How to Write Limitations of the Study (with examples)
This blog emphasizes the importance of recognizing and effectively writing about limitations in research. It discusses the types of limitations, their significance, and provides guidelines for writing about them, highlighting their role in advancing scholarly research.
Updated on August 24, 2023

No matter how well thought out, every research endeavor encounters challenges. There is simply no way to predict all possible variances throughout the process.
These uncharted boundaries and abrupt constraints are known as limitations in research . Identifying and acknowledging limitations is crucial for conducting rigorous studies. Limitations provide context and shed light on gaps in the prevailing inquiry and literature.
This article explores the importance of recognizing limitations and discusses how to write them effectively. By interpreting limitations in research and considering prevalent examples, we aim to reframe the perception from shameful mistakes to respectable revelations.

What are limitations in research?
In the clearest terms, research limitations are the practical or theoretical shortcomings of a study that are often outside of the researcher’s control . While these weaknesses limit the generalizability of a study’s conclusions, they also present a foundation for future research.
Sometimes limitations arise from tangible circumstances like time and funding constraints, or equipment and participant availability. Other times the rationale is more obscure and buried within the research design. Common types of limitations and their ramifications include:
- Theoretical: limits the scope, depth, or applicability of a study.
- Methodological: limits the quality, quantity, or diversity of the data.
- Empirical: limits the representativeness, validity, or reliability of the data.
- Analytical: limits the accuracy, completeness, or significance of the findings.
- Ethical: limits the access, consent, or confidentiality of the data.
Regardless of how, when, or why they arise, limitations are a natural part of the research process and should never be ignored . Like all other aspects, they are vital in their own purpose.
Why is identifying limitations important?
Whether to seek acceptance or avoid struggle, humans often instinctively hide flaws and mistakes. Merging this thought process into research by attempting to hide limitations, however, is a bad idea. It has the potential to negate the validity of outcomes and damage the reputation of scholars.
By identifying and addressing limitations throughout a project, researchers strengthen their arguments and curtail the chance of peer censure based on overlooked mistakes. Pointing out these flaws shows an understanding of variable limits and a scrupulous research process.
Showing awareness of and taking responsibility for a project’s boundaries and challenges validates the integrity and transparency of a researcher. It further demonstrates the researchers understand the applicable literature and have thoroughly evaluated their chosen research methods.
Presenting limitations also benefits the readers by providing context for research findings. It guides them to interpret the project’s conclusions only within the scope of very specific conditions. By allowing for an appropriate generalization of the findings that is accurately confined by research boundaries and is not too broad, limitations boost a study’s credibility .
Limitations are true assets to the research process. They highlight opportunities for future research. When researchers identify the limitations of their particular approach to a study question, they enable precise transferability and improve chances for reproducibility.
Simply stating a project’s limitations is not adequate for spurring further research, though. To spark the interest of other researchers, these acknowledgements must come with thorough explanations regarding how the limitations affected the current study and how they can potentially be overcome with amended methods.
How to write limitations
Typically, the information about a study’s limitations is situated either at the beginning of the discussion section to provide context for readers or at the conclusion of the discussion section to acknowledge the need for further research. However, it varies depending upon the target journal or publication guidelines.
Don’t hide your limitations
It is also important to not bury a limitation in the body of the paper unless it has a unique connection to a topic in that section. If so, it needs to be reiterated with the other limitations or at the conclusion of the discussion section. Wherever it is included in the manuscript, ensure that the limitations section is prominently positioned and clearly introduced.
While maintaining transparency by disclosing limitations means taking a comprehensive approach, it is not necessary to discuss everything that could have potentially gone wrong during the research study. If there is no commitment to investigation in the introduction, it is unnecessary to consider the issue a limitation to the research. Wholly consider the term ‘limitations’ and ask, “Did it significantly change or limit the possible outcomes?” Then, qualify the occurrence as either a limitation to include in the current manuscript or as an idea to note for other projects.
Writing limitations
Once the limitations are concretely identified and it is decided where they will be included in the paper, researchers are ready for the writing task. Including only what is pertinent, keeping explanations detailed but concise, and employing the following guidelines is key for crafting valuable limitations:
1) Identify and describe the limitations : Clearly introduce the limitation by classifying its form and specifying its origin. For example:
- An unintentional bias encountered during data collection
- An intentional use of unplanned post-hoc data analysis
2) Explain the implications : Describe how the limitation potentially influences the study’s findings and how the validity and generalizability are subsequently impacted. Provide examples and evidence to support claims of the limitations’ effects without making excuses or exaggerating their impact. Overall, be transparent and objective in presenting the limitations, without undermining the significance of the research.
3) Provide alternative approaches for future studies : Offer specific suggestions for potential improvements or avenues for further investigation. Demonstrate a proactive approach by encouraging future research that addresses the identified gaps and, therefore, expands the knowledge base.
Whether presenting limitations as an individual section within the manuscript or as a subtopic in the discussion area, authors should use clear headings and straightforward language to facilitate readability. There is no need to complicate limitations with jargon, computations, or complex datasets.
Examples of common limitations
Limitations are generally grouped into two categories , methodology and research process .
Methodology limitations
Methodology may include limitations due to:
- Sample size
- Lack of available or reliable data
- Lack of prior research studies on the topic
- Measure used to collect the data
- Self-reported data

The researcher is addressing how the large sample size requires a reassessment of the measures used to collect and analyze the data.
Research process limitations
Limitations during the research process may arise from:
- Access to information
- Longitudinal effects
- Cultural and other biases
- Language fluency
- Time constraints

The author is pointing out that the model’s estimates are based on potentially biased observational studies.
Final thoughts
Successfully proving theories and touting great achievements are only two very narrow goals of scholarly research. The true passion and greatest efforts of researchers comes more in the form of confronting assumptions and exploring the obscure.
In many ways, recognizing and sharing the limitations of a research study both allows for and encourages this type of discovery that continuously pushes research forward. By using limitations to provide a transparent account of the project's boundaries and to contextualize the findings, researchers pave the way for even more robust and impactful research in the future.
Charla Viera, MS
See our "Privacy Policy"
Ensure your structure and ideas are consistent and clearly communicated
Pair your Premium Editing with our add-on service Presubmission Review for an overall assessment of your manuscript.
- USC Libraries
- Research Guides
Organizing Your Social Sciences Research Paper
- Limitations of the Study
- Purpose of Guide
- Design Flaws to Avoid
- Independent and Dependent Variables
- Glossary of Research Terms
- Reading Research Effectively
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Extending the Timeliness of a Topic Idea
- Academic Writing Style
- Applying Critical Thinking
- Choosing a Title
- Making an Outline
- Paragraph Development
- Research Process Video Series
- Executive Summary
- The C.A.R.S. Model
- Background Information
- The Research Problem/Question
- Theoretical Framework
- Citation Tracking
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tiertiary Sources
- Scholarly vs. Popular Publications
- Qualitative Methods
- Quantitative Methods
- Insiderness
- Using Non-Textual Elements
- Common Grammar Mistakes
- Writing Concisely
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Generative AI and Writing
- USC Libraries Tutorials and Other Guides
- Bibliography
The limitations of the study are those characteristics of design or methodology that impacted or influenced the interpretation of the findings from your research. Study limitations are the constraints placed on the ability to generalize from the results, to further describe applications to practice, and/or related to the utility of findings that are the result of the ways in which you initially chose to design the study or the method used to establish internal and external validity or the result of unanticipated challenges that emerged during the study.
Price, James H. and Judy Murnan. “Research Limitations and the Necessity of Reporting Them.” American Journal of Health Education 35 (2004): 66-67; Theofanidis, Dimitrios and Antigoni Fountouki. "Limitations and Delimitations in the Research Process." Perioperative Nursing 7 (September-December 2018): 155-163. .
Importance of...
Always acknowledge a study's limitations. It is far better that you identify and acknowledge your study’s limitations than to have them pointed out by your professor and have your grade lowered because you appeared to have ignored them or didn't realize they existed.
Keep in mind that acknowledgment of a study's limitations is an opportunity to make suggestions for further research. If you do connect your study's limitations to suggestions for further research, be sure to explain the ways in which these unanswered questions may become more focused because of your study.
Acknowledgment of a study's limitations also provides you with opportunities to demonstrate that you have thought critically about the research problem, understood the relevant literature published about it, and correctly assessed the methods chosen for studying the problem. A key objective of the research process is not only discovering new knowledge but also to confront assumptions and explore what we don't know.
Claiming limitations is a subjective process because you must evaluate the impact of those limitations . Don't just list key weaknesses and the magnitude of a study's limitations. To do so diminishes the validity of your research because it leaves the reader wondering whether, or in what ways, limitation(s) in your study may have impacted the results and conclusions. Limitations require a critical, overall appraisal and interpretation of their impact. You should answer the question: do these problems with errors, methods, validity, etc. eventually matter and, if so, to what extent?
Price, James H. and Judy Murnan. “Research Limitations and the Necessity of Reporting Them.” American Journal of Health Education 35 (2004): 66-67; Structure: How to Structure the Research Limitations Section of Your Dissertation. Dissertations and Theses: An Online Textbook. Laerd.com.
Descriptions of Possible Limitations
All studies have limitations . However, it is important that you restrict your discussion to limitations related to the research problem under investigation. For example, if a meta-analysis of existing literature is not a stated purpose of your research, it should not be discussed as a limitation. Do not apologize for not addressing issues that you did not promise to investigate in the introduction of your paper.
Here are examples of limitations related to methodology and the research process you may need to describe and discuss how they possibly impacted your results. Note that descriptions of limitations should be stated in the past tense because they were discovered after you completed your research.
Possible Methodological Limitations
- Sample size -- the number of the units of analysis you use in your study is dictated by the type of research problem you are investigating. Note that, if your sample size is too small, it will be difficult to find significant relationships from the data, as statistical tests normally require a larger sample size to ensure a representative distribution of the population and to be considered representative of groups of people to whom results will be generalized or transferred. Note that sample size is generally less relevant in qualitative research if explained in the context of the research problem.
- Lack of available and/or reliable data -- a lack of data or of reliable data will likely require you to limit the scope of your analysis, the size of your sample, or it can be a significant obstacle in finding a trend and a meaningful relationship. You need to not only describe these limitations but provide cogent reasons why you believe data is missing or is unreliable. However, don’t just throw up your hands in frustration; use this as an opportunity to describe a need for future research based on designing a different method for gathering data.
- Lack of prior research studies on the topic -- citing prior research studies forms the basis of your literature review and helps lay a foundation for understanding the research problem you are investigating. Depending on the currency or scope of your research topic, there may be little, if any, prior research on your topic. Before assuming this to be true, though, consult with a librarian! In cases when a librarian has confirmed that there is little or no prior research, you may be required to develop an entirely new research typology [for example, using an exploratory rather than an explanatory research design ]. Note again that discovering a limitation can serve as an important opportunity to identify new gaps in the literature and to describe the need for further research.
- Measure used to collect the data -- sometimes it is the case that, after completing your interpretation of the findings, you discover that the way in which you gathered data inhibited your ability to conduct a thorough analysis of the results. For example, you regret not including a specific question in a survey that, in retrospect, could have helped address a particular issue that emerged later in the study. Acknowledge the deficiency by stating a need for future researchers to revise the specific method for gathering data.
- Self-reported data -- whether you are relying on pre-existing data or you are conducting a qualitative research study and gathering the data yourself, self-reported data is limited by the fact that it rarely can be independently verified. In other words, you have to the accuracy of what people say, whether in interviews, focus groups, or on questionnaires, at face value. However, self-reported data can contain several potential sources of bias that you should be alert to and note as limitations. These biases become apparent if they are incongruent with data from other sources. These are: (1) selective memory [remembering or not remembering experiences or events that occurred at some point in the past]; (2) telescoping [recalling events that occurred at one time as if they occurred at another time]; (3) attribution [the act of attributing positive events and outcomes to one's own agency, but attributing negative events and outcomes to external forces]; and, (4) exaggeration [the act of representing outcomes or embellishing events as more significant than is actually suggested from other data].
Possible Limitations of the Researcher
- Access -- if your study depends on having access to people, organizations, data, or documents and, for whatever reason, access is denied or limited in some way, the reasons for this needs to be described. Also, include an explanation why being denied or limited access did not prevent you from following through on your study.
- Longitudinal effects -- unlike your professor, who can literally devote years [even a lifetime] to studying a single topic, the time available to investigate a research problem and to measure change or stability over time is constrained by the due date of your assignment. Be sure to choose a research problem that does not require an excessive amount of time to complete the literature review, apply the methodology, and gather and interpret the results. If you're unsure whether you can complete your research within the confines of the assignment's due date, talk to your professor.
- Cultural and other type of bias -- we all have biases, whether we are conscience of them or not. Bias is when a person, place, event, or thing is viewed or shown in a consistently inaccurate way. Bias is usually negative, though one can have a positive bias as well, especially if that bias reflects your reliance on research that only support your hypothesis. When proof-reading your paper, be especially critical in reviewing how you have stated a problem, selected the data to be studied, what may have been omitted, the manner in which you have ordered events, people, or places, how you have chosen to represent a person, place, or thing, to name a phenomenon, or to use possible words with a positive or negative connotation. NOTE : If you detect bias in prior research, it must be acknowledged and you should explain what measures were taken to avoid perpetuating that bias. For example, if a previous study only used boys to examine how music education supports effective math skills, describe how your research expands the study to include girls.
- Fluency in a language -- if your research focuses , for example, on measuring the perceived value of after-school tutoring among Mexican-American ESL [English as a Second Language] students and you are not fluent in Spanish, you are limited in being able to read and interpret Spanish language research studies on the topic or to speak with these students in their primary language. This deficiency should be acknowledged.
Aguinis, Hermam and Jeffrey R. Edwards. “Methodological Wishes for the Next Decade and How to Make Wishes Come True.” Journal of Management Studies 51 (January 2014): 143-174; Brutus, Stéphane et al. "Self-Reported Limitations and Future Directions in Scholarly Reports: Analysis and Recommendations." Journal of Management 39 (January 2013): 48-75; Senunyeme, Emmanuel K. Business Research Methods. Powerpoint Presentation. Regent University of Science and Technology; ter Riet, Gerben et al. “All That Glitters Isn't Gold: A Survey on Acknowledgment of Limitations in Biomedical Studies.” PLOS One 8 (November 2013): 1-6.
Structure and Writing Style
Information about the limitations of your study are generally placed either at the beginning of the discussion section of your paper so the reader knows and understands the limitations before reading the rest of your analysis of the findings, or, the limitations are outlined at the conclusion of the discussion section as an acknowledgement of the need for further study. Statements about a study's limitations should not be buried in the body [middle] of the discussion section unless a limitation is specific to something covered in that part of the paper. If this is the case, though, the limitation should be reiterated at the conclusion of the section.
If you determine that your study is seriously flawed due to important limitations , such as, an inability to acquire critical data, consider reframing it as an exploratory study intended to lay the groundwork for a more complete research study in the future. Be sure, though, to specifically explain the ways that these flaws can be successfully overcome in a new study.
But, do not use this as an excuse for not developing a thorough research paper! Review the tab in this guide for developing a research topic . If serious limitations exist, it generally indicates a likelihood that your research problem is too narrowly defined or that the issue or event under study is too recent and, thus, very little research has been written about it. If serious limitations do emerge, consult with your professor about possible ways to overcome them or how to revise your study.
When discussing the limitations of your research, be sure to:
- Describe each limitation in detailed but concise terms;
- Explain why each limitation exists;
- Provide the reasons why each limitation could not be overcome using the method(s) chosen to acquire or gather the data [cite to other studies that had similar problems when possible];
- Assess the impact of each limitation in relation to the overall findings and conclusions of your study; and,
- If appropriate, describe how these limitations could point to the need for further research.
Remember that the method you chose may be the source of a significant limitation that has emerged during your interpretation of the results [for example, you didn't interview a group of people that you later wish you had]. If this is the case, don't panic. Acknowledge it, and explain how applying a different or more robust methodology might address the research problem more effectively in a future study. A underlying goal of scholarly research is not only to show what works, but to demonstrate what doesn't work or what needs further clarification.
Aguinis, Hermam and Jeffrey R. Edwards. “Methodological Wishes for the Next Decade and How to Make Wishes Come True.” Journal of Management Studies 51 (January 2014): 143-174; Brutus, Stéphane et al. "Self-Reported Limitations and Future Directions in Scholarly Reports: Analysis and Recommendations." Journal of Management 39 (January 2013): 48-75; Ioannidis, John P.A. "Limitations are not Properly Acknowledged in the Scientific Literature." Journal of Clinical Epidemiology 60 (2007): 324-329; Pasek, Josh. Writing the Empirical Social Science Research Paper: A Guide for the Perplexed. January 24, 2012. Academia.edu; Structure: How to Structure the Research Limitations Section of Your Dissertation. Dissertations and Theses: An Online Textbook. Laerd.com; What Is an Academic Paper? Institute for Writing Rhetoric. Dartmouth College; Writing the Experimental Report: Methods, Results, and Discussion. The Writing Lab and The OWL. Purdue University.
Writing Tip
Don't Inflate the Importance of Your Findings!
After all the hard work and long hours devoted to writing your research paper, it is easy to get carried away with attributing unwarranted importance to what you’ve done. We all want our academic work to be viewed as excellent and worthy of a good grade, but it is important that you understand and openly acknowledge the limitations of your study. Inflating the importance of your study's findings could be perceived by your readers as an attempt hide its flaws or encourage a biased interpretation of the results. A small measure of humility goes a long way!
Another Writing Tip
Negative Results are Not a Limitation!
Negative evidence refers to findings that unexpectedly challenge rather than support your hypothesis. If you didn't get the results you anticipated, it may mean your hypothesis was incorrect and needs to be reformulated. Or, perhaps you have stumbled onto something unexpected that warrants further study. Moreover, the absence of an effect may be very telling in many situations, particularly in experimental research designs. In any case, your results may very well be of importance to others even though they did not support your hypothesis. Do not fall into the trap of thinking that results contrary to what you expected is a limitation to your study. If you carried out the research well, they are simply your results and only require additional interpretation.
Lewis, George H. and Jonathan F. Lewis. “The Dog in the Night-Time: Negative Evidence in Social Research.” The British Journal of Sociology 31 (December 1980): 544-558.
Yet Another Writing Tip
Sample Size Limitations in Qualitative Research
Sample sizes are typically smaller in qualitative research because, as the study goes on, acquiring more data does not necessarily lead to more information. This is because one occurrence of a piece of data, or a code, is all that is necessary to ensure that it becomes part of the analysis framework. However, it remains true that sample sizes that are too small cannot adequately support claims of having achieved valid conclusions and sample sizes that are too large do not permit the deep, naturalistic, and inductive analysis that defines qualitative inquiry. Determining adequate sample size in qualitative research is ultimately a matter of judgment and experience in evaluating the quality of the information collected against the uses to which it will be applied and the particular research method and purposeful sampling strategy employed. If the sample size is found to be a limitation, it may reflect your judgment about the methodological technique chosen [e.g., single life history study versus focus group interviews] rather than the number of respondents used.
Boddy, Clive Roland. "Sample Size for Qualitative Research." Qualitative Market Research: An International Journal 19 (2016): 426-432; Huberman, A. Michael and Matthew B. Miles. "Data Management and Analysis Methods." In Handbook of Qualitative Research . Norman K. Denzin and Yvonna S. Lincoln, eds. (Thousand Oaks, CA: Sage, 1994), pp. 428-444; Blaikie, Norman. "Confounding Issues Related to Determining Sample Size in Qualitative Research." International Journal of Social Research Methodology 21 (2018): 635-641; Oppong, Steward Harrison. "The Problem of Sampling in qualitative Research." Asian Journal of Management Sciences and Education 2 (2013): 202-210.
- << Previous: 8. The Discussion
- Next: 9. The Conclusion >>
- Last Updated: Sep 4, 2024 9:40 AM
- URL: https://libguides.usc.edu/writingguide
- Privacy Policy

Home » Limitations in Research – Types, Examples and Writing Guide
Limitations in Research – Types, Examples and Writing Guide
Table of Contents

Limitations in Research
Limitations in research refer to the factors that may affect the results, conclusions , and generalizability of a study. These limitations can arise from various sources, such as the design of the study, the sampling methods used, the measurement tools employed, and the limitations of the data analysis techniques.
Types of Limitations in Research
Types of Limitations in Research are as follows:
Sample Size Limitations
This refers to the size of the group of people or subjects that are being studied. If the sample size is too small, then the results may not be representative of the population being studied. This can lead to a lack of generalizability of the results.
Time Limitations
Time limitations can be a constraint on the research process . This could mean that the study is unable to be conducted for a long enough period of time to observe the long-term effects of an intervention, or to collect enough data to draw accurate conclusions.
Selection Bias
This refers to a type of bias that can occur when the selection of participants in a study is not random. This can lead to a biased sample that is not representative of the population being studied.
Confounding Variables
Confounding variables are factors that can influence the outcome of a study, but are not being measured or controlled for. These can lead to inaccurate conclusions or a lack of clarity in the results.
Measurement Error
This refers to inaccuracies in the measurement of variables, such as using a faulty instrument or scale. This can lead to inaccurate results or a lack of validity in the study.
Ethical Limitations
Ethical limitations refer to the ethical constraints placed on research studies. For example, certain studies may not be allowed to be conducted due to ethical concerns, such as studies that involve harm to participants.
Examples of Limitations in Research
Some Examples of Limitations in Research are as follows:
Research Title: “The Effectiveness of Machine Learning Algorithms in Predicting Customer Behavior”
Limitations:
- The study only considered a limited number of machine learning algorithms and did not explore the effectiveness of other algorithms.
- The study used a specific dataset, which may not be representative of all customer behaviors or demographics.
- The study did not consider the potential ethical implications of using machine learning algorithms in predicting customer behavior.
Research Title: “The Impact of Online Learning on Student Performance in Computer Science Courses”
- The study was conducted during the COVID-19 pandemic, which may have affected the results due to the unique circumstances of remote learning.
- The study only included students from a single university, which may limit the generalizability of the findings to other institutions.
- The study did not consider the impact of individual differences, such as prior knowledge or motivation, on student performance in online learning environments.
Research Title: “The Effect of Gamification on User Engagement in Mobile Health Applications”
- The study only tested a specific gamification strategy and did not explore the effectiveness of other gamification techniques.
- The study relied on self-reported measures of user engagement, which may be subject to social desirability bias or measurement errors.
- The study only included a specific demographic group (e.g., young adults) and may not be generalizable to other populations with different preferences or needs.
How to Write Limitations in Research
When writing about the limitations of a research study, it is important to be honest and clear about the potential weaknesses of your work. Here are some tips for writing about limitations in research:
- Identify the limitations: Start by identifying the potential limitations of your research. These may include sample size, selection bias, measurement error, or other issues that could affect the validity and reliability of your findings.
- Be honest and objective: When describing the limitations of your research, be honest and objective. Do not try to minimize or downplay the limitations, but also do not exaggerate them. Be clear and concise in your description of the limitations.
- Provide context: It is important to provide context for the limitations of your research. For example, if your sample size was small, explain why this was the case and how it may have affected your results. Providing context can help readers understand the limitations in a broader context.
- Discuss implications : Discuss the implications of the limitations for your research findings. For example, if there was a selection bias in your sample, explain how this may have affected the generalizability of your findings. This can help readers understand the limitations in terms of their impact on the overall validity of your research.
- Provide suggestions for future research : Finally, provide suggestions for future research that can address the limitations of your study. This can help readers understand how your research fits into the broader field and can provide a roadmap for future studies.
Purpose of Limitations in Research
There are several purposes of limitations in research. Here are some of the most important ones:
- To acknowledge the boundaries of the study : Limitations help to define the scope of the research project and set realistic expectations for the findings. They can help to clarify what the study is not intended to address.
- To identify potential sources of bias: Limitations can help researchers identify potential sources of bias in their research design, data collection, or analysis. This can help to improve the validity and reliability of the findings.
- To provide opportunities for future research: Limitations can highlight areas for future research and suggest avenues for further exploration. This can help to advance knowledge in a particular field.
- To demonstrate transparency and accountability: By acknowledging the limitations of their research, researchers can demonstrate transparency and accountability to their readers, peers, and funders. This can help to build trust and credibility in the research community.
- To encourage critical thinking: Limitations can encourage readers to critically evaluate the study’s findings and consider alternative explanations or interpretations. This can help to promote a more nuanced and sophisticated understanding of the topic under investigation.
When to Write Limitations in Research
Limitations should be included in research when they help to provide a more complete understanding of the study’s results and implications. A limitation is any factor that could potentially impact the accuracy, reliability, or generalizability of the study’s findings.
It is important to identify and discuss limitations in research because doing so helps to ensure that the results are interpreted appropriately and that any conclusions drawn are supported by the available evidence. Limitations can also suggest areas for future research, highlight potential biases or confounding factors that may have affected the results, and provide context for the study’s findings.
Generally, limitations should be discussed in the conclusion section of a research paper or thesis, although they may also be mentioned in other sections, such as the introduction or methods. The specific limitations that are discussed will depend on the nature of the study, the research question being investigated, and the data that was collected.
Examples of limitations that might be discussed in research include sample size limitations, data collection methods, the validity and reliability of measures used, and potential biases or confounding factors that could have affected the results. It is important to note that limitations should not be used as a justification for poor research design or methodology, but rather as a way to enhance the understanding and interpretation of the study’s findings.
Importance of Limitations in Research
Here are some reasons why limitations are important in research:
- Enhances the credibility of research: Limitations highlight the potential weaknesses and threats to validity, which helps readers to understand the scope and boundaries of the study. This improves the credibility of research by acknowledging its limitations and providing a clear picture of what can and cannot be concluded from the study.
- Facilitates replication: By highlighting the limitations, researchers can provide detailed information about the study’s methodology, data collection, and analysis. This information helps other researchers to replicate the study and test the validity of the findings, which enhances the reliability of research.
- Guides future research : Limitations provide insights into areas for future research by identifying gaps or areas that require further investigation. This can help researchers to design more comprehensive and effective studies that build on existing knowledge.
- Provides a balanced view: Limitations help to provide a balanced view of the research by highlighting both strengths and weaknesses. This ensures that readers have a clear understanding of the study’s limitations and can make informed decisions about the generalizability and applicability of the findings.
Advantages of Limitations in Research
Here are some potential advantages of limitations in research:
- Focus : Limitations can help researchers focus their study on a specific area or population, which can make the research more relevant and useful.
- Realism : Limitations can make a study more realistic by reflecting the practical constraints and challenges of conducting research in the real world.
- Innovation : Limitations can spur researchers to be more innovative and creative in their research design and methodology, as they search for ways to work around the limitations.
- Rigor : Limitations can actually increase the rigor and credibility of a study, as researchers are forced to carefully consider the potential sources of bias and error, and address them to the best of their abilities.
- Generalizability : Limitations can actually improve the generalizability of a study by ensuring that it is not overly focused on a specific sample or situation, and that the results can be applied more broadly.
About the author
Muhammad Hassan
Researcher, Academic Writer, Web developer
You may also like

Figures in Research Paper – Examples and Guide

Research Objectives – Types, Examples and...

Implications in Research – Types, Examples and...

Theoretical Framework – Types, Examples and...

Research Paper Title – Writing Guide and Example

How to Publish a Research Paper – Step by Step...
21 Research Limitations Examples

Chris Drew (PhD)
Dr. Chris Drew is the founder of the Helpful Professor. He holds a PhD in education and has published over 20 articles in scholarly journals. He is the former editor of the Journal of Learning Development in Higher Education. [Image Descriptor: Photo of Chris]
Learn about our Editorial Process
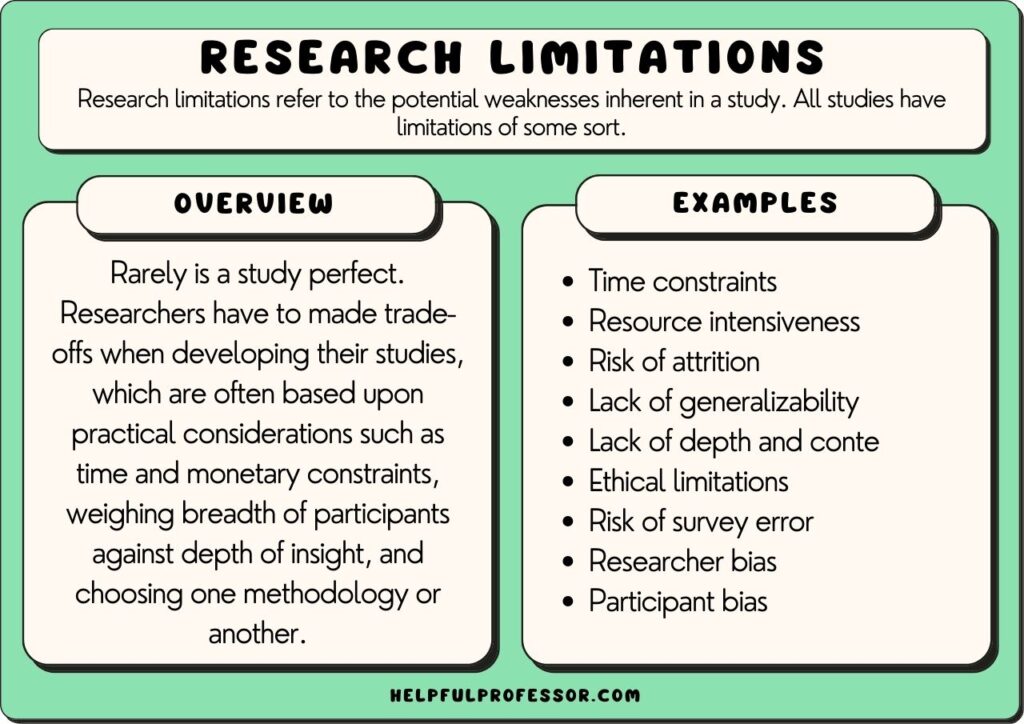
Research limitations refer to the potential weaknesses inherent in a study. All studies have limitations of some sort, meaning declaring limitations doesn’t necessarily need to be a bad thing, so long as your declaration of limitations is well thought-out and explained.
Rarely is a study perfect. Researchers have to make trade-offs when developing their studies, which are often based upon practical considerations such as time and monetary constraints, weighing the breadth of participants against the depth of insight, and choosing one methodology or another.
In research, studies can have limitations such as limited scope, researcher subjectivity, and lack of available research tools.
Acknowledging the limitations of your study should be seen as a strength. It demonstrates your willingness for transparency, humility, and submission to the scientific method and can bolster the integrity of the study. It can also inform future research direction.
Typically, scholars will explore the limitations of their study in either their methodology section, their conclusion section, or both.
Research Limitations Examples
Qualitative and quantitative research offer different perspectives and methods in exploring phenomena, each with its own strengths and limitations. So, I’ve split the limitations examples sections into qualitative and quantitative below.
Qualitative Research Limitations
Qualitative research seeks to understand phenomena in-depth and in context. It focuses on the ‘why’ and ‘how’ questions.
It’s often used to explore new or complex issues, and it provides rich, detailed insights into participants’ experiences, behaviors, and attitudes. However, these strengths also create certain limitations, as explained below.
1. Subjectivity
Qualitative research often requires the researcher to interpret subjective data. One researcher may examine a text and identify different themes or concepts as more dominant than others.
Close qualitative readings of texts are necessarily subjective – and while this may be a limitation, qualitative researchers argue this is the best way to deeply understand everything in context.
Suggested Solution and Response: To minimize subjectivity bias, you could consider cross-checking your own readings of themes and data against other scholars’ readings and interpretations. This may involve giving the raw data to a supervisor or colleague and asking them to code the data separately, then coming together to compare and contrast results.
2. Researcher Bias
The concept of researcher bias is related to, but slightly different from, subjectivity.
Researcher bias refers to the perspectives and opinions you bring with you when doing your research.
For example, a researcher who is explicitly of a certain philosophical or political persuasion may bring that persuasion to bear when interpreting data.
In many scholarly traditions, we will attempt to minimize researcher bias through the utilization of clear procedures that are set out in advance or through the use of statistical analysis tools.
However, in other traditions, such as in postmodern feminist research , declaration of bias is expected, and acknowledgment of bias is seen as a positive because, in those traditions, it is believed that bias cannot be eliminated from research, so instead, it is a matter of integrity to present it upfront.
Suggested Solution and Response: Acknowledge the potential for researcher bias and, depending on your theoretical framework , accept this, or identify procedures you have taken to seek a closer approximation to objectivity in your coding and analysis.
3. Generalizability
If you’re struggling to find a limitation to discuss in your own qualitative research study, then this one is for you: all qualitative research, of all persuasions and perspectives, cannot be generalized.
This is a core feature that sets qualitative data and quantitative data apart.
The point of qualitative data is to select case studies and similarly small corpora and dig deep through in-depth analysis and thick description of data.
Often, this will also mean that you have a non-randomized sample size.
While this is a positive – you’re going to get some really deep, contextualized, interesting insights – it also means that the findings may not be generalizable to a larger population that may not be representative of the small group of people in your study.
Suggested Solution and Response: Suggest future studies that take a quantitative approach to the question.
4. The Hawthorne Effect
The Hawthorne effect refers to the phenomenon where research participants change their ‘observed behavior’ when they’re aware that they are being observed.
This effect was first identified by Elton Mayo who conducted studies of the effects of various factors ton workers’ productivity. He noticed that no matter what he did – turning up the lights, turning down the lights, etc. – there was an increase in worker outputs compared to prior to the study taking place.
Mayo realized that the mere act of observing the workers made them work harder – his observation was what was changing behavior.
So, if you’re looking for a potential limitation to name for your observational research study , highlight the possible impact of the Hawthorne effect (and how you could reduce your footprint or visibility in order to decrease its likelihood).
Suggested Solution and Response: Highlight ways you have attempted to reduce your footprint while in the field, and guarantee anonymity to your research participants.
5. Replicability
Quantitative research has a great benefit in that the studies are replicable – a researcher can get a similar sample size, duplicate the variables, and re-test a study. But you can’t do that in qualitative research.
Qualitative research relies heavily on context – a specific case study or specific variables that make a certain instance worthy of analysis. As a result, it’s often difficult to re-enter the same setting with the same variables and repeat the study.
Furthermore, the individual researcher’s interpretation is more influential in qualitative research, meaning even if a new researcher enters an environment and makes observations, their observations may be different because subjectivity comes into play much more. This doesn’t make the research bad necessarily (great insights can be made in qualitative research), but it certainly does demonstrate a weakness of qualitative research.
6. Limited Scope
“Limited scope” is perhaps one of the most common limitations listed by researchers – and while this is often a catch-all way of saying, “well, I’m not studying that in this study”, it’s also a valid point.
No study can explore everything related to a topic. At some point, we have to make decisions about what’s included in the study and what is excluded from the study.
So, you could say that a limitation of your study is that it doesn’t look at an extra variable or concept that’s certainly worthy of study but will have to be explored in your next project because this project has a clearly and narrowly defined goal.
Suggested Solution and Response: Be clear about what’s in and out of the study when writing your research question.
7. Time Constraints
This is also a catch-all claim you can make about your research project: that you would have included more people in the study, looked at more variables, and so on. But you’ve got to submit this thing by the end of next semester! You’ve got time constraints.
And time constraints are a recognized reality in all research.
But this means you’ll need to explain how time has limited your decisions. As with “limited scope”, this may mean that you had to study a smaller group of subjects, limit the amount of time you spent in the field, and so forth.
Suggested Solution and Response: Suggest future studies that will build on your current work, possibly as a PhD project.
8. Resource Intensiveness
Qualitative research can be expensive due to the cost of transcription, the involvement of trained researchers, and potential travel for interviews or observations.
So, resource intensiveness is similar to the time constraints concept. If you don’t have the funds, you have to make decisions about which tools to use, which statistical software to employ, and how many research assistants you can dedicate to the study.
Suggested Solution and Response: Suggest future studies that will gain more funding on the back of this ‘ exploratory study ‘.
9. Coding Difficulties
Data analysis in qualitative research often involves coding, which can be subjective and complex, especially when dealing with ambiguous or contradicting data.
After naming this as a limitation in your research, it’s important to explain how you’ve attempted to address this. Some ways to ‘limit the limitation’ include:
- Triangulation: Have 2 other researchers code the data as well and cross-check your results with theirs to identify outliers that may need to be re-examined, debated with the other researchers, or removed altogether.
- Procedure: Use a clear coding procedure to demonstrate reliability in your coding process. I personally use the thematic network analysis method outlined in this academic article by Attride-Stirling (2001).
Suggested Solution and Response: Triangulate your coding findings with colleagues, and follow a thematic network analysis procedure.
10. Risk of Non-Responsiveness
There is always a risk in research that research participants will be unwilling or uncomfortable sharing their genuine thoughts and feelings in the study.
This is particularly true when you’re conducting research on sensitive topics, politicized topics, or topics where the participant is expressing vulnerability .
This is similar to the Hawthorne effect (aka participant bias), where participants change their behaviors in your presence; but it goes a step further, where participants actively hide their true thoughts and feelings from you.
Suggested Solution and Response: One way to manage this is to try to include a wider group of people with the expectation that there will be non-responsiveness from some participants.
11. Risk of Attrition
Attrition refers to the process of losing research participants throughout the study.
This occurs most commonly in longitudinal studies , where a researcher must return to conduct their analysis over spaced periods of time, often over a period of years.
Things happen to people over time – they move overseas, their life experiences change, they get sick, change their minds, and even die. The more time that passes, the greater the risk of attrition.
Suggested Solution and Response: One way to manage this is to try to include a wider group of people with the expectation that there will be attrition over time.
12. Difficulty in Maintaining Confidentiality and Anonymity
Given the detailed nature of qualitative data , ensuring participant anonymity can be challenging.
If you have a sensitive topic in a specific case study, even anonymizing research participants sometimes isn’t enough. People might be able to induce who you’re talking about.
Sometimes, this will mean you have to exclude some interesting data that you collected from your final report. Confidentiality and anonymity come before your findings in research ethics – and this is a necessary limiting factor.
Suggested Solution and Response: Highlight the efforts you have taken to anonymize data, and accept that confidentiality and accountability place extremely important constraints on academic research.
13. Difficulty in Finding Research Participants
A study that looks at a very specific phenomenon or even a specific set of cases within a phenomenon means that the pool of potential research participants can be very low.
Compile on top of this the fact that many people you approach may choose not to participate, and you could end up with a very small corpus of subjects to explore. This may limit your ability to make complete findings, even in a quantitative sense.
You may need to therefore limit your research question and objectives to something more realistic.
Suggested Solution and Response: Highlight that this is going to limit the study’s generalizability significantly.
14. Ethical Limitations
Ethical limitations refer to the things you cannot do based on ethical concerns identified either by yourself or your institution’s ethics review board.
This might include threats to the physical or psychological well-being of your research subjects, the potential of releasing data that could harm a person’s reputation, and so on.
Furthermore, even if your study follows all expected standards of ethics, you still, as an ethical researcher, need to allow a research participant to pull out at any point in time, after which you cannot use their data, which demonstrates an overlap between ethical constraints and participant attrition.
Suggested Solution and Response: Highlight that these ethical limitations are inevitable but important to sustain the integrity of the research.
For more on Qualitative Research, Explore my Qualitative Research Guide
Quantitative Research Limitations
Quantitative research focuses on quantifiable data and statistical, mathematical, or computational techniques. It’s often used to test hypotheses, assess relationships and causality, and generalize findings across larger populations.
Quantitative research is widely respected for its ability to provide reliable, measurable, and generalizable data (if done well!). Its structured methodology has strengths over qualitative research, such as the fact it allows for replication of the study, which underpins the validity of the research.
However, this approach is not without it limitations, explained below.
1. Over-Simplification
Quantitative research is powerful because it allows you to measure and analyze data in a systematic and standardized way. However, one of its limitations is that it can sometimes simplify complex phenomena or situations.
In other words, it might miss the subtleties or nuances of the research subject.
For example, if you’re studying why people choose a particular diet, a quantitative study might identify factors like age, income, or health status. But it might miss other aspects, such as cultural influences or personal beliefs, that can also significantly impact dietary choices.
When writing about this limitation, you can say that your quantitative approach, while providing precise measurements and comparisons, may not capture the full complexity of your subjects of study.
Suggested Solution and Response: Suggest a follow-up case study using the same research participants in order to gain additional context and depth.
2. Lack of Context
Another potential issue with quantitative research is that it often focuses on numbers and statistics at the expense of context or qualitative information.
Let’s say you’re studying the effect of classroom size on student performance. You might find that students in smaller classes generally perform better. However, this doesn’t take into account other variables, like teaching style , student motivation, or family support.
When describing this limitation, you might say, “Although our research provides important insights into the relationship between class size and student performance, it does not incorporate the impact of other potentially influential variables. Future research could benefit from a mixed-methods approach that combines quantitative analysis with qualitative insights.”
3. Applicability to Real-World Settings
Oftentimes, experimental research takes place in controlled environments to limit the influence of outside factors.
This control is great for isolation and understanding the specific phenomenon but can limit the applicability or “external validity” of the research to real-world settings.
For example, if you conduct a lab experiment to see how sleep deprivation impacts cognitive performance, the sterile, controlled lab environment might not reflect real-world conditions where people are dealing with multiple stressors.
Therefore, when explaining the limitations of your quantitative study in your methodology section, you could state:
“While our findings provide valuable information about [topic], the controlled conditions of the experiment may not accurately represent real-world scenarios where extraneous variables will exist. As such, the direct applicability of our results to broader contexts may be limited.”
Suggested Solution and Response: Suggest future studies that will engage in real-world observational research, such as ethnographic research.
4. Limited Flexibility
Once a quantitative study is underway, it can be challenging to make changes to it. This is because, unlike in grounded research, you’re putting in place your study in advance, and you can’t make changes part-way through.
Your study design, data collection methods, and analysis techniques need to be decided upon before you start collecting data.
For example, if you are conducting a survey on the impact of social media on teenage mental health, and halfway through, you realize that you should have included a question about their screen time, it’s generally too late to add it.
When discussing this limitation, you could write something like, “The structured nature of our quantitative approach allows for consistent data collection and analysis but also limits our flexibility to adapt and modify the research process in response to emerging insights and ideas.”
Suggested Solution and Response: Suggest future studies that will use mixed-methods or qualitative research methods to gain additional depth of insight.
5. Risk of Survey Error
Surveys are a common tool in quantitative research, but they carry risks of error.
There can be measurement errors (if a question is misunderstood), coverage errors (if some groups aren’t adequately represented), non-response errors (if certain people don’t respond), and sampling errors (if your sample isn’t representative of the population).
For instance, if you’re surveying college students about their study habits , but only daytime students respond because you conduct the survey during the day, your results will be skewed.
In discussing this limitation, you might say, “Despite our best efforts to develop a comprehensive survey, there remains a risk of survey error, including measurement, coverage, non-response, and sampling errors. These could potentially impact the reliability and generalizability of our findings.”
Suggested Solution and Response: Suggest future studies that will use other survey tools to compare and contrast results.
6. Limited Ability to Probe Answers
With quantitative research, you typically can’t ask follow-up questions or delve deeper into participants’ responses like you could in a qualitative interview.
For instance, imagine you are surveying 500 students about study habits in a questionnaire. A respondent might indicate that they study for two hours each night. You might want to follow up by asking them to elaborate on what those study sessions involve or how effective they feel their habits are.
However, quantitative research generally disallows this in the way a qualitative semi-structured interview could.
When discussing this limitation, you might write, “Given the structured nature of our survey, our ability to probe deeper into individual responses is limited. This means we may not fully understand the context or reasoning behind the responses, potentially limiting the depth of our findings.”
Suggested Solution and Response: Suggest future studies that engage in mixed-method or qualitative methodologies to address the issue from another angle.
7. Reliance on Instruments for Data Collection
In quantitative research, the collection of data heavily relies on instruments like questionnaires, surveys, or machines.
The limitation here is that the data you get is only as good as the instrument you’re using. If the instrument isn’t designed or calibrated well, your data can be flawed.
For instance, if you’re using a questionnaire to study customer satisfaction and the questions are vague, confusing, or biased, the responses may not accurately reflect the customers’ true feelings.
When discussing this limitation, you could say, “Our study depends on the use of questionnaires for data collection. Although we have put significant effort into designing and testing the instrument, it’s possible that inaccuracies or misunderstandings could potentially affect the validity of the data collected.”
Suggested Solution and Response: Suggest future studies that will use different instruments but examine the same variables to triangulate results.
8. Time and Resource Constraints (Specific to Quantitative Research)
Quantitative research can be time-consuming and resource-intensive, especially when dealing with large samples.
It often involves systematic sampling, rigorous design, and sometimes complex statistical analysis.
If resources and time are limited, it can restrict the scale of your research, the techniques you can employ, or the extent of your data analysis.
For example, you may want to conduct a nationwide survey on public opinion about a certain policy. However, due to limited resources, you might only be able to survey people in one city.
When writing about this limitation, you could say, “Given the scope of our research and the resources available, we are limited to conducting our survey within one city, which may not fully represent the nationwide public opinion. Hence, the generalizability of the results may be limited.”
Suggested Solution and Response: Suggest future studies that will have more funding or longer timeframes.
How to Discuss Your Research Limitations
1. in your research proposal and methodology section.
In the research proposal, which will become the methodology section of your dissertation, I would recommend taking the four following steps, in order:
- Be Explicit about your Scope – If you limit the scope of your study in your research question, aims, and objectives, then you can set yourself up well later in the methodology to say that certain questions are “outside the scope of the study.” For example, you may identify the fact that the study doesn’t address a certain variable, but you can follow up by stating that the research question is specifically focused on the variable that you are examining, so this limitation would need to be looked at in future studies.
- Acknowledge the Limitation – Acknowledging the limitations of your study demonstrates reflexivity and humility and can make your research more reliable and valid. It also pre-empts questions the people grading your paper may have, so instead of them down-grading you for your limitations; they will congratulate you on explaining the limitations and how you have addressed them!
- Explain your Decisions – You may have chosen your approach (despite its limitations) for a very specific reason. This might be because your approach remains, on balance, the best one to answer your research question. Or, it might be because of time and monetary constraints that are outside of your control.
- Highlight the Strengths of your Approach – Conclude your limitations section by strongly demonstrating that, despite limitations, you’ve worked hard to minimize the effects of the limitations and that you have chosen your specific approach and methodology because it’s also got some terrific strengths. Name the strengths.
Overall, you’ll want to acknowledge your own limitations but also explain that the limitations don’t detract from the value of your study as it stands.
2. In the Conclusion Section or Chapter
In the conclusion of your study, it is generally expected that you return to a discussion of the study’s limitations. Here, I recommend the following steps:
- Acknowledge issues faced – After completing your study, you will be increasingly aware of issues you may have faced that, if you re-did the study, you may have addressed earlier in order to avoid those issues. Acknowledge these issues as limitations, and frame them as recommendations for subsequent studies.
- Suggest further research – Scholarly research aims to fill gaps in the current literature and knowledge. Having established your expertise through your study, suggest lines of inquiry for future researchers. You could state that your study had certain limitations, and “future studies” can address those limitations.
- Suggest a mixed methods approach – Qualitative and quantitative research each have pros and cons. So, note those ‘cons’ of your approach, then say the next study should approach the topic using the opposite methodology or could approach it using a mixed-methods approach that could achieve the benefits of quantitative studies with the nuanced insights of associated qualitative insights as part of an in-study case-study.
Overall, be clear about both your limitations and how those limitations can inform future studies.
In sum, each type of research method has its own strengths and limitations. Qualitative research excels in exploring depth, context, and complexity, while quantitative research excels in examining breadth, generalizability, and quantifiable measures. Despite their individual limitations, each method contributes unique and valuable insights, and researchers often use them together to provide a more comprehensive understanding of the phenomenon being studied.
Attride-Stirling, J. (2001). Thematic networks: an analytic tool for qualitative research. Qualitative research , 1 (3), 385-405. ( Source )
Atkinson, P., Delamont, S., Cernat, A., Sakshaug, J., & Williams, R. A. (2021). SAGE research methods foundations . London: Sage Publications.
Clark, T., Foster, L., Bryman, A., & Sloan, L. (2021). Bryman’s social research methods . Oxford: Oxford University Press.
Köhler, T., Smith, A., & Bhakoo, V. (2022). Templates in qualitative research methods: Origins, limitations, and new directions. Organizational Research Methods , 25 (2), 183-210. ( Source )
Lenger, A. (2019). The rejection of qualitative research methods in economics. Journal of Economic Issues , 53 (4), 946-965. ( Source )
Taherdoost, H. (2022). What are different research approaches? Comprehensive review of qualitative, quantitative, and mixed method research, their applications, types, and limitations. Journal of Management Science & Engineering Research , 5 (1), 53-63. ( Source )
Walliman, N. (2021). Research methods: The basics . New York: Routledge.

- Chris Drew (PhD) https://helpfulprofessor.com/author/chris-drew-phd-2/ 10 Reasons you’re Perpetually Single
- Chris Drew (PhD) https://helpfulprofessor.com/author/chris-drew-phd-2/ 20 Montessori Toddler Bedrooms (Design Inspiration)
- Chris Drew (PhD) https://helpfulprofessor.com/author/chris-drew-phd-2/ 21 Montessori Homeschool Setups
- Chris Drew (PhD) https://helpfulprofessor.com/author/chris-drew-phd-2/ 101 Hidden Talents Examples
Leave a Comment Cancel Reply
Your email address will not be published. Required fields are marked *
Educational resources and simple solutions for your research journey
How to Present the Limitations of a Study in Research?
The limitations of the study convey to the reader how and under which conditions your study results will be evaluated. Scientific research involves investigating research topics, both known and unknown, which inherently includes an element of risk. The risk could arise due to human errors, barriers to data gathering, limited availability of resources, and researcher bias. Researchers are encouraged to discuss the limitations of their research to enhance the process of research, as well as to allow readers to gain an understanding of the study’s framework and value.
Limitations of the research are the constraints placed on the ability to generalize from the results and to further describe applications to practice. It is related to the utility value of the findings based on how you initially chose to design the study, the method used to establish internal and external validity, or the result of unanticipated challenges that emerged during the study. Knowing about these limitations and their impact can explain how the limitations of your study can affect the conclusions and thoughts drawn from your research. 1
Table of Contents
What are the limitations of a study
Researchers are probably cautious to acknowledge what the limitations of the research can be for fear of undermining the validity of the research findings. No research can be faultless or cover all possible conditions. These limitations of your research appear probably due to constraints on methodology or research design and influence the interpretation of your research’s ultimate findings. 2 These are limitations on the generalization and usability of findings that emerge from the design of the research and/or the method employed to ensure validity internally and externally. But such limitations of the study can impact the whole study or research paper. However, most researchers prefer not to discuss the different types of limitations in research for fear of decreasing the value of their paper amongst the reviewers or readers.

Importance of limitations of a study
Writing the limitations of the research papers is often assumed to require lots of effort. However, identifying the limitations of the study can help structure the research better. Therefore, do not underestimate the importance of research study limitations. 3
- Opportunity to make suggestions for further research. Suggestions for future research and avenues for further exploration can be developed based on the limitations of the study.
- Opportunity to demonstrate critical thinking. A key objective of the research process is to discover new knowledge while questioning existing assumptions and exploring what is new in the particular field. Describing the limitation of the research shows that you have critically thought about the research problem, reviewed relevant literature, and correctly assessed the methods chosen for studying the problem.
- Demonstrate Subjective learning process. Writing limitations of the research helps to critically evaluate the impact of the said limitations, assess the strength of the research, and consider alternative explanations or interpretations. Subjective evaluation contributes to a more complex and comprehensive knowledge of the issue under study.
Why should I include limitations of research in my paper
All studies have limitations to some extent. Including limitations of the study in your paper demonstrates the researchers’ comprehensive and holistic understanding of the research process and topic. The major advantages are the following:
- Understand the study conditions and challenges encountered . It establishes a complete and potentially logical depiction of the research. The boundaries of the study can be established, and realistic expectations for the findings can be set. They can also help to clarify what the study is not intended to address.
- Improve the quality and validity of the research findings. Mentioning limitations of the research creates opportunities for the original author and other researchers to undertake future studies to improve the research outcomes.
- Transparency and accountability. Including limitations of the research helps maintain mutual integrity and promote further progress in similar studies.
- Identify potential bias sources. Identifying the limitations of the study can help researchers identify potential sources of bias in their research design, data collection, or analysis. This can help to improve the validity and reliability of the findings.
Where do I need to add the limitations of the study in my paper
The limitations of your research can be stated at the beginning of the discussion section, which allows the reader to comprehend the limitations of the study prior to reading the rest of your findings or at the end of the discussion section as an acknowledgment of the need for further research.
Types of limitations in research
There are different types of limitations in research that researchers may encounter. These are listed below:
- Research Design Limitations : Restrictions on your research or available procedures may affect the research outputs. If the research goals and objectives are too broad, explain how they should be narrowed down to enhance the focus of your study. If there was a selection bias in your sample, explain how this may affect the generalizability of your findings. This can help readers understand the limitations of the study in terms of their impact on the overall validity of your research.
- Impact Limitations : Your study might be limited by a strong regional-, national-, or species-based impact or population- or experimental-specific impact. These inherent limitations on impact affect the extendibility and generalizability of the findings.
- Data or statistical limitations : Data or statistical limitations in research are extremely common in experimental (such as medicine, physics, and chemistry) or field-based (such as ecology and qualitative clinical research) studies. Sometimes, it is either extremely difficult to acquire sufficient data or gain access to the data. These limitations of the research might also be the result of your study’s design and might result in an incomplete conclusion to your research.
Limitations of study examples
All possible limitations of the study cannot be included in the discussion section of the research paper or dissertation. It will vary greatly depending on the type and nature of the study. These include types of research limitations that are related to methodology and the research process and that of the researcher as well that you need to describe and discuss how they possibly impacted your results.
Common methodological limitations of the study
Limitations of research due to methodological problems are addressed by identifying the potential problem and suggesting ways in which this should have been addressed. Some potential methodological limitations of the study are as follows. 1
- Sample size: The sample size 4 is dictated by the type of research problem investigated. If the sample size is too small, finding a significant relationship from the data will be difficult, as statistical tests require a large sample size to ensure a representative population distribution and generalize the study findings.
- Lack of available/reliable data: A lack of available/reliable data will limit the scope of your analysis and the size of your sample or present obstacles in finding a trend or meaningful relationship. So, when writing about the limitations of the study, give convincing reasons why you feel data is absent or untrustworthy and highlight the necessity for a future study focused on developing a new data-gathering strategy.
- Lack of prior research studies: Citing prior research studies is required to help understand the research problem being investigated. If there is little or no prior research, an exploratory rather than an explanatory research design will be required. Also, discovering the limitations of the study presents an opportunity to identify gaps in the literature and describe the need for additional study.
- Measure used to collect the data: Sometimes, the data gathered will be insufficient to conduct a thorough analysis of the results. A limitation of the study example, for instance, is identifying in retrospect that a specific question could have helped address a particular issue that emerged during data analysis. You can acknowledge the limitation of the research by stating the need to revise the specific method for gathering data in the future.
- Self-reported data: Self-reported data cannot be independently verified and can contain several potential bias sources, such as selective memory, attribution, and exaggeration. These biases become apparent if they are incongruent with data from other sources.
General limitations of researchers
Limitations related to the researcher can also influence the study outcomes. These should be addressed, and related remedies should be proposed.
- Limited access to data : If your study requires access to people, organizations, data, or documents whose access is denied or limited, the reasons need to be described. An additional explanation stating why this limitation of research did not prevent you from following through on your study is also needed.
- Time constraints : Researchers might also face challenges in meeting research deadlines due to a lack of timely participant availability or funds, among others. The impacts of time constraints must be acknowledged by mentioning the need for a future study addressing this research problem.
- Conflicts due to biased views and personal issues : Differences in culture or personal views can contribute to researcher bias, as they focus only on the results and data that support their main arguments. To avoid this, pay attention to the problem statement and data gathering.
Steps for structuring the limitations section
Limitations are an inherent part of any research study. Issues may vary, ranging from sampling and literature review to methodology and bias. However, there is a structure for identifying these elements, discussing them, and offering insight or alternatives on how the limitations of the study can be mitigated. This enhances the process of the research and helps readers gain a comprehensive understanding of a study’s conditions.
- Identify the research constraints : Identify those limitations having the greatest impact on the quality of the research findings and your ability to effectively answer your research questions and/or hypotheses. These include sample size, selection bias, measurement error, or other issues affecting the validity and reliability of your research.
- Describe their impact on your research : Reflect on the nature of the identified limitations and justify the choices made during the research to identify the impact of the study’s limitations on the research outcomes. Explanations can be offered if needed, but without being defensive or exaggerating them. Provide context for the limitations of your research to understand them in a broader context. Any specific limitations due to real-world considerations need to be pointed out critically rather than justifying them as done by some other author group or groups.
- Mention the opportunity for future investigations : Suggest ways to overcome the limitations of the present study through future research. This can help readers understand how the research fits into the broader context and offer a roadmap for future studies.
Frequently Asked Questions
- Should I mention all the limitations of my study in the research report?
Restrict limitations to what is pertinent to the research question under investigation. The specific limitations you include will depend on the nature of the study, the research question investigated, and the data collected.
- Can the limitations of a study affect its credibility?
Stating the limitations of the research is considered favorable by editors and peer reviewers. Connecting your study’s limitations with future possible research can help increase the focus of unanswered questions in this area. In addition, admitting limitations openly and validating that they do not affect the main findings of the study increases the credibility of your study. However, if you determine that your study is seriously flawed, explain ways to successfully overcome such flaws in a future study. For example, if your study fails to acquire critical data, consider reframing the research question as an exploratory study to lay the groundwork for more complete research in the future.
- How can I mitigate the limitations of my study?
Strategies to minimize limitations of the research should focus on convincing reviewers and readers that the limitations do not affect the conclusions of the study by showing that the methods are appropriate and that the logic is sound. Here are some steps to follow to achieve this:
- Use data that are valid.
- Use methods that are appropriate and sound logic to draw inferences.
- Use adequate statistical methods for drawing inferences from the data that studies with similar limitations have been published before.
Admit limitations openly and, at the same time, show how they do not affect the main conclusions of the study.
- Can the limitations of a study impact its publication chances?
Limitations in your research can arise owing to restrictions in methodology or research design. Although this could impact your chances of publishing your research paper, it is critical to explain your study’s limitations to your intended audience. For example, it can explain how your study constraints may impact the results and views generated from your investigation. It also shows that you have researched the flaws of your study and have a thorough understanding of the subject.
- How can limitations in research be used for future studies?
The limitations of a study give you an opportunity to offer suggestions for further research. Your study’s limitations, including problems experienced during the study and the additional study perspectives developed, are a great opportunity to take on a new challenge and help advance knowledge in a particular field.
References:
- Brutus, S., Aguinis, H., & Wassmer, U. (2013). Self-reported limitations and future directions in scholarly reports: Analysis and recommendations. Journal of Management , 39 (1), 48-75.
- Ioannidis, J. P. (2007). Limitations are not properly acknowledged in the scientific literature. Journal of Clinical Epidemiology , 60 (4), 324-329.
- Price, J. H., & Murnan, J. (2004). Research limitations and the necessity of reporting them. American Journal of Health Education , 35 (2), 66.
- Boddy, C. R. (2016). Sample size for qualitative research. Qualitative Market Research: An International Journal , 19 (4), 426-432.
R Discovery is a literature search and research reading platform that accelerates your research discovery journey by keeping you updated on the latest, most relevant scholarly content. With 250M+ research articles sourced from trusted aggregators like CrossRef, Unpaywall, PubMed, PubMed Central, Open Alex and top publishing houses like Springer Nature, JAMA, IOP, Taylor & Francis, NEJM, BMJ, Karger, SAGE, Emerald Publishing and more, R Discovery puts a world of research at your fingertips.
Try R Discovery Prime FREE for 1 week or upgrade at just US$72 a year to access premium features that let you listen to research on the go, read in your language, collaborate with peers, auto sync with reference managers, and much more. Choose a simpler, smarter way to find and read research – Download the app and start your free 7-day trial today !
Related Posts

What is Research Impact: Types and Tips for Academics

Research in Shorts: R Discovery’s New Feature Helps Academics Assess Relevant Papers in 2mins
Instant insights, infinite possibilities
How to present limitations in research
Last updated
30 January 2024
Reviewed by
Short on time? Get an AI generated summary of this article instead
Limitations don’t invalidate or diminish your results, but it’s best to acknowledge them. This will enable you to address any questions your study failed to answer because of them.
In this guide, learn how to recognize, present, and overcome limitations in research.
- What is a research limitation?
Research limitations are weaknesses in your research design or execution that may have impacted outcomes and conclusions. Uncovering limitations doesn’t necessarily indicate poor research design—it just means you encountered challenges you couldn’t have anticipated that limited your research efforts.
Does basic research have limitations?
Basic research aims to provide more information about your research topic . It requires the same standard research methodology and data collection efforts as any other research type, and it can also have limitations.
- Common research limitations
Researchers encounter common limitations when embarking on a study. Limitations can occur in relation to the methods you apply or the research process you design. They could also be connected to you as the researcher.
Methodology limitations
Not having access to data or reliable information can impact the methods used to facilitate your research. A lack of data or reliability may limit the parameters of your study area and the extent of your exploration.
Your sample size may also be affected because you won’t have any direction on how big or small it should be and who or what you should include. Having too few participants won’t adequately represent the population or groups of people needed to draw meaningful conclusions.
Research process limitations
The study’s design can impose constraints on the process. For example, as you’re conducting the research, issues may arise that don’t conform to the data collection methodology you developed. You may not realize until well into the process that you should have incorporated more specific questions or comprehensive experiments to generate the data you need to have confidence in your results.
Constraints on resources can also have an impact. Being limited on participants or participation incentives may limit your sample sizes. Insufficient tools, equipment, and materials to conduct a thorough study may also be a factor.
Common researcher limitations
Here are some of the common researcher limitations you may encounter:
Time: some research areas require multi-year longitudinal approaches, but you might not be able to dedicate that much time. Imagine you want to measure how much memory a person loses as they age. This may involve conducting multiple tests on a sample of participants over 20–30 years, which may be impossible.
Bias: researchers can consciously or unconsciously apply bias to their research. Biases can contribute to relying on research sources and methodologies that will only support your beliefs about the research you’re embarking on. You might also omit relevant issues or participants from the scope of your study because of your biases.
Limited access to data : you may need to pay to access specific databases or journals that would be helpful to your research process. You might also need to gain information from certain people or organizations but have limited access to them. These cases require readjusting your process and explaining why your findings are still reliable.
- Why is it important to identify limitations?
Identifying limitations adds credibility to research and provides a deeper understanding of how you arrived at your conclusions.
Constraints may have prevented you from collecting specific data or information you hoped would prove or disprove your hypothesis or provide a more comprehensive understanding of your research topic.
However, identifying the limitations contributing to your conclusions can inspire further research efforts that help gather more substantial information and data.
- Where to put limitations in a research paper
A research paper is broken up into different sections that appear in the following order:
Introduction
Methodology
The discussion portion of your paper explores your findings and puts them in the context of the overall research. Either place research limitations at the beginning of the discussion section before the analysis of your findings or at the end of the section to indicate that further research needs to be pursued.
What not to include in the limitations section
Evidence that doesn’t support your hypothesis is not a limitation, so you shouldn’t include it in the limitation section. Don’t just list limitations and their degree of severity without further explanation.
- How to present limitations
You’ll want to present the limitations of your study in a way that doesn’t diminish the validity of your research and leave the reader wondering if your results and conclusions have been compromised.
Include only the limitations that directly relate to and impact how you addressed your research questions. Following a specific format enables the reader to develop an understanding of the weaknesses within the context of your findings without doubting the quality and integrity of your research.
Identify the limitations specific to your study
You don’t have to identify every possible limitation that might have occurred during your research process. Only identify those that may have influenced the quality of your findings and your ability to answer your research question.
Explain study limitations in detail
This explanation should be the most significant portion of your limitation section.
Link each limitation with an interpretation and appraisal of their impact on the study. You’ll have to evaluate and explain whether the error, method, or validity issues influenced the study’s outcome and how.
Propose a direction for future studies and present alternatives
In this section, suggest how researchers can avoid the pitfalls you experienced during your research process.
If an issue with methodology was a limitation, propose alternate methods that may help with a smoother and more conclusive research project . Discuss the pros and cons of your alternate recommendation.
Describe steps taken to minimize each limitation
You probably took steps to try to address or mitigate limitations when you noticed them throughout the course of your research project. Describe these steps in the limitation section.
- Limitation example
“Approaches like stem cell transplantation and vaccination in AD [Alzheimer’s disease] work on a cellular or molecular level in the laboratory. However, translation into clinical settings will remain a challenge for the next decade.”
The authors are saying that even though these methods showed promise in helping people with memory loss when conducted in the lab (in other words, using animal studies), more studies are needed. These may be controlled clinical trials, for example.
However, the short life span of stem cells outside the lab and the vaccination’s severe inflammatory side effects are limitations. Researchers won’t be able to conduct clinical trials until these issues are overcome.
- How to overcome limitations in research
You’ve already started on the road to overcoming limitations in research by acknowledging that they exist. However, you need to ensure readers don’t mistake weaknesses for errors within your research design.
To do this, you’ll need to justify and explain your rationale for the methods, research design, and analysis tools you chose and how you noticed they may have presented limitations.
Your readers need to know that even when limitations presented themselves, you followed best practices and the ethical standards of your field. You didn’t violate any rules and regulations during your research process.
You’ll also want to reinforce the validity of your conclusions and results with multiple sources, methods, and perspectives. This prevents readers from assuming your findings were derived from a single or biased source.
- Learning and improving starts with limitations in research
Dealing with limitations with transparency and integrity helps identify areas for future improvements and developments. It’s a learning process, providing valuable insights into how you can improve methodologies, expand sample sizes, or explore alternate approaches to further support the validity of your findings.
Should you be using a customer insights hub?
Do you want to discover previous research faster?
Do you share your research findings with others?
Do you analyze research data?
Start for free today, add your research, and get to key insights faster
Editor’s picks
Last updated: 18 April 2023
Last updated: 27 February 2023
Last updated: 22 August 2024
Last updated: 5 February 2023
Last updated: 16 August 2024
Last updated: 9 March 2023
Last updated: 30 April 2024
Last updated: 12 December 2023
Last updated: 11 March 2024
Last updated: 4 July 2024
Last updated: 6 March 2024
Last updated: 5 March 2024
Last updated: 13 May 2024
Latest articles
Related topics, .css-je19u9{-webkit-align-items:flex-end;-webkit-box-align:flex-end;-ms-flex-align:flex-end;align-items:flex-end;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-flex-direction:row;-ms-flex-direction:row;flex-direction:row;-webkit-box-flex-wrap:wrap;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;-webkit-box-pack:center;-ms-flex-pack:center;-webkit-justify-content:center;justify-content:center;row-gap:0;text-align:center;max-width:671px;}@media (max-width: 1079px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}}@media (max-width: 799px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}} decide what to .css-1kiodld{max-height:56px;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;}@media (max-width: 1079px){.css-1kiodld{display:none;}} build next, decide what to build next, log in or sign up.
Get started for free
- The Scientist University
How to Present a Research Study’s Limitations
All studies have imperfections, but how to present them without diminishing the value of the work can be tricky..

Nathan Ni holds a PhD from Queens University. He is a science editor for The Scientist’s Creative Services Team who strives to better understand and communicate the relationships between health and disease.
View full profile.
Learn about our editorial policies.

Scientists work with many different limitations. First and foremost, they navigate informational limitations, work around knowledge gaps when designing studies, formulating hypotheses, and analyzing data. They also handle technical limitations, making the most of what their hands, equipment, and instruments can achieve. Finally, researchers must also manage logistical limitations. Scientists will often experience sample scarcity, financial issues, or simply be unable to access the technology or materials that they want.
All scientific studies have limitations, and no study is perfect. Researchers should not run from this reality, but engage it directly. It is better to directly address the specific limitations of the work in question, and doing so is actually a way to demonstrate an author’s proficiency and aptitude.
Do: Be Transparent
From a practical perspective, being transparent is the main key to directly addressing the specific limitations of a study. Was there an experiment that the researchers wanted to perform but could not, or a sample that existed that the scientists could not obtain? Was there a piece of knowledge that would explain a question raised by the data presented within the current study? If the answer is yes, the authors should mention this and elaborate upon it within the discussion section.
Asking and addressing these questions demonstrates that the authors have knowledge, understanding, and expertise of the subject area beyond what the study directly investigated. It further demonstrates a solid grasp of the existing literature—which means a solid grasp of what others are doing, what techniques they are using, and what limitations impede their own studies. This information helps the authors contextualize where their study fits within what others have discovered, thereby mitigating the perceived effect of a given limitation on the study’s legitimacy. In essence, this strategy turns limitations, often considered weaknesses, into strengths.
For example, in their 2021 Cell Reports study on macrophage polarization mechanisms, dermatologist Alexander Marneros and colleagues wrote the following. 1
A limitation of studying macrophage polarization in vitro is that this approach only partially captures the tissue microenvironment context in which many different factors affect macrophage polarization. However, it is likely that the identified signaling mechanisms that promote polarization in vitro are also critical for polarization mechanisms that occur in vivo. This is supported by our observation that trametinib and panobinostat inhibited M2-type macrophage polarization not only in vitro but also in skin wounds and laser-induced CNV lesions.
This is a very effective structure. In the first sentence ( yellow ), the authors outlined the limitation. In the next sentence ( green ), they offered a rationalization that mitigates the effect of the limitation. Finally, they provided the evidence ( blue ) for this rationalization, using not just information from the literature, but also data that they obtained in their study specifically for this purpose.

Don't: Be Defensive
It can feel natural to avoid talking about a study’s limitations. Scientists may believe that mentioning the drawbacks still present in their study will jeopardize their chances of publication. As such, researchers will sometimes skirt around the issue. They will present “boilerplate faults”—generalized concerns about sample size/diversity and time limitations that all researchers face—rather than honestly discussing their own study. Alternatively, they will describe their limitations in a defensive manner, positioning their problems as something that “could not be helped”—as something beyond what science can currently achieve.
However, their audience can see through this, because they are largely peers who understand and have experienced how modern research works. They can tell the difference between global challenges faced by every scientific study and limitations that are specific to a single study. Avoiding these specific limitations can therefore betray a lack of confidence that the study is good enough to withstand problems stemming from legitimate limitations. As such, researchers should actively engage with the greater scientific implications of the limitations that they face. Indeed, doing this is actually a way to demonstrate an author’s proficiency and aptitude.
In an example, neurogeneticist Nancy Bonini and colleagues, in their publication in Nature , discussed a question raised by their data that they have elected not to directly investigate in this study, writing “ Among the intriguing questions raised by these data is how senescent glia promote LDs in other glia. ” To show both the legitimacy of the question and how seriously they have considered it, the authors provided a comprehensive summary of the literature in the following seven sentences, offering two hypotheses backed by a combined eight different sources. 2 Rather than shying away from a limitation, they attacked it as something to be curious about and to discuss. This is not just a very effective way of demonstrating their expertise, but it frames the limitation as something that, when overcome, will build upon the present study rather than something that negatively affects the legitimacy of their current findings.
Striking the Right Balance
Scientists have to navigate the fine line between acknowledging the limitations of their study while also not diminishing the effect and value of their own work. To be aware of legitimate limitations and properly assess and dissect them shows a profound understanding of a field, where the study fits within that field, and what the rest of the scientific community are doing and what challenges they face.
All studies are parts of a greater whole. Pretending otherwise is a disservice to the scientific community.
Looking for more information on scientific writing? Check out The Scientist’ s TS SciComm section. Looking for some help putting together a manuscript, a figure, a poster, or anything else? The Scientist ’s Scientific Services may have the professional help that you need.
- He L, et al. Global characterization of macrophage polarization mechanisms and identification of M2-type polarization inhibitors . Cell Rep . 2021;37(5):109955.
- Byrns CN, et al. Senescent glia link mitochondrial dysfunction and lipid accumulation . Nature . 2024.

Writing Limitations of Research Study — 4 Reasons Why It Is Important!
It is not unusual for researchers to come across the term limitations of research during their academic paper writing. More often this is interpreted as something terrible. However, when it comes to research study, limitations can help structure the research study better. Therefore, do not underestimate significance of limitations of research study.
Allow us to take you through the context of how to evaluate the limits of your research and conclude an impactful relevance to your results.
Table of Contents
What Are the Limitations of a Research Study?
Every research has its limit and these limitations arise due to restrictions in methodology or research design. This could impact your entire research or the research paper you wish to publish. Unfortunately, most researchers choose not to discuss their limitations of research fearing it will affect the value of their article in the eyes of readers.
However, it is very important to discuss your study limitations and show it to your target audience (other researchers, journal editors, peer reviewers etc.). It is very important that you provide an explanation of how your research limitations may affect the conclusions and opinions drawn from your research. Moreover, when as an author you state the limitations of research, it shows that you have investigated all the weaknesses of your study and have a deep understanding of the subject. Being honest could impress your readers and mark your study as a sincere effort in research.
Why and Where Should You Include the Research Limitations?
The main goal of your research is to address your research objectives. Conduct experiments, get results and explain those results, and finally justify your research question . It is best to mention the limitations of research in the discussion paragraph of your research article.
At the very beginning of this paragraph, immediately after highlighting the strengths of the research methodology, you should write down your limitations. You can discuss specific points from your research limitations as suggestions for further research in the conclusion of your thesis.
1. Common Limitations of the Researchers
Limitations that are related to the researcher must be mentioned. This will help you gain transparency with your readers. Furthermore, you could provide suggestions on decreasing these limitations in you and your future studies.
2. Limited Access to Information
Your work may involve some institutions and individuals in research, and sometimes you may have problems accessing these institutions. Therefore, you need to redesign and rewrite your work. You must explain your readers the reason for limited access.
3. Limited Time
All researchers are bound by their deadlines when it comes to completing their studies. Sometimes, time constraints can affect your research negatively. However, the best practice is to acknowledge it and mention a requirement for future study to solve the research problem in a better way.
4. Conflict over Biased Views and Personal Issues
Biased views can affect the research. In fact, researchers end up choosing only those results and data that support their main argument, keeping aside the other loose ends of the research.
Types of Limitations of Research
Before beginning your research study, know that there are certain limitations to what you are testing or possible research results. There are different types that researchers may encounter, and they all have unique characteristics, such as:
1. Research Design Limitations
Certain restrictions on your research or available procedures may affect your final results or research outputs. You may have formulated research goals and objectives too broadly. However, this can help you understand how you can narrow down the formulation of research goals and objectives, thereby increasing the focus of your study.
2. Impact Limitations
Even if your research has excellent statistics and a strong design, it can suffer from the influence of the following factors:
- Presence of increasing findings as researched
- Being population specific
- A strong regional focus.
3. Data or statistical limitations
In some cases, it is impossible to collect sufficient data for research or very difficult to get access to the data. This could lead to incomplete conclusion to your study. Moreover, this insufficiency in data could be the outcome of your study design. The unclear, shabby research outline could produce more problems in interpreting your findings.
How to Correctly Structure Your Research Limitations?
There are strict guidelines for narrowing down research questions, wherein you could justify and explain potential weaknesses of your academic paper. You could go through these basic steps to get a well-structured clarity of research limitations:
- Declare that you wish to identify your limitations of research and explain their importance,
- Provide the necessary depth, explain their nature, and justify your study choices.
- Write how you are suggesting that it is possible to overcome them in the future.
In this section, your readers will see that you are aware of the potential weaknesses in your business, understand them and offer effective solutions, and it will positively strengthen your article as you clarify all limitations of research to your target audience.
Know that you cannot be perfect and there is no individual without flaws. You could use the limitations of research as a great opportunity to take on a new challenge and improve the future of research. In a typical academic paper, research limitations may relate to:
1. Formulating your goals and objectives
If you formulate goals and objectives too broadly, your work will have some shortcomings. In this case, specify effective methods or ways to narrow down the formula of goals and aim to increase your level of study focus.
2. Application of your data collection methods in research
If you do not have experience in primary data collection, there is a risk that there will be flaws in the implementation of your methods. It is necessary to accept this, and learn and educate yourself to understand data collection methods.
3. Sample sizes
This depends on the nature of problem you choose. Sample size is of a greater importance in quantitative studies as opposed to qualitative ones. If your sample size is too small, statistical tests cannot identify significant relationships or connections within a given data set.
You could point out that other researchers should base the same study on a larger sample size to get more accurate results.
4. The absence of previous studies in the field you have chosen
Writing a literature review is an important step in any scientific study because it helps researchers determine the scope of current work in the chosen field. It is a major foundation for any researcher who must use them to achieve a set of specific goals or objectives.
However, if you are focused on the most current and evolving research problem or a very narrow research problem, there may be very little prior research on your topic. For example, if you chose to explore the role of Bitcoin as the currency of the future, you may not find tons of scientific papers addressing the research problem as Bitcoins are only a new phenomenon.
It is important that you learn to identify research limitations examples at each step. Whatever field you choose, feel free to add the shortcoming of your work. This is mainly because you do not have many years of experience writing scientific papers or completing complex work. Therefore, the depth and scope of your discussions may be compromised at different levels compared to academics with a lot of expertise. Include specific points from limitations of research. Use them as suggestions for the future.
Have you ever faced a challenge of writing the limitations of research study in your paper? How did you overcome it? What ways did you follow? Were they beneficial? Let us know in the comments below!
Frequently Asked Questions
Setting limitations in our study helps to clarify the outcomes drawn from our research and enhance understanding of the subject. Moreover, it shows that the author has investigated all the weaknesses in the study.
Scope is the range and limitations of a research project which are set to define the boundaries of a project. Limitations are the impacts on the overall study due to the constraints on the research design.
Limitation in research is an impact of a constraint on the research design in the overall study. They are the flaws or weaknesses in the study, which may influence the outcome of the research.
1. Limitations in research can be written as follows: Formulate your goals and objectives 2. Analyze the chosen data collection method and the sample sizes 3. Identify your limitations of research and explain their importance 4. Provide the necessary depth, explain their nature, and justify your study choices 5. Write how you are suggesting that it is possible to overcome them in the future
Excellent article ,,,it has helped me big
This is very helpful information. It has given me an insight on how to go about my study limitations.
Good comments and helpful
the topic is well covered
Rate this article Cancel Reply
Your email address will not be published.

Enago Academy's Most Popular Articles

- Publishing Research
- Trending Now
- Understanding Ethics
Understanding the Impact of Retractions on Research Integrity – A global study
As we reach the midway point of 2024, ‘Research Integrity’ remains one of the hot…

- Diversity and Inclusion
The Silent Struggle: Confronting gender bias in science funding
In the 1990s, Dr. Katalin Kariko’s pioneering mRNA research seemed destined for obscurity, doomed by…

- Promoting Research
Plain Language Summary — Communicating your research to bridge the academic-lay gap
Science can be complex, but does that mean it should not be accessible to the…

Addressing Barriers in Academia: Navigating unconscious biases in the Ph.D. journey
In the journey of academia, a Ph.D. marks a transitional phase, like that of a…

- Manuscripts & Grants
- Reporting Research
Unraveling Research Population and Sample: Understanding their role in statistical inference
Research population and sample serve as the cornerstones of any scientific inquiry. They hold the…
Research Problem Statement — Find out how to write an impactful one!
How to Develop a Good Research Question? — Types & Examples
5 Effective Ways to Avoid Ghostwriting for Busy Researchers

Sign-up to read more
Subscribe for free to get unrestricted access to all our resources on research writing and academic publishing including:
- 2000+ blog articles
- 50+ Webinars
- 10+ Expert podcasts
- 50+ Infographics
- 10+ Checklists
- Research Guides
We hate spam too. We promise to protect your privacy and never spam you.
- Industry News
- AI in Academia
- Career Corner
- Infographics
- Expert Video Library
- Other Resources
- Enago Learn
- Upcoming & On-Demand Webinars
- Peer Review Week 2024
- Open Access Week 2023
- Conference Videos
- Enago Report
- Journal Finder
- Enago Plagiarism & AI Grammar Check
- Editing Services
- Publication Support Services
- Research Impact
- Translation Services
- Publication solutions
- AI-Based Solutions
- Thought Leadership
- Call for Articles
- Call for Speakers
- Author Training
- Edit Profile
I am looking for Editing/ Proofreading services for my manuscript Tentative date of next journal submission:

Which among these features would you prefer the most in a peer review assistant?
- Affiliate Program

- UNITED STATES
- 台灣 (TAIWAN)
- TÜRKIYE (TURKEY)
- Academic Editing Services
- - Research Paper
- - Journal Manuscript
- - Dissertation
- - College & University Assignments
- Admissions Editing Services
- - Application Essay
- - Personal Statement
- - Recommendation Letter
- - Cover Letter
- - CV/Resume
- Business Editing Services
- - Business Documents
- - Report & Brochure
- - Website & Blog
- Writer Editing Services
- - Script & Screenplay
- Our Editors
- Client Reviews
- Editing & Proofreading Prices
- Wordvice Points
- Partner Discount
- Plagiarism Checker
APA Citation Generator
MLA Citation Generator
Chicago Citation Generator
Vancouver Citation Generator
- - APA Style
- - MLA Style
- - Chicago Style
- - Vancouver Style
- Writing & Editing Guide
- Academic Resources
- Admissions Resources
Limitations of the Study – How to Write & Examples
What are the limitations of a study?
The limitations of a study are the elements of methodology or study design that impact the interpretation of your research results. The limitations essentially detail any flaws or shortcomings in your study. Study limitations can exist due to constraints on research design, methodology, materials, etc., and these factors may impact the findings of your study. However, researchers are often reluctant to discuss the limitations of their study in their papers, feeling that bringing up limitations may undermine its research value in the eyes of readers and reviewers.
In spite of the impact it might have (and perhaps because of it) you should clearly acknowledge any limitations in your research paper in order to show readers—whether journal editors, other researchers, or the general public—that you are aware of these limitations and to explain how they affect the conclusions that can be drawn from the research.
In this article, we provide some guidelines for writing about research limitations, show examples of some frequently seen study limitations, and recommend techniques for presenting this information. And after you have finished drafting and have received manuscript editing for your work, you still might want to follow this up with academic editing before submitting your work to your target journal.
Why do I need to include limitations of research in my paper?
Although limitations address the potential weaknesses of a study, writing about them toward the end of your paper actually strengthens your study by identifying any problems before other researchers or reviewers find them.
Furthermore, pointing out study limitations shows that you’ve considered the impact of research weakness thoroughly and have an in-depth understanding of your research topic. Since all studies face limitations, being honest and detailing these limitations will impress researchers and reviewers more than ignoring them.

Where should I put the limitations of the study in my paper?
Some limitations might be evident to researchers before the start of the study, while others might become clear while you are conducting the research. Whether these limitations are anticipated or not, and whether they are due to research design or to methodology, they should be clearly identified and discussed in the discussion section —the final section of your paper. Most journals now require you to include a discussion of potential limitations of your work, and many journals now ask you to place this “limitations section” at the very end of your article.
Some journals ask you to also discuss the strengths of your work in this section, and some allow you to freely choose where to include that information in your discussion section—make sure to always check the author instructions of your target journal before you finalize a manuscript and submit it for peer review .
Limitations of the Study Examples
There are several reasons why limitations of research might exist. The two main categories of limitations are those that result from the methodology and those that result from issues with the researcher(s).
Common Methodological Limitations of Studies
Limitations of research due to methodological problems can be addressed by clearly and directly identifying the potential problem and suggesting ways in which this could have been addressed—and SHOULD be addressed in future studies. The following are some major potential methodological issues that can impact the conclusions researchers can draw from the research.
Issues with research samples and selection
Sampling errors occur when a probability sampling method is used to select a sample, but that sample does not reflect the general population or appropriate population concerned. This results in limitations of your study known as “sample bias” or “selection bias.”
For example, if you conducted a survey to obtain your research results, your samples (participants) were asked to respond to the survey questions. However, you might have had limited ability to gain access to the appropriate type or geographic scope of participants. In this case, the people who responded to your survey questions may not truly be a random sample.
Insufficient sample size for statistical measurements
When conducting a study, it is important to have a sufficient sample size in order to draw valid conclusions. The larger the sample, the more precise your results will be. If your sample size is too small, it will be difficult to identify significant relationships in the data.
Normally, statistical tests require a larger sample size to ensure that the sample is considered representative of a population and that the statistical result can be generalized to a larger population. It is a good idea to understand how to choose an appropriate sample size before you conduct your research by using scientific calculation tools—in fact, many journals now require such estimation to be included in every manuscript that is sent out for review.
Lack of previous research studies on the topic
Citing and referencing prior research studies constitutes the basis of the literature review for your thesis or study, and these prior studies provide the theoretical foundations for the research question you are investigating. However, depending on the scope of your research topic, prior research studies that are relevant to your thesis might be limited.
When there is very little or no prior research on a specific topic, you may need to develop an entirely new research typology. In this case, discovering a limitation can be considered an important opportunity to identify literature gaps and to present the need for further development in the area of study.
Methods/instruments/techniques used to collect the data
After you complete your analysis of the research findings (in the discussion section), you might realize that the manner in which you have collected the data or the ways in which you have measured variables has limited your ability to conduct a thorough analysis of the results.
For example, you might realize that you should have addressed your survey questions from another viable perspective, or that you were not able to include an important question in the survey. In these cases, you should acknowledge the deficiency or deficiencies by stating a need for future researchers to revise their specific methods for collecting data that includes these missing elements.
Common Limitations of the Researcher(s)
Study limitations that arise from situations relating to the researcher or researchers (whether the direct fault of the individuals or not) should also be addressed and dealt with, and remedies to decrease these limitations—both hypothetically in your study, and practically in future studies—should be proposed.
Limited access to data
If your research involved surveying certain people or organizations, you might have faced the problem of having limited access to these respondents. Due to this limited access, you might need to redesign or restructure your research in a different way. In this case, explain the reasons for limited access and be sure that your finding is still reliable and valid despite this limitation.
Time constraints
Just as students have deadlines to turn in their class papers, academic researchers might also have to meet deadlines for submitting a manuscript to a journal or face other time constraints related to their research (e.g., participants are only available during a certain period; funding runs out; collaborators move to a new institution). The time available to study a research problem and to measure change over time might be constrained by such practical issues. If time constraints negatively impacted your study in any way, acknowledge this impact by mentioning a need for a future study (e.g., a longitudinal study) to answer this research problem.
Conflicts arising from cultural bias and other personal issues
Researchers might hold biased views due to their cultural backgrounds or perspectives of certain phenomena, and this can affect a study’s legitimacy. Also, it is possible that researchers will have biases toward data and results that only support their hypotheses or arguments. In order to avoid these problems, the author(s) of a study should examine whether the way the research problem was stated and the data-gathering process was carried out appropriately.
Steps for Organizing Your Study Limitations Section
When you discuss the limitations of your study, don’t simply list and describe your limitations—explain how these limitations have influenced your research findings. There might be multiple limitations in your study, but you only need to point out and explain those that directly relate to and impact how you address your research questions.
We suggest that you divide your limitations section into three steps: (1) identify the study limitations; (2) explain how they impact your study in detail; and (3) propose a direction for future studies and present alternatives. By following this sequence when discussing your study’s limitations, you will be able to clearly demonstrate your study’s weakness without undermining the quality and integrity of your research.
Step 1. Identify the limitation(s) of the study
- This part should comprise around 10%-20% of your discussion of study limitations.
The first step is to identify the particular limitation(s) that affected your study. There are many possible limitations of research that can affect your study, but you don’t need to write a long review of all possible study limitations. A 200-500 word critique is an appropriate length for a research limitations section. In the beginning of this section, identify what limitations your study has faced and how important these limitations are.
You only need to identify limitations that had the greatest potential impact on: (1) the quality of your findings, and (2) your ability to answer your research question.
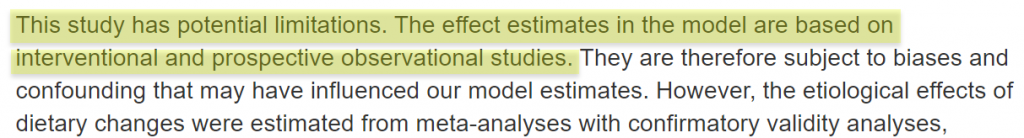
Step 2. Explain these study limitations in detail
- This part should comprise around 60-70% of your discussion of limitations.
After identifying your research limitations, it’s time to explain the nature of the limitations and how they potentially impacted your study. For example, when you conduct quantitative research, a lack of probability sampling is an important issue that you should mention. On the other hand, when you conduct qualitative research, the inability to generalize the research findings could be an issue that deserves mention.
Explain the role these limitations played on the results and implications of the research and justify the choice you made in using this “limiting” methodology or other action in your research. Also, make sure that these limitations didn’t undermine the quality of your dissertation .
Step 3. Propose a direction for future studies and present alternatives (optional)
- This part should comprise around 10-20% of your discussion of limitations.
After acknowledging the limitations of the research, you need to discuss some possible ways to overcome these limitations in future studies. One way to do this is to present alternative methodologies and ways to avoid issues with, or “fill in the gaps of” the limitations of this study you have presented. Discuss both the pros and cons of these alternatives and clearly explain why researchers should choose these approaches.
Make sure you are current on approaches used by prior studies and the impacts they have had on their findings. Cite review articles or scientific bodies that have recommended these approaches and why. This might be evidence in support of the approach you chose, or it might be the reason you consider your choices to be included as limitations. This process can act as a justification for your approach and a defense of your decision to take it while acknowledging the feasibility of other approaches.
P hrases and Tips for Introducing Your Study Limitations in the Discussion Section
The following phrases are frequently used to introduce the limitations of the study:
- “There may be some possible limitations in this study.”
- “The findings of this study have to be seen in light of some limitations.”
- “The first is the…The second limitation concerns the…”
- “The empirical results reported herein should be considered in the light of some limitations.”
- “This research, however, is subject to several limitations.”
- “The primary limitation to the generalization of these results is…”
- “Nonetheless, these results must be interpreted with caution and a number of limitations should be borne in mind.”
- “As with the majority of studies, the design of the current study is subject to limitations.”
- “There are two major limitations in this study that could be addressed in future research. First, the study focused on …. Second ….”
For more articles on research writing and the journal submissions and publication process, visit Wordvice’s Academic Resources page.
And be sure to receive professional English editing and proofreading services , including paper editing services , for your journal manuscript before submitting it to journal editors.
Wordvice Resources
Proofreading & Editing Guide
Writing the Results Section for a Research Paper
How to Write a Literature Review
Research Writing Tips: How to Draft a Powerful Discussion Section
How to Captivate Journal Readers with a Strong Introduction
Tips That Will Make Your Abstract a Success!
APA In-Text Citation Guide for Research Writing
Additional Resources
- Diving Deeper into Limitations and Delimitations (PhD student)
- Organizing Your Social Sciences Research Paper: Limitations of the Study (USC Library)
- Research Limitations (Research Methodology)
- How to Present Limitations and Alternatives (UMASS)
Article References
Pearson-Stuttard, J., Kypridemos, C., Collins, B., Mozaffarian, D., Huang, Y., Bandosz, P.,…Micha, R. (2018). Estimating the health and economic effects of the proposed US Food and Drug Administration voluntary sodium reformulation: Microsimulation cost-effectiveness analysis. PLOS. https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1002551
Xu, W.L, Pedersen, N.L., Keller, L., Kalpouzos, G., Wang, H.X., Graff, C,. Fratiglioni, L. (2015). HHEX_23 AA Genotype Exacerbates Effect of Diabetes on Dementia and Alzheimer Disease: A Population-Based Longitudinal Study. PLOS. Retrieved from https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1001853

CPS Online Graduate Studies Research Paper (UNH Manchester Library): Limitations of the Study
- Overview of the Research Process for Capstone Projects
- Types of Research Design
- Selecting a Research Problem
- The Title of Your Research Paper
- Before You Begin Writing
- 7 Parts of the Research Paper
- Background Information
- Quanitative and Qualitative Methods
- Qualitative Methods
- Quanitative Methods
- Resources to Help You With the Literature Review
- Non-Textual Elements
Limitations of the Study
- Format of Capstone Research Projects at GSC
- Editing and Proofreading Your Paper
- Acknowledgements
- UNH Scholar's Repository
The limitations of the study are those characteristics of design or methodology that impacted or influenced the interpretation of the findings from your research. They are the constraints on generalizability, applications to practice, and/or utility of findings that are the result of the ways in which you initially chose to design the study and/or the method used to establish internal and external validity.
Price, James H. and Judy Murnan. “Research Limitations and the Necessity of Reporting Them.” American Journal of Health Education 35 (2004): 66-67.
Always acknowledge a study's limitations. It is far better that you identify and acknowledge your study’s limitations than to have them pointed out by your professor and be graded down because you appear to have ignored them.
Keep in mind that acknowledgement of a study's limitations is an opportunity to make suggestions for further research. If you do connect your study's limitations to suggestions for further research, be sure to explain the ways in which these unanswered questions may become more focused because of your study.
Acknowledgement of a study's limitations also provides you with an opportunity to demonstrate that you have thought critically about the research problem, understood the relevant literature published about it, and correctly assessed the methods chosen for studying the problem. A key objective of the research process is not only discovering new knowledge but to also confront assumptions and explore what we don't know.
Claiming limitations is a subjective process because you must evaluate the impact of those limitations . Don't just list key weaknesses and the magnitude of a study's limitations. To do so diminishes the validity of your research because it leaves the reader wondering whether, or in what ways, limitation(s) in your study may have impacted the results and conclusions. Limitations require a critical, overall appraisal and interpretation of their impact. You should answer the question: do these problems with errors, methods, validity, etc. eventually matter and, if so, to what extent?
Price, James H. and Judy Murnan. “Research Limitations and the Necessity of Reporting Them.” American Journal of Health Education 35 (2004): 66-67; Structure: How to Structure the Research Limitations Section of Your Dissertation . Dissertations and Theses: An Online Textbook. Laerd.com.
Descriptions of Possible Limitations
All studies have limitations . However, it is important that you restrict your discussion to limitations related to the research problem under investigation. For example, if a meta-analysis of existing literature is not a stated purpose of your research, it should not be discussed as a limitation. Do not apologize for not addressing issues that you did not promise to investigate in the introduction of your paper.
Here are examples of limitations related to methodology and the research process you may need to describe and to discuss how they possibly impacted your results. Descriptions of limitations should be stated in the past tense because they were discovered after you completed your research.
Possible Methodological Limitations
- Sample size -- the number of the units of analysis you use in your study is dictated by the type of research problem you are investigating. Note that, if your sample size is too small, it will be difficult to find significant relationships from the data, as statistical tests normally require a larger sample size to ensure a representative distribution of the population and to be considered representative of groups of people to whom results will be generalized or transferred. Note that sample size is less relevant in qualitative research.
- Lack of available and/or reliable data -- a lack of data or of reliable data will likely require you to limit the scope of your analysis, the size of your sample, or it can be a significant obstacle in finding a trend and a meaningful relationship. You need to not only describe these limitations but to offer reasons why you believe data is missing or is unreliable. However, don’t just throw up your hands in frustration; use this as an opportunity to describe the need for future research.
- Lack of prior research studies on the topic -- citing prior research studies forms the basis of your literature review and helps lay a foundation for understanding the research problem you are investigating. Depending on the currency or scope of your research topic, there may be little, if any, prior research on your topic. Before assuming this to be true, though, consult with a librarian. In cases when a librarian has confirmed that there is no prior research, you may be required to develop an entirely new research typology [for example, using an exploratory rather than an explanatory research design]. Note again that discovering a limitation can serve as an important opportunity to identify new gaps in the literature and to describe the need for further research.
- Measure used to collect the data -- sometimes it is the case that, after completing your interpretation of the findings, you discover that the way in which you gathered data inhibited your ability to conduct a thorough analysis of the results. For example, you regret not including a specific question in a survey that, in retrospect, could have helped address a particular issue that emerged later in the study. Acknowledge the deficiency by stating a need for future researchers to revise the specific method for gathering data.
- Self-reported data -- whether you are relying on pre-existing data or you are conducting a qualitative research study and gathering the data yourself, self-reported data is limited by the fact that it rarely can be independently verified. In other words, you have to take what people say, whether in interviews, focus groups, or on questionnaires, at face value. However, self-reported data can contain several potential sources of bias that you should be alert to and note as limitations. These biases become apparent if they are incongruent with data from other sources. These are: (1) selective memory [remembering or not remembering experiences or events that occurred at some point in the past]; (2) telescoping [recalling events that occurred at one time as if they occurred at another time]; (3) attribution [the act of attributing positive events and outcomes to one's own agency but attributing negative events and outcomes to external forces]; and, (4) exaggeration [the act of representing outcomes or embellishing events as more significant than is actually suggested from other data].
Possible Limitations of the Researcher
- Access -- if your study depends on having access to people, organizations, or documents and, for whatever reason, access is denied or limited in some way, the reasons for this need to be described.
- Longitudinal effects -- unlike your professor, who can literally devote years [even a lifetime] to studying a single topic, the time available to investigate a research problem and to measure change or stability over time is pretty much constrained by the due date of your assignment. Be sure to choose a research problem that does not require an excessive amount of time to complete the literature review, apply the methodology, and gather and interpret the results. If you're unsure whether you can complete your research within the confines of the assignment's due date, talk to your professor.
- Cultural and other type of bias -- we all have biases, whether we are conscience of them or not. Bias is when a person, place, or thing is viewed or shown in a consistently inaccurate way. Bias is usually negative, though one can have a positive bias as well, especially if that bias reflects your reliance on research that only support for your hypothesis. When proof-reading your paper, be especially critical in reviewing how you have stated a problem, selected the data to be studied, what may have been omitted, the manner in which you have ordered events, people, or places, how you have chosen to represent a person, place, or thing, to name a phenomenon, or to use possible words with a positive or negative connotation.
NOTE: If you detect bias in prior research, it must be acknowledged and you should explain what measures were taken to avoid perpetuating that bias.
- Fluency in a language -- if your research focuses on measuring the perceived value of after-school tutoring among Mexican-American ESL [English as a Second Language] students, for example, and you are not fluent in Spanish, you are limited in being able to read and interpret Spanish language research studies on the topic. This deficiency should be acknowledged.
Aguinis, Hermam and Jeffrey R. Edwards. “Methodological Wishes for the Next Decade and How to Make Wishes Come True.” Journal of Management Studies 51 (January 2014): 143-174; Brutus, Stéphane et al. "Self-Reported Limitations and Future Directions in Scholarly Reports: Analysis and Recommendations." Journal of Management 39 (January 2013): 48-75; Senunyeme, Emmanuel K. Business Research Methods . Powerpoint Presentation. Regent University of Science and Technology; ter Riet, Gerben et al. “All That Glitters Isn't Gold: A Survey on Acknowledgment of Limitations in Biomedical Studies.” PLOS One 8 (November 2013): 1-6.
Structure and Writing Style
Information about the limitations of your study are generally placed either at the beginning of the discussion section of your paper so the reader knows and understands the limitations before reading the rest of your analysis of the findings, or, the limitations are outlined at the conclusion of the discussion section as an acknowledgement of the need for further study. Statements about a study's limitations should not be buried in the body [middle] of the discussion section unless a limitation is specific to something covered in that part of the paper. If this is the case, though, the limitation should be reiterated at the conclusion of the section. If you determine that your study is seriously flawed due to important limitations, such as, an inability to acquire critical data, consider reframing it as an exploratory study intended to lay the groundwork for a more complete research study in the future. Be sure, though, to specifically explain the ways that these flaws can be successfully overcome in a new study. But, do not use this as an excuse for not developing a thorough research paper! Review the tab in this guide for developing a research topic. If serious limitations exist, it generally indicates a likelihood that your research problem is too narrowly defined or that the issue or event under study is too recent and, thus, very little research has been written about it. If serious limitations do emerge, consult with your professor about possible ways to overcome them or how to revise your study. When discussing the limitations of your research, be sure to: Describe each limitation in detailed but concise terms; Explain why each limitation exists; Provide the reasons why each limitation could not be overcome using the method(s) chosen to acquire or gather the data [cite to other studies that had similar problems when possible]; Assess the impact of each limitation in relation to the overall findings and conclusions of your study; and, If appropriate, describe how these limitations could point to the need for further research. Remember that the method you chose may be the source of a significant limitation that has emerged during your interpretation of the results [for example, you didn't interview a group of people that you later wish you had]. If this is the case, don't panic. Acknowledge it, and explain how applying a different or more robust methodology might address the research problem more effectively in a future study. A underlying goal of scholarly research is not only to show what works, but to demonstrate what doesn't work or what needs further clarification. Aguinis, Hermam and Jeffrey R. Edwards. “Methodological Wishes for the Next Decade and How to Make Wishes Come True.” Journal of Management Studies 51 (January 2014): 143-174; Brutus, Stéphane et al. "Self-Reported Limitations and Future Directions in Scholarly Reports: Analysis and Recommendations." Journal of Management 39 (January 2013): 48-75; Ioannidis, John P.A. "Limitations are not Properly Acknowledged in the Scientific Literature." Journal of Clinical Epidemiology 60 (2007): 324-329; Pasek, Josh. Writing the Empirical Social Science Research Paper: A Guide for the Perplexed. January 24, 2012. Academia.edu; Structure: How to Structure the Research Limitations Section of Your Dissertation. Dissertations and Theses: An Online Textbook. Laerd.com; What Is an Academic Paper? Institute for Writing Rhetoric. Dartmouth College; Writing the Experimental Report: Methods, Results, and Discussion. The Writing Lab and The OWL. Purdue University.
Information about the limitations of your study are generally placed either at the beginning of the discussion section of your paper so the reader knows and understands the limitations before reading the rest of your analysis of the findings, or, the limitations are outlined at the conclusion of the discussion section as an acknowledgement of the need for further study. Statements about a study's limitations should not be buried in the body [middle] of the discussion section unless a limitation is specific to something covered in that part of the paper. If this is the case, though, the limitation should be reiterated at the conclusion of the section.
If you determine that your study is seriously flawed due to important limitations , such as, an inability to acquire critical data, consider reframing it as an exploratory study intended to lay the groundwork for a more complete research study in the future. Be sure, though, to specifically explain the ways that these flaws can be successfully overcome in a new study.
But, do not use this as an excuse for not developing a thorough research paper! Review the tab in this guide for developing a research topic . If serious limitations exist, it generally indicates a likelihood that your research problem is too narrowly defined or that the issue or event under study is too recent and, thus, very little research has been written about it. If serious limitations do emerge, consult with your professor about possible ways to overcome them or how to revise your study.
When discussing the limitations of your research, be sure to:
- Describe each limitation in detailed but concise terms;
- Explain why each limitation exists;
- Provide the reasons why each limitation could not be overcome using the method(s) chosen to acquire or gather the data [cite to other studies that had similar problems when possible];
- Assess the impact of each limitation in relation to the overall findings and conclusions of your study; and,
- If appropriate, describe how these limitations could point to the need for further research.
Remember that the method you chose may be the source of a significant limitation that has emerged during your interpretation of the results [for example, you didn't interview a group of people that you later wish you had]. If this is the case, don't panic. Acknowledge it, and explain how applying a different or more robust methodology might address the research problem more effectively in a future study. A underlying goal of scholarly research is not only to show what works, but to demonstrate what doesn't work or what needs further clarification.
Aguinis, Hermam and Jeffrey R. Edwards. “Methodological Wishes for the Next Decade and How to Make Wishes Come True.” Journal of Management Studies 51 (January 2014): 143-174; Brutus, Stéphane et al. "Self-Reported Limitations and Future Directions in Scholarly Reports: Analysis and Recommendations." Journal of Management 39 (January 2013): 48-75; Ioannidis, John P.A. "Limitations are not Properly Acknowledged in the Scientific Literature." Journal of Clinical Epidemiology 60 (2007): 324-329; Pasek, Josh. Writing the Empirical Social Science Research Paper: A Guide for the Perplexed . January 24, 2012. Academia.edu; Structure: How to Structure the Research Limitations Section of Your Dissertation . Dissertations and Theses: An Online Textbook. Laerd.com; What Is an Academic Paper? Institute for Writing Rhetoric. Dartmouth College; Writing the Experimental Report: Methods, Results, and Discussion . The Writing Lab and The OWL. Purdue University.
- << Previous: The Discussion
- Next: Conclusion >>
- Last Updated: Nov 6, 2023 1:43 PM
- URL: https://libraryguides.unh.edu/cpsonlinegradpaper

Organizing Academic Research Papers: Limitations of the Study
- Purpose of Guide
- Design Flaws to Avoid
- Glossary of Research Terms
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Extending the Timeliness of a Topic Idea
- Academic Writing Style
- Choosing a Title
- Making an Outline
- Paragraph Development
- Executive Summary
- Background Information
- The Research Problem/Question
- Theoretical Framework
- Citation Tracking
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tertiary Sources
- What Is Scholarly vs. Popular?
- Qualitative Methods
- Quantitative Methods
- Using Non-Textual Elements
- Limitations of the Study
- Common Grammar Mistakes
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Annotated Bibliography
- Dealing with Nervousness
- Using Visual Aids
- Grading Someone Else's Paper
- How to Manage Group Projects
- Multiple Book Review Essay
- Reviewing Collected Essays
- About Informed Consent
- Writing Field Notes
- Writing a Policy Memo
- Writing a Research Proposal
- Acknowledgements
The limitations of the study are those characteristics of design or methodology that impacted or influenced the application or interpretation of the results of your study. They are the constraints on generalizability and utility of findings that are the result of the ways in which you chose to design the study and/or the method used to establish internal and external validity.
Importance of...
Always acknowledge a study's limitations. It is far better for you to identify and acknowledge your study’s limitations than to have them pointed out by your professor and be graded down because you appear to have ignored them.
Keep in mind that acknowledgement of a study's limitations is an opportunity to make suggestions for further research. If you do connect your study's limitations to suggestions for further research, be sure to explain the ways in which these unanswered questions may become more focused because of your study.
Acknowledgement of a study's limitations also provides you with an opportunity to demonstrate to your professor that you have thought critically about the research problem, understood the relevant literature published about it, and correctly assessed the methods chosen for studying the problem. A key objective of the research process is not only discovering new knowledge but also to confront assumptions and explore what we don't know.
Claiming limitiations is a subjective process because you must evaluate the impact of those limitations . Don't just list key weaknesses and the magnitude of a study's limitations. To do so diminishes the validity of your research because it leaves the reader wondering whether, or in what ways, limitation(s) in your study may have impacted the findings and conclusions. Limitations require a critical, overall appraisal and interpretation of their impact. You should answer the question: do these problems with errors, methods, validity, etc. eventually matter and, if so, to what extent?
Structure: How to Structure the Research Limitations Section of Your Dissertation . Dissertations and Theses: An Online Textbook. Laerd.com.
Descriptions of Possible Limitations
All studies have limitations . However, it is important that you restrict your discussion to limitations related to the research problem under investigation. For example, if a meta-analysis of existing literature is not a stated purpose of your research, it should not be discussed as a limitation. Do not apologize for not addressing issues that you did not promise to investigate in your paper.
Here are examples of limitations you may need to describe and to discuss how they possibly impacted your findings. Descriptions of limitations should be stated in the past tense.
Possible Methodological Limitations
- Sample size -- the number of the units of analysis you use in your study is dictated by the type of research problem you are investigating. Note that, if your sample size is too small, it will be difficult to find significant relationships from the data, as statistical tests normally require a larger sample size to ensure a representative distribution of the population and to be considered representative of groups of people to whom results will be generalized or transferred.
- Lack of available and/or reliable data -- a lack of data or of reliable data will likely require you to limit the scope of your analysis, the size of your sample, or it can be a significant obstacle in finding a trend and a meaningful relationship. You need to not only describe these limitations but to offer reasons why you believe data is missing or is unreliable. However, don’t just throw up your hands in frustration; use this as an opportunity to describe the need for future research.
- Lack of prior research studies on the topic -- citing prior research studies forms the basis of your literature review and helps lay a foundation for understanding the research problem you are investigating. Depending on the currency or scope of your research topic, there may be little, if any, prior research on your topic. Before assuming this to be true, consult with a librarian! In cases when a librarian has confirmed that there is a lack of prior research, you may be required to develop an entirely new research typology [for example, using an exploratory rather than an explanatory research design]. Note that this limitation can serve as an important opportunity to describe the need for further research.
- Measure used to collect the data -- sometimes it is the case that, after completing your interpretation of the findings, you discover that the way in which you gathered data inhibited your ability to conduct a thorough analysis of the results. For example, you regret not including a specific question in a survey that, in retrospect, could have helped address a particular issue that emerged later in the study. Acknowledge the deficiency by stating a need in future research to revise the specific method for gathering data.
- Self-reported data -- whether you are relying on pre-existing self-reported data or you are conducting a qualitative research study and gathering the data yourself, self-reported data is limited by the fact that it rarely can be independently verified. In other words, you have to take what people say, whether in interviews, focus groups, or on questionnaires, at face value. However, self-reported data contain several potential sources of bias that should be noted as limitations: (1) selective memory (remembering or not remembering experiences or events that occurred at some point in the past); (2) telescoping [recalling events that occurred at one time as if they occurred at another time]; (3) attribution [the act of attributing positive events and outcomes to one's own agency but attributing negative events and outcomes to external forces]; and, (4) exaggeration [the act of representing outcomes or embellishing events as more significant than is actually suggested from other data].
Possible Limitations of the Researcher
- Access -- if your study depends on having access to people, organizations, or documents and, for whatever reason, access is denied or otherwise limited, the reasons for this need to be described.
- Longitudinal effects -- unlike your professor, who can literally devote years [even a lifetime] to studying a single research problem, the time available to investigate a research problem and to measure change or stability within a sample is constrained by the due date of your assignment. Be sure to choose a topic that does not require an excessive amount of time to complete the literature review, apply the methodology, and gather and interpret the results. If you're unsure, talk to your professor.
- Cultural and other type of bias -- we all have biases, whether we are conscience of them or not. Bias is when a person, place, or thing is viewed or shown in a consistently inaccurate way. It is usually negative, though one can have a positive bias as well. When proof-reading your paper, be especially critical in reviewing how you have stated a problem, selected the data to be studied, what may have been omitted, the manner in which you have ordered events, people, or places and how you have chosen to represent a person, place, or thing, to name a phenomenon, or to use possible words with a positive or negative connotation. Note that if you detect bias in prior research, it must be acknowledged and you should explain what measures were taken to avoid perpetuating bias.
- Fluency in a language -- if your research focuses on measuring the perceived value of after-school tutoring among Mexican-American ESL [English as a Second Language] students, for example, and you are not fluent in Spanish, you are limited in being able to read and interpret Spanish language research studies on the topic. This deficiency should be acknowledged.
Brutus, Stéphane et al. Self-Reported Limitations and Future Directions in Scholarly Reports: Analysis and Recommendations. Journal of Management 39 (January 2013): 48-75; Senunyeme, Emmanuel K. Business Research Methods . Powerpoint Presentation. Regent University of Science and Technology.
Structure and Writing Style
Information about the limitations of your study are generally placed either at the beginning of the discussion section of your paper so the reader knows and understands the limitations before reading the rest of your analysis of the findings, or, the limitations are outlined at the conclusion of the discussion section as an acknowledgement of the need for further study. Statements about a study's limitations should not be buried in the body [middle] of the discussion section unless a limitation is specific to something covered in that part of the paper. If this is the case, though, the limitation should be reiterated at the conclusion of the section.
If you determine that your study is seriously flawed due to important limitations , such as, an inability to acquire critical data, consider reframing it as a pilot study intended to lay the groundwork for a more complete research study in the future. Be sure, though, to specifically explain the ways that these flaws can be successfully overcome in later studies.
But, do not use this as an excuse for not developing a thorough research paper! Review the tab in this guide for developing a research topic . If serious limitations exist, it generally indicates a likelihood that your research problem is too narrowly defined or that the issue or event under study is too recent and, thus, very little research has been written about it. If serious limitations do emerge, consult with your professor about possible ways to overcome them or how to reframe your study.
When discussing the limitations of your research, be sure to:
- Describe each limitation in detailed but concise terms;
- Explain why each limitation exists;
- Provide the reasons why each limitation could not be overcome using the method(s) chosen to gather the data [cite to other studies that had similar problems when possible];
- Assess the impact of each limitation in relation to the overall findings and conclusions of your study; and,
- If appropriate, describe how these limitations could point to the need for further research.
Remember that the method you chose may be the source of a significant limitation that has emerged during your interpretation of the results [for example, you didn't ask a particular question in a survey that you later wish you had]. If this is the case, don't panic. Acknowledge it, and explain how applying a different or more robust methodology might address the research problem more effectively in any future study. A underlying goal of scholarly research is not only to prove what works, but to demonstrate what doesn't work or what needs further clarification.
Brutus, Stéphane et al. Self-Reported Limitations and Future Directions in Scholarly Reports: Analysis and Recommendations. Journal of Management 39 (January 2013): 48-75; Ioannidis, John P.A. Limitations are not Properly Acknowledged in the Scientific Literature. Journal of Clinical Epidemiology 60 (2007): 324-329; Pasek, Josh. Writing the Empirical Social Science Research Paper: A Guide for the Perplexed . January 24, 2012. Academia.edu; Structure: How to Structure the Research Limitations Section of Your Dissertation . Dissertations and Theses: An Online Textbook. Laerd.com; What Is an Academic Paper? Institute for Writing Rhetoric. Dartmouth College; Writing the Experimental Report: Methods, Results, and Discussion. The Writing Lab and The OWL. Purdue University.
Writing Tip
Don't Inflate the Importance of Your Findings! After all the hard work and long hours devoted to writing your research paper, it is easy to get carried away with attributing unwarranted importance to what you’ve done. We all want our academic work to be viewed as excellent and worthy of a good grade, but it is important that you understand and openly acknowledge the limitiations of your study. Inflating of the importance of your study's findings in an attempt hide its flaws is a big turn off to your readers. A measure of humility goes a long way!
Another Writing Tip
Negative Results are Not a Limitation!
Negative evidence refers to findings that unexpectedly challenge rather than support your hypothesis. If you didn't get the results you anticipated, it may mean your hypothesis was incorrect and needs to be reformulated, or, perhaps you have stumbled onto something unexpected that warrants further study. Moreover, the absence of an effect may be very telling in many situations, particularly in experimental research designs. In any case, your results may be of importance to others even though they did not support your hypothesis. Do not fall into the trap of thinking that results contrary to what you expected is a limitation to your study. If you carried out the research well, they are simply your results and only require additional interpretation.
Yet Another Writing Tip
A Note about Sample Size Limitations in Qualitative Research
Sample sizes are typically smaller in qualitative research because, as the study goes on, acquiring more data does not necessarily lead to more information. This is because one occurrence of a piece of data, or a code, is all that is necessary to ensure that it becomes part of the analysis framework. However, it remains true that sample sizes that are too small cannot adequately support claims of having achieved valid conclusions and sample sizes that are too large do not permit the deep, naturalistic, and inductive analysis that defines qualitative inquiry. Determining adequate sample size in qualitative research is ultimately a matter of judgment and experience in evaluating the quality of the information collected against the uses to which it will be applied and the particular research method and purposeful sampling strategy employed. If the sample size is found to be a limitation, it may reflect your judgement about the methodological technique chosen [e.g., single life history study versus focus group interviews] rather than the number of respondents used.
Huberman, A. Michael and Matthew B. Miles. Data Management and Analysis Methods. In Handbook of Qualitative Research. Norman K. Denzin and Yvonna S. Lincoln, eds. (Thousand Oaks, CA: Sage, 1994), pp. 428-444.
- << Previous: 8. The Discussion
- Next: 9. The Conclusion >>
- Last Updated: Jul 18, 2023 11:58 AM
- URL: https://library.sacredheart.edu/c.php?g=29803
- QuickSearch
- Library Catalog
- Databases A-Z
- Publication Finder
- Course Reserves
- Citation Linker
- Digital Commons
- Our Website
Research Support
- Ask a Librarian
- Appointments
- Interlibrary Loan (ILL)
- Research Guides
- Databases by Subject
- Citation Help
Using the Library
- Reserve a Group Study Room
- Renew Books
- Honors Study Rooms
- Off-Campus Access
- Library Policies
- Library Technology
User Information
- Grad Students
- Online Students
- COVID-19 Updates
- Staff Directory
- News & Announcements
- Library Newsletter
My Accounts
- Interlibrary Loan
- Staff Site Login
FIND US ON
Diving Deeper into Limitations and Delimitations

If you are working on a thesis, dissertation, or other formal research project, chances are your advisor or committee will ask you to address the delimitations of your study. When faced with this request, many students respond with a puzzled look and then go on to address what are actually the study’s limitations.
In a previous article , we covered what goes into the limitations, delimitations, and assumptions sections of your thesis or dissertation. Here, we will dive a bit deeper into the differences between limitations and delimitations and provide some helpful tips for addressing them in your research project—whether you are working on a quantitative or qualitative study.
Acknowledging Weaknesses vs. Defining Boundaries
These concepts are easy to get confused because both limitations and delimitations restrict (or limit) the questions you’ll be able to answer with your study, most notably in terms of generalizability.
However, the biggest difference between limitations and delimitations is the degree of control you have over them—that is, how much they are based in conscious, intentional choices you made in designing your study.
Limitations occur in all types of research and are, for the most part, outside the researcher’s control (given practical constraints, such as time, funding, and access to populations of interest). They are threats to the study’s internal or external validity.
Limitations may include things such as participant drop-out, a sample that isn’t entirely representative of the desired population, violations to the assumptions of parametric analysis (e.g., normality, homogeneity of variance), the limits of self-report, or the absence of reliability and validity data for some of your survey measures.
Limitations can get in the way of your being able to answer certain questions or draw certain types of inferences from your findings. Therefore, it’s important to acknowledge them upfront and make note of how they restrict the conclusions you’ll be able to draw from your study. Frequently, limitations can get in the way of our ability to generalize our findings to the larger populations or to draw causal conclusions, so be sure to consider these issues when you’re thinking about the potential limitations of your study.
Delimitations are also factors that can restrict the questions you can answer or the inferences you can draw from your findings. However, they are based on intentional choices you make a priori (i.e., as you’re designing the study) about where you’re going to draw the boundaries of your project. In other words, they define the project’s scope.
Like limitations, delimitations are a part of every research project, and this is not a bad thing. In fact, it’s very important! You can’t study everything at once. If you try to do so, your project is bound to get huge and unwieldy, and it will become a lot more difficult to interpret your results or come to meaningful conclusions with so many moving parts. You have to draw the line somewhere, and the delimitations are where you choose to draw these lines.
One of the clearest examples of a delimitation that applies to almost every research project is participant exclusion criteria. In conducting either a quantitative or a qualitative study, you will have to define your population of interest. Defining this population of interest means that you will need to articulate the boundaries of that population (i.e., who is not included). Those boundaries are delimitations.
For example, if you’re interested in understanding the experiences of elementary school teachers who have been implementing a new curriculum into their classrooms, you probably won’t be interviewing or sending a survey to any of the following people: non-teachers, high-school teachers, college professors, principals, parents of elementary school children, or the children themselves. Furthermore, you probably won’t be talking to elementary school teachers who have not yet had the experience of implementing the curriculum in question. You would probably only choose to gather data from elementary school teachers who have had this experience because that is who you’re interested in for the purposes of your study. Perhaps you’ll narrow your focus even more to elementary school teachers in a particular school district who have been teaching for a particular length of time. The possibilities can go on. These are choices you will need to make, both for practical reasons (i.e., the population you have access to) and for the questions you are trying to answer.
Of course, for this particular example, this does not mean that it wouldn’t be interesting to also know what principals think about the new curriculum. Or parents. Or elementary school children. It just means that, for the purposes of your project and your research questions, you’re interested in the experience of the teachers, so you’re excluding anyone who does not meet those criteria. Having delimitations to your population of interest also means that you won’t be able to answer any questions about the experiences of those other populations; this is ok because those populations are outside of the scope of your project . As interesting as their experiences might be, you can save these questions for another study. That is the part of the beauty of research: there will always be more studies to do, more questions to ask. You don’t have to (and can’t) do it all in one project.
Continuing with the previous example, for instance, let’s suppose that the problem you are most interested in addressing is the fact that we know relatively little about elementary school teachers’ experiences of implementing a new curriculum. Perhaps you believe that knowing more about teachers’ experiences could inform their training or help administrators know more about how to support their teachers. If the identified problem is our lack of knowledge about teachers’ experiences, and your research questions focus on better understanding these experiences, that means that you are choosing not to focus on other problems or questions, even those that may seem closely related. For instance, you are not asking how effective the new curriculum is in improving student test scores or graduation rates. You might think that would be a very interesting question, but it will have to wait for another study. In narrowing the focus of your research questions, you limit your ability to answer other questions, and again, that’s ok. These other questions may be interesting and important, but, again, they are beyond the scope of your project .
Common Examples of Limitations
While each study will have its own unique set of limitations, some limitations are more common in quantitative research, and others are more common in qualitative research.
In quantitative research, common limitations include the following:
– Participant dropout
– Small sample size, low power
– Non-representative sample
– Violations of statistical assumptions
– Non-experimental design, lack of manipulation of variables, lack of controls
– Potential confounding variables
– Measures with low (or unknown) reliability or validity
– Limits of an instrument to measure the construct of interest
– Data collection methods (e.g., self-report)
– Anything else that might limit the study’s internal or external validity
In qualitative research, common limitations include the following:
– Lack of generalizability of findings (not the goal of qualitative research, but still worth mentioning as a limitation)
– Inability to draw causal conclusions (again, not the goal of qualitative research, but still worth mentioning)
– Researcher bias/subjectivity (especially if there is only one coder)
– Limitations in participants’ ability/willingness to share or describe their experiences
– Any factors that might limit the rigor of data collection or analysis procedures
Common Examples of Delimitations
As noted above, the two most common sources of delimitations in both quantitative and qualitative research include the following:
– Inclusion/exclusion criteria (or how you define your population of interest)
– Research questions or problems you’ve chosen to examine
Several other common sources of delimitations include the following:
– Theoretical framework or perspective adopted
– Methodological framework or paradigm chosen (e.g., quantitative, qualitative, or mixed-methods)
– In quantitative research, the variables you’ve chosen to measure or manipulate (as opposed to others)
Whether you’re conducting a quantitative or qualitative study, you will (hopefully!) have chosen your research design because it is well suited to the questions you’re hoping to answer. Because these questions define the boundaries or scope of your project and thus point to its delimitations, your research design itself will also be related to these delimitations.
Questions to Ask Yourself
As you are considering the limitations and delimitations of your project, it can be helpful to ask yourself a few different questions.
Questions to help point out your study’s limitations :
1. If I had an unlimited budget, unlimited amounts of time, access to all possible populations, and the ability to manipulate as many variables as I wanted, how would I design my study differently to be better able to answer the questions I want to answer? (The ways in which your study falls short of this will point to its limitations.)
2. Are there design issues that get in the way of my being able to draw causal conclusions?
3. Are there sampling issues that get in the way of my being able to generalize my findings?
4. Are there issues related to the measures I’m using or the methods I’m using to collect data? Do I have concerns about participants telling the truth or being able to provide accurate responses to my questions?
5. Are there any other factors that might limit my study’s internal or external validity?
Questions that help point out your study’s delimitations :
1. What are my exclusion criteria? Who did I not include in my study, and why did I make this choice?
2. What questions did I choose not to address in my study? (Of course, the possibilities are endless here, but consider related questions that you chose not to address.)
3. In what ways did I narrow the scope of my study in order to hone in on a particular issue or question?
4. What other methodologies did I not use that might have allowed me to answer slightly different questions about the same topic?
How to Write About Limitations and Delimitations
Remember, having limitations and delimitations is not a bad thing. They’re present in even the most rigorous research. The important thing is to be aware of them and to acknowledge how they may impact your findings or the conclusions you can draw.
In fact, writing about them and acknowledging them gives you an opportunity to demonstrate that you can think critically about these aspects of your study and how they impact your findings, even if they were out of your control.
Keep in mind that your study’s limitations will likely point to important directions for future research. Therefore, when you’re getting ready to write about your recommendations for future research in your discussion, remember to refer back to your limitations section!
As you write about your delimitations in particular, remember that they are not weaknesses, and you don’t have to apologize for them. Good, strong research projects have clear boundaries. Also, keep in mind that you are the researcher and you can choose whatever delimitations you want for your study. You’re in control of the delimitations. You just have to be prepared—both in your discussion section and in your dissertation defense itself—to justify the choices you make and acknowledge how these choices impact your findings.
Browse More on PhDStudent

Everything You Need to Know About References and Citations: Part 1
When you conduct your research, it is important to record the details of all the information you find to provide accurate references, …

How to Write a Proposal: For a Master’s Thesis or Dissertation
Note: Many thanks to fellow PhDStudent blogger Ryan Krone for his contributions and insight to this post. Your thesis/dissertation proposal provides an …

How to Find Free Money for Graduate School Part 2
Getting into graduate school is already a challenge on its own, and funding the program once admitted is even harder. Graduate studies …

How to Find Free Money for Graduate School
You’ve finally earned your Bachelor’s degree and have made it into graduate school. Whether you already have massive student loans from undergrad …

Part 3 of How to Pick Your Defense Committee
What strategies can a doctoral student employ to maneuver the trials and tribulations of a dissertation committee? In Part 2, we …
Best Dissertation Proofreading and Editing Tips to Make Your Work Spotless
You’ve heard this statement many times before: “the dissertation is the most important project you’ve ever worked on.” That may sound like …

Part 2 of How to Pick Your Defense Committee
Choosing a committee can be a daunting task for a doctoral student. We’ve already covered two strategies that can help you through this …


Part 1 of How to Pick Your Defense Committee
So you’re ready to pick your committee members; there are a few things to keep in mind first—after all, it is a …

Intro To Series on How to Pick Your Defense Committee
Choosing the right defense committee can potentially be the difference between a smooth transition of receiving your doctoral degree or dodging bullets …
On Babies and Dissertations: Part 3
I recently had the experience of expecting my first baby a month before I graduated. Throughout the process, I accidentally learned several …

On Babies and Dissertations: Part 2

On Babies and Dissertations: Part 1
I recently had the experience of expecting my first baby a month before I graduated and accidentally learned tips on graduating on time with a …
Click here to cancel reply.
You must be logged in to post a comment.
Copyright © 2024 PhDStudent.com. All rights reserved. Designed by Divergent Web Solutions, LLC .

Research Limitations & Delimitations
What they are and how they’re different (with examples)
By: Derek Jansen (MBA) | Expert Reviewed By: David Phair (PhD) | September 2022
If you’re new to the world of research, you’ve probably heard the terms “ research limitations ” and “ research delimitations ” being thrown around, often quite loosely. In this post, we’ll unpack what both of these mean, how they’re similar and how they’re different – so that you can write up these sections the right way.
Overview: Limitations vs Delimitations
- Are they the same?
- What are research limitations
- What are research delimitations
- Limitations vs delimitations
First things first…
Let’s start with the most important takeaway point of this post – research limitations and research delimitations are not the same – but they are related to each other (we’ll unpack that a little later). So, if you hear someone using these two words interchangeably, be sure to share this post with them!
Research Limitations
Research limitations are, at the simplest level, the weaknesses of the study , based on factors that are often outside of your control as the researcher. These factors could include things like time , access to funding, equipment , data or participants . For example, if you weren’t able to access a random sample of participants for your study and had to adopt a convenience sampling strategy instead, that would impact the generalizability of your findings and therefore reflect a limitation of your study.
Research limitations can also emerge from the research design itself . For example, if you were undertaking a correlational study, you wouldn’t be able to infer causality (since correlation doesn’t mean certain causation). Similarly, if you utilised online surveys to collect data from your participants, you naturally wouldn’t be able to get the same degree of rich data that you would from in-person interviews .
Simply put, research limitations reflect the shortcomings of a study , based on practical (or theoretical) constraints that the researcher faced. These shortcomings limit what you can conclude from a study, but at the same time, present a foundation for future research . Importantly, all research has limitations , so there’s no need to hide anything here – as long as you discuss how the limitations might affect your findings, it’s all good.
Research Delimitations
Alright, now that we’ve unpacked the limitations, let’s move on to the delimitations .
Research delimitations are similar to limitations in that they also “ limit ” the study, but their focus is entirely different. Specifically, the delimitations of a study refer to the scope of the research aims and research questions . In other words, delimitations reflect the choices you, as the researcher, intentionally make in terms of what you will and won’t try to achieve with your study. In other words, what your research aims and research questions will and won’t include.
As we’ve spoken about many times before, it’s important to have a tight, narrow focus for your research, so that you can dive deeply into your topic, apply your energy to one specific area and develop meaningful insights. If you have an overly broad scope or unfocused topic, your research will often pull in multiple, even opposing directions, and you’ll just land up with a muddy mess of findings .
So, the delimitations section is where you’ll clearly state what your research aims and research questions will focus on – and just as importantly, what they will exclude . For example, you might investigate a widespread phenomenon, but choose to focus your study on a specific age group, ethnicity or gender. Similarly, your study may focus exclusively on one country, city or even organization. As long as the scope is well justified (in other words, it represents a novel, valuable research topic), this is perfectly acceptable – in fact, it’s essential. Remember, focus is your friend.
Need a helping hand?
Conclusion: Limitations vs Delimitations
Ok, so let’s recap.
Research limitations and research delimitations are related in that they both refer to “limits” within a study. But, they are distinctly different. Limitations reflect the shortcomings of your study, based on practical or theoretical constraints that you faced.
Contrasted to that, delimitations reflect the choices that you made in terms of the focus and scope of your research aims and research questions. If you want to learn more about research aims and questions, you can check out this video post , where we unpack those concepts in detail.

Psst... there’s more!
This post was based on one of our popular Research Bootcamps . If you're working on a research project, you'll definitely want to check this out ...
19 Comments
Good clarification of ideas on how a researcher ought to do during Process of choice
Thank you so much for this very simple but explicit explanation on limitation and delimitation. It has so helped me to develop my masters proposal. hope to recieve more from your site as time progresses
Thank you for this explanation – very clear.
Thanks for the explanation, really got it well.
This website is really helpful for my masters proposal
Thank you very much for helping to explain these two terms
I spent almost the whole day trying to figure out the differences
when I came across your notes everything became very clear
thanks for the clearly outlined explanation on the two terms, limitation and delimitation.
Very helpful Many thanks 🙏
Excellent it resolved my conflict .
I would like you to assist me please. If in my Research, I interviewed some participants and I submitted Questionnaires to other participants to answered to the questions, in the same organization, Is this a Qualitative methodology , a Quantitative Methodology or is it a Mixture Methodology I have used in my research? Please help me
How do I cite this article in APA format
Really so great ,finally have understood it’s difference now
Getting more clear regarding Limitations and Delimitation and concepts
I really appreciate your apt and precise explanation of the two concepts namely ; Limitations and Delimitations.
This is a good sources of research information for learners.
thank you for this, very helpful to researchers
Very good explained
Great and clear explanation, after a long confusion period on the two words, i can now explain to someone with ease.
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.28(1); Jan-Mar 2024
- PMC10882193

Limitations in Medical Research: Recognition, Influence, and Warning
Douglas e. ott.
Mercer University, Macon, Georgia, USA.
Background:
As the number of limitations increases in a medical research article, their consequences multiply and the validity of findings decreases. How often do limitations occur in a medical article? What are the implications of limitation interaction? How often are the conclusions hedged in their explanation?
To identify the number, type, and frequency of limitations and words used to describe conclusion(s) in medical research articles.
Search, analysis, and evaluation of open access research articles from 2021 and 2022 from the Journal of the Society of Laparoscopic and Robotic Surgery and 2022 Surgical Endoscopy for type(s) of limitation(s) admitted to by author(s) and the number of times they occurred. Limitations not admitted to were found, obvious, and not claimed. An automated text analysis was performed for hedging words in conclusion statements. A limitation index score is proposed to gauge the validity of statements and conclusions as the number of limitations increases.
A total of 298 articles were reviewed and analyzed, finding 1,764 limitations. Four articles had no limitations. The average was between 3.7% and 6.9% per article. Hedging, weasel words and words of estimative probability description was found in 95.6% of the conclusions.
Conclusions:
Limitations and their number matter. The greater the number of limitations and ramifications of their effects, the more outcomes and conclusions are affected. Wording ambiguity using hedging or weasel words shows that limitations affect the uncertainty of claims. The limitation index scoring method shows the diminished validity of finding(s) and conclusion(s).
INTRODUCTION
As the number of limitations in a medical research article increases, does their influence have a more significant effect than each one considered separately, making the findings and conclusions less reliable and valid? Limitations are known variables that influence data collection and findings and compromise outcomes, conclusions, and inferences. A large body of work recognizes the effect(s) and consequence(s) of limitations. 1 – 77 Other than the ones known to the author(s), unknown and unrecognized limitations influence research credibility. This study and analysis aim to determine how frequently and what limitations are found in peer-reviewed open-access medical articles for laparoscopic/endoscopic surgeons.
This research is about limitations, how often they occur and explained and/or justified. Failure to disclose limitations in medical writing limits proper decision-making and understanding of the material presented. All articles have limitations and constraints. Not acknowledging limitations is a lack of candor, ignorance, or a deliberate omission. To reduce the suspicion of invalid conclusions limitations and their effects must be acknowledged and explained. This allows for a clearer more focused assessment of the article’s subject matter without explaining its findings and conclusions using hedging and words of estimative probability. 78 , 79
An evaluation of open access research/meta-analysis/case series/methodologies/review articles published in the Journal of the Society of Laparoendoscopic and Robotic Surgery ( JSLS ) for 2021 and 2022 (129) and commentary/guidelines/new technology/practice guidelines/review/SAGES Masters Program articles in Surgical Endoscopy ( Surg Endosc ) for 2022 (169) totaling 298 were read and evaluated by automated text analysis for limitations admitted to by the paper’s authors using such words as “limitations,” “limits,” “shortcomings,” “inadequacies,” “flaws,” “weaknesses,” “constraints,” “deficiencies,” “problems,” and “drawbacks” in the search. Limitations not mentioned were found by reading the paper and assigning type and frequency. The number of hedging and weasel words used to describe the conclusion or validate findings was determined by reading the article and adding them up.
For JSLS , there were 129 articles having 63 different types of limitations. Authors claimed 476, and an additional 32 were found within the article, totaling 508 limitations (93.7% admitted to and 6.3% discovered that were not mentioned). This was a 3.9 limitation average per article. No article said it was free of limitations. The ten most frequent limitations and their rate of occurrence are in Table 1 . The total number of limitations, frequency, and visual depictions are seen in Figures 1A and and 1B 1B .

( A ) Visual depiction of the ranked frequency of limitations for JSLS articles reviewed.
The Ten Most Frequent Limitations Found in JSLS and Surg Endosc Articles
| top 10 limitations | Total number of limitations | Number of articles | Percent of total number of limitations | top 10 limitations | Total number of limitations | Number of articles | Percent of total number of limitations |
|---|---|---|---|---|---|---|---|
| Results not generalizable | 33 | 33/508 | 6.5% | Results not generalizable | 86 | 86/1256 | 6.8% |
| Retrospective study | 32 | 32/508 | 6.3% | Selection bias | 83 | 83/1256 | 6.6% |
| Small sample size | 32 | 32/508 | 6.3% | Confounding variables and comorbidities | 72 | 72/1256 | 5.7% |
| Confounding variables and comorbidities | 23 | 23/508 | 4.5% | Retrospective study | 69 | 69/1256 | 5.5% |
| Selection bias | 21 | 21/508 | 4.1% | Small sample size | 63 | 63/1256 | 5.0% |
| Incomplete data | 20 | 20/508 | 3.9% | Incomplete data | 58 | 58/1256 | 4.6% |
| Limited patient selection criteria | 16 | 16/508 | 3.1% | Lack of standardized treatment | 55 | 55/1256 | 4.4% |
| Limited data availability | 16 | 16/508 | 5.1% | Measurement problems | 53 | 53/1256 | 4.2% |
| No long-term follow-up | 15 | 15/508 | 3.0% | Limited analysis | 47 | 47/1256 | 3.7% |
| Reporting errors | 14 | 14/508 | 2.8% | Problems with study design | 39 | 39/1259 | 3.1% |
| 222/508 | 625/1256 |
There were 169 articles for Surg Endosc , with 78 different named limitations the authors claimed for a total of 1,162. An additional 94 limitations were found in the articles, totaling 1,256, or 7.4 per article. The authors explicitly stated 92.5% of the limitations, and an additional 7.5% of additional limitations were found within the article. Five claimed zero limitations (5/169 = 3%). The ten most frequent limitations and their rate of occurrence are in Table 1 . The total number of limitations and frequency is shown in Figures 1A and and 1B 1B .
Conclusions were described in hedged, weasel words or words of estimative probability 95.6% of the time (285/298).
A research hypothesis aims to test the idea about expected relationships between variables or to explain an occurrence. The assessment of a hypothesis with limitations embedded in the method reaches a conclusion that is inherently flawed. What is compromised by the limitation(s)? The result is an inferential study in the presence of uncertainty. As the number of limitations increases, the validity of information decreases due to the proliferation of uncertain information. Information gathered and conclusions made in the presence of limitations can be functionally unsound. Hypothesis testing of spurious conditions with limitations and then claiming a conclusion is not a reliable method for generating factual evidence. The authors’ reliance on limitation gathered “evidence” data and asserting that this is valid is spurious reasoning. The bridge between theory and evidence is not through limitations that unquestionably accept findings. A range of conclusion possibilities exists being some percent closer to either more correct or incorrect. Relying on leveraging the pursuit of “fact” in the presence of limitations as the safeguard is akin to the fox watching the hen house. Acknowledgment of the uncertainty limitations create in research and discounting the finding’s reliability would give more credibility to the effort. Shortcomings and widespread misuses of research limitation justifications make findings suspect and falsely justified in many instances.
The JSLS instructions to authors say that in the discussion section of the paper the author(s) must “Comment on any methodological weaknesses of the study” ( http://jsls.sls.org/guidelines-for-authors/ ). In their instructions for authors, Surg Endosc says that in the discussion of the paper, “A paragraph discussing study limitations is required” ( https://www.springer.com/journal/464/submission-guidelines ). A comment for a written article about a limitation should express an opinion or reaction. A paragraph discussing limitations, especially, if there is more than one, requires just that: a paragraph and discussion. These requirements were not met or enforced by JSLS 86% (111/129) of the time and 92.3% (156/169) for Surg Endosc . This is an error in peer reviewing, not adhering to established research publication best practices, and the journals needing to adhere to their guidelines. The International Committee of Medical Journal Editors, uniform requirements for manuscripts recommends that authors “State the limitations of your study, and explore the implications of your findings for future research and for clinical practice or policy. Discuss the influence or association of variables, such as sex and/or gender, on your findings, where appropriate, and the limitations of the data.” It also says, “describe new or substantially modified methods, give reasons for using them, and evaluate their limitations” and “Include in the Discussion section the implications of the findings and their limitations, including implications for future research” and “give references to established methods, including statistical methods (see below); provide references and brief descriptions for methods that have been published but are not well known; describe new or substantially modified methods, give reasons for using them, and evaluate their limitations.” 65 “Reporting guidelines (e.g., CONSORT, 1 ARRIVE 2 ) have been proposed to promote the transparency and accuracy of reporting for biomedical studies, and they often include discussion of limitations as a checklist item. Although such guidelines have been endorsed by high-profile biomedical journals, and compliance with them is associated with improved reporting quality, 3 adherence remains suboptimal.” 4 , 5
Limitations start in the methodologic design phase of research. They require troubleshooting evaluations from the start to consider what limitations exist, what is known and unknown, where, and how to overcome them, and how they will affect the reasonableness and assessment of possible conclusions. A named limitation represents a category with numerous components. Each factor has a unique effect on findings and collectively influences conclusion assessment. Even a single limitation can compromise the study’s implementation and adversely influence research parameters, resulting in diminished value of the findings, outcomes, and conclusions. This becomes more problematic as the number of limitations and their components increase. Any limitation influences a research paper. It is unknown how much and to what extent any limitation affects other limitations, but it does create a cascading domino effect of ever-increasing interactions that compromise findings and conclusions. Considering “research” as a system, it has sensitivity and initial conditions (methodology, data collection, analysis, etc.). The slightest alteration of a study due to limitations can profoundly impact all aspects of the study. The presence and influence of limitations introduce a range of unpredictable influences on findings, results, and conclusions.
Researchers and readers need to pay attention to and discount the effects limitations have on the validity of findings. Richard Feynman said in “Cargo cult science” “the first principle is that you must not fool yourself and you are the easiest person to fool.” 73 We strongly believe our own nonsense or wrong-headed reasoning. Buddhist philosophers say we are attached to our ignorance. Researchers are not critical enough about how they fool themselves regarding their findings with known limitations and then pass them on to readers. The competence of findings with known limitations results in suspect conclusions.
Authors should not ask for dismissal, disregard, or indulgence of their limitations. They should be thoughtful and reflective about the implications and uncertainty the limitations create 67 ; their uncertainties, blind spots, and impact on the research’s relevance. A meaningful presentation of study limitations should describe the limitation, explain its effect, provide possible alternative approaches, and describe steps taken to mitigate the limitation. This was largely absent from the articles reviewed.
Authors use synonyms and phrases describing limitations that hide, deflect, downplay, and divert attention from them, i.e., some drawbacks of the study are …, weaknesses of the study are…, shortcomings are…, and disadvantages of the study are…. They then say their finding(s) lack(s) generalizability, meaning the findings only apply to the study participants or that care, sometimes extreme, must be taken in interpreting the results. Which limitation components are they referring to? Are the authors aware of the extent of their limitations, or are they using convenient phrases to highlight the existence of limitations without detailing their defects?
Limitations negatively weigh on both data and conclusions yet no literature exists to provide a quantifiable measure of this effect. The only acknowledgment is that limitations affect research data and conclusions. The adverse effects of limitations are both specific and contextual to each research article and is part of the parameters that affect research. All the limitations are expressed in words, excuses, and a litany of mea culpas asking for forgiveness and without explaining the extent or magnitude of their impact. It is left to the writer and reader to figure out. It is not known what value writers put on their limitations in the 298 articles reviewed from JSLS and Surg Endosc . Listing limitations without comment and effect on the findings and conclusions is a compromising red flag. Therefore, a limitation scoring method was developed and is proposed to assess the level of suspicion generated by the number of limitations.
It is doubtful that a medical research article is so well designed and executed that there are no limitations. This is doubtful since there are unknown unknowns. This study showed that authors need to acknowledge all the limitations when they are known. They acknowledge the ones they know but do not consider other possibilities. There are the known known limitations; the ones the author(s) are aware of and can be measured, some explained, most not. The known unknowns: limitations authors are aware of but cannot explain or quantify. The unknown unknown limitations: the ones authors are not aware of and have unknown influence(s), i.e., the things they do not know they do not know. These are blind spots (not knowing what they do not know or black swan events). And the unknown knowns; the limitations authors may be aware of but have not disclosed, thoroughly reported, understood, or addressed. They are unexpected and not considered. See Table 2 . 74
Limitations of Known and Unknowns as They Apply to Limitations
| Things we are aware of and understand. | Things we are aware of but don’t understand. | |
| Things we understand but are not aware of. | Things we are neither aware of nor understand. | |
It is possible that authors did not identify, want to identify, or acknowledge potential limitations or were unaware of what limitations existed. Cumulative complexity is the result of the presence of multiple limitations because of the accumulation and interaction of limitations and their components. Just mentioning a limitation category and not the specific parts that are the limitation(s) is not enough. Authors telling readers of their known research limitations is a caution to discount the findings and conclusions. At what point does the caution for each limitation, its ramifications, and consequences become a warning? When does the piling up of mistakes, bad and missing data, biases, small sample size, lack of generalizability, confounding factors, etc., reach a point when the findings become s uninterpretable and meaningless? “Caution” indicates a level of potential hazard; a warning is more dire and consequential. Authors use the word “caution” not “warning” to describe their conclusions. There is a point when the number of limitations and their cumulative effects surpasses the point where a caution statement is no longer applicable, and a warning statement is required. This is the reason for establishing a limitations risk score.
Limitations put medical research articles at risk. The accumulation of limitations (variables having additional limitation components) are gaps and flaws diluting the probability of validity. There is currently no assessment method for evaluating the effect(s) of limitations on research outcomes other than awareness that there is an effect. Authors make statements warning that their results may not be reliable or generalizable, and need more research and larger numbers. Just because the weight effect of any given limitation is not known, explained, or how it discounts findings does not negate a causation effect on data, its analysis, and conclusions. Limitation variables and the ramifications of their effects have consequences. The relationship is not zero effect and accumulates with each added limitation.
As a result of this research, a limitation index score (LIS) system and assessment tool were developed. This limitation risk assessment tool gives a scores assessment of the relative validity of conclusions in a medical article having limitations. The adoption of the LIS scoring assessment tool for authors, researchers, editors, reviewers, and readers is a step toward understanding the effects of limitations and their causal relationships to findings and conclusions. The objective is cleaner, tighter methodologies, and better data assessment, to achieve more reliable findings. Adjustments to research conclusions in the presence of limitations are necessary. The degree of modification depends on context. The cumulative effect of this burden must be acknowledged by a tangible reduction and questioning of the legitimacy of statements made under these circumstances. The description calculating the LIS score is detailed in Appendix 1 .
A limitation word or phrase is not one limitation; it is a group of limitations under the heading of that word or phrase having many additional possible components just as an individual named influence. For instance, when an admission of selection bias is noted, the authors do not explain if it was an exclusion criterion, self-selection, nonresponsiveness, lost to follow-up, recruitment error, how it affects external validity, lack of randomization, etc., or any of the least 263 types of known biases causing systematic distortions of the truth whether unintentional or wanton. 40 , 76 Which forms of selection bias are they identifying? 63 Limitations have branches that introduce additional limitations influencing the study’s ability to reach a useful conclusion. Authors rarely tell you the effect consequences and extent limitations have on their study, findings, and conclusions.
This is a sample of limitations and a few of their component variables under the rubric of a single word or phrase. See Table 3 .
A Limitation Word or Phrase is a Limitation Having Additional Components That Are Additional Limitations. When an Author Uses the Limitation Composite Word or Phrase, They Leave out Which One of Its Components is Contributory to the Research Limitations. Each Limitation Interacts with Other Limitations, Creating a Cluster of Cross Complexities of Data, Findings, and Conclusions That Are Tainted and Negatively Affect Findings and Conclusions
| Small Sample Size | Retrospective Study | Selection Bias |
|---|---|---|
| Low statistical power | Missing information | Affects internal validity |
| Estimates not reliable | Recall bias | Nonrandom selection |
| Prone to biased samples | Observer bias | Leads to confounding |
| Not generalizable | Misclassification bias | Not generalizable |
| Prone to false negative error | Observer bias | Inaccurate relation to variables |
| Prone to false positive error | Evidence less robust than prospective study | Observer bias |
| Sampling error | Missing data | Sampling bias |
| Confounding factors | Volunteer bias | |
| Selection bias | Survivorship bias |
Limitations rarely occur alone. If you see one there are many you do not see or appreciate. Limitation s components interact with their own and other limitations, leading to complex connections interacting and discounting the reliability of findings. By how much is context dependent: but it is not zero. Limitations are variables influencing outcomes. As the number of limitations increases, the reliability of the conclusions decreases. How many variables (limitations) does it take to nullify the claims of the findings? The weight and influence of each limitation, its aggregate components, and interconnectedness have an unknown magnitude and effect. The result is a disorderly concoction of hearsay explanations. Table 4 is an example of just two single explanation limitations and some of their components illustrating the complex compounding of their effects on each other.
An Example of Interactions between Only Two Limitations and Some of Their Components Causes 16 Interactions
| Retrospective Study | Small Sample Size |
|---|---|
The novelty of this paper on limitations in medical science is not the identification of research article limitations or their number or frequency; it is the recognition of the multiplier effect(s) limitations and the influence they have on diminishing any conclusion(s) the paper makes. It is possible that limitations contribute to the inability of studies to replicate and why so many are one-time occurrences. Therefore, the generalizability statement that should be given to all readers is BEWARE THERE IS A REDUCTION EFFECT ON THE CONCLUSIONS IN THIS ARTICLE BECAUSE OF ITS LIMITATIONS.
Journals accept studies done with too many limitations, creating forking path situations resulting in an enormous number of possible associations of individual data points as multiple comparisons. 79 The result is confusion, a muddled mess caused by interactions of limitations undermining the ability to make valid inferences. Authors know and acknowledge but rarely explain them or their influence. They also use incomplete and biased databases, biased methods, small sample sizes, and not eliminating confounders, etc., but persist in doing research with these circumstances. Why is that? Is it because when limitations are acknowledged, authors feel justified in their conclusions? It wasn’t my poor research design; it was the limitation(s). How do peer reviewers score and analyze these papers without a method to discount the findings and conclusions in the presence of limitations? What are the calculus editors use to justify papers with multiple limitations, reaching compromised or spurious conclusions? How much caution or warning should a journal say must be taken in interpreting article results? How much? Which results? When? Under what circumstance(s)?
Since a critical component of research is its limitations, the quality and rigor of research are largely defined by, 75 these constraints making it imperative that limitations be exposed and explained. All studies have limitations admitted to or not, and these limitations influence outcomes and conclusions. Unfortunately, they are given insufficient attention, accompanied by feeble excuses, but they all matter. The degrees of freedom of each limitation influence every other limitation, magnifying their ramifications and confusion. Limitations of a scientific article must put the findings in context so the reader can judge the validity and strength of the conclusions. While authors acknowledge the limitations of their study, they influence its legitimacy.
Not only are limitations not properly acknowledged in the scientific literature, 8 but their implications, magnitude, and how they affect a conclusion are not explained or appreciated. Authors work at claiming their work and methods “overcome,” “avoid,” or “circumvent” limitations. Limitations are explained away as “Failure to prove a difference does not prove lack of a difference.” 60 Sample size, bias, confounders, bad data, etc. are not what they seem and do not sully the results. The implication is “trust me.” But that’s not science. Limitations create cognitive distortions and framing (misperception of reality) for the authors and readers. Data in studies with limitations is data having limitations. It was real but tainted.
Limitations are not a trivial aspect of research. It is a tangible something, positive or negative, put into a data set to be analyzed and used to reach a conclusion. How did these extra somethings, known unknowns, not knowns, and unknown knowns, affect the validity of the data set and conclusions? Research presented with the vagaries of explicit limitations is intensified by additional limitations and their component effects on top of the first limitation s , quickly diluting any conclusion making its dependability questionable.
This study’s analysis of limitations in medical articles averaged 3.9% per article for JSLS and 7.4% for Surg Endosc . Authors admit to some and are aware of limitations, but not all of them and discount or leave out others. Limitations were often presented with misleading and hedging language. Authors do not give weight or suggest the percent discount limitations have on the reliance of conclusion(s). Since limitations influence findings, reliability, generalizability, and validity without knowing the magnitude of each and their context, the best that can be said about the conclusions is that they are specific to the study described, context-driven, and suspect.
Limitations mean something is missing, added, incorrect, unseen, unaware of, fabricated, or unknown; circumstances that confuse, confound, and compromise findings and information to the extent that a notice is necessary. All medical articles should have this statement, “Any conclusion drawn from this medical study should be interpreted considering its limitations. Readers should exercise caution, use critical judgement, and consult other sources before accepting these findings. Findings may not be generalizable regardless of sample size, composition, representative data points, and subject groups. Methodologic, analytic, and data collection may have introduced biases or limitations that can affect the accuracy of the results. Controlling for confounding variables, known and unknown, may have influenced the data and/or observations. The accuracy and completeness of the data used to draw a conclusion may not be reliable. The study was specific to time, place, persons, and prevailing circumstances. The weight of each of these factors is unknown to us. Their effect may be limited or compounded and diminish the validity of the proposed conclusions.”
This study and findings are limited and constrained by the limitations of the articles reviewed. They have known and unknown limitations not accounted for, missing data, small sample size, incongruous populations, internal and external validity concerns, confounders, and more. See Tables 2 and and 3 . 3 . Some of these are correctible by the author’s awareness of the consequences of limitations, making plans to address them in the methodology phase of hypothesis assessment and performance of the research to diminish their effects.
Limitations in research articles are expected, but they can be reduced in their effect so that conclusions are closer to being valid. Limitations introduce elements of ignorance and suspicion. They need to be explained so their influence on the believability of the study and its conclusions is closer to meeting construct, content, face, and criterion validity. As the number of limitations increases, common sense, skepticism, study component acceptability, and understanding the ramifications of each limitation are necessary to accept, discount, or reject the author’s findings. As the number of hedging and weasel words used to explain conclusion(s) increases, believability decreases, and raises suspicion regarding claims. Establishing a systematic limitation scoring index limitations for authors, editors, reviewers, and readers and recognizing their cumulative effects will result in a clearer understanding of research content and legitimacy.
How to calculate the Limitation Index Score (LIS). See Tables 5 – 5 . Each limitation admitted to by authors in the article equals (=) one (1) point. Limitations may be generally stated by the author as a broad category, but can have multiple components, such as a retrospective study with these limitation components: 1. data or recall not accurate, 2. data missing, 3. selection bias not controlled, 4. confounders not controlled, 5. no randomization, 6. no blinding, 7. difficult to establish cause and effect, and 8. cannot draw a conclusion of causation. For each component, no matter how many are not explained and corrected, add an additional one (1) point to the score. See Table 2 .
The Limitation Scoring Index is a Numeric Limitation Risk Assessment Score to Rank Risk Categories and Discounting Probability of Validity and Conclusions. The More Limitations in a Study, the Greater the Risk of Unreliable Findings and Conclusions
| Number of limitations | Word description of discounting | Proposed percent discounting of conclusions | Outcome probability | Increasing level of less reliable conclusions |
|---|---|---|---|---|
| 0 | Unknown unknowns | 1–10% | May have valid conclusion(s) | Warning |
| 1–2 | Some | 15–25% | ↓ | ↓ |
| 3–4 | Probable | 35–45% | ↓ | Caution |
| 5–6 | Likely | 70–80% | ↓ | ↓ |
| 7–8 | Highly likely | 85–95% | ↓ | ↓ |
| >8 | Certain | 97–100% | Very questionable conclusion(s) | Danger |
Limitations May Be Generally Stated by the Author but Have Multiple Components, Such as a Retrospective Study Having Disadvantage Components of 1. Data or Recall Not Accurate, 2. Data Missing, 3. Selection Bias Not Controlled, 4. Confounders Not Controlled, 5. No Randomization, 6. No Blinding, 7 Difficult to Establish Cause and Effect, 8. Results Are Hypothesis Generating, and 9. Cannot Draw a Conclusion of Causation. For Each Component, Not Explained and Corrected, Add an Additional One (1) Point Is Added to the Score. Extra Blanks Are for Additional Limitations
| One point for each limitation | |
|---|---|
| One additional point for each component of each limitation | |
| Retrospective study | |
| Small sample size | |
| Not generalizable | |
| Selection bias | |
| Not controlling for confounders | |
| Not controlling for comorbidities | |
| Incomplete or missing data | |
| No long-term follow-up | |
| Reporting errors | |
| Measurement problems | |
| Study design problems | |
| Lack of standardized treatment | |
| Subtotal for Table 2 |
An Automatic 2 Points is Added for Meta-Analysis Studies Since They Have All the Retrospective Detrimental Components. 44 Data from Insurance, State, National, Medicare, and Medicaid, Because of Incorrect Coding, Over Reporting, and Under-Reporting, Etc. Each Component of the Limitation Adds One Additional Point. For Surveys and Questionnaires Add One Additional Point for Each Bias. Extra Blanks Are for Additional Limitations
| Two points for these limitations | |
|---|---|
| One additional point for each limitation and one additional point for each limitation component. | |
| Meta-analysis | |
| Data from Medicare, Medicaid, insurance companies, disease, state, and national databases | |
| Surveys and questionnaires | |
| Each limitation not admitted to | |
| Subtotal for Table 3 |
Automatic Five (5) Points for Manufacturer and User Facility Device Experience (MAUDE) Database Articles. The FDA Access Data Site Says Submissions Can Be “Incomplete, Inaccurate, Untimely, Unverified, or Biased” and “the Incidence or Prevalence of an Event Cannot Be Determined from This Reporting System Alone Due to Under-Reporting of Events, Inaccuracies in Reports, Lack of Verification That the Device Caused the Reported Event, and Lack of Information” and “DR Data Alone Cannot Be Used to Establish Rates of Events, Evaluate a Change in Event Rates over Time or Compare Event Rates between Devices. The Number of Reports Cannot Be Interpreted or Used in Isolation to Reach Conclusions” 80
| Five points for MAUDE based articles | |
|---|---|
| One additional point for each additional limitation and one point for each of its components. | |
| Subtotal for Table 4 |
Total Limitation Index Score
| Limitations | Calculation |
|---|---|
| Subtotal for Table 2 | |
| Subtotal for Table 3 | |
| Subtotal for Table 4 | |
| Total Limitation Index Score |
Each limitation not admitted to = two (2) points. A meta-analysis study gets an automatic 2 points since they are retrospective and have detrimental components that should be added to the 2 points. Data from insurance, state, national, Medicare, and Medicaid, because of incorrect coding, over-reporting, and underreporting, etc., score 2 points, and each component adds one additional point. Surveys and questionnaires get 2 points, and add one additional point for each bias. See Table 3 .
Manufacturer and User Facility Device Experience (MAUDE) database articles receive an automatic five (5) points. The FDA access data site says, submissions can be “incomplete, inaccurate, untimely, unverified, or biased” and “the incidence or prevalence of an event cannot be determined from this reporting system alone due to underreporting of events, inaccuracies in reports, lack of verification that the device caused the reported event, and lack of information” and “MDR data alone cannot be used to establish rates of events, evaluate a change in event rates over time or compare event rates between devices. The number of reports cannot be interpreted or used in isolation to reach conclusions.” 80 See Table 4 . Add one additional point for each additional limitation noted in the article.
Add one additional point for each additional limitation and one point for each of its components. Extra blanks are for additional
limitations and their component scores.
Funding sources: none.
Disclosure: none.
Conflict of interests: none.
Acknowledgments: Author would like to thank Lynda Davis for her help with data collection.
References:
All references have been archived at https://archive.org/web/
What are the limitations in research and how to write them?
Learn about the potential limitations in research and how to appropriately address them in order to deliver honest and ethical research.
It is fairly uncommon for researchers to stumble into the term research limitations when working on their research paper. Limitations in research can arise owing to constraints on design, methods, materials, and so on, and these aspects, unfortunately, may have an influence on your subject’s findings.
In this Mind The Graph’s article, we’ll discuss some recommendations for writing limitations in research , provide examples of various common types of limitations, and suggest how to properly present this information.
What are the limitations in research?
The limitations in research are the constraints in design, methods or even researchers’ limitations that affect and influence the interpretation of your research’s ultimate findings. These are limitations on the generalization and usability of findings that emerge from the design of the research and/or the method employed to ensure validity both internally and externally.
Researchers are usually cautious to acknowledge the limitations of their research in their publications for fear of undermining the research’s scientific validity. No research is faultless or covers every possible angle. As a result, addressing the constraints of your research exhibits honesty and integrity .
Why should include limitations of research in my paper?
Though limitations tackle potential flaws in research, commenting on them at the conclusion of your paper, by demonstrating that you are aware of these limitations and explaining how they impact the conclusions that may be taken from the research, improves your research by disclosing any issues before other researchers or reviewers do .
Additionally, emphasizing research constraints implies that you have thoroughly investigated the ramifications of research shortcomings and have a thorough understanding of your research problem.
Limits exist in any research; being honest about them and explaining them would impress researchers and reviewers more than disregarding them.
Remember that acknowledging a research’s shortcomings offers a chance to provide ideas for future research, but be careful to describe how your study may help to concentrate on these outstanding problems.
Possible limitations examples
Here are some limitations connected to methodology and the research procedure that you may need to explain and discuss in connection to your findings.
Methodological limitations
Sample size.
The number of units of analysis used in your study is determined by the sort of research issue being investigated. It is important to note that if your sample is too small, finding significant connections in the data will be challenging, as statistical tests typically require a larger sample size to ensure a fair representation and this can be limiting.
Lack of available or reliable data
A lack of data or trustworthy data will almost certainly necessitate limiting the scope of your research or the size of your sample, or it can be a substantial impediment to identifying a pattern and a relevant connection.
Lack of prior research on the subject
Citing previous research papers forms the basis of your literature review and aids in comprehending the research subject you are researching. Yet there may be little if any, past research on your issue.
The measure used to collect data
After finishing your analysis of the findings, you realize that the method you used to collect data limited your capacity to undertake a comprehensive evaluation of the findings. Recognize the flaw by mentioning that future researchers should change the specific approach for data collection.
Issues with research samples and selection
Sampling inaccuracies arise when a probability sampling method is employed to choose a sample, but that sample does not accurately represent the overall population or the relevant group. As a result, your study suffers from “sampling bias” or “selection bias.”
Limitations of the research
When your research requires polling certain persons or a specific group, you may have encountered the issue of limited access to these interviewees. Because of the limited access, you may need to reorganize or rearrange your research. In this scenario, explain why access is restricted and ensure that your findings are still trustworthy and valid despite the constraint.
Time constraints
Practical difficulties may limit the amount of time available to explore a research issue and monitor changes as they occur. If time restrictions have any detrimental influence on your research, recognize this impact by expressing the necessity for a future investigation.
Due to their cultural origins or opinions on observed events, researchers may carry biased opinions, which can influence the credibility of a research. Furthermore, researchers may exhibit biases toward data and conclusions that only support their hypotheses or arguments.
The structure of the limitations section
The limitations of your research are usually stated at the beginning of the discussion section of your paper so that the reader is aware of and comprehends the limitations prior to actually reading the rest of your findings, or they are stated at the end of the discussion section as an acknowledgment of the need for further research.
The ideal way is to divide your limitations section into three steps:
1. Identify the research constraints;
2. Describe in great detail how they affect your research;
3. Mention the opportunity for future investigations and give possibilities.
By following this method while addressing the constraints of your research, you will be able to effectively highlight your research’s shortcomings without jeopardizing the quality and integrity of your research.
Present your research or paper in an innovative way
If you want your readers to be engaged and participate in your research, try Mind The Graph tool to add visual assets to your content. Infographics may improve comprehension and are easy to read, just as the Mind The Graph tool is simple to use and offers a variety of templates from which you can select the one that best suits your information.
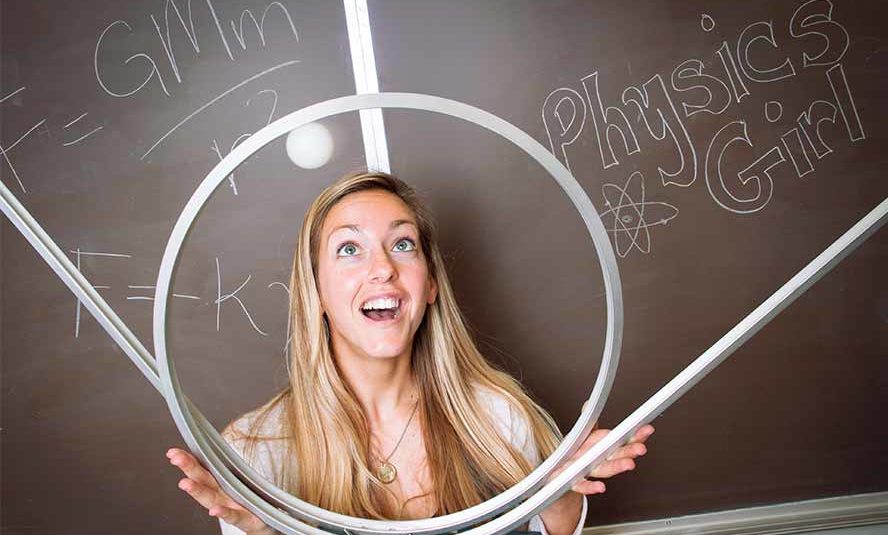
Subscribe to our newsletter
Exclusive high quality content about effective visual communication in science.
Sign Up for Free
Try the best infographic maker and promote your research with scientifically-accurate beautiful figures
no credit card required
About Jessica Abbadia
Jessica Abbadia is a lawyer that has been working in Digital Marketing since 2020, improving organic performance for apps and websites in various regions through ASO and SEO. Currently developing scientific and intellectual knowledge for the community's benefit. Jessica is an animal rights activist who enjoys reading and drinking strong coffee.
Content tags
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Limited by our limitations
Affiliations.
- 1 Medical School, University of Michigan, Ann Arbor, MI, USA. [email protected].
- 2 Medical School, University of Michigan, Ann Arbor, MI, USA.
- PMID: 31347033
- PMCID: PMC6684501
- DOI: 10.1007/s40037-019-00530-x
Study limitations represent weaknesses within a research design that may influence outcomes and conclusions of the research. Researchers have an obligation to the academic community to present complete and honest limitations of a presented study. Too often, authors use generic descriptions to describe study limitations. Including redundant or irrelevant limitations is an ineffective use of the already limited word count. A meaningful presentation of study limitations should describe the potential limitation, explain the implication of the limitation, provide possible alternative approaches, and describe steps taken to mitigate the limitation. This includes placing research findings within their proper context to ensure readers do not overemphasize or minimize findings. A more complete presentation will enrich the readers' understanding of the study's limitations and support future investigation.
Keywords: Limitations; Research.
PubMed Disclaimer
Similar articles
- Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. Crider K, Williams J, Qi YP, Gutman J, Yeung L, Mai C, Finkelstain J, Mehta S, Pons-Duran C, Menéndez C, Moraleda C, Rogers L, Daniels K, Green P. Crider K, et al. Cochrane Database Syst Rev. 2022 Feb 1;2(2022):CD014217. doi: 10.1002/14651858.CD014217. Cochrane Database Syst Rev. 2022. PMID: 36321557 Free PMC article.
- Discussing study limitations in reports of biomedical studies- the need for more transparency. Puhan MA, Akl EA, Bryant D, Xie F, Apolone G, ter Riet G. Puhan MA, et al. Health Qual Life Outcomes. 2012 Feb 23;10:23. doi: 10.1186/1477-7525-10-23. Health Qual Life Outcomes. 2012. PMID: 22360847 Free PMC article.
- The future of Cochrane Neonatal. Soll RF, Ovelman C, McGuire W. Soll RF, et al. Early Hum Dev. 2020 Nov;150:105191. doi: 10.1016/j.earlhumdev.2020.105191. Epub 2020 Sep 12. Early Hum Dev. 2020. PMID: 33036834
- Impact of summer programmes on the outcomes of disadvantaged or 'at risk' young people: A systematic review. Muir D, Orlando C, Newton B. Muir D, et al. Campbell Syst Rev. 2024 Jun 13;20(2):e1406. doi: 10.1002/cl2.1406. eCollection 2024 Jun. Campbell Syst Rev. 2024. PMID: 38873396 Free PMC article. Review.
- Research integrity and academic medicine: the pressure to publish and research misconduct. Kearney M, Downing M, Gignac EA. Kearney M, et al. J Osteopath Med. 2024 Feb 27;124(5):187-194. doi: 10.1515/jom-2023-0211. eCollection 2024 May 1. J Osteopath Med. 2024. PMID: 38407191 Review.
- Parenteral Nutrition in Palliative Cancer Care: Detrimental, Futile, or Beneficial? Løhre ET, Solheim TS, Jakobsen G, Vagnildhaug OM, Schmidberger Karlsen TL, Habberstad RH, Balstad TR, Thronæs M. Løhre ET, et al. Curr Oncol. 2024 May 11;31(5):2748-2757. doi: 10.3390/curroncol31050208. Curr Oncol. 2024. PMID: 38785489 Free PMC article.
- Long-term incidence of arrhythmias in extracardiac conduit Fontan and comparison between systemic left and right ventricle. Di Mambro C, Yammine ML, Tamborrino PP, Giordano U, Righi D, Unolt M, Cantarutti N, Maiolo S, Albanese S, Carotti A, Amodeo A, Galletti L, Drago F. Di Mambro C, et al. Europace. 2024 May 2;26(5):euae097. doi: 10.1093/europace/euae097. Europace. 2024. PMID: 38650062 Free PMC article.
- Limitations in Medical Research: Recognition, Influence, and Warning. Ott DE. Ott DE. JSLS. 2024 Jan-Mar;28(1):e2023.00049. doi: 10.4293/JSLS.2023.00049. JSLS. 2024. PMID: 38405216 Free PMC article.
- Harnessing Reliable Evidence in the Post-COVID Era: A Practice Guide to Navigating the Ocean of Medical Literature. Ooi C, Nalliah S. Ooi C, et al. Cureus. 2024 Jan 22;16(1):e52746. doi: 10.7759/cureus.52746. eCollection 2024 Jan. Cureus. 2024. PMID: 38384650 Free PMC article.
- Effects of a Comprehensive Dietary Intervention Program, Promoting Nutrition Literacy, Eating Behavior, Dietary Quality, and Gestational Weight Gain in Chinese Urban Women with Normal Body Mass Index during Pregnancy. Li Q, Piaseu N, Phumonsakul S, Thadakant S. Li Q, et al. Nutrients. 2024 Jan 10;16(2):217. doi: 10.3390/nu16020217. Nutrients. 2024. PMID: 38257110 Free PMC article. Clinical Trial.
- Connelly LM. Limitation Section. Medsurg Nurs. 2013;22:325–336. - PubMed
- Puhan M, Akl E, Bryant D, Zie F, Apolone G, ter Riet G. Discussing study limitations in reports of biomedical studies-the need for more transparency. Health Qual Life Outcomes. 2012 - PMC - PubMed
- Wang M, Bolland M, Grey A. Reporting of limitations of observational research. Jama Intern Med. 2015;175:1571–1572. doi: 10.1001/jamainternmed.2015.2147. - DOI - PubMed
- Ringsted C, Hodges B, Scherpbier A. The research compass: an introduction to research in medical education: AMEE guide no. 56. Med Teach. 2001;33:695–709. doi: 10.3109/0142159X.2011.595436. - DOI - PubMed
- Norman G. Research in medical education: three decades of progress. BMJ. 2002;324:1560–1562. doi: 10.1136/bmj.324.7353.1560. - DOI - PMC - PubMed
- Search in MeSH
LinkOut - more resources
Full text sources.
- Europe PubMed Central
- PubMed Central
- Ubiquity Press

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

Research Limitations
It is for sure that your research will have some limitations and it is normal. However, it is critically important for you to be striving to minimize the range of scope of limitations throughout the research process. Also, you need to provide the acknowledgement of your research limitations in conclusions chapter honestly.
It is always better to identify and acknowledge shortcomings of your work, rather than to leave them pointed out to your by your dissertation assessor. While discussing your research limitations, don’t just provide the list and description of shortcomings of your work. It is also important for you to explain how these limitations have impacted your research findings.
Your research may have multiple limitations, but you need to discuss only those limitations that directly relate to your research problems. For example, if conducting a meta-analysis of the secondary data has not been stated as your research objective, no need to mention it as your research limitation.
Research limitations in a typical dissertation may relate to the following points:
1. Formulation of research aims and objectives . You might have formulated research aims and objectives too broadly. You can specify in which ways the formulation of research aims and objectives could be narrowed so that the level of focus of the study could be increased.
2. Implementation of data collection method . Because you do not have an extensive experience in primary data collection (otherwise you would not be reading this book), there is a great chance that the nature of implementation of data collection method is flawed.
3. Sample size. Sample size depends on the nature of the research problem. If sample size is too small, statistical tests would not be able to identify significant relationships within data set. You can state that basing your study in larger sample size could have generated more accurate results. The importance of sample size is greater in quantitative studies compared to qualitative studies.
4. Lack of previous studies in the research area . Literature review is an important part of any research, because it helps to identify the scope of works that have been done so far in research area. Literature review findings are used as the foundation for the researcher to be built upon to achieve her research objectives.
However, there may be little, if any, prior research on your topic if you have focused on the most contemporary and evolving research problem or too narrow research problem. For example, if you have chosen to explore the role of Bitcoins as the future currency, you may not be able to find tons of scholarly paper addressing the research problem, because Bitcoins are only a recent phenomenon.
5. Scope of discussions . You can include this point as a limitation of your research regardless of the choice of the research area. Because (most likely) you don’t have many years of experience of conducing researches and producing academic papers of such a large size individually, the scope and depth of discussions in your paper is compromised in many levels compared to the works of experienced scholars.
You can discuss certain points from your research limitations as the suggestion for further research at conclusions chapter of your dissertation.
My e-book, The Ultimate Guide to Writing a Dissertation in Business Studies: a step by step assistance offers practical assistance to complete a dissertation with minimum or no stress. The e-book covers all stages of writing a dissertation starting from the selection to the research area to submitting the completed version of the work within the deadline. John Dudovskiy
Enjoy a completely custom, expertly-written dissertation. Choose from hundreds of writers, all of whom are career specialists in your subject.
Limitations of a Study: The Complete Guide

Research limitations make most studies imperfect. At its core, the research aims to investigate a specific question or questions about a topic. However, some things can hinder your ability to investigate the question or questions extensively. While this can make achieving your goals challenging, it enables you to point areas that require further studies.
That’s why you should demonstrate how future studies can provide answers to your unanswered questions if you encounter study limitations that affect your findings. Presenting the limitations of a study properly shows the readers that you understand your research problem.
After presenting your research findings, your assessment committee wants to see that you did your work professionally. And presenting limitations in a study shows that you carefully thought about your study problem and performed a review of the available literature while analyzing your preferred methods.
What Are Limitations in Research?
Well, limitations mean anything that might affect the generalizability or reliability of the outcomes of an experiment or a study. And this can relate to research design, like your approach or methods. It can also be something to do with how you carried out your research, like running out of resources or time before completing the study.
Either way, students should include their limitations when writing up their studies. In most cases, researchers include limitations in their analysis and discussions. But different schools can provide varying guidelines on how to include limitations in a research paper. Therefore, seek advice from your educator or check your writing style guide to know where to include the limitations of a study when writing a dissertation.
Common Study Limitations
Each study can have unique limitations. However, most students encounter common study limitations when writing academic papers. Here are some of the most common limitations you’re likely to encounter when writing your academic papers.
Sample profile or size: Most researchers encounter sampling as a limitation for their studies. That’s because they have difficulties finding the right sample with the necessary characteristics and size parameters. And this hinders the generalizability of their study results. Also, different sampling techniques are prone to bias and errors. And this can influence the study outcomes. In some cases, researchers have difficulties selecting their samples and opt to pick their participants selectively. Some researchers can even include irrelevant subjects in their general pool to hit their preferred sample size. Availability of previous research or information: Theoretical concepts or previous knowledge form the basis of studies on specific topics. And this provides a sound foundation on which a researcher can develop a research problem for their investigation and a design. However, a topic can be relatively specific or very progressive. In that case, the lack of or inadequate knowledge and previous studies can limit the analysis scope. And this can cause inaccuracies in the arguments or present a significant error margin in several methodologies and research aspects. Methodology errors: Modern research complexity can cause potential methodology limitations. In most cases, these research limitations relate to how the researchers collect and analyze data. That’s because these aspects can influence the outcomes of a study. Researchers use different techniques to gather data. While these techniques may suit a study design, they can present limitations in terms of inappropriate detail levels, distractions, and privacy. Bias: Bias is a potential limitation whose effects can influence the outcome of every study. However, a researcher can avoid this limitation by eliminating prejudiced or emotional attitudes towards their topic and conflict of interest. Researchers should also establish an oversight level by referring to peer-review procedures or an ethics committee. Bias is an inherent trait for human beings. Even the most objective people exhibit a bias to some extent. Nevertheless, a researcher should remain objective while trying to control potential inaccuracies or bias during the research process.
A researcher may not have control over the limitation of study. However, the limitation can be the condition, influence, or shortcoming that places restrictions on their conclusions or methodology. Therefore, researchers should mention all limitations that can influence their results.
Limitations of the Study Example
The purpose of most studies is to confirm or establish facts, reaffirm a previous study’s outcomes, solve current or new issues, develop a new theory, or support theorems. Research should also enable experts to develop knowledge on specific subjects. And people research different subjects, depending on their interests. However, researchers experience limitations of quantitative research and qualitative research. Here are the most common limitations in research.
Lack or inadequate interactions: Researchers might lack adequate interactions with government institutions and businesses. Consequently, they do not tap a substantial data amount. Researchers should arrange interaction programs with other establishments. That way, they can identify issues that warrant investigation and the necessary data for conducting research, as well as, the benefits of their studies. Overlapping studies can lead fritter resources away or duplicate the findings. Appropriate revision and compilation at regular intervals can solve this problem. Costly publishing: After researching a topic, a researcher should find ways to publish their findings. However, international journals cost a lot of money to publish a study. And this can discourage a researcher from publishing their work. For instance, a study involving females only or carried out in a specific town can have limitations like sample size, gender, and location. What’s more, the entire study could be limited to the researcher’s perception. Lack of or inadequate training: The research process doesn’t have a systematic methodology. Many researchers do not understand the research method when carrying out their work. Consequently, most researchers experience methodological limitations. Essentially, most researchers replicate the methodologies of similar studies. Even some research guides don’t explain the methodologies accurately. And this can limit the outcome of some studies. Lack of code of conduct: Researchers don’t have a code of conduct. And this causes inter-university and inter-departmental rivalries. Library functioning and management are not adequate in most places. Consequently, some researchers spend a lot of energy and time tracing the necessary books, reports, and journals for their studies. Such energy and time can be spent tracing relevant materials. Lack of confidence: The lack of confidence is among the most common limitations of research studies because company managers think that a researcher can misuse the data they disclose to them. Consequently, they don’t want to reveal their business information. And this can affect studies, yet data from researchers can help the same institutions. Therefore, organizations and researchers should implement confidence-building strategies to encourage companies to share data, knowing that researchers will use it productively.
Why Write the Limitations of a Study?
When writing a research paper or a thesis, some people think including study limitations is counterintuitive. That’s particularly the case for researchers that experienced something wrong. However, mentioning the limitations of your study is imperative for the following reasons.
- It tells the readers that you understand that no study lacks some limitations, and you took the time to analyze your work critically.
- It provides opportunities for further studies.
- It enables you to discuss the impacts of the limitations on your analysis and how future studies can address the challenges you encountered if granted a chance to do the study again.
- It presents your study as a transparent undertaking, making the results useful and credible for other people.
Most professors spot problems with the students’ work even if they don’t mention them. Consequently, embracing the limitations of your study and including them in your analysis is the best approach. Leaving out the limitations of research or vital aspects of a study can be detrimental to the entire study field. That’s because it can establish a potentially fallacious and incomplete depiction of the study.
In the academic world, players expect researchers to include the limitations of their works. And this includes a section that demonstrates a holistic and comprehensive understanding of a topic and research process by the author. Discussing limitations is a learning process for assessing the magnitude while critically evaluating the extenuating effect of the stated limitations.
Stating the limitations of a study also improves the validity and quality of future studies. And this includes limitations whose basis is the transparency principle in scientific research, whose purpose is to promote further progress while maintaining mutual integrity in similar studies.
How to Write Study Limitations
When writing your research limitations, do it in a way that demonstrates your understanding of the core concepts of confounding, analytical self-criticism, and bias. Highlighting every limitation might not be necessary. However, include every limitation with a direct impact on your research problem or study results.
Present your thought process as a researcher and explain the pros and cons of your decisions. Also, explain circumstances that may have led to a research limitation. Here’s how you should structure your limitations.
- Identification and description of the limitation: Use professional terminology to identify and describe the limitation. Also, include all necessary accompanying definitions. The limitation explanation should be precise and brief to ensure that the audience can easily understand the issue. Additionally, make sure that your audience can follow your thought pattern.
- Outline the possible impact or influence of the limitation: Explain to your readers how the limitation may have affected or influenced your study. And this comprises elements like the impact’s magnitude, occurrence likelihood, and the general direction the specific limitation could have driven your findings. Researchers generally accept that a limitation can have a more profound influence on a study than others. Therefore, highlight the effect or influence of a limitation to help readers decide on the issues to consider while examining your topic. And this is vital because a limitation whose value bias is null is less dangerous.
- Discuss alternative approaches to limitations: You can also discuss alternative ways to approach the limitations of your research question. However, the researcher should support the methodology or approach they selected in their study. Also, a research paper should explain why the study context warranted the methodology or approach, regardless of the limitation’s nature. Some researchers even provide persuasive evidence while discussing alternative decisions to some extent. And this shows thought transparency while reassuring readers that the researcher chose the best approach, despite the possible laminations.
- Description of the techniques for minimizing risks: Any limitation in research comes with some risks. Therefore, a researcher should describe possible techniques for minimizing the potential risk from the stated limitations. Such techniques can include a reference of previous studies and suggestions for improving data analysis and research design.
Don’t forget that acknowledging your study limitations provides a chance to suggest the direction for further studies. Therefore, connect the limitations of your study to the suggestions you make for further research. Also, explain how your study can make the unanswered questions more focused.
Also, acknowledging the limitation of the study enables you to demonstrate to the professor that you have critically thought about your research problem and understood the importance of the already-published literature. What’s more, it shows that you’ve carefully assessed the methods for studying your study problem. In research, a key objective is to discover new knowledge while confronting assumptions as you explore what others might not know.
Writing limitations should be a subjective process. That’s because you must analyze the impacts of the limitations and include them in your paper. In this section, don’t include the key weaknesses only. Instead, highlight the magnitude of the limitations of your research. And doing this requires you to demonstrate your study’s validity. Show the readers how the limitations have impacted your study outcomes and conclusions. Thus, writing the limitations section of your paper requires an overall, critical interpretation and appraisal of the impact. Essentially, this section should tell the readers why the problems with methods, errors, validity, and other limitations matter and to what extent.
Practical Tips for Writing Research Limitations
When writing a research paper, include information about your study’s limitations at the beginning of the discussion section. That way, your readers can understand your study limitations before delving into the deeper analysis. In some cases, authors bring out limitations when concluding their research discussion and highlighting the essence of further study on the subject. Here are practical tips to help you write the limitations of your study more effectively.
- Check some examples of limitations in research first: To understand the best way to include or present the limitations of your study, check how other authors do it. The internet is awash with good sample papers with a section for limitations. Checking such samples can help you write a limitations section for your academic paper.
- Include essential limitations only: Don’t come up with a list of limitations in your research paper. That’s because doing so can discredit the entire research project. Instead, highlight up to 3 limitations whose influence on your work was the highest. Also, explain how each of the limitations affected your work and research findings.
- Be brief and direct to the point: Identify the limitation, what caused it, and its impact on your research. Don’t expound on the limitation beyond this because the limitation section should be a small part of your paper.
- Be sincere: Don’t make up some lies or disguise your research limitations. That’s because doing so could prove you aren’t prepared. Therefore, be true and sincere with the audience. As you might see in good examples of study limitations, this section tells the audience what could be different or better.
- Explain what caused the limitations of your study: Your audience should have an easy time identifying the reason for the limitations. Therefore, make sure that you have explained everything correctly. Telling the readers about a limiting factor without explaining it can give them the impression that you’re outside your research project.
- Make suggestions for further studies: An ideal way for reversing points that other researchers can explore is to suggest future research paths. Your study could have failed in certain aspects. Maybe you didn’t achieve your expected results. However, it can prompt other researchers to take different directions in their future studies. Also, explain how other researchers can overcome the limitations you encountered in your study. You can even demonstrate why additional studies on the topic or subject are essential.
- Don’t confuse negative results with limitations: If your study brings out negative results, don’t confuse them for limitations. What negative outcomes mean is that you should support your hypothesis instead of opposing it. Perhaps, you can check sample limitations to understand what qualifies as a limitation. However, you can reformulate your hypothesis if you get negative results. Even when you stumble onto something you didn’t expect, don’t highlight it as a limitation.
Final Thoughts
When working on the limitations section of a research paper, be precise and clear. If writing this section becomes challenging, follow the tips shared in this article or seek assistance. That way, you can impress your educator by highlighting the limitations of your study properly.
Frequently Asked Questions
Richard Ginger is a dissertation writer and freelance columnist with a wealth of knowledge and expertise in the writing industry. He handles every project he works on with precision while keeping attention to details and ensuring that every work he does is unique.

Succeed With A Perfect Dissertation

Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
As Putin continues killing civilians, bombing kindergartens, and threatening WWIII, Ukraine fights for the world's peaceful future.
Ukraine Live Updates
- Open access
- Published: 12 September 2024
Frailty as a sequela of burn injury: a post hoc analysis of the “RE-ENERGIZE” multicenter randomized-controlled trial and the National Health Interview Survey
- Adriana C. Panayi ORCID: orcid.org/0000-0003-4053-9855 1 ,
- Daren K. Heyland 2 ,
- Christian Stoppe 3 , 4 ,
- Marc G. Jeschke 5 ,
- Samuel Knoedler 6 ,
- Christian Tapking 1 ,
- Oliver Didzun 1 ,
- Valentin Haug 7 ,
- Amir K. Bigdeli 1 ,
- Ulrich Kneser 1 ,
- Dennis P. Orgill 6 &
- Gabriel Hundeshagen 1
Military Medical Research volume 11 , Article number: 63 ( 2024 ) Cite this article
Metrics details
With advancements in burn treatment and intensive care leading to decreased mortality rates, a growing cohort of burn survivors is emerging. These individuals may be susceptible to frailty, characterized by reduced physiological reserve and increased vulnerability to stressors commonly associated with aging, which significantly complicates their recovery process. To date, no study has investigated burns as a potential risk factor for frailty. This study aimed to determine the short-term prevalence of frailty among burn survivors’ months after injury and compare it with that of the general population.
A post hoc analysis was conducted on the Randomized Trial of Enteral Glutamine to Minimize the Effects of Burn Injury (RE-ENERGIZE) trial, an international randomized-controlled trial involving 1200 burn injury patients with partial- or full-thickness burns. Participants who did not complete the 36-Item Short Form Health Survey (SF-36) questionnaire were excluded. Data for the general population were obtained from the 2022 National Health Interview Survey (NHIS). Frailty was assessed using the FRAIL (Fatigue, Resistance, Ambulation, Illness, Loss of weight) scale. Due to lack of data on loss of weight, for the purposes of this study, malnutrition was used as the fifth variable. Illness and malnutrition were based on admission data, while fatigue, resistance, and ambulation were determined from post-discharge responses to the SF-36. The burn cohort and general population groups were matched using propensity score matching and compared in terms of frailty status. Within the burn group, patients were divided into different subgroups based on their frailty status, and the differences in their (instrumental) activities of daily living (iADL and ADL) were compared. A multivariable analysis was performed within the burn cohort to identify factors predisposing to frailty as well as compromised iADL and ADL.
Out of the 1200 burn patients involved in the study, 600 completed the required questionnaires [follow-up time: (5.5 ± 2.3) months] and were matched to 1200 adults from the general population in the U.S. In comparison to the general population, burn patients exhibited a significantly higher likelihood of being pre-frail (42.3% vs. 19.8%, P < 0.0001), or frail (13.0% vs. 1.0%, P < 0.0001). When focusing on specific components, burn patients were more prone to experiencing fatigue (25.8% vs. 13.5%, P < 0.0001), limited resistance (34.0% vs. 2.7%, P < 0.0001), and restricted ambulation (41.8% vs. 3.8%, P < 0.0001). Conversely, the incidence rate of illness was observed to be higher in the general population (1.2% vs. 2.8%, P = 0.03), while no significant difference was detected regarding malnutrition (2.3% vs. 2.6%, P = 0.75). Furthermore, in comparison with robust burn patients, it was significantly more likely for pre-frail and frail patients to disclose compromise in ADL and iADL. The frail cohort reported the most pronounced limitation.
Conclusions
Our findings suggest a higher incidence of post-discharge frailty among burn survivors in the short-term following injury. Burn survivors experience compromised fatigue, resistance, and ambulation, while rates of illness and malnutrition were lower or unchanged, respectively. These results underscore the critical need for early identification of frailty after a burn injury, with timely and comprehensive involvement of a multidisciplinary team including burn and pain specialists, community physicians, physiotherapists, nutritionists, and social workers. This collaborative effort can ensure holistic care to address and mitigate frailty in this patient population.
It is estimated that up to 33,000 people each day—7 to 12 million people per year—sustain a burn injury that requires medical care and can lead to limitations in quality of life or result in death [ 1 ]. Given the backdrop of an aging population, there has been a burgeoning interest in evaluating post-burn outcomes among older adults. The assessment of the impact of “aging” on post-burn outcomes requires analysis through the lens of frailty, whereby frailty denotes an augmented susceptibility to stressors due to decreased physiological reserve and diminished capacity to maintain homeostasis [ 2 ].
A systematic review conducted in 2023 synthesized all published research on frailty and burns, identifying 18 studies dating back to 2013, with one-third of the studies published in 2022 [ 3 ]. All studies explored frailty as a risk factor for adverse outcomes of acute burns, yet the reverse hypothesis—that burn injury itself is a risk factor for long-term frailty—remains entirely unexplored. This gap in research is significant, considering that the long-term consequences of burns align with the criteria of most frailty indices [ 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 ]. Despite this, a history of burns is not included in such assessments.
The hypothesis proposed here is that individuals with a history of burns may exhibit a higher prevalence of frailty compared to the general population, and these differences become apparent a few months post-discharge, which is typically when burn survivors are reintegrating into their normal lives. By highlighting the severity of this issue and outlining its impact on quality of life, we aim to identify potential opportunities and pathways for informing clinical practice, future research, and policymaking efforts.
Source of data for burn patients
The burn population was identified from the previously published Randomized Trial of Enteral Glutamine to Minimize the Effects of Burn Injury (RE-ENERGIZE). RE-ENERGIZE was an international, multicenter, double-blinded, randomized-controlled trial that investigated the effects of enteral glutamine supplementation (0.5 g/kg) in severe burn patients. Severe burns were defined as those of partial- or full-thickness that would necessitate surgery [ 12 ]. The data collection period for RE-ENERGIZE spanned 10 years (2011–2021), and the findings were published by Heyland et al. [ 12 ] in 2022. In summary, a total of 1209 patients from 54 burn units across 14 countries were enrolled. The eligible total body surface area (TBSA) burned criteria was: > 20% for individuals aged 18 to 39 years, > 15% within concomitant inhalation injury, > 15% for individuals aged 40 to 59 years, and > 10% for those over age 60. Therefore, patients admitted with severe burns covering an average TBSA burn of 33% underwent randomization. A total of 1200 individuals were included in the final analysis, of which 596 belonged to the glutamine group while 604 were in the placebo group. Since no beneficial effect was observed from glutamine in the original trial, both groups were combined for our burn cohort analysis. The relevant data collected encompassed details about burn centers (such as geographic regions), patient demographics [including sex, age, race/ethnicity, body mass index (BMI), substance use like alcohol or smoking], and injury specifics [such as cause and extent of burn (TBSA)], as well as outcomes [comprising length of stay in the intensive care unit (ICU), length of hospital stay (LOHS), and discharge destination].
Source of normative data
The 2022 National Health Interview Survey (NHIS) served as the primary data source for the general population. Administered by the National Center for Health Statistics through telephone or face-to-face (household) interviews, NHIS collects annual cross-sectional data on the health status of the U.S. population. The dataset employs a multistage probability study design to ensure that the data are representative of both household and non-institutionalized civilian populations in the U.S. Additionally, there is an oversampling of Black, Asian, and Hispanic populations [ 13 ]. Eligible participants include residents living in households or non-institutional settings, including rooming houses, group homes, and homeless shelters.
Data availability and ethical approval
This study is a post hoc analysis of the RE-ENERGIZE (NCT00985205) trial, in which the analyzed data of the burn cohort have been previously published [ 12 ]. The complete dataset is not publicly accessible due to its inclusion of sensitive information that could potentially compromise the privacy of research participants. The RE-ENERGIZE trial protocol was approved by the Research Ethics Committees at Queen’s University, Kingston, Ontario, Canada (Approval No. NCT00985205; https://clinicaltrials.gov/study/NCT00985205 ), and all participating centers and the informed consent form underwent review and approved by the Research Ethics Board (REB approval NO. 6013407). Before randomization, each patient or their designated surrogate provided written informed consent. All documentation regarding the ethical approval can be found in the published protocol [ 14 ]. Data concerning the normative population are openly accessible from the Centers for Disease Control and Prevention National Health Center for Health Statistics at https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm , 2022 NHIS document.
FRAIL (Fatigue, Resistance, Ambulation, Illness, Loss of weight) scale
The FRAIL scale consists of 5 components: fatigue, resistance, ambulation, illness, and loss of weight [ 15 ]. This is a widely used and extensively studied tool with previous research supporting its validity in frailty assessment in various populations, although not specifically in a burn injury cohort [ 16 , 17 , 18 , 19 , 20 ]. On average, 3 to 6 months after hospital discharge, the patients were contacted to complete the 36-Item Short Form Health Survey (SF-36) questionnaire. Fatigue, resistance, and ambulation were determined from responses to the SF-36 or NHIS questionnaires and are indicative of the post-discharge status. Illness indicated the presence of more than 5 of the following conditions: hypertension, diabetes, cancer other than minor skin cancer, chronic lung disease, myocardial infarction, congestive heart failure or coronary artery disease, angina, asthma, arthritis, and stroke. Kidney disease was excluded from the analysis because of missing data in the NHIS. Due to insufficient data in both burn injury and control cohorts, the concept of “loss of weight” was substituted with “malnutrition”, using recognized definitions from the World Health Organization and the European Society for Clinical Nutrition and Metabolism [ 21 ]. Therefore, in terms of time point, the onset of illness and loss of weight occurred at the time of hospital admission, while fatigue, resistance, and ambulation were assessed at 3–6 months after hospital discharge. A score of 0 on the FRAIL scale indicates robustness, a score of 1–2 indicates pre-frailty, and a score of 3–5 indicates frailty. Figure 1 provides an overview of the questions and scoring methodology [ 21 ]. The relationship between TBSA and frailty was investigated by comparing the distribution of TBSA among three groups: robustness ( n = 268), pre-frailty ( n = 254), and frailty ( n = 78).

Components of the FRAIL scale. FRAIL scale is an acronym for fatigue, resistance, ambulation, illness, and loss of weight. Respondents were asked to report their level of tiredness over the past 4 weeks. Those who felt “all of the time” or “most of the time” scored 1 point on the fatigue component. Similarly, respondents were asked to query about any difficulty walking up 10 steps alone without resting or aids. Those answering “Yes” scored 1 point on the resistance component. Additionally, respondents were asked if they had any difficulty walking several hundred yards alone without aids. A positive response also scored 1 point on the ambulation component. Finally, individuals reporting 5 or more out of 11 specified illnesses (hypertension, diabetes, cancer other than minor skin cancer, COPD/chronic lung disease, myocardial infarction, congestive heart failure or coronary artery disease, angina, asthma, arthritis, stroke, and kidney disease), scored 1 point on the illness component. Kidney disease is excluded because of missing data in the NHIS. Due to insufficient data on weight change in both the Randomized Trial of Enteral Glutamine to Minimize the Effects of Burn Injury (RE-ENERGIZE) and National Health Interview Survey (NHIS) cohorts, loss of weight was replaced by malnutrition. Using accepted definitions of malnutrition from the World Health Organization and the European Society for Clinical Nutrition and Metabolism [ 21 ], individuals with a body mass index (BMI) lower than 18.5 kg/m 2 , those aged between 65–70 years with BMI < 20 kg/m 2 , and those aged over 70 years with BMI < 22 kg/m 2 were assigned a score of 1 point on the malnutrition component. Finally, each component on the FRAIL scale contributes 1 point to overall scores ranging from 0–5, where a score of 0 indicates robustness, while scores between 1–2 indicate pre-frailty and scores between 3–5 indicate frailty
The post-discharge independence of burn patients was evaluated through the assessment of their responses to the Katz index of activities of daily living (ADL) [ 22 ] and the Lawton index of instrumental activities of daily living (iADL) [ 23 ] questionnaires, as previously described [ 19 ]. ADL and iADL are two commonly assessed domains on self-reported questionnaires for measuring functional disability [ 24 ], both considered significant predictors of long-term care service use [ 25 ]. ADL includes 4 components (toileting, transferring, continence, and feeding), while iADL comprises 8 components (ability to use a telephone, shopping, food preparation, housekeeping, laundry, mode of transportation, responsibility for own medications, and ability to handle finances). Any response indicating less than complete independence was classified as an ADL limitation. The utilization of both the Katz index for assessing ADL independence and the Lawton index for evaluating iADL has been prevalent in prior research due to its comprehensive insight into an individual’s functional abilities [ 26 , 27 , 28 , 29 , 30 , 31 ]. While, ADL to self-care tasks essential for basic survival and well-being, such as toileting, bathing, eating, and dressing, iADL involves more complex tasks supporting daily life within the home and community. Examples include tasks such as household management, financial administration, telephone usage, grocery procurement, and medication compliance [ 32 ]. The combined iADL and ADL scores were calculated and plotted against the follow-up period. For example, when computing the iADL score, each component was assigned a point score which was then summed to yield an overall score. For instance, the component “Ability to use the telephone” was scored as follows: “Operates telephone on own initiative, looks up and dials numbers” scored 0, “Dials a few well-known numbers” scored 1, “Answers telephone, but does not dial” scored 2, and “Does not use the phone at all” scored 3. Consequently, higher scores indicate greater dependence. ADL and iADL assessments were conducted 2 to 15 months post-hospital discharge.
Statistical analysis
All data from both databases were collected and matched in Microsoft Excel ® 2024 (Microsoft, Redmond, WA, USA). Propensity score matching was performed in R software (version 4.1.2) using the Matchlt package. Each treated unit “burn patient” was paired with two controls “general population” through a nearest-neighbor one-to-two matching technique to enhance study precision as previously described [ 33 ]. Matching variables included age, sex, race/ethnicity, BMI, history of alcohol misuse, and current smoking status. The quality of the matching was visualized with histograms and jitter plots (Additional file 1 : Figs. S1, S2). The resulting matched cohorts were subsequently utilized for assessing frailty by comparing all 5 components of the FRAIL scale. Continuous data (age, BMI) were presented as means and standard deviations (SD) and compared using a Student’s t -test, while categorical data were presented as absolute n (%) and compared using a χ 2 or Fishers exact test, as appropriate. Finally, a multivariable linear regression analysis was performed on the burns cohort to identify factors associated with frailty, compromised ADL, and iADL. Included variables were age, alcohol misuse, smoking, type of burn (scald, chemical, other), BMI, TBSA, LOHS, glutamine administration, sex, and race. All statistical analysis was conducted in GraphPad Prism (version 9) and the data were visualized in GraphPad Prism and Adobe Illustrator. All P -values less than 0.05 were considered significant.
Cohort demographics and characteristics
In the RE-ENERGIZE trial, there were a total of 1200 participants, of whom 600 completed the necessary questionnaires to meet the eligibility criteria for this post-hoc study. The patient recruitment process is detailed in Fig. 2 . Average follow-up time was (5.5 ± 2.3) months post-burn. A total of 1200 adults from the general population were included matched (Table 1 ). The burn population was well-matched to the general population, with both cohorts consisting predominantly of males (> 70.0%) and individuals of White ethnicity (> 70%). The cohorts were similar in terms of age [(48.7 ± 17.1) years vs. (48.3 ± 17.8) years, P = 0.65] and BMI [(28.3 ± 6.0) kg/m 2 vs. (28.0 ± 7.6) kg/m 2 , P = 0.50]. The burn cohort had a higher percentage of Native American subjects (3.0% vs. 1.0%, P = 0.002), while the normative cohort had a higher percentage of Black or African American subjects (6.3% vs. 10.8%, P = 0.002; Table 1 ).

Patient recruitment process. ADL activities of daily living, iADL instrumental activities of daily living, NHIS National Health Interview Survey
Prevalence of frailty
Out of 600 burn patients, there were 268 classified as robustness, while 254 were categorized as pre-frailty, and another 78 as frailty individuals within this cohort group. Additionally, burn patients exhibited a notably lower likelihood of being classified as robustness compared to their counterparts in normative populations (44.7% vs. 79.2%, P < 0.0001), but showed a substantially higher probability of being categorized as pre-frail (42.3% vs. 19.8%, P < 0.0001), or frail individuals (13.0% vs. 1.0%, P < 0.0001; Table 1 ). Furthermore, when examining specific components of the FRAIL scale among these patients with burns, it became evident that they had an increased tendency towards experiencing fatigue (25.8% vs. 13.5%, P < 0.0001), increased resistance (34.0% vs. 2.7%, P < 0.0001), and restricted ambulation (41.8% vs. 3.8%, P < 0.0001). Moreover, the incidence of illness appeared higher in the general population compared to that observed among those with burns (1.2% vs. 2.8%, P = 0.03). However, malnutrition rates did not display significant differences between these two groups (2.3% vs. 2.6%, P = 0.75; Table 1 ). Lastly, an analysis focusing on various comorbidities encompassed within the illness component revealed that individuals from general populations demonstrated a notably greater likelihood of having conditions such as asthma, arthritis, congestive heart failure (CHF) or coronary heart disease (CHD), chronic obstructive pulmonary disease (COPD)/chronic lung disease, hypertension and myocardial infarction ( P < 0.05) whereas those from the burn patient group displayed a markedly elevated probability for cancer other than minor skin cancer and diabetes ( P < 0.01).
TBSA and frailty in the burn population
When examining the relationship between TBSA and frailty, we observed that the majority of robust patients (score 0) had a TBSA ranging from 20 to 29% (102/268; accounting for 38.1% of all robust patients), followed by a TBSA range of 10 to 19% (60/268; representing 22.4% of all robust patients). The overall TBSA range for robust patients was from 10 to 76%. Similarly, most pre-frail patients (score 1–2) exhibited a TBSA between 20 and 29% (87/254; constituting 34.3% of all pre-frail patients), followed by a TBSA between 30 and 39% (58/254; representing 22.8% of all pre-frail patients). The total TBSA range for pre-frail patients was from 10 to 93%. Finally, the majority of frail patients (score 3–5) had a TBSA between 20 and 29% (24/78; accounting for 30.8% of all frail patients), followed by a TBSA ranging from 10 to 19% (17/78; constituting 21.8% of all frail patients). The total TBSA range for frail patients was from 10 to 85% (Fig. 3 a). When considering the entire cohort, most patients exhibited robust and had a TBSA of 20–29% (102/600; 17.0% of all patients), followed by pre-frail patients with a TBSA of 20–29% (87/600; 14.5% of all patients), and then robust patients with a TBSA of 10–19% (60/600; 10.0% of all patients; Fig. 3 b).

Association between TBSA and frailty. a The distribution of TBSA percentages across frailty score groups indicates that the majority of robust, pre-frail, and frail patients had a TBSA between 20 and 29%. As TBSA increases, there is a corresponding increase in the percentage of pre-frail and frail patients. b The distribution of TBSA among the patient cohort is visualized as a percentage. The majority of patients demonstrated robustness with a TBSA of 20–29% (102/600; 17.0% of all patients), followed by pre-frail patients within the same TBSA range (87/600; 14.5% of all patients)
ADL in the burn population
In comparison to robust burn patients, pre-frail burn patients exhibited a significantly higher likelihood of requiring assistance in toileting (11.4% vs. 2.6%, P < 0.0001), transferring (10.6% vs. 0.7%, P < 0.0001), continence (9.1% vs. 1.1%, P < 0.0001), and feeding (6.7% vs. 1.1%, P < 0.0001). Similarly, frail burn patients were notably more likely than robust patients to necessitate assistance in toileting (30.8% vs. 2.6%, P < 0.0001), transferring (28.2% vs. 0.7%, P < 0.0001), continence (20.5% vs. 1.1%, P < 0.0001), and feeding (17.9% vs. 1.1%, P = 0.001; Table 2 ). The distribution of ADL score over follow-up time is depicted in Additional file 1 : Fig. S3.
iADL in the burn population
Compared to robust patients, pre-frail burn patients demonstrated significantly lower levels of independently in using the telephone (87.0% vs. 95.5%, P = 0.002), shopping (48.4% vs. 81.7%, P < 0.0001), meal preparation (53.9% vs. 81.3%, P < 0.0001), housekeeping (37.0% vs. 72.4%, P < 0.0001), laundry (60.6% vs. 81.3%, P < 0.0001), travel (55.1% vs. 82.1%, P < 0.0001), managing their medication (73.2% vs. 92.9%, P < 0.0001), and financial management (69.3% vs. 88.4%, P < 0.0001; Table 2 ).
In comparison to robust patients, frail burn patients showed significantly lower levels of independence in using the telephone (80.8% vs. 95.5%, P < 0.0001), shopping (21.8% vs. 81.7%, P < 0.0001), preparing meals (26.9% vs. 81.3%, P < 0.0001), housekeeping (14.1% vs. 72.4%, P < 0.0001), laundry (33.3% vs. 81.3%, P < 0.0001), travel (34.6% vs. 82.1%, P < 0.0001), managing their medication (51.3% vs. 92.9%, P < 0.0001), and financial management (48.7% vs. 88.4%, P < 0.0001; Table 2 ). The distribution of iADL score against follow-up time is shown in Additional file 1 : Fig. S3.
Factors associated with frailty and limitations in ADL or iADL in the burn cohort
The entire burn cohort was utilized to conduct a multivariable linear regression analysis aimed at identifying risk factors for frailty, as well as limitations in ADL and iADL. The results revealed that age ( P < 0.0001) and smoking ( P = 0.04) were independent risk factors for frailty. Furthermore, the chemical burn was identified as an independent risk factor for ADL limitations ( P = 0.0003), while both chemical burn ( P = 0.01) and scald burn ( P = 0.04) were identified as independent risk factors for iADL limitations. Additionally, individuals of Asian or Pacific Islander race were found to have a protective effect against iADL limitations ( P = 0.01, Table 3 ).
Advancements in both burn care and intensive care have led to decreased mortality rates, with reports showing a survival rate of 96.7% among individuals treated at burn centers across the U.S. [ 1 ]. There has been a notable increase in post-burn morbidity within the expanding community of burn survivors [ 34 , 35 ]. Put differently, as these survivors live longer lives, they are increasingly confronted with enduring consequences from their injuries. Frailty, characterized by diminished physiological reserve and increased susceptibility to stressors, can significantly complicate efforts to manage and rehabilitate these individuals (Additional file 1 : Fig. S4) [ 11 , 36 ]. This underscores the necessity for an enhanced comprehension regarding long-term susceptibility to frailty in this patient population. In the discussion, we leverage findings from this study to propose diverse strategies aimed at mitigating and limiting frailty among burn survivors.
Early recognition and assessment
Our analysis indicates a higher prevalence of frailty in the burn population, approximately 5 months after injury (Fig. 4 ). The components of fatigue, resistance, and ambulation were all significantly more restricted in the burn survivors, while the variables of frailty assessed on hospital admission, that is, illness and malnutrition, were higher or did not differ in the normative population, respectively. This provides evidence that although the patients were not frail upon admission to the hospital, they experienced a significant increase in frailty shortly after discharge. This emphasizes the importance of early recognition and assessment of frailty following a burn injury as a critical component of comprehensive burn care. Importantly, the RE-ENERGIZE data did not include information on the pre-burn frail status of patients. Therefore, an exact inference about which patients became frail after the injury cannot be made.

Long-term trajectory of frailty among burn patients is influenced by targeted intervention. Following burn injuries in the short term, patients may face compromised resistance and ambulation while concurrently experiencing fatigue stemming from various factors such as inadequate pain management leading to disrupted sleep patterns or heightened anxiety and depression related to trauma-induced sequelae. Collectively impacting patient independence including (instrumental) activities of daily living, these challenges encompass essential tasks, such as shopping and cooking, cleaning and managing medications, as well as finances. In the long run, this could result in malnutrition, an increase in chronic illnesses, and a notable elevation across all 5 components measured by the FRAIL score. Hypothetically, prompt long-standing engagement with a multidisciplinary team comprising rehabilitation services, community physicians, nutritionists, pain and mental health specialists, as well as social support, holds promise for mitigating fatigue, resistance compromises, and averting prolonged illness and malnutrition
Interestingly, our multivariable analysis of predisposing factors did not reveal TBSA to have a significant impact on the development of frailty, while age was a predictable predictor. Although there was a slight trend suggesting that patients with higher TBSA were also more likely to have higher FRAIL scores (Fig. 3 ), the multivariate analysis showed no significant correlation between TBSA and frailty. TBSA is one of the most powerful indicators of burn trauma severity and strongly correlates with adverse outcomes and short- and long-term morbidity [ 37 , 38 ]. This finding highlights the multifactorial nature of frailty in general and certainly emphasizes the need for more advanced screening methods that go beyond mere burn size [ 39 , 40 , 41 ].
Multidisciplinary approach
The management of severe burn injuries in general, and frailty in severely burned patients in particular, requires a multidisciplinary team approach involving burn specialists, community physicians, geriatricians, pain management experts, physiotherapists, occupational therapists, mental health professionals, nutritionists, and social workers (Fig. 4 ).
The long-term trajectory of burn survivors is characterized by low resistance and low ambulation which limits patients’ independence, predisposing to illness. At the same time increased fatigue and malnutrition also predispose to illness. A multidisciplinary collaborative effort ensures comprehensive care for addressing the diverse needs of frail patients, including rehabilitation to minimize the loss of ambulation and resistance, medical management to promptly identify and treat illnesses such as cardiovascular compromise and diabetes, nutritional support to prevent malnutrition and thus limit illness, and psychosocial interventions [ 42 ]. By maintaining ambulation and resistance, independence is maximized which in turn limits malnutrition, illness and fatigue. For example, occupational therapy can promote well-being through occupation by enabling burn survivors to engage in meaningful activities of everyday life. Occupational therapy achieves this by collaborating with patients and their community to enhance the survivors’ ability to engage in their chosen or necessary occupation or by modifying their occupation or environment to better support their engagement [ 43 ].
We have identified significant limitations in iADL and ADL among frail burn survivors, which compromise their independence and predispose these patients to further frailty. Approximately 25% of frail burn survivors report being unable to dispense their medication, compared to 1% of robust survivors. This notable limitation may have multiple contributing factors (e.g., disability due to a hand burn, presence of compression garments, and the type and shape of medication bottles), presenting a multidisciplinary challenge for resolution. The inability to adhere to medications could result in untreated illness and consequently increase frailty [ 44 , 45 ]. Addressing this issue may require modified medication bottles, adaptive aids promoting independence, as well as specialized situational training through physiotherapy and occupational therapy. Additionally, social support can enhance adherence and overall well-being. The retrospective nature of this post hoc analysis limited our ability to consider certain variables that may influence our results, such as the body location of the burn injury (e.g., extremities or face), depth of the burn (e.g., second or third degree), setting of the injury (e.g., work-related or home-related), post-discharge care options (e.g., inpatient physiotherapy, outpatient physiotherapy or occupational therapy, treatment by mental health or pain specialists), as well as the socioeconomic status of the patients.
Optimizing nutrition and rehabilitation
Frailty often leads to impaired nutritional status and decreased muscle mass [ 46 , 47 ], which can impede wound healing and functional recovery in burn patients [ 48 , 49 ]. Our multivariable analysis revealed no association between glutamine administration and the extent of frailty, ADL, and iADL. Similarly, previous literature on amino acid supplementation in the treatment of sarcopenia and frailty has yielded conflicting results [ 50 , 51 , 52 ]. Although hydroxyl-methyl butyrate has been reported to enhance muscle protein synthesis when combined with arginine and glutamine, glutamine alone has not been shown to prevent muscle deterioration [ 53 ]. Following a burn injury, the body’s energy and nutrient demand increase dramatically to support tissue repair and wound healing [ 5 ]. During the acute phase, adequate nutrition, including sufficient calories, protein, vitamins, and minerals, is crucial for facilitating the regeneration of damaged tissues, while minimizing complications such as infections, and promoting faster wound closure [ 54 ]. Preventing malnutrition during this high-demand period can reduce the risk of long-term frailty associated with prolonged healing and impaired tissue integrity [ 55 ]. In the medium- and long-term, severe burn injuries result in muscle wasting and loss of lean body mass due to increased protein breakdown and decreased protein synthesis [ 56 ].
In turn, a significant reduction in muscle mass and strength can severely impact the activity and energy levels of burn survivors. They often experience chronic fatigue, decreased stamina, and overall weakness, making it challenging to perform even basic ADLs such as dressing and bathing [ 57 ]. Our findings indicated that frailer burn survivors are more likely to require assistance with feeding, rely on parenteral feeding, and need help with shopping. More than 40% of frail burn survivors required their meals to be prepared and served compared to only 3% of robust survivors. Furthermore, diminished energy and physical capacity compromise the ability to participate in social and recreational activities, further affecting the quality of life [ 58 ]. As a result, survivors may increasingly depend on caregivers or adaptive aids, impacting their sense of independence and self-esteem. Additionally, the combination of physical limitations and increased dependency can contribute to a cycle of reduced physical activity, further exacerbating muscle wasting and frailty. Optimal nutrition, particularly high-quality protein intake, is crucial for preserving muscle mass, strength, and function, which are essential for mobility, independence, and overall resilience against frailty (Additional file 1 : Fig. S4) [ 59 ]. Adequate nutrition is essential for providing the energy required for daily activities, rehabilitation, and physical therapy. It plays a crucial role in maintaining muscle strength, endurance, and functional independence. These factors are fundamental prerequisites for implementing a comprehensive rehabilitation program that includes nutritional support, physical therapy, and occupational therapy to help mitigate these effects [ 58 ]. Such programs aim to restore muscle mass, improve energy levels, and enhance the individual’s ability to participate in ADL, ultimately promoting greater independence and quality of life.
Long-term follow-up and care
Burn patients are at increased risk of experiencing long-term complications, such as chronic pain, functional impairment, and recurrent hospitalizations, which have been shown to contribute to frailty (Additional file 1 : Fig. S4) [ 8 , 35 , 39 ]. In a recent post hoc analysis of the same burn cohort, our research team identified a strong correlation between chronic pain, anxiety, and depression in these patients [ 60 ]. Previous research has also established a significant link between poor mental health and long-term frailty [ 61 ]. This highlights the necessity for comprehensive care that integrates both mental health support and physical rehabilitation to optimize the long-term outcomes of burn survivors. Establishing structured long-term follow-up programs is essential for monitoring progress, addressing ongoing needs, and preventing future frailty-related events. Losing track of burn patients during follow-up poses a significant concern both clinically and scientifically: comparison of the burn patients who were “lost to follow-up” with those included as responders revealed notable differences in baseline characteristics. Non-responders were on average younger, more likely to be smokers, less likely to be Hispanic but more likely to be African American. They were also more likely to have had inhalation injury or been transferred to another hospital ward with shorter hospital and ICU stays. This inherent limitation present in all prospective research regarding short- and long-term burn survivors emphasizes the importance of standardized 6-month follow-ups that extend beyond evaluating the need for secondary reconstructive procedures.
Although early detection of frailty and ADL deficiencies has been established, little information exists regarding their longitudinal progression. It is essential to collect outcome measures over time [ 62 , 63 ], and implement extended, standardized, and interdisciplinary long-term protocols. A recent meta-analysis found that follow-up for burn patients seldom extends 5 years post-injury, which is considered long term [ 39 ]. Currently, all specialized follow-up care for burn survivors is exclusively provided by surgical institutions involved in secondary reconstruction. After achieving satisfactory reconstruction and reaching an acceptable level of scarring control, pain management effectiveness, and functional capability improvement, patient monitoring becomes sporadic or ceases altogether. There remains a lack of comprehensive protocols for diagnosing and treating long-term organ damage across disciplines while assessing their respective contributions to complex phenomena such as frailty. It is essential to identify long-term complications that may appear unrelated but are linked with an increased risk of developing diabetes and cardiovascular disease over decades. The establishment of a standardized interdisciplinary system for monitoring burn patients in the long term is crucial. This system could involve lifelong, follow-up appointments every 5 years similar to those offered for cancer patients after hospital discharge. To validate our preliminary findings comprehensively and ensure their applicability across different contexts, independent studies or datasets should confirm them. Conducting a prospective study comparing frailty levels upon admission with those at early (within months) and long-term (after years) post-discharge intervals, while examining diverse post-discharge care options like physiotherapy or occupational therapy would significantly enhance our understanding of chronic burn injury effects.
Limitations
The response data are based on self-reporting, which is inherently susceptible to inaccuracies. Due to differences in the questionnaire protocols of the two databases (RE-ENERGIZE and NHIS), certain questions and response options were adjusted to achieve consensus. Although the RE-ENERGIZE data spans 6 years (2016–2021), we chose to utilize only the 2022 NHIS data as it provided all the necessary frailty assessment information due to its rotating design. The use of a general population database and propensity score matching helps to minimize this limitation. Another limitation of our study is that while the NHIS data is US-centric, the RE-ENERGIZE data collection was international, with the majority of patients based in North America. Given that only a limited subset of both populations was sampled, generalizability poses a concern. The extent to which our results can be applied to other populations and settings, particularly low- and middle-income countries, remains uncertain. Baseline differences in co-morbidities were observed between the two groups. The existing literature on illness present on admission following an acute burn is limited and inconclusive [ 64 , 65 ]. Therefore, further research is necessary to determine whether there are genuine disparities in the baseline health of acute burn injury patients compared to the general population. The specific body location is particularly relevant, as injuries to the head and neck, as well as upper and lower extremities, are associated with higher levels of disability and would consequently be linked with elevated FRAIL scores [ 66 ]. Although data on the exact depth of the burns were not provided, all eligible patients for the trial had partial- or full-thickness burns requiring surgery. Generalizability may also pose a concern since only a restricted subset of both populations was sampled. The burn cohort analyzed in this study was defined post hoc and had not been considered in the original power calculation of the sample size. Therefore, it has been previously proposed that statistical hypotheses from post hoc analyses are inherently regarded as exploratory only [ 67 ]. Finally, due to the cross-sectional design of the study, making causal inferences is precluded.
In this study, we conducted an analysis of one of the largest multicenter cohorts of patients with extensive burns to determine the prevalence of frailty in such patients’ months after injury, comparing it to a non-burned general population. Patients with a history of burns exhibit a higher prevalence of frailty compared to the general population group, and these differences are apparent a few months post-discharge, which is typically when burn survivors return to their normal lives. Additionally, we investigated the interrelationship between the presence of frailty and compromise in (instrumental) ADL. By establishing the severity of the issue and describing its impact on quality of life, we aim to identify potential opportunities and avenues for guiding clinical practice, future research, and policymaking efforts.
Data availability
Datasets generated and analyzed to provide the findings in this study are available from the corresponding author upon reasonable request.
Abbreviations
- Activities of daily living
Body mass index
Congestive heart failure/coronary heart disease
Chronic obstructive pulmonary disease
Fatigue, Resistance, Ambulation, Illness, Loss of weight
Instrumental activities of daily living
Intensive care unit
Length of hospital stay
National Health Interview Survey
Randomized Trial of Enteral Glutamine to Minimize the Effects of Burn Injury
36-Item Short Form Health Survey questionnaire
Total body surface area
James SL, Lucchesi LR, Bisignano C, Castle CD, Dingels ZV, Fox JT, et al. Epidemiology of injuries from fire, heat and hot substances: global, regional and national morbidity and mortality estimates from the global burden of Disease 2017 study. Inj Prev. 2020;26(Supp 1):i36–45.
Article PubMed Google Scholar
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–62.
Shafiee A, Arabzadeh Bahri R, Rajai S, Ahoopai M, Seighali N, Amini MJ. Frailty as a predictor of adverse outcomes in burn patients: a systematic review. BMC Geriatr. 2023;23(1):680.
Article PubMed PubMed Central Google Scholar
Pereira C, Murphy K, Jeschke M, Herndon DN. Post burn muscle wasting and the effects of treatments. Int J Biochem Cell Biol. 2005;37(10):1948–61.
Article CAS PubMed Google Scholar
Clark A, Imran J, Madni T, Wolf SE. Nutrition and metabolism in burn patients. Burns Trauma. 2017;5:11.
Dauber A, Osgood PF, Breslau AJ, Vernon HL, Carr DB. Chronic persistent pain after severe burns: a survey of 358 burn survivors. Pain Med. 2002;3(1):6–17.
Duke J, Rea S, Semmens J, Edgar DW, Wood F. Burn and cancer risk: a state-wide longitudinal analysis. Burns. 2012;38(3):340–7.
Barrett LW, Fear VS, Waithman JC, Wood FM, Fear MW. Understanding acute burn injury as a chronic disease. Burns Trauma. 2019;7:23.
Pompermaier L, Steinvall I, Elmasry M, Eladany MM, Abdelrahman I, Fredrikson M, et al. Long-term mortality after self-inflicted burns. Burns. 2024;50(1):252–61.
Pompermaier L, Steinvall I, Fredrikson M, Thorfinn J, Sjöberg F. Long-term survival after burns in a Swedish population. Burns. 2017;43(1):157–61.
Panayi AC, Herndon DN, Branski L, Sjöberg F, Hundeshagen G. Bridging frailty and burns: defining acute burn injury as a cause of long-term frailty. Maturitas. 2024;187:108061.
Heyland DK, Wibbenmeyer L, Pollack J, Friedman B, Turgeon AF, Eshraghi N, et al. A randomized trial of enteral glutamine for treatment of burn injuries. N Engl J Med. 2022;387(11):1001–10.
Institute of Medicine (US). Committee on a National Surveillance System for Cardiovascular and Select Chronic diseases. A nationwide framework for surveillance of cardiovascular and chronic lung diseases. Washington (DC): National Academies Press (US); 2011.
Google Scholar
Heyland DK, Wischmeyer P, Jeschke MG, Wibbenmeyer L, Turgeon AF, Stelfox HT, et al. A RandomizEd trial of ENtERal glutamine to minimIZE thermal injury (the RE-ENERGIZE trial): a clinical trial protocol. Scars Burn Heal. 2017;3:2059513117745241.
PubMed PubMed Central Google Scholar
van Abellan G, Rolland YM, Morley JE, Vellas B. Frailty: toward a clinical definition. J Am Med Dir Assoc. 2008;9(2):71–2.
Article Google Scholar
Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14(6):392–7.
Hyde Z, Flicker L, Almeida OP, Hankey GJ, McCaul KA, Chubb SA, et al. Low free testosterone predicts frailty in older men: the health in men study. J Clin Endocrinol Metab. 2010;95(7):3165–72.
Lopez D, Flicker L, Dobson A. Validation of the frail scale in a cohort of older Australian women. J Am Geriatr Soc. 2012;60(1):171–3.
Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African americans. J Nutr Health Aging. 2012;16(7):601–8.
Article CAS PubMed PubMed Central Google Scholar
Woo J, Leung J, Morley JE. Comparison of frailty indicators based on clinical phenotype and the multiple deficit approach in predicting mortality and physical limitation. J Am Geriatr Soc. 2012;60(8):1478–86.
Wolters M, Volkert D, Streicher M, Kiesswetter E, Torbahn G, O’Connor EM, et al. Prevalence of malnutrition using harmonized definitions in older adults from different settings - a MaNuEL study. Clin Nutr. 2019;38(5):2389–98.
Shelkey M, Wallace M. Katz index of independence in activities of daily living (ADL). Director. 2000;8(2):72–3.
CAS PubMed Google Scholar
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–86.
Yang M, Ding X, Dong B. The measurement of disability in the elderly: a systematic review of self-reported questionnaires. J Am Med Dir Assoc. 2014;15(2):e1501–9.
Palmer M, Harley D. Models and measurement in disability: an international review. Health Policy Plan. 2012;27(5):357–64.
Ren C, Hao X, Chen X, Liu X. Loneliness, functional disability and lower urinary tract symptoms suggestive of benign prostatic hyperplasia in aging men: insights from the China health and retirement longitudinal study. Geriatr Nurs. 2024;58:304–9.
Pinto JO, Pontes D, Dores AR, Peixoto B, Barbosa F. Activities of daily living inventory (ADLI): proposal of a new instrument and preliminary data. Appl Neuropsychol Adult. 2024:1–18.
Ren Z, Nie L, Du Y, Zhou T, Sun J, Liu J. Joint daily functional trajectory and risk of new-onset Alzheimer’s disease and related dementias in older adults with normal and abnormal weight. J Affect Disord. 2024;358:157–62.
Huang MH, Tsai CF, Lin YS, Kuo YS, Hsu CC, Fuh JL. A national survey on health-related quality of life for people with dementia in residential long-term care institutions. J Formos Med Assoc. 2024;123(7):764–72.
Flanagan KD, Cornell DJ, Mangano KM, Zhang X, Tucker KL, Noel SE. Adherence to mediterranean, dietary approaches to stop hypertension and healthy eating indices are associated with lower risk of disability among Puerto Rican adults from the longitudinal Boston Puerto Rican Health study. Am J Clin Nutr. 2024:S0002-9165(24)00528-8.
Woldemariam S, Stein VK, Haider S, Dorner TE. Trends over time in the deficit of (instrumental) activities of daily living in the Austrian population aged 65 years and older: results from the Austrian health interview Survey series. Wien Klin Wochenschr. 2024. https://doi.org/10.1007/s00508-024-02388-4 .
Pashmdarfard M, Azad A. Assessment tools to evaluate activities of daily living (ADL) and instrumental activities of daily living (IADL) in older adults: a systematic review. Med J Islam Repub Iran. 2020;34:33.
Rassen JA, Shelat AA, Myers J, Glynn RJ, Rothman KJ, Schneeweiss S. One-to-many propensity score matching in cohort studies. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 2):69–80.
Jeschke MG, van Baar ME, Choudhry MA, Chung KK, Gibran NS, Logsetty S. Burn injury. Nat Rev Dis Primers. 2020;6(1):11.
Haug VF, Tapking C, Panayi AC, Thiele P, Wang AT, Obed D, et al. Long-term sequelae of critical illness in sepsis, trauma and burns: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2021;91(4):736–47.
Goede V, Neuendorff NR, Schulz RJ, Hormigo AI, Martinez-Peromingo FJ, Cordoba R. Frailty assessment in the care of older people with haematological malignancies. Lancet Healthy Longev. 2021;2(11):e736–45.
Bourgi J, Sleiman Z, Fazaa E, Maasarani D, Chahine Y, Nassif E, et al. Predictors of generic and burn-specific quality of life among adult burn patients admitted to a Lebanese burn care center: a cross-sectional single-center study. Int J Burns Trauma. 2020;10(3):81–9.
Jafaryparvar Z, Adib M, Ghanbari A, Ali Yazdanipour M. Predictors of short-term outcomes of burn in a newly established burn centre in Iran. Nurs Open. 2021;8(6):2986–95.
Hundeshagen G, Herndon DN, Clayton RP, Wurzer P, McQuitty A, Jennings K, et al. Long-term effect of critical illness after severe paediatric burn injury on cardiac function in adolescent survivors: an observational study. Lancet Child Adolesc Health. 2017;1(4):293–301.
Hussain A, Dunn KW. Predicting length of stay in thermal burns: a systematic review of prognostic factors. Burns. 2013;39(7):1331–40.
Pompermaier L, Steinvall I, Fredrikson M, Sjöberg F. Inclusion of coexisting morbidity in a TBSA% and age based model for the prediction of mortality after burns does not increase its predictive power. Burns. 2015;41(8):1868–76.
Karam E, Lévesque MC, Jacquemin G, Delure A, Robidoux I, Laramée MT, et al. Building a multidisciplinary team for burn treatment - lessons learned from the Montreal tendon transfer experience. Ann Burns Fire Disasters. 2014;27(1):3–7.
CAS PubMed PubMed Central Google Scholar
World Federation of Occupational Therapists. World federation of occupational therapists’ position statement on telehealth. Int J Telerehabil. 2014;6(1):37–9.
Article PubMed Central Google Scholar
Lemay J, Waheedi M, Al-Sharqawi S, Bayoud T. Medication adherence in chronic illness: do beliefs about medications play a role? Patient Prefer Adherence. 2018;12:1687–98.
Kvarnström K, Westerholm A, Airaksinen M, Liira H. Factors contributing to medication adherence in patients with a chronic condition: a scoping review of qualitative research. Pharmaceutics. 2021;13(7):1100.
Lang PO, Michel JP, Zekry D. Frailty syndrome: a transitional state in a dynamic process. Gerontology. 2009;55(5):539–49.
Bales CW, Ritchie CS. Sarcopenia, weight loss, and nutritional frailty in the elderly. Annu Rev Nutr. 2002;22:309–23.
Price C. Nutrition: reducing the hypermetabolic response to thermal injury. Br J Nurs. 2018;27(12):661–70.
Adjepong M, Agbenorku P, Brown P, Oduro I. The role of antioxidant micronutrients in the rate of recovery of burn patients: a systematic review. Burns Trauma. 2016;4:18.
Haba Y, Fujimura T, Oyama K, Kinoshita J, Miyashita T, Fushida S, et al. Effect of oral branched-chain amino acids and glutamine supplementation on skeletal muscle atrophy after total gastrectomy in rat model. J Surg Res. 2019;243:281–8.
Mignon M, Lêvêque L, Bonnel E, Meynial-Denis D. Does glutamine supplementation decrease the response of muscle glutamine synthesis to fasting in muscle in adult and very old rats? JPEN J Parenter Enter Nutr. 2007;31(1):26–31.
Article CAS Google Scholar
Meynial-Denis D. Glutamine metabolism in advanced age. Nutr Rev. 2016;74(4):225–36.
Maykish A, Sikalidis AK. Utilization of hydroxyl-methyl butyrate, leucine, glutamine and arginine supplementation in nutritional management of Sarcopenia-implications and clinical considerations for type 2 diabetes mellitus risk modulation. J Pers Med. 2020;10(1):19.
Smith-Ryan AE, Hirsch KR, Saylor HE, Gould LM, Blue MNM. Nutritional considerations and strategies to facilitate injury recovery and rehabilitation. J Athl Train. 2020;55(9):918–30.
Volkert D, Beck AM, Cederholm T, Cereda E, Cruz-Jentoft A, Goisser S, et al. Management of malnutrition in older patients-current approaches, evidence and open questions. J Clin Med. 2019;8(7):974.
Dombrecht D, Van Daele U, Van Asbroeck B, Schieffelers D, Guns PJ, Gebruers N, et al. Molecular mechanisms of post-burn muscle wasting and the therapeutic potential of physical exercise. J Cachexia Sarcopenia Muscle. 2023;14(2):758–70.
Evans WJ. Skeletal muscle loss: cachexia, Sarcopenia, and inactivity. Am J Clin Nutr. 2010;91(4):S1123–7.
Rivas E, Tran J, Gutierrez IL, Chapa M, Herndon DN, Suman OE. Rehabilitation exercise increases physical activity levels in severely burned children while improving aerobic exercise capacity and strength. J Burn Care Res. 2018;39(6):881–6.
Disseldorp LM, Nieuwenhuis MK, Van Baar ME, Mouton LJ. Physical fitness in people after burn injury: a systematic review. Arch Phys Med Rehabil. 2011;92(9):1501–10.
Panayi AC, Heyland DK, Stoppe C, Jeschke MG, Didzun O, Matar D, et al. The long-term intercorrelation between post-burn pain, anxiety, and depression: a post hoc analysis of the RE-ENERGIZE double-blind, randomized, multicenter placebo-controlled trial. Crit Care. 2024;28(1):95.
Mutz J, Choudhury U, Zhao J, Dregan A. Frailty in individuals with depression, bipolar disorder and anxiety disorders: longitudinal analyses of all-cause mortality. BMC Med. 2022;20(1):274.
Meuli JN, Pantet O, Berger MM, Waselle L, Raffoul W. Massive burns: retrospective analysis of changes in outcomes indicators across 18 years. J Burn Care Res. 2022;43(1):232–9.
Gong J, Singer Y, Cleland H, Wood F, Cameron P, Tracy LM, et al. Driving improved burns care and patient outcomes through clinical registry data: a review of quality indicators in the Burns Registry of Australia and New Zealand. Burns. 2021;47(1):14–24.
Salehi SH, As’adi K, Abbaszadeh-Kasbi A. The prevalence of comorbidities among acute burn patients. Trauma. 2019;21(2):134–40.
Aggarwal A, Chittoria RK, Chavan VK, Gupta S, Reddy CL, PMohan PB, et al. The role of comorbidieites in the prognosis of thermal burns. Indian J Burn. 2019;27:16–9.
McAleavey AA, Wyka K, Peskin M, Difede J. Physical, functional, and psychosocial recovery from burn injury are related and their relationship changes over time: a burn Model System study. Burns. 2018;44(4):793–9.
Günter CI, Ilg FP, Hapfelmeier A, Egert-Schwender S, Jelkmann W, Giri S, et al. Relation between gender and concomitant medications with erythropoietin-treatment on wound healing in burn patients. Post hoc subgroup-analysis of the randomized, placebo-controlled clinical trial EPO in burns. Front Pharmacol. 2022;13:812888.
Download references
Acknowledgements
This work was supported by the U.S. Department of Defense (W81XWH-09-2-0194 for the pilot phase), and the Canadian Institutes of Health Research (MCT-94834 for the pilot phase and 14238 for the definitive phase).
Author information
Authors and affiliations.
Department of Hand, Plastic and Reconstructive Surgery, Burn Center, BG Trauma Center Ludwigshafen, University of Heidelberg, 67071, Ludwigshafen, Germany
Adriana C. Panayi, Christian Tapking, Oliver Didzun, Amir K. Bigdeli, Ulrich Kneser & Gabriel Hundeshagen
Clinical Evaluation Research Unit, Department of Critical Care Medicine, Queen’s University, Kingston, ON, K7L 3N6, Canada
Daren K. Heyland
Department of Anaesthesiology, Intensive Care, Emergency and Pain Medicine, University Hospital Würzburg, 97080, Würzburg, Germany
Christian Stoppe
Department of Cardiac Anesthesiology and Intensive Care Medicine, Charité Berlin, 10117, Berlin, Germany
Hamilton Health Sciences Research, Department of Surgery, McMaster University, Hamilton, ON, L8S 4L8, Canada
Marc G. Jeschke
Division of Plastic Surgery, Department of Surgery, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, 02115, USA
Samuel Knoedler & Dennis P. Orgill
Burns Center and Plastic Surgery, Unfallkrankenhaus Berlin, 12683, Berlin, Germany
Valentin Haug
You can also search for this author in PubMed Google Scholar
Contributions
ACP was involved in the conceptualization of the study, data collection, methodology, statistical analysis, data visualization, and writing of the original draft. DKH, CS, and MGJ were involved in the data collection and the review and editing of the manuscript. SK was involved in the methodology, statistical analysis, and the review and editing of the manuscript. CT was involved in the writing of the original draft. OD, VH, AKB, and UK were involved in the review and editing of the manuscript. DPO was involved in the methodology and the review and editing of the manuscript. GH was involved in the conceptualization of the study, data collection, methodology, and writing of the original draft.
Corresponding author
Correspondence to Gabriel Hundeshagen .
Ethics declarations
Ethics approval and consent to participate.
The protocol for the RE-ENERGIZE trial was approved by the Ethics Committees at Queen’s University, Kingston, Ontario, Canada (Approval number: NCT00985205; https://clinicaltrials.gov/study/NCT00985205 ) and at all other participating centers. The entities that provided support, financial or product, had no role in the protocol design, conduct of the trial, or data analysis. The also did not have access to the data or manuscript prior to publication. Written informed consent was obtained from each subject or a designated surrogate prior to randomization.
Consent for publication
No applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: fig. s1.
Quality of matching visualized as a histogram. Fig. S2 Quality of matching visualized as a jitter plot. Fig. S3 ADL and iADL scores assessed over the follow-up period in months. Fig. S4 Theoretic schematic depicting the potential impact of frailty on patients with a history of burn injury.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Panayi, A.C., Heyland, D.K., Stoppe, C. et al. Frailty as a sequela of burn injury: a post hoc analysis of the “RE-ENERGIZE” multicenter randomized-controlled trial and the National Health Interview Survey. Military Med Res 11 , 63 (2024). https://doi.org/10.1186/s40779-024-00568-x
Download citation
Received : 20 April 2024
Accepted : 19 August 2024
Published : 12 September 2024
DOI : https://doi.org/10.1186/s40779-024-00568-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Burn injury
- Quality of life
Military Medical Research
ISSN: 2054-9369
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Iowa Reading Research Center

Research Article of the Month: September 2024
This blog post is part of our Research Article of the Month series. For this month, we highlight “ Universal Screening in Grades K–2: A Systematic Review and Meta-Analysis of Early Reading Curriculum-Based Measures ,” an article published in the Journal of School Psychology in 2020. Important words related to research are bolded, and definitions of these terms are included at the end of the article in the “Terms to Know” section.
Why Did We Pick This Paper?
A universal screener is a tool teachers use to identify students who may be at risk for literacy difficulties. It is an assessment given to all students several times a year to identify which students are below, at, or above a certain benchmark at a specific point in time. Screening helps teachers identify students who could benefit from additional support or accelerated instruction. It is especially important in early elementary grades so potential difficulties with reading can be identified and addressed as early as possible.
One kind of assessment used for universal screening is a curriculum-based measure (CBM). CBMs are short, timed assessments that track an individual student’s progress toward a learning goal. Some CBMs measure a specific skill associated with reading ability, such as word identification or letter-sound knowledge. For example, a CBM that assesses letter-sound knowledge might require a student to produce the sounds associated with each letter from a list.
Given the prevalence of CBM assessments in universal screening, it is important to understand the validity of these assessments—the extent to which these assessments measure the skill they are designed to measure. This includes concurrent validity (the extent to which student performance on one assessment is confirmed by their performance on another assessment designed to measure the same skill) and predictive validity (the extent to which student performance on one assessment predicts their performance on another assessment administered at a later time). Understanding the validity of CBMs can help educators select universal screening measures that accurately identify students who would benefit from additional support in reading.
What Are the Research Questions or Purpose?
The researchers aim to evaluate the validity of early reading CBMs administered in Grades K – 2. The purposes of the study are as follows:
- Measure concurrent and predictive validity of early reading CBMs with other measures of reading outcomes.
- Determine whether administration lag (the time lapse between the administration of the CBM and the administration of another assessment of student reading outcomes) affected the relationship between students’ performance on the CBM and another outcome measure.
Note: The authors also intended to assess the classification accuracy of CBMs, but the majority of articles in this meta-analysis did not report the data necessary for this analysis, so the authors were unable to address this purpose of the study. To learn more about the classification accuracy of screeners, read our January 2024 Research Article of the Month .
What Methodology Do the Authors Employ?
The authors conducted a meta-analysis of 54 empirical studies that examined the relationship between early reading CBMs and other measures of reading outcomes. To be included in the analysis, the studies needed to:
- Include an early reading CBM assessment as a predictor of a reading outcome
- Focus on students in Grades K–2
- Report correlation coefficients or the figures necessary to calculate them
- Specify the timeframe in which the measures were administered
- Occur in a general education classroom
- Be published in English
For each of the included studies, researchers examined the students’ performance on a CBM and another student reading outcome measure (e.g., broad reading achievement, reading comprehension and vocabulary, language and listening, oral reading, phonics, or phonological and phonemic awareness).
Researchers also took into account other variables in the studies that could affect students’ reading outcomes. These variables included:
- Race and ethnicity
- Language status
- Free and reduced lunch status
- Special education status
- Publisher (FastBridge, DIBELS, easyCBM, aimsweb)
- Measure type (onset sounds, letter names, phoneme segmentation, word identification, nonsense words)
- Screening seasons (fall, winter, spring)
- Reading outcome measure (broad reading achievement, reading comprehension and vocabulary, language and listening, oral reading, phonics, phonological and phonemic awareness)
- Administration lag in months
The researchers conducted separate random effects models for concurrent and predictive validity to estimate the correlation between early reading CBMs and other reading outcome measures. The researchers calculated the correlation coefficients for each reading outcome separately, when possible. However, when there were insufficient data to support this kind of analysis, the outcome measures were aggregated to ensure more reliable results.
For the purposes of this study, correlation coefficients were classified as concurrent when the reading outcome measure was administered less than a month after the CBM, and as predictive when the reading outcome measure was administered a month or more after the CBM. The researchers examined the extent to which this administration lag moderated the correlation between early reading CBMs and other reading outcome measures.
What Are the Key Findings?
Alphabet knowledge.
In the studies included in this meta-analysis, there were two early reading CBMs that measured alphabet knowledge: letter sounds and letter naming. These CBMs were only administered in kindergarten and first grade. There was a large concurrent correlation (r = 0.552) between the letter sounds CBM and the composite outcome measure, consisting of phonics, oral reading, and broad reading. Similarly, there was a large concurrent correlation (r = 0.571) between the letter naming CBM and the aggregated outcome measure, consisting of phonics, broad reading, and oral reading. Concerning the abilities of these CBMs to predict students’ future performance, the letter sounds CBM had a large predictive association (r = 0.56) with complex reading skills (a composite of phonics, comprehension, and broad reading outcomes). Similarly, the predictive association between the letter naming CBM and other reading outcomes was also large, ranging from 0.52 for broad reading to 0.64 for oral reading. However, the predictive ability of the letter naming CBM was moderated by administration lag. For every month increase in the lag between the administration of the letter naming CBM and the administration of the outcome measure, the correlation coefficient decreased by 0.01. In other words, the more time that passes between the administration of both assessments, the less accurately the letter naming CBM predicts a student’s later performance.
Phoneme Awareness
In the studies included in this meta-analysis, there were two early reading CBMs that measured phonemic awareness: onset sounds and phoneme segmenting. Onset sounds was only administered in kindergarten, whereas phoneme segmenting was administered in both kindergarten and first grade. The correlation coefficients of these CBMs were smaller than those of the alphabet knowledge CBMs. The onset sounds CBM had a medium concurrent correlation (r = 0.43) with more complex reading skills. Similarly, the phoneme segmenting CBM had a medium concurrent correlation with both phonics and phonological awareness (r = 0.43) and complex reading skills (r = 0.34). Concerning the predictive abilities of these CBMs, there was a medium predictive correlation (r = 0.424) between the onset sounds CBM and the aggregated outcome measure, consisting of phonics, oral reading, broad reading, and comprehension. Similarly, there was a medium predictive correlation between the phoneme-segmenting CBM and the other outcome measures, ranging from 0.350 for oral reading to 0.376 for phonics. These predictive correlations were not moderated by administration lag.
Two CBMs in the studies included in this meta-analysis measured decoding skills: nonsense words and word identification. The nonsense words CBM was administered across Grades K–2, whereas the word identification CBM was administered primarily in first grade. Concurrent associations between the nonsense words CBM and other reading skills were large, ranging from 0.60 for broad reading ability to 0.75 for oral reading. Similarly, the word identification CBM had a large concurrent association with complex reading skills (r = 0.70). Concerning the ability of these CBMs to predict students’ later performance, the nonsense words CBM had large predictive correlations with outcome measures, ranging from 0.52 for oral reading to 0.68 for broad reading. However, administration lag was a significant moderator for the nonsense words CBM. Predictive correlations between the word identification CBM and other reading outcomes were also large, ranging from 0.71 for broad reading and comprehension to 0.83 for oral reading. In contrast to the nonsense words CBM, administration lag was not significant for the word identification CBM.
What Are the Practical Applications of Key Findings?
The study explores the validity of early reading CBMs in identifying at-risk students in Grades K–2. One of the key findings is that CBMs can reliably predict later reading outcomes, particularly for skills including phonics, oral reading, and letter naming. Practically, these findings underscore the importance of timely and frequent assessments to accurately predict students’ later performance and shed light on their reading development. For teachers, this suggests that using CBMs frequently, such as multiple times per school year, can help them identify students who could benefit from additional support or early intervention. Additionally, schools can choose CBM tools that align closely with their instructional goals and refine their universal screening processes to identify early signs of potential reading difficulties. For example, if the goal is to predict decoding skills, CBMs that assess nonsense words and word identification have demonstrated strong predictive validity. These CBMs could support data-based decisions in the classroom and help ensure that students receive appropriate support in the early stages of reading development.
What Are the Limitations of This Paper?
Due to the lack of data reported in the included studies, the researchers were unable to explore how student demographic factors, such as race and ethnicity, socioeconomic background, or English Learner status might have influenced the findings. Thus, it is unclear whether CBMs perform comparably well for all student groups. Furthermore, it is difficult to know if these assessments might have different levels of accuracy or predictive validity for students from diverse backgrounds. Further research on these demographic factors would benefit educators and schools to ensure that CBMs are equitable and effective for all learners. Additionally, the study showed large variability, or heterogeneity, between the included studies, in terms of the sample sizes, regions, and specific CBM tools used. While a robust variance estimation method was used to account for this, the variability in how and when CBMs were administered across different contexts could affect the generalizability of the results.
Terms to Know
- Validity: Validity refers to the extent to which an assessment measures what it was designed to measure.
- Concurrent validity: Concurrent validity is the extent to which one measurement is confirmed by another measurement administered at roughly the same time.
- Predictive validity: Predictive validity is the extent to which a student’s performance on one measure predicts their performance on another measure later. For example, if a student’s score on a nonsense word reading assessment predicts their later performance on a standardized state assessment, this nonsense word reading assessment would have predictive validity.
- Classification accuracy: Classification accuracy refers to the extent to which one measure (e.g., a universal screener) accurately identifies students as “at risk” or “not at risk” based on their performance on another measure (e.g., a standardized state assessment). An assessment with high classification accuracy minimizes false positives (i.e., proficient readers who are incorrectly identified as at risk) and false negatives (at-risk students who are incorrectly identified as proficient readers). Using screeners with high classification accuracy is important to ensure that time and resources are allocated efficiently and that students receive the appropriate level of support in reading.
- Empirical: Empirical research is a way of gaining knowledge through observation or experience. Empirical research contrasts with theoretical research, which relies on systems of logic, beliefs, and assumptions.
- Predictor: A predictor variable, is a factor that influences another variable in a correlational study. For example, the length of a reading intervention in total minutes (predictor variable) may forecast a student’s composite reading score.
- Correlation coefficient: A correlation coefficient is a measure of the strength of the relationship between two variables. A correlation between variables means that when one variable changes, another variable also changes in a specific direction. For example, if the length of intervention and reading comprehension are correlated, then when the length of reading intervention increases, student reading comprehension will also increase. A common correlation coefficient is Pearson’s correlation coefficient, which is represented by r. Pearson’s correlation coefficient ranges from -1 to 1. Negative values indicate a negative correlation between variables (as one variable changes, the other variable changes in the opposite direction); positive values indicate a positive correlation (as one variable changes, the other variable changes in the same direction). The absolute value, or distance from zero, indicates the strength of the relationship between the variables. A correlation coefficient of ±0.2 is generally considered a small correlation, ±0.3 a medium correlation, and ±0.5 a large correlation (Cohen, 2013).
- Random effects model: A random effects model is a type of statistical model that measures how an independent variable affects a dependent variable across a number of different samples or studies. Unlike a fixed effects model, a random effects model accounts for variability between different groups in a dataset.
- Effect size: In statistics, effect size is a measure of the strength of the relationship between two variables in statistical analyses. A commonly used interpretation is to refer to effect size as small (g = 0.2), medium (g = 0.5), and large (g = 0.8) based on the benchmarks suggested by Cohen (1988), where “g” refers to Hedge’s g, a statistical measure of effect size.
- Moderator: Moderators are variables that affect the relationship between two other variables. For example, the relationship between the length of a reading intervention and reading comprehension may be stronger for students who are at risk for reading disabilities versus students who are not at risk. In this case, at-risk status would be a moderator.
- Generalizability: Generalizability refers to the extent to which the findings of one study can be extended to other people, settings, or past/future situations.
Cohen, J. (2013). Statistical power analysis for the behavioral sciences . Routledge.
January, S. A., & Klingbeil, D. A. (2020). Universal screening in grades K–2: A systematic review and meta-analysis of early reading curriculum-based measures. Journal of School Psychology , 82 , 103–122. https://doi.org/10.1016/j.jsp.2020.08.007
- literacy data
- Research Article of the Month
- universal screening

Research Article of the Month: August 2024

Research Article of the Month: January 2024

Research Article of the Month: June 2024
- Open access
- Published: 06 September 2024
The state of decentralization of the healthcare system and nutrition programs in the Lao People’s Democratic Republic: an organizational study
- Phonevilay Viphonephom 1 ,
- Sengchanh Kounnavong 2 &
- Daniel Reinharz 1
BMC Health Services Research volume 24 , Article number: 1037 ( 2024 ) Cite this article
Metrics details
The Lao People’s Democratic Republic (Lao PDR), a lower-middle income country, has a higher malnutrition rate than other Southeast Asian countries. The decentralization of healthcare is a determinant of the effectiveness of programs to reduce malnutrition, but no study has focused on this factor in this country. This organizational study explores the state of decentralization of the healthcare system in Lao PDR that underlies the nutrition programs in the country.
A qualitative study, which is based on a neo-institutional theory conceptual framework, explored factors related to dominant structure (laws, regulations, resources) and interpretative schemes (dominant ideas and beliefs) that characterize the nutrition services provided in the Lao healthcare system. Twenty-four semistructured interviews were performed with representatives of healthcare institutions involved in nutrition programs at different government levels, external donors and civil society organizations. The interviews were completed with relevant documents. The analysis focused on the convergence of interpretative schemes of the organizations concerned and the coherence between the structure underpinning the nutrition programs and the interpretative schemes.
Services deployed to reduce malnutrition in the Lao PDR remain largely centralized, despite factors specific to the country that led it to promote decentralization of its services. The convergence of interpretive schemes and the coherence between the observed structure and the interpretative schemes of actors at all governance levels ensure the stability of this state of decentralization, which has persisted for almost 50 years.
Nutrition programs in the Laos PDR are largely under the responsibility of the central government. The transformations in the healthcare system, notably with the use of new information technologies and the fact that the provinces are populated by a growing number of professionals trained in nutrition in addition to factors that push the system to be decentralized, such as ethnic diversity, the increasing availability of human resources in provinces, and the use of communication technologies, are not strong enough to change the balance of power between governance levels. The deconcentration that characterizes decentralization is therefore likely to continue for the foreseeable future.
Peer Review reports
The World Health Organization (WHO) defines malnutrition as deficiencies, excesses, or imbalances in a person’s intake of energy and/or nutrients, encompassing three broad groups of conditions: undernutrition (including wasting, stunting, and underweight); micronutrient-related malnutrition (including deficiencies or excesses of essential vitamins and minerals); and overweight, obesity, and diet-related noncommunicable diseases [ 1 ]. Undernutrition and micronutrient-related malnutrition are the main issues generally addressed by nutrition interventions aimed at five-year-old children in developing countries [ 2 , 3 ]. Children under 5 in lower-middle-income countries are particularly vulnerable to undernutrition and its lifelong effects [ 4 , 5 ], which manifest as wasting (acute undernutrition or severe weight loss due to insufficient food intake and/or infectious disease), stunting (chronic undernutrition leading to low height-for-age and irreversible long-term physical and cognitive damage), and underweight (low weight-for-age, potentially indicating stunting, wasting, or both) [ 5 ]. The WHO highlights that nearly half of deaths among children under 5 years of age are linked to undernutrition. These deaths predominantly occur in low-and middle-income countries [ 1 ].
Undernutrition among children under five years of age is a public health priority in the Lao PDR [ 6 ]. The prevalence of stunting, an indicator often used to estimate the prevalence of chronic malnutrition, is among the highest in East Asia [ 7 ], with a national rate estimated at 31.5% in 2022 [ 8 ]. This rate surpasses those in neighboring lower-middle-income countries, such as Vietnam (20%), Cambodia (22%), and Myanmar (27%) [ 9 ]. According to the WHO standards, stunting is considered critical if it exceeds the threshold of 30% [ 5 ]. Acute malnutrition, estimated by the prevalence of wasting, is still a public health problem among children under five years of age in Lao PDR. The prevalence of wasting is 10%, which is the same as that in Cambodia but higher than that in Myanmar (7%) and Vietnam (5%) [ 9 ]. Furthermore, the problem of malnutrition is unevenly distributed across the territory of Lao PDR. Rural and ethnic minority children are at greater risk of stunting than are urban and majority ethnic groups [ 10 ]. There was a 15% lower risk of stunting for urban children than for their rural counterparts (24% vs. 39%). In Phongsaly Province, the stunting prevalence is as high as 54%, in contrast to the 14% reported in the Vientiane Capital. Additionally, the prevalence of wasting was the lowest in the province of Luangnamtha (3%) and highest in the province of Xayabury (19%) [ 11 ].
The state of healthcare system decentralization has been shown to be a determinant of nutritional status in developing countries [ 12 , 13 ]. Decentralization involves transferring power and responsibility from the central government to lower levels of governance, impacting healthcare service accessibility, quality, and equity [ 14 , 15 , 16 , 17 ]. Decentralization is commonly categorized into three major forms: 1) Deconcentration involves the central government handing over some authority to local administrative offices within the health ministry, allowing local management to handle health-related activities with some discretion; 2) Delegation entails the central government transferring defined managerial and administrative functions to institutions outside the central government's hierarchical structure, which are indirectly controlled by the health ministry; and 3) Devolution refers to the central government legally transferring power to locally elected political organs that operate independently of the central government in specific functions [ 15 ].
Lao PDR has a deconcentration form of decentralization [ 18 , 19 ]. While local levels can provide input for program adaptation to local needs, ultimate control remains with the central government, which can veto decisions made by regional or local health offices [ 20 , 21 ]. In Lao PDR, the dynamics and forces influencing the current state of decentralization are shaped by the country's unique historical-political context and distinctive population characteristics. These factors contribute to the complex nature of power sharing across different government levels. The first factor is related to the historical concept of Lao PDR, which is rooted in the notion of " meuang "[ 22 ]. A meuang is a walled city led by a local ruler overseeing surrounding settlements and villages [ 22 , 23 ]. Each meuang maintained its governance, with oversight and protection from the kingdom but without interference in internal affairs. While the nineteenth century shift toward a centralized state model introduced Western administrative practices, the meuang concept remains deeply ingrained in Lao society, lending historical legitimacy to decentralization forces [ 22 , 24 ]. The second factor is the country's ethnic diversity. The country has 49 official minority groups constituting nearly half the population. Minorities often reside in remote areas [ 25 ]. Decentralizing power and assigning responsibilities to local levels is expected to empower authorities to more effectively customize health programs to meet the diverse needs of the population.
These decentralizing forces are counterbalanced by centralizing forces due in great part to the sociocultural context influenced by Confucianist ideology, which emphasizes social harmony and respect for authority and promotes political centralization in East Asia, including Lao PDR [ 26 , 27 , 28 ]. Moreover, the limited human and financial resources of the central government, which still rely heavily on donor funding, push toward the centralization of the healthcare system and program functioning [ 29 , 30 , 31 ]. From an organizational perspective, these factors create a complex balance between decentralization and centralization in the Lao healthcare system.
Little work has been done in Lao PDR on how the state of decentralization affects the functioning of public health programs, despite being an organizational determinant of health. This organizational study examines the status of decentralization of the healthcare system in Lao PDR and its influence on the National Nutrition Policy.
Conceptual framework
The conceptual framework used in this study was based on neo-institutional theory (NIT) [ 32 , 33 ]. NITs view organizations as social structures that must conform to the expectations and pressures of their institutional environment, which includes normative and regulatory forces [ 34 , 35 ]. This approach was considered relevant for this study because decentralization is an institutionalized concept. The form of decentralization that underlies the nutrition policy in the country arises from sociohistorical and legal factors that institutionalize the distribution of powers that govern the functioning of the policy.
Different NIT conceptual frameworks have been proposed. The one used in this study is the one that was proposed by Hinings and Greenwood in 1988 [ 36 ]. It considers the dialectic between the structure, i.e., the laws, rules, and resources that constrain the work performed in an organization, and the interpretive schemes and their meaning-making processes that shape individual and collective behavior that are dominant in a society, i.e., the dominant ideas and beliefs [ 36 , 37 ]. This dialectic approach has been widely used in studies on public policies concerning the nature of institutional structures [ 38 , 39 , 40 , 41 , 42 ]. From these two dimensions, the structural dimension emphasizes the importance of formalizing corporate values and standards in the organization’s standardized policies and procedures, formalizing decision-making processes, and creating hierarchical structures to ensure compliance with institutionalized environmental factors. On the other hand, the interpretive schemes dimension focuses on the importance of shared meanings and beliefs in shaping organizational behaviors [ 32 , 43 ]. This dimension emphasizes that organizations are influenced by both individual and shared beliefs, values, and norms within their institutional environment. These elements shape the organizational actors' understanding and interpretation of what constitutes legitimate and appropriate behaviors [ 35 , 44 , 45 ]. By doing so, organizations can gain legitimacy and ensure their survival in complex and dynamic institutional environments [ 34 , 35 , 45 , 46 ].
Study design
A case study based on an ethnographic design was conducted to examine patterns of social organization and ideational systems that underlie formal/informal structures, as well as the dominant values, behaviors and beliefs of the groups involved in nutrition interventions in Lao PDR [ 47 , 48 , 49 ]. The data were collected from documents and semistructured interviews with representatives of governmental organizations, nongovernmental organizations (NGOs), and civil society organizations (CSOs) involved in nutrition programs in four provinces of Lao PDR. The nutrition programs in this study are those that align with the Lao National Nutrition Plans and Strategies; they encompass interventions and programs from the health and other sectors that are expected to positively influence nutritional indicators. The data were collected between January and June 2022.
Data collection
Interview Guide
An interview guide (see Fig. 1 ) was developed for this study based on the dimensions of the conceptual framework. This interview guide included a pretest with three members of the Lao Tropical and Public Health Institute (Lao TPHI), who has experience in nutrition research in Lao PDR. These individuals were not part of the study's participants. The participants were asked about their current state of malnutrition in Lao PDR and changes over time, as well as insights into power sharing among government levels and external actors. The questions also covered the organization’s experiences and responsibilities in the field of nutrition. Discussions have further explored perspectives on structural elements (policies, regulations, rules) and common beliefs affecting the healthcare system's ability to address nutrition issues.
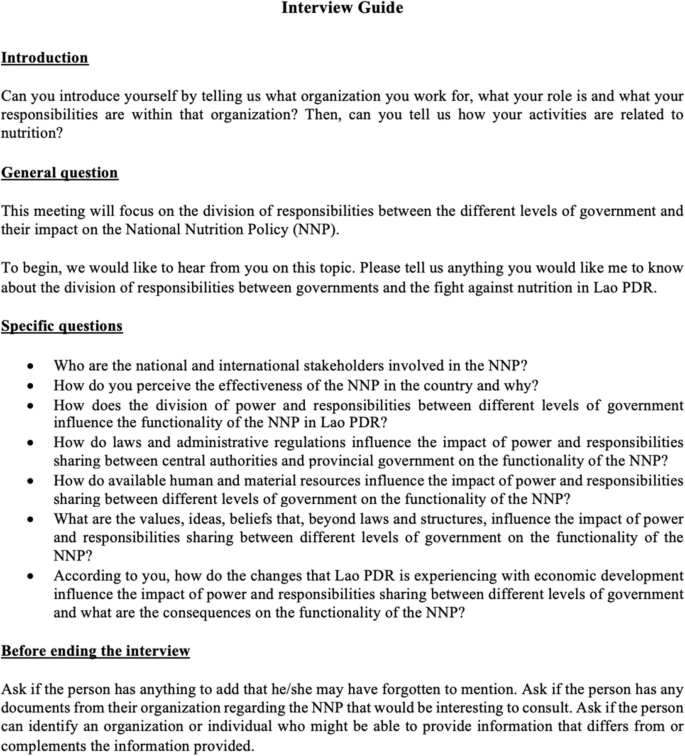
Study sites
To capture the diversity of the country, the latest available national-level data on nutritional status were presented for three provinces with contrasting nutrition situations: Luangnamtha, Xayabury, and Saravan (Table 1 ). Vientiane capital was chosen because of its status as the location of the Ministry of Health (MoH) and national child nutrition-focused institutions (Maternal and Child Health Center and Nutrition Center), as well as the headquarters of development donors and civil society organizations. Luangnamtha, a northern province and one of the most economically developed in the country, has seen remarkable improvements in nutrition indicators. Xayabury, which is also in the north and adjacent to the capital, has experienced little improvement in terms of stunting and underweight rates, with an increase in wasting in recent years. Saravan, in the southern region and one of the poorest provinces of the country, has among the highest prevalence rates of all types of malnutrition, with no significant changes in recent years [ 50 , 51 ].
Source of information
Two sources of information were used for the analysis in this study: interviews with representatives of key institutions and relevant documents [ 52 ].
Representatives of key institutions
The following criteria were used to recruit participants for individual interviews. The participants had to 1) occupy a formal position in relation to nutrition within their organization; 2) be in their current position for at least one year; 3) be authorized to speak on behalf of their organization regarding projects related to nutrition in children under five years of age; and 4) be able to speak one of the languages spoken by the interviewer: Lao (official language), English, or French.
A purposeful sampling approach was used to constitute the sample [ 53 , 54 ]. A preliminary list of participants was created by one of the researchers (SK). At the end of each interview, the participants were asked to suggest additional organizations or individuals who could offer different perspectives. This snowball sampling method aimed to diversify opinions until data saturation was achieved [ 47 , 55 ].
Following administrative protocols, a project summary and discussion topics were initially sent to organization directors for approval. The latter identified individuals within their organization who might have participated in the study. These persons were contacted and asked for their permission to receive project details via fax, WhatsApp, or email. Any queries were addressed through phone calls. If the solicited person agreed, they signed a consent form. The interviews were subsequently scheduled at a mutually convenient time. The participants could choose between face-to-face or online videoconference interviews (Zoom or Google Meet). The interviews, which lasted 45 to 90 min, were audio-recorded with consent, and handwritten notes were taken for documentation and impressions.
To supplement the information provided during the interviews, all documents written in English, Lao, or French on nutrition policies and power sharing between different government levels in Lao PDR were also analyzed. These documents included published academic papers, documents provided by individuals who were interviewed, and documents found on the website of their organization.
Data analysis
All interviews conducted in Lao or French were translated into English by the interviewer and sent to the coauthor who has the least mastery of the Lao language. The realism of the translation was verified by sending a first version of the analyses to three people interviewed, who had to confirm that they found their opinions there. The interviews and document content were analyzed using NVivo 11 software. The interviews and document contents were subsequently analyzed through four main steps: 1) data coding (where data were segmented into meaningful units such as phrases, sentences, or paragraphs); 2) categorization (coded data were then grouped into themes or concepts); 3) coding of themes in connection with the conceptual framework; and 4) comparison of emerging information with published studies on the topic [ 56 ].
The analysis was performed using an inductive-deductive approach [ 57 , 58 ]. The validity of the results was ensured by four elements: 1) credibility based on the triangulation of information provided by multiple sources; 2) transferability through a detailed description of the participants, research process and study context to help the reader judge the relevance of the results for another context [ 59 , 60 ]; 3) reliability based on analyses performed independently by the researcher and one of her supervisors and the search for a consensus between them in case of discrepancy; and 4) confirmability through a detailed and transparent record of the research process, including the data collection, analysis, interpretation and discussion notes from the meetings with coresearchers [ 61 ].
Twenty-four semistructured interviews were conducted with representatives of key organizations: government institutions, United Nations (UN) agencies, international nongovernmental organizations (NGOs), and civil society organizations (CSOs). The participants were primarily women (16 out of 24). The average age was 47 years, with a range from 32 to 61 years. Three participants worked in the healthcare system at the central level, five at the provincial level, five at the district level, and three in health centers (formally known as small hospitals). Three participants worked for UN agencies, and two worked for NGOs. One was a consultant, and two were active members of civil society associations. Twenty-two interviews were conducted in the Lao language (Table 2 ).
Eleven documents were analyzed: 1) Fiscal Decentralization in the People’s Democratic Republic of Lao; 2) Decentralization in Lao PDR: A case study of the Effectiveness of Three Build Directive Policy on Local Authority; 3) the role of Marxism in the Lao political system in the contemporary era; 4) the health system review of Lao PDR in 2014; 5) the Prime Minister’s Decree No. 570 on the organizations and operations of the Ministry of Health in 2021; 6) the National Plan of Action on Nutrition (NPAN) 2021–2025; 7) the National Immunization Programme. Updated Comprehensive Multi-Year Plan Lao PDR 2019–2023; 8) Government spending on health in Lao PDR in 2012; 9) National Nutrition Policy in 2008; 10) National Nutrition strategies to 2025 and Plan of Action 2016–2020; and 11) Operational guideline for the implementation of the National Plan of Action on Nutrition (NPAN) 2021 to 2025 [ 6 , 18 , 19 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 ].
State of decentralization of the Lao healthcare system
Formally, the decentralization of the Lao health system is of the deconcentration type (Fig. 2 ). The Ministry of Health (MoH) oversees the entire healthcare system, which operates across three levels of governance: central, provincial, and district. Provincial and district health authorities’ main responsibility is to ensure that health facilities comply with centrally defined rules [ 6 , 65 ]. Private providers must adhere to centrally defined regulations [ 6 ].
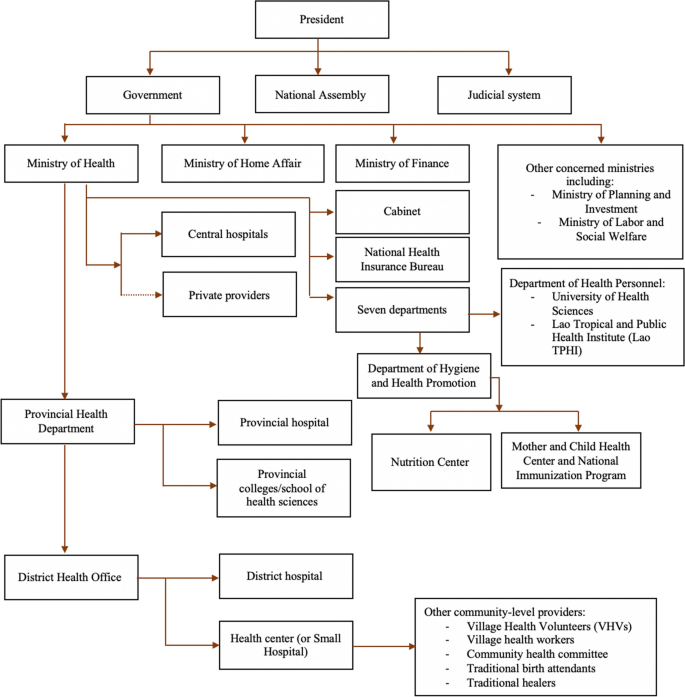
Government-level power sharing in Lao PDR. Sources: Health System Review in Lao 2014; National Plan of Action on Nutrition (NPAN) 2021–2025; National Immunization Programme: Updated Comprehensive Multi-Year Plan Lao PDR 2019–2023; and the Prime Minister’s Decree No. 570 on the organizations and operations of the Ministry of Health in 2021 [ 6 , 63 , 64 , 68 ]
All decisions concerning human and financial resources in the health care sector must be routed through the central level, represented by the MoH and other ministries, notably the Ministry of Finance (MoF), which is responsible for overall fiscal policy and sectoral allocations of the annual recurrent budget. Other ministries are also involved. The Ministry of Planning and Investment (MPI) oversees capital budget allocation, whereas the Ministry of Home Affairs (MHA) manages the total number of civil servants and sectoral allocations of human resource quotas, including the annual recruitment of health personnel at all administrative levels [ 6 , 65 ].
Most respondents (19/24) highlighted the fact that in practice, the power dynamics between levels of governance are complex because constitutional power-sharing arrangements are also under political influence. Official documents support this assertion when they emphasize that in the Lao PDR, the Lao People's Revolutionary Party (LPRP) is the body that has the constitutional mandate to exercise leadership across all levels of government [ 18 , 62 ].
Power sharing between government levels and nutrition programs in Lao PDR
The Lao MoH has the ultimate responsibility for uni- and multisectoral nutrition programs. While the Provincial Health Department (PHD) and District Health Office (DHO) are responsible for implementing and ensuring the functionality of services, the central government retains control over which interventions to offer and over the allocation of human, financial, and material resources [ 66 , 69 ] (Table 3 ).
At the central level, operational leadership in the field of nutrition is formally led by the Multisectoral National Nutrition Committee (MSNNC), which comprises the Ministry of Health, Ministry of Planning and Investment, Ministry of Agriculture and Forestry, Ministry of Education and Sports, and other ministries and mass organizations. The MSNNC defines priorities, assesses local needs, and oversees the implementation of centrally sanctioned interventions at local levels (Table 3 ). Although the responsibility for the MSNNC falls under the MoH, the MSNNC is chaired by the Deputy Prime Minister and deputy chaired by the Deputy Minister of Health. Its members consist of deputy ministers of eight ministries and the vice-director or the secretary of the LPRP’s mass organizations. The MSNNC serves as the central committee overseeing the hierarchical structure of other nutrition committees at the provincial, district, and village levels. The MSNNC structure has been conceived with the idea of having leadership able to promote intersectionality of nutrition interventions [ 6 , 63 , 64 , 66 ].
Yet, under the authority of the Politburo of the LPRP, the Lao national government holds supreme authority, whereas provincial governments possess financial responsibilities and managerial duties. Provincial administration is directly supervised by the central government under the principle of democratic centralism [ 18 , 19 ].
Structure and interpretive schemes underlying the decentralization state of nutrition programs in the Lao PDR
Seven factors related to the structure and interpretative schemes that influence the effectiveness of nutrition programs emerged from the analysis of interviews and documents (Fig. 3 ).
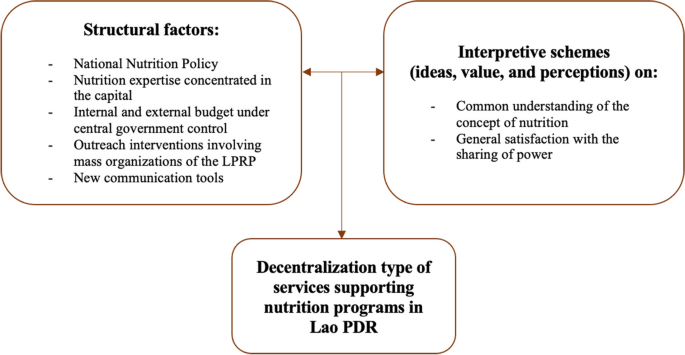
Factors associated with the decentralization type of nutrition programs in Lao PDR
Structural factors
Five main structural factors emerge from the data underlying the decentralization state of nutrition programs in Lao PDR: 1) the existence of a public policy; 2) the availability of human resources; 3) the source of funding; 4) the key role of mass organizations; and 5) communication tools.
A national nutrition public policy
Interventions on malnutrition in Lao PDR are primarily based on a public policy, the National Nutrition Policy (NNP), which was enacted in 2008. This policy provides the legal framework for mobilizing and coordinating actors that can contribute to improving nutrition indicators, regardless of their sector. The policy is operationalized through formal strategic plans developed by the MoH. These official documents define the responsibilities of agencies addressing malnutrition among the different levels of government in the country [ 63 , 66 , 69 ]. All participants agreed that a public policy on nutrition is essential for ensuring intersectoral collaboration at various levels of governance. The policy is seen as a structural foundation that, while centralizing, guarantees the ability of the concerned players to act.
Human resources
The second structuring element that emerges from the data is the fact emphasized by almost all respondents (21/24) and all documents dealing with nutrition [ 6 , 63 , 66 ] that the shortage of expertise outside the capital limits local governments from taking charge of nutrition programs more independently. The respondents also highlighted the fact that a shortage of human resources is compounded by a high turnover rate at all local levels. Turnover weakens the capacity to coordinate the numerous actors involved. Moreover, it drains a considerable part of the local budget, as it leads to continual staff training for nutrition interventions. In brief, all the participants recognized that the state of human resources made it difficult to imagine a program to combat malnutrition run by local authorities.
The health system, from the central to the village levels, is funded from three main sources: a budget allocated by the Ministry of Finance, direct payments at health facilities from users of health services, and funding from external donors, such as NGOs. Funds allocated by the central government are sent to provincial authorities, who then allocate these funds to districts according to planned budgets. These funds are designed for civil servants’ salaries as defined by the central government, as well as for the equipment needs of health establishments. Most of the money paid by service users can be kept by the hospital and used for recurrent costs, including staff wages, allowances, maintenance, utilities, and supplies. The rest (approximately 20%) should be handed over to the provincial or district finance department. Money provided by external donors for projects deployed in provinces and districts must be approved at the central level. One consequence of having multiple sources of financing nutrition activities is the variability in available funds for health services among districts and provinces [ 6 , 18 , 65 ].
The annual budget planning for nutrition interventions involves consultations and reports sent from the district to the provincial levels. The MoH then finalizes and submits it for approval by the National Assembly. In other words, nutrition programs are mainly under central government management. The majority of local-level participants (9/13) feel that this system is not optimal, the main reason being the uncertainty regarding the availability of financial resources over time. These respondents also deplore frequent delays in budget transfers, particularly transfers to remote areas. Above all, nearly all participants at the district and health center levels (6/8) mentioned that nutrition-targeted budgets are often merged with funds intended for non-nutrition public health interventions, as indicated in the following quotation.
“ There’s no other source of money. For the education or agriculture sector, the money would go to each sector separately. For these sectors, they have their own money for nutrition, but we don’t have. So, we need to depend on the integrated work. … Mainly, when we request to the central level, they said they don’t have money for our province anymore; there is only our provincial health office and their help that includes the budget, like they would include the nutrition on the integrated work, and then they manage the staff for it. The structure that divides clearly, it’s not always suitable in real situations ” said by the participant from the provincial level (P11)
The irregular flow of funds is partially offset by the availability of external funding, such as from NGOs [ 63 , 66 ]. However, activities funded by external entities require preapproval from the central government.
The fact that no respondent was able to propose solutions to the problem of funding uncertainty suggests that current funding mechanisms contribute significantly to the solidity of the structure underpinning the decentralization of nutrition programs and hence to the stability of the decentralization type that underlies nutrition programs.
LPRP’s mass organizations
In Lao PDR, the LPRP’s mass organizations, particularly Lao Women’s Union (LWU), are unavoidable collaborators in nearly all programs implemented at the population and community levels that aim to reduce the prevalence of malnutrition. Even if these organizations do not necessarily have expertise in health education which is one of their main contributions, there is a consensus among participants that they have proven to be a valuable substitute for the shortage of professionals in the field. This is expressed in the following quotation:
“…there are the LPRP grassroot members in the meeting (nutrition committee meeting at the district level), who we invited to join us, as well as the standing and district LPRP committee who divides the responsibility for guiding each population group, whoever is responsible for our target group, we would take them to the field, as well as the mass organization, especially the Lao Front for National Development as a main actor to discuss this, second is the Women Union that we can’t forget them, we would take them going to the field with us.” said by the participant from the district level (P17)
This general feeling is also recorded in several official documents [ 6 , 62 , 66 ].
In short, the constant presence of mass organizations whose primary function, in addition to contributing to health education programs, is to increase LPRP values in the population reinforces the power of the central level in nutrition programs deployed in communities.
Communication tools
All the participants underscore the pivotal role of social networks, such as Facebook and WhatsApp, in expediting decision-making processes that previously relied on formal communication channels and informal social gatherings. According to the participants, social media has increased the capacity of nutrition programs to reach their objectives by enabling professionals involved in nutrition programs everywhere to be easily reached and to ask questions without navigating through time consuming and poorly effective bureaucratic procedures. The participants also highlighted that these new technologies inject a sense of dynamism through the competition they foster among teams. This sentiment is captured in the following quotation:
“In the groups, there are staff (DHO staff) and department level (PHD staff) together... If the department (PHD staff) is not in the group, they will send the responsible staff to join the group. So, we always exchange (information) with each other. Whenever the central level (staff) sends messages in the group, everyone always responds. They couldn’t act like they haven’t seen it (messages) because we have the responsibilities for our work, and they also have their responsibilities. If they don’t answer, it means that they haven’t followed up (on the work)” said by the participant from the central level (P01)
There is a consensus that new communication tools have reshaped the power dynamics between central and local levels of governance in Lao PDR. They allow overpassing the traditional hierarchical structure of the healthcare system that is supported by communication channels such as those based on the exchange of information by paper (including faxes). This trend empowers lower levels to directly engage with higher-level actors at the central level, fostering a possible emerging capacity for a more decentralized dynamic inside the field of nutrition programs.
Interpretive schemes
Two main interpretive factors emerged from the data underlying the decentralization state of nutrition programs in Lao PDR: 1) the understanding of the causes and consequences of malnutrition; and 2) the perception of the roles of different levels of government in implementing malnutrition interventions.
Understanding the causes and consequences of malnutrition
The participants across different levels of governance in Lao PDR share a common understanding of the causes and challenges of malnutrition. All the participants recognized that malnutrition is a multifaceted issue requiring attention on both the demand and supply sides. They emphasized the fact that in a resource-limited country such as Lao PDR, factors such as a lack of human and financial resources, combined with contextual challenges in vulnerable communities such as poverty, cultural barriers, and food insecurity must all be considered. Additionally, there is a consensus among participants that addressing malnutrition necessitates multisectoral programs, as programs limited to calories and micronutrients may have a limited impact on improving the condition of malnourished children. Numerous other issues, such as water, sanitation, and hygiene (WASH), gender, and the educational levels of parents, have been found to be key determinants of nutrition. They require significant collaboration from different sectors and stakeholders. In short, there is a broad consensus among stakeholders on interpretive schemes.
Perception of the capacity of the different levels of governance to assume nutrition responsibilities
The majority of participants across various levels of government (10/16) spontaneously declared that interventions to address malnutrition should be led by the central government, citing the fact that the government has expertise and control over the human, financial and material resources necessary for the programs. It is also recognized that district-level health workers, particularly in remote regions, may lack sufficient training and resources. The remaining six participants did not express an opinion on this matter. Although half of the participants at the local level mentioned that regions are increasingly populated by well-trained healthcare professionals, they believe that this trend cannot have a significant impact on the power sharing arrangements for nutrition programs due to the shortage of human resources, especially in remote regions and because local health volunteers and mass organizations largely compensate for human resource needs.
Therefore, there is no question among participants regarding the state of decentralization of services that underpin nutrition programs in the country.
Dialectic between structure and interpretive schemes
In brief, there is coherence between the structure and interpretive schemes that underlie the sharing of responsibilities across governance levels in nutrition programs and interventions in Lao PDR. This coherence is reinforced by the respondents' belief that the desired effects of socioeconomic changes, such as an increase in the number of well-trained nutrition professionals and the use of communication tools empowering regional health workers, cannot sufficiently alleviate human resource needs in the provinces. The system of division of responsibilities between governance levels that has lasted for approximately fifty years is therefore likely to be stable. It is likely to remain so for the foreseeable future.
In Lao PDR, powerful forces are pushing the Lao healthcare system toward more centralization than decentralization, despite factors that support greater autonomy for local authorities.
Every organization concerned with nutrition programs seems to be satisfied with this situation and perceives it as a determinant of the effectiveness of nutrition programs. None of the respondents suggested an alternative approach, despite acknowledging that socioeconomic changes are endowing regions with the capacity to manage public health programs that were previously unimaginable. Therefore, there is convergence of interpretive schemes among concerned actors, as well as coherence between structure and interpretive schemes. This convergence signifies a shared vision of nutrition challenges in the country and the capacity to address them, regardless of organizational concerns or hierarchical levels of governance. The coherence between structure and interpretive schemes reveals a general feeling that the current distribution power among governance levels is the most appropriate way to meet the nutritional needs of the population.
From an organizational perspective seen through a neoinstitutional lens [ 70 ], the main consequence is that the distribution of responsibilities in nutrition services among different government levels has remained stable since the event of the Lao PDR in 1975.
The findings of this study highlight how a country's sociopolitical context influences the state of decentralization and the functioning of its public health programs. In the case of immunization programs in Lao PDR, three notable factors impact their implementation: the Lao sociopolitical background, the availability of resources, and the use of new technologies such as WhatsApp by health professionals. These elements have reshaped the dynamics of the deconcentrated healthcare system and its program operation [ 31 ].
Theoretically, a centralized healthcare system should lead to more standardized public health programs and health services across the country if it ensures consistent application, quality of care, and equitable distribution of resources [ 71 , 72 , 73 ]. However, given the diverse contexts among provinces, a one-size-fits-all approach may not be optimal, especially for complex and multisectoral interventions like nutrition programs. These programs often require adaptation to the specific needs and capacities of local contexts and populations in different communities to be truly effective [ 74 , 75 ].
In a diverse country like Lao PDR, public health interventions require adaptation and more flexible interventions and activities to meet the varied needs of different communities. Empowering local authorities, who are more familiar with local contexts and issues, could improve the management of activities and resources, leading to better interventions that address the specific needs of their populations. In other single-party countries, decentralization has been shown to effectively strengthen public health programs and enhance their effectiveness [ 76 , 77 ].
The documents and interview findings from this study indicate that the formal structure of the healthcare system in Lao PDR is well defined. The organizational structures of the NNP identify the roles and responsibilities of stakeholders from the central level of the MoH to the implementation level of the village. However, in practice, the implemented programs aimed at reducing the prevalence of malnutrition in children under age 5 in the country are far more challenging than the formal structure suggests [ 78 ]. Addressing nutrition outcomes requires a long-term and multifaceted approach, particularly when contributions among actors and power-sharing roles involve local governments working with multiple stakeholders at all levels.
Indeed, Lao PDR faces challenges in reversing the conditions that would allow local governments to put more of their own initiatives into nutrition programs. Unlike in neighboring countries like Vietnam or Thailand, in Lao PDR, the only training on nutrition is a course integrated into a public health master’s program. Additionally, Lao PDR, a country as large as the United Kingdom with a population of 7.7 million inhabitants, is a sparsely populated country. Fifteen of its eighteen provinces have fewer than 500,000 inhabitants. Only one has more than a million [ 79 ]. A small population reduces the likelihood of building a critical mass of people from a given province with expertise in nutrition. Although constraints on qualified human resources are common in many low-resource countries [ 80 , 81 ], these constraints, coupled with the population context in Lao PDR, obviously significantly contribute to the centralization of the Lao healthcare system. In fact, this need for expertise is not limited to nutrition. Optimizing interventions to reduce the prevalence of malnutrition in children under 5 years of age requires tailored approaches that consider the diverse cultural and regional contexts of the population and address multisectoral programs and interventions including food security, water, sanitation, hygiene, maternal education, and social protection. The complexity of these interventions requires multidisciplinary teams [ 63 , 67 , 82 ]. Poorly populated provinces might not be able to gather all this desired expertise. Finally, Lao PDR receives funding for its nutrition program from several external donors and NGOs. This necessitates central-level coordination that might be even more crucial once the country has left, supposedly in 2026, the group of the least developed countries [ 83 ]. Leaving this group will have consequences for the support provided by external actors. Expectations are that the central government will assume more responsibilities for its nutrition programs in the near future.
Finally, advancements in communication technologies and the arrival of better-trained human resources offer hope for addressing the shortage of quality human resources that hinder local authorities' leadership in nutrition programs. An increasing number of graduated individuals living in the provinces are proficient in the use of new technologies [ 84 ]. This increased utilization of technology is anticipated to further transform traditional barriers that govern interactions among stakeholders. Additionally, interpretive patterns are likely to evolve as professionals in provinces become better informed and more willing to customize nutrition programs to meet the specific needs of local populations. However, owing resource shortages and uneven population distribution in Lao PDR, there are unequal opportunities for local levels to assume more responsibility for nutrition interventions, with little to no chance for decision-making at the local level. This is expected to limit the capacity of sub-national levels from contributing more substantially to nutrition programs than they currently do.
None of the respondents evoked a future where nutrition programs would be more decentralized. Nevertheless, they acknowledged that the current state of decentralization is suboptimal. They recognized that one of the undesirable effects of centralization is the difficulty in adapting services to the specific needs of diverse populations.
Limitations
This study has several limitations. First, respondents were selected by their organization directors following administrative procedures mandated by research projects in Lao PDR. While this method has likely allowed to capture a diverse range of perspectives on malnutrition, it may have excluded individuals who disagreed with the official discourse. Although the two coders felt that additional interviews would not yield new information, it is possible that additional insights might have been generated by more interviews if soliciting directly potential participants directly could have been done.
Second, as is common in qualitative studies, unconscious subjectivity and bias among researchers may have influenced some interpretations. However, the risk is mitigated by ensuring the validity of four elements of the results, particularly through the triangulation of information from interviews and document reviews, as well as through independent analyses conducted by two researchers.
Finally, the generalizability of the results may be limited. The Lao context is unique, and nutrition programs have specificities that may differ from those of other national health programs functioning in the country. Consequently, the findings of this study may not be directly applicable to other programs or countries, including those with single-party governance structures.
Decentralization of the Lao healthcare system is of the deconcentrated type, i.e. a system largely under the responsibility of the central government. The transformations taking place in the healthcare system, notably with the use of new information technologies, are changing relationships between individuals across different levels of government and the fact that the provinces are populated by a growing number of professionals trained in nutrition. These factors could lead people to believe that the system would give more responsibility to provincial governments to improve their malnutrition status at local levels. However, the data show that these changes are probably not yet strong enough to change a structure that has endured for approximately fifty years. The deconcentration that characterizes decentralization is therefore likely to continue for the foreseeable future.
Availability of data and materials
The datasets during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
Civil society organizations
District health offices
Lao People’s Democratic Republic
Lao People's Revolutionary Party
Lao Women's Union
Ministry of Home Affairs
Multi-sectorial National Nutrition Committee
Ministry of finance
Ministry of health
Ministry of planning and investment
Nongovernmental organizations
National Nutrition Policy
National Nutrition Strategy and Plan of Action
National Plan of Action on Nutrition
- Neo-institutional Theory
Provincial health departments
United Nations
Village health volunteers
World Health Organization
World Health Organization. Malnutrition 2024. Available from: https://www.who.int/news-room/fact-sheets/detail/malnutrition .
Caulfield LE, Richard SA, Rivera JA, Musgrove P, Black RE. Stunting, wasting, and micronutrient deficiency disorders. In: Disease Control Priorities in Developing Countries 2nd edition. The International Bank for Reconstruction and Development / The World Bank. New York: Oxford University Press; 2006.
Google Scholar
Muller O, Krawinkel M. Malnutrition and health in developing countries. CMAJ. 2005;173(3):279–86.
Article PubMed PubMed Central Google Scholar
UNICEF. Child Malnutrition 2023. Available from: https://data.unicef.org/topic/nutrition/malnutrition/ .
World Health Organization, United Nations Children's Fund (UNICEF) & World Bank. Levels and trends in child malnutrition: UNICEF / WHO / The World Bank Group joint child malnutrition estimates: key findings of the 2021 edition. World Health Organization. 2021. https://iris.who.int/handle/10665/341135 .
World Health Organization. The Lao People’s Democratic Republic: Health System Review. Asia Pacific Observatory on Health Systems and Policies; 2014. Contract No.: 1.
World Bank. Lao PDR: New Financing to Improve Access to Health and Nutrition Services. 2020.
Save the Children, CARE, EU, CCL, ChildFund. Partnership for Improved Nutrition in Lao PDR Pillar 3: Sustainable Change Achieved through Linking Improved Nutrition and Governance. Vientiane: Lao Social Research; 2022.
UNICEF/WHO/World Bank Joint Child Malnutrition Estimates Expanded Database. Malnutrition data 2023. Available from: https://data.unicef.org/resources/dataset/malnutrition-data/ .
Ministry of Health, World Health Organization. Overview of Lao health system development 2009–2017. Manila, Philippines: World Health Organization Regional Office for the Western Pacific; 2018. Report No.: Licence: CC BY-NC-SA 3.0 IGO.
UNICEF/WHO/World Bank Joint Child Malnutrition Estimates Expanded Database. Malnutrition data 2022. Available from: https://data.unicef.org/resources/dataset/malnutrition-data/ .
Constantinides SV. Determinants of Nutrition Agenda Setting in the Context of the Double Burden of Malnutrition in Tamil Nadu, India. South Carolina: University of South Carolina; 2020.
Acosta AM, Fanzo J. Sussex: Institute of Development Studies; 2012.
Boko SH. Decentralization_Definitions, theories and debates. Decentralization and Reform in Africa. Boston: Sringer; 2002. p. 1–10.
Book Google Scholar
Frumence G, Nyamhanga T, Mwangu M, Hurtig AK. Challenges to the implementation of health sector decentralization in Tanzania: experiences from Kongwa district council. Glob Health Action. 2013;6:20983.
Article PubMed Google Scholar
Mosca I. Decentralization as a determinant of health care expenditure: empirical analysis for OECD countries. Appl Econ Lett. 2007;14(7):511–5.
Article Google Scholar
Saltman RB, Bankauskaite V, Vrangbaek K. Decentralization in Health Care. Maidenhead: Mcgraw-Hill House; 2007.
Martinez-Vazquez J, Gomez JL, Yao G. Fiscal Decentralization in the People’s Democratic Republic of Lao. Georgia, United States: Georgia State University; 2006. Contract No.: Working Paper 06–22.
Luangrath S. Decentralization in Lao PDR: A Case Study of the Effectiveness of Three Build Directive Policy on Local Authority. Seoul, Korea: Seoul National University; 2019.
Litvack J, Seddon J. Decentralization briefly notes. Washington, DC: World Bank Institute; 1999.
Hutchinson PL, LaFond AK. Monitoring and Evaluation of Decentralization Reforms in Developing Country Health Sectors. Maryland, United States: Abt Associates Inc.; 2004.
Stuart-Fox M. Politics and Reform in the Lao People’s Democratic Republic. Working Paper No. 126, Asia Research Center, Murdoch, University. 2005.
Pholsena V, Banomyong R. Laos: From buffer state to crossroads? Chiang Mai, Thailand: Mekong Press; 2006.
Stuart-Fox M. Political Culture and Power in the Lao People’s Democratic Republic. J Asiatic Stud. 2009;138:222–54.
United Nations in Lao PDR. Country Analysis Report: Lao PDR: Analysis to inform the Lao People’s Democratic Republic-United Nations Partnership Framework (2017–2021). Vientiane: United Nations; 2015.
Nawrot KA. Does Confucianism promote cooperation and integration in East Asia? Int Commun Chin Culture. 2020;7(1):1–30.
Jiang Y-H. Confucian political theory in contemporary China. Annu Rev Polit Sci. 2018;21:155–73.
Kim Y, Lee H-K, Park S. The Confucian Tradition and Politics. Oxford Research Encyclopedia of Politics. 2019.
Dickovick JT. Foreign aid and decentralization: Policies for autonomy and programming for responsiveness. Helsinki: The United Nations University World Institute for Development Economics Research (UNU-WIDER); 2013.
Dickovick JT. Foreign aid and decentralization: limitations on impact in autonomy and responsiveness. Public Admin Dev. 2014;34(3):194–206.
Viphonephom P, Kounnavong S, Reinharz D. Decentralization and immunization program in a single-party state: the case of the Lao People’s Democratic Republic. Trop Med Health. 2024;52(1):35.
Meyer JW, Rowan B. Institutionalized organizations: formal structure as myth and ceremony. Am J Sociol. 1977;83(2):340–63.
DiMaggio PJ, Powell WW. The iron cage revisited: institutional isomorphism and collective rationality in organizational fields. Am Sociol Rev. 1983;48(2):147–60.
Marschlich S. Conceptual Framework: Sociological Neo-Institutionalism, Legitimacy, and Public Relations. Corporate Diplomacy: How Multinational Corporations Gain Organizational Legitimacy: A Neo-Institutional Public Relations Perspective. Amsterdam: University of Amsterdam; 2022.
Swaminathan A, Wade JB. Institutional Environment. The Palgrave Encyclopedia of Strategic Management. London: Palgrave Macmillan; 2016. p. 1–7.
Hinings CR, Royston G. The Dynamics of Strategic Change. Oxford: Basil Blackwell Ltd.; 1988.
Hinings CR, Greenwood R, Reay T, Suddaby R. Dynamics of change in Organizational field. Handbook of Organizational Change and Innovation: Oxford University Press; 2003.
Harimanana A, Barennes H, Reinharz D. Organizational analysis of maternal mortality reduction programs in Madagascar. Int J Health Plann Manage. 2011;26(3):e186–96.
Peyrot M. Institutional and organizational dynamics in community-based drug abuse treatment. Soc Probl. 1991;38(1):20–33.
Morrill C, Yalda C, Adelman M, Musheno M, Bejarano C. Telling tales in school- youth culture and conflict narratives. Law Soc Rev. 2000;34(3):521–65.
Addicott R, Furlie E. Sedimented archetype change in public sector organisations: the example of managed clinical networks for cancer. CQUniversity. Conference contribution. 2006. https://hdl.handle.net/10018/8418 .
Breunig KJ, Skjølsvik T. The virtual future of professional service firms: Identifying emerging interpretive schemes caused by technology enactment. Acad Manag Proc. 2016. https://hdl.handle.net/10642/4407 .
Greenwood R, Hinings CR. Understanding radical organizational change: Bringing together the old and the new institutionalism. Acad Manag Rev. 1996;21(4):1022–54.
Senge K. The ‘New Institutionalism’ in organization theory: Bringing society and culture back in. Am Sociol. 2013;44(1):76–95.
Scott WR. Institutions and organizations : ideas, interests and identities. 4th ed. Thousand Oaks: SAGE Publications, Inc.; 2013.
Rouleau L. Théories des organisations : Approches calssiques, contemporaines et de l’avant-garde. Quebec, Canada: Presse de Université du Québec; 2007.
Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. London, United Kingdom: SAGE Publications Inc; 2013.
Huby G, Hart E, McKevitt C, Sobo E. Addressing the complexity of health care: The practical potential of ethnography. J Health Serv Res Policy. 2007;12(4):193–4.
Kielmann K. The ethnographic lens. In: Gilson L, editor. Health policy and systems research: A methodology reader. Geneva, Switzerland: World Health Organization; 2012. p. 235–52.
Lao Statistic Bureau. Lao PDR: Lao Social Indicator Survey 2011–2012 (Multiple Indicator Cluster Survey/Demographic and Health Survey). Vientiane: Lao Statistic Bureau and UNICEF; 2012.
Lao Statistic Bureau. Lao Social Indicator Survey II 2017. Vientiane: Lao Statistic Bureau and UNICEF; 2018.
Pope C. Qualitative Research in Health Care. Hoboken: Wiley-Blackwell; 2020. p. 2020.
Creswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research. 2nd ed. Los Angeles: Sage Publications; 2011.
Palinkas AP, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health. 2015;42(5):533–44.
Naderifar M, Goli H, Ghaljaie F. Snowball sampling: a purposeful method of sampling in qualitative research. Strides Dev Med Educ. 2017;14(3):1–4.
Fortin M-F, Gagnon J. Fondements et étapes du processus de recherche: Méthodes quantitatives et qualitatives. 3rd ed. Montreal: Chenelière éducation; 2016.
Park D, Bahrudin FI, Han J. Circular reasoning for the evolution of research through a strategic construction of research methodologies. Int J Quant Qual Res Methods. 2020;8(3):1–23.
CAS Google Scholar
Proudfoot K. Inductive/Deductive Hybrid Thematic Analysis in Mixed Methods Research. J Mixed Methods Res. 2022;0(0):1–19.
Ponterotto JG. Brief note on the origins, evolution, and meaning of the qualitative research concept “Thick Description.” Qual Rep. 2006;11(3):538–49.
Kharel D. VIsual enthnography, thick description and cultural representation. Dhaulagiri J Sociol Anthropol. 2015;9:147–60.
Korstjens I, Moser A. Series: Practical guidance to qualitative research. Part 4: Trustworthiness and publishing. Eur J Gen Pract. 2018;24(1):120–4.
Dahuai Y, Phoutthaphone S, Jing W. The role of Marxism in the Lao political system in the contemporary era. Int J Soc Sci Human Invent. 2017;4(12):4216–26.
Ministry of Health. National Plan of Action on Nutrition (NPAN) 2021–2025. Vientiane: Ministry of Health; 2021.
Lao PDR National Immunization Programme. Updated Comprehensive Multi-Year Plan Lao PDR 2019–2023. Vientiane: Ministry of Health, GAVI, UNICEF/WHO; 2018.
World Bank. Government spending on health in Lao PDR: Evidence and issues. Vientiane: World Bank; 2012.
Ministry of Health. National Nutrition strategies to 2025 and Plan of Action 2016–2020. Vientiane: Ministry of Health; 2015.
Secretariat National Nutrition Committee. Operational guideline for the implementation of the National Plan of Action on Nutrition (NPAN) 2021 to 2025. Vientiane: National Nutrition Committee Secretariat; 2023.
Bureau PM. Prime Minister’s Decree No. 570 on the organization and activities of the Ministry of Health. Vientiane; 2021.
Ministry of Health. National Nutrition Policy. Vientiane: Ministry of Health; 2008.
Greenwood R, Hinings CRB. Radical organizational change. SAGE Publications Ltd. 2006.
Ostermann M, Vincent J-L. How much centralization of critical care services in the era of telemedicine? Crit Care. 2019;23(1):423.
Kobayashi D, Otsubo T, Imanaka Y. The effect of centralization of health care services on travel time and its equality. Health Policy. 2015;119(3):298–306.
Elson S. Regionalization of health care from a political and structural perspective. Healthc Manage Forum. 2009;22(1):6–11. https://doi.org/10.1016/S0840-4704(10)60279-7 .
Sanders D, Chopra M. Implementing comprehensive and decentralised health systems: the quest for integrated care in post-apartheid South Africa. Int J Integr Care. 2001;1:e33.
Kesale AM, Mahonge C, Muhanga M. Effects of decentralization on the functionality of health facility governing committees in lower and middle-income countries: a systematic literature review. Glob Health Action. 2022;15(1):2074662.
Zhu J, Ge Z, Xia J, Liu Q, Ran Q, Yang Y. Status quo and problem analysis of cervical cancer screening program in China: Based on RE-AIM framework. Front Public Health. 2022;10:987787. https://doi.org/10.3389/fpubh.2022.987787 .
Huang X, Yang B, Liu Q, Zhang R, Tang S, Story M. Improving maternal and child nutrition in China: an analysis of nutrition policies and programs initiated during the 2000–2015 Millennium Development Goals era and implications for achieving the Sustainable Development Goals. J Health Popul Nutr. 2020;39(1):12.
Sengchaleun V, Samri MA, Kounnavong S, Reinharz D. Advocacy Coalition by External Actors and Strategies Used to Influence the Emergence of the National Nutrition Policy in Lao PDR. Health. 2021;13(08):812–29.
World Health Organization. World Health Organization Data 2020. Available from: https://data.who.int/countries .
Delisle H, Shrimpton R, Blaney S, Du Plessis L, Atwood S, Sanders D, et al. Capacity-building for a strong public health nutrition workforce in low-resource countries. Bull World Health Organanization. 2017;95(5):385–8.
Diasso D, Doudou MH, Levrak MC, Sedutto HD, Savadogo A. Municipalities’ organisational capacity to support the implementation of the Multi-Sector Nutrition Plan in Burkina Faso. Glob Health Action. 2021;14(1):1979279.
European Union, UNICEF. Review of costing of the National Plan of Action for Nutrition 2016–2020. Vientiane: European Union and UNICEF; 2020.
Ministry of Foreign Affairs. Lao PDR is recommended to graduate in 2026 from the Least Developed Country Category with an extended preparatory period. Vientiane, Lao PDR: Ministry of Foreign Affairs 2021. Available from: http://www.mofa.gov.la/index.php/activities/state-leaders/3999-lao-pdr-is-recommended-to-graduate-in-2026-from-the-least-developed-country-category-with-an-extended-preparatory-period .
World Bank. Positioning The Lao PDR for a Digital Future. Vientiane: World Bank; 2021.
Download references
Acknowledgements
We would like to express our sincere thanks to all the participants who generously shared their valuable experiences with us. We would also like to express our thanks to the organizations that assisted us in participant recruitment. The first author P.V. extends her special thanks to the Canadian Francophonie Scholarship Program (CFSP) for their support during her doctoral studies.
This research was supported by the Canadian Francophonie Scholarship Program, under the Canadian Bureau for International Education, Government of Canada.
Author information
Authors and affiliations.
Department of Social and Preventive Medicine, Laval University, Quebec City, QC, Canada
Phonevilay Viphonephom & Daniel Reinharz
Lao Tropical and Public Health Institute (Lao TPHI, Ministry of Health, Vientiane, Lao PDR
Sengchanh Kounnavong
You can also search for this author in PubMed Google Scholar
Contributions
PV: conceptualization and design; acquisition of data; analysis and interpretation of data; writing original draft; and writing review and editing of the manuscript. SK: recruitment of participants; writing review and editing the manuscript; and supervision. DR: conceptualization and design; analysis and interpretation of data; writing review and editing of the manuscript and supervision. All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Phonevilay Viphonephom .
Ethics declarations
Ethics approval and consent to participate.
All methods were carried out in accordance with relevant guidelines and regulations. Written consent was obtained from all participants before data collection. Ethical approval for the study was obtained from the Research Ethics Board of Laval University, Quebec, Canada (number “2021–259/23–09-2021”) and the National Ethics Committee for Health Research, Ministry of Health, Vientiane, Lao PDR (number “08/NECHR”, 14/01/2022).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Viphonephom, P., Kounnavong, S. & Reinharz, D. The state of decentralization of the healthcare system and nutrition programs in the Lao People’s Democratic Republic: an organizational study. BMC Health Serv Res 24 , 1037 (2024). https://doi.org/10.1186/s12913-024-11513-y
Download citation
Received : 04 October 2023
Accepted : 29 August 2024
Published : 06 September 2024
DOI : https://doi.org/10.1186/s12913-024-11513-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Decentralization
- Single-party state
- Lower-middle income country
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Effectiveness of...
Effectiveness of modified vaccinia Ankara-Bavarian Nordic vaccine against mpox infection: emulation of a target trial
Linked research.
Measures of how well a vaccine works
- Related content
- Peer review
- Christine Navarro , public health physician 1 2 3 ,
- Cindy Lau , senior research analyst 4 ,
- Sarah A Buchan , scientist 1 2 3 4 ,
- Ann N Burchell , scientist 2 4 5 6 ,
- Sharifa Nasreen , postdoctoral fellow 2 4 7 ,
- Lindsay Friedman , research coordinator 1 ,
- Evaezi Okpokoro , research scientist 8 ,
- Peter C Austin , senior scientist 4 9 ,
- Darrell H S Tan , scientist 6 9 10 11 ,
- Jonathan B Gubbay , medical microbiologist 1 12 ,
- Jeffrey C Kwong , senior scientist 1 2 3 4 5 11 13 ,
- on behalf of the Canadian Immunization Research Network Provincial Collaborative Network Investigators
- 1 Public Health Ontario, Toronto, ON, Canada
- 2 Dalla Lana School of Public Health, University of Toronto, Toronto, ON, Canada
- 3 Centre for Vaccine Preventable Diseases, University of Toronto, Toronto, ON, Canada
- 4 ICES, Toronto, ON, Canada
- 5 Department of Family and Community Medicine, University of Toronto, Toronto, ON, Canada
- 6 MAP Centre for Urban Health Solutions, Li Ka Shing Knowledge Institute, Unity Health Toronto, Toronto, ON, Canada
- 7 School of Public Health, SUNY Downstate Health Sciences University, New York, NY, USA
- 8 International Research Centre of Excellence, Institute of Human Virology Nigeria, Abuja, Nigeria
- 9 Institute of Health Policy, Management and Evaluation, University of Toronto, Toronto, ON, Canada
- 10 Department of Medicine, Temerty Faculty of Medicine, University of Toronto, Toronto, ON, Canada
- 11 Institute of Medical Science, Temerty Faculty of Medicine, University of Toronto, Toronto, ON, Canada
- 12 Department of Pathology and Laboratory Medicine, BC Children’s and Women’s Health Centre, Vancouver, BC, Canada
- 13 University Health Network, Toronto, ON, Canada
- Correspondence to: S Mishra Li Ka Shing Knowledge Institute, Toronto, ON, M5B 1T8, Canada sharmistha.mishra{at}utoronto.ca (or @mishrash on X)
- Accepted 19 August 2024
Objective To estimate the real world effectiveness of modified vaccinia Ankara-Bavarian Nordic (MVA-BN) vaccine against mpox infection.
Design Emulation of a target trial.
Setting Linked databases in Ontario, Canada.
Participants 9803 men aged ≥18 years with a history of being tested for syphilis and a laboratory confirmed bacterial sexually transmitted infection (STI) in the previous year, or who filled a prescription for HIV pre-exposure prophylaxis in the previous year. On each day between 12 June 2022 and 27 October 2022, those who had been vaccinated 15 days previously were matched 1:1 with unvaccinated men by age, geographical region, past HIV diagnosis, number of bacterial STI diagnoses in the previous three years, and receipt of any non-MVA-BN vaccine in the previous year.
Main outcome measure The main outcome measure was vaccine effectiveness ((1–hazard ratio)×100) of one dose of subcutaneously administered MVA-BN against laboratory confirmed mpox infection. A Cox proportional hazards model was used to estimate hazard ratios to compare the rate of laboratory confirmed mpox between the two groups.
Results 3204 men who received the vaccine were matched to 3204 unvaccinated controls. A total of 71 mpox infections were diagnosed, with 0.09 per 1000 person days (95% confidence interval (CI) 0.05 to 0.13) in the vaccinated group and 0.20 per 1000 person days (0.15 to 0.27) in the unvaccinated group over the study period of 153 days. Estimated vaccine effectiveness of one dose of MVA-BN against mpox infection was 58% (95% CI 31% to 75%).
Conclusion The findings of this study, conducted in the context of a targeted vaccination programme and evolving outbreak of mpox, suggest that one dose of MVA-BN is moderately effective in preventing mpox infection.
Introduction
In May 2022, more than 20 countries where mpox had not been previously identified reported infections to the World Health Organization. 1 On 23 July 2022, the global mpox outbreak was declared a public health emergency of international concern, and targeted use of second or third generation smallpox vaccines was recommended for control of the outbreak. 2
Modified vaccinia Ankara-Bavarian Nordic (MVA-BN) vaccine (trade names Imvamune, Jynneos, and Imvanex) is a third generation, live attenuated, non-replicating vaccine against smallpox. 3 In Ontario, Canada, MVA-BN was introduced in June 2022 as post-exposure prophylaxis for high risk contacts (but few doses were given in this context) and pre-exposure prophylaxis for gay, bisexual, and other men who have sex with men, and sex workers at high risk of exposure to mpox. 4 Although MVA-BN is approved in Canada as a series of two doses 28 days apart, Ontario initially employed a dose sparing strategy such that vaccine candidates could only receive one dose owing to concerns about limited vaccine supply. A two dose (0.5 mL each, subcutaneously) programme was subsequently implemented on 30 September 2022.
Before the global mpox outbreak, clinical or real world data on the use of MVA-BN to prevent mpox infection were limited. 5 6 Estimates of the effectiveness of a single dose of MVA-BN obtained using various observational study designs have since emerged in the literature, ranging from 36% to 86%. 7 8 9 10 11 12 13 14 15 As with all observational studies, each report discussed the potential for residual confounding and selection biases. Only one study to date emulated a target trial to address these biases, but it was restricted to HIV negative men who had used HIV pre-exposure prophylaxis. 10 In the current study we estimated the vaccine effectiveness of one dose of MVA-BN against laboratory confirmed mpox infection in a broader population through a target trial emulation to reduce biases.
Study design, setting, and population
We conducted a target trial emulation to answer the causal question of interest (see supplementary figure S1 and table S1) and to reduce biases, particularly from confounding. 16 Laboratory, vaccination, reportable diseases, and health administrative data were used from Ontario (population 15.1 million as of July 2022), which has a single payer healthcare system. All datasets included in the analysis (see supplementary methods) were linked using unique encoded identifiers and analysed at ICES.
The study period captured the beginning of the availability of pre-exposure vaccination (12 June 2022 to 26 November 2022, during which time mpox was diagnosed in 691 people in Ontario; fig 1 , also see supplementary table S2 for Ontario surveillance definitions of mpox). 17 The end date was chosen based on several indicators, including weekly percentage positivity <5% and the last individual with outbreak associated mpox reported on 10 November 2022. 18 Eligibility for single dose, pre-exposure vaccination comprised gay, bisexual, and other men who have sex with men reporting one or more of a diagnosis of bacterial sexually transmitted infection (STI) in the previous two months; currently engaging in or anticipating sex with two or more sexual partners; attending sex-on-premises venues; or engaging in anonymous sex. Eligibility for pre-exposure vaccination also included individuals engaged in sex work, immunocompromised individuals, or pregnant individuals if they were contacts of people at risk, as defined above. 19

Confirmed mpox infections and number of MVA-BN vaccine doses administered by week in Ontario, Canada, 1 May to 25 December 2022. MVA-BN= modified vaccinia Ankara-Bavarian Nordic
- Download figure
- Open in new tab
- Download powerpoint
Because the administrative data do not include information on each of the specific criteria laid out by Ontario’s MVA-BN vaccine programme, we used proxies for potential sexual exposure to mpox to define our eligible population for the trial specification. That is, if a randomised control trial were to be possible but was restricted to using variables available in the health administrative data, our approach to target trial specification would make use of these variables as proxies for sexual activity (see supplementary table S1). Eligibility criteria for the target trial were conceptualised to reduce confounding between vaccination status and risk of subsequent infection. The study population was restricted to men aged ≥18 years as of 12 June 2022 with at least one of the following proxies for risk of exposure to mpox as of the date of matching (ie, time zero, which could occur between 12 June 2022 and 27 October 2022, to ensure each person could have at least 30 days of observation): at least one syphilis test in the previous year and a new diagnosis of one bacterial STI or more (chlamydia, gonorrhoea, or syphilis) in the year before matching; or a filled prescription for HIV pre-exposure prophylaxis in the year before matching (see supplementary table S3 for definitions). We excluded individuals with a documented positive polymerase chain reaction test result for mpox before 12 June 2022.
Intervention and outcome
The intervention of interest was vaccination with a single dose of MVA-BN. We were unable to estimate the effectiveness of a second dose because only a few individuals had received such a dose (13.7% of those who received one dose) by the end of the study period (26 November 2022) and few people received an mpox diagnosis in October and November. The outcome of interest was polymerase chain reaction confirmed mpox infection, based on the specimen collection date. Based on immunogenicity data, an individual was classified as vaccinated >14 days after the first dose. 20
Specification and emulation of the target trial
On each day between 12 June 2022 and 27 October 2022, men who had been vaccinated with a single dose of MVA-BN 15 days previously were matched in a 1:1 ratio to unvaccinated controls. We followed individuals until the earliest date of any of the following events: outcome, death, 15 days after receipt of a first vaccine dose (for unvaccinated controls), 15 days after receipt of a second dose, or end of the study period. Individuals who initially contributed observation time as an unvaccinated control were censored (along with their matched vaccinated individual) 15 days after receipt of MVA-BN and were re-matched as a vaccinated individual with a new unvaccinated control (see supplementary table S1). 21
To balance the distribution of measured baseline covariates that are associated with the probability of vaccination and mpox infection between vaccine recipients and controls, we matched vaccine recipients and controls on age (within five years), geographical region (since the epidemic trajectory and vaccine uptake varied regionally), proxies for sexual exposures (number of bacterial STIs in the previous three years, HIV status), and a proxy for vaccine confidence (receipt of any non-MVA-BN vaccine in the previous year). These covariates were defined using 12 June 2022. The supplementary methods section provides details of the matching algorithm. For vaccinated individuals, time zero was 15 days after vaccination, whereas unvaccinated controls inherited the time zero of the vaccinated person to whom they were matched.
We conducted three sensitivity analyses. To explore the potential for residual confounding by risk of sexual exposures, we used two negative control outcomes that should not be directly affected by the receipt of MVA-BN but for which the effect of vaccination might be confounded. 22 Firstly, we measured the risk of mpox during the first 14 days after the first dose, when no difference between vaccinated and unvaccinated groups would be expected (the negative outcome period). Secondly, we used a negative tracer outcome by estimating vaccine effectiveness against bacterial STI >14 days after vaccination; MVA-BN vaccine presumably has no benefit against infection with chlamydia, gonorrhoea, or syphilis. However, an STI diagnosis could be influenced by differential rates of testing after vaccination. Thus we compared syphilis testing among vaccinated and unvaccinated groups over the study period to aid interpretation of the negative tracer outcome. Finally, we examined the potential for residual confounding related to socioeconomic status by adjusting for income at neighbourhood level, given that sexual networks and infection risks are shaped by systemic barriers to engagement in healthcare and access to vaccines.
Statistical analysis
We examined covariate balance after matching using standardised mean differences, and considered a difference of ≥0.1 as potentially clinically meaningful. 23 Cumulative incidence functions were estimated for the vaccinated and unvaccinated groups and we used a Cox proportional hazards model to estimate the hazard ratio comparing the hazard of mpox between the two groups, using a robust variance estimator to account for the matched design. 24 We calculated vaccine effectiveness as ((1–hazard ratio)×100). Analyses were performed using SAS software version 9.4 (SAS Institute, Cary, NC).
Patient and public involvement
This work was undertaken in response to questions about the effectiveness of MVA-BN by public health, clinical, and community members. Participants were not involved in the original design of this study. We shared study results with diverse community representatives interested in the mpox response.
A total of 9803 men aged ≥18 years were eligible for the study, of whom 272 received a diagnosis of mpox during the study period, including 15 who required hospital admission with mpox. A total of 3204 men who received the vaccine were matched to 3204 unvaccinated controls ( fig 2 ). The matched population was similar to the eligible population for baseline characteristics (see supplementary table S4). All measured variables were well balanced between the vaccinated and unvaccinated groups ( table 1 ). The median age of matched participants was 35 years (interquartile range (IQR) 29-46 years) and more than half of the participants (66.1%) were residents of Toronto.

Cohort enrolment process and selection of individuals for emulation of a target trial evaluating effectiveness of the modified vaccinia Ankara-Bavarian Nordic. OHIP=Ontario Health Insurance Plan; STI=sexually transmitted infection
Personal and sexual risk characteristics of the study population for the target trial emulation design. Values are number (percentage) unless stated otherwise
- View inline
During a median follow-up of 85 days (IQR 32-110 days) after the first dose among vaccinated individuals and 86 (31-111) days among unvaccinated individuals, we observed a total of 71 infections, with 21 in the vaccinated group (0.09 per 1000 person days, 95% confidence interval (CI) 0.05 to 0.13) and 50 in the unvaccinated group (0.20 per 1000 person days, 0.15 to 0.27) over the study period of 153 days. We censored 293 (9.1%) individuals owing to receipt of a second dose. Figure 3 shows the cumulative incidence functions for the vaccinated and unvaccinated groups during the study period. The hazard ratio for infection in the vaccinated group compared with unvaccinated group was 0.42 (95% CI 0.25 to 0.69), thus the estimated vaccine effectiveness for a single dose of MVA-BN against mpox infection was 58% (95% CI 31% to 75%; fig 4 ).

Cumulative incidence functions of confirmed mpox infection in Ontario, Canada, 12 June 2022 to 26 November 2022. Shaded areas represent 95% confidence intervals. *Estimates that could lead to back calculation of small cells have been shown with a range of values instead of the exact value

Estimates of vaccine effectiveness of one dose of MVA-BN between 12 June 2022 and 26 November 2022 in Ontario, Canada, primary and sensitivity analyses. MVA-BN=modified vaccinia Ankara-Bavarian Nordic; STI=sexually transmitted infection
Examination for residual confounding using negative outcomes showed a vaccine effectiveness of –15% (–92% to 31%) during the first 14 days post-vaccination, and vaccine effectiveness of –89% (–125% to –58%) against bacterial STI (see cumulative incidence functions in supplementary figure S2). Rates of a first syphilis test post-vaccination were 0.05 per 1000 person days in the vaccinated group and 0.03 per 1000 person days in the unvaccinated group. Finally, we did not identify a meaningful change in vaccine effectiveness against mpox infection after additionally adjusting for neighbourhood level income (vaccine effectiveness 60%, 34% to 76%).
Using a target trial emulation, we estimated the effectiveness of a single dose of MVA-BN vaccine to be moderate (58%, 31% to 75%) for preventing mpox infection in the context of a targeted vaccination programme in Ontario, Canada. To confirm the specificity of this association, we determined that MVA-BN was not associated with a reduced rate of mpox infection during the first 14 days post-vaccination (before developing an adequate antibody response) nor bacterial STI diagnoses (against which no protection would be expected).
Comparison with other studies
Our estimate of vaccine effectiveness falls within the range observed across previous studies conducted in jurisdictions with similar epidemic dynamics and targeted vaccination programmes. Our findings are most consistent with studies that restricted the study population to those at greatest risk of exposure to mpox and that reduced time based and risk based confounding. 8 10 11 14 15 In the Canadian province of Quebec, a test negative study that used health administrative data and adjusted for exposure risks based on similar proxies as in our study (ie, previous bacterial STI), estimated vaccine effectiveness against mpox infection to be 35% (95% CI 2% to 59%). 14 After further adjusting for self-reported measures of exposure risks (restricting analyses to those who completed a detailed questionnaire), vaccine effectiveness was estimated to be 65% (1% to 87%), similar to our estimate. Our estimate is lower than (but still compatible with) an estimate of 86% (95% CI 59% to 95%) from a retrospective cohort study in Israel that used more restrictive study eligibility criteria (ie, living with HIV and a recent diagnosis of bacterial STI, or receipt of HIV pre-exposure prophylaxis), 8 and an estimate of 79% (95% CI 33% to 100%) from a target trial emulation conducted in Spain with even more restrictive study eligibility (ie, enrolment restricted to men receiving HIV pre-exposure prophylaxis). 10
Strengths and limitations of this study
Our study has several strengths. Firstly, we used linked population based databases within a publicly funded healthcare system to identify all MVA-BN vaccination events and all mpox related laboratory tests in Ontario. Secondly, to address the risks of residual confounding present in any observational study, we conducted rigorous matching across key potential confounders of the causal effect of vaccination on mpox infection. Risk confounding is particularly important when estimating vaccine effectiveness because Ontario, like other jurisdictions, specifically targeted vaccination to individuals at greatest risk of infection. Evidence of exchangeability includes the similarity between groups for proxies of sexual exposure risks, and similar outcomes during the negative control period before the vaccine was expected to confer protection. We examined this negative control period based on immunogenicity data, recognising that some protection may have been conferred in the first 14 days, if the dose was administered deliberately or inadvertently within the window for post-exposure prophylaxis. 25 26 The negative tracer outcome analysis involving bacterial STI suggests that the observed vaccine effect is unlikely to be explained by differential reductions in sexual activity among gay, bisexual, and other men who have sex with men over the study period. In contrast, our finding of higher rates of newly diagnosed bacterial STIs among vaccinated men suggests that the vaccination programme successfully reached those most at risk of mpox and/or vaccinated men engaged in increased sexual activity post-vaccination. This means that vaccinated individuals may have engaged in more sexual activity than their unvaccinated counterparts after vaccination. Indeed, given the focus of vaccine campaign messaging on preventing future exposure risks, individual decisions about the vaccine could be shaped by anticipating future sexual partnerships, irrespective of the past. The higher rates of bacterial STIs post-vaccination could also stem from additional STI testing opportunities and detection after engagement in preventive care with vaccination, as evidenced by higher syphilis testing rates during the post-vaccination period. However, the negative tracer findings suggest that residual confounding could be present due to differential increases in sexual activity, and thus our estimate of vaccine effectiveness may be underestimated. Finally, the study period included a rapidly evolving outbreak, with risks of exposure to mpox declining quickly before a large fraction of the study eligible population was vaccinated, thus the risk for time varying confounding due to differential exposure risks was substantial, which we reduced by emulating a target trial.
Our study also has limitations. Firstly, the rigorous matching meant that our final cohort comprised only 65% of the eligible population, with 71 outcomes for analysis. Thus, the final cohort comprised 8.8% of the 36 312 first dose vaccinations and 10% of all mpox diagnoses in Ontario during the study period. Although the characteristics of included and eligible participants were similar, a reduction in confounding came at the price of decreased sample size and precision. It also meant that subgroup analyses, such as among individuals aged >50 years, who may have received earlier generation smallpox vaccines, were not possible. Secondly, we were limited to routinely collected data, and information on previous smallpox vaccination, sexual exposures, and individual level measures of social determinants of health were not available. Information on neighbourhood level income was available but was not used for matching to limit further loss of sample size, and because area level median income may not capture the ways in which individual level income, or other individual level social determinants, might influence sexual networks. 27 Furthermore, comparison across groups and the third sensitivity analysis suggested no residual confounding by neighbourhood level income. Thirdly, although we included men with a history of bacterial STIs, our study eligibility population could be missing men who are at risk of mpox infection but have negligible access to healthcare and/or healthcare engagement (thus leading to a selection bias). Fourthly, although data from other studies showed added protective benefit of two vaccine doses, 9 11 12 we could not evaluate the two dose regimen because of low second dose coverage during the study period, nor could we evaluate duration of protection. Finally, vaccination could also reduce symptoms and signs of mpox and thus result in less testing, 28 which would mean a higher chance of under-ascertainment of people with subclinical infection among the vaccinated group, which would lead to overestimation of vaccine effectiveness against infection.
Conclusions
Vaccination with a single dose of MVA-BN vaccine was found to be moderately effective against laboratory confirmed mpox infection in this population based study of an evolving outbreak and using a target trial emulation to reduce biases. One implication of our finding is that single dose vaccination may have been a contributing factor in helping to slow transmission in Ontario in 2022. Mpox infections in Canada and across the globe are rising again in 2024, with most diagnoses among individuals who have not yet been vaccinated or have received only a single dose of vaccine. 29 30 Given the moderate effectiveness of a single dose, achieving high coverage with a full course could be important to prevent and manage ongoing transmission globally and prevent a large resurgence. 31 32 In the absence of randomised clinical trials, our findings strengthen the evidence that MVA-BN is effective at preventing mpox infection and should be made available and accessible to communities at risk.
What is already known on this topic
No randomised clinical trials of vaccination against mpox have been conducted
Estimates of vaccine effectiveness of a single dose of vaccination range from 36% to 86%, but these observational designs noted residual confounding as a major concern given vaccine implementation was appropriately prioritised to individuals most at risk of infection
Estimates of vaccine effectiveness, using approaches to minimise biases, are needed
What this study adds
In an emulated target trial to reduce biases, the effectiveness of a single dose of modified vaccinia Ankara-Bavarian Nordic (MVA-BN) vaccine against mpox infection was 58% (95% confidence interval 31% to 75%)—a finding that was robust to further sensitivity analysis for residual confounding
In the absence of data from randomised controlled trials, the study findings strengthen the evidence that MVA-BN is effective at preventing mpox infection and should be made available and accessible to communities at risk
Ethics statements
Ethical approval.
ICES is a prescribed entity under Ontario’s Personal Health Information Protection Act (PHIPA). Section 45 of PHIPA authorises ICES to collect personal health information, without consent, for the purpose of analysis or compiling statistical information with respect to the management of, evaluation or monitoring of, the allocation of resources to or planning for all or part of the health system. Projects that use data collected by ICES under section 45 of PHIPA, and use no other data, are exempt from REB review. The use of the data in this project is authorised under section 45 and approved by ICES’ Privacy and Legal Office. Ethical approval for this study was obtained from Public Health Ontario’s Ethics Review Board.
Data availability statement
The dataset from this study is held securely in coded form at ICES. While legal data sharing agreements between ICES and data providers (eg, healthcare organisations and government) prohibit ICES from making the dataset publicly available, access may be granted to those who meet prespecified criteria for confidential access, available at https://www.ices.on.ca/DAS (email [email protected] ). The full dataset creation plan and underlying analytical code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification. Correspondence and requests for materials should be addressed to JCK or SM.
Acknowledgments
We acknowledge colleagues at Public Health Ontario for access to vaccination data from the Digital Health Information Repository, case level data from the integrated Public Health Information System, and laboratory data from LabWare. We also thank the staff of Ontario’s public health units who are responsible for mpox case and contact management and data collection. We acknowledge the work of more than 30 community based organisations across Ontario who led vaccine mobilisation and implementation with public health units and healthcare providers. This document used data adapted from the Statistics Canada Postal Code Conversion File, which is based on data licensed from Canada Post Corporation, and/or data adapted from the Ontario Ministry of Health Postal Code Conversion File, which contains data copied under license from Canada Post Corporation and Statistics Canada. Parts of this material are based on data and/or information compiled and provided by the Ontario Ministry of Health, Canadian Institute for Health Information, Statistics Canada, and IQVIA Solutions Canada. The analyses, conclusions, opinions, and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred. Adapted from Statistics Canada, Canadian Census 2016. This does not constitute an endorsement by Statistics Canada of this product. We thank IQVIA Solutions Canada for use of their Drug Information File. Finally, we thank Nicholas Brousseau and Sara Carazo Perez, Institut national de santé publique du Québec, for helpful discussions about methodological approaches and confounders.
Contributors: JCK and SM designed the study and analysis plan and are joint senior authors with equal contribution. SAB, CN, JCK, and LF acquired the data for the work. CL designed the data extraction and assembly workflow. CL analysed the data. All authors made substantial contributions to the analysis plan and the interpretation of the data. JCK and SM vouch for the data analysis. CN, SM, and JCK wrote the first draft of the manuscript. All authors critically reviewed the manuscript and decided to proceed with publication. SM and JCK are responsible for the overall content as guarantors and accept full responsibility for the work and conduct of the study and had access to the data and controlled the decision to publish. The corresponding authors attest that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and the Ministry of Long-Term Care. This study also received funding from the Canadian Immunization Research Network through a grant from the Public Health Agency of Canada and the Canadian Institutes of Health Research (CNF 151944). The Canada-Africa Mpox Partnership, of which this study is one component, was also supported by the Canadian Institutes of Health Research Rapid Mpox Research (MRR-184812). The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding sources. Funders had no role in the design or conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. JCK is supported by a clinician-scientist award and ANB is supported by a non-clinician scientist award from the University of Toronto Department of Family and Community Medicine. SM, DT, and ANB are supported by Tier 2 Canada Research Chairs.
Competing interests: All authors have completed the ICMJE uniform disclosure form at https://www.icmje.org/disclosure-of-interest/ and declare: support from ICES and the Canadian Immunization Research Network; no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Transparency: The corresponding author (the manuscript’s guarantor) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: Preliminary results of this study have been made available to the public on a preprint server and have been shared with the Ministry of Health and ICES. After peer review publication, they will be further disseminated by ICES through news media and social media. It is not possible to send study results to participants because all personal identifying information has been removed from the dataset.
Provenance and peer review: Not commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- ↵ World Health Organization. Disease Outbreak News; Multi-country monkeypox outbreak in non-epidemic countries: Update; 2022 [cited 14 Aug 2024]. https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON388
- ↵ World Health Organization. Second meeting of the International Health Regulations (2005) (IHR) Emergency Committee regarding the multi-country outbreak of monkeypox. Geneva, Switzerland: World Health Organization; 2022 [cited 14 Aug 2024]. https://www.who.int/news/item/23-07-2022-second-meeting-of-the-international-health-regulations-(2005)-(ihr)-emergency-committee-regarding-the-multi-country-outbreak-of-monkeypox
- ↵ Public Health Agency of Canada. Smallpox and mpox (monkeypox) vaccine: Canadian Immunization Guide. Ottawa, Ontario: King’s Printer for Canada; 2024 [cited 14 Aug 2024]. https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-4-active-vaccines/page-21-smallpox-vaccine.html
- ↵ Ontario Ministry of Health. Mpox Vaccine (Imvamune®) Guidance for Health Care Providers, Version 3.1. Queen’s Printer for Ontario, 2022.
- ↵ United Kingdom Health Security Agency. Green Book Chapter 29: Smallpox and monkeypox. England, UK: Her Majesty’s Stationery Office; 2022 [cited 14 Aug 2024]. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1106454/Green-Book-chapter-29_Smallpox-and-monkeypox_26September2022.pdf
- ↵ Public Health Agency of Canada. An Advisory Committee Statement (ACS) National Advisory Committee on Immunization (NACI) NACI Rapid Response – Interim guidance on the use of Imvamune® in the context of monkeypox outbreaks in Canada. Ottawa, Ontario: Queen’s Publisher of Canada; 2022 [cited 14 Aug 2024]. https://www.canada.ca/content/dam/phac-aspc/documents/services/immunization/national-advisory-committee-on-immunization-naci/guidance-imvamune-monkeypox/guidance-imvamune-monkeypox-en.pdf
- Wolff Sagy Y ,
- Hammerman A ,
- Rosenberg ES ,
- Dorabawila V ,
- Hart-Malloy R ,
- Fontan-Vela M ,
- Hernando V ,
- Deputy NP ,
- Deckert J ,
- Dalton AF ,
- Diallo AO ,
- CDC Multijurisdictional Mpox Case-Control Study Group ,
- CDC Multijurisdictional Mpox Case Control Study Group
- Charles H ,
- Thorley K ,
- Brousseau N ,
- Febriani Y ,
- Bertran M ,
- Andrews N ,
- Davison C ,
- Hernán MA ,
- ↵ Ontario Ministry of Health. Appendix 1: Case Definitions and Disease-Specific Information. Disease: Smallpox and other Orthopoxviruses including mpox. Toronto, Ontario: King’s Printer for Ontario; 2024 [cited 14 Aug 2024]. https://www.ontario.ca/files/2024-04/moh-ophs-smallpox-en-2024-04-01.pdf
- Zygmunt A ,
- Saunders A ,
- Navarro C ,
- Collinson S
- ↵ Ontario Ministry of Health. Monkeypox vaccine (Imvamune®) Guidance for Health Care Providers, Version 2.1. Queen’s Printer for Ontario, 2022.
- Pittman PR ,
- Lipsitch M ,
- Tchetgen Tchetgen E ,
- Arciuolo RJ ,
- Pathela P ,
- Montero Morales L ,
- Barbas Del Buey JF ,
- Alonso García M ,
- Madrid Surveillance Network and Vaccination Centre of Madrid Region
- Abuelezam NN ,
- Reshef YA ,
- SHARE-NET writing group
- ↵ US Centers for Disease Control and Prevention. U.S. Mpox Case Trends Reported to CDC. Atlanta, Georgia: US Centers for Disease Control and Prevention; 2024 [cited 14 Aug 2024]. https://www.cdc.gov/poxvirus/mpox/response/2022/mpx-trends.html
- ↵ Ontario Agency for Health Protection and Promotion (PHO). Enhanced epidemiological summary: Mpox in Ontario: 1 Jan 2023 to 31 May 2024. Toronto, Ontario: King’s Printer for Ontario; 2024. https://www.publichealthontario.ca/-/media/Documents/M/24/mpox-ontario-epi-summary.pdf?rev=a8a6a202096242d891ef521e00e05603&sc_lang=en )
- Sachdeva H ,
- ↵ World Health Organization Regional Office for Europe. An mpox resurgence in the European Region this spring and summer? To prevent that, key measures must continue; 2023 [cited 14 Aug 2024]. https://www.who.int/europe/news/item/17-05-2023-an-mpox-resurgence-in-the-european-region-this-spring-and-summer--to-prevent-that--key-measures-must-continue
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 10 September 2024
Restorative dentistry
Is SDF better than the SMART (silver modified atraumatic restorative technique) in the management of molar incisor hypomineralisation molars with initial caries?
- Meenakshi Lall 1
Evidence-Based Dentistry ( 2024 ) Cite this article
12 Accesses
Metrics details
- Caries sealants
- Dental caries
- Glass-ionomer cement
A prospective, randomized, split-mouth clinical study by the two previously trained and calibrated pediatric dentists without blinding operators and patients due to different protocols in both treatment groups. An SDF + potassium iodide (KI) and SDF + KI + glass ionmer cement (GIC) on International Caries Detection and Assessment System (ICDAS) 1/2 molar was received by each patient on either side of mouth. The local Ethics Committee approved this study.
Data source
Sample size calculation was not performed due to the lack of published studies on the longevity of SMART sealant on MIH-affected molars and the absence of research on the apparent difference between the effectiveness of SMART and SDF treatments in preventing further caries and sensitivity.
Study selection
These were children between the ages of 6 years to 13 years, who visited the Pediatric Dentistry Clinic at XX University School of Dentistry for routine exams and treatment between July 2019 to May 2020. They were in good health and had at least two fully erupted permanent first molars with MIH as per the European Academy of Pediatric Dentistry, ICDAS code 1/2. This study recorded 12 months of treatment outcomes on hypomineralised molars of 48 children with a follow-up of three years. Children were excluded with specific syndromes associated with enamel malformation, lack of cooperation, ongoing orthodontic treatment, and teeth with ICDAS 3/4/5/6 lesions, existing restorations, fluorosis, or pulpal symptoms.
Data analysis
Mann-Whitney U Test was used to assess differences between independent groups (SDF and SMART) and the Friedman Test between dependent groups at different time points. Kaplan-Meier analysis to evaluate the cumulative survival of SMART sealants and survival of caries-free hypomineralised molars in both groups. Chi-Square test was used to compare the success percentages of the SDF and SMART groups. To assess the changes in success percentages at three different time intervals for the caries preventive effect of SDF and SMART, and to evaluate the retention percentages for the SMART group. McNemar’s test with a Bonferroni correction was used for significant differences. Cohen’s kappa test indicated that the inter-examiner reliability determining the presence of MIH was 0.87. The intra-examiner reliability for US Public Health Service (USPHS)-Modified criteria was 0.90. The statistical significance level was set at p < 0.05 for all statistical analyses.
At 12, 24 and 36 months the caries preventive effect was 100%, 67.9%, and 65.4% for SDF + KI-treated teeth; and 100%, 97.6%, and 94.7% for SMART (SDF + KI + GIC) respectively. During the recall period, there was no substantial difference in hypersensitivity scores between the groups. There was no hypersensitivity in teeth at 18 months and beyond. Compared to the baseline Schiff Cold Air Sensitivity Scale (SCASS) score 26 molar with initial hypersensitivity to hypomineralisation had a massive reduction at evaluation periods. The mean survival probabilities for the caries-preventive effect were considerably lower in SDF + KI-treated teeth (31.01 months) than in SMART-treated teeth (35.61 months) (p < 0.001).
Considering the limitation of the study, both SMART (SDF + KI + GIC) sealants and 6-monthly application of SDF + KI, provided similar and substantial levels of desensitisation on the permanent MIH molars. When used as a sealing material on non-cavitated permanent MIH molars, the clinical retention rate for SMART was 88.7%, 73.1%, and 66.6% at 1, 2, and 3 years respectively. The caries preventive effect of SMART (SDF + KI + GIC) sealants was superior to SDF + KI application in hypomineralised teeth, however, a long-term monitoring and review is essential due to the gradual decrease in retention of SMART sealants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
251,40 € per year
only 62,85 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Weerheijm KL, Duggal M, Mejàre I, Papagiannoulis L, Koch G, Martens LC, et al. Judgement criteria for molar incisor hypomineralisation (MIH) in epidemiologic studies: a summary of the European meeting on MIH held in Athens, 2003. Eur J Paediatr Dent. 2003;4:110–3.
PubMed CAS Google Scholar
Fagrell TG, Dietz W, Jälevik B, Norén JG. Chemical, mechanical and morphological properties of hypomineralized enamel of permanent first molars. Acta Odontol Scand. 2010;68:215–22.
Article PubMed CAS Google Scholar
Jälevik B, Dietz W, Norén JG. Scanning electron micrograph analysis of hypomineralized enamel in permanent first molars. Int J Paediatr Dent. 2005;15:233–40.
Article PubMed Google Scholar
Farah R, Drummond B, Swain M, Williams S. Linking the clinical presentation of molar-incisor hypomineralisation to its mineral density. Int J Paediatr Dent. 2010;20:353–60.
Lygidakis NA, Garot E, Somani C, Taylor GD, Rouas P, Wong FSL. Best clinical practice guidance for clinicians dealing with children presenting with molar-incisor-hypomineralisation (MIH): an updated European Academy of Paediatric Dentistry policy document. Eur Arch Paediatr Dent. 2022;23:3–21.
de Oliveira DC, Favretto CO, Cunha RF. Molar incisor hypomineralization: considerations about treatment in a controlled longitudinal case. J Indian Soc Pedod Prev Dent. 2015;33:152–5.
Unverdi GE, Ballikaya E, Cehreli ZC. Clinical comparison of silver diamine fluoride (SDF) or silver-modified atraumatic restorative technique (SMART) on hypomineralised permanent molars with initial carious lesions: 3-year results of a prospective, randomised trial. J Dent. 2024;147:105098.
Article Google Scholar
Fragelli CMB, Souza JF, Bussaneli DG, Jeremias F, Santos-Pinto LD, Cordeiro RCL. Survival of sealants in molars affected by molar-incisor hypomineralization: 18-month follow-up. Braz Oral Res. 2017;31:e30.
Bekes K, Amend S, Priller J, Zamek C, Stamm T, Krämer N. Hypersensitivity relief of MIH-affected molars using two sealing techniques: a 12-week follow-up. Clin Oral Investig. 2022;26:1879–88.
Schraverus MS, Olegário IC, Bonifácio CC, González APR, Pedroza M, Hesse D. Glass ionomer sealants can prevent dental caries but cannot prevent posteruptive breakdown on molars affected by molar incisor hypomineralization: one-year results of a randomized clinical trial. Caries Res. 2021;55:301–9.
Ruff RR, Barry-Godín T, Niederman R. Effect of silver diamine fluoride on caries arrest and prevention: the carried away school-based randomized clinical trial. JAMA Netw Open. 2023;6:e2255458.
Article PubMed PubMed Central Google Scholar
Erbas Unverdi G, Ballikaya E, Cehreli ZC. Clinical comparison of silver diamine fluoride (SDF) or silver-modified atraumatic restorative technique (SMART) on hypo mineralised permanent molars with early diagnosis and management to initial carious lesions: 3-year results of a prospective, Early diagnosis and management to randomised trial. J Dent. 2024;147:105098.
Download references
Author information
Authors and affiliations.
Stourcote Dental Practice, Stourbridge, Birmingham, DY8 1TS, UK
Meenakshi Lall
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Meenakshi Lall .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Lall, M. Is SDF better than the SMART (silver modified atraumatic restorative technique) in the management of molar incisor hypomineralisation molars with initial caries?. Evid Based Dent (2024). https://doi.org/10.1038/s41432-024-01062-y
Download citation
Received : 31 July 2024
Accepted : 02 August 2024
Published : 10 September 2024
DOI : https://doi.org/10.1038/s41432-024-01062-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

The library building will be open from 9:00am-3:00pm on Friday, March 29th. Our services will be available online 7:45am-4:30pm for your convenience.
- University of Wisconsin-Superior
- Jim Dan Hill Library
- Help Guides
- TRIO McNair Undergraduate Research Guide
- Limitations of the Study
TRIO McNair Undergraduate Research Guide: Limitations of the Study
- Purpose of Guide
- Design Flaws to Avoid
- Glossary of Research Terms
- Ethics of Research
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Expanding the Timeliness of a Topic Idea
- Writing a Research Proposal
- Academic Writing Style
- Choosing a Title
- Making an Outline
- Paragraph Development
- The Abstract
- Background Information
- The Research Problem/The Question
- Theoretical Framework
- Citation Mining
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tertiary Sources
- Scholarly v. Popular Sources
- Qualitative Methods
- Quantitative Methods
- Using Non-Textual Elements
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Annotated Bibliography
- Preparing Your Poster
- Dealing with Nervousness
- Using Visual Aids
- Peer Review Process
- Informed Consent
- Writing Field Notes
The limitations of the study are those characteristics of design or methodology that impacted or influenced the application or interpretation of the results of your study. They are the constraints on generalizability and utility of findings that are the result of the ways in which you chose to design the study and/or the method used to establish internal and external validity.
Importance of...
Always acknowledge a study's limitations. It is far better for you to identify and acknowledge your study’s limitations than to have them pointed out by your professor and be graded down because you appear to have ignored them.
Keep in mind that acknowledgement of a study's limitations is an opportunity to make suggestions for further research . If you do connect your study's limitations to suggestions for further research, be sure to explain the ways in which these unanswered questions may become more focused because of your study.
Acknowledgement of a study's limitations also provides you with an opportunity to demonstrate to your professor that you have thought critically about the research problem, understood the relevant literature published about it, and correctly assessed the methods chosen for studying the problem. A key objective of the research process is not only discovering new knowledge but also to confront assumptions and explore what we don't know.
Claiming limitations is a subjective process because you must evaluate the impact of those limitations. Don't just list key weaknesses and the magnitude of a study's limitations. To do so diminishes the validity of your research because it leaves the reader wondering whether, or in what ways, limitation(s) in your study may have impacted the findings and conclusions. Limitations require a critical, overall appraisal and interpretation of their impact. You should answer the question: do these problems with errors, methods, validity, etc. eventually matter and, if so, to what extent?
Structure: How to Structure the Research Limitations Section of Your Dissertation . Dissertations and Theses: An Online Textbook. Laerd.com.
Descriptions of Possible Limitations
All studies have limitations. However, it is important that you restrict your discussion to limitations related to the research problem under investigation. For example, if a meta-analysis of existing literature is not a stated purpose of your research, it should not be discussed as a limitation. Do not apologize for not addressing issues that you did not promise to investigate in your paper.
Here are examples of limitations you may need to describe and to discuss how they possibly impacted your findings. Descriptions of limitations should be stated in the past tense.
Possible Methodological Limitations
Sample size -- the number of the units of analysis you use in your study is dictated by the type of research problem you are investigating. Note that, if your sample size is too small, it will be difficult to find significant relationships from the data, as statistical tests normally require a larger sample size to ensure a representative distribution of the population and to be considered representative of groups of people to whom results will be generalized or transferred.
Lack of available and/or reliable data -- a lack of data or of reliable data will likely require you to limit the scope of your analysis, the size of your sample, or it can be a significant obstacle in finding a trend and a meaningful relationship. You need to not only describe these limitations but to offer reasons why you believe data is missing or is unreliable. However, don’t just throw up your hands in frustration; use this as an opportunity to describe the need for future research.
Lack of prior research studies on the topic -- citing prior research studies forms the basis of your literature review and helps lay a foundation for understanding the research problem you are investigating. Depending on the currency or scope of your research topic, there may be little, if any, prior research on your topic. Before assuming this to be true, consult with a librarian! In cases when a librarian has confirmed that there is a lack of prior research, you may be required to develop an entirely new research typology [for example, using an exploratory rather than an explanatory research design]. Note that this limitation can serve as an important opportunity to describe the need for further research.
Measure used to collect the data -- sometimes it is the case that, after completing your interpretation of the findings, you discover that the way in which you gathered data inhibited your ability to conduct a thorough analysis of the results. For example, you regret not including a specific question in a survey that, in retrospect, could have helped address a particular issue that emerged later in the study. Acknowledge the deficiency by stating a need in future research to revise the specific method for gathering data.
Self-reported data -- whether you are relying on pre-existing self-reported data or you are conducting a qualitative research study and gathering the data yourself, self-reported data is limited by the fact that it rarely can be independently verified. In other words, you must take what people say, whether in interviews, focus groups, or on questionnaires, at face value. However, self-reported data contain several potential sources of bias that should be noted as limitations: (1) selective memory (remembering or not remembering experiences or events that occurred at some point in the past); (2) telescoping [recalling events that occurred at one time as if they occurred at another time]; (3) attribution [the act of attributing positive events and outcomes to one's own agency but attributing negative events and outcomes to external forces]; and, (4) exaggeration [the act of representing outcomes or embellishing events as more significant than is actually suggested from other data].
Possible Limitations of the Researcher
Access -- if your study depends on having access to people, organizations, or documents and, for whatever reason, access is denied or otherwise limited, the reasons for this need to be described.
Longitudinal effects -- unlike your professor, who can devote years [even a lifetime] to studying a single research problem, the time available to investigate a research problem and to measure change or stability within a sample is constrained by the due date of your assignment. Be sure to choose a topic that does not require an excessive amount of time to complete the literature review, apply the methodology, and gather and interpret the results. If you're unsure, talk to your professor.
Cultural and other types of bias -- we all have biases, whether we are conscience of them or not. Bias is when a person, place, or thing is viewed or shown in a consistently inaccurate way. It is usually negative, though one can have a positive bias as well. When proof-reading your paper, be especially critical in reviewing how you have stated a problem, selected the data to be studied, what may have been omitted, the way you have ordered events, people, or places and how you have chosen to represent a person, place, or thing, to name a phenomenon, or to use possible words with a positive or negative connotation. Note that if you detect bias in prior research, it must be acknowledged, and you should explain what measures were taken to avoid perpetuating bias.
Fluency in a language -- if your research focuses on measuring the perceived value of after-school tutoring among Mexican American ESL [English as a Second Language] students, for example, and you are not fluent in Spanish, you are limited in being able to read and interpret Spanish language research studies on the topic. This deficiency should be acknowledged.
Brutus, Stéphane et al. Self-Reported Limitations and Future Directions in Scholarly Reports: Analysis and Recommendations. Journal of Management 39 (January 2013): 48-75; Senunyeme, Emmanuel K. Business Research Methods . Powerpoint Presentation. Regent University of Science and Technology.
Structure and Writing Style
Information about the limitations of your study is generally placed either at the beginning of the discussion section of your paper so the reader knows and understands the limitations before reading the rest of your analysis of the findings, or the limitations are outlined at the conclusion of the discussion section as an acknowledgement of the need for further study. Statements about a study's limitations should not be buried in the body [middle] of the discussion section unless a limitation is specific to something covered in that part of the paper. If this is the case, though, the limitation should be reiterated at the conclusion of the section.
If you determine that your study is seriously flawed due to important limitations, such as an inability to acquire critical data, consider reframing it as a pilot study intended to lay the groundwork for a more complete research study in the future. Be sure, though, to specifically explain the ways that these flaws can be successfully overcome in later studies.
But do not use this as an excuse for not developing a thorough research paper! Review the tab in this guide for developing a research topic. If serious limitations exist, it generally indicates a likelihood that your research problem is too narrowly defined or that the issue or event under study is too recent and, thus, very little research has been written about it. If serious limitations do emerge, consult with your professor about possible ways to overcome them or how to reframe your study.
When discussing the limitations of your research, be sure to:
Describe each limitation in detailed but concise terms;
Explain why each limitation exists;
Provide the reasons why each limitation could not be overcome using the method(s) chosen to gather the data [cite to other studies that had similar problems when possible];
Assess the impact of each limitation in relation to the overall findings and conclusions of your study; and,
If appropriate, describe how these limitations could point to the need for further research.
Remember that the method you chose may be the source of a significant limitation that has emerged during your interpretation of the results [for example, you didn't ask a particular question in a survey that you later wish you had]. If this is the case, don't panic. Acknowledge it and explain how applying a different or more robust methodology might address the research problem more effectively in any future study. An underlying goal of scholarly research is not only to prove what works, but to demonstrate what doesn't work or what needs further clarification.
Brutus, Stéphane et al. Self-Reported Limitations and Future Directions in Scholarly Reports: Analysis and Recommendations. Journal of Management 39 (January 2013): 48-75; Ioannidis, John P.A. Limitations are not Properly Acknowledged in the Scientific Literature. Journal of Clinical Epidemiology 60 (2007): 324-329; Pasek, Josh. Writing the Empirical Social Science Research Paper: A Guide for the Perplexed . January 24, 2012. Academia.edu; Structure: How to Structure the Research Limitations Section of Your Dissertation . Dissertations and Theses: An Online Textbook. Laerd.com; What Is an Academic Paper? Institute for Writing Rhetoric. Dartmouth College; Writing the Experimental Report: Methods, Results, and Discussion. The Writing Lab and The OWL. Purdue University.
Writing Tip
Don't Inflate the Importance of Your Findings! After all the hard work and long hours devoted to writing your research paper, it is easy to get carried away with attributing unwarranted importance to what you’ve done. We all want our academic work to be viewed as excellent and worthy of a good grade, but it is important that you understand and openly acknowledge the limitations of your study. Inflating the importance of your study's findings in an attempt to hide its flaws is a big turn off to your readers. A measure of humility goes a long way!
Another Writing Tip
Negative Results are Not a Limitation!
Negative evidence refers to findings that unexpectedly challenge rather than support your hypothesis. If you didn't get the results you anticipated, it may mean your hypothesis was incorrect and needs to be reformulated, or perhaps you have stumbled onto something unexpected that warrants further study. Moreover, the absence of an effect may be very telling in many situations, particularly in experimental research designs. In any case, your results may be of importance to others even though they did not support your hypothesis. Do not fall into the trap of thinking that results contrary to what you expected is a limitation to your study. If you carried out the research well, they are simply your results and only require additional interpretation.
Yet Another Writing Tip
A Note about Sample Size Limitations in Qualitative Research
Sample sizes are typically smaller in qualitative research because, as the study goes on, acquiring more data does not necessarily lead to more information. This is because one occurrence of a piece of data, or a code, is all that is necessary to ensure that it becomes part of the analysis framework. However, it remains true that sample sizes that are too small cannot adequately support claims of having achieved valid conclusions and sample sizes that are too large do not permit the deep, naturalistic, and inductive analysis that defines qualitative inquiry. Determining adequate sample size in qualitative research is ultimately a matter of judgment and experience in evaluating the quality of the information collected against the uses to which it will be applied, and the particular research method and purposeful sampling strategy employed. If the sample size is found to be a limitation, it may reflect your judgement about the methodological technique chosen [e.g., single life history study versus focus group interviews] rather than the number of respondents used.
Huberman, A. Michael and Matthew B. Miles. Data Management and Analysis Methods. In Handbook of Qualitative Research. Norman K. Denzin and Yvonna S. Lincoln, eds. (Thousand Oaks, CA: Sage, 1994), pp. 428-444.
- << Previous: The Discussion
- Next: The Conclusion >>

COMMENTS
Common types of limitations and their ramifications include: Theoretical: limits the scope, depth, or applicability of a study. Methodological: limits the quality, quantity, or diversity of the data. Empirical: limits the representativeness, validity, or reliability of the data. Analytical: limits the accuracy, completeness, or significance of ...
Possible Limitations of the Researcher. Access-- if your study depends on having access to people, organizations, data, or documents and, for whatever reason, access is denied or limited in some way, the reasons for this needs to be described.Also, include an explanation why being denied or limited access did not prevent you from following through on your study.
Limitations in Research. Limitations in research refer to the factors that may affect the results, conclusions, and generalizability of a study.These limitations can arise from various sources, such as the design of the study, the sampling methods used, the measurement tools employed, and the limitations of the data analysis techniques.
In research, studies can have limitations such as limited scope, researcher subjectivity, and lack of available research tools. Acknowledging the limitations of your study should be seen as a strength. It demonstrates your willingness for transparency, humility, and submission to the scientific method and can bolster the integrity of the study.
Research limitations are one of those things that students tend to avoid digging into, and understandably so. No one likes to critique their own study and point out weaknesses. Nevertheless, being able to understand the limitations of your study - and, just as importantly, the implications thereof - a is a critically important skill. In this post, we'll unpack some of the most common ...
sentence tha. signals what you're about to discu. s. For example:"Our study had some limitations."Then, provide a concise sentence or two identifying each limitation and explaining how the limitation may have affected the quality. of the study. s findings and/or their applicability. For example:"First, owing to the rarity of the ...
Writing the limitations of the research papers is often assumed to require lots of effort. However, identifying the limitations of the study can help structure the research better. Therefore, do not underestimate the importance of research study limitations. 3. Opportunity to make suggestions for further research.
Methodology limitations. Not having access to data or reliable information can impact the methods used to facilitate your research. A lack of data or reliability may limit the parameters of your study area and the extent of your exploration. Your sample size may also be affected because you won't have any direction on how big or small it ...
How scientists present them can make a big difference. iStock, Jacob Wackerhausen. Scientists work with many different limitations. First and foremost, they navigate informational limitations, work around knowledge gaps when designing studies, formulating hypotheses, and analyzing data. They also handle technical limitations, making the most of ...
3. Identify your limitations of research and explain their importance. 4. Provide the necessary depth, explain their nature, and justify your study choices. 5. Write how you are suggesting that it is possible to overcome them in the future. Limitations can help structure the research study better.
Limited by our limitations. Study limitations represent weaknesses within a research design that may influence outcomes and conclusions of the research. Researchers have an obligation to the academic community to present complete and honest limitations of a presented study. Too often, authors use generic descriptions to describe study limitations.
Step 1. Identify the limitation (s) of the study. This part should comprise around 10%-20% of your discussion of study limitations. The first step is to identify the particular limitation (s) that affected your study. There are many possible limitations of research that can affect your study, but you don't need to write a long review of all ...
Acknowledgement of a study's limitations also provides you with an opportunity to demonstrate that you have thought critically about the research problem, understood the relevant literature published about it, and correctly assessed the methods chosen for studying the problem. A key objective of the research process is not only discovering new ...
The limitations of the study are those characteristics of design or methodology that impacted or influenced the application or interpretation of the results of your study. They are the constraints on generalizability and utility of findings that are the result of the ways in which you chose to design the study and/or the method used to ...
While each study will have its own unique set of limitations, some limitations are more common in quantitative research, and others are more common in qualitative research. In quantitative research, common limitations include the following: - Participant dropout. - Small sample size, low power. - Non-representative sample.
Research Limitations. Research limitations are, at the simplest level, the weaknesses of the study, based on factors that are often outside of your control as the researcher. These factors could include things like time, access to funding, equipment, data or participants.For example, if you weren't able to access a random sample of participants for your study and had to adopt a convenience ...
A large body of work recognizes the effect(s) and consequence(s) of limitations. 1-77 Other than the ones known to the author(s), unknown and unrecognized limitations influence research credibility. This study and analysis aim to determine how frequently and what limitations are found in peer-reviewed open-access medical articles for ...
The ideal way is to divide your limitations section into three steps: 1. Identify the research constraints; 2. Describe in great detail how they affect your research; 3. Mention the opportunity for future investigations and give possibilities. By following this method while addressing the constraints of your research, you will be able to ...
Answer: The limitations of a study are its flaws or shortcomings which could be the result of unavailability of resources, small sample size, flawed methodology, etc. No study is completely flawless or inclusive of all possible aspects. Therefore, listing the limitations of your study reflects honesty and transparency and also shows that you ...
Abstract. Study limitations represent weaknesses within a research design that may influence outcomes and conclusions of the research. Researchers have an obligation to the academic community to present complete and honest limitations of a presented study. Too often, authors use generic descriptions to describe study limitations.
Research limitations in a typical dissertation may relate to the following points: 1. Formulation of research aims and objectives. You might have formulated research aims and objectives too broadly. You can specify in which ways the formulation of research aims and objectives could be narrowed so that the level of focus of the study could be ...
For instance, a study involving females only or carried out in a specific town can have limitations like sample size, gender, and location. What's more, the entire study could be limited to the researcher's perception. Lack of or inadequate training: The research process doesn't have a systematic methodology.
One of the key defining characteristics of rapid qualitative research and evaluation is their iterative design (Beebe, 2001, McNall et al., 2004).The term 'iterative' refers to a repetitive, circular, constantly changing research process where 'cycles' or 'loops' are used to generate evidence, reflect on the findings, obtain feedback, and inform changes in the original study design.
The average readability of informed consent forms of federally funded clinical trials exceeds the reading comprehension skills of the majority of adults in the U.S., potentially undermining clinical trial participant retention rates. Future work should explore the use of large language models and other tools as possible means to close this literacy barrier and potentially enhancing clinical ...
Background With advancements in burn treatment and intensive care leading to decreased mortality rates, a growing cohort of burn survivors is emerging. These individuals may be susceptible to frailty, characterized by reduced physiological reserve and increased vulnerability to stressors commonly associated with aging, which significantly complicates their recovery process. To date, no study ...
Empirical: Empirical research is a way of gaining knowledge through observation or experience. Empirical research contrasts with theoretical research, which relies on systems of logic, beliefs, and assumptions. Predictor: A predictor variable, is a factor that influences another variable in a correlational study. For example, the length of a ...
This study has several limitations. First, respondents were selected by their organization directors following administrative procedures mandated by research projects in Lao PDR. While this method has likely allowed to capture a diverse range of perspectives on malnutrition, it may have excluded individuals who disagreed with the official ...
Objective To estimate the real world effectiveness of modified vaccinia Ankara-Bavarian Nordic (MVA-BN) vaccine against mpox infection. Design Emulation of a target trial. Setting Linked databases in Ontario, Canada. Participants 9803 men aged ≥18 years with a history of being tested for syphilis and a laboratory confirmed bacterial sexually transmitted infection (STI) in the previous year ...
A prospective, randomized, split-mouth clinical study by the two previously trained and calibrated pediatric dentists without blinding operators and patients due to different protocols in both ...
Don't just list key weaknesses and the magnitude of a study's limitations. To do so diminishes the validity of your research because it leaves the reader wondering whether, or in what ways, limitation(s) in your study may have impacted the findings and conclusions. Limitations require a critical, overall appraisal and interpretation of their ...