An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- World J Psychiatry
- v.11(7); 2021 Jul 19

History of the dopamine hypothesis of antipsychotic action
Mary v seeman.
Department of Psychiatry, University of Toronto, Toronto M5P 3L6, Ontario, Canada. [email protected]
Corresponding author: Mary V Seeman, OC, MDCM, DSc, Professor Emerita, Department of Psychiatry, University of Toronto, 260 Heath Street West, Suite #605, Toronto M5P 3L6, Ontario, Canada. [email protected]
The dopamine hypothesis of how antipsychotic drugs exert their beneficial effect in psychotic illness has an interesting history that dates back to 1950. This hypothesis is not to be confused with the dopamine hypothesis of schizophrenia; the aim of the latter is to explain the etiology of schizophrenia. The present review does not deal with schizophrenia but, rather, with the historical development of our current understanding of the dopamine-associated actions of the drugs that reduce the symptoms of psychosis. This historical review begins with the serendipitous discovery of chlorpromazine, a drug synthesized around a chemical core that initially served to produce man-made dyes. This molecular core subsequently contributed to the chemistry of antihistamines. It was with the aim of producing a superior antihistamine that chlorpromazine was synthesized; instead, it revolutionized the treatment of psychosis. The first hypothesis of how this drug worked was that it induced hypothermia, a cooling of the body that led to a tranquilization of the mind. The new, at the time, discoveries of the presence of chemical transmitters in the brain soon steered investigations away from a temperature-related hypothesis toward questioning how this drug, and other drugs with similar properties and effects, modulated endogenous neurotransmission. As a result, over the years, researchers from around the world have begun to progressively learn what antipsychotic drugs do in the brain.
Core Tip: This history starts with the synthesis of chlorpromazine in 1950 and traces the steps taken to discover how this drug, and related drugs, work to reduce, sometimes to reverse, the delusions and hallucinations associated with psychosis. The task to understand how these drugs work in the brain continues, as many unknowns remain.
INTRODUCTION
The synthesis of chlorpromazine in 1950 marks the beginning of modern psychopharmacology. While the clinical usefulness of this drug was almost immediately recognized, it took another 20 years to begin to uncover its mode of action. This review covers the history of these years and the steps that were taken to arrive at the dopamine hypothesis of antipsychotic drug action. It more briefly also outlines how this hypothesis has fared over the ensuing years (Table (Table1). 1 ).
Major steps in the dopamine hypothesis of antipsychotic drug action
| 1950 | Synthesis of chlorpromazine[ ] |
| 1952 | Preliminary evidence of antipsychotic effect of chlorpromazine[ , , ] |
| 1958 | Synthesis of haloperidol[ ] |
| 1960 | Parkinson basal ganglia are deficient in dopamine[ ] |
| 1963 | Neuroleptics raise level of monoamine metabolites[ ] |
| 1966 | Neuroleptics may antagonize dopamine receptors[ ] |
| 1971 | 2 nmol haloperidol in plasma effective in psychosis[ ] |
| 1974 | Synthesis of (+-) butaclamol[ ] |
| 1975 | Tritiated haloperidol binds DA receptors[ ] |
| 1975 | Effective neuroleptic dose correlates with D2 block[ ] |
| 1979 | Multiple dopamine receptors[ ] |
| 1984 | Bimodal D2 distribution in schizophrenia[ ] |
| 1984 | High and low affinity states for D2[ ] |
| 1988 | Cloning of the D2 receptor[ ] |
| 1988 | imaging of D2 occupancy[ ] |
| 1990 | Cloning of D3[ ] |
| 1999 | Fast-off theory[ ] |
| 2000 | Multiple genetic variants of D2 receptor[ - ] |
| 2000 | Impact of the D3 receptor[ ] |
| 2005 | Impact of other neurotransmitter receptors[ ] |
| 2010 | Impact of receptor heterodimers[ ] |
| 2017 | Impact of D2 high affinity state[ ] |
| 2021 | Structure and specificities of D1, D2 signaling complexes[ ] |
Prior to the availability of chlorpromazine, many drugs had been used in psychiatry to tranquilize agitated patients, but this was the first psychoactive agent to not only calm patients, but also to decrease the intensity of their psychotic symptoms. Synthesized by Paul Charpentier of the French pharmaceutical company Rhône-Poulenc, chlorpromazine was the product of a long process that began in the mid-1800s, starting out as a search for a method to synthesize dyes. This search led, in 1883, to the identification by August Bernthsen of a molecular structure, which he called a phenothiazine nucleus, around which later generations of chemists began to make antihistamine drugs for the treatment of allergies. In 1947, the pharmaceutical company, Rhône-Poulenc, produced promethazine, a first generation antihistamine[ 1 ] (Figure (Figure1). 1 ).

Promethazine.
Promethazine induced hypothermia in laboratory animals so, in 1949, French military surgeon, Laborit[ 2 ] tried giving it to soldiers in order to lower their body temperature and prevent shock before, during, and after surgical operations. He noted that promethazine induced a “euphoric quietude” in his soldiers[ 2 ].
Hoping to increase the potency of promethazine, on December 11, 1950, Charpentier et al [ 3 ] introduced a chlorine atom into one of the rings of promethazine (Figure (Figure2). 2 ).

Chlorpromazine.
The new drug was called RP (for Rhône-Poulenc) 4560. It was tested on rats and produced “detachment, slow reaction to stimuli, and a decrease in initiative.” The compound was again sent for human trials to Laborit, now at the Val de-Grâce Hospital in Paris, and, because of its psychological effects in animals, to a variety of French psychiatrists as well.
The first published report of its effect in humans was by Laborit and his team in February 1952. They reported that the drug calmed anxious patients without producing oversedation[ 4 ]. Three psychiatrists reported on the effect of the drug one month later[ 5 ]. This team concluded that 50-100 mg of RP4560, diluted in a glucose solution and given intravenously to patients with mania, kept them calm for 3 to 18 h, as long as an analgesic or a barbiturate was administered concurrently.
In May 1952, psychiatrists Delay and Deniker[ 6 ] published their observation on the soothing effect of the drug in patients with psychosis[ 6 ]. In June, this team once again reported positive results[ 7 ]. Going on the theory that the drug worked by cooling the body, a therapeutic intervention commonly used by psychiatrists at the time[ 8 - 10 ], in July, Delay et al [ 11 ] published more detailed results of 8 cases treated with RP4560[ 11 ]. They diagnosed six of these patients as suffering from acute mania, one was said to show “excited delirium.” One patient showed “recurrent excitement” and was described as having “trouble thinking” and using “over rationalization.” In today’s classification systems, this patient might be diagnosed with schizophrenia. In this clinical group’s hands, RP4560 was administered without adjuncts, by injection, with oral tablets substituted for injections usually by the 10 th treatment day. The results were remarkable–calm was induced in all patients, with minimum sedation. This created such a sensation in psychiatric circles that, by November 1952, the drug had become available by prescription in France[ 12 ].
The pharmaceutical firm Smith Klein and French bought the American rights to the drug and, in 1954, received Food and Drug Administration approval to market it in the United States under the name, Thorazine. The advertisement in the May 1954 issue of the American Journal of Psychiatry read: “Thorazine is useful in controlling anxiety, tension, agitation, confusion, delirium, or hostility, whether occurring in schizophrenic, manic-depressive, toxic, or functional states.” [ 1 ]. In France and also in Canada[ 13 - 15 ], the drug was called Largactil. Since it was mainly used in hospitalized patients who, for the most part, suffered from psychotic disorders, it swiftly gained a worldwide reputation for being able to reverse the symptoms of psychosis.
The phenothiazine core molecule was malleable and comparably easy to copy so that compounds with very similar efficacy were readily produced. By 1964, a variety of pharmaceutical companies had synthesized and marketed their own phenothiazines: promazine, triflupromazine, methoxypromazine, trifluoperazine, fluphenazine, thioridazine, and prochlorperazine. In 1958, haloperidol, a non-phenothiazine drug [a butyrophenone synthesized on the base of an opioid analgesic, meperidine (Demerol)] was created by pharmaceutical genius, Paul Janssen. This compound proved to be more potent against delusions and hallucinations than the phenothiazines[ 16 ].
Both phenothiazines and butyrophenones were initially called ‘major tranquilizers’ to distinguish them from the ‘minor tranquilizer,’ meprobamate[ 17 ], which was being widely marketed at the time for anxiety.
Searching for the mode of action of major tranquilizers, in 1963, Carlsson and Londqvist[ 18 ] reported that this category of drugs increased the level of metabolites of catecholamines. They suggested ‘‘. . . that chlorpromazine and haloperidol block monoaminergic receptors in brain . . . .” It was not possible at the time to selectively distinguish among alpha-adrenoceptors, beta-adrenoceptors, and dopamine receptors.
There were, nevertheless, several reasons to believe that it was the dopamine pathway that was involved. Firstly, the clinical side effects of chlorpromazine and haloperidol were tremor, rigidity, and akinesia - e.g. Parkinsonian signs and, by then, Parkinson’s disease had been linked to a deficiency of dopamine[ 19 ]. Secondly, it had already been suggested that dopamine-mimetic drugs such as amphetamine acted via dopamine receptors[ 20 ] and that amphetamines could induce schizophrenia-like psychotic symptoms in patients[ 21 , 22 ]. Disulfiram (Antabuse), in clinical use to prevent alcohol addiction, was known to inhibits dopamine beta-hydroxylase, the enzyme that converts dopamine to noradrenaline, and this drug, too, was capable of inducing psychosis[ 23 ].
There were also reports of chlorpromazine accelerating the turnover of dopamine[ 24 ]. Van Rossum[ 25 ] had noticed in 1965 that major tranquilizers (or neuroleptics as they were called by this time), though not, as was first thought, particularly antiadrenergic, were, instead, potent amphetamine antagonists[ 25 ].
The significance of dopamine for the action of antipsychotic drugs, a breakthrough often attributed to Arvid Carlsson (who did not seriously consider dopamine in the context of the action of these drugs until much later) was first formulated by Jacques van Rossum. In 1966, van Rossum[ 26 ] hypothesized that dopamine receptor blockade was a likely explanation for the mechanism of action of this group of drugs. He referred to neuroleptics as the first available dopamine antagonists. In 1967, van Rossum[ 27 ] wrote: “When the hypothesis of dopamine blockade by neuroleptic agents can be further substantiated, it may have far going consequences for the pathophysiology of schizophrenia. Overstimulation of dopamine receptors could then be part of the aetiology. Obviously such an overstimulation might be caused by overproduction of dopamine, production of substances with dopamine actions (methoxy derivatives), abnormal susceptibility of the receptors, etc. ”[ 27 ].
Van Rossum, thus, formulated two dopamine hypotheses (1) The hypothesis that dopamine receptor blockade was responsible for the antipsychotic effects of drugs like chlorpromazine, haloperidol, and similar drugs; and (2) The hypothesis that an excess of dopamine might be part of the etiology of schizophrenia. These two distinct hypotheses are often conflated[ 28 ].
They are conflated because, in the 1970s, it was hoped that the discovery of how neuroleptics work could lead to understanding the nature of schizophrenia itself. Based on the fact that amphetamine releases dopamine and amphetamine-induced psychosis is clinically very similar to an acute episode of schizophrenia[ 29 ], van Rossum[ 27 ] thought that schizophrenia might be due to an overproduction of dopamine[ 27 ].
From today’s standpoint, overactivity of dopamine, while possibly explaining the hallucinations and delusions of schizophrenia, does not shed light on the more fundamental negative and cognitive symptoms of schizophrenia. Over the years, many attempts have been made to elaborate and expand on van Rossum’s dopamine hypothesis of schizophrenia to account for symptoms other than delusions and hallucinations[ 30 , 31 ]. It remains the case, however, that schizophrenia is too multifaceted and heterogeneous a disorder to be fully explained by dopamine overactivity alone. That being said, it is still possible that the secretion and transmission of dopamine serves as a final common pathway to the expression of specific schizophrenia symptoms[ 32 ].
Van Rossum’s first hypothesis-that neuroleptics (today referred to as antipsychotics) exert their effect through dopamine receptors–has enjoyed a longer life than his second. In 2020, Kaar et al [ 33 ], in their review of mechanisms underlying clinical response to antipsychotics, conclude that “all currently licensed antipsychotic drugs show appreciable binding to dopamine D2 receptors at therapeutic doses, and this action is core to their therapeutic action.”
Van Rossum[ 25 - 27 ] had pointed out that overstimulation by dopamine could result from a number of potential causes, from overproduction by the secreting cell to oversensitivity of receptors on the post-synaptic cell. By extension, antipsychotic drugs could theoretically act by blocking dopamine synthesis or secretion or by interfering with its transport across the synapse or by blocking membrane receptors.
In 1971, Zingales[ 34 ] reported that the concentration of haloperidol in the plasma of treated patients was approximately 3 nanograms per millilitre of plasma (3 nmol)[ 34 ]. Because over 90% of haloperidol in plasma is bound to plasma proteins, the actual free concentration that enters the brain would then have to be approximately 1 nmol. This was a problem for the radioactive tagging needed in the search for specific targets of haloperidol action. The classical way to find a drug target was to tag the drug with a radioactive marker. In this case, however, because the drug needed to be diluted down to 1 nmol and still have enough radioactivity left for the experiment to succeed, the radioactive label had to be extra powerful. No such label existed at the time.
In November 1971, Philip Seeman, a Toronto physician/pharmacologist, asked Paul Janssen to persuade the company, I.R.E. Belgique, to prepare radioactive haloperidol at a high specificity of 10.5 Curies per millimole, which the company succeeded in doing in 1974.
True drug receptor targets have to take up the radioactively labelled ligand; a second important criterion in identifying a specific site of action is stereoselectivity–the configuration of the relevant molecule must fit the configuration of the target[ 35 ]. Seeman obtained mirror image antipsychotic molecules (+butaclamol and -butaclamol), the first one active, the second inactive[ 36 , 37 ]. A specific antipsychotic target was confirmed when the site was blocked by +butaclamol to a significantly greater degree than it was by -butaclamol. This more or less settled the identity of the antipsychotic receptor. A further step was to see which of the endogenous neurotransmitters had the most affinity for this location. When tested against noradrenaline, acetylcholine, serotonin, and dopamine, dopamine proved to be the most potent. This meant that the antipsychotic receptor was a dopamine receptor[ 38 ].
Soon after discovering the receptor, Seeman et al [ 39 , 40 ] showed that the published clinical doses of all antipsychotic drugs available at the time, regardless of their molecular structure, directly correlated with their ability to displace radioactive haloperidol[ 39 , 40 ]. This graph has recently been called “the most famous graph in schizophrenia therapeutics.”[ 41 ]. The findings from the Seeman laboratory were soon confirmed by binding studies from other labs[ 42 - 44 ]. A further confirmatory finding was that treatment with antipsychotic drugs increased the density of dopamine receptors in post mortem brain tissue of individuals with schizophrenia[ 45 ].
In vivo molecular imaging studies were not initially available but, when they were, they were eventually able to confirm striatal dopamine D2 receptor blockade at clinically effective doses of all antipsychotic drugs, including first and second-generation agents and dopamine partial agonists[ 46 - 52 ]. The initial molecular imaging studies in patients with treated schizophrenia suggested a therapeutic window (relatively good response without unacceptable extrapyramidal adverse effects) of between 60% and 80% D2 receptor occupancy. The definition of ‘response,’ of course, varies and non-response did not necessarily correlate with low occupancy rates[ 53 ].
Since then, the field of dopamine receptors has considerably expanded[ 54 ]. The receptor labeled by [3H] haloperidol was called D2[ 55 , 56 ], because, by the mid 1980s, five dopamine receptors, all belonging to a G-protein coupled set of receptors, had been isolated. Today, D1 and D5 are known to stimulate the cyclic adenosine monophosphate signaling pathway through G _ s G-proteins, whereas D2R, D3, and D4 inhibit this signal via G _ i/o G-proteins[ 57 ]. Moreover, each of these receptors can exist, as can all G-protein linked receptors, in a state of high or low affinity for their ligand[ 58 , 59 ]. Of the 5 known dopamine receptors, D1, D4, and D5 were cloned in the Seeman laboratory[ 60 - 62 ].
The dopamine D2 receptor was cloned in 1988 in the Civelli lab[ 63 , 64 ]. In 1989, Grandy et al [ 65 ] used in situ hybridization to map the gene to the 11q22–q23 junction.
Because of the excellent correlation between the affinity for striatal D2 receptors and the average clinical dose of antipsychotic drugs given to patients with schizophrenia, there was at first general agreement that all effective antipsychotic drugs must act by not only blocking dopamine D2 receptors in the striatum, but also blocking them in the mesolimbic system, where symptoms of psychosis are thought to originate[ 66 ].
In 1990, the D3 receptor (closely related to D2) was cloned in the laboratory of Jean-Claude Schwartz[ 67 ].
Soon after, the 2 nd generation antipsychotic drugs were brought to market, and they appeared to have much lower affinity for the D2/D3 receptors (they induced far fewer extrapyramidal symptoms) but to be just as potent against psychotic symptoms (delusions and hallucinations) as the older drugs. Clozapine, in particular, the best antipsychotic in that patients resistant to all other drugs often respond when prescribed clozapine, attached to many neurotransmitter receptors besides D2/D3[ 68 ]. Many of the new drugs[ 69 ], including clozapine[ 70 ] had affinity for serotonin 2AR, which was thought explain their much lower relative rate of extrapyramidal effects.
Another explanation was that the antipsychotics drugs that do not elicit extrapyramidal symptoms, such as clozapine and quetiapine, bind to the D2 receptor more loosely than dopamine itself so that endogenous dopamine displaces them very quickly from the target receptor. Drugs that bind most tightly to the D2 receptor (chlorpromazine, trifluoperazine, fluphenazine, haloperidol, risperidone) stay on the receptor for 20-30 min and it is this long continuous occupation that may be responsible for parkinsonism[ 71 , 72 ]. This explanation suggests that, though a certain threshold percentage of D2 receptors still need to be bound in order to obtain an antipsychotic effect, the binding need not be of long duration. ‘Hit and run’ or ‘fast-off’ binding is able to prevent some of the adverse effects while still maintaining efficacy against psychosis.
An unresolved continuing problem with respect to antipsychotic drug action is that at least one third of patients with schizophrenia do not respond to drugs that block D2, whether transiently or for long periods, whether with or without serotonin 2A binding. One possible explanation is that individuals inherit different genetic variants of the D2 receptor[ 73 - 76 ], and that these variants determine response. Since the functional state of the dopamine receptor in the anterior pituitary[ 58 ], and perhaps everywhere in the brain[ 77 ], is its high affinity form, it is perhaps the relative duration of time that these receptors spend in their various affinity states that determines the extent of clinical response. It has been hypothesized that an interaction between D1 and D2 receptors influences the time spent in the high affinity functional state[ 78 ]. Every year, more knowledge accumulates about the signaling complexes of D1 and D2 receptors[ 79 ] and new radioactive ligands are available that bind specifically to high affinity sites[ 80 ].
Although binding to the D2 receptor continues to be considered as the cornerstone of antipsychotic action, the original hypothesis has undergone several refinements, such as the acknowledgement that other dopamine receptors as well as other neurotransmitter receptors play a part[ 81 - 84 ]. There now exist effective antipsychotic drugs that defy the earlier established D2 receptor occupancy threshold, which makes it difficult to attribute antipsychotic effect to any single neurotransmitter receptor[ 85 - 87 ].
Dopamine D2 receptor blockade remains necessary in order to obtain antipsychotic response in most patients. Individuals differ, however, and it remains possible, even probable, that specific subgroups of patients showing psychotic symptoms may respond most robustly to pharmaceutical agents that mainly affect brain chemical transmitters other than dopamine. Pimavanserin, for instance, a serotonin 2A receptor antagonist, has had some success in treating the psychosis associated with Parkinson’s disease, a condition of dopamine deficiency[ 88 ], but the Food and Drug Administration in the United States has recently found it insufficiently effective for the psychosis associated with Alzheimer’s dementia. Differently caused psychoses may respond to differently configured drugs. Looking for the mechanism of action of drugs for psychosis continues, and, as new mechanisms are found, the secrets of the multiple causes of psychotic disorders may be decoded.
ACKNOWLEDGEMENTS
Thank you to Dr. Gary Remington for suggestions and editing.
Conflict-of-interest statement: I am the widow of one of the investigators mentioned in the text.
Manuscript source: Invited manuscript
Peer-review started: February 25, 2021
First decision: April 20, 2021
Article in press: June 22, 2021
Specialty type: Psychiatry
Country/Territory of origin: Canada
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Soriano-Ursúa MA S-Editor: Fan JR L-Editor: A P-Editor: Wang LYT
All Subjects
AP Psychology
Dopamine Hypothesis
The dopamine hypothesis is a theory that suggests an excess of dopamine activity in certain brain areas is associated with the development and symptoms of schizophrenia. It proposes that abnormal levels of dopamine neurotransmitters contribute to the occurrence of this mental disorder.
Related terms
Neurotransmitters : These are chemical messengers in the brain that transmit signals between neurons.
Schizophrenia : A severe mental disorder characterized by hallucinations, delusions, disorganized thinking, and impaired social functioning.
Antipsychotic Medications : Drugs used to treat symptoms of psychosis, including schizophrenia. They work by targeting dopamine receptors and reducing dopamine activity in the brain.
" Dopamine Hypothesis " appears in:
Subjects ( 4 ).
- Abnormal Psychology
- Intro to Psychology
- Introduction to Brain and Behavior
- Neuroscience
Practice Questions ( 3 )
- How does dopamine hypothesis explain the occurrence of schizophrenia?
- What would be a valid critique of solely using the dopamine hypothesis in explaining schizophrenia?
- Which alternative hypothesis could best explain the neurodevelopmental origin of schizophrenia beyond the dopamine hypothesis?
© 2024 Fiveable Inc. All rights reserved.
Ap® and sat® are trademarks registered by the college board, which is not affiliated with, and does not endorse this website..

Dopamine (DA) Hypothesis
The Dopamine (DA) Hypothesis proposes that imbalances in the neurotransmitter dopamine are responsible for the development and symptoms of certain psychiatric conditions, particularly schizophrenia and bipolar disorder.
Neurotransmitter: Dopamine
Dopamine is a chemical messenger (neurotransmitter) in the brain that plays a crucial role in various physiological and psychological functions. It is involved in regulating movement, motivation, cognition, reward, pleasure, and emotional responses.
Overview of the Hypothesis
The Dopamine Hypothesis suggests that abnormalities in the functioning of dopamine systems within the brain contribute to the development and manifestation of psychiatric disorders. It proposes that an excess or dysregulation of dopamine transmission can result in the characteristic symptoms observed in certain conditions.
Schizophrenia
In the context of schizophrenia, the DA Hypothesis suggests that an increase in dopamine activity in specific brain regions, such as the mesolimbic pathway, contributes to the positive symptoms of the disorder, including hallucinations and delusions. Medications that block dopamine receptors, known as antipsychotics, are commonly used in the treatment of schizophrenia.
Bipolar Disorder
Regarding bipolar disorder, the DA Hypothesis proposes that there is an imbalance in dopamine levels between manic and depressive episodes. During manic episodes, there is a surge in dopamine activity, leading to heightened energy, euphoria, and impulsivity. In contrast, reduced dopamine levels during depressive episodes may contribute to the lack of motivation and pleasure commonly experienced by individuals with bipolar disorder.
Limitations and ongoing research
The DA Hypothesis has provided valuable insights into the understanding and treatment of schizophrenia and bipolar disorder. However, it is important to note that the hypothesis does not fully explain the complexity of these disorders, as multiple neurotransmitters and brain systems are involved. Ongoing research aims to refine the Dopamine Hypothesis and explore other contributing factors, such as glutamate and serotonin, to gain a more comprehensive understanding of these conditions.

DOPAMINE HYPOTHESIS
The Dopamine Hypothesis has been a prominent area of study in the field of neuroscience for several decades. It is the idea that the neurotransmitter dopamine plays a central role in the pathology of schizophrenia. This hypothesis was first proposed by Carlsson and Lindqvist in 1963, and since then it has been the subject of much research and debate.
A key component of the dopamine hypothesis is that dopamine is involved in the development of psychotic symptoms, such as hallucinations and delusions. It is thought that an imbalance in the dopamine system, either too much or too little dopamine in certain areas of the brain, can lead to the symptoms of schizophrenia. This is because dopamine plays an important role in regulating certain cognitive processes, such as memory, learning, and attention.
Several lines of evidence support the dopamine hypothesis. Neuroimaging studies have shown differences in dopamine levels in the brains of people with schizophrenia, compared to those without the disorder. Pharmacological studies have also shown that antipsychotic medications, which work by blocking the effects of dopamine, can reduce psychotic symptoms. Additionally, genetic studies have identified several genes that are associated with an increased risk of schizophrenia, and many of these genes are involved in the dopamine system.
Despite the evidence for the dopamine hypothesis, it is still an area of active research and debate. Many studies have suggested that other neurotransmitters, such as glutamate, may also be involved in the development of schizophrenia. Additionally, it is still unclear exactly how dopamine imbalances lead to the symptoms of schizophrenia, and how these imbalances can be treated.
In conclusion, the dopamine hypothesis is a widely accepted theory that is supported by a large body of evidence. However, further research is needed to fully understand the role of dopamine in schizophrenia and to develop effective treatments for this disorder.
Carlsson, A., & Lindqvist, M. (1963). Effect of chlorpromazine or haloperidol on the formation of 3-methoxytyramine and normetanephrine in mouse brain. Acta Pharmacologica et Toxicologica, 20(2), 140–144.
Howes, O., & Kapur, S. (2009). The dopamine hypothesis of schizophrenia: Version III—the final common pathway. Schizophrenia Bulletin, 35(3), 549–562.
Lam, D. H., & Weickert, C. S. (2008). The dopamine hypothesis of schizophrenia: Making sense of the data. Schizophrenia Research, 102(1–3), 1–11.
Yolken, R. H., & Fatemi, S. H. (2012). Neurodevelopment in schizophrenia: From genes to environment. Neuroscience & Biobehavioral Reviews, 36(1), 131–145.
Related terms
Depo-provera, dereflection, descending reticular system, design matrix, desynchronization.
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Sweepstakes
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
The Relationship Between Schizophrenia and Dopamine
Alla Bielikova / Getty Images
- Dopamine and Schizophrenia Symptoms
- Implications for Treatment
What Does This Mean for Patients?
- Causes of Schizophrenia
- High vs. Low Dopamine
- Implications
Serotonin and Schizophrenia
Experts do not fully understand what causes schizophrenia, but evidence suggests that dopamine abnormalities may play a role. High and low levels of dopamine in certain regions of the brain can also affect different symptoms of schizophrenia.
Schizophrenia is a debilitating mental disorder with a multitude of symptoms. These can range from disorganized speech and behavior to delusions and hallucinations. Some cases are far more disabling than others, but in most cases, people with this disorder require lifelong treatment and care.
Current research suggests that schizophrenia is a neurodevelopmental disorder with an important dopamine component. Four decades of research have focused on the role of dopamine in schizophrenia, and it seems clear that excesses or deficiencies in dopamine can lead to schizophrenic symptoms.
At a Glance
While other factors also play a role in the development of schizophrenia, dopamine imbalances have been identified as a key factor affecting symptoms. Too much dopamine in key areas of the brain results in delusions and hallucinations (positive symptoms) or cognitive deficits and reduced social/emotional activity (negative symptoms). Understanding the factors that contribute to dopamine symptoms can help doctors treat the condition more effectively.
What Is the Dopamine Hypothesis of Schizophrenia?
The dopamine hypothesis of schizophrenia was one of the first neurobiological theories for this disease.
Dopamine Hypothesis
This theory suggests that an imbalance of dopamine is responsible for schizophrenic symptoms. In other words, dopamine plays a role in controlling our sense of reality, and too much or too little can cause delusions and hallucinations.
The evidence for this theory comes from many sources, including post-mortem studies that have imbalances of dopamine as well as its metabolites in schizophrenic patients. In addition, drugs that block the receptors for dopamine can help control schizophrenic symptoms.
How Does Dopamine Cause Schizophrenic Symptoms?
There are two types of schizophrenia symptoms that an excess of dopamine may cause: positive and negative . Positive symptoms include delusions and hallucinations. Negative symptoms include a decrease in social activity, emotional range, and cognitive function.
Positive Symptoms
Positive symptoms are those that appear to come from outside the person. These can include delusions, hallucinations, or thought disorders.
Dopamine contributes to the development of positive symptoms through its effects on subtype-3A dopamine receptors (D3) of cortical neurons. The subtype-3A receptor is found in the prefrontal cortex, which controls planning, thinking, and other cortical areas.
When these receptors are activated by dopamine, they overstimulate neurons. This can lead to all three types of positive symptoms. Evidence for this idea comes from studies that show that patients with schizophrenia have significantly lower levels of the D3 receptor than healthy people.
Negative Symptoms
While positive symptoms appear to come from outside, negative symptoms appear to be internal. These include decreased social activity and emotional range, as well as cognitive deficits like poor problem-solving or memory deficit.
The mechanisms contributing to negative symptoms are linked to dopamine levels in the limbic system . Dopamine excess leads to an increase in the activity of dopamine receptors, creating overstimulation similar to that seen in positive symptoms.
Some researchers suggest that this overactivity decreases neuronal inhibition , leading to decreased social behavior and cognitive deficits.
Treatment Implications of the Dopamine Hypothesis
The dopamine hypothesis has important treatment implications. The vast majority of current antipsychotic medications target dopamine, and this makes sense, given that these drugs were discovered through serendipitous observations of their effect on schizophrenia.
The most important dopamine-affecting medications are the typical antipsychotics, which increase post-synaptic receptor stimulation by blocking dopamine receptors.
Unfortunately, these medications produce a number of debilitating side effects, most notably extrapyramidal symptoms (EPS) like tardive dyskinesia . Newer second-generation antipsychotics have fewer side effects, but none are perfect.
Treatment with dopamine agonists is a third possibility suggested by the dopamine hypothesis. Dopamine agonists stimulate post-synaptic dopamine receptors directly, and as such, they can be used to treat schizophrenia without producing EPS.
Being diagnosed with schizophrenia can be extremely hard on patients and their families. It's important that doctors and researchers continually investigate new treatments that could improve the lives of people living with this disorder.
However, it's also important to remember that schizophrenia is a complex disorder, and there are many ways the disease can manifest. Dopamine hyperactivity may not be the primary cause of schizophrenia in all patients. Furthermore, even if dopamine hyperactivity is the primary cause it still doesn't explain why some patients respond more strongly than others to the same treatment.
The best way for patients and their loved ones to navigate these issues is by staying informed and asking questions about any new or experimental treatments. They should also work with doctors to develop a personalized treatment plan that's appropriate for their own needs.
Does Too Much Dopamine Cause Schizophrenia?
Increased activity of the mesolimbic pathway is related to positive symptoms of schizophrenia (delusions, hallucinations, etc.). This means that increasing the activity of dopamine receptors in this brain system could theoretically reduce delusions and hallucinations.
A closely related idea is that by blocking post-synaptic dopamine receptors, scientists can reduce the psychotic symptoms of schizophrenia.
As mentioned previously, this is what most modern medications do: they block post-synaptic dopamine receptors in order to reduce psychotic symptoms. Unfortunately, when scientists block all available dopamine receptors they also produce a number of debilitating side effects such as extrapyramidal symptoms (EPS) and tardive dyskinesia.
Is Dopamine High or Low in Schizophrenia?
The most common theory about the cause of schizophrenia is that there are too many dopamine receptors in certain parts of the brain, specifically the mesolimbic pathway. This causes an increase in mesolimbic activity which results in delusions, hallucinations, and other psychotic symptoms.
Other research suggests that schizophrenia might be caused by a lack of dopamine activity in other parts of the brain. For example, scientists have discovered that the hippocampus is overactive in schizophrenia.
Schizophrenia might also be characterized by low dopamine in the prefrontal cortex, but again the evidence is inconclusive. Some studies have found that schizophrenics have elevated levels of dopamine in this region, while others suggest that there are too few dopamine receptors.
Implications of the Dopamine Hypothesis
It's important to note that schizophrenia is a complex disorder. Even if dopamine hyperactivity is the primary cause, certain types of schizophrenia might be characterized by increased activity in certain brain areas while others are characterized by reduced activity in certain brain areas.
Furthermore, it's also possible that different patients will respond to treatment differently based on how their disease manifests.
It's important for healthcare providers and researchers to continue investigating how schizophrenia works in the brain. This will help them develop better treatments for this complex disorder.
Research also implicates serotonin as a regulator of dopamine release. Antipsychotic medications, including olanzapine and clozapine , reduce serotonin activity and increase dopamine activity.
For example, olanzapine-induced reductions in serotonin metabolism were associated with significant improvements in negative and positive symptoms, but not cognitive deficits.
Schizophrenia is a severe mental disorder that can be treated. If you or someone you know was recently diagnosed with schizophrenia, you might be wondering what the future holds. Healthcare professionals can help you manage your symptoms and chart a course for the best possible outcome.
Sometimes, there may be periods of remission that allow you to live a productive life even when coping with schizophrenia. As new treatments are continually being developed, we can look forward to better options for people who experience this disorder in the future.
Murray RM, Lappin J, Di Forti M. Schizophrenia: from developmental deviance to dopamine dysregulation . Eur Neuropsychopharmacol . 2008;18 Suppl 3:S129-S134. doi:10.1016/j.euroneuro.2008.04.002
Brisch R, Saniotis A, Wolf R, et al. The role of dopamine in schizophrenia from a neurobiological and evolutionary perspective: old fashioned, but still in vogue [published correction appears in Front Psychiatry. 2014;5:110. Braun, Anna Katharina [corrected to Braun, Katharina]; Kumaritlake, Jaliya [corrected to Kumaratilake, Jaliya]]. Front Psychiatry . 2014;5:47. Published 2014 May 19. doi:10.3389/fpsyt.2014.00047
Purves-Tyson TD, Owens SJ, Rothmond DA, et al. Putative presynaptic dopamine dysregulation in schizophrenia is supported by molecular evidence from post-mortem human midbrain . Transl Psychiatry . 2017;7(1):e1003. Published 2017 Jan 17. doi:10.1038/tp.2016.257
Ceraso A, Lin JJ, Schneider-Thoma J, et al. Maintenance treatment with antipsychotic drugs for schizophrenia . Cochrane Database Syst Rev . 2020;8:CD008016. doi:10.1002/14651858.CD008016.pub3
Guma E, Rocchetti J, Devenyi GA, et al. Role of D3 dopamine receptors in modulating neuroanatomical changes in response to antipsychotic administration . Sci Rep . 2019;9(1):7850. doi:10.1038/s41598-019-43955-4
Maia TV, Frank MJ. An Integrative Perspective on the Role of Dopamine in Schizophrenia . Biol Psychiatry . 2017;81(1):52-66. doi:10.1016/j.biopsych.2016.05.021
Weiner I. The "two-headed" latent inhibition model of schizophrenia: modeling positive and negative symptoms and their treatment . Psychopharmacology (Berl) . 2003;169(3-4):257-297. doi:10.1007/s00213-002-1313-x
Stępnicki P, Kondej M, Kaczor AA. Current concepts and treatments of schizophrenia . Molecules . 2018;23(8):2087. doi:10.3390/molecules23082087
Preda A, Shapiro BB. A safety evaluation of aripiprazole in the treatment of schizophrenia . Expert Opin Drug Saf . 2020;19(12):1529-1538. doi:10.1080/14740338.2020.1832990
Gomes FV, Zhu X, Grace AA. Stress during critical periods of development and risk for schizophrenia . Schizophr Res . 2019;213:107-113. doi:10.1016/j.schres.2019.01.030
McCutcheon RA, Krystal JH, Howes OD. Dopamine and glutamate in schizophrenia: biology, symptoms and treatment . World Psychiatry . 2020;19(1):15-33. doi:10.1002/wps.20693
Correll CU. Current Treatment Options and Emerging Agents for Schizophrenia . J Clin Psychiatry . 2020;81(3):MS19053BR3C. Published 2020 Apr 14. doi:10.4088/JCP.MS19053BR3C
Bever KA, Perry PJ. Olanzapine: a serotonin-dopamine-receptor antagonist for antipsychotic therapy . Am J Health Syst Pharm . 1998;55(10):1003-1016. doi:10.1093/ajhp/55.10.1003
By Arlin Cuncic, MA Arlin Cuncic, MA, is the author of The Anxiety Workbook and founder of the website About Social Anxiety. She has a Master's degree in clinical psychology.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Perspective
- Published: 25 July 2024
Explaining dopamine through prediction errors and beyond
- Samuel J. Gershman ORCID: orcid.org/0000-0002-6546-3298 1 , 2 ,
- John A. Assad 3 ,
- Sandeep Robert Datta ORCID: orcid.org/0000-0002-8068-3862 3 ,
- Scott W. Linderman ORCID: orcid.org/0000-0002-3878-9073 4 ,
- Bernardo L. Sabatini ORCID: orcid.org/0000-0003-0095-9177 2 , 3 , 5 ,
- Naoshige Uchida ORCID: orcid.org/0000-0002-5755-9409 6 &
- Linda Wilbrecht ORCID: orcid.org/0000-0003-3492-8141 7
Nature Neuroscience ( 2024 ) Cite this article
4145 Accesses
44 Altmetric
Metrics details
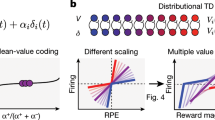
- Neuroscience
The most influential account of phasic dopamine holds that it reports reward prediction errors (RPEs). The RPE-based interpretation of dopamine signaling is, in its original form, probably too simple and fails to explain all the properties of phasic dopamine observed in behaving animals. This Perspective helps to resolve some of the conflicting interpretations of dopamine that currently exist in the literature. We focus on the following three empirical challenges to the RPE theory of dopamine: why does dopamine (1) ramp up as animals approach rewards, (2) respond to sensory and motor features and (3) influence action selection? We argue that the prediction error concept, once it has been suitably modified and generalized based on an analysis of each computational problem, answers each challenge. Nonetheless, there are a number of additional empirical findings that appear to demand fundamentally different theoretical explanations beyond encoding RPE. Therefore, looking forward, we discuss the prospects for a unifying theory that respects the diversity of dopamine signaling and function as well as the complex circuitry that both underlies and responds to dopaminergic transmission.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others

Dopamine-independent effect of rewards on choices through hidden-state inference
A distributional code for value in dopamine-based reinforcement learning

A feature-specific prediction error model explains dopaminergic heterogeneity
Schultz, W., Dayan, P. & Montague, P. R. A neural substrate of prediction and reward. Science 275 , 1593–1599 (1997).
Article CAS PubMed Google Scholar
Montague, P. R., Dayan, P. & Sejnowski, T. J. A framework for mesencephalic dopamine systems based on predictive Hebbian learning. J. Neurosci. 16 , 1936–1947 (1996).
Article CAS PubMed PubMed Central Google Scholar
Bayer, H. M. & Glimcher, P. W. Midbrain dopamine neurons encode a quantitative reward prediction error signal. Neuron 47 , 129–141 (2005).
Eshel, N. et al. Arithmetic and local circuitry underlying dopamine prediction errors. Nature 525 , 243–246 (2015).
Eshel, N., Tian, J., Bukwich, M. & Uchida, N. Dopamine neurons share common response function for reward prediction error. Nat. Neurosci. 19 , 479–486 (2016).
Steinberg, E. E. et al. A causal link between prediction errors, dopamine neurons and learning. Nat. Neurosci. 16 , 966–973 (2013).
Chang, C. Y. et al. Brief optogenetic inhibition of dopamine neurons mimics endogenous negative reward prediction errors. Nat. Neurosci. 19 , 111–116 (2016).
Reynolds, J. N. J. & Wickens, J. R. Dopamine-dependent plasticity of corticostriatal synapses. Neural Netw. 15 , 507–521 (2002).
Article PubMed Google Scholar
Morita, K., Morishima, M., Sakai, K. & Kawaguchi, Y. Reinforcement learning: computing the temporal difference of values via distinct corticostriatal pathways: (Trends in Neurosciences 35, 457–467; 2012). Trends Neurosci. 40 , 453 (2017).
Watabe-Uchida, M., Eshel, N. & Uchida, N. Neural circuitry of reward prediction error. Annu. Rev. Neurosci. 40 , 373–394 (2017).
Starkweather, C. K. & Uchida, N. Dopamine signals as temporal difference errors: recent advances. Curr. Opin. Neurobiol. 67 , 95–105 (2021).
Howe, M. W., Tierney, P. L., Sandberg, S. G., Phillips, P. E. M. & Graybiel, A. M. Prolonged dopamine signalling in striatum signals proximity and value of distant rewards. Nature 500 , 575–579 (2013).
Niv, Y. Neuroscience: dopamine ramps up. Nature 500 , 533–535 (2013).
Berke, J. D. What does dopamine mean? Nat. Neurosci. 21 , 787–793 (2018).
Hamid, A. A. et al. Mesolimbic dopamine signals the value of work. Nat. Neurosci. 19 , 117–126 (2016).
Mohebi, A. et al. Publisher correction: dissociable dopamine dynamics for learning and motivation. Nature 571 , E3 (2019).
Krausz, T. A., Comrie, A. E., Frank, L. M., Daw, N. D. & Berke, J. D. Dual credit assignment processes underlie dopamine signals in a complex spatial environment. Neuron 111 , 3465–3478 (2023).
Hamilos, A. E. et al. Slowly evolving dopaminergic activity modulates the moment-to-moment probability of reward-related self-timed movements. eLife 10 , e62583 (2021).
Collins, A. L. et al. Dynamic mesolimbic dopamine signaling during action sequence learning and expectation violation. Sci. Rep. 6 , 20231 (2016).
Gershman, S. J. Dopamine ramps are a consequence of reward prediction errors. Neural Comput. 26 , 467–471 (2014).
Kim, H. R. et al. A unified framework for dopamine signals across timescales. Cell 183 , 1600–1616 (2020).
Mikhael, J. G., Kim, H. R., Uchida, N. & Gershman, S. J. The role of state uncertainty in the dynamics of dopamine. Curr. Biol. 32 , 1077–1087 (2022).
Kato, A. & Morita, K. Forgetting in reinforcement learning links sustained dopamine signals to motivation. PLoS Comput. Biol. 12 , e1005145 (2016).
Article PubMed PubMed Central Google Scholar
Beron, C. C., Neufeld, S. Q., Linderman, S. W. & Sabatini, B. L. Mice exhibit stochastic and efficient action switching during probabilistic decision making. Proc. Natl Acad. Sci. USA 119 , e2113961119 (2022).
Niv, Y. et al. Reinforcement learning in multidimensional environments relies on attention mechanisms. J. Neurosci. 35 , 8145–8157 (2015).
Ito, M. & Doya, K. Validation of decision-making models and analysis of decision variables in the rat basal ganglia. J. Neurosci. 29 , 9861–9874 (2009).
Lloyd, K. & Dayan, P. Tamping ramping: algorithmic, implementational, and computational explanations of phasic dopamine signals in the accumbens. PLoS Comput. Biol. 11 , e1004622 (2015).
Hamid, A. A., Frank, M. J. & Moore, C. I. Wave-like dopamine dynamics as a mechanism for spatiotemporal credit assignment. Cell 184 , 2733–2749 (2021).
Guru, A., Seo, C., Kullakanda, D. S., Schaffer, J. A. & Warden, M. R. Ramping activity in midbrain dopamine neurons signifies the use of a cognitive map. Preprint at bioRxiv https://doi.org/10.1101/2020.05.21.108886 (2020).
Amo, R. et al. A gradual temporal shift of dopamine responses mirrors the progression of temporal difference error in machine learning. Nat. Neurosci. 25 , 1082–1092 (2022).
Ljungberg, T., Apicella, P. & Schultz, W. Responses of monkey dopamine neurons during learning of behavioral reactions. J. Neurophysiol. 67 , 145–163 (1992).
Horvitz, J. C. Mesolimbocortical and nigrostriatal dopamine responses to salient non-reward events. Neuroscience 96 , 651–656 (2000).
Steinfels, G. F., Heym, J., Strecker, R. E. & Jacobs, B. L. Behavioral correlates of dopaminergic unit activity in freely moving cats. Brain Res. 258 , 217–228 (1983).
Gonzalez, L. S. et al. Ventral striatum dopamine release encodes unique properties of visual stimuli in mice. eLife 12 , e85064 (2023).
Kakade, S. & Dayan, P. Dopamine: generalization and bonuses. Neural Netw. 15 , 549–559 (2002).
Menegas, W., Babayan, B. M., Uchida, N. & Watabe-Uchida, M. Opposite initialization to novel cues in dopamine signaling in ventral and posterior striatum in mice. eLife 6 , e21886 (2017).
Akiti, K. et al. Striatal dopamine explains novelty-induced behavioral dynamics and individual variability in threat prediction. Neuron 110 , 3789–3804 (2022).
Morrens, J., Aydin, Ç., Janse van Rensburg, A., Esquivelzeta Rabell, J. & Haesler, S. Cue-evoked dopamine promotes conditioned responding during learning. Neuron 106 , 142–153 (2020).
Gershman, S. J. & Niv, Y. Novelty and inductive generalization in human reinforcement learning. Top. Cogn. Sci. 7 , 391–415 (2015).
Kobayashi, S. & Schultz, W. Reward contexts extend dopamine signals to unrewarded stimuli. Curr. Biol. 24 , 56–62 (2014).
Bromberg-Martin, E. S. & Hikosaka, O. Midbrain dopamine neurons signal preference for advance information about upcoming rewards. Neuron 63 , 119–126 (2009).
Iigaya, K., Story, G. W., Kurth-Nelson, Z., Dolan, R. J. & Dayan, P. The modulation of savouring by prediction error and its effects on choice. eLife 5 , e13747 (2016).
Ogasawara, T. et al. A primate temporal cortex-zona incerta pathway for novelty seeking. Nat. Neurosci. 25 , 50–60 (2022).
Sharpe, M. J. et al. Dopamine transients are sufficient and necessary for acquisition of model-based associations. Nat. Neurosci. 20 , 735–742 (2017).
Chang, C. Y., Gardner, M., Di Tillio, M. G. & Schoenbaum, G. Optogenetic blockade of dopamine transients prevents learning induced by changes in reward features. Curr. Biol. 27 , 3480–3486 (2017).
Takahashi, Y. K. et al. Dopamine neurons respond to errors in the prediction of sensory features of expected rewards. Neuron 95 , 1395–1405 (2017).
Langdon, A. J., Sharpe, M. J., Schoenbaum, G. & Niv, Y. Model-based predictions for dopamine. Curr. Opin. Neurobiol. 49 , 1–7 (2018).
Gardner, M. P. H., Schoenbaum, G. & Gershman, S. J. Rethinking dopamine as generalized prediction error. Proc. Biol. Sci. 285 , 20181645 (2018).
PubMed PubMed Central Google Scholar
Dayan, P. Improving generalization for temporal difference learning: the successor representation. Neural Comput. 5 , 613–624 (1993).
Article Google Scholar
Gershman, S. J. The successor representation: its computational logic and neural substrates. J. Neurosci. 38 , 7193–7200 (2018).
Stachenfeld, K. L., Botvinick, M. M. & Gershman, S. J. The hippocampus as a predictive map. Nat. Neurosci. 20 , 1643–1653 (2017).
Engelhard, B. et al. Specialized coding of sensory, motor and cognitive variables in VTA dopamine neurons. Nature 570 , 509–513 (2019).
Solié, C., Girard, B., Righetti, B., Tapparel, M. & Bellone, C. VTA dopamine neuron activity encodes social interaction and promotes reinforcement learning through social prediction error. Nat. Neurosci. 25 , 86–97 (2022).
Matsumoto, M. & Hikosaka, O. Two types of dopamine neuron distinctly convey positive and negative motivational signals. Nature 459 , 837–841 (2009).
Cai, L. X. Distinct signals in medial and lateral VTA dopamine neurons modulate fear extinction at different times. eLife 9 , e54936 (2020).
Parker, N. F. et al. Reward and choice encoding in terminals of midbrain dopamine neurons depends on striatal target. Nat. Neurosci. 19 , 845–854 (2016).
Menegas, W. et al. Dopamine neurons projecting to the posterior striatum form an anatomically distinct subclass. eLife 4 , e10032 (2015).
Menegas, W., Akiti, K., Amo, R., Uchida, N. & Watabe-Uchida, M. Dopamine neurons projecting to the posterior striatum reinforce avoidance of threatening stimuli. Nat. Neurosci. 21 , 1421–1430 (2018).
Tsutsui-Kimura, I. et al. Distinct temporal difference error signals in dopamine axons in three regions of the striatum in a decision-making task. eLife 9 , e62390 (2020).
De Jong, J. W. et al. A neural circuit mechanism for encoding aversive stimuli in the mesolimbic dopamine system. Neuron 101 , 133–151 (2019).
Lammel, S., Ion, D. I., Roeper, J. & Malenka, R. C. Projection-specific modulation of dopamine neuron synapses by aversive and rewarding stimuli. Neuron 70 , 855–862 (2011).
Stalnaker, T. A. et al. Dopamine neuron ensembles signal the content of sensory prediction errors. eLife 8 , e49315 (2019).
Lee, R. S., Engelhard, B., Witten, I. B. & Daw, N. D. A vector reward prediction error model explains dopaminergic heterogeneity. Preprint at bioRxiv https://doi.org/10.1101/2022.02.28.482379 (2022).
Da Silva, J. A., Tecuapetla, F., Paixão, V. & Costa, R. M. Dopamine neuron activity before action initiation gates and invigorates future movements. Nature 554 , 244–248 (2018).
Coddington, L. T. & Dudman, J. T. The timing of action determines reward prediction signals in identified midbrain dopamine neurons. Nat. Neurosci. 21 , 1563–1573 (2018).
Howe, M. W. & Dombeck, D. A. Rapid signalling in distinct dopaminergic axons during locomotion and reward. Nature 535 , 505–510 (2016).
Lee, R. S., Mattar, M. G., Parker, N. F., Witten, I. B. & Daw, N. D. Reward prediction error does not explain movement selectivity in DMS-projecting dopamine neurons. eLife 8 , e42992 (2019).
Markowitz, J. E. et al. Spontaneous behaviour is structured by reinforcement without explicit reward. Nature 614 , 108–117 (2023).
Exley, R. & Cragg, S. J. Presynaptic nicotinic receptors: a dynamic and diverse cholinergic filter of striatal dopamine neurotransmission. Br. J. Pharmacol. 153 , S283–S297 (2008).
Bamford, N. S., Wightman, R. M. & Sulzer, D. Dopamine’s effects on corticostriatal synapses during reward-based behaviors. Neuron 97 , 494–510 (2018).
Lindsey, J. & Litwin-Kumar, A. Action-modulated midbrain dopamine activity arises from distributed control policies. Adv. Neural Inform. Process. Syst. 35 , 5535–5548 (2022).
Google Scholar
Greenstreet, F. et al. Action prediction error: a value-free dopaminergic teaching signal that drives stable learning. Preprint at bioRxiv https://doi.org/10.1101/2022.09.12.507572 (2022).
Howard, C. D., Li, H., Geddes, C. E. & Jin, X. Dynamic nigrostriatal dopamine biases action selection. Neuron 93 , 1436–1450 (2017).
Fry, B. R., Pence, N. T., McLocklin, A. & Johnson, A. W. Disruptions in effort-based decision-making following acute optogenetic stimulation of ventral tegmental area dopamine cells. Learning Memory 28 , 104–108 (2021).
Bova, A. et al. Precisely timed dopamine signals establish distinct kinematic representations of skilled movements. eLife 9 , e61591 (2020).
Lee, K. et al. Temporally restricted dopaminergic control of reward-conditioned movements. Nat. Neurosci. 23 , 209–216 (2020).
Eshel, N. et al. Striatal dopamine integrates cost, benefit, and motivation. Neuron 112 , 500–514 (2024).
Möller, M. & Bogacz, R. Learning the payoffs and costs of actions. PLoS Comput. Biol. 15 , e1006285 (2019).
Van Swieten, M. M. H. & Bogacz, R. Modeling the effects of motivation on choice and learning in the basal ganglia. PLoS Comput. Biol. 16 , e1007465 (2020).
Wan, Y., Naik, A. & Sutton, R. S. Learning and planning in average-reward Markov decision processes. In International Conference on Machine Learning , 10653–10662 (PMLR, 2021).
Daw, N. D. & Touretzky, D. S. Long-term reward prediction in TD models of the dopamine system. Neural Comput. 14 , 2567–2583 (2002).
Aberman, J. E. & Salamone, J. D. Nucleus accumbens dopamine depletions make rats more sensitive to high ratio requirements but do not impair primary food reinforcement. Neuroscience 92 , 545–552 (1999).
Niv, Y., Daw, N. D., Joel, D. & Dayan, P. Tonic dopamine: opportunity costs and the control of response vigor. Psychopharmacology 191 , 507–520 (2007).
Berridge, K. C. & Robinson, T. E. What is the role of dopamine in reward: hedonic impact, reward learning, or incentive salience? Brain Res. Brain Res. Rev. 28 , 309–369 (1998).
Sippy, T. & Tritsch, N. X. Unraveling the dynamics of dopamine release and its actions on target cells. Trends Neurosci. 46 , 228–239 (2023).
Collins, A. G. E. & Frank, M. J. Opponent actor learning (OpAL): modeling interactive effects of striatal dopamine on reinforcement learning and choice incentive. Psychol. Rev. 121 , 337–366 (2014).
McClure, S. M., Daw, N. D. & Montague, P. R. A computational substrate for incentive salience. Trends Neurosci. 26 , 423–428 (2003).
Jaskir, A. & Frank, M. J. On the normative advantages of dopamine and striatal opponency for learning and choice. eLife 12 , e85107 (2023).
Bogacz, R. Dopamine role in learning and action inference. eLife 9 , e53262 (2020).
Kutlu, M. G. & Schmajuk, N. A. Solving Pavlov’s puzzle: attentional, associative, and flexible configural mechanisms in classical conditioning. Learn. Behav. 40 , 269–291 (2012).
Kutlu, M. G. et al. Dopamine release in the nucleus accumbens core signals perceived saliency. Curr. Biol. 31 , 4748–4761 (2021).
Kutlu, M. G. et al. Dopamine signaling in the nucleus accumbens core mediates latent inhibition. Nat. Neurosci. 25 , 1071–1081 (2022).
Gershman, S. J. Dopamine, inference, and uncertainty. Neural Comput. 29 , 3311–3326 (2017).
Möller, M., Manohar, S. & Bogacz, R. Uncertainty-guided learning with scaled prediction errors in the basal ganglia. PLoS Comput. Biol. 18 , e1009816 (2022).
Jeong, H. et al. Mesolimbic dopamine release conveys causal associations. Science 378 , eabq6740 (2022).
Qian, L. et al. The role of prospective contingency in the control of behavior and dopamine signals during associative learning. Preprint at bioRxiv https://doi.org/10.1101/2024.02.05.578961 (2024).
Coddington, L. T., Lindo, S. E. & Dudman, J. T. Mesolimbic dopamine adapts the rate of learning from action. Nature 614 , 294–302 (2023).
Lee, S. J. et al. Cell-type-specific asynchronous modulation of PKA by dopamine in learning. Nature 590 , 451–456 (2021).
Lee, S. J., Chen, Y., Lodder, B. & Sabatini, B. L. Monitoring behaviorally induced biochemical changes using fluorescence lifetime photometry. Front. Neurosci. 13 , 766 (2019).
Wiltschko, A. B. et al. Mapping sub-second structure in mouse behavior. Neuron 88 , 1121–1135 (2015).
Hamid, A. A. Dopaminergic specializations for flexible behavioral control: linking levels of analysis and functional architectures. Curr. Opin. Behav. Sci. 41 , 175–184 (2021).
Hughes, R. N. et al. Ventral tegmental dopamine neurons control the impulse vector during motivated behavior. Curr. Biol. 30 , 2681–2694 (2020).
De Jong, J. W., Liang, Y., Verharen, J. P. H., Fraser, K. M. & Lammel, S. State and rate-of-change encoding in parallel mesoaccumbal dopamine pathways. Nat. Neurosci. 27 , 309–318 (2024).
Gerfen, C. R. & Surmeier, D. J. Modulation of striatal projection systems by dopamine. Annu. Rev. Neurosci. 34 , 441–466 (2011).
Durstewitz, D. & Seamans, J. K. The dual-state theory of prefrontal cortex dopamine function with relevance to catechol-o-methyltransferase genotypes and schizophrenia. Biol. Psychiatry 64 , 739–749 (2008).
Mahadevia, D. et al. Dopamine promotes aggression in mice via ventral tegmental area to lateral septum projections. Nat. Commun. 12 , 6796 (2021).
Dabney, W. et al. A distributional code for value in dopamine-based reinforcement learning. Nature 577 , 671–675 (2020).
Lowet, A. S. et al. An opponent striatal circuit for distributional reinforcement learning. Preprint at bioRxiv https://doi.org/10.1101/2024.01.02.573966 (2024).
Grace, A. A. Phasic versus tonic dopamine release and the modulation of dopamine system responsivity: a hypothesis for the etiology of schizophrenia. Neuroscience 41 , 1–24 (1991).
Kilpatrick, M. R., Rooney, M. B., Michael, D. J. & Wightman, R. M. Extracellular dopamine dynamics in rat caudate-putamen during experimenter-delivered and intracranial self-stimulation. Neuroscience 96 , 697–706 (2000).
Download references
Acknowledgements
We are grateful to the many students and postdocs who have worked on aspects of this research with us. The ideas presented here also benefited from conversations with N. Daw. This work was supported by the National Institutes of Health (U19-NS-113201-01) and the Air Force Office of Scientific Research (FA9550-20-1-0413).
Author information
Authors and affiliations.
Department of Psychology and Center for Brain Science, Harvard University, Cambridge, MA, USA
Samuel J. Gershman
Kempner Institute for the Study of Natural and Artificial Intelligence, Harvard University, Cambridge, MA, USA
Samuel J. Gershman & Bernardo L. Sabatini
Department of Neurobiology, Harvard Medical School, Boston, MA, USA
John A. Assad, Sandeep Robert Datta & Bernardo L. Sabatini
Department of Statistics and Wu Tsai Neurosciences Institute, Stanford University, Stanford, CA, USA
Scott W. Linderman
Howard Hughes Medical Institute, Chevy Chase, MD, USA
Bernardo L. Sabatini
Department of Molecular and Cellular Biology, Harvard University, Cambridge, MA, USA
Naoshige Uchida
Department of Psychology and Helen Wills Neuroscience Institute, University of California, Berkeley, CA, USA
Linda Wilbrecht
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Samuel J. Gershman .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Nature Neuroscience thanks Arif Hamid and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Gershman, S.J., Assad, J.A., Datta, S.R. et al. Explaining dopamine through prediction errors and beyond. Nat Neurosci (2024). https://doi.org/10.1038/s41593-024-01705-4
Download citation
Received : 24 April 2023
Accepted : 13 June 2024
Published : 25 July 2024
DOI : https://doi.org/10.1038/s41593-024-01705-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Architecture and Design
- Asian and Pacific Studies
- Business and Economics
- Classical and Ancient Near Eastern Studies
- Computer Sciences
- Cultural Studies
- Engineering
- General Interest
- Geosciences
- Industrial Chemistry
- Islamic and Middle Eastern Studies
- Jewish Studies
- Library and Information Science, Book Studies
- Life Sciences
- Linguistics and Semiotics
- Literary Studies
- Materials Sciences
- Mathematics
- Social Sciences
- Sports and Recreation
- Theology and Religion
- Publish your article
- The role of authors
- Promoting your article
- Abstracting & indexing
- Publishing Ethics
- Why publish with De Gruyter
- How to publish with De Gruyter
- Our book series
- Our subject areas
- Your digital product at De Gruyter
- Contribute to our reference works
- Product information
- Tools & resources
- Product Information
- Promotional Materials
- Orders and Inquiries
- FAQ for Library Suppliers and Book Sellers
- Repository Policy
- Free access policy
- Open Access agreements
- Database portals
- For Authors
- Customer service
- People + Culture
- Journal Management
- How to join us
- Working at De Gruyter
- Mission & Vision
- De Gruyter Foundation
- De Gruyter Ebound
- Our Responsibility
- Partner publishers

Your purchase has been completed. Your documents are now available to view.
Does the dopamine hypothesis explain schizophrenia?
Chi-Ieong David Lau is a Consultant Neurologist whose research interests focus on the cognitive neuroscience underpinning neurological diseases. His recent work includes the investigation of the visual system in migraine, as well as the modulation of slow-wave-sleep-related memory consolidation using a variety of methods, including EEG, neuroimaging, brain stimulation, and genetics. He completed his medical degree and neurology training in Taiwan and postgraduate studies at the University College London and the University of Oxford, supported by the British Chevening Scholarship.
Han-Cheng Wang is a Consultant Neurologist at Shin Kong Wu Ho-Su Memorial Hospital, with specialist clinics for Parkinson’s disease and movement disorders. He is Assistant Professor of Neurology at the College of Medicine, National Taiwan University. He is the former President and present Standing Member of the Executive Board of Taiwan Movement Disorder Society. His research interests include understanding basic neurophysiology underlying human movements and movement disorders. He is interested in linking clinical features with functional connectivity of the brain, reflected in his recent works correlating regional cerebral blood flow (CBF) changes and tract-specific abnormalities with severity of Parkinsonism.
Jung-Lung Hsu is a Clinical Neurologist. He is interested in behavioral/cognitive neuroscience. His main study is focused on brain structural change and human behavior. He is also participating in the event-related potential (ERP) study (P50 and MMN) of schizophrenia patients.
Mu-En Liu’s research interests include biological psychiatry and geriatric psychiatry. Some of the study topics are novel in the genetic study of cognitive ageing. Recently, he examined genetic effects on age-related morphologic changes in the brain. His researches may clarify the underlying molecular mechanisms of brain aging.
The dopamine hypothesis has been the cornerstone in the research and clinical practice of schizophrenia. With the initial emphasis on the role of excessive dopamine, the hypothesis has evolved to a concept of combining prefrontal hypodopaminergia and striatal hyperdopaminergia, and subsequently to the present aberrant salience hypothesis. This article provides a brief overview of the development and evidence of the dopamine hypothesis. It will argue that the current model of aberrant salience explains psychosis in schizophrenia and provides a plausible linkage between the pharmacological and cognitive aspects of the disease. Despite the privileged role of dopamine hypothesis in psychosis, its pathophysiological rather than etiological basis, its limitations in defining symptoms other than psychosis, as well as the evidence of other neurotransmitters such as glutamate and adenosine, prompt us to a wider perspective of the disease. Finally, dopamine does explain the pathophysiology of schizophrenia, but not necessarily the cause per se. Rather, dopamine acts as the common final pathway of a wide variety of predisposing factors, either environmental, genetic, or both, that lead to the disease. Other neurotransmitters, such as glutamate and adenosine, may also collaborate with dopamine to give rise to the entire picture of schizophrenia.
About the authors

The authors would like to thank Miss Frankie Wing See Tam for her valuable comments on the manuscript.
Conflicts of interest: The authors have no conflicts of interest relevant to this article.
Abbott, C.C., Jaramillo, A., Wilcox, C.E., and Hamilton, D.A. (2013). Antipsychotic drug effects in schizophrenia: a review of longitudinal FMRI investigations and neural interpretations. Curr. Med. Chem. 20 , 428–437. Search in Google Scholar
Abi-Dargham, A. (2003). Probing cortical dopamine function in schizophrenia: what can D1 receptors tell us? World Psychiatry 2 , 166–171. Search in Google Scholar
Abi-Dargham, A. and Moore, H. (2003). Prefrontal DA transmission at D1 receptors and the pathology of schizophrenia. Neuroscientist 9 , 404–416. 10.1177/1073858403252674 Search in Google Scholar
Abi-Dargham, A., Gil, R., Krystal, J., Baldwin, R.M., Seibyl, J.P., Bowers, M., van Dyck, C.H., Charney, D.S., Innis, R.B., and Laruelle, M. (1998). Increased striatal dopamine transmission in schizophrenia: confirmation in a second cohort. Am. J. Psychiatry 155 , 761–767. Search in Google Scholar
Abi-Dargham, A., Mawlawi, O., Lombardo, I., Gil, R., Martinez, D., Huang, Y., Hwang, D.R., Keilp, J., Kochan, L., Van Heertum, R., et al. (2002). Prefrontal dopamine D1 receptors and working memory in schizophrenia. J. Neurosci. 22 , 3708–3719. 10.1523/JNEUROSCI.22-09-03708.2002 Search in Google Scholar
Abi-Dargham, A., Xu, X., Thompson, J.L., Gil, R., Kegeles, L.S., Urban, N.B., Narendran, R., Hwang, D., Laruelle, M., and Slifstein, M. (2012). Increased prefrontal cortical D(1) receptors in drug naive patients with schizophrenia: a PET study with [(1)(1)C]NNC112. J. Psychopharmacol. 26 , 794–805. 10.1177/0269881111409265 Search in Google Scholar
Agid, O., Seeman, P., and Kapur, S. (2006). The “delayed onset” of antipsychotic action–an idea whose time has come and gone. J. Psychiatry Neurosci. 31 , 93–100. Search in Google Scholar
Akil, M., Pierri, J.N., Whitehead, R.E., Edgar, C.L., Mohila, C., Sampson, A.R., and Lewis, D.A. (1999). Lamina-specific alterations in the dopamine innervation of the prefrontal cortex in schizophrenic subjects. Am. J. Psychiatry 156 , 1580–1589. 10.1176/ajp.156.10.1580 Search in Google Scholar
Allen, N.C., Bagade, S., McQueen, M.B., Ioannidis, J.P., Kavvoura, F.K., Khoury, M.J., Tanzi, R.E., and Bertram, L. (2008). Systematic meta-analyses and field synopsis of genetic association studies in schizophrenia: the SzGene database. Nat. Genet. 40 , 827–834. 10.1038/ng.171 Search in Google Scholar
Andreasen, N.C. (1982). Negative symptoms in schizophrenia. Definition and reliability. Arch. Gen. Psychiatry 39 , 784–788. 10.1001/archpsyc.1982.04290070020005 Search in Google Scholar
Barch, D.M. and Ceaser, A. (2012). Cognition in schizophrenia: core psychological and neural mechanisms. Trends Cognit. Sci. 16 , 27–34. 10.1016/j.tics.2011.11.015 Search in Google Scholar
Barch, D.M., Carter, C.S., Braver, T.S., Sabb, F.W., MacDonald, A. 3rd., Noll, D.C., and Cohen, J.D. (2001). Selective deficits in prefrontal cortex function in medication-naive patients with schizophrenia. Arch. Gen. Psychiatry 58 , 280–288. 10.1001/archpsyc.58.3.280 Search in Google Scholar
Berridge, K.C. and Robinson, T.E. (1998). What is the role of dopamine in reward: hedonic impact, reward learning, or incentive salience? Brain Res. Brain Res. Rev. 28 , 309–369. 10.1016/S0165-0173(98)00019-8 Search in Google Scholar
Berton, O., McClung, C.A., DiLeone, R.J., Krishnan, V., Renthal, W., Russo, S.J., Graham, D., Tsankova, N.M., Bolanos, C.A., Rios, M., et al. (2006). Essential role of BDNF in the mesolimbic dopamine pathway in social defeat stress. Science 311 , 864–868. 10.1126/science.1120972 Search in Google Scholar PubMed
Boison, D., Singer, P., Shen, H.Y., Feldon, J., and Yee, B.K. (2013). Adenosine hypothesis of schizophrenia – opportunities for pharmacotherapy. Neuropharmacology 62 , 1527–1543. 10.1016/j.neuropharm.2011.01.048 Search in Google Scholar
Boksa, P. and El-Khodor, B.F. (2003). Birth insult interacts with stress at adulthood to alter dopaminergic function in animal models: possible implications for schizophrenia and other disorders. Neurosci. Biobehav. Rev. 27 , 91–101. 10.1016/S0149-7634(03)00012-5 Search in Google Scholar
Bossong, M.G., van Berckel, B.N., Boellaard, R., Zuurman, L., Schuit, R.C., Windhorst, A.D., van Gerven, J.M., Ramsey, N.F., Lammertsma, A.A., and Kahn, R.S. (2009). Delta 9-tetrahydrocannabinol induces dopamine release in the human striatum. Neuropsychopharmacology 34 , 759–766. 10.1038/npp.2008.138 Search in Google Scholar PubMed
Breier, A., Su, T.P., and Pickar, D. (1997). Schizophrenia is associated with elevated amphetamine-induced synaptic dopamine concentrations: evidence from a novel positron emission tomography method. Proc. Natl. Acad. Sci. USA 94 , 2569–2574. 10.1073/pnas.94.6.2569 Search in Google Scholar PubMed PubMed Central
Brody, A.L., Olmstead, R.E., London, E.D., Farahi, J., Meyer, J.H., Grossman, P., Lee, G.S., Huang, J., Hahn, E.L., and Mandelkern, M.A. (2004). Smoking-induced ventral striatum dopamine release. Am. J. Psychiatry. 161 , 1211–1218. 10.1176/appi.ajp.161.7.1211 Search in Google Scholar PubMed
Butwell, M., Jamieson, E., Leese, M., and Taylor, P. (2000). Trends in special (high-security) hospitals. 2: Residency and discharge episodes, 1986–1995. Br. J. Psychiatry 176 , 260–265. 10.1192/bjp.176.3.260 Search in Google Scholar PubMed
Carlsson, A. and Lindqvist, M. (1963). Effect of chlorpromazine or haloperidol on formation of 3methoxytyramine and normetanephrine in mouse brain. Acta Pharmacol. Toxicol. 20 , 140–144. 10.1111/j.1600-0773.1963.tb01730.x Search in Google Scholar PubMed
Caspi, A., Moffitt, T.E., Cannon, M., McClay, J., Murray, R., Harrington, H., Taylor, A., Arseneault, L., Williams, B., Braithwaite, A., et al. (2005). Moderation of the effect of adolescent-onset cannabis use on adult psychosis by a functional polymorphism in the catechol-O-methyltransferase gene: longitudinal evidence of a gene X environment interaction. Biol. Psychiatry 57 , 1117–1127. 10.1016/j.biopsych.2005.01.026 Search in Google Scholar PubMed
Catafau, A.M., Corripio, I., Pérez, V., Martin, J.C., Schotte, A., Carrió, I., and Alvarez, E. (2006). Dopamine D2 receptor occupancy by risperidone: implications for the timing and magnitude of clinical response. Psychiatry Res. 148 , 175–183. 10.1016/j.pscychresns.2006.02.001 Search in Google Scholar PubMed
Coyle, J.T. (2006). Glutamate and schizophrenia: beyond the dopamine hypothesis. Cell. Mol. Neurobiol. 26 , 365–384. 10.1007/s10571-006-9062-8 Search in Google Scholar PubMed
Crawley, J.C., Owens, D.G., Crow, T.J., Poulter, M., Johnstone, E.C., Smith, T., Oldland, S.R., Veall, N., Owen, F., Zanelli. G.D. (1986). Dopamine D2 receptors in schizophrenia studied in vivo. Lancet 2 , 224–225. 10.1016/S0140-6736(86)92525-0 Search in Google Scholar
da Silva Alves, F., Figee, M., van Avamelsvoort, T., Veltman, D., and de Haan, L. (2008). The revised dopamine hypothesis of schizophrenia: evidence from pharmacological MRI studies with atypical antipsychotic medication. Psychopharmacol. Bull. 41 , 121–132. Search in Google Scholar
Davis, K.L., Kahn, R.S., Ko, G., and Davidson, M. (1991). Dopamine in schizophrenia: a review and reconceptualization. Am. J. Psychiatry 148 , 1474–1486. 10.1176/ajp.148.11.1474 Search in Google Scholar PubMed
Dold, M., Li, C., Tardy, M., Khorsand, V., Gillies, D., and Leucht, S. (2012). Benzodiazepines for schizophrenia. Cochrane Database Syst. Rev. 11, CD006391. 10.1002/14651858.CD006391.pub2 Search in Google Scholar PubMed PubMed Central
Fusar-Poli, P., Howes, O.D., Allen, P., Broome, M., Valli, I., Asselin, M.C., Grasby, P.M., and McGuire, P.K. (2010). Abnormal frontostriatal interactions in people with prodromal signs of psychosis: a multimodal imaging study. Arch. Gen. Psychiatry 67 , 683–691. 10.1001/archgenpsychiatry.2010.77 Search in Google Scholar PubMed
Fusar-Poli, P. and Meyer-Lindenberg, A. (2013). Striatal presynaptic dopamine in schizophrenia, part I: meta-analysis of dopamine active transporter (DAT) density. Schizophr. Bull. 39 , 22–32. 10.1093/schbul/sbr111 Search in Google Scholar PubMed PubMed Central
Goldman-Rakic, P.S. and Selemon, L.D. (1997). Functional and anatomical aspects of prefrontal pathology in schizophrenia. Schizophr. Bull. 23 , 437–458. 10.1093/schbul/23.3.437 Search in Google Scholar PubMed
Gordon, J.A. (2010). Testing the glutamate hypothesis of schizophrenia. Nat. Neurosci. 13 , 2–4. 10.1038/nn0110-2 Search in Google Scholar PubMed
Guo, N., Hwang, D.R., Lo, E.S., Huang, Y.Y., Laruelle, M., and Abi-Dargham, A. (2003). Dopamine depletion and in vivo binding of PET D1 receptor radioligands: implications for imaging studies in schizophrenia. Neuropsychopharmacology 28 , 1703–1711. 10.1038/sj.npp.1300224 Search in Google Scholar PubMed
Heinrichs, R.W. (2007). Cognitive improvement in response to antipsychotic drugs: neurocognitive effects of antipsychotic medications in patients with chronic schizophrenia in the CATIE Trial. Arch. Gen. Psychiatry 64 , 631–632. 10.1001/archpsyc.64.6.631 Search in Google Scholar PubMed
Honey, G.D., Bullmore, E.T., Soni, W., Varatheesan, M., Williams, S.C.R., and Sharma, T. (1999). Differences in frontal cortical activation by a working memory task after substitution of risperidone for typical antipsychotic drugs in patients with schizophrenia. Proc. Natl. Acad. Sci. USA 96 , 13432–13437. 10.1073/pnas.96.23.13432 Search in Google Scholar PubMed PubMed Central
Howes, O.D., Egerton, A., Allan, V., McGuire, P., Stokes, P., and Kapur, S. (2009a). Mechanisms underlying psychosis and antipsychotic treatment response in schizophrenia: insights from PET and SPECT imaging. Curr. Pharm. Des. 15 , 2550–2559. 10.2174/138161209788957528 Search in Google Scholar
Howes, O.D., Montgomery, A.J., Asselin, M.C., Murray, R.M., Valli, I., Tabraham, P., Bramon-Bosch, E., Valmaggia, L., Johns, L., Broome, M., et al. (2009b). Elevated striatal dopamine function linked to prodromal signs of schizophrenia. Arch. Gen. Psychiatry 66 , 13–20. 10.1001/archgenpsychiatry.2008.514 Search in Google Scholar
Huttunen, J., Heinimaa, M., Svirskis, T., Nyman, M., Kajander, J., Forsback, S., Solin, O., Ilonen, T., Korkeila, J., Ristkari, T., et al. (2008). Striatal dopamine synthesis in first-degree relatives of patients with schizophrenia. Biol. Psychiatry 63 , 114–117. 10.1016/j.biopsych.2007.04.017 Search in Google Scholar
Isaac, S.O. and Berridge, C.W. (2003). Wake-promoting actions of dopamine D1 and D2 receptor stimulation. J. Pharmacol. Exp. Ther. 307 , 386–394. 10.1124/jpet.103.053918 Search in Google Scholar
Jones, H.M., Brammer, M.J., O′Toole, M., Taylor, T., Ohlsen, R.I., Brown, R.G., Purvis, R., Williams, S., and Pilowsky, L.S. (2004). Cortical effects of quetiapine in first-episode schizophrenia: a preliminary functional magnetic resonance imaging study. Biol. Psychiatry 56 , 938–942. 10.1016/j.biopsych.2004.08.006 Search in Google Scholar
Kahn, R.S., Harvey, P.D., Davidson, M., Keefe, R.S., Apter, S., Neale, J.M., Mohs, R.C., and Davis, K.L. (1994). Neuropsychological correlates of central monoamine function in chronic schizophrenia: relationship between CSF metabolites and cognitive function. Schizophr. Res. 11 , 217–224. 10.1016/0920-9964(94)90015-9 Search in Google Scholar
Kapur, S. (2003). Psychosis as a state of aberrant salience: a framework linking biology, phenomenology, and pharmacology in schizophrenia. Am. J. Psychiatry 160 , 13–23. 10.1176/appi.ajp.160.1.13 Search in Google Scholar PubMed
Kapur, S., Zipursky, R.B., and Remington, G. (1999). Clinical and theoretical implications of 5-HT2 and D2 receptor occupancy of clozapine, risperidone, and olanzapine in schizophrenia. Am. J. Psychiatry 156 , 286–293. 10.1176/ajp.156.2.286 Search in Google Scholar
Karlsson, P., Farde, L., Halldin, C., and Sedvall, G. (2002). PET study of D(1) dopamine receptor binding in neuroleptic-naive patients with schizophrenia. Am. J. Psychiatry 159 , 761–767. 10.1176/appi.ajp.159.5.761 Search in Google Scholar PubMed
Kebabian, J.W. and Calne, D.B. (1979). Multiple receptors for dopamine. Nature 277 , 93–96. 10.1038/277093a0 Search in Google Scholar PubMed
Kestler, L.P., Walker, E., and Vega, E.M. (2001). Dopamine receptors in the brains of schizophrenia patients: a meta-analysis of the findings. Behav. Pharmacol. 12 , 355–371. 10.1097/00008877-200109000-00007 Search in Google Scholar PubMed
King, M.V., Seeman, P., Marsden, C.A., and Fone, K.C. (2009). Increased dopamine D2High receptors in rats reared in social isolation. Synapse 63 , 476–483. 10.1002/syn.20624 Search in Google Scholar
Kirsch, P., Ronshausen, S., Mier, D., and Gallhofer, B. (2007). The influence of antipsychotic treatment on brain reward system reactivity in schizophrenia patients. Pharmacopsychiatry 40 , 196–198. 10.1055/s-2007-984463 Search in Google Scholar
Knable, M.B., Hyde, T.M., Herman, M.M, Carter, J.M, Bigelow, L., and Kleinman, J.E. (1994). Quantitative autoradiography of dopamine-D1 receptors, D2 receptors, and dopamine uptake sites in postmortem striatal specimens from schizophrenic patients. Biol. Psychiatry 36 , 827–835. 10.1016/0006-3223(94)90593-2 Search in Google Scholar
Knable, M.B., Hyde, T.M., Murray, A.M., Herman, M.M., and Kleinman, J.E. (1996). A postmortem study of frontal cortical dopamine D1 receptors in schizophrenics, psychiatric controls, and normal controls. Biol. Psychiatry 40 , 1191–1199. 10.1016/S0006-3223(96)00116-3 Search in Google Scholar
Kosaka, J., Takahashi, H., Ito, H., Takano, A., Fujimura, Y., Matsumoto, R., Nozaki, S., Yasuno, F., Okubo, Y., Kishimoto, T., et al. (2010). Decreased binding of [11C]NNC112 and [11C]SCH23390 in patients with chronic schizophrenia. Life Sci. 86 , 814–818. 10.1016/j.lfs.2010.03.018 Search in Google Scholar
Kraguljac, N.V., Reid, M., White, D., Jones, R., den Hollander, J., Lowman, D., and Lahti, A.C. (2012). Neurometabolites in schizophrenia and bipolar disorder – a systematic review and meta-analysis. Psychiatry Res. 203 , 111–125. 10.1016/j.pscychresns.2012.02.003 Search in Google Scholar
Laruelle, M. (2000). The role of endogenous sensitization in the pathophysiology of schizophrenia: implications from recent brain imaging studies. Brain Res. Brain Res. Rev. 31 , 371–384. 10.1016/S0165-0173(99)00054-5 Search in Google Scholar
Laruelle, M., Abi-Dargham, A., Gil, R., Kegeles, L., and Innis, R. (1999). Increased dopamine transmission in schizophrenia: relationship to illness phases. Biol. Psychiatry 46, 56–72. 10.1016/S0006-3223(99)00067-0 Search in Google Scholar
Laruelle, M., Abi-Dargham, A., van Dyck, C.H., Gil, R., D’Souza, C.D., Erdos, J., McCance, E., Rosenblatt, W., Fingado, C., Zoghbi, S.S., et al. (1996). Single photon emission computerized tomography imaging of amphetamine-induced dopamine release in drug-free schizophrenic subjects. Proc. Natl. Acad. Sci. USA 93 , 9235–9240. 10.1073/pnas.93.17.9235 Search in Google Scholar PubMed PubMed Central
Leucht, S., Busch, R., Hamann, J., Kissling, W., and Kane, J.M. (2005). Early-onset hypothesis of antipsychotic drug action: a hypothesis tested, confirmed and extended. Biol. Psychiatry 57 , 1543–1549. 10.1016/j.biopsych.2005.02.023 Search in Google Scholar PubMed
Lewis, R., Kapur, S., Jones, C., DaSilva, J., Brown, G.M., Wilson, A.A., Houle, S., and Zipursky, R.B. (1999). Serotonin 5-HT2 receptors in schizophrenia: a PET study using [18F]setoperone in neuroleptic-naive patients and normal subjects. Am. J. Psychiatry 156 , 72–78. 10.1176/ajp.156.1.72 Search in Google Scholar
Lund, A., Kroken, R., Thomsen, T., Hugdahl, K., Smievoll, A.I., Barndon, R., Iversen, J., Landrø, N.I., Sundet, K., Rund, B.R., et al. (2002). “Normalization” of brain activation in schizophrenia. An fMRI study. Schizophr. Res. 58 , 333–335. 10.1016/S0920-9964(01)00369-3 Search in Google Scholar
Martinot, J.L., Paillere-Martinot, M.L., Loc′h, C., Hardy, P., Poirier, M.F., Mazoyer, B., Beaufils, B., Mazière, B., Allilaire, J.F., and Syrota, A. (1991). The estimated density of D2 striatal receptors in schizophrenia. A study with positron emission tomography and 76Br-bromolisuride. Br. J. Psychiatry 158 , 346–350. 10.1192/bjp.158.3.346 Search in Google Scholar PubMed
Martinot, J.L., Paillere-Martinot, M.L., Loc′h, C., Lecrubier, Y., Dao-Castellana, M.H., Aubin, F., Allilaire, J.F., Mazoyer, B., Mazière, B., and Syrota, A. (1994). Central D2 receptors and negative symptoms of schizophrenia. Br. J. Psychiatry 164, 27–34. 10.1192/bjp.164.1.27 Search in Google Scholar PubMed
McClelland, G.R., Cooper, S.M., and Pilgrim, A.J. (1990). A comparison of the central nervous system effects of haloperidol, chlorpromazine and sulpiride in normal volunteers. Br. J. Clin. Pharmacol. 30 , 795–803. 10.1111/j.1365-2125.1990.tb05444.x Search in Google Scholar PubMed PubMed Central
McGowan, S., Lawrence, A.D., Sales, T., Quested, D., and Grasby, P. (2004). Presynaptic dopaminergic dysfunction in schizophrenia: a positron emission tomographic [18F]fluorodopa study. Arch. Gen. Psychiatry 61 , 134–142. 10.1001/archpsyc.61.2.134 Search in Google Scholar PubMed
Meisenzahl, E.M., Scheuerecker, J., Zipse, M., Ufer, S., Wiesmann, M., Frodl, T., Koutsouleris, N., Zetzsche, T., Schmitt, G., Riedel, M., et al (2006). Effects of treatment with the atypical neuroleptic quetiapine on working memory function: a functional MRI follow-up investigation. Eur. Arch. Psychiatry Clin. Neurosci. 256 , 522–531. 10.1007/s00406-006-0687-x Search in Google Scholar PubMed
Meltzer, H.Y. (1979). Clinical evidence for multiple dopamine receptors in man. Commun. Psychopharmacol. 3 , 457–470. Search in Google Scholar
Meltzer, H.Y. (1989). Clinical studies on the mechanism of action of clozapine: the dopamine-serotonin hypothesis of schizophrenia. Psychopharmacology 99 Suppl , S18–S27. 10.1007/BF00442554 Search in Google Scholar PubMed
Meltzer, H.Y., Sommers, A.A., and Luchins, D.J. (1986). The effect of neuroleptics and other psychotropic drugs on negative symptoms in schizophrenia. J. Clin. Psychopharmacol. 6 , 329–338. 10.1097/00004714-198612000-00002 Search in Google Scholar
Meyer, U. and Feldon, J. (2009). Prenatal exposure to infection: a primary mechanism for abnormal dopaminergic development in schizophrenia. Psychopharmacology 206 , 587–602. 10.1007/s00213-009-1504-9 Search in Google Scholar PubMed
Monchi, O., Taylor, J.G., and Dagher, A. (2000). A neural model of working memory processes in normal subjects, Parkinson’s disease and schizophrenia for fMRI design and predictions. Neural Networks 13 , 953–973. 10.1016/S0893-6080(00)00058-7 Search in Google Scholar
Moncrieff, J. (2009). A critique of the dopamine hypothesis of schizophrenia and psychosis. Harv. Rev. Psychiatry 17 , 214–225. 10.1080/10673220902979896 Search in Google Scholar PubMed
Nieratschker, V., Nothen, M.M., and Rietschel, M. (2010). New genetic findings in schizophrenia: Is there still room for the dopamine hypothesis of schizophrenia? Front Behav. Neurosci. 4 , 1–10. doi: 10.3389/fnbeh.2010.00023. 10.3389/fnbeh.2010.00023 Search in Google Scholar PubMed PubMed Central
Nikolaus, S., Antke, C., and Müller, H.W. (2009). In vivo imaging of synaptic function in the central nervous system: II. Mental and affective disorders. Behav. Brain Res. 204 , 32–66. 10.1016/j.bbr.2009.06.009 Search in Google Scholar PubMed
Ogawa, S. and Lee, T.M. (1990). Magnetic resonance imaging of blood vessels at high fields: in vivo and in vitro measurements and image simulation. Magn. Reson. Med. 16 , 9–18. 10.1002/mrm.1910160103 Search in Google Scholar PubMed
Okubo, Y., Suhara, T., Suzuki, K., Kobayashi, K., Inoue, O., Terasaki, O., Someya, Y., Sassa, T., Sudo, Y., Matsushima, E., et al. (1997). Decreased prefrontal dopamine D1 receptors in schizophrenia revealed by PET. Nature 385 , 634–636. 10.1038/385634a0 Search in Google Scholar PubMed
Patil, S. T., Zhang, L., Martenyi, F., Lowe, S.L., Jackson, K.A., Andreev, B.V, Avedisova, A.S, Bardenstein, L.M, Gurovich, I.Y., Morozova, M.A., et al. (2007). Activation of mGlu2/3 receptors as a new approach to treat schizophrenia: a randomized Phase 2 clinical trial. Nat. Med. 13 , 1102–1107. 10.1038/nm1632 Search in Google Scholar PubMed
Pearce, R.K., Seeman, P., Jellinger, K., and Tourtellotte, W.W. (1990). Dopamine uptake sites and dopamine receptors in Parkinson’s disease and schizophrenia. Eur. Neurol. 30 Suppl 1 , 9–14. 10.1159/000117168 Search in Google Scholar PubMed
Pearlson, G.D., Tune, L.E., Wong, D.F., Aylward, E.H., Barta, P.E., Powers, R.E., Tien, A.Y., Chase, G.A., Harris, G.J., Rabins, P.V. (1993). Quantitative D2 dopamine receptor PET and structural MRI changes in late-onset schizophrenia. Schizophr. Bull. 19 , 783–795. 10.1093/schbul/19.4.783 Search in Google Scholar PubMed
Pilowsky, L.S., Bressan, R.A., Stone, J.M., Erlandsson, K., Mulligan, R.S., Krystal, J.H., and Ell, P.J. (2006). First in vivo evidence of an NMDA receptor deficit in medication-free schizophrenic patients. Mol. Psychiatry 11 , 118–119. 10.1038/sj.mp.4001751 Search in Google Scholar PubMed
Pilowsky, L.S., Costa, D.C., Ell, P.J., Murray, R.M., Verhoeff, N.P., and Kerwin, R.W. (1992). Clozapine, single photon emission tomography, and the D2 dopamine receptor blockade hypothesis of schizophrenia. Lancet 340 , 199–202. 10.1016/0140-6736(92)90467-H Search in Google Scholar
Pilowsky, L.S., Costa, D.C., Ell, P.J., Murray, R.M., Verhoeff, N.P., and Kerwin, R.W. (1993). Antipsychotic medication, D2 dopamine receptor blockade and clinical response: a 123I IBZM SPET (single photon emission tomography) study. Psychol. Med. 23 , 791–797. 10.1017/S0033291700025575 Search in Google Scholar
Port, J.D. and Agarwal, N. (2011). MR spectroscopy in schizophrenia. J. Magn. Reson. Imaging 34 , 1251–1261. 10.1002/jmri.22787 Search in Google Scholar
Pruessner, J.C., Champagne, F., Meaney, M.J., and Dagher, A. (2004). Dopamine release in response to a psychological stress in humans and its relationship to early life maternal care: a positron emission tomography study using [ 11 C]raclopride. J. Neurosci. 24 , 2825–2831. 10.1523/JNEUROSCI.3422-03.2004 Search in Google Scholar
Remington, G. and Kapur, S. (1999). D2 and 5-HT2 receptor effects of antipsychotics: bridging basic and clinical findings using PET. J. Clin. Psychiatry 60 (Suppl 10) , 15–19. Search in Google Scholar
Roiser, J.P., Stephan, K.E., and Joyce, E.M. (2009). Do patients with schizophrenia exhibit aberrant salience? Psychol. Med. 39, 199–209. Search in Google Scholar
Rothman, R.B., Baumann, M.H., Dersch, C.M., Romero, D.V., Rice, K.C., Carroll, F.I., and Partilla, J.S. (2001). Amphetamine-type central nervous system stimulants release norepinephrine more potently than they release dopamine and serotonin. Synapse 39 , 32–41. 10.1002/1098-2396(20010101)39:1<32::AID-SYN5>3.0.CO;2-3 Search in Google Scholar
Rowland, L.M., Kontson, K., West, J., Edden, R.A., Zhu, H., Wijtenburg, S.A., Holcomb, H.H., and Barker, P.B. (2012). In vivo measurements of glutamate, GABA, and NAAG in schizophrenia. Schizophr. Bull. Oct 18. [Epub ahead of print]. 10.1016/S0920-9964(12)70871-X Search in Google Scholar
Rzanny, R., Klemm, S., Reichenbach, J.R., Pfleiderer, S.O., Schmidt, B., Volz, H.P., Blanz, B., and Kaiser, W.A. (2003). 31P-MR spectroscopy in children and adolescents with a familial risk of schizophrenia. Eur. Radiol. 13 , 763–770. 10.1007/s00330-002-1565-1 Search in Google Scholar
Seeman, P. and Lee, T. (1975). Antipsychotic drugs: direct correlation between clinical potency and presynaptic action on dopamine neurons. Science 188 , 1217–1219. 10.1126/science.1145194 Search in Google Scholar
Snitz, B.E., MacDonald, A. 3rd, Cohen, J.D., Cho, R.Y., Becker, T., and Carter, C.S. (2005). Lateral and medial hypofrontality in first-episode schizophrenia: functional activity in a medication-naive state and effects of short-term atypical antipsychotic treatment. Am. J. Psychiatry 162 , 2322–2329. 10.1176/appi.ajp.162.12.2322 Search in Google Scholar
Stanley, J.A., Williamson, P.C., Drost, D.J., Carr, T.J., Rylett, R.J., Morrison-Stewart, S., and Thompson, R.T. (1994). Membrane phospholipid metabolism and schizophrenia. An in vivo 31P-MR spectroscopy study. Schizophr. Res. 13 , 209–215. 10.1016/0920-9964(94)90044-2 Search in Google Scholar
Stefanis, N.C., Henquet, C., Avramopoulos, D., Smyrnis, N., Evdokimidis, I., Myin-Germeys, I., Stefanis, C.N., and Van Os, J. (2007). COMT Val158Met moderation of stress-induced psychosis. Psychol. Med. 37 , 1651–1656. 10.1017/S0033291707001080 Search in Google Scholar
Taylor, D.M. and Duncan-McConnell, D. (2000). Refractory schizophrenia and atypical antipsychotics. J. Psychopharmacol. 14 , 409–418. 10.1177/026988110001400411 Search in Google Scholar
Taylor, K.I., Zach, P., and Brugger, P. (2002). Why is magical ideation related to leftward deviation on an implicit line bisection task? Cortex 38 , 247–252. 10.1016/S0010-9452(08)70653-1 Search in Google Scholar
Taylor, S.F., Koeppe, R.A., Tandon, R., Zubieta, J.K., and Frey, K.A. (2000). In vivo measurement of the vesicular monoamine transporter in schizophrenia. Neuropsychopharmacology 23 , 667–675. 10.1016/S0893-133X(00)00165-2 Search in Google Scholar
Thomas, M.A., Ke, Y., Levitt, J., Caplan, R., Curran, J., Asarnow, R., and McCracken, J. (1998). Preliminary study of frontal lobe 1H MR spectroscopy in childhood-onset schizophrenia. J. Magn. Reson. Imaging 8 , 841–846. 10.1002/jmri.1880080413 Search in Google Scholar
Tune, L., Barta, P., Wong, D., Powers, R.E., Pearlson, G., Tien, A.Y., and Wagner, H.N. (1996). Striatal dopamine D2 receptor quantification and superior temporal gyrus: volume determination in 14 chronic schizophrenic subjects. Psychiatry Res. 67 , 155–158. 10.1016/0925-4927(96)02728-X Search in Google Scholar
Ujike, H. (2002). Stimulant-induced psychosis and schizophrenia: the role of sensitization. Curr. Psychiatry Rep. 4 , 177–184. 10.1007/s11920-002-0024-7 Search in Google Scholar
van Os, J. (2009). A salience dysregulation syndrome. Br. J. Psychiatry 194 , 101–103. 10.1192/bjp.bp.108.054254 Search in Google Scholar
van Os, J., Rutten, B.P., and Poulton, R. (2008). Gene-environment interactions in schizophrenia: review of epidemiological findings and future directions. Schizophr. Bull. 34 , 1066–1082. 10.1093/schbul/sbn117 Search in Google Scholar
Vollenweider, F.X., Vontobel, P., Oye, I., Hell, D., and Leenders, K.L. (2000). Effects of (S)-ketamine on striatal dopamine: a [11C]raclopride PET study of a model psychosis in humans. J. Psychiatr. Res. 34 , 35–43. 10.1016/S0022-3956(99)00031-X Search in Google Scholar
Waddington, J.L., O’Callaghan, E., Buckley, P., Larkin, C., Redmond, O., Stack, J., and Ennis, J.T. (1992). MR imaging and spectroscopy in schizophrenia in relation to the neurodevelopmental hypothesis. Clin. Neuropharmacol. 15 Suppl 1 Pt A , 118A–119A. 10.1097/00002826-199201001-00064 Search in Google Scholar
Walsh, E., Leese, M., Taylor, P., Johnston, I., Burns, T., Creed, F., Higgit, A., and Murray, R. (2002). Psychosis in high-security and general psychiatric services: report from the UK700 and special hospitals’ treatment resistant schizophrenia groups. Br. J. Psychiatry 180 , 351–357. 10.1192/bjp.180.4.351 Search in Google Scholar
Walter, H., Heckers, S., Kassubek, J., Erk, S., Frasch, K., and Abler, B. (2010). Further evidence for aberrant prefrontal salience coding in schizophrenia. Front. Behav. Neurosci. 3, 1–9. doi: 10.3389/neuro.08.062.2009. 10.3389/neuro.08.062.2009 Search in Google Scholar
Walter, H., Kammerer, H., Frasch, K., Spitzer, M., and Abler, B. (2009). Altered reward functions in patients on atypical antipsychotic medication in line with the revised dopamine hypothesis of schizophrenia. Psychopharmacology 206 , 121–132. 10.1007/s00213-009-1586-4 Search in Google Scholar
Weiss, E.M., Siedentopf, C., Golaszewski, S., Mottaghy, F.M., Hofer, A., Kremser, C., Felber, S., and Fleischhacker, W.W. (2007). Brain activation patterns during a selective attention test–a functional MRI study in healthy volunteers and unmedicated patients during an acute episode of schizophrenia. Psychiatry Res. 154 , 31–40. 10.1016/j.pscychresns.2006.04.009 Search in Google Scholar
Wise, R.A., Spindler, J., deWit, H., and Gerberg, G.J. (1978). Neuroleptic-induced “anhedonia” in rats: pimozide blocks reward quality of food. Science 201 , 262–264. 10.1126/science.566469 Search in Google Scholar
Wolf, R.C., Vasic, N., Höse, A., Spitzer, M., and Walter, H.. (2007). Changes over time in frontotemporal activation during a working memory task in patients with schizophrenia. Schizophr. Res. 91 , 141–150. 10.1016/j.schres.2006.12.001 Search in Google Scholar
Wong, D.F., Wagner, H.N. Jr., Tune, L.E., Dannals, R.F., Pearlson, G.D., Links, J.M., Tamminga, C.A., Broussolle, E.P., Ravert, H.T., Wilson, A.A, et al. (1986). Positron emission tomography reveals elevated D2 dopamine receptors in drug-naive schizophrenics. Science 234 , 1558–1563. 10.1126/science.2878495 Search in Google Scholar
Yamasue, H., Fukui, T., Fukuda, R., Yamada, H., Yamasaki, S., Kuroki, N., Abe, O., Kasai, K., Tsujii, K., Iwanami, A., et al. (2002). 1H-MR spectroscopy and gray matter volume of the anterior cingulate cortex in schizophrenia. Neuroreport 13 , 2133–2137. 10.1097/00001756-200211150-00029 Search in Google Scholar
Zakzanis, K.K. and Hansen, K.T. (1998). Dopamine D2 densities and the schizophrenic brain. Schizophr. Res. 32 , 201–206. 10.1016/S0920-9964(98)00041-3 Search in Google Scholar
©2013 by Walter de Gruyter Berlin Boston
- X / Twitter
Supplementary Materials
Please login or register with De Gruyter to order this product.
Journal and Issue
Articles in the same issue.
Learning Materials
- Business Studies
- Combined Science
- Computer Science
- Engineering
- English Literature
- Environmental Science
- Human Geography
- Macroeconomics
- Microeconomics
- The Dopamine Hypothesis
Often called the ‘feel-good’ hormone, dopamine is in charge of making you feel happy, satisfied, and motivated. When you feel good because you have accomplished something, your brain experiences a dopamine spike. What occurs, though, when there is an imbalance? Could this imbalance play a role in the development of schizophrenia ? This is where the dopamine hypothesis of schizophrenia enters the picture, examining how the imbalance of dopamine levels and the abundance of dopamine receptors contributes to schizophrenia.
Create learning materials about The Dopamine Hypothesis with our free learning app!
- Instand access to millions of learning materials
- Flashcards, notes, mock-exams and more
- Everything you need to ace your exams
Millions of flashcards designed to help you ace your studies
- Cell Biology
What is dopamine?
What is a synapse?
Issues with dopamine production in the ________ nigra contributes to symptoms of schizophrenia.
What did Farde et al. (1990) find in their study into the dopamine hypothesis?
The dopamine hypothesis is a deterministic theory. Why is this a limitation?
How does Parkinson's treatment, L-Dopa, support the dopamine hypothesis?
Are antipsychotics able to cure schizophrenia for good?
True or False: The dopamine hypothesis was later revised as research revealed schizophrenic patients may also have too many dopamine receptors, which can also contribute to the disorder.
Excess dopamine in the mesolimbic pathway (ventral tegmental area and nucleus accumbens) contributes to ________ symptoms of schizophrenia.
True or False: Damage to dopaminergic neurons in the substantia nigra is correlated with the development of Parkinson's.
When did Van Rossum propose the dopamine hypothesis?
Review generated flashcards
to start learning or create your own AI flashcards
Start learning or create your own AI flashcards
- Approaches in Psychology
- Basic Psychology
- Biological Bases of Behavior
- Biopsychology
- Careers in Psychology
- Clinical Psychology
- Cognition and Development
- Cognitive Psychology
- Data Handling and Analysis
- Developmental Psychology
- Eating Behaviour
- Emotion and Motivation
- Famous Psychologists
- Forensic Psychology
- Health Psychology
- Individual Differences Psychology
- Issues and Debates in Psychology
- Personality in Psychology
- Psychological Treatment
- Relationships
- Research Methods in Psychology
- Schizophrenia
- Biological Explanations for Schizophrenia
- Cognitive Behavioural Therapy
- Cognitive Explanations for Schizophrenia
- Diagnosis and Classification of Schizophrenia
- Dysfunctional Family
- Family Therapy
- Interactionist Approach Schizophrenia
- Neural Correlates
- Psychological Explanations for Schizophrenia
- Psychological Therapies for Schizophrenia
- Reliability and Validity in Diagnosis and Classification of Schizophrenia
- Role Of Cannabis
- Schizophrenia Genetics
- Token Economy
- Treatment and Therapies for Schizophrenia
- Typical and Atypical Antipsychotics
- Ventricular Size
- Scientific Foundations of Psychology
- Scientific Investigation
- Sensation and Perception
- Social Context of Behaviour
- Social Psychology
- We will discuss the dopamine hypothesis of schizophrenia .
- First, we will provide a dopamine hypothesis psychology definition.
- Then, we explore the various aspects of the biological explanations of the schizophrenia dopamine hypothesis. including the dopamine hypothesis of psychosis.
- Finally, we will examine the d opamine hypothesis's strengths and weaknesses through an evaluation of the dopamine hypothesis.

The D opamine Hypothesis of Schizophrenia: Definition
The dopamine hypothesis, first proposed by Van Rossum in 1967, is the theory that too much dopamine in the subcortical and limbic regions of the brain may cause positive schizophrenic symptoms . According to the dopamine hypothesis, negative symptoms are associated with less dopamine in the prefrontal cortex .
The dopamine hypothesis was later revised as research revealed schizophrenic patients might also have too many dopamine receptors.
Dopamine is a neurotransmitter that helps the brain send messages to specific body parts. Neurotransmitters are chemical messengers within the brain .
Neurotransmitters bind to receptors in nerve cells after they cross a small gap between them called the synapse. Dopamine is a neurotransmitter involved in our brain’s pleasure and reward systems. The receptors of dopamine are implicated in the dopamine hypothesis of schizophrenia, in that some researchers theorise too many receptors contribute to the overactivity of dopamine in the brain and any subsequent schizophrenic developments.
Biological Explanations of Schizophrenia: Dopamine Hypothesis
The dopamine hypothesis is a biological explanation of schizophrenia, so how does it work? What parts of the brain are involved in the dopamine hypothesis?
- Dopamine is produced in different areas of the brain, and for schizophrenia, we are concerned with the substantia nigra and the ventral tegmental area .
The dopamine produced in the substantia nigra helps us trigger physical movements, including the parts of the face and mouth needed for speech. Problems with this may be responsible for some symptoms of schizophrenia , such as alogia (lack of speech) and psychomotor disturbances.
Damage to dopaminergic neurons in the substantia nigra is correlated with the development of Parkinson's.
Dopamine produced in the ventral tegmental area is released when we expect or receive a reward. This helps both animals and humans modify their behaviour to be more likely to result in a reward or positive experience. An excess of dopamine can lead to hallucinations and delusional or confused thinking, all of which are symptoms of schizophrenia .

Studies of amphetamines given to people without a history of schizophrenia showed that the effect of high levels of dopamine the drug had induced led to symptoms very similar to those of paranoid schizophrenia.
Later revisions of the hypothesis stated that possibly an excess of dopamine in the mesolimbic areas of the brain contributes to positive symptoms, and a low level of dopamine in the brain’s prefrontal cortex contributes to negative symptoms.
Dopamine Hypothesis of Psychosis: Development of the Dopamine Hypothesis
In the 1960s and 1970s, research was conducted into the use of amphetamine drugs and their effect on dopamine levels within the brain. The researchers found that psychotic symptoms increased when these drugs were consumed, sparking the idea that dopamine may help us understand how psychotic symptoms in schizophrenia patients may come to be.
The Dopamine Hypothesis: Strengths and Weaknesses
The dopamine hypothesis has been around for close to 60 years, and has gone through a series of developments alongside facing scrutiny in research. Let's evaluate the dopamine hypothesis of schizophrenia and examine its strengths and weaknesses.
Weaknesses of the Dopamine Hypothesis
The dopamine hypothesis, like any other, has its weaknesses.
- Cause and Effect: One problem with this explanation is that it is not certain whether a dopamine imbalance causes schizophrenia or whether schizophrenia causes a dopamine imbalance. Since the causal nature of the argument is unclear, it is crucial to be careful in determining cause and effect in the development of schizophrenia.
- Farde et al. (1990): Farde et al. (1990) found no difference between the dopamine receptor (D2) levels of schizophrenia patients and control patients. Farde et al.'s (1990) finding suggests that the dopamine hypothesis may not apply to all patients with schizophrenia.
- Determinism: The dopamine hypothesis can be considered deterministic (the belief that factors beyond our control determine human behaviour) because it assumes that the development of schizophrenia depends on the amount of dopamine or dopamine receptors in our brains, which does not correspond to psychological explanations of schizophrenia. It ignores how the environment affects the development of the disorder.Deterministic theories have their limitations, as they are not compatible with societal notions of responsibility, free will and self-control, on which many of our legal and moral norms are based.
Strengths of the Dopamine Hypothesis
On the other hand, some studies are sympathetic to the role dopamine plays in the development of schizophrenia.
- Parkinson's Disease and Levodopa (L-Dopa): Some patients are given levodopa when treating Parkinson’s disease, a drug that increases dopamine levels in the brain. These patients are reported to experience psychotic side effects similar to schizophrenia symptoms, such as hallucinations and dyskinesia. The dopamine aspect supports the role that dopamine plays in the development of schizophrenic symptoms.
- Abi-Dargham et al. (2000): Abi-Dargham et al. (2000) investigated whether there was a true increased level of dopamine and dopamine 2 (D2) receptors within the brain for schizophrenic people compared to controls, accounting for the effects of patients taking antipsychotics and artificially elevating their levels. They found that their results indicated, that for the levels to match up, schizophrenic patients must have an increased level of both dopamine and dopamine receptors compared to controls.

Practical Applications of the Dopamine Hypothesis
Now that we have gained some insight into the dopamine hypothesis’s theoretical aspects, let us look at how it is applied in practice.
Typical Antipsychotic Drugs: First Generation
The dopamine hypothesis has contributed to the development of antipsychotics for schizophrenia and several other disorders in which sufferers experience psychosis.
Typical antipsychotic drugs work by blocking D2 receptors in the brain, limiting dopamine activity. Blocking dopamine receptors can help reduce positive symptoms such as hallucinations
Typical antipsychotics tend to block dopamine in all areas of the brain, not just those that cause schizophrenic symptoms, which can lead to harmful side effects.
Examples of typical antipsychotics include chlorpromazine and haloperidol .
Atypical Antipsychotic Drugs: Second Generation
Atypical antipsychotic s are newer drugs that usually do not have as severe side effects as typical antipsychotics.
Atypical antipsychotics only inhibit dopamine receptors in the limbic system rather than throughout the brain.
They help control the symptoms of schizophrenia without interfering with other systems and potentially causing the same side effects as the previous generation of medications.Atypical antipsychotics bind to dopamine receptors and act on glutamate (an excitatory neurotransmitter) and serotonin. This means that these drugs can help with positive symptoms and reduce negative symptoms such as low mood and impaired cognitive function.
Because of their effect on serotonin, these antipsychotics can also help treat some comorbidities associated with schizophrenia, such as anxiety and depression .
Evaluating Practical Applications of the Dopamine Hypothesis
Considering the practical applications of the dopamine hypothesis affect patients, it's important we evaluate it thoroughly before moving forwards.
Drug treatments such as antipsychotics, developed based on the dopamine hypothesis, help patients manage their daily lives and quality of life. These drugs are relatively easy to make and administer and can positively impact healthcare providers and the economy. This is because they help people with schizophrenia to leave treatment and return to their daily lives, such as their jobs, allowing more people to be treated.
While these drugs help with schizophrenic symptoms, it is essential to point out that they cannot cure schizophrenia. This means that we need more research to find a long-term solution to the disease.
There are some ethical questions about these drugs. In some hospitals, antipsychotic medications may be used to benefit staff rather than patients to make it easier to work with patients.
Antipsychotic medications can have serious side effects, such as tardive dyskinesia, a condition that involves involuntary facial ‘tics’ such as rapid blinking, chewing movements, or rolling of the tongue. Sometimes the side effects can be worse than the initial symptoms of schizophrenia.
The Dopamine Hypothesis - Key takeaways
- The dopamine hypothesis, first proposed by Van Rossum in 1967, is the theory that high dopamine levels may cause schizophrenic symptoms.
- In the 1960s and 70s, researchers studied amphetamines and their effect on dopamine levels in the brain. Researchers found that psychotic symptoms increased when these drugs were used. This finding gave us the idea that this could help us understand the cause of psychotic symptoms in schizophrenia patients.
- Problems with dopamine production and imbalances in dopamine in the substantia nigra and ventral tegmental area may be responsible for the symptoms of schizophrenia, such as alogia, hallucinations, and psychomotor disturbances.
- It is difficult to establish cause and effect in the dopamine hypothesis, however, many studies support the evidence that imbalances in the brain concerning dopamine are related to psychotic and negative symptoms. More research is needed to identify what causes schizophrenia.

Flashcards in The Dopamine Hypothesis 13
A neurotransmitter associated with the rewards system of our brains.
A small gap between neurons across which messages are fired through neurotransmitters.
substantia.
No difference in dopamine (D2) receptor levels between schizophrenic and non-schizophrenic participants.
Deterministic theories have their limitations, as they are not compatible with societal notions of responsibility and self-control, on which many of our legal and moral norms are based.
Some patients are given levodopa (L-Dopa) when treating Parkinson’s disease, a drug that increases dopamine levels in the brain. These patients are reported to experience psychotic side effects similar to schizophrenia symptoms. This supports the role that dopamine plays in the development of schizophrenic symptoms.
Learn with 13 The Dopamine Hypothesis flashcards in the free StudySmarter app
We have 14,000 flashcards about Dynamic Landscapes.
Already have an account? Log in
Frequently Asked Questions about The Dopamine Hypothesis
What is the dopamine hypothesis of schizophrenia in psychology?
The dopamine hypothesis, first proposed by Van Rossum in 1967, is the theory that high or low levels of dopamine may cause schizophrenic symptoms.
What is the role of dopamine in schizophrenia?
The dopamine hypothesis suggests dopamine level imbalances and too many dopamine receptors play a role in the development of symptoms of schizophrenia. However, the dopamine hypothesis does not fully explain how the disorder develops. Newer antipsychotics that are generally more effective than previous drug treatments target more neurotransmitters than just dopamine, suggesting that it may not exclusively be dopamine that causes schizophrenia.
What is the original dopamine hypothesis of schizophrenia?
The original dopamine hypothesis states that too much dopamine within an individual's brain causes the onset of schizophrenic symptoms, such as hallucinations.
Do people with schizophrenia have low levels of dopamine?
Schizophrenic people may have low levels of dopamine. The dopamine hypothesis suggests both low and high levels of dopamine in certain areas of the brain may be responsible for schizophrenic symptoms. Low levels of dopamine, for instance, may result in negative symptoms.
Test your knowledge with multiple choice flashcards
Join the StudySmarter App and learn efficiently with millions of flashcards and more!
Keep learning, you are doing great.
Discover learning materials with the free StudySmarter app

About StudySmarter
StudySmarter is a globally recognized educational technology company, offering a holistic learning platform designed for students of all ages and educational levels. Our platform provides learning support for a wide range of subjects, including STEM, Social Sciences, and Languages and also helps students to successfully master various tests and exams worldwide, such as GCSE, A Level, SAT, ACT, Abitur, and more. We offer an extensive library of learning materials, including interactive flashcards, comprehensive textbook solutions, and detailed explanations. The cutting-edge technology and tools we provide help students create their own learning materials. StudySmarter’s content is not only expert-verified but also regularly updated to ensure accuracy and relevance.

StudySmarter Editorial Team
Team Psychology Teachers
- 9 minutes reading time
- Checked by StudySmarter Editorial Team
Study anywhere. Anytime.Across all devices.
Create a free account to save this explanation..
Save explanations to your personalised space and access them anytime, anywhere!
By signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Sign up to highlight and take notes. It’s 100% free.
Join over 22 million students in learning with our StudySmarter App
The first learning app that truly has everything you need to ace your exams in one place
- Flashcards & Quizzes
- AI Study Assistant
- Study Planner
- Smart Note-Taking

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Does the dopamine hypothesis explain schizophrenia?
- PMID: 23843581
- DOI: 10.1515/revneuro-2013-0011
The dopamine hypothesis has been the cornerstone in the research and clinical practice of schizophrenia. With the initial emphasis on the role of excessive dopamine, the hypothesis has evolved to a concept of combining prefrontal hypodopaminergia and striatal hyperdopaminergia, and subsequently to the present aberrant salience hypothesis. This article provides a brief overview of the development and evidence of the dopamine hypothesis. It will argue that the current model of aberrant salience explains psychosis in schizophrenia and provides a plausible linkage between the pharmacological and cognitive aspects of the disease. Despite the privileged role of dopamine hypothesis in psychosis, its pathophysiological rather than etiological basis, its limitations in defining symptoms other than psychosis, as well as the evidence of other neurotransmitters such as glutamate and adenosine, prompt us to a wider perspective of the disease. Finally, dopamine does explain the pathophysiology of schizophrenia, but not necessarily the cause per se. Rather, dopamine acts as the common final pathway of a wide variety of predisposing factors, either environmental, genetic, or both, that lead to the disease. Other neurotransmitters, such as glutamate and adenosine, may also collaborate with dopamine to give rise to the entire picture of schizophrenia.
PubMed Disclaimer
Similar articles
- The dopamine hypothesis of schizophrenia: version III--the final common pathway. Howes OD, Kapur S. Howes OD, et al. Schizophr Bull. 2009 May;35(3):549-62. doi: 10.1093/schbul/sbp006. Epub 2009 Mar 26. Schizophr Bull. 2009. PMID: 19325164 Free PMC article. Review.
- [Investigation of the dopamine dysregulation hypothesis of schizophrenia with neuroimaging techniques]. Szekeres G, Pávics L, Janka Z. Szekeres G, et al. Ideggyogy Sz. 2002 Jul 20;55(7-8):226-32. Ideggyogy Sz. 2002. PMID: 12201230 Review. Hungarian.
- Glutamate and schizophrenia: phencyclidine, N-methyl-D-aspartate receptors, and dopamine-glutamate interactions. Javitt DC. Javitt DC. Int Rev Neurobiol. 2007;78:69-108. doi: 10.1016/S0074-7742(06)78003-5. Int Rev Neurobiol. 2007. PMID: 17349858 Review.
- Schizophrenia: from developmental deviance to dopamine dysregulation. Murray RM, Lappin J, Di Forti M. Murray RM, et al. Eur Neuropsychopharmacol. 2008 Aug;18 Suppl 3:S129-34. doi: 10.1016/j.euroneuro.2008.04.002. Epub 2008 May 21. Eur Neuropsychopharmacol. 2008. PMID: 18499406 Review.
- Is dopamine neurotransmission altered in prodromal schizophrenia? A review of the evidence. Bauer M, Praschak-Rieder N, Kasper S, Willeit M. Bauer M, et al. Curr Pharm Des. 2012;18(12):1568-79. doi: 10.2174/138161212799958611. Curr Pharm Des. 2012. PMID: 22280434 Review.
- Risperidone Decreases Expression of Serotonin Receptor-2A (5-HT2A) and Serotonin Transporter (SERT) but Not Dopamine Receptors and Dopamine Transporter (DAT) in PBMCs from Patients with Schizophrenia. Alvarez-Herrera S, Rosel Vales M, Pérez-Sánchez G, Becerril-Villanueva E, Flores-Medina Y, Maldonado-García JL, Saracco-Alvarez R, Escamilla R, Pavón L. Alvarez-Herrera S, et al. Pharmaceuticals (Basel). 2024 Jan 28;17(2):167. doi: 10.3390/ph17020167. Pharmaceuticals (Basel). 2024. PMID: 38399382 Free PMC article.
- Xanomeline-Trospium and Muscarinic Involvement in Schizophrenia. Kidambi N, Elsayed OH, El-Mallakh RS. Kidambi N, et al. Neuropsychiatr Dis Treat. 2023 May 10;19:1145-1151. doi: 10.2147/NDT.S406371. eCollection 2023. Neuropsychiatr Dis Treat. 2023. PMID: 37193547 Free PMC article. Review.
- Antipsychotic- and Anxiolytic-like Properties of a Multimodal Compound JJGW08 in Rodents. Żmudzka E, Lustyk K, Głuch-Lutwin M, Mordyl B, Zakrzewska-Sito A, Mierzejewski P, Jaśkowska J, Kołaczkowski M, Sapa J, Pytka K. Żmudzka E, et al. Int J Mol Sci. 2022 Dec 14;23(24):15929. doi: 10.3390/ijms232415929. Int J Mol Sci. 2022. PMID: 36555568 Free PMC article.
- Insights into the Promising Prospect of G Protein and GPCR-Mediated Signaling in Neuropathophysiology and Its Therapeutic Regulation. Rahman MM, Islam MR, Mim SA, Sultana N, Chellappan DK, Dua K, Kamal MA, Sharma R, Emran TB. Rahman MM, et al. Oxid Med Cell Longev. 2022 Sep 21;2022:8425640. doi: 10.1155/2022/8425640. eCollection 2022. Oxid Med Cell Longev. 2022. PMID: 36187336 Free PMC article. Review.
- Modeling Schizophrenia In Vitro: Challenges and Insights on Studying Brain Cells. Brandão-Teles C, Zuccoli GS, Smith BJ, Vieira GM, Crunfli F. Brandão-Teles C, et al. Adv Exp Med Biol. 2022;1400:35-51. doi: 10.1007/978-3-030-97182-3_3. Adv Exp Med Biol. 2022. PMID: 35930224
Publication types
- Search in MeSH
Related information
- PubChem Compound (MeSH Keyword)
LinkOut - more resources
Full text sources, other literature sources.
- scite Smart Citations
- Genetic Alliance
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Schizophrenia A-level Revisions Notes
Bruce Johnson
A-level Psychology Teacher
B.A., Educational Psychology, University of Exeter
Bruce Johnson is an A-level psychology teacher, and head of the sixth form at Caterham High School.
Learn about our Editorial Process
Saul McLeod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul McLeod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
On This Page:
What do the examiners look for?
- Accurate and detailed knowledge
- Clear, coherent, and focused answers
- Effective use of terminology (use the “technical terms”)
In application questions, examiners look for “effective application to the scenario” which means that you need to describe the theory and explain the scenario using the theory making the links between the two very clear. If there is more than one individual in the scenario you must mention all of the characters to get to the top band.
Difference between AS and A level answers
The descriptions follow the same criteria; however you have to use the issues and debates effectively in your answers. “Effectively” means that it needs to be clearly linked and explained in the context of the answer.
Read the model answers to get a clearer idea of what is needed.
Exam Advice
You MUST revise everything – because the exam board could choose any question, however, it does make sense to spend more time on those topics which have not appeared for a while.
With these particular questions there is a sizeable risk that people don’t understand the difference between the questions, and then write about the wrong thing.
Make sure you know which is which, for example do you understand the difference between “genetic explanation” and “neural correlates explanation”, and do you have a model essay for each?
Schizophrenia is a severe mental illness where contact with reality and insight are impaired, an example of psychosis.
Section 1: Diagnosis and Classification of Schizophrenia
Classification is the process of organising symptoms into categories based on which symptoms cluster together in sufferers. Psychologists use the DSM and ICD to diagnose a patient with schizophrenia.
Diagnosis refers to the assigning of a label of a disorder to a patient. The ICD-10 (only negative symptoms need to be present) is used worldwide and the DSM-5 (only positive symptoms need to be present) is used in America.
In order to diagnose Schizophrenia the Mental Health Profession developed the DSM (Diagnostic and Statistical Manual) still used today as a method of classifying mental disorders (particularly in the USA).
It is also used as a basis for the ICD (International Classification of Diseases) used by the World Health Organisation in classifying all disorders (mental and physical).
Note: you may come across the terms DSM-IV and ICD-10. These refer to the latest editions of the two classification systems.
Positive Symptoms
an excess or distortion of normal functions: including hallucinations and delusions.
Positive symptoms are an excess or distortion of normal functions, for example hallucinations, delusions and thought disturbances such as thought insertion.
• Hallucinations are usually auditory or visual perceptions of things that are not present. Imagined stimuli could involve any of the senses. Voices are usually heard coming from outside the person’s head giving instructions on how to behave. • Delusions are false beliefs. Usually the person has convinced him/herself that he/she is someone powerful or important, such as Jesus Christ, the Queen (e.g. Delusions of Grandeur). There are also delusions of being paranoid, worrying that people are out to get them. • Psychomotor Disturbances: Stereotypyical – Rocking backwards and forwards, twitches, & repetitive behaviors. Catatonia- staying in position for hours/days on end, cut off from the world.
Negative Symptoms
where normal functions are limited: including speech poverty and avolition.
Negative symptoms are a diminution or loss of normal functions such as psychomotor disturbances, avolition (the reduction of goal-directed behavior), disturbances of mood and thought disorders.
• Thought disorder in which there are breaks in the train of thought and the person appears to make illogical jumps from one topic to another (loose association). Words may become confused and sentences incoherent (so called ‘word salad). Broadcasting is a thought disorder whereby a person believes their thoughts are being broadcast to others, for example over the radio or through TV. Alogia – aka speech poverty – is a thought disorder were correct words are used but with little meaning. • Avolition: Lack of volition (i.e. desire): in which a person becomes totally apathetic and sits around waiting for things to happen. They engage in no self motivated behavior. Their get up and go has got up and gone!
Classification
Slater & Roth (1969) say that hallucinations are the least important of all the symptoms, as they are not exclusive to schizophrenic people.
Classification and diagnosis does have advantages as it allows doctors to communicate more effectively about a patient and use similar terminology when discussing them. In addition, they can then predict the outcome of the disorder and suggest related treatment to help the patient.
Scheff (1966) points out that diagnosis classification labels the individual, and this can have many adverse effects, such as a self-fulfilling prophecy (patients may begin to act how they are expected to act), and lower self-esteem.
Ethics – do the benefits of classification (care, treatment, safety) outweigh the costs (possible misdiagnosis, mistreatment, loss of rights and responsibility, prejudice due to labelling).
Reliability and Validity in Diagnosis and Classification of Schizophrenia
with reference to co-morbidity, culture and gender bias and symptom overlap.
Reliability
For the classification system to be reliable, differfent clinicians using the same system (e.g. DSM) should arrive at the same diagnosis for the same individual.
Reliability is the level of agreement on the diagnosis by different psychiatrists across time and cultures; stability of diagnosis over time given no change in symptoms.
Diagnosis of schizophrenia is difficult as the practitioner has no physical signs but only symptoms (what the patient reports) to make a decision on.
Jakobsen et al. (2005) tested the reliability of the ICD-10 classification system in diagnosing schizophrenia. A hundred Danish patients with a history of psychosis were assessed using operational criteria, and a concordance rate of 98% was obtained. This demonstrates the high reliability of the clinical diagnosis of schizophrenia using up-to-date classification.
Comorbidity describes people who suffer from two or more mental disorders. For example, schizophrenia and depression are often found together. This makes it more difficult to confidently diagnose schizophrenia. Comorbidity occurs because the symptoms of different disorders overlap. For example, major depression and schizophrenia both involve very low levels of motivation. This creates problems of reliability. Does the low motivation reflect depression or schizophrenia, or both?
Gender bias: Loring and Powell (1988) found that some behavior which was regarded as psychotic in males was not regarded as psychotic in females.
Validity – the extent to which schizophrenia is a unique syndrome with characteristics, signs and symptoms.
For the classification system to be valid it should be meaningful and classify a real pattern of symptoms, which result from a real underlying cause.
The validity of schizophrenia as a single disorder is questioned by many. This is a useful point to emphasise in any essay on the disorder. There is no such thing as a ‘normal’ schizophrenic exhibiting the usual symptoms.
Since their are problems with the validity of diagnois classification, unsuitable treatment may be administered, sometimes on an involuntary basis. This raises practical and ethical issues when selecting different types of tretment.
Problems of validity: Are we really testing what we think we are testing? In the USA only 20% of psychiatric patients were classed as having schizophrenia in the 1930s but this rose to 80% in the 1950s . In London the rate remained at 20%, suggesting neither group had a valid definition of schizophrenia.
Neuropsychologist Michael Foster Green suggests that neurocognitive deficits in basic functions such as memory, attention, central executive and problem solving skills may combine to have an outcome which we are labelling “Schizophrenia” as if it was the cause when in fact it is simply an umbrella term for a set of effects.
Predictive validity. If diagnosis leads to successful treatment, the diagnosis can be seen as valid. But in fact some Schizophrenics are successfully treated whereas others are not. Heather (1976) there is only a 50% chance of predicting what treatment a patient will receive based on diagnosis, suggesting that diagnosis is not valid.
Aetiological validity – for a diagnosis to be valid, all patients diagnosed as schizophrenic should have the same cause for their disorder. This is not the case with schizophrenia: The causes may be one of biological or psychological or both.
David Rosenhan (1973) famous experiment involving Pseudopatients led to 8 normal people being kept in hospital despite behaving normally. This suggests the doctors had no valid method for detecting schizophrenia. They assumed the bogus patients were schizophrenic with no real evidence. In a follow up study they rejected genuine patients whom they assumed were part of the deception.
Culture – One of the biggest controversies in relation to classification and diagnosis is to do with cultural relativism and variations in diagnosis. For example in some Asian countries people are not expected to show emotional expression, whereas in certain Arabic cultures public emotion is encouraged and understood. Without this knowledge a person displaying overt emotional behavior in a Western culture might be regarded as abnormal. Cochrane (1977) reported that the incidence of schizophrenia in the West Indies and the UK is 1 %, but that people of Afro-Caribbean origin are seven times more likely to be diagnosed as schizophrenic when living in the UK.
Cultural bias – African Americans and those of Afro-carribean descent are more likely to be diagnosed than their white counterparts but diagnostic rates in Africa and the West Indies is low – Western over diagnosis is a result of cultural norms and the diagnosis lacks validity.
Section 2: Biological Explanations for Schizophrenia
Family studies find individuals who have schizophrenia and determine whether their biological relatives are similarly affected more often than non-biological relatives.
There are two types of twins – identical (monozygotic) and fraternal (dizygotic). To form identical twins, one fertilised egg (ovum) splits and develops two babies with exactly the same genetic information.
• Gottesman (1991) found that MZ twins have a 48% risk of getting schizophrenia whereas DZ twins have a 17% risk rate. This is evidence that the higher the degree of genetic relativeness, the higher the risk of getting schizophrenia. • Benzel et al. (2007) three genes: COMT, DRD4, AKT1 – have all been associated with excess dopamine in specific D2 receptors, leading to acute episodes, positive symptoms which include delusions, hallucinations, strange attitudes. • Research by Miyakawa et al. (2003) studied DNA from human families affected by schizophrenia and found that those with the disease were more likely to have a defective version of a gene, called PPP3CC which is associated with the production of calcineurin which regulates the immune system. Also, research by Sherrington et al. (1988) has found a gene located on chromosome 5 which has been linked in a small number of extended families where they have the disorder. • Evidence suggests that the closer the biological relationship, the greater the risk of developing schizophrenia. Kendler (1985) has shown that first-degree relatives of those with schizophrenia are 18 times more at risk than the general population. Gottesman (1991) has found that schizophrenia is more common in the biological relatives of a schizophrenic, and that the closer the degree of genetic relatedness, the greater the risk.
Very important to note genetics are only partly responsible, otherwise identical twins would have 100% concordance rates.
One weakness of the genetic explanation of schizophrenia is that there are methodological problems. Family, twin and adoption studies must be considered cautiously because they are retrospective, and diagnosis may be biased by knowledge that other family members who may have been diagnosed. This suggests that there may be problems of demand characteristics.
A second weakness is the problem of nature-v-Nurture. It is very difficult to separate out the influence of nature-v-nurture. The fact that the concordance rates are not 100% means that schizophrenia cannot wholly be explained by genes and it could be that the individual has a pre-disposition to schizophrenia and simply makes the individual more at risk of developing the disorder. This suggests that the biological account cannot give a full explanation of the disorder.
A final weakness of the genetic explanation of schizophrenia is that it is biologically reductionist. The Genome Project has increased understanding of the complexity of the gene. Given that a much lower number of genes exist than anticipated, it is now recognised that genes have multiple functions and that many genes behavior.
Schizophrenia is a multi-factorial trait as it is the result of multiple genes and environmental factors. This suggests that the research into gene mapping is oversimplistic as schizophrenia is not due to a single gene.
The Dopamine Hypothesis
• Dopamine is a neurotransmitter. It is one of the chemicals in the brain which causes neurons to fire. The original dopamine hypothesis stated that schizophrenia suffered from an excessive amount of dopamine. This causes the neurons that use dopamine to fire too often and transmit too many messages. • High dopamine activity leads to acute episodes, and positive symptoms which include: delusions, hallucinations, confused thinking. • Evidence for this comes from that fact that amphetamines increase the amounts of dopamine . Large doses of amphetamine given to people with no history of psychological disorders produce behavior which is very similar to paranoid schizophrenia. Small doses given to people already suffering from schizophrenia tend to worsen their symptoms. • A second explanation developed, which suggests that it is not excessive dopamine but that fact that there are more dopamine receptors. More receptors lead to more firing and an over production of messages. Autopsies have found that there are generally a large number of dopamine receptors (Owen et al., 1987) and there was an increase in the amount of dopamine in the left amygdale (falkai et al. 1988) and increased dopamine in the caudate nucleus and putamen (Owen et al, 1978).
One criticism of the dopamine hypothesis is there is a problem with the chicken and egg. Is the raised dopamine levels the cause of the schizophrenia, or is it the raised dopamine level the result of schizophrenia?
It is not clear which comes first. This suggests that one needs to be careful when establishing cause and effect relationships in schizophrenic patients.
One of the biggest criticisms of the dopamine hypothesis came when Farde et al found no difference between schizophrenics’ levels of dopamine compared with ‘healthy’ individuals in 1990.
Noll (2009) also argues around one third of patients do not respond to drugs which block dopamine so other neurotransmitters may be involved.
A final weakness of the dopamine hypothesis is that it is biologically deterministic. The reason for this is because if the individual does have excessive amounts of dopamine then does it really mean that thy ey will develop schizophrenia? This suggests that the dopamine hypothesis does not account for freewill.
Neural Correlates
• Neural correlates are patterns of structure or activity in the brain that occur in conjunction with schizophrenia • People with schizophrenia have abnormally large ventricles in the brain . Ventricles are fluid filled cavities (i.e. holes) in the brain that supply nutrients and remove waste. This means that the brains of schizophrenics are lighter than normal. The ventricles of a person with schizophrenia are on average about 15% bigger than normal (Torrey, 2002).
A strength is that the research into enlarged ventricles and neurotransmitter levels have high reliability. The reason for this is because the research is carried out in highly controlled environments, which specialist, high tech equipment such as MRI and PET scans.
These machines take accurate readings of brain regions such as the frontal and pre-frontal cortex, the basil ganglia, the hippocampus and the amygdale. This suggests that if this research was tested and re-tested the same results would be achieved.
Supporting evidence for the brain structure explanation comes from further empirical support from Suddath et al. (1990). He used MRI (magnetic resonance imaging) to obtain pictures of the brain structure of MZ twins in which one twin was schizophrenic.
The schizophrenic twin generally had more enlarged ventricles and a reduced anterior hypothalamus. The differences were so large the schizophrenic twins could be easily identified from the brain images in 12 out of 15 pairs.
This suggests that there is wider academic credibility for enlarged ventricles determining the likelihood of schizophrenia developing.
A second weakness of the neuroanatomical explanations is that it is biologically deterministic. The reason for this is because if the individual does have large ventricles then does it really mean that they will develop schizophrenia? This suggests that the dopamine hypothesis does not account for freewill.
Section 3: Psychological Explanations for Schizophrenia
Family dysfunction.
Family Dysfunction refers to any forms of abnormal processes within a family such as conflict, communication problems, cold parenting, criticism, control and high levels of expressed emotions. These may be risk factors for the development and maintenance of schizophrenia.
• Laing and others rejected the medical / biological explanation of mental disorders. They did not believe that schizophrenia was a disease. They believed that schizophrenia was a result of social pressures from life. Laing believed that schizophrenia was a result of the interactions between people, especially in families. • Bateson et al. (1956) suggested the double bind theory, which suggests that children who frequently receive contradictory messages from their parents are more likely to develop schizophrenia. For example parents who say they care whilst appearing critical or who express love whilst appearing angry. They did not believe that schizophrenia was a disease. They believed that schizophrenia was a result of social pressures from life. • Prolonged exposure to such interactions prevents the development of an internally coherent construction of reality; in the long run, this manifests itself as typically schizophrenic symptoms such as flattening affect, delusions and hallucinations, incoherent thinking and speaking, and in some cases paranoia. • Another family variable associated with schizophrenia is a negative emotional climate, or more generally a high degree of expressed emotion (EE). EE is a family communication style that involves criticism, hostility and emotional over-involvement. The researchers concluded that this is more important in maintaining schizophrenia than in causing it in the first place, (Brown et al 1958). Schizophrenics returning to such a family were more likely to relapse into the disorder than those returning to a family low in EE. The rate of relapse was particularly high if returning to a high EE family was coupled with no medication.
One strength of the double bind explanation comes from further empirical support provided by Berger (1965). They found that schizophrenics reported a higher recall of double bind statements by their mothers than non-schizophrenics.
However, evidence may not be reliable as patient’s recall may be affected by their schizophrenia. This suggests that there is wider academic credibility for the idea of contradictory messages causing schizophrenia.
A second strength of the research into expressed emotion (EE) is that it has practical applications. For example Hogarty (1991) produced a type of therapy session, which reduced social conflicts between parents and their children which reduced EE and thus relapse rates.
This suggests that gaining an insight into family relationships allows psychiatric professionals to help improve the quality of patient’s lives.
Individual differences – EE is associated with relapse but not all patients who live in high EE families relapse and not all patients in low EE families avoid relapse – Family dysfunction is an incomplete explanation for schizophrenia.
A weakness of the family relationsships appraoch is that there is a problem of cause and effect. Mischler & Waxler (1968) found significant differences in the way mothers spoke to their schizophrenic daughters compared to their normal daughters, which suggests that dysfunctional communication may be a result of living with the schizophrenic rather than the cause of the disorder.
This suggests that there is a problem of the chicken and egg scenario in relation to expressed emotion causing schizophrenia.
A second weakness of the double bind theory is that there are ethical issues. There are serious ethical concerns in blaming the family, particularly as there is little evidence upon which to base this.
Gender bias is also an issue as the mother tends to be blamed the most, which means such research is highly socially sensitive. This suggests that the research therefore does not protect individuals from harm.
Cause and effect – It remains unclear whether cognitive factors cause schizophrenia or if schizophrenia causes these cognitions – Family dysfunction may not be a valid explanation for schizophrenia.
Cognitive explanations
including dysfunctional thought processing.
Cognitive approaches examine how people think, how they process information. Researchers have focused on two factors which appear to be related to some of the experiences and behaviors of people diagnosed with schizophrenia.
First, cognitive deficits which are impairments in thought processes such as perception, memory and attention. Second, cognitive biases are present when people notice, pay attention to, or remember certain types of information better than other.
Cognitive Deficits
• There is evidence that people diagnosed as schizophrenic have difficulties in processing various types of information, for example visual and auditory information. Research indicates their attention skills may be deficient – they often appear easily distracted. • A number of researchers have suggested that difficulties in understanding other people’s behavior might explain some of the experiences of those diagnosed as schizophrenic. Social behavior depends, in part, on using other people’s actions as clues for understanding what they might be thinking. Some people who have been diagnosed as schizophrenic appear to have difficulties with this skill. • Cognitive deficits have been suggested as possible explanations for a range of behaviors associated with schizophrenia. These include reduced levels of emotional expression, disorganised speech and delusions.
Cognitive Biases
• Cognitive biases refer to selective attention. The idea of cognitive biases has been used to explain some of the behaviors which have been traditionally regarded as ‘symptoms’ of ‘schizophrenia’. • Delusions: The most common delusion that people diagnosed with schizophrenia report is that others are trying to harm or kill them – delusions of persecution. Research suggests that these delusions are associated with specific biases in reasoning about and explaining social situations. Many people who experience feelings of persecution have a general tendency to assume that other people cause the things that go wrong with their lives.
A strength of the cognitive explanation is that it has practical applications. Yellowless et al. (2002) developed a machine that produced virtual hallucinations, such as hearing the television telling you to kill yourself or one person’s face morphing into another’s.
The intention is to show schizophrenics that their hallucinations are not real. This suggests that understanding the effects of cognitive deficits allows psychologists to create new initiatives for schizophrenics and improve the quality of their lives.
A final strength is that it takes on board the nurture approach to the development of schizophrenia. For example, it suggests that schizophrenic behavior is the cause of environmental factors such as cognitive factors.
One weakness of the cognitive explanation is that there are problems with cause and effect. Cognitive approaches do not explain the causes of cognitive deficits – where they come from in the first place.
Is it the cognitive deficits which causes the schizophrenic behavior or is the schizophrenia that causes the cognitive deficits? This suggests that there are problems with the chicken and egg problem.
A second weakness of the cognitive model is that it is reductionist. The reason for this is because the approach does not consider other factors such as genes.
It could be that the problems caused by low neurotransmitters creates the cognitive deficits. This suggests that the cognitive approach is oversimplistic when consider the explanation of schizophrenia.
Section 4: Drug Therapy: typical and atypical antipsychotics
Drug therapy is a biological treatment for schizophrenia. Antipsychotic drugs are used to reduce the intensity of symptoms (particularly positive symptoms).
Typical Antipsychotics
• First generation Antipsychotics are called “Typical Antipsychotics” Eg. Chlorpromazine and Haloperidol. • Typical antipsychotic drugs are used to reduce the intensity of positive symptoms, blocking dopamine receptors in the synapses of the brain and thus reducing the action of dopamine. • They arrest dopamine production by blocking the D2 receptors in synapses that absorb dopamine, in the mesolimbic pathway thus reducing positive symptoms, such as auditory hallucinations. • But they tended to block ALL types of dopamine activity, (in other parts of the brain as well) and this caused side effects and may have been harmful.
Atypical Antipsychotics
• Newer drugs, called “atypical antipsychotics” attempt to target D2 dopamine activity in the limbic system but not D3 receptors in other parts of the brain. • Atypical antipsychotics such as Clozapine bind to dopamine, serotonin and glutamate receptors. • Atypical antipsychotic drugs work on negative symptoms, improving mood, cognitive functions and reducing depression and anxiety. • They also have some effect on other neurotransmitters such as serotonin . They generally have fewer side effects eg. less effect on movement Eg. Clozapine, Olazapine and Risperidone.
Since the mid-1950s antipsychotic medications have greatly improved treatment. Medications reduce positive symptoms particularly hallucinations and delusions; and usually allow the patient to function more effectively and appropriately.
Antipsychotic drugs are highly effective as they are relatively cheap to produce, easy to administer and have a positive effect on many sufferers. However they do not “cure” schizophrenia, rather they dampen symptoms down so that patients can live fairly normal lives in the community.
Kahn et al. (2008) found that antipsychotics are generally effective for at least one year, but second- generation drugs were no more effective than first-generation ones.
Some sufferers only take a course of antipsychotics once, while others have to take a regular dose in order to prevent symptoms from reappearing.
There is a sizeable minority who do not respond to drug treatment. Pills are not as helpful with other symptoms, especially emotional problems.
Older antipsychotics like haloperidol or chlorpromazine may produce side effects Sometimes when people with schizophrenia become depressed, so it is common to prescribe anti-depressants at the same time as the anti-psychotics.
All patients are in danger of relapsing but without medication the relapses are more common and more severe which suggests the drugs are effective.
Clozapine targets multiple neurotransmitters, not just dopamine, and has been shown to be more effective than other antipsychotics, although the possibility of severe side effects – in particular, loss of the white blood cells that fight infection.
Even newer antipsychotic drugs, such as risperidone and olanzapine are safer, and they also may be better tolerated. They may or may not treat the illness as well as clozapine, however.
Meta–analysis by Crossley Et Al (2010) suggested that Atypical antipsychotics are no more effective, but do have less side effects.
Recovery may be due to psychological factors – The placebo effect is when patients’ symptoms are reduced because they believe that it should.
However, Thornley et al carried out a meta-analysis comparing the effects of Chlorpromazine to placebo conditions and found Chlorpromazine to be associated with better overall functioning – Drug therapy is an effective treatment for SZ.
RWA – Offering drugs can lead to an enhanced quality of life as patients are given independence – Positive impact on the economy as patients can return to work and no longer need to be provided with institutional care.
Ethical issues – Antipsychotics have been used in hospitals to calm patients and make them easier for staff to work with rather than for the patients’ benefit – Can lead to the abuse of the Human Rights Act (no one should be subject to degrading treatment).
Severe side effects – Long term use can result in tardive dyskinesia which manifests as involuntary facial movements such as blinking and lip smacking – While they may be effective, the severity of the side effects mean the costs outweigh the benefits therefore they are not an appropriate treatment.
In most cases the original “typical antipsychotics” have more side effects, so if the exam paper asks for two biological therapies you can write about typical anti-psychotics and emphasise the side effects, then you can write about the atypical antipsychotics and give them credit for having less side effects.
Section 5: Psychological Therapies for Schizophrenia
Family therapy.
Family therapy is a form of therapy carried out with members of the family with the aim of improving their communication and reducing the stress of living as a family.
Family Therapy aims to reduce levels of expressed emotion, and reduced the likelihood of relapse.
Aims of Family Therapy
• To educate relatives about schizophrenia. • To stabilize the social authority of the doctor and the family. • To improve how the family communicated and handled the situation. • To teach patients and carers more effective stress management techniques.
Methods used in Family Therapy
• Pharoah identified examples of how family therapy works: It helps family members achieve a balance between caring for the individual and maintaining their own lives, it reduces anger and guilt, it improves their ability to anticipate and solve problems and forms a therapeutic alliance. • Families taught to have weekly family meetings solving problems on family and individual goals, resolve conflict between members, and pinpoint stressors. • Preliminary analysis: Through interviews and observation the therapist identifies strengths and weaknesses of family members and identifies problem behaviors. • Information transfer – teaching the patient and the family the actual facts about the illness, it’s causes, the influence of drug abuse, and the effect of stress and guilt. • Communication skills training – teach family to listen, to express emotions and to discuss things. Additional communication skills are taught, such as “compromise and negotiation,” and “requesting a time out” . This is mainly aimed at lowering expressed emotion.
A study by Anderson et al. (1991) found a relapse rate of almost 40% when patients had drugs only, compared to only 20 % when Family Therapy or Social Skills training were used and the relapse rate was less than 5% when both were used together with the medication.
Pharaoh et al. (2003) meta – analysis found family interventions help the patient to understand their illness and to live with it, developing emotional strength and coping skills, thus reducing rates of relapse.
Pharoah identified examples of how family therapy works: It helps family members achieve a balance between caring for the individual and maintaining their own lives, it reduces anger and guilt, it improves their ability to anticipate and solve problems and forms a therapeutic alliance.
Economic Benefits: Family therapy is highly cost effective because it reduces relapse rates, so the patients are less likely to take up hospital beds and resources. The NICE review of family therapy studies demonstrated that it was associated with significant cost savings when offered to patients alongside the standard care – Relapse rates are also lower which suggests the savings could be even higher.
Lobban (2013) reports that other family members felt they were able to cope better thanks to family therapy. In more extreme cases the patient might be unable to cope with the pressures of having to discuss their ideas and feelings and could become stressed by the therapy, or over-fixated with the details of their illness.
Token Economy
• Token economies aim to manage schizophrenia rather than treat it. • They are a form of behavioral therapy where desirable behaviors are encouraged by the use of selective reinforcement and is based on operant conditioning. • When desired behavior is displayed eg. Getting dressed, tokens (in the form of coloured discs) are given immediately as secondary reinforcers which can be exchanged for rewards eg. Sweets and cigarettes. • This manages schizophrenia because it maintains desirable behavior and no longer reinforces undesirable behavior. • The focus of a token economy is on shaping and positively reinforcing desired behaviors and NOT on punishing undesirable behaviors. The technique alleviates negative symptoms such as poor motivation, and nurses subsequently view patients more positively, which raises staff morale and has beneficial outcomes for patients. • It can also reduce positive symptoms by not rewarding them, but rewarding desirable behavior instead. Desirable behavior includes self-care, taking medication, work skills, and treatment participation.
Paul and Lentz (1977) Token economy led to better overall patient functioning and less behavioral disturbance, More cost-effective (lower hospital costs)
Upper and Newton (1971) found that the weight gain associated with taking antipsychotics was addressed with token economy regimes. Chronic schizophrenics achieved 3lbs of weight loss a week.
McMonagle and Sultana (2000) reviewed token economy regimes over a 15-year period, finding that they did reduce negative symptoms, though it was unclear if behavioral changes were maintained beyond the treatment programme.
It is difficult to keep this treatment going once the patients are back at home in the community. Kazdin et al. Found that changes in behavior achieved through token economies do not remain when tokens are with¬drawn, suggesting that such treatments address effects of schizophrenia rather than causes. It is not a cure.
There have also been ethical concerns as such a process is seen to be dehumanising, subjecting the patient to a regime which takes away their right to make choices.
In the 1950s and 60s nurses often “rewarded” patients with cigarettes. Due to the pivotal role of dopamine in schizophrenia this led to a culture of heavy smoking an nicotine addiction in psychiatric hospitals of the era.
Ethical issues – Severely ill patients can’t get privileges because they are less able to comply with desirable behaviors than moderately ill patients – They may suffer from discrimination
Cognitive Behavioral Therapy
In CBT, patients may be taught to recognise examples of dysfunctional or delusional thinking, then may receive help on how to avoid acting on these thoughts. This will not get rid of the symptoms of schizophrenia but it can make patients better able to cope with them.
Central idea: Patients problems are based on incorrect beliefs and expectations. CBT aims to identify and alter irrational thinking including regarding:
- General beliefs.
- Self image.
- Beliefs about what others think.
- Expectations of how others will act.
- Methods of coping with problems.
In theory, when the misunderstandings have been swept away, emotional attitudes will also improve.
Assessment : The therapist encourages the patient to explain their concerns.
• describing delusions • reflecting on relationships • laying out what they hope to achieve through the therapy.
Engagement :
The therapist wins the trust of the patient, so they can work together. This requires honesty, patience and unconditional acceptance. The therapist needs to accept that the illusions may seem real to the patient at the time and should be dealt with accordingly.
ABC : Get the patients to understand what is really happening in their life:
A: Antecedent – what is triggering your problem ? B: behavior – how do you react in these situations ? C: Consequences – what impact does that have on your relationships with others?
Normalisation :
Help the patient realise it is normal to have negative thoughts in certain situations. Therefore there is no need to feel stressed or ashamed about them.
Critical Collaborative Analysis :
Carrying on a logical discussion till the patient begins to see where their ideas are going wrong and why they developed. Work out ways to recognise negative thoughts and test faulty beliefs when they arise, and then challenge and re-think them.
Developing Alternative Explanations :
Helping the patient to find logical reasons for the things which trouble them Let the patient develop their own alternatives to their previous maladaptive behavior by looking at coping strategies and alternative explanations.
Another form of CBT: Coping Strategy Enhancement (CSE)
• Tarrier (1987) used detailed interview techniques, and found that people with schizophrenia can often identify triggers to the onset of their psychotic symptoms, and then develop their own methods of coping with the distress caused. These might include things as simple as turning up the TV to drown out the voices they were hearing! • At least 73% of his sample reported that these strategies were successful in managing their symptoms. • CSE aims to teach individuals to develop and apply effective coping strategies which will reduce the frequency, intensity and duration of psychotic symptoms and alleviate the accompanying distress. There are two components: 1. Education and rapport training: therapist and client work together to improve the effectiveness of the client’s own coping strategies and develop new ones. 2. Symptom targeting: a specific symptom is selected for which a particular coping strategy can be devised Strategies are practised within a session and the client is helped through any problems in applying it. They are then given homework tasks to practice, and keep a record of how it worked.
CBT does seem to reduce relapses and readmissions to hospital (NICE 2014). However, the fact that these people were on medication and having regular meetings with doctors would be expected to have that effect anyway.
Turkington et al. (2006) CBT is highly effective and should be used as a mainstream treatment for schizophrenia wherever possible.
Tarrier (2005) reviewed trials of CBT, finding evidence of reduced symptoms, especially positive ones, and lower relapse rates.
Requires self-awareness and willingness to engage – Held back by the symptoms schizophrenics encounter – It is an ineffective treatment likely to lead to disengagement.
Lengthy – It takes months compared to drug therapy that takes weeks which leads to disengaged treatment as they don’t see immediate effects – A patient who is very distressed and perhaps suicidal may benefit better in the short term from antipsychotics.
Addington and Addington (2005) claim that CBT is of little use in the early stages of an acute schizophrenic episode, but perhaps more useful when the patient is more calm and beginning to worry about how life will be after they recover. In other words, it doesn’t cure schizophrenia, it just helps people get over it.
Research in Hampshire, by Kingdon and Kirschen (2006) found that CBT is not suitable for all patients, especially those who are too thought disorientated or agitated, who refuse medication, or who are too paranoid to form trusting alliances with practitioners.
As there is strong evidence that relapse is related to stress and expressed emotion within the family, it seems likely that CBT should be employed alongside family therapy in order to reduce the pressures on the individual patient.
Section 6: Interactionist Approach
The Interactionist approach acknowledges that there are a range of factors (including biological and psychological) which are involved in the development of schizophrenia.
The Diathesis-stress Model
• The diathesis-stress model states that both a vulnerability to SZ and a stress trigger are necessary to develop the condition. • Zubin and Spring suggest that a person may be born with a predisposition towards schizophrenia which is then triggered by stress in everyday life. But if they have a supportive environment and/or good coping skills the illness may not develop. • Concordance rates are never 100% which suggests that environmental factors must also play a role in the development of SZ. MZ twins may have the same genetic vulnerability but can be triggered by different stressors. • Tienari Et. A. (2004): Adopted children from families with schizophrenia had more chance of developing the illness than children from normal families. This supports a genetic link. However, those children from families schizophrenia were less likely to develop the illness if placed in a “good” family with kind relationships, empathy, security, etc. So environment does play a part in triggering the illness.
Holistic – Identifies that patients have different triggers, genes etc. – Patients can receive different treatments for their SZ which will be more effective.
Falloon et al (1996) stress – such as divorce or bereavement, causes the brain to be flooded with neurotransmitters which brings on the acute episode.
Brown and Birley (1968) 50% people who had an acute schizophrenic episode had experienced a major life event in 3 weeks prior.
Substance abuse: Amphetamine and Cannabis and other drugs have also been identified as triggers as they affect serotonin and glutamate levels.
Vasos (2012) Found the risk of schizophrenia was 2.37 times greater in cities than it was in the countryside, probably due to stress levels. Hickling (1999) the stress of urban living made African-Carribean immigrants in Britain 8 to 10 times more likely to experience schizophrenia.
Faris and Dunham (1939) found clear pattern of correlation between inner city environments and levels of psychosis. Pederson and Mortensen (Denmark 2001) found Scandanavian villages have very LOW levels of psychosis, but 15 years of living in a city increased risk.
Fox (1990): It is more likely that factors associated with living in poorer conditions (e.g. stress) may trigger the onset of schizophrenia, rather than individuals with schizophrenia moving down in social status.
Bentall’s meta-analysis (2012) shows that stress arising from abuse in childhood increases the risk of developing schizophrenia.
Toyokawa, Et. Al (2011) suggest many aspects of urban living – ranging from life stressors to the use of drugs, can have an effect on human epigenetics. So the stressors of modern living could cause increased schizophrenia in future generations.

One Way the Brain Gets Flooded With Too Much Dopamine
Genetic mechanisms may disrupt how the caudate nucleus regulates dopamine flow..
Posted November 4, 2022 | Reviewed by Ekua Hagan
- What Is Dopamine?
- Find counselling near me
- The dopamine hypothesis of schizophrenia (SCZ) posits that having too much dopamine in the brain causes SCZ symptoms such as psychosis.
- New post-mortem research on hundreds of human brains identifies a causative link between schizophrenia and unregulated dopamine flow.
- In patients with schizophrenia, gene expression in the striatum's caudate nucleus disrupts D2-autoreceptors' ability to regulate dopamine flow.
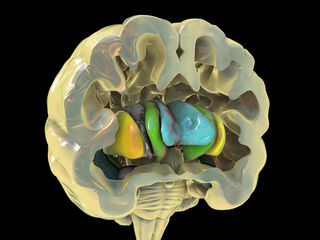
Since the 1950s, scientists have been trying to figure out why having too much dopamine in the brain is associated with schizophrenia. The dopamine hypothesis of schizophrenia posits that in people with this brain illness, the flow of dopamine along various pathways becomes dysregulated in ways that flood the brain with excessive amounts of this neurotransmitter.
It's well-established that dopamine pathways are involved in the pathophysiology of schizophrenia and psychosis . However, researchers are still trying to figure out exactly how and why dopamine pathways get flooded with too much dopamine.
D2-Autoreceptors Slow the Flow of Dopamine Along Specific Pathways
There are four major dopamine pathways in the human brain. Of these four dopaminergic pathways, the nigrostriatal and mesolimbic dopamine systems—which play a key role in reward-seeking behavior, motivation , motor control, and addiction —flow through the caudate nucleus region of the basal ganglia's striatum.
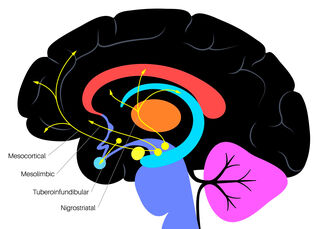
The regulation of striatal dopamine release in the caudate nucleus is controlled by a subset of inhibitory dopamine receptors called D2-autoreceptors . When these autoreceptors function properly, they maintain a "Goldilocks zone" of just enough dopamine but not too much.
In healthy individuals not experiencing schizophrenic or psychotic symptoms, these presynaptic autoreceptors act like gatekeepers that slow the flow of dopamine. But if autoreceptors are compromised and can't inhibit the amount of dopamine released from presynaptic dopaminergic neurons, the brain gets flooded with too much dopamine.
Ideally, autoreceptors in the caudate nucleus inhibit dopamine flow in ways that help maintain a dynamic equilibrium between its release and reuptake via dopaminergic pathways that travel to other parts of the brain. Antipsychotic medications turbocharge the ability of autoreceptors to inhibit the synthesis and release of dopamine, which prevents it from flooding the brain.
The molecular mechanisms that facilitate the inhibition of dopamine release by D2-autoreceptors and precisely how antipsychotics bolster autoreceptors' ability to regulate dopamine flow aren't fully understood. However, pioneering post-mortem brain research sheds light on how genetic mechanisms may alter the ability of autoreceptors in the caudate nucleus to slow dopamine's flow.
A Vexing Riddle: What's the Link Between Dopamine and Schizophrenia?
A new study ( Benjamin et al., 2022 ) on the dopamine hypothesis of schizophrenia by researchers at the Lieber Institute for Brain Development (LIBD) gives us fresh clues about how gene expression in the caudate nucleus may affect autoreceptors' ability to inhibit the flow of dopamine in people with schizophrenia.
The findings of this recent post-mortem analysis of the genetic and transcriptional landscape of the striatum's caudate nucleus in 443 people (245 neurotypical individuals, 154 with schizophrenia, 44 with bipolar disorder ) were published on November 1 in the peer-reviewed journal Nature Neuroscience .
"Most studies of gene expression in the brains of individuals with schizophrenia have focused on cortical regions, but subcortical nuclei such as the striatum are prominently implicated in the disease, and current antipsychotic drugs target the striatum's dense dopaminergic innervation," the authors explain. The researchers note that they "identified many genes associated with schizophrenia risk" and found that antipsychotic medications have an "extensive influence on caudate gene expression."

The LIBD researchers identified specific genetic mechanisms that disrupt D2-autoreceptors' ability to regulate dopamine flow in individuals with schizophrenia. "If autoreceptors are compromised, the flow of dopamine within the brain is poorly controlled, and too much dopamine flows for too long," Benjamin et al. explain.
"Until now, scientists have been unable to decipher whether the dopamine link was a causative factor or solely a way to treat schizophrenia," senior author Daniel Weinberger said in a November 2022 news release . "We have the first evidence that dopamine is a causative factor in schizophrenia."
"One of the major side effects of the drugs used to treat schizophrenia is lack of pleasure and joy," co-author Jennifer Erwin added. "In theory, if we could target the dopamine receptor specifically with drugs, that could be a new strategy for treatment that would not limit a patient's joy as much."
In 1976 , Solomon Snyder, a neuroscientist from Johns Hopkins University School of Medicine, unearthed how antipsychotic drugs help patients with schizophrenia by reducing dopamine levels in the brain. In a November 2022 statement, Snyder, who wasn't involved in Benjamin et al.'s recent study, hailed the latest LIBD findings as a "breakthrough many decades in the making."
"For decades, people have debated the dopamine connection to schizophrenia," Snyder said. "They used to say, 'Well, this is interesting to speculate about, but there's no solid evidence.' But now that we have much more rigorous data available, we keep coming back to the same story. You don't have to call it a hypothesis anymore."
Autoreceptors in the Caudate Nucleus Could Be a New Therapeutic Target
The latest (2022) study by Benjamin et al. provides fresh insights into genetic mechanisms that disrupt the ability of D2-autoreceptors in the caudate nucleus to inhibit the flow of dopamine. Identifying these autoreceptors' vital role in preventing the brain from getting flooded with too much dopamine could lead to new psychopharmacology targets in the caudate nucleus.
Kynon J. M. Benjamin, Qiang Chen, Andrew E. Jaffe, Joshua M. Stolz, Leonardo Collado-Torres, Louise A. Huuki-Myers, Emily E. Burke, Ria Arora, Arthur S. Feltrin, André Rocha Barbosa, Eugenia Radulescu, Giulio Pergola, Joo Heon Shin, William S. Ulrich, Amy Deep-Soboslay, Ran Tao, the BrainSeq Consortium, Thomas M. Hyde, Joel E. Kleinman, Jennifer A. Erwin, Daniel R. Weinberger & Apuã C. M. Paquola. "Analysis of the Caudate Nucleus Transcriptome in Individuals With Schizophrenia Highlights Effects of Antipsychotics and New Risk Genes." Nature Neuroscience (First published: November 01, 2022) DOI: 10.1038/s41593-022-01182-7
Christopher P. Ford. "The Role of D2-Autoreceptors in Regulating Dopamine Neuron Activity and Transmission." Neuroscience (First published: January 23, 2014) DOI: 10.1016/j.neuroscience.2014.01.025
Ian Creese, David R. Burtand, Solomon H. Snyder. "Dopamine Receptor Binding Predicts Clinical and Pharmacological Potencies of Antischizophrenic Drugs." Science (First published: April 30, 1976) DOI: 10.1126/science.3854

Christopher Bergland is a retired ultra-endurance athlete turned science writer, public health advocate, and promoter of cerebellum ("little brain") optimization.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

Sticking up for yourself is no easy task. But there are concrete skills you can use to hone your assertiveness and advocate for yourself.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
psychologyrocks
The dopamine hypothesis.
Excess dopamine: hyperdopaminergia

Two explanations gained favour; firstly that low levels beta hydroxylase, the enzyme which breaks down dopamine, may be responsible for a buildup of excess dopamine in the synapse and secondly that a proliferation of D2 dopamine receptors on the post-synaptic cells may be responsible for hyperdopaminergic activity.
Dopamine deficiency: hypodopaminergia

In 1991, Kenneth Davis suggested that positive symptoms of schizophrenia (e.g. delusions and hallucinations) may result from excess of dopaminergic activity in a region called the called meso-limbic pathway whereas the negative symptoms (e.g. flat affect and mutism) may result from hypodopaminergia , meaning a lack of dopaminergic activity in the meso-cortical pathway , (see image below).
Moving on from the dopamine hypothesis…
Serotonin and negative symptoms

Back to dopamine again!
Version 3 of the dopamine hypothesis
Oliver Howes and Shitij Kapur (2009) describe ‘ dopamine dysregulation ’ in the striatum as the common pathway to psychosis . These researchers have also suggested that attention be turned to presynaptic dopamine levels as opposed to irregularities of D2 receptors. They also focus on interactions between genetic, environmental and socio-cultural factors and believe that the dopamine hypothesis should be softened and viewed as an explanation of “psychosis proneness” not an explanation of schizophrenia.
Share this:

- Already have a WordPress.com account? Log in now.
- Subscribe Subscribed
- Copy shortlink
- Report this content
- View post in Reader
- Manage subscriptions
- Collapse this bar
- Search Menu
Sign in through your institution
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Numismatics
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Papyrology
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Social History
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Evolution
- Language Reference
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Media
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Legal System - Costs and Funding
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Restitution
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business Ethics
- Business History
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Social Issues in Business and Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic History
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Management of Land and Natural Resources (Social Science)
- Natural Disasters (Environment)
- Pollution and Threats to the Environment (Social Science)
- Social Impact of Environmental Issues (Social Science)
- Sustainability
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- Ethnic Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Behaviour
- Political Economy
- Political Institutions
- Political Theory
- Politics and Law
- Politics of Development
- Public Administration
- Public Policy
- Qualitative Political Methodology
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Disability Studies
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >

33 The Cultural Psychology of Social Cognition
Shinobu Kitayama, Professor, University of Michigan
Martha K. Berg, PhD Student, University of Michigan
- Published: 21 August 2024
- Cite Icon Cite
- Permissions Icon Permissions
How does culture influence social cognition? This chapter takes stock of the progress in this research field over the past two decades. The cumulative evidence suggests the cultural environment has two significant influences. First, this environment affects the frequency or saliency of various stimuli and representations which affects the fluency of processing such stimuli and representations. Second, the environment is also organized by cultural models, including independent or interdependent selves, which influence social cognition. The chapter next turns to the issue of cultural acquisition, proposing that the mechanism of cultural acquisition is an integral part of each person’s effort to establish an individual identity. This effort involves sampling select elements of culture and weaving them into a unified profile. Individual profiles may appear random when examined cross-sectionally, however it may show longitudinal stability. The chapter concludes by pointing to some critical directions for future research.
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
- Add your ORCID iD
Institutional access
Sign in with a library card.
- Sign in with username/password
- Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

IMAGES
COMMENTS
Dopamine is a neurotransmitter that serves as a chemical messenger in the brain. It can function as both an excitatory and inhibitory neurotransmitter, leading to diverse effects on the brain, body, and behavior. Dopamine is transferred between neurons in the brain through a process called synaptic transmission, where dopamine molecules are ...
Dopamine. Dopamine is known as the feel-good neurotransmitter—a chemical that ferries information between neurons. The brain releases it when we eat food that we crave or while we have sex ...
Dopamine hypothesis. The dopamine hypothesis of ADHD is based on the facts: (1) that symptoms of ADHD are reduced by stimulant treatment which blocks the dopamine reuptake mechanism in the striatum; and (2) that some patients with ADHD have abnormalities in genes responsible for dopamine regulation. However, this hypothesis has been questioned.
APA Dictionary of Psychology. Search Button. dopamine hypothesis. Share button. Updated on 04/19/2018. the influential theory that schizophrenia is caused by an excess of dopamine in the brain, due either to an overproduction of dopamine or a deficiency of the enzyme needed to convert dopamine to norepinephrine (adrenaline). There is some ...
dopamine (DA) n. a catecholamine neurotransmitter that has an important role in motor behavior and is implicated in numerous mental conditions and emotional states (see catecholamine hypothesis; dopamine hypothesis ). It is found in dopaminergic neurons in the brain and elsewhere. It is synthesized from the dietary amino acid tyrosine, which in ...
The dopamine hypothesis is the oldest neurochemical theory of the pathophysiology of psychosis. Established in the last century based on clinical observations, the theory received considerable scientific attention in past decades. ... SCH23390, a later work by Knable and co-workers (1994) failed to define differences in striatal D 2 and D 1 ...
The dopamine hypothesis of how antipsychotic drugs exert their beneficial effect in psychotic illness has an interesting history that dates back to 1950. This hypothesis is not to be confused with the dopamine hypothesis of schizophrenia; the aim of the latter is to explain the etiology of schizophrenia. The present review does not deal with ...
Psychology Definition of DOPAMINE HYPOTHESIS: The theory that schizophrenia is caused by an excess of dopamine in the brain. See glutamate hypothesis.
AP Psychology; Dopamine Hypothesis; Dopamine Hypothesis. Definition. The dopamine hypothesis is a theory that suggests an excess of dopamine activity in certain brain areas is associated with the development and symptoms of schizophrenia. It proposes that abnormal levels of dopamine neurotransmitters contribute to the occurrence of this mental ...
The Dopamine (DA) Hypothesis proposes that imbalances in the neurotransmitter dopamine are responsible for the development and symptoms of certain psychiatric conditions…
The Dopamine Hypothesis has been a prominent area of study in the field of neuroscience for several decades. It is the idea that the neurotransmitter dopamine plays a central role in the pathology of schizophrenia. This hypothesis was first proposed by Carlsson and Lindqvist in 1963, and since then it has been the subject of much research and ...
Dopamine Hypothesis. This theory suggests that an imbalance of dopamine is responsible for schizophrenic symptoms. In other words, dopamine plays a role in controlling our sense of reality, and too much or too little can cause delusions and hallucinations. The evidence for this theory comes from many sources, including post-mortem studies that ...
Dopamine (DA) Hypothesis. The dopamine (DA) hypothesis is a theory that proposes a biological cause of schizophrenia. This is the oldest theory about the cause of schizophrenia and was first presented in the 1960s. It suggests that schizophrenia is caused by too much DA transmission in the brain.
The hypothesis that dopamine reports reward prediction errors has been both influential and controversial. This Perspective characterizes the present state of evidence, indicating where it ...
The dopamine hypothesis of schizophrenia postulates that an excess of dopamine subcortically is associated with the positive symptoms. At the same time, the negative and cognitive symptoms of schizophrenia are thought to arise from a deficit of dopamine in the cortex. Evidence for the co-existence of subcortical dopamine excess and cortical ...
The dopamine hypothesis has been the cornerstone in the research and clinical practice of schizophrenia. With the initial emphasis on the role of excessive dopamine, the hypothesis has evolved to a concept of combining prefrontal hypodopaminergia and striatal hyperdopaminergia, and subsequently to the present aberrant salience hypothesis. This article provides a brief overview of the ...
The dopamine hypothesis in schizophrenia was based primarily on observational results in its introduction. Since then, numerous studies pointing at a definite link between dopamine changes and ...
The D opamine Hypothesis of Schizophrenia: Definition. The dopamine hypothesis, first proposed by Van Rossum in 1967, is the theory that too much dopamine in the subcortical and limbic regions of the brain may cause positive schizophrenic symptoms.According to the dopamine hypothesis, negative symptoms are associated with less dopamine in the prefrontal cortex.
The dopamine hypothesis has been the cornerstone in the research and clinical practice of schizophrenia. With the initial emphasis on the role of excessive dopamine, the hypothesis has evolved to a concept of combining prefrontal hypodopaminergia and striatal hyperdopaminergia, and subsequently to the present aberrant salience hypothesis.
The original dopamine hypothesis stated that schizophrenia suffered from an excessive amount of dopamine. This causes the neurons that use dopamine to fire too often and transmit too many messages. • High dopamine activity leads to acute episodes, and positive symptoms which include: delusions, hallucinations, confused thinking.
The dopamine hypothesis of schizophrenia (SCZ) posits that having too much dopamine in the brain causes SCZ symptoms such as psychosis. New post-mortem research on hundreds of human brains ...
The dopamine hypothesis. In the 1950s two drugs called chlorpromazine and reserpine were found to be helpful in alleviating the symptoms of schizophrenia however, both drugs also induced tremors and muscle rigidity. These side-effects are symptomatic of Parkinson's disease, a condition caused by low levels of dopamine.
Kitayama, Shinobu, and Martha K. Berg, 'The Cultural Psychology of Social Cognition', in Donal E. Carlston, Kurt Hugenberg, ... a more productive and valid hypothesis that psychological processes, including various forms of cognition, are universally available to all humans. But the hallmark of these processes is malleability and plasticity in ...