Meeting of the American Education Research Association (New York, 1996). Available at: https://eric.ed.gov/?id=ED399878.
Gardner, S. K. Student and faculty attributions of attrition in high and low-completing doctoral programs in the United States. High. Educ. 58 , 97–112 (2009).
Lovitts, B. E. Leaving the Ivory Tower: The Causes and Consequences of Departure from Doctoral Study (Rowman & Littlefield Publishers, 2001).
Rigler Jr, K. L., Bowlin, L. K., Sweat, K., Watts, S. & Throne, R. Agency, socialization, and support: a critical review of doctoral student attrition. In: Proceedings of the Third International Conference on Doctoral Education: Organizational Leadership and Impact , University of Central Florida, Orlando, (2017).
Golde, C. M. The role of the department and discipline in doctoral student attrition: Lessons from four departments. J. High. Educ. 76 , 669–700 (2005).
Council of Graduate Schools. PhD Completion and Attrition: Analysis of Baseline Program Data from the PhD Completion Project (Council of Graduate Schools, 2008).
National Research Council. A Data-Based Assessment of Research-Doctorate Programs in the United States (The National Academies Press, 2011).
Akhtar, P. et al. Prevalence of depression among university students in low and middle income countries (LMICs): A systematic review and meta-analysis. J. Affect. Disord. 274 , 911–919 (2020).
Mortier, P. et al. The prevalence of suicidal thoughts and behaviours among college students: A meta-analysis. Psychol. Med. 48 , 554–565 (2018).
Article CAS PubMed Google Scholar
Rotenstein, L. S. et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: A systematic review and meta-analysis. JAMA 316 , 2214–2236 (2016).
Tsai, J. W. & Muindi, F. Towards sustaining a culture of mental health and wellness for trainees in the biosciences. Nat. Biotechnol. 34 , 353–355 (2016).
Levecque, K., Anseel, F., De Beuckelaer, A., Van der Heyden, J. & Gisle, L. Work organization and mental health problems in PhD students. Res. Policy 46 , 868–879 (2017).
Nagy, G. A. et al. Burnout and mental health problems in biomedical doctoral students. CBE Life Sci. Educ. 18 , 1–14 (2019).
Garcia-Williams, A., Moffitt, L. & Kaslow, N. J. Mental health and suicidal behavior among graduate students. Acad. Psychiatry 28 , 554–560 (2014).
Sheldon, K. M. Emotionality differences between artists and scientists. J. Res. Pers. 28 , 481–491 (1994).
Lightstone, S. N., Swencionis, C. & Cohen, H. W. The effect of bioterrorism messages on anxiety levels. Int. Q. Community Health Educ. 24 , 111–122 (2006).
Clark, C. R., Mercer, S. H., Zeigler-Hill, V. & Dufrene, B. A. Barriers to the success of ethnic minority students in school psychology graduate programs. School Psych. Rev. 41 , 176–192 (2012).
Eisenberg, D., Gollust, S. E., Golberstein, E. & Hefner, J. L. Prevalence and correlates of depression, anxiety, and suicidality among university students. Am. J. Orthopsychiatry 77 , 534–542 (2007).
Farrer, L. M., Gulliver, A., Bennett, K., Fassnacht, D. B. & Griffiths, K. M. Demographic and psychosocial predictors of major depression and generalised anxiety disorder in Australian university students. BMC Psychiatry 16 , 241 (2016).
Lipson, S. K., Zhou, S., Wagner, B. III., Beck, K. & Eisenberg, D. Major differences: Variations in undergraduate and graduate student mental health and treatment utilization across academic disciplines. J. Coll. Stud. Psychother. 30 , 23–41 (2016).
Lilly, F. R. W. et al. The influence of racial microaggressions and social rank on risk for depression among minority graduate and professional students. Coll. Stud. J. 52 , 86–104 (2018).
Lipson, S. K., Raifman, J., Abelson, S. & Reisner, S. L. Gender minority mental health in the U.S.: Results of a national survey on college campuses. Am. J. Prev. Med. 57 , 293–301 (2019).
Lipson, S. K., Kern, A., Eisenberg, D. & Breland-Noble, A. M. Mental health disparities among college students of color. J. Adolesc. Health 63 , 348–356 (2018).
Baker, A. J. L. & Chambers, J. Adult recall of childhood exposure to parental conflict: Unpacking the black box of parental alienation. J. Divorce Remarriage 52 , 55–76 (2011).
Golberstein, E., Eisenberg, D. & Gollust, S. E. Perceived stigma and mental health care seeking. Psychiatr. Serv. 59 , 392–399 (2008).
Hindman, R. K., Glass, C. R., Arnkoff, D. B. & Maron, D. D. A comparison of formal and informal mindfulness programs for stress reduction in university students. Mindfulness 6 , 873–884 (2015).
Hirai, R., Frazier, P. & Syed, M. Psychological and sociocultural adjustment of first-year international students: Trajectories and predictors. J. Couns. Psychol. 62 , 438–452 (2015).
Lee, J. S. & Jeong, B. Having mentors and campus social networks moderates the impact of worries and video gaming on depressive symptoms: A moderated mediation analysis. BMC Public Health 14 , 1–12 (2014).
Corral-Frias, N. S., Velardez Soto, S. N., Frias-Armenta, M., Corona-Espinosa, A. & Watson, D. Concurrent validity and reliability of two short forms of the mood and anxiety symptom questionnaire in a student sample from Northwest Mexico. J. Psychopathol. Behav. Assess. 41 , 304–316 (2019).
Meghani, D. T. & Harvey, E. A. Asian Indian international students’ trajectories of depression, acculturation, and enculturation. Asian Am. J. Psychol. 7 , 1–14 (2016).
Barry, K. M., Woods, M., Martin, A., Stirling, C. & Warnecke, E. A randomized controlled trial of the effects of mindfulness practice on doctoral candidate psychological status. J. Am. Coll. Health 67 , 299–307 (2019).
Bolotnyy, V., Basilico, M. & Barreira, P. Graduate student mental health: lessons from American economics departments. J. Econ. Lit. (in press).
Barry, K. M., Woods, M., Warnecke, E., Stirling, C. & Martin, A. Psychological health of doctoral candidates, study-related challenges and perceived performance. High. Educ. Res. Dev. 37 , 468–483 (2018).
Boyle, K. M. & McKinzie, A. E. The prevalence and psychological cost of interpersonal violence in graduate and law school. J. Interpers. Violence 36 , 6319-6350 (2021).
Heinrich, D. L. The causal influence of anxiety on academic achievement for students of differing intellectual ability. Appl. Psychol. Meas. 3 , 351–359 (1979).
Hish, A. J. et al. Applying the stress process model to stress-burnout and stress-depression relationships in biomedical doctoral students: A cross-sectional pilot study. CBE Life Sci. Educ. 18 , 1–11 (2019).
Jamshidi, F. et al. A cross-sectional study of psychiatric disorders in medical sciences students. Mater. Sociomed. 29 , 188–191 (2017).
Liu, C. et al. Prevalence and associated factors of depression and anxiety among doctoral students: The mediating effect of mentoring relationships on the association between research self-efficacy and depression/anxiety. Psychol. Res. Behav. Manag. 12 , 195–208 (2019).
Sverdlik, A. & Hall, N. C. Not just a phase: Exploring the role of program stage on well-being and motivation in doctoral students. J. Adult Contin. Educ. 26 , 1–28 (2019).
University of California Office of the President. The University of California Graduate student Well-Being Survey Report (University of California, 2017).
The Graduate Assembly. Graduate Student Happiness & Well-Being Report (University of California at Berkeley, 2014).
Richardson, C. M., Trusty, W. T. & George, K. A. Trainee wellness: Self-critical perfectionism, self-compassion, depression, and burnout among doctoral trainees in psychology. Couns. Psychol. Q. 33 , 187-198 (2020).
Radloff, L. S. The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1 , 385–401 (1977).
Spitzer, R. L., Kroenke, K., Williams, J. B. W. & Lowe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 166 , 1092–1097 (2006).
Mata, D. A. et al. Prevalence of depression and depressive symptoms among residents physicians: A systematic review and meta-analysis. JAMA 314 , 2373–2383 (2015).
Gloria, C. T. & Steinhardt, M. A. Flourishing, languishing, and depressed postdoctoral fellows: Differences in stress, anxiety, and depressive symptoms. J. Postdoct. Aff. 3 , 1–9 (2013).
Levis, B. et al. Patient Health Questionnaire-9 scores do not accurately estimate depression prevalence: Individual participant data meta-analysis. J. Clin. Epidemiol. 122 , 115-128.e111 (2020).
Tsai, A. C. Reliability and validity of depression assessment among persons with HIV in sub-Saharan Africa: Systematic review and meta-analysis. J. Acquir. Immune Defic. Syndr. 66 , 503–511 (2014).
Baxter, A. J., Scott, K. M., Vos, T. & Whiteford, H. A. Global prevalence of anxiety disorders: A systematic review and meta-regression. Psychol. Med. 43 , 897–910 (2013).
Ferrari, A. et al. Global variation in the prevalence and incidence of major depressive disorder: A systematic review of the epidemiological literature. Psychol. Med. 43 , 471–481 (2013).
Hasin, D. S. et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry 75 , 336–346 (2018).
US Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health (Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, 2020).
Kessler, R. C. et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 62 , 593–602 (2005).
Working Group report to the Advisory Committee to the NIH Director. Changing the Culture to End Sexual Harassment (U. S. National Institutes of Health, 2019).
National Academies of Sciences Engineering and Medicine. Sexual Harassment of Women: Climate, Culture, and Consequences in Academic Sciences, Engineering, and Medicine (The National Academies Press, 2018).
Wadman, M. A hidden history. Science 360 , 480–485 (2018).
Hockfield, S., Magley, V. & Yoshino, K. Report of the External Review Committee to Review Sexual Harassment at Harvard University (External Review Committee to Review Sexual Harassment at Harvard University, 2021).
Bartlett, T. & Gluckman, N. She left Harvard. He got to stay. Chronicle High. Educ. 64 , A14 (2021). Available at: https://www.chronicle.com/article/she-left-harvard-he-got-to-stay/.
Tseng, M. et al. Strategies and support for Black, Indigenous, and people of colour in ecology and evolutionary biology. Nat. Ecol. Evol. 4 , 1288–1290 (2020).
Williams, D. R. et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: Results from the National Survey of American Life. Arch. Gen. Psychiatry 64 , 305–315 (2007).
Wu, A. H. Gender bias in rumors among professionals: An identity-based interpretation. Rev. Econ. Stat. 102 , 867–880 (2020).
Kessler, R. C. Epidemiology of women and depression. J. Affect. Disord. 74 , 5–13 (2003).
Mattheis, A., Cruz-Ramirez De Arellano, D. & Yoder, J. B. A model of queer STEM identity in the workplace. J. Homosex 67 , 1839–1863 (2020).
Semlyen, J., King, M., Varney, J. & Hagger-Johnson, G. Sexual orientation and symptoms of common mental disorder or low wellbeing: Combined meta-analysis of 12 UK population health surveys. BMC Psychiatry 16 , 1–19 (2016).
Lark, J. S. & Croteau, J. M. Lesbian, gay, and bisexual doctoral students’ mentoring relationships with faculty in counseling psychology: A qualitative study. Couns. Psychol. 26 , 754–776 (1998).
Jaremka, L. M. et al. Common academic experiences no one talks about: Repeated rejection, imposter syndrome, and burnout. Perspect Psychol Sci 15 , 519–543 (2020).
Allen, H. K. et al. Substance use and mental health problems among graduate students: Individual and program-level correlates. J. Am. Coll. Health https://doi.org/10.1080/07448481.2020.1725020 (2020).
Turner, A. & Berry, T. Counseling center contributions to student retention and graduation: A longitudinal assessment. J. Coll. Stud. Dev. 41 , 627–636 (2000).
Dyrbye, L. N., Thomas, M. R. & Shanafelt, T. D. Medical student distress: Causes, consequences, and proposed solutions. Mayo Clin. Proc. 80 , 1613–1622 (2005).
Tija, J., Givens, J. L. & Shea, J. A. Factors associated with undertreatment of medical student depression. J. Am. Coll. Health 53 , 219–224 (2005).
Dearing, R., Maddux, J. & Tangney, J. Predictors of psychological help seeking in clinical and counseling psychology graduate students. Prof. Psychol. Res. Pract. 36 , 323–329 (2005).
Langin, K. Amid concerns about grad student mental health, one university takes a novel approach. Science https://doi.org/10.1126/science.caredit.aay7113 (2019).
Guillory, D. Combating anti-blackness in the AI community. arXiv , arXiv:2006.16879 (2020).
Galán, C. A. et al. A call to action for an antiracist clinical science. J. Clin. Child Adolesc. Psychol 50 , 12-57 (2021).
Wyman, P. A. et al. Effect of the Wingman-Connect upstream suicide prevention program for air force personnel in training: A cluster randomized clinical trial. JAMA Netw Open 3 , e2022532 (2020).
Knox, K. L. et al. The US Air Force Suicide Prevention Program: Implications for public health policy. Am. J. Public Health 100 , 2457–2463 (2010).
Inclusive Climate Subcommittee of the Government Department Climate Change Committee. Government Department Climate Change: Final Report and Recommendations (Government Department, Harvard University, 2019).
Inclusive Climate Subcommittee of the Government Department Climate Change Committee. Government Department Climate Survey Report (Government Department, Harvard University, 2019).
Magoqwana, B., Maqabuka, Q. & Tshoaedi, M. “Forced to care” at the neoliberal university: Invisible labour as academic labour performed by Black women academics in the South African university. S. Afr. Rev. Sociol. 50 , 6–21 (2019).
Jones, H. A., Perrin, P. B., Heller, M. B., Hailu, S. & Barnett, C. Black psychology graduate students’ lives matter: Using informal mentoring to create an inclusive climate amidst national race-related events. Prof. Psychol. Res. Pract. 49 , 75–82 (2018).
Mathur, A., Meyers, F. J., Chalkley, R., O’Brien, T. C. & Fuhrmann, C. N. Transforming training to reflect the workforce. Sci. Transl. Med. 7 , 285 (2015).
Scharff, V. Advice: Prepare your Ph.D.s for diverse career paths. Chronicle High. Educ. 65 , 30 (2018).
Beattie, T. S., Smilenova, B., Krishnaratne, S. & Mazzuca, A. Mental health problems among female sex workers in low- and middle-income countries: A systematic review and meta-analysis. PLoS Med. 17 , e1003297 (2020).
Ismail, Z. et al. Prevalence of depression in patients with mild cognitive impairment: A systematic review and meta-analysis. JAMA Psychiatry 74 , 58–67 (2017).
Lim, G. Y. et al. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci. Rep. 8 , 1–10 (2018).
Article ADS Google Scholar
Jones-White, D. R., Soria, K. M., Tower, E. K. B. & Horner, O. G. Factors associated with anxiety and depression among U.S. doctoral students: Evidence from the gradSERU survey. J. Am. Coll. Health https://doi.org/10.1080/07448481.2020.1865975 (2021).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 151 , 264–269 (2009).
Helmers, K. F., Danoff, D., Steinert, Y., Leyton, M. & Young, S. N. Stress and depressed mood in medical students, law students, and graduate students at McGill University. Acad. Med. 72 , 708–714 (1997).
Rabkow, N. et al. Facing the truth: A report on the mental health situation of German law students. Int. J. Law Psychiatry 71 , 101599 (2020).
Bergin, A. & Pakenham, K. Law student stress: Relationships between academic demands, social isolation, career pressure, study/life imbalance and adjustment outcomes in law students. Psychiatr. Psychol. Law 22 , 388–406 (2015).
Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 25 , 603–605 (2010).
Freeman, M. F. & Tukey, J. W. Transformations related to the angular and the square root. Ann. Math. Stat. 21 , 607–611 (1950).
Article MathSciNet MATH Google Scholar
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control Clin. Trials 7 , 177–188 (1986).
Wilson, E. B. Probable inference, the law of succession, and statistical inference. J. Am. Stat. Assoc. 22 , 209–212 (1927).
Newcombe, R. G. Two-sided confidence intervals for the single proportion: Comparison of seven methods. Stat. Med. 17 , 857–872 (1998).
Higgins, J. P. T. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21 , 1539–1558 (2002).
Kroenke, K., Spitzer, R. L. & Williams, J. B. W. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 16 , 606–613 (2001).
Download references
Acknowledgements
We thank the following investigators for generously sharing their time and/or data: Gordon J. G. Asmundson, Ph.D., Amy J. L. Baker, Ph.D., Hillel W. Cohen, Dr.P.H., Alcir L. Dafre, Ph.D., Deborah Danoff, M.D., Daniel Eisenberg, Ph.D., Lou Farrer, Ph.D., Christy B. Fraenza, Ph.D., Patricia A. Frazier, Ph.D., Nadia Corral-Frías, Ph.D., Hanga Galfalvy, Ph.D., Edward E. Goldenberg, Ph.D., Robert K. Hindman, Ph.D., Jürgen Hoyer, Ph.D., Ayako Isato, Ph.D., Azharul Islam, Ph.D., Shanna E. Smith Jaggars, Ph.D., Bumseok Jeong, M.D., Ph.D., Ju R. Joeng, Nadine J. Kaslow, Ph.D., Rukhsana Kausar, Ph.D., Flavius R. W. Lilly, Ph.D., Sarah K. Lipson, Ph.D., Frances Meeten, D.Phil., D.Clin.Psy., Dhara T. Meghani, Ph.D., Sterett H. Mercer, Ph.D., Masaki Mori, Ph.D., Arif Musa, M.D., Shizar Nahidi, M.D., Ph.D., Arthur M. Nezu, Ph.D., D.H.L., Angelo Picardi, M.D., Nicole E. Rossi, Ph.D., Denise M. Saint Arnault, Ph.D., Sagar Sharma, Ph.D., Bryony Sheaves, D.Clin.Psy., Kennon M. Sheldon, Ph.D., Daniel Shepherd, Ph.D., Keisuke Takano, Ph.D., Sara Tement, Ph.D., Sherri Turner, Ph.D., Shawn O. Utsey, Ph.D., Ron Valle, Ph.D., Caleb Wang, B.S., Pengju Wang, Katsuyuki Yamasaki, Ph.D.
A.C.T. acknowledges funding from the Sullivan Family Foundation. This paper does not reflect an official statement or opinion from the County of San Mateo.
Author information
Authors and affiliations.
Center for Global Health, Massachusetts General Hospital, Boston, MA, USA
Emily N. Satinsky & Alexander C. Tsai
San Mateo County Behavioral Health and Recovery Services, San Mateo, CA, USA
Tomoki Kimura
Department of Epidemiology and Population Health, Stanford University, Palo Alto, CA, USA
Mathew V. Kiang
Center for Population Health Sciences, Stanford University School of Medicine, Palo Alto, CA, USA
Harvard Society of Fellows, Harvard University, Cambridge, MA, USA
Rediet Abebe
Department of Electrical Engineering and Computer Science, University of California Berkeley, Berkeley, CA, USA
Department of Economics, Hankamer School of Business, Baylor University, Waco, TX, USA
Scott Cunningham
Department of Sociology, Washington University in St. Louis, St. Louis, MO, USA
Department of Microbiology, Immunology, and Molecular Genetics, Institute for Quantitative and Computational Biosciences, University of California Los Angeles, Los Angeles, CA, USA
Xiaofei Lin
Departments of Newborn Medicine and Psychiatry, Brigham and Women’s Hospital, Boston, MA, USA
Cindy H. Liu
Harvard Medical School, Boston, MA, USA
Cindy H. Liu & Alexander C. Tsai
Centre for Global Health, Edinburgh Medical School, Usher Institute, University of Edinburgh, Edinburgh, Scotland, UK
Department of Psychiatry, University of Michigan, Ann Arbor, MI, USA
Department of Global Health, Institute for Life Course Health Research, Stellenbosch University, Cape Town, South Africa
Mark Tomlinson
School of Nursing and Midwifery, Queens University, Belfast, UK
Fielding School of Public Health, Los Angeles Area Health Services Research Training Program, University of California Los Angeles, Los Angeles, CA, USA
Miranda Yaver
Mongan Institute, Massachusetts General Hospital, Boston, MA, USA
Alexander C. Tsai
You can also search for this author in PubMed Google Scholar
Contributions
A.C.T. conceptualized the study and provided supervision. T.K. conducted the search. E.N.S. contacted authors for additional information not reported in published articles. E.N.S. and T.K. extracted data and performed the quality assessment appraisal. E.N.S. and A.C.T. conducted the statistical analysis and drafted the manuscript. T.K., M.V.K., R.A., S.C., H.L., X.L., C.H.L., I.R., S.S., M.T. and M.Y. contributed to the interpretation of the results. All authors provided critical feedback on drafts and approved the final manuscript.
Corresponding authors
Correspondence to Emily N. Satinsky or Alexander C. Tsai .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Satinsky, E.N., Kimura, T., Kiang, M.V. et al. Systematic review and meta-analysis of depression, anxiety, and suicidal ideation among Ph.D. students. Sci Rep 11 , 14370 (2021). https://doi.org/10.1038/s41598-021-93687-7
Download citation
Received : 31 March 2021
Accepted : 24 June 2021
Published : 13 July 2021
DOI : https://doi.org/10.1038/s41598-021-93687-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
How to improve academic well-being: an analysis of the leveraging factors based on the italian case.
- Alice Tontodimamma
- Emiliano del Gobbo
- Antonio Aquino
Quality & Quantity (2024)
Suicidal affective risk among female college students: the impact of life satisfaction
- Dawei Huang
- Xianbin Wang
Current Psychology (2024)
A single-center assessment of mental health and well-being in a biomedical sciences graduate program
- Sarah K. Jachim
- Bradley S. Bowles
- Autumn J. Schulze
Nature Biotechnology (2023)
Mental Health Problems Among Graduate Students in Turkey: a Cross-Sectional Study
- Cafer Kılıç
- Faika Şanal Karahan
International Journal for the Advancement of Counselling (2023)
A study in University of Ruhuna for investigating prevalence, risk factors and remedies for psychiatric illnesses among students
- Patikiri Arachchige Don Shehan Nilm Wijesekara
Scientific Reports (2022)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

COMMENTS
When a 2018 study revealed that Ph.D. students suffer from depression at rates far higher than the general population, it sparked a landslide of concern about graduate student mental health, with some calling it a mental health crisis.The study highlighted a need to understand what aspects of graduate school affect depression, says Katelyn Cooper, an assistant professor at Arizona State ...
The mental health of PhD researchers demands urgent ...
More than 40% of PhD students met the criteria for moderate to severe depression or anxiety. In contrast, 32% of working professionals met these criteria for depression, and 26% for anxiety. The ...
The end result is that students and academics are much more likely to experience depression and anxiety than is the general population. ... PhD students compete in a team-building relay race at a ...
Interestingly, female PhD students, who were slightly less likely than men to experience significant depression, showed a greater tendency to use good coping approaches compared to their counterparts.
PhD and master's students worldwide report rates of depression and anxiety that are six times higher than those in the general public (T. M. Evans et al. Nature Biotech. 36, 282-284; 2018).The ...
students from 28 institutions, we examined how research and teaching affect depression in PhD students and how depression in turn affects students' experiences teaching and re - searching. Using inductive coding, we identified factors that either positively or negatively affected student depression.
A PhD student's experience is often marked by high rates of depression, a concern echoed in studies from universities like the University of California and Arizona State University. If you are embarking on a PhD journey, make sure you are aware of the issue, and develop strategies to cope with the stress, so you do not end up with depression.
Graduate students are more than six times as likely to experience depression compared with the general population. However, few studies have examined how graduate school specifically affects depression. In this qualitative interview study of 50 life sciences PhD students from 28 institutions, we exa …
Depression and anxiety among students in higher education are well-established public health concerns with rates that have steadily increased over the past several decades. The global COVID-19 pandemic caused a need for rapid transition on campuses to online learning, a disruption of research, and uncertainty about meeting program requirements and employment. Graduate students often feel ...
Overall, 71% of PhD students and 62% of working professionals who responded to the survey from April 2018 to November 2019 had experienced signs of at least mild depression. Seventy-four percent ...
Warren Wong/Creative Commons. Approximately one-third of Ph.D. students are at risk of having or developing a common psychiatric disorder like depression, a recent study reports. Although these results come from a small sample—3659 students at universities in Flanders, Belgium, 90% of whom were studying the sciences and social sciences—they ...
A PhD candidate was 2.4 times more likely to develop psychiatric health problems than someone in the general population with a bachelor's degree. 3 Bernstein reported that 42% of PhD students in science and 48% of PhD students in engineering at the University of California were depressed on the Center for Epidemiologic Studies Depression ...
Factors explaining PhD students' depression. Our second contribution is to explain-within the UK PhD population-whose mental health is more affected by the pandemic-induced research disruption. We find that several factors have a significant impact on PhD students to have or develop mental health issues during a period of research disruption.
Sadly, 42% of PhD students reported that they believed having a mental health problem during your PhD is the norm. We also found similar numbers saying they have considered taking a break from their studies for mental health reasons, with 14% actually taking a mental health-related break. Finally, 35% of PhD students have considered ending ...
Signs of depression and anxiety soar among US graduate students during pandemic. Signs of depression and anxiety soar among US graduate students during pandemic. Nature. 2020 Sep;585 (7823):147-148. doi: 10.1038/d41586-020-02439-6.
Navigating mental health challenges in graduate school
Over 3,000 PhD students completed the survey, as well as a matched control group of 1,168 working professionals. PhD students reported significant anxiety and depression levels, a difference which was not explained by a higher rate of pre-existing mental health problems.
Post-Grad Depression: Signs, Causes, and Coping Tips
7 Reasons Why Your PhD Is Causing Stress And Depression
Signs of depression among graduate students in the United States have apparently doubled during the COVID-19 pandemic, according to a survey that drew responses from more than 15,000 graduate and ...
Graduate students are more than six times as likely to experience depression compared with the general population. However, few studies have examined how graduate school specifically affects depression. In this qualitative interview study of 50 life sciences PhD students from 28 institutions, we examined how research and teaching affect depression in PhD students and how depression in turn ...
We are pleased to announce that Nadine Melhem, PhD, has been promoted to Professor of Psychiatry by the University of Pittsburgh School of Medicine. Dr. Melhem earned her PhD in psychiatric epidemiology from the University of Pittsburgh School of Public Health. She has dedicated her research career to improving our understanding of the risk for psychiatric disorders in children who have ...
Systematic review and meta-analysis of depression ...