- Patient Care & Health Information
- Diseases & Conditions
- Schizophrenia
Schizophrenia is a serious mental health condition that affects how people think, feel and behave. It may result in a mix of hallucinations, delusions, and disorganized thinking and behavior. Hallucinations involve seeing things or hearing voices that aren't observed by others. Delusions involve firm beliefs about things that are not true. People with schizophrenia can seem to lose touch with reality, which can make daily living very hard.
People with schizophrenia need lifelong treatment. This includes medicine, talk therapy and help in learning how to manage daily life activities.
Because many people with schizophrenia don't know they have a mental health condition and may not believe they need treatment, many research studies have examined the results of untreated psychosis. People who have psychosis that is not treated often have more-severe symptoms, more stays in a hospital, poorer thinking and processing skills and social outcomes, injuries, and even death. On the other hand, early treatment often helps control symptoms before serious complications arise, making the long-term outlook better.

Products & Services
- A Book: Mayo Clinic Family Health Book
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Schizophrenia involves a range of problems in how people think, feel and behave. Symptoms may include:
- Delusions. This is when people believe in things that aren't real or true. For example, people with schizophrenia could think that they're being harmed or harassed when they aren't. They could think that they're the target for certain gestures or comments when they aren't. They may think they're very famous or have great ability when that's not the case. Or they could feel that a major disaster is about to occur when that's not true. Most people with schizophrenia have delusions.
- Hallucinations. These usually involve seeing or hearing things that other people don't observe. For people with schizophrenia, these things seem real. Hallucinations can occur with any of the senses, but hearing voices is most common.
- Disorganized speech and thinking. Disorganized speech causes disorganized thinking. It can be hard for people with schizophrenia to talk with other people. The answers people with schizophrenia give to questions may not be related to what's being asked. Or questions may not be answered fully. Rarely, speech may include putting together unrelated words in a way that can't be understood. Sometimes this is called word salad.
- Extremely disorganized or unusual motor behavior. This may show in several ways, from childlike silliness to being agitated for no reason. Behavior isn't focused on a goal, so it's hard to do tasks. People with schizophrenia may not want to follow instructions. They may move in ways that are not typical or not appropriate to the social setting. Or they may not move much or respond at all.
- Negative symptoms. People with schizophrenia may not be able to function in the way they could before their illness started. For example, they may not bathe, make eye contact or show emotions. They may speak in a monotone voice and not be able to feel pleasure. Also, they may lose interest in everyday activities, socially withdraw and have a hard time planning ahead.
Symptoms can vary in type and how severe they are. At times, symptoms may get better or worse. Some symptoms may be present at all times.
People with schizophrenia usually are diagnosed in the late teen years to early 30s. In men, schizophrenia symptoms usually start in the late teens to early 20s. In women, symptoms usually begin in the late 20s to early 30s. There also is a group of people — usually women — who are diagnosed later in life. It isn't common for children to be diagnosed with schizophrenia.
Symptoms in teenagers
Schizophrenia symptoms in teenagers are like those in adults, but the condition may be harder to pinpoint. That's because some early symptoms of schizophrenia — those that occur before hallucinations, delusions and disorganization — are commonly seen in many teens, such as:
- Withdrawing from friends and family.
- Not doing well in school.
- Having trouble sleeping.
- Feeling irritable or depressed.
- Lacking motivation.
Also, the use of recreational drugs, such as marijuana, stimulants like cocaine and methamphetamines, or hallucinogens, can cause similar symptoms. Compared with adults with schizophrenia, teens with the condition may be less likely to have delusions and more likely to have hallucinations.
When to see a doctor
People with schizophrenia often don't know that they have a mental condition that needs medical attention. As a result, family or friends often need to get them help.
Helping someone who may have schizophrenia
If people you know have symptoms of schizophrenia, talk to them about your concerns. While you can't force them to seek help, you can offer encouragement and support. You also can help them find a healthcare professional or mental health professional.
If people are a danger to themselves or others, or they don't have food, clothing or shelter, you may need to call 911 in the U.S. or other emergency responders for help. A mental health professional needs to evaluate them.
Some people may need an emergency stay in a hospital. Laws on mental health treatment against a person's will vary by state. You can contact community mental health agencies or police departments in your area for details.
Suicidal thoughts and behavior
Suicidal thoughts and attempts are much higher than average in people with schizophrenia. If a person is in danger of suicide or has made a suicide attempt, make sure that someone stays with that person. Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week. Or use the Lifeline Chat. Services are free and confidential. The Suicide & Crisis Lifeline in the U.S. has a Spanish language phone line at 1-888-628-9454 (toll-free).
Proper treatment of schizophrenia can reduce the risk of suicide.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
It isn't known what causes schizophrenia. But researchers believe that a mix of genetics, brain chemistry and environment can play a part.
Changes in certain naturally occurring brain chemicals, including neurotransmitters called dopamine and glutamate, may play a part in schizophrenia. Neuroimaging studies show changes in the brain structure and central nervous systems of people with schizophrenia. While researchers haven't yet been able to apply these findings to new treatments, the findings show that schizophrenia is a brain disease.
Risk factors
Although the cause of schizophrenia is not known, these factors seem to make schizophrenia more likely:
- A family history of schizophrenia.
- Life experiences, such as living in poverty, stress or danger.
- Some pregnancy and birth issues, such as not getting enough nutrition before or after birth, low birth weight, or exposure to toxins or viruses before birth that may affect brain development.
- Taking mind-altering — also called psychoactive or psychotropic — drugs as a teen or young adult.
Complications
Left untreated, schizophrenia can lead to severe problems that affect every area of life.
Complications that schizophrenia may cause or be related to include:
- Suicide, suicide attempts and thoughts of suicide.
- Anxiety disorders and obsessive-compulsive disorder, also known as OCD.
- Depression.
- Misuse of alcohol or other drugs, including nicotine.
- Not being able to work or attend school.
- Money problems and homelessness.
- Social isolation.
- Health and medical problems.
- Being victimized.
- Aggressive or violent behavior, though people with schizophrenia are more likely to be assaulted rather than assault others.
There's no sure way to prevent schizophrenia. But staying with your treatment plan can help stop symptoms from returning or getting worse. Researchers hope that learning more about risk factors for schizophrenia may lead to earlier diagnosis and treatment.
- Schizophrenia spectrum and other psychotic disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5-TR. 5th ed. American Psychiatric Association; 2022. https://dsm.psychiatryonline.org. Accessed Jan. 18, 2024.
- Fischer BA, et al. Schizophrenia in adults: Clinical features, assessment, and diagnosis. https://www.uptodate.com/contents/search. Accessed Jan. 18, 2024.
- Stroup TS, et al. Schizophrenia in adults: Maintenance therapy and side effect management. https://www.uptodate.com/contents/search. Accessed Jan. 18, 2024.
- Fisher DJ, et al. The neurophysiology of schizophrenia: Current update and future directions. International Journal of Psychophysiology. 2019; doi:10.1016/j.ijpsycho.2019.08.005.
- Schizophrenia. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/schizophrenia. Accessed Jan. 18, 2024.
- Schizophrenia. National Alliance on Mental Illness. https://www.nami.org/About-Mental-Illness/Mental-Health-Conditions/Schizophrenia. Accessed Jan. 18, 2024.
- What is schizophrenia? American Psychiatric Association. https://www.psychiatry.org/patients-families/schizophrenia/what-is-schizophrenia. Accessed Jan. 18, 2024.
- Schizophrenia. Merck Manual Professional Version. https://www.merckmanuals.com/professional/psychiatric-disorders/schizophrenia-and-related-disorders. Accessed Jan. 18, 2024.
- Supporting a family member with serious mental illness. American Psychological Association. https://www.apa.org/topics/mental-health/support-serious-mental-illness. Accessed Jan. 18, 2024.
- For friends and family members. Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/mental-health/how-to-talk/friends-and-family-members. Accessed Jan. 18, 2024.
- For people with mental health problems. Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/mental-health/how-to-talk/people-with-mental-health-problems. Accessed Jan. 18, 2024.
- Roberts LW, et al. Schizophrenia spectrum and other psychotic disorders. In: The American Psychiatric Association Publishing Textbook of Psychiatry. 7th ed. American Psychiatric Association Publishing; 2019. https://psychiatryonline.org. Accessed Jan. 18, 2024.
- Allen ND (expert opinion). Mayo Clinic. April 17, 2024.
- Leung JG (expert opinion). Mayo Clinic. April 16, 2024.
- Antipsychotic drugs. Merck Manual Professional Version. https://www.merckmanuals.com/professional/psychiatric-disorders/schizophrenia-and-related-disorders/antipsychotic-drugs. Accessed Jan. 19, 2024.
Associated Procedures
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Help transform healthcare
Your donation can make a difference in the future of healthcare. Give now to support Mayo Clinic's research.
Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Fact sheets /
Schizophrenia
- Schizophrenia causes psychosis and is associated with considerable disability and may affect all areas of life including personal, family, social, educational, and occupational functioning.
- Stigma, discrimination, and violation of human rights of people with schizophrenia are common.
- More than two out of three people with psychosis in the world do not receive specialist mental health care.
- A range of effective care options for people with schizophrenia exist and at least one in three people with schizophrenia will be able to fully recover.
Schizophrenia is characterised by significant impairments in the way reality is perceived and changes in behaviour related to:
- persistent delusions: the person has fixed beliefs that something is true, despite evidence to the contrary;
- persistent hallucinations: the person may hear, smell, see, touch, or feel things that are not there;
- experiences of influence, control or passivity: the experience that one’s feelings, impulses, actions, or thoughts are not generated by oneself, are being placed in one’s mind or withdrawn from one’s mind by others, or that one’s thoughts are being broadcast to others;
- disorganized thinking, which is often observed as jumbled or irrelevant speech;
- highly disorganised behaviour e.g. the person does things that appear bizarre or purposeless, or the person has unpredictable or inappropriate emotional responses that interfere with their ability to organise their behaviour;
- “negative symptoms” such as very limited speech, restricted experience and expression of emotions, inability to experience interest or pleasure, and social withdrawal; and/or
- extreme agitation or slowing of movements, maintenance of unusual postures.
People with schizophrenia often also experience persistent difficulties with their cognitive or thinking skills, such as memory, attention, and problem-solving.
At least one third of people with schizophrenia experiences complete remission of symptoms (1). Some people with schizophrenia experience worsening and remission of symptoms periodically throughout their lives, others a gradual worsening of symptoms over time.
Magnitude and impact
Schizophrenia affects approximately 24 million people or 1 in 300 people (0.32%) worldwide. This rate is 1 in 222 people (0.45%) among adults (2). It is not as common as many other mental disorders. Onset is most often during late adolescence and the twenties, and onset tends to happen earlier among men than among women.
Schizophrenia is frequently associated with significant distress and impairment in personal, family, social, educational, occupational, and other important areas of life.
People with schizophrenia are 2 to 3 times more likely to die early than the general population (3). This is often due to physical illnesses, such as cardiovascular, metabolic, and infectious diseases.
People with schizophrenia often experience human rights violations both inside mental health institutions and in community settings. Stigma against people with this condition is intense and widespread, causing social exclusion, and impacting their relationships with others, including family and friends. This contributes to discrimination, which in turn can limit access to general health care, education, housing, and employment.
During humanitarian and public health emergencies, extreme stress and fear, breakdown of social supports, isolation and disruption of health-care services and supply of medication can occur. These changes can have an impact on the lives of people with schizophrenia, such as exacerbation of existing symptoms. During emergencies, people with schizophrenia are more vulnerable than others to various human rights violations, including neglect, abandonment, homelessness, abuse and exclusion.
Causes of schizophrenia
Research has not identified one single cause of schizophrenia. It is thought that an interaction between genes and a range of environmental factors may cause schizophrenia. Psychosocial factors may also affect the onset and course of schizophrenia. Heavy use of cannabis is associated with an elevated risk of the disorder.
Currently, the vast majority of people with schizophrenia around the world are not receiving mental health care. Approximately 50% of people in mental hospitals have a schizophrenia diagnosis (4). Only 31.3% of people with psychosis receive specialist mental health care (5). Most resources for mental health services are inefficiently spent on care within mental hospitals.
There is clear evidence that mental hospitals are not effective in providing the care that people with mental health conditions need and, regularly, violate the basic human rights of persons with schizophrenia. Efforts to transfer care from mental health institutions to the community need to be expanded and accelerated. Such efforts start with the development of a range of quality community-based mental health services. Options for community-based mental health care include integration in primary health and general hospital care, community mental health centres, day centres, supported housing, and outreach services for home-based support. The engagement of the person with schizophrenia, family members and the wider community in providing support is important.
Management and support
A range of effective care options for people with schizophrenia exist, and these include medication, psychoeducation, family interventions, cognitive-behavioural therapy and psychosocial rehabilitation (e.g., life skills training). Facilitated assisted living, supported housing and supported employment are essential care options that should be available for people with schizophrenia. A recovery-oriented approach – giving people agency in treatment decisions – is essential for people with schizophrenia and for their families and/or caregivers as well.
WHO response
WHO’s Comprehensive Mental Health Action Plan 2013-2030 highlights the steps required to provide appropriate services for people with mental disorders including schizophrenia. A key recommendation of the Action Plan is to shift services from institutions to the community. The WHO Special Initiative for Mental Health aims to further progress towards objectives of the Comprehensive Mental Health Action Plan 2013-2030 by ensuring 100 million more people have access to quality and affordable care for mental health conditions.
WHO's Mental Health Gap Action Programme (mhGAP) uses evidence-based technical guidance, tools and training packages to expand service in countries, especially in resource-poor settings. It focuses on a prioritized set of conditions, including psychosis, directing capacity building towards non-specialized health-care providers in an integrated approach that promotes mental health at all levels of care. Currently mhGAP is being implemented in more than 100 WHO Member States.
The WHO QualityRights Project involves improving the quality of care and human rights conditions in mental health and social care facilities and to empower organizations to advocate for the health of people with mental health conditions and psychosocial disabilities.
The WHO guidance on community mental health services and person-centred and rights-based approaches provides information and support to all stakeholders who wish to develop or transform their mental health system and services to align with international human rights standards including the UN Convention on the Rights of Persons with Disabilities.
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J. Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
(2) Institute of health Metrics and Evaluation (IHME). Global Health Data Exchange (GHDx). http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/27a7644e8ad28e739382d31e77589dd7 (Accessed 25 September 2021)
(3) Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annual Review of Clinical Psychology , 2014;10, 425-438.
(4) WHO. Mental health systems in selected low- and middle-income countries: a WHO-AIMS cross-national analysis. WHO: Geneva, 2009
(5) Jaeschke K et al. Global estimates of service coverage for severe mental disorders: findings from the WHO Mental Health Atlas 2017 Glob Ment Health 2021;8:e27.
WHO’s Comprehensive Mental Health Action Plan 2013-2030
WHO Special Initiative for Mental Health
WHO's Mental Health Gap Action Programme (mhGAP )
WHO QualityRights Project
WHO guidance on community mental health services and person-centred and rights-based approaches
More on mental health
- What is Schizophrenia?
Schizophrenia is a chronic brain disorder that affects less than one percent of the U.S. population. When schizophrenia is active, symptoms can include delusions, hallucinations, disorganized speech, trouble with thinking and lack of motivation. However, with treatment, most symptoms of schizophrenia will greatly improve and the likelihood of a recurrence can be diminished.
While there is no cure for schizophrenia, research is leading to innovative and safer treatments. Experts also continue to unravel the causes of the disease by studying genetics, conducting behavioral research, and using advanced imaging to look at the brain’s structure and function. These approaches hold the promise of new, and more effective therapies.
The complexity of schizophrenia may help explain why there are misconceptions about the disease. Despite the origin of the word, from the Latin meaning "split mind," schizophrenia does not mean split personality or multiple personality. Most people with schizophrenia are not any more dangerous or violent than people in the general population and may, in fact, be more vulnerable to being the victims of crimes. While limited mental health resources in the community may lead to homelessness and frequent hospitalizations, it is a misconception that people with schizophrenia end up homeless or living in hospitals. Most people with schizophrenia live with their family, in group homes or on their own.
Research has shown that schizophrenia affects men and women fairly equally but may have an earlier onset in males. Rates are similar around the world. People with schizophrenia are more likely to die younger than the general population, largely because of high rates of co-occurring medical conditions, such as heart disease and diabetes.
Definitions
- Psychosis refers to a set of symptoms characterized by a loss of touch with reality due to a disruption in the way that the brain processes information. When someone experiences a psychotic episode, the person’s thoughts and perceptions are disturbed, and the individual may have difficulty understanding what is real and what is not.
- Delusions are fixed false beliefs held despite clear or reasonable evidence that they are not true. Persecutory (or paranoid) delusions, when a person believes they are being harmed or harassed by another person or group, are the most common.
- Hallucinations are the experience of hearing, seeing, smelling, tasting, or feeling things that are not there. They are vivid and clear with an impression similar to normal perceptions. Auditory hallucinations, or “hearing voices,” are the most common in schizophrenia and related psychotic disorders.
- Disorganized thinking and speech refer to thoughts and speech that are jumbled or do not make sense. For example, the person may switch from one topic to another or respond with an unrelated topic in conversation. The symptoms are severe enough to cause substantial problems with normal communication.
- Disorganized or abnormal motor behavior are movements that can range from childlike silliness to unpredictable agitation or can manifest as repeated movements without purpose. When the behavior is severe, it can cause problems in the performance of activities of daily life. It includes catatonia, when a person appears as if in a daze with little movement or response to the surrounding environment.
When the disease is active, it can be characterized by episodes in which the person is unable to distinguish between real and unreal experiences. As with any illness, the severity, duration and frequency of symptoms can vary; however, in persons with schizophrenia, the incidence of severe psychotic symptoms often decreases as the person becomes older. Not taking medications as prescribed, the use of alcohol or illicit drugs, and stressful situations tend to increase symptoms. Symptoms fall into three major categories:
- Positive symptoms (those abnormally present): Hallucinations, such as hearing voices or seeing things that do not exist, paranoia and exaggerated or distorted perceptions, beliefs and behaviors.
- Negative symptoms (those abnormally absent): Impaired emotional expression (affective flattening), decreased speech output (alogia), reduced desire to have social contact (asociality), reduced drive to initiate and persist in self-directed purposeful activities (avolition), and decreased experience of pleasure (anhedonia).
- Disorganized symptoms: Confused and disordered thinking and speech, trouble with logical thinking, and sometimes bizarre behavior or abnormal movements.
Cognition is another area of functioning that is affected in schizophrenia leading to problems with attention, concentration, and memory, and to declining educational performance.
Symptoms of schizophrenia usually first appear in early adulthood and must persist for at least six months for a diagnosis to be made. Men often experience initial symptoms in their late teens or early 20s while women tend to show first signs of the illness in their 20s and early 30s. More subtle signs may be present earlier, including troubled relationships, poor school performance and reduced motivation.
Before a diagnosis can be made, however, a psychiatrist should conduct a thorough medical examination to rule out substance misuse or other neurological or medical illnesses whose symptoms may mimic schizophrenia.
Risk Factors
Researchers believe that several genetic and environmental factors contribute to risk of developing schizophrenia, and life stressors may play a role in the start of symptoms and their course. Since multiple factors may contribute, scientists cannot yet be specific about the exact cause in each individual case.
Though there is no cure for schizophrenia, many patients under treatment do well with minimal symptoms. A variety of antipsychotic medications are effective in reducing the psychotic symptoms present in the acute phase of the illness, and they also help reduce the potential for future acute episodes and their severity. Psychological treatments such as cognitive behavioral therapy or supportive psychotherapy may reduce symptoms and enhance function. Other treatments are aimed at reducing stress, supporting employment and improving social skills.
Diagnosis and treatment can be complicated by substance misuse. People with schizophrenia are at greater risk of substance-related disorder than the general population. If a person shows signs of addiction, treatment for the addiction should occur along with treatment for schizophrenia.
Schizophrenia and Lack of Insight (Anosognosia) . Some individuals with psychosis may lack insight or awareness of their disorder, a phenomenon known as anosognosia . This lack of insight includes unawareness of symptoms of schizophrenia and may be present throughout the entire course of the illness. Anosognosia is typically a symptom of schizophrenia itself rather than a coping strategy. People with anosognosia are less likely to stay in treatment and more likely to relapse, experience involuntary treatments, and to have poorer psychosocial functioning.
Rehabilitation and Living with Schizophrenia
Treatment can help many people with schizophrenia lead highly productive and rewarding lives. As with other chronic illnesses, some patients do extremely well while others continue to be symptomatic and need support and assistance.
After the symptoms of schizophrenia are controlled, various types of therapy should continue to help people manage the illness and improve their lives. Therapy and psychosocial supports can help people learn social skills, cope with stress, identify early warning signs of relapse and prolong periods of remission. Because schizophrenia typically strikes in early adulthood, individuals with the disorder often benefit from rehabilitation to help develop life-management skills, complete vocational or educational training, and hold a job. For example, supported employment programs have been found to help people with schizophrenia achieve self-sufficiency. These programs provide people with severe mental illness competitive jobs in the community.
For many people living with schizophrenia family support is particularly important to their health and well-being. It is also essential for families to be informed and supported themselves. Organizations such as the Schizophrenia and Psychosis Action Alliance, Mental Health America (MHA) and the National Alliance on Mental Illness (NAMI) offer resources and support to individuals with schizophrenia and other mental illnesses and their families. (See Additional Resources below.)
Optimism is important and patients, family members and mental health professionals need to be mindful that many patients have a favorable course of illness, that challenges can often be addressed, and that patients have many personal strengths that must be recognized and supported.
Related Conditions
Below are brief descriptions of several other mental health disorders with characteristics and symptoms similar to schizophrenia including delusional disorder, brief psychotic disorder, schizophreniform disorder and schizoaffective disorder.
Delusional Disorder
Delusional disorder involves a person having false beliefs (delusions) that persist for at least one month. The delusions can be bizarre (about things that cannot possibly occur) or non-bizarre (things that are possible but not likely, such as a belief about being followed or poisoned).
Apart from the delusion(s), delusional disorder does not involve other symptoms. The person may not appear to have any problems with functioning and behavior except when they talk about or act on the delusion.
Delusional beliefs can lead to problems with relationships or at work, and to legal troubles. Delusional disorder is rare with a lifetime prevalence estimated at around 0.2%. Delusional disorder is treated with individual psychotherapy, although people rarely seek treatment as they often do not feel they needed it.
Brief Psychotic Disorder
Brief psychotic disorder occurs when a person experiences a sudden short period of psychotic behavior. This episode lasts between one day and one month and then the symptoms completely disappear with the person fully returning to their previous level of functioning.
Brief psychotic disorder involves one (or more) of the following symptoms:
- Hallucinations
- Disorganized speech
- Grossly disorganized or catatonic behavior
Although the disturbance is short, individuals with brief psychotic disorder typically experience emotional turmoil or overwhelming confusion. Brief psychotic disorder can occur at any age, though the average age at onset is the mid-30s.
It is important to distinguish symptoms of brief psychotic disorder from culturally appropriate responses. For example, in some religious ceremonies, an individual may report hearing voices, but these do not generally persist and are not perceived as abnormal by most members of the individual’s community.
Schizophreniform Disorder
The symptoms of schizophreniform disorder are similar to those of schizophrenia, but the symptoms only last a short time—at least one month but less than six months. If the symptoms last longer than six months, then the diagnosis changes to schizophrenia.
Schizophreniform disorder involves two or more of the following symptoms, each present for a significant portion of time during a one-month period (or less if successfully treated)::
- Grossly disorganized behavior or catatonic behavior
- Negative symptoms
A diagnosis of schizophreniform disorder does not require problems in social or occupational functioning (as schizophrenia does). In the U.S., schizophreniform disorder is significantly less common than schizophrenia. About one-third of individuals with an initial diagnosis of schizophreniform disorder recover within the 6-month period and schizophreniform disorder is their final diagnosis. Most of the remaining two-thirds of individuals will eventually receive a diagnosis of schizophrenia or schizoaffective disorder.
Schizoaffective Disorder
People with schizoaffective disorder experience symptoms of a major mood episode of depression or bipolar disorder (major depression or mania) at the same time as symptoms of schizophrenia (delusions, hallucinations, disorganized speech, grossly disorganized behavior, or negative symptoms). Symptoms of a major mood episode must be present for the majority of the duration of the active illness and there must be a period of at least two weeks when delusions or hallucinations are present in the absence of a mood episode.
Schizoaffective disorder is about one-third as common as schizophrenia, affecting about 0.3% of people at some time in their lives. The typical age at onset of schizoaffective disorder is early adulthood, although it can begin anywhere from adolescence to late in life. A significant number of individuals initially diagnosed with another psychotic illness later receive the diagnosis of schizoaffective disorder when the pattern of mood episodes becomes apparent.
Physician Review
Felix Torres, M.D., MBA, FACHE, DFAPA, CCHP-MH
More on Schizophrenia
- Find a local support group
- Discussion groups
- What is schizophrenia?
- Clinical trials
Medical leadership for mind, brain and body.
Mobile menu.
- Psychiatrists
- Residents & Medical Students
- Patients and Families
- Advocacy & APAPAC
- Diversity & Health Equity
- Research & Registry
- Meetings & Events
- Search Directories & Databases
- International
- Medical Students
- What is Psychiatry?
- Find a Psychiatrist
- Addiction and Substance Use Disorders
- Dementia and Alzheimer's Disease
- Alcohol Use Disorder
- Anxiety Disorders
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- Autism Spectrum Disorder
- Bipolar Disorders
- Climate Change and Mental Health Connections
- Coping After Disaster
- Disruptive, Impulse-Control and Conduct Disorders
- Dissociative Disorders
- Domestic Violence
- Eating Disorders
- E-Cigarettes and Vaping
- Gambling Disorder
- Gender Dysphoria
- Helping a Loved One Cope with Mental Illness
- Hoarding Disorder
- Integrated Behavioral Healthcare
- Intellectual Disability
- Internet Gaming
- Obsessive-Compulsive Disorder
- Opioid Use Disorder
- Perinatal Depression (formerly Postpartum)
- Personality Disorders
- Posttraumatic Stress Disorder (PTSD)
- Prolonged Grief Disorder
- Schizophrenia
- Seasonal Affective Disorder (SAD)
- Sleep Disorders
- Somatic Symptom Disorder
- Specific Learning Disorders
- Stigma, Prejudice and Discrimination Against People with Mental Illness
- Suicide Prevention
- Technology Addictions: Social Media, Online Gaming, and More
- Warning Signs of Mental Illness
- Electroconvulsive Therapy (ECT)
- What is Mental Illness?
- What is Psychotherapy?
- What is Telepsychiatry?
- La Salud Mental
- Childhood Disorders: Medication Guides for Parents
- Lifestyle to Support Mental Health
- Member Benefits
- Honorary Fellowship (FAPA & DFAPA)
- Awards & Leadership Opportunities
- Get Involved
- Directories, Contact Info & FAQs
- District Branches
- APA's Vision, Mission, Values, and Goals
- Meet Our Organization
- Read APA Organization Documents and Policies
- Work At APA
- About APA's Headquarters
- Policy Finder
- News Releases
- Messages from the APA President
- Reporting on Mental Health Conditions
- Goldwater Rule
- Annual Meeting Press Registration + Guidelines
- APA Public Opinion Polls
- Reporter Toolkit: Recommendations on Covering the AAPI Community
- Comunicados de prensa en español
- APA Annual Meeting
- APA Communities
- APA Foundation
- APA JobCentral
- APA Learning Center
- APA Publishing
- Center for Workplace Mental Health
- Melvin Sabshin, M.D. Library & Archives
- Psychiatric News
- Psychiatry Online
- Annual Meeting
- APA On Demand
- At the APA Educational Series
- Books and Journals
- Certification and Licensure
- Diversity and Health Equity Education Resources
- Meeting Submission and Guidelines
- Mental Health Innovation Zone
- The Mental Health Services Conference
- The Virtual Immersive
- Virtual Paid Courses
- Clinical Practice Guidelines
- Covid-19 / Coronavirus
- Digital Mental Health
- Helping Patients Access Care
- Media and Communications
- Mental Health Apps
- Mental Health Parity
- Practice Management
- Professional Interests
- Quality Improvement
- Risk Management
- Social Media
- Sunshine Act
- Telepsychiatry
- The Clozapine Risk Evaluation and Mitigation Strategy (REMS) Program
- Transition to Practice and Early Career Resources
- Well-being and Burnout
- Mental Health and Faith Community Partnership
- Mental Health Equity Looking Beyond Series
- Minority and Underrepresented (M/UR) Caucuses
- Moore Equity in Mental Health Initiative
- News and Updates
- Striving for Excellence Series
- AMNet: Addiction Medicine Practice Based Research Network
- PsychPRO: APA's Mental Health Registry
- Research Colloquium for Junior Psychiatrist Investigators
- Perinatal Mental Health Toolkit
- Psychiatric Bed Crisis Report
- Advocacy Action Center
- Congressional Advocacy Network
- Election Resource Center
- Federal Affairs
- State Affairs
- Implementing 9-8-8
- Advocacy Update Webinars
- 2025 Annual Meeting
- The 2024 Mental Health Services Conference
- Addressing Structural Racism Town Hall Series
- APA Meetings App
- Governance Meetings
- Mental Health Equity Fireside Chat Series
- Moore Equity in Mental Health 5K
- Policy & Practice Insights Series
- September Component Meetings
- Social Determinants of Mental Health Town Hall Series
- Amicus Briefs
- Assembly Directory
- Component Directory
- Conference Publications
- Library and Archive
- Member Directory
- Member Obituaries
- Practice Guidelines
- Resource Documents
- International Trainees
- International Humanitarian Opportunities
- Global Mental Health
- International Medical Graduates Resources
- Residents' Journal
- Featured Publications
- APAF Fellowships
- External Fellowships and Awards
- Helping Residents Cope with a Patient Suicide
- Vacant Resident Positions
- Leadership Positions
- SET for Success
- Apply for Psychiatric Residency
- Choosing a Career in Psychiatry
- Building a Career in Psychiatry
- Medical Student Programs
- Resident-Fellow Census
- Transitioning to Residency During COVID-19
- What Is a Substance Use Disorder?
- Expert Q&A: Addiction and Substance Use Disorders
- What Are Dementia and Alzheimer’s Disease?
- Expert Q&A: Dementia and Alzheimer's Disease
- What are Anxiety Disorders?
- Expert Q&A: Anxiety Disorders
- What is ADHD?
- Expert Q&A: ADHD
- What Is Autism Spectrum Disorder?
- Expert Q&A: Autism Spectrum Disorder
- What Are Bipolar Disorders?
- Expert Q&A: Bipolar Disorder
- How Extreme Weather Events Affect Mental Health
- Who Is Affected by Climate Change?
- What Is Depression?
- Expert Q&A: Depression
- What are Disruptive, Impulse Control and Conduct Disorders?
- Expert Q&A: Disruptive, Impulse Control and Conduct Disorders
- What Are Dissociative Disorders?
- Expert Q&A: Dissociative Disorders
- What are Eating Disorders?
- Expert Q&A: Eating Disorders
- What is Gambling Disorder?
- Expert Q&A: Gambling Disorder
- What is Gender Dysphoria?
- Expert Q&A: Gender Dysphoria
- What is Hoarding Disorder?
- Expert Q&A: Hoarding Disorder
- What is Intellectual Disability?
- Expert Q&A: Intellectual Disability
- What Is Obsessive-Compulsive Disorder?
- Expert Q&A: Obsessive-Compulsive Disorder
- What is Perinatal Depression (formerly Postpartum)?
- Expert Q&A: Perinatal Depression
- What are Personality Disorders?
- Expert Q&A: Personality Disorders
- What is Posttraumatic Stress Disorder (PTSD)?
- Expert Q&A: Posttraumatic Stress Disorder (PTSD)
- Expert Q&A: Schizophrenia
- What are Sleep Disorders?
- Expert Q&A: Sleep Disorders
- What is Somatic Symptom Disorder?
- Expert Q&A: Somatic Symptom Disorder
- What Are Specific Learning Disorders?
- Expert Q&A: Specific Learning Disorders
- What is Technology Addiction?
- Expert Q&A: Technology Addiction
- Cigarrillos electrónicos y vapeo
- Trastorno del espectro autista
- Trastorno por consumo de alcohol
- Trastorno por consumo de opioides
- Trastorno de estrés postraumático (TEPT)
- Adicción a la tecnología: redes sociales, juegos en línea, y más
- ¿Qué es la psiquiatría?
- Conexiones entre el cambio climático y la salud mental
- Más temas de salud mental
- General Members
- Early Career Psychiatrists
- Residents and Fellows
- International Resident-Fellows
- Semi-Retired and Retired
- View Your Profile
- Resident-Fellow Members
- Fellow of the APA
- Distinguished Fellow of the APA
- International Fellow of the APA
- International Distinguished Fellow of the APA
- 2024 Class of Honorary Fellows
- 2025 APA National Elections
- Councils, Committees and Components
- Resident-Fellow Leadership Opportunities
- Advocacy and APAPAC
- APA/APAF Fellowships
- APA Insider Sessions
- APA Specialty Interest Caucuses, Listservs & Communities
- Leadership, Equity and Diversity Institute
- Mentorship Program for APA/APAF Fellows
- Research Colloquium
- Contact Your Membership Specialist
- Contact Your District Branch
- Membership FAQs
- Semi-Retired and Retired FAQs
- Lump Sum Dues
- 2025 APA Dues Rate Changes FAQs
- District Branch Resources
- District Branch Dues for General Members
- District Branch Dues for Residents and Fellows

Schizophrenia Clinical Presentation
- Author: Frances R Frankenburg, MD; Chief Editor: Glen L Xiong, MD more...
- Sections Schizophrenia
- Practice Essentials
- Pathophysiology
- Epidemiology
- Patient Education
- Physical Examination
- Complications
- Approach Considerations
- Antipsychotic Pharmacotherapy
- Other Pharmacotherapy
- Psychosocial Interventions
- Diet and Activity
- Other Treatments
- Medication Summary
- Antipsychotics, 1st Generation
- Antipsychotics, 2nd Generation
- Serotonin-Dopamine Activity Modulators
- Questions & Answers
- Media Gallery
Information about the medical and psychiatric history of the family, details about pregnancy and early childhood, history of travel, and history of medications and substance abuse are all important. This information is helpful in ruling out other causes of psychotic symptoms.
The patient usually had an unexceptional childhood. In retrospect, family members may describe the person with schizophrenia as a physically clumsy and emotionally aloof child. The child may have been anxious and preferred to play by himself or herself. The child may have been late to learn to walk and may have been a bed wetter. [ 60 , 61 ]
A noticeable change in personality and a decrease in academic, social, and interpersonal functioning often begin during middle-to-late adolescence. Usually, 1–2 years pass between the onset of these vague symptoms and the first visit to a psychiatrist. [ 62 ] The first psychotic episode usually occurs between the late teenage years and the mid 30s.
The symptoms of schizophrenia may be divided into the following 4 domains:
Positive symptoms - Psychotic symptoms, such as hallucinations, which are usually auditory; delusions; and disorganized speech and behavior
Negative symptoms - A decrease in emotional range, poverty of speech, and loss of interests and drive; the person with schizophrenia has tremendous inertia
Cognitive symptoms - Neurocognitive deficits (eg, deficits in working memory and attention and in executive functions, such as the ability to organize and abstract); patients also find it difficult to understand nuances and subtleties of interpersonal cues and relationships
Mood symptoms - Patients often seem cheerful or sad in a way that is difficult to understand; they often are depressed
The findings from a general physical examination are usually noncontributory. This examination is necessary to rule out other illnesses.
It is sometimes helpful to perform a neurologic examination as a baseline before initiating antipsychotic medications, because these drugs themselves can cause some neurological signs. Some patients with schizophrenia have motor disturbances before exposure to antipsychotic agents. Schizophrenia has been associated with left and mixed handedness, minor physical anomalies, and soft neurologic signs.
Mental status examination
On a detailed mental status examination (MSE), the following observations may be made in a severely ill patient with schizophrenia:
The patient may be unduly suspicious of the examiner or be socially awkward
The patient may express a variety of odd beliefs or delusions
The patient often has a flat affect (ie, little range of expressed emotion)
The patient may admit to hallucinations or respond to auditory or visual stimuli that are not apparent to the examiner
The patient may show thought blocking, in which long pauses occur before he or she answers a question
The patient’s speech may be difficult to follow because of the looseness of his or her associations; the sequence of thoughts follows a logic that is clear to the patient but not to the interviewer
The patient has difficulty with abstract thinking, demonstrated by inability to understand common proverbs or idiosyncratic interpretation of them
The speech may be circumstantial (ie, the patient takes a long time and uses many words in answering a question) or tangential (ie, the patient speaks at length but never actually answers the question)
The patient’s thoughts may be disorganized, stereotyped, or perseverative
The patient may make odd movements (which may elated to neuroleptic medication)
The patient may have little insight into his or her problems (ie, anosognosia)
Orientation is usually intact (ie, patients know who and where they are and what time it is)
Persons with schizophrenia may display strange and poorly understood behaviors. These include drinking water to the point of intoxication, staring at themselves in the mirror, performing stereotyped activities, hoarding useless objects, and mutilating themselves. Their wake-sleep cycle may be disturbed.
Substance abuse
Alcohol and drug abuse (especially nicotine) are common in schizophrenia, for reasons that are not entirely clear. For some people, these drugs provide relief from symptoms of the illness or the adverse effects of antipsychotic drugs, and the drive for this relief is strong enough to allow even patients who are impoverished and disorganized to find substances to abuse. [ 63 ]
Comorbid substance abuse occurs in 20–70% of patients with schizophrenia, particularly younger male patients, and is associated with increased hostility, crime, violence, suicidality, noncompliance with medication, homelessness, poor nutrition, and poverty. Drug use and abuse can also increase symptoms. For example, cannabis use has been shown to be associated with an earlier onset of psychosis and to correlate, in a bidirectional way, with an adverse course of psychotic symptoms in persons with schizophrenia. That is, people with more severe psychotic symptoms are more likely to use cannabis, and cannabis, in turn, seems to worsen psychotic symptoms. [ 64 ] However, other research has shown that the use of cannabis is associated with better cognitive functioning. [ 65 ]
A register-based study of more than 3000 inpatients from Scotland who experienced substance-induced psychoses showed that episodes of psychosis induced from several types of illicit substances are significantly linked to a later clinical diagnosis of schizophrenia. [ 66 ]
Patients who abuse substances may fare better in dual-diagnosis treatment programs, in which principles from the mental health field can be integrated with principles from the chemical dependency field.
Many patients with schizophrenia report symptoms of depression. It is unclear whether such depression is an independent problem, part of the schizophrenia, a reaction to the schizophrenia, or a complication of treatment. Addressing this issue is important because of the high rate of suicide in patients with schizophrenia.
The research evidence for the use of antidepressant agents in schizophrenic patients is mixed. Further complicating the situation are the findings that antipsychotic agents may have antidepressant properties. [ 67 ] One meta-analysis suggested that the addition of antidepressants to antipsychotics might help treat the negative symptoms of chronic schizophrenia, which can be difficult to distinguish from depression. [ 68 ]
Suicide attempts are lower in people treated with clozapine than with other antipsychotic agents. [ 69 ]
Many patients with schizophrenia report symptoms of anxiety. It is unclear whether such anxiety is an independent problem, part of the schizophrenia, a reaction to the schizophrenia, or a complication of treatment. Some adverse effects of medications, such as akathisia, may be experienced as anxiety. Anxiety may precede the onset of schizophrenia by several years. [ 70 ]
Treatment is keyed to the source of the anxiety. Antipsychotics usually relieve anxiety that is part of an acute psychotic episode; only limited data are available on treatment of comorbid anxiety disorders. Following treatment recommendations for primary anxiety disorder would be reasonable in many cases; however, fluvoxamine and other selective serotonin reuptake inhibitors (SSRIs) should be used cautiously in patients receiving clozapine; they can raise clozapine blood levels. Benzodiazepines may be helpful but carry their own risks. [ 71 , 72 ]
Obsessive-compulsive symptoms
A number of patients with schizophrenia display obsessive-compulsive symptoms, such as the need to check, count, or repeat certain activities. As is similar to anxiety or depression, the connection between these symptoms and schizophrenia is not understood. Obsessive-compulsive symptoms are a known adverse effect of some antipsychotic medications, particularly clozapine. Patients with schizophrenia and obsessive-compulsive symptoms tend to do more poorly. There is no clear consensus on how to treat the obsessive-compulsive symptoms.
Most people with schizophrenia are not violent. However, a few may act violently, sometimes as a result of command hallucinations or delusions. [ 68 ] Because the violent acts carried out by these few patients may be unpredictable and bizarre, they are often highly publicized, and the intense publicity has the unfortunate consequence of exacerbating the stigma of the disease.
Violence may be associated with substance abuse. However, the rate of violence in patients with schizophrenia who do not abuse substances is higher than that in people without schizophrenia. [ 73 , 74 ] Clozapine is sometimes recommended for treatment of patients with schizophrenia who are violent.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision . Washington, DC: American Psychiatric Association; 2022.
Wright IC, Rabe-Hesketh S, Woodruff PW, et al. Meta-analysis of regional brain volumes in schizophrenia. Am J Psychiatry . 2000 Jan. 157(1):16-25. [QxMD MEDLINE Link] .
Tamminga CA, Stan AD, Wagner AD. The hippocampal formation in schizophrenia. Am J Psychiatry . 2010 Oct. 167(10):1178-93. [QxMD MEDLINE Link] .
Mattai A, Hosanagar A, Weisinger B, Greenstein D, Stidd R, Clasen L. Hippocampal volume development in healthy siblings of childhood-onset schizophrenia patients. Am J Psychiatry . 2011 Apr. 168(4):427-35. [QxMD MEDLINE Link] .
Sigmundsson T, Suckling J, Maier M, et al. Structural abnormalities in frontal, temporal, and limbic regions and interconnecting white matter tracts in schizophrenic patients with prominent negative symptoms. Am J Psychiatry . 2001 Feb. 158(2):234-43. [QxMD MEDLINE Link] .
Ellison-Wright I, Bullmore E. Meta-analysis of diffusion tensor imaging studies in schizophrenia. Schizophr Res . 2009 Mar. 108(1-3):3-10. [QxMD MEDLINE Link] .
McIntosh AM, Owens DC, Moorhead WJ, Whalley HC, Stanfield AC, Hall J, et al. Longitudinal volume reductions in people at high genetic risk of schizophrenia as they develop psychosis. Biol Psychiatry . 2011 May 15. 69(10):953-8. [QxMD MEDLINE Link] .
Olabi B, Ellison-Wright I, McIntosh AM, et al. Are there progressive brain changes in schizophrenia? A meta-analysis of structural magnetic resonance imaging studies. Biol Psychiatry . 2011 Jul 1. 70(1):88-96. [QxMD MEDLINE Link] .
Coyle JT. The glutamatergic dysfunction hypothesis for schizophrenia. Harv Rev Psychiatry . 1996 Jan-Feb. 3(5):241-53. [QxMD MEDLINE Link] .
Cioffi CL. Modulation of NMDA receptor function as a treatment for schizophrenia. Bioorg Med Chem Lett . 2013 Jul 19. [QxMD MEDLINE Link] .
Drexhage RC, Weigelt K, van Beveren N, Cohen D, Versnel MA, Nolen WA, et al. Immune and neuroimmune alterations in mood disorders and schizophrenia. Int Rev Neurobiol . 2011. 101:169-201. [QxMD MEDLINE Link] .
Fan X, Goff DC, Henderson DC. Inflammation and schizophrenia. Expert Rev Neurother . 2007 Jul. 7(7):789-96. [QxMD MEDLINE Link] .
Selten JP, Cantor-Graae E, Kahn RS. Migration and schizophrenia. Curr Opin Psychiatry . 2007 Mar. 20(2):111-5. [QxMD MEDLINE Link] .
Bourque F, van der Ven E, Malla A. A meta-analysis of the risk for psychotic disorders among first- and second-generation immigrants. Psychol Med . 2011 May. 41(5):897-910. [QxMD MEDLINE Link] .
Kirkbride J, Coid JW, Morgan C, et al. Translating the epidemiology of psychosis into public mental health: evidence, challenges and future prospects. J Public Ment Health . 2010 Jun. 9(2):4-14. [QxMD MEDLINE Link] .
Kety SS, Wender PH, Jacobsen B, et al. Mental illness in the biological and adoptive relatives of schizophrenic adoptees. Replication of the Copenhagen Study in the rest of Denmark. Arch Gen Psychiatry . 1994 Jun. 51(6):442-55. [QxMD MEDLINE Link] .
Cheng W, Frei O, van der Meer D, Wang Y, O'Connell KS, Chu Y, et al. Genetic Association Between Schizophrenia and Cortical Brain Surface Area and Thickness. JAMA Psychiatry . 2021 Jun 23. [QxMD MEDLINE Link] .
Brooks M. New Schizophrenia Genes Identified. Medscape Medical News . Jul 22 2014. [Full Text] .
Biological insights from 108 schizophrenia-associated genetic loci. Nature . 2014 Jul 24. 511(7510):421-7. [QxMD MEDLINE Link] .
Caspi A, Moffitt TE, Cannon M, et al. Moderation of the effect of adolescent-onset cannabis use on adult psychosis by a functional polymorphism in the catechol-O-methyltransferase gene: longitudinal evidence of a gene X environment interaction. Biol Psychiatry . 2005 May 15. 57(10):1117-27. [QxMD MEDLINE Link] .
Shifman S, Johannesson M, Bronstein M, et al. Genome-wide association identifies a common variant in the reelin gene that increases the risk of schizophrenia only in women. PLoS Genet . 2008 Feb. 4(2):e28. [QxMD MEDLINE Link] .
Wratten NS, Memoli H, Huang Y, Dulencin AM, Matteson PG, Cornacchia MA, et al. Identification of a schizophrenia-associated functional noncoding variant in NOS1AP. Am J Psychiatry . April/2009. 166:434-41. [QxMD MEDLINE Link] .
O'Brien NL, Way MJ, Kandaswamy R, et al. The functional GRM3 Kozak sequence variant rs148754219 affects the risk of schizophrenia and alcohol dependence as well as bipolar disorder. Psychiatr Genet . 2014 Jul 18. [QxMD MEDLINE Link] .
Bassett AS, Costain G, Fung WL, Russell KJ, Pierce L, Kapadia R, et al. Clinically detectable copy number variations in a Canadian catchment population of schizophrenia. J Psychiatr Res . 2010 Nov. 44(15):1005-9. [QxMD MEDLINE Link] .
Bassett AS, Scherer SW, Brzustowicz LM. Copy number variations in schizophrenia: critical review and new perspectives on concepts of genetics and disease. Am J Psychiatry . 2010 Aug. 167(8):899-914. [QxMD MEDLINE Link] . [Full Text] .
Owen MJ, O'Donovan MC, Thapar A, Craddock N. Neurodevelopmental hypothesis of schizophrenia. Br J Psychiatry . 2011 Mar. 198:173-5. [QxMD MEDLINE Link] .
Sahoo T, Theisen A, Rosenfeld JA, et al. Copy number variants of schizophrenia susceptibility loci are associated with a spectrum of speech and developmental delays and behavior problems. Genet Med . 2011 Oct. 13(10):868-80. [QxMD MEDLINE Link] .
Corvin AP, Morris DW, McGhee K, Schwaiger S, Scully P, Quinn J, et al. Confirmation and refinement of an 'at-risk' haplotype for schizophrenia suggests the EST cluster, Hs.97362, as a potential susceptibility gene at the Neuregulin-1 locus. Mol Psychiatry . 2004 Feb. 9(2):208-13. [QxMD MEDLINE Link] .
Ekelund J, Hennah W, Hiekkalinna T, Parker A, Meyer J, Lönnqvist J, et al. Replication of 1q42 linkage in Finnish schizophrenia pedigrees. Mol Psychiatry . 2004 Nov. 9(11):1037-41. [QxMD MEDLINE Link] .
Hennah W, Thomson P, McQuillin A, Bass N, Loukola A, Anjorin A, et al. DISC1 association, heterogeneity and interplay in schizophrenia and bipolar disorder. Mol Psychiatry . 2009 Sep. 14(9):865-73. [QxMD MEDLINE Link] .
Huffaker SJ, Chen J, Nicodemus KK, Sambataro F, Yang F, Mattay V, et al. A primate-specific, brain isoform of KCNH2 affects cortical physiology, cognition, neuronal repolarization and risk of schizophrenia. Nat Med . 2009 May. 15(5):509-18. [QxMD MEDLINE Link] . [Full Text] .
Kirov G, Ivanov D, Williams NM, Preece A, Nikolov I, Milev R, et al. Strong evidence for association between the dystrobrevin binding protein 1 gene (DTNBP1) and schizophrenia in 488 parent-offspring trios from Bulgaria. Biol Psychiatry . 2004 May 15. 55(10):971-5. [QxMD MEDLINE Link] .
Mirnics K, Middleton FA, Stanwood GD, Lewis DA, Levitt P. Disease-specific changes in regulator of G-protein signaling 4 (RGS4) expression in schizophrenia. Mol Psychiatry . 2001 May. 6(3):293-301. [QxMD MEDLINE Link] .
Morris DW, Rodgers A, McGhee KA, Schwaiger S, Scully P, Quinn J, et al. Confirming RGS4 as a susceptibility gene for schizophrenia. Am J Med Genet B Neuropsychiatr Genet . 2004 Feb 15. 125B(1):50-3. [QxMD MEDLINE Link] .
Schindler KM, Pato MT, Dourado A, Macedo A, Azevedo MH, Kennedy JL, et al. Association and linkage disequilibrium between a functional polymorphism of the dopamine-2 receptor gene and schizophrenia in a genetically homogeneous Portuguese population. Mol Psychiatry . 2002. 7(9):1002-5. [QxMD MEDLINE Link] .
Shifman S, Bronstein M, Sternfeld M, Pisanté-Shalom A, Lev-Lehman E, Weizman A, et al. A highly significant association between a COMT haplotype and schizophrenia. Am J Hum Genet . 2002 Dec. 71(6):1296-302. [QxMD MEDLINE Link] . [Full Text] .
Stefansson H, Sarginson J, Kong A, et al. Association of neuregulin 1 with schizophrenia confirmed in a Scottish population. Am J Hum Genet . 2003 Jan. 72(1):83-7. [QxMD MEDLINE Link] . [Full Text] .
Steinberg S, Mors O, Børglum AD, Gustafsson O, Werge T, Mortensen PB, et al. Expanding the range of ZNF804A variants conferring risk of psychosis. Mol Psychiatry . 2011 Jan. 16(1):59-66. [QxMD MEDLINE Link] . [Full Text] .
Tang JX, Chen WY, He G, Zhou J, Gu NF, Feng GY, et al. Polymorphisms within 5' end of the Neuregulin 1 gene are genetically associated with schizophrenia in the Chinese population. Mol Psychiatry . 2004 Jan. 9(1):11-2. [QxMD MEDLINE Link] .
Williams HJ, Norton N, Dwyer S, Moskvina V, Nikolov I, Carroll L, et al. Fine mapping of ZNF804A and genome-wide significant evidence for its involvement in schizophrenia and bipolar disorder. Mol Psychiatry . 2011 Apr. 16(4):429-41. [QxMD MEDLINE Link] .
Xu B, Roos JL, Dexheimer P, et al. Exome sequencing supports a de novo mutational paradigm for schizophrenia. Nat Genet . 2011 Aug 7. 43(9):864-8. [QxMD MEDLINE Link] .
Girard SL, Gauthier J, Noreau A, et al. Increased exonic de novo mutation rate in individuals with schizophrenia. Nat Genet . 2011 Jul 10. 43(9):860-3. [QxMD MEDLINE Link] .
Brooks M. De Novo Gene Mutations Linked to Schizophrenia. Medscape Medical News. Available at https://www.medscape.com/viewarticle/819742. . Accessed: February 4, 2014.
Fromer M, Pocklington AJ, Kavanagh DH, Williams HJ, Dwyer S, Gormley P, et al. De novo mutations in schizophrenia implicate synaptic networks. Nature . 2014 Jan 22. [QxMD MEDLINE Link] .
Ripke S, O'Dushlaine C, Chambert K, et al. Genome-wide association analysis identifies 13 new risk loci for schizophrenia. Nat Genet . 2013 Oct. 45(10):1150-9. [QxMD MEDLINE Link] . [Full Text] .
Lencz T, Guha S, Liu C, Rosenfeld J, Mukherjee S, Derosse P. Genome-wide association study implicates NDST3 in schizophrenia and bipolar disorder. Nat Commun . 2013 Nov 19. 4:2739. [QxMD MEDLINE Link] .
Sullivan PF, Kendler KS, Neale MC. Schizophrenia as a complex trait: evidence from a meta-analysis of twin studies. Arch Gen Psychiatry . 2003 Dec. 60(12):1187-92. [QxMD MEDLINE Link] .
Brown AS, Derkits EJ. Prenatal infection and schizophrenia: a review of epidemiologic and translational studies. Am J Psychiatry . 2010 Mar. 167(3):261-80. [QxMD MEDLINE Link] .
Brown AS, Begg MD, Gravenstein S, Schaefer CA, Wyatt RJ, Bresnahan M, et al. Serologic evidence of prenatal influenza in the etiology of schizophrenia. Arch Gen Psychiatry . 2004 Aug. 61 (8):774-80. [QxMD MEDLINE Link] .
Torrey EF, Bowler AE, Rawlings R, Terrazas A. Seasonality of schizophrenia and stillbirths. Schizophr Bull . 1993. 19(3):557-62. [QxMD MEDLINE Link] .
Clarke MC, Tanskanen A, Huttunen M, Whittaker JC, Cannon M. Evidence for an interaction between familial liability and prenatal exposure to infection in the causation of schizophrenia. Am J Psychiatry . 2009 Sep. 166(9):1025-30. [QxMD MEDLINE Link] .
Anderson P. Teen Marijuana Use Linked to Earlier Psychosis Onset. Medscape Medical News . May 14 2014. [Full Text] .
Bhugra D. The global prevalence of schizophrenia. PLoS Med . 2005 May. 2(5):e151; quiz e175. [QxMD MEDLINE Link] . [Full Text] .
Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of schizophrenia. PLoS Med . 2005 May. 2(5):e141. [QxMD MEDLINE Link] . [Full Text] .
Haro JM, Novick D, Bertsch J, et al. Cross-national clinical and functional remission rates: Worldwide Schizophrenia Outpatient Health Outcomes (W-SOHO) study. Br J Psychiatry . 2011 Sep. 199:194-201. [QxMD MEDLINE Link] .
Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol . 2010 Nov. 24(4 Suppl):81-90. [QxMD MEDLINE Link] . [Full Text] .
Hoang U, Stewart R, Goldacre MJ. Mortality after hospital discharge for people with schizophrenia or bipolar disorder: retrospective study of linked English hospital episode statistics, 1999-2006. BMJ . 2011 Sep 13. 343:d5422. [QxMD MEDLINE Link] . [Full Text] .
Zhuo C and Triplett PT. Association of Schizophrenia With the Risk of Breast Cancer Incidence. JAMA Psychiatry . March 7, 2018. [Full Text] .
Xia J, Merinder LB, Belgamwar MR. Psychoeducation for schizophrenia. Cochrane Database Syst Rev . 2011 Jun 15. CD002831. [QxMD MEDLINE Link] .
Hyde TM, Deep-Soboslay A, Iglesias B, et al. Enuresis as a premorbid developmental marker of schizophrenia. Brain . 2008 Sep. 131:2489-98. [QxMD MEDLINE Link] . [Full Text] .
Jones P, Rodgers B, Murray R, Marmot M. Child development risk factors for adult schizophrenia in the British 1946 birth cohort. Lancet . 1994 Nov 19. 344(8934):1398-402. [QxMD MEDLINE Link] .
Ho BC, Andreasen NC. Long delays in seeking treatment for schizophrenia. Lancet . 2001 Mar 24. 357(9260):898-900. [QxMD MEDLINE Link] .
Green AI, Drake RE, Brunette MF, Noordsy DL. Schizophrenia and co-occurring substance use disorder. Am J Psychiatry . 2007 Mar. 164(3):402-8. [QxMD MEDLINE Link] .
Foti DJ, Kotov R, Guey LT, Bromet EJ. Cannabis use and the course of schizophrenia: 10-year follow-up after first hospitalization. Am J Psychiatry . 2010 Aug. 167(8):987-93. [QxMD MEDLINE Link] .
Yücel M, Bora E, Lubman DI, et al. The impact of cannabis use on cognitive functioning in patients with schizophrenia: a meta-analysis of existing findings and new data in a first-episode sample. Schizophr Bull . 2012 Mar. 38(2):316-30. [QxMD MEDLINE Link] . [Full Text] .
Brauser D. Cannabis Not the Only Illicit Drug Linked to Schizophrenia. Medscape Medical News. Available at https://www.medscape.com/viewarticle/807520 . Accessed: July 17, 2013.
Robertson MM, Trimble MR. Major tranquillisers used as antidepressants. A review. J Affect Disord . 1982 Sep. 4(3):173-93. [QxMD MEDLINE Link] .
Singh SP, Singh V, Kar N, Chan K. Efficacy of antidepressants in treating the negative symptoms of chronic schizophrenia: meta-analysis. Br J Psychiatry . 2010 Sep. 197(3):174-9. [QxMD MEDLINE Link] .
Meltzer HY, Alphs L, Green AI, et al. Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT). Arch Gen Psychiatry . 2003 Jan. 60(1):82-91. [QxMD MEDLINE Link] .
Shioiri T, Shinada K, Kuwabara H, Someya T. Early prodromal symptoms and diagnoses before first psychotic episode in 219 inpatients with schizophrenia. Psychiatry Clin Neurosci . 2007 Aug. 61(4):348-54. [QxMD MEDLINE Link] .
Kripke DF, Langer RD, Kline LE. Hypnotics' association with mortality or cancer: a matched cohort study. BMJ Open . 2012. 2(1):e000850. [QxMD MEDLINE Link] . [Full Text] .
Tiihonen J, Suokas JT, Suvisaari JM, Haukka J, Korhonen P. Polypharmacy with antipsychotics, antidepressants, or benzodiazepines and mortality in schizophrenia. Arch Gen Psychiatry . 2012 May. 69(5):476-83. [QxMD MEDLINE Link] .
Bennett DJ, Ogloff JR, Mullen PE, et al. Schizophrenia disorders, substance abuse and prior offending in a sequential series of 435 homicides. Acta Psychiatr Scand . 2011 Sep. 124(3):226-33. [QxMD MEDLINE Link] .
Fazel S, Långström N, Hjern A, Grann M, Lichtenstein P. Schizophrenia, substance abuse, and violent crime. JAMA . 2009 May 20. 301(19):2016-23. [QxMD MEDLINE Link] .
Cummings JL, Gosenfeld LF, Houlihan JP, McCaffrey T. Neuropsychiatric disturbances associated with idiopathic calcification of the basal ganglia. Biol Psychiatry . 1983 May. 18(5):591-601. [QxMD MEDLINE Link] .
Rosebush PI, MacQueen GM, Clarke JT, et al. Late-onset Tay-Sachs disease presenting as catatonic schizophrenia: diagnostic and treatment issues. J Clin Psychiatry . 1995 Aug. 56(8):347-53. [QxMD MEDLINE Link] .
Pope HG Jr, Katz DL. Psychiatric and medical effects of anabolic-androgenic steroid use. A controlled study of 160 athletes. Arch Gen Psychiatry . 1994 May. 51(5):375-82. [QxMD MEDLINE Link] .
Reuler JB, Girard DE, Cooney TG. Current concepts. Wernicke's encephalopathy. N Engl J Med . 1985 Apr 18. 312(16):1035-9. [QxMD MEDLINE Link] .
Salokangas RK. Medical problems in schizophrenia patients living in the community (alternative facilities). Curr Opin Psychiatry . 2007 Jul. 20(4):402-5. [QxMD MEDLINE Link] .
Pillinger T, Beck K, Gobjila C, Donocik JG, Jauhar S, Howes OD. Impaired Glucose Homeostasis in First-Episode Schizophrenia: A Systematic Review and Meta-analysis. JAMA Psychiatry . 2017 Jan 11. [QxMD MEDLINE Link] .
Brauser D. Long-term Injectable Drug Effective for Schizophrenia. Medscape Medical News . May 11 2012. [Full Text] .
Cassels C. FDA Approves Once-Monthly Treatment for Schizophrenia. Medscape Medical News . Mar 1 2013. [Full Text] .
Kane JM, Sanchez R, Perry PP, et al. Aripiprazole intramuscular depot as maintenance treatment in patients with schizophrenia: a 52-week, multicenter, randomized, double-blind, placebo-controlled study. J Clin Psychiatry . 2012 May. 73(5):617-24. [QxMD MEDLINE Link] . [Full Text] .
Citrome L. New second-generation long-acting injectable antipsychotics for the treatment of schizophrenia. Expert Rev Neurother . 2013 Jul. 13(7):767-83. [QxMD MEDLINE Link] .
Secuado (asenapine transdermal system) [package insert]. Japan Saga Tosu: Hisamitsu Pharmaceutical Co. Inc. October 2019. Available at [Full Text] .
Lieberman JA, Stroup TS. The NIMH-CATIE Schizophrenia Study: what did we learn?. Am J Psychiatry . 2011 Aug. 168(8):770-5. [QxMD MEDLINE Link] .
Jones PB, Barnes TR, Davies L, Dunn G, Lloyd H, Hayhurst KP, et al. Randomized controlled trial of the effect on Quality of Life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1). Arch Gen Psychiatry . 2006 Oct. 63(10):1079-87. [QxMD MEDLINE Link] .
Subotnik KL, Casaus LR, Ventura J, Luo JS, Hellemann GS, Gretchen-Doorly D, et al. Long-Acting Injectable Risperidone for Relapse Prevention and Control of Breakthrough Symptoms After a Recent First Episode of Schizophrenia : A Randomized Clinical Trial. JAMA Psychiatry . 2015 Jun 24. [QxMD MEDLINE Link] .
Kahn RS, Fleischhacker WW, Boter H, Davidson M, Vergouwe Y, Keet IP, et al. Effectiveness of antipsychotic drugs in first-episode schizophrenia and schizophreniform disorder: an open randomised clinical trial. Lancet . 2008 Mar 29. 371(9618):1085-97. [QxMD MEDLINE Link] .
McEvoy JP, Lieberman JA, Perkins DO, Hamer RM, Gu H, Lazarus A, et al. Efficacy and tolerability of olanzapine, quetiapine, and risperidone in the treatment of early psychosis: a randomized, double-blind 52-week comparison. Am J Psychiatry . 2007 Jul. 164(7):1050-60. [QxMD MEDLINE Link] .
[Guideline] Buchanan RW, Kreyenbuhl J, Kelly DL, Noel JM, Boggs DL, Fischer BA, et al. The 2009 schizophrenia PORT psychopharmacological treatment recommendations and summary statements. Schizophr Bull . 2010 Jan. 36(1):71-93. [QxMD MEDLINE Link] . [Full Text] .
Wunderink L, Nieboer RM, Wiersma D, Sytema S, Nienhuis FJ. Recovery in remitted first-episode psychosis at 7 years of follow-up of an early dose reduction/discontinuation or maintenance treatment strategy: long-term follow-up of a 2-year randomized clinical trial. JAMA Psychiatry . 2013 Sep. 70(9):913-20. [QxMD MEDLINE Link] .
Lieberman JA, Phillips M, Gu H, Stroup S, Zhang P, Kong L, et al. Atypical and conventional antipsychotic drugs in treatment-naive first-episode schizophrenia: a 52-week randomized trial of clozapine vs chlorpromazine. Neuropsychopharmacology . 2003 May. 28(5):995-1003. [QxMD MEDLINE Link] .
Woerner MG, Robinson DG, Alvir JM, Sheitman BB, Lieberman JA, Kane JM. Clozapine as a first treatment for schizophrenia. Am J Psychiatry . 2003 Aug. 160(8):1514-6. [QxMD MEDLINE Link] .
Moore TA, Buchanan RW, Buckley PF, Chiles JA, Conley RR, Crismon ML, et al. The Texas Medication Algorithm Project antipsychotic algorithm for schizophrenia: 2006 update. J Clin Psychiatry . 2007 Nov. 68(11):1751-62. [QxMD MEDLINE Link] .
Agid O, Arenovich T, Sajeev G, Zipursky RB, Kapur S, Foussias G, et al. An algorithm-based approach to first-episode schizophrenia: response rates over 3 prospective antipsychotic trials with a retrospective data analysis. J Clin Psychiatry . 2011 Nov. 72(11):1439-44. [QxMD MEDLINE Link] .
Essock SM, Schooler NR, Stroup TS, McEvoy JP, Rojas I, Jackson C, et al. Effectiveness of switching from antipsychotic polypharmacy to monotherapy. Am J Psychiatry . 2011 Jul. 168(7):702-8. [QxMD MEDLINE Link] .
Correll CU, Rummel-Kluge C, Corves C, Kane JM, Leucht S. Antipsychotic combinations vs monotherapy in schizophrenia: a meta-analysis of randomized controlled trials. Schizophr Bull . 2009 Mar. 35(2):443-57. [QxMD MEDLINE Link] . [Full Text] .
Honer WG, MacEwan GW, Gendron A, Stip E, Labelle A, Williams R, et al. A randomized, double-blind, placebo-controlled study of the safety and tolerability of high-dose quetiapine in patients with persistent symptoms of schizophrenia or schizoaffective disorder. J Clin Psychiatry . 2012 Jan. 73(1):13-20. [QxMD MEDLINE Link] .
Asmal L, Flegar SJ, Wang J, Rummel-Kluge C, Komossa K, Leucht S. Quetiapine versus other atypical antipsychotics for schizophrenia. Cochrane Database Syst Rev . 2013 Nov 18. 11:CD006625. [QxMD MEDLINE Link] .
Rosenheck RA, Krystal JH, Lew R, Barnett PG, Fiore L, Valley D, et al. Long-acting risperidone and oral antipsychotics in unstable schizophrenia. N Engl J Med . 2011 Mar 3. 364(9):842-51. [QxMD MEDLINE Link] .
Kishimoto T, Robenzadeh A, Leucht C, Leucht S, Watanabe K, Mimura M, et al. Long-Acting Injectable vs Oral Antipsychotics for Relapse Prevention in Schizophrenia: A Meta-Analysis of Randomized Trials. Schizophr Bull . 2013 Jan 2. [QxMD MEDLINE Link] .
Subotnik KL, Nuechterlein KH, Ventura J, et al. Risperidone nonadherence and return of positive symptoms in the early course of schizophrenia. Am J Psychiatry . 2011 Mar. 168(3):286-92. [QxMD MEDLINE Link] .
Takeuchi H, Suzuki T, Remington G, et al. Effects of risperidone and olanzapine dose reduction on cognitive function in stable patients with schizophrenia: an open-label, randomized, controlled, pilot study. Schizophr Bull . 2013 Sep. 39(5):993-8. [QxMD MEDLINE Link] . [Full Text] .
Glassman AH, Bigger JT Jr. Antipsychotic drugs: prolonged QTc interval, torsade de pointes, and sudden death. Am J Psychiatry . 2001 Nov. 158(11):1774-82. [QxMD MEDLINE Link] .
Strom BL, Eng SM, Faich G, Reynolds RF, D'Agostino RB, Ruskin J, et al. Comparative mortality associated with ziprasidone and olanzapine in real-world use among 18,154 patients with schizophrenia: The Ziprasidone Observational Study of Cardiac Outcomes (ZODIAC). Am J Psychiatry . 2011 Feb. 168(2):193-201. [QxMD MEDLINE Link] .
Vieweg WV. New Generation Antipsychotic Drugs and QTc Interval Prolongation. Prim Care Companion J Clin Psychiatry . 2003 Oct. 5(5):205-215. [QxMD MEDLINE Link] . [Full Text] .
Newcomer JW. Metabolic considerations in the use of antipsychotic medications: a review of recent evidence. J Clin Psychiatry . 2007. 68 Suppl 1:20-7. [QxMD MEDLINE Link] .
Kessing LV, Thomsen AF, Mogensen UB, Andersen PK. Treatment with antipsychotics and the risk of diabetes in clinical practice. Br J Psychiatry . 2010 Oct. 197(4):266-71. [QxMD MEDLINE Link] .
Stroup TS, McEvoy JP, Ring KD, Hamer RH, LaVange LM, Swartz MS, et al. A randomized trial examining the effectiveness of switching from olanzapine, quetiapine, or risperidone to aripiprazole to reduce metabolic risk: comparison of antipsychotics for metabolic problems (CAMP). Am J Psychiatry . 2011 Sep. 168(9):947-56. [QxMD MEDLINE Link] .
Correll CU, Newcomer JW, Silverman B, DiPetrillo L, Graham C, Jiang Y, et al. Effects of Olanzapine Combined With Samidorphan on Weight Gain in Schizophrenia: A 24-Week Phase 3 Study. Am J Psychiatry . 2020 Dec 1. 177 (12):1168-1178. [QxMD MEDLINE Link] .
Wang M, Tong JH, Zhu G, Liang GM, Yan HF, Wang XZ. Metformin for treatment of antipsychotic-induced weight gain: a randomized, placebo-controlled study. Schizophr Res . 2012 Jun. 138(1):54-7. [QxMD MEDLINE Link] .
Hägg S, Spigset O, Söderström TG. Association of venous thromboembolism and clozapine. Lancet . 2000 Apr 1. 355(9210):1155-6. [QxMD MEDLINE Link] .
Thomassen R, Vandenbroucke JP, Rosendaal FR. Antipsychotic drugs and venous thromboembolism. Lancet . 2000 Jul 15. 356(9225):252. [QxMD MEDLINE Link] .
Lowry F. Psychotropic Drugs Can Reduce Bone Mass in Kids. Medscape Medical News . Jun 24 2014. [Full Text] .
Ho BC, Andreasen NC, Ziebell S, Pierson R, Magnotta V. Long-term antipsychotic treatment and brain volumes: a longitudinal study of first-episode schizophrenia. Arch Gen Psychiatry . 2011 Feb. 68(2):128-37. [QxMD MEDLINE Link] .
Kern RS, Glynn SM, Horan WP, Marder SR. Psychosocial treatments to promote functional recovery in schizophrenia. Schizophr Bull . 2009 Mar. 35(2):347-61. [QxMD MEDLINE Link] . [Full Text] .
[Guideline] Dixon LB, Dickerson F, Bellack AS, Bennett M, Dickinson D, Goldberg RW, et al. The 2009 schizophrenia PORT psychosocial treatment recommendations and summary statements. Schizophr Bull . 2010 Jan. 36(1):48-70. [QxMD MEDLINE Link] . [Full Text] .
Guo X, Zhai J, Liu Z, Fang M, Wang B, Wang C, et al. Effect of antipsychotic medication alone vs combined with psychosocial intervention on outcomes of early-stage schizophrenia: A randomized, 1-year study. Arch Gen Psychiatry . 2010 Sep. 67(9):895-904. [QxMD MEDLINE Link] .
Wexler BE, Bell MD. Cognitive remediation and vocational rehabilitation for schizophrenia. Schizophr Bull . 2005 Oct. 31(4):931-41. [QxMD MEDLINE Link] .
Wykes T, Huddy V, Cellard C, McGurk SR, Czobor P. A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry . 2011 May. 168(5):472-85. [QxMD MEDLINE Link] .
Grant PM, Huh GA, Perivoliotis D, Stolar NM, Beck AT. Randomized trial to evaluate the efficacy of cognitive therapy for low-functioning patients with schizophrenia. Arch Gen Psychiatry . 2012 Feb. 69(2):121-7. [QxMD MEDLINE Link] .
Puig O, Penadés R, Baeza I, De la Serna E, Sánchez-Gistau V, Bernardo M, et al. Cognitive remediation therapy in adolescents with early-onset schizophrenia: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry . 2014 Aug. 53(8):859-68. [QxMD MEDLINE Link] .
Brooks, M. Cognitive Therapy a Viable Monotherapy for Schizophrenia?. Medscape Medical News. Available at https://www.medscape.com/viewarticle/820258 . Accessed: February 19, 2014.
Morrison, Anthony P., Turkington, D., Pyle, M., et al. Cognitive therapy for people with schizophrenia spectrum disorders not taking antipsychotic drugs: a single-blind randomised controlled trial. The Lancet . February 2014. [Full Text] .
Bond GR, Drake RE. Making the Case for IPS Supported Employment. Adm Policy Ment Health . 2012 Nov 17. [QxMD MEDLINE Link] .
McHugo GJ, Drake RE, Xie H, Bond GR. A 10-year study of steady employment and non-vocational outcomes among people with serious mental illness and co-occurring substance use disorders. Schizophr Res . 2012 Jul. 138(2-3):233-9. [QxMD MEDLINE Link] .
Pharoah F, Mari J, Rathbone J, Wong W. Family intervention for schizophrenia. Cochrane Database Syst Rev . 2010 Dec 8. CD000088. [QxMD MEDLINE Link] .
Mohammadi A, Sadighi G, Nazeri Astaneh A, Tajabadi-Ebrahimi M, Dejam T. Co-administration of probiotic and vitamin D significantly improves cognitive function in schizophrenic patients: A double-blinded randomized controlled trial. Neuropsychopharmacol Rep . 2024 Apr 10. [QxMD MEDLINE Link] .
Hegelstad WT, Larsen TK, Auestad B, Evensen J, Haahr U, Joa I, et al. Long-term follow-up of the TIPS early detection in psychosis study: effects on 10-year outcome. Am J Psychiatry . 2012 Apr. 169(4):374-80. [QxMD MEDLINE Link] .
Weiser M. Early intervention for schizophrenia: the risk-benefit ratio of antipsychotic treatment in the prodromal phase. Am J Psychiatry . 2011 Aug. 168(8):761-3. [QxMD MEDLINE Link] .
Bechdolf A, Wagner M, Ruhrmann S, Harrigan S, Putzfeld V, Pukrop R, et al. Preventing progression to first-episode psychosis in early initial prodromal states. Br J Psychiatry . 2012 Jan. 200(1):22-9. [QxMD MEDLINE Link] .
Rosenberg O, Gersner R, Klein LD, Kotler M, Zangen A, Dannon P. Deep transcranial magnetic stimulation add-on for the treatment of auditory hallucinations: a double-blind study. Ann Gen Psychiatry . 2012 May 6. 11:13. [QxMD MEDLINE Link] . [Full Text] .
Levkovitz Y, Rabany L, Harel EV, Zangen A. Deep transcranial magnetic stimulation add-on for treatment of negative symptoms and cognitive deficits of schizophrenia: a feasibility study. Int J Neuropsychopharmacol . 2011 Aug. 14(7):991-6. [QxMD MEDLINE Link] .
Keepers GA, Fochtmann LJ, Anzia JM, Benjamin S, Lyness JM, Mojtabai R, et al. The American Psychiatric Association Practice Guideline for the Treatment of Patients With Schizophrenia. Am J Psychiatry . 2020 Sep 1. 177 (9):868-872. [QxMD MEDLINE Link] .
Cassels, C. Antipsychotic Linked to Potentially Fatal Skin Reaction. Medscape Medical News. Available at https://www.medscape.com/viewarticle/836427 . Accessed: December 13, 2014.
Baldessarini RJ, Frankenburg FR. Clozapine. A novel antipsychotic agent. N Engl J Med . 1991 Mar 14. 324(11):746-54. [QxMD MEDLINE Link] .
Brauser D. Psychosocial Interventions May Help Nip Psychosis in the Bud. Medscape Medical News. Available at https://www.medscape.com/viewarticle/829526 . Accessed: August 9, 2014.
Correll CU, Robinson DG, Schooler NR, et al. Cardiometabolic Risk in Patients With First-Episode Schizophrenia Spectrum Disorders: Baseline Results From the RAISE-ETP Study. JAMA Psychiatry . Oct 8 2014.
Essali A, Al-Haj Haasan N, Li C, Rathbone J. Clozapine versus typical neuroleptic medication for schizophrenia. Cochrane Database Syst Rev . 2009 Jan 21. CD000059. [QxMD MEDLINE Link] .
Kane JM, Peters-Strickland T, Baker RA, Hertel P, Eramo A, Jin N, et al. Aripiprazole once-monthly in the acute treatment of schizophrenia: findings from a 12-week, randomized, double-blind, placebo-controlled study. J Clin Psychiatry . 2014 Nov. 75(11):1254-60. [QxMD MEDLINE Link] . [Full Text] .
Kane JM, Peters-Strickland T, Baker RA, Hertel P, Eramo A, Jin N, et al. Aripiprazole once-monthly in the acute treatment of schizophrenia: findings from a 12-week, randomized, double-blind, placebo-controlled study. J Clin Psychiatry . 2014 Nov. 75(11):1254-60. [QxMD MEDLINE Link] .
Keller DM. Parkinsonism a major mortality risk factor in schizophrenia. Medscape Medical News . March 5, 2014. [Full Text] .
Kwentus J, Riesenberg RA, Marandi M, Manning RA, Allen MH, Fishman RS, et al. Rapid acute treatment of agitation in patients with bipolar I disorder: a multicenter, randomized, placebo-controlled clinical trial with inhaled loxapine. Bipolar Disord . 2012 Feb. 14(1):31-40. [QxMD MEDLINE Link] .
Lesem MD, Tran-Johnson TK, Riesenberg RA, Feifel D, Allen MH, Fishman R, et al. Rapid acute treatment of agitation in individuals with schizophrenia: multicentre, randomised, placebo-controlled study of inhaled loxapine. Br J Psychiatry . 2011 Jan. 198(1):51-8. [QxMD MEDLINE Link] . [Full Text] .
Lowry F. Rapid Rise in Cardiometabolic Risk in Early Schizophrenia. Medscape Medical News . Oct 14 2014. [Full Text] .
Miklowitz DJ, O'Brien MP, Schlosser DA, Addington J, Candan KA, Marshall C, et al. Family-focused treatment for adolescents and young adults at high risk for psychosis: results of a randomized trial. J Am Acad Child Adolesc Psychiatry . 2014 Aug. 53(8):848-58. [QxMD MEDLINE Link] . [Full Text] .
Schoepf D, Uppal H, Potluri R, Heun R. Physical comorbidity and its relevance on mortality in schizophrenia: a naturalistic 12-year follow-up in general hospital admissions. Presented at: The 22nd European Congress of Psychiatry (EPA); March 3, 2014; Munich, Germany. Abstract FC07. Eur Arch Psychiatry Clin Neurosci . 2014 Feb. 264(1):3-28. [QxMD MEDLINE Link] . [Full Text] .
- Cortical activation patterns during verbal working memory maintenance. Healthy controls (A), patients with schizophrenia (B), and significantly different activation between groups (subtraction of SZ-CO) (C) are shown. The time series plots in the middle column show activation associated with true memory maintenance (red lines) relative to the baseline activities (blue line). Bright parts in the middle of each plot represent 1-volume (1.5 s) after onset, and offset of the maintenance phase (4.5 secs). All p-values are corrected with false discovery rate of q< 0.005. Image courtesy of Kim J, Matthews NL, and Park S. An event-related fMRI study of phonological verbal working memory in schizophrenia. PLoS One. 2010; 5(8): e12068.
- Cortical activation patterns during false memory trials. (A) False memory, baseline in controls (CO). (B) False memory, baseline in schizophrenia (SZ). (C) SZ – CO. All p-values are corrected with a false discovery rate of q< 0.005. The time course plots show false memory-related activities (yellow) and true memory-related activities (red) relative to the baseline (blue). Image courtesy of Kim J, Matthews NL, and Park S. An event-related fMRI study of phonological verbal working memory in schizophrenia. PLoS One. 2010; 5(8): e12068.
- Magnetic resonance imaging showing differences in brain ventricle size in twins. The twin on the right has schizophrenia, whereas the twin on the left does not. Image courtesy of Dr. Daniel Weinberger, Clinical Brain Disorders Branch, National Institutes of Health.

Contributor Information and Disclosures
Frances R Frankenburg, MD Professor, Department of Psychiatry, Boston University School of Medicine; Chief of Inpatient Psychiatry and Consulting Psychiatrist, Edith Nourse Rogers Memorial Veterans Administration Medical Center; Associate Psychiatrist, McLean Hospital Frances R Frankenburg, MD is a member of the following medical societies: Alpha Omega Alpha , American Psychiatric Association Disclosure: Nothing to disclose.
Glen L Xiong, MD Associate Clinical Professor, Department of Psychiatry and Behavioral Sciences, Department of Internal Medicine, University of California, Davis, School of Medicine; Medical Director, Sacramento County Mental Health Treatment Center Glen L Xiong, MD is a member of the following medical societies: AMDA - The Society for Post-Acute and Long-Term Care Medicine , American College of Physicians , American Psychiatric Association , Central California Psychiatric Society Disclosure: Serve(d) as a director, officer, partner, employee, advisor, consultant or trustee for: SafelyYou, Blue Cross Blue Shield<br/>book co-editor for: Wolter Kluwer, American Psychiatric Publishing Inc.
Ronald C Albucher, MD Chief Medical Officer, Westside Community Services; Consulting Staff, California Pacific Medical Center
Ronald C Albucher, MD is a member of the following medical societies: American Psychiatric Association
Disclosure: Nothing to disclose.
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Medscape Salary Employment
What would you like to print?
- Print this section
- Print the entire contents of
- Print the entire contents of article

- Schizophrenia
- Emergent Treatment of Schizophrenia
- Childhood-Onset Schizophrenia
- Fast Five Quiz: What Do You Know About Schizophrenia?
- Fast Five Quiz: Schizophrenia Comorbidities
- Trending Clinical Topic: Schizophrenia
- Paranoia and Hallucinations About Martians
- Gut Signature for Treatment-Resistant Schizophrenia?
- TMS Promising for Psychomotor Slowing in Schizophrenia
- Clozapine Underutilized in Black Patients With Schizophrenia

- Drug Interaction Checker
- Pill Identifier
- Calculators

- 2002805988-overviewDiseases & Conditions Diseases & Conditions Emergent Treatment of Schizophrenia
- 3D Brain Atlas
- Clinical Education Grants
- Alzheimer’s
- Schizophrenia
- Parkinson’s
Schizophrenia – Course, Natural History and Prognosis
This slide covers course, natural history and prognosis of Schizophrenia. Schizophrenia is a progressive and recurring disease characterized by multiple psychotic relapses.
This slide deck is schedules for update summer 2022 .
Schizophrenia is a progressive and recurring disease characterized by multiple psychotic relapses. This slide deck covers the course, natural history and prognosis of schizophrenia. Other slides discuss the key components of non-adherence in patients with schizophrenia, highlighting the value of a support system.
This slide deck has been developed in collaboration with the former Lundbeck International Neuroscience Foundation.
Index for slide deck
Course, natural history and prognosis, course of schizophrenia, schizophrenia is a heterogeneous disease with many dimensions, schizophrenia: a broad range of symptoms.
Source (slide): APA 2013, Pages 99–102; APA 2000, Page 299; Wilk et al. Neuropsychology 2005; 19 (6): 778–786, Page 778; NICE clinical guideline 178, Page 4.
Source (notes): APA 2013, Pages 99–102; APA 2000, Page 299–302; Wilk et al. Neuropsychology 2005; 19 (6): 778–786,…
Schizophrenia progression may lead to functional decline
Key message: Schizophrenia is a progressive and recurring disease characterized by multiple psychotic relapses. Following a relapse, patients often fail to recover to baseline health and this may lead to functional decline.
Background:
- The majority of patients with schiz…
Typical Course of Schizophrenia
Review as stated on slide.
Please note, this slide builds
Key message: Many patients experience symptoms that are not fully controlled with treatment, with social withdrawal and impoverished thought being the two most common negative symptoms, and disordered thought and bizarre behavior the two mos…
Symptoms that are not fully controlled are significantly associated with impaired global functioning
Key message: In a study of patients in remission, those with residual symptoms had significantly worse global functioning that those without residual symptoms.
- Patients (aged 18–65) in remission with and without residual symptoms were compared regarding psych…
Disorganization, a common residual symptom,1 is associated with impaired community functioning
Key message: Conceptual disorganization is a common residual symptom in patients with schizophrenia, and is a reliable predictor of several aspects of community functioning, as measured by the Life Skills Profile (which was specifically designed to assess constructs of re…
Positive symptoms of schizophrenia are inversely correlated with ability to function
Key message: Increase in positive symptoms is directly correlated with a reduction in functional capacity. The correlation between positive symptoms and depression is predictive of impairment in real-world performance measures (as measured by interpersonal skills, communi…
Primary negative symptoms of schizophrenia can impact domains of functioning directly1
Key message: Negative symptoms and cognitive deficits can cause patients functional impairment. Primary negative symptoms of schizophrenia can impact different domains of functioning directly, including interpersonal relations, use of common objects and activities, and in…
Take home points
Related content.
In this video Professor Christoph Correll discusses the challenges with available schizophrenia treatments & what clinicians should keep in mind when considering the emerging treatment options for schizophrenia.

The table summarizes the high-level clinical characteristics of the existing and newly emerging pharmacological treatments for schizophrenia with at least one positive placebo-controlled trial.

LDT=Laterodorsal tegmental nucleus; NAc = Nucleus Accumbens; SN = Substantia Nigra; VTA = Ventral Tegmental Area.
-300x169.jpg)
Permissions
Permissions for creative use of the resources from neurotorium.
Permission is granted to download images, slides and videos and use them in your own presentations, provided that copyright notices and the Neurotorium logo are not hidden or removed. For use in publications and on websites, proper attribution must be provided together with a link to Neurotorium.org
Your slides will download now. Do you want to get our latest information?
Sign up to our newsletter and receive news in your inbox. We send newsletters every 1-2 months.
You have been subscribed to our newsletter!
Share or print.
Share content with anyone.
Save to workspace
Select language.
We have detected that you are from “France”. You have the option of switching the language to French, if you would prefer that?.
This site uses cookies
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua.
Sign up for our newsletter
Fill in you information below and stay up to date with the latest content on Neurotorium.
We send newsletters every 1-2 months, keeping you up to date with our latest educational content. You will receive a welcome e-mail immediately after you sign up for our newsletter. If you do not receive an e-mail, please check your spam folder. Contact support at [email protected] if you require help.
Welcome back
Please enter your details below.
- Schizophrenia
- Schizophrenia in Teens
- Schizophrenia in Children
- Overview of Symptoms
- Positive Symptoms
- Negative Symptoms
- Tests & Diagnosis
- Overview of Treatment
- Drug Therapies
- Medication Side Effects
- Medication Compliance
- Complementary & Alternative Therapies
- Hospitalization
- Complications
- Diet & Exercise
- Family & Relationships
- View Full Guide
A Visual Guide to Schizophrenia

What Is Schizophrenia?
It’s a serious mental illness that can be disabling without care. About 1% of Americans have it. People with the condition may hear voices, see imaginary sights, or believe other people control their thoughts. These sensations can frighten the person and lead to erratic behavior. Although there is no cure, treatment can usually manage the most serious symptoms. Contrary to popular misunderstanding, schizophrenia is is not the same as multiple personality disorder.

What Are the Symptoms?
They include:
- Hallucinations: hearing or seeing imaginary things
- Delusions: strongly held false beliefs
- Catatonia: a condition in which the person becomes physically fixed in a single position for a very long time, engages in bizarre movements, or doesn't respond appropriately to others."
Some signs, such as lack of enjoyment in everyday life and withdrawal from social activities, may mimic depression.
How It Affects Thoughts
People with schizophrenia may have trouble organizing their thoughts or making logical connections. They may feel like their mind is jumping from one unrelated thought to another. Sometimes they have "thought withdrawal," a feeling that thoughts are removed from their head, or "thought blocking," when someone's flow of thinking suddenly gets interrupted.

Effects on Behavior
The disease has a major impact in many ways. People may talk and not make sense, or they make up words. They may be agitated or show no expression. Many have trouble keeping themselves or their homes clean. Some repeat behaviors, such as pacing. Despite stigma , the risk of violence against others is small.

Who Gets Schizophrenia?
Anyone can. It’s equally common among men and women and among ethnic groups. Symptoms usually start between ages 16 and 30. Early symptoms may present weeks, months or even years before the first incident of full psychosis . It tends to begin earlier in men than in women. Schizophrenia rarely starts during childhood or after age 45. People with schizophrenia or other psychotic disorders in their family may be more likely to get it.

What Causes It?
Scientists don’t know the cause of schizophrenia. A person’s genes, experiences, and setting may all be involved. Theories include how active and how well certain areas of the brain work, as well as problems with brain chemicals such as dopamine and glutamate. There may be structural differences, too, like loss of nerve cells that result in larger fluid-filled cavities or "ventricles” in the brain.

How Doctors Diagnose It
There are no lab tests to find schizophrenia, so doctors usually base a diagnosis on a person’s history and symptoms. They will first rule out other medical causes. In teens, a combination of family history and certain behaviors can help predict the start of schizophrenia. The period when symptoms first start to arise and before the first episode of psychosis (FEP) is called the prodromal period. It can last days, weeks or even a years. Sometime it can be difficult to recognize because there is usually no specific trigger. Prodrome is accompanied by what can be perceived as subtle behavioral changes, especially in teens. These behaviors include withdrawing from social groups and expressing unusual suspicions, but that’s not enough for a diagnosis.

Medicines That Treat It
Prescription drugs can reduce symptoms such as abnormal thinking, hallucinations, and delusions. Some people have troubling side effects, including tremors and gaining weight. Drugs may also interfere with other medicines or supplements. But in most cases, medication is a must to treat schizophrenia.
The Role of Therapy
Counseling can help people develop better ways to recognize and handle their problem behaviors and thoughts, and improve how they relate to others. The earlier treatment is sought, the better the outcome. In cognitive behavioral therapy (CBT), people learn to test the reality of their thoughts and better manage symptoms. Other forms of therapy aim to improve self-care, communication, and relationship skills.

Navigating the World
Rehabilitation programs for schizophrenia teach people how to do everyday things, like use public transportation, manage money, shop for groceries, or find and keep a job . These programs work best when incorporated into a team approach like Coordinated Specialty Care (CSC). This treatment includes medications, therapy, and social services along with employment and educational interventions.

Staying on the Plan
People with schizophrenia sometimes quit their medications because of side effects or not understanding their illness. This raises the risk of serious symptoms returning, which can lead to a psychotic episode (in which someone loses touch with reality). Regular counseling can help people stick with their treatment and avoid a relapse or the need for hospitalization.

Challenges at Work
People with schizophrenia often have trouble finding or keeping a job. This is partly because the disease affects thinking, concentration, and communication. But it also stems from the fact that symptoms start in young adulthood, when many people are starting their careers. Vocational and occupational rehabilitation can help people develop practical job skills.


When a Loved One Has It
Relationships can be rocky for people with schizophrenia. Their unusual thoughts and behaviors may keep friends, co-workers, and family members away. Treatment can help. One form of therapy focuses on forming and nurturing relationships. If you are close to someone who has schizophrenia, you may want to join a support group or get counseling yourself, so you can get support and learn more about what they are going through.

Alcohol, Drugs Are a Risk
People with schizophrenia are much more likely than other people to abuse alcohol or illicit drugs . Some substances, including marijuana and cocaine, can make symptoms worse. Drug abuse also interferes with treatments for schizophrenia. If you know someone who’s dealing with that, look for substance abuse programs designed for people with schizophrenia.

Discuss Before Pregnancy
Women with schizophrenia who plan to get pregnant should talk with their doctors to make sure that their medications are OK to take during pregnancy. Studies of schizophrenia drug safety during pregnancy are encouraging. But although there are no definitive links between medications for schizophrenia and birth defects or serious pregnancy complications, it’s important to talk about it with your doctor first.

When It’s a Relative
It can be hard to convince someone with schizophrenia to get help. Treatment often begins when a psychotic episode results in a hospital stay. Once the person is stabilized, family members can do these things to help prevent a relapse:
- Encourage the person to stay on medication
- Go with them to their follow-up appointments
- Be supportive and respectful
Where to Learn More
To learn more about schizophrenia, contact the National Institute of Mental Health (NIMH) or the National Alliance on Mental Illness (NAMI). NAMI can put you in touch with local support groups for patients and their families.
IMAGES PROVIDED BY:
1) Roger Harris/Photo Researchers, ISM/Phototake 2) Dejan Patic/Taxi 3) Harnett,Hanzon/Photodisc 4) Henry Spencer/Photographer’s Choice 5) Sandra Baker/Stone 6) Photo courtesy of Drs E. Fuller Torrey and Daniel Weinberger 7) Thomas Northcut/Lifesize 8) Huntstock 9) Steve Pomberg/WebMD 10) Frank Saragnese/Workbook Stock 11) Pixtal Images 12) Sot/Riser 13) Laurie LIDJI/StockImage 14) Radius Images 15) Chad Ehlers/Stock Connection 16) Ghislain&Marie David Lossy/The Image Bank 17) Tetra Images
REFERENCES:
American Academy of Family Physicians: "Schizophrenia."
American Psychiatric Association: "Schizophrenia."
New England Journal of Medicine.
American Journal of Psychiatry.
National Institute of Mental Health: "What Causes Schizophrenia?" "Schizophrenia;" and "Mental Health Medications."
National Alliance on Mental Illness: "Mental Illness: Schizophrenia."
Top doctors in ,
Find more top doctors on, related links.
- Schizophrenia Health News
- Schizophrenia Health Reference
- Schizophrenia Health Slideshows
- Schizophrenia Health Blogs
- Schizophrenia Health Videos
- Schizophrenia Health Medications
- Schizophrenia Health Crisis Assistance
- Find a Psychiatrist
- Anxiety/Panic Disorders
- Bipolar Disorder
- Drug Interaction Checker
- Mental Health
- Psychotic Depression
- Schizoaffective Disorder
- Schizophreniform Disorder
- Smoking Cessation
Schizophrenia
Apr 14, 2013
780 likes | 1.68k Views
Schizophrenia. Features, Diagnosis, Epidemiology, Etiology, Treatment, Neurochemistry Jack Foust, MD Assistant Professor, Department of Psychiatry and Behavioral Sciences Medical University of South Carolina. Features of Schizophrenia - Positive Symptoms. Hallucinations
Share Presentation
- moghaddam b et al
- hallucinations
- environmental influences
- less likely
- temporal lobe structures
- res brain res rev

Presentation Transcript
Schizophrenia • Features, Diagnosis, Epidemiology, Etiology, Treatment, Neurochemistry • Jack Foust, MD • Assistant Professor, Department of Psychiatry and Behavioral Sciences • Medical University of South Carolina
Features of Schizophrenia - Positive Symptoms • Hallucinations • Disorganized speech/thinking/behavior • Delusions
(from The Hour of the Wolf, directed by Ingmar Bergman)
Features of Schizophrenia - Negative Symptoms • Affective flattening • Alogia • Avolition • Anhedonia • Social Withdrawal
Features of Schizophrenia - Cognitive Deficits • Attention • Memory • Executive functions (organization, planning)
Schizophrenia - DSM Diagnostic Criterion “A” • Characteristic Sxs (2 + for 1 month) • delusions • hallucinations • disorganized speech • grossly disorganized or catatonic behavior • negative Sxs (flat affect, alogia, avolition) • (Only one element required if delusions bizarre, • or hallucinations commentary 2 voices conversing )
Schizophrenia - DSM Diagnostic Criteria B - F • Social/occupational dysfunction (decline) • Duration - 6 months total, 1 month “A” Sxs • Exclusion - SAFD, mood d/o • Exclusion - sub abuse, gen med condition • PDD/Autism - at least 1 month delusions or hallucinations
Schizophrenia - Comorbid Conditions • Depression • Anxiety • Aggression • Substance use disorder
Schizophrenia: Who is at Risk? • Lifetime prevalence • Epidemiologic Catchment Area Study: 1.3% • National Comorbidity Survey: 0.7% • Demographic characteristics • Age - typical onset late teens/early twenties • Gender - earlier age of onset among men • Marital status - less likely to be married
Schizophrenia: Who is at Risk? • Predisposing factors • Season of birth • Pregnancy and birth complications • Genetic background • Precipitating factors • Stress • Substance Abuse
“In addition to interfering with normal brain development, heavy marijuana use in adolescents may also lead to an earlier onset of schizophrenia in individuals who are genetically predisposed” Dr Sanjiv Kumra, Albert Einstein College of Medicine
“Carriers of the COMT valine158 allele were most likely to exhibit psychotic symptoms and to develop schizophreniform disorder if they used cannabis. Cannabis use had no such adverse influence on individuals with two copies of the methionine allele.” Caspi A, et al. Biological Psychiatry.2005; 57:1117-1127.
Genetic Risk Factors
Etiology: Neurodevelopmental Hypothesis • Possible insult during gestation, environmental influences • Disturbance in normal brain maturation • Reduced size medial temporal lobe structures - amygdala, hippocampus • Disturbed cytoarchitecture in hippocampus, entorhinal cortex
Treatment: Psychosocial Interventions • Supportive therapy • Behavioral family therapy • Family education • Social skills training • Community support • Lower relapse; improved functioning, compliance and social adjustment
Treatment: Antipsychotics • Used to treat psychotic disorders, such as schizophrenia, mania, psychotic depression • Include both “typicals” (Haldol) and “atypicals” (Clozaril, Risperdal)
Typical Antipsychotics • Chlopromazine (Thorazine) - prototype • Thioridazine (Mellaril) • Fluphenazine (Prolixin) • Haloperidol (Haldol)
Typical Antipsychotics: Drug/Receptor Effects • Antidopaminergic (D2) • Anticholinergic • Antihistaminic • Anti-alpha 1
Effects of Typical Antipsychotics • Four dopamine pathways • Mesocortical (negative symptoms) • Mesolimbic (positive symptoms) • Nigrostriatal (EPS, TD) • Tuberoinfundibular (hyperprolactinemia)
Guillin O and Laruelle M. Cellscience Reviews. 2005; 2:79-107
DA Receptor Distribution • D1- prefrontal cortex, striatum • D5 - hippocampus and entorhinal cortex • D2 – striatum, low concentration in medial temporal structures (hippocampus, entorhinal cortex, amygdala), thalamus, prefrontal cortex • D3 – striatum and ventral striatum • D4 - prefrontal cortex and hippocampus (have not been detected in the striatum)
Side Effects of Typical Neuroleptics • Extra-pyramidal syndrome (EPS) • Tardive dyskinesia (TD) • Neuroleptic malignant syndrome (NMS) • Prolactin elevation
Extra-Pyramidal Syndrome (EPS) • Acute dystonia • Akathesia • Muscle rigidity • Bradykinesia • Treatment – typically treated with anticholinergic compounds (Cogentin, Benadryl, Artane), Beta-blockers
Tardive Dyskinesia(TD) • 25-year continuous exposure risk: 68% in Yale Incidence Study • Annual incidence: 5% • Risk factors • Increased age • African-American race • Dose and duration of drug exposure • Early and severe EPS
Neuroleptic Malignant Syndrome (NMS) • Potentially fatal complication of neuroleptic Tx • Temperature dysregulation: T >104°F/40°C • Muscle rigidity • Elevated CPK • Elevated WBC • Associated with TaqI A polymorphism in DRD2 • Tx: withdraw neuroleptics, cooling, dantrolene, bromocriptine (DA agonist)
Summary: Limitations of Typical Antipsychotics • Limited efficacy against negative symptoms • A substantial portion of patients (25% to 40%) respond poorly to treatment • EPS occurs at clinically effective doses • Side effects other than EPS (such as NMS) • Liable to cause tardive dyskinesia • Serum prolactin elevation
Advantages of Typical Antipsychotics • No blood monitoring • Efficacious for positive symptoms • Parenteral and depot preparations available • Low-cost
Antipsychotics: Atypical • Clozapine (Clozaril) - prototype • Risperidone (Risperdal) • Olanzepine (Zyprexa) • Quetiapine (Seroquel) • Ziprasidone (Geodon) • Aripiprazole (Abilify)
Atypical Antipsychotics: Clinical and Drug/Receptor Characteristics • Clinically display less EPS, more effective against negative symptoms, some improvement in cognition • Balanced D2/D1 antagonism • Strong 5HT2 antagonists
Serotonin-Dopamine Antagonists and TD: Hypothesized “Site-Specific” Neuromechanisms Psychosis EPS and TD Limbic Cortical Caudate/Putamen A10 A9 Ventral Tegmental Area Substantia Nigra Dopamine/5HT Antagonist Conventional Antipsychotic Agents
Atypical Antipsychotics
Antipsychotic Receptor Affinities • Haloperidol (Haldol)
Antipsychotic Receptor Affinities • Clozapine (Clozaril)
Antipsychotic Receptor Affinities • Risperidone (Risperdal)
Antipsychotic Receptor Affinities • Olanzepine (Zyprexa)
Antipsychotic Receptor Affinities • Quetiapine (Seroquel)
Ziprasidone (Geodon) • High affinity (antagonist) for D2, D3, 5HT2a, 5HT2c, 5HT1d • High affinity (agonist) for 5HT1a • Inhibits re-uptake of 5HT and NE • Moderate affinity for H1, α1 • Low affinity for D1, α2 • Negligible affinity for M1
Ziprasidone (Geodon), cont. • Positive symptoms improved (PANSS) • Negative symptoms improved (PANSS) • Depressive symptoms improved (MADRS) • Low EPS (5HT2a/D2, 5HT1a) • Low weight gain (H1) • Low sexual dysfunction • Minimal CYP450, CBC, LFT or CV effects (some QTc prolongation)
Neurotransmitter Systems Implicated in Schizophrenia Dopamine Acetylcholine Serotonin Norepinephrine GABA Neuropeptides Glutamate
Dopamine Hypothesis • Induction or worsening of psychotic symptoms with dopamine agonists • Amelioration of psychotic symptoms with antipsychotic drugs that are D2-receptor antagonists
Serotonin (5HT) Hypothesis • M-CPP (m-chlorophenylpiperazine) selective 5HT receptor agonist worsens psychotic symptoms • Pretreatment with ritanserin (5HT antagonist) attenuates psychotic symptoms
Glutamate Hypothesis • Psychotomimetic effects of phencyclidine (PCP), a potent N-methyl-D-aspartate (NMDA) type glutamate receptor antagonist - mimics negative, positive and disorganization symptoms • Possible beneficial effects of cycloserine, glutamate receptor agonist
Glutamate, Dopamine, Ketamine • “Subanesthetic doses of ketamine, a noncompetitive NMDA receptor antagonist, impair prefrontal cortex (PFC) function in the rat and produce symptoms in humans similar to those observed in schizophrenia.” • “These findings suggest that ketamine may disrupt dopaminergic neurotransmission in the PFC as well as cognitive functions associated with this region, in part, by increasing the release of glutamate, thereby stimulating postsynaptic non-NMDA glutamate receptors.” Moghaddam B et al. J Neurosci 1997; 17: 2921-2927.
Aghajanian GK, Marek GJ. Brain Res Brain Res Rev 2000; 31:302-312.
Neuronal Circuits in Schizophrenia • Thalamic nuclei relay sensory information to pyramidal neurons in limbic cortex and neocortex through glutaminergic excitatory afferents • Excessive response of pyramidal neurons is putative mechanism of psychosis (overstimulation) Freedman R. Schizophrenia. NEJM. 2003; 349:1738-1749.
- More by User
A group of severe disorders characterized by… disorganized and delusional thinking disturbed perceptions inappropriate emotions and behaviors. Schizophrenia. Often linked to the neurotransmitter dopamine. How Prevalent is Schizophrenia?.
3.37k views • 14 slides
Schizophrenia. Chapter 16. Schizophrenia. Fascinated and confounded healers for centuries One of most severe mental illnesses 1/3 of population 2.5% of direct costs of total budget $46 billion in indirect costs. History of Schizophrenia.
1.58k views • 55 slides
Schizophrenia. Tutorial (6/7/06) O.Arikawe. Definition: Splitting of psychic functions . Incidence : Low incidence but relatively high prevalence Annual incidence using current diagnostic criteria is 0.17 and 0.54 per 1000 population. Types. Acute and chronic
633 views • 16 slides
Schizophrenia. Schizophrenia: The Facts. Affects about .8% of Americans are afflicted Throughout the world over 24 million people suffer from this disease Strikes most commonly in early twenties Affects men and women equally “split mind”. 2. Symptoms of Schizophrenia.
418 views • 11 slides
Schizophrenia. Definition. Schizophrenia is a mental illness that effects the brain that makes the person view reality abnormally. This can consist of delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior. Types.
361 views • 7 slides
Schizophrenia. Chapter 11. Schizophrenia. Positive Symptoms: Type I Delusions Persecutory Delusions of Reference Grandiose Delusions. Schizophrenia. Hallucinations Disorganized Thoughts and Speech Disorganized or Catatonic Behavior http://www.wimp.com/schizophrenicsymptoms/.
389 views • 14 slides
Schizophrenia. By Garren Richardson. What is Schizophrenia?. Schizophrenia is a psychological disorder classified separately from other disorders because it is not easily categorized as an anxiety or mood disorder
393 views • 10 slides
Schizophrenia. The Unwell Brain. Disturbance in the Neurochemistry. The first discovery in the mid 1950s was that chronic usage of large daily doses of Amphetamines could produce a psychosis that was virtually indistinguishable from schizophrenia.
305 views • 12 slides

Schizophrenia. Schizophrenia. Two or more of the following, each present for a significant portion of the time during a 1-month period** Delusions Hallucinations Disorganized speech Grossly disorganized or catatonic behavior Negative symptoms . Schizophrenia.
996 views • 20 slides
Schizophrenia. By Rebecca Stipp. History. Definition. a severe mental disorder characterized by some, but not necessarily all, of the following features: emotional blunting, intellectual deterioration, social isolation, disorganized speech and behavior, delusions, and hallucinations.
278 views • 10 slides
Schizophrenia. What is schizophrenia?. Most disabling and chronic of all mental illnesses Psychosis: type of mental illness- cannot distinguish reality from imagination Psychotic episodes Distorts: Thinking (may believe others are controlling their thoughts) Expression of emotions
304 views • 14 slides
Schizophrenia. Definition Psychotic disorder Thought Disorder Loose associations “Split” from reality NOT split or multiple personality. Symptoms of Schizophrenia. Positive Symptoms Loose associations Word salad Delusions Hallucinations Negative Symptoms Poverty of speech content
577 views • 24 slides
SCHIZOPHRENIA
SCHIZOPHRENIA. Andy Cortez Julian Cruz Period 05. Peter Green. He is the founder of Fleetwood Mac, a famous band He was diagnosed with schizophrenia in the mid 70’s Spent time in psychiatric hospitals and went through electroconvulsive therapy
362 views • 7 slides
Schizophrenia. Unfolding Case Study By Amanda Eymard , DNS, RN and Linda Manfrin-Ledet , DNS, APRN. Assigned Reading to be completed prior to case study. Prior to conducting this unfolding case study, students should read the following:
4.27k views • 82 slides
Schizophrenia. Lecture of 2-14-07. Symptoms. Psychosis Lack of touch with reality Delusions Erroneous beliefs Hallucinations False sensory perceptions Too much dopamine or not enough glutamate. Paranoid Schizophrenia. Delusions of grandeur Believe they are special with special powers
409 views • 22 slides
Schizophrenia. Stacy Zeigler. NIMH. Schizophrenia is a chronic, severe, and disabling brain disorder Affects 1.1% of the U.S. population age 18 and older in a given year.
774 views • 60 slides
Schizophrenia. A group of severe disorders characterized by disorganized and delusional thinking, disturbed perceptions, and inappropriate emotions and behaviours. Those with paranoid tendencies are particularly prone to delusions of persecution.
1.56k views • 7 slides
Schizophrenia. Lyudmyla T. Snovyda. Schizophrenia -.
1.06k views • 36 slides
Schizophrenia. www.psychlotron.org.uk. Schizophrenia is not a multiple personality A psychotic disorder involving a break with reality Many different manifestations with a few shared features. Schizophrenia diagnosis. Positive Symptoms:
913 views • 24 slides

Schizophrenia. Tiffany Becker Denise Keown Heather Baltz. Overview of Schizophrenia. What is schizophrenia? Schizophrenia behaviors Does schizophrenia affect the brain? What causes schizophrenia? Who gets schizophrenia? Early Onset Schizophrenia Schizophrenia Facts.
1.12k views • 37 slides

Rochelle Blumenstock. Schizophrenia. Etiology. Genetics 10% chance of developing the disorder if you have an immediate relative with it 40-65% chance of both twins being diagnosed with the disorder No single gene associated Many rare genetic mutations . Environment
358 views • 17 slides
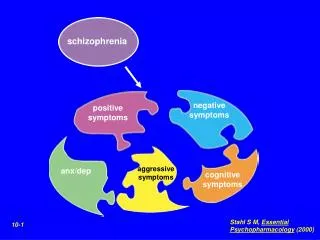
schizophrenia
schizophrenia. negative symptoms. positive symptoms. aggressive symptoms. anx/dep. cognitive symptoms. Stahl S M, Essential Psychopharmacology (2000). 10-1. Positive Symptoms of Schizophrenia. Negative Symptoms of Schizophrenia. Stahl S M, Essential Psychopharmacology (2000). 10-20.
693 views • 14 slides

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Chapter 18. Psychological Disorders
Schizophrenia
Leanne Stevens; Jennifer Stamp; and Kevin LeBlanc (editors)
Approximate reading time: 18 minutes
Schizophrenia is a devastating psychological disorder that is characterised by major disturbances in thought, perception, emotion and behaviour. About 1% of Canadians aged 10 and older are diagnosed with schizophrenia (Public Health Agency of Canada, 2019). The disorder is commonly first diagnosed in young adulthood, with a significant number of new cases identified between the ages of 20 and 34, highlighting the critical period of early adulthood for the onset of this mental illness (Public Health Agency of Canada, 2019).
Most people with schizophrenia experience significant difficulties in many day-to-day activities, such as holding a job, paying bills, caring for oneself (grooming and hygiene), and maintaining relationships with others. Frequent hospitalisations are more often the rule rather than the exception with schizophrenia. Even when they receive the best treatments available, many with schizophrenia will continue to experience serious social and occupational impairment throughout their lives.
What is schizophrenia? First, schizophrenia is not a condition involving a split personality; that is, schizophrenia is not the same thing as dissociative identity disorder (better known as multiple personality disorder). These disorders are sometimes confused because the word schizophrenia, first coined by the Swiss psychiatrist Eugen Bleuler in 1911, derives from Greek words that refer to a “splitting” (schizo) of psychic functions (phrene) (Green, 2001).
Schizophrenia is considered a psychotic disorder, or one in which the person’s thoughts, perceptions and behaviours are impaired to the point where she is not able to function normally in life. In informal terms, one who suffers from a psychotic disorder (that is, has a psychosis) is disconnected from the world in which most of us live.
Symptoms of Schizophrenia
The main symptoms of schizophrenia include hallucinations, delusions, disorganised thinking, disorganised or abnormal motor behaviour, and negative symptoms (APA, 2013). A hallucination is a perceptual experience that occurs in the absence of external stimulation. Auditory hallucinations (hearing voices) occur in roughly two-thirds of patients with schizophrenia and are by far the most common form of hallucination (Andreasen, 1987). The voices may be familiar or unfamiliar, they may have a conversation or argue, or the voices may provide a running commentary on the person’s behaviour (Tsuang, Farone, & Green, 1999).
Less common are visual hallucinations (seeing things that are not there) and olfactory hallucinations (smelling odours that are not actually present).
Delusions are beliefs that are contrary to reality and are firmly held even in the face of contradictory evidence. Many of us hold beliefs that some would consider odd, but a delusion is easily identified because it is clearly absurd. A person with schizophrenia may believe that their mother is plotting with the FBI to poison their coffee, or that their neighbour is an enemy spy who wants to kill them. These kinds of delusions are known as paranoid delusions , which involve the (false) belief that other people or agencies are plotting to harm the person. People with schizophrenia also may hold grandiose delusions , beliefs that one holds special power, has unique knowledge, or is extremely important.
For example, the person who claims to be Cleopatra, or who claims to be a traveler, or claims to have a superpower, is experiencing grandiose delusions. Other delusions include the belief that one’s thoughts are being removed (thought withdrawal) or thoughts have been placed inside one’s head (thought insertion). Another type of delusion is somatic delusion , which is the belief that something highly abnormal is happening to one’s body (e.g., that one’s kidneys are being eaten by cockroaches).
Disorganised thinking refers to disjointed and incoherent thought processes, which are usually detected by what a person says. The person might ramble, exhibit loose associations (jump from topic to topic), or talk in a way that is so disorganised and incomprehensible that it seems as though the person is randomly combining words. Disorganised thinking is also exhibited by blatantly illogical remarks (e.g., “The CN Tower is in Toronto. I live in Toronto. Therefore, I live at the CN Tower.”) and by tangentiality — responding to others’ statements or questions with remarks that are either barely related or unrelated to what was said or asked. For example, if a person diagnosed with schizophrenia is asked if she is interested in receiving special job training, she might state that she once rode on a train somewhere. To a person with schizophrenia, the tangential (slightly related) connection between job training and riding a train are sufficient enough to cause such a response.
Disorganised or abnormal motor behaviour refers to unusual behaviours and movements: becoming unusually active, exhibiting silly child-like behaviours (giggling and self-absorbed smiling), engaging in repeated and purposeless movements, or displaying odd facial expressions and gestures. In some cases, the person will exhibit catatonic behaviours that show decreased reactivity to the environment, such as posturing, in which the person maintains a rigid and bizarre posture for long periods of time, or catatonic stupor, a complete lack of movement and verbal behaviour.
Negative symptoms are those that reflect noticeable decreases and absences of certain behaviours, emotions, or drives (Green, 2001). A person who exhibits diminished emotional expression shows no emotion in his facial expressions, speech or movements, even when such expressions are normal or expected. Avolition is characterised by a lack of motivation to engage in self-initiated and meaningful activity, including the most basic of tasks, such as bathing and grooming. Alogia refers to reduced speech output; in simple terms, patients do not say much. Another negative symptom is asociality , or social withdrawal and lack of interest in engaging in social interactions with others. A final negative symptom, anhedonia , refers to an inability to experience pleasure. One who exhibits anhedonia expresses little interest in what most people consider to be pleasurable activities, such as hobbies, recreation, or sexual activity.
Causes of Schizophrenia
There is considerable evidence suggesting that schizophrenia has a genetic basis. The risk of developing schizophrenia is nearly 6 times greater if one has a parent with schizophrenia than if one does not (Goldstein, Buka, Seidman, & Tsuang, 2010). Additionally, one’s risk of developing schizophrenia increases as genetic relatedness to family members diagnosed with schizophrenia increases (Gottesman, 2001).
When considering the role of genetics in schizophrenia, as in any disorder, conclusions based on family and twin studies are subject to criticism. This is because family members who are closely related (such as siblings) are more likely to share similar environments than are family members who are less closely related (such as cousins); further, identical twins may be more likely to be treated similarly by others than might fraternal twins. Thus, family and twin studies cannot completely rule out the possible effects of shared environments and experiences.
Such problems can be corrected by using adoption studies, in which children are separated from their parents at an early age. One of the first adoption studies of schizophrenia conducted by Heston (1966) followed 97 adoptees, including 47 who were born to mothers with schizophrenia, over a 36-year period. Five of the 47 adoptees (11%) whose mothers had schizophrenia were later diagnosed with schizophrenia, compared to none of the 50 control adoptees. Other adoption studies have consistently reported that for adoptees who are later diagnosed with schizophrenia, their biological relatives have a higher risk of schizophrenia than do adoptive relatives (Shih, Belmonte, & Zandi, 2004).
Although adoption studies have supported the hypothesis that genetic factors contribute to schizophrenia, they have also demonstrated that the disorder most likely arises from a combination of genetic and environmental factors, rather than just genes themselves. For example, investigators in one study examined the rates of schizophrenia among 303 adoptees (Tienari et al., 2004). A total of 145 of the adoptees had biological mothers with schizophrenia; these adoptees constituted the high genetic risk group. The other 158 adoptees had mothers with no psychiatric history; these adoptees composed the low genetic risk group. The researchers managed to determine whether the adoptees’ families were either healthy or disturbed.
For example, the adoptees were considered to be raised in a disturbed family environment if the family exhibited a lot of criticism, conflict, and a lack of problem-solving skills. The findings revealed that adoptees whose mothers had schizophrenia (high genetic risk) and who had been raised in a disturbed family environment were much more likely to develop schizophrenia or another psychotic disorder (36.8%) than were adoptees whose biological mothers had schizophrenia but who had been raised in a healthy environment (5.8%), or than adoptees with a low genetic risk who were raised in either a disturbed (5.3%) or healthy (4.8%) environment. Because the adoptees who were at high genetic risk were likely to develop schizophrenia only if they were raised in a disturbed home environment, this study supports a diathesis-stress interpretation of schizophrenia — both genetic vulnerability and environmental stress are necessary for schizophrenia to develop; genes alone do not show the complete picture.
Neurotransmitters
If we accept that schizophrenia is at least partly genetic in origin, as it seems to be, it makes sense that the next step should be to identify biological abnormalities commonly found in people with the disorder. Perhaps not surprisingly, a number of neurobiological factors have indeed been found to be related to schizophrenia. One such factor that has received considerable attention for many years is the neurotransmitter dopamine. Interest in the role of dopamine in schizophrenia was stimulated by two sets of findings; drugs that increase dopamine levels can produce schizophrenia-like symptoms, and medications that block dopamine activity reduce the symptoms (Howes & Kapur, 2009). The dopamine hypothesis of schizophrenia proposed that an overabundance of dopamine or too many dopamine receptors are responsible for the onset and maintenance of schizophrenia (Snyder, 1976). More recent work in this area suggests that abnormalities in dopamine vary by brain region and thus contribute to symptoms in unique ways. In general, this research has suggested that an overabundance of dopamine in the limbic system may be responsible for some symptoms, such as hallucinations and delusions, whereas low levels of dopamine in the prefrontal cortex might be responsible primarily for the negative symptoms (avolition, alogia, asociality and anhedonia) (Davis, Kahn, Ko, & Davidson, 1991). In recent years, serotonin has received attention, and newer antipsychotic medications used to treat the disorder work by blocking serotonin receptors (Baumeister & Hawkins, 2004).
Brain Anatomy
Brain imaging studies reveal that people with schizophrenia have enlarged ventricles , the cavities within the brain that contain cerebral spinal fluid (Green, 2001). This finding is important because larger than normal ventricles suggests that various brain regions are reduced in size, thus implying that schizophrenia is associated with a loss of brain tissue. In addition, many people with schizophrenia display a reduction in grey matter (cell bodies of neurons) in the frontal lobes (Lawrie & Abukmeil, 1998), and many show less frontal lobe activity when performing cognitive tasks (Buchsbaum et al., 1990). The frontal lobes are important in a variety of complex cognitive functions, such as planning and executing behaviour, attention, speech, movement, and problem solving. Hence, abnormalities in this region offer legitimate reasons why people with schizophrenia experience deficits in these areas.
Events During Pregnancy
Why do people with schizophrenia have these brain abnormalities? A number of environmental factors that could impact normal brain development might be at fault. High rates of obstetric complications in the births of children who later developed schizophrenia have been reported (Cannon, Jones, & Murray, 2002). In addition, people are at an increased risk for developing schizophrenia if the pregnant parent was exposed to influenza or experienced nutritional deficiencies or maternal stress during the first trimester of pregnancy (Brown et al., 2004; Brown, 2011; Fineberg et al., 2016; Pugliese et al., 2019).
Research has also suggested that a pregnant parent’s emotional stress during pregnancy may increase the risk of schizophrenia in offspring. One study reported that the risk of schizophrenia is elevated substantially in offspring whose pregnant parent experienced the death of a relative during the first trimester of pregnancy (Khashan et al., 2008). This research demonstrates the importance of maternal stress, medical illnesses, and obstetric complications as risk factors for schizophrenia in adulthood (Paquin et al., 2021; Pugliese et al., 2019).
Another variable that is linked to schizophrenia is cannabis (marijuana) use. Although a number of reports have shown that individuals with schizophrenia are more likely to use cannabis than are individuals without schizophrenia (Thornicroft, 1990), such investigations cannot determine if cannabis use leads to schizophrenia, or vice versa. However, a number of longitudinal studies have suggested that cannabis use is, in fact, a risk factor for schizophrenia. A classic investigation of over 45,000 Swedish conscripts followed up with them after 15 years and found that those individuals who had reported using cannabis at least once by the time of conscription were more than twice as likely to develop schizophrenia during the ensuing 15 years than were those who reported never using cannabis; those who had indicated using cannabis 50 or more times were 6 times as likely to develop schizophrenia (Andréasson, Allbeck, Engström, & Rydberg, 1987).
More recently, a review of 35 longitudinal studies found a substantially increased risk of schizophrenia and other psychotic disorders in people who had used cannabis, with the greatest risk in the most frequent users (Moore et al., 2007). Other work has found that cannabis use is associated with an onset of psychotic disorders at an earlier age (Large, Sharma, Compton, Slade, & Nielssen, 2011). The National Institute on Drug Abuse (NIDA) highlights that considerable evidence, though not universally consistent, has linked cannabis use to an earlier onset of psychosis in individuals with genetic risk factors for psychotic disorders, including schizophrenia. Various factors, such as the amount of drug consumed, the frequency of use, the potency of the cannabis product, and the age at first use, play significant roles in influencing this relationship (National Institute on Drug Abuse, 2023a).
One massive study revealed that young men with cannabis use disorder have an increased risk of developing schizophrenia. The research, which analysed data from over 6 million people in Denmark, suggested that up to 30% of schizophrenia cases among men aged 21-30 might have been preventable by preventing cannabis use disorder (National Institute on Drug Abuse, 2023b).
One plausible interpretation of the data is that early cannabis use may disrupt normal brain development during important early maturation periods in adolescence (Trezza, Cuomo, & Vanderschuren, 2008). Thus, early cannabis use may set the stage for the development of schizophrenia and other psychotic disorders, especially among individuals with an established vulnerability (Casadio et al., 2011).
While cannabis is a much safer drug than alcohol in terms of risk of death, cannabis is not harmless, contrary to popular belief. Specifically, depending on their prenatal, genetic, or environmental stresses, some young adult men are at risk of their cannabis use triggering schizophrenia — especially if they use cannabis frequently. Overall, the available evidence seems to indicate that cannabis use plays a cause-and-effect role in the development of schizophrenia.
It is important to point out, however, that cannabis use is not an essential or sufficient risk factor (i.e., cannabis use cannot cause schizophrenia on its own without some other risk factors also present) since not all people with schizophrenia have used cannabis and the majority of cannabis users do not develop schizophrenia (Casadio, Fernandes, Murray, & Di Forti, 2011).
Watch this video: Tricky Topics: Causes of Schizophrenia (9.5 minutes)
“Tricky Topics: Causes of Schizophrenia” video by FirstYearPsych Dalhousie is licensed under the Standard YouTube licence. Here is the Tricky Topics: Causes of Schizophrenia transcript .
Schizophrenia: Early Warning Signs
Early detection and treatment of conditions such as heart disease and cancer have improved survival rates and quality of life for people who suffer from these conditions. A new approach involves identifying people who show minor symptoms of psychosis, such as unusual thought content, paranoia, odd communication, delusions, problems at school or work, and a decline in social functioning — which are called prodromal symptoms — and following these individuals over time to determine which of them develop a psychotic disorder and which factors best predict such a disorder.
A number of factors have been identified that predict a greater likelihood that prodromal individuals will develop a psychotic disorder: genetic risk (a family history of psychosis), recent deterioration in functioning, high levels of unusual thought content, high levels of suspicion or paranoia, poor social functioning, and a history of substance abuse (Fusar-Poli et al., 2013). Further research will enable a more accurate prediction of those at greatest risk for developing schizophrenia, and thus to whom early intervention efforts should be directed.
To calculate this time, we used a reading speed of 150 words per minute and then added extra time to account for images and videos. This is just to give you a rough idea of the length of the chapter section. How long it will take you to engage with this chapter will vary greatly depending on all sorts of things (the complexity of the content, your ability to focus, etc).
Schizophrenia Copyright © 2024 by Leanne Stevens; Jennifer Stamp; and Kevin LeBlanc (editors) is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
Schizophrenia
- Download PDF
- Order a free hardcopy
What is schizophrenia?
Schizophrenia is a serious mental illness that affects how a person thinks, feels, and behaves. People with schizophrenia may appear to have lost touch with reality, which can be distressing for them and their family and friends. The symptoms of schizophrenia can make it difficult to participate in usual, everyday activities, but effective treatments are available. Treatment can help people remain in school, maintain employment, achieve independence, and enjoy personal relationships.
What are the signs and symptoms of schizophrenia?
It’s important to recognize the symptoms of schizophrenia and seek help as early as possible. People with schizophrenia are usually diagnosed between the ages of 16 and 30, after the first episode of psychosis. Starting treatment as soon as possible following the first episode of psychosis is an important step toward recovery. However, research shows that gradual changes in thinking, mood, and social functioning often appear before the first episode of psychosis. Schizophrenia is rare in younger children.
Schizophrenia symptoms can differ from person to person, but they generally fall into three main categories: psychotic, negative, and cognitive.
Psychotic symptoms
Psychotic symptoms include changes in the way a person thinks, acts, and experiences the world. A person experiencing psychotic symptoms often has disrupted thoughts and perceptions, and they may have difficulty recognizing what is real and what is not. For some people, these symptoms come and go. For others, the symptoms become stable over time. Psychotic symptoms include hallucinations, delusions, and thought disorder.
- Hallucinations are when a person sees, hears, smells, tastes, or feels things that are not there. Hearing voices is common among people with schizophrenia. People who hear voices may hear them for a long time before family or friends notice a problem.
- Delusions are when a person has strong beliefs that are not objectively true and may seem irrational to others. For example, individuals experiencing delusions may believe that people on the radio and television are sending special messages that require a certain response, or they may believe that they are in danger or that others are trying to hurt them.
- Thought disorder is when a person has ways of thinking that are unusual or illogical. People with thought disorder may have trouble organizing their thoughts and speech. They may stop talking in the middle of a thought, jump from topic to topic, or make up words that have no meaning.
Negative symptoms
Negative symptoms include loss of motivation, loss of interest or enjoyment in daily activities, withdrawal from social life, difficulty showing emotions, and difficulty functioning normally. Negative symptoms include:
- Having trouble planning and sticking with routine activities, such as grocery shopping
- Having trouble anticipating and being motivated by pleasure in everyday life
- Talking in a dull voice and showing limited facial expression
- Avoiding social interaction or interacting in socially awkward ways
- Having very low energy and spending a lot of time in passive activities. In extreme cases, a person might stop moving or talking for periods of time, which is a rare condition called catatonia.
These negative symptoms are sometimes mistaken for symptoms of depression or other mental illnesses.
Cognitive symptoms
Cognitive symptoms include problems with attention, concentration, and memory. These symptoms can make it hard to follow a conversation, learn new things, or remember appointments. A person’s level of cognitive functioning is one of the best predictors of their day-to-day functioning. Health care providers use specific tests to evaluate cognitive functioning. Cognitive symptoms include:
- Having trouble processing information to make decisions
- Having trouble using information immediately after learning it
- Having trouble focusing or paying attention
Risk of violence
Most people with schizophrenia are not violent. Overall, people with schizophrenia are more likely than those without the illness to be harmed by others. For people with schizophrenia, the risk of self-harm and violence to others is most significant when the illness is untreated or co-occurs with alcohol or substance misuse. It is important to help people who are showing symptoms get treatment as quickly as possible.
Schizophrenia vs. dissociative identity disorder
Although some of the symptoms may seem similar on the surface, schizophrenia is not dissociative identity disorder (which used to be called multiple personality disorder or split personality). People with dissociative identity disorder have two or more independent identities with distinct behaviors and memories.
What causes schizophrenia?
Several factors may contribute to a person’s risk of developing schizophrenia.
Schizophrenia sometimes runs in families. However, just because one family member has schizophrenia, it does not mean that other members of the family also will have it. Studies suggest that many different genes may increase a person’s chances of developing schizophrenia and that no single gene causes the disorder by itself.
Environment
Research suggests that a combination of genetic factors and aspects of a person’s environment and life experiences may play a role in the development of schizophrenia. These environmental factors may include poverty, stressful or dangerous surroundings, and exposure to viruses or nutritional problems before birth.
Brain structure and function
Research shows that people with schizophrenia may be more likely to have subtle differences in the size of certain brain areas and in connections between brain areas. Some of these brain differences may develop before birth. Researchers are working to better understand how brain structure and function may relate to schizophrenia.
How is schizophrenia treated?
Current treatments for schizophrenia focus on helping individuals manage their symptoms, improve day-to-day functioning, and achieve personal life goals, such as completing education, pursuing a career, and having fulfilling relationships.
Antipsychotic medication
Antipsychotic medication can help make psychotic symptoms less intense and less frequent. This type of medication is usually taken every day in a pill or liquid form. Some forms may be given as an injection once or twice a month. Learn more about antipsychotic medication .
If a person’s symptoms do not improve with usual antipsychotic medication, they may be prescribed clozapine. People who take clozapine must have regular blood tests to check for a potentially dangerous side effect that occurs in 1% to 2% of patients.
People respond to antipsychotic medication in different ways. It is important to report any side effects to a health care provider. Many people taking antipsychotic medication experience side effects such as weight gain, dry mouth, restlessness, and drowsiness when they start taking these medications. Some side effects may go away over time, while others may last.
Do not stop taking a medication without first talking to a health care provider . They can work with you to monitor your health and adjust your treatment plan safely and effectively. Some people may need to try several medications before finding the one that works best.
Read the most up-to-date information on medications, side effects, and warnings on the U.S. Food and Drug Administration (FDA) website .
Psychosocial treatments
Psychosocial treatments help people find solutions to everyday challenges and manage symptoms while attending school, working, and forming relationships. These treatments are often used together with antipsychotic medication. People who participate in regular psychosocial treatment are less likely to have symptoms reoccur or to be hospitalized.
Examples of this kind of treatment include cognitive behavioral therapy, behavioral skills training, supported employment, and cognitive remediation interventions.
Learn more about psychosocial treatments and therapies .
Family education and support
Educational programs can help family and friends learn about symptoms of schizophrenia, treatment options, and strategies for helping loved ones with the illness. These programs can help friends and family manage their own distress, boost their coping skills, and strengthen their ability to provide support.
Coordinated specialty care
Coordinated specialty care (CSC) programs are recovery-focused programs for people with first episode psychosis, an early stage of schizophrenia. Health professionals and specialists work together as a team to provide CSC, which includes psychotherapy, medication, case management, employment and education services, and family education and support. The treatment team works collaboratively with the individual to make treatment decisions, involving family members as much as possible.
Compared with typical care, CSC is more effective in reducing symptoms, improving quality of life, and increasing involvement in work or school.
Assertive community treatment
Assertive community treatment is designed to help individuals with schizophrenia who are likely to experience multiple hospitalizations or homelessness. This type of treatment is usually delivered by a team of health care providers who work together to provide care to patients in the community.
Treatment for drug and alcohol misuse
People with schizophrenia may also have problems with drugs and alcohol. A treatment program that includes treatment for both schizophrenia and substance use is important for recovery because substance use can interfere with treatment for schizophrenia.
How can I find help?
If you have concerns about your mental health, talk to a primary care provider. They can refer you to a qualified mental health professional, such as a psychologist, psychiatrist, or clinical social worker, who can help you figure out the next steps. Find tips for talking with a health care provider about your mental health.
You can learn more about getting help on the NIMH website. You can also learn about finding support and locating mental health services in your area on the Substance Abuse and Mental Health Services Administration (SAMHSA) website.
If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide and Crisis Lifeline at 988 or chat at 988lifeline.org . In life-threatening situations, call 911 .
How can I help a friend or relative with schizophrenia?
It can be difficult to know how to help someone who is experiencing psychosis. Here are some things you can do:
- Help them get treatment and encourage them to stay in treatment.
- Remember that their beliefs or hallucinations seem very real to them.
- Be respectful, supportive, and kind without tolerating dangerous or inappropriate behavior.
- Look for support groups and family education programs, such as those offered by the National Alliance on Mental Illness .
What are clinical trials and why are they important?
Clinical trials are research studies that look at ways to prevent, detect, or treat diseases and conditions. These studies help show whether a treatment is safe and effective in people. Some people join clinical trials to help doctors and researchers learn more about a disease and improve health care. Other people, such as those with health conditions, join to try treatments that aren’t widely available.
NIMH supports clinical trials across the United States. Talk to a health care provider about clinical trials and whether one is right for you. Learn more about participating in clinical trials .
For more information
Learn more about mental health disorders and topics . For information about various health topics, visit the National Library of Medicine’s MedlinePlus .
The information in this publication is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES National Institutes of Health NIH Publication No. 24-MH-8082 Revised 2024
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Schizophrenia.
Manassa Hany ; Baryiah Rehman ; Abid Rizvi ; Jennifer Chapman .
Affiliations
Last Update: February 23, 2024 .
- Continuing Education Activity
Schizophrenia, a serious mental illness, affects 1% of the global population and is marked by hallucinations, delusions, disorganized speech, grossly disorganized behavior, and negative signs and symptoms such as reduced emotional expression, avolition, and cognitive impairment. Symptoms generally emerge in late adolescence or early adulthood, and the disorder may be more common in men. Causes include genetic, environmental, and neurobiological factors. No single gene is responsible; there is an interplay of multiple genetic factors. Environmental influences include prenatal and obstetrical risks, psychosocial stressors, and cannabis use. Neurobiologically, schizophrenia is associated with neurotransmitter dysfunction in dopamine and glutamate systems, as well as brain structural changes. Individualized comprehensive management plans, including antipsychotic medications for positive symptoms and evidence-based psychosocial interventions, are essential for improving patient quality of life. This activity describes the epidemiology, genetics, clinical presentation, and management of schizophrenia, providing healthcare professionals with the knowledge and tools to improve patient care for this complex and disabling condition.
- Identify the varied signs and symptoms of schizophrenia through thorough patient assessments and diagnostic tools.
- Differentiate between schizophrenia and other mental health conditions to ensure accurate diagnosis when individuals present with psychotic symptoms.
- Implement evidence-based treatment approaches tailored to individual patient needs.
- Collaborate with the interdisciplinary team to enhance care coordination for patients with schizophrenia and comorbid psychiatric and medical disorders.
- Introduction
Schizophrenia is a disabling psychiatric condition impacting around 1% of people worldwide and ranking among the top 10 global disability causes. [1] Schizophrenia is characterized by positive psychotic symptoms such as hallucinations, delusions, disorganized speech, and disorganized or catatonic behavior; negative symptoms such as reduced motivation and expressiveness; and cognitive impairments affecting executive function, memory, and mental processing speed. [2] The effect of schizophrenia on daily life varies greatly, with many individuals facing significant disability and incomplete recovery. Even those with more favorable outcomes confront challenges such as social isolation, stigma, and reduced opportunities for forming close relationships. Unemployment rates among people with schizophrenia are notably high. Factors such as poor diet, weight gain, smoking, and concurrent use of substances are prevalent, collectively shortening life expectancy by an estimated 13 to 15 years. [3] [4] The lifetime risk of death by suicide in patients with schizophrenia is 5% to 10%. [5]
Although current diagnostic and treatment approaches in schizophrenia primarily emphasize psychotic symptoms, the disorder's negative and cognitive symptoms play a significant role in impairing social and occupational functioning and often show limited response to antipsychotic medications. [4] [2] This perspective aligns with historical views on the condition: Emil Kraepelin initially described "dementia praecox," which Eugen Bleuler later renamed "schizophrenia." Notably, both Kraepelin and Bleuler did not regard delusions and hallucinations (positive) symptoms as the central characteristics of the illness, suggesting a need for a broader focus on understanding and managing schizophrenia. [4]
The clinical diagnosis of schizophrenia is made after obtaining a detailed psychiatric history and mental status examination and after ruling out other psychiatric and medical causes of psychosis. Risk factors include birthing complications, the season of birth, severe maternal malnutrition, maternal influenza during pregnancy, family history, childhood trauma, social isolation, cannabis use, minority ethnicity, and urbanization. [6] [7] The disorder's etiology and pathophysiological mechanisms remain elusive due to its complexity and heterogeneity. Despite its relatively low prevalence, schizophrenia significantly contributes to the global burden of disease. More than half of those diagnosed with schizophrenia have multiple comorbidities, both psychiatric and medical. [8]
Multifaceted interactions between genetic and environmental risk factors give rise to schizophrenia. These risk factors also affect early brain development and shape the biological response to life experiences, thereby influencing the onset and progression of the disorder. [9]
Twin and family studies indicate that genetic factors can explain approximately 80% of the risk for schizophrenia. [1] While linked common genetic variants have less impact on risk, rare mutations have a more significant impact. [10] One such rare mutation is the chromosome 22q11.2 deletion, which increases lifetime risk 25-fold. [4] Genome-wide association studies have identified 130 genes predominantly associated with neural differentiation, organization, and transmission, which increase the risk of schizophrenia. [11] Most of these genes are not found in coding regions but exert their influence through gene expression modulation. [11] Notably, nearly 30% of these genes are involved in the functioning of the presynaptic and postsynaptic elements of the glutamatergic synapse by impacting N -methyl-D-aspartic acid (NMDA) receptor transmission. [11] Thus, schizophrenia is a polygenic disorder resulting from the combined effects of multiple genes spread across the genome, each contributing modestly.
The approximately 60% concordance rate for schizophrenia in monozygotic twins highlights the substantial role of environmental factors in shaping the expression of genetic risk for the disorder. [11] Environmental influences, such as complications during childbirth, early-life adversities, growing up in urban settings, and migrant status, are thought to interact with genetic predispositions to affect the likelihood of developing schizophrenia. [1] [9]
Patients with schizophrenia exhibit both structural and functional brain abnormalities. Lateral ventricle enlargement by about 25%, coupled with an approximate 2% reduction in overall brain volume, primarily in the grey matter, is seen in schizophrenia. [1] This decrease in grey matter is noted predominantly in the frontal and temporal lobes and the hippocampus. There is evidence of reduced activity in the dorsolateral prefrontal cortex both at rest and during executive tasks, along with increased activity in the medial frontal cortex. [2]
The use of cannabis or its psychoactive ingredient, tetrahydrocannabinol (THC), is known to induce temporary psychotic effects. THC may exacerbate preexisting psychotic conditions and is a risk factor for schizophrenia. Studies indicate a heightened schizophrenia risk among young cannabis users and heavy cannabis users, with the risk seeming dose-dependent and more pronounced in those who begin using at an earlier age or consume more potent strains. [4] In one study, heavy cannabis users were at 6 times greater risk than nonusers of receiving a diagnosis of schizophrenia. [12]
Several neurotransmitter systems have been implicated in the development of schizophrenia, with the dopaminergic and glutamatergic systems the leading contenders.
The neurodevelopmental hypothesis of schizophrenia proposes that a mix of genetic risks and environmental factors during early brain development leads to the disorder. These influences, particularly significant in the prenatal and early life stages, set the stage for the emergence of symptoms of schizophrenia in early adulthood. [13]
- Epidemiology
The lifetime risk of developing schizophrenia is around 1%. Men are more likely to receive the diagnosis than women, with an incidence rate ratio of approximately 1.7 (95% CI, 1.46–1.97). [2] [14] In men, the peak incidence is in the early twenties and then declines; women have a peak incidence later in their twenties, with a slower decline in incidence. Notably, after the mid-forties, new schizophrenia diagnoses become more common in women than in men. [2] Men typically exhibit an earlier onset of the disease, poorer functioning before the illness becomes apparent, more pronounced negative symptoms, and a higher incidence of alcohol and substance use disorders. [15] [16] While gradual onset during adolescence is common, childhood-onset schizophrenia, defined as younger than 13 years, is rare and typically represents a more severe form of the illness with a poor response to antipsychotic medication. [17] Additionally, a higher rate of schizophrenia is linked to urban living and migrant status. [2]
- Pathophysiology
Multiple molecular and neural circuit changes are linked to schizophrenia's pathophysiology, but whether these changes are direct causes or adaptive responses to upstream dysfunctions is unclear. [5] No present model of the pathophysiology of schizophrenia can comprehensively explain all the changes observed.
Neurotransmitter abnormalities are central to the pathophysiology of schizophrenia, with dopamine, serotonin, glutamate, and gamma-aminobutyric acid (GABA) all playing roles. [1] The link between dopamine and schizophrenia emerged from the accidental discovery of dopamine D 2 receptor blockers' effectiveness in alleviating psychotic symptoms. [1] Four key dopamine pathways have been identified in the brain: mesolimbic, mesocortical, tuberoinfundibular, and nigrostriatal. [18] Excessive dopamine activity in the mesolimbic pathway, which runs from the ventral tegmental area to the limbic regions, is thought to contribute to the positive symptoms of schizophrenia. Reduced dopamine levels in the mesocortical pathway, connecting the ventral tegmental area to the cortex, may underlie negative symptoms and cognitive deficits. [19] These observations suggest distinct pathophysiological mechanisms for schizophrenia's positive and negative symptoms. Additionally, the nigrostriatal pathway is linked to extrapyramidal motor side effects caused by D 2 receptor blockers, while the tuberoinfundibular pathway is associated with the hyperprolactinemia observed with D 2 receptor blocker use.
Recent advancements in cognitive neuroscience have elucidated the activation of mesostriatal dopamine neurons in response to "reward prediction error," a phenomenon describing the mismatch between anticipated and actual rewards. [20] This dopaminergic activity is crucial in assigning "salience" to environmental stimuli, a process integral to learning and updating our internal model of the external world. In schizophrenia, there is a noted dysregulation in the firing of these neurons, which leads to a decoupling of dopamine signaling from genuinely salient stimuli, resulting in the misattribution of importance to irrelevant objects or events. This aberrant salience processing plays a significant role in the emergence and persistence of delusions and possibly hallucinations in schizophrenia, as patients might assign undue significance to neutral stimuli. [20]
Understanding dopamine's role in schizophrenia extends beyond the traditional dopamine hypothesis. There is a 2- to 4-week delay between antipsychotic medications' peak blockade of D 2 receptors and the clinical response. [1] This suggests that the antipsychotic effects of these drugs might depend on secondary neurochemical mechanisms triggered by sustained D 2 receptor blockade rather than reduced dopamine transmission alone. [1]
Moreover, the interplay between dopamine, glutamate, and GABA is critical in modulating the function of excitatory and inhibitory interneurons within cortical circuits. Postmortem studies indicate alterations in the microstructure and functioning of these microcircuits in schizophrenia. These findings have steered researchers towards exploring the potential of targeting glutamate and GABA signaling pathways in addition to dopamine for more effective therapeutic interventions in schizophrenia. [1] [19]
- History and Physical
In diagnosing schizophrenia, the patient is evaluated by taking a comprehensive history and conducting a mental status examination. Assessing risks of harm to oneself or others and considering the influence of substance use are critical components of this assessment. Collateral information from family members or close contacts is essential. The primary objective is to eliminate the possibility of other medical or psychiatric conditions presenting similarly and confirm the diagnosis based on the Diagnostic and Statistical Manual of Mental Disorders , 5th ed., Text Revision (DSM-5-TR), or the International Classification of Diseases , Tenth Revision (ICD-10) criteria.
The following are essential elements of history-taking:
- History of present illness : Details of the chronology of symptom presentation and predisposing, precipitating, and perpetuating factors. A review of psychiatric symptoms and comorbid diagnoses is conducted. One should obtain a relevant negative history that could help differentiate schizophrenia from other medical or psychiatric conditions.
- Past psychiatric history : This encompasses recording previous manic and depressive episodes, hospitalizations, treatments (including electroconvulsive therapy), adherence to treatments, the effects and adverse effects of medication, and any history of suicidality (ideas, plans, or attempts, including details), self-injury, and aggressive ideas or behavior.
- Substance use history : The patient’s use of tobacco, alcohol, other substances, and prescription medications is documented.
- Medical history : One should record the patient’s current medical conditions, medications, allergies, medical illnesses, treatments, surgeries, parity, and other relevant health information, such as neurological conditions and sleep issues. The clinician should review potential organic causes of psychosis, including Parkinson disease, multiple sclerosis, syphilis, HIV/AIDS, brain lesions, heavy metal toxicity, delirium, metabolic/endocrine disorders, and dementias, such as Alzheimer disease, frontotemporal dementia, and Lewy body disease.
- Family history : Family history of psychiatric illness, treatment and response to treatment, and history of suicidal or aggressive behaviors in biological relatives are noted.
- Personal and social history : The patient’s language preferences, life circumstances, relationships, children, employment history, cultural and societal views on psychiatric illness, stressors, trauma history, access to weapons, and legal concerns are considered. The patient's sociocultural background and its potential impact on the expression of the illness are inquired, as some beliefs may be delusional in one setting but culturally sanctioned in another and not necessarily a manifestation of psychiatric illness.
- Developmental history : Complications during childbirth, early development, history of trauma and abuse (including head trauma), education, and life experiences are explored. [21]
Physical Examination
Physical examination of a patient with schizophrenia poses unique challenges in meeting the patient's needs. The assessment should be performed with heightened sensitivity and awareness of the patient’s trauma history and potential anxiety, paranoia, aggression, or other psychiatric symptoms. In the physical examination of patients with schizophrenia, assessing general appearance, including hygiene and grooming, offers insights into self-care habits. Vital signs such as blood pressure and heart rate are crucial in identifying underlying health issues. A comprehensive examination covers neurological, cardiovascular, respiratory, and abdominal assessments, highlighting the importance of checking for medication side effects and coexisting conditions. A dermatological examination helps detect signs of substance use or skin infections. Assessing for metabolic syndrome is also essential, mainly due to the risks associated with certain antipsychotic medications.
Mental status examination
The Mental Status Examination (MSE) for schizophrenia varies based on symptom severity, specific manifestations, and coexisting conditions.
- Appearance and behavior : Patients often present with disheveled or unusual attire, reflecting a lack of self-care. Behavior may range from psychomotor retardation to agitation, and patient responses can vary from being cooperative to being unpredictable, withdrawn, or hostile.
- Psychomotor activity : There may be psychomotor agitation or retardation. Some patients may exhibit grossly disorganized or abnormal motor behavior, including catatonic behaviors, such as stupor, mutism, odd gestures, or posturing.
- Speech : Speech patterns can be disorganized, tangential, or incoherent (word salad). Patients' speech may include neologisms (creating new words or phrases without meaning).
- Mood and affect : Assess the degree of hopelessness. Affect can be flat, blunted, or inappropriate to the context of the conversation. Affect may be incongruent with the reported mood, such as laughing when discussing sad events.
- Thought content : Delusions (fixed false beliefs) may be present and bizarre (extremely implausible). Thought broadcasting, thought insertion, or withdrawal may also be reported.
- Thought process : Thought processes (inferred from the patient's speech) may be disorganized, leading to illogical connections, loose associations, or thought blocking when the patient suddenly stops speaking mid-sentence.
- Perceptual abnormalities: Hallucinations, mainly auditory, are common but may be in any sensory modality. Patients may report hearing voices commenting on their actions or conversing with each other. It is important to assess for command hallucinations that tell the patient to engage in violent or dangerous behavior.
- Risk: Assess current suicidality (ideas, plans, access to weapons), self-injury (ideas or behaviors), and aggressive ideas or behaviors.
- Cognition : Cognitive deficits may affect memory, attention, and executive functions. Assess for orientation to person, place, and date.
- Insight and judgment : Insight varies, with some patients partially aware of their condition while others lack insight completely. Judgment is often impaired, affecting the ability to make sound decisions or understand the consequences of actions.
No laboratory, psychometric, or radiologic studies currently exist for diagnosing schizophrenia.
Diagnostic criteria for schizophrenia
The 2 systems used in diagnosing schizophrenia are DSM-5-TR and ICD-10, which have slight variations.
1. DSM-5-TR: According to the DSM-5-TR, published by the American Psychiatric Association (APA) in 2022, the following are the diagnostic criteria of schizophrenia:
Two (or more) of the following, each present for a significant portion of time during 1 month (or less if successfully treated). At least one of these must be (1), (2), or (3):
- Hallucinations
- Disorganized speech (eg, frequent derailment or incoherence)
- Grossly disorganized or catatonic behavior
- Negative symptoms (ie, diminished emotional expression or avolition)
Significant functional decline in areas like work or relationships must be observed to diagnose this disorder since symptom onset. Continuous signs must persist for at least 6 months, including at least 1 month of active-phase symptoms, which might be less if treated. Symptoms can be prodromal or residual, including negative or attenuated active-phase symptoms. Schizoaffective, depressive, or bipolar disorders with psychotic features must be excluded. The symptoms should not be due to substance use, medication, or another medical condition. If a developmental disorder is present, the diagnosis additionally requires at least 1 month of prominent delusions or hallucinations.
2. ICD-10: The patient must exhibit at least one of the following for a period greater than or equal to 1 month:
- Thought echo, thought insertion or withdrawal, echo, and thought broadcasting
- Delusions of control, influence, or passivity; delusional perceptions
- Hallucinatory voices giving a running commentary on the patient or discussing the patient among themselves
- Persistent delusions that are culturally inappropriate or implausible
Or at least 2 of the following symptoms must be observed for a period greater than or equal to 1 month:
- Persistent hallucinations in any modality, when accompanied by fleeting or half-formed delusions
- Breaks or interpolations in thought resulting in incoherence, irrelevant speech, or neologisms
- Catatonic behavior
- Negative symptoms
- Significant and consistent transformation in the overall quality of behavior manifesting as loss of interest and social withdrawal [22]
Unlike the DSM-5-TR, the ICD-10 further categorizes schizophrenia based on the key presenting symptoms as either paranoid schizophrenia, hebephrenic schizophrenia, catatonic schizophrenia, undifferentiated schizophrenia, post-schizophrenic depression, residual schizophrenia, simple schizophrenia, schizophrenia, other, and schizophrenia, unspecified.
Schizophrenia is primarily a clinical diagnosis and necessitates specific laboratory and radiographic investigations to exclude other potential causes. The American Psychiatric Association Practice Guideline for the Treatment of Patients With Schizophrenia recommends the following investigations for an initial evaluation of a patient with schizophrenia. [21]
Hematology: A complete blood count (CBC) to check for anemia or signs of infection that mimic symptoms of schizophrenia. Absolute neutrophil count (ANC) should be obtained if considering or being treated with clozapine.
Blood chemistry panel : This includes testing electrolytes, renal function, liver function, and thyroid-stimulating hormone (TSH). Hypothyroidism can mimic psychiatric disorders, including depression and cognitive impairment.
Pregnancy test : A pregnancy test is recommended for women of childbearing age.
Electroencephalogram : An electroencephalogram (EEG) may be indicated based on the neurological examination or history to rule out a seizure disorder.
Imaging : Brain imaging, either CT or MRI (with MRI preferred), may be indicated based on the neurological examination or history.
Genetic testing : Chromosomal testing is suggested if indicated by physical examination or history, including developmental history.
Drug toxicology screen: This screen may be clinically indicated to detect substance use that could cause psychotic symptoms.
Additional tests
- Rapid plasma reagin (RPR) test is used to screen for syphilis, which can cause psychiatric symptoms.
- HIV testing may be advisable, as HIV infection can mimic psychiatric disorders.
- Electrocardiogram (ECG) is performed before initiating treatment with chlorpromazine, droperidol, iloperidone, pimozide, thioridazine, or ziprasidone, especially for patients with cardiac risk factors, elevated baseline QTc intervals, or when adding other medications that can increase QTc intervals.
- Abnormal Involuntary Movement Scale (AIMS) or Dyskinesia Identification System: The Condensed Use Scale (DISCUS) is used to assess baseline abnormal movements and is conducted every 6 to 12 months after initiating antipsychotic medication.
The American Psychiatric Association (APA) advises that the initial evaluation of a patient suspected of having a psychotic disorder should incorporate a quantitative assessment. This assessment aims to identify and evaluate the severity of symptoms and functional impairments, which could be crucial treatment targets. [21]
Some objective quantitative rating scales that can be used in evaluation include:
- The Positive and Negative Syndrome Scale (PANSS) is used for measuring the symptom severity of patients with schizophrenia and for monitoring improvement. There are 2 versions, the PANSS-30 and the PANSS-6. The PANSS-30 is a comprehensive tool that includes 30 items, subdivided into positive symptoms, negative symptoms, and general psychopathology. The PANSS-6 is a shorter version, focusing on 6 essential items, and correlates well with the longer version.
- The Brief Psychiatric Rating Scale (BPRS) assesses the positive, negative, and affective/anxiety symptoms of individuals with psychotic disorders. It contains 18 items and is known for its usefulness in evaluating symptom changes over time.
- The World Health Organization Disability Assessment Schedule (WHODAS) is a tool designed to measure health and disability across various domains of life. It assesses the level of impairment in daily activities and participation in society, thereby providing a holistic view of a patient's functioning.
- Treatment / Management
In the treatment of schizophrenia, a patient-centered treatment plan is essential, integrating nonpharmacological and pharmacological modalities to relieve symptoms and enhance patient functioning. Elements include selecting an appropriate treatment setting, managing risks, addressing barriers to adherence, and engaging the patient’s support network in recognizing early signs of relapse and how to access and use community resources. Informed consent is essential to this process and encompasses educating patients and their families about the potential benefits and risks of various treatment options. [21]
Antipsychotic Medications
The APA recommends that patients with schizophrenia be treated with antipsychotic medication and observed for effectiveness and side effects. [21]
Antipsychotic medications are divided into first-generation antipsychotics (FGAs) and second-generation antipsychotics (SGAs). While SGAs typically have fewer extrapyramidal side effects and cause less tardive dyskinesia than FGAs, most SGAs, like olanzapine, quetiapine, clozapine, and risperidone, carry a higher risk of metabolic syndrome, especially olanzapine and clozapine. [23] [24] Despite these differences, no clear preference exists between SGAs and FGAs overall, and individual efficacy varies, with clozapine potentially more effective in treatment-resistant schizophrenia and for those patients with a high risk for aggression or suicide. [21] The selection of specific treatments considers factors such as the severity of the illness, patient history of treatment response, the balance between medication efficacy and side effects, and patient preferences. Both FGA and SGA long-acting injectable (LAI) antipsychotic medications can be used to address treatment nonadherence or based on patient preference. [25]
The primary goal of antipsychotic treatment is to alleviate symptoms and restore the patient’s normal functioning, followed by maintenance therapy to prevent symptom recurrence, reduce hospitalizations, and improve quality of life. [26] The initial dose of antipsychotic medication is influenced by factors such as drug formulation, patient characteristics, and history of antipsychotic use. Except for clozapine, dosages of most antipsychotics can be rapidly escalated to therapeutic levels once initial tolerance is confirmed, while also considering that it may take 2 to 4 weeks for patients to show an initial response. [21] The dose-response relationship for antipsychotics typically follows a hyperbolic pattern, reaching a plateau. Dosages above the approved range generally do not yield greater efficacy. While some evidence suggests that olanzapine may be more effective at doses up to 40 mg daily, this must be weighed against the potential for increased adverse effects. [27]
Antipsychotic drugs achieve efficacy when their concentrations in the central nervous system are adequate to occupy around 70% of dopamine D 2 receptors. Clozapine and quetiapine are exceptions to this rule, showing lower D 2 receptor occupancies at their effective clinical doses . [1]
Careful medication selection and lower initial dosing should be considered in younger individuals experiencing their first episode of psychosis due to increased risks of weight gain and metabolic side effects. [21] Lower initial doses can reduce side effects and improve treatment adherence. First episodes often respond more quickly and to lower doses of medication than in subsequent episodes. [28] Based on pharmacokinetic considerations, older patients, especially those with health issues and taking multiple medications, should be started with one-quarter to one-half of the typical adult dose. [21]
Determining the ideal dosage in acute antipsychotic treatment presents a challenge, as there is often a delay between the start of treatment, the initial response (usually 2 to 4 weeks), and the full therapeutic effect, which can span from 4 to 6 weeks or more. [21] Accelerating the dosage increase too quickly can affect tolerability and may give a false sense of the drug’s effectiveness. If there is not at least minimal improvement within the first 2 weeks at a therapeutic dose, it is unlikely that significant improvement will be observed after 4 to 6 weeks of treatment. [29] [21]
Management of Treatment-Resistant Schizophrenia
Approximately one-third of patients with schizophrenia are classified as having treatment-resistant schizophrenia, characterized by the persistent presence of symptoms despite 2 or more trials of antipsychotic medications at adequate doses and durations, with documented adherence. [30] For these patients, clozapine is the recommended treatment option, with about 40% of those with treatment-resistant schizophrenia responding. [30] [31] Despite these encouraging outcomes, clozapine is underutilized in clinical practice, indicating the need for earlier consideration and integration into treatment strategies. Clozapine is also recommended for patients with schizophrenia with persistent, substantial risks of suicide or aggression despite other treatments. [21]
A gradual increase in the dose of clozapine is required to reduce the likelihood of adverse effects such as seizures, orthostatic hypotension, and sedation. Effective clozapine dosages are in the range of 300 mg daily to 450 mg daily. [21] If clozapine is tolerated but ineffective, one should increase the dose to achieve a trough blood level between 350 ng/mL and 600 ng/mL. [21] Maintaining this dosage for at least 8 weeks is recommended for efficacy assessment. [21] Regular tracking of the absolute neutrophil count (ANC) is mandatory to mitigate the risk of agranulocytosis, starting with testing before the initiation of clozapine, weekly checks for the first 6 months, every 2 weeks for the next 6 months, and then monthly monitoring as long as the patient is receiving clozapine. [32] Due to the risk of agranulocytosis, all patients on clozapine are registered in the U.S. Clozapine Risk Evaluation and Mitigation Strategy (REMS) Program (www.clozapinerems.com) that tracks absolute neutrophil counts over time. Clozapine's adverse effect profile differs from other antipsychotic medications. In addition to the rare but severe risk of neutropenia, there is also an increased risk of seizure with high doses or rapid dose escalation and myocarditis. [32] Clozapine can cause gastrointestinal hypomotility, constipation with fecal impaction, ileus, and death; a prophylactic bowel regimen may be required. [33]
Sialorrhea, a common adverse effect of clozapine present in 90% of patients, can be initially managed with nonpharmacologic methods. [34] If these are ineffective, the next step is topical treatments such as ipratropium or atropine. Prompt management is essential to prevent discomfort, stigma, and aspiration pneumonia. [35]
The APA recommends that patients with schizophrenia whose symptoms have improved with antipsychotic medication continue their treatment with the same medication for effective ongoing symptom management. [21] Electroconvulsive therapy can be considered in treatment-resistant cases where its efficacy rates range from 40% to 70%. [36]
Psychosocial Interventions
Besides medication, there are important evidence-based psychosocial interventions for patients with schizophrenia, including:
- Psychoeducation
- Assertive community treatment if there is a history of poor engagement with services
- Coordinated specialty care programs for people experiencing a first episode of psychosis
- Cognitive-behavioral therapy for psychosis (CBTp)
- Supported employment services
- Supportive psychotherapy
- Social Skills Training
- Family interventions
- Cognitive remediation [21]
- Differential Diagnosis
As psychotic features are present in various other mental disorders, according to the Diagnostic and Statistical Manual of Mental Disorders , 5th ed, Text Revision (DSM-5-TR), the differential diagnoses for schizophrenia are wide, including but not limited to:
Major depressive or bipolar disorder with psychotic or catatonic features: If hallucinations or delusions occur only during major depressive or manic episodes, the diagnosis is a depressive or bipolar disorder with psychotic features, depending on the timing and severity of mood disturbances.
Schizoaffective disorder: This diagnosis requires concurrent depressive or manic episodes with active-phase schizophrenia symptoms, with mood symptoms prevalent for most of the active phase.
Schizophreniform and brief psychotic disorder: Schizophreniform disorder is diagnosed when psychotic symptoms last less than 6 months, whereas brief psychotic disorder spans from 1 day to less than 1 month.
Delusional disorder: Distinguished from schizophrenia by the absence of other characteristic schizophrenia symptoms like pronounced hallucinations or disorganized speech.
Schizotypal personality disorder: Characterized by subthreshold schizophrenia symptoms in conjunction with persistent personality traits.
Obsessive-compulsive and body dysmorphic disorder: These disorders involve intense preoccupations with obsessions, compulsions, or body-focused concerns, differing from schizophrenia, although the obsessions can reach delusional proportions.
Posttraumatic stress disorder : PTSD includes hallucinatory flashbacks and hypervigilance that reach paranoia but is diagnosed based on experiencing a traumatic event and specific symptom patterns related to the event.
Autism spectrum and communication disorders: These disorders may include psychotic-like symptoms but are distinguished by social interaction deficits and repetitive behaviors. Schizophrenia is diagnosed concurrently only if there are significant hallucinations or delusions for at least 1 month.
Other mental disorders with psychotic episodes: Schizophrenia is diagnosed when the psychosis is persistent and not attributable to substances or other medical conditions, as can be seen in patients with delirium or substance-induced psychotic disorders.
- Toxicity and Adverse Effect Management
The adverse effects of antipsychotic medications can be divided into the following categories:
Extrapyramidal Symptoms
- Tardive syndromes: Tardive dyskinesia (TD), tardive dystonia, and tardive akathisia can develop after prolonged exposure to antipsychotic medications and are characterized by involuntary movements in the lower face, limbs, and trunk. Symptoms such as grimacing, lip-smacking, tongue protrusions, and excessive blinking may become permanent even after discontinuing the medication. Compared to first-generation antipsychotic medications (FGAs), second-generation antipsychotic medications (SGAs) are thought to pose a lower risk of inducing tardive syndromes. The APA recommends treating tardive dyskinesia with a reversible inhibitor of the vesicular monoamine transporter 2 (VMAT2), such as valbenazine or deutetrabenazine.
- Parkinsonism: Antipsychotic-induced parkinsonism involves bradykinesia, tremor, rigidity, and akinesia and can be managed via a reduction in dose, changing medications, or using amantadine or an anticholinergic medication such as benztropine.
- Akathisia: The restlessness of akathisia is characterized by near-constant motion and can cause dysphoria and even suicidality. It generally develops over days to weeks of antipsychotic treatment. FGAs and aripiprazole are particularly associated with akathisia, while SGAs such as clozapine, olanzapine, and quetiapine carry lower risk. Reducing the dose of the antipsychotic medication, changing medications, adding a benzodiazepine, or adding a beta-adrenergic antagonist medication are suggestions for treating akathisia.
- Acute dystonia: This painful condition comes on suddenly and can be triggered by antipsychotic medications, causing prolonged muscle contractions manifesting as oculogyric crisis, torticollis, and laryngospasm (which can be life-threatening). FGAs appear to precipitate acute dystonia more frequently than SGAs. The APA recommends treatment with anticholinergic medication.
Neuroleptic Malignant Syndrome
Neuroleptic malignant syndrome (NMS) is a rare but potentially lethal effect of antipsychotic medications, affecting 0.02% to 0.04% of patients with a 5% mortality rate. NMS is a medical emergency. Risk factors include the use of high-potency FGAs, rapid dose escalation, and a prior history of NMS (there may be up to a 40% recurrence rate). Symptoms include muscle rigidity, autonomic instability, altered mental status, fever, and elevated creatinine phosphokinase. [35]
Treatment involves immediately stopping all antipsychotic medications, aggressive intravenous hydration, electrolyte correction, and transfer to a higher level of care. Dantrolene and bromocriptine are used to treat moderate to severe NMS, and electroconvulsive therapy (ECT) is an option for treatment-resistant NMS. [35]
Prolactin Elevation
High-potency FGAs and some SGAs (risperidone, paliperidone, and amisulpride) have a greater propensity to cause prolactin elevation. This is due to dopamine D 2 receptor antagonism in the anterior pituitary, leading to disruptions in the hypothalamic-pituitary-gonadal axis and symptoms such as breast enlargement, galactorrhea, sexual dysfunction, and menstrual irregularities. Management strategies include lowering the dosage of the current antipsychotic medication, switching to an antipsychotic medication with a lower risk of increasing prolactin levels, or considering the addition of bromocriptine, a dopamine agonist. [35]
If symptoms such as headache and vision changes are present in concert with elevated prolactin levels 4 times the upper limit of normal, assessment for possible pituitary tumors is warranted.
Research indicates an association between antipsychotics that elevate prolactin levels, a decrease in bone mineral density, and a higher incidence of hip fractures. [35] Although evidence is limited, there may be a link between elevated prolactin levels and increased breast cancer risk in patients with schizophrenia. [35]
Anticholinergic Effects
Antipsychotic medications may cause anticholinergic adverse effects, including urinary retention, blurred vision, tachycardia, and constipation, as well as cognitive difficulties, especially in older patients. Decreasing the dose is the first-choice management strategy for anticholinergic adverse effects. [35]
Cardiovascular Effects
- Hyperlipidemia, especially with clozapine and olanzapine
- Myocarditis and cardiomyopathy are rare side effects of clozapine
- Orthostatic hypotension due to alpha-receptor blocking effects, especially with clozapine and quetiapine
- QTc interval prolongation, raising the risk for ventricular tachyarrhythmia (torsades de pointes)
- Tachycardia as a response to orthostatic hypotension of anticholinergic effects
Metabolic Effects
Second-generation antipsychotic medications can cause significant weight gain and hypertension and elevate lipid and glucose levels. These adverse effects raise the risk of diabetes and cardiovascular disease and contribute to adverse health outcomes. Regular monitoring for metabolic side effects is crucial. Olanzapine and clozapine carry the most significant risk for metabolic syndrome. [35]
Initial management involves lifestyle changes and structured behavioral programs. Switching to an antipsychotic with a lower metabolic risk can also help with weight loss and improve metabolic health. Symptomatic treatments include statins for dyslipidemia, antihypertensives for hypertension, and metformin for weight loss. New weight loss drugs have not been tested explicitly for antipsychotic-induced weight gain and may exacerbate gastric hypomotility. Stimulant weight loss medications are not advised due to the risk of exacerbating psychosis. [35]
Insidious onset, childhood or adolescent onset, poor premorbid adjustment, substance use, and cognitive impairment are indicative of a poor prognostic outcome in schizophrenia. Acute onset and living in a developed country signal comparatively better prognostic factors. Suicide is the most common cause of premature death in schizophrenia, with two-thirds of patients reporting at least one episode of suicidal ideation. [37] While positive symptoms respond to antipsychotics, there is little evidence that antipsychotics substantially improve negative or cognitive symptoms other than in situations in which these are secondary to positive symptoms. [5] With appropriate psychopharmacological and psychosocial interventions, patients with schizophrenia can have improved outcomes; however, complete recovery is only seen in 13.5% of patients. [2] The life expectancy of someone with schizophrenia is about 15 years less than the general population. [5]
- Complications
Schizophrenia can lead to numerous complications. Patients often experience severe cognitive impairments, such as memory, attention, and decision-making difficulties, which can significantly affect daily functioning. Social withdrawal and isolation are common, as the struggle with social interactions leads to loneliness. There is a heightened risk of substance use disorders. Individuals with schizophrenia are also more susceptible to physical health issues like cardiovascular, metabolic, and infectious diseases. A significant complication is the increased risk of suicidal thoughts and behaviors. Maintaining employment and stable housing can be challenging due to the symptoms or frequent hospitalizations. Impaired personal care and hygiene, co-occurring mental health disorders like anxiety and depression, legal and financial problems, and the experience of stigmatization and discrimination further compound the challenges faced by those with schizophrenia. Effective management strategies, including medication, therapy, and comprehensive support services, such as housing and supportive employment, are crucial in mitigating these complications and improving overall quality of life.
- Deterrence and Patient Education
Educating patients about the diagnosis of schizophrenia and the benefits and risks of various psychopharmacological and psychosocial treatments is crucial in helping establish a therapeutic alliance and facilitating recovery. Contacting the 988 Suicide and Crisis Lifeline if the patient feels like harming themselves or someone else should be strongly encouraged. Patients should also be educated about the importance of compliance with antipsychotic medication, as well as with primary care to monitor the common medical comorbidities associated with serious mental illness and antipsychotic medication. Education about the risks of substance use and available treatments for any comorbid substance use disorder, including smoking cessation, is warranted.
- Enhancing Healthcare Team Outcomes
Providing patient-centered care for individuals with schizophrenia necessitates an interdisciplinary approach. The healthcare team includes psychiatrists, primary care physicians, advanced practitioners, psychologists, nurses, pharmacists, vocational rehabilitation therapists, occupational therapists, and social workers. Healthcare providers must have a deep understanding of schizophrenia's clinical aspects, including diagnosis, symptom management, and the complexities of psychopharmacological and psychotherapeutic treatments. This expertise is critical in interpreting psychiatric assessments, recognizing the range of symptoms, and understanding the challenges in managing acute and chronic phases of schizophrenia. In treating schizophrenia, ethical considerations are paramount, especially in respecting patient autonomy and ensuring informed consent for treatment plans.
Interprofessional collaboration is essential, with each team member contributing specialized knowledge and skills to optimize patient care. Effective communication within the team is critical to creating an environment where information is shared, concerns are addressed, and patient-centric strategies are developed. Physicians, advanced practitioners, nurses, pharmacists, and other healthcare professionals must work together to streamline the patient's journey, from diagnosis through treatment and follow-up. This coordination is vital for minimizing treatment errors, reducing delays in care, and enhancing patient safety. Ultimately, this leads to improved outcomes and patient-centered care that prioritizes the recovery of individuals with schizophrenia.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Manassa Hany declares no relevant financial relationships with ineligible companies.
Disclosure: Baryiah Rehman declares no relevant financial relationships with ineligible companies.
Disclosure: Abid Rizvi declares no relevant financial relationships with ineligible companies.
Disclosure: Jennifer Chapman declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Hany M, Rehman B, Rizvi A, et al. Schizophrenia. [Updated 2024 Feb 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- [Frontal dementia or dementia praecox? A case report of a psychotic disorder with a severe decline]. [Encephale. 2003] [Frontal dementia or dementia praecox? A case report of a psychotic disorder with a severe decline]. Vanderzeypen F, Bier JC, Genevrois C, Mendlewicz J, Lotstra F. Encephale. 2003 Mar-Apr; 29(2):172-80.
- [A rare and not very studied disorder: childhood-onset schizophrenia. A case report]. [Encephale. 2004] [A rare and not very studied disorder: childhood-onset schizophrenia. A case report]. Bailly D, de Chouly de Lenclave MB. Encephale. 2004 Nov-Dec; 30(6):540-7.
- Review [What support of young presenting a first psychotic episode, when schooling is being challenged?]. [Encephale. 2017] Review [What support of young presenting a first psychotic episode, when schooling is being challenged?]. Vacheron MN, Veyrat-Masson H, Wehbe E. Encephale. 2017 Dec; 43(6):570-576. Epub 2017 Nov 8.
- Psychiatry's contribution to the public stereotype of schizophrenia: Historical considerations. [J Eval Clin Pract. 2018] Psychiatry's contribution to the public stereotype of schizophrenia: Historical considerations. Katschnig H. J Eval Clin Pract. 2018 Oct; 24(5):1093-1100. Epub 2018 Aug 15.
- Review Prevention of suicide and attempted suicide in Denmark. Epidemiological studies of suicide and intervention studies in selected risk groups. [Dan Med Bull. 2007] Review Prevention of suicide and attempted suicide in Denmark. Epidemiological studies of suicide and intervention studies in selected risk groups. Nordentoft M. Dan Med Bull. 2007 Nov; 54(4):306-69.
Recent Activity
- Schizophrenia - StatPearls Schizophrenia - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Now Leaving PsychU
This link will take you outside of the psychu community website, sorry, this content is no longer available..
- Section Advisors
- Meet Our Field Medical Affairs Team
- Speakers Bureau
- Supporting Organizations
- Health Care Professionals
- Patient & Caregiver Resource Center
- Mental Health Disorders
- Bipolar Disorder
- PTSD/Trauma
- Schizophrenia
- Substance Use Disorders
- Topics of Interest
- Care Coordination
- Digital Health
- Diversity, Equity, & Inclusion
- Health Care Policy, Quality & Payer Administration
- Long-Term Care
- Suicide Awareness
- Virtual & Live Events
- Supporter Events
- Request a Presentation
- On-Demand Webinars
- Infographics
- Learning Tracks
- Shareable/Downloadable Content
- PsychU Roleplay
- Frameworks In Health & Quality Resources
- Mental Health System Guidebooks
- Psychiatric Scales
- Psychopharmacology
In this topic library devoted to schizophrenia you’ll find helpful resources for diagnosis and treatment—best-practice guidelines, decision-support tools, and research summaries. Each week, new content publishes, so check back often to stay up to date.

- Resource Library
Featured Resources
Editor's picks, most popular.

Trace Amine-Associated Receptor 1 (TAAR1): A Potential New Target For The Treatment Of Schizophrenia

Multiple States Easing Formulary Restrictions On Antipsychotics
The curious case of metabolic dysfunction in schizophrenia: who’s susceptible & why, linking neural circuits to dysfunction in schizophrenia.
Filter By Format
Filter By Topic
Social Determinants Of Health & Disruptive Life Events Among Patients With Schizophrenia Or Bipolar Disorder
Hot topics: clinical questions in schizophrenia – question ii, hot topics: clinical questions in schizophrenia – question i, hot topics: clinical questions in schizophrenia (part 6), trace amine-associated receptor 1 (taar1): a potential new target for the treatment of schizophrenia, antipsychotic-related stigma & the impact on treatment choices.
Upcoming Events
Virtual event – pathophysiology of agitation associated with alzheimer’s dementia (ad) – the potential role of the norepinephrine, serotonin & dopamine (nsd) neurotransmitter systems, virtual event – wellness in mental health: examining its neurobiology & clinical application, clinical perspectives on the impact of agitation in alzheimer’s dementia among the hispanic community, the danger of post-traumatic stress disorder (ptsd) stigma among marginalized communities.

Christoph Correll, MD
Schizophrenia Section Advisor
Ask A Question About Schizophrenia
Enter your question in the box below and click “Ask My Question” to submit your inquiry.
You must be logged in to ask a question in this section.
Disclaimer: The information provided by PsychU is intended for your educational benefit only. It is not intended as, nor is it a substitute for medical care or advice or professional diagnosis. Treatment-related questions will not be addressed. Users seeking medical advice should consult with their physician or other healthcare professional. Otsuka Pharmaceutical Development & Commercialization, Inc. (OPDC) operates in a highly regulated and scrutinized industry. Therefore, we may not be able to address every questions or topic submitted. Topics which may not be addressed may include, but are not limited to questions related to: (1) specific medications, (2) branded items, (3) clinical or treatment advice relating to specific patient conditions. The lack of response to certain questions or comments should not be taken as an agreement with the view posed or an admission of any kind.
REQUEST A PRESENTATION
Request a free educational program for your organization or region today! These customizable PsychU presentations are available both online and in-person, and cover a range of topics including: schizophrenia, major depressive disorder, bipolar disorder, care coordination, quality standards, and more.
Top Requested Presentations
Social Determinants Of Health
Agitation Associated With Alzheimer’s Dementia Disease State Education
The Importance Of Population Health: A Mental Health Perspective

Not sure where to start on the thousands of resources in the PsychU library? PsychU has created learning tracks to give community members a resource guide! Pick a learning track, review the materials outlined, and complete the Test Your Knowledge questions to participate in a resource ‘crash-course’ on one of the topics listed below.
Learning Tracks Topics
- Agitation In Dementia Associated With Alzheimers Disease
- Care Coordination & Integration
- Decriminalization Of Mental Illness
- Early Intervention In Psychosis
- Fundamentals of Pseudobulbar-Affect (PBA)
- Fundamentals of Schizophrenia
- Introduction To Neurobiology & Psychopharmacology
- Measurement-Based Care
- Metabolic Considerations In Depression
- PCP/Integrated Care
- PCP/Measurement Based Care
- Suicide Awareness & Prevention
Stay Connected:
- Anxiety Disorders
- Eating Disorders
- Personality Disorders
- Women’s Health
- Early Episode Psychosis
- Health Care Policy & Legislation
- Neuroscience
- Payer & Financing Models
- Quality Standards & Performance Measures
- Supporter Event
- Webinar Archive

IMAGES
COMMENTS
Schizophrenia is a serious mental health condition that affects how people think, feel and behave. It may result in a mix of hallucinations, delusions, and disorganized thinking and behavior. Hallucinations involve seeing things or hearing voices that aren't observed by others. Delusions involve firm beliefs about things that are not true.
Schizophrenia is frequently associated with significant distress and impairment in personal, family, social, educational, occupational, and other important areas of life. People with schizophrenia are 2 to 3 times more likely to die early than the general population (3). This is often due to physical illnesses, such as cardiovascular, metabolic ...
Print. Schizophrenia is a chronic brain disorder that affects less than one percent of the U.S. population. When schizophrenia is active, symptoms can include delusions, hallucinations, disorganized speech, trouble with thinking and lack of motivation. However, with treatment, most symptoms of schizophrenia will greatly improve and the ...
The symptoms of schizophrenia may be divided into the following 4 domains: Positive symptoms - Psychotic symptoms, such as hallucinations, which are usually auditory; delusions; and disorganized speech and behavior. Negative symptoms - A decrease in emotional range, poverty of speech, and loss of interests and drive; the person with ...
Schizophrenia is a progressive and recurring disease characterized by multiple psychotic relapses. This slide deck covers the course, natural history and prognosis of schizophrenia. Other slides discuss the key components of non-adherence in patients with schizophrenia, highlighting the value of a support system.
Schizophrenia is not one disorder, but rather a family of related disorders that displays characteristics of disorganized and delusional thinking, disturbed perceptions of reality, and inappropriate emotions and behaviors. Facts: Schizophrenia occurs in about 1 percent of the population (about 25 million people worldwide). It affects both men ...
Key facts. • Schizophrenia is a mental illness that affects • The diagnosis of schizophrenia is best made how the brain works. by a psychiatrist - a doctor with special training in mental illness. • People with schizophrenia experience psychosis, which means they can have • When someone with schizophrenia gets the serious problems ...
A presentation on 'Schizophrenia' that systematically gives an overview of the following:• Introduction (1:02)• Clinical features (2:04)• Schizophrenia in IC...
Challenges at Work. People with schizophrenia often have trouble finding or keeping a job. This is partly because the disease affects thinking, concentration, and communication. But it also stems ...
Schizophrenia is a serious mental illness that affects how a person thinks, feels, and behaves. People with schizophrenia may appear to have lost touch with reality, which can be distressing for them and their family and friends. The symptoms of schizophrenia can make it difficult to participate in usual, everyday activities, but effective ...
Schizophrenia is a serious mental illness that affects how a person thinks, feels, and behaves. People with schizophrenia may seem like they have lost touch with reality, which can be distressing for them and for their family and friends. The symptoms of schizophrenia can make it difficult to participate in usual, everyday activities, but ...
Presentation Transcript. Schizophrenia: Who is at Risk? • Lifetime prevalence • Epidemiologic Catchment Area Study: 1.3% • National Comorbidity Survey: 0.7% • Demographic characteristics • Age - typical onset late teens/early twenties • Gender - earlier age of onset among men • Marital status - less likely to be married.
isolating oneself from friends and family. changing friends or social groups. a change in focus and concentration. sleep problems. irritability and agitation. difficulties with schoolwork, or poor ...
INTRODUCTION. Schizophrenia is a psychiatric disorder involving chronic or recurrent psychosis. It is commonly associated with impairments in social and occupational functioning [].It is among the most disabling and economically catastrophic medical disorders, ranked by the World Health Organization as one of the top 10 illnesses contributing to the global burden of disease [].
Schizophrenia Leanne Stevens; Jennifer Stamp; and Kevin LeBlanc (editors) Approximate reading time: 18 minutes Schizophrenia is a devastating psychological disorder that is characterised by major disturbances in thought, perception, emotion and behaviour. About 1% of Canadians aged 10 and older are diagnosed with schizophrenia (Public Health Agency of Canada, 2019).
CLINICAL PRESENTATION. Schizophrenia is the most common functional psychotic disorder, and (as noted previously) individuals with the disorder can present with a variety of manifestations. Contrary to portrayals of the illness in the media, schizophrenia does not involve a "split personality." Rather, it is a chronic psychotic disorder that ...
Schizophrenia is a serious mental disorder in which people interpret reality abnormally—resulting in a combination of hallucinations, delusions, and exaggerated or irrational thinking and behavior. Less than one percent of people in the United States suffer from this illness. When people first experience symptoms and episodes, they are often ...
Schizophrenia is a serious mental illness that affects how a person thinks, feels, and behaves. People with schizophrenia may appear to have lost touch with reality, which can be distressing for them and their family and friends. The symptoms of schizophrenia can make it difficult to participate in usual, everyday activities, but effective ...
At least one of these must be (1), (2), or (3): Delusions. Hallucinations. Disorganized speech (e.g., frequent derailment or incoherence). Grossly disorganized or catatonic behavior. Negative symptoms (i.e., diminished emotional expression or avolition). Decreased functioning 2.6 months of symptoms with 1 month meeting criterion A. 3.Not ...
Schizophrenia is a disabling psychiatric condition impacting around 1% of people worldwide and ranking among the top 10 global disability causes.[1] Schizophrenia is characterized by positive psychotic symptoms such as hallucinations, delusions, disorganized speech, and disorganized or catatonic behavior; negative symptoms such as reduced motivation and expressiveness; and cognitive ...
REQUEST A PRESENTATION. Request a free educational program for your organization or region today! These customizable PsychU presentations are available both online and in-person, and cover a range of topics including: schizophrenia, major depressive disorder, bipolar disorder, care coordination, quality standards, and more. Top Requested ...