Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Fact sheets /

Climate change
- Climate change is directly contributing to humanitarian emergencies from heatwaves, wildfires, floods, tropical storms and hurricanes and they are increasing in scale, frequency and intensity.
- Research shows that 3.6 billion people already live in areas highly susceptible to climate change. Between 2030 and 2050, climate change is expected to cause approximately 250 000 additional deaths per year, from undernutrition, malaria, diarrhoea and heat stress alone.
- The direct damage costs to health (excluding costs in health-determining sectors such as agriculture and water and sanitation) is estimated to be between US$ 2–4 billion per year by 2030.
- Areas with weak health infrastructure – mostly in developing countries – will be the least able to cope without assistance to prepare and respond.
- Reducing emissions of greenhouse gases through better transport, food and energy use choices can result in very large gains for health, particularly through reduced air pollution.
Climate change presents a fundamental threat to human health. It affects the physical environment as well as all aspects of both natural and human systems – including social and economic conditions and the functioning of health systems. It is therefore a threat multiplier, undermining and potentially reversing decades of health progress. As climatic conditions change, more frequent and intensifying weather and climate events are observed, including storms, extreme heat, floods, droughts and wildfires. These weather and climate hazards affect health both directly and indirectly, increasing the risk of deaths, noncommunicable diseases, the emergence and spread of infectious diseases, and health emergencies.
Climate change is also having an impact on our health workforce and infrastructure, reducing capacity to provide universal health coverage (UHC). More fundamentally, climate shocks and growing stresses such as changing temperature and precipitation patterns, drought, floods and rising sea levels degrade the environmental and social determinants of physical and mental health. All aspects of health are affected by climate change, from clean air, water and soil to food systems and livelihoods. Further delay in tackling climate change will increase health risks, undermine decades of improvements in global health, and contravene our collective commitments to ensure the human right to health for all.
Climate change impacts on health
The Intergovernmental Panel on Climate Change's (IPCC) Sixth Assessment Report (AR6) concluded that climate risks are appearing faster and will become more severe sooner than previously expected, and it will be harder to adapt with increased global heating.
It further reveals that 3.6 billion people already live in areas highly susceptible to climate change. Despite contributing minimally to global emissions, low-income countries and small island developing states (SIDS) endure the harshest health impacts. In vulnerable regions, the death rate from extreme weather events in the last decade was 15 times higher than in less vulnerable ones.
Climate change is impacting health in a myriad of ways, including by leading to death and illness from increasingly frequent extreme weather events, such as heatwaves, storms and floods, the disruption of food systems, increases in zoonoses and food-, water- and vector-borne diseases, and mental health issues. Furthermore, climate change is undermining many of the social determinants for good health, such as livelihoods, equality and access to health care and social support structures. These climate-sensitive health risks are disproportionately felt by the most vulnerable and disadvantaged, including women, children, ethnic minorities, poor communities, migrants or displaced persons, older populations, and those with underlying health conditions.

Figure: An overview of climate-sensitive health risks, their exposure pathways and vulnerability factors. Climate change impacts health both directly and indirectly, and is strongly mediated by environmental, social and public health determinants.
Although it is unequivocal that climate change affects human health, it remains challenging to accurately estimate the scale and impact of many climate-sensitive health risks. However, scientific advances progressively allow us to attribute an increase in morbidity and mortality to global warming, and more accurately determine the risks and scale of these health threats.
WHO data indicates 2 billion people lack safe drinking water and 600 million suffer from foodborne illnesses annually, with children under 5 bearing 30% of foodborne fatalities. Climate stressors heighten waterborne and foodborne disease risks. In 2020, 770 million faced hunger, predominantly in Africa and Asia. Climate change affects food availability, quality and diversity, exacerbating food and nutrition crises.
Temperature and precipitation changes enhance the spread of vector-borne diseases. Without preventive actions, deaths from such diseases, currently over 700 000 annually, may rise. Climate change induces both immediate mental health issues, like anxiety and post-traumatic stress, and long-term disorders due to factors like displacement and disrupted social cohesion.
Recent research attributes 37% of heat-related deaths to human-induced climate change. Heat-related deaths among those over 65 have risen by 70% in two decades. In 2020, 98 million more experienced food insecurity compared to the 1981–2010 average. The WHO conservatively projects 250 000 additional yearly deaths by the 2030s due to climate change impacts on diseases like malaria and coastal flooding. However, modelling challenges persist, especially around capturing risks like drought and migration pressures.
The climate crisis threatens to undo the last 50 years of progress in development, global health and poverty reduction, and to further widen existing health inequalities between and within populations. It severely jeopardizes the realization of UHC in various ways, including by compounding the existing burden of disease and by exacerbating existing barriers to accessing health services, often at the times when they are most needed. Over 930 million people – around 12% of the world’s population – spend at least 10% of their household budget to pay for health care. With the poorest people largely uninsured, health shocks and stresses already currently push around 100 million people into poverty every year, with the impacts of climate change worsening this trend.
Climate change and equity
In the short- to medium-term, the health impacts of climate change will be determined mainly by the vulnerability of populations, their resilience to the current rate of climate change and the extent and pace of adaptation. In the longer-term, the effects will increasingly depend on the extent to which transformational action is taken now to reduce emissions and avoid the breaching of dangerous temperature thresholds and potential irreversible tipping points.
While no one is safe from these risks, the people whose health is being harmed first and worst by the climate crisis are the people who contribute least to its causes, and who are least able to protect themselves and their families against it: people in low-income and disadvantaged countries and communities.
Addressing climate change's health burden underscores the equity imperative: those most responsible for emissions should bear the highest mitigation and adaptation costs, emphasizing health equity and vulnerable group prioritization.
Need for urgent action
To avert catastrophic health impacts and prevent millions of climate change-related deaths, the world must limit temperature rise to 1.5°C. Past emissions have already made a certain level of global temperature rise and other changes to the climate inevitable. Global heating of even 1.5°C is not considered safe, however; every additional tenth of a degree of warming will take a serious toll on people’s lives and health.
WHO response
WHO’s response to these challenges centres around 3 main objectives:
- Promote actions that both reduce carbon emissions and improve health: supporting a rapid and equitable transition to a clean energy economy; ensuring that health is central to climate change mitigation policy; accelerating mitigation actions that bring the greatest health gains; and mobilizing the strength of the health community to drive policy change and build public support.
- Build better, more climate-resilient and environmentally sustainable health systems: ensuring core services, environmental sustainability and climate resilience as central components of UHC and primary health care (PHC); supporting health systems to leapfrog to cheaper, more reliable and cleaner solutions, while decarbonizing high-emitting health systems; and mainstreaming climate resilience and environmental sustainability into health service investments, including the capacity of the health workforce.
- Protect health from the wide range of impacts of climate change : assessing health vulnerabilities and developing health plans; integrating climate risk and implementing climate-informed surveillance and response systems for key risks, such as extreme heat and infectious disease; supporting resilience and adaptation in health-determining sectors such as water and food; and closing the financing gap for health adaptation and resilience.
Leadership and Raising Awareness : WHO leads in emphasizing climate change's health implications, aiming to centralize health in climate policies, including through the UNFCCC. Partnering with major health agencies, health professionals and civil society, WHO strives to embed climate change in health priorities like UHC and target carbon neutrality by 2030.
Evidence and Monitoring : WHO, with its network of global experts, contributes global evidence summaries, provides assistance to nations in their assessments, and monitors progress. The emphasis is on deploying effective policies and enhancing access to knowledge and data.
Capacity Building and Country Support : Through WHO offices, support is given to ministries of health, focusing on collaboration across sectors, updated guidance, hands-on training, and support for project preparation and execution as well as for securing climate and health funding. WHO leads the Alliance for Transformative Action on Climate and Health (ATACH) , bringing together a range of health and development partners, to support countries in achieving their commitments to climate-resilient and low carbon health systems.

Why climate change is still the greatest threat to human health
Polluted air and steadily rising temperatures are linked to health effects ranging from increased heart attacks and strokes to the spread of infectious diseases and psychological trauma.
People around the world are witnessing firsthand how climate change can wreak havoc on the planet. Steadily rising average temperatures fuel increasingly intense wildfires, hurricanes, and other disasters that are now impossible to ignore. And while the world has been plunged into a deadly pandemic, scientists are sounding the alarm once more that climate change is still the greatest threat to human health in recorded history .
As recently as August—when wildfires raged in the United States, Europe, and Siberia—World Health Organization Director-General Tedros Adhanom Ghebreyesus said in a statement that “the risks posed by climate change could dwarf those of any single disease.”
On September 5, more than 200 medical journals released an unprecedented joint editorial that urged world leaders to act. “The science is unequivocal,” they write. “A global increase of 1.5°C above the pre-industrial average and the continued loss of biodiversity risk catastrophic harm to health that will be impossible to reverse.”
Despite the acute dangers posed by COVID-19, the authors of the joint op-ed write that world governments “cannot wait for the pandemic to pass to rapidly reduce emissions.” Instead, they argue, everyone must treat climate change with the same urgency as they have COVID-19.
Here’s a look at the ways that climate change can affect your health—including some less obvious but still insidious effects—and why scientists say it’s not too late to avert catastrophe.
Air pollution
Climate change is caused by an increase of carbon dioxide and other greenhouse gases in Earth’s atmosphere, mostly from fossil fuel emissions. But burning fossil fuels can also have direct consequences for human health. That’s because the polluted air contains small particles that can induce stroke and heart attacks by penetrating the lungs and heart and even traveling into the bloodstream. Those particles might harm the organs directly or provoke an inflammatory response from the immune system as it tries to fight them off. Estimates suggest that air pollution causes anywhere between 3.6 million and nine million premature deaths a year.
“The numbers do vary,” says Andy Haines , professor of environmental change and public health at the London School of Hygiene and Tropical Medicine and author of the recently published book Planetary Health . “But they all agree that it’s a big public health burden.”

People over the age of 65 are most susceptible to the harmful effects of air pollution, but many others are at risk too, says Kari Nadeau , director of the Sean N. Parker Center for Allergy and Asthma Research at Stanford University. People who smoke or vape are at increased risk, as are children with asthma.
Air pollution also has consequences for those with allergies. Carbon dioxide increases the acidity of the air, which then pulls more pollen out from plants. For some people, this might just mean that they face annoyingly long bouts of seasonal allergies. But for others, it could be life-threatening.
“For people who already have respiratory disease, boy is that a problem,” Nadeau says. When pollen gets into the respiratory pathway, the body creates mucus to get rid of it, which can then fill up and suffocate the lungs.
Even healthy people can have similar outcomes if pollen levels are especially intense. In 2016, in the Australian state of Victoria, a severe thunderstorm combined with high levels of pollen to induce what The Lancet has described as “the world’s largest and most catastrophic epidemic of thunderstorm asthma.” So many residents suffered asthma attacks that emergency rooms were overwhelmed—and at least 10 people died as a result.
Climate change is also causing wildfires to get worse, and wildfire smoke is especially toxic. As one recent study showed, fires can account for 25 percent of dangerous air pollution in the U.S. Nadeau explains that the smoke contains particles of everything that the fire has consumed along its path—from rubber tires to harmful chemicals. These particles are tiny and can penetrate even deeper into a person’s lungs and organs. ( Here’s how breathing wildfire smoke affects the body .)
Extreme heat
Heat waves are deadly, but researchers at first didn’t see direct links between climate change and the harmful impacts of heat waves and other extreme weather events. Haines says the evidence base has been growing. “We have now got a number of studies which has shown that we can with high confidence attribute health outcomes to climate change,” he says.

Most recently, Haines points to a study published earlier this year in Nature Climate Change that attributes more than a third of heat-related deaths to climate change. As National Geographic reported at the time , the study found that the human toll was even higher in some countries with less access to air conditioning or other factors that render people more vulnerable to heat. ( How climate change is making heat waves even deadlier .)
That’s because the human body was not designed to cope with temperatures above 98.6°F, Nadeau says. Heat can break down muscles. The body does have some ways to deal with the heat—such as sweating. “But when it’s hot outside all the time, you cannot cope with that, and your heart muscles and cells start to literally die and degrade,” she says.
If you’re exposed to extreme heat for too long and are unable to adequately release that heat, the stress can cause a cascade of problems throughout the body. The heart has to work harder to pump blood to the rest of the organs, while sweat leeches the body of necessary minerals such as sodium and potassium. The combination can result in heart attacks and strokes .
Dehydration from heat exposure can also cause serious damage to the kidneys, which rely on water to function properly. For people whose kidneys are already beginning to fail—particularly older adults—Nadeau says that extreme heat can be a death sentence. “This is happening more and more,” she says.
Studies have also drawn links between higher temperatures and preterm birth and other pregnancy complications. It’s unclear why, but Haines says that one hypothesis is that extreme heat reduces blood flow to the fetus.
Food insecurity
One of the less direct—but no less harmful—ways that climate change can affect health is by disrupting the world’s supply of food.
You May Also Like

2024 hurricane season forecasted to be record-breaking year

Extreme heat is the future. Here are 10 practical ways to manage it.

The U.S. plans to limit PFAS in drinking water. What does that really mean?
Climate change both reduces the amount of food that’s available and makes it less nutritious. According to an Intergovernmental Panel on Climate Change (IPCC) special report , crop yields have already begun to decline as a result of rising temperatures, changing precipitation patterns, and extreme weather events. Meanwhile, studies have shown that increased carbon dioxide in the atmosphere can leech plants of zinc, iron, and protein—nutrients that humans need to survive.

Malnutrition is linked to a variety of illnesses, including heart disease, cancer, and diabetes. It can also increase the risk of stunting, or impaired growth , in children, which can harm cognitive function.
Climate change also imperils what we eat from the sea. Rising ocean temperatures have led many fish species to migrate toward Earth’s poles in search of cooler waters. Haines says that the resulting decline of fish stocks in subtropic regions “has big implications for nutrition,” because many of those coastal communities depend on fish for a substantial amount of the protein in their diets.
This effect is likely to be particularly harmful for Indigenous communities, says Tiff-Annie Kenny, a professor in the faculty of medicine at Laval University in Quebec who studies climate change and food security in the Canadian Arctic. It’s much more difficult for these communities to find alternative sources of protein, she says, either because it’s not there or because it’s too expensive. “So what are people going to eat instead?” she asks.
Infectious diseases
As the planet gets hotter, the geographic region where ticks and mosquitoes like to live is getting wider. These animals are well-known vectors of diseases such as the Zika virus, dengue fever, and malaria. As they cross the tropics of Cancer and Capricorn, Nadeau says, mosquitoes and ticks bring more opportunities for these diseases to infect greater swaths of the world.
“It used to be that they stayed in those little sectors near the Equator, but now unfortunately because of the warming of northern Europe and Canada, you can find Zika in places you wouldn’t have expected,” Nadeau says.
In addition, climate conditions such as temperature and humidity can impact the life cycle of mosquitoes. Haines says there’s particularly good evidence showing that, in some regions, climate change has altered these conditions in ways that increase the risk of mosquitos transmitting dengue .
There are also several ways in which climate change is increasing the risk of diseases that can be transmitted through water, such as cholera, typhoid fever, and parasites. Sometimes that’s fairly direct, such as when people interact with dirty floodwaters. But Haines says that drought can have indirect impacts when people, say, can’t wash their hands or are forced to drink from dodgier sources of freshwater.
Mental health
A common result of any climate-linked disaster is the toll on mental health. The distress caused by drastic environmental change is so significant that it has been given its own name— solastalgia .

Nadeau says that the effects on mental health have been apparent in her studies of emergency room visits arising from wildfires in the western U.S. People lose their homes, their jobs, and sometimes their loved ones, and that takes an immediate toll. “What’s the fastest acute issue that develops? It’s psychological,” she says. Extreme weather events such as wildfires and hurricanes cause so much stress and anxiety that they can lead to post-traumatic stress disorder and even suicide in the long run.
Another common factor is that climate change causes disproportionate harm to the world’s most vulnerable people. On September 2, the Environmental Protection Agency (EPA) released an analysis showing that racial and ethnic minority communities are particularly at risk . According to the report, if temperatures rise by 2°C (3.6°F), Black people are 40 percent more likely to live in areas with the highest projected increases in related deaths. Another 34 percent are more likely to live in areas with a rise in childhood asthma.
Further, the effects of climate change don’t occur in isolation. At any given time, a community might face air pollution, food insecurity, disease, and extreme heat all at once. Kenny says that’s particularly devastating in communities where the prevalence of food insecurity and poverty are already high. This situation hasn’t been adequately studied, she says, because “it’s difficult to capture these shocks that climate can bring.”
Why there’s reason for hope
In recent years, scientists and environmental activists have begun to push for more research into the myriad health effects of climate change. “One of the striking things is there’s been a real dearth of funding for climate change and health,” Haines says. “For that reason, some of the evidence we have is still fragmentary.”
Still, hope is not lost. In the Paris Agreement, countries around the world have pledged to limit global warming to below 2°C (3.6°F)—and preferably to 1.5°C (2.7°F)—by cutting their emissions. “When you reduce those emissions, you benefit health as well as the planet,” Haines says.
Meanwhile, scientists and environmental activists have put forward solutions that can help people adapt to the health effects of climate change. These include early heat warnings and dedicated cooling centers, more resilient supply chains, and freeing healthcare facilities from dependence on the electric grid.
Nadeau argues that the COVID-19 pandemic also presents an opportunity for world leaders to think bigger and more strategically. For example, the pandemic has laid bare problems with efficiency and equity that have many countries restructuring their healthcare facilities. In the process, she says, they can look for new ways to reduce waste and emissions, such as getting more hospitals using renewable energy.
“This is in our hands to do,” Nadeau says. “If we don’t do anything, that would be cataclysmic.”
Related Topics
- AIR POLLUTION
- WATER QUALITY
- NATURAL DISASTERS
- PUBLIC HEALTH
- CLIMATE CHANGE

Here’s what extreme heat does to the body

This summer's extreme weather is a sign of things to come

Some antibiotics are no longer as effective. That's as concerning as it sounds.

This African lake may literally explode—and millions are at risk

We got rid of BPA in some products—but are the substitutes any safer?
- Photography
- Environment
History & Culture
- History & Culture
- History Magazine
- Paid Content
- Terms of Use
- Privacy Policy
- Your US State Privacy Rights
- Children's Online Privacy Policy
- Interest-Based Ads
- About Nielsen Measurement
- Do Not Sell or Share My Personal Information
- Nat Geo Home
- Attend a Live Event
- Book a Trip
- Inspire Your Kids
- Shop Nat Geo
- Visit the D.C. Museum
- Learn About Our Impact
- Support Our Mission
- Advertise With Us
- Customer Service
- Renew Subscription
- Manage Your Subscription
- Work at Nat Geo
- Sign Up for Our Newsletters
- Contribute to Protect the Planet
Copyright © 1996-2015 National Geographic Society Copyright © 2015-2024 National Geographic Partners, LLC. All rights reserved
- Ways to Give
- Contact an Expert
- Explore WRI Perspectives
Filter Your Site Experience by Topic
Applying the filters below will filter all articles, data, insights and projects by the topic area you select.
- All Topics Remove filter
- Climate filter site by Climate
- Cities filter site by Cities
- Energy filter site by Energy
- Food filter site by Food
- Forests filter site by Forests
- Freshwater filter site by Freshwater
- Ocean filter site by Ocean
- Business filter site by Business
- Economics filter site by Economics
- Finance filter site by Finance
- Equity & Governance filter site by Equity & Governance
Search WRI.org
Not sure where to find something? Search all of the site's content.

How Climate Change Affects Health and How Countries Can Respond
- Climate Resilience
- adaptation finance
- climate change
- climatewatch-pinned
Since early 2020, the world’s attention has been on the global coronavirus pandemic. The pandemic continues to put massive stress on existing health systems, exposing their fault lines. As nations think about how to make health systems more resilient to current and future threats, one threat must not be overlooked: climate change is also impacting human health and straining heavily burdened health services everywhere.
Health-related risks linked to climate change range widely, from increased likelihood of transmitting vector-borne diseases to decreased access to services as a result of natural disasters. For example, air pollution — the sources of which are often the same as those that drive climate change — kills 4.2 million people every year and makes countless more sick and debilitated. Ground-level ozone, a key component of air pollution, is even more harmful to human health when temperatures are higher. Climate change events like hurricanes and floods can also destroy or limit access to health infrastructure and services.
Human health is a priority in 59% of countries’ national climate adaptation commitments under the Paris Agreement and close to half of countries acknowledge the negative health effects of climate change. However, countries struggle to understand specific climate risks to health, as well as how to identify and fund comprehensive health adaptation actions. Only 0.5% of multilateral climate finance targets health projects. Domestic funding for this issue is also minimal or nonexistent.
This is unacceptable considering the need for resilient and stable health systems.
A new paper by WRI showcases how countries can integrate health-related risks from climate change into their national climate and health strategies and put them into action. Doing so is essential, not only in preventing the worst impacts of climate change, but in keeping people healthy and nations prosperous.
How Does Climate Change Affect Human Health?
There are many ways health risks link to climate change, which often intersect with one another. Common risks include:
1. Increased risk of vector- and water-borne diseases.
Climate change is redistributing and increasing the optimal habitats for mosquitoes and other pathogens that carry disease. In some cases, these pathogens are bringing infectious diseases into communities that had not encountered them before. For example, warmer temperatures expand mosquito breeding ranges, causing malaria to shift upslope into new villages.
One study projects that, because of climate change, up to an additional 51.3 million people will be at risk from exposure to malaria in Western Africa by 2050. These shifts can heighten suffering, increase countries’ burdens of disease and cause epidemics. The World Health Organization (WHO) estimates that one-sixth of illness and disability suffered globally is due to vector-borne diseases, which are predicted to spread due to climate change.
Climate effects related to changing rainfall patterns, water quality and water scarcity can also trigger or worsen diseases within a country. For example, Ghana is now facing a higher prevalence of cholera, diarrhea, malaria and meningitis because flooding contaminates and exacerbates sanitation problems and water quality. Cholera outbreaks in Ghana have a high fatality rate and are particularly frequent during the rainy seasons and in coastal regions.
2. Increased risks to lives and livelihoods.
Similarly, higher temperatures and extreme events — such as intense rainfall, stronger cyclones and increased risk of landslides — can cause physical injuries, water contamination , decreased labor productivity and mental stress such as anxiety, depression and post-traumatic stress disorders. Hot weather and more intense heat waves reduce people’s ability to work and stay healthy; an environment that is too hot and humid makes it impossible for the human body to sweat and can lead to overheating and death.
Changes in the rainy seasons and other, slower-onset climate change risks like salt intrusion from rising sea levels can also negatively impact crop yields and food quality over time. This can lead to greater food insecurity and undernutrition. Bangladesh has the largest delta of any country in the world, and increasing salinity has already negatively affected its crop, fish and livestock production.
Even in places where agriculture yields may be boosted due to climate change, evidence has emerged that such increases can come at the expense of nutrition. These food security threats, in turn, affect people’s every day health, especially when it comes to child growth and development .
Environmental degradation and natural resources instability and competition exacerbated by climate impacts can also contribute to forced migration and social conflict . This can expose people to physical and mental health stressors, exacerbate existing health issues, lead to poorer living conditions and reduce access to affordable medical care.
3. Greater risk of social inequities.
The effects of climate change are especially felt by the most vulnerable , including people living in poverty, those who are marginalized or socially excluded, women, children, the elderly and those who are already ill or living with a disability. Without adequate support and funding, vulnerable groups will continue to suffer the most from the impacts of climate change on health.
The rising frequency, intensity and duration of extreme weather events will disproportionately impact the physical and economic capacities of people and households already struggling with weakened health and chronic disease. Due to their already debilitated or weakened immune systems, people with cardiovascular diseases, respiratory diseases and other pre-existing health conditions are at higher risk of injury or sickness from natural disasters and other climate-related risks.
The elderly and people who perform heavy physical labor, including agricultural laborers, are especially at risk from the effects of increasing heat and heat wave events, which stress the heart (possibly leading to cardiac arrest) and can cause severe dehydration, which damages other vital organs like the kidneys.
When combined with poorer nutrition and water stress, the result is often worse existing health problems, which can further entrench generational poverty and systemic vulnerabilities . This, in turn, contributes to heightened mortality and morbidity at a wider scale, increasing countries’ disease burdens.

What Are the Challenges to Integrating Climate Adaptation into Health Plans?
Several technical and financial challenges remain when it comes to incorporating climate-sensitive risks into health systems. Many countries and groups lack a strong understanding of the links between climate change and health. This is made more complicated when considering that cause-and-effect is difficult, and at times impossible, to prove.
While environmental health and public health officers can see the connections, policymakers may not understand them without proper training. These knowledge gaps can lead to inconsistent policies and a lack of adaptation activities in health budgets.
Many countries also have inadequate finance to implement adaptation and health activities.
As our case study illustrates, in Ghana, for instance, policymakers have limited human resources and skills available to identify and develop appropriate adaptation measures to reduce climate-sensitive health risks. As a result, it is difficult to persuade Parliament to dedicate an adequate budget for such activities. Frequent changes in administration can also make it difficult to ensure consistent allocation of public resources for adaptation in the health sector.
Despite being a priority in national policies and international commitments, technical and financial support requests to the NDC Partnership and multilateral climate funds like the Green Climate Fund often vastly underrepresent health-specific activities.
In a global review of more than 100 countries, the UN found that only one in five countries is spending enough to implement climate-related health commitments. This gap will be further exacerbated by 2030, when the direct damage costs to health are expected to be between $2 billion to $4 billion per year — even without considering indirect effects.
How Can Governments Adapt to Protect Human Health from the Effects of Climate Change?
While it can be difficult to identify, understand and reduce climate-sensitive health risks, a lack of information should not prevent action or delay no-regrets adaptation measures to strengthen health care systems. No-regrets measures include actions that protect communities whether climate impacts materialize as severely as expected or not, such as building robust food and medical supply chains, retrofitting technology and equipment, increasing training of medical staff and establishing protections against interrupted health services.
Governments can establish policy frameworks and collaboration mechanisms to provide needed guidance and support for no-regrets adaptation measures. Champions of climate and health issues inside and outside of the health sector can rally critical supporters and resources to influence policies and drive action.
Fiji, one of the most climate-vulnerable countries in the world, provides an excellent example of how to advance solutions. The nation developed and implemented its national Climate Change and Health Strategic Action Plan and integrated it into various policies and plans. The adaptation and health activities in Fiji’s plan are expected to increase the nation’s ability to provide and use reliable information on climate-sensitive health risks through an early warning system; improve capacity within health sector institutions to respond to these risks; and allow the nation to pilot disease prevention measures in higher-risk areas.
Fiji also set up a Climate Change and Health Unit within its Ministry of Health and allocated domestic funding to advance climate-health activities, like early warning systems, and build the capacity of health institutions to respond to climate threats. Health and climate change also remain on the political agenda thanks to the continuous efforts of and leadership from its Permanent Secretaries of the Ministry of Health, who encourage collaboration with other ministries.

Protecting the Health of Current and Future Generations
The links between climate change and health continue to grow in clarity and evidence. Policymakers can seize on the political momentum created by the global pandemic to strengthen their countries’ abilities to respond to a range of shocks and stressors — including the linked challenges of infectious disease and climate change. Strengthening the overall capacities and resources of health systems will increase adaptive capacity to deal with climate impacts, ensuring that current and future generations remain healthy.
Relevant Work
Key investments can build resilience to pandemics and climate change, 6 big findings from the ipcc 2022 report on climate impacts, adaptation and vulnerability, global emissions and local deforestation are combining to create dangerous levels of heat stress in the tropics, how floods in pakistan threaten global security, how you can help.
WRI relies on the generosity of donors like you to turn research into action. You can support our work by making a gift today or exploring other ways to give.
Stay Informed
World Resources Institute 10 G Street NE Suite 800 Washington DC 20002 +1 (202) 729-7600
© 2024 World Resources Institute
Envision a world where everyone can enjoy clean air, walkable cities, vibrant landscapes, nutritious food and affordable energy.
Newsroom Post
Climate change: a threat to human wellbeing and health of the planet. taking action now can secure our future.
BERLIN, Feb 28 – Human-induced climate change is causing dangerous and widespread disruption in nature and affecting the lives of billions of people around the world, despite efforts to reduce the risks. People and ecosystems least able to cope are being hardest hit, said scientists in the latest Intergovernmental Panel on Climate Change (IPCC) report, released today.
“This report is a dire warning about the consequences of inaction,” said Hoesung Lee, Chair of the IPCC. “It shows that climate change is a grave and mounting threat to our wellbeing and a healthy planet. Our actions today will shape how people adapt and nature responds to increasing climate risks.”
The world faces unavoidable multiple climate hazards over the next two decades with global warming of 1.5°C (2.7°F). Even temporarily exceeding this warming level will result in additional severe impacts, some of which will be irreversible. Risks for society will increase, including to infrastructure and low-lying coastal settlements.
The Summary for Policymakers of the IPCC Working Group II report, Climate Change 2022: Impacts, Adaptation and Vulnerability was approved on Sunday, February 27 2022, by 195 member governments of the IPCC, through a virtual approval session that was held over two weeks starting on February 14.
Urgent action required to deal with increasing risks
Increased heatwaves, droughts and floods are already exceeding plants’ and animals’ tolerance thresholds, driving mass mortalities in species such as trees and corals. These weather extremes are occurring simultaneously, causing cascading impacts that are increasingly difficult to manage. They have exposed millions of people to acute food and water insecurity, especially in Africa, Asia, Central and South America, on Small Islands and in the Arctic.
To avoid mounting loss of life, biodiversity and infrastructure, ambitious, accelerated action is required to adapt to climate change, at the same time as making rapid, deep cuts in greenhouse gas emissions. So far, progress on adaptation is uneven and there are increasing gaps between action taken and what is needed to deal with the increasing risks, the new report finds. These gaps are largest among lower-income populations.
The Working Group II report is the second instalment of the IPCC’s Sixth Assessment Report (AR6), which will be completed this year.
“This report recognizes the interdependence of climate, biodiversity and people and integrates natural, social and economic sciences more strongly than earlier IPCC assessments,” said Hoesung Lee. “It emphasizes the urgency of immediate and more ambitious action to address climate risks. Half measures are no longer an option.”
Safeguarding and strengthening nature is key to securing a liveable future
There are options to adapt to a changing climate. This report provides new insights into nature’s potential not only to reduce climate risks but also to improve people’s lives.
“Healthy ecosystems are more resilient to climate change and provide life-critical services such as food and clean water”, said IPCC Working Group II Co-Chair Hans-Otto Pörtner. “By restoring degraded ecosystems and effectively and equitably conserving 30 to 50 per cent of Earth’s land, freshwater and ocean habitats, society can benefit from nature’s capacity to absorb and store carbon, and we can accelerate progress towards sustainable development, but adequate finance and political support are essential.”
Scientists point out that climate change interacts with global trends such as unsustainable use of natural resources, growing urbanization, social inequalities, losses and damages from extreme events and a pandemic, jeopardizing future development.
“Our assessment clearly shows that tackling all these different challenges involves everyone – governments, the private sector, civil society – working together to prioritize risk reduction, as well as equity and justice, in decision-making and investment,” said IPCC Working Group II Co-Chair Debra Roberts.
“In this way, different interests, values and world views can be reconciled. By bringing together scientific and technological know-how as well as Indigenous and local knowledge, solutions will be more effective. Failure to achieve climate resilient and sustainable development will result in a sub-optimal future for people and nature.”
Cities: Hotspots of impacts and risks, but also a crucial part of the solution
This report provides a detailed assessment of climate change impacts, risks and adaptation in cities, where more than half the world’s population lives. People’s health, lives and livelihoods, as well as property and critical infrastructure, including energy and transportation systems, are being increasingly adversely affected by hazards from heatwaves, storms, drought and flooding as well as slow-onset changes, including sea level rise.
“Together, growing urbanization and climate change create complex risks, especially for those cities that already experience poorly planned urban growth, high levels of poverty and unemployment, and a lack of basic services,” Debra Roberts said.
“But cities also provide opportunities for climate action – green buildings, reliable supplies of clean water and renewable energy, and sustainable transport systems that connect urban and rural areas can all lead to a more inclusive, fairer society.”
There is increasing evidence of adaptation that has caused unintended consequences, for example destroying nature, putting peoples’ lives at risk or increasing greenhouse gas emissions. This can be avoided by involving everyone in planning, attention to equity and justice, and drawing on Indigenous and local knowledge.
A narrowing window for action
Climate change is a global challenge that requires local solutions and that’s why the Working Group II contribution to the IPCC’s Sixth Assessment Report (AR6) provides extensive regional information to enable Climate Resilient Development.
The report clearly states Climate Resilient Development is already challenging at current warming levels. It will become more limited if global warming exceeds 1.5°C (2.7°F). In some regions it will be impossible if global warming exceeds 2°C (3.6°F). This key finding underlines the urgency for climate action, focusing on equity and justice. Adequate funding, technology transfer, political commitment and partnership lead to more effective climate change adaptation and emissions reductions.
“The scientific evidence is unequivocal: climate change is a threat to human wellbeing and the health of the planet. Any further delay in concerted global action will miss a brief and rapidly closing window to secure a liveable future,” said Hans-Otto Pörtner.
For more information, please contact:
IPCC Press Office, Email: [email protected] IPCC Working Group II: Sina Löschke, Komila Nabiyeva: [email protected]
Notes for Editors
Climate Change 2022: Impacts, Adaptation and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change
The Working Group II report examines the impacts of climate change on nature and people around the globe. It explores future impacts at different levels of warming and the resulting risks and offers options to strengthen nature’s and society’s resilience to ongoing climate change, to fight hunger, poverty, and inequality and keep Earth a place worth living on – for current as well as for future generations.
Working Group II introduces several new components in its latest report: One is a special section on climate change impacts, risks and options to act for cities and settlements by the sea, tropical forests, mountains, biodiversity hotspots, dryland and deserts, the Mediterranean as well as the polar regions. Another is an atlas that will present data and findings on observed and projected climate change impacts and risks from global to regional scales, thus offering even more insights for decision makers.
The Summary for Policymakers of the Working Group II contribution to the Sixth Assessment Report (AR6) as well as additional materials and information are available at https://www.ipcc.ch/report/ar6/wg2/
Note : Originally scheduled for release in September 2021, the report was delayed for several months by the COVID-19 pandemic, as work in the scientific community including the IPCC shifted online. This is the second time that the IPCC has conducted a virtual approval session for one of its reports.
AR6 Working Group II in numbers
270 authors from 67 countries
- 47 – coordinating authors
- 184 – lead authors
- 39 – review editors
- 675 – contributing authors
Over 34,000 cited references
A total of 62,418 expert and government review comments
(First Order Draft 16,348; Second Order Draft 40,293; Final Government Distribution: 5,777)
More information about the Sixth Assessment Report can be found here .
Additional media resources
Assets available after the embargo is lifted on Media Essentials website .
Press conference recording, collection of sound bites from WGII authors, link to presentation slides, B-roll of approval session, link to launch Trello board including press release and video trailer in UN languages, a social media pack.
The website includes outreach materials such as videos about the IPCC and video recordings from outreach events conducted as webinars or live-streamed events.
Most videos published by the IPCC can be found on our YouTube channel. Credit for artwork
About the IPCC
The Intergovernmental Panel on Climate Change (IPCC) is the UN body for assessing the science related to climate change. It was established by the United Nations Environment Programme (UNEP) and the World Meteorological Organization (WMO) in 1988 to provide political leaders with periodic scientific assessments concerning climate change, its implications and risks, as well as to put forward adaptation and mitigation strategies. In the same year the UN General Assembly endorsed the action by the WMO and UNEP in jointly establishing the IPCC. It has 195 member states.
Thousands of people from all over the world contribute to the work of the IPCC. For the assessment reports, IPCC scientists volunteer their time to assess the thousands of scientific papers published each year to provide a comprehensive summary of what is known about the drivers of climate change, its impacts and future risks, and how adaptation and mitigation can reduce those risks.
The IPCC has three working groups: Working Group I , dealing with the physical science basis of climate change; Working Group II , dealing with impacts, adaptation and vulnerability; and Working Group III , dealing with the mitigation of climate change. It also has a Task Force on National Greenhouse Gas Inventories that develops methodologies for measuring emissions and removals. As part of the IPCC, a Task Group on Data Support for Climate Change Assessments (TG-Data) provides guidance to the Data Distribution Centre (DDC) on curation, traceability, stability, availability and transparency of data and scenarios related to the reports of the IPCC.
IPCC assessments provide governments, at all levels, with scientific information that they can use to develop climate policies. IPCC assessments are a key input into the international negotiations to tackle climate change. IPCC reports are drafted and reviewed in several stages, thus guaranteeing objectivity and transparency. An IPCC assessment report consists of the contributions of the three working groups and a Synthesis Report. The Synthesis Report integrates the findings of the three working group reports and of any special reports prepared in that assessment cycle.
About the Sixth Assessment Cycle
At its 41st Session in February 2015, the IPCC decided to produce a Sixth Assessment Report (AR6). At its 42nd Session in October 2015 it elected a new Bureau that would oversee the work on this report and the Special Reports to be produced in the assessment cycle.
Global Warming of 1.5°C , an IPCC special report on the impacts of global warming of 1.5 degrees Celsius above pre-industrial levels and related global greenhouse gas emission pathways, in the context of strengthening the global response to the threat of climate change, sustainable development, and efforts to eradicate poverty was launched in October 2018.
Climate Change and Land , an IPCC special report on climate change, desertification, land degradation, sustainable land management, food security, and greenhouse gas fluxes in terrestrial ecosystems was launched in August 2019, and the Special Report on the Ocean and Cryosphere in a Changing Climate was released in September 2019.
In May 2019 the IPCC released the 2019 Refinement to the 2006 IPCC Guidelines for National Greenhouse Gas Inventories , an update to the methodology used by governments to estimate their greenhouse gas emissions and removals.
In August 2021 the IPCC released the Working Group I contribution to the AR6, Climate Change 2021, the Physical Science Basis
The Working Group III contribution to the AR6 is scheduled for early April 2022.
The Synthesis Report of the Sixth Assessment Report will be completed in the second half of 2022.
For more information go to www.ipcc.ch
Related Content
Remarks by the ipcc chair during the press conference to present the working group ii contribution to the sixth assessment report.
Monday, 28 February 2022 Distinguished representatives of the media, WMO Secretary-General Petteri, UNEP Executive Director Andersen, We have just heard …
February 2022
Fifty-fifth session of the ipcc (ipcc-55) and twelfth session of working group ii (wgii-12), february 14, 2022, working group report, ar6 climate change 2022: impacts, adaptation and vulnerability.

Climate Change: Evidence and Causes: Update 2020 (2020)
Chapter: conclusion, c onclusion.
This document explains that there are well-understood physical mechanisms by which changes in the amounts of greenhouse gases cause climate changes. It discusses the evidence that the concentrations of these gases in the atmosphere have increased and are still increasing rapidly, that climate change is occurring, and that most of the recent change is almost certainly due to emissions of greenhouse gases caused by human activities. Further climate change is inevitable; if emissions of greenhouse gases continue unabated, future changes will substantially exceed those that have occurred so far. There remains a range of estimates of the magnitude and regional expression of future change, but increases in the extremes of climate that can adversely affect natural ecosystems and human activities and infrastructure are expected.
Citizens and governments can choose among several options (or a mixture of those options) in response to this information: they can change their pattern of energy production and usage in order to limit emissions of greenhouse gases and hence the magnitude of climate changes; they can wait for changes to occur and accept the losses, damage, and suffering that arise; they can adapt to actual and expected changes as much as possible; or they can seek as yet unproven “geoengineering” solutions to counteract some of the climate changes that would otherwise occur. Each of these options has risks, attractions and costs, and what is actually done may be a mixture of these different options. Different nations and communities will vary in their vulnerability and their capacity to adapt. There is an important debate to be had about choices among these options, to decide what is best for each group or nation, and most importantly for the global population as a whole. The options have to be discussed at a global scale because in many cases those communities that are most vulnerable control few of the emissions, either past or future. Our description of the science of climate change, with both its facts and its uncertainties, is offered as a basis to inform that policy debate.
A CKNOWLEDGEMENTS
The following individuals served as the primary writing team for the 2014 and 2020 editions of this document:
- Eric Wolff FRS, (UK lead), University of Cambridge
- Inez Fung (NAS, US lead), University of California, Berkeley
- Brian Hoskins FRS, Grantham Institute for Climate Change
- John F.B. Mitchell FRS, UK Met Office
- Tim Palmer FRS, University of Oxford
- Benjamin Santer (NAS), Lawrence Livermore National Laboratory
- John Shepherd FRS, University of Southampton
- Keith Shine FRS, University of Reading.
- Susan Solomon (NAS), Massachusetts Institute of Technology
- Kevin Trenberth, National Center for Atmospheric Research
- John Walsh, University of Alaska, Fairbanks
- Don Wuebbles, University of Illinois
Staff support for the 2020 revision was provided by Richard Walker, Amanda Purcell, Nancy Huddleston, and Michael Hudson. We offer special thanks to Rebecca Lindsey and NOAA Climate.gov for providing data and figure updates.
The following individuals served as reviewers of the 2014 document in accordance with procedures approved by the Royal Society and the National Academy of Sciences:
- Richard Alley (NAS), Department of Geosciences, Pennsylvania State University
- Alec Broers FRS, Former President of the Royal Academy of Engineering
- Harry Elderfield FRS, Department of Earth Sciences, University of Cambridge
- Joanna Haigh FRS, Professor of Atmospheric Physics, Imperial College London
- Isaac Held (NAS), NOAA Geophysical Fluid Dynamics Laboratory
- John Kutzbach (NAS), Center for Climatic Research, University of Wisconsin
- Jerry Meehl, Senior Scientist, National Center for Atmospheric Research
- John Pendry FRS, Imperial College London
- John Pyle FRS, Department of Chemistry, University of Cambridge
- Gavin Schmidt, NASA Goddard Space Flight Center
- Emily Shuckburgh, British Antarctic Survey
- Gabrielle Walker, Journalist
- Andrew Watson FRS, University of East Anglia
The Support for the 2014 Edition was provided by NAS Endowment Funds. We offer sincere thanks to the Ralph J. and Carol M. Cicerone Endowment for NAS Missions for supporting the production of this 2020 Edition.
F OR FURTHER READING
For more detailed discussion of the topics addressed in this document (including references to the underlying original research), see:
- Intergovernmental Panel on Climate Change (IPCC), 2019: Special Report on the Ocean and Cryosphere in a Changing Climate [ https://www.ipcc.ch/srocc ]
- National Academies of Sciences, Engineering, and Medicine (NASEM), 2019: Negative Emissions Technologies and Reliable Sequestration: A Research Agenda [ https://www.nap.edu/catalog/25259 ]
- Royal Society, 2018: Greenhouse gas removal [ https://raeng.org.uk/greenhousegasremoval ]
- U.S. Global Change Research Program (USGCRP), 2018: Fourth National Climate Assessment Volume II: Impacts, Risks, and Adaptation in the United States [ https://nca2018.globalchange.gov ]
- IPCC, 2018: Global Warming of 1.5°C [ https://www.ipcc.ch/sr15 ]
- USGCRP, 2017: Fourth National Climate Assessment Volume I: Climate Science Special Reports [ https://science2017.globalchange.gov ]
- NASEM, 2016: Attribution of Extreme Weather Events in the Context of Climate Change [ https://www.nap.edu/catalog/21852 ]
- IPCC, 2013: Fifth Assessment Report (AR5) Working Group 1. Climate Change 2013: The Physical Science Basis [ https://www.ipcc.ch/report/ar5/wg1 ]
- NRC, 2013: Abrupt Impacts of Climate Change: Anticipating Surprises [ https://www.nap.edu/catalog/18373 ]
- NRC, 2011: Climate Stabilization Targets: Emissions, Concentrations, and Impacts Over Decades to Millennia [ https://www.nap.edu/catalog/12877 ]
- Royal Society 2010: Climate Change: A Summary of the Science [ https://royalsociety.org/topics-policy/publications/2010/climate-change-summary-science ]
- NRC, 2010: America’s Climate Choices: Advancing the Science of Climate Change [ https://www.nap.edu/catalog/12782 ]
Much of the original data underlying the scientific findings discussed here are available at:
- https://data.ucar.edu/
- https://climatedataguide.ucar.edu
- https://iridl.ldeo.columbia.edu
- https://ess-dive.lbl.gov/
- https://www.ncdc.noaa.gov/
- https://www.esrl.noaa.gov/gmd/ccgg/trends/
- http://scrippsco2.ucsd.edu
- http://hahana.soest.hawaii.edu/hot/
| was established to advise the United States on scientific and technical issues when President Lincoln signed a Congressional charter in 1863. The National Research Council, the operating arm of the National Academy of Sciences and the National Academy of Engineering, has issued numerous reports on the causes of and potential responses to climate change. Climate change resources from the National Research Council are available at . | |
| is a self-governing Fellowship of many of the world’s most distinguished scientists. Its members are drawn from all areas of science, engineering, and medicine. It is the national academy of science in the UK. The Society’s fundamental purpose, reflected in its founding Charters of the 1660s, is to recognise, promote, and support excellence in science, and to encourage the development and use of science for the benefit of humanity. More information on the Society’s climate change work is available at |

Climate change is one of the defining issues of our time. It is now more certain than ever, based on many lines of evidence, that humans are changing Earth's climate. The Royal Society and the US National Academy of Sciences, with their similar missions to promote the use of science to benefit society and to inform critical policy debates, produced the original Climate Change: Evidence and Causes in 2014. It was written and reviewed by a UK-US team of leading climate scientists. This new edition, prepared by the same author team, has been updated with the most recent climate data and scientific analyses, all of which reinforce our understanding of human-caused climate change.
Scientific information is a vital component for society to make informed decisions about how to reduce the magnitude of climate change and how to adapt to its impacts. This booklet serves as a key reference document for decision makers, policy makers, educators, and others seeking authoritative answers about the current state of climate-change science.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
- Research article
- Open access
- Published: 01 June 2010
Reframing climate change as a public health issue: an exploratory study of public reactions
- Edward W Maibach 1 ,
- Matthew Nisbet 1 , 2 ,
- Paula Baldwin 1 ,
- Karen Akerlof 1 &
- Guoqing Diao 3
BMC Public Health volume 10 , Article number: 299 ( 2010 ) Cite this article
55k Accesses
264 Citations
213 Altmetric
Metrics details
Climate change is taking a toll on human health, and some leaders in the public health community have urged their colleagues to give voice to its health implications. Previous research has shown that Americans are only dimly aware of the health implications of climate change, yet the literature on issue framing suggests that providing a novel frame - such as human health - may be potentially useful in enhancing public engagement. We conducted an exploratory study in the United States of people's reactions to a public health-framed short essay on climate change.
U.S. adult respondents (n = 70), stratified by six previously identified audience segments, read the essay and were asked to highlight in green or pink any portions of the essay they found "especially clear and helpful" or alternatively "especially confusing or unhelpful." Two dependent measures were created: a composite sentence-specific score based on reactions to all 18 sentences in the essay; and respondents' general reactions to the essay that were coded for valence (positive, neutral, or negative). We tested the hypothesis that five of the six audience segments would respond positively to the essay on both dependent measures.
There was clear evidence that two of the five segments responded positively to the public health essay, and mixed evidence that two other responded positively. There was limited evidence that the fifth segment responded positively. Post-hoc analysis showed that five of the six segments responded more positively to information about the health benefits associated with mitigation-related policy actions than to information about the health risks of climate change.
Conclusions
Presentations about climate change that encourage people to consider its human health relevance appear likely to provide many Americans with a useful and engaging new frame of reference. Information about the potential health benefits of specific mitigation-related policy actions appears to be particularly compelling. We believe that the public health community has an important perspective to share about climate change, a perspective that makes the problem more personally relevant, significant, and understandable to members of the public.
Peer Review reports
Climate change is already taking a toll on human health in the United States [ 1 ] and other nations worldwide [ 2 ]. Unless greenhouse gas emissions worldwide are sharply curtailed - and significant actions taken to help communities adapt to changes in their climate that are unavoidable - the human toll of climate change is likely to become dramatically worse over the next several decades and beyond [ 3 ]. Globally, the human health impacts of climate change will continue to differentially affect the world's poorest nations, where populations endemically suffer myriad health burdens associated with extreme poverty that are being exacerbated by the changing climate. As stated in a recent British Medical Journal editorial, failure of the world's nations to successfully curtail emissions will likely lead to a "global health catastrophe" [ 4 ]. In developed countries such as the United States, the segments of the population most at risk are the poor, the very young, the elderly, those already in poor health, the disabled, individuals living alone, those with inadequate housing or basic services, and/or individuals who lack access to affordable health care or who live in areas with weak public health systems. These population segments disproportionately include racial, ethnic, and indigenous minorities [ 5 ].
While legislation to reduce U.S. greenhouse gas (GHG) emissions has stalled in Congress, in December 2009 the Environmental Protection Agency (EPA) moved toward regulating carbon dioxide and five other of the gases under the Clean Air Act, citing its authority to protect public health and welfare from the impacts of global warming [ 5 ]. The agency found that global warming poses public health risks - including increased morbidity and mortality - due to declining air quality, rising temperatures, increased frequency of extreme weather events, and higher incidences of food- and water-borne pathogens and allergens.
This finding comes as a relatively small group of public health professionals are working rapidly to better comprehend and quantify the nature and magnitude of these threats to human health and wellbeing [ 6 ]. This new but rapidly advancing public health focus has received minimal news media attention, even at internationally leading news organizations such as the New York Times [unpublished data]. It is not surprising therefore that the public also has yet to fully comprehend the public health implications of climate change. Recent surveys of Americans [ 7 ], Canadians [ 8 ], and Maltese [ 9 ] demonstrate that the human health consequences of climate change are seriously underestimated and/or poorly understood, if grasped at all. About half of American survey respondents, for example, selected "don't know" (rather than "none," "hundreds," "thousands," or "millions") when asked the estimated number of current and future (i.e. 50 years hence) injuries and illnesses, and death due to climate change. An earlier survey of Americans [ 10 ] demonstrated that most people see climate change as a geographically and temporally distant threat to the non-human environment. Notably, not a single survey respondent freely associated climate change as representing a threat to people. Similarly, few Canadians, without prompting, can name any specific human health threat linked to climate change impacts in their country [ 8 ].
Cognitive research over the past several decades has shown that how people "frame" an issue - i.e., how they mentally organize and discuss with others the issue's central ideas - greatly influences how they understand the nature of the problem, who or what they see as being responsible for the problem, and what they feel should be done to address the problem [ 11 , 12 ]. The polling data cited above [ 7 – 9 ] suggests that the dominant mental frame used by most members of the public to organize their conceptions about climate change is that of "climate change as an environmental problem." However, when climate change is framed as an environmental problem, this interpretation likely distances many people from the issue and contributes to a lack of serious and sustained public engagement necessary to develop solutions. This focus is also susceptible to a dominant counter frame that the best solution is to continue to grow the economy - paying for adaptive measures in the future when, theoretically, society will be wealthier and better able to afford them - rather than focus on the root causes of the environmental problem [ 13 ]. This economic frame likely leaves the public ambivalent about policy action and works to the advantage of industries that are reluctant to reduce their carbon intensity. Indeed, it is precisely the lack of a countervailing populist movement on climate change that has made policy solutions so difficult to enact [ 13 , 14 ].
Significant efforts have been made over the past several years by public health organizations to raise awareness of the public health implications of climate change and prepare the public health workforce to respond, although as noted above, it is not clear the extent to which public health professionals, journalists, or most importantly, the public and policy makers have taken notice. In the United States, National Public Health Week 2008 was themed "Climate Change: Our Health in the Balance," the Centers for Disease Control and Prevention created a Climate Change and Public Health program, and several professional associations assessed the public health system's readiness to respond to the emerging threat [ 15 – 17 ]. Globally, World Health Day 2008 was themed "Protecting Health from Climate Change," and the World Health Organization has developed a climate change and health work plan, the first objective of which is "raising awareness of the effects of climate change on health, in order to prompt action for public health measures" [ 18 ]. Several prominent medical journals have released special issues on climate change and health [ 19 – 21 ], and these and other medical journals [ 4 ] have issued strongly worded editorials urging health professionals to give voice to the health implications of climate change.
An important assumption in these calls to action is that there may be considerable value in introducing a public health frame into the ongoing public - and policy - dialogue about climate change. While there is indeed solid theoretical basis for this assumption, to the best of our knowledge there is not yet empirical evidence to support the validity of the assumption [ 22 ].
The purpose of this study therefore was to explore how American adults respond to an essay about climate change framed as a public health issue. Our hypothesis was that a public health-framed explanation of climate change would be perceived as useful and personally relevant by readers, with the exception of members of one small segment of Americans who dismiss the notion that human-induced climate change is happening. We used two dependent measures in this hypothesis: a composite score based on respondent reactions to each sentence in the essay, and the overall valence of respondents' general comments made after reading the essay.
Our study builds on previous research that identified six distinct segments of Americans, termed Global Warming's Six Americas [ 7 ]. These six segments of Americans - the Alarmed (18% of the adult population), the Concerned (33%), the Cautious (19%), the Disengaged (12%), the Doubtful (11%), and the Dismissive (7%) - fall along a continuum from those who are engaged on the issue and looking for ways to take appropriate actions (the Alarmed) to those who actively deny its reality and are looking for ways to oppose societal action (the Dismissive; see Figure 1 ). The four segments in the middle of the continuum are likely to benefit most from a reframing of climate change as a human health problem because, to a greater or lesser degree, they are not yet sure that they fully understand the issue and are still, if motivated to do so, relatively open to learning about new perspectives.
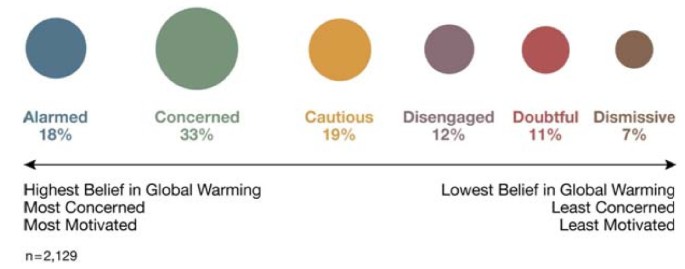
Global Warming's Six Americas . A nationally representative sample of American adults classified into six unique audience segments based on their climate change-related beliefs, behaviors and policy preferences.
Between May and August 2009, 74 adults were recruited to participate in semi-structured in-depth elicitation interviews that lasted an average of 43 minutes (ranging from 16 to 124 minutes) and included the presentation of a public health framed essay on climate change. The recruitment process was designed to yield completed interviews with a demographically and geographically diverse group of at least 10 people from each of the previously identified "Six Americas" [ 7 ]. Four respondents were dropped from this study due to incomplete data, leaving a sample size of 70. Audience segment status (i.e., which one of the "Six Americas" a person belonged) was assessed with a previously developed 15-item screening questionnaire that identifies segment status with 80% accuracy [unpublished data].
To achieve demographic diversity in the sample, we recruited an approximately balanced number of men and women, and an approximately balanced number of younger (18 to 30), middle-aged (31 to 50), and older (51 and older) adults (see Table 1 ). We did not set recruitment quotas for racial/ethnic groups, but did make an effort to recruit a mix of people from various racial/ethnic backgrounds.
To achieve geographic diversity, we recruited participants in one of two ways. The majority of participants (n = 56) were recruited - and then interviewed - face-to-face in one of two locations: out-of-town visitors were interviewed at a central location on the National Mall in Washington, DC (a national park situated between the U.S. Capitol, the Smithsonian Museum buildings, and the Lincoln Memorial); and shoppers were interviewed at an "outlet" mall (i.e., discount branded merchandise shopping mall) adjacent to an interstate freeway in Hagerstown, MD. The outlet mall is more than an hour driving distance outside of Washington, DC and attracts shoppers from Maryland, Pennsylvania, and West Virginia, as well as visitors from further away who are driving the interstate freeway. The remaining study participants were recruited via email from among participants to a nationally representative survey that we conducted in Fall 2008 [ 7 ]. They were interviewed subsequently by telephone, after being mailed a copy of the test "public health essay" - described below - in a sealed envelope marked "do not open until asked to do so by the interviewer." As an incentive to participate, all respondents were given a $50 gift card upon completion of their interview. George Mason University Human Subjects Review Board provided approval for the study protocol (reference #6161); all potential respondents received written consent information prior to participation.
The 70 study participants resided in 29 states. Using U.S. Census Bureau classifications, 14% (n = 10) were from the Northeast region, 21% (n = 15) were from the Midwest, 40% (n = 28) from the South, and 23% (n = 16) were from the West; state and region were unknown for one participant. In 2006, the geographic distribution of the overall U.S. population was 18%, 22%, 36% and 23% in the Northeast, Midwest, South and West, respectively [ 23 ].
Data Collection and Coding
The majority of the interview was devoted to open-ended questions intended to establish the respondent's emotions, attitudes, beliefs, knowledge and behavior relative to global warming's causes and consequences. For example, respective open-ended questions asked alternatively if, how, and for whom global warming was a problem; how global warming is caused; if and how global warming can be stopped or limited; and what, if anything, an individual could do to help limit global warming. Toward the end of the interview, respondents were asked to read "a brief essay about global warming" (see Appendix 1), which was designed to frame climate change as a human health issue. Respondents were also given a green and a pink highlighting pen and asked to "use the green highlighter pen to mark any portions of the essay that you feel are especially clear or helpful, and use the pink highlighter pen to mark any portions of the essay that are particularly confusing or unhelpful."
As shown in Appendix 1, the one page essay was organized into four sections: an opening paragraph that introduced the public health frame (5 total sentences); a paragraph that emphasized how human health will be harmed if action is not taken to stop, limit, and/or protect against global warming (i.e., a description of the threat; 7 sentences); a paragraph that discussed several mitigation-focused policy actions and their human health-related benefits if adopted (4 sentences); and a brief concluding paragraph intended to reinforce the public health frame (2 sentences).
When respondents finished the reading, they were asked to describe in an open-ended format their "general reaction to this essay." (Note: This question was inadvertently not asked of one respondent, therefore the sample size for analysis of this data is 69.) For each portion of the essay they marked in green, they were subsequently asked: "What about each of these sentences was especially clear or helpful to you?" For each portion of the essay they marked in pink, they were also asked: "What about each of these sentences was especially confusing or unhelpful to you?"
To evaluate the respondent's general reactions to the essay we reviewed their individual statements (n = 193), defined as discrete thoughts or concepts. Based on this review, we iteratively developed eight thematic categories that captured the range of statements made by respondents. Table 2 defines and describe these themes.
Two graduate student coders were then trained to code each statement into one of the thematic categories. The coders were also instructed to assess the overall valence of each respondent's statements - the first of our dependent measures - rating them as: -1 (entirely negative comments); 0 (mixed, including both positive and negative comments); or 1 (entirely positive comments). Following standard content analysis procedures, we tested inter-coder agreement on approximately 50 statements, making sure that a full range of possible types of coding decisions were required of the coders. To assess reliability, we used Krippendorff's alpha [ 24 , 25 ], a conservative measure that corrects for chance agreement among coders; a K-alpha of .70 or higher is considered sufficient and .80 or higher is considered excellent. For 7 of the 8 thematic categories, we achieved a reliability of .80 or higher; "Lack of Evidence or Stylistically Confusing" was the exception, with an inter-coder reliability of .70. After establishing reliability, the two coders then went on to categorize the rest of the remaining statements from the sample of respondents.
To code the respondent's sentence-specific reactions made with the highlighting pens, sentences marked with only green on at least one word were scored +1 (i.e. indicating "especially clear or useful"), sentences marked with only pink on at least one word were scored -1 (i.e. indicating "especially confusing or unhelpful), and sentences with either no highlighting, or both green and pink, were scored 0. Composite scores were created for each of the four sections of the essay - the opening, the threat section, the benefit section, and the conclusion - by summing the sentence-specific scores in the section and dividing by the number of sentences. A composite score for the entire essay - the second of the dependent measures in our hypothesis - was created by summing the sentence scores across each segment and dividing by the number of respondents per segment. Population estimates, which can be taken solely as preliminary indicators given the non-probabilistic nature of our sampling, were estimated by weighting the mean values for each of the six segments according to its prevalence in the U.S. population (see Figure 1 ).
Data Analysis
To test the between-segment differences in our dependent measures - overall reactions to the essay (i.e., valence) and composite sentence-specific reactions to the entire essay - we used the nonparametric Kruskal-Wallis test (see Figures 2 , 3 ). To test if the median response to the essay on each dependent measure was greater than zero (i.e., a positive reaction) for our full sample, we used the Wilcoxon signed rank test. Lastly, for both dependent measures, we used the Wilcoxon signed rank test to test our hypothesis that five of the six segments (the Dismissive being the one exception) would respond positively to the essay; the null hypothesis was that the median score for each of the five segments did not differ from zero. The Wilcoxon signed rank test is appropriate for small sample sizes and non-normal distributions, both of which are the case for at least some segments in our data.
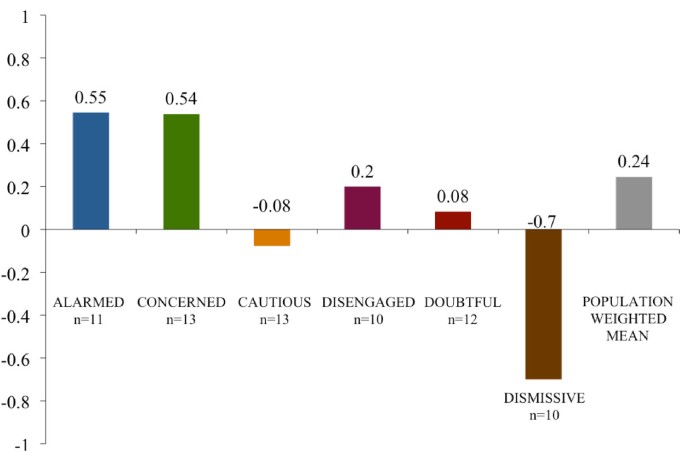
Average valence of respondents' general essay comments . The mean valence of respondent comments when asked their general reactions to the public health essay by audience segment and by a national population estimate. Note: 1 = (entirely positive comments); 0 = (mixed, including both positive and negative comments); and -1 = (entirely negative comments).
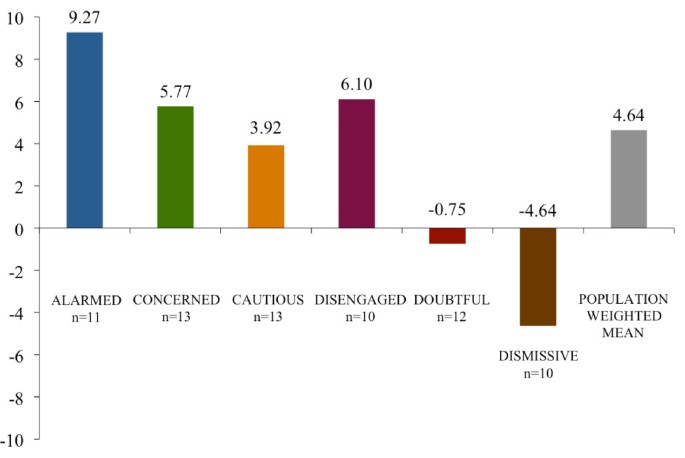
Composite essay scores by segment . Scores reflect respondent average values by segment for the difference between the number of times each of 18 sentences were marked "especially clear or helpful" and "especially confusing or unhelpful" with a full range of possible values between 18 and -18. The scores are adjusted for unequal numbers of respondents within each segment by re-weighting values to represent n = 10.
Post-hoc - after examining the visualized data (see Figures 4 , 5 and 6 ) - we decided to test for two possible main effects in the data. To examine the possibility that the essay's later focus on the public health benefits of mitigation-related policy actions was seen by respondents as clearer and more useful than the essay's earlier focus on public health-related threats, we calculated the difference between the re-scaled (by a factor of 10) average response to both the benefit and the threat sections and then used the Wilcoxon signed rank test to test, by segment, whether the median of these differences was greater than zero. We then evaluated the overall main effect of the essay - across all segments - using the weighted t-test on the differences with weights corresponding to the frequencies of the segments in the population.
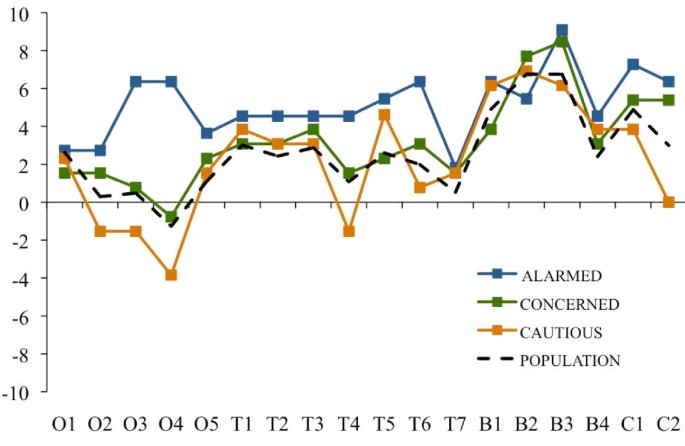
Essay evaluations by sentence: Alarmed, Concerned and Cautious segments . Sentence-specific evaluations of the public health essay by respondents in the Alarmed, Concerned and Cautious segments and by a national population estimate. Note: Scores reflect the difference between the number of times a sentence was marked as "especially clear or helpful" and the number of times it was marked as "especially confusing or unhelpful," adjusting for unequal numbers of respondents within each segment by re-weighting values to represent n = 10. Sentence abbreviations correspond to O = opening section (5 sentences); T = climate change health threat related section (7 sentences); B = mitigation-related policy actions and their health benefits (4 sentences); and C = concluding section (2 sentences). The national population estimate was created by weighting the values for each of the six segments according to their relative proportion of American adults.
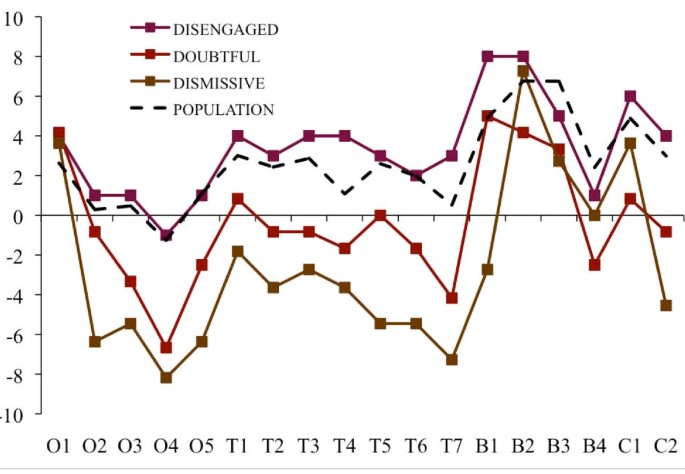
Essay evaluations by sentence: Disengaged, Doubtful and Dismissive segments . Sentence-specific evaluations of the public health essay by respondents in the Disengaged, Doubtful and Dismissive segments and by a national population estimate. Note: Scores reflect the difference between the number of times within a sentence was marked as "especially clear or helpful" and the number of times it was marked as "especially confusing or unhelpful," adjusting for unequal numbers of respondents within each segment by re-weighting values to represent n = 10. Sentence abbreviations correspond to O = opening section (5 sentences); T = climate change health threat related section (7 sentences); B = mitigation-related policy actions and their health benefits (4 sentences); and C = concluding section (2 sentences). The national population estimate was created by weighting the values for each of the six segments according to their relative proportion of American adults.
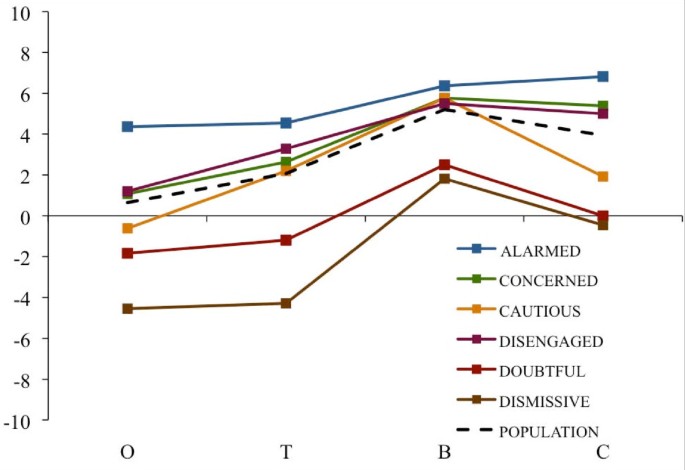
Essay evaluations by section (opening, threat, benefits, closing) . Average section-specific evaluations of the public health essay by respondents in each of the six audience segments and by a national population estimate. Note: Scores reflect the difference between the number of sentences within each section marked by a respondent as "especially clear or helpful" and those marked as "especially confusing or unhelpful" with those values averaged across the number of sentences per section and rescaled by a factor of 10. Section abbreviations correspond to O = opening section (5 sentences); T = climate change health threat related section (7 sentences); B = mitigation-related policy actions and their health benefits (4 sentences); and C = concluding section (2 sentences). The national population estimate was created by weighting the mean values for each of the six segments according to their relative proportion of American adults.
Lastly, to examine for the possibility that the concluding framing section of the essay was perceived by respondents as clearer and more useful than the opening framing section, we calculated the difference between the re-scaled average response to both the opening and the concluding sections and then used the Wilcoxon signed rank test to test, by segment, whether the median of these differences was greater than zero. We then evaluated the overall main effect - across all segments - using the weighted t-test on the differences with weights corresponding to the frequencies of the segments in the population.
Overall Sample Response and Between-Group Differences
The results of non-parametric Kruskal-Wallis tests indicate that there are significant between-group differences for both dependent measures: valence ( p = .001)and the composite sentence-specific score ( p < .0001). For the overall sample, the Wilcoxon signed rank tests indicated a positive response on the sentence-specific composite score ( p < .001) but not on the valence score ( p = .12). The average valence scores - on a scale of 1 to -1 - spanned from .55 (Alarmed) to -.7 (Dismissive) (see Figure 2 ). The average sentence-specific composite scores - on a scale of 18 to -18 - ranged from 9.27 (Alarmed) to -4.64 (Dismissive) (see Figure 3 ).
Hypothesis Test
The Wilcoxon signed rank tests indicated only partial support for our hypothesis. Using valence as the dependent measure, the null hypothesis can be rejected only for the Alarmed ( p = .04) and Concerned ( p = .02) segments, but not for the Cautious ( p = .50), Disengaged ( p = .36) or Doubtful segments ( p = .50). Using the composite sentence-specific score as the dependent measure, the null hypothesis can be rejected for the Alarmed ( p = .001), Concerned ( p < .01) and Cautious ( p = .01) segments, and marginally rejected for the Disengaged segment ( p = .06), but not for the Doubtful segment ( p = .61) segment.
In sum, there was clear evidence that the Alarmed and Concerned segments responded positively to the public health essay, and mixed evidence that the Cautious and Disengaged responded positively. There was no evidence that the Doubtful responded positively. It is worthy of note, however, that all six segments agreed with the essay's opening frame device (O1) that "good health is a great blessing," suggesting that human health and wellbeing is a widely shared value.
Table 3 summarizes the thematic content of the statements made by respondents when they were asked to discuss their general reactions to the public health essay. Across segments, not surprisingly, a substantial proportion of comments focused on the presentation of evidence or the stylistic tone of the essay. For the Alarmed and Concerned segments, roughly a third of their statements reflected personal agreement with the essay. In contrast, among the Dismissive, roughly a third of their statements characterized the essay as biased or alarmist. Relative to other possible reactions, substantial proportions of the statements made by the Concerned (18%), Cautious (19%), Disengaged (13%); and Doubtful (16%) indicated that the essay was informative and/or thought provoking.
Benefit versus Threat Statements
The Wilcoxon signed rank tests used to compare segments on the perceived clarity and helpfulness of the threat statements in the first part of the essay against the health benefits of mitigation-related policy actions in the second part of the essay showed a significant main effect ( p ≤ .05) for all segments except the Alarmed ( p = .17). The Dismissive segment showed the largest difference between the sections of the essay (6.10), followed by the Doubtful (3.69), the Cautious (3.57), the Concerned (3.13), and the Disengaged (2.12). Using a weighted t-test, the estimated gain from the Threat to Benefits sections across all segments was 3.17 ( p < .0001), with a 95% confidence interval of 1.85 to 4.49. In short, the health benefits associated with mitigation-related policy actions were seen as clearer and more useful than the preceding threat statements in the essay.
Also worthy of note, as Figures 4 and 5 indicate, is that all six segments reacted positively to the following statements focusing on specific mitigation-related policy actions that lead to human health benefits:
"Taking actions to limit global warming - by making our energy sources cleaner and our cars and appliances more efficient, by making our cities and towns friendlier to trains, buses, and bikers and walkers, and by improving the quality and safety of our food - will improve the health of almost every American."
"Cleaner energy sources and more efficient use of energy will lead to healthier air for children and adults to breathe."
"Improving the design of our cities and towns in ways that make it easier to get around on foot, by bike and on mass transit will reduce the number of cars and help people become more physically active, lose weight."
Conversely, respondents in all segments responded less positively to the statement:
"Increasing our consumption of fruits and vegetables, and reducing our intake of meat - especially beef - will help people maintain a healthy weight, will help prevent heart disease and cancer, and will play an important role in limiting global warming."
Opening versus Concluding Framing Statements
The Wilcoxon signed rank test used to compare segments on their reactions to the opening versus concluding framing statements for each segment showed a significant or marginally significant main effect in the Alarmed ( p = .07), Concerned ( p < .01), Cautious ( p = .05), Disengaged ( p = .03) and Dismissive ( p < .01) segments; the trend was not significant in the Doubtful ( p = .14) segment. The largest differences were seen in the Concerned segment (4.31), followed by the Dismissive (4.09), Disengaged (3.8), Cautious (2.54) and the Alarmed segment (2.45). Again using a weighted t-test, the estimated increase from the Opening to Concluding sections across all segments was 3.30 ( p < .0001), with a 95% confidence interval of 2.14 to 4.47.
On the whole, people who read our public health-framed essay about climate change reacted positively to the information. People in the Alarmed and the Concerned segments demonstrated consistent positive response to the information, while people in the Cautious, Disengaged, and Doubtful segments were less consistent. Although we did not treat it as a dependent measure per se, many of the respondents in all five segments made open-ended comments about the essay that demonstrated a positive engagement with the material. For example, nearly half (44%) of the comments made by the Disengaged segment indicated that the essay reflected their personal point of view, was informative or thought-provoking, or offered valuable prescriptive information on how to take action relative to the climate problem. Similarly, 39% of the comments made by respondents in the Doubtful segment reflected one of these three themes. Moreover, the ascending sentence-specific evaluations between the opening and concluding sections of the essay, for the sample overall and for all of the segments (excluding the Dismissive), suggest that the value of the public health frame may not be immediate, but rather may manifest more fully after people have had time to consider the evidence, especially when this evidence is presented with specific mitigation-related policy actions that are likely to have human health benefits.
One of the most intriguing findings in the study - albeit not definitive due to the order effect of the information in the essay - is the robustness of the response across all six segments to information about the health benefits of taking action to address global warming.
Overall, we interpret these collective findings as providing partial support for our hypothesis that information about climate change framed in ways that encourage people to consider its human health context provides many Americans with a useful and engaging new frame of reference and that this new interpretation may broaden the personal significance and relevance of the issue. Our methods were exploratory, however, and additional research on this question is needed. To that end, we are further analyzing the data already collected to determine more systematically which specific ideas are most and also least resonant with members of each segment. We are also planning an experimental test of climate education material framed in various ways, including a public health frame. Additional research is needed to determine if these findings generalize across nations and other populations.
In the U.S., these findings are especially relevant given the "issue fatigue" that appears to be developing with regard to climate change among at least certain segments of the American public [ 26 ]. Recent public opinion polls in the U.S. have shown a marked decline in the proportion of adults who are worried about global warming, and even relative to the proportion who are convinced that global warming is happening [ 27 – 29 ]. The public health voice may offer an important hedge against such issue fatigue.
Suggesting a novel frame for climate change - i.e., a frame that people had not previously considered - is potentially useful when it helps people understand the issue more clearly by providing additional personal and societal relevance [ 30 , 31 ]. Re-defining climate change in public health terms should help people make connections to already familiar problems such as asthma, allergies, and infectious diseases experienced in their communities, while shifting the visualization of the issue away from remote Arctic regions, and distant peoples and animals. In the process, giving climate change a public health focus suggests that there is a need to both mitigate (i.e. reduce greenhouse gas emissions) and adapt to the problem (i.e. protect communities and people from current and future health related impacts). The frame also presents the opportunity to involve additional trusted communication partners on the issue, notably public health experts and local community leaders [ 13 ].
In conclusion, we believe that the public health community has an important perspective to share about climate change, a perspective that potentially offers the public a more salient way to comprehend an issue that has proven deeply difficult for many people to fully comprehend. Moreover, the public health perspective offers a vision of a better, healthier future - not just a vision of environmental disaster averted, and it focuses on a range of possible policy actions that offer local as well as global benefits. Many leading experts in climate change communication, including the present authors, have suggested that a positive vision for the future and a localization of the issue is precisely what has been missing from the public dialogue on climate change thus far [ 13 , 22 , 32 ].
Not all aspects of the public health implications, however, may be engaging. Certain key recommendations, such as eating less meat, tended to elicit counter-arguments among people in many of the segments in our research. Our research provides clues about specific public health messages that might not be helpful, and suggests the need in future research to look carefully for examples or associations that trigger counter-arguments and negative reactions.
There is an urgent need for the public health community to successfully educate the public and policy makers about the serious human health implications of climate change, and to engage those publics in appropriate preventive and adaptive responses. As a point of strategy, however, our findings may suggest that continuing to communicate about the problem of climate change is not likely to generate wider public engagement. Instead public health voices may be wise to focus their communication on the solutions and the many co-benefits that matter most to people.
Global Warming is a Threat to Peoples' Health & Wellbeing
Most people agree with the sentiment that "good health is a great blessing." Although not yet widely known, global warming poses a very real threat to the health and wellbeing of Americans and other people around the world. Experts at the World Health Organization say that global warming is already leading to an increase in the rate of some diseases and is causing many deaths. If our government and other governments around the world do not soon take steps to limit global warming, a growing number of people in the United States will likely be harmed and killed. Conversely, if our government does take steps to limit global warming, our health and wellbeing will likely improve in a number of important ways.
Our health will suffer if we don't take action
Global warming can harm people both directly and indirectly. Directly, global warming causes more extreme weather patterns including more frequent heat waves, more violent storms, and rising sea-levels - all of which can lead to people being harmed or killed. Indirectly, global warming harms the quality of our water, air and food, and our ecosystems, all of which can lead to increasing rates of disease and death. If we do not act now to limit global warming, experts at the U.S. Centers for Disease Control and Prevention say that global warming will harm people in every region of the United States. As a result of the poor air quality caused by global warming, children will become more likely to develop asthma, and the asthma they suffer from will be more severe; adults who have heart and lung diseases will become more likely to be hospitalized or die from their illness. An increasing number of extreme heat waves, floods, storms, fires and droughts caused by the changes in our climate will lead to more people being injured or killed. New infectious diseases (such as West Nile Virus) and old infectious diseases that we had previously eradicated from the United States (such as malaria and Dengue Fever) are likely to become an increasing problem for us as our climate warms.
Our health will benefit if we do take action
According to a recent study published in the medical journal Lancet, taking actions to limit global warming - by making our energy sources cleaner and our cars and appliances more efficient, by making our cities and towns friendlier to trains, buses, and bikers and walkers, and by improving the quality and safety of our food - will improve the health of almost every American. Cleaner energy sources and more efficient use of energy will lead to healthier air for children and adults to breathe. Improving the design of our cities and towns in ways that make it easier and safer to get around on foot, by bike and on mass transit will reduce the number of cars on our roads and will help people become more physically active and lose weight. Increasing our consumption of fruits and vegetables, and reducing our intake of meat - especially beef - will help people maintain a healthy weight, will help prevent heart disease and cancer, and will play an important role in limiting global warming.
Peoples' health is dependent on the health of the environment in which we live. Global warming offers America an opportunity to make choices that are healthier for us, and for our climate.
Karl TR, Melillo JM, Peterson TC, (Eds): Global climate change impacts in the United States. 2009, Cambridge University Press
Google Scholar
IPCC: Climate change 2007: impacts, adaptation and vulnerability. Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Edited by: Parry ML, Canziani OF, Palutikof JP, van der Linden PJ, Hanson CE. 2007, Cambridge University Press
Frumkin H, McMichael AJ: Climate change and public health: thinking, acting and communicating. American Journal of Preventive Medicine. 2008, 35 (5): 403-410. 10.1016/j.amepre.2008.08.019.
Article PubMed Google Scholar
Jay M, Marmot MG: Health and climate change: will a global commitment be made at the UN climate change conference in December?. BMJ. 2009, 339: 645-646. 10.1136/bmj.b3669.
Article Google Scholar
Environmental Protection Agency: Endangerment and cause or contribute findings for greenhouse gases under Section 202(a) of the Clean Air Act. Federal Register. 2009, 74 (239): 66495-66546. [ http://www.epa.gov/climatechange/endangerment/downloads/Federal_Register-EPA-HQ-OAR-2009-0171-Dec.15-09.pdf ]
McMichael AJ, Woodruff RE, Hales S: Climate change and human health: present and future risks. Lancet. 2006, 367: 859-69. 10.1016/S0140-6736(06)68079-3.
Maibach EW, Roser-Renouf C, Leiserowitz A: Global warming's Six Americas 2009: an audience segmentation analysis. 2009, [ http://climatechange.gmu.edu ]
Berry P, Clarke K, Pajot M, Hutton D, Verret M: The role of risk perception and health communication in adapting to the health impacts of climate change in Canada. Natural Resources Canada. 2009, Ottawa, Canada
DeBono R: Maltese public perceptions on climate change and health. MPH thesis. 2009, University of Malta, Faculty of Medicine and Surgery
Leiserowitz A: American risk perceptions: is climate change dangerous?. Risk Anal. 2005, 25: 1433-42. 10.1111/j.1540-6261.2005.00690.x.
Gamson WA, Croteau D, Hoynes W, Sasson T: Media images and the social construction of reality. Annual Review of Sociology. 1992, 18: 373-93. 10.1146/annurev.so.18.080192.002105.
Price V, Nir L, Capella JN: Framing public discussion of gay civil unions. Public Opinion Quarterly. 2005, 69 (2): 179-212. 10.1093/poq/nfi014.
Nisbet MC: Communicating climate change: why frames matter to public engagement. Environment. 2009, 51 (2): 514-518.
Ockwell D, Whitmarsh L, O'Neill S: Reorienting climate change communication for effective mitigation: forcing people to be green or fostering grass roots engagement?. Science Communication. 2009, 30 (3): 305-327. 10.1177/1075547008328969.
Balbus J, Ebi K, Finzer L, Malina C, Chadwick A, McBride D, Chuk M, Maibach E: Are we ready?: preparing for the public health challenges of climate change. Environmental Defense Fund. 2008
Maibach EW, Chadwick A, McBride D, Chuk M, Ebi K, Balbus J: Climate change and local public health in the United States: Preparedness, programs and perceptions of local public health department directors. PLoS ONE. 2008, 3 (7): 10.1371/journal.pone.0002838.
Association of State and Territorial Health Officials: Climate change: a serious threat to public health. 2009, [ http://www.astho.org/Search.aspx?s=climate%20change ]
World Health Organization: WHO workplan on climate change and health. 2009, [ http://www.who.int/globalchange/wha_plans_objectives/en/index1.html ]
The Lancet. 2007, 370 (9591):
The Lancet. 2009, 374 (9707):
Frumkin H, McMichael AJ, Hess JJ, (Eds): Climate change and the health of the public. American Journal of Preventive Medicine. 2008, 35 (5):
Maibach EW, Roser-Renouf C, Leiserowitz A: Communication and marketing as climate change-intervention assets: A public health perspective. American Journal of Preventive Medicine. 2008, 35 (5): 488-500. 10.1016/j.amepre.2008.08.016.
U. S. Census Bureau: Census Bureau Regions and Divisions with State FIPS Codes. Retrieved April 21, 2010, [ http://www.census.gov/geo/www/us_regdiv.pdf ]
Hayes AF, Krippendorff K: Answering the call for a standard reliability measure for coding data. Communication Methods and Measures. 2007, 1: 77-89.
Krippendorff K: Content Analysis: An Introduction to Its Methodology. 1980, Newbury Park, CA: Sage
Kerr RA: Amid worrisome signs of warming, 'climate fatigue' sets in. Science. 2009, 326: 926-928. 10.1126/science.326.5955.926.
Article CAS PubMed Google Scholar
ABC News/Washington Post: Conservatives, Republicans move away from belief that the Earth is warming. [ http://abcnews.go.com/images/PollingUnit/1096a7GlobalWarming.pdf ]
Pew Research Center for the People & the Press: Fewer Americans see solid evidence of global warming. [ http://people-press.org/report/556/global-warming ]
Gallup: Increased number think global warming is "exaggerated.". [ http://www.gallup.com/poll/116590/Increased-Number-Think-Global-Warming-Exaggerated.aspx ]
Price V, Tewksbury D: News values and public opinion: a theoretical account of media priming and framing. Progress in the Communication Sciences. Edited by: Barnett GA, Boster FJ. 1997, New York: Ablex, 13: 173-212.
Scheufele DA, Tewksbury D: Framing, agenda setting and priming: the evolution of three media effects models. Journal of Communication. 2007, 57 (1): 9-20.
Moser SC, Dilling L: Creating a Climate for Change: Communicating Climate Change and Facilitating Social Change. 2007, Cambridge, UK: Cambridge University Press
Book Google Scholar
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-2458/10/299/prepub
Download references
Acknowledgements
This research was supported by a Robert Wood Johnson Foundation Health Policy Investigator Award.
Author information
Authors and affiliations.
Center for Climate Change Communication, Department of Communication, George Mason University, Fairfax, VA, USA
Edward W Maibach, Matthew Nisbet, Paula Baldwin & Karen Akerlof
School of Communication, American University, Washington, DC, USA
Matthew Nisbet
Department of Statistics, George Mason University, Fairfax, VA, USA
Guoqing Diao
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Edward W Maibach .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
EWM and MN developed the research question, participated in all aspects of the research, and wrote the first draft of the paper. PB coded and conducted preliminary data analysis. KA managed the data collection, conducted data analysis and prepared all figures and tables. GD conducted the final data analysis. All authors contributed to the final draft of the paper.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, authors’ original file for figure 3, authors’ original file for figure 4, authors’ original file for figure 5, authors’ original file for figure 6, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Maibach, E.W., Nisbet, M., Baldwin, P. et al. Reframing climate change as a public health issue: an exploratory study of public reactions. BMC Public Health 10 , 299 (2010). https://doi.org/10.1186/1471-2458-10-299
Download citation
Received : 04 January 2010
Accepted : 01 June 2010
Published : 01 June 2010
DOI : https://doi.org/10.1186/1471-2458-10-299
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Climate Change
- Global Warming
- West Nile Virus
- Dependent Measure
- Public Engagement
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
National Institute of Environmental Health Sciences
Your environment. your health., human health impacts of climate change.
Climate change impacts human health in both direct and indirect ways 1 , 2 . Extreme heat waves, rising sea level, changes in precipitation resulting in flooding and droughts, and intense hurricanes can directly cause injury, illness, and even death 3 . The effects of climate change can also indirectly affect health through alterations to the environment. For example, worsening air pollution levels can have negative impacts on respiratory and cardiovascular conditions 4 . Changes in temperature and rainfall can alter the survival, distribution, and behavior of insects and other species that can lead to changes in infectious diseases 5 . Increases in precipitation, storm surge, and sea temperature can lead to more water-related illnesses 6 . Climate change can also affect food safety, exposing people to contaminated foods that can result in foodborne illnesses 7 . In addition, climate change can affect mental health and well-being 8 , 9 .
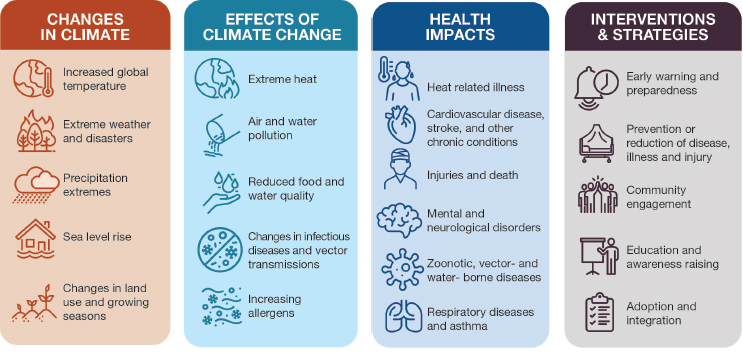
Exposure to climate-related hazards can include biological, chemical, or physical stressors and can differ in time, locations, populations, and severity. These are referred to as exposure pathways. These threats can occur simultaneously, resulting in compounding health impacts. Climate change threats may also accumulate over time, leading to longer-term changes in resilience and health.
Climate change can affect human health by changing the severity, duration, or frequency of health problems and by creating unprecedented or unanticipated health problems or health threats in places or populations where they have not previously occurred 10 . While everyone is exposed to climate-related health threats, not everyone experiences the same harms. Individuals may experience greater risk from climate-related health effects because: they have greater exposure to climate-related hazards; they are more sensitive to the effects of climate stressors; their own present state of health and wellbeing; or they do not have sufficient capacity or resources to cope or remove themselves from harm 11 . An effective public health response to mitigate the risks of climate change is essential to preventing injuries and illnesses and enhancing overall public health preparedness.
NIEHS supports research that can be used to make decisions that can help reduce the threats of climate change. In the 2016 report by the U.S. Global Change Research Program, The Impacts of Climate Change on Human Health: A Scientific Assessment , the Interagency Working Group on Climate Change and Health describes seven different types of health threats that help outline the major research areas. These include the following:
- Foodborne Illness and Nutrition
- Health Impacts of Air Quality
- Health Impacts of Extreme Weather Events
- Mental Health and Well-being
- People Who Are Vulnerable to Climate Change
- Temperature-Related Death and Illness
- Vector-borne Diseases
- Water-related Illnesses
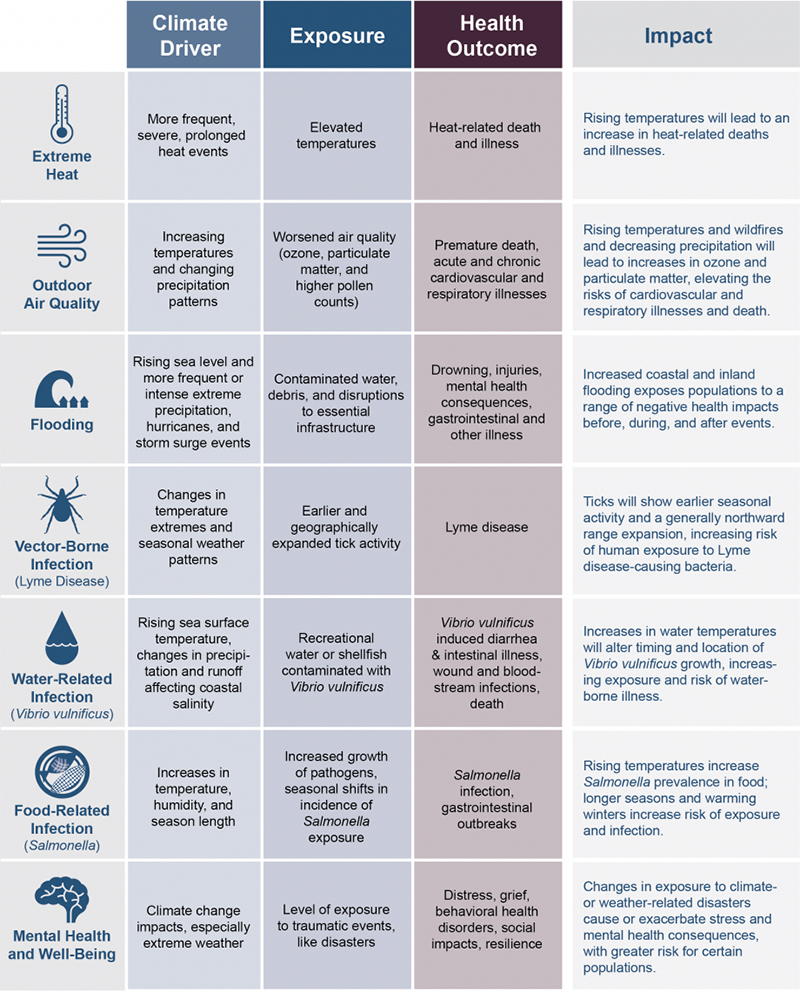
- Ebi K.L, Balbus JM, Luber G, Bole A, Crimmins A, Glass G, Saha S, Shimamoto MM, Trtanj J, and White-Newsome JL. 2018: Human Health. In Impacts, Risks, and Adaptation in the United States: Fourth National Climate Assessment, Volume II [Reidmiller, D.R., C.W. Avery, D.R. Easterling, K.E. Kunkel, K.L.M. Lewis, T.K. Maycock, and B.C. Stewart (eds.)]. U.S. Global Change Research Program, Washington, DC, USA, pp. 539–571. doi: 10.7930/NCA4. 2018. CH14. [ Full Text Ebi K.L, Balbus JM, Luber G, Bole A, Crimmins A, Glass G, Saha S, Shimamoto MM, Trtanj J, and White-Newsome JL. 2018: Human Health. In Impacts, Risks, and Adaptation in the United States: Fourth National Climate Assessment, Volume II [Reidmiller, D.R., C.W. Avery, D.R. Easterling, K.E. Kunkel, K.L.M. Lewis, T.K. Maycock, and B.C. Stewart (eds.)]. U.S. Global Change Research Program, Washington, DC, USA, pp. 539–571. doi: 10.7930/NCA4. 2018. CH14. ]
- IPCC, 2022: Climate Change 2022: Impacts, Adaptation, and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change [H.-O. Pörtner, D.C. Roberts, M. Tignor, E.S. Poloczanska, K. Mintenbeck, A. Alegría, M. Craig, S. Langsdorf, S. Löschke, V. Möller, A. Okem, B. Rama (eds.)]. Cambridge University Press. In Press. [ Full Text IPCC, 2022: Climate Change 2022: Impacts, Adaptation, and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change [H.-O. Pörtner, D.C. Roberts, M. Tignor, E.S. Poloczanska, K. Mintenbeck, A. Alegría, M. Craig, S. Langsdorf, S. Löschke, V. Möller, A. Okem, B. Rama (eds.)]. Cambridge University Press. In Press. ]
- IPCC, 2021: Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change [Masson-Delmotte, V., P. Zhai, A. Pirani, S.L. Connors, C. Péan, S. Berger, N. Caud, Y. Chen, L. Goldfarb, M.I. Gomis, M. Huang, K. Leitzell, E. Lonnoy, J.B.R. Matthews, T.K. Maycock, T. Waterfield, O. Yelekçi, R. Yu, and B. Zhou (eds.)]. Cambridge University Press. In Press. [ Full Text IPCC, 2021: Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change [Masson-Delmotte, V., P. Zhai, A. Pirani, S.L. Connors, C. Péan, S. Berger, N. Caud, Y. Chen, L. Goldfarb, M.I. Gomis, M. Huang, K. Leitzell, E. Lonnoy, J.B.R. Matthews, T.K. Maycock, T. Waterfield, O. Yelekçi, R. Yu, and B. Zhou (eds.)]. Cambridge University Press. In Press. ]
- Mills, Nicholas L., et al. Adverse cardiovascular effects of air pollution. Nature Clinical Practice Cardiovascular Medicine 6.1 (2009): 36-44. [ Full Text Mills, Nicholas L., et al. Adverse cardiovascular effects of air pollution. Nature Clinical Practice Cardiovascular Medicine 6.1 (2009): 36-44. ]
- Hunter, Paul R. Climate change and waterborne and vector‐borne disease. Journal of Applied Microbiology 94 (2003): 37-46. [ Full Text Hunter, Paul R. Climate change and waterborne and vector‐borne disease. Journal of Applied Microbiology 94 (2003): 37-46. ]
- Rose, Joan B., et al. Climate variability and change in the United States: potential impacts on water-and foodborne diseases caused by microbiologic agents. Environmental Health Perspectives 109.suppl 2 (2001): 211-221. [ Full Text Rose, Joan B., et al. Climate variability and change in the United States: potential impacts on water-and foodborne diseases caused by microbiologic agents. Environmental Health Perspectives 109.suppl 2 (2001): 211-221. ]
- Lake, Iain R., et al. A re-evaluation of the impact of temperature and climate change on foodborne illness. Epidemiology & Infection 137.11 (2009): 1538-1547. [ Full Text Lake, Iain R., et al. A re-evaluation of the impact of temperature and climate change on foodborne illness. Epidemiology & Infection 137.11 (2009): 1538-1547. ]
- Cissé, G., R. McLeman, H. Adams, P. Aldunce, K. Bowen, D. Campbell-Lendrum, S. Clayton, K.L. Ebi, J. Hess, C. Huang, Q. Liu, G. McGregor, J. Semenza, and M.C. Tirado, 2022: Health, Wellbeing, and the Changing Structure of Communities. In: Climate Change 2022: Impacts, Adaptation, and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change [H.-O. Pörtner, D.C. Roberts, M. Tignor, E.S. Poloczanska, K. Mintenbeck, A. Alegría, M. Craig, S. Langsdorf, S. Löschke, V. Möller, A. Okem, B. Rama (eds.)]. Cambridge University Press. In Press. [ Full Text Cissé, G., R. McLeman, H. Adams, P. Aldunce, K. Bowen, D. Campbell-Lendrum, S. Clayton, K.L. Ebi, J. Hess, C. Huang, Q. Liu, G. McGregor, J. Semenza, and M.C. Tirado, 2022: Health, Wellbeing, and the Changing Structure of Communities. In: Climate Change 2022: Impacts, Adaptation, and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change [H.-O. Pörtner, D.C. Roberts, M. Tignor, E.S. Poloczanska, K. Mintenbeck, A. Alegría, M. Craig, S. Langsdorf, S. Löschke, V. Möller, A. Okem, B. Rama (eds.)]. Cambridge University Press. In Press. ]
- Cianconi P, Betrò S, and Janiri L. 2020 The impact of climate change on mental health: a systematic descriptive review. Frontiers in Psychiatry, 11 (2020): 74. [ Abstract Cianconi P, Betrò S, and Janiri L. 2020 The impact of climate change on mental health: a systematic descriptive review. Frontiers in Psychiatry, 11 (2020): 74. ] [ Full Text Cianconi P, Betrò S, and Janiri L. 2020 The impact of climate change on mental health: a systematic descriptive review. Frontiers in Psychiatry, 11 (2020): 74. ]
- Balbus J, Crimmins A, Gamble JL, Easterling DR, Kunkel KE, Saha S, Sarofim MC. 2016. Chapter 1: Introduction: Climate Change and Human Health. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment. U.S. Global Change Research Program, Washington, DC, 25–42 . [ Abstract Balbus J, Crimmins A, Gamble JL, Easterling DR, Kunkel KE, Saha S, Sarofim MC. 2016. Chapter 1: Introduction: Climate Change and Human Health. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment. U.S. Global Change Research Program, Washington, DC, 25–42. ] [ Full Text Balbus J, Crimmins A, Gamble JL, Easterling DR, Kunkel KE, Saha S, Sarofim MC. 2016. Chapter 1: Introduction: Climate Change and Human Health. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment. U.S. Global Change Research Program, Washington, DC, 25–42. ]
- Benevolenza MA, DeRigne L. 2019. The impact of climate change and natural disasters on vulnerable populations: A systematic review of literature, Journal of Human Behavior in the Social Environment. 29:2, 266-281 . [ Abstract Benevolenza MA, DeRigne L. 2019. The impact of climate change and natural disasters on vulnerable populations: A systematic review of literature, Journal of Human Behavior in the Social Environment. 29:2, 266-281. ]
- Ebi K.L, Balbus JM, Luber G, Bole A, Crimmins A, Glass G, Saha S, Shimamoto MM, Trtanj J, and White-Newsome JL. 2018: Human Health. In Impacts, Risks, and Adaptation in the United States: Fourth National Climate Assessment, Volume II [Reidmiller, D.R., C.W. Avery, D.R. Easterling, K.E. Kunkel, K.L.M. Lewis, T.K. Maycock, and B.C. Stewart (eds.)]. U.S. Global Change Research Program, Washington, DC, USA, pp. 539–571. doi: 10.7930/NCA4. 2018. CH14. [ Full Text Ebi K.L, Balbus JM, Luber G, Bole A, Crimmins A, Glass G, Saha S, Shimamoto MM, Trtanj J, and White-Newsome JL. 2018: Human Health. In Impacts, Risks, and Adaptation in the United States: Fourth National Climate Assessment, Volume II [Reidmiller, D.R., C.W. Avery, D.R. Easterling, K.E. Kunkel, K.L.M. Lewis, T.K. Maycock, and B.C. Stewart (eds.)]. U.S. Global Change Research Program, Washington, DC, USA, pp. 539–571. doi: 10.7930/NCA4. 2018. CH14. ]
- IPCC, 2022: Climate Change 2022: Impacts, Adaptation, and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change [H.-O. Pörtner, D.C. Roberts, M. Tignor, E.S. Poloczanska, K. Mintenbeck, A. AlegrÃa, M. Craig, S. Langsdorf, S. Löschke, V. Möller, A. Okem, B. Rama (eds.)]. Cambridge University Press. In Press. [ Full Text IPCC, 2022: Climate Change 2022: Impacts, Adaptation, and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change [H.-O. Pörtner, D.C. Roberts, M. Tignor, E.S. Poloczanska, K. Mintenbeck, A. AlegrÃa, M. Craig, S. Langsdorf, S. Löschke, V. Möller, A. Okem, B. Rama (eds.)]. Cambridge University Press. In Press. ]
- IPCC, 2021: Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change [Masson-Delmotte, V., P. Zhai, A. Pirani, S.L. Connors, C. Péan, S. Berger, N. Caud, Y. Chen, L. Goldfarb, M.I. Gomis, M. Huang, K. Leitzell, E. Lonnoy, J.B.R. Matthews, T.K. Maycock, T. Waterfield, O. Yelekçi, R. Yu, and B. Zhou (eds.)]. Cambridge University Press. In Press. [ Full Text IPCC, 2021: Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change [Masson-Delmotte, V., P. Zhai, A. Pirani, S.L. Connors, C. Péan, S. Berger, N. Caud, Y. Chen, L. Goldfarb, M.I. Gomis, M. Huang, K. Leitzell, E. Lonnoy, J.B.R. Matthews, T.K. Maycock, T. Waterfield, O. Yelekçi, R. Yu, and B. Zhou (eds.)]. Cambridge University Press. In Press. ]
- Hunter, Paul R. Climate change and waterborne and vectorâ€borne disease. Journal of Applied Microbiology 94 (2003): 37-46. [ Full Text Hunter, Paul R. Climate change and waterborne and vectorâ€borne disease. Journal of Applied Microbiology 94 (2003): 37-46. ]
- Lake, Iain R., et al. A re-evaluation of the impact of temperature and climate change on foodborne illness. Epidemiology & Infection 137.11 (2009): 1538-1547. [ Full Text Lake, Iain R., et al. A re-evaluation of the impact of temperature and climate change on foodborne illness. Epidemiology & Infection 137.11 (2009): 1538-1547. ]
- Cissé, G., R. McLeman, H. Adams, P. Aldunce, K. Bowen, D. Campbell-Lendrum, S. Clayton, K.L. Ebi, J. Hess, C. Huang, Q. Liu, G. McGregor, J. Semenza, and M.C. Tirado, 2022: Health, Wellbeing, and the Changing Structure of Communities. In: Climate Change 2022: Impacts, Adaptation, and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change [H.-O. Pörtner, D.C. Roberts, M. Tignor, E.S. Poloczanska, K. Mintenbeck, A. AlegrÃa, M. Craig, S. Langsdorf, S. Löschke, V. Möller, A. Okem, B. Rama (eds.)]. Cambridge University Press. In Press. [ Full Text Cissé, G., R. McLeman, H. Adams, P. Aldunce, K. Bowen, D. Campbell-Lendrum, S. Clayton, K.L. Ebi, J. Hess, C. Huang, Q. Liu, G. McGregor, J. Semenza, and M.C. Tirado, 2022: Health, Wellbeing, and the Changing Structure of Communities. In: Climate Change 2022: Impacts, Adaptation, and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change [H.-O. Pörtner, D.C. Roberts, M. Tignor, E.S. Poloczanska, K. Mintenbeck, A. AlegrÃa, M. Craig, S. Langsdorf, S. Löschke, V. Möller, A. Okem, B. Rama (eds.)]. Cambridge University Press. In Press. ]
- Cianconi P, Betrò S, and Janiri L. 2020 The impact of climate change on mental health: a systematic descriptive review. Frontiers in Psychiatry, 11 (2020): 74. [ Abstract Cianconi P, Betrò S, and Janiri L. 2020 The impact of climate change on mental health: a systematic descriptive review. Frontiers in Psychiatry, 11 (2020): 74. ] [ Full Text Cianconi P, Betrò S, and Janiri L. 2020 The impact of climate change on mental health: a systematic descriptive review. Frontiers in Psychiatry, 11 (2020): 74. ]
- Balbus J, Crimmins A, Gamble JL, Easterling DR, Kunkel KE, Saha S, Sarofim MC. 2016. Chapter 1: Introduction: Climate Change and Human Health. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment. U.S. Global Change Research Program, Washington, DC, 25–42 . [ Abstract Balbus J, Crimmins A, Gamble JL, Easterling DR, Kunkel KE, Saha S, Sarofim MC. 2016. Chapter 1: Introduction: Climate Change and Human Health. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment. U.S. Global Change Research Program, Washington, DC, 25–42. ] [ Full Text Balbus J, Crimmins A, Gamble JL, Easterling DR, Kunkel KE, Saha S, Sarofim MC. 2016. Chapter 1: Introduction: Climate Change and Human Health. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment. U.S. Global Change Research Program, Washington, DC, 25–42. ]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Climate Change, Health and Existential Risks to Civilization: A Comprehensive Review (1989–2013)
Associated data.
Background: Anthropogenic global warming, interacting with social and other environmental determinants, constitutes a profound health risk. This paper reports a comprehensive literature review for 1989–2013 (inclusive), the first 25 years in which this topic appeared in scientific journals. It explores the extent to which articles have identified potentially catastrophic, civilization-endangering health risks associated with climate change. Methods: PubMed and Google Scholar were primarily used to identify articles which were then ranked on a three-point scale. Each score reflected the extent to which papers discussed global systemic risk. Citations were also analyzed. Results : Of 2143 analyzed papers 1546 (72%) were scored as one. Their citations (165,133) were 82% of the total. The proportion of annual papers scored as three was initially high, as were their citations but declined to almost zero by 1996, before rising slightly from 2006. Conclusions : The enormous expansion of the literature appropriately reflects increased understanding of the importance of climate change to global health. However, recognition of the most severe, existential, health risks from climate change was generally low. Most papers instead focused on infectious diseases, direct heat effects and other disciplinary-bounded phenomena and consequences, even though scientific advances have long called for more inter-disciplinary collaboration.
1. Introduction
In 1988 the leading climate scientist James Hansen, of the National Aeronautics and Space Administration, with three other senior researchers, testified to a U.S. Congressional committee that it was 99 percent certain that the warming trend in Earth’s temperature that was then observed was not natural variation but was caused by the accumulation of carbon dioxide and other “greenhouse” gases. This testimony was reported prominently in the New York Times [ 1 , 2 ]. Hansen was criticized then, and many times since, for his “adventurous” interpretation of climate data, however the publicity which followed his testimony, itself reflecting a decade of growing agitation about the geo-political impacts of climate change [ 2 ] may have influenced health workers to think more deeply about the issues. In any case, within a year, a Lancet editorial discussed health and the “greenhouse effect” [ 3 ], possibly the first such publication in a health journal, eight years after a chapter concerning climate change and parasitic disease appeared [ 4 ]. At least six other chapters on this topic were published in the 1980s, as well as at least two reports. For details, see [ 5 ]. Two other journal articles concerning climate change and health were also published in 1989 [ 6 , 7 ].
The 1989 editorial stated “global warming, increased ultraviolet flux, and higher levels of tropospheric ozone will reduce crop production, with potentially devastating effects on world food supplies. Malnutrition (sic) might then become commonplace, even among developed nations, and armed conflicts would be more likely as countries compete for a dwindling supply of natural resources” [ 3 ]. In the New England Journal of Medicine, Leaf warned, also in 1989, of sea level rise, especially in the south-eastern U.S. state of Florida, higher precipitation, millions of environmental refugees, an increased risk of drought and the possibility that warming at higher latitudes would not fully compensate any climate change related loss of agricultural productivity towards the equator [ 6 ]. The third paper published that year [ 7 ] was even more direct, warning of “catastrophic” consequences to human health and well-being.
In the early 1990s, warnings of potentially catastrophic consequences of climate change continued to dominate. Yet, by the turn of the millennium, the author had formed the impression that the scientific publishing milieu was becoming less receptive to the message that climate change and other forms of “planetary overload” [ 8 ] pose existential, civilization-wide risks. This was disturbing, as my own confirmation bias seemed to support the case that the evidence of existential risk was continuing to rise [ 9 , 10 ].
That the health risks from climate change are indeed extraordinarily high was stressed in the 2009 publication of the lengthy (41 page) article by the Lancet and University College London Institute for Global Health Commission, which described climate change as the “biggest global health threat of the 21st century” [ 11 ]. Yet, although this paper attracted considerable attention at the time, the long-term outlook for climate change and health has since continued to deteriorate.
By existential, I mean related to the word “existence”. But it is not the continued existence of Earth that is in doubt, but instead the existence of a high level of function of civilization, one in which prospects of “health for many” (though no longer “health for all”) are realistic and even improving [ 12 ]. Existential risk does not necessarily mean that global civilization will collapse. Nor does it exclude pockets of order and even prosperity enduring for generations, from which global or quasi-global civilization may one day emerge, provided worst case scenarios are avoided, such as runaway climate change and nuclear war leading to nuclear winter [ 13 ]. Compared to today, such prospects should be recognized as catastrophic. Unchecked climate change could generate similar, or bleaker, global futures. Seeking to minimize such possibilities should be seen as a major responsibility for all workers concerned with sustaining and improving global public health.
There is reticence [ 14 , 15 ], shared by many authors, reviewers, journals, funders and media outlets to discuss the possibility of such existential risks. Nonetheless, the consequences for health are so vast that discussion is warranted. This paper seeks to do that, in the process conducting the largest review on the topic of climate change and health yet to be published.
1.1. Climate Change Science, Risk and the 2015 Paris Agreement
The scientific knowledge that gases, accumulating mainly from the burning of fossil fuels and the clearing of forests, add to the natural “greenhouse effect” has been known since the 19th century [ 16 ]. In 1957 scientists observed “human beings are now carrying out a largescale geophysical experiment of a kind which could not have happened in the past nor be reproduced in the future. Within a few hundred years we are returning to the air and oceans the concentrated organic carbon stored over hundreds of millions of years” [ 17 ].
In 2015 the Paris climate change agreement, negotiated by representatives of 196 parties (195 nations and the European Union) committed countries (thus, effectively, civilization), upon ratification, to actions that would seek to restrict average global warming to “well below” 2 °C above “pre-industrial” levels and to “pursue efforts” to limit the rise to 1.5 °C. The text of the Paris Agreement defines neither the pre-industrial temperature nor the time for this baseline, but most experts agree that it means the temperature in the late 18th or 19th century, soon after the start of the industrial revolution, when coal burning increased. This time is after the end of the Little Ice Age, which itself was accompanied by a rebound in average temperatures, independent of the slow rise in greenhouse gases (chiefly methane and nitrous oxide as well as carbon dioxide) that occurred throughout the 19th century. Estimates of global warming for the period 1861–1880 until 2015 range from 0.93 °C [ 18 ] to 1.12 °C [ 19 ].
Although the goal of 1.5 °C is widely known, there is less understanding that meeting this challenge would not guarantee safety from a climate change perspective [ 20 ]. Indeed, if it were to be more widely accepted that climate change has already contributed to the Syrian war [ 21 , 22 ], to the rise in global food prices which accompanied the 2010 drought and heatwave in Russia [ 23 , 24 ], and the 2018 wildfire season in the Northern Hemisphere, then the threshold of danger might already be widely seen as having long been exceeded.
In recent years the science concerning the physical impacts of climate has continued to expand and to disturb. Average global temperatures continue to rise [ 25 ], apparently in a process more “stepped” than as a trend [ 26 ] with record average global heat in both El Niño and La Niña years. Loss of ice from both Antarctica and Greenland is increasing and the rate of sea level rise is consequently accelerating [ 27 ]. Property values in parts of the U.S. East Coast may soon fall, due to sea level rise [ 28 ]. There is growing concern about more intense rainfall [ 29 , 30 ], fires worsened by heat and drought [ 31 ], a weakening Gulf Stream [ 32 ] and increased sinuosity of the jet stream, which can cause unusual cold at lower latitudes, even if the average global temperature is rising [ 33 , 34 ]. The projected trend toward a weaker and poleward-shifted jet stream is also consistent with projections of a significantly increased risk of worsening extreme heat and dryness in the Northern Hemisphere [ 35 ].
There is also growing evidence of greenhouse effect-intensifying feedbacks in the Earth system [ 36 ] that might release enormous quantities of carbon dioxide and methane, independent of fossil fuel combustion, agriculture or deforestation, from sources including warming tundra and increased fires, both of peat and forests [ 37 , 38 ]. Such releases could dwarf the climate saving made possible by the putative implementation of the Paris climate agreement. The strength of the oceanic carbon sink is also weakening [ 39 ]. If this intensifies it is likely to accelerate warming of the atmosphere, ocean and land.
1.2. Interaction, Attribution, and Causation
All, or virtually all, environmental health effects interact with social and technological factors as well as other “purely” environmental determinants. For example, the effects of heat upon individual health are influenced by temperature, humidity, exercise, hydration, age, pre-existing health status, and also by occupation, clothing, behavior, autonomy, vulnerability, and sense of obligation. Does the person affected by heat, perhaps a brick maker in India, have the capacity to regulate her heat exposure; or might they be an elite athlete or emergency worker voluntarily pushing their limits? Other factors influencing the heath impact of heat include housing quality, the presence of absence of affordable air conditioning and energy subsidies, if any. In turn, these factors are influenced by governance and socio-economic status. Thus, the health-harming effects of heat can be seen to have many contributing causes, of which climate change is only one. As McMichael (and before him David Hume, among others) pointed out, causal attribution is to an extent philosophical; it is influenced by the “focal depth” of the examiner’s “causal lens” [ 40 ]. Consider a mass shooting in a school: Some will see underlying social and legal factors as contributing; others may see only the shooter. Yet, a major role and goal of public health is to seek to identify and reduce “deep” or “underlying” causes [ 41 ]. A world in which only the most “proximal” causes are identified will not function well.
Attributing the fraction of human-caused (anthropogenic) climate change to physical events such as storms, floods and heatwaves is similarly contested and assumption-dependent. The contribution of climate change to more indirect, strongly socially mediated effects such as migration, famine or conflict is even more difficult and contentious [ 22 , 42 , 43 ]. Perhaps in part because of these causal complications, issues such as famine, genocide, large-scale population dislocation and conflict have, with rare exceptions [ 44 ], been peripheral to public health. This is despite the obvious large-scale adverse health effects of these phenomena.
Rigorous methods have been developed to detect and attribute the health effects of phenomena that are more directly or obviously related to climate change, such as heat and infectious diseases [ 45 ]. However, excessive caution risks a type II error, the overlooking of genuine effects [ 46 , 47 ]. To reduce this risk, the authors of a recent study on attribution acknowledged the role for “well-informed judgments, based on understanding of underlying processes and matching of patterns of health, climate, and other determinants of human well-being” [ 45 ]. This paper makes many such judgments.
1.3. Integrative Risk and the Sustainability of Civilization
Publications in health journals about nuclear war and health date at least to 1962 [ 48 ]. In 1992 the Union of Concerned Scientists coordinated the “World Scientist’s warning to humanity”, signed by over 1700 leading scientists (but no public health workers) [ 49 ]. This warning was repeated in 2017, with far more signatories (including many health workers) [ 50 ].
Many authors outside health have warned of the fragility of modern civilization [ 51 , 52 ]. However, comparatively few writers with a health background have contributed [ 9 , 10 , 53 , 54 ]. Tony McMichael, who led the first Intergovernmental Panel on Climate Change chapter on health [ 55 ] frequently wrote and spoke of eroding “life support mechanisms” [ 56 , 57 ], a term probably introduced into the health literature in 1972 by Sargent [ 58 ]. Certainly, McMichael wanted to convey, when using this term, a profound risk to human well-being and health.
If civilization is to collapse then effects such as conflict, population displacement and famine are likely to be involved. A heatwave, on its own, is unlikely to cause the collapse of civilization, nor even ruin an economy for a decade. It needs social co-factors to do this. For example, a series of heatwaves damaging crop yields and contributing to internal migration has been postulated as contributing to the Syrian civil war that started in 2011 [ 21 , 22 , 59 , 60 , 61 , 62 ]. Prolonged heat, especially if in a humid setting, could cause some regions to be completely abandoned [ 63 , 64 , 65 ].
A severely damaged health system, allied with worsening undernutrition and poverty, could provide a milieu for a devastating epidemic, including a resurgence of HIV/AIDS [ 66 ]. An increase in infectious diseases, if of sufficient scale, could contribute to integrative cascades of failure generating regional or even global civilization collapse. Infectious diseases, as well as unfavorable eco-climatic change, contributed to the collapse of the Roman Empire [ 67 ].
While such consequences may seem far-fetched to some, the prospect of sea level rise of one meter or more by 2100 (perhaps sooner), proliferating nuclear weapons, millions of refugees, xenophobia and tribalism which limits integration, and growing cases of state failure is disquieting. Few, if any, formal scenarios, as exercises by senior scientists, are as bleak, but funding and other pressures constrain the realism of such exercises [ 15 ]. Already, the number of forcibly displaced people exceeds 68 million [ 68 ], a rise that has been linked with tightening limits to growth, including climate change [ 69 ].
It is stressed, again, that the idea that any single climate related event, such as heat, drought, sea level rise, conflict or migration will cause the collapse of civilization is simplistic. It is far more plausible to conceive that collapse (or quasi-collapse) could arise via a “milieu” of multi-factorial risk, enhancing, inflaming and interacting with climate change and other factors [ 43 , 70 ].
1.4. Hypothesis
This article seeks to test the hypothesis that the early literature relevant to climate change and health was more willing to describe catastrophic, potentially civilization disrupting health effects including famine, mass migration and conflict than it was to become, at least until 2014.
To explore this hypothesis, a database of articles relevant to climate change and health was assembled, relying mainly on PubMed and Google Scholar. This had six steps (see Appendix for details). Due to limited resources, the main search was restricted to the period 1980–2013, and the terms “climate change” and health or “global warming” and health. After eliminating duplicates, remaining papers were checked to see if they met eligibility criteria (see Box 1 ).
inclusion and exclusion criteria.
Included: Articles, editorials, commentaries, journalistic pieces with bylines.
Excluded: Reports, books, book sections including e-chapters, letters, factsheets, monographs, un-credited journalistic entries, non-English publications, papers concerning stratospheric ozone depletion, podcast transcripts, journalistic pieces that could not easily be recovered.
The search was not restricted to health or to multidisciplinary journals. However, papers outside health journals had to meet more exacting requirements to be included. They had to include health (or a synonym such as nutrition) in their title, abstract, keywords or text, even if they focused on an effect with health implications, such as population displacement, conflict or food insecurity.
The title of each identified paper was read, followed by the abstract of each paper, assessed as possibly eligible. If a score was still unclear, the full text was obtained and searched for words and phrases that suggested a broader interpretation of the indirect effects of climate change, such as “population displacement”, “migration”, “conflict”, “war”, “famine”, and “food insecurity”.
Eligible papers were scored as one if they exclusively concerned an effect other than conflict, migration, population displacement or large-scale undernutrition or famine. They also needed to exclude statements (even if introductory) such as “climate change has been recognized as the greatest risk to health in the 21st century”.
Papers were scored as two if they either mentioned such an effect and/or contained statements recognizing the potentially enormous scale of the health impacts from climate change. A synonym for this understanding was the phrase eroding “life support mechanisms”.
Papers were scored as three if they included a more detailed explanation or assertion of the future (or current) existence and importance of conflict, migration or famine, perhaps suggesting an interaction among them. A score of three was more likely if they also warned of the general severity of climate change. The score was also influenced by the tone of the language, and the space devoted to these issues (see Appendix for further details).
In addition, PubMed was searched for papers published from 2014–2017 matching the criteria “climate change” and “health”. A sample of 156 of these articles was randomly selected, approximately 5% in each year, after the elimination of a proportion of ineligible articles. Each was then scored, using the method described above for papers published from 1989 to 2013 (inclusive). Bootstrapping was then used to estimate the average score and 95% confidence interval of these articles, by taking ten thousand resamples, each of 156 papers, with replacement from this set (so that in each iteration some papers will appear more than once, while others will not appear at all).
A total of 2143 unique articles and journalistic essays satisfied the inclusion criteria, for the period 1989–2013 inclusive. The full database is available in the supplementary material . This shows the year, lead author (at least), journal, title and primary search method. It also lists the number of Google Scholar citations and the date these were identified. Table A1 ( Appendix ) tabulates the primary search method of papers, by each year.
No paper published before 1989 was eligible for retention in the final database. One potential publication [ 71 ] was cited by Kalkstein and Smoyer [ 5 ] as published in 1988, but it could not be located. About half the total papers (1142 or 53%) were published since 2009 (see Figure 1 ). Most papers (1546 papers, 72%) were scored as one, while only 189 (3.3%) were scored as three. The difference in these scores is statistically significant ( p < 0.01 ANOVA). The average score of these 2143 papers was 1.37 (see Table A2 in Appendix ).

Number of papers in each category. Since 1989 the number of papers concerning climate change and health has expanded considerably, particularly since 2008. As this article did not review the entire literature, the actual number of papers published, even in English, is more than shown. The average score of these papers declined from 1.9 in the first quintile to 1.34 in the final five years.
The increase in the size of literature reflects growing awareness of the risks to health from climate change. Over 50% of the papers published in the first quintile (1989–1993) were scored as two or three, although the total number in that time (27) was small (see Figure 1 ). Since 1993 the majority of papers have focused on effects such as heat, infectious diseases, allergies or asthma. The number of papers scored as two or three increased slightly after its trough (23%) in the third quintile (1999–2004) but was only 26% for 2009–2013 inclusive.
Papers scored as three were particularly uncommon in the third quintile (1999–2003), representing only 2.6% of the total published papers in that period. Even in the first quintile (1989–1993) most citations were for papers scored as one (see Figure 2 ).

Number of citations per annum for each score of paper. Most citations were for papers scored as one. Note that in 2005–2007 three extensively cited papers were scored as two (these are discussed in the Appendix A ).
3.1. Citations
Citation data were available for 2105 papers (98%). Over 201,000 citations were identified by Google Scholar (see Table A3 in Appendix ). Thirty two percent of these citations were for papers published since 2009 (see Figure 2 ). Of these citations, the great majority (82%) were for papers scored as one, each of which was cited an average of 107 times. Papers scored 2 were cited an average of 73 times, representing 15% of the total. Papers scored as three were cited 35 times each on average and accounted for 3% of the total. The difference in these citation scores is also statistically significant ( p < 0.01 ANOVA). Citations for papers scored as three from 1995 to 2008 inclusive were even lower, accounting for less than 1% of the total citations in each year of this period (see Figure 3 ). The fraction of the literature discussing existential risk remained lower in the last 5 years of this database than in the first five years (see Figure 1 ). The shift in the ratio of annual citations from the early period to the more recent years is evident in Figure 3 . Until 1991, the majority of citations were for papers scored as three. From 1994 the fraction of citations for papers scored as three was almost zero (3% or less) in every year until 2009. In 2013 it again fell to 3%.

The proportion of citations each year for papers scored as one and three. Since 1991 most citations have been for papers scored as 1. The Lancet UCL paper published in 2009 [ 11 ] led to a resurgence of citations for papers scored as 3, but this effect declined. Three individual papers, each scored as two (published in 2005, 2006 and 2007), were disproportionately cited. In each year at least some papers scored two or three, but their proportion of citations fell steeply after the first quintile. In 2003 no paper was scored as three, and for almost a decade (1997–2005 inclusive) virtually no papers scored as three were cited.
3.2. Coverage of Topics
All papers published in 1989 discussed multiple potential health effects of climate change. However, from 1990, journal articles focusing exclusively on infectious diseases and climate change appeared [ 72 , 73 , 74 ]. Early papers also focused on heat [ 75 ] and allergies [ 76 ]. From 2000, the foci of concerns expanded greatly. Additional topics included reduced micronutrient concentrations in food [ 77 ], asthma [ 78 ], thunderstorm asthma [ 79 ], chronic diseases and obesity [ 80 ], toxin exposure (such as from increased concentrations in Arctic mammals [ 81 ] and increased algal blooms [ 82 ]), forest fires [ 83 ], mental health [ 84 ] and respiratory [ 85 ], cardio-vascular [ 86 ], renal [ 87 ], fetal [ 88 ], genito-urinal [ 89 ] and skin conditions [ 90 ]. By 2000, papers were also appearing arguing that the impact of climate change for malaria was overstated [ 91 , 92 ].
Articles also appeared on the impact of climate change on groups such as indigenous people [ 93 ], children [ 94 ], the elderly [ 95 ] and regions and locations, including cities [ 96 ], the Arctic [ 97 ] and small island states [ 98 ] as well as many individual nations. Other themes appeared, including on how the health sector might reduce its carbon footprint [ 99 ], on “co-benefits” [ 100 ], on climate change as a great opportunity to improve public health [ 101 ], on medical education [ 102 ], pharmaceuticals [ 103 ] and on the health risks of adaptation and geoengineering, including of carbon capture and storage [ 104 ].
3.3. The Leadership Role of Some Journals
Many journals played prominent, even campaigning roles, especially the Lancet, BMJ and Environmental Health Perspectives. Several journals had special issues, including Global Health Action, the American Journal of Preventive Medicine, the Asia Pacific Journal of Public Health and Health Promotion International. Seven journals published at least 28 articles each, including editorials and news items (see Table A4 in Appendix ). At least 34 journals published editorials, which, with an average score of 2.2, were more likely to be scored as two or three than journal articles (average score 1.3). News items and other journalistic pieces had an average score of 1.6. At least 21 articles were published in nursing journals, with an average score of 1.67.
3.4. Papers for the Period 2014–2017
A total of 3377 papers were identified by PubMed as published from 2014–2017. Of these, 346 were found to be ineligible, although the true number would be higher, if all candidates were examined. Of the potentially eligible remainder, 113 papers were published in 2018, but recorded by PubMed as e-published in 2017. Slightly over five percent of the articles for each year was randomly selected, resulting in 156 articles (see Table A5 in Appendix ). Their average score and 95% confidence interval, estimated by bootstrapping, was 1.29 (95% CI 1.21–1.39) (see Figure A2 in Appendix ). Details of these 156 papers are in the supplementary material . Note that their citations were not checked.
4. Discussion
This paper describes the first published analysis of the extent to which the literature on climate change and health has described or in other ways engaged with “existential” risk. By including 2000 articles, 60 editorials and 83 news items (2143 “papers” in total) on climate change and health, it is by far the largest review of the climate change and health literature to have so far been published. Lack of resources currently prevents an extension of the fuller analysis to more recent years. However, a randomly selected sample of 156 articles for papers identified by PubMed as published in the period 2014–2017 found that these papers had an average score lower than the average score for any quintile from 1989–2013, other than for 1999–2003 (see Table A2 and Table A5 in Appendix ).
Several systematic and other reviews of topics related to climate change and health have been published, but on a much smaller scale, and with different research questions. Ford and Pearce systematically reviewed 420 papers, published between 1990 and 2009, exploring the topic of climate change vulnerability in the Canadian western Arctic [ 105 ]. Two systematic reviews concerned heat. Huang et al. [ 106 ] searched for papers published between 1980 and July 2010, projecting the heat related mortality under climate change scenarios. Only 14 papers were included in their final analysis. Xu et al. [ 107 ] explored the relationship between heat waves and children’s health, but selected twelve, an even small number. A systematic review into dengue fever and climate change (for the period 1991–2012) included 16 studies [ 108 ].
Nichols et al. (2009) [ 109 ] undertook a systematic review on health, climate change and energy vulnerability, searching for papers published in English between 1998 and 2008. They retrieved 114 papers but included only 36 in their final analysis. Bouzid et al. (2013) undertook a “systematic review of systematic reviews” to explore the effectiveness of public health interventions to reduce the health impact of climate change [ 110 ]. This identified over 3100 unique records, but of these, only 85 full papers were assessed, with 33 included in the final review.
This may also be the first review paper concerning climate change and health to use a citation analysis [ 111 ] as an indicator of influence. Citations in Google Scholar were used for convenience and cost. Although such citations are prone to error, and include essays in the gray literature, they still reflect influence. Some reports in the gray literature may be more widely read and more influential than more scholarly work.
4.1. Selection and Other Forms of Bias
A systematic review was not undertaken. However, all papers identified by searching using PubMed and at least 100 papers for each year identified by Google Scholar were considered for inclusion. The search term relevant to health was restricted to a single word, rather than synonyms such as “disease”, “morbidity”, “illness”, or “mortality”. Undoubtedly, a search using additional terms will identify more papers, as would a systematic review.
To examine the possibility that a more extensive search strategy would alter the conclusions, PubMed was also searched for the terms “climate change” and “morbidity” for papers published in 2013. This strategy identified 261 papers, compared to 496 when searching for “climate change” and “health”. Of these 261 papers, 30 had not previously been identified by the other search methods used, and met the other inclusion criteria. However, all of these additional papers were scored as one. Their inclusion in the final analysis was considered likely to bias the paper away from the null hypothesis, by accentuating the fraction of papers not scored as two or three. This bias towards papers scored one (i.e., identified by searching for “morbidity”) seems plausible because the term morbidity may be more likely to be associated with specific diseases than the term “health”. These papers therefore were not added to the analysis.
The search was supplemented by the addition of 17 papers first identified from the author’s own database, but not later found by the search strategy using Google Scholar or PubMed (steps 2–3) as described in Figure A1 . Eight of these 17 papers, five of which the author wrote or co-wrote, were scored as three. Their average score was 2.17, far higher than for the balance (1.23). This group also includes two editorials, one published in the Lancet, one in the BMJ. The inclusion of one of these editorials (scored as three, published in 1989) has biased the findings in favor of the hypothesis that highly scored papers were more common in the early period of this literature. Note, however, that no citations were recorded for this editorial.
The inclusion of these higher scoring papers later in the period of analysis has biased the result to the null, that is, away from the hypothesis that fewer such papers were published from about 2000. The most influential of these 17 papers, judged by Google Scholar citations, was cited 272 times. It was the first to report that rising levels of carbon dioxide depress micronutrient concentrations in food [ 77 ]. The other 16 papers were cited 405 times between them, an average of 25, which is low compared to the average citation number (94). Twenty eight other papers were included, mostly identified from special issues. Their average score was 1.9. One paper was identified post-review, by chance. It was scored as two (perhaps generously) and was included because it was judged that to exclude it would bias the result away from the null hypothesis.
Bias is also likely to have been introduced in the scoring process, but not to the extent that it could challenge the main conclusions. The rigor of this paper would be improved if the scores could be checked by a third party, blind to the first score. Unfortunately, no resources were available for this purpose. Some classification errors are likely, especially for papers for which the author had no previous familiarity, and if published after 2009, when, due to time pressure, many papers were scored rapidly. On the other hand, in the process of ranking over 2000 papers the author became skilled at making rapid decisions, especially for most papers scored as one. The difference between papers scored one and two was generally more apparent than for papers scored between two and three. In cases of doubt a higher score was always selected.
The likelihood of bias and error is unlikely to explain the difference in the character of the papers in the early period and those which later dominated. Although the widely cited paper by Costello et al. [ 11 ] (1583 citations as of June 2018) may have refreshed appreciation of the potentially catastrophic nature of climate change, the majority of papers and their citations published between 2010 and 2013 continued to focus on specific issues. This trend appears to have persisted in the years since, judged by the analysis of a randomly selected sample, identified by PubMed as published between 2014 and 2018.
4.2. Reasons for the Apparent Conservatism of the Literature
There are several plausible, overlapping and interacting explanations for the decline in the proportion of papers scored as two or three (and for their comparatively fewer citations) following 1996, and also in the failure for papers published since 2009 to fully amplify the most severe warnings. One likely contributing explanation is self-censorship. The topic of climate change and health is unfamiliar territory for many health editors and writers. Climate change has become politicized in many English-speaking countries, especially in the U.S. and Australia. Although comparatively few health workers have expertise concerning climate change and health, the readership of some health journals seems judged, by their editor, to be skeptical of, or even to reject climate science. For example, one editor, defending the decision to publish a paper (scored, possibly generously, as two) [ 112 ] seemed almost apologetic, writing “On its face, the paper by Hess and colleagues is largely a political commentary and a departure from the types of articles found in Academic Emergency Medicine” [ 113 ].
Thus, for some health workers and editors, even broaching the topic of climate change and health may be a courageous act. The publication of papers in health journals that describe potential pathways that could threaten civilization would appear even bolder. It is unsurprising that such papers are still fairly uncommon, at least until 2014, and particularly in journals which do not yet have a long tradition of publishing papers or editorials on this topic.
In the early period of the climate and health literature (1989–1993) some of the most outspoken articles were editorials. Perhaps at that time, there was a certain sense of shock concerning climate change, which has since waned. It was also a time when concerns about overpopulation were slightly less taboo [ 114 , 115 , 116 ]. However, editorials in more years also tend to have a higher index of concern than other articles.
Another likely contributor to the comparative degree of restraint is the view, backed by some research, that an excess of fear is counter-productive [ 117 ]. However, the smell of smoke in a theater requires the sounding of a vigorous alarm. Compounding the difficulty of communicating the risk over climate change is the lag between the whiff of smoke and the onset of visible fire. Hansen warned of great danger over thirty years ago, and he, with others, have issued many warnings since [ 118 ]. Sceptics are still waiting to see the metaphorical “flames” of climate change, even disputing the link between literal flames (fires) and climate change.
On the other hand, science, though not infallible, has delivered countless miracles such as antisepsis, anesthesia, penicillin and the jet engine. It has long warned of the physical changes of climate change. We who work in health should not be amazed if the predictions of climate and Earth scientists prove broadly accurate. Social science is less precise than climatology [ 43 ], however the links between food insecurity, drought, sea level rise, migration and, in some places, conflict are, also, surely not far-fetched. Papers that fail to express appreciation of the extraordinary risks we face as civilization may be judged by people of the future as having failed in their duty of care to protect health.
Another likely reason for the general restraint in the literature is the fragmentation of science and limited funding for multidisciplinary work. Comparatively few authors, other than if collaborating in large, multidisciplinary teams (rare for most authors primarily concerned with health), are rewarded or funded for thinking systemically. This problem is possibly worsening. Related to this, many recent papers are by sub-disciplines of health that have not previously published on the topic of climate change. Such papers are probably less likely to discuss existential risk.
As the effects of climate change have become increasingly clear the need for adaptation has become overwhelming. A stress on adaptation does not necessarily reflect any underestimation of the eventual severity of climate change. However, a stress on adaptation at the expense of mitigation may do so. In many countries, political leadership favors adaptation.
5. Conclusions
In 1989, thirty two years after the International Geophysical Year, the first papers on global warming and health appeared in the world’s leading medical journals [ 3 , 6 , 7 ]. All three of these early papers warned of severe, even existential risk and were each scored as three.
In 1990 McCally and Cassel warned that “progression of these environmental changes could lead to unprecedented human suffering” [ 119 ]. Also, in 1990, Fiona Godlee, then deputy editor of the BMJ, wrote “Countries in the developing world would suffer both the direct effects of drought and flood and the knock-on effect of agricultural and economic decline in the West. The already present problems of feeding the world’s growing population would be compounded by the increasing numbers of displaced people unable to grow their own food” [ 120 ]. In 1992 Powles observed “It is possible that adverse lagged effects of current industrial (and military) activities will disrupt the habitat of future generations of our species through processes such as stratospheric ozone depletion, global warming and others as yet unpredicted” [ 121 ]. However, in the following years, this sense of urgency largely dissipated, until the long paper by Costello et al. in 2009 [ 11 ].
Conditioned by growing up during the Cold War, the author has long been apprehensive about civilization’s survival. However, my timeline for global health disaster has always been multi-decadal. Civilizational collapse, if it is to occur, will not necessarily be in my own lifetime [ 54 ]. My concerns are not based solely on climate change. Climate change, by itself, is most unlikely to cripple civilization. A well-functioning global society, motivated to do so, could easily eliminate hunger and poverty, not only today, but under all but worst-case climate change. Refugees from inundated islands, war-torn Syria or the drought-stricken Chad basin [ 122 ] could easily be accommodated in more fertile and more elevated parts of the world. Unfortunately, humans currently do not co-operate on such a scale, and this behavior may, in part, be driven by inborn, “hard-wired”, evolutionary-shaped traits [ 123 ]. If civilization is to endure we may need to collectively overcome our seemingly deep wiring for tribalism and separation.
Acknowledgments
My thanks to John Potter for his help with locating obscure references, and to Andy Morse and Kristie Ebi for their very helpful comments, and Joseph Guillaume for his statistical advice. I especially thank Ivan Hanigan for the bootstrap analysis. I also thank three anonymous reviewers.
Supplementary Materials
The following are available online at http://www.mdpi.com/1660-4601/15/10/2266/s1 .
Appendix A.1. Detailed Methods and Results
The search method had six steps (see Figure A1 ). Initial exploration used the author’s Endnote database, of over 35,000 references, to find relevant articles. The second step was to search, using Google Scholar, for up to the first 100 results for each year in the search period (1980–2013), using the terms “climate change” and health or “global warming” and “health”. For the first decade in which relevant articles were found (1989–1998) both pairs of terms were used, but from 1999 to 2013 inclusive, only the former terms were used (“climate change” and “health”). In the third step, the search was expanded by seeking the same terms, using PubMed, for the same period; 1980–2013 (inclusive). After eliminating duplicates, all remaining papers were checked to ensure that they met the eligibility criteria listed in Box 1 . In stage 4, several papers were included if they appeared in special issues of journals, together with articles identified by PubMed, or suggested by colleagues. In stage 5, the BMJ database for news items about climate change and health was searched explored, because although PubMed found a few the proportion it identified was low. Finally, in stage 6, several other papers were found by chance, such as in reviews, in the references of cited papers, or by searching for other papers.

Outline of the six stage search strategy for papers published from 1989–2013.
Appendix A.2. Further Scoring Details
The following details are provided in order to provide additional information about the scoring process. It discusses the scoring process for three highly cited papers (from 2005–2007), each of which was scored as two. The first (cited 2059 times) had no mention of population displacement or conflict, but included the sentence “Projections of the effect of climate change on food crop yield production globally appear to be broadly neutral, but climate change will probably exacerbate regional food supply inequalities” [ 124 ]. This statement was assessed as accepting the possibility of a degree of food scarcity judged to be more severe than that described by many papers (particularly concerning the Arctic) which discuss a likely impairment in regional nutrition, but do not forecast insufficient calories or nutrients, let alone famine. Although the conclusion regarding overall global food security in this paper was reassuring, there are already four acknowledged famines in African nations and one in Yemen [ 125 ]. Any exacerbation of regional food supply inequalities is therefore likely to result in aggravated famines, unless future famines are eliminated; an unlikely prospect. Because this paper was cited so frequently a lower score would impact the overall result. If there is a bias from scoring this paper as two it is towards the null hypothesis.
In 2006 a widely cited paper [ 126 ] stated “Other important climatic risks to health, from changes in regional food yields, disruption of fisheries, loss of livelihoods, and population displacement (because of sea-level rise, water shortages, etc.) are less easy to study than these factors and their causal processes and effects are less easily quantified”. This is a more comprehensive list of civilization-endangering effects than the paper discussed above, but the language is restrained and brief. It was scored as a two.
In 2007 another widely cited paper included the sentences “Climate change will, itself, affect food yields around the world unevenly. Although some regions, mostly at mid-to-high latitude, could experience gains, many (e.g., in sub-Saharan Africa) are likely to be adversely affected, with impairment of both nutrition and incomes. Population displacement and conflict are also likely, because of various factors including food insecurity, desertification, sea-level rise, and increased extreme weather events” [ 127 ]. Of the three papers discussed here this provided the most comprehensive list of such effects and also explores their interaction. However, it did not speculate about civilization collapse, nor describe climate change as the biggest threat to global public health.
A gradient exists between papers scored two or three, rather than a clear threshold. Papers were not scored as three simply by including a more detailed explanation or assertion of the existence and importance of conflict, migration or famine, even if an interaction among them was suggested. They needed something extra. For example, one paper [ 128 ] stated (referring to Costello et al. [ 11 ]) “a watershed paper … suggests that climate change represents the biggest potential threat to human health in the twenty-first century … a recent report … also estimates that four billion people are vulnerable and 500 million people are at extreme risk”. This paper was scored as three even though the paper focused on medical education. Although the phrase “the biggest potential threat to human health in the twenty-first century” can, with repetition, lose its capacity to shock, its meaning, if taken literally, is surely sufficiently dire to be scored as three.
Another paper (scored as three) stated “global health, population growth, economic development, environmental degradation, and climate change are the main challenges we face in the 21st century” [ 129 ]. It also stated that “significant mass migration is likely to occur in response to climate change”.
The interpretation of papers was not excessively generous. For example, a paper that noted: “Changes in the frequency and intensity of extreme weather and climate events have had profound effects on both human society and the natural environment” was scored as one because there was no discussion of this aspect in the abstract or further in the text. It was also considered that the words “have had profound” was insufficiently clear. Nor did the paper discuss conflict, migration or famine.
In contrast, two papers about climate change and health in Nepal were scored as two, as they included the statements “Climate change is becoming huge threat to health especially for those from developing countries” (sic) [ 130 ] and “Climate change is a global issue in this century which has challenged the survival of living creatures affecting the life supporting systems of the earth: atmosphere, hydrosphere and lithosphere” [ 131 ].
Appendix A.3. Sources (Detailed)
Seventeen articles were identified from the author’s database, but not found via PubMed or Google Scholar. Other sources are shown in Table A4 .
This shows the primary source of the 2146 included articles. 18 articles were from special issues, 5 were found accidentally, 1 was from a review and 1 was from a colleague. Many articles were found using multiple methods. The papers listed here in the GS column were not found by PM but may also have been identified by CB. Abbreviations: PM = PubMed, GS = Google Scholar, CB = Colin Butler.
| Year | PM | GS | BMJ | Other | CB | Total |
|---|---|---|---|---|---|---|
| 2 | 1 | 3 | ||||
| 2 | 3 | 2 | 7 | |||
| 14 | 1 | 15 | ||||
| 1 | 8 | 2 | 11 | |||
| 7 | 7 | 14 | ||||
| 11 | 11 | 22 | ||||
| 13 | 17 | 1 | 31 | |||
| 12 | 18 | 30 | ||||
| 16 | 21 | 37 | ||||
| 15 | 17 | 1 | 1 | 34 | ||
| 10 | 19 | 29 | ||||
| 30 | 16 | 1 | 1 | 3 | 51 | |
| 34 | 8 | 2 | 1 | 45 | ||
| 28 | 8 | 1 | 1 | 38 | ||
| 17 | 8 | 1 | 1 | 27 | ||
| 29 | 12 | 2 | 43 | |||
| 35 | 18 | 4 | 2 | 59 | ||
| 55 | 11 | 2 | 68 | |||
| 67 | 16 | 3 | 3 | 89 | ||
| 134 | 22 | 7 | 1 | 1 | 164 | |
| 109 | 54 | 18 | 1 | 2 | 184 | |
| 186 | 106 | 6 | 14 | 2 | 314 | |
| 176 | 93 | 5 | 1 | 275 | ||
| 158 | 108 | 2 | 1 | 269 | ||
| 154 | 126 | 2 | 2 | 284 | ||
Appendix A.4. Score, Citation and Journal Details
This shows the number of articles and their average score for each quintile from 1989–1993.
| Quintile | Number of Articles | Average Score |
|---|---|---|
| 50 | 1.90 | |
| 154 | 1.40 | |
| 190 | 1.26 | |
| 423 | 1.42 | |
| 1326 | 1.34 | |
This shows the number of papers and citations in each category divided into five quintiles for the 25 years of analysis. Note that in the third quintile (1999–2003) only 5 articles were ranked as three. Ironically, the paper scored as three in 2002 was a news item which quoted Andrew Sims, policy director of the New Economics Foundation as lamenting “Health is not even being talked about here [Delhi], although the potential health impact is a devastating one, almost unimaginable” [ 132 ].
| Papers Scored as 1 | Papers Scored as 2 | Papers Scored as 3 | ||||
|---|---|---|---|---|---|---|
| Number | Citations | Number | Citations | Number | Citations | |
| 23 | 1996 | 9 | 197 | 18 | 802 | |
| 105 | 16,545 | 36 | 1910 | 13 | 172 | |
| 146 | 40,352 | 39 | 3985 | 5 | 78 | |
| 286 | 39,128 | 96 | 12,590 | 41 | 836 | |
| 986 | 67,112 | 229 | 10,916 | 114 | 4748 | |
Ten journals published at least 22 articles on climate change and health in the period 1989–2013.
| Journal | Articles | Editorials | News Items | Total |
|---|---|---|---|---|
| 35 | 12 | 71 | ||
| 107 | 4 | |||
| 55 | 8 | 2 | ||
| 53 | ||||
| 39 | ||||
| 38 | ||||
| 28 | ||||
| 26 | ||||
| 24 | ||||
| 19 | 3 |
Appendix A.5. Additional Papers 2014–2018
PubMed was searched for the terms “climate change” and “health” for the period 2014–2017 inclusive. This found 3377 papers, which were grouped by year of publication and listed alphabetically, by surname of the first author. Every 20th paper (in each year) was then examined. If a paper was found to be ineligible, successive consecutive (alphabetical) candidates were examined until at least 5% of the total maximum number for each year had been found eligible and analyzed. In total, 156 papers were scored. This sample represented 5.1% of the 3036 papers which remained after 341 of the original pool had been eliminated. More would be excluded, given a more thorough inspection. The average score of these 156 articles and their 95% confidence interval, determined by bootstrapping, was 1.29 (1.21–1.39). The average score of these papers is lower than for the papers published from 2009–2013 (1.37). Although the 95% confidence interval for the period 2014–2018 overlaps with this, there is no evidence to suggest that the more recent literature better recognizes existential risk. See Table A5 and Figure A2 .
This shows the number, number analyzed and scores for the 156 papers that were analyzed for the period 2014–2018, tabulated by year. Note that some of the candidate papers would be culled after further examination.
| Year | Candidate Papers | Papers Analyzed | % Analyzed | Average Score |
|---|---|---|---|---|
| 649 | 34 | 5.2% | 1.4 | |
| 639 | 32 | 5.0% | 1.3 | |
| 816 | 43 | 5.3% | 1.2 | |
| 813 | 41 | 5.0% | 1.3 | |
| 113 | 6 | 5.1% | 1.2 | |

This shows the density of means and distributions for each year (2014–2017), based on 10,000 bootstrapped resamples (with replacement from the set for each year) and also for papers from 2013–2018 inclusive.
This research received no external funding.
Conflicts of Interest
The author declares no conflict of interest.
Climate Change and Human Health
- Chapter (PDF)
- Citation (RIS)
- Figures (ZIP)

Introduction
Lead authors.
- John Balbus National Institutes of Health
- Allison R. Crimmins U.S. Environmental Protection Agency
- Janet L. Gamble U.S. Environmental Protection Agency
Contributing Authors
- David R. Easterling National Oceanic and Atmospheric Administration
- Kenneth E. Kunkel Cooperative Institute for Climate and Satellites - NC
- Shubhayu Saha Centers for Disease Control and Prevention
- Marcus C. Sarofim U.S. Environmental Protection Agency
Balbus, J., A. Crimmins, J.L. Gamble, D.R. Easterling, K.E. Kunkel, S. Saha, and M.C. Sarofim, 2016: Ch. 1: Introduction: Climate Change and Human Health. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment . U.S. Global Change Research Program, Washington, DC, 25–42. http://dx.doi.org/10.7930/J0VX0DFW
Human health has always been influenced by climate and weather . Changes in climate and climate variability , particularly changes in weather extremes, affect the environment that provides us with clean air, food, water, shelter, and security. Climate change , together with other natural and human-made health stressors, threatens human health and well-being in numerous ways. Some of these health impacts are already being experienced in the United States.
Given that the impacts of climate change are projected to increase over the next century, certain existing health threats will intensify and new health threats may emerge. Connecting our understanding of how climate is changing with an understanding of how those changes may affect human health can inform decisions about mitigating (reducing) the amount of future climate change, suggest priorities for protecting public health, and help identify research needs.
1.1 Our Changing Climate
Observed climate change.
The fact that the Earth has warmed over the last century is unequivocal. Multiple observations of air and ocean temperatures, sea level, and snow and ice have shown these changes to be unprecedented over decades to millennia. Human influence has been the dominant cause of this observed warming. 1 The 2014 U.S. National Climate Assessment (2014 NCA ) found that rising temperatures, the resulting increases in the frequency or intensity of some extreme weather events, rising sea levels, and melting snow and ice are already disrupting people’s lives and damaging some sectors of the U.S. economy. 2
The concepts of climate and weather are often confused. Weather is the state of the atmosphere at any given time and place. Weather patterns vary greatly from year to year and from region to region. Familiar aspects of weather include temperature, precipitation, clouds, and wind that people experience throughout the course of a day. Severe weather conditions include hurricanes, tornadoes, blizzards, and droughts. Climate is the average weather conditions that persist over multiple decades or longer. While the weather can change in minutes or hours, identifying a change in climate has required observations over a time period of decades to centuries or longer. Climate change encompasses both increases and decreases in temperature as well as shifts in precipitation, changing risks of certain types of severe weather events, and changes to other features of the climate system.
Figure 1.1: Major U.S. Climate Trends
Observed changes in climate and weather differ at local and regional scales (Figure 1.1). Some climate and weather changes already observed in the United States include: 2 , 3
Figure 1.2: Change in Number of Extreme Precipitation Events

- U.S. average temperature has increased by 1.3°F to 1.9°F since recordkeeping began in 1895; most of this increase has occurred since about 1970. The first decade of the 2000s (2000–2009) was the warmest on record throughout the United States.
- Average U.S. precipitation has increased since 1900, but some areas have experienced increases greater than the national average, and some areas have experienced decreases.
- Heavy downpours are increasing nationally, especially over the last three to five decades. The largest increases are in the Midwest and Northeast, where floods have also been increasing. Figure 1.2 shows how the annual number of heavy downpours, defined as extreme two-day precipitation events, for the contiguous United States has increased, particularly between the 1950s and the 2000s.
- Drought has increased in the West. Over the last decade, the Southwest has experienced the most persistent droughts since record keeping began in 1895. 4 Changes in precipitation and runoff, combined with changes in consumption and withdrawal, have reduced surface and groundwater supplies in many areas.
- There have been changes in some other types of extreme weather events over the last several decades. Heat waves have become more frequent and intense, especially in the West. Cold waves have become less frequent and intense across the nation.
- The intensity, frequency, and duration of North Atlantic hurricanes, as well as the frequency of the strongest (category 4 and 5) hurricanes, have all increased since the early 1980s. The relative contributions of human and natural causes to these increases remain uncertain.
Projected Climate Change
Projections of future climate conditions are based on results from climate models—sophisticated computer programs that simulate the behavior of the Earth’s climate system. These climate models are used to project how the climate system is expected to change under different possible scenarios. These scenarios describe future changes in atmospheric greenhouse gas concentrations, land use , other human influences on climate, and natural factors. The most recent set of coordinated climate model simulations use a set of scenarios called Representative Concentration Pathways (RCPs) , which describe four possible trajectories in greenhouse gas concentrations. 1 Actual future greenhouse gas concentrations, and the resulting amount of future climate change, will still largely be determined by choices society makes about emissions . 2 The RCPs, and the temperature increases associated with these scenarios, are described in more detail in Appendix 1: Technical Support Document and in the 2014 NCA. 3 , 5 , 6
Figure 1.3: Projected Changes in Temperature and Precipitation by Mid-Century
Interact with the Figure Below
Some of the projected changes in climate in the United States as described in the 2014 NCA are listed below: 2 , 3
- Temperatures in the United States are expected to continue to rise. This temperature rise has not been, and will not be, uniform across the country or over time (Figure 1.3).
- Increases are also projected for extreme temperature conditions. The temperature of both the hottest day and coldest night of the year are projected to increase (Figure 1.4).
- More winter and spring precipitation is projected for the northern United States, and less for the Southwest, over this century (Figure 1.3).
- Increases in the frequency and intensity of extreme precipitation events are projected for all U.S. areas (Figure 1.4).
- Short-term (seasonal or shorter) droughts are expected to intensify in most U.S. regions. Longer-term droughts are expected to intensify in large areas of the Southwest, the southern Great Plains, and the Southeast. Trends in reduced surface and groundwater supplies in many areas are expected to continue, increasing the likelihood of water shortages for many uses.
- Heat waves are projected to become more intense, and cold waves less intense, everywhere in the United States.
- Hurricane-associated storm intensity and rainfall rates are projected to increase as the climate continues to warm.
Figure 1.4: Projected Changes in the Hottest/Coldest and Wettest/Driest Day of the Year
1.2 how does climate change affect health.
The influences of weather and climate on human health are significant and varied. They range from the clear threats of temperature extremes and severe storms to connections that may seem less obvious. For example, weather and climate affect the survival, distribution, and behavior of mosquitoes, ticks, and rodents that carry diseases like West Nile virus or Lyme disease . Climate and weather can also affect water and food quality in particular areas, with implications for human health. In addition, the effects of global climate change on mental health and well-being are integral parts of the overall climate-related human health impact.
A useful approach to understand how climate change affects health is to consider specific exposure pathways and how they can lead to human disease. The concept of exposure pathways is adapted from its use in chemical risk assessment , and in this context describes the main routes by which climate change affects health (see Figure 1.5) . Exposure pathways differ over time and in different locations, and climate change related exposures can affect different people and different communities to different degrees. While often assessed individually, exposure to multiple climate change threats can occur simultaneously, resulting in compounding or cascading health impacts. Climate change threats may also accumulate over time, leading to longer-term changes in resilience and health.
Whether or not a person is exposed to a health threat or suffers illness or other adverse health outcomes from that exposure depends on a complex set of vulnerability factors. Vulnerability is the tendency or predisposition to be adversely affected by climate-related health effects, and encompasses three elements: exposure, sensitivity or susceptibility to harm, and the capacity to adapt or to cope (see also Figure 9.1 in Ch. 9: Populations of Concern ). Because multiple disciplines use these terms differently and multiple definitions exist in the literature, the distinctions between them are not always clear. 8 All three of these elements can change over time and are place- and system-specific. 9 In the context of this report, we define the three elements of vulnerability as follows:
- Exposure is contact between a person and one or more biological, psychosocial, chemical, or physical stressors, including stressors affected by climate change. Contact may occur in a single instance or repeatedly over time, and may occur in one location or over a wider geographic area.
- Sensitivity is the degree to which people or communities are affected, either adversely or beneficially, by climate variability or change.
- Adaptive capacity is the ability of communities, institutions, or people to adjust to potential hazards, to take advantage of opportunities, or to respond to consequences. A related term, resilience , is the ability to prepare and plan for, absorb, recover from, and more successfully adapt to adverse events.
(definitions adapted from IPCC 2014 and NRC 2012). 10 , 11
Vulnerability, and the three components of vulnerability, are factors that operate at multiple levels, from the individual and community to the country level, and affect all people to some degree. 9 For an individual, these factors include human behavioral choices and the degree to which that person is vulnerable based on his or her level of exposure, sensitivity, and adaptive capacity. Vulnerability is also influenced by social determinants of health (see Ch. 9 Populations of Concern ), including those that affect a person’s adaptive capacity, such as social capital and social cohesion (for example, the strength of interpersonal networks and social patterns in a community).
At a larger community or societal scale, health outcomes are strongly influenced by adaptive capacity factors, including those related to the natural and built environments (for example, the state of infrastructure ), governance and management (health-protective surveillance programs, regulations and enforcement, or community health programs), and institutions (organizations operating at all levels to form a national public health system). 12 , 13 For example, water resource, public health, and environmental agencies in the United States provide many public health safeguards, such as monitoring water quality and issuing advisories to reduce risk of exposure and illness if water becomes contaminated. Some aspects of climate change health impacts in the United States may therefore be mediated by factors like strong social capital, fully functional governance/management, and institutions that maintain the Nation’s generally high level of adaptive capacity. On the other hand, the evidence base regarding the effectiveness of public health interventions in a climate change context is still relatively weak. 14 Current levels of adaptive capacity may not be sufficient to address multiple impacts that occur simultaneously or in close succession, or impacts of climate change that result in unprecedented damages. 2 , 13
The three components of vulnerability (exposure, sensitivity, and adaptive capacity) are associated with social and demographic factors, including level of wealth and education, as well as other characteristics of people and places, such as the condition of infrastructure and extent of ecosystem degradation. For example, poverty can leave people more exposed to climate and weather threats, increase sensitivity because of associations with higher rates of illness and nutritional deficits, and limit people’s adaptive capacity. As another example, people living in a city with degraded coastal ecosystems and inadequate water and wastewater infrastructure may be at greater risk of health consequences from severe storms. Figure 1.5 demonstrates the interactions among climate drivers, health impacts, and other factors that influence people’s vulnerability to health impacts.
Figure 1.5: Climate Change and Health
We are already experiencing changes in the frequency, severity, and even the location of some weather and climate phenomena, including extreme temperatures, heavy rains and droughts, and some other kinds of severe weather, and these changes are projected to continue. This means that areas already experiencing health-threatening weather and climate phenomena, such as severe heat or hurricanes, are likely to experience worsening impacts, such as even higher temperatures and increased storm intensity, rainfall rates, and storm surge . It also means that some areas will experience new climate-related health threats. For example, areas previously unaffected by toxic algal blooms or waterborne diseases because of cooler water temperatures may face these hazards in the future as increasing water temperatures allow the organisms that cause these health risks to thrive. Even areas that currently experience these health threats may see a shift in the timing of the seasons that pose the greatest risk to human health.
Climate change can therefore affect human health in two main ways: first, by changing the severity or frequency of health problems that are already affected by climate or weather factors; and second, by creating unprecedented or unanticipated health problems or health threats in places where they have not previously occurred.
1.3 Our Changing Health
In order to understand how climate change creates or exacerbates health problems, assessments of climate change health impacts must start with what is known about the current state and observed trends in a wide array of health conditions. In addition, because preexisting health conditions, socioeconomic status, and life stage all contribute to vulnerability to climate-related and weather -related health effects, assessments of climate change health impacts should be informed by projected changes in these factors. In cases where people’s health or socioeconomic status is getting worse, climate change may accentuate the health burdens associated with those worsening trends. Conversely, in cases where people’s health or socioeconomic status is improving, the effect of climate change may be to slow or reduce that improvement. Where the state of scientific understanding allows, the inclusion of projected trends in health and socioeconomic conditions into models of climate change impacts on health can provide useful insights into these interactions between non-climate factors and climate change effects.
Demographic and Socioeconomic Trends
The United States is in the midst of several significant demographic changes: the population is aging, growing in number, becoming more ethnically diverse, and demonstrating greater disparities between the wealthy and the poor. Immigration is having a major influence on both the size and age distribution of the population. 15 Each of these demographic trends has implications for climate change related human health impacts (see Ch. 9: Populations of Concern ). Some of these trends and projections are summarized below:
Trends in population growth
- The total U.S. population has more than doubled since 1950, from 151,325,798 persons in 1950 to 308,745,538 in 2010. 16
- The Census Bureau projects that the U.S. population will grow to almost 400 million by 2050 (from estimates of about 320 million in 2014). 17
Trends in the elderly population
- The nation’s older adult population (ages 65 and older) will nearly double in number from 2015 through 2050, from approximately 48 million to 88 million. 18 Of those 88 million older adults, a little under 19 million will be 85 years of age and older. 19
Trends in racial and ethnic diversity
- As the United States becomes more diverse, the aggregate minority population is projected to become the majority by 2042. 18 The non-Hispanic or non-Latino White population will increase, but more slowly than other racial groups. Non-Hispanic Whites are projected to become a minority by 2050. 20
- Projections for 2050 suggest that nearly 19% of the population will be immigrants, compared with 12% in 2005. 20
- The Hispanic population is projected to nearly double from 12.5% of the U.S. population in 2000 to 24.6% in 2050. 21
Trends in economic disparity
- Income inequality rose and then stabilized during the last 30 years, and is projected to resume rising over the next 20 years, though at a somewhat slower overall rate that declines to near zero by 2035. 22 For example, the Gini coefficient, a measure of income inequality, is estimated to have risen by 18% between 1984 and 2000, and is projected to rise by an additional 17% for all workers between 2009 and 2035. 22
- America’s communities of color have disproportionately higher poverty rates and lower income levels. While racial disparities in household wealth were higher in the late 1980s than now, trends in more recent years have been toward greater inequality. The ratio of the median net household worth of White, non-Hispanic versus non-White or Hispanic households increased from 6.0 to 7.8 between 2007 and 2013. 23 In 2009, 25.8% of non-Hispanic Blacks and 25.3% of Hispanics had incomes below the poverty level as compared to 9.4% of non-Hispanic Whites and 12.5% of Asian Americans. 24 In 2014, the median income level for a non-Hispanic Black household was approximately $35,000, $25,000 lower than a non-Hispanic White household. 25
Population growth and migration in the United States may place more people at risk of the health impacts of climate change, especially as more people are located in and around vulnerable areas, such as coastal, low-lying, or flood-prone zones; 26 densely populated urban areas; 27 and drought -stricken or wildfire -prone regions. Increases in racial and ethnic diversity and in the number of persons living near the poverty line may increase the risk of health impacts from climate change. Economic disparity can make it difficult for some populations to respond to dangerous weather conditions, especially when evacuation is necessary or when the aftermath requires rebuilding of homes and businesses not covered by home or property insurance.
Trends in Health Status

Storm-damaged home after Hurricane Sandy
© iStockPhoto. com/Aneese
As a nation, trends in the population’s health are mixed. Some major indicators of health, such as life expectancy, are consistently improving, while others, such as rate and number of diabetes deaths, are getting worse. Changes in these metrics may differ across populations and over time. For example, though rates of obesity have increased in both children and adults over the last 30 years or more, rates over just the last decade have remained steady for adults but increased among children. 28
Climate change impacts to human health will act on top of these underlying trends. Some of these underlying health conditions can increase sensitivity to climate change effects such as heat waves and worsening air quality (see Ch. 2: Temperature-Related Death and Illness ; Ch. 3: Air Quality Impacts; Ch. 9: Populations of Concern ). Understanding the trends in these conditions is therefore important in considering how many people are likely to experience illness when exposed to these climate change effects. Potential climate change related health impacts may reduce the improvements that would otherwise be expected in some indicators of health status and accentuate trends towards poorer health in other health indicators. 1 , 29
Examples of health indicators that have been improving between 2000 and 2013 include the following:
- Life expectancy at birth increased from 76.8 to 78.8 years. 30
- Death rates per 100,000 people from heart disease and cancer decreased from 257.6 to 169.8 and from 199.6 to 163.2, respectively. 30
- The percent of people over age 18 who say they smoke decreased from 23.2% to 17.8%. 30

Diabetes increases sensitivity to heat stress.
© Monkey Business Images/Corbis
At the same time, some health trends related to the prevalence of chronic diseases, self-reported ill health, and disease risk factors have been getting worse. For example:
- The percentage of adult (18 years and older) Americans describing their health as “poor or fair” increased from 8.9% in 2000 to 10.3% in 2012. 30
- Prevalence of physician-diagnosed diabetes among adults aged 20 and over increased from 5.2% in 1988-1994 to 8.4% in 2009-2012. 30
- The prevalence of obesity among adults (aged 20–74) increased by almost three-fold from 1960–1962 (13.4% of adults classified as obese) to 2009–2010 (36.1% of adults classified as obese). 31
- In the past 30 years, obesity has more than doubled in children and quadrupled in adolescents in the United States. The percentage of children aged 6–11 who were obese increased from 7% in 1980 to nearly 18% in 2012. Similarly, the percentage of adolescents aged 12–19 years who were obese increased from 5% to nearly 21% over the same period. In 2012, approximately one-third of American children and adolescents were overweight or obese. 32
Table 1.1 shows some examples of underlying health conditions that are associated with increased vulnerability to health effects from climate change related exposures (see Ch. 9: Populations of Concern for more details) and provides information on current status and future trends.
Health status is often associated with demographics and socioeconomic status. Changes in the overall size of the population, racial and ethnic composition, and age distribution affect the health status of the population. Poverty, educational attainment, access to care, and discrimination all contribute to disparities in the incidence and prevalence of a variety of medical conditions (see Ch. 9: Populations of Concern ). Some examples of these interactions include:
Older Adults. In 2013, the percentage of adults age 75 and older described as persons in fair or poor health totaled 27.6%, as compared to 6.2% for adults age 18 to 44. 30 Among adults age 65 and older, the number in nursing homes or other residential care facilities totaled 1.8 million in 2012, with more than 1 million utilizing home health care. 33

Asthma affects approximately 9% of children in the United States.
© Stephen Welstead/LWA/ Corbis
Children. Approximately 9.0% of children in the United States have asthma. Between 2011 and 2013, rates for Black (15.3%) and Hispanic (8.6%) children were higher than the rate for White (7.8%) children. 30 Rates of asthma were also higher in poor children who live below 100% of the poverty level (12.4%). 30
Non-Hispanic Blacks. In 2014, the percentage of non-Hispanic Blacks of all ages who were described as persons in fair or poor health totaled 14.3% as compared to 8.7% for Whites. Health risk factors for this population include high rates of smoking, obesity, and hypertension in adults, as well as high infant death rates. 30
Hispanics. The percentage of Hispanics of all ages who were described as persons in fair or poor health totaled 12.7% in 2014. Health disparities for Hispanics include moderately higher rates of smoking in adults, low birth weights, and infant deaths. 30
The impacts of climate change may worsen these health disparities by exacerbating some of the underlying conditions they create. For example, disparities in life expectancy may be exacerbated by the effects of climate change related heat and air pollution on minority populations that have higher rates of hypertension, smoking, and diabetes. Conversely, public health measures that reduce disparities and overall rates of illness in populations would lessen vulnerability to worsening of health status from climate change effects.
Table 1.1: Current estimates and future trends in chronic health conditions that interact with the health risks associated with climate change
Click on a table row for more information.
| Conditions | Current Estimates | Future Trends | Possible Influences of |
|---|---|---|---|
| ALZHEIMER'S DISEASE | Approximately 5 million Americans over 65 had Alzheimer's disease in 2013. | of Alzheimer’s is expected to triple to 13.8 million by 2050. | Persons with impairments are vulnerable to extreme events that require evacuation or other emergency responses. |
| Average asthma prevalence in the U.S. was higher in children (9% in 2014) than in adults (7% in 2013). Since the 1980s, asthma prevalence increased, but rates of asthma deaths and hospital admissions declined. | Stable and increasing prevalence of asthma is projected in the U.S. in coming decades.
| Asthma is exacerbated by changes in pollen season and allergenicity and in exposures to air pollutants affected by changes in temperature, humidity, and wind. | |
| ( ) | In 2012, approximately 6.3% of adults had COPD. Deaths from chronic lung diseases increased by 50% from 1980 to 2010. | Chronic diseases are the third leading cause of death and are expected to become some of the most costly illnesses in coming decades. | COPD patients are more sensitive than the general population to changes in ambient air quality associated with climate change. |
| In 2012, approximately 9% of the total U.S. population had diabetes. Approximately 18,400 people younger than age 20 were newly diagnosed with type 1 diabetes in 2008–2009; an additional 5,000 were diagnosed with type 2. | New diabetes cases are projected to increase from about 8 cases per 1,000 in 2008 to about 15 per 1,000 in 2050. If recent increases continue, prevalence is projected to increase to 33% of Americans by 2050. | Diabetes increases to heat stress; medication and dietary needs may increase during and after extreme weather events.
| |
| DISEASE | Cardiovascular disease ( ) is the leading cause of death in the U.S. | By 2030, approximately 41% of the U.S. population is projected to have some form of CVD. | Cardiovascular disease increases sensitivity to heat stress. |
| MENTAL ILLNESS | is one of the most common types of mental illness, with approximately 7% of adults reporting a major episode in the past year. Lifetime prevalence is approximately twice as high for women as for men. Lifetime prevalence is more than 15% for disorders and nearly 4% for bipolar disorder. | By 2050, the total number of U.S. adults with depressive disorder is projected to increase by 35%, from 33.9 million to 45.8 million, with those over age 65 having a 117% increase. | Mental illness may impair responses to ; certain medications increase sensitivity to heat stress. |
| In 2009–2010, approximately 35% of American adults were obese. In 2012, approximately 32% of youth (aged 2–19) were overweight or obese. | By 2030, 51% of the U.S. population is expected to be obese. Projections suggest a 33% increase in obesity and a 130% increase in severe obesity. | Obesity increases sensitivity to high ambient temperatures. | |
| Approximately 18.7% of the U.S. population has a disability. In 2010, the percent of American adults with a disability was approximately 16.6% for those age 21–64 and 49.8% for persons 65 and older. | The number of older adults with activity limitations is expected to grow from 22 million in 2005 to 38 million in 2030. | Persons with disabilities may find it hard to respond when evacuation is required and when there is no available means of transportation or easy exit from residences. |
1.4 Quantifying Health Impacts
For some changes in exposures to health risks related to climate change , the future rate of a health impact associated with any given environmental exposure can be estimated by multiplying three values: 1) the baseline rate of the health impact, 2) the expected change in exposure, and 3) the exposure–response function. An exposure–response function is an estimate of how the risk of a health impact changes with changes in exposures, and is related to sensitivity , one of the three components of vulnerability . For example, an exposure–response function for extreme heat might be used to quantify the increase in heat-related deaths in a region (the change in health impact) for every 1°F increase in daily ambient temperature (the change in exposure).

The ability to quantify many types of health impacts is dependent on the availability of data on the baseline incidence or prevalence of the health impact, the ability to characterize the future changes in the types of exposures relevant to that health impact, and how well the relationship between these exposures and health impacts is understood. Health impacts with many intervening factors, like infectious diseases, may require different and more complex modeling approaches. Where our understanding of these relationships is strong, some health impacts, even those occurring in unprecedented places or times of the year, may in fact be predictable. Where there is a lack of data or these relationships are poorly understood, health impacts are harder to project. For more information on exposure–response (also called dose–response or concentration–response) functions, see the Exposure–Response section in Appendix 1: Technical Support Document .
Information on trends in underlying health or background rates of health impacts is summarized in Section 1.3 , “Our Changing Health.” Data on the incidence and prevalence of health conditions are obtained through a complicated system of state- and city-level surveillance programs, national health surveys, and national collection of data on hospitalizations, emergency room visits, and deaths. For example, data on the incidence of a number of infectious diseases are captured through the National Notifiable Diseases Surveillance System. 51 This system relies first on the mandatory reporting of specific diseases by health care providers to state, local, territorial, and tribal health departments. These reporting jurisdictions then have the option of voluntarily providing the Centers for Disease Control and Prevention ( CDC ) with data on a set of nationally notifiable diseases. Because of challenges with getting health care providers to confirm and report specific diagnoses of reportable diseases in their patients, and the lack of requirements for reporting a consistent set of diseases and forwarding data to CDC, incidence of infectious disease is generally believed to be underreported, and actual rates are uncertain. 52
Characterizing certain types of climate change related exposures can be a challenge. Exposures can consist of temperature changes and other weather conditions, inhaling air pollutants and pollens, consuming unsafe food supplies or contaminated water, or experiencing trauma or other mental health consequences from weather disasters. For some health impacts, the ability to understand the relationships between climate-related exposures and health impacts is limited by these difficulties in characterizing exposures or in obtaining accurate data on the occurrence of illnesses. For these health impacts, scientists may not have the capability to project changes in a health outcome (like incidence of diseases), and can only estimate how risks of exposure will change. For example, modeling capabilities allow projections of the impact of rising water temperatures on the concentration of Vibrio bacteria , which provides an understanding of geographic changes in exposure but does not capture how people may be exposed and how many will actually become sick (see Ch. 6: Water-Related Illness ). Nonetheless, the ability to project changes in exposure or in intermediate determinants of health impacts may improve understanding of the change in health risks , even if modeling quantitative changes in health impacts is not possible. For example, seasonal temperature and precipitation projections may be combined to assess future changes in ambient pollen concentrations (the exposure that creates risk), even though the potential associated increase in respiratory and allergic diseases (the health impacts) cannot be directly modeled (see Ch. 3: Air Quality Impacts ).
Modeling Approaches Used in this Report
Four chapters within this assessment— Ch. 2: Temperature-Related Death and Illness , Ch. 3: Air Quality Impacts , Ch. 5: Vector-Borne Diseases , and Ch. 6: Water-Related Illness —include new peer-reviewed, quantitative analyses based on modeling. The analyses highlighted in these chapters mainly relied on climate model output from the Coupled Model Intercomparison Project Phase 5 (CMIP5). Due to limited data availability and computational resources, the studies highlighted in the four chapters analyzed only a subset of the full CMIP5 dataset, with most of the studies including at least one analysis based on RCP6.0, an upper midrange greenhouse gas concentration pathway, to facilitate comparisons across chapters. For example, the air quality analysis examined results from two different RCPs, with a different climate model used for each, while the waterborne analyses examined results from 21 of the CMIP5 models for a single RCP . See the Guide to the Report and Appendix 1: Technical Support Document for more on modeling and scenarios.
Adverse health effects attributed to climate change can have many economic and social consequences, including direct medical costs, work loss, increased care giving, and other limitations on everyday activities. Though economic impacts are a crucial component to understanding risk from climate change, and may have important direct and secondary impacts on human health and well-being by reducing resources available for other preventative health measures, economic valuation of the health impacts was not reported in this assessment.
Uncertainty in Health Impact Assessments
Figure 1.6 illustrates different sources of uncertainty along the exposure pathway.
Figure 1.6: Sources of Uncertainty
Two of the key uncertainties in projecting future global temperatures are 1) uncertainty about future concentrations of greenhouse gases , and 2) uncertainty about how much warming will occur for a given increase in greenhouse gas concentrations. The Intergovernmental Panel on Climate Change’s Fifth Assessment Report found that the most likely response of the climate system to a doubling of carbon dioxide concentrations lies between a 1.5 and 4.5 (2.7°F to 8.1°F) increase in global average temperature. 1 Future concentrations depend on both future emissions and how long these emissions remain in the atmosphere (which can vary depending on how natural systems process those emissions). To capture these uncertainties, climate modelers often use multiple models, analyze multiple scenarios, and conduct sensitivity analyses to assess the significance of these uncertainties.
Uncertainty in current and future estimates of health or socioeconomic status is related to several factors. In general, estimates are more uncertain for less-prevalent health conditions (such as rare cancers versus cardiovascular disease), smaller subpopulations (such as Hispanic subpopulations versus White adults), smaller geographic areas (census tracts versus state or national scale), and time periods further into the future (decades versus seasons or years). Most current estimates of disease prevalence or socioeconomic status have uncertainty expressed as standard errors or confidence intervals that are derived from sampling methods and sample sizes. When modeling health impacts using data on health prevalence or socioeconomic status, these measures of uncertainty are typically included in the analysis to help establish a range of plausible results. Expert judgment is typically used to assess the overall effects of uncertainty from estimates of health or socioeconomic status when assessing the scientific literature.
The factors related to uncertainty in exposure–response functions are similar to those for the projections of health or socioeconomic status. Estimates are more uncertain for smaller subpopulations, less-prevalent health conditions, and smaller geographic areas. Because these estimates are based on observations of real populations, their validity when applied to populations in the future is more uncertain the further into the future the application occurs. Uncertainty in the estimates of the exposure–outcome relationship also comes from factors related to the scientific quality of relevant studies, including appropriateness of methods, source of data, and size of study populations. Expert judgment is used to evaluate the validity of an individual study as well as the collected group of relevant studies in assessing uncertainty in estimates of exposure–outcome relationships.
Approach to Reporting Uncertainty in Key Findings
Despite the sources of uncertainty described above, the current state of the science allows an examination of the likely direction of and trends in the health impacts of climate change. Over the past ten years, the models used for climate and health assessments have become more useful and more accurate (for example, Melillo et al. 2014). 6 , 53 , 54 This assessment builds on that improved capability. A more detailed discussion of the approaches to addressing uncertainty from the various sources can be found in the Guide to the Report and Appendix 1: Technical Support Document .
Two kinds of language are used when describing the uncertainty associated with specific statements in this report: confidence language and likelihood language (see below). Confidence in the validity of a finding is expressed qualitatively and is based on the type, amount, quality, strength, and consistency of evidence and the degree of expert agreement on the finding. Likelihood, or the projected probability of an impact occurring, is based on quantitative estimates or measures of uncertainty expressed probabilistically (in other words, based on statistical analysis of observations or model results, or on expert judgment). Whether a Key Finding has a confidence level associated with it or, where findings can be quantified, both a confidence and likelihood level associated with it, involves the expert assessment and consensus of the chapter author teams.
Likelihood and Confidence Level
| ≥9 in 10 | ≥2 in 3 | ≈ 1 in 2 | ≤ 1 in 3 | ≤1 in 10 |
Confidence Level
- Akinbami, L. J., J. E. Moorman, C. Bailey, H. S. Zahran, M. King, C. A. Johnson, and X. Liu , 2012: Trends in Asthma Prevalence, Health Care Use, and Mortality in the United States, 2001–2010. NCHS Data Brief. No. 94, May 2012 . Array, 8 pp., National Center for Health Statistics, Hyattsville, MD. URL | Detail
- Board of Governors of the Federal Reserve System, 2014: 2013 Survey of Consumer Finances: SCF Chartbook . URL | Detail
- Bouzid, M., L. Hooper, and P. R. Hunter , 2013: The effectiveness of public health interventions to reduce the health impact of climate change: A systematic review of systematic reviews . PLoS ONE , 8 , e62041. doi:10.1371/journal.pone.0062041 | Detail
- Brault, M. W. , 2012: Americans With Disabilities: 2010 . 23 pp., U.S. Census Bureau, Washington, D.C. URL | Detail
- CDC, cited 2014: National Notifiable Disease Surveillance System (NNDSS) . Centers for Disease Control and Prevention. URL | Detail
- CDC, cited 2015: Lyme Disease Surveillance and Available Data . Centers for Disease Control and Prevention. URL | Detail
- Cutter, S. L., W. Solecki, N. Bragado, J. A. Carmin, M. Fragkias, M. Ruth, and T. Wilbanks , 2014: Ch. 11: Urban Systems, Infrastructure, and Vulnerability . Climate Change Impacts in the United States: The Third National Climate Assessment , J.M. Melillo, Richmond, T. (T.C.), and Yohe, G.W., Eds. , U.S. Global Change Research Program, 282-296. doi:10.7930/J0F769GR | Detail
- DeNavas-Walt, C., and B. D. Proctor , 2015: Income and Poverty in the United States: 2014 . U.S. Census Bureau, Washington, D.C. URL | Detail
- Ebi, K. L., and J. C. Semenza , 2008: Community-based adaptation to the health impacts of climate change . American Journal of Preventive Medicine , 35 , 501-507. doi:10.1016/j.amepre.2008.08.018 | Detail
- EPA, 2012: Climate Change Indicators in the United States, 2nd Edition . 84 pp., U.S. Environmental Protection Agency, Washington, D.C. URL | Detail
- Fryar, C. D., M. D. Carroll, and C. L. Ogden , 2012: Prevalence of Overweight, Obesity, and Extreme Obesity Among Adults: United States, Trends 1960-1962 through 2009-2010 . CDC National Center for Health Statistics. URL | Detail
- Gabe, T. , 2010: Poverty in the United States, 2009 . Congressional Research Service, Washington, D.C. URL | Detail
- Gallopin, G. C. , 2006: Linkages between vulnerability, resilience, and adaptive capacity . Global Environmental Change , 16 , 293-303. doi:10.1016/j.gloenvcha.2006.02.004 | Detail
- Harris-Kojetin, L., M. Sengupta, E. Park-Lee, and R. Valverde , 2013: Long-Term Care Services in the United States: 2013 Overview . 107 pp., National Center for Health Statistics, Hyattsville, MD. URL | Detail
- Heo, M., C. F. Murphy, K. R. Fontaine, M. L. Bruce, and G. S. Alexopoulos , 2008: Population projection of US adults with lifetime experience of depressive disorder by age and sex from year 2005 to 2050 . International Journal of Geriatric Psychiatry , 23 , 1266-1270. doi:10.1002/gps.2061 | Detail
- Hess, J. J., J. Z. McDowell, and G. Luber , 2012: Integrating climate change adaptation into public health practice: Using adaptive management to increase adaptive capacity and build resilience . Environmental Health Perspectives , 120 , 171-179. doi:10.1289/ehp.1103515 | Detail
- IPCC, 2013: Climate Change 2013: The Physical Science Basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change . 1535 pp., Cambridge University Press, Cambridge, UK and New York, NY. doi:10.1017/CBO9781107415324 | Detail
- IPCC, 2014: Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change . 1132 pp., Cambridge University Press, Cambridge, UK and New York, NY. URL | Detail
- Johnson, N. B., L. D. Hayes, K. Brown, E. C. Hoo, and K. A. Ethier , 2014: CDC National Health Report: Leading Causes of Morbidity and Mortality and Associated Behavioral Risk and Protective Factors - United States, 2005-2013 . Morbidity and Mortality Weekly Report - Supplements , 63 , 3-27. PMID: 25356673 | Detail
- Kosacz, N. M., and others , 2012: Chronic obstructive pulmonary disease among adults - United States, 2011 . MMWR: Morbidity and Mortality Weekly Report , 61 , 938-943. URL | Detail
- Luber, G., and others , 2014: Ch. 9: Human Health . Climate Change Impacts in the United States: The Third National Climate Assessment , J.M. Melillo, Richmond, T. (T.C.), and Yohe, G.W., Eds. , U.S. Global Change Research Program, 220-256. doi:10.7930/J0PN93H5 | Detail
- Melillo, J. M., T. (T. C. ) Richmond, and G. W. Yohe , 2014: Appendix 5: Scenarios and Models . Climate Change Impacts in the United States: The Third National Climate Assessment , U.S. Global Change Research Program, 821-825. doi:10.7930/J0B85625 | Detail
- Melillo, J. M., T. (T. C. ) Richmond, and G. W. Yohe, eds. , 2014: Climate Change Impacts in the United States: The Third National Climate Assessment . U.S. Global Change Research Program, 841 pp. doi:10.7930/J0Z31WJ2 | Detail
- Moorman, J. E., L. J. Akinbami, C. M. Bailey, H. S. Zahran, M. E. King, C. A. Johnson, and X. Liu , 2012: National Surveillance of Asthma: United States, 2001-2010 . National Center for Health Statistics. URL | Detail
- Moser, S. C., M. A. Davidson, P. Kirshen, P. Mulvaney, J. F. Murley, J. E. Neumann, L. Petes, and D. Reed , 2014: Ch. 25: Coastal Zone Development and Ecosystems . Climate Change Impacts in the United States: The Third National Climate Assessment , J.M. Melillo, Richmond, T. (T.C.), and Yohe, G.W., Eds. , U.S. Global Change Research Program, 579-618. doi:10.7930/J0MS3QNW | Detail
- NCHS, 2015: Health, United States, 2014: With Special Feature on Adults Aged 55-64 . 473 pp., National Center for Health Statistics, Centers for Disease Control and Prevention, Hyattsville, MD. URL | Detail
- NRC, 2006: Hispanics and the Future of America . M. Tienda and Mitchell, F., Eds. , National Research Council. The National Academies Press, 502 pp. URL | Detail
- NRC, 2012: Disaster Resilience: A National Imperative . National Academies Press, 244 pp. | Detail
- Ogden, C. L., M. D. Carroll, B. K. Kit, and K. M. Flegal , 2014: Prevalence of childhood and adult obesity in the United States, 2011-2012 . JAMA: The Journal of the American Medical Association , 311 , 806-814. doi:10.1001/jama.2014.732 | Detail
- Passel, J. S., and D. Cohen , 2008: U.S. Population Projections: 2005-2050 . 49 pp., Pew Research Center, Washington, D.C. URL | Detail
- Post, E. S., and others , 2012: Variation in estimated ozone-related health impacts of climate change due to modeling choices and assumptions . Environmental Health Perspectives , 120 , 1559-1564. doi:10.1289/ehp.1104271 | Detail
- Schwabish, J. A. , 2013: Modeling Individual Earnings in CBO’s Long-term Microsimulation Model . 28 pp., Congressional Budget Office, Washington, D.C. URL | Detail
- Shrestha, L. B., and E. J. Heisler , 2011: The Changing Demographic Profile of the United States . 32 pp., Congressional Research Service. URL | Detail
- Smit, B., and J. Wandel , 2006: Adaptation, adaptive capacity and vulnerability . Global Environmental Change , 16 , 282-292. doi:10.1016/j.gloenvcha.2006.03.008 | Detail
- Sun, L., K. E. Kunkel, L. E. Stevens, A. Buddenberg, J. G. Dobson, and D. R. Easterling , 2015: Regional Surface Climate Conditions in CMIP3 and CMIP5 for the United States: Differences, Similarities, and Implications for the U.S. National Climate Assessment . Array, 111 pp., National Oceanic and Atmospheric Administration, National Environmental Satellite, Data, and Information Service. doi:10.7289/V5RB72KG | Detail
- Tamerius, J. D., E. K. Wise, C. K. Uejio, A. L. McCoy, and A. C. Comrie , 2007: Climate and human health: Synthesizing environmental complexity and uncertainty . Stochastic Environmental Research and Risk Assessment , 21 , 601-613. doi:10.1007/s00477-007-0142-1 | Detail
- U.S. Census Bureau, cited 2010: U.S. Census 2010: Resident Population Data . U.S. Department of Commerce. URL | Detail
- U.S. Census Bureau, 2010: The Next Four Decades, The Older Population in the United States: 2010 to 2050, Population Estimates and Projections . Array, 16 pp., U.S. Department of Commerce, Economics and Statistics Division, U.S. Census Bureau, Washington, D.C. URL | Detail
- U.S. Census Bureau, cited 2014: 2014 National Population Projections: Summary Tables. Table 9. Projections of the Population by Sex and Age for the United States: 2015 to 2060 . U.S. Department of Commerce. URL | Detail
- U.S. Census Bureau, cited 2014: 2014 National Population Projections: Summary Tables. Table 1. Projections of the Population and Components of Change for the United States: 2015 to 2060 (NP2014-T1) . U.S. Department of Commerce. URL | Detail
- Walsh, J., and others , 2014: Ch. 2: Our Changing Climate . Climate Change Impacts in the United States: The Third National Climate Assessment , J.M. Melillo, Richmond, T. (T.C.), and Yohe, G.W., Eds. , U.S. Global Change Research Program, 19-67. doi:10.7930/J0KW5CXT | Detail
- Walsh, J., and others , 2014: Appendix 3: Climate Science Supplement . Climate Change Impacts in the United States: The Third National Climate Assessment , J.M. Melillo, Richmond, T. (T.C.), and Yohe, G.W., Eds. , U.S. Global Change Research Program, 735-789. doi:10.7930/J0KS6PHH | Detail
Documenting Uncertainty: This assessment relies on two metrics to communicate the degree of certainty in Key Findings. See Appendix 4: Documenting Uncertainty for more on assessments of likelihood and confidence.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- News Feature
- Published: 06 August 2024
Doctors prepare for the “enormous health consequences” of climate change
- Sofia Moutinho 1
Nature Medicine ( 2024 ) Cite this article
126 Accesses
8 Altmetric
Metrics details
Student doctors push for the health impacts of extreme weather to be taught in medical schools, as the carbon emissions from healthcare come under greater scrutiny.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Zhang, Y. & Steiner, A. L. Nat. Commun. 13 , 1234 (2022).
Article CAS PubMed PubMed Central Google Scholar
Chung, J. W. & Meltzer, D. O. JAMA 302 , 1970–1972 (2009).
Article CAS PubMed Google Scholar
Berniak-Woźny, J. & Rataj, M. Int. J. Environ. Res. Public Health 20 , 908 (2023).
Article PubMed PubMed Central Google Scholar
Baker, N. et al. Front. Public Health 8 , 590275 (2020).
Vrijsen, B. E. L. et al. Ann. Med. Surg. 51 , 48–53 (2020).
Article CAS Google Scholar
Philipsborn, R. P. et al. Acad. Med. 96 , 355–367 (2021).
Article PubMed Google Scholar
Download references
Author information
Authors and affiliations.
Freelance writer, Rio de Janeiro, Brazil
Sofia Moutinho
You can also search for this author in PubMed Google Scholar
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Moutinho, S. Doctors prepare for the “enormous health consequences” of climate change. Nat Med (2024). https://doi.org/10.1038/s41591-024-03160-x
Download citation
Published : 06 August 2024
DOI : https://doi.org/10.1038/s41591-024-03160-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Artificial Intelligence
- Science & Tech
- Middle East & North Africa
Research, ideas, and leadership for a more secure, peaceful world
Climate Change Impacts Health: Six Things You Should Know
- View Citation
Author Syra Madad

Author Sarah Brown

Author Komal Bajaj
Author Birgitte Messerschmidt

The warming climate doesn’t only melt ice caps and bleach coral reefs but also puts your health at risk. Climate change is no longer a far-removed issue, able to be cast off as a problem “of tomorrow.” Climate change alters health both through long-term stressors, such as air pollution 1 and vector-borne diseases 2 , and through acute events, such as heat waves 3 and hurricanes. 4 These long and short term elements collectively influence public health around the world. Climate change has health consequences from the scale of entire populations all the way down to the level of your cells. 5 Here are six things that are sometimes forgotten regarding climate and health:
Climate change is associated with infectious disease spread
As temperatures rise, disease vectors like mosquitoes and ticks move northward into newly habitable terrain. 2,6,7 This means that diseases that were previously only endemic to the tropics are expanding to new areas. The spread of Legionella in New York 8–10 and the northward movement of Valley fever in California 11–13 are examples of how the landscape of infectious disease spread is changing. 7,14
Climate change results in poorer air quality
With drier and hotter summers, wildfires are increasing in prevalence and intensity. 15–17 Due to the extensive amount of smoke produced, the impact of wildfires reaches beyond the areas destroyed by flames. 18 The smoke becomes even more polluting when wildfires consume our built environment in the Wildland Urban Interface (WUI). WUI fire smoke causes acute air pollution events in places far removed from the actual fires, such as the June 2023 orange haze in New York, as well as long periods of bad air quality elsewhere, such as California during recent summers. Wildfire air pollution has been linked not only to respiratory issues but also to cardiovascular, psychiatric, gastrointestinal, and skin disorders. 19–27 The specific components of smoke, including particulates and toxic gasses, contribute to both immediate and sustained health challenges.
Climate change worsens heat-related diseases
Heat waves are becoming more frequent and intense. 3,28 Thus, experts indicate that climate change will increase the number of fatalities due to heat-related incidents. 29–31 In addition to the heightened death toll, heat waves pose neurological, pulmonary, metabolic, and renal risks. 32,33 With stressed electrical systems during high-temperature days, the stability of cooling systems decreases which leads to more power outages and further exacerbates vulnerabilities to heat. 34
Climate change disrupts healthcare delivery
Climate change intensifies hurricanes, which, in turn, stress health systems. 4 Storms of this nature cause injuries directly through trauma from water and wind, and indirectly by overwhelming hospitals with patient surges. 4,35,36 In extreme weather situations that cause power outages or the need to evacuate, those that require electricity-powered medical devices must seek care outside of the home. The influx of patients often results in overextended health systems and delays in care. 37–39
Climate change hurts mental health
Climate factors, both physical and psychological, take a toll on mental health. Climate-related exposures, such as to wildfire, drought, floods, humidity, and heat, are associated with psychological distress, increased mortality among those with pre-existing mental health conditions, higher rates of psychiatric hospitalizations, and increased suicide rates. 40 Climate change also exacerbates psychological stressors by contributing to job insecurity, forced displacement, resource insecurity, and decreased community identity, among other social vulnerabilities. 40,41 A majority of U.S. adults (68%) have reported feeling at least some climate-related anxiety. 42
Climate change threatens proper nutrition
Elevated CO 2 concentrations reduce the nutritional content of some essential foods like grains and legumes, which show lower levels of zinc and iron. 43–45 Additionally, unstable weather conditions decrease food security, making nutritious food more expensive and less accessible. 44,46,47 These factors contribute to malnutrition, including both obesity and undernutrition, as well as diet-related non-communicable diseases such as diabetes and cardiovascular disorders. 43
Taking Action:
While these health impacts may seem discouraging, it’s possible to mitigate and prepare for the damages through actionable steps. Start by educating yourself about the risks specific to your locality and taking preventative measures. Reduce your carbon footprint and support policies that address climate change. Engage with local climate initiatives or educational programs to foster a community that is aware of and resilient to these changes. Climate change connects all of us and it will take our collective action to address its consequences.
Syra Madad, Sarah Brown, Komal Bajaj and Birgitte Messerschmidt. “Climate Change Impacts Health: Six Things You Should Know.” Belfer Center for Science and International Affairs , July 23, 2024
- US EPA. Climate Change Impacts on Air Quality. Published October 19, 2022. Accessed March 18, 2024. https://www.epa.gov/climateimpacts/climate-change-impacts-air-quality
- Rocklöv J, Dubrow R. Climate change: an enduring challenge for vector-borne disease prevention and control. Nat Immunol . 2020;21(5):479-483. doi:10.1038/s41590-020-0648-y
- US EPA. Climate Change Indicators: Heat Waves. Published February 4, 2021. Accessed March 18, 2024. https://www.epa.gov/climate-indicators/climate-change-indicators-heat-waves
- Knutson T. Global Warming and Hurricanes. Accessed March 18, 2024. https://www.gfdl.noaa.gov/global-warming-and-hurricanes/
- US EPA. Climate Change and Human Health. Published March 20, 2022. Accessed March 18, 2024. https://www.epa.gov/climateimpacts/climate-change-and-human-health
- Ainsworth C. Tropical diseases move north. Nature . Published online November 9, 2023. doi:10.1038/d41586-023-03476-7
- Mora C, McKenzie T, Gaw IM, et al. Over half of known human pathogenic diseases can be aggravated by climate change. Nat Clim Chang . 2022;12(9):869-875. doi:10.1038/s41558-022-01426-1
- Moffa MA, Rock C, Galiatsatos P, Gamage SD, Schwab KJ, Exum NG. Legionellosis on the rise: A scoping review of sporadic, community-acquired incidence in the United States. Epidemiol Infect . 2023;151:e133. doi:10.1017/S0950268823001206
- Han XY. Effects of climate changes and road exposure on the rapidly rising legionellosis incidence rates in the United States. PLoS One . 2021;16(4):e0250364. doi:10.1371/journal.pone.0250364
10. Legionellosis (Legionella) | Tompkins County NY. Accessed March 18, 2024. https://www.tompkinscountyny.gov/health/legionellosis
11. Valley Fever Basics. Accessed March 18, 2024. https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/ValleyFeverBasics.aspx#drought
12. Monserrat L. Valley fever. OEHHA. Published May 13, 2022. Accessed March 18, 2024. https://oehha.ca.gov/climate-change/epic-2022/impacts-human-health/valley-fever
13. American Lung Association. How Climate Change Has Led to an Increase in Valley Fever. Accessed March 18, 2024. https://www.lung.org/blog/how-climate-change-has-led-to-an-increase-in-valle
14. Climate and infectious diseases | What We Do | NCEZID | CDC. Published February 16, 2024. Accessed March 29, 2024. https://www.cdc.gov/ncezid/what-we-do/climate-change-and-infectious-diseases/index.html
15. Wildfire climate connection | National Oceanic and Atmospheric Administration. Accessed March 18, 2024. https://www.noaa.gov/noaa-wildfire/wildfire-climate-connection
16. Jolly WM, Cochrane MA, Freeborn PH, et al. Climate-induced variations in global wildfire danger from 1979 to 2013. Nat Commun . 2015;6(1):7537. doi:10.1038/ncomms8537
17. Abatzoglou JT, Williams AP. Impact of anthropogenic climate change on wildfire across western US forests. Proceedings of the National Academy of Sciences . 2016;113(42):11770-11775. doi:10.1073/pnas.1607171113
18. Messerschmidt B. The Smoke Problem. Accessed June 4, 2024. https://www.nfpa.org/news-blogs-and-articles/nfpa-journal/2024/02/13/research-column-spring-24
19. Aguilera R, Corringham T, Gershunov A, Benmarhnia T. Wildfire smoke impacts respiratory health more than fine particles from other sources: observational evidence from Southern California. Nat Commun . 2021;12(1):1493. doi:10.1038/s41467-021-21708-0
20. Kondo MC, De Roos AJ, White LS, et al. Meta-Analysis of Heterogeneity in the Effects of Wildfire Smoke Exposure on Respiratory Health in North America. Int J Environ Res Public Health . 2019;16(6):960. doi:10.3390/ijerph16060960
21. Thurston G, Yu W, Luglio D. An Evaluation of the Asthma Impact of the June 2023 New York City Wildfire Air Pollution Episode. Am J Respir Crit Care Med . 2023;208(8):898-900. doi:10.1164/rccm.202306-1073LE
22. Jones CG, Rappold AG, Vargo J, et al. Out-of-Hospital Cardiac Arrests and Wildfire-Related Particulate Matter During 2015-2017 California Wildfires. J Am Heart Assoc . 2020;9(8):e014125. doi:10.1161/JAHA.119.014125
23. Eisenman DP, Galway LP. The mental health and well-being effects of wildfire smoke: a scoping review. BMC Public Health . 2022;22(1):2274. doi:10.1186/s12889-022-14662-z
24. D’Evelyn SM, Jung J, Alvarado E, et al. Wildfire, Smoke Exposure, Human Health, and Environmental Justice Need to be Integrated into Forest Restoration and Management. Curr Environ Health Rep . 2022;9(3):366-385. doi:10.1007/s40572-022-00355-7
25. Li J, He C, Ying J, et al. Air pollutants, genetic susceptibility, and the risk of incident gastrointestinal diseases: A large prospective cohort study. Environ Res . 2024;247:118182. doi:10.1016/j.envres.2024.118182
26. Roberts W. Air pollution and skin disorders. Int J Womens Dermatol . 2020;7(1):91-97. doi:10.1016/j.ijwd.2020.11.001
27. Verhoeven JI, Allach Y, Vaartjes ICH, Klijn CJM, Leeuw FE de. Ambient air pollution and the risk of ischaemic and haemorrhagic stroke. The Lancet Planetary Health . 2021;5(8):e542-e552. doi:10.1016/S2542-5196(21)00145-5
28. Perkins-Kirkpatrick SE, Lewis SC. Increasing trends in regional heatwaves. Nat Commun . 2020;11(1):3357. doi:10.1038/s41467-020-16970-7
29. Lüthi S, Fairless C, Fischer EM, et al. Rapid increase in the risk of heat-related mortality. Nat Commun . 2023;14(1):4894. doi:10.1038/s41467-023-40599-x
30. Climate Change and Health: Extreme Heat. Published March 12, 2024. Accessed March 29, 2024. https://www.nrdc.org/resources/climate-change-and-health-extreme-heat
31. Extreme heat projected to increase cardiovascular deaths. National Institutes of Health (NIH). Published October 27, 2023. Accessed March 29, 2024. https://www.nih.gov/news-events/news-releases/extreme-heat-projected-increase-cardiovascular-deaths
32. Temperature Extremes | CDC. Published September 9, 2022. Accessed March 29, 2024. https://www.cdc.gov/climateandhealth/effects/temperature_extremes.htm
33. Temperature-related Death and Illness. National Institute of Environmental Health Sciences. Accessed March 29, 2024. https://www.niehs.nih.gov/research/programs/climatechange/health_impacts/heat
34. Stone BJr, Gronlund CJ, Mallen E, et al. How Blackouts during Heat Waves Amplify Mortality and Morbidity Risk. Environ Sci Technol . 2023;57(22):8245-8255. doi:10.1021/acs.est.2c09588
35. Laboratory BAC Ph D, NASA’s Jet Propulsion. A Force of Nature: Hurricanes in a Changing Climate. Climate Change: Vital Signs of the Planet. Accessed March 18, 2024. https://climate.nasa.gov/news/3184/a-force-of-nature-hurricanes-in-a-changing-climate
36. How climate change makes hurricanes more destructive - Environmental Defense Fund. Accessed March 29, 2024. https://www.edf.org/climate/how-climate-change-makes-hurricanes-more-destructive
37. Tarabochia-Gast AT, Michanowicz DR, Bernstein AS. Flood Risk to Hospitals on the United States Atlantic and Gulf Coasts From Hurricanes and Sea Level Rise. GeoHealth . 2022;6(10):e2022GH000651. doi:10.1029/2022GH000651
38. The surge after the storm: the impact of Hurricane Sandy on hospitals in New York City | PreventionWeb. Published February 6, 2018. Accessed March 29, 2024. https://www.preventionweb.net/publication/surge-after-storm-impact-hurricane-sandy-hospitals-new-york-city
39. Hundreds of Hospitals on Atlantic and Gulf Coasts at Risk of Flooding from Hurricanes. C-CHANGE | Harvard T.H. Chan School of Public Health. Published September 29, 2022. Accessed March 29, 2024. https://www.hsph.harvard.edu/c-change/news/hundreds-of-hospitals-on-atlantic-and-gulf-coasts-at-risk-from-hurricanes/
40. Charlson F, Ali S, Benmarhnia T, et al. Climate Change and Mental Health: A Scoping Review. International Journal of Environmental Research and Public Health . 2021;18(9):4486. doi:10.3390/ijerph18094486
41. Hough E, Counts N. How Climate Change Affects Our Mental Health, and What We Can Do About It. doi:10.26099/rk6r-ne98
42. Majority of US adults believe climate change is most important issue today. https://www.apa.org. Accessed May 21, 2024. https://www.apa.org/news/press/releases/2020/02/climate-change
43. Fanzo JC, Downs SM. Climate change and nutrition-associated diseases. Nat Rev Dis Primers . 2021;7(1):1-2. doi:10.1038/s41572-021-00329-3
44. Owino V, Kumwenda C, Ekesa B, et al. The impact of climate change on food systems, diet quality, nutrition, and health outcomes: A narrative review. Front Clim . 2022;4. doi:10.3389/fclim.2022.941842
45. Climate Change & Nutrition. C-CHANGE | Harvard T.H. Chan School of Public Health. Published January 7, 2019. Accessed March 29, 2024. https://www.hsph.harvard.edu/c-change/subtopics/climate-change-nutrition/
46. Climate Change, Global Food Security, and the U.S. Food System | USDA. Accessed March 29, 2024. https://www.usda.gov/oce/energy-and-environment/food-security
47. Climate Explainer: Food Security and Climate Change. World Bank. Accessed March 29, 2024. https://www.worldbank.org/en/news/feature/2022/10/17/what-you-need-to-know-about-food-security-and-climate-change
Environment & Climate Change

The Covid-19 Response in New York City
Understanding CDC's Latest COVID-19 Isolation Guidance

Sarah Brown
Komal bajaj, birgitte messerschmidt.

International Trade and Climate Change Policy: A Conversation with Robert Lawrence

Harvard Project Director Robert Stavins Moderates Climate Action Week Panel on “Strategies for Mitigating Global Methane Emissions”

Land Use Policy and Climate Change: A Conversation with Charles Taylor
Climate Change and Health: Essay on the Limits of Naturalism
- First Online: 07 April 2023
Cite this chapter

- Marina Prieto Afonso Lencastre 5 , 6 ,
- Diogo Guedes Vidal 7 ,
- Eduardo Paz Barroso 5 , 8 ,
- Álvaro Campelo 5 , 6 , 9 ,
- Teresa Martinho Toldy 5 , 10 ,
- Susana Magalhães 5 , 11 ,
- Ana Gabriela Frazão-Nogueira 5 , 12 &
- Rui Estrada 5 , 13
Part of the book series: Climate Change Management ((CCM))
453 Accesses
1 Citations
One of the main problems of the twenty-first century is climate change and its impacts on global health. Nonetheless, there is a certain optimism that is rooted in the new world opened up by the possibilities of technoscience, namely in the control of health and climatic and environmental hazards. But on the horizon of these possibilities, there are increasingly clear signs that technological and scientific naturalism alone is running out of capacity to contain its own challenges. Naturalism has problems in resolving climate change impacts on health, founding ethics and epistemology, and defining relations with non-humans. In an era that is largely dependent on the actions that result from our thinking, there is a call to imagine multiverses or different versions of what naturalism seems to present as a single reality. This essay aims to explore the limits of naturalism to address climate change health hazards.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

Climate Change and the Role of Public Health in Egypt

Climate Change and Global Health
1POINTFIVE (2022) 1PointFive is developing practical decarbonization solutions at scale. https://www.1pointfive.com/about . Accessed 22 Jun 2022
Barroso EP, Estrada R (2018) De Hípias Menor a Trump: das virtudes do erro (e da mentira) ao erro da pós-verdade [From Hippias minor to Trump: from the virtues of error (and lies) to post-truth error]. Estud em Comun: 301–309. https://doi.org/10.20287/ec.n26.v1.a17
Beck U (2016) The metamorphosis of the world how climate change is transforming our concept of the world. Polity Press, Cambridge
Google Scholar
Bekoff M (2015) A vida emocional dos animais [The emotional life of animals]. Texto Editores, Lisboa
Bostrom N (2005) A history of transhumanist thought. J Evol Technol 14:1–25
Brymer E, Freeman E, Richardson M (2019) Editorial: One health: The well-being impacts of human-nature relationships. Front Psychol 10. https://doi.org/10.3389/fpsyg.2019.01611
Callicott B, Frodeman R (eds) (2009) Encyclopedia of climate change ethics and philosophy. Macmillan Gale, USA
Campelo A (2020) Como se faz o corpo. A construção da antropologia: da antropologia física à antropologia da saúde. In: Jorge VO (ed) (Coord,). Modos de Fazer / Ways of Making, Porto: Universidade do Porto—CITCEM, pp 137–158
Darwin C (1872) The expression of the emotions in man and animals. John Murray, London
Book Google Scholar
Delio I (2012) Transhumanism or ultrahumanism? Teilhard de chardin on technology, religion and evolution. Theol Sci 10:153–166. https://doi.org/10.1080/14746700.2012.669948
Article Google Scholar
Descola P (2005) Par-delà nature et culture [Beyond nature and culture]. Gallimard, Paris
Descola P (2018) Conversation: Philippe Descola. In: Fond. Louis Vuitt. https://www.youtube.com/watch?v=sTtBDfTLkhg&t=4464s
van Eersel P (2017) À la recherche de la vie intérieure [In search of inner life]. Albin Michel, Paris
Farahat A, Abuelgasim A (2022) Effect of cloud seeding on aerosol properties and particulate matter variability in the United Arab Emirates. Int J Environ Sci Technol 19:951–968. https://doi.org/10.1007/s13762-020-03057-5
Article CAS Google Scholar
Funtowicz SO, Ravetz JR (1993) Science for the post-normal age. Futures 25:739–755. https://doi.org/10.1016/0016-3287(93)90022-L
Gielen UP, Fish JM, Draguns JG (2004) Handbook of culture, therapy, and healing. Lawrence Erlbaum Associates Publishers, Mahwah
Goodall J, Hudson G (2015) Seeds of hope: wisdom and wonder from the world of plants. Grand Central Publishing, New York
Greco J (2003) Virtues in epistemology. In: Moser P (ed) The Oxford handbook of epistemology. Oxford University Press, New York, pp 287–312
Harari YN (2018) Sapiens. História Breve da Humanidade [Sapies. Brief history of humanity]. Elsinore, Amadora
Horin A, Lee K, Colloca L (2014) Placebo effects in therapeutic outcomes. Curr Clin Pharmacol 9:116–122. https://doi.org/10.2174/1574884708999140101145528
IPCC (2018) The Intergovernmental Panel on Climate Change. In: Glob. Warm. 1.5 °C. https://www.ipcc.ch/sr15/ . Accessed 21 Sep 2020
Kellert S (1991) Japanese perceptions of wildlife. Conserv Biol 5:297–308. https://doi.org/10.1111/j.1523-1739.1991.tb00141.x
Latour B (2016) Reset modernity! MIT Press, Cambridge, MA
Latour B (2017) Où atterrir ? Comment s’orienter en politique [Where to land? How to orient yourself in politics]. Ed. La Découverte, Paris
Lencastre MPA (2015) Ecologias e concepções culturais de saúde, doença e cura: Reflexões iniciais [Ecologies and cultural conceptions of health, illness and healing: initial reflections]. Sensos IO—Rev do Cent Investig e Inovação em Educ 5:169–184
Levin BW, Browner CH (2005) The social production of health: critical contributions from evolutionary, biological, and cultural anthropology. Soc Sci Med 61:745–750. https://doi.org/10.1016/j.socscimed.2004.08.048
Lewis-Fernández R, Kirmayer LJ (2019) Cultural concepts of distress and psychiatric disorders: understanding symptom experience and expression in context. Transcult Psychiatry 56:786–803. https://doi.org/10.1177/1363461519861795
Morin E (2000) Les Sept savoirs nécessaires à l’éducation du futur [The seven knowledges necessary for the education of the future]. Seuil, Paris
Nussbaum MC (2019) Sem Fins Lucrativos. Porque Precisa a Democracia das Humanidades [Non-profit. Why humanities need democracy]. Edições 70, Lisboa
Papa Francisco (2015) Laudato Sí. Sobre o cuidado da casa comum [Laudato Si. About the care of the common home]. Ed. Paulus, Apelação
Pecharroman LC (2018) Rights of nature: rivers that can stand in court. Resources 7. https://doi.org/10.3390/resources7010013
Pinker S (2018) Enlightment now. The case for reason, science, humanism and progress. Penguin Random House LLC, New York
Pinto MJ V (2005) Introdução. Os Sofistas e a Sofística [Introduction. The sophists and sophistry]. In: Sofistas. Testemunhos e Fragmentos. IN-CM, Lisboa, pp 11–39
Pires JC (1997) De profundis, valsa lenta [From deep, slow waltz]. Relógio D’Água, Lisboa
Platão (1973) Górgias. Verbo, Lisboa
Riviere C (1992) Attitudes africaines face à l’environnement [African attitudes towards the environment]. ANTHROPOS 87:365–378
Rossa-Roccor V, Giang A, Kershaw P (2021) Framing climate change as a human health issue: enough to tip the scale in climate policy? Lancet Planet Heal 5:e553–e559. https://doi.org/10.1016/S2542-5196(21)00113-3
Schmidt M, Soentgen J, Zapf H (2020) Environmental humanities: an emerging field of transdisciplinary research. GAIA Ecol Perspect Sci Soc 29:225–229. https://doi.org/10.14512/gaia.29.4.6
Singer M, Erickson PI (2011) A companion to medical anthropology. Wiley-Blackwell Ed, United Kingdom
Steffen W, Persson A, Deutsch L et al (2011) The anthropocene: from global change to planetary stewardship. Ambio 40:739–761. https://doi.org/10.1007/s13280-011-0185-x
Stuart-Smith S (2020) The well gardened mind. Rediscovering nature in the modern world. Harper Collins Publishers, London
Sussman LK (2004) The role of culture in definitions, interpretations, and management of illness. In: Gielen UP, Fish JM, Draguns JG (eds) Handbook of culture, therapy, and healing. Lawrence Erlbaum Associates Publishers, Mahwah, pp 37–65
The Royal Society of Medicine (2021) Confronting the health challenges of climate change. https://www.rsm.ac.uk/latest-news/2021/confronting-the-health-challenges-of-climate-change/ . Accessed 8 Apr 2022
Toldy T, Estrada R (2017) A vulnerabilidade como lugar ético: sobre De Profundis, Valsa Lenta, de José Cardoso Pires [Vulnerability as an ethical place: on De Profundis, Valsa Lenta, by José Cardoso Pires]. Didaskalia 47. https://doi.org/10.34632/didaskalia.2017.3272
Turnpenny J, Jones M, Lorenzoni I (2011) Where now for post-normal science?: A critical review of its development, definitions, and uses. Sci Technol Hum Values 36:287–306. https://doi.org/10.1177/0162243910385789
Viaene L (2022) Can rights of nature save us from the anthropocene catastrophe? Some critical reflections from the field. Asian J Law Soc 1–20. https://doi.org/10.1017/als.2022.2
Vidal DG, Oliveira GM, Pontes M et al (2022) The influence of social and economic environment on health. In: Prata JC, Isabel A (eds) One health. Elsevier, Amsterdam, pp 205–229
Chapter Google Scholar
Virilio P (1998) La bombe informatique, Galillé, Paris
De Waal WF (2009) The age of empathy: nature’s lessons for a kinder society. Harmony, USA
Watanabe M (1974) The conception of nature in Japanese culture. Science (80) 183:279–282. https://doi.org/10.1126/science.183.4122.279
Wohlleben P (2017) A vida secreta das plantas [The secret life of plants]. Sextante, Rio de Janeiro
Download references
Acknowledgements
This paper is based on the Introduction to the network project “Composing worlds: humanities, well-being and health in the 21st century” (Compor mundos: humanidades, bem-estar e saúde no século XXI), supported by Fundação Ensino e Cultura Fernando Pessoa (FFP).
Author information
Authors and affiliations.
FP-I3ID, Faculty of Human and Social Sciences, University Fernando Pessoa (UFP), Praça Nove de Abril, 349, 4249-004, Porto, Portugal
Marina Prieto Afonso Lencastre, Eduardo Paz Barroso, Álvaro Campelo, Teresa Martinho Toldy, Susana Magalhães, Ana Gabriela Frazão-Nogueira & Rui Estrada
Fernando Pessoa Behaviour and Social Sciences Research Centre (FP-B2S), University Fernando Pessoa (UFP), Praça Nove de Abril, 349, 4249-004, Porto, Portugal
Marina Prieto Afonso Lencastre & Álvaro Campelo
Centre for Functional Ecology—Science for People & the Planet (CFE), TERRA Associate Laboratory, Department of Life Sciences, University of Coimbra, Calçada Martim de Freitas, 3000-456, Coimbra, Portugal
Diogo Guedes Vidal
LabCom–Communication & Arts Research Unit, University of Beira Interior, Rua Marquês D’Ávila E Bolama, 6201-001, Covilhã, Portugal
Eduardo Paz Barroso
Centre for Research in Anthropology (CRIA), Edifício ISCTE, Sala 2w2, 1649-026, Lisbon, Portugal
Álvaro Campelo
Centre for Social Studies (CES), University of Coimbra, Colégio de S. Jerónimo, Apartado 3087, 3000-995, Coimbra, Portugal
Teresa Martinho Toldy
Instituto de Investigação e Inovação em Saúde (i3S), Universidade Do Porto, 4200-135, Porto, Portugal
Susana Magalhães
ICNOVA—Instituto de Comunicação da NOVA, Faculdade de Ciências Sociais E Humanas, Universidade NOVA de Lisboa, Lisbon, Portugal
Ana Gabriela Frazão-Nogueira
Center for Transdisciplinary Research «Culture, Space and Memory» (CITCEM), Faculty of Arts and Humanities of the University of Porto (FLUP), Via Panorâmica Edgar Cardoso S/N, 4150-564, Porto, Portugal
Rui Estrada
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
Faculty of Life Sciences, Hamburg University of Applied Sciences, Hamburg, Germany
Walter Leal Filho
Centre for Functional Ecology - Science for People & the Planet (CFE), TERRA Associate Laboratory, Department of Life Sciences (DCV), University of Coimbra (UC), Coimbra, Portugal
UFP Energy, Environment and Health Research Unit (FP-ENAS), University Fernando Pessoa (UFP), Porto, Portugal
Maria Alzira Pimenta Dinis
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Lencastre, M.P.A. et al. (2023). Climate Change and Health: Essay on the Limits of Naturalism. In: Leal Filho, W., Vidal, D.G., Dinis, M.A.P. (eds) Climate Change and Health Hazards. Climate Change Management. Springer, Cham. https://doi.org/10.1007/978-3-031-26592-1_2
Download citation
DOI : https://doi.org/10.1007/978-3-031-26592-1_2
Published : 07 April 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-26591-4
Online ISBN : 978-3-031-26592-1
eBook Packages : Earth and Environmental Science Earth and Environmental Science (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Climate Change Essay for Students and Children
500+ words climate change essay.
Climate change refers to the change in the environmental conditions of the earth. This happens due to many internal and external factors. The climatic change has become a global concern over the last few decades. Besides, these climatic changes affect life on the earth in various ways. These climatic changes are having various impacts on the ecosystem and ecology. Due to these changes, a number of species of plants and animals have gone extinct.

When Did it Start?
The climate started changing a long time ago due to human activities but we came to know about it in the last century. During the last century, we started noticing the climatic change and its effect on human life. We started researching on climate change and came to know that the earth temperature is rising due to a phenomenon called the greenhouse effect. The warming up of earth surface causes many ozone depletion, affect our agriculture , water supply, transportation, and several other problems.
Reason Of Climate Change
Although there are hundreds of reason for the climatic change we are only going to discuss the natural and manmade (human) reasons.
Get the huge list of more than 500 Essay Topics and Ideas
Natural Reasons
These include volcanic eruption , solar radiation, tectonic plate movement, orbital variations. Due to these activities, the geographical condition of an area become quite harmful for life to survive. Also, these activities raise the temperature of the earth to a great extent causing an imbalance in nature.
Human Reasons
Man due to his need and greed has done many activities that not only harm the environment but himself too. Many plant and animal species go extinct due to human activity. Human activities that harm the climate include deforestation, using fossil fuel , industrial waste , a different type of pollution and many more. All these things damage the climate and ecosystem very badly. And many species of animals and birds got extinct or on a verge of extinction due to hunting.
Effects Of Climatic Change
These climatic changes have a negative impact on the environment. The ocean level is rising, glaciers are melting, CO2 in the air is increasing, forest and wildlife are declining, and water life is also getting disturbed due to climatic changes. Apart from that, it is calculated that if this change keeps on going then many species of plants and animals will get extinct. And there will be a heavy loss to the environment.
What will be Future?
If we do not do anything and things continue to go on like right now then a day in future will come when humans will become extinct from the surface of the earth. But instead of neglecting these problems we start acting on then we can save the earth and our future.

Although humans mistake has caused great damage to the climate and ecosystem. But, it is not late to start again and try to undo what we have done until now to damage the environment. And if every human start contributing to the environment then we can be sure of our existence in the future.
{ “@context”: “https://schema.org”, “@type”: “FAQPage”, “mainEntity”: [ { “@type”: “Question”, “name”: “What is climate change and how it affects humans?”, “acceptedAnswer”: { “@type”: “Answer”, “text”: “Climate change is a phenomenon that happens because of human and natural reasons. And it is one of the most serious problems that not only affect the environment but also human beings. It affects human in several ways but in simple language, we can say that it causes many diseases and disasters that destroy life on earth.” } }, { “@type”: “Question”, “name”: “Can we stop these climatic changes?”, “acceptedAnswer”: { “@type”: “Answer”, “text”: “Yes, we can stop these climatic changes but for that, every one of us has to come forward and has to adapt ways that can reduce and control our bad habits that affect the environment. We have to the initiative and make everyone aware of the climatic changes.” } } ] }
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Climate Change and Health: A Position Paper of the American College of Physicians
- PMID: 27089232
- DOI: 10.7326/M15-2766
Climate change could have a devastating effect on human and environmental health. Potential effects of climate change on human health include higher rates of respiratory and heat-related illness, increased prevalence of vector-borne and waterborne diseases, food and water insecurity, and malnutrition. Persons who are elderly, sick, or poor are especially vulnerable to these potential consequences. Addressing climate change could have substantial benefits to human health. In this position paper, the American College of Physicians (ACP) recommends that physicians and the broader health care community throughout the world engage in environmentally sustainable practices that reduce carbon emissions; support efforts to mitigate and adapt to the effects of climate change; and educate the public, their colleagues, their community, and lawmakers about the health risks posed by climate change. Tackling climate change is an opportunity to dramatically improve human health and avert dire environmental outcomes, and ACP believes that physicians can play a role in achieving this goal.
PubMed Disclaimer
- Addressing Air Quality and Health as a Strategy to Combat Climate Change. Joy EA, Horne BD, Bergstrom S. Joy EA, et al. Ann Intern Med. 2016 May 3;164(9):626-7. doi: 10.7326/M16-0507. Epub 2016 Apr 19. Ann Intern Med. 2016. PMID: 27089453 No abstract available.
- Climate Change and Health. Crowley RA, Moyer DV, DeLong DM. Crowley RA, et al. Ann Intern Med. 2016 Nov 15;165(10):747-748. doi: 10.7326/L16-0411. Ann Intern Med. 2016. PMID: 27842409 No abstract available.
- Climate Change and Health. Berman DS. Berman DS. Ann Intern Med. 2016 Nov 15;165(10):746. doi: 10.7326/L16-0412. Ann Intern Med. 2016. PMID: 27842410 No abstract available.
- Climate Change and Health. Mondrow E. Mondrow E. Ann Intern Med. 2016 Nov 15;165(10):745-746. doi: 10.7326/L16-0413. Ann Intern Med. 2016. PMID: 27842411 No abstract available.
- Climate Change and Health. Reines EJ. Reines EJ. Ann Intern Med. 2016 Nov 15;165(10):746-747. doi: 10.7326/L16-0414. Ann Intern Med. 2016. PMID: 27842412 No abstract available.
Similar articles
- Climate changes, environment and infection: facts, scenarios and growing awareness from the public health community within Europe. Bezirtzoglou C, Dekas K, Charvalos E. Bezirtzoglou C, et al. Anaerobe. 2011 Dec;17(6):337-40. doi: 10.1016/j.anaerobe.2011.05.016. Epub 2011 Jun 2. Anaerobe. 2011. PMID: 21664978
- Climate Change, Human Rights, and Social Justice. Levy BS, Patz JA. Levy BS, et al. Ann Glob Health. 2015 May-Jun;81(3):310-22. doi: 10.1016/j.aogh.2015.08.008. Ann Glob Health. 2015. PMID: 26615065 Review.
- The physician's response to climate change. Sarfaty M, Abouzaid S. Sarfaty M, et al. Fam Med. 2009 May;41(5):358-63. Fam Med. 2009. PMID: 19418286
- The Changing Climate: Managing Health Impacts. Parker CL, Wellbery CE, Mueller M. Parker CL, et al. Am Fam Physician. 2019 Nov 15;100(10):618-626. Am Fam Physician. 2019. PMID: 31730308 Review.
- What would an environmentally sustainable reproductive technology industry look like? Richie C. Richie C. J Med Ethics. 2015 May;41(5):383-7. doi: 10.1136/medethics-2013-101716. Epub 2014 Jul 24. J Med Ethics. 2015. PMID: 25060852
- Patients' perceptions of climate-sensitive health counselling in primary care: Qualitative results from Germany. Griesel S, Schwerdtle PN, Quitmann C, Danquah I, Herrmann A. Griesel S, et al. Eur J Gen Pract. 2023 Dec;29(1):2284261. doi: 10.1080/13814788.2023.2284261. Epub 2023 Nov 27. Eur J Gen Pract. 2023. PMID: 38010828 Free PMC article.
- "Green informed consent" in the classroom, clinic, and consultation room. Richie C. Richie C. Med Health Care Philos. 2023 Dec;26(4):507-515. doi: 10.1007/s11019-023-10163-x. Epub 2023 Aug 16. Med Health Care Philos. 2023. PMID: 37584839 Free PMC article.
- Climate Change and Pregnancy: Risks, Mitigation, Adaptation, and Resilience. Fan W, Zlatnik MG. Fan W, et al. Obstet Gynecol Surv. 2023 Apr;78(4):223-236. doi: 10.1097/OGX.0000000000001116. Obstet Gynecol Surv. 2023. PMID: 37043299 Free PMC article.
- How Ophthalmologists Can Decarbonize Eye Care: A Review of Existing Sustainability Strategies and Steps Ophthalmologists Can Take. Sherry B, Lee S, Ramos Cadena MLA, Laynor G, Patel SR, Simon MD, Romanowski EG, Hochman SE, Schuman JS, Prescott C, Thiel CL. Sherry B, et al. Ophthalmology. 2023 Jul;130(7):702-714. doi: 10.1016/j.ophtha.2023.02.028. Epub 2023 Mar 6. Ophthalmology. 2023. PMID: 36889466 Free PMC article. Review.
- Climate Change and Household Debt in Rural India. Kandikuppa S, Gray C. Kandikuppa S, et al. Clim Change. 2022 Aug;173(3-4):20. doi: 10.1007/s10584-022-03407-x. Epub 2022 Aug 6. Clim Change. 2022. PMID: 36872918 Free PMC article.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
Other Literature Sources
- scite Smart Citations
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
August 8, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Increasing clinicians' knowledge about climate change's impact on health and health care sustainability
by Massachusetts General Hospital

An educational program emphasizing the relationship that climate change has with health and health care environmental sustainability was well-received by physicians, according to a recent survey-based study published in JAMA Network Open and conducted by investigators at Massachusetts General Hospital (MGH), a founding member of the Mass General Brigham health care system.
The program provided a foundation about climate change and the impact of fossil fuel-related pollution on health; the health care system's contribution to carbon pollution; and opportunities to address these challenges. To the team's knowledge, MGH is the first academic medical center to offer incentivized educational programs on climate change and environmental sustainability in health care.
"Climate change is a fundamental threat that is recognized by many to be the greatest health crisis humans have ever faced. However, surveys show that the majority of physicians do not feel prepared to address climate change's impact on health or to take action," said lead author Wynne Armand, MD, an associate director of the Center for the Environment and Health at MGH and an assistant professor of medicine at Harvard Medical School.
In their study, Armand and her colleagues surveyed the response to climate change–focused educational modules offered at MGH, an academic medical center, through an existing biannual physician quality incentive program.
Among a total of 2,559 eligible physicians and psychologists, 2,417 (94.5%) completed the educational modules. Of these participants, 73.1% thought that the modules were relevant or very relevant to their lives, and 65.4% found the modules relevant or very relevant to their clinical practices.
Age did not influence the degree to which physicians thought climate-related education was relevant to their individual lives or practices. Clinicians identifying as female were more likely to consider the education as relevant compared with male clinicians.
As expected, physicians in specialties that specifically treat problems more directly exacerbated by climate change, like emergency medicine /urgent care, allergy and primary care , were more likely to find the trainings relevant to their practices.
"Our findings indicate that educational strategies should be tailored by specialty to better engage clinicians in learning about climate change's health effects and ways to mitigate health sector contributions," said Armand.
Optional comments were provided by 446 (18.5%) of respondents—56.1% were positive, 36.5% were neutral, and 7.4% were negative. Many positive comments supported the importance of the topic and provided suggestions for reducing the carbon footprint of the hospital. Others asked for additional ways to get involved.
Negative comments stated that quality improvement trainings should focus on patient care and that providing climate information to clinicians is inappropriate given their limited influence on hospital-wide policies.
Overall, the survey results indicate that most physicians believe that education on the complex relationships between climate change and health care is important, and they welcome opportunities for action. Importantly, participants felt that their knowledge on these topics increased after completing the modules.
Similar efforts across the health care sector may help all those involved to recognize and address the health risks of climate change and take steps to minimize their contribution to the problem.
Explore further
Feedback to editors

US health regulator rejects MDMA treatment for PTSD, for now
Aug 10, 2024

Study finds baked potatoes can improve heart health for diabetics
Aug 9, 2024

National study shows how internal medicine chief residency has changed over 20 years

Vegan diet better than Mediterranean, finds new research

Memory problems in old age linked to a key enzyme, study in mice finds

Key factor found in drug-context links, relapse

Researchers outline promises, challenges of understanding AI for biological discovery

The dengue vaccine is effective and safe: Confirmation from the first global meta-analysis

'PTNM' system provides new classification for Peyronie's disease and penile curvature

Researchers crack a key celiac mystery: Where the gluten reaction begins
Related stories.

Girls more anxious about climate change than boys, study shows
Aug 6, 2024

Recommendations address impact of climate change on child health
Feb 20, 2024

Nearly half of mental health practitioners say they are unprepared to help clients cope with climate change
Aug 28, 2023

Public health beliefs predict support for climate action, study shows
Jun 25, 2024
Climate change: University researchers feel powerless to take action, says survey
Jan 31, 2024

Survey finds that physicians are concerned about private equity investment in the health care sector
Mar 12, 2024
Recommended for you

A new way to measure bipolar disorder: Focus on the 'spikes'

Pathways linking body and brain health and impacts to mental health revealed
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
- Diagnostics
- Health Tech
- Medical Devices

How climate change is affecting your health
Climate crisis is also becoming a health crisis. know how the ramifications of the phenomenon are impacting people worldwide..

The fishing communities of Sri Lanka are facing an alarming health crisis. According to a recent report published in The New York Times, young men in their 30s and 40s have been turning up at hospitals with late-stage kidney failure, needing dialysis or even transplants. In some communities, as many as one in five young men is affected. Although the exact cause of their condition is not clear, experts say the illness is most likely the result of exposure to extreme heat, exacerbated in recent years by climate change, among other reasons.
Similarly, a new study published in the journal Nature Communications shows that climate change is directly affecting the survival of newborns in low- and middle-income countries, with 4.3% of neonatal deaths during the study period (2001-2019) attributed to non-optimal temperatures with both high and low ambient temperatures posing a risk.

The list goes on. The International Labour Organization (ILO), in its report ‘Ensuring Safety and Health at Work in a Changing Climate’, highlights that the global workforce is facing a serious health crisis due to the negative impacts of climate change. The report says that the climate crisis could expose 2.4 billion workers to health hazards like cancer, cardiovascular illness, kidney dysfunction, and physical injury. It says that excessive heat affects 70% of the global workforce of 3.4 billion people. Amid such an evident and real threat of climate change, it becomes imperative to understand how the ramifications of the phenomenon, directly and indirectly, impact human health worldwide.

Crisis is real
Experts say climate change is intimately linked to our health, habits and well-being. It is affecting and influencing the food we eat, the water we drink, the air we breathe, and the weather we experience —all of which pose a health risk. “The impact can be as direct as physical injury caused by floods and hurricanes or it can be as insidious as the long-term harm caused by global warming and worsening air pollution,” says Dr Vineet Talwar, director of medical oncology at Rajiv Gandhi Cancer Institute and Research Centre, Delhi.
It has been seen that changes in humidity, temperature and particulate pollutants in the air affect the respiratory and cardiovascular systems, especially in those with underlying heart or lung ailments. Rising temperatures lead to heat-related illnesses including heat stroke, cardiovascular problems and kidney disease. Extreme weather events like floods and hurricanes can cause injuries, drownings, and mental health issues.
Air pollution, exacerbated by climate change, increases respiratory diseases and allergies. Vector-borne diseases such as malaria and dengue fever spread to new areas as temperatures rise. Food and water insecurity resulting from changing weather patterns can lead to malnutrition and waterborne illnesses.
“The health impacts of climate change are wide-ranging and affect vulnerable populations disproportionately, including children, the elderly, and those in low-income areas,” says Dr Rakesh Gupta, senior consultant, internal medicine, Indraprastha Apollo Hospitals , Delhi.
Dr Sameer Punia, senior consultant, paediatric intensivist, Aakash Healthcare in Delhi, also notes that the effects of climate change on mother and infant health are both direct and indirect. “Unfavourable health consequences, including miscarriage, low birth weight, starvation, and respiratory illness, can result from exposure to stressors associated with the environment,” he says.
Kidney diseases
A recent report in The Lancet has found that chronic kidney disease patients living in the hottest countries experienced an additional 8% drop in kidney function each year compared to those living in temperate climates. Additionally, for every 1 degree Celsius rise in temperature, the estimated risk of hospitalisation for renal diseases lasting up to 7 days increased by 0.9%, affecting mostly children, women, and the elderly population, according to a study of ambient temperature and hospitalisation for renal diseases in Brazil during 2000–2015. According to scientific data, a 1 degree-Celsius increase in temperature increases the risk of kidney failure by 1.1% and the risk of death from kidney failure, urolithiasis, acute kidney injury (AKI), and urinary tract infection (UTI) by 3.1%.
So how is the kidney becoming a direct victim of climate change? “As the temperature rises, there are increased chances of dehydration, and gastrointestinal infections. It can cause people, especially those working in extreme climates, to have heat stroke and impact their kidneys,” says Dr Vikram Kalra, consultant nephrologist, CK Birla Hospital, Delhi.
“Heat stress, a direct consequence of rising temperatures, can lead to chronic kidney disease by causing repeated dehydration and electrolyte imbalances. The kidneys are especially vulnerable due to their role in fluid regulation and waste removal,” explains Dr Gupta of Indraprastha Apollo Hospitals. “When the kidneys lack adequate water, they enter a shock state, producing less urine, which results in acute kidney injury. Significant damage to the kidneys from acute kidney injury can lead to chronic kidney disease in the future,” further elaborates Dr Sanjiv Saxena, chairman of PSRI Institute of Nephrology in Delhi.
Neonatal deaths
The study published in Nature Communications categorically says that climate change was responsible for 32% of heat-related neonatal deaths while simultaneously decreasing the toll from cold temperatures by 30%.
Paediatricians explain how climate change can cause neonatal deaths. Dr Poonam Sidana, director of neonatology and paediatrics at CK Birla Hospital in Delhi, says newborn babies are vulnerable as their body cannot control their temperature.
“Even in a healthy newborn, we say that if you keep the baby in a cold environment, the baby will get cold very easily. They have a high surface area, they are not able to curl up like what we adults can do and they are not able to shiver and generate heat,” she explains, adding that they cannot sweat either. Hence, higher temperatures put a demand on their vulnerable and
under-developed physiology and thermoregulatory systems, and they get dehydrated very quickly which can cause electrolyte imbalances, hyperthermia, lethargy, feeding less, and higher heat rates, causing more oxygen demands, also leading to thromboembolism (blood clot). “This can result in severe complications such as seizures, organ failure and death,” explains Dr Gupta of Indraprastha Apollo Hospitals.
Maternal heat stress during pregnancy can lead to preterm birth and low birth weight, increasing neonatal mortality risks. Climate-driven food insecurity may also contribute to maternal and neonatal malnutrition, further compromising newborn health and survival, doctors say. At the same time, they note that air pollution exacerbated by climate change can cause respiratory distress in newborns and cause development problems.
It is needless to highlight that extreme weather events may disrupt healthcare services, affecting neonatal care. Extreme weather events and food insecurity due to climate change can lead to malnutrition and hindered growth, further increasing the risk of neonatal deaths, says Dr Punia of Aakash Healthcare in Delhi.
Cancer development
Research shows that climate change cannot just increase the occurrence of cancer but also have a detrimental impact on its diagnosis, treatment, and overall care. Dr Mandeep Singh Malhotra, director of surgical oncology at CK Birla Hospital in Delhi, says with temperature rise, particulate matter in the air will also increase and persist for a longer period, and cases of cancer-related to air pollution, oral cancer, lung cancer, food pipe cancer, and cervical cancer will increase.
He also says that virus-induced cancers by HPV, EBV (Epstein-Barr virus), and Hepatitis virus will increase with their virulence. With an enlarged hole in the ozone layer, and increased penetration of UV rays, instances of skin cancer will be higher. “It increases the risk of skin cancer and the kind of aggressive skin cancer known as melanoma by about 25% when the ozone layer is damaged,” says Dr Puneet Gupta, chairman, oncology, Asian Hospital, Faridabad.
The carcinogenic effect of pesticides and contaminants in water will be higher as high temperature increases their chemical reaction and oxidation, he says, adding, “smog or industrial waste, pesticides, and herbicides, everything becomes more potentiated when there is a higher temperature. That is what is hypothesised that this would cause an overall increase in cancer.”
He also says that toxins released by fungi in the air such as aflatoxins which cause lung cancer or aspergillosis, will increase resulting in higher cases of lung-related cancer and other diseases. Immunity in particular gets reduced with heat and heat strokes, especially in vulnerable populations like children and the elderly increasing the mortality of cancer. In terms of diagnosis and treatment, doctors say that screening will have to be heightened and tolerance to treatment, chemotherapy, radiation, and recovery from surgery will be reduced resulting in the recurrence of cancer. “Climate change is closely interwoven with not only the etiology of cancer but also treatment tolerance and compliance among cancer patients,” comments Dr Talwar of Rajiv Gandhi Cancer Institute and Research Centre.
“By 2030, there is going to be a global cancer epidemic. If global warming rises to 1.5 degrees, then this deadly combination will be catastrophic to many human populations all around the globe,” warns Dr Gupta of Asian Hospital.
Get live Share Market updates, Stock Market Quotes , and the latest India News … Read More and business news on Financial Express. Download the Financial Express App for the latest finance news.
- Stock Market Stats
Related News
The Paris Olympics 2024 has come to a close after two weeks of intense competition, with the US finishing at the top of the medal tally with 126 medals. Novak Djokovic won his first Olympic medal and St Lucia and Pakistan celebrated their first-ever individual Gold medals. India’s Vinesh Phogat made history as the country’s first female wrestler to reach the Olympic finals.
Photo Gallery
21 Anubhuti coaches with aircraft-like features to replace Shatabdi 1st-AC Executive chair cars; 20 amazing facts
9 Rs 50, Rs 200, Rs 500 and Rs 2000 notes images: Here are the new currency notes released by RBI
10 Indian Railways tickets: All you want to know about your ticket in 10 slides
Trending Topics
- Mutual Funds
- IPO’s Open and Upcoming 6
- Top Indices Performance
- Stock Analysis
- Financial Literacy
- Gold Rate Today
- NSE Top Gainers 1636
- NSE Top Losers 994
- BSE Top Gainers 2756
- BSE Top Losers 1950
- NSE 52-Week High 0
- NSE 52-Week Low 0
- BSE 52-Week High 0
- BSE 52-Week Low 0
- NSE Price Shocker
- NSE Volume Shocker
- BSE Price Shocker
- BSE Volume Shocker
- NSE Sellers
- BSE Sellers
- Silver Rate Today
- Petrol Rate Today
- Diesel Rate Today
Advertisement
Where Tim Walz Stands on the Issues
As governor of Minnesota, he has enacted policies to secure abortion protections, provide free meals for schoolchildren, allow recreational marijuana and set renewable energy goals.
- Share full article

By Maggie Astor
- Aug. 6, 2024
Gov. Tim Walz of Minnesota, the newly announced running mate to Vice President Kamala Harris, has worked with his state’s Democratic-controlled Legislature to enact an ambitious agenda of liberal policies: free college tuition for low-income students, free meals for schoolchildren, legal recreational marijuana and protections for transgender people.
“You don’t win elections to bank political capital,” Mr. Walz wrote last year about his approach to governing. “You win elections to burn political capital and improve lives.”
Republicans have slammed these policies as big-government liberalism and accused Mr. Walz of taking a hard left turn since he represented a politically divided district in Congress years ago.
Here is an overview of where Mr. Walz stands on some key issues.
Mr. Walz signed a bill last year that guaranteed Minnesotans a “fundamental right to make autonomous decisions” about reproductive health care on issues such as abortion, contraception and fertility treatments.
Abortion was already protected by a Minnesota Supreme Court decision, but the new law guarded against a future court reversing that precedent as the U.S. Supreme Court did with Roe v. Wade, and Mr. Walz said this year that he was also open to an amendment to the state’s Constitution that would codify abortion rights.
Another bill he signed legally shields patients, and their medical providers, if they receive an abortion in Minnesota after traveling from a state where abortion is banned.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .

COMMENTS
Climate change affects food availability, quality and diversity, exacerbating food and nutrition crises. Temperature and precipitation changes enhance the spread of vector-borne diseases. Without preventive actions, deaths from such diseases, currently over 700 000 annually, may rise. Climate change induces both immediate mental health issues ...
Air pollution is detrimental to human health. Malnutrition is linked to a variety of illnesses, including heart disease, cancer, and diabetes. It can also increase the risk of stunting, or ...
One study projects that, because of climate change, up to an additional 51.3 million people will be at risk from exposure to malaria in Western Africa by 2050. These shifts can heighten suffering, increase countries' burdens of disease and cause epidemics. The World Health Organization (WHO) estimates that one-sixth of illness and disability ...
These changes pose fundamental threats to human well-being and health. 4,7 For example, a positive relationship has been observed between regional trends in climate (rising temperatures and ...
Introduction. The environmental consequences of climate change such as sea-level rise, increasing temperatures, more extreme weather events, increased droughts, flooding and wildfires are impacting human health and lives. 1 2 Previous studies and reviews have documented the multiple health impacts of climate change, including an increase in infectious diseases, respiratory disorders, heat ...
Climate change has been identified as potentially the greatest health challenge of the twenty-first century 2, 3. It is bringing more deadly extreme heat and wildfires, increasing noncommunicable ...
People's health, lives and livelihoods, as well as property and critical infrastructure, including energy and transportation systems, are being increasingly adversely affected by hazards from heatwaves, storms, drought and flooding as well as slow-onset changes, including sea level rise. ... Climate Change 2022: Impacts, Adaptation and ...
Climate change (CC) is responsible for the rapid dissemination and exaggeration of certain epidemics and pandemics. In addition to the vast apparent impacts of climate change on health, forestry, agriculture, etc., it may also have psychological implications on vulnerable societies.
Talking about climate change and health. Nature Climate Change 14 , 409 ( 2024) Cite this article. The climate crisis is also an urgent and ongoing health crisis with diverse human impacts leading ...
C ONCLUSION. This document explains that there are well-understood physical mechanisms by which changes in the amounts of greenhouse gases cause climate changes. It discusses the evidence that the concentrations of these gases in the atmosphere have increased and are still increasing rapidly, that climate change is occurring, and that most of ...
Climate change arguably represents one of the greatest global health threats of our time. Health professionals can advocate for global efforts to reduce emissions and protect people from climate change; however, evidence of their willingness to do so remains scarce. In this Viewpoint, we report findings from a large, multinational survey of health professionals (n=4654) that examined their ...
Tackling the health impacts of climate change in the twenty-first century Footnote * * The winner of the 2017 Holdstock-Piachaud Student Essay Prize, in memory of Douglas Holdstock and Jack Piachaud who were for many years inspirational editors of this journal, were Nicholas Heng and Anna Nakamura.
climate change on human health so that we can both mitigate and adapt to the environmental effects of climate change in the healthiest and most efficient ways. Although the group recog nizes the global nature of climate change's impacts on human health, the primary focus of this paper is on the situation in the United States.
Climate change is taking a toll on human health, and some leaders in the public health community have urged their colleagues to give voice to its health implications. Previous research has shown that Americans are only dimly aware of the health implications of climate change, yet the literature on issue framing suggests that providing a novel frame - such as human health - may be potentially ...
Climate change impacts human health in both direct and indirect ways 1 , 2 . Extreme heat waves, rising sea level, changes in precipitation resulting in flooding and droughts, and intense hurricanes can directly cause injury, illness, and even death 3 . The effects of climate change can also indirectly affect health through alterations to the ...
The rapid anthropogenic climate change that is being experienced in the early twenty-first century is intimately entwined with the health and functioning of the biosphere. ... We close this section of the thematic issue with a thought-provoking essay by ... (2023) The Effects of Climate Change on Human Health and the Healthcare Sector Climate ...
A total of 2143 unique articles and journalistic essays satisfied the inclusion criteria, for the period 1989-2013 inclusive. The full database is available in the supplementary material. This shows the year, lead author (at least), journal, title and primary search method. ... In contrast, two papers about climate change and health in Nepal ...
Average global temperatures have increased by 2.2 degrees Fahrenheit, or 1.2 degrees Celsius, since 1880, with the greatest changes happening in the late 20th century. Land areas have warmed more ...
Human health has always been influenced by climate and weather.Changes in climate and climate variability, particularly changes in weather extremes, affect the environment that provides us with clean air, food, water, shelter, and security. Climate change, together with other natural and human-made health stressors, threatens human health and well-being in numerous ways.
The World Health Organization (WHO) calls climate change "the biggest global health threat of the twenty-first century". Human-caused climate change is increasing the frequency and intensity ...
Climate change alters health both through long-term stressors, such as air pollution 1 and vector-borne diseases 2, and through acute events, such as heat waves 3 and hurricanes. 4 These long and short term elements collectively influence public health around the world. Climate change has health consequences from the scale of entire populations ...
Naturalism and Climate Change. The Intergovernmental Panel on Climate Change states that if an immediate and important decrease in greenhouse emissions does not take place, the goal of a 1.5 °C global temperature rise will be overcome, and result in increasing heat waves and long warmer, and short colder seasons.This CC will have critical effects on agriculture and health.
Climate change refers to the change in the environmental conditions of the earth. This happens due to many internal and external factors. The climatic change has become a global concern over the last few decades. Besides, these climatic changes affect life on the earth in various ways. These climatic changes are having various impacts on the ...
Climate change can have a range of impacts on physical, mental, and community health. A warmer climate is expected to increase the risk of illnesses and death from extreme heat and poor air quality. Climate change will likely increase the frequency and strength of extreme events (such as floods, droughts, and storms) that threaten human health ...
Addressing climate change could have substantial benefits to human health. In this position paper, the American College of Physicians (ACP) recommends that physicians and the broader health care community throughout the world engage in environmentally sustainable practices that reduce carbon emissions; support efforts to mitigate and adapt to ...
The program provided a foundation about climate change and the impact of fossil fuel-related pollution on health; the health care system's contribution to carbon pollution; and opportunities to ...
The last climate resolution adopted by the WHA (in 2008) was primarily focused on adapting the health sector to climate change impacts. This new resolution describes a broader and more proactive role for member states and their health sectors in efforts to become more sustainable while responding to those risks that cannot be avoided. Member ...
Crisis is real. Experts say climate change is intimately linked to our health, habits and well-being. It is affecting and influencing the food we eat, the water we drink, the air we breathe, and ...
As governor of Minnesota, he has enacted policies to secure abortion protections, provide free meals for schoolchildren, allow recreational marijuana and set renewable energy goals.