Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals

Multiple sclerosis articles from across Nature Portfolio
Multiple sclerosis is an autoimmune disease in which immune cells attack and destroy the protective myelin sheaths that surround nerve fibres, leading to neurological disturbances.
Latest Research and Reviews

Spin-lock based fast whole-brain 3D macromolecular proton fraction mapping of relapsing–remitting multiple sclerosis
- Zongyou Cai
- Tiffany Y. So
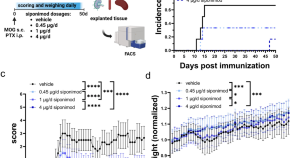
Siponimod treatment response shows partial BDNF dependency in multiple sclerosis models
- Hasan Hüseyin Hendek
- Alina Blusch
- Simon Faissner
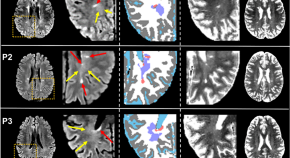
Detection of diffusely abnormal white matter in multiple sclerosis on multiparametric brain MRI using semi-supervised deep learning
- Benjamin C. Musall
- Refaat E. Gabr
- Khader M. Hasan
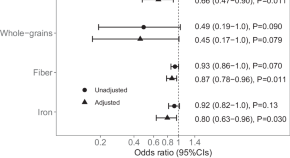
Mediterranean diet and associations with the gut microbiota and pediatric-onset multiple sclerosis using trivariate analysis
Mirza et al. assess the relationship between diet, the gut microbiota, and pediatric-onset multiple sclerosis. They observe that a higher Mediterranean diet score and nutrient intakes, such as fiber, are associated with a lower odds of having multiple sclerosis, and that the gut microbiota might mediate this protective relationship.
- Ali I. Mirza
- Helen Tremlett

BACH2 regulates diversification of regulatory and proinflammatory chromatin states in T H 17 cells
Regulating the balance between T H 17 cells that drive autoimmune inflammation and nonpathogenic T H 17 cells is critical for limiting autoimmune pathology. Here, the authors extensively characterize these two cell states at the transcriptomic and epigenetic levels and show how BACH2 is protective in this context.
- Pratiksha I. Thakore
- Alexandra Schnell
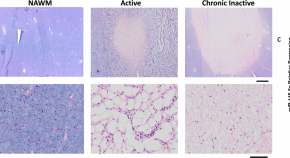
Loss of miR-145 promotes remyelination and functional recovery in a model of chronic central demyelination
Loss of miR-145 promotes remyelination in a chronically demyelinated animal model, implicating it as a factor in remyelination failure in human Multiple Sclerosis lesions and highlighting in as a potential therapeutic target for progressive MS.
- Samantha F. Kornfeld
- Sarah E. Cummings
- Rashmi Kothary
News and Comment
Rubella virus might increase risk of ms, putting the sting in ms.
- Stephanie Houston
Additive effects of EBV and HHV-6A on MS risk
- Heather Wood
Precision neuroimmunology in multiple sclerosis — the horizon is near
Immunological profiling has revealed biological signatures of multiple sclerosis (MS) that could help with early, accurate diagnosis of the disease and with identifying disease subtypes that could inform treatment decisions. The findings are important steps along the path towards precision medicine for people with MS.
- Amit Bar-Or
BTK inhibitor falters in multiple sclerosis trials
Findings of phase III trials of the Bruton’s tyrosine kinase inhibitor evobrutinib in patients with relapsing multiple sclerosis were recently presented at the ACTRIMS Forum.
EBV-specific T cells in multiple sclerosis
New data recently reported at the ACTRIMS Forum add to growing evidence of an aetiological role for Epstein–Barr virus infection in multiple sclerosis.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

Multiple Sclerosis
What is multiple sclerosis.
Multiple sclerosis (MS) is the most common disabling neurological disease of young adults with symptom onset generally occurring between the ages of 20 to 40 years.
In MS, the immune system cells that normally protect us from viruses, bacteria, and unhealthy cells mistakenly attack myelin in the central nervous system (brain, optic nerves, and spinal cord). Myelin is a substance that makes up the protective sheath (myelin sheath) that coats nerve fibers (axons).
MS is a chronic disease that affects people differently. A small number of people with MS will have a mild course with little to no disability, whereas others will have a steadily worsening disease that leads to increased disability over time. Most people with MS, however, will have short periods of symptoms followed by long stretches of relative quiescence (inactivity or dormancy), with partial or full recovery. The disease is rarely fatal and most people with MS have a normal life expectancy.
Myelin and the immune system
MS attacks axons in the central nervous system protected by myelin, which are commonly called white matter. MS also damages the nerve cell bodies, which are found in the brain's gray matter, as well as the axons themselves in the brain, spinal cord, and optic nerves that transmit visual information from the eye to the brain. As the disease progresses, the outermost layer of the brain, called the cerebral cortex, shrinks in a process known as cortical atrophy.
The term multiple sclerosis refers to the distinctive areas of scar tissue (sclerosis—also called plaques or lesions) that result from the attack on myelin by the immune system. These plaques are visible using magnetic resonance imaging (MRI). Plaques can be as small as a pinhead or as large as a golf ball.
The symptoms of MS depend on the severity of the inflammatory reaction as well as the location and extent of the plaques, which primarily appear in the brain stem, cerebellum (involved with balance and coordination of movement, among other functions), spinal cord, optic nerves, and the white matter around the brain ventricles (fluid-filled cavaties).
Signs and symptoms of MS
The natural course of MS is different for each person, which makes it difficult to predict. The onset and duration of MS symptoms usually depend on the specific type but may begin over a few days and go away quickly or develop more slowly and gradually over many years.
There are four main types of MS, named according to the progression of symptoms over time:
- Relapsing-remitting MS—Symptoms in this type come in the form of attacks. In between attacks, people recover or return to their usual level of disability. When symptoms occur in this form of MS, it is called an attack, a relapse, or exacerbation. The periods of disease inactivity between MS attacks are referred to as remission. Weeks, months, or even years may pass before another attack occurs, followed again by a period of inactivity. Most people with MS are initially diagnosed with this form of the disease.
- Secondary-progressive MS—People with this form of MS usually have had a previous history of MS attacks but then start to develop gradual and steady symptoms and deterioration in their function over time. Most individuals with severe relapsing-remitting MS may go on to develop secondary progressive MS if they are untreated.
- Primary-progressive MS—This type of MS is less common and is characterized by progressively worsening symptoms from the beginning with no noticeable relapses or exacerbations of the disease, although there may be temporary or minor relief from symptoms.
- Progressive-relapsing MS—The rarest form of MS is characterized by a steady worsening of symptoms from the beginning with acute relapses that can occur over time during the disease course.
There are some rare and unusual variants of MS, such as:
- Marburg variant MS (also known as malignant MS) causes swift and relentless symptoms and decline in function, and may result in significant disability or even death shortly after disease onset.
- Balo's concentric sclerosis causes concentric rings of myelin destruction that can be seen on an MRI and is another variant type of MS that can progress rapidly.
Early MS symptoms often include:
- Vision problems such as blurred or double vision, or optic neuritis, which causes pain with eye movement and rapid vision loss
- Muscle weakness, often in the hands and legs, and muscle stiffness accompanied by painful muscle spasms
- Tingling, numbness, or pain in the arms, legs, trunk, or face
- Clumsiness, especially difficulty staying balanced when walking
- Bladder control problems
- Intermittent or constant dizziness
MS may also cause later symptoms, such as:
- Mental or physical fatigue which accompanies the early symptoms during an attack
- Mood changes such as depression or difficulty with emotional expression or control
- Cognitive dysfunction—problems concentrating, multitasking, thinking, learning, or difficulties with memory or judgment
Muscle weakness, stiffness, and spasms may be severe enough to affect walking or standing. In some cases, MS leads to partial or complete paralysis and the use of a wheelchair is not uncommon, particularly in individuals who are untreated or have advanced disease. Many people with MS find that weakness and fatigue are worse when they have a fever or when they are exposed to heat. MS exacerbations may occur following common infections.
Pain is rarely the first sign of MS but pain often occurs with optic neuritis and trigeminal neuralgia, a disorder that affects one of the nerves that provides sensation to different parts of the face. Painful limb spasms and sharp pain shooting down the legs or around the abdomen can also be symptoms of MS.
Conditions associated with MS
- Transverse myelitis (an inflammation of the spinal cord) may develop in those with MS. Transverse myelitis can affect spinal cord function over several hours to several weeks before partial or complete recovery. It usually begins as a sudden onset of lower back pain, muscle weakness, abnormal sensations in the toes and feet, or difficulties with bladder control or bowel movements. This can rapidly progress to more severe symptoms, including arm and/or leg paralysis. In most cases, people recover at least some function within the first 12 weeks after an attack begins.
- Neuromyelitis optica is a disorder associated with transverse myelitis as well as optic nerve inflammation (also known as optic neuritis). People with this disorder usually have abnormal antibodies (proteins that normally target viruses and bacteria) against a specific channel in optic nerves, the brain stem or spinal cord, called the aquaporin-4 channel. These individuals respond to certain treatments, which are different than those commonly used to treat MS.
- Trigeminal neuralgia is a chronic pain condition that causes sporadic, sudden burning or shock-like facial pain. The condition is more common in young adults with MS and is caused by lesions in the brain stem, the part of the brain that controls facial sensation.
Who is more likely to get multiple sclerosis?
Females are more frequently affected than males. Researchers are looking at several possible explanations for why the immune system attacks central nervous system myelin, including:
- Fighting an infectious agent (e.g., a virus) that has components that mimic components of the brain (molecular mimicry)
- Destroying brain cells because they are unhealthy
- Mistakenly identifying normal brain cells as foreign
There is also something known as the blood-brain barrier, which separates the brain and spinal cord from the immune system. If there is a break in this barrier, it exposes the brain to the immune system. When this happens, the immune system may misinterpret structures in the brain, such as myelin, as “foreign.”
Research shows that genetic vulnerabilities combined with environmental factors may cause MS.
Genetic susceptibility
MS itself is not inherited, but susceptibility to MS may be inherited. Studies show that some individuals with MS have one or more family member or relative who also have MS.
Current research suggests that dozens of genes and possibly hundreds of variations in the genetic code (gene variants) combine to create vulnerability to MS. Some of these genes have been identified, and most are associated with functions of the immune system. Many of the known genes are similar to those that have been identified in people with other autoimmune diseases as type 1 diabetes, rheumatoid arthritis, or lupus.
Infectious factors and viruses
Several viruses have been found in people with MS, but the virus most consistently linked to the development of MS is the Epstein-Barr virus (EBV) which causes infectious mononucleosis.
Only about five percent of the population has not been infected by EBV. These individuals are at a lower risk for developing MS than those who have been infected. People who were infected with EBV in adolescence or adulthood, and who therefore develop an exaggerated immune response to EBV, are at a significantly higher risk for developing MS than those who were infected in early childhood. This suggests that it may be the type of immune response to EBV that may lead to MS, rather than EBV infection itself. However, there is still no proof that EBV causes MS and the mechanisms that underlie this process are poorly understood.
Environmental factors
Several studies indicate that people who spend more time in the sun and those with relatively higher levels of vitamin D are less likely to develop MS or have a less severe course of disease and fewer relapses. Bright sunlight helps human skin produce vitamin D. Researchers believe that vitamin D may help regulate the immune system in ways that reduce the risk of MS or autoimmunity in general. People from regions near the equator, where there is a great deal of bright sunlight, generally have a much lower risk of MS than people from temperate areas such as the U.S. and Canada.
Studies have found that people who smoke are more likely to develop MS and have a more aggressive disease course. Indeed, people who smoke tend to have more brain lesions and brain shrinkage than non-smokers.
How is multiple sclerosis diagnosed and treated?
Diagnosing MS
There is no single test used to diagnose MS. The disease is confirmed when symptoms and signs develop and are related to different parts of the nervous system at more than one interval and after other alternative diagnoses have been excluded.
Doctors use different tests to rule out or confirm the diagnosis. In addition to a complete medical history, physical examination, and a detailed neurological examination, a doctor may recommend:
- MRI scans of the brain and spinal cord to look for the characteristic lesions of MS. A special dye or contrast agent may be injected into a vein to enhance brain images of the active MS lesions.
- Lumbar puncture (sometimes called a spinal tap) to obtain a sample of cerebrospinal fluid and examine it for proteins and inflammatory cells associated with the disease. Spinal tap analysis also can rule out diseases that may look like MS.
- Evoked potential tests, which use electrodes placed on the skin and painless electric signals to measure how quickly and accurately the nervous system responds to stimulation.
Treating MS
There is no cure for MS, but there are treatments that can reduce the number and severity of relapses and delay the long-term disability progression of the disease.
- Corticosteroids, such as intravenous (infused into a vein) methylprednisolone, are prescribed over the course of three to five days. Intravenous steroids quickly and potently suppress the immune system and reduce inflammation. They may be followed by a tapered dose of oral corticosteroids. Clinical trials have shown that these drugs hasten recovery from MS attacks, but do not alter the long-term outcome of the disease.
- Plasma exchange (plasmapheresis) can treat severe flare-ups in people with relapsing forms of MS who do not have a good response to methylprednisolone. Plasma exchange involves taking blood out of the body and removing components in the blood's plasma that are thought to be harmful. The rest of the blood, plus replacement plasma, is then transfused back into the body. This treatment has not been shown to be effective for secondary progressive or chronic progressive MS.
Disease-modifying treatments
Current therapies approved by the U.S. Food and Drug Administration (FDA) for MS are designed to modulate or suppress the inflammatory reactions of the disease. They are most effective for relapsing-remitting MS at early stages of the disease.
Injectable medications include:
- Beta interferon drugs are among the most common medications used to treat MS. Interferons are signaling molecules that regulate immune cells. Potential side effects of these drugs include flu-like symptoms (which usually fade with continued therapy), depression, or elevation of liver enzymes. Some individuals will notice a decrease in the effectiveness of the drugs after 18 to 24 months of treatment. If flare-ups occur or symptoms worsen, doctors may switch treatment to alternative drugs.
- Glatiramer acetate changes the balance of immune cells in the body, but how it works is not entirely clear. Side effects are usually mild and consist of local injection site reactions or swelling.
Infusion treatments include:
- Natalizumab is administered intravenously once a month. It works by preventing cells of the immune system from entering the brain and spinal cord. It is very effective but is associated with an increased risk of a serious and potentially fatal viral infection of the brain called progressive multifocal leukoencephalopathy (PML). Natalizumab is generally recommended only for individuals who have not responded well to or who are unable to tolerate other first-line therapies.
- Ocrelizumab is administered intravenously every six months and treats adults with relapsing or primary progressive forms of MS. It is the only FDA-approved disease-modifying therapy for primary-progressive MS. The drug targets the circulating immune cells that produce antibodies, which also play a role in the formation of MS lesions. Side effects include infusion-related reactions and increased risk of infections. Ocrelizumab may increase the risk of cancer as well.
- Alemtuzumab is administered for five consecutive days followed by three days of infusions one year later. It targets proteins on the surface of immune cells. Because this drug increases the risk of autoimmune disorders it is recommended for those who have had inadequate responses to two or more MS therapies.
- Mitoxantrone, which is administered intravenously four times a year, has been approved for especially severe forms of relapsing-remitting and secondary progressive MS. Side effects include the development of certain types of blood cancers in up to one percent of those with MS, as well as with heart damage. This drug should be considered as a last resort to treat people with a form of MS that leads to rapid loss of function and for whom other treatments did not work.
Oral treatments include:
- Fingolimod is a once-daily medication that reduces the MS relapse rate in adults and children. It is the first FDA-approved drug to treat MS in adolescents and children ages 10 years and older. The drug prevents white blood cells called lymphocytes from leaving the lymph nodes and entering the blood, brain, and spinal cord. Fingolimod may result in a slow heart rate and eye problems when first taken. Fingolimod can also increase the risk of infections, such as herpes virus infections, or in rare cases be associated with PML.
- Dimethyl fumarate is a twice-daily medication used to treat relapsing forms of MS. Its exact mechanism of action is not currently known. Side effects of dimethyl fumarate are flushing, diarrhea, nausea, and lowered white blood cell count.
- Teriflunomide is a once-daily medication that reduces the rate of proliferation of activated immune cells. Teriflunomide side effects can include nausea, diarrhea, liver damage, and hair loss.
- Cladribine is administered as two courses of tablets about one year apart. Cladribine targets certain types of white blood cells that drive immune attacks in MS. The drug may increase the risk of developing cancer and should be considered for individuals who have not responded well to other MS treatments.
- Diroximel fumarate is a twice-daily drug similar to dimethyl fumarate (brand name Tecfidera) but with fewer gastrointestinal side effects. Scientists suspect these drugs, which have been approved to treat secondary progressive MS, reduce damage to the brain and spinal cord by making the immune response less inflammatory, although their exact mechanism of action is poorly understood.
- Siponimod tablets (Mayzent) is taken orally and has a similar mechanism of action to fingolimod. Siponimod has been approved by the FDA to treat secondary-progressive MS.
Clinical trials have shown that cladribine, diroximel fumarate, and dimethyl fumarate decrease the number of relapses, delay the progress of physical disability, and slow the development of brain lesions.
Managing MS symptoms
MS causes a variety of symptoms that can interfere with daily activities but can usually be treated or managed. Many of these issues are best treated by neurologists who have advanced training in the treatment of MS and who can prescribe specific medications to treat these problems.
Eye and vision problems are common in people with MS but rarely result in permanent blindness. Inflammation of the optic nerve (optic neuritis) or damage to the myelin that covers the nerve fibers in the visual system can cause blurred or grayed vision, temporary blindness in one eye, loss of normal color vision, depth perception, or loss of vision in parts of the visual field. Uncontrolled horizontal or vertical eye movements (nystagmus), “jumping vision" (opsoclonus), and double vision (diplopia) are common in people with MS. Intravenous steroid medications, special eyeglasses, and periodically resting the eyes may be helpful.
Muscle weakness and spasticity is common in MS. Mild spasticity can be managed by stretching and exercising muscles using water therapy, yoga, or physical therapy. Medications such as gabapentin or baclofen can reduce spasticity. It is very important that people with MS stay physically active because physical inactivity can contribute to worsening stiffness, weakness, pain, fatigue, and other symptoms.
Tremor, or uncontrollable shaking, develops in some people with MS. Assistive devices and weights attached to utensils or even limbs are sometimes helpful for people with tremor. Deep brain stimulation and drugs, such as clonazepam, may also be useful.
Problems with walking and balance occur in many people with MS. The most common walking problem is ataxia—unsteady, uncoordinated movements—due to damage to the areas of the brain that coordinate muscle balance. People with severe ataxia generally benefit from the use of a cane, walker, or other assistive device. Physical therapy also can reduce walking problems. The FDA has approved the drug dalfampridine to improve walking speed in people with MS.
Fatigue is a common symptom of MS and may be both physical (tiredness in the arms or legs) and cognitive (slowed processing speed or mental exhaustion). Daily physical activity programs of mild to moderate intensity can significantly reduce fatigue, although people should avoid excessive physical activity and minimize exposure to hot weather conditions or ambient temperature. Other drugs that may reduce fatigue include amantadine, methylphenidate, and modafinil. Occupational therapy can help people learn how to walk using an assistive device or in a way that saves physical energy. Stress management programs, relaxation training, membership in an MS support group, or individual psychotherapy may help some people.
Pain from MS can be felt in different parts of the body. Trigeminal neuralgia (facial pain) is treated with anticonvulsant or antispasmodic drugs, or less commonly, painkillers. Central pain, a syndrome caused by damage to the brain and/or spinal cord, can be treated with gabapentin and nortriptyline. Treatments for chronic back or other musculoskeletal pain may include heat, massage, ultrasound, and physical therapy.
Problems with bladder control and constipation may include urinary frequency, urgency, or the loss of bladder control. A small number of individuals retain large amounts of urine. Medical treatments are available for bladder-related problems. Constipation is also common and can be treated with a high-fiber diet, laxatives, and stool softeners.
Sexual dysfunction can result from damage to nerves running through the spinal cord. Sexual problems may also stem from MS symptoms such as fatigue, cramped or spastic muscles, and psychological factors. Some of these problems can be corrected with medications. Psychological counseling may be helpful.
Clinical depression is frequent among people with MS. MS may cause depression as part of the disease process and chemical imbalance in the brain. Depression can intensify symptoms of fatigue, pain, and sexual dysfunction. It is most often treated with cognitive behavioral therapy, and selective serotonin reuptake inhibitor (SSRI) antidepressant medications, which are less likely than other antidepressant medications to cause fatigue.
Inappropriate and involuntary expressions of laughter, crying, or anger—symptoms of a condition called pseudobulbar affect—sometimes are associated with MS. These expressions are often incongruent with mood; for example, people with MS may cry when they are actually happy or laugh when they are not especially happy. The combination treatment of the drugs dextromethorphan and quinidine can treat pseudobulbar affect, as can other drugs such as amitriptyline or citalopram.
Cognitive impairment—a decline in the ability to think quickly and clearly and to remember easily—affects up to 75 percent of people with MS. These cognitive changes may appear at the same time as the physical symptoms or they may develop gradually over time. Drugs such as donepezil may be helpful in some cases.
Complementary and alternative therapies
Many people with MS benefit from complementary or alternative approaches such as acupuncture, aromatherapy, ayurvedic medicine, touch and energy therapies, physical movement disciplines such as yoga and tai chi, herbal supplements, and biofeedback.
Because of the risk of interactions between alternative and conventional therapies, people with MS should discuss all the therapies they are using with their doctor, especially herbal supplements. Herbal supplements have biologically active ingredients that could have harmful effects on their own or interact harmfully with other medications.
What are the latest updates on multiple sclerosis?
The National Institute of Neurological Disorders and Stroke (NINDS), a component of the National Institutes of Health (NIH), is the leading federal funder of research on the brain and nervous system, including research on MS.
In addition to NINDS, other NIH Institutes—including the National Institute of Allergy and Infectious Diseases (NIAID)—fund research on multiple sclerosis. Find more information on NIH research efforts through NIH RePORTER , a searchable database of current and past research projects supported by NIH and other federal agencies. RePORTER also includes links to publications and patents citing support from these projects.
Although researchers have not been able to identify the cause of MS with any certainty, there has been excellent progress in other areas of MS research—especially in the development of new treatments to prevent exacerbations of the disease. New discoveries are constantly changing MS treatment options and helping to reduce MS-related disability.
Research projects conducted by NINDS scientists or through NIH grants to universities and other sites across the U.S. cover a wide range of topics such as comorbidities, mechanisms of cognitive impairment, blood-brain barrier breakdown in MS, the role of sleep and circadian rhythms, rehabilitation strategies, and telehealth. Other topics include:
- Biomarkers to accurately diagnose MS and monitor disease progression, including blood and imaging tests (e.g., MRI)
- Genetic and environmental risk factors for MS, such as low Vitamin D or the Epstein-Barr virus
- The role of the gut microbiome and diet in MS
- Mechanisms that underlie gender differences in the incidence and presentation of MS
- MS risk factors and disease course in African American and Hispanic populations, and disparities in care
- The role of the immune system in MS, including its function in the central nervous system (CNS)
- The role and crosstalk of various cell types in the CNS with relation to MS
- Basic functions of myelination, demyelilnation, and axonal degeneration, and strategies to overcome axonal and myelin loss
Scientists sponsored by NIAID are testing an experimental stem cell treatment titled, autologous hematopoietic stem cell transplantation (AHSCT), against the best available biologic therapies for severe forms of relapsing MS.
Investigators in the clinical trial BEAT-MS (BEst Available Therapy versus autologous hematopoietic stem cell transplant for Multiple Sclerosis) are removing some immune cells and then infusing some of the person's own blood-forming stem cells to reset the immune system so it no longer attacks the CNS.
Genetic research funded by NINDS is exploring the roles of "susceptibility genes"—genes that are associated with an increased risk for MS. Several candidate genes have been identified and researchers are studying their function in the nervous system to discover how they may lead to the development of MS.
Other studies aim to develop better neuroimaging tools, such as more powerful MRI methods, to diagnose MS, track disease progression, and assess treatments. NINDS scientists are collecting MRIs of the brain and spinal cord and scans of the retina, along with other clinical and biological data, from more than 100 individuals with MS and 50 individuals without the disease over a period of years to observe changes in the course of MS. Investigators are using MRI to study the natural history of MS and to help define the mechanism of action and cause of side effects of disease modifying therapies.
Intramural research programs on MS
NINDS and other NIH Institutes have a very active MS intramural research program among scientists working at NIH. Together, they have:
- Established and continue to develop MRI as a critical tool for examining the natural course of the disease in humans, monitoring disease progression, assessing effects of treatments in clinical trials, and understanding MS biology
- Played an important role in understanding why some patients develop a rare and potentially fatal brain infection (progressive multifocal leukoencephalopathy) when taking potent MS drugs, and they are developing new treatments for this infection
- Unraveled mechanisms by which viruses, especially the Epstein-Barr virus, contribute to the development of MS
- Conducted next-generation treatment trials targeting specific mechanisms of disease progression, using advanced MRI and fluid biomarkers as outcome measures
- Developed the first MRI method to visualize the lymph vessels surrounding the brain, which play a critical role in neuro-immune communication
Translational research
NIH supports translational studies to develop therapies that will stop or reverse the course of the disease, focusing on pathways that modify immune system function, repair damaged myelin, or protect neurons from damage. Researchers are also developing animal models of MS to more accurately predict drug response in human disease. However, current animal models share some of the disease mechanisms and symptoms of MS but do not fully mimic the disease, especially in its clinically progressive phase.
Focus on progressive MS therapies
Scientists continue to study the biology and mechanisms of relapsing-remitting MS while increasing efforts to stop or prevent the steady decline in function that occurs in progressive MS. In the MS-SPRINT trial, the NINDS NeuroNEXT clinical trials network tested the drug ibudilast as a potential neuroprotective drug for progressive MS and showed that the drug slowed the rate of brain shrinkage as compared to a placebo. NINDS Intramural scientists are conducting proof-of-concept clinical trials to address a key driver of clinical progression called the “slowly expanding lesion.”
Focus on biomarkers
As part of a larger effort to develop and validate effective biomarkers (signs that may indicate risk of a disease or be used to monitor its progression) for neurological disease, NINDS is supporting two definitive multicenter MS studies:
- The Central Vein Sign in MS (CAVS-MS) study, which is testing whether a rapid MRI approach designed by NINDS Intramural scientists can use the detection of a central vein passing through brain plaques to differentiate MS from other common neurological disorders that can mimic MS. The goal is to develop a reliable imaging test for MS in order to achieve rapid yet accurate diagnosis and reduce misdiagnosis, which may affect up to 20 percent of people currently diagnosed with MS.
- A study to test whether a simple new blood test that measures small amounts of neuron-derived proteins (neurofilaments) can be used to predict the severity of disease and help determine whether MS drugs are working to protect brain tissues.
How can I or my loved one help improve care for people with multiple sclerosis?
Consider participating in a clinical trial so clinicians and scientists can learn more about MS and related disorders. Clinical research uses human volunteers to help researchers learn more about a disorder and perhaps find better ways to safely detect, treat, or prevent disease.
All types of volunteers are needed—those who are healthy or may have an illness or disease—of all different ages, sexes, races, and ethnicities to ensure that study results apply to as many people as possible, and that treatments will be safe and effective for everyone who will use them.
For information about participating in clinical research visit NIH Clinical Research Trials and You . Learn about clinical trials currently looking for people with MS at Clinicaltrials.gov .
Where can I find more information about multiple sclerosis?
Information may be available from the following organizations and resources:
Accelerated Cure Project for Multiple Sclerosis Phone: 781-487-0008
Autoimmune Association Phone: 586-776-3900
Multiple Sclerosis Association of America (MSAA) Phone: 856-488-4500 or 800-532-7667
Multiple Sclerosis Foundation (MS Focus) Phone: 954-776-6805 or 888 673-6287
Myelin Repair Foundation (MRF) Phone: 408-871-2410
National Ataxia Foundation (NAF) Phone: 763-553-0020
National Multiple Sclerosis Society Phone: 800-344-4867
National Organization for Rare Disorders (NORD) Phone: 203-744-0100
National Rehabilitation Information Center (NARIC) Phone: 301-459-5900 or 800-346-2742; 301-459-5984
Paralyzed Veterans of America Phone: 202-872-1300 or 800-555-9140
Journal logo
American academy of neurology.
Then and Now: 20 Years Later, What Has Changed in MS?
- For Your Patients
- Multiple Sclerosis
By Dawn Fallik
August 19, 2021, article in brief.
Specialists in multiple sclerosis (MS) look at the advances in detection, prognosis, and treatment of MS that have been made in the last 20 years.
When interviewed about their experiences over the past two decades treating patients with multiple sclerosis (MS), MS specialists said they easily remembered a time when patients were told that exercise was bad for them and that getting pregnant would exacerbate their disease. There were few therapies, and they could offer little hope.
Now it seems doctors can barely keep up with the progress being made, and they say this with joy and optimism.
“Something I say to patients who are being diagnosed now is that the field is moving faster than their disease, and we are just going to get further out in front of it,” said Stephen Krieger, MD, FAAN, professor of neurology at the Icahn School of Medicine at Mount Sinai in New York.
There seems to be only one thing that hasn't progressed about the way the neurologic disease is treated, taught, and diagnosed: the origins of MS itself. It is frustrating, the neurologists said, that it is still unclear what exactly triggers the disease.
The Advent of Technology
All the neurologists agreed that one particular technological invention drastically changed the course of MS treatment and diagnosis—MRI, which became widely used in the 1990s and 2000s.
Robert P. Lisak, MD, FAAN, FRCP, FANA, the Parker Webber Chair in Neurology and professor of neurology at Wayne State University School of Medicine in Detroit, told Neurology Today he entered the MS field after becoming intrigued by his neuroanatomy and microbiology/immunology courses in medical school.
“There are very few fields that have benefited more in clinical practice and research from the MRI than MS,” he said. “What we knew before, we only knew from the brains of patients at autopsy.”
Teaching about MS itself has changed dramatically, he said. Medical school courses on MS described the disease as a “white matter” disease, primarily impacting the myelin, the white matter of the brain and spinal cord, with relative sparing of the axons. The thought was that the disease's effect on gray matter, which forms the superficial layers of the brain, as well as deeper structures, came later in the disease, said Dr. Lisak. It turns out, we've rediscovered and, with modern research, expanded our understanding, that the teaching was wrong and MS does impact the gray matter as well as axons early on in the disease.
Aaron Miller, MD, FAAN, medical director of the Corinne Goldsmith Dickinson Center for MS and professor of neurology at the Icahn School of Medicine at Mount Sinai, said it's hard to understate the role of the MRI in diagnosis and treating patients. When he first started in the field, MS was thought to be a slow viral disease, and he was drawn to the field because he could work with patients and their families over many years.
The establishment of formal diagnostic criteria by Professor W. Ian McDonald in 2001, which incorporated MRI, has helped. The criteria specifically use MRI to look at damage to the central nervous system over time and in different areas. The criteria have been revised several times, most recently in 2017.
“Proper application of the McDonald criteria will allow for an earlier diagnosis, and if the criteria are applied properly, it will help prevent misdiagnosis,” said Dr. Miller, adding that misdiagnosis was happening more frequently 20 years ago when there was not a clear set of diagnostic criteria that all doctors could follow.
Therapy Options
Several MS specialists used the word “dramatic” to describe the change in treatment options over the past 20 years. Interferon-beta became available in the mid-90s and was the first disease-modifying therapy that reduced relapse rates and delayed the onset of disability. But now there are more than 20 therapies available in different forms.
“MS therapies used to be covered in one slide at the end of a talk,” said Dr. Krieger. “Now you can't cover them in one lecture, you need to space it out, and it takes a residency and fellowship to learn the nuances, which is a wonderful problem to have.”

“We may still change from one medication to another, but it's because of side effects or risks from side effects, or patients wanting to change their mode of treatment—say from an intravenous option to an oral option, or from an oral options to an intravenous option, but at least we're using therapies that are much different.”—DR. LAUREN KRUPP
Patricia K. Coyle, MD, FAAN, FANA, professor of neurology and director of the MS Comprehensive Care Center at the State University of New York at Stony Brook, said she remembers when MS was mostly an “untreatable” disease, except for steroids, cyclophosphamide, and anti-depressants drugs to treat symptoms, not the disease itself.
Although originally MS research focused on T cells, now the focus is more on monoclonal antibodies that target B cells, a type of white blood cells that create an abnormal immune response, attacking the nervous system.
All these new therapies have been a game-changer for patients, particularly young ones.
“So you would make the diagnosis in young people, and it was going to be potluck with regard to how they would do and what would happen,” Dr. Coyle said. “We now have over 25 distinct agents counting the generics, covering 10 distinct mechanisms of action, and we have a much better understanding of MS and the importance of early treatment.”
She also emphasized how much treatment has changed to focus on the patient as an individual, to try and maximize their CNS reserve by promoting wellness programs, and to optimize lifestyle choices, particularly by recognizing and treating co-morbidities, such as obesity and smoking, early on.
“We're taking a much more global approach to what's considered treatment. The disease-modifying therapies are fundamental, but if you just focus on that, it will not be sufficient. “
The way the medications themselves are taken has changed the way patients approach their disease, said Lauren Krupp, MD, FAAN, director of New York University's MS Comprehensive Care Center and Glickenhaus Pier Professor of Pediatric Neuropsychiatry. In 2001, when most of the medications were injectables, the goal was mainly to control relapses. This was particularly a problem in young people who had a high relapse rate, and they would often rotate from one to the other because of frequent breakthroughs. By 2005, more effective therapies that patients could take in oral forms started appearing on the market.
“We may still change from one medication to another, but it's because of side effects or risks from side effects, or patients wanting to change their mode of treatment—say from an intravenous option to an oral option, or from an oral options to an intravenous option, but at least we're using therapies that are much different,” she said.
Education About MS
Barbara Giesser, MD, FAAN, FANA, a staff physician at the Pacific Neuroscience Institute in Santa Monica, became interested in MS during her residency at Albert Einstein College of Medicine in New York, under Dr. Labe C. Scheinberg, who died in 2004. She loved that, even 39 years ago, MS care had a multidisciplinary approach, involving the patient's family, social workers, occupational therapists and psychologists.
Dr. Giesser said although the team approach existed long ago, the idea of addressing wellness—diet, exercise, sleep—was not incorporated
“When I started, almost 40 years ago, the conventional wisdom was that people with MS shouldn't exercise and shouldn't exert themselves, and what I tell my patients now is that if you could have picked the single worst thing we could have told people, that was probably it,” Dr. Giesser said. “Studies have shown that not only can people with MS tolerate exercise, but it's actually very good for them.”
Over the past 20 years, there's been a lot of movement toward understanding who the disease impacts. Dr. Giesser said MS used to be taught as a disease mainly of White people, but now it is known that the incidence in African Americans is much higher than previously believed, and that they may respond differently to some of the disease-modifying therapies—and this has become the focus of new research.
Dr. Krupp said researchers also believed that MS was an adult disease, and often teens were misdiagnosed, in part because doctors did not want to diagnose children with a chronic, incurable illness. In 2002, she founded the Lourie Center for Pediatric MS at Stony Brook Children's Hospital, partially inspired by a 16-year-old MS patient.
“Many of the MS centers at that time had adult neurologists who would say ‘OK, this kid has MS, but we don't treat kids,’ and would refer them to a pediatric neurologist, who would say ‘Yeah, I treat kids, but I have no idea how to use these new medications on them,’” said Dr. Krupp.
The Patient Mix
Overwhelmingly, the patients in the waiting room of an MS clinic have changed dramatically, those interviewed said.
“Twenty years ago, the patients would largely be composed of those with a great disability, and now it includes many, many people who you would never know had MS by looking at them,” said Dr. Krieger. “The difference between an MS center then versus now, that couldn't provide a clearer picture of what progress looks like.”
Dr. Coyle agreed, saying that the change is due to a combination of treatment and changes to environment and healthy lifestyle.
“The very interesting thing is that this disease appears to be becoming milder. We're not seeing the very disabled very much, individuals coming in in a wheelchair, unable to use more than one extremity,” she said. “It's much more common to see people walking around that you would never suspect had a neurologic disease—that's the new face of MS.”
The Challenges Ahead
Doctors expressed frustration that there is still a general lack of understanding of the pathophysiology of the disease, and therapies to address progressive disease.
“It does take time, but we are really lacking treatments for progressive MS, and we're lacking CNS repair strategies, although there are some interesting trials going on in that area,” said Dr. Coyle.
Dr. Giesser agreed, saying that it's frustrating that there are no medications to repair and rebuild the damage that's been done.
“That's the next frontier, and certainly that's one of the big impetuses for early treatment, because once it's gone, it's gone,” she said. “So what I hope is that, in the very near future, instead of saying to someone ‘You have MS, and I can give you medicine to stop the progress,’ we can say ‘I'm also going to give you medication that will repair what was lost.’”
One of the challenges in developing those therapies is the fundamental lack of understanding of the disease. Dr. Miller said he thought “we would have a better clue about the clear triggers of MS,” and Dr. Krieger said he thought there might be better biomarkers to help choose the right medicine for the right patient.
In 2021, there are still debates at national meetings about how MS works and whether it is a neurodegenerative or inflammatory disease—“and these are fundamental questions of cause and effect that are still unknown,” he said.
Dr. Lisak noted that it's still unclear if MS starts in the nervous system and then patients have an inflammatory response or if the immune system gets attacked, and it might be different in different patients.
“There are some patients with no relapses and no new lesions, and yet the disease is progressing somewhere else,” he said.
Those interviewed said they did not think MS would have been cured by now—few diseases have been “cured” entirely. But some, like Dr. Krupp, hoped that there would have been a way of stopping MS by now.
“I was hoping we might, and I would like to think that we might accomplish that before the next 20 years,” she said.
20 Years: Then and Now
To mark Neurology Today's twentieth year of publication, we are publishing a series of stories that look back at the ways in which the practice and subspecialties of neurology have changed in 20 years. This article is the first in the series.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
- Permissions
Vol. 21, Issue 16 - p. 1-23
doi: 10.1097/01.NT.0000790204.54971.52
Save my selection
- Patient Care & Health Information
- Diseases & Conditions
- Multiple sclerosis
- What is multiple sclerosis? An expert explains
Learn more from neurologist Oliver Tobin, M.B., B.Ch., B.A.O., Ph.D.
I'm Dr. Oliver Tobin, a neurologist specializing in multiple sclerosis at Mayo Clinic. In this video, we'll be covering the basics of multiple sclerosis. What is it? Who gets it? The symptoms, diagnosis, and treatment. Whether you're looking for answers about your own health or that of someone you love, we're here to provide you with the best information available. Multiple sclerosis is a disorder in which the body's immune system attacks the protective covering of the nerve cells in the brain, optic nerve and spinal cord, called the myelin sheath. And this sheath is often compared to the insulation on an electrical wire. When that covering is damaged, it exposes the actual nerve fiber, which can slow or block the signals being transmitted within it. The nerve fibers themselves might also be damaged. The body can repair damage to the myelin sheath, but it's not perfect. The resulting damage leaves lesions or scars, and this is where the name comes from: multiple sclerosis, multiple scars. Now everyone loses brain cells and spinal cord cells as they get older. But if part of the brain or spinal cord has been damaged by MS, the nerve cells in that area will die off faster than the areas around it that are normal. This happens very slowly, usually over decades and typically shows up as gradual walking difficulty happening over several years. When you read about multiple sclerosis, you may hear about different types -- the most frequent being relapsing-remitting multiple sclerosis. And this is characterized by attacks, or relapses.
We don't know what causes MS, but there are certain factors that may increase the risk or trigger its onset. So while MS can occur at any age, it mostly makes its first appearance in people between the ages of 20 and 40. Low levels of vitamin D and low exposure to sunlight, which enables our body to make vitamin D, are associated with an increased risk of developing MS. As people who have MS who have low vitamin D tend to have more severe disease. So people who are overweight are more likely to develop MS and people who have MS and are overweight tend to have more severe disease and a faster onset of progression. People who have MS and who smoke tend to have more relapses, worse progressive disease, and worse cognitive symptoms. Women are up to three times as likely as men to have relapsing-remitting MS. The risk for MS in the general population is about 0.5%. If a parent or sibling has MS, your risk is about twice that or about 1%. Certain infections are also important. A variety of viruses have been linked to MS, including Epstein-Barr virus, which causes mono. Northern and southern latitudes have a higher prevalence, including Canada, the northern US, New Zealand, southeastern Australia, and Europe. White people, especially of northern European descent, are at the highest risk. People of Asian, African, and Native American ancestry have the lowest risk. A slightly increased risk is seen if a patient already has autoimmune thyroid disease, pernicious anemia, psoriasis, type 1 diabetes, or inflammatory bowel disease.
Symptoms of a relapse usually come on over 24 to 48 hours, last for a few days to a few weeks and then improve in the region of 80 to a 100 percent. Those symptoms include loss of vision in an eye, loss of power in an arm or leg or a rising sense of numbness in the legs. Other common symptoms associated with MS include spasms, fatigue, depression, incontinence issues, sexual dysfunction, and walking difficulties.
There's currently no single test to make a diagnosis of MS. However, there are four key features which help to secure the diagnosis. Firstly, are there typical symptoms of multiple sclerosis? Again, those are loss of vision in an eye, loss of power in an arm or leg, or sensory disturbance in an arm or leg lasting for more than 24 hours. Secondly, do you have any physical examination findings consistent with MS? Next, is the MRI of your brain or spine consistent with MS? Now here it's important to note that 95 percent of people over the age of 40 have an abnormal brain MRI, just the same as many of us have wrinkles on our skin. Lastly, are the results of the spinal fluid analysis consistent with MS? Your doctor may recommend blood tests to check for other diseases that share the same symptoms. They may also recommend an OCT test or optical coherence tomography. This is a short scan of the thickness of the layers at the back of your eye.
So the best thing to do when living with MS is to find a trusted interdisciplinary medical team that can help you monitor and manage your health. Having a multidisciplinary team is essential for addressing the individual symptoms that you're experiencing. If you have an MS attack or relapse, your doctor may prescribe you corticosteroids to reduce or improve your symptoms. And if your attack symptoms do not respond to steroids, another option is plasmapheresis or plasma exchange, which is a treatment similar to dialysis. About 50 percent of people who do not respond to steroids have a significant improvement with a short course of plasma exchange. There are over 20 medications currently approved for prevention of MS attacks and prevention of new MRI lesions.
As learning to function with MS can be challenging, there are medical experts ready to work with you to help you manage it, so you can still live a full life. Consulting with a physiatrist, physical or occupational therapist can help you deal with physical difficulties. Physical activity is strongly recommended for all people with MS. Mental health is also an important consideration. So keeping up personal connections with friends and family and trying to stay involved with your hobbies is important. But also be kind to yourself and realistic about what you're up for. This can change from day to day, so it's okay to give yourself permission if something seems like too much or if you need to cancel plans. You may also find support groups helpful to connect with people who understand what you are going through and discuss your feelings and concerns with a doctor or a counselor. Meanwhile, scientists are hard at work, expanding our understanding of this disease and developing new treatments and medications which are ever more effective. If you want to learn more, watch more of our videos or visit mayoclinic.org. We wish you well.
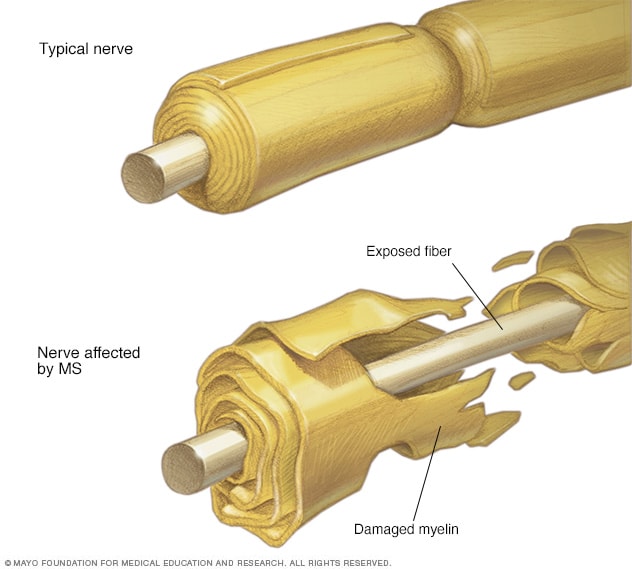
In multiple sclerosis, the protective coating on the nerve fibers (myelin) is damaged and may eventually be destroyed. Depending on where the nerve damage occurs, MS can affect vision, sensation, coordination, movement, and bladder or bowel control.
Multiple sclerosis (MS) is a potentially disabling disease of the brain and spinal cord (central nervous system).
In MS , the immune system attacks the protective sheath (myelin) that covers nerve fibers and causes communication problems between your brain and the rest of your body. Eventually, the disease can cause permanent damage or deterioration of the nerve fibers.
Signs and symptoms of MS vary widely between patients and depend on the location and severity of nerve fiber damage in the central nevous system. Some people with severe MS may lose the ability to walk independently or ambulate at all. Other individuals may experience long periods of remission without any new symptoms depending on the type of MS they have.
There's no cure for multiple sclerosis. However, there are treatments to help speed the recovery from attacks, modify the course of the disease and manage symptoms.
Products & Services
- A Book: Mayo Clinic Family Health Book
- Newsletter: Mayo Clinic Health Letter — Digital Edition
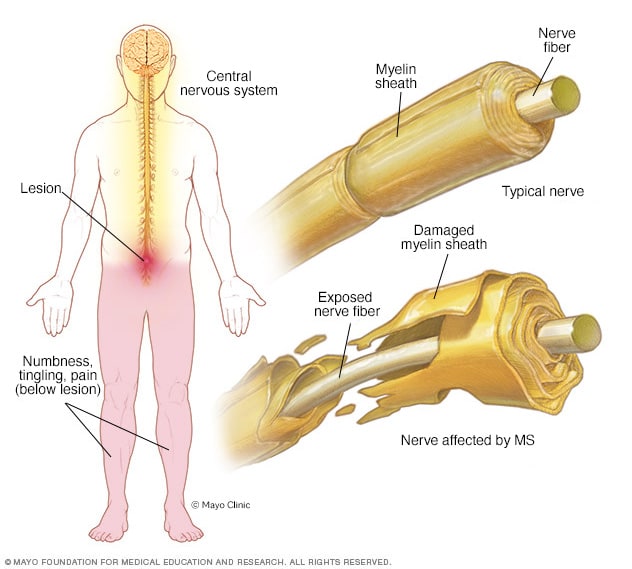
- Myelin damage and the nervous system
In multiple sclerosis, the protective coating on nerve fibers (myelin) in the central nervous system is damaged. This creates a lesion that, depending on the location in the central nervous system, may cause symptoms such as numbness, pain or tingling in parts of the body.
Multiple sclerosis signs and symptoms may differ greatly from person to person and over the course of the disease depending on the location of affected nerve fibers.
Common symptoms include:
- Numbness or weakness in one or more limbs that typically occurs on one side of your body at a time
- Electric-shock sensations that occur with certain neck movements, especially bending the neck forward (Lhermitte sign)
- Lack of coordination
- Unsteady gait or inability to walk
- Partial or complete loss of vision, usually in one eye at a time, often with pain during eye movement
- Prolonged double vision
- Blurry vision
- Problems with sexual, bowel and bladder function
- Slurred speech
- Cognitive problems
- Mood disturbances
When to see a doctor
See a doctor if you experience any of the above symptoms for unknown reasons.
Disease course
Most people with MS have a relapsing-remitting disease course. They experience periods of new symptoms or relapses that develop over days or weeks and usually improve partially or completely. These relapses are followed by quiet periods of disease remission that can last months or even years.
Small increases in body temperature can temporarily worsen signs and symptoms of MS . These aren't considered true disease relapses but pseudorelapses.
At least 20% to 40% of those with relapsing-remitting MS can eventually develop a steady progression of symptoms, with or without periods of remission, within 10 to 20 years from disease onset. This is known as secondary-progressive MS .
The worsening of symptoms usually includes problems with mobility and gait. The rate of disease progression varies greatly among people with secondary-progressive MS .
Some people with MS experience a gradual onset and steady progression of signs and symptoms without any relapses, known as primary-progressive MS .
More Information
Multiple sclerosis care at Mayo Clinic
- Multiple sclerosis: Can it cause seizures?
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
The cause of multiple sclerosis is unknown. It's considered an immune mediated disease in which the body's immune system attacks its own tissues. In the case of MS , this immune system malfunction destroys the fatty substance that coats and protects nerve fibers in the brain and spinal cord (myelin).
Myelin can be compared to the insulation coating on electrical wires. When the protective myelin is damaged and the nerve fiber is exposed, the messages that travel along that nerve fiber may be slowed or blocked.
It isn't clear why MS develops in some people and not others. A combination of genetics and environmental factors appears to be responsible.
Risk factors
These factors may increase your risk of developing multiple sclerosis:
- Age. MS can occur at any age, but onset usually occurs around 20 and 40 years of age. However, younger and older people can be affected.
- Sex. Women are more than 2 to 3 times as likely as men are to have relapsing-remitting MS .
- Family history. If one of your parents or siblings has had MS , you are at higher risk of developing the disease.
- Certain infections. A variety of viruses have been linked to MS , including Epstein-Barr, the virus that causes infectious mononucleosis.
- Race. White people, particularly those of Northern European descent, are at highest risk of developing MS . People of Asian, African or Native American descent have the lowest risk. A recent study suggests that the number of Black and Hispanic young adults with multiple sclerosis may be greater than previously thought.
- Climate. MS is far more common in countries with temperate climates, including Canada, the northern United States, New Zealand, southeastern Australia and Europe. Your birth month may also affect the chances of developing multiple sclerosis, since exposure to the sun when a mother is pregnant seems to decrease later development of multiple sclerosis in these children.
- Vitamin D. Having low levels of vitamin D and low exposure to sunlight is associated with a greater risk of MS .
- Your genes. A gene on chromosome 6p21 has been found to be associated with multiple sclerosis.
- Obesity. An association with obesity and multiple sclerosis has been found in females. This is especially true for female childhood and adolescent obesity.
- Certain autoimmune diseases. You have a slightly higher risk of developing MS if you have other autoimmune disorders such as thyroid disease, pernicious anemia, psoriasis, type 1 diabetes or inflammatory bowel disease.
- Smoking. Smokers who experience an initial symptom that may signal MS are more likely than nonsmokers to develop a second event that confirms relapsing-remitting MS .
Complications
People with multiple sclerosis may also develop:
- Muscle stiffness or spasms
- Severe weakness or paralysis, typically in the legs
- Problems with bladder, bowel or sexual function
- Cognitive problems, like forgetfulness or word finding difficulties
- Mood problems, such as depression, anxiety or mood swings
- Seizures, though very rare
- What is multiple sclerosis? National Multiple Sclerosis Society. https://www.nationalmssociety.org/What-is-MS. Accessed June 2, 2022.
- Daroff RB, et al. Multiple sclerosis and other inflammatory demyelinating diseases of the central nervous system. In: Bradley's Neurology in Clinical Practice. 7th ed. Philadelphia, Pa.: Elsevier Saunders; 2012. https://www.clinicalkey.com. Accessed June 2, 2022.
- Ferri FF. Multiple sclerosis. In: Ferri's Clinical Advisor 2019. Philadelphia, Pa.: Elsevier; 2019. https://www.clinicalkey.com. Accessed June 2, 2022.
- Olek MJ. Clinical presentation, course, and prognosis of multiple sclerosis in adults. https://www.uptodate.com/contents/search. Accessed June 2, 2022.
- Wingerchuk DM (expert opinion). Mayo Clinic, Phoenix/Scottsdale, Ariz. Jan. 21, 2019.
- Ciccarelli O. Multiple sclerosis in 2018: New therapies and biomarkers. The Lancet. 2019; doi: 10.1016/S14744422 (18)30455-1.
- Keegan BM. Therapeutic decision making in a new drug era in multiple sclerosis. Seminars in Neurology. 2013; doi:10.1055/s0033-1345709.
- Goldman L, et al., eds. Multiple sclerosis and demyelinating conditions of the central nervous system. In: Goldman-Cecil Medicine. 25th ed. Philadelphia, Pa.: Saunders Elsevier; 2016. https://www.clinicalkey.com. Accessed Jun. 2, 2022.
- Lotze TE. Pathogenesis, clinical features, and diagnosis of pediatric multiple sclerosis. https://www.uptodate.com/contents/search. Accessed June 2, 2022.
- Kantarci OH, et al. Novel immunomodulatory approaches for the management of multiple sclerosis. Clinical Pharmacology & Therapeutics. 2014; doi:10.1038/clpt.2013.196.
- Olek MJ. Disease-modifying treatment of relapsing-remitting multiple sclerosis in adults. https://www.uptodate.com/contents/search. Accessed June 2, 2022.
- Olek MJ, et al. Treatment of acute exacerbations of multiple sclerosis in adults. https://www.uptodate.com/contents/search. Accessed June 2, 2022.
- Wingerchuk DM. Multiple sclerosis: Current and emerging disease-modifying therapies and treatment strategies. Mayo Clinic Proceedings. 2014; doi:10.1016/j.mayocp.2013.11.002.
- Pizzorno JE, et al. Multiple sclerosis. In: Textbook of Natural Medicine. 4th ed. St. Louis, Mo.: Churchill Livingstone Elsevier; 2013. https://www.clinicalkey.com. Accessed June 2, 2022.
- Olek MJ, et al. Evaluation and diagnosis of multiple sclerosis in adults. https://www.uptodate.com/contents/search. Accessed June 2, 2022.
- Gaetani L, et al. 2017 revisions of McDonald criteria shorten the time to diagnosis of multiple sclerosis in clinically isolated syndromes. Journal of Neurology. 2018;265:2684.
- http://onlinelibrary.wiley.com/doi/10.1002/ana.22366.
- Olek MJ, et al. Pathogenesis and epidemiology of multiple sclerosis.
- Ingram G, et al. Cannabis and multiple sclerosis. Practical Neurology. 2019; doi:10.1136/practneurol-2018-002137.
- Olek MJ, et al. Symptom management of multiple sclerosis in adults. https://www.uptodate.com/contents/search. Accessed June 2, 2022.
- Yadav Y, et al. Summary of evidence-based guideline: Complementary and alternative medicine in multiple sclerosis. Neurology. 2014; doi: 10.1212/WNL.0000000000000250.
- Nimmagadda R. Allscripts EPSi. Mayo Clinic. April 22, 2022.
- National MS Society. Network of Pediatric MS Centers. https://www.nationalmssociety.org/What-is-MS/Who-Gets-MS/Pediatric-MS/Care-for-Pediatric-MS. Accessed June 2, 2022.
- Rodriguez M. Plasmapheresis in acute episodes of fulminant CNS inflammatory demyelination. Neurology. 1993; doi:10.1212/wnl.43.6.1100.
- Deb C. CD8+ T cells cause disability and axon loss in a mouse model of multiple sclerosis. PLoS One. 2010; doi:101371/journal.pone.0012478.
- FDA approves new drug to treat multiple sclerosis. U.S. Food & Drug Administration. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm549325.htm. Accessed June 1, 2022.
- Keegan BM (expert opinion). Mayo Clinic, Rochester, Minn. January 15, 2019.
- FDA approves new oral drug to treat multiple sclerosis. U.S. Food and Drug Administration. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm634469.htm. Accessed June 2, 2022.
- Kappos L, et al. Siponimod versus placebo in secondary progressive multiple sclerosis (EXPAND): A double-blind, randomized, phase 3 study. The Lancet. 2018; doi: 10.1016/S0140-6736(18)30475-6.
- Marin Collazo IV (expert opinion). Mayo Clinic, Rochester, Minn. April 2, 2019.
- AskMayoExpert. Multiple sclerosis. Mayo Clinic; 2020.
- AskMayoExpert. Medication monitoring guidelines. Mayo Clinic; 2020.
- Vumerity. National MS Society. https://www.nationalmssociety.org/Treating-MS/Medications/Vumerity. Accessed March 16, 2020.
- Gianfrancesco M, et al. Obesity during childhood and adolescence increases susceptibility to multiple sclerosis after accounting for established genetic and environmental risk factors. Obesity Research and Clinical Practice. 2014; doi.org/10.1016/j.orcp.2014.01.002.
- Pantavou KG, et al. Season of birth and multiple sclerosis: A systematic review and multivariate meta-analysis. Journal of Neurology. 2020; doi:10.1007/s00415019-09346-5.
- Cifu DX, et al., eds. Multiple sclerosis. In Braddom's Physical Medicine and Rehabilitation. 6th ed. Elsevier; 2021 https://www.clinicalkey.com. Accessed Jun. 2, 2022.
- Langer-Gould AM, et al. Racial and ethnic disparities in multiple sclerosis prevalence. Neurology. 2022; doi:10.1212/WNL.0000000000200151.
- Kasper LH, et al. Immunomodulatory activity of interferon-beta. Annals of Clinical and Translational Neurology. 2014; doi:10.1002/acn3.84.
- Goldschmidt CH, et al. Re-evaluating the use of IFN-B and relapsing multiple sclerosis: Safety, efficacy and place in therapy. Degenerative Neurological and Neuromuscular Disease. 2020; doi:10.2147/DNND.S224912.
- Kieseie BC. The mechanism of action of interferon-B in relapsing multiple sclerosis. Central Nervous System Drugs. 2011; doi:10.1007/s10067-008-0972-3.
- Betaseron. Bayer AG; 1993. www.bayer.com. Accessed Jun. 1, 2022.
- Hauser SL, et al. Ofatumumab versus teriflunomide in multiple sclerosis. The New England Journal of Medicine. 2020; doi:10.1056/NEJMoa1917246.
- Kesimpta. Novartis; 2020. www.novartis.com. Accessed Jun. 1, 2022.
- Marin Collazo V (expert opinion). Mayo Clinic. June 13, 2020.
- Olek MJ. Treatment of progressive multiple sclerosis in adults. https://www.uptodate.com/contents/search. Accessed Jun. 2, 2022.
- Wingerchuk DM, et al. Disease modifying therapies for relapsing multiple sclerosis. British Medical Journal. 2016; doi:10.1136/bmj.i3518.
- Saadeh RS, et al. CSF kappa free light chains: Cutoff validation for diagnosing multiple sclerosis. Mayo Clinic Proceedings. 2022; doi:10.1016/j.mayocp.2021.09.014.
- Goldschmidt C, et al. Advances in the treatment of multiple sclerosis. Neurologic Clinics. 2021; doi:10.1016/j.ncl.2020.09.002.
- Bafiertam. Banner Life Sciences LLC; 2013. www.bannerls.com. Accessed Jun. 1, 2022.
- Baliertam delayed release capsule. Banner Life Sciences LLC; 2013. www.bannerls.com. Accessed Jun. 1, 2022.
- Oral ponesimod versus teriflunomide in relapsing multiple sclerosis (OPTIMUM). ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT02425644. Accessed Jun. 2, 2022.
- Ponvory. Janssen Pharmaceuticals; 2021. www.janssen.com. Accessed Jun. 1, 2022.
- Torke S, et al. Inhibition of Bruton's tyrosine kinase as a novel therapeutic approach in multiple sclerosis. Expert Opinion on Investigational Drugs. 2020.
- Nash RA, et al. High-dose immunosuppressive therapy and autologous hematopoietic cell transplantation for relapsing-remitting multiple sclerosis (HALT-MS): A 3-year interim report. Journal of the American Medical Association Neurology. 2015; doi:10.1001/jamaneurol.2014.3780.
- Reston, et al. Autologous hematopoietic cell transplantation for multiple sclerosis: A systematic review. Multiple Sclerosis. 2011; doi:10,1177/1352458510383609.
- Petrou P, et al. Beneficial effects of autologous mesenchymal stem cell transplantation in active progressive multiple sclerosis. Brain. 2020; doi:10.1093/brain/awaa333.
- Liang J, et al. Allogenic mesenchymal stem cell transplantation in the treatment of multiple sclerosis. Multiple Sclerosis. 2009; doi:10.1177/1352458509104590.
- Wingerchuk DM, et al. Multiple sclerosis: Current and emerging disease-modifying therapies and treatment strategies. Mayo Clinic Proceedings. 2014; doi:101016/j.mayocp.2013.11.002.
- Multiple sclerosis information page. National institute of neurological disorders and stroke. https://www.ninds.nih.gov/Disorders/All-Disorders/Multiple-Sclerosis-Information-Page. Accessed Jun. 2, 2022.
- Sadovnick AD. Genetic background of multiple sclerosis. Autoimmunity Reviews. 2012; doi:10.1016/j.autrev.2011.05.007.
- Acetyl-L-carnitine: Can it relieve MS fatigue?
- Demyelinating disease: What can you do about it?
- Emerging treatments for multiple sclerosis
- Exercise and multiple sclerosis
- Explaining multiple sclerosis
- Infographic: Multiple Sclerosis
- MRI multiple sclerosis lesions
- Multiple sclerosis FAQs
- Physical therapy for multiple sclerosis
- Vitamin D and MS: Any connection?
- Vitamins for MS: Do supplements make a difference?
Associated Procedures
- Lumbar puncture (spinal tap)
Mayo Clinic in Rochester, Minnesota, Mayo Clinic in Phoenix/Scottsdale, Arizona, and Mayo Clinic in Jacksonville, Florida, have been ranked among the best Neurology & Neurosurgery hospitals in the nation for 2024-2025 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Help transform healthcare
Your donation can make a difference in the future of healthcare. Give now to support Mayo Clinic's research.

Connect with others who understand.

- All Resources MS Symptoms Mental Health Symptoms
Does Multiple Sclerosis Cause Lack of Empathy?

Empathy can be described as “the action of understanding, being aware of, being sensitive to, and vicariously experiencing the feelings, thoughts, and experience of another.” While sympathy means having a genuine concern for others, empathy goes deeper. Empathy is the ability to put yourself in someone else’s shoes and feel what they’re feeling.
Research has raised questions about whether multiple sclerosis (MS) changes people’s empathy levels. However, results showing reduced empathy with MS are not proven in all studies and certainly don’t apply to everyone. In people with MS, the level of empathy can vary widely due to factors like personality differences. This means some people may show more empathy than others.
Everyone has different levels of empathy. Empathy may be determined by your natural-born personality, your emotional awareness, how you were raised, and your capacity for connection based on current and past life circumstances.
If you find yourself with less mental and emotional space for others, you’re not alone. The physical changes of MS, along with the social impacts, can change how you view and interact with the people around you.
Here’s how MyMSTeam members have described their experiences and what the research says about MS and empathy.
Impact of Fatigue and Other MS Symptoms
The physical effects of MS, like fatigue , can leave you with less energy and motivation to express empathy with others. Fatigue can make it harder to actively listen to others for long periods of time. In addition, there’s evidence that higher levels of MS-related fatigue are associated with lower levels of empathy.
If you cut a conversation short because you need to rest, others may mistake this as a lack of empathy. “I feel so guilty for frequently mentally ‘checking out’ with my family,” said a MyMSTeam member. Communicating and educating your loved ones about why you can’t always be as emotionally available when you’re tired can help.

“I feel so guilty for frequently mentally 'checking out' with my family.” — A MyMSTeam member
MS also affects cognitive functions. Brain lesions from MS may lead to executive functioning changes that affect how you think and process information. Research suggests that around half of people with MS experience cognitive impairments. People with MS may also have reduced social understanding, which is separate from any other cognitive difficulties they might experience. Doctors think that brain dysfunction could affect aspects of empathy, such as the ability to understand another person’s emotions. While research shows that people with MS may struggle to interpret other people’s facial expressions, this doesn’t necessarily translate to social problems like a lack of empathy.
Mental and Emotional Changes From MS
MyMSTeam members have said they struggle with sensory overload and depression that make it more difficult to be open and present with loved ones.
“Sensory overload is a huge problem I have, and it leads to feeling extremely overwhelmed and agitated,” described one member. “Sometimes when this happens, I get angry and snap over simple things. In addition, I have a hard time focusing and a poor attention span. Friends tell me sometimes it seems like I’m daydreaming, and I just stare into space. … I have become depressed and extremely moody .”
Other members have trouble opening up and being vulnerable. “Emotional issues sometimes make it hard to communicate with people — among other things, about the emotional issues, which is a catch-22,” explained one member.
Another wrote, “Very rarely do I confide in people about personal matters … be it health or marriage or anything sensitive. I come from quite a stoic family, and it just isn’t done. I’ve also narrowed down my pool of friends to what I can now count on one hand.”
It shouldn’t come as a surprise that a major life change, like an MS diagnosis, affects your social life and well-being. Sometimes issues like being easily distracted or emotionally “closed” are heightened by the added stress of MS . In addition, depression and anxiety are common in MS and may cause a disconnection from others.
Feeling Misunderstood by Loved Ones
These problems can go both ways. Many MyMSTeam members feel a lack of empathy from their loved ones. Insensitive remarks put them on the defensive. As a result, they’re reluctant to share and connect with others.
“My family tries to be supportive,” said one member. “They have noticed the changes, and when I apologize after getting angry, they say, ‘It’s OK, I know it's because of your MS.’ But sometimes I can't help but think they don’t truly understand even though they try to. I do often feel alone. So in response to the people who tell me, ‘You are lucky,’ I say no, I am not lucky. I have MS. I have many more symptoms that I struggle with on a daily basis than you can see.”
“My family tries to be supportive. But sometimes I can't help but think they don't truly understand, even though they try to. I do often feel alone." — A MyMSTeam member
Another member wrote, “While my husband and kids are wonderfully supportive, my immediate family continue to deny and ignore my ‘situation.’ Having your sister continually refer to being on long-term disability as being retired and ‘able to do whatever I want’ is not only frustrating, but it hurts.”
Other members have said the physical changes of MS affect their self-esteem and lead to isolation.
“I don’t like myself, although I know it’s only the MS. For years, when I was not able to walk, I didn't want to associate with anyone. There was little understanding of what I was going through from my wife and children, who went on living their lives and having friends. I did not want friends. I wanted nobody,” explained one member.
Hearing the experiences of others helps by letting you know you’re not alone. Although these negative feelings are normal, they can also be temporary and change over time.
Getting Help for Mood Changes
MyMSTeam members have detailed their hard times and shared how they found a positive path forward.
“This time last year, I had a double relapse and was off work for over four months,” said one member. “My specialist recommended for me to see a psychologist. It was life-changing. I had 10 hour-long sessions with a professional who understood MS medically and emotionally. We talked about the grieving process, how my body was changing, and that I didn’t feel feminine anymore. I couldn’t talk about how I really felt with loved ones because I could see the sadness in their eyes. We talked about how sad I felt because I couldn’t run and walk anymore. We talked about mindfulness and acceptance, and strategies for coping if I felt down.”
“My specialist recommended for me to see a psychologist. It was life-changing." — A MyMSTeam member
Other members have discovered how to adjust their mindset regarding stress and relationships.
“Learning to let go of things that are out of our control has helped me tremendously,” said one member. “Once I did this, other stresses became more apparent. I’ve been eliminating those sources of stress (and those people, too) from my life. It has given me such a greater quality of life and, I believe, helped me manage my MS more, too.”
Another described how they found a new sense of hope and peace. “My life has improved in a lot of ways, has changed in other ways, for the best. I’ve had to remove myself from very unhealthy relationships and distance myself from people I love because they didn’t understand what my life is like on a daily basis. I don’t push myself on anyone and don’t expect anyone to be in my life if they don’t want to be.”
If you’re feeling stuck in a negative place, a licensed mental health professional can help you adjust your thinking and manage your expectations of others to help reduce feelings of disappointment and anger. z is also a good option to improve communication and understanding.
Finding Support and Compassion on MyMSTeam
Research tells one side of the story, but real people with MS tell another. Empathy is easy to find on MyMSTeam where members offer valuable insights on living well with MS.
“You have to remember, it’s still the lovely you inside your body even though your body is slow,” said one member. “Keep your sense of humor, talk openly to your friends when you need to, and have a good laugh and cry. We only have one chance at happiness and loving our families, friends, and experiences.”
Feeling misunderstood by family and friends is a common experience for members of MyMSTeam. But tapping into your emotions and practicing empathy with others (who simply may not understand or have the capacity to accept your disease) can help you from feeling alone. You deserve empathy from others, too. Seek support from your team, your primary care doctor, and communities of people with MS who get what you’re going through.
Talk With Others Who Understand
MyMSTeam is the social network for people with multiple sclerosis and their family members. On MyMSTeam, more than 214,000 members come together to ask questions, give advice, and share their stories with others who understand life with MS.
Do you find it harder to be empathetic since being diagnosed with MS? Have you been able to find empathy from others for your experiences with MS? Share your story in a comment below or on MyMSTeam .
- Empathy and Theory of Mind in Multiple Sclerosis: A Meta-Analysis — Frontiers in Psychiatry
- Empathy in Multiple Sclerosis — Correlates With Cognitive, Psychological and Occupational Functioning — Multiple Sclerosis and Related Disorders
- Symptoms Multiple Sclerosis — NHS
- Emotional Changes — National Multiple Sclerosis Society
RELATED QUESTIONS
- What are conditions related to MS? See answer
- What parts of the body can MS cause issues? See answer
- How does MS progress over time? See answer
- What complications can come from MS? See answer
Get medically-reviewed resources delivered to your inbox
Thank you for subscribing, become a member to get even more:.

sign up for free
Attach a gif
Click on a gif to attach it
We'd love to hear from you! Please share your name and email to post and read comments.
You'll also get the latest articles directly to your inbox.
Subscribe now to ask your question, get answers, and stay up to date on the latest articles.
Get updates directly to your inbox.

Hormones and MS: 8 Facts To Know
Related articles, how does ms cause disability 4 ways it can affect mobility and function.

8 Tips for Managing Stress With MS (VIDEO)

MS Symptoms and COVID-19 Vaccines: Is There a Relapse Risk?

From Triathlete to MS Champion: How Paige Found Her New Path

How I Learned To Listen to My Body With MS

MS Symbols: Ribbons, Butterflies, and Why Awareness Matters

Recent Articles
How is ms fatigue measured.

The Marburg Course: Understanding Severe and Rapid MS

Healthy Eating and Multiple Sclerosis

5 Uncommon Symptoms of Relapsing MS

Top 5 Most Common MS Symptoms Reported by MyMSTeam Members

Vitamin D Levels and MS: Top Facts You Need To Know

Browse By Subject
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
August 7, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
Current challenges evaluated for measuring and treating fatigue in multiple sclerosis
by Kessler Foundation
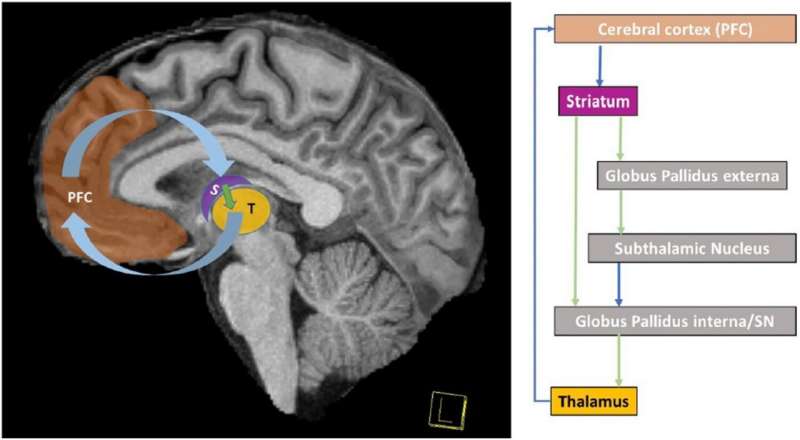
Kessler Foundation research scientist John DeLuca, Ph.D., has published a clinical article in Journal of Neurology , shedding light on the elusive nature of fatigue in multiple sclerosis (MS) and its implications for treatment. The study provides a comprehensive review of current challenges in defining, measuring, and treating MS-related fatigue, offering new insights and directions for future research.
The article, "Fatigue in multiple sclerosis: can we measure it and can we treat it?" , was published on July 5, 2024. It highlights the multidimensional nature of fatigue, emphasizing the ongoing struggle to define it accurately and measure it effectively. Dr. DeLuca identified over 250 scales used to assess fatigue but noted significant content validity issues, raising questions about their effectiveness.
"Our ability to define, measure, and treat fatigue in MS has only marginally improved despite over a century of research," said Dr. DeLuca, senior vice president for research and training at the Foundation.
"This study underscores the need for innovative approaches to better understand and address this complex symptom. It also highlights the necessity of distinguishing fatigue from other related symptoms and developing more precise measurement tools. Addressing these challenges is crucial for improving the quality of life for individuals with MS."
Fatigue affects up to 90 percent of individuals with MS, significantly impacting their daily lives. Despite its prevalence, defining fatigue remains challenging due to its subjective and multifaceted nature.
The article reviews historical and contemporary definitions of fatigue, critiques existing measurement tools for their lack of clarity and consistency, and explores the subjective nature of fatigue and its correlation with other symptoms such as depression, pain, and cognitive complaints.
Furthermore, Dr. DeLuca examines the brain's role in fatigue, proposing that disruptions in the cortico-striato-thalamo-cortical loop contribute to central fatigue.
"Advanced MRI imaging techniques have shown that central fatigue correlates with disruptions in this brain network. Recent research indicates that motivational incentives can reduce fatigue by stimulating the fronto-striatal network, suggesting new potential treatment approaches," he emphasized.
How can we treat fatigue?
The study discusses both pharmacological and non-pharmacological treatments for fatigue in MS. Pharmacological treatments, such as amantadine, modafinil, and methylphenidate, have shown limited effectiveness.
In contrast, the article also explores non-pharmacological treatments for fatigue, such as cognitive-behavioral therapy and exercise, which have shown moderate to large effects in reducing fatigue symptoms. Additionally, the potential of novel approaches involving the brain's reward system is mentioned, suggesting that motivational incentives could play a crucial role in managing fatigue in MS patients.
Explore further
Feedback to editors

Pre-surgical antibody treatment might prevent heart transplant rejection
5 hours ago

Researchers enhance natural killer cells to target pediatric brain cancer

Study reveals OLAH enzyme underpins lethal respiratory viral disease

MRI technique accurately predicts heart failure risk in general population
6 hours ago

Harnessing deep learning, new research suggests phased COVID-19 vaccine rollout was a mixed bag for mental health
7 hours ago

New findings suggest alternative mechanisms behind Alzheimer's disease

Hooked on a feeling: Opioids evoke positive feelings through a newly identified brain region

Comprehensive atlas of normal breast cells offers new tool for understanding breast cancer origin


Parents who use humor have better relationships with their children, study finds

Researchers urge Medicare coverage of driving assessments for at-risk, older adults
Related stories.

Psoriasis, with or without psoriatic arthritis, associated with fatigue
Jul 1, 2024

Fatigue with rheumatoid arthritis tied to disease activity, education level
Jun 26, 2024

Neurodivergent children are twice as likely to experience chronic disabling fatigue in adolescence
Jul 29, 2024

Study of cognitive fatigue across different tasks and populations provides new insights
Dec 27, 2023

Coping with cancer-related fatigue
Jun 18, 2024

Pupil contraction indicates hidden cognitive fatigue in prolonged esports play across various skill levels
Apr 8, 2024
Recommended for you

State-of-the-art brain recordings reveal how neurons resonate
10 hours ago

Biodegradable electronic tent technology offers less invasive brain disease diagnosis
9 hours ago

How experience shapes neural connectivity in the brain
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Multiple Sclerosis & Anxiety: What’s the Link?
- Coping Strategies
How to Get Help
Frequently asked questions.
Many people with multiple sclerosis (MS) experience mental health symptoms, including anxiety . The uncertain nature of the condition—in which relapses and new symptoms seemingly can strike at any time—is thought to be a major reason why. But the immune system's attack on the brain and the resulting neuroinflammation and neurological changes also seem to play a role.
Read on to learn about how MS can lead to anxiety and how to cope.
FG Trade / Getty Images
MS and Anxiety
It's common for people with MS to experience symptoms of anxiety or have anxiety disorders.
The exact prevalence of people with MS experiencing anxiety symptoms varies among studies, but it is believed to be between 34% and 43%. This is much higher than the estimated prevalence of about 18% in the U.S. population overall.
Despite the high occurrence, anxiety in people with MS remains understudied.
There is some evidence that anxiety may be related to neuroinflammation and deficits in frontal lobe functioning (including attention, problem-solving, and memory retrieval) that occur with MS. Research also suggests that it may be due to living with the unpredictability of MS rather than the physical disease process.
MS symptoms and progression can vary. Concern about the potential seriousness of symptoms and outcome of future episodes may contribute to severe and/or prolonged anxiety in people with MS. Research suggests that anxiety tends to be higher at the onset of the condition.
Increased anxiety in people with MS is also associated with:
- Gender (both MS itself and anxiety in MS are more common in women )
- The presence of moderate to severe depression
- Substance use, including smoking and alcohol
- Pain and fatigue
- Lower disability levels
- Younger age of onset
- Greater social stress
- Limited social support
Demyelination (damage to the protective covering surrounding nerve cells), damage to nerve fibers, and some of the medications used to treat MS (such as corticosteroids ) may also contribute to emotional changes and anxiety in people with MS.
Left untreated, anxiety in people with MS can lead to:
- Impaired social functioning and decreased social interaction
- Impaired cognitive functioning
- Lowered treatment compliance
- Lower quality of life
- Physical symptoms or worsening MS symptoms
- Increased thoughts or actions of self-harm or suicide (particularly if depression is also present)
Help Is Available
If you or a loved one is having thoughts of suicide, call 911 or the National Suicide Prevention Lifeline at 988 . For more mental health resources, see our National Helpline Database.
Symptoms of Anxiety
Anxiety can have both physiological and psychological symptoms.
Physiological symptoms may include:
- Shortness of breath
- Increased heart rate or heart palpitations
- Hot or cold sensations
- Tense muscles
- Restlessness
- Sleep difficulties, especially trouble falling asleep
- Frequent urination
Psychological symptoms include:
- Frequently feeling worried, guilty, or out of control
- Racing thoughts
- Difficulty making decisions
- Chronic feelings of unhappiness
- Feeling inadequate, criticized, or easily embarrassed
- Inflexibility and being less willing to make changes
- Hostility or anger toward others
- Repeating certain behaviors or thoughts
- Over-anticipating things
- Excessive concern with physical health
- Thinking negatively about the future
Anxiety or MS Symptoms?
Anxiety symptoms can overlap with MS symptoms. Talk with your healthcare provider about all of your symptoms to get an overall picture of what you are experiencing.
Strategies for Coping With MS Anxiety
Anxiety with MS can be managed with professional treatment and coping strategies.
For some, medication may be beneficial. Options include:
- Antidepressants : Including Celexa ( citalopram ), Lexapro ( escitalopram ), Effexor ( venlafaxine ), and Cymbalta ( duloxetine hydrochloride )
- Antianxiety medications (or benzodiazepines) : Including Valium ( diazepam ), for short-term use
Working with a mental health professional can help a person with MS learn to manage their anxiety symptoms.
Some strategies include:
- Cognitive behavioral therapy (CBT) : Learning to identify problematic thoughts and behaviors and changing them into productive ones
- Biofeedback : Learning to control body responses
- Acceptance and commitment therapy (ACT) : Identifying what is most valuable to the person and finding a way to pursue it
- Support groups : Interacting with others who are also living with anxiety and MS
Mindfulness
Practicing mindfulness techniques and exercises, whether led by a professional or on your own, may help with anxiety. Meditation and mindfulness help the brain develop more interconnections and physically change the brain for good.
Examples include:
- Guided imagery
- Body scan exercise
- Mindfulness-based stress reduction (MBSR)
Other Measures
Physical exercise and being mobile to the best of your ability may help improve anxiety symptoms. Practicing yoga is a great way to combine physical activity with mindfulness.
Increased social support—including emotional, technical, and informational support—from people such as family members, friends, coworkers, healthcare professionals, and other people with MS has been shown to help mitigate the impact of anxiety and depression.
Don't Ignore Symptoms
Identifying anxiety early can make a big difference in treating and living with the condition. If you notice signs of anxiety , don't wait to talk to your healthcare provider.
Finding the help that works best for you is important. You can start by talking to your healthcare provider. They can help you find resources and make a referral to a specialist or mental health professional if necessary.
The format with which you receive help is also important. In-person sessions are an option, but remote therapy is also a promising choice, especially if access is an issue.
When looking for a therapist or other professional to help with your anxiety, it can help to have some questions prepared ahead of time. For example:
- What is your experience working with people who have MS and anxiety?
- Which therapies and relaxation techniques do you use?
- Are your services covered by my insurance?
- Do you involve care partners and family members in the treatment?
- What are your feelings on using medication for anxiety?
The National Multiple Sclerosis Society provides a search tool that can help you find different types of resources available to you.
It is common for people with MS to experience symptoms of anxiety or anxiety disorders. This may be due to neuroinflammation as a result of MS, or the psychological stress that comes with being diagnosed with a chronic condition. Left untreated, this anxiety can affect functioning and quality of life.
Treatments like medication, therapy, and mindfulness exercises can help with anxiety management. Physical activity, such as yoga, and increased social support can also provide benefits.
A Word From Verywell
While looking after your physical health with MS, it's just as important to care for your mental health. If you are experiencing symptoms of anxiety, talk to your healthcare provider or a mental health professional about what you're feeling. Anxiety can be treated and managed alongside MS.
If left untreated, anxiety can negatively affect many areas of your health, including MS symptoms.
Neuroinflammation (an inflammatory response within the brain or spinal cord) plays a role in the presence of anxiety with MS. Anxiety can also be the result of being diagnosed with a life-changing condition like MS.
Gay MC, Bungener C, Thomas S, et al. Anxiety, emotional processing and depression in people with multiple sclerosis . BMC Neurol . 2017;17(1):43. doi:10.1186/s12883-017-0803-8
Rossi S, Studer V, Motta C, et al. Neuroinflammation drives anxiety and depression in relapsing-remitting multiple sclerosis . Neurology . 2017;89(13):1338-1347. doi:10.1212/WNL.0000000000004411
Multiple Sclerosis Association of America. Anxiety .
Boeschoten RE, Braamse AMJ, Beekman ATF, Cuijpers P, van Oppen P, Dekker J, Uitdehaag. Prevalence of depression and anxiety in Multiple Sclerosis: A systematic review and meta-analysis . J Neurol Sci . 2017;372:331-341. doi:10.1016/j.jns.2016.11.067
Anxiety and Depression Association of America. Did you know? .
Pham T, Jetté N, Bulloch AGM, Burton JM, Wiebe S, Patten SB. The prevalence of anxiety and associated factors in persons with multiple sclerosis . Multiple Sclerosis and Related Disorders . 2018;19:35-39. doi:10.1016/j.msard.2017.11.003
Guimarães J, Sá MJ. Cognitive dysfunction in multiple sclerosis . Front Neur . 2012;3. doi:10.3389/fneur.2012.00074
Butler E, Matcham F, Chalder T. A systematic review of anxiety amongst people with multiple sclerosis . Multiple Sclerosis and Related Disorders . 2016;10:145-168. doi:10.1016/j.msard.2016.10.003
Podda J, Ponzio M, Messmer Uccelli M, et al. Predictors of clinically significant anxiety in people with multiple sclerosis: A one-year follow-up study . Multiple Sclerosis and Related Disorders . 2020;45:102417. doi:10.1016/j.msard.2020.102417
Hanna M, Strober LB. Anxiety and depression in multiple sclerosis (MS): antecedents, consequences, and differential impact on well-being and quality of life . Multiple Sclerosis and Related Disorders . 2020;44:102261. doi:10.1016/j.msard.2020.102261
Henry A, Tourbah A, Camus G, et al. Anxiety and depression in patients with multiple sclerosis: the mediating effects of perceived social support . Multiple Sclerosis and Related Disorders . 2019;27:46-51. doi:10.1016/j.msard.2018.09.039
National Multiple Sclerosis Society. Emotional changes .
Johns Hopkins Medicine. Multiple sclerosis and mental health: 3 common challenges .
Vissicchio NA, Altaras C, Parker A, et al. Relationship between anxiety and cognition in multiple sclerosis . International Journal of MS Care . 2019;21(4):151-156. doi:10.7224/1537-2073.2018-027
Kidd T, Carey N, Mold F, et al. A systematic review of the effectiveness of self-management interventions in people with multiple sclerosis at improving depression, anxiety and quality of life . PLoS ONE . 2017;12(10):e0185931. doi:10.1371/journal.pone.0185931
Lardone A, Liparoti M, Sorrentino P, et al. Mindfulness meditation is related to long-lasting changes in hippocampal functional topology during resting state: a magnetoencephalography study . Neural Plast . 2018;2018:5340717. doi:10.1155/2018/5340717
Kolahkaj B, Zargar F. Effect of mindfulness-based stress reduction on anxiety, depression and stress in women with multiple sclerosis . Nurs Midwifery Stud . 2015;4(4):e29655. doi:10.17795/nmsjournal29655
Hasanpour-Dehkordi A, Jivad N, Solati K. Effects of yoga on physiological indices, anxiety and social functioning in multiple sclerosis patients: a randomized trial . J Clin Diagn Res . 2016;10(6):VC01-VC05. doi:10.7860/JCDR/2016/18204.7916
By Heather Jones Jones is a freelance writer with a strong focus on health, parenting, disability, and feminism.

- Acthar Gel self-injection option available in US, Mallinckrodt says
Pre-filled device available in two dosages, aimed at simplifying treatment

by Esteban Domínguez Cerezo, MS | August 9, 2024
Share this article:
People with multiple sclerosis (MS) and other conditions who use Mallinckrodt ‘s treatment Acthar Gel (repository corticotropin injection) now have a self-injection option, the company said.
Acthar Gel Single-Dose Pre-filled SelfJect is available in two dosages — 40 USP units/0.5 ml and 80 USP units/1.0 mL — that patients can give themselves subcutaneously (under the skin) by pressing a handle. The treatment had been available only in a multi-dose, vial-and-syringe package that required patients or their caregivers to draw precise amounts of the medication before administering it.
“The launch of SelfJect is a significant advancement for patients who take Acthar Gel as it is designed to simplify the injection process, help ensure accurate dosing, and has enhanced safety features,” Kostas Botsoglou, MD, managing partner of the Rheumatology Center of Western New York, said in a Mallinckrodt press release . “SelfJect supports patients by helping to make treatment easier to administer than a multi-dose vial and syringe, particularly for patients with dexterity issues.”
Acthar Gel contains a mixture of molecules similar to the adrenocorticotropic hormone (ACTH) and other small proteins that are made by the brain’s pituitary gland. The ACTH hormone can stimulate the production of cortisol, a natural anti-inflammatory molecule, which makes it suitable for a range of inflammatory and autoimmune conditions.
In MS, Acthar Gel is approved to treat acute relapses , or periods of worsening symptoms, to help patients recover faster and more effectively. It is usually considered as an alternative for patients who fail to respond adequately or cannot tolerate corticosteroids — medications that mimic the immune-suppressing action of cortisol and are also used to help control MS relapses. While the treatment does not alter the long-term course of the disease, it provides a tool for managing acute symptoms of MS .

Learning how to maintain good health was a lesson in endurance
Saving time, minimizing risk.
“I’m looking forward to being able to provide this option to appropriate patients in my practice to help them adhere to their treatment plans, which are intended to better their chances for improved outcomes,” Botsoglou said.
The recommended Acthar Gel dosage for MS relapse treatment is 80–120 units, given daily for two to three weeks. The pre-filled, color-coded devices will reduce preparation time and minimize the risk of accidental punctures with needles, Mallinckrodt said.
The multi-dose vial version, administered as a subcutaneous or intramuscular (into-the-muscle) injection, may involve several steps and require extra medical supplies such as needles and syringes, in addition to training for patients and caregivers. The older version will continue to be available for people who prefer that administration method or require doses other than 40 or 80 units, the company said.
“We know that managing chronic and acute inflammatory and autoimmune conditions can be difficult, and we’re proud to offer this new delivery device, designed to better support patients, caregivers, and medical professionals in managing appropriate conditions,” said Lisa French, Mallinckrodt executive vice president and chief commercial officer.
About the Author

Recent Posts
- Crying at Donald Duck, and other strange emotional reactions
- PIPE-307 shows potential to repair myelin in MS mouse model
Recommended reading
MS patients prefer Tysabri injection to intravenous infusion: Study
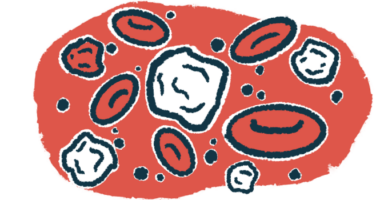
Immune signatures may predict MS course, treatment response
Briumvi, an infusion treatment for MS, granted 3 more patents
Subscribe to our newsletter.
Get regular updates to your inbox.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Neurol Ther
- v.7(1); 2018 Jun

Vitamin D and Multiple Sclerosis: A Comprehensive Review
Martina b. sintzel.
1 Medical Communication Services, Erlenbach, Zurich, Switzerland
Mark Rametta
2 Bayer HealthCare Pharmaceuticals, Whippany, NJ USA
Anthony T. Reder
3 Department of Neurology, University of Chicago, Chicago, IL USA
Associated Data
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Numerous observational studies have suggested that there is a correlation between the level of serum vitamin D and MS risk and disease activity. To explore this hypothesis, a literature search of large, prospective, observation studies, epidemiological studies, and studies using new approaches such as Mendelian randomization was conducted. Available data and ongoing research included in this review suggest that the level of serum vitamin D affects the risk of developing MS and also modifies disease activity in MS patients. Newer Mendelian randomization analyses suggest there is a causal relationship between low vitamin D level and the risk of MS. Post-hoc evaluations from two phase 3 studies, BENEFIT and BEYOND, support the findings of observational trials. Study limitations identified in this review recognize the need for larger controlled clinical trials to establish vitamin D supplementation as the standard of care for MS patients. Though there is increasing evidence indicating that lower vitamin D levels are associated with increased risk of MS and with greater clinical and brain MRI activity in established MS, the impact of vitamin D supplementation on MS activity remains inadequately investigated.
Introduction
Knowledge of the widespread effects of vitamin D on skeletal and non-skeletal functions, including immune functions, has developed considerably over the past 3 decades. Higher levels of vitamin D are associated with reduced risk for developing multiple sclerosis (MS), and with reduced clinical activity in established MS, including decreased risk of relapse and reduction in disease activity on brain MRI [ 1 , 2 ]. Vitamin D supplementation may diminish the risk of MS in the general population, as well as in children of mothers supplemented before and during pregnancy [ 3 ]. In the information that follows, we will summarize the available data on vitamin D, with a focus on vitamin D’s effects on the risk of onset of MS and on the disease course of MS.
Sources, Metabolism, and Biological Functions of Vitamin D
Vitamin D is a lipid-soluble vitamin, but acts like a hormone. Unlike a vitamin, which is an essential organic compound that cannot be synthesized by the body and must be ingested, vitamin D can be synthesized [ 4 ]. The active form of vitamin D, 1,25-dihydroxyvitamin D (1,25[OH] 2 VD), also known as calcitriol (Fig. 1 ) [ 5 ] has chemical similarities to typical hormones such as testosterone, estrogen, and cortisol [ 6 ]. The main sources of vitamin D are sunlight, diet, and supplementation (Fig. 2 ) [ 7 ]. UVB in the 290–315-nm range photolyses 7-dehydrocholesterol in the skin to form pre-vitamin D3, which then isomerizes to vitamin D3 or cholecalciferol [ 8 ]. Foods rich in vitamin D include fatty fish (e.g., salmon, mackerel), cod liver oil, egg yolk, and shiitake mushrooms. The plant form of vitamin D is called vitamin D2 or ergocalciferol [ 9 ]. Cholecalciferol and ergocalciferol are also available from fortified foods (e.g., milk, cereal, some orange juice, and cheeses) and vitamin supplements.

Chemical structures of the physiologically inactive vitamin D2 ( a ) and vitamin D3 ( b ); the main circulating vitamin D3 intermediate, 25-hydroxyvitamin D (25[OH]D) ( c ); and the bioactive vitamin D3 metabolite 1,25-dihydroxyvitamin D (1,25[OH] 2 VD) ( d ), or calcitriol if derived from vitamin D3 [ 5 ]

Sources and metabolism of vitamin D: The main sources of vitamin D are sunlight, diet, and supplementation. The primary forms of vitamin D are biologically inactive and need for their activation two hydroxylation steps in the liver and kidney. The hormonally active final product is 1,25-dihydroxyvitamin D [1,25(OH) 2 VDO]. 1,25(OH) 2 VD has a half-life of several hours, while the intermediate vitamin D form 25-hydroxyvitamin D [25(OH)D] has a relatively long half-life (20–60 days), and thus more accurately exemplifies the overall vitamin D stores in the body [ 7 ].
Reprinted from [ 7 ], with permission from Elsevier
Relative to sun exposure, diet is a poor source of vitamin D, providing only 40–400 IU per food serving, whereas whole-body UVB exposure for 20 min for a light-skinned person during the summer months will produce upwards of 10,000 IU of vitamin D [ 7 , 10 ]. However, UVB exposure and vitamin D production through the skin may be reduced with increased skin pigmentation, age, use of sunscreen, and environmental factors such as winter season, high latitude, pollution, cloud cover, and ozone levels [ 7 ]. For instance, sun exposure during most of the winter at latitudes above ~ 33° North (e.g., Atlanta, GA, USA; Casablanca, Morocco) and below ~ 33 degrees South (e.g., Santiago, Chile; New South Wales, Australia; Southern Cape of Africa) provides minimal, if any, vitamin D production [ 11 ].
Both forms of vitamin D, cholecalciferol, and ergocalciferol are biologically inactive and undergo an enzymatic transformation in the liver to 25(OH)D (calcidiol). Stimulated by parathyroid hormone, 25(OH)D goes through a second hydroxylation in the kidney or other tissues to 1,25(OH) 2 VD (also known as calcitriol if derived from vitamin D3), which is the active metabolite (Figs. 1 and and2) 2 ) [ 5 , 7 ]. 1,25(OH) 2 VD has a half-life of several hours, while 25(OH)D has a relatively long half-life (20–60 days), and thus more accurately exemplifies the overall vitamin D stores in the body. This supports the standard practice of measuring 25(OH)D in serum, and represents an integrated measure of vitamin D derived from both UVB exposure and diet. As a side note, most assays that evaluate 25(OH)D do not discriminate between the original forms of vitamin D (vitamin D3 or D2). However, the latter is usually a minor component because natural sources of ergocalciferol are scarce, and ergocalciferol is more rapidly catabolized than cholecalciferol [ 7 ].
The active metabolite 1,25(OH) 2 VD is released into the bloodstream and transported in the blood. It binds to the vitamin D binding protein in blood and on the surface of target tissues. 1,25(OH) 2 VD mediates its biological effects by binding to intracellular vitamin D receptor (VDR), which then recruits cofactors to form a transcriptional complex that binds to vitamin D response elements [ 12 ]. This association regulates the expression of at least 500 genes that drive a variety of physical functions [ 7 ]. The VDR is found in almost all human tissues, not just those participating in the classic actions of vitamin D, such as bone, gut, and kidney. The non-classic actions of VDR can be allocated to three main categories: regulation of hormone secretion, regulation of immune function, and regulation of cellular proliferation and differentiation [ 12 ].
Vitamin D deficiency has been classically attributed to bone health. In the early 1900s, rickets, a consequence of vitamin D deficiency, was very common among children in industrialized cities, and observations were made that sunlight exposure or cod liver oil may help to prevent this condition [ 10 ]. Other musculoskeletal consequences of vitamin D deficiency include secondary hyperparathyroidism, increased bone turnover, bone loss, and risk of low-trauma fractures. Today, we understand that VDR is widely distributed throughout the human body and involved in many biological functions. Vitamin D deficiency has been associated with numerous diseases including cancers, cardiovascular diseases, type 2 diabetes mellitus, infectious diseases, mental disorders, and autoimmune disorders such as type 1 diabetes mellitus, Crohn’s disease, and MS [ 10 , 13 ]. These diseases are all linked to vitamin D levels that are sufficient to prevent rickets, but are still suboptimal. Curiously, as rickets is no longer a problem, one might assume that the vitamin D deficiency problem is also no longer an issue. However, now that we know that autoimmunity may be related to low vitamin D levels, and that the incidence of autoimmune diseases has increased, we must consider if there is a higher vitamin D threshold related to autoimmunity, or if the environment changed since the Industrial Revolution.
Roles of Vitamin D in Immunity
Since multiple sclerosis (MS) is considered an autoimmune disease, it is of interest to review briefly the potential effects of vitamin D related to immune function. The active form of vitamin D plays an essential role in lymphocyte activation and proliferation, T-helper cell differentiation, tissue-specific lymphocyte homing, the production of specific antibody isotypes, and regulation of the immune response [ 14 ]. Targeted immune cell types include macrophages, dendritic cells, and T and B cells. Mora and colleagues (Fig. 3 ) [ 14 ] summarized the roles and effects of vitamin D on these immune cell types [ 14 ]:
- Macrophages and dendritic cells (DCs) constitutively express VDRs, whereas VDR expression in T cells is upregulated only after activation.
- In macrophages and monocytes, 1,25(OH) 2 VD positively impacts its own effects by increasing the expression of VDR and the cytochrome P450 protein, CYP27B1.
- Certain Toll-like receptor (TLR)-mediated signals also can increase the expression of VDRs.
- The active form of vitamin D induces monocyte proliferation and the expression of interleukin-1 (IL-1) and cathelicidin (an antimicrobial peptide) by macrophages, contributing to innate immune responses to some bacteria.
- 1,25(OH) 2 VD decreases DC maturation, inhibiting upregulation of the expression of MHC class II, CD40, CD80, and CD86. In addition, it decreases IL-12 production by DCs while inducing the production of IL-10.
- In T cells, 1,25(OH) 2 VD reduces the production of IL-2, IL-17, and interferon-γ (IFNγ) and attenuates the cytotoxic activity and proliferation of CD4+ and CD8+ T cells.
- The active metabolite of vitamin D might also promote the development of forkhead box protein 3 (FOXP3)+ regulatory T ( T Reg ) cells and IL-10-producing T regulatory type 1 (TR1) cells.
- 1,25(OH) 2 VD blocks B cell proliferation, plasma cell differentiation, and immunoglobulin production.

Potential mechanisms of vitamin D immunomodulation: systemic 1,25(OH)2VD3 affects several immune-cell types, including macrophages, dendritic cells (DCs), T and B cells. Macrophages and DCs constantly express vitamin D receptor (VDR), whereas VDR expression in T cells is only upregulated following activation.
Reprinted by permission from Macmillan Publishers Ltd: [ 14 ]
Notable in the context of this review, many of the mechanisms of vitamin D on immune processes have similarities to mechanisms described for interferon-beta [ 15 ].
Definition of Vitamin D Deficiency and Targeted Levels of Vitamin D
The clinical definition of vitamin D deficiency and what constitutes optimal levels has been the subject of debate. Two organizations, the Institute of Medicine (IOM) and the Endocrine Society, have released separate recommendations regarding vitamin D requirements [ 4 , 11 , 16 ]. Blood levels of 25(OH)D as suggested by the IOM and the Endocrine Society and the recommended dietary allowances (RDAs) by both organizations are provided in Table 1 [ 4 , 11 , 16 ].
Table 1
Definition of vitamin D status [as measured by blood levels of 25(OH)D] and daily vitamin D intake recommended by the Institute of Medicine (IOM) and the Endocrine Society [ 4 , 11 , 13 , 16 ]
| Institute of medicine | Endocrine society | |
|---|---|---|
| Vitamin D status | ||
| “Deficient” | – | ≤ 20 ng/mL (≤ 50 nmol/L) |
| “Insufficient” | – | 21–29 ng/mL (51–74 nmol/L) |
| “Sufficient” | 20 ng/mL (50 nmol/L) | ≥ 30 ng/mL (≥ 75 nmol/L) |
| “Ideal” | – | 40–60 ng/mL (100–150 nmol/L) |
| Considered “safe” | – | ≤ 100 ng/mL (≤ 250 nmol/L) |
| Daily vitamin D intake recommendations (upper limits) | ||
| Infants | 400 IU/day (1000–1500 IU/day) | 400–1000 IU/day (2000 IU/day) |
| Children | 600 IU/day (2500–3000 IU/day) | 600–1000 IU/day (4000 IU/day) |
| Adults | 600 IU/day (4000 IU/day), 800 IU/day for seniors | 1500–2000 IU/day (10,000 IU/day) |
The foundational basis for the recommendations by these two organizations are fundamentally different. The IOM guidelines based their recommendation on a population model and focused on bone health (calcium absorption, bone mineral density, and osteomalacia/rickets) aiming to prevent vitamin D deficiency in 97.5% of the general population. Based on the model applied, no evidence was found that a serum 25(OH)D concentration > 20 ng/mL (50 nmol/L) had beneficial effects at a population level. Therefore, the IOM concluded that the daily requirements for vitamin D were adequate to reach the “sufficient” 25(OH)D level of 20 ng/mL (50 nmol/L), and that these levels were generally attained by most of the population [ 4 , 16 ].
Alternatively, the Endocrine Society concluded that a level of 20 ng/mL (50 nmol/L) was not sufficient. The Endocrine Society based their recommendations on a medical model taking into consideration available evidence on skeletal and extraskeletal effects of vitamin D, in addition to the few negative studies. Moreover, they took into consideration the low toxicity potential of vitamin D supplementation. In their view, serum 25(OH)D levels of ≥ 30 ng/mL (≥ 75 nmol/L) are “sufficient” for children and adults, levels of 40–60 ng/mL (100–150 nmol/L) are “ideal” (considering assay variability), and levels of up to 100 ng/mL (250 nmol/L) could be considered “safe” [ 11 , 13 ].
The Endocrine Society advocates for screening and corrective action for individuals at risk of vitamin D deficiency. Such individuals include African American and Hispanic children and adults; pregnant and lactating women; older adults with a history of falls or nontraumatic fractures; obese children and adults (BMI > 30 kg/m 2 ); and patients with musculoskeletal diseases, chronic kidney disease, hepatic failure, malabsorption syndromes, and some lymphomas [ 11 ]. Furthermore, the group recommends supplementation at suggested daily intake and tolerable-upper-limit levels, depending on age and clinical circumstances (Table 1 ) [ 4 , 11 , 13 , 16 ].
Supplemental Vitamin D
The recommended dietary allowance (RDA) for vitamin D and the tolerable-upper-limit levels vary with age and under certain circumstances such as those involving pregnancy, obesity, or comorbidities. A daily dose of 600–800 IU should satisfy the requirements for optimal bone health [ 16 ], but a higher intake (1000–2000 IU) is needed to achieve and maintain 25(OH)D levels > 30 ng/mL (75 nmol/L) [ 11 ]. Vitamin D supplements can be administered daily, weekly, monthly, or every 4 months to reach an adequate serum 25(OH)D concentration. For cases of extreme vitamin D deficiency, a bolus application of vitamin D has been proposed, but a steady-state serum 25(OH)D concentration is more likely to be maintained by more frequent, lower doses of vitamin D [ 13 ]. Vitamin D3 (cholecalciferol) is widely preferred over vitamin D2 (ergocalciferol), as it has proven to be the more potent form of vitamin D in all primate species, including humans [ 17 ]. Vitamin D supplementation at doses of 1500–2000 IU/day for adults as suggested by the Endocrine Society appears to be well tolerated, with relatively minor concerns about toxicity for most patients [ 11 ]. Caution should be exercised in patients with impairment of renal function, cardiovascular diseases, chronic granuloma-forming disorders (sarcoidosis or tuberculosis), or chronic fungal infections. Some patients with lymphoma have activated macrophages that produce 1,25(OH) 2 VD in an unregulated fashion.
Vitamin D Safety Risks and Vitamin D Intoxication
1,25(OH) 2 VD stimulates intestinal calcium absorption [ 18 ]. Without vitamin D, only 10–15% of dietary calcium and about 60% of phosphorus are absorbed. Vitamin D sufficiency enhances absorption of calcium by 30–40% and phosphorus by 80% [ 11 , 19 , 20 ]. Vitamin D intoxication is characterized by hypercalcemia, hypercalciuria, and hyperphosphatemia and in the long term, can lead to soft tissue and vascular calcification and nephrolithiasis [ 13 ]. After review of available literature, the Endocrine Practice Guidelines Committee concluded that vitamin D toxicity is a rare event caused by inadvertent or intentional ingestion of excessively high amounts of vitamin D [ 11 ]. Concerns were expressed for people with 25(OH)D levels of 150 ng/mL (375 nmol/L) or higher, when daily doses of vitamin D exceed 10,000 IU or when high intake of vitamin D is combined with high intake of calcium. A dose-ranging study reported that 10,000 IU/day of vitamin D3 for 5 months in healthy men did not alter their serum calcium or their urinary calcium excretion, which is the most sensitive indicator for potential vitamin D intoxication [ 21 ]. However, there is a paucity of evidence supporting the use of higher levels of vitamin D over a prolonged time [ 11 ].
Safety findings in three studies conducted in patients with MS using doses of vitamin D above 10,000 IU/day are noteworthy. One open-label trial of vitamin D in patients with MS evaluated the safety of a dose-escalation protocol from 4000 to 40,000 IU/day (mean of 14,000 IU/day). Concomitantly, patients received 1200 mg of calcium per day vs . a control group (allowed up to 4000 IU/day of vitamin D and supplemental calcium if desired) over 1 year [ 22 ]. All calcium-related measures within and between groups were normal. Despite a mean peak 25(OH)D level of 165 ng/mL (413 nmol/L), no significant adverse events occurred. The safety results were in line with a previously conducted, smaller study in 12 patients with MS also using doses of up to 40,000 IU [ 23 ]. In the third study, 15 patients with relapsing–remitting MS (RRMS) were supplemented with 20,000 IU/day of vitamin D3 for 12 weeks [ 24 ]. The median vitamin D level increased from 50 nmol/L (range: 31–175 nmol/L) at week 0–380 nmol/L (range: 151–535 nmol/L) at week 12 ( P < 0.001). All patients completed the observation period without side effects, hypercalcemia, or hypercalciuria [ 24 ].
There are cases in the literature in which exceptionally high doses (considerably above the daily upper limit of 10,000 IU) led to vitamin D toxicity:
- Bell and coworkers described a 67-year-old woman with vitamin D intoxication. Because of a compounding error by the pharmacy, the woman had taken 600,000 IU (rather than the intended 600 IU) of cholecalciferol daily for more than 3 years, leading to reversible hypercalcemia and partially reversible renal impairment [ 25 ].
- Fragoso and colleagues reported considerable vitamin D toxicity in 21 MS patients who were exposed to levels ranging from 8000 IU/day to extremely high, supra-physiological doses of 150,000 IU/day (average 87,000 IU) [ 26 ].
In order to assess the correlation between vitamin D and MS, a literature search of large, prospective, observational studies, epidemiological studies, and studies using new approaches such as Mendelian randomization was conducted.
Compliance and Ethics Guidelines
This article is based on previously conducted studies, and as such, does not involve any new studies of human or animal subjects performed by any of the authors.
Vitamin D Levels and MS Susceptibility
Since vitamin D was proposed as an important factor in MS development in the 1970s, numerous experimental and epidemiologic studies have been conducted to answer key questions such as Does vitamin D prevent MS? How does vitamin D impact MS activity? and Can vitamin D supplementation favorably alter the course of MS? Observational study data does suggest that adequate vitamin D levels may reduce the risk of MS and affect the course of the disease. However, study limitations restrict the extent to which inverse associations can be attributed to vitamin D, and additional studies are needed to further understand the nature of this association [ 2 ].
Epidemiologic Study Data
Epidemiologic studies substantiate that the prevalence of MS is greater at higher latitudes and tends to peak in areas with the lowest exposure to ultraviolet light [ 27 – 32 ]. Additionally, to some degree, diets rich in vitamin D-containing oily fish may offset this risk [ 27 , 28 ]. In “historical” cohorts, the risk of MS decreased among people who migrate from higher to lower latitudes [ 33 ]. However, this latitudinal finding has appeared to decline in recent decades and may be linked to an increased trend towards avoiding sun exposure or staying indoors for longer portions of the day, even in warmer climates [ 7 , 34 ].
An Australian case–control study examined whether leisure sun exposure, combined with 25(OH)D status impacts the risk of a first demyelinating event and whether this was related to a latitude gradient [ 35 ]. Independently, higher levels of sun exposure (past, recent, and cumulative), higher actinic skin damage and higher 25(OH)D levels were associated with significantly reduced risks of a demyelinating event. The investigators calculated that the differences in leisure sun exposure, serum 25(OH)D level, and skin type would additively account for a 32.4% increase in the incidence of first demyelinating events from the low to high latitude regions in Australia [ 35 ]. The independent association of sun exposure and MS risk suggests that UV light itself may influence MS risk. Partially supporting this is research that showed that experimental autoimmune encephalitis (EAE) could be prevented in mice through whole-body irradiation with UV light [ 36 ]. However, this research did not discriminate between vitamin D-related and nonrelated effects of UV light. The research did note that in the Northern Hemisphere, significantly more people with MS are born in May (9.1%), when there is less sunlight during pregnancy than in November (8.5%), when there is an increased amount of sunlight [ 37 ]. Some argue that this is an artifact of more births during certain months [ 38 ] though others disagree [ 39 ].
Dietary Intake of Vitamin D and MS Risk
Using data from two large cohorts of the Nurses’ Health Study involving more than 187,000 women (including 300 who developed MS during the study), Munger and colleagues evaluated the association between calculated vitamin D intake from diet or supplements and the risk of developing MS [ 40 ]. Women who had a higher intake of dietary vitamin D (approximately 700 IU/day) had a 33% lower incidence of MS compared with those with lower intake. In addition, women who used vitamin D supplements (≥ 400 IU/day) had a 41% reduced risk of developing MS compared to non-users. Having higher levels of 25(OH)D (irrespective of dietary vitamin D intake) also seems to predict a lower risk of MS onset. Using a longitudinal study design, Munger and colleagues evaluated serum vitamin D levels derived from blood samples of seven million US military personnel. Those with 25(OH)D levels greater than 100 nmol/L (40 ng/mL) had a 62% lower chance of subsequently developing MS [ 1 ].
Vitamin D Levels During Pregnancy and MS Risk in Offspring
The Finnish Maternity Cohort is a comprehensive registry, established in 1983, that includes more than 800,000 women and more than 1.5 million serum samples. This cohort also served as a basis for examining the association of vitamin D levels during pregnancy and MS risk [ 3 ]. One hundred ninety-three patients with a diagnosis of MS, whose mothers were captured in the registry and had an available serum sample from the pregnancy with the affected child, were matched with 326 controls. Vitamin D levels were low in both groups, but lower in the mothers of MS patients than in controls [34.6 nmol/L (13.9 ng/mL) vs. 37.5 nmol/L (15.0 ng/mL); P = 0.006]. Moreover, MS risk was 90% higher in the offspring of vitamin D-deficient mothers [25(OH)D < 30 nmol/L (12.0 ng/mL)] compared with offspring of mothers who were not vitamin D deficient [relative risk, 1.90; 95% confidence interval (CI), 1.20–3.01; P = 0.006] [ 3 ]. These data suggest that insufficient vitamin D levels during pregnancy may increase the risk of MS [ 3 ].
The association between neonatal 25(OH)D status and risk of MS was examined in a large population-based case–control study using data from the nationwide Danish MS Registry and the Danish Newborn Screening Biobank (DNSB) [ 41 ]. Data from 521 patients with MS and 972 controls were investigated. The analysis by quintiles revealed individuals with the highest risk of MS were in the lowest quintile group of 25(OH)D (< 20.7 nmol/L), and individuals the lowest risk were in the highest quintile group (≥ 48.9 nmol/L); with an odds ratio for highest vs. lowest group of 0.53 (95% CI 0.36–0.78). Children born with 25(OH)D levels < 30 nmol/L seemed to be at an especially high risk of developing MS. The additional benefits of higher levels of 25(OH)D were less pronounced [ 41 ].
Studies Utilizing Mendelian Randomization to Measure MS Risk
Data on vitamin D and risk of MS have been largely based on observational studies that measure an inverse association. However, MS is identified as the primary cause of low 25(OH)D) and thus cannot be excluded with these methods. Mendelian randomization (MR) analyses use genetic associations to test the effects of biomarkers, such as 25(OH)D, on the risk of disease, because inherited alleles are not affected by most confounding variables or disease status [ 42 , 43 ]. Thus, the possibility of confounding or reverse causation can largely be excluded. Three recent publications made use of this epidemiological approach. Mokry and colleagues applied genome-wide data on genetic variants that predicted blood 25(OH)D levels from the Canadian Multicentre Osteoporosis Study to participants in the International MS Genetics Consortium study [ 42 ]. They found that a genetically determined decrease in blood 25(OH)D level predicted increased MS susceptibility. An increase of 25(OH)D levels by 50% decreased the odds of getting MS by approximately 50% [ 42 , 44 ]. Similar findings were seen from MR analyses using data from two populations, a US administrative claim database and two population-based case–control studies from Sweden [ 45 ]. The third publication, from the Network of Pediatric Multiple Sclerosis Centers, again investigated the US and Swedish datasets [ 43 ]. Genetic risk scores were used to estimate the causal association between low 25(OH)D levels and pediatric-onset MS. This data also supports independent and causal effects of decreased 25(OH)D levels on susceptibility to pediatric-onset MS [ 43 ].
Studies Contradicting the Association of Vitamin D Levels with MS Risk
Ueda and colleagues investigated the link between vitamin D status at birth and risk of adult-onset MS in a population-based, multicenter, case–control study in Sweden [ 46 ]. The authors analyzed stored neonatal dried blood samples of 459 MS subjects and 663 controls (matched on sex, age, and residential area). There was no association between neonatal serum 25(OH)D quintiles and risk of MS as adults. When the findings were adjusted for confounding factors in early life (e.g., month of birth, latitude of birth, and breastfeeding), in adult life (e.g., sun exposure, intake of vitamin D-rich dairy products, fatty fish consumption, smoking, and body mass index at 20 years of age), ancestry, MS heredity, and socioeconomic group, results were not considerably affected [ 46 ]. Whether the study provided conclusive results was the subject of debate for two primary reasons: (1) blood samples at birth were not well preserved and may have been affected by substantial degradation of 25(OH)D; and (2) the range of 25(OH)D levels at birth was narrow and mostly low (mean = 29.7 nmol/L, median = 25.6, interquartile range = 17.0–38.4 nmol/L) [ 47 ].
Optic neuritis (ON) is a common first symptom of MS. Pihl-Jensen and coworkers conducted a cross-sectional study to assess whether 25(OH)D levels can predict later development of MS in acute ON by evaluating the differences in mean serum 25(OH)D levels between subjects with ON ( n = 164) and those with MS ( n = 948) [ 48 ]. Deseasonalized serum 25(OH)D levels of the ON onset group were used for statistical analyses. The majority (56.1%) of the patients had 25(OH)D levels below 50 nmol/L (mean 47.64 ± 21.48 nmol/L). There were no significant differences in 25(OH)D levels between ON subjects who developed MS and those who did not develop MS during the median follow-up time of 741 days ( P = 0.279), indicating no statistically significant effect on the hazard of MS development. However, significant associations were found between 25(OH)D levels and elevated IgG index levels or CSF pleocytosis, both markers of inflammatory activity or risk of MS. The interpretation of the latter finding was difficult due to the risk of reverse causation. Although the role of using 25(OH)D levels as a predictor for the development of MS after acute ON could not be demonstrated, the study data do suggest that there may be a link between development of MS after acute ON. They also provide a rationale for additional research for a possible role of vitamin D in the early stages of MS [ 48 ].
Levels of Dietary Vitamin D Intake and Risk of MS–Implications for Public Health
Whether a daily dose of vitamin D or a gestational dose of vitamin D per day “keeps the MS doctor away” is not yet proven [ 49 ]. Additionally, it is not known what level of serum 25(OH)D would prevent MS in a large majority of individuals. Most studies in this review reported 25(OH)D levels below 50 nmol/L (20 ng/mL) in a significant proportion of their investigated populations, which is below the healthy minimum level. Indicating that establishing a target in the general population general population, pregnant women, and their offspring to achieve the minimum levels of 25(OH)D may be considered an important goal for health (i.e., 50 nmol/L (20 ng/mL), according to IOM [ 4 , 15 ] or 75 nmol/L (30 ng/mL), according to the Endocrine Society) [ 11 , 13 ].
Effects of Vitamin D Status and MS Disease Activity
Understanding how existing vitamin D levels and vitamin D exposure affect clinical relapses and MS lesion activity is critically important to this review. As such, the findings from larger studies investigating these effects are summarized below.
Impact of Vitamin D Levels on Disease Activity in RRMS: Observational Studies
In a prospective longitudinal study from the Netherlands, 25(OH)D was measured every 8 weeks for a mean of 1.7 years in 73 patients with RRMS [ 50 ]. Fifty-eight patients experienced a total of 139 exacerbations during the study period. Relapse risk was significantly reduced in those with medium [50–100 nmol/L (20–40 ng/mL)] and high [> 100 nmol/L (> 40 ng/mL)] serum vitamin D levels (vs. < 50 mol/L or 20 ng/mL) compared to those with low levels [ 50 ]. For each doubling of serum vitamin D concentration from baseline of 10, 20, 30, MS relapse risk decreased by 27%. Although this suggests a beneficial effect of vitamin D on MS, it must be noted that there is also a possibility that conditions associated with MS relapse had an effect on serum vitamin D levels [ 50 ].
Incident rate ratios (RR) for relapse in relation to serum vitamin D levels were measured in a retrospective study of 110 patients with pediatric-onset MS [ 51 ]. After adjusting for several factors (age, gender, race, ethnicity, disease duration, and treatment), the authors found that every 10 ng/mL (25 nmol/L) increase in 25(OH)D level was associated with a 34% decrease in relapse risk. Similar findings were seen in a prospective cohort study from Tasmania, Australia, in a group of 145 adults with RRMS, in which 25(OH)D levels were measured twice a year for a period of 3 years [ 52 ]. For each 10 nmol/L increase in serum vitamin D level, there was an associated 12% lower risk of MS relapse. Adjustment for potential confounders, such as timing of the blood testing, did not affect the results. Most of the participants in this study (82%) were receiving immunomodulatory therapy. The authors concluded that raising 25(OH)D levels by 50 nmol/L could decrease the hazard of a relapse by up to 50% (Fig. 4 ) [ 52 ].

Association of vitamin D and relapse risk in MS. The graph shows risk of relapse according to 25(OH)D levels, adjusted for age and month of serum measurement. Size of points is proportional to the inverse of the variance (larger bubbles represent greater precision).
Reprinted with permission from Wiley Company [ 52 ]
The EPIC natural history study was a 5-year cohort study conducted at the University of California, San Francisco which sought to determine the associations between serum or plasma vitamin D levels and MRI activity in a group of 469 white, mostly non-Hispanic patients with MS or clinically isolated syndrome (CIS) [ 53 ]. Sixty-four percent received disease-modifying therapy within the previous 12 months. Vitamin D levels increased significantly during the study, especially for those patients using supplements. Only 9% of patients were taking vitamin D supplements at baseline, but 43% were taking them by year 5. Patients who reported using vitamin D supplements had an 8.7 ng/mL (21.75 nmo/L) higher vitamin D level, on average, compared with those who did not. Additionally, lower vitamin D levels were strongly associated with development of new T2 lesions and with contrast-enhancing lesions on brain MRI. Each additional 10 ng/mL (25 nmol/L) increment of 25(OH)D was associated with a 15% lower risk of new T2 lesions and a 32% lower risk of enhancing lesions (Fig. 5 ) [ 53 ]. Higher vitamin D levels were associated with a lower (but not statistically significantly) risk of MS relapses. Findings from this study also showed strong “within-person” effects of vitamin D levels in individual patients with MS. The authors concluded that “individuals with CIS/RRMS with higher vitamin D levels are at much lower risk of the subsequent development of new lesions and of gadolinium (Gd+)-enhancing lesions on brain MRI, even after accounting for potential confounding factors” [ 53 ].

Magnetic resonance imaging outcomes associated with quintiles of vitamin D in the EPIC study. EPIC is a 5-year longitudinal MS cohort study at the University of California at San Francisco, USA. Participants ( N = 469) had clinical evaluations, brain MRI, and blood draws annually. MRI outcomes were associated with quintiles of vitamin D. In multivariate analyses, each 10 ng/mL (25 nmol/L) higher 25-hydroxyvitamin D level was associated with a 15% lower risk of a new T2 lesion (incidence rate ratio [IRR],0.85; 95% confidence interval [CI], 0.76–0.95; P = 0.004) and a 32% lower risk of a gadolinium-enhancing lesion (IRR, 0.68; 95% CI, 0.53–0.87; P + 0.002).
Reprinted with permission from Wiley Company [ 53 ]
More recently, Mowry and colleagues examined the association of vitamin D levels with brain volume measures and new lesions in patients with CIS ( N = 65) [ 54 ]. The scientific rationale for these data are based on the concept that brain volume is thought to reflect neurodegeneration better than classical MRI parameters such as T2 lesion load and Gd+-enhancing lesions [ 54 ]. Each 25-nmol/L increase in 25(OH)D level was associated with 7.8-mL higher gray matter volume ( P = 0.025). Higher levels of 25(OH)D also were associated with the composite endpoint of ≥ 3 new brain T2 lesions or ≥ 1 relapse within 1 year ( P = 0.096). Despite the limitations of the small sample size, these findings suggest that higher vitamin D levels in CIS may slow neurodegeneration [ 54 ].
Lower vitamin D levels also correlate with other surrogates of MS disease activity, including lower odds of remaining relapse free in MS [ 55 ], greater disability and disease severity in MS [ 53 , 55 – 57 ], conversion from CIS to clinically definite MS (CDMS) [ 58 ], and poorer nonverbal long-term memory performance [ 59 ]. These data were largely generated by observational studies that restrict the extent to which inverse associations can be attributed specifically to vitamin D. Properly designed and conducted clinical trials are needed to further define the nature of this association.
Impact of Vitamin D Levels on Disease Activity Based on Post-Hoc Analyses from BENEFIT and BEYOND
To our knowledge, no large randomized, double-blind, controlled, prospectively phase 3 trials have been conducted to study the impact of vitamin D levels on MS activity as a primary endpoint. However, in two phase 3 studies, the BENEFIT study [ 60 ], and the BEYOND study [ 61 ] post hoc analyses were conducted to investigate this potential link.
The BENEFIT (Betaseron ® in Newly Emerging Multiple Sclerosis for Initial Treatment) study was a randomized trial originally designed to evaluate the impact of early versus delayed IFNB-1b treatment in patients with CIS [ 62 – 64 ]. Patients with a first event suggestive of MS and a minimum of two clinically silent lesions on MRI were randomly assigned to receive interferon beta-1b (IFNB-1b) 250 μg ( n = 292; early treatment) or placebo ( n = 176; delayed treatment) subcutaneously every other day for 2 years or until diagnosis of CDMS, in which case they could switch to IFNB-1b therapy. All patients were then eligible to enter a prospective follow-up phase with open-label IFNB-1b for up to 5 years after randomization. Patients and study personnel remained unaware of initial treatment allocation throughout the study up to year 5. During the observation period, regular study visits were scheduled to collect clinical and MRI data, with visits at baseline and months 3, 6, 9, 12, 18, 24, 36, 48, and 60 [ 64 ]. A post hoc analyses aimed to determine whether vitamin D status [serum 25(OH)D levels] would predict disease activity and prognosis up to 5 years after the first attack in early-disease CIS patients [ 60 ]. Serum samples were collected at baseline, 6, 12, and 24 months and levels of 25(OH)D were measured (by ELISA). Of the 468 patients included in BENEFIT, 465 patients had at least one 25(OH)D measurement, 417 had two or more, 396 had three or more, and 303 had all four measurements. 25(OH)D levels were seasonally adjusted to obtain an estimate of long-term 25(OH)D status. To minimize the possibility that lower 25(OH)D levels were a consequence, rather than the cause, of MS severity, the cumulative average 25(OH)D levels at 12 months were related to the outcomes between 12 and 60 months or between 24 and 60 months (thereby allowing inserting a 1-year lag between 25[OH]D measurements and the assessment of MS activity or progression) [ 60 ]. Three sets of analyses were performed: (1) continuous 50-nmol/L (20-ng/mL) increments to determine the overall linear trend; (2) quintiles to explore the dose response; and (3) categorical analysis using ≥ 50 nmol/L versus < 50 nmol/L (20 ng/mL) [ 60 ].
Findings indicated that patient characteristics affected vitamin D levels. Those with higher (seasonally adjusted) 25(OH)D levels tended to be younger and to have a lower body mass index (BMI), a lower number of T2 lesions, and a higher brain volume at the CIS stage, but otherwise were similar to patients with lower levels of 25(OH)D [ 60 ].
Over the 5-year follow-up period, 81.3% (377 patients) converted to MS according to the McDonald 2001 criteria that include MRI lesions [ 65 ] and 46.6% (216 patients) converted to CDMS based on exacerbations or progression alone. The hazard of conversion decreased with increasing serum 25(OH)D and mean serum 25(OH)D levels at 12 months predicted subsequent conversions to McDonald MS ( P = 0.02) and CDMS ( P = 0.05) [ 60 ].
An increasing serum 25(OH)D level was associated with a decreasing rate of new active lesions on MRI; this effect was particularly strong in patients with both 6- and 12-month serum 25(OH)D measurements. A 50 nmol/L (20 ng/mL) increment in average serum 25(OH)D levels within the first 12 months predicted a 57% lower rate of new active lesions (RR, 95% CI: 0.43 (0.26–0.70), P < 0.001) and a 57% lower relapse rate (RR (95% CI): 0.43 (0.20–0.92, P = 0.03). In evaluating the potential progression of MS on MRI, higher levels of serum 25(OH)D were associated with less T2 lesion volume accumulation over time. For a 50 nmol/L increase in serum 25(OH)D, the relative decrease in T2 lesion volume was 20% per year ( P < 0.001). Restricting results to patients with both 6-month and 12-month serum 25(OH)D measures, tended to strengthen results [ 60 ].
The dichotomous analysis of serum 25(OH)D levels (< 50 vs. ≥ 50 nmol/L) is shown in Fig. 6 [ 60 ]. For instance, the percentage loss of brain volume over time was lower in patients with 25(OH)D levels ≥ 50 nmol/L at the 12-month time point compared with those with serum 25(OH)D levels < 50 nmol/L ( P = 0.005). Although a 50 nmol/L increase in 25(OH)D levels did not reach significance for a reduction in the average expanded disability status scale (EDSS) score ( P = 0.11), patients with serum 25(OH)D levels ≥ 50 nmol/L had a significantly lower annualized change in EDSS score compared with those patients with serum 25(OH)D levels < 50 nmol/L ( P = 0.004) while on IFN-b-1b. Across all analyses, associations were generally stronger for MRI than for clinical outcomes. Nevertheless, “the latter were still remarkable considering the overall low rate of relapses (0.2 per year) and small EDSS score change (median change, 0.0) in BENEFIT” [ 60 ].

Multiple sclerosis outcomes according to dichotomous serum 25(OH)D levels. Analyses are based on patients with averaged 6- and 12-month measurements of 25(OH)D. Group comparisons are adjusted for age, sex, treatment, time of follow-up, and T2 lesion score at baseline. The graphs show the probability of conversion to CDMS after 12 months ( a ); the cumulative number of new active lesions on brain MRI ( b ); the percentage change in T2 lesion volume from year 1 to year 5 on brain MRI ( c ); and the percentage change in brain volume from year 1 to year 5 ( d ). The error bars indicate the standard error of the mean (SEM).
Reproduced with permission from [ 60 ]. Copyright©2014 American Medical Association. All rights reserved
Strengths of the BENEFIT study included (1) its longitudinal design, (2) the exclusive recruitment of patients at the CIS stage, (3) the use of repeated serum 25(OH)D measurements, (4) the large number of patients, (5) standardized treatment (e.g., early vs. late IFNB-1b), and (6) rigorous clinical and MRI assessment of all patients during a 5-year period. Limitations of the study included (1) the fact that most patients were eventually treated with IFNB-1b and some crossed over during the 2 years of the study, and (2) while a clear dose response was observed for the most sensitive MRI outcomes, the effects did not reach a plateau level, and, therefore, serum 25(OH)D levels greater than the median 69 nmol/L could have had a greater effect. According to the authors, a low 25(OH)D level early in the disease course is a strong risk factor for long-term MS activity and progression in patients with early MS who were treated with IFNB-1b [ 60 ].
The BENEFIT cohort had an early treatment group and a delayed treatment group. The associations of 25(OH)D levels and MS activity were more pronounced for patients in the early treatment group than for those in the delayed treatment group (Table 2 [ 60 ] and Fig. 7 [ 66 ]), although a test for interaction between 25(OH)D levels and treatment assignment was significant only for the time to CDMS ( P = 0.04) [ 62 ]. These results suggest that early treatment with IFNB-1b may have an additive effect along with 25(OH)D to reduce disease severity and progression in both clinical and imaging outcomes.
Table 2
Comparison of clinical and MRI outcomes in patients with plasma 25(OH)D levels < 50 nmol/L versus ≥ 50 nmol/L in all patients and those with early or delayed start of interferon beta-1b.
| All patients | Early treatment | Delayed treatment | |
|---|---|---|---|
| Probability of conversion CDMS up to year 5, RR (95% CI) | 0.65 (0.42–0.99), = 0.05 | 0.48 (0.28–0.83), = 0.008 | 1.22 (0.59–2.5), = 0.6 |
| Cumulative number of new lesions up to year 5, RR (95% CI) | 0.73 (0.60–0.90), = 0.002 | 0.70 (0.55–0.90), = 0.005 | 0.71 (0.52–0.97), = 0.03 |
| Percent change in T2 volume from year 1–5, % (95% CI) | − 8.99 (− 15.1 to − 2.5), = 0.008 | − 11.0 (− 19.0 to − 2.2), = 0.02 | − 8.84 (− 17.14 to 0.29), = 0.06 |
| Percent change in brain volume from year 1–5, % (95% CI) | 0.34 (0.10–0.57), = 0.005 | 0.43 (0.14–0.72), = 0.004 | 0.17 (− 0.24 to 0.58), = 0.4 |
All data were adjusted for age, sex, treatment, time of follow-up, and T2 lesion score at baseline
CDMS Clinically definite multiple sclerosis, RR rate ratio
a Includes new T2 lesions, new Gd + -enhancing lesions, and enlarging T2 lesions

Data from the Vitamin D analysis of the BENEFIT trial. Comparison of probability of conversion to CDMS in patients with plasma 25(OH)D < 50 nmol/L versus ≥ 50 nmol/L in all patients and those with early or delayed start of interferon beta-1b.
Reproduced with permission from [ 66 ]
To explore the mechanistic rationale for the potential additive effects of 25(OH)D levels and early IFNB-1b treatment, Munger and colleagues conducted a global gene expression analysis in which expression profiles were measured at various time points among participants in the BENEFIT clinical trial [ 67 ]. The relationship between genes or gene sets expressed in association with 25(OH)D and those associated with MS activity was examined. The numbers of Gd+-enhancing lesions served as a marker of disease activity. A 50 nmol/L increase in serum 25(OH) levels reduced the Gd+ lesion count by 55%. Adjusting for gender, age, treatment, and treatment − 25(OH)D interaction did not alter the significance of the findings. Gene expression in whole blood was studied in 295 individuals, evaluating approximately 19,000 genes. Reduced Gd+ lesion count was significantly associated with increased expression of 25(OH)D-related genes, an effect that was independent of IFNB-1b treatment. This effect was also noticed when looking at single genes that were associated with regulation of 25(OH)D levels. The authors hypothesized that there was an additive effect of 25(OH)D and IFNB-1bin reducing Gd+ lesion counts [ 67 ].
The second data set from randomized, double-blind, phase 3 trials in MS was derived from the BEYOND (Betaseron ® Efficacy Yielding Outcomes of a New Dose) study [ 61 ]. Compared with the BENEFIT study, the BEYOND study included patients with established MS (vs. patients with CIS) and was shorter in duration (2 vs. 5 years). It also included considerably more patients (1482 vs. 465) and was conducted in different geographical regions (North America, Western and Eastern Europe, Southern Hemisphere vs. Europe and Canada).
BEYOND was a large, phase 3, prospective, multicenter, blinded, randomized clinical trial. Patients were monitored for at least 2 years. Clinical visits were scheduled every 3 months, and an MRI was performed at baseline and annually thereafter. A post hoc analysis assessed 25(OH)D levels and the subsequent MS disease course and disease progression as characterized by MRI and clinical endpoints [ 58 ]. Eligible patients for the vitamin D analyses included 1482 participants randomized to receive 250, or 500 μg of IFNB-1b with at least two measurements of 25(OH)D obtained 6 months apart. Serum 25(OH)D measurements were performed at baseline, 6, and 12 months.
In longitudinal analyses, 25(OH)D was inversely correlated with the cumulative number of active lesions between baseline and the last MRI (average follow-up time, 2 years). A 50-nmol/L higher level of serum 25(OH)D was associated with a 31% lower rate of new lesions [relative rate (RR), 0.69; 95% CI, 0.55–0.86; P = 0.001]. This inverse association was also strong and significant in analyses restricted to patients with 25(OH)D levels > 50 nmol/L (RR, 0.62; 95% CI, 0.46–0.84; P = 0.002) and was consistent in each of the four geographic regions (Fig. 8 ) [ 61 ]. The lowest rate of new lesions was observed among patients with 25(OH)D levels > 100 nmol/L (RR, 0.53; 95% CI, 0.37–0.78; P = 0.002). No significant associations were found between 25(OH)D levels and change in brain volume, relapse rates, or EDSS scores [ 61 ]. Strengths of this study include the large number of participants, the regionally diverse population with varying baseline characteristics, and the repeated measurements of 25(OH)D, which helped characterize patients’ long-term vitamin D status. The relatively short follow-up is the most important limitation of this study. This limited follow-up may explain the lack of association between serum 25(OH)D levels and measures of brain atrophy or clinical endpoints, both of which were modified by 25(OH)D in the longer BENEFIT study [ 60 , 61 ]. Regarding targeted vitamin D levels, the authors stated: “Our observation of the lowest level of MS activity among patients with serum 25(OH)D levels above 100.0 nmol/L [40 ng/mL] is consistent with the results of a previous investigation in the US [ 50 ], and suggests that the 25(OH)D levels in most patients with MS who are not receiving supplemental vitamin D may be suboptimal” [ 53 ].

The relative rate of cumulative new active lesions (NALs) vs. average of baseline, 6-month, and 12-month 25[OH]D levels stratified by geographic region. The solid lines and shaded regions represent the relative rate ratios of cumulative NALs for changes in 25 (OH)D relative to the median level and the corresponding 95% CIs, respectively. Analyses were adjusted for age, sex, randomization status, baseline EDSS score, and disease duration. Models assume a linear association between the logarithm of the rate of cumulative NALs and serum 25(OH)D. Analyses using cubic splines revealed no significant deviation from linearity. (To convert 25[OH]D values to ng/mL, divide by 2.496).
Reproduced with permission from [ 61 ]. Copyright©2015 American Medical Association. All rights reserved
Effects of Disease-Modifying Therapies on Vitamin D Levels in MS Patients
MS disease activity may be additively affected by vitamin D and IFNB-1b [ 60 ]. This hypothesis is supported by investigations from the same researchers suggesting that processes regulated and triggered by 25(OH)D may be additively enhanced by IFNB-1b [ 67 ], and independently by observations from Stewart and colleagues from the Menzies Research Institute in Tasmania [ 68 ]. In an observational cohort study, conducted in 178 patients with MS, vitamin D levels were measured every 6 months over an average of 2.2 years. Patients who took an interferon had significantly higher 25(OH)D levels than those who did not ( P < 0.001). Each 10-nmol/L increase in serum vitamin D was associated with a 10% lower relapse rate. Interestingly, interferon treatment was protective only against relapse among persons with higher vitamin D levels. Among those with insufficient vitamin D, there was an increased risk of relapse despite interferon treatment. The investigators hypothesized that treatment with IFNB may increase serum vitamin D levels through enhanced responsiveness to sun exposure and recommended that persons being treated with IFNB should have vitamin D status monitored and maintained in the sufficiency range [ 68 ]. Also, noteworthy from these data, this group did not find similar associations for glatiramer acetate (GA) therapy and vitamin D.
The notion of complementary or even synergistic effects of IFNB and vitamin D is further supported by observations from Rotstein and coworkers based on the CLIMB (Comprehensive Longitudinal Investigation of MS at Brigham and Women’s Hospital) cohort [ 69 ]. The CLIMB cohort is a prospective cohort study that began enrolling patients in 2000. The objective of the study was to determine whether 25(OH)D levels predicted new disease activity in MS patients treated with IFN-β ( n = 96) or GA ( n = 151). Separately, due to different selection criteria, a similar analysis was conducted for patients treated with fingolimod (FTY, n = 77). Serum 25(OH)D concentration was adjusted for season, and patients were divided into subgroups by 25(OH)D tertile. The primary study endpoint was ‘time to first inflammatory event’, defined as a combination of either first relapse or first Gd+ lesion, using a Cox model adjusted for age, sex, and disease duration. The results demonstrated higher 25(OH)D levels associated with a longer time to the combined first event in the IFNB subgroup [hazard ratio (HR) IFNB = 0.58; P IFNB = 0.012], but not in GA-treated participants (HR GA = 0.89; P GA = 0.50). For Gd+ lesions alone, there was a significant association observed in GA and IFNB subgroups, although the effect was more pronounced with IFNB (HR GA = 0.57; P GA = 0.039 vs. HR IFNB = 0.41; P IFNB = 0.022). No significant associations were found for relapses. There were some sampling difficulties in this cohort and, therefore, the results need to be interpreted with certain caution. For FTY, due to the mandated first-dose observation, samples were available for all patients. Higher 25(OH)D was associated with a longer time to the first event (HR FTY = 0.48; P FTY = 0.016) and with relapses (HR FTY = 0.50; P FTY = 0.046), but not with Gd+ lesions [ 69 ]. The large, prospective cohort and the prolonged follow-up times were strengths of this study, as well as the availability of two 25(OH)D measurements for the majority of patients. However, more regular 25(OH)D measurements would have been ideal and offered greater insights into study conclusions [ 69 ].
Studies Contradicting the Association of Vitamin D Levels with Disease Activity
Contradictory to the aforementioned information are findings reported by researchers from Norway [ 70 ]. In this small prospective cohort study, 88 patients with RRMS were followed with regular MRI and 25(OH)D measurements during 6 months before and up to 18 months after initiation of IFNB. During the pre–IFNB treatment phase, higher levels of 25(OH)D were associated with reduced MRI activity; each 10-nmol/L increase in 25(OH)D was associated with 12.7% ( P = 0.037) lower odds for new T1 Gd + lesions, 11.7% ( P = 0.044) lower odds for new T2 lesions, and 14.1% ( P = 0.024) lower odds for combined unique activity. However, there was no association between 25(OH)D and disease activity after initiation of IFNB. With clinical measures, neither the occurrence of relapses nor EDSS progression was associated with 25(OH)D levels during both study phases. Strengths of the study were the prospective design and the frequent MRI and 25(OH)D assessments during the observation period. Limitations were the relatively short time on IFNB and the small number of participants, as well as the minimal 4 nmol/L increase in serum vitamin D levels following vitamin D supplementation. In the discussion of the study results, the authors expressed their surprise about the lack of an association between 25(OH)D levels and MRI after initiation of IFNB, “as there is no evidence suggesting that the immunomodulatory effects of vitamin D are counteracted by IFNB or vice versa. A reasonable explanation is that IFNB reduced radiologic disease activity, leaving relatively little left to be reduced” by vitamin D [ 70 ].
The Role of Supplemental Vitamin D in MS
When reviewing available data discussing the effects of vitamin D and MS, of key interest is whether vitamin D supplementation can favorably alter the course of MS. Unfortunately, current evidence does not offer consensus to answer this question. Studies with vitamin D alone or with vitamin D as an add-on to a disease-modifying therapy are conflicting [ 22 , 71 – 81 ]. Although these studies are generally small, largely uncontrolled, and used highly variable doses of vitamin D, it can be noted that there are initial promising data arguing for vitamin D supplementation in patients with MS [ 22 , 75 – 81 ]. Furthermore, recent investigations with immunological response markers suggest that vitamin D supplementation in patients with MS exhibits in vivo pleiotropic immunomodulatory effects in MS [ 82 ], and lacking evidence of a treatment effect does not necessarily demonstrate proof of no effect.
Studies Supporting the Benefit of Supplemental Vitamin D
Researchers from Finland conducted a 1-year, randomized, double-blind, placebo-controlled trial with vitamin D3 as an add-on treatment to IFNB-1b in patients with MS. Thirty-four patients were randomly assigned to the treatment group (vitamin D, 20,000 IU/week vitamin D3 (cholecalciferol), and IFNB-1b) and 32 to the control group (placebo and IFNB-1b) [ 75 ]. The primary outcome measure was an MRI T2 burden of disease (BOD), which tended to increase more in the placebo group (median change of 287 mm 3 ) than in the vitamin D group (median change of 83 mm 3 ); however, the difference was not statistically significant ( P = 0.105) (Fig. 9 ) [ 75 ]. Results for other MRI outcomes were mixed. The number of T1 Gd+ lesions decreased in both groups ( P = 0.002), but the change was significantly higher in the vitamin D group ( P = 0.04). New/enlarging T2 lesions at the 12-month point trended higher in the placebo group, but the differences were not statistically significant ( P = 0.286). The percentage of patients with MRI activity (12-month time point) trended lower in the vitamin D group, but these differences also did not reach significance ( P = 0.322). While there was no significant difference in annual relapse rate demonstrated between groups, there was a tendency toward reduced disability accumulation as measured by EDSS ( P = 0.071) and toward improved timed tandem walk ( P = 0.076). There were no significant differences in adverse events between the groups. The authors concluded that larger randomized, controlled trials with more than 1 year of follow-up are warranted to confirm the promising MRI results and to fully address clinical outcomes [ 75 ].

Change in MRI T2 burden of disease (BOD) from baseline to month 12 in the vitamin D-treated and placebo-treated patients. Data are mean ± standard error of 34 patients in the vitamin D group and 32 patients in the placebo group at baseline and 32 in the vitamin D group and 30 in the placebo group at 12 months. The P value for the difference between vitamin D and placebo is 0.105 (trend).
Reproduced from [ 75 ], with permission from BMJ Publishing Group Ltd
A study by Burton and colleagues introduced earlier in this manuscript in the context of the safety profile of higher doses of vitamin D supplementation also offers insight into the role of vitamin D supplementation and the disease course of MS [ 22 ]. In this open-label, controlled trial, patients were randomized to a vitamin D treatment group ( n = 25, escalation protocol 4000–40,000 IU/day, mean 14,000 IU/day) or to a control group ( n = 24, received vitamin D3 4000 IU/day if desired). Despite the high doses of vitamin D, no significant adverse events occurred during the 52-week study period. The annualized relapse rate during the trial year was lower in the treatment group than in the control group (0.26 vs. 0.45; P = 0.09), and more patients in the treatment group remained relapse free. Additionally, the treated patients reported a persistent reduction in T-cell proliferation compared with controls, and treatment group patients appeared to have fewer relapse events and a persistent reduction in T-cell proliferation compared to controls. Study limitations included the use of supplementation or other agents in the control group, the small sample-size, and thus the limited power [ 22 ].
The Danish Multiple Sclerosis Center prospectively gathered data in a cohort of 170 natalizumab-treated patients during winter 2009–2010 (baseline) with follow-up during the subsequent winter [ 78 ]. Patients with insufficient serum 25(OH)D levels (selected cut-off 50 nmol/L) at baseline were advised to take Vitamin D supplements according to Danish recommendations: 2000 IU for patients with levels between 25 and 50 nmol/L, 3000 IU for those with levels between 25 and 12.5 nmol/L and 4000 IU for those with levels below 12.5 nmol/L. 134 patients were included in the clinical data set. Of the 134 patients, 43 had taken vitamin D supplements due to vitamin D insufficiency (mean 25(OH)D levels: 34 nmol/L). Their levels increased significantly by 32.6 nmol/L (95% CI: 24.4–40.8 nmol/L, P < 0.0001) from baseline to follow-up. Moreover, a significant inverse relationship with the annualized relapse rate (ARR) was found: for each nmol/l increase in 25(OH)D, a 0.014 (95% CI − 0.026 to − 0.003) decrease in ARR was observed ( P = 0.02). Overall, the data suggest that correcting vitamin D insufficiency by the means of vitamin D supplements in patients with MS may be beneficial [ 78 ].
Darwish and colleagues looked into the cognitive effects of vitamin D supplementation of patients with MS on IFNB [ 79 ]. At baseline, patients were stratified into a vitamin D-deficient group (25(OH)D levels < 25 ng/mL or 62.5 nmol/L, N = 39) and a vitamin D-sufficient group (25(OH)D levels > 35 ng/mL or 87.5 nmol/L). “Deficient” patients received 10,000 IU vitamin D3 daily for 3 months and reported a significant increase of 25(OH)D levels to 49.0 ± 14.6 ng/mL (122.5 ± 36.5 nmol/L). Additionally, after 3 months these “deficient” patients scored better on the Brief Visuospatial Memory test delayed recall (BVMT-DR, P = 0.02) and the montreal cognitive assessment (MoCA, P = 0.006), but not on the symbol digit modalities test (SDMT) and Stroop. The authors concluded that the lack of significant change on the SDMR and Stroop testing was due to the short disease duration and the propensity for study participants to perform within normal ranges for these tests.
Alternatively, “sufficient” patients continued their usual treatment that may have included vitamin D3 supplementation at various dosages. These patients reported 25(OH)D levels at 64.2 ± 18.7 ng/mL (160.5 ± 46.8 nmol/L) at study end. Sufficient 25(OH)D levels predicted better cognitive performance on the BVMT-DR at baseline and 3 months after adjusting for all measured confounding variables. Study limitations included a small study population ( N = 88), short study duration (3 months), and a quarter of the patients not returning to the month 3 visit. The authors also described not allowing true control for other sources of vitamin D as other possible confounders, such as sun exposure and dietary vitamin D [ 79 ].
Only available in abstract format are the results of two studies which evaluated the benefits and risks associated with high-dose vitamin D supplementation in patients treated with IFNB-1a. Although both failed to demonstrate an effect on clinical parameters, their MRI results demonstrated positive results.
- SOLAR is a randomized, double-blind, placebo-controlled, multicenter, phase 2 study. Two hundred and twenty-nine patients with a 25(OH)D serum level below 150 nmol/L were randomly assigned to cholecalciferol at a dose of 14,000 IU per day or placebo [ 80 ]. All patients received subcutaneous IFNB-1a. After recruitment delays, the study design was adjusted and the percentage of patients with “disease activity free” status (defined as no relapses, no EDSS progression, and no new Gd+ or T2 MRI lesions) at week 48 were introduced as a new primary endpoint. This endpoint was not met (37.2% for cholecalciferol group vs. 35.3% for placebo group, P = 0.912). Likewise, no differences between groups for other clinical parameters such as ARR or EDSS were found. However, results regarding the MRI parameters were promising with a significant 32% reduction in the number of new, combined, unique active lesions in the cholecalciferol group ( P = 0.005). Furthermore, there was a trend toward more cholecalciferol recipients being free from new T1 hypointense lesions, which became significant in those aged 18–30 years. The short duration of the trial (48 weeks) and the relatively small sample size (229 patients) may have led to the lack of significance of the clinical outcomes. For comparisons, most randomized trials of new MS drugs recruited over 800 patients to be able to demonstrate a significant effect vs. placebo. Despite the large sizes, some were not able to show a significant effect on disability progression (e.g. CONFIRM study [ 83 ] TRANSFORMS [ 84 ]). Additionally, these data are not placebo-controlled, but rather an active comparator. Also, the power analysis is not designed to assess a minor effect and would require > 10,000 patients.
- Likewise, the second study was a randomized, placebo-controlled, phase 2 study [ 81 ]. One hundred and twenty-nine patients ( N = 129) were randomly assigned to receive 100,000 IU of cholecalciferol twice monthly (equivalent to a daily dose of 7143 IU) in addition to IFNB-1a over a 24-month period. Again, significant effects in favor of vitamin D supplementation were found for selected MRI parameters such as new or enlarged weighted T1 and T2 lesion, but no effect was found for clinical parameters [ 81 ].
A preliminary study from Iran conducted by Etemadifar and colleagues assessed the safety and efficacy of high-dose vitamin D supplementation during pregnancy in women with MS [ 76 ]. Fifteen pregnant women with confirmed MS and with serum 25(OH)D levels < 50 nmol/L (20 ng/mL) were randomly allocated to received 50,000 IU/week (daily dose of 7143 IU) vitamin D3 or routine care from 12 to 16 weeks of gestation until delivery. 25(OH)D levels increased significantly and no significant adverse events occurred. The women in the vitamin D group had significantly fewer relapses during pregnancy (0 vs. 5; P < 0.05), a tendency for fewer relapses up to 6 months after pregnancy (0 vs. 4; statistically nonsignificant), and a more stable EDSS than those without supplementation. The authors advocated for adding high-dose vitamin D3 supplementation during pregnancy to the routine care of women with MS. Study limitations included a small sample size, and conclusions are limited by the loss to follow-up of 37 out of 52 of the original baseline cohort [ 76 ].
The role of vitamin D supplementation in patients with MS was also evaluated by Jelinek and colleagues, with the authors taking a very different epidemiological approach [ 77 ]. This was an internet survey among 2301 patients with MS who self-reported data on geographical location, intentional sun exposure for health, supplementation with vitamin D, and other lifestyle variables, as well as self-reported doctor-diagnosed relapse rates and disability (Patient Determined Disease Steps). Survey participants were asked to respond to a health-related quality-of-life (HRQoL) questionnaire. Bivariate and multivariate analyses were used for comparisons, including multiple linear regression modeling. Nearly two thirds of respondents (64.6%) lived in the Northern Hemisphere, mostly in developed countries. Most (82.3%) were female, with a median age of 45 years (interquartile range [IQR]: 38–53 years) and a median time since diagnosis of 6 years (IQR: 3–12 years), with the majority (61.6%) having RRMS. More than 80% of the patients indicated that they took vitamin D supplements, mostly between 2000 and 5000 IU daily (Table 3 ) [ 77 ], and 67% reported intentional sun exposure to raise vitamin D levels.
Table 3
Self-reported average daily dose of supplemental vitamin D in an Internet survey among 2301 patients with MS.
Originally published on BioMed Central, an open access journal, in [ 77 ]
| Vitamin D dose | Percentage | |
|---|---|---|
| > 5000 IU | 447 | 20.4 |
| 2001–5000 IU | 734 | 33.5 |
| 1–2000 IU | 613 | 28.0 |
| None | 399 | 18.2 |
Unadjusted regression modeling incorporating deliberate sun exposure, latitude, and vitamin D supplementation showed strong associations between sun exposure and HRQoL. However, the effect disappeared when controlling for age, disability, physical activity, and fish consumption. In contrast, the associations between supplementation of vitamin D and HRQoL were maintained when adjusting for these variables, with a dose–response effect. The beneficial effect of vitamin D supplementation on HRQoL was considered to be of “clinically significant magnitude” [ 77 ]. Lower annualized relapse rates were significantly associated with taking vitamin D supplementation vs. not taking supplements. The dose taken seemed to be of less importance. No effect on disability was found for either supplementation or deliberate sun exposure, but an increase of latitude by 1° (farther from the equator) predicted increased odds of moderate or high disability [ 77 ].
The large data set may compensate for some of the limitations of this study design. Vitamin D supplementation (along with all other measures) was self-reported and not validated with blood tests. No validated tool exists for quantifying variables like deliberate sun exposure; in this study, the question required simply a yes/no answer [ 78 ]. Furthermore, there might be a selection bias in terms of the patients included, as respondents to such Internet surveys are patients who are typically very “engaged” with their situation and disease.
Studies Contradicting the Benefit of Supplemental Vitamin D
A study by Stein and colleagues is widely discussed among those not supporting vitamin D supplementation [ 72 ]. In this 6-month, double-blind, placebo-controlled, randomized trial, patients were allocated to either high or low dose of vitamin D2. The high-dose regimen was 6000 IU twice daily, the low-dose regimen 1000 IU daily. Twenty-three patients were included (11 in the treatment arm, 12 in the control group). There were no significant differences between the groups on the two primary endpoints—cumulative number of new Gd+ lesions and change in the total volume of T2 lesions—nor were there differences on clinical outcome measures, such as number of relapses and effect on EDSS [ 72 ]. Neurology , in which the manuscript was published, ranked the study as providing class I evidence, but this rating is arguable. Although the study was double-blind, placebo-controlled, and randomized, the sample size was very small ( N = 23). Moreover, there were withdrawals (two in the low-dose group, one in the high-dose group), and one patient from the low-dose group was partially excluded from MRI analyses due to brain surgery. Although the authors stated that the two groups were well matched, one patient (in the high-dose group) had 38 Gd+ lesions at baseline, while all other patients had between two and five Gd+ lesions at baseline. The low-dose group was, on average, 10.5 years older than the high-dose group; importantly, the number of exacerbations in MS declines over time, biasing the data in favor of the low-dose group. In addition, this study compared low-dose and high-dose vitamin D administration and did not utilize a concurrent control group of subjects that did not receive any supplemental vitamin D. Finally, even though vitamin D2 seems to be a less potent form of vitamin D than vitamin D3 in all primate species [ 17 ], the 1000-IU/day regimen for the low-dose group is above what the IOM recommends in terms of daily intake [ 4 ] and both groups may have benefited from vitamin D supplementation.
In a 96-week, randomized, controlled trial designed to evaluate the effects of supplementation with 20,000 IU/week of vitamin D (averaged to approximately 2800 IU/day) on bone mineral density in 35 MS patients, Kampman and colleagues found that consumption of vitamin D did not result in beneficial effects on the measured MS-related outcomes, which included annualized relapse rates. However, the study was not powered to address clinical outcomes [ 73 ]. The authors suggested that the low annualized relapse rate seen at baseline could have contributed to the absence of significant effects in this study. Study limitations included a small sample size ( N = 68), which may be inadequate for assessing effects on clinical outcomes [ 73 ].
Furthermore, two studies from Iran did not find a beneficial effect of vitamin D supplementation on clinical or MRI outcome measures in patients with RRMS. Shaygannejad and colleagues studied 50 patients in a 12-month, randomized, double-blind, placebo-controlled, phase 2 clinical trial [ 74 ]. The 25 patients in the treatment group received 4000 IU/day of vitamin D for the first 2 weeks and were thereafter escalated to 8000 IU/day in addition to their disease-modifying agent. The control group ( n = 25) was treated with placebo combined with disease-modifying therapy. In a separate study, Mosayebi and colleagues evaluated the effects of vitamin D3 supplementation at a dose of 300,000 IU/month vs. placebo in a randomized, prospective study with 62 patients [ 71 ]. Over the 6-month observation period, no differences between groups on either EDSS or Gd+ lesion count were observed, but immune-inhibitory transforming growth factor beta and interleukin 10 were significantly higher in the vitamin D-supplemented group compared with placebo [ 71 ].
Several of the studies above were included in a meta-analysis conducted by James and colleagues evaluating the effect of vitamin D-related intervention trials on MS relapses [ 85 ]. The five studies [ 22 , 72 – 75 ] included 129 patients with high-dose vitamin D supplementations and 125 controls. Administered doses of vitamin D supplementations, study designs, patient populations, outcome parameters, and observation period were considerably variable among the assessed studies. Given these differences, the numerous limitations of each of these studies and the mixed reported study results, it is not surprising that the meta-analysis did not find a significant association between vitamin D treatment and the relative risk of relapse in MS [ 85 ]. In the view of the authors, “further larger and more prolonged studies…are merited” to better understand the role of vitamin D supplementation in MS [ 85 ].
Ongoing Studies Evaluating the Role of Supplemental Vitamin D in MS
A search of recently initiated and ongoing clinical studies evaluating the role of supplemental vitamin D in MS revealed the following:
- The Efficacy of Vitamin D Supplementation in Multiple Sclerosis (EVIDIMS) study ( {"type":"clinical-trial","attrs":{"text":"NCT01440062","term_id":"NCT01440062"}} NCT01440062 ) [ 86 , 87 ] is a German multicenter, stratified, randomized, controlled, double-blind, clinical phase 2 study. Eighty patients with CIS or MS whose disease courses were stable while taking IFNB-1b were randomized to receive either high-dose (on average, 10,200 IU/day) or low-dose (on average 200 IU/day) vitamin D3 for 18 months as a supplement. The primary outcome measure is the number of new T2 lesions. Secondary endpoints include additional MRI and optical coherence tomography (OCT) parameters, clinical parameters, as well as cognition, fatigue, depression, and quality of life. Safety and tolerability of high-dose vitamin D supplementation are additional outcome measures. This study is ongoing, and results are expected in 2018 or 2019.
- The Vitamin D to Ameliorate Multiple Sclerosis (VIDAMS) study ( {"type":"clinical-trial","attrs":{"text":"NCT01490502","term_id":"NCT01490502"}} NCT01490502 ) [88, 90] is a randomized, controlled, phase 3 study that aims to include 172 patients in the US. After a run-in phase of 1 month on GA, patients will be assigned to low-dose (600 IU/day) vs. high-dose (5000 IU/day) vitamin D3 as an add-on therapy to GA. This academic study is currently recruiting patients and will terminate in 2018 [ 86 , 88 ]. Clinical and MRI parameters will also be evaluated.
Summary and Conclusions
Evidence available to date suggests that the level of serum vitamin D affects the risk of developing MS and also modifies disease activity in MS patients. Until several years ago, evidence that higher levels of vitamin D are associated with favorable effects on MS risk and a reduction in MS activity was supported largely by observational studies. Limitations of these studies restricted confidence in a specific effect of vitamin D in MS. Newer data with Mendelian randomization analyses suggest there is a causal relationship between low vitamin D level and the risk of MS. Furthermore, post hoc evaluations from the phase 3 BENEFIT and BEYOND studies substantiate findings of observational trials. Across all trials, associations between 25(OH) levels and MS and its activity are generally stronger for MRI than for clinical outcomes, which may be due to the higher sensitivity of MRI compared to typical clinical parameters. Low or even insufficient 25(OH)D levels were common in many earlier cohorts. Patients in more recent studies have higher baseline vitamin D levels, potentially changing the immunopathology of MS and altering responses to some therapeutic drugs.
In aggregate, studies suggest that vitamin D supplementation may be beneficial for patients with MS and others. However, the study limitations identified in this review recognize the need for larger controlled clinical trials to establish vitamin D supplementation as the standard of care for MS patients. Though there is increasing evidence indicating that lower vitamin D levels are associated with increased risk of MS and greater clinical and brain MRI activity in established MS, the impact of vitamin D supplementation on MS activity remains inadequately investigated. There is no consensus on “sufficient” vitamin D levels. In the view of IOM, 25(OH)D levels greater than 50 nmol/L (20 ng/mL) are sufficient. The Endocrine Society argues for 75 nmol/L (30 ng/mL) or higher, based on a medical model which takes into account skeletal and non-skeletal health. Numerous studies suggest that serum 25(OH)D levels of approximately 100 nmol/L (40 ng/mL) are the lower limit for controlling MRI and clinical activity in patients with MS. More research is needed to establish the recommended levels of vitamin D supplementation necessary to reduce the risk for MS and MS clinical activity.
In conclusion, based on the data reviewed, identification and correction of vitamin D insufficiency with supplementation at recommended doses is a sensible clinical action/course/target/objective and one that provides a favorable risk–benefit profile for vitamin D for most patients with MS.
Acknowledgements
Funding for medical writing assistance, as well as any applicable article processing fees and Open Access fee was provided by Bayer HealthCare Pharmaceuticals.
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Writing Assistance
Editorial assistance in the preparation of this manuscript was provided by Staci Brandt, PA-C, MBA, MS and Maria Bavishi, MS from Global Prairie Marketing, LLC.
Disclosures
Martina B Sintzel, PhD has received consultancy fees from Bayer and Fresenius. Mark Rametta, D.O is employed by Bayer. Anthony T. Reder, MD has received unrestricted grant and clinical trials support from Bayer, Biogen, Novartis, Serono, and Teva.
Compliance with Ethics Guidelines
This article is based on previously conducted studies, and as such, and does not involve any new studies of human or animal subjects performed by any of the authors.
Data Availability
Open access.
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License ( http://creativecommons.org/licenses/by-nc/4.0/ ), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/F5FCF060794BDA24 .
Medindia » News » Clinical Trials News » Hope for Multiple Sclerosis: A Breakthrough Drug Developed
Hope for Multiple Sclerosis: A Breakthrough Drug Developed
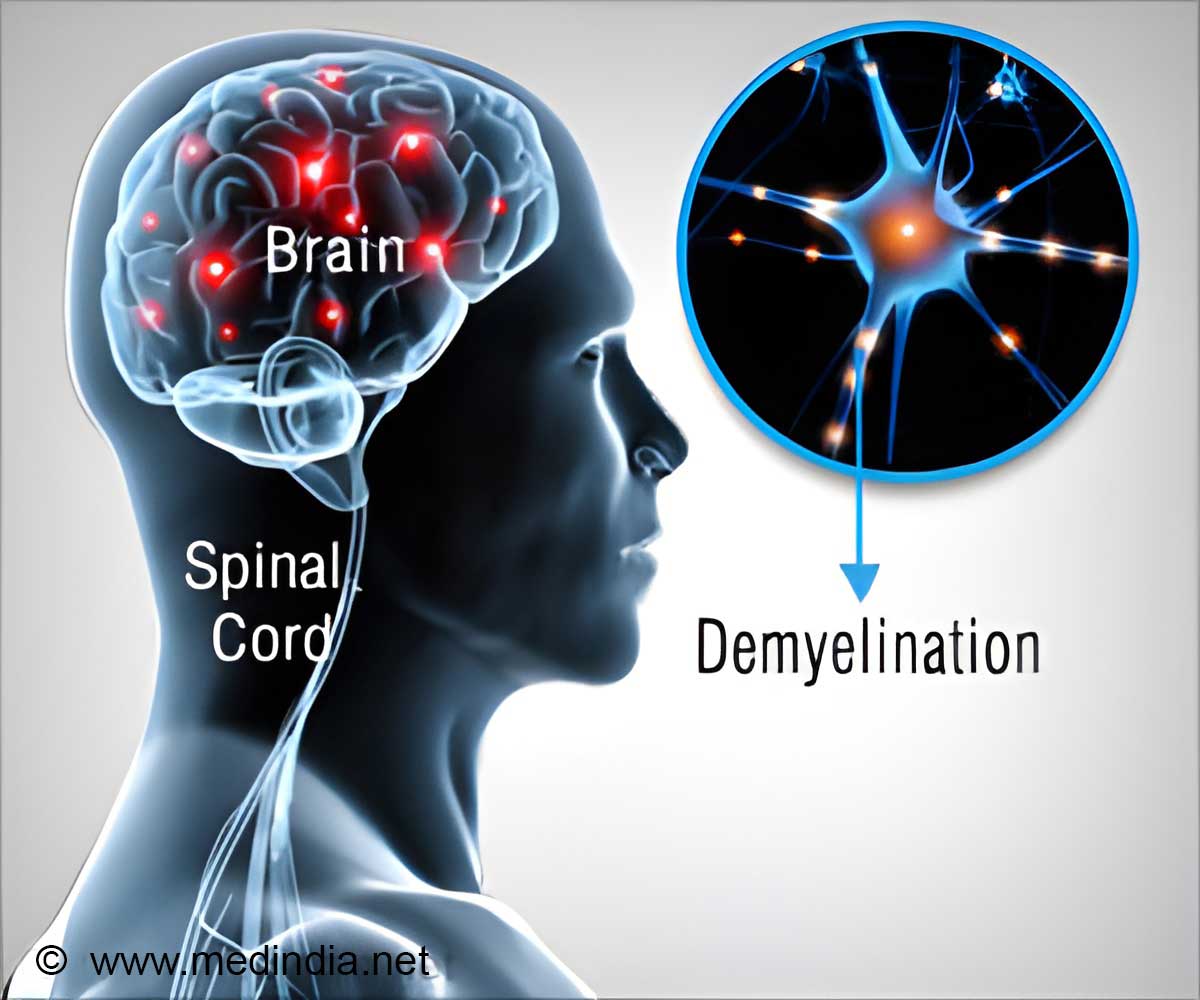
Multiple Sclerosis and its Effects

How the New Drug Would Help Multiple Sclerosis?

How Clemastine - An Antihistaminic, Led to the New Drug!
A Snake Toxin Guided to the Target Receptors!
New drug and its clinical trials â a potential for halting and curing the disease.
- A cure for multiple sclerosis? Scientists say within our lifetime - (https:www.universityofcalifornia.edu/news/cure-multiple-sclerosis-scientists-say-within-our-lifetime)
| --> --> |

- Consult Online Doctor
- Take Telemedicine course
- Health Centers
- Health Tools
- Health info by Speciality
- Know Your Body
- Health and Wellness
- Web Stories
- Newsletters
- Health Tips
- Nutrition Facts
- Lifestyle & Wellness
- Beauty Tips
- Diet & Nutrition
- Home Remedies
- Obesity & Weight Loss
- Complementary Medicine
- Special Reports
- Press Releases
- Health Guide
- Health articles
- Health Quiz
- Health Facts
- Travel Health
- Medicine and Movies
- Symptom Articles
- Diabetes Tools
- Pediatric Calculators
- Men's Health
- Women's Health
- Height Weight Tools
- Cardiac Tools
- Pharma Tools
- Wellness Interactive Tools
- Drug Information
- Drugs by Condition
- Drug Price List - Brand Names
- Drug Interaction with Food
- Drug Price List - Generic Names
- Drugs - Side Effects
- Drug Videos
- Drug Database
- Allopathy Doctors
- Alternative Medicine Doctors
- Physiotherapist
- Speech Therapist
- Sexologists
- Hospital Directory
- Diagnostic Lab Directory
- Pharmacy or Chemist
- Medical Equipment Suppliers
- Pharma Directory
- Emergency Services
- PG Education
- Family Medicine
- Other Resources
- Medical Aphorism
- Health Acts in India
- Health Quotations
- Medical Conference
- Amazing Body Facts
- Health poll

- Editorial Team
- Exclusive Interviews
- In the News
- Partners & Affiliates
- Advertise With Us
- हिन्दी
- français
- Español
- 中文
Daniel Bandari, MD, MS - Multiple Sclerosis Center of California
Photos & videos.
See all 7 photos

Review Highlights

“ Ashley goes above and beyond in her position as the office manager. ” in 4 reviews

“ Dr Bandari has been treating my MS for several years and I wouldn't trust anyone else to take care of me. ” in 11 reviews

“ I have taken my sister to ER in Palm Springs and have witnessed Dr. ” in 2 reviews
Location & Hours
Suggest an edit
24012 Calle De La Plata
Laguna Hills, CA 92653
| Closed now | |
Amenities and More
Ask the community.
Ask a question
Yelp users haven’t asked any questions yet about Daniel Bandari, MD, MS - Multiple Sclerosis Center of California .
People also searched for
Mayo Clinic
Headache Specialist
Psychologists
Infusion Center
Pediatric Neurologist
Recommended Reviews

IMAGES
COMMENTS
Multiple Sclerosis (MS) is a growing global health challenge affecting nearly 3 million people with significant public health and economic impacts. 1 While substantial progress has been made in the development of more than a dozen effective disease-modifying treatments (DMTs) for relapsing forms of MS, we still lack a fundamental understanding of all the pathological processes driving disease ...
Introduction. Multiple sclerosis (MS) is a chronic autoimmune disease of the central nervous system (CNS) in which the immune system attacks myelin sheaths, the insulating layer that forms around the nerves of the CNS, leading to the accumulation of nerve damage over time [].This neurodegeneration can lead to a variety of clinical symptoms that can vary from patient to patient.
It was approved for use in 2019 after it was shown to possess the same medicinal benefits with fewer side effects. Ozanimod (Zeposia): This medication has been approved to treat three types of MS: clinically isolated syndrome, relapsing-remitting MS, and active secondary progression MS. It received FDA approval in March 2020.
A generation ago, most people with multiple sclerosis could expect to rely on walkers and wheelchairs or be limited to their bed within 15 years of diagnosis. Today, UC San Francisco's discoveries are keeping millions with MS healthier for longer - many disability-free. Now, the university is paving the way for an MS cure in our lifetimes.
MS Research. Our Pathways to Cures initiative is the biggest, most collaborative MS research effort of our time. MS organizations and scientific leaders from across the globe have chosen this roadmap as the way forward to stop disease progression, restore lost function and end MS forever. Our vision is nothing less than a world free of MS.
Multiple sclerosis (MS) is a chronic autoimmune disease of the central nervous system (CNS) characterized by inflammation and neurodegeneration. ... Dietary antioxidant factors can dampen oxidative stress and may help against chronic demyelination and ... omega-3 PUFAs, and polyphenol compounds. However, further research is needed in order to ...
The treatment of multiple sclerosis has been transformed by the successful development of immunotherapies that efficiently reduce disease activity and related clinical relapses during the relapsing-remitting phase of the disease. However, the prevention of disability progression, which is due to axonal and neuronal damage and loss, has yet to be achieved and is therapeutically challenging ...
Multiple sclerosis (MS) is the most common chronic inflammatory, demyelinating and neurodegenerative disease of the central nervous system in young adults. This disorder is a heterogeneous ...
Jeffrey Dunn, who is running the first trial of Kyverna's CAR T cells in the United States, will be watching closely for brain toxicity, which he says seems to be linked to the number of B cells ...
Multiple sclerosis is an autoimmune disease in which immune cells attack and destroy the protective myelin sheaths that surround nerve fibres, leading to neurological disturbances. Latest Research ...
There is no cure for multiple sclerosis. Treatment typically focuses on speeding recovery from attacks, reducing new radiographic and clinical relapses, slowing the progression of the disease, and managing MS symptoms. Some people have such mild symptoms that no treatment is necessary. Multiple sclerosis research laboratory at Mayo Clinic.
The term multiple sclerosis refers to the distinctive areas of scar tissue (sclerosis—also called plaques or lesions) that result from the attack on myelin by the immune system. These plaques are visible using magnetic resonance imaging (MRI). Plaques can be as small as a pinhead or as large as a golf ball.
Summary of main results. This review systematically summarised the best, up‐to‐date evidence from published Cochrane Reviews for the effectiveness of rehabilitation interventions in people with multiple sclerosis (pwMS). Rehabilitation is considered to be a key supportive treatment in MS.
Through research in the Center for Multiple Sclerosis and Autoimmune Neurology, Mayo Clinic is at the forefront of scientific advances to uncover the inner workings of MS, to better understand disease progression and to identify new targets for therapy. Using our unique, team-based model of research, we apply the latest knowledge and resources ...
Several MS specialists used the word "dramatic" to describe the change in treatment options over the past 20 years. Interferon-beta became available in the mid-90s and was the first disease-modifying therapy that reduced relapse rates and delayed the onset of disability. But now there are more than 20 therapies available in different forms.
By participating in MS research studies, you can help shape the future for those affected by MS. Learn more about the various opportunities for participation. ... The National Multiple Sclerosis Society is proud to be a source of information on multiple sclerosis related topics. Unless otherwise indicated, the information provided is based on ...
People with multiple sclerosis may also develop: Muscle stiffness or spasms. Severe weakness or paralysis, typically in the legs. Problems with bladder, bowel or sexual function. Cognitive problems, like forgetfulness or word finding difficulties. Mood problems, such as depression, anxiety or mood swings.
Multiple sclerosis is driven by inflammation in the brain and spinal cord, which causes damage to the myelin sheath, a fatty covering around nerve fibers that helps nerves to send electrical signals.
Multiple sclerosis is an unpredictable disease of the central nervous system. The central nervous system includes the brain, spinal cord and optic nerves. This system controls everything we do. MS disrupts the flow of information within the brain, and between the brain and body. An individual's experience with MS may change from day to day ...
Multiple sclerosis (MS) degrades the protective insulation around nerve cells, leaving their axons, which carry electrical impulses, exposed like bare wires. This can cause devastating problems ...
Multiple sclerosis (MS) degrades the protective insulation around nerve cells, leaving their axons, which carry electrical impulses, exposed like bare wires. This can cause devastating problems with movement, balance and vision; and without treatment, it can lead to paralysis, loss of independence and a shortened lifespan.
Research has raised questions about whether multiple sclerosis (MS) changes people's empathy levels. However, results showing reduced empathy with MS are not proven in all studies and certainly don't apply to everyone. In people with MS, the level of empathy can vary widely due to factors like personality differences.
Abstract. Multiple sclerosis (MS) is a chronic inflammatory disease characterized by central nervous system (CNS) lesions that can lead to severe physical or cognitive disability as well as neurological defects. Although the etiology and pathogenesis of MS remains unclear, the present documents illustrate that the cause of MS is multifactorial ...
Kessler Foundation research scientist John DeLuca, Ph.D., has published a clinical article in Journal of Neurology, shedding light on the elusive nature of fatigue in multiple sclerosis (MS) and ...
Anxiety is a common symptom of multiple sclerosis (MS). Learn more about the link between MS and anxiety, and find out how to get help. ... and memory retrieval) that occur with MS. Research also suggests that it may be due to living with the unpredictability of MS rather than the ... They can help you find resources and make a referral to a ...
People with multiple sclerosis (MS) and other conditions who use Mallinckrodt's treatment Acthar Gel (repository corticotropin injection) now have a self-injection option, the company said ...
Since multiple sclerosis (MS) is considered an autoimmune disease, it is of interest to review briefly the potential effects of vitamin D related to immune function. The active form of vitamin D plays an essential role in lymphocyte activation and proliferation, T-helper cell differentiation, tissue-specific lymphocyte homing, the production of ...
A promising new medication for treating multiple sclerosis is currently undergoing clinical trials. The new drug is a result of a decade of dedicated research, aided by the green mamba snake!
The stronger research only includes truly sober people who do not have a history of alcohol consumption. ... What It's Like Getting Diagnosed With Multiple Sclerosis in Your 20s. 01.23.24. By ...
Specialties: Multiple Sclerosis Center of California provides comprehensive multiple sclerosis (MS) care in Laguna Hills, California. Founder and medical director Daniel Bandari, MD, takes pride in the care he provides to the patients living with MS, NMO and other demyelinating diseases of CNS locally, nationally, and internationally that come to the center, becoming known as the MS physician ...