NEED A PERFECT PAPER? PLACE YOUR FIRST ORDER AND SAVE 15% USING COUPON:

Sign In / Register
Place Order

Writing a Medical Laboratory Science Personal Statement

Embarking on the journey into the realm of Medical Laboratory Science is a testament to one’s passion for scientific exploration and commitment to advancing healthcare. The medical laboratory science personal statement serves as a window into the unique blend of skills, qualities, and aspirations that an individual brings to this critical field. In this essay , we navigate through the intricacies of crafting a compelling personal statement, addressing key questions and shedding light on the importance of medical laboratory science.
The Core Competencies of a Medical Laboratory Scientist
A personal statement for medical laboratory science should meticulously highlight the core competencies essential for success in this field. These encompass a profound understanding of laboratory techniques, meticulous attention to detail, analytical prowess, and effective communication skills. The statement should weave a narrative that demonstrates how these competencies have been cultivated through academic pursuits, hands-on experiences, and a genuine enthusiasm for the scientific process.
Profound Understanding of Laboratory Techniques
An effective personal statement should showcase a comprehensive grasp of laboratory procedures , methodologies, and instrumentation. Detailing experiences in conducting experiments, handling lab equipment, and applying various analytical methods demonstrates proficiency in executing laboratory protocols.
Meticulous Attention to Detail
Precision and accuracy are paramount in laboratory settings. The personal statement should emphasize a track record of meticulousness, focusing on the ability to adhere to standard operating procedures, ensuring accurate measurements, and maintaining meticulous records to yield reliable results.
Analytical Prowess
Highlighting strong analytical skills is vital. Applicants should discuss their ability to interpret data, analyze results critically, and draw meaningful conclusions. This might involve detailing experiences in data analysis, experimental design, statistical interpretation, and problem-solving in laboratory scenarios.
Effective Communication Skills
The ability to convey complex scientific concepts concisely is fundamental. The personal statement should demonstrate adeptness in communicating scientific findings through clear and articulate writing, presentations, and effective collaboration within multidisciplinary teams. This skill is crucial for conveying research findings and collaborating with healthcare professionals.
Demonstrated Development of Competencies
Providing specific examples of how these competencies were acquired and honed is key. Discussing relevant coursework, internships, research projects, or laboratory experiences that required the application of these skills strengthens the narrative. It’s essential to link experiences to the development of each competency and how they contribute to the applicant’s readiness for the field.
A robust personal statement showcasing these competencies provides a comprehensive view of an applicant’s preparedness, aligning their skills with the demands and expectations of a medical laboratory scientist role.

The Personality of a Medical Laboratory Scientist
Exploring the personality traits integral to a medical laboratory scientist is pivotal in crafting an impactful personal statement. Traits such as precision, reliability, adaptability, and an unwavering commitment to accuracy are paramount. The statement should provide glimpses into real-life scenarios where these traits were exercised, underscoring their role in navigating the challenges of a clinical laboratory environment.
The personal statement should underscore the importance of precision in every aspect of laboratory work. Discuss instances where meticulous attention to detail was crucial, whether in sample preparation, measurements, or data recording. This trait ensures that results are reliable, contributing to accurate diagnoses and informed healthcare decisions.
Reliability
Reliability is a cornerstone of the medical laboratory scientist’s personality. Applicants should share experiences that highlight their dependability in meeting deadlines, consistently producing accurate results, and being a reliable team member. This trait is crucial in maintaining the integrity of laboratory processes.
Adaptability
Given the dynamic nature of scientific research and healthcare, an ability to adapt is essential. The personal statement should provide examples of situations where adaptability was demonstrated, whether in handling unexpected challenges, adjusting to new technologies, or collaborating effectively in diverse team settings.
Commitment to Accuracy
Emphasizing an unwavering commitment to accuracy is pivotal. Narratives should showcase instances where the applicant prioritized accuracy over speed, ensuring that laboratory procedures were meticulously followed, and results were beyond reproach. This commitment is integral to upholding the standards of the medical laboratory.
Team Collaboration
The ability to work collaboratively within a team is a vital personality trait. Sharing experiences of successful teamwork in a laboratory or academic setting highlights the applicant’s capacity to collaborate, communicate effectively, and contribute to a harmonious working environment.
The personal statement can touch on instances where resilience was demonstrated in the face of setbacks or challenges. This trait is essential for navigating the complexities of scientific research, troubleshooting unexpected issues, and persisting in the pursuit of accurate and meaningful results.
By weaving these personality traits into the personal statement, applicants can paint a compelling picture of how their unique qualities align with the demands and expectations of a medical laboratory scientist role. Providing concrete examples enhances the authenticity and impact of the narrative.
Read Also: Top 5 Homework Writing Services for Students
The importance of medical laboratory science.
An effective personal statement should articulate the significance of medical laboratory science in the broader context of healthcare. It should delve into the pivotal role laboratory scientists play in disease diagnosis, treatment monitoring, and the overall improvement of patient outcomes. Demonstrating an understanding of the interconnectedness between laboratory results and clinical decision-making is crucial in conveying the gravity of this profession.
Disease Diagnosis and Treatment Monitoring
The personal statement should highlight the pivotal role medical laboratory scientists play in disease diagnosis and treatment monitoring. Discussing specific cases or experiences where laboratory results directly influenced patient diagnoses or treatment plans underscores the tangible impact of this profession on healthcare outcomes. This showcases the applicant’s appreciation for the critical link between laboratory science and clinical decision-making.
Patient-Centric Focus
Emphasizing the patient-centric aspect of medical laboratory science is essential. Sharing anecdotes or insights into how accurate and timely laboratory results contribute to improved patient care demonstrates a holistic understanding of the profession. It reflects the applicant’s awareness that behind every sample is a patient relying on precise and reliable laboratory analyses for their well-being.
Contribution to Medical Research
Acknowledging the role of medical laboratory scientists in advancing medical research enhances the personal statement. Discussing experiences or aspirations related to research projects, the development of new diagnostic techniques, or contributions to scientific publications underscores the applicant’s commitment to the continuous improvement and innovation within the field.
Interdisciplinary Collaboration
The personal statement should touch on the interdisciplinary nature of medical laboratory science. Highlighting instances where collaboration with clinicians, nurses, and other healthcare professionals was essential showcases the applicant’s understanding of the interconnectedness of healthcare disciplines. This collaboration ensures a comprehensive and integrated approach to patient care.
Quality Assurance and Patient Safety
Stressing the commitment to quality assurance and patient safety is crucial. Discussing experiences in implementing quality control measures, participating in accreditation processes, or addressing challenges in the pursuit of excellence reinforces the applicant’s dedication to upholding the highest standards in laboratory practice.
By weaving these elements into the personal statement, applicants can convey not only their technical proficiency but also their appreciation for the broader impact of medical laboratory science on individual patients and the healthcare system as a whole. This elevates the narrative and emphasizes the noble and vital nature of the profession.

Qualifications and Skills for Medical Laboratory Science:
Addressing qualifications and skills necessitates a balance between academic achievements and hands-on experiences. The personal statement should delineate academic accomplishments, relevant coursework, and any specialized training. Additionally, it should showcase practical skills acquired during internships, research projects, or laboratory work, accentuating how these experiences have honed one’s abilities for a seamless transition into the professional realm.
Academic Achievements
The personal statement should succinctly outline academic achievements relevant to medical laboratory science. This includes academic degrees, specialized coursework, and any honors or awards received. The emphasis should be on how these academic pursuits have provided a solid foundation for understanding the theoretical aspects of laboratory science.
Laboratory Techniques Mastery
Detailing proficiency in fundamental laboratory techniques is vital. The personal statement should specify the hands-on skills gained during academic coursework, internships, or laboratory experiences. This could encompass skills such as pipetting, sample preparation, microscopy, and molecular biology techniques. Highlighting any advanced techniques or specialized training further strengthens the portrayal of technical competence.
Analytical Thinking
Expressing a strong aptitude for analytical thinking is crucial. The personal statement should showcase instances where the applicant successfully employed critical thinking skills to analyze complex data, troubleshoot issues in laboratory procedures, or interpret results accurately. This underscores the ability to approach challenges with a systematic and analytical mindset.
Attention to Detail
Emphasizing an unwavering attention to detail is key. The personal statement should provide examples of situations where meticulous attention to detail was pivotal, ensuring accurate and reliable laboratory results. Attention to detail is a cornerstone skill in medical laboratory science, and the applicant’s experiences should reflect this commitment.
Communication Skills
The personal statement should highlight effective communication skills , both written and verbal. Discussing experiences where the applicant conveyed complex scientific information in a clear and concise manner, collaborated with colleagues, or presented findings demonstrates the ability to communicate effectively within the laboratory and with other healthcare professionals.
Time Management
Demonstrating effective time management skills is essential. The personal statement should feature instances where the applicant successfully managed multiple tasks, met deadlines for experiments or projects, and maintained a high level of productivity. This illustrates the capacity to handle the fast-paced and dynamic nature of laboratory work.
By weaving these qualifications and skills into the personal statement, applicants can present a holistic picture of their readiness for a career in medical laboratory science. This balance between academic achievements and practical skills showcases the applicant’s preparedness to contribute meaningfully to the field.
Read Also: Personal Statement Writing Help
The crafting process for a medical laboratory science personal statement:.
Guidance on how to write a medical lab CV and personal statement for laboratory technician roles is integral. The statement should commence with a compelling introduction that encapsulates the applicant’s passion for medical laboratory science. It should progress to discuss academic and practical experiences in a structured manner, emphasizing their direct relevance to the field. The narrative should be authentic, allowing the applicant’s voice to resonate throughout the document.
Introduction
Begin the personal statement with a captivating introduction that expresses genuine passion for medical laboratory science. Engage the reader by sharing a personal anecdote or experience that ignited the interest in pursuing this career path. This sets the tone for the rest of the statement.
Academic Background
Detail academic achievements, including degrees earned, relevant coursework, and any academic honors or awards received. Highlight specialized courses that directly relate to medical laboratory science and elaborate on how these academic pursuits have equipped you with a strong foundation in the field.
Professional Experience
Discuss practical experiences, such as internships, laboratory work , or research projects, that demonstrate hands-on skills and their direct application to medical laboratory science. Focus on specific tasks, techniques learned, or projects undertaken, emphasizing their relevance to the position you’re seeking.
Key Skills and Competencies
Incorporate key skills and competencies essential for medical laboratory science roles. Highlight analytical thinking, attention to detail, communication skills, and proficiency in laboratory techniques. Provide concrete examples or instances where these skills were employed effectively.
Passion and Motivation
Reiterate your passion for the field and your motivation to pursue a career in medical laboratory science. Emphasize how your experiences have solidified your commitment to contributing meaningfully to the field and improving patient care outcomes.
CV for Laboratory Technician Roles
For the CV, organize information in a clear and structured format . Include sections such as education, work experience, skills, certifications, and any relevant extracurricular activities or volunteer work. Tailor the CV to highlight laboratory-related experiences, technical skills, and academic achievements.
Authenticity and Proofreading
Ensure that both the personal statement and CV reflect your authentic voice and experiences. Proofread meticulously to eliminate errors in grammar, spelling, or formatting. Seek feedback from mentors, professors, or career advisors to enhance the content and clarity of your documents.
Crafting a compelling personal statement and CV for medical laboratory science roles involves presenting a cohesive narrative that showcases your academic prowess, practical skills, and genuine enthusiasm for the field. Tailoring these documents to highlight your qualifications and aligning them with the specific role you’re applying for can significantly enhance your application.

Challenges and Rewards
In the dynamic field of medical laboratory science, navigating challenges is an inevitable part of the journey. In crafting a personal statement, it’s essential to candidly acknowledge these challenges while also illuminating the valuable lessons and rewards derived from overcoming them.
Challenges:
- Complex Procedures: Medical laboratory science involves intricate procedures and methodologies. Acknowledge the initial complexity of mastering these techniques and the learning curve associated with becoming proficient in various laboratory processes.
- Time Management: Balancing academic demands, practical experiences, and personal commitments can be challenging. Discuss how you’ve grappled with time management issues and evolved strategies to effectively prioritize tasks.
- Accuracy and Precision: The demand for precision in laboratory work can be daunting. Address how you’ve confronted the pressure to deliver accurate results consistently and the steps taken to enhance your skills in maintaining precision.
- Interdisciplinary Collaboration: In the medical field , collaboration with diverse professionals is crucial. Reflect on challenges encountered in interdisciplinary settings and how you’ve learned to communicate effectively with colleagues from different backgrounds.
- Professional Growth: Emphasize how facing these challenges has contributed to your professional growth. Discuss specific instances where overcoming obstacles has enhanced your proficiency and adaptability in medical laboratory science.
- Critical Thinking: Highlight the development of critical thinking skills through problem-solving in the laboratory. Share examples of instances where you had to analyze complex situations and formulate effective solutions.
- Resilience: Discuss your resilience in the face of challenges. Illustrate how setbacks have fueled your determination to persevere and improve, emphasizing the importance of resilience in the fast-paced and demanding field of medical laboratory science .
- Personal Fulfillment: Beyond professional growth, underscore the personal fulfillment derived from successfully navigating challenges. Share moments of accomplishment and the sense of pride in contributing to meaningful advancements in healthcare through your work.
By openly addressing challenges and showcasing the rewards, your personal statement becomes a nuanced narrative that reflects both the realism of the medical laboratory science journey and the intrinsic motivation and resilience that drive you forward. This holistic perspective enhances the authenticity and impact of your personal statement.
In summary, a well-crafted medical laboratory science personal statement is a testament to the alignment of an individual’s skills, aspirations, and personality with the demands of this critical profession. Through thoughtful reflection, genuine storytelling, and a keen focus on the profession’s significance, the personal statement becomes a compelling narrative that sets the stage for a promising career in medical laboratory science.
Read Also: The Future of Dental Hygiene : Navigating Trends and Innovations
WRITING SERVICE AT YOUR CONVENIENCE Reliable Custom Essay Writing on Any Subject
Reliable Essay Writing Service for Students Kessay.com is home to reliable and
Providing Reliable Essay Writing Services Globally For 10+ Years 5/5 Research
Calculate Price

Revision Policy
Refund Policy
Privacy Policy
Equity HSE, Kikuyu, Kiambu, Kenya
How Our Service is Used:
Our essays are NOT intended to be forwarded as finalized work as it is only strictly meant to be used for research and study purposes. We do not endorse or condone any type of plagiarism.

© 2024 Kessays. All rights reserved. K-Essays will be listed as ‘Writing Help’ on your bank statement. 4
- REQUEST INFO
BSHS in Medical Laboratory Sciences

Learn About BSHS Programs in MLS at GW
Hybrid or 100% Online
24 Months*
Medical Laboratory Sciences (MLS) is a challenging and rewarding health care profession that has great impact on patient care. Working in a variety of settings, medical laboratory scientists are essential members of the health care team, providing vital information about the status and function of the body and its systems. The data obtained by medical laboratory scientists is utilized in the diagnosis, treatment, monitoring, and prevention of disease.
The George Washington University (GW) School of Medicine and Health Sciences (SMHS) offers a Bachelor of Science in Health Sciences degree in as little as 24 - 28 months. The Medical Laboratory Sciences program has two routes for completion:
- Degree completion program for non-MLTs
- A combination of online and in-person courses
- Degree completion program for certified MLTs
To learn more about our programs, you can register for our upcoming events .
* The total number of credits and duration of the program depend on the number of transferred credits
* Indicates required field
By providing your phone number on this request information form, you have authorized the George Washington University, and its representatives, to send you SMS/Text messages in conjunction with the services you have requested. Message and data rates may apply.
If you no longer wish to receive SMS/Text communications from GW SMHS, you will have the option to opt-out.
By submitting this form, you confirm you have read the Privacy Notice .
Accreditation and Rankings
- GW is accredited by the Middle States Commission on Higher Education
- #62 Best National University*
- #13 Best Online Bachelor's Programs*
- #7 Best Online Programs for Veterans*
* The U.S. News & World Report – 2024 Rankings

Program Highlights
- GW grads have a 93.03% overall five year pass rate for the ASCP MLS board of certification exam vs. 78.60% for the national average
- 99.72% of students who enter Phase II of the MLS program graduate
- Greater than 95% of graduates are employed in the field within three months of program completion
- Clinical Laboratory Technicians named No. 1 in Best Health Care Support Jobs
- Available fully online for MLT-certified professionals or “blended” online and in-person for professionals who are not MLT-certified
- Applicants with clinical laboratory experience may be eligible to waive individual clinical practicum requirements
Hybrid (Blended)
The hybrid Medical Laboratory Science (MLS) route requires 60 credits of GW coursework.
Students without MLT certification enter into the hybrid program and will complete 38 credit hours of core courses, 6 credits of in-person lab courses at the GW Virginia Science and Technology Campus (VSTC) in Ashburn, VA, and 16 credits of practicum courses at an approved diagnostic laboratory.
100% Online
The 100% online in Medical Laboratory Science (MLS) route requires 60 credits of GW coursework.
Students with MLT certification enter into the fully online program and will complete 38 credit hours of core courses, 14 credits of health sciences, and eight credits of clinical experience in their local area.
VIEW COURSES
Program Outcomes
When you complete this program, you’ll be able to sit for the ASCP Board of Certification exam, Route 1, and understand how to:
- Apply the principles of traditional and molecular laboratory procedures to perform diagnostic analyses
- Correlate laboratory data and quality control data to assess patient test results
- Apply knowledge of laboratory science principles as they relate to human disease diagnosis
- Comply with laboratory safety regulations and regulatory policies
- Apply ethical decision-making to issues related to clinical laboratory practice
| GW MLS Graduation Rates:* | GW MLS Placement Rates:** |
*Students graduating that began the second half of the program. **Students who found employment (in the field or in a closely related field) and/or continued their education within one year of graduation. ***Students who passed within the first year of graduation †Not a final result; rate calculation currently in progress Who Is the Ideal Student for This Program?Medical Laboratory Sciences (MLS) is a profession that combines the challenges of medicine, the basic sciences, and clinical sciences into a highly satisfying and valued career. Medical laboratory scientists function as detectives, investigating and determining the causes of disease. They utilize the latest biomedical instruments and molecular techniques to perform both routine and complex testing. As vital members of the health care team, medical laboratory scientists (sometimes called medical technologists) find great satisfaction in making a direct impact on medical care. Today's medical laboratory science graduates work in diverse settings including hospital laboratories, physician offices, clinics, commercial and research laboratories, pharmaceutical and biotechnology firms, as well as government and public health facilities. Learn more about Careers in Laboratory Sciences . State Licensure InformationWhile the completion of this program will make graduates eligible to register for an ASCP Board of Certification Exam, this does not automatically guarantee a graduate will also meet their state’s requirements for state licensure (if applicable). Since each state may have different requirements for licensure, each student is encouraged to contact their state’s regulating agency and review these requirements prior to beginning any degree program. State’s requiring licensure may require extended duration of practicum experiences, additional academic courses (outside the student’s program of study), etc. These additional requirements may require you to take a course or courses outside of GW. In particular, New York and California have additional requirements for state licensure. Both NY and CA require extended times for practicum rotations. Please also be aware that the BSHS in MLS program may not meet the student lab requirements for NY state licensure. We recommend that students who live in New York or California or plan to relocate to New York or California do research to determine the NY and CA licensure requirements. Career OutlookThe U.S. Bureau of Labor Statistics projects that an increase in the aging population is expected to lead to a greater need to diagnose medical conditions, like cancer or type 2 diabetes, through laboratory procedures. Overall employment of medical laboratory technologists and technicians is expected to grow 11% from 2018 to 2028, faster than the average for all occupations, with a median salary of $52,330 per year. 1 According to Burning Glass, from May 2017 to May 2018, these high-demand, high-paying metro areas were seeking medical laboratory technicians with a bachelor’s degree:
Admission RequirementsTo be accepted into this program, you must have:
SEE ALL REQUIREMENTS Tuition DetailsThe BSHS in Medical Laboratory Sciences program at GW consists of 60 credit hours. Please find the cost per credit hour and total estimated program costs here . Note: Tuition rates are subject to change and additional fees may vary by program. GET TUITION DETAILS Meet the Program Director GW’s experienced faculty provide you with the rich, practical knowledge and support needed for you to succeed in the program and in your career. Cliff Cymrot, DHSc, MHA, MLS(ASCP) CM , SH CM , MT(AAB), MT(AMT)Dr. Cliff Cymrot is the current Program Director for Medical Laboratory Sciences (MLS) and has over 10 years of experience in combined teaching and clinical laboratory practice. In addition to his program director duties, Dr. Cymrot teaches a range of courses within the MLS program, both online and face-to-face, such as Hematology lecture and lab, Bacteriology lab, Immunohematology lab, Molecular Diagnostics, and Capstone. Prior to his arrival at George Washington University (GW), Dr. Cymrot worked as a medical laboratory technician at a medium-sized, 200-bed hospital in upstate NY. In 2008, Dr. Cymrot worked for Advance Magazine for Laboratory Professionals providing storylines for the comic strip “Lab out Loud” that he worked on with his brother-in-law. He has also been a contributor for several chapters in the Textbook of Diagnostic Microbiology by Mahon, Lehman, and Manuselis, as well as having various research publications. He is also a member of the DC chapter for the American Society for Clinical Laboratory Science (ASCLS), American Medical Technologists (AMT), and the American Association of Bioanalysts (AAB). He also holds certifications in ASCP, AMT, and AAB in Medical Laboratory Science, and Specialist in Hematology. In 2010, he earned his B.S. in Medical Technology from the University of Cincinnati (UC). He was then promoted to medical laboratory scientist and soon after began working as an adjunct instructor for SUNY Orange teaching Microbiology for Health Professionals, Fundamentals of Anatomy and Physiology, and Certification Preparation. In 2014 he earned his a master’s degree in Health Administration from UC. After graduation, he received an offer to facilitate an online graduate level course in health systems management at UC. In 2015 he was offered a position at GW to teach all of the laboratory courses in the newly created BSHS in MLS blended/hybrid program. After three years he was offered the Program Director position for the undergraduate MLS program here at GW. In 2022 he then went on to complete his doctorate in health sciences at GW. In 2024 he was offered the Program Director position for the MSHS in Laboratory Medicine program here at GW. Dr. Cymrot is actively involved in the MLS profession and loves teaching, research, and promoting MLS. Curriculum Details: Hybrid (Blended)The hybrid Medical Laboratory Science (MLS) program requires 60 credits of GW coursework. Program completion time is 2 years.
Note: These are examples of course sequencing. Summer IS included in our program. Students will work closely with their academic advisor regarding any edits that need to be made to the plan based on successful course completion or offerings. Download example as a PDF MLS 2007W - Writing in the Health Sciences (3 credits) - 8 weeks Introduction to the health sciences literature Emphasis is on construction, evaluation and organization of written communication of health sciences information. MLS 3001W - Professional Ethics for MLS (3 credits) - 8 weeks Ethical and professional conduct of and dilemmas encountered by medical laboratory professionals. Restricted to students in the medical laboratory science programs. Includes a significant engagement in writing as a form of critical inquiry and scholarly expression to satisfy the WID requirement. MLS 4141 - Immunology and Serology (3 credits) - 15 weeks Principles of the immune system’s components, functions, interactions with microorganisms, and the clinical applications of immunologic assays to human health and disease. MLS 4158 - Laboratory Management (3 credits) - 8 weeks Introduction to critical concepts of lab management, including leadership theory, management principles, human resource management, financial management, quality management, and laboratory operations. Proctor fee. MLS 4116 - Clinical Bacteriology I (3 credits) - 8 weeks Principles of clinical microbiology with emphasis on pathogenic characteristics, isolation, and identification of bacteria related to human disease; theoretical approach to the current diagnostic techniques and identification systems used in clinical practice. Restricted to students in the medical laboratory science program. Prerequisites: BISC 1111. MLS 4117 - Clinical Bacteriology II (2 credits) - 8 weeks The etiology of infectious diseases in different body sites with an emphasis on the epidemiology, pathogenic mechanisms, and laboratory identification of suspected etiologic agents; specimen collection and handling, diagnosis and treatment of medically significant bacteria. Restricted to students in the medical laboratory science program. Prerequisites: BISC 1111. MLS 4119 - Parasitology, Mycology, and Virology (2 credits) - 15 weeks Principles and procedures involved in the diagnosis of parasitic, fungal, and viral infections; disease causation, specimen collection and handling, laboratory identification and treatment of medically significant fungi, parasites, and viruses. Proctor fee. Restricted to students in the medical laboratory science program. Prerequisites: BISC 1112; or BISC 1116 and BISC 1126. MLS 4216 - Clinical Bacteriology Lab (1 credit) - 15 weeks Hands-on experience in current diagnostic techniques and identification systems used in clinical practice; principles, procedures, techniques and data interpretation for the isolation and identification of clinically significant bacteria. Restricted to students in the medical laboratory science program. Prerequisites: BISC 1111. Corequisites: MLS 4116. MLS 4219 - Parasitology, Mycology, and Virology Laboratory (1 credit) Principles and procedures involved in the diagnosis of parasitic, fungal, and viral infections; disease causation, specimen collection and handling, laboratory identification and treatment of medically significant fungi, parasites and viruses. Laboratory fee. Corequisite MLS 4119. Restricted to students in the medical laboratory science program. Prerequisites: BISC 1112; or BISC 1116 and BISC 1126. MLS 4145 - Clinical Biochemistry I (3 credits) - 8 weeks This course studies the methodologies employed in the chemical analysis of human blood and body fluids. This includes an examination of the fundamentals of measurement and the principles of instrumentation as they relate to the assay of each analyte studied. In addition, the laboratory results are correlated with the clinical significance and pathophysiology which may generate changes in the analyte. Throughout the course, the quality assurance measures required to ensure reliability and validity of the laboratory results are also emphasized. [add to end of description: Proctor fee. MLS 4146 - Clinical Biochemistry II (3 credits) - 8 weeks This second course in clinical biochemistry continues the study of the measurement and interpretation of chemical constituents in human blood and body fluids. The laboratory results of each analyte are correlated with the clinical significance and pathophysiology which may generate changes in the analyte. Throughout the course, the quality assurance measures required to ensure reliability and validity of the laboratory results are also emphasized. MLS 4151 - Molecular Diagnostics (3 credits) - 15 weeks Introduction to the molecular techniques used to diagnose human disease; technology, theory, and methodology of specific molecular protocols that can be used within a clinical laboratory setting to aid in disease diagnostics including those of genetic, oncogenic, and infections origin. Proctor fee. MLS 4246 - Clinical Biochemistry Lab (1 credit) - 15 weeks Practical laboratory course covering the principles and procedures of various diagnostic testing procedures performed in the clinical biochemistry laboratory; measurement and interpretation of chemical constituents in human blood and body fluids. Laboratory fee. Corequisite: MLS 4145. Prerequisites: CHEM 1111 and CHEM 1112. MLS 4251 - Molecular Diagnostics Lab (1 credit) - 15 weeks An introduction to the theory of and laboratory techniques in molecular biology with an emphasis on molecular and serological techniques, including DNA extraction and quantitation, restriction enzyme digestion, polymerase chain reaction, agarose gel electrophoresis, flow cytometry, and ELISA. Restricted to students in the medical laboratory science program. MLS 4130 - Hematology I (3 credits) - 8 weeks Study of the blood and blood-forming tissues with emphasis on hematologic techniques and cell identification; anemias and non-malignant leukocyte disorders. Restricted to students in the medical laboratory science program. Prerequisites: BISC 1111. MLS 4131 - Hematology II (3 credits) - 8 weeks Study of the blood and blood-forming tissues with emphasis on white blood cell disorders; introduction to the hemostatic system and associated coagulation disorders. Restricted to students in the medical laboratory science program. Prerequisites: MLS 4130. MLS 4150 - Immunohematology (3 credits) - 15 weeks The major blood group systems that affect the practice of transfusion medicine and examines the processing and distribution of blood products supplied by transfusion services. Proctor fee. MLS 4230 - Hematology Lab (1 credit) - 15 weeks Diagnostic analyses used to evaluate disease states associated with human blood cells; quality assurance in the hematology lab and on the evaluation of stained blood smears and microscopic differentiation of blood cells. Restricted to students in the medical laboratory science program. Prerequisites: BISC 1111. Corequisites: MLS 4130. MLS 4250 - Immunohematology Lab (1 credit) - 15 weeks Performance of routine blood banking procedures, including blood group and Rh typing, antibody screens, antibody identification, cross matching, and elution and absorption techniques. Restricted to students in the medical laboratory science program. MLS 4159 - Capstone Seminar (1 credit) - 15 weeks Comprehensive review of medical laboratory science, which prepares students to sit for the board of certification examination. Integration of knowledge gained in didactic and practicum courses within the various laboratory disciplines, including hematology, microbiology, chemistry, and immunohematology. Proctor fee. MLS 4160 - Blood Bank Practicum (4 credits) - 15 weeks Clinical practicum in which students apply medical knowledge and clinical skills gained in MLS 4150. Prerequisites: MLS 4150. MLS 4161 - Clinical Biochemistry Practicum (4 credits) - 15 weeks Application of the medical knowledge and clinical skills gained in the didactic clinical biochemistry I and clinical biochemistry II courses. Proctor fee. MLS 4162 - Hematology Practicum (2 credits) - 15 weeks Analyses and laboratory testing of human blood specimens. MLS 4164 - Clinical Microbiology Practicum (4 credits) - 15 weeks Students apply medical knowledge and clinical skills gained in MLS 4123 (Clinical Microbiology I), MLS 4124 (Clinical Microbiology II), and MLS 4151 (Molecular Diagnostics). Proctor fee. MLS 4165 - Urinalysis Practicum (1 credit) - 15 weeks Active engagement in applying medical knowledge and clinical skills in the analysis of urine and body fluids. MLS 4166 - Coagulation Practicum (1 credit) - 15 weeks One-week required rotation for students in the Bachelor of Science in Health Science in Medical Laboratory Science (MLS), Post-baccalaureate MLS, or Post-baccalaureate in Hematology for MLS certificate programs. Focus on analyses and laboratory testing of human blood specimens. Curriculum Details: 100% OnlineStudents with MLT certification enter into the 100% online program and will complete 38 credit hours of core courses, 14 – 29 credits of electives (determine by the number brought in at admission), and eight credits of clinical experience in their local area.
Download example as a PDF MLS 2007W - Writing in the Health Sciences (3 credits) - 15 weeks MLS 3000 - Clinical Lab Mathematics (3 credits) - 8 weeks Basic mathematical techniques used in the clinical laboratory, including exponential and logarithms, measurement systems, solutions and concentrations, proportionality, graphing, statistics and quality control, and method evaluation; practical applications of data analysis. An equivalent college-level mathematics course or permission of the program director may be substituted for the prerequisite. Restricted to students in the medical laboratory science program. Prerequisite: HSCI 2117. MLS 4136 - Clinical Experience I (2 credits) - 15 weeks Supervised clinical experience in clinical chemistry. Proctor fee. MLS 4137 - Clinical Experience II (2 credits) - 15 weeks Supervised clinical experience in microbiology. Proctor fee. MLS 4138 - Clinical Experience III (2 credits) - 15 weeks Supervised clinical experience in hematology, coagulation and urinalysis. Proctor fee. MLS 4139 - Clinical Experience IV (2 credits) - 15 weeks Supervised clinical experience in transfusion medicine and serology. Proctor fee. Elective (12 credits)
GW SMHS does not admit first-time college freshmen or provide general education courses; therefore, students are expected to enroll at another institution of higher education for at least one semester during an academic year following their high school graduation, and prior to transferring into GW. To apply for the BSHS in Medical Laboratory Sciences (Hybrid or 100% Online) , you’ll need:
Transfer credit may include dual enrollment coursework. It may also be considered from Advanced Placement (AP), International Baccalaureate Credit (IB) credit as well as the College Level Examination Program (CLEP exams). Please refer to GW Undergraduate Admissions for information on maximum credits, minimum scores, and GW course equivalents for AP and IB credits. If you have an associate degree from a participating D.C., Maryland, Virginia community college, you may be eligible for guaranteed admission to this program. Review the list of participating institutions . International StudentsInternational students should check with individual programs regarding eligibility for visa sponsorship. Generally, online and hybrid programs are not eligible for student visa sponsorship from GW. This would include transfer students from any other institution with an existing visa. Official transcripts from institutions outside the U.S. must be accompanied by an official transcript evaluation from an accredited independent evaluating agency. Please be sure you request a detailed evaluation that includes all course titles, credit hours, grades, U.S. degree equivalency, grade-point averages (GPA), and date of degree conferral. For a list of acceptable foreign credential evaluation services, please visit NACES . Applicants who are not U.S. citizens are also required to submit official test scores for the Test of English as a Foreign Language (TOEFL) or Pearson’s Test of English (PTE) Academics or the academic International English Language Test System (IELTS). To be considered for admission, there are required scores that you will need to meet. Score requirements may differ by school and program so check the admissions requirements for your program . Supporting Documents and Official TranscriptDocuments and Official Transcripts not submitted online should be mailed to: Mail: George Washington University ATTN: Transcript Processing Center 1415 W 22 nd St. Suite 220 Oak Brook, IL 60523 Alternatively, official electronic transcripts can be sent to: [email protected] As you explore our programs at George Washington University, our dedicated staff is here to support you. If you have any questions or want to know more, click the "Request More Information" button below, or email [email protected] . Request More Information  Clinical Lab SciencesThere are many pieces to the clinical lab scientist training program application, including your gpa, personal statement, list of experiences, letters of recommendation, and biographical information. use the navigation below to explore each aspect of preparing for a clinical lab scientist training program..
Clinical (or Medical) Laboratory Scientists work with pathologists, other physicians, and scientists who specialize in clinical chemistry, microbiology, or other biological sciences. Together, they detect, diagnose, and treat many patient diseases. As part of this health care team, Clinical Laboratory Scientists are responsible for performing tests and developing data on the patient's blood tissues and body fluids. They have the knowledge of the principles behind these tests, the ability to recognize physiological conditions affecting test results, and the ability to develop data that may be used by a physician in determining the presence, extent, and the cause of disease. In addition to working in a clinical laboratory, jobs for clinical laboratory scientists are available in departments of public health, industrial labs, pharmaceutical companies, the armed forces, the National Institutes of Health (NIH), and the World Health Organization (WHO). Clinical laboratory scientist licenses may be general (for all areas of the clinical lab), or limited to performing procedures in one particular area (clinical chemistry, clinical microbiology, immunohematology, and toxicology).
Before starting a training program, you obtain a Trainee License through the California Department of Public Health. This license permits you to train, not work, as a licensed Clinical Laboratory Scientist. To obtain a trainee license, you must have a bachelor's degree and must have completed the following coursework: Visit the California Department of Public Health to apply for a trainee license. CLS Training ProgramsMost training programs in California are run by universities (e.g. UCs, CSUs, Loma Linda) and take place in hospitals; some programs are run by the hospitals where training occurs, and others by private companies (e.g. Blood Source). Training programs are 12 months. CLS LicenseAfter completing a training program, candidates are eligible to take a national exam to be a certified Clinical Laboratory Scientist.
* Check your major requirements before choosing classes. * If you have already taken BIS 105, we encourage having the syllabus ready to share with schools. Applicants don’t necessarily need to take additional classes before they apply. Requirements vary by school. Please call HPA’s Express Advising for questions. Updated 2/2023. See the Clinical Lab Sciences Program Prerequisite Chart for a sample list of CLS programs and their requirements. Note: The above courses are only suggested, not absolute. Although no particular undergraduate major is required, some schools prefer students majoring in one of the biological sciences or chemistry. As long as all prerequisites are met, any major may be chosen. Prerequisites and minimum GPAs differ by program.
Each CLS program has a set of "Essential Functions" that are expected of their CLS students. Applicants should have good laboratory technique, strong critical thinking skills, the ability to work under stressful conditions, and a professional attitude. Any experiences that you have had that can demonstrate these skills will make you a stronger applicant. Laboratory experience is essential in building and demonstrating your laboratory skills and abilities and can be gained through working in a college laboratory, research laboratory, or volunteering in a hospital-based clinical laboratory.
Standardized ExamThe GRE is not required for CLS programs. Personal StatementExplain your interest in a career in clinical lab sciences. Letters of RecommendationPrograms require three letters of recommendations from either professors or employers; many require two to be from instructors. Some schools also require letter writers to complete a form in which they should be able to address familiarity, the applicant’s strengths and weaknesses, the applicant’s ability to do independent work, and the applicant’s profile (e.g., reliability, emotional control, laboratory skills, etc.). Most programs require personal interviews prior to acceptance into clinical training. Some will contact you directly to schedule your interview, while other require that you request an interview. Choosing ProgramsThere are 227 accredited CLS programs in the nation as of October 2015. In California, there are thirteen CLS programs with ten nationally approved programs and 3 CA-only approved programs, including those at CSU Los Angeles, Physician’s Automated Lab, and Children’s Hospital Central California. Each program varies in terms of minimum GPA, prerequisites, class size, tuition/fees, etc. When selecting programs to apply to, be sure to take these factors into consideration as you may not need to pay any tuition for some, while others can be much more costly. Also, while programs typically last for only a year, there are a couple of programs that may last longer. If you have any questions in regards to selecting programs, please come see an advisor at Health Professions Advising.
CLS Programs in California.pdf CLS_InfoPacket.pdf Guide to Writing a Medical School Personal Statementjacoblund / Getty Images
Don't underestimate the importance of your personal statement in your medical school application . Your GPA and MCAT scores show that you are academically capable, but they do not tell the admissions committee what type of person you are. Who you are matters, and the personal statement is the place to tell your story. Tips for a Winning Med School Personal Statement
The medical school admissions process is holistic , and the admissions folks want to enroll students who are articulate, empathetic, and passionate about medicine. Your personal statement provides you an opportunity to make the case that you have what it takes to succeed in medical school and that you will contribute to the campus community in positive ways. You will want to put significant thought and time into your personal statement since it will play a role in all of your medical school applications. Nearly all medical schools in the United States use the American Medical College Application Service (AMCAS) to manage their applications, much like hundreds of undergraduate institutions use the Common Application. With AMCAS, the prompt for the personal statement is pleasingly (and perhaps frustratingly) broad: Use the space provided to explain why you want to go to medical school. This simple prompt allows you to write about almost anything, but some topics will be much more effective than others. Choosing Personal Statement TopicsA medical school personal statement is relatively short (less than 1/3 the length of this article), so you'll need to be selective when deciding what to include. As you identify your areas of focus, always keep the prompt in mind—your personal statement needs to explain why you want to go to medical school. If you find yourself straying from that goal, you'll want to refocus and get back on track. Successful medical applicants typically include several of these topics in their personal statements:
Topics to Avoid in Your Personal StatementWhile you have many choices about the type of content you can include in your personal statement, there are several topics that you would be wise to avoid.
How to Structure Your Personal StatementThere is no single best way to structure your personal statement, and the admissions committee would get quite bored if every statement followed the exact same outline. That said, you do want to make sure each point you make in your statement flows logically from what precedes it. This sample structure will give you a good starting point for conceptualizing and crafting your own personal statement:
Again, this is just a suggested outline. A personal statement may have four paragraphs, or it may have more than five. Some students have unique situations or experiences that aren't included in this outline, and you may find that a different method of organization works best for telling your story. Finally, as you outline your personal statement, don't worry about being exhaustive and covering everything you have done. You'll have plenty of space elsewhere to list and describe all of your extracurricular and research experiences, and your transcript will give a good indication of your academic preparation. You don't have a lot of space, so identify a couple important experiences from your undergraduate years and a couple character traits you want to emphasize, and then weave that material into a focused narrative. Tips for Personal Statement SuccessWell-structured, carefully-selected content is certainly essential to a successful medical school personal statement, but you need to consider a few more factors as well.
Call us : +88 (0) 1712969390, +44 (0) 7495942849, +44 (0) 7459725824 Sign in | Sign up  SOP - BSc (Hons) Biomedical Science
  05 August, 2022Sop - bsc (hons) biomedical science share.
I am aspiring to study a BSc (Hons) Biomedical Science Programme at the University of Bedfordshire It will provide knowledge as well as graduate-level analytical and transferable skills to prepare for a wide range of careers or further study. My goal in studying biomedical science is to gain a deeper understanding of the human body. This course provides a solid foundation in laboratory science used to research, diagnose, and treat disease. The course will enable me to gain an in-depth understanding of how the human body works, and the molecular, cellular and organ-level processes that take place in the human body. Moreover, I believe that this course will help me demonstrate my academic and intellectual abilities. I have seen the course modules, syllabus, and learning outcomes of the BSc (Hons) Biomedical Science programme at the University of Bedfordshire this course provides the education, skills, and training required to pursue a career as a professional. The course supports meaningful learning through a curriculum that provides intellectually challenging and practical relevant competencies for future careers in the biomedical sciences. Laboratory-based practical skills are an essential part of this course and will help in developing various practical strategies for a career in biomedical sciences including various biomedical industries and biomedical research. This course teaching method includes practical classes, tutorials, seminars, workshops, Project work, Team- working, IT-based teaching and learning, Case studies and problem-based learning, and guided study. Moreover, the course demonstrates a thorough foundation in theory and practice in human anatomy, physiology and reproductive science, molecular and clinical genetics, clinical immunology, medical microbiology, cellular pathology, clinical biochemistry, hematology, and transfusion science. The assessment methods used across this course include opportunities for Coursework, examinations, Literature review, Research dissertation, Problem-based learning activities, oral presentations, and laboratory practical work. Having the opportunity to study this course I am looking forward to improving my skills and knowledge. This course will help me gain an understanding of the biomedical science method and provide career opportunities through the techniques and skills used. After completing this course, I would like to join the reputed institutes of my country as a Biomedical Scientist or Clinical Research Associate to build my professional career. So, I believe this course will be suitable for my career planning and professional development objectives. I completed my Secondary and Intermediate from the science groups respectively. While I studied in school and college, I was involved in various types of curriculum activities such as Attend Seminars and Workshops, Debating, Volunteering, Socializing, and Fund Rising. Since I am interested to expand my knowledge in biomedical science, I have come to the conclusion that I need a higher degree from abroad that will enrich my knowledge and skills. I think I should gain more knowledge in the field of Biomedical Science so I decided to continue my further studies with this course. I think I should gain more knowledge in the field of Biomedical Science so I decided to continue my further studies with this course. It will help me develop a broader and more balanced understanding of basic Biomedical Science. In addition, I am eager to gain complete knowledge and skills from this course. Moreover, this course applies the standard method for understanding and evaluating risks and for working safely and solving problems with practical skills in the laboratory. So, I believe this course will be the right choice for me as I am looking for a successful career in this course. It was difficult for me to choose a specialization as an alternative to the courses available to me, but I finally decided to pursue a career in Biomedical Science. As a science student, studying these course modules would not be difficult for me. The modules include Microbiology and Biochemistry, Human Anatomy & Physiology, Cell Biology, Molecular Genetics, Skills in Biomedical Science, Chemistry, Skills in Science, Human Metabolism, Medical Physiology, Immunology, Medical Microbiology, Haematology & Transfusion Science, Genetics, Cellular Pathology, Biomedical Science Research Project, Applications of Microbiology, Clinical Biochemistry, Applications of Immunology, Human Genetics, Biology of Disease, and Molecular Biology. So, I hope my chosen course will make me better and further open doors for my profession. There are several reasons I aspire to study in the UK because the UK is famous for profession. Because this country has had a great reputation for quality higher education since its inception. It is true that the UK is a well-known country and has huge popularity. The UK maintains a quality management system with high standards in all fields. In recent years, most reputed companies in Bangladesh are emphasizing hiring Bangladeshi graduates with degrees from abroad. Where the study environment in my country follows theoretical systems of education and no practical skills are gained. Academically the UK prepares students and provides soft skills that are useful for future careers. UK accommodation and living expenses, and tuition fees are also reasonable. The affordable tuition fees attracted me the most. Furthermore, an academic degree from the UK is recognized and appreciated by employers around the world. This is why I chose the UK as my preferred destination and goal. According to a recent study of international graduation results in 2019 by iGraduate by Universities UK International 82% of overseas graduates believe their UK degree is beneficial for financial investment, and a similar number of graduates said they were satisfied or very satisfied with their careers. Approximately 83% believe a UK degree helped them get a job. So, it will be a big achievement for me if I can study this course at the University of Bedfordshire . The University of Bedfordshire is a specialty selection from the various options available to me as it is incredibly welcoming to international students. With more than 18,985 students, the university has a significant mature student body and provides outstanding higher education to people from more than 150 countries. University has invested heavily in their facilities to support students in order to create a physical and intellectual environment for learning. In addition, the University of Bedfordshire is dedicated to supporting international students to develop the skills, emotional intelligence, and creativity needed to thrive in a constantly changing world and the competitive job market. Universities have invested heavily in their facilities to support students in order to create a physical and intellectual environment for learning. Also, the university has a reputation for teaching, research, and business partnerships. Moreover, the university has a well-equipped campus. According to DLHE 2018, 91% of graduates are working and/or further studying within six months of graduation. So, if I get the chance to study this course at the University of Bedfordshire I will never look back and it will be a great achievement for me. Find more resources
Read similar resourcesBA (Hons) Business Management (Final Year)Business success requires a breadth of knowledge and abilities of efficient management to survive in fierce global co... BA (Hons) Business and MarketingModern business is a dynamic environment in which customer wants and needs constantly change at an ever-faster pace. ... Association of Chartered Certified AccountantsFollowing my MSc in Financial Management qualification in 2012, I have been in constant search for a real career for ... Are you looking to study abroad? Touch your dream with University Admission Expert
Newsletter SubscriptionKeep up to date with the latest news on UK student visa, courses, universities, scholarships, start dates, study guides etc. Post CommentUsername or email * Password * Forgotten password? [email protected] +44 (0)20 8834 4579 Medicine Personal Statement ExamplesGet some inspiration to start writing your Medicine Personal Statement with these successful examples from current Medical School students. We've got Medicine Personal Statements which were successful for universities including Imperial, UCL, King's, Bristol, Edinburgh and more. Personal Statement Examples
Personal Statement Example 1Check out this Medicine Personal Statement which was successful for Imperial, UCL, QMUL and King's. Personal Statement Example 2This Personal Statement comes from a student who received Medicine offers from Bristol and Plymouth - and also got an interview at Cambridge. Personal Statement Example 3Have a look at this Medicine Personal Statement which was successful for Imperial, Edinburgh, Dundee and Newcastle. Personal Statement Example 4Take a look at this Medicine Personal Statement which was successful for King's, Newcastle, Bristol and Sheffield. Personal Statement Example 5Pick up tips from this Medicine Personal Statement which was successful for Imperial, Birmingham and Manchester. Personal Statement Example 6This Personal Statement comes from a student who got into Graduate Entry Medicine at King's - and also had interviews for Undergraduate Medicine at King's, QMUL and Exeter. Loading More Content
Personal Statement Writing
An applicant’s personal statement is one of the most important pieces of your application materials. It is the school and admission’s committee first opportunity to hear from you about why you are passionate about your career choice. Fall and Spring Personal Statement Writing WorkshopHeld every fall and spring The Writing Center presents a workshop for how to craft a strong personal statement essay for your health professions applications.
No matter where you are in the writing process, this workshop is designed to help you brainstorm or refine your essay. Here are some other resources that will help you unlock your writing potential.
University Health Professions OfficePhone: (210) 458-5185 Email: [email protected] Student Union 2.02.04 The University of Texas at San Antonio One UTSA Circle San Antonio, TX, 78249 The Health Professions Office is part of UTSA’s Career-Engaged Learning ecosystem of offices, services, and opportunities that helps students connect what they are learning in the classroom to future career goals. We support experiential learning opportunities, encourage cross-disciplinary collaboration, foster partnerships with the community and aid in the articulations of marketable skills. Career-Engaged Learning Quick Links
Get the Reddit appMedical Lab Scientists Medical Lab Technicians Cytogeneticists Cytotechnologists Histologists Phlebotomists Lab Processors Application Personal StatementI'm planning to apply for the CLS program and am currently working on my personal statement. However, I'm really unclear what direction to take it in. I've heard from many people that the personal statement should work more like a cover letter that explains your experiences, and that the CLS program does not generally care for sob stories. However, I have heard from a few people (with minimal experience and subpar grades, I might add) that they wrote a more humanities-based essay about their struggles and personal skills and still got accepted into the program. Can anyone who got into the program share a general idea of what they wrote about? Or if anyone is a CLS director, can you share what you look for in an application essay? Thanks! By continuing, you agree to our User Agreement and acknowledge that you understand the Privacy Policy . Enter the 6-digit code from your authenticator appYou’ve set up two-factor authentication for this account. Enter a 6-digit backup codeCreate your username and password. Reddit is anonymous, so your username is what you’ll go by here. Choose wisely—because once you get a name, you can’t change it. Reset your passwordEnter your email address or username and we’ll send you a link to reset your password Check your inboxAn email with a link to reset your password was sent to the email address associated with your account Choose a Reddit account to continueCookies on this websiteWe use cookies to ensure that we give you the best experience on our website. If you click 'Accept all cookies' we'll assume that you are happy to receive all cookies and you won't see this message again. If you click 'Reject all non-essential cookies' only necessary cookies providing core functionality such as security, network management, and accessibility will be enabled. Click 'Find out more' for information on how to change your cookie settings. 
Biomedical Sciences: Advice on the Personal StatementYou can also download this page as a pdf document . Your personal statement is an important part of your application to Oxford. It allows you to tell us about your interests, achievements and ambitions in your own words. Although we do not formally score your statement we read it carefully and use the information it contains as part of our short-listing exercise. If you are invited for interview, the statement is likely to provide a focus for the questions that you are asked. It is therefore essential that your statement is an accurate, unembellished account of your activities. We may check the claims that you make on your statement: discovery of fabricated or exaggerated material – during the admissions exercise, or even later on during your time as a student – may bring into question your suitability to study on the course. Present yourself in the best light: the same basic facts about yourself (in terms of education, interests, experience), when presented differently, can quite dramatically convey positive or negative messages about you to tutors. For Biomedical Sciences, whilst your academic record and BMAT performance data will come into play when candidates are being short-listed for interview, time spent in drafting an effective personal statement should also help your overall chances of success. Every detail becomes even more important once you have reached the interviews and are being considered for a place. DO NOT BE SHY IN DECLARING ANY MITIGATING CIRCUMSTANCESThese may help us to put your achievements or personality within a finer context. We actively look for reasons why you may have under-performed in examinations, or performed well against the odds. These may be factors associated with your schooling, health or domestic circumstances. If you are returning to study after a break, or switching vocation, it is even more important to highlight your reasons for choosing a course at Oxford, and for you to demonstrate your determination, resilience, ability and commitment. DO NOT SIMPLY RECOUNT EVERYTHING YOU HAVE DONEWe’re looking for quality, not quantity! Remember that large numbers of candidates apply for our courses. Tell us in what ways you will stand out from the crowd. In choosing to talk about an activity, describe what you have drawn from the experience: has it changed you as a person? Did it surprise you? WE WANT TO LEARN ABOUT YOU AS A PERSON, NOT JUST ABOUT YOUR ACADEMIC QUALIFICATIONSIf you have undertaken extra-curricular activities, or hold positions of responsibility at school, tell us why you sought these, and why they are important to you. You will not impress us by simply recounting that you took up a placement in Thailand, but we might be more appreciative if you tell us what you personally learnt from the experience, about your interaction with local people, and about shadowing the medical team working within your village. Example: I have become involved with a city music and drama group, and work especially with the younger members. I find this exciting and more than occasionally challenging. Coaching for the group has given me experience in organising others, as well as teaching them. Watching group members learn and progress is thrilling, especially in the case of one of them who has ADHD. At first he was incapable of remaining still, silent or attentive for even a few minutes, but eventually became far more focused and calmer, making excellent progress in many areas. DIRECTLY ADDRESS OUR SELECTION CRITERIA
Example: My interest has always been in how the body works in the way it does, and why. This was triggered early on by my mother's cancer, and I felt compelled to find out all about this condition, and what could be done to help treat it. I am thirsty for new knowledge, and am fascinated by the interrelatedness of systems in the human body.
Example: I read beyond the syllabus topics covered at A-level extensively, and decided to research and write an extended essay discussing ethics and science, with particular emphasis on 'living wills'. I enjoyed the challenge and discipline of studying independently, and follow recent developments and debate in this area.
Example 1: I have worked as a hotel waitress during the summer conference season, which allowed me to develop teamwork skills, and work under various time pressures. It also allowed me to interact with many different members of the public. Example 2: I took part in my school's open day, and demonstrated experiments in the Chemistry lab. During the last year I have also participated in a reading scheme, helping younger pupils with learning difficulties.
YOU WILL NOT BE ALONE IN TRYING TO OPEN WITH AN ATTENTION-GRABBING INTRODUCTION...If you try this, make sure it helps tutors to learn something about what motivates and enthuses you. Example: My vast collection of books and videos on "How the Body Works" when I was 7 years old first triggered my interest in the functions of the body. Watching the little personified, cartoon blobs that represented red blood cells run around an animated yet functioning body fascinated me and I longed to find out more. As a result, when a friend received a letter explaining their little girl had just been diagnosed with X at just 14 months old, I was intrigued to find out what this was. THE STATEMENT IS CALLED PERSONAL FOR A REASONIt should be written by you, not by your parents, siblings, or teachers. Do not plagiarise material that you find on the web as there is a great chance that such deception will be discovered. DO NOT FEEL THAT THERE IS A PRECISE TEMPLATE TO FOLLOW THAT WILL SCORE YOU POINTSWe look for bright and independent thinkers, so try to be original!
The Department of Biomedical Laboratory Sciences Biomedical Laboratory Sciences (BLS) is a challenging and rewarding health care profession that has great impact on patient care. Working in a variety of settings, laboratory scientists are essential members of the health care team who provide vital information about the status and function of the body and its systems. The data obtained by laboratory professionals is utilized in the diagnosis, treatment, and prevention of disease.  The continued success of the Department of Biomedical Laboratory Sciences is my highest priority and I am honored to serve as the chair of this important department. OUR FACULTY  Betselot Zelalem, BSHS ’20, chose to enroll in the Medical Laboratory Sciences Program at GW because it combined her interest in the molecular level of science and medicine.  “The MSHS program in clinical microbiology helped me advance to new career opportunities and increase my salary,” said Zara Tariq. “It has also given me the confidence to further my studies and driven me to continue learning in the health sciences.” 
Applying to the CLS ProgramCourtney Santos “Applying to the Clinical Laboratory Science major was the best decision I have ever made.” – Courtney Santos The CLS program will prepare students for entry-level laboratory positions and a future in a constantly growing area of health care. Now is a great time to start a career in the clinical laboratory profession, because there is a nationwide shortage of clinical laboratory personnel. Our graduates have multiple job offers when they complete the program and go on to have rewarding careers in a wide variety of positions. We look forward to receiving applications and talking about the exciting field of clinical laboratory science. Students typically enter the Clinical Laboratory Science program after completing general education requirements and prerequisite courses. Successful completion of the prerequisite courses listed under the major does not guarantee admission to the program. CLS students are selected on the basis of science and math prerequisite courses, grades, a written application, interviews, and letters of recommendation. Students who already have a baccalaureate degree and have the CLS prerequisite courses may apply for admission to the program and request a second baccalaureate degree from UNC-CH. Because enrollment is limited, students are encouraged to begin the application process early in the fall preceding the year of enrollment. Completed applications received by the second Tuesday in January will receive first consideration for admissions. Completed applications received after that date will be considered if there are positions available in the program. Transfer students should note that the last day to apply to the CLS program through Undergraduate Admissions is February 15th. Transfer students are encouraged to apply as early as possible to allow ample time for transcript evaluation. Please also review our “ Information for Transfer Students ” page. Please note: If you intend to work in a state that requires licensure of clinical laboratory personnel, you are advised to read the information on our Certification and Licensure page before completing your application for the CLS program. Beginning the application:
Within the online application, it will ask for information including:
Please remember, as applicants complete the online application they should:
Application Assistance:If students have questions about the application process, they should email [email protected] . If there are any technical difficulties, please contact the UNC help desk at (919)962-HELP (919-962-4357).
Guide to GCSE Results Day Finding a job after school or college Retaking GCSEs In this sectionChoosing GCSE Subjects Post-GCSE Options GCSE Work Experience GCSE Revision Tips Why take an Apprenticeship? Applying for an Apprenticeship Apprenticeships Interviews Apprenticeship Wage Engineering Apprenticeships What is an Apprenticeship? Choosing an Apprenticeship Real Life Apprentices Degree Apprenticeships Higher Apprenticeships A Level Results Day 2024 AS Levels 2024 Clearing Guide 2024 Applying to University SQA Results Day Guide 2024 BTEC Results Day Guide Vocational Qualifications Guide Sixth Form or College International Baccalaureate Post 18 options Finding a Job Should I take a Gap Year? Travel Planning Volunteering Gap Year Blogs Top Rated Personal Statements Personal Statement Examples Writing Your Personal Statement Postgraduate Personal Statements International Student Personal Statements Gap Year Personal Statements Personal Statement Length Checker Personal Statement Examples By University Personal Statement Editing and Review Service Personal Statement Changes 2025 Personal Statement Template Job Interviews Types of Postgraduate Course Writing a Postgraduate Personal Statement Postgraduate Funding Postgraduate Study Internships Choosing A College Ivy League Universities Common App Essay Examples Universal College Application Guide How To Write A College Admissions Essay College Rankings Admissions Tests Fees & Funding Scholarships Budgeting For College Online Degree Platinum Express Editing and Review Service Gold Editing and Review Service Silver Express Editing and Review Service UCAS Personal Statement Editing and Review Service Oxbridge Personal Statement Editing and Review Service Postgraduate Personal Statement Editing and Review Service You are hereBiomedical sciences personal statement example 38. The University of Oxford defines biomedical science as the “focus on how cells, organs and systems function in the human body” but to me, this is a very basic definition of something that means a lot to me. It is the chance to learn more about the subject that I am passionate about, the chance to be able to diagnose diseases in advance and prolong someone’s life, the chance to make a difference in the world. For as long as I can remember, I have always been surrounded by medical based subjects from first-hand experience while at the doctor to work experience and TV shows based around the subject. I am applying to the biomedical science courses as it is something I have a great interest and passion in. By taking biology and chemistry at a higher level, I have expanded on my knowledge on the subjects but I am still not satisfied with just this knowledge and wish to learn more. Gaining a qualification in the biomedical spectrum would allow me to get a job as a biomedical scientist which is my main goal for the future. I feel like by gaining this qualification and being able to get a job, I will be able to do something that I love everyday while having the opportunity to learn new things every day. Spending my days in a hospital laboratory feels like the right career path suited to me as a person and my interests. My main aim in life would to be to gain this qualification after 4 years of studying hard and be able to work as a biomedical scientist in a hospital lab researching, diagnosing and treating diseases. This is a career option that very much excites and motivates me to be the best in my studies and further education. I am interested in all the subjects under biomedical science including clinical biochemistry, haematology, histopathology, cytopathology, medical microbiology and blood transfusion and would love to be able to have a deep enough understanding of them all so that I may find one that I am most suited to and continue with it in a full time lab environment. I have taken part in several different work experience opportunities including working at a local primary school gaining people skills and working at a vet practice gaining lab, people and general world of work skills for a working environment. In summer 2015, I organised a work experience placement which I felt would help me gain a further understanding in the career of a biomedical scientist and so over a few month of emailing several people in the field I was able to arrange a week work experience placement in the holiday. This was extremely beneficial as I worked in all different fields and undertook several different jobs within these fields to gain first hand skills and knowledge I would not be able to get from the internet or a classroom. I was lucky enough to be able to get a work experience opportunity in the biomedical sector at Aberdeen Royal Infirmary, where I had the chance to experience each individual segment of biomedical science they had to offer including pathology, microbiology and haematology which I found the most interesting. Alongside myself in the lab were current biomedical students as well as qualified ones. This was important for me as I could ask questions regarding their study and work, get answers and see different opinions on what it is like. I have gained many qualities from volunteer work, school experiences, extra-curricular and hobbies that I believe are crucial to university life and in the world of work. I have been volunteering as a youth leader in a young choir called ACE. Empowerment of people to believe in themselves through a wide range of activates such as singing, dancing, outdoor activities and performing. Through this group I have developed a wide range of skills such as leadership and teamwork. An example of my skills gained in leadership can be seen when I took control and planned and carried out a performance at a local care home and organised donations for the home. Teamwork can be regularly seen when working with young children, people the same age as me and older people in order to get a job done. Through ACE choir I have achieved my 500 hour Saltire volunteering award as a sign of my dedication and hard work over the years. I am currently working towards a new award and am at 700+ hours. During summer 2015, I spent 2 weeks volunteering as part of the staff team at the Aberdeen International Youth Festival as a member of the Events Team. During this time, I stayed in university dorms and mingled with many current students. Through this experience, I gained skills such as management, time keeping and team skills which I feel could help me if I were to get a place at university. I have undertaken many roles in my time at secondary school. I have achieved junior, half and full colours for my dedication to clubs over the years such as debating, choir and rock challenge. In S5 I was given the title of a prefect and was again awarded it in S6. Throughout my time as a prefect I have gained time management, organisation and public speaking skills which I believe are very important not just at university but later in life when perusing a career. In 2014/2015 school year, I worked towards my leadership award. This was a challenging course that involved researching, planning and executing an activity off our own backs. I found this a lot of fun and learned a lot about myself and my skills and qualities through it. I also have the title of a school mentor and assistant librarian within the school. This has helped me with my interpersonal skills. I spend my time assisting people with their queries on different subjects, checking in and out books and promoting the library throughout the school. Being a mentor has really helped me mature as I have to out others feelings and needs before my own. As well as classes and revision classes, I am involved in many activities. After being let down by my school, I organised for myself and several friends to complete our bronze Duke of Edinburgh award with an open award centre. It was a daunting process but we completed it with smiles on our faces. I then proceeded to silver and the gold with the award centre where I worked with people I had just met and created lifelong friends and memories. Being asthmatic, the expeditions were always a struggle for me but I pushed forward. This is a great example of the fact that if I put my mind towards something I will get it done. After finishing my Gold Duke of Edinburgh, I was invited back to become a Bronze level leader where I will help and encourage those who are involved. My hobbies include music, science and Japanese culture and language. I am a self-taught ukulele player and love to sign and write music. I have not yet preformed with my ukulele but have plans to do so in the near future. I have performed by myself, as a duo and as part of a choir many times and love the thrill of performing for others and doing what I love. From this I have acquired a lot more confidence when preforming and further developed my time management skills while balancing my hobbies, revision, school work and having time for family and friends. During my years at school I have always loved science and more importantly biology, because of this I have been enrolled in the OU course entitled Molecules, Medicines and Drugs: A Chemical Story. Through this course I am gaining a SCQF 7 grade (equivalent to an SQA graded advanced higher Scottish baccalaureate) I which I will receive at the end of the course after I sit my exam in February. This course involves standalone study which, alongside group work, is a key element of further education. The fact that this course is related to what I want to study in further education reflects my dedication to the subject as it is a lot of work. For many years I have been interested in Japanese language and culture. Recently, I decided to take this interest more seriously and have begun to self-study Japanese language. Despite it being a hard subject to learn, I have not given up and continue to push through. Profile infoThere is no profile associated with this personal statement, as the writer has requested to remain anonymous. This personal statement is unrated Related Personal StatementsAdd new comment. ORIGINAL RESEARCH articleDairy farmers’ considerations for antimicrobial treatment of clinical mastitis in british columbia and alberta, canada. 
Introduction: Clinical mastitis (CM) treatment decision-making is a multifaceted process that remains relatively understudied, despite CM being one of the most prevalent diseases on dairy farms worldwide, contributing greatly to the use of antimicrobials in the dairy industry. This study aimed to gain insights into decision-making mechanisms employed by dairy farmers in British Columbia and Alberta, Canada, when dealing with CM. Methods: Interviews were held with 15 dairy farmers in the Canadian provinces of British Columbia and Alberta and analyzed using reflexive thematic analysis to develop both the decision-pathway and overarching themes influencing the CM decisions by farmers in this region. Results and discussion: The analysis generated a decision-making process that begins with identification and classification of CM, guided by visual characteristics of milk and the udder, available milk production and quality data, presence of systemic signs, and additional diagnostics. Subsequently, CM cases are assessed based on the likelihood of cure, value of the cow, and herd goals to decide whether antimicrobial treatment is desired. Next, a treatment choice is made by evaluating severity and urgency of the case, availability of drugs and timing of the case. Finally, definition of treatment success and progression over time following the treatment decision guides the termination of treatment. Three overarching themes were generated that shape the decision-making process: ‘Personal attributes’, including personal approach and experiential knowledge; ‘Inter-actor dynamics’, such as shared decision-making and dynamics among producers, veterinarians, and milkers; and ‘Moving beyond protocols’, which highlights the dynamic nature of mastitis decision-making. These insights have the potential to inform the development of effective interventions to improve CM antimicrobial use that align with the reality of farming operations within Western Canada, and potentially beyond. 1 IntroductionMastitis is an inflammation of the udder, marked by various physical and chemical changes in the milk and the udder tissue ( 1 ). Visual confirmation of changes to the milk classifies clinical mastitis (CM), with more moderate cases also showing inflammatory signs in the affected quarter(s), and severe cases including signs of systemic illness ( 2 ). While yeast, algae, external particles, and udder trauma can cause mastitis, CM is predominantly caused by bacterial pathogens. Therefore, intramammary antimicrobial administration is the recommended and widely adapted treatment for CM, often accompanied by systemic antimicrobials and pain medication in severe cases ( 3 ). Mastitis is one of the most prevalent diseases on dairy farms world-wide ( 4 ), with an average CM incidence in Canada of 19 cases per 100 cow-year ( 5 ). With treatment rates averaging between 90 and 100% ( 6 – 8 ), CM treatments contribute greatly to the total amount of antimicrobials used on dairy farms. When coupled with dry cow therapy, intramammary antimicrobial use accounted for 66% of total antimicrobial use on Canadian dairy farms during 2019 and 2020 ( 9 ). While direct implications of mastitis to the farm owner primarily include economic losses stemming from preventative measures, culling, reduced milk yield and milk discard—estimated at CA$744 per CM case ( 5 )—implications of mastitis-related antimicrobial use extend to broader concerns surrounding antimicrobial resistance ( 10 ), which necessitates responsible use of antimicrobials on dairy farms. In addition, due to the frequent nature of mastitis, in many countries including Canada, farmers are allowed to administer antimicrobial intramammary treatments following protocols and antimicrobials prescribed by their herd veterinarian, adding depth to their role as farmer. In the context of mastitis management, many Canadian dairy farmers have embraced practices aimed at improving udder health within their herd, such as proper milking procedures and vaccines, although the latter are still not widely adopted ( 5 , 11 ). The practice of analyzing CM milk samples to guide antimicrobial treatment decisions has existed for some time, their importance to reducing antimicrobial use further highlighted in recent efforts ( 12 ). However, the adoption of analyzing CM samples is less than optimal, as evidenced by a survey among Canadian farmers ( 8 ). To ensure effective adoption of such interventions and to enhance antimicrobial stewardship among dairy farmers, a comprehensive understanding of on-farm CM treatments decision behavior remains critical ( 12 , 13 ) and is often overlooked when implementing or suggesting interventions, leading to a lower-than-expected compliance ( 14 ). The decision-making process for treating CM with antimicrobials is multifaceted and has a complex decision structure. Vaarst et al. ( 15 ) described in the early 2000s for Danish dairy farmers, that their decision-making included weighing various information sources including SCC, CM case history, lactation stage, reproduction status, value of the cow, availability of replacement heifers, bulk tank SCC, and availability of alternative treatments. Recent survey results highlighted the differences in priority of these decision-factors among Canadian farmers ( 8 ). Although these results suggest that these priorities shape the decision-making process of individual farmers, the quantitative study design did not allow for an exploration of underlying causes. This is particularly of interest as research into general antimicrobial use has underlined that intrinsic and extrinsic factors impact antimicrobial use decisions. These factors include attempts to increase the chance of cure by treating as quickly as possible, motivation to improve animal welfare, perceived efficacy of chosen treatments, and external referents such as other farmers and the herd veterinarian ( 16 – 18 ). Although it is unsure how these factors play a role in CM decision-making. To address the lack of a comprehensive and nuanced understanding of CM-related antimicrobial treatment decisions among dairy farmers, given the modern landscape where numerous tools and techniques are available to the farmer to enhance udder health and refine antimicrobial treatment choices, this study used a qualitative approach to investigate the core of dairy farmers’ practices and decision-making mechanisms around CM treatment decisions. As opposed to quantitative research, qualitative research can facilitate in-depth exploration with farmers, thereby allowing participants to share their experiences, priorities and thought processes. Interviews also offer a personalized and contextual understanding. As such, the qualitative approach of this study will be able to capture insights in CM decision-making that quantitative methods might overlook. 2 Materials and methodsThis study was reviewed and approved by the University of Calgary Conjoint Faculties Research Ethics Board (# REB21-0699). This report was written according to the Consolidated Criteria for Reporting Qualitative Research (COREQ) framework ( 19 ). 2.1 Positionality statementThe lead author (EdJ) is female, 29 years old, and holds a PhD in Veterinary Medical Science from the University of Calgary. Her PhD research focused on mastitis-related antimicrobial use on dairy farms, a topic on which she and her colleagues have published several manuscripts. EDJ’s knowledge of the dairy industry came from research projects conducted in the Netherlands and Canada as part of her BSc and MSc degrees in Animal Sciences at Wageningen University in the Netherlands, and from her work in her PhD. EdJ comes from a family of dairy farmers, and though her grandparents were the last ones to own a farm, many relatives still work in the agri-business. EdJ lived in the Netherlands until the age of 24 years, and thus shares a cultural background with many of the participants as Dutch ancestry is common among Western Canadian dairy farmers. EdJ is a dairy product consumer and a left libertarian according to the economic/social political compass. Since EdJ’s research has been largely quantitative in nature, she familiarized herself with qualitative research methods and analysis through auditing courses, extensive reading, and collaboration with colleagues with experience using qualitative methods. All other authors work or study in dairy veterinary science and have a range of training in, and experience with, qualitative research methodologies. 2.2 Data collectionData were collected through semi-structured interviews between June 2022 and August 2023. Participants in the Canadian provinces of Alberta and British Colombia were recruited through existing connections of the researchers and through extension events. As such, participants were aware of the study interests of the researchers. Potential participants were shortlisted based on their herd size, milking type, and location to ensure a variety in farm management practices. A telephone script was used for recruitment by phone. During the recruitment, special attention was paid to scheduling the interview with those responsible for most CM treatment decisions. Consent was sought either on paper prior to the interview or orally, if the participant was unable to sign the paper consent form ahead of the interview. A short online questionnaire, using the software platform Qualtrics (Seattle, WA, United States), was sent ahead of the interview to acquire information regarding milking system, number of milking cows and production parameters for each farm ( https://data.mendeley.com/datasets/hv9h7k499b/1 ; 8 ). Interviews were conducted using Zoom (Zoom Video Communications, San Jose, CA, United States) or in-person upon the producers request if the location of the farm was within 200 km of the University of Calgary. One interview was conducted by phone due to lack of an internet connection on the farm. In-person and phone interviews were voice-recorded using 2 recording devices (Philips VoiceTracer DVT2050). Zoom-interviews were video- and voice-recorded using both the recording device as well as the Zoom recording function. All interviews were conducted by EdJ, except for 5 interviews which were conducted by EdJ and IvdV together. Interviews were guided by a semi-structured interview script and consisted of 3 parts ( https://data.mendeley.com/datasets/hv9h7k499b/1 ; 8 ). First, questions were asked to build rapport and gain an understanding of the farmer’s background and the farm itself, including personnel situation and the farm’s strengths and challenges. Throughout this text, ‘farmer’ refers to an individual who has financial ownership and investment in the farm. In the case of some participants, this person may also participate as a milker, train employees on recommended milking procedures, and, in collaboration with the herd veterinarian, may assist in the development and implementation of mastitis diagnosis and treatment protocols. This individual may also be responsible for relaying that information to other on-farm employees who will implement established protocols. All participants were in a position of decision-making autonomy either solely or in collaboration with another farm owner. Secondly, participants were asked to describe their most recent CM cases, using their own definition of CM. Follow-up questions covered case identification, information sources consulted, communication between farm personnel and veterinarians, treatments considered (both antimicrobial and non-antimicrobial, including anti-inflammatory), and treatment expectations. Various CM cases were discussed with each participant, until both the interviewer and the interviewed farmer were satisfied that the full range of scenarios on the farm had been discussed. Lastly, questions were asked regarding on-farm antimicrobial stewardship, which will be analyzed and published separately. The interview guide was not pretested, but the researchers revised and adapted the guide in an iterative fashion at several instances during the data collection process to further explore generated themes. The interviewers were free to rephrase questions and use probing questions throughout the interview. Duration of interviews averaged 55 min ranging from 35 to 79 min. The interviews were transcribed verbatim with the help of the automated transcription program Otter.ai (Los Altos, CA, United States) and checked for accuracy. The first 5 interviews transcripts were checked by both IvdV and EdJ, the other 10 transcripts were checked by EdJ. Participants received an anonymous participant ID and are referred to in the paper as P#. 2.3 AnalysisThe CM decision-making process can be classified as multifaceted and complex in nature ( 20 ), which warrants considering them within a broad context that goes beyond traditional hierarchical decision research ( 21 , 22 ). Reflexive thematic analysis was therefore chosen for this research, as its reflective approach allows for use of the critical realist paradigm compared to the constructivist paradigm of the classical decision research concept ( 23 – 25 ). All interviews were analyzed by the principal researcher (EdJ). After familiarization with the data, segments of text that captured meaningful information related to the farmers’ CM treatment decisions were paraphrased into codes. The inductively generated codes were recorded in the online diagramming tool draw.io (JGraph Ltd) and collated to generate the different facets of CM treatment decisions, as well as to simultaneously generate themes that ‘overarch’ the core concepts of the CM treatment decision pathway. Codes and themes were refined and revised by re-reading transcripts and identifying quotes to provide context. This iterative process, in combination with extensive discussions between EdJ and A-MS regarding data interpretation, ensured rigorous and insightful representation of the data. After the analysis was finalized, all participants were offered the opportunity to validate the draft manuscript to ensure that their views were accurately captured ( 26 ). An assessment of ‘information power’ was used to identify whether enough interviews were conducted to obtain a good understanding of farmer decision making regarding clinical mastitis treatment in Western Canada. Information power is preferred over ‘data saturation’ in reflexive thematic analysis ( 25 ), because it aligns with the understanding that meaning is generated through interpretation rather than being discovered, making the determination of sufficient data inherently subjective and context-dependent ( 27 ). Information power suggests that the more relevant information the sample holds for the actual study, the fewer participants are needed ( 28 ). Information power depends on the width of the study aims, sample density, the use of an established theory, or not, quality of dialog, and analysis strategy ( 28 ), and was assessed continuously throughout the iterative process of data collection and analysis to determine the sample size. Fifteen interviews were conducted with 17 dairy farmers in the Canadian provinces of Alberta ( n = 11) and British Columbia ( n = 6). In total, 24 farmers were approached, of which 4 could not participate due a lack of time, 3 were unable to respond to scheduling requests, 1 did not feel the interest of the study aligned with their farm goals, and 1 was no longer in operation. Participants were either farm owners or herd managers, each actively involved in CM diagnosis, treatment decisions and udder health management. The farms were a mixture of those milking in a parlor (n = 8) and with automated milking systems (AMS) ( n = 7). One farm produced grass-fed milk; the other 14 farms operated conventionally, meaning they were not required to adhere to specific production labels such as organic or grass fed. As organic dairy farms have to adhere to more strict regulations regarding AMU ( 29 ) which can affect decision-making mechanisms on treatment of CM, organic dairy farmers were excluded from this study. One farm was part of a Hutterite colony. Hutterites, a German speaking community, have a distinct communal structure and are accountable for a substantial portion of dairy production in Alberta ( 30 ). Almost all farms were staffed by a combination of family members and external employees, with the larger parlor farms employing additional individuals to aid with milking. Most interviews were conducted with 1 interviewee, whereas during 2 interviews 2 interviewees were present. In total, 15 farmers were male and 2 were female. Production characteristics of the dairy farms are described in Table 1 ; study sample averages are in accordance with provincial averages. 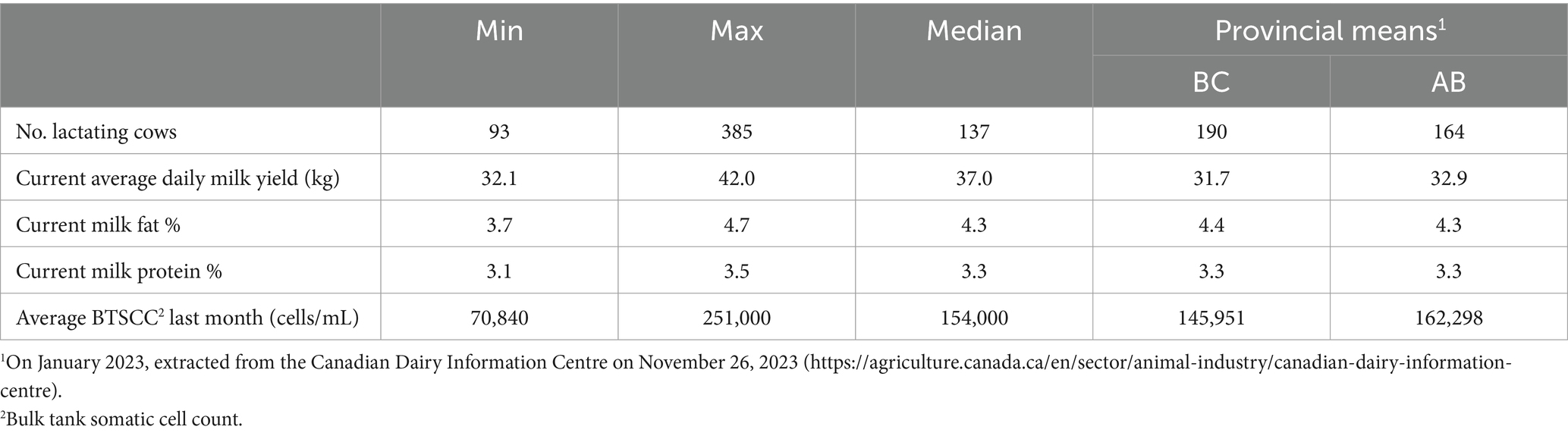 Table 1 . Milk production characteristics of the study farms ( n = 15) associated with the participants interviewed ( n = 17) between June 2022 and July 2023. 3.1 Clinical mastitis decision pathwayUpon thematic analysis of the transcripts, a decision pathway ( Figure 1 ) was developed that all farmers followed regarding their CM antimicrobial treatment decisions. This pathway included various considerations at each step. Identification and classification of CM cases formed the start of this pathway (which differed depending on milking system), followed by an evaluation of likelihood of cure, perceived value of the cow, and herd goals to arrive at a treatment approach. Next, treatment options were considered based on severity, drug availability, clinical signs, and timing of the case. The decision pathway ended with an assessment of treatment expectations and progression to determine treatment termination. 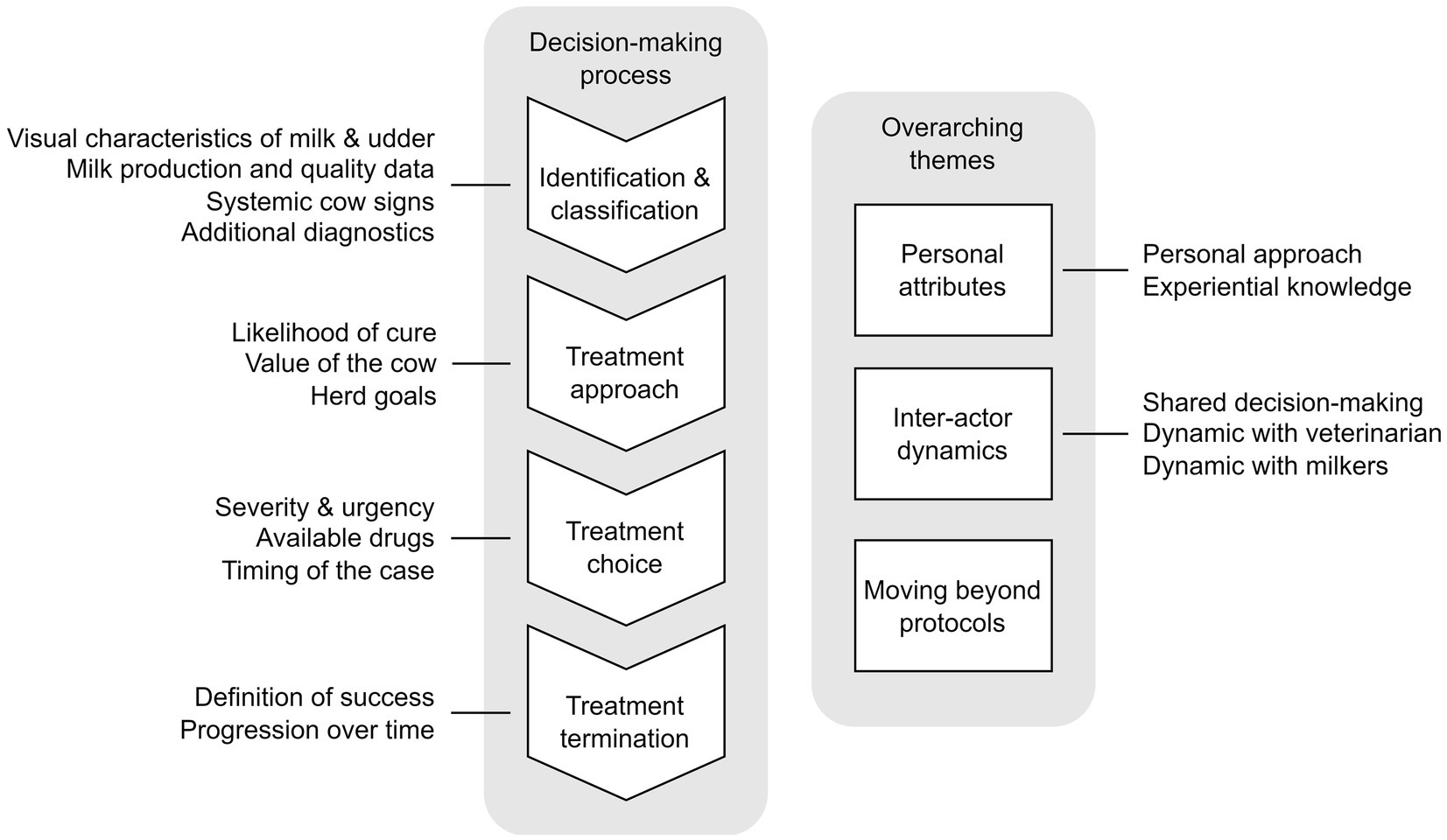 Figure 1 . Sequence of considerations for antimicrobial treatment of clinical mastitis cases and overarching themes, based on interviews ( n = 15) with Canadian dairy farmers ( n = 17) in Alberta and British Colombia between June 2022 and July 2023. 3.1.1 Identification and classificationAll participants described direct visual confirmation of clinical signs to be most important in identifying CM, which includes presence of flakes, discoloration, and milk consistency, as well as hardness and temperature of the udder quarters. One farmer described this as: “Usually you see any abnormality like the color of the milk, or any kind of swelling of the quarter or chunks or watery milk or anything like that” (P4). These observations often took place during the fore-stripping process in the parlor. Some farmers described their high proficiency to identify CM cases by relying on subtle indicators such as differences in udder shape. One farmer described: “You use a teat dip cup. You touch the udder with the top. So, you have another option that you think like hey, this is maybe not right” (P6). Next, to visual identification in the parlor, participants also used milk production and milk quality data to shortlist cows with a high likelihood of CM, after which identified cows were subjected to visual examination. Specific indicators include changes in milk production, SCC data obtained from DHI records or AMS, conductivity, instances of milk filters clogging due to the presence of clots or cows milked with AMS who had incomplete milkings: “I look at my cell count list when I do DHI, and I’ll see if there’s anybody high that’s surprising” (P4), and “As soon as one cow has something that will stick on the milk filter, it is noticeable. So really, that’s the first line” (P13). Indicators were used alone or in combination. On farms with AMS, missed visits to the AMS were also viewed as an indicator for udder health problems: “I’d say my biggest ones are they are not going to the robot and they are down in milk” (P17). The selection of the milk production and quality indicators was guided by data availability. However, these data were not prioritized and valued similarly by the interviewed farmers. For example, for one farmer low milk production was the starting point of CM identification: “When she comes into the parlor and there’s little milk yield, we’ll go back to the data” (P15). After having identified cows with a high likelihood of CM, the California Mastitis Test (CMT) was typically used to pin-point the inflamed quarter. A farmer detailed this process, explaining: “We’ll flag them in the parlor so that we see them. And then we’ll do a California Mastitis Test on them” (P16). The third route to identify CM included an overall assessment of the cow’s wellbeing, including behavioral pain indicators such as kicking during milking, reduced activity levels, decreased rumination and other systemic inflammation signs such as fever. This was described by one producer as: “If we were to visually see that the cow is dropping in milk, or if she’s looking skinny—we also have the Heatime system [real-time monitoring through ear or neck tag; Heatime® Pro+, Allflex, Saint-Hyacinthe, QC, Canada], so the rumination and the activity. If we start seeing them going down that way, we would intervene” (P5). More specifically, for severe CM cases, farmers described the presence of a hard quarter, watery milk, a severe decline in milk production, a sore udder, or behavioral pain indicators such as kicking: “She’s downhill for real. Milk clear, watery looking, and swollen udder, fever” (P16). A rapid onset of these clinical signs was also mentioned as an indicator for severity: “… speed of onset and severity of symptoms. If the whole quarter is packed right full of junk right away then I’m not gonna put out, I’ll treat her right away” (P4). Severe cases that included the combination of a hard quarter and watery milk were referred to by many farms as “ coliform” mastitis, or “ E. coli” despite the absence of diagnostic culturing to confirm causal pathogen: “And then we have coliform which comes out as orange [milk] and the udder is hard, rock hard” (P17). Definition of chronic cases varied among the interviewed farmers, but commonly mentioned were cows with persistent high SCC and those with frequent recurrence of CM, as detailed by the farmers: “They have flakes, and they do not go away. Every milking, they come in and you strip them out and you’ll mint the udder and for weeks” (P1), and “… anything that regularly has a cell count over 250–300,000” (P4). The interplay of these three identification pathways: (1) direct visual confirmation of clinical signs and milk characteristics, (2) cows with a high likelihood of CM based on specific indicators, and (3) overall assessment of the cow’s wellbeing was intricate and farm-specific and was further influenced by the milking set-up (AMS vs. parlor). For example, on AMS farms, identification through data often preceded visual checks. One of the interviewed farmers milking with an AMS explained: “I track our mastitis through conductivity per quarter via the robots, and from there we paddle test with CMT, and make our assessment from overall look of the cow, the look of the milk, the volume of the milk and how well the cow is eating” (P14). In contrast, on parlor farms, visual confirmation overall preceded analyzing data, as other farmers who milk in a parlor explained: “Then [after the milker calls with a case of mastitis] I pop onto the computer and check the history, whether she was down in previous milkings or not” (P1). All farmers underscored the significance of visual confirmation of clinical signs before treating a cow: “I would want to be seeing a drop in milk, I want to be seeing changing [milk] color, CMT paddle tests, all that before treatment goes into place” (P14). Farmers also highlighted the significance of other subtle differences in identification of CM in AMS vs. parlor systems. AMS are less able to detect flakes in the milk, which can change the perception of CM by the farmer. As one farmer stated: “When we were pre-stripping in the parlor and she had pieces, we would treat them. But now you have got the robots. And you do not see all the pieces, and the cows are fine. So, it has been a gradual progression here. Mastitis is always going to be there, but it does not all have to be treated” (P10). However, it was also mentioned that AMS allow for more frequent SCC reports, making an interpretation of high SCC values possible within the context of an extended period: “Now that we are every day seeing their somatic cell score, and you realize that what we would have thought with DHI as a clinical case of this cow, that 2 million, in robots, she might be 2 million for a few days, and then she’s down to nothing” (P5). Some farmers adopted an analytic approach by regular culture of milk samples through their DHI laboratory or veterinary clinic. Although some farmers cultured each CM case, it was more common among the interviewed farmers to only submit samples of specific cows or cases for culturing to confirm the presence of pathogens in the udder or determine the causal agent of an abnormal cluster of CM cases: “To see whether they actually had bugs in the quarters, or if it was just inflammation causing flakes to show up” (P1). Testing fresh cows was common, as described by one farmer: “We test all the fresh cows for Staph. at day six and day eight” (P12). This method allowed for the identification of intramammary infections at the start of the lactation. Seldomly were diagnostic tests used to evaluate treatment efficacy: “It’s when we see issues with the treatment, like if it’s not working being effective, then we’ll culture to see if there’s a new bug, or if we should be using a different antibiotic” (P14). Identifying other potential causes of clinical signs was also an essential aspect of making treatment decisions. Noting these served as an additional tool to identify cases that might not benefit from antimicrobial treatment. This ranged from improper milking settings to the presence of malformed teat ends: “Some older cows will potentially have a bad teat end, or something that’s just not perfect. It does not seem like it’s dangerous to them. It’s not milk you want to drink or ship, but they will recover on their own” (P13). 3.1.2 Treatment approachAfter CM cases were identified, a treatment approach was determined. Farmers described starting with an assessment of the potential efficacy of antimicrobial intervention as compared to non-antimicrobial approaches, followed by an evaluation of the value of the cow, herd goals and weighing of alternative treatment options. These aspects interacted with each other and were considered together to determine a treatment approach with or without antimicrobials. To determine the likelihood of cure when administering antimicrobial treatment, the same indicators were often used as those used for identification and classification of CM cases. More specifically, where changes in milk production, SCC, and conductivity were used to identify CM cases, farm-specific thresholds were used by some to inform the likelihood of cure and presence of chronic infections: “like maybe a 50% drop in milk” (P1), and: “The vet considers a mastitis case anything over 400 [thousand]. To me, that’s not worth the headache or the treatment. Because give her some time, and she might drop back under 400 without treatment. Because somatic cell count numbers can be all over the place” (P8). If cases did not meet the threshold, antimicrobial treatment was often withheld. The assessment of cure also included an evaluation of lactation stage. A more pro-active treatment approach was often taken with fresh cows experiencing CM, as the transition period is known to increase physiological stress. Farmers expressed worry about the occurrence of other health conditions, and progression to worse forms of mastitis in fresh cows if left untreated: “They’re under a big transition, so they just do not have any reserves. And I think that’s when it [mastitis] can go [get worse]. It can be more deadly. They just do not have the same fight, or the same immune response [as cows later in lactation]. Their body is worried about 100 other things” (P13). For most cases, history of CM in the same quarter was evaluated, although thresholds and associated actions differed by farm. Where one farmer had a strict rule: “If it’s the third time, we never treat again” (P3), others also considered the timing of repeated cases: “I would say if they relapsed right away, we would have them on a beef truck. But if they relapse in a couple of weeks, we would retreat them” (P17). The reason for this threshold was explained as: “I usually find that the treatment does not work [in those instances]” (P17). Similarly, if cows were deemed ‘chronic’, it was likely that she will not receive treatment: “If she’s chronic, sometimes I do not treat her and [farm owner 2] will say ‘beef her’” (P17). By incorporating these different elements, farmers tailored their treatment strategies to individual CM cases. For those farmers who used additional diagnostics by sending milk samples to a laboratory for bacteriological culture or cultured milk samples on farm, outcomes of these tests were almost never factored into decisions regarding the treatment approach. Instead, they informed general herd trends or allowed for identification of subclinical mastitis among fresh and chronic cows. However, farmers articulated a level of confidence gained from the test results: “This incubator did not change my protocol at all, because I should have treated her anyway. So, it was good. Yeah. But it is nice to know” (P1). Non-severe CM treatment approaches were often tied closely to culling considerations. An assessment was made of the cow’s contribution to the herd’s overall value. As such, low producing cows, non-pregnant cows and cows with chronic mastitis were more likely to be put on the cull or do-not-breed lists instead of receiving treatment for non-severe CM. In contrast, pregnant or high-producing cows were less likely to be culled and were thus more likely to be considered for treatment: “If a cow was pregnant, and she has good genetics, and she’s at 200 days in milk, and she develops a chronic mastitis, we’ll just milk her and dump it in the ground for the rest of her lactation with the eye to either trying to clean up in the dry period, or the worst case scenario if we get one more calf out of her” (P3). Cows in their first lactation were also less likely to receive treatment and be culled instead: “If it’s a first lactation, forget it, she’s probably gone. We’re not going to mess around. First lactation heifers should have zero issues” (P17). The farmer’s personal feelings toward specific cows also played a role. A cherished animal might receive more attentive care than her counterparts, potentially leading to antimicrobial treatment. One farmer explained: “If it’s secondary [case in lactation], and I really liked her [personally], then, you know, she has a good chance of being treated again” (P3). Certain herd goals also came into play when selecting a treatment approach, including milk production incentives under the Canadian milk supply system and limitations imposed by provincial milk boards on the level of bulk tank SCC (BTSCC). In scenarios where mild CM cases did not adversely affect overall milk quality, farmers described opting to withhold antimicrobial treatment or stop treatment as soon as improvements were seen, to fulfill targets. One farmer described: “If I see enough improvement, then I do not continue for another [additional treatment] day because I do like to see milk in the tank” (P12), and another described: “Depending on how we are doing with our quota that month, they [cows positive for Staph. aureus ] either get shipped, or if we need to, we keep milking them for a while” (P12). 3.1.3 Treatment choiceAfter selecting a treatment approach, different treatment choices were considered by the interviewed farmers, depending on severity, drug availability, and other factors. For severe CM cases, common practice among the farmers was to invoke an assertive and comprehensive treatment approach, which farmer P13 referred to as the ‘shotgun’ approach, where a combination of intramammary and systemic antimicrobials, alongside anti-inflammatories and pain medication were administered: “First, Cefa-Lak [cephapirin sodium] in the quarter. Then I will separate her out and if she has a fever of like, 102–103 [degrees Fahrenheit] and above, I’ll do Trimidox iv [trimethoprim-sulfadoxine]. And then, like, Banamine [flunixin meglumine] for pain” (P13). Such an aggressive therapeutic strategy was motivated by several critical factors: a sense of urgency to address the cow’s need promptly, to prevent further decline of the cow’s health, and to increase the cows’ survival chances, as underscored by the following statement: “before she goes septic, to get that IV antibiotics in her system. The main objective: save the cow” (P14). This also holds for CM cases that initially were classified as non-severe but showed a worsening of clinical signs in the following days. For moderate and mild CM cases, intramammary antimicrobials were deemed sufficient by most of the interviewed farmers: “When a cow has mastitis, our main mode of treatment is Cefa-Lak [cephapirin sodium]” (P5), and cases were monitored for worsening of signs. Only a few farmers took a more aggressive approach for non-severe cases. For example, one farmer used a protocol where a 5-day course intramuscular antibiotic was provided for any case: “Everybody gets Metacam [meloxicam] because they usually come with a fever. Everybody gets intramammary. In that quarter, we use Cefa-Lak [cephapirin sodium]. And then everybody gets 5 days of Trimidox [trimethoprim-sulfadoxine] treatment” (P17). Limited intramammary antimicrobial products were available to the interviewed farmers due to discontinuation of products and new regulations. For example, because of the discontinuation of the intramammary drug Special Formula 17,900 (a combination of penicillin G procaine, dihydrostreptomycin sulfate, novobiocin sodium, polymyxin B sulfate, hydrocortisone acetate, and hydrocortisone sodium succinate), alternatives were sought. One of the interviewed farmers described limited availability as the reason they used Cefa-Lak (cephapirin sodium), explaining: “It used to be 17,900; they do not make that anymore, right?” (P13). Another farmer co-administered a steroidal anti-inflammatory alongside intramammary antimicrobials: “In the Spectramast syringe [ceftiofur hydrochloride] we do add dexamethasone, just to get the inflammation out of the udder” (P1). Participants were divided regarding co-administration of pain medication in cows with non-severe CM. Some farmers provided pain medication in the presence of certain clinical signs of non-severe CM cases: “If we see that their [cows with non-severe CM] quarter’s hard or they are looking a little sad, we will give them also a dose of Metacam [meloxicam]” (P5). Other farmers stated that they did not give pain medication to cows with non-severe CM: “A mild mastitis? Yeah, no, probably not. I would not give pain medication” (P7). These farmers conveyed the belief that non-severe CM does not appear to cause significant pain in cows, or that cows do not show and therefore experience pain in the same way as humans do. “They’re not painful, if they are still milking 50 to 70 percent of their expected milk volumes. They just have an infection, but it is not slowing them down; it is not disrupting their eating, it is not disrupting their production substantially” (P14). This perception influenced the decision-making process, resulting in a limited use of pain medication for non-severe CM cases. In situations where cows developed CM nearing the weekend, farmers tended to adopt a more aggressive treatment approach, primarily driven by the constrained availability of veterinarians and limited options for culling during weekends. Farmers opted to mitigate the likelihood of further deterioration of the cows’ condition. This was illustrated by one interviewed farmer who said: “If it’s a Friday or a Thursday, I always treat them because we have to keep them for the weekend” (P17). For non-severe CM cases that would not qualify for antimicrobial treatment according to protocols, udder mint cream was popular among some of the farmers, as well as essential oils (such as calendula). Cream and oils were also used for more severe cases in combination with antimicrobial treatments in attempts to offer relief to signs such as hard and swollen udders. Nevertheless, a sense of skepticism existed regarding the effectiveness of these alternatives, and their use often stemmed from the desire to take immediate action of non-severe CM cases without resorting to antimicrobials: “She would maybe have gotten better on her own. But maybe it feels good. You’re doing something” (P1). Only 2 farmers mentioned the use of oxytocin: “I’m under the belief that oxytocin will, right off the bat, potentially just let [the milk] down. I’m under the belief that if the cow can let it out, that’s, eh, less to fight” (P13). 3.1.4 Treatment terminationFollowing the chosen treatment, each farmer described a process where CM cases were monitored until a set outcome was reached. These outcomes were influenced by the severity of the CM case at time of identification. When asked about assessing the cure of non-severe CM cases, the interviewed farmers provided a comprehensive list of clinical signs and production characteristics as determining factors. These included the absence of flakes in the milk, lower SCC, resolution of udder tenderness, and restoration of milk production to normal levels. For example, one farmer shared: “You hope to see a cow with low somatic cell and milk production back to expected [levels] or higher” (P14). For severe CM cases, treatment expectations were more temperate and included indicators such as an increase in milk production, absence of clinical and systemic signs, and survival of the cow. More specifically, farmers expressed pessimism regarding the recovery of cows from severe CM cases if substantial inflammatory signs were present at time of diagnosis: “If she does not respond within a few days, the outcome is not very good. Then she will probably be dead within five days” (P7). Similarly, for chronic cases, treatment expectations were also tempered: “Chronic cases that kind of get it [CM], and then it goes away. And then they have a high somatic cell count for a while. Some of those ones do not always respond to treatment” (P16). Multiple farmers discussed the option of drying off quarters after unsuccessful treatment. For instance, one farmer shared: “If they are chronic, and treated them or they will not respond to treatment, we have dried off quarters in the past […] And then we’ll have a three-quarter cow who still milks good. Cheaper to keep her that way” (P16). Practices diverged when the endpoint of antimicrobial treatment was discussed. Some farmers did not adhere to label instructions, discontinuing antimicrobial treatment after 2–3 days: “If they are still clinical, we will not just keep treating them because we should; maybe it’s already cleared up” (P16). Conversely, some farmers extended antimicrobial courses up to 5–7 days until all clinical signs had completely subsided. Some switched drugs during this period, although this was typically accompanied by a consultation with the veterinarian: “If the search [for a cure] gets longer than 4 or 5 days, I’ll start talking with my vet” (P4). Regardless, there was consensus that visible improvement of non-severe cases was expected within 3–4 days and cure was expected within a week when treatment was successful: “If we see a response, then we’d call that a success. I would assume within a week or so” (P5). 3.2 Overarching themesIn addition to the decision-pathway, three themes were generated from the interviews that ‘overarched’ every aspect of the CM treatment decision-pathway which can be described as ‘Personal attributes’, ‘Inter-actor dynamics’, and ‘Moving beyond protocols’. 3.2.1 Personal attributes3.2.1.1 personal approach. The influence of differences in approach among owners, herd managers, and milkers on dairies (where multiple people share the decision making) appeared to hold significant importance. Contrasting perspectives of the owner and the farm manager were evident during several interviews. In one interview, the owner leaned toward a more relaxed approach, preferring to observe the situation before acting, while the farm manager advocated for a proactive stance, leading to a more liberal use of antimicrobials for treating CM cases: “I [full-time farm hand] tend to treat them quicker. I am more like ‘Oh, she had flakes tonight, I’ll start treating her’. I’m quicker [to treat] where he [farm owner] will just wait and see what happens for 12 or 24 h” (P12). On this farm, it also translated into differing durations of intramammary antibiotic treatments: “I think that I [full-time farm hand] treat them longer than [farm owner] would have done too” (P12). 3.2.1.2 Experiential knowledgeThe evaluation of the factors in each step in the decision-making sequence ( Figure 1 ) was often attributed to experience by the interviewed farmers. This included generational knowledge, where certain products have been used to treat CM previously, including by older generations of farmers: “The way our dad taught us is just basically give three treatments. Give Cefa-Lak [cephapirin sodium], let us say, for example, at 5 pm, and then the next day at 5 pm as well, and the next day at 5 pm. That’s the protocol at this point” (P9). Another farmer’s perspective exemplified this generational continuity regarding abstaining from treating certain cases: “For 16 years, my dad always had the idea: ‘If they get E. coli , you just got to let them be and they either fight it and win or they do not” (P5). Experiential knowledge of outcomes of previous decisions was also important. Sometimes this pertained to previous CM cases in the same cow: “So, if we did not use Metacam [meloxicam] in the first case, or if we used Spectramast [ceftiofur hydrochloride], now we’ll use something else” (P3), and: “That one older cow, that [CM] will sometimes come in waves. We do not treat her and that’s just kind of the way I do it” (P13). Experiential knowledge also encompassed treatment outcomes of other cows with similar CM cases: “Sometimes you just think, it did not work for the last cow, is it going to work for this cow?” (P6). Farmers also linked the historical efficacy of certain treatment choices and products to treatment decisions: “I have been doing this for a little while. You can safely assume that miscellaneous case that recurs every three weeks, it’s probably a chronic Staph.” (P3), and: “Our vets have in the past said a saline solution IV helps, but we have tried, and we just give them time and put them in a straw pack and see what they do” (P5). 3.2.2 Inter-actor dynamics3.2.2.1 shared decision making. On non-AMS farms, milkers played a crucial role in identifying CM cases. Almost all interviewed farmers shared the on-farm labor with family members or external staff. The interviewed farmers detailed a close relationship between the milking staff and the farm owners. Often, the situation was described where milkers identify CM, but herd managers and owners were consulted before making treatment decisions: “They’ll either call or text me when they see a problem cow” (P4). The manager or owner typically assumed the responsibility of maintaining records for treated cows and their respective mastitis history: “I’m sort of the person that decides and has a database of what cows might be chronic, why they might be treated or not treated if they have been treated multiple times” (P3). When multiple persons on a farm were involved in the CM treatment decision making, a discussion typically only took place when cases were more complex. “If there’s a question about it, then usually [co-owner] and myself will talk: ‘Okay this cow’s got mastitis’. We take a look at her: ‘Is she one we want to cull or is she one we want to treat?’ and make that decision then” (P16). Less complex cases that aligned with protocols typically did not require consultation with other decision makers before acting, explained by one farmer as: “Sometimes there is a little bit of a discussion involved but most of the time it is automatically done” (P15). It became apparent from the interviews that if multiple decision-makers were present on a farm, their perception of cow value often differed, as well as their experience regarding the consequences of treatment decisions. This influenced treatment decision making. In one interview, these differences were highlighted: “Because he [farm owner 1] is not in here doing all the work. Right? Where she [farm owner 2] and I take turns, we have to treat these cows, find these cows and deal with these cows. And she [farm owner 2] is a lot more ‘out you go’ than he [farm owner 1] ever is” (P17). These varying stances underscore the dynamic interplay between various actors involved in treatment decisions. 3.2.2.2 Dynamics with veterinariansInterviewed farmers described that veterinarians were consulted to discuss treatment protocols as well as evaluate previous CM cases, causative organisms, the general udder health status of the herd, and chronic cases: “While the decision [to treat] lays with us, he’s [the veterinarian] with herd health. We sit down and discuss some things.” (P8). Urgency was provided as a reason not to consult the veterinarian for the treatment of specific cases, as described by one farmer: “If you wait ‘til tomorrow ‘til the vet comes out, you have waited too long” (P13). Nonetheless, farmers underlined that their herd veterinarians were approachable and easy to reach: “If I have any questions, I’ll reach out to him, and he’ll respond within a couple of hours usually” (P4). 3.2.2.3 Dynamics with milkersFarmers expressed challenges in ensuring employee adherence to protocols, especially when it came to monitoring cows with few clinical mastitis signs. Another challenge raised was that employees may not always feel entirely comfortable administering antimicrobial treatment: “It depends on who’s milking. If they are, if they know how to treat the cow or not” (P1). Employees sometimes also lack the knowledge to safely administer intramammary antimicrobials or to identify CM cases: “For the past few years, the staff I have aren’t capable. They’re very good milkers, but they just do not have that diagnostic experience and treatment” (P4). Issues with milkers were also encountered when choosing the appropriate treatment: “Although the milkers tend to want to treat [severe cases with] intramammary anyway, the treatment is generally Metacam [meloxicam]” (P3). 3.2.3 Moving beyond protocolsThroughout the interviews, farmers referred to on-farm protocols, which were often oral in nature although they remain a requirement for the mandatory Canadian national quality assurance program proAction. However, when delving deeper and probing into exceptions and exceptional circumstances where deviation from the protocol occurred, the more intricate decision-making process detailed in this manuscript emerged. For example, one interviewed farmer described their protocol with a one-liner: “Treating? Anything over a million” (P8); which was later revised, and a more nuanced picture was given that followed the various considerations depicted in Figure 1 . Similarly, for another farmer, when asked if there ever were situations to not treat cows, information about pregnancy and cull list emerged which was not included in their protocol: “If the cow’s a cull, she’s always going to be culled. And if she is only making 20 or 25 kg, we probably would not put the time or effort into that [to start treatment]” (P9). These examples illustrate that ‘exceptional’ situations occur often, and that, in practice, moving beyond the set protocol is more common than is often recognized. 4 DiscussionIn this study, we examined CM treatment decision making on 15 Western Canadian dairy farms by describing the intricacy of identification and classification of CM, factors considered during antimicrobial treatment decision making as well as subsequent drug choices and considerations around treatment termination. Three overarching themes that influenced this decision-making process were generated: ‘Personal attributes’, ‘Inter-actor dynamics’, and ‘Moving beyond the protocol’. The presented decision-making diagram aligns with conclusions drawn by Vaarst et al. ( 15 ), which covers decisions made based on clinical signs, individual cows, and the entire herd. Nonetheless, our study adds a new layer of information by specifically highlighting decision-making around treatment choice, which includes considerations of alternatives to antimicrobials and urgency of action, an aspect not studied by Vaarst et al. ( 15 ). Regardless, the overall similarity between the 2 studies underscores a consistency across 2 decades in Canada and Norway, where farmers are shown to consider the same aspects. Key aspects of the CM decision-making process as indicated in the current study have also been reported in other studies, such as the importance of case severity, SCC, suspected pathogen, and the comparison with other cases on the farm ( 31 , 32 ). These factors aid the farmer in minimizing uncertainty regarding treatment outcome, an important determinant driving on-farm antimicrobial use ( 17 ). Recent work also suggests a variability among farmers in terms of prioritization of these different decision factors ( 8 ). However, because the current study approach did not intend to quantify the relative importance of each decision factor, but rather to provide insight into the intricacies and complexities of the decision-making process, no claims can be made regarding variation in the relative importance of each of the factors among our participants. Our study also describes the process of identifying and classifying CM, highlighting differences between farms with AMS and traditional milking parlors in prioritizing the use of various types of data. Although farms with both types of milking system used milk production and quality data in addition to visual evaluation of the udder to identify CM, AMS farmers generally had access to data from more sensors and more frequent data reports, a benefit also highlighted by Swedish ( 33 ) and Ontario farmers ( 16 ). These data allow for identifying inflammation without visual evaluation, which is often the starting point of the CM identification process on parlor farms. All AMS farmers in the study reported performing a visual assessment of the udder after evaluation of data reports suggested CM, which has also been reported by German farmers ( 34 ). It is important to note, however, that farms with AMS need to regularly review available data to prevent high false-positive rates and to minimize workload ( 35 ). This is especially important when built-in algorithms are used to predict the presence of CM, as sensitivity ranges around 60–80% ( 36 ). Differences in antibiotic treatment choices between parlor and AMS farms were not assessed in the current study, although research from the Netherlands suggests that AMS farms are more likely to treat with systemic antimicrobials compared to intramammary antimicrobials due to difficulties administering intramammary antimicrobials outside the milking parlor ( 37 ). Other tools used by farmers to identify and characterize CM cases in this study included assessment of rumination and activity data. Decreased rumination is an established indicator of reduced feed intake, which has been associated with the presence of CM ( 38 ). Reduced lying time has also been described as one of the behaviors occurring during mastitis ( 39 , 40 ). Some farmers also employed additional diagnostics in the form of culturing CM milk samples. Most commonly, cultures were employed to identify intramammary infections among fresh cows, although some farmers cultured all CM cases, similar to what has been previously reported by U.S. producers ( 31 ). As such, most farmers initiated treatment without awareness of causative agent. Since certain non-severe cases (e.g., those caused by E. coli or CM cases where bacteria are not present in the udder) do not require antimicrobial treatment, culturing of confirmed CM cases is recommended before initiating antimicrobial treatment ( 12 ). Non-severe CM cases that were selected for antimicrobial treatment often received only intramammary antimicrobials, with severe cases also receiving systemic antimicrobials, reflecting protocols suggested by research in the United States ( 41 ). Although protocols were established with herd veterinarians, veterinarians were rarely consulted for individual cases throughout the decision-making process. Administration of systemic antimicrobials is considered extra label in many countries, and their effectiveness for treating severe CM cases is debatable ( 12 ). However, although administration of systemic antimicrobials should only occur after veterinary approval (and preferably after diagnostic testing), the interviews indicated that this was not always the case. Although co-administering NSAIDs has been shown to improve bacteriological and clinical cure outcomes ( 42 , 43 ), few farmers reported using pain medication for non-severe CM cases, in contrast to frequent use by Danish farmers ( 32 ). Extending CM treatments beyond label prescription was common practice, similar to what has been documented in Germany and the Netherlands ( 44 , 45 ). The predominant reason for extended treatment in our study was a continuation of clinical signs, which raises concerns about farmers inability to differentiate between intramammary infections versus just the presence of clinical signs. After a normal course of antimicrobial treatment, underlying infections are unlikely to persist for most cases with a bacteriological cause, although signs of inflammation might still be present ( 46 ). Although an assessment of a milk sample after treatment is the only way to confirm bacteriological clearance ( 47 ), this was not employed by any of the farmers in our study, likely due to time and financial constraints, although this was not covered in the interview. Regardless, awareness of the distinction between infection and inflammation among farmers is essential to prevent unnecessary antimicrobial use and risk of antimicrobial resistance ( 48 ). Through the Canadian dairy industry’s national quality assurance program proAction, dairy farms are required to have standard operating protocols (SOPs) for common antimicrobial treatments. Although such SOPs are valued by farmers ( 31 , 49 ), farmers are also known to deviate from these protocols ( 50 ), similar to results described in this study. Delving deeper into the theme ‘Beyond the protocol’ allows us to make inferences regarding the ‘thinking systems’ used by interviewed farmers. According to dual process theories, cognitive operations can be categorized into 2 thinking systems: intuitive (‘System 1’) and reflective (‘System 2’) ( 51 ). The intuitive approach involves quick, automatic decisions, often relying on associations. In contrast, the reflective approach is more deliberate, carefully considering all alternatives before arriving at a decision. The quickness with which farmers summarized their protocols early in the interviews suggests they mainly used an intuitive cognitive system when handling CM cases that fit normal descriptions. However, in complex situations such as CM decision making, cognitive operations can move from reflective to intuitive, as skills and experience develop, in line with observations in our study ( 52 ). Only when asked to delve into details of CM treatment decisions, or when discussing cases where treatment expectations were not met, did the controlled, self-aware, reflective approach emerge. This implies that most farmers’ CM decisions are more likely to be automatic and associative, where past experiences and context are considered subconsciously ( 53 ). Use of the intuitive cognitive approach for mild and moderate CM cases can introduce cognitive biases, including choices geared toward short-term gains ( 54 ). This may make antimicrobial treatments more appealing than improvements in udder health management. In contrast to the more mentally taxing reflective approach, intuitive cognitive processes place higher value on the first information that comes to mind (the ‘anchoring bias’) and tend to overestimate the likelihood of specific outcomes because they are plausible ( 54 ). These heuristic judgments are inherent biases to the intuitive cognitive process and can be mitigated through a deliberate effort to reason ( 52 ). However, they represent a challenge when trying to improve CM decision making on the farmer level. Veterinarians, in contrast to farmers, have received extensive training on the use of antimicrobials and their impacts, shaping their intuitive decision-making to include long-term gains. We suggest that interventions aimed at improving CM decision making among farmers should target methods of slowing down the decision-making process, to allow for new cognitive associations to be made which will help make more sustainable CM treatment decisions. We can also extrapolate the interplay between intuitive and reflective thinking approaches to the theme ‘Personal attributes’, especially regarding the use of different types of experiential knowledge in the decision-making process. Often, farmers displayed assessing experiential knowledge when they drew associations between the current case explored in the interview and previous cases - an example of practices guiding intuitive decisions. When treatment outcome expectations were not met, however, farmers seemed to move to the reflective approach, drawing on other experiences (such as efficacy of medication on previous cases of the same cow) to aid in decision making. The role of experiential knowledge in antimicrobial treatment decision making has also been seen in U.K. and U.S. farmers ( 17 , 49 ). Rees et al. ( 17 ) also described experimental knowledge, which relies on the outcome of deliberate testing and trials of different treatments. Experimental knowledge, however, did not emerge from the interviews in this study; this might indicate that, although it plays a role in other on-farm antimicrobial decision-making processes, this type of decision making might not play an important role in CM decision specifically. Another overarching theme generated was ‘Inter-actor dynamics’. While most CM treatment decisions were made by the herd manager, regular discussions among the operational team, co-owners, milkers, and veterinarians were common. These discussions revolved around operating protocols and herd goals. Participants described that ad hoc meetings between 2 or more actors took place to discuss cases requiring special attention. This behavior implies that actors believed that the group would reach better quality decisions together compared to solo, a characteristic of a synergetic group dynamic ( 55 ). In case of treatment decisions for CM cases that do not follow normal patterns, this assumption is likely correct, as each actor holds different pieces of information relevant to the decision making: the milker and the herd manager have daily contact with the affected cows, whereas the owner is more informed on the long-term herd goals, and the veterinarian has insight into the disease risk factors and etiology. A certain decision hierarchy, and thereby power imbalance, also seemed to be present, with owners and older generations having more decision power, a feature also recognized by Rees et al. ( 17 ) during interviews with U.K. farmers regarding general on-farm antimicrobial use. This decision hierarchy can lead to tensions, and can be a source of stress, an important aspect to recognize and mitigate when proposing the adoption of novel CM treatment protocols ( 17 ). The role of the veterinarian in on-farm decision making is well-established and documented ( 45 ). More specifically, dynamics between veterinarians and dairy farmers have been described extensively (e.g., 56 , 57 ). However, the dynamics between the actors in these decision-making teams on dairy farms have not been described, and therefore, cannot be used to contextualize our findings. Studying group dynamics is complex ( 58 ), yet is common practice in healthcare settings ( 59 , 60 ), and studying team dynamics can help identify areas for improved antimicrobial stewardship, [(e.g., 61 )]. Other actors – other farmers and nutritionists previously mentioned by Swinkels et al. ( 45 ) – were not mentioned in our interviews. This could be attributed to their more indirect impact on treatment decisions, primarily influencing protocols rather than specific case decisions. The lack of involvement of the veterinarian in case-by-case decision-making can be considered a consequence of the structure of current dairy practice in the region. As part of the shift toward progressive dairy medicine, emphasis has been placed on training producers and on-farm employees to recognize clinical signs of commonly occurring medical conditions, such as CM, and to follow an established protocol. Additionally, feasibility concerns have been described by producers and shed light on the lack of involvement of the veterinarian at this level ( 62 ). These include: the availability of the veterinarian to visit the farm for each CM case, the additional cost to the producer, and the geographic landscape of the region (i.e., farms are considered relatively far apart). While the expectation that the veterinarian participate in decision-making regarding each CM case may not be considered practical for producers and veterinarians in this context, direct involvement of the veterinarian in protocol development is important and was not thoroughly discussed by participants in the sample. The data collected through the interview process do not allow us to know that the veterinarian was not involved in the protocol development process. However, they do highlight the lack of involvement of the veterinarian in individual cases and demonstrate that the producer does not view the veterinarian as a first line resource for decision-making regarding CM cases. The current legal framework in Canada ( 63 ) states that a prescription is needed to purchase antimicrobials, and antimicrobials are only to be prescribed within a current veterinarian-client-patient relationship ( 64 ). This relationship demands veterinarians having sufficient knowledge on which to base the assessment, diagnosis, and treatment of cases, and clients assuming responsibility to communicate the needs of the animal to the veterinarian. Therefore, based on the current legal framework, the veterinarian should be contacted in cases that do not allow the producer or on-farm employee to easily follow the protocol so that an individual assessment can be made. Based on information gleaned through this study, further assessment of veterinarian-producer relationships is warranted and may allow us to further unpack the lack of involvement of the veterinarian in decision-making surrounding CM. In reflecting on the lead researchers’ perspectives and position, and its potential impact on the presented results, it is important to note that EdJ’s background in clinical mastitis was primarily theoretical, derived from scientific literature, rather than practical experience—as she is not a veterinarian. This lack of direct clinical experience facilitated an open and non-judgmental environment during the interviews, encouraging farmers to share their practices more freely. Regarding the information power of the final sample size, EdJ’s initial unfamiliarity with qualitative research required additional interviews to cover all topics; as the participating farmers were all involved in their CM treatment decisions and farmed on conventional farms, the narrow study aim was more easily addressed. The differences between farms with AMS and conventional milking systems did require additional interviews to sufficiently describe each situation’s intricacies.” The iterative fashion in which the results were generated by EdJ, including discussions with the rest of the research team, allowed for continuous reflection on the achievement of sufficient information power to answer the research question. In reflecting on the interview method used, the data obtained from Zoom interviews matched the quality and richness of in-person interviews; similar themes and concepts were brought forward. This similarity is consistent with research comparing the quality of Zoom with in-person interviews ( 65 ). While our study has provided valuable insight into CM decision making, it is important to acknowledge several limitations that might impact the findings. Interviews rely on respondents’ ability to accurately recall details about their decision-making process, which can be challenging, considering most of the CM events discussed occurred in the past – sometimes multiple weeks or months ago. An ethnographic approach, where participant and direct observation are at the core of data collection, can help mitigate this issue and provide deeper insights into social dynamics. However, it is important to note that this method is time-consuming and resource intensive. In contrast to focus groups, interviews allow for more in-depth exploration of individual experiences. Although both interviews and focus groups may be susceptible to socially desirable responses from participants, the interviewer took specific measures to build rapport with farmers and maintain a nonjudgmental and curious stance throughout the interviews. Surveys could be employed in future research as they are a tool to capture quantifiable data and allow for describing trends among farmers with AMS and those milking with parlors. Similarly, surveys would allow for inferences regarding the use frequency of described practices and could quantify the reported treatment considerations among the broader dairy farmer population in Canada. In conclusion, CM treatment decision-making is a multifaceted process, and can be classified into 4 steps: identification and classification, treatment approach, treatment choice, and treatment termination. At each of these steps, farmers considered many different factors leading to CM treatment decisions, including evaluation of milk production and quality data, visual characteristics, systemic signs, additional diagnostics, likelihood of cure, value of the cow, herd goals, urgency of treatment, available drugs, timing of the case, definition of success and progression over time. Three themes shaped these decisions: ‘Personal attributes’, including approach and experiential knowledge; ‘Inter-actor dynamics’, such as shared decision making and dynamics among producers, veterinarians, and milkers; and ‘Moving beyond protocols’, which highlights the dynamic nature of their decision making. While tools and techniques are available to assist farmers in improving udder health and refining antimicrobial choices, understanding the generated themes is key for designing effective interventions for CM that align with the reality of farming operations. Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation. Ethics statementThe studies involving humans were approved by the University of Calgary Conjoint Faculties Research Ethics Board (#REB21-0699). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Author contributionsEdJ: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. IvdV: Data curation, Formal analysis, Methodology, Writing – original draft. A-MS: Conceptualization, Formal analysis, Methodology, Writing – review & editing. JI: Conceptualization, Formal analysis, Methodology, Writing – review & editing. KR: Conceptualization, Formal analysis, Methodology, Writing – review & editing. DK: Formal analysis, Writing – review & editing. HB: Conceptualization, Methodology, Supervision, Writing – review & editing. The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Canada’s Natural Sciences and Engineering Research Council (NSERC) Industrial Research Chair Program granted to HB, with industry contributions from Alberta Milk (Edmonton, AB, Canada), Dairy Farmers of Canada (Ottawa, ON, Canada), Dairy Farmers of Manitoba (Winnipeg, MB, Canada), British Columbia Dairy Association (Burnaby, BC, Canada), WestGen Endowment Fund (Abbotsford, BC, Canada), Lactanet (Guelph, ON, Canada), SaskMilk (Regina, SK, Canada), and MSD Animal Health (Boxmeer, Netherlands). EdJ was supported by an NSERC CREATE in Milk Quality Program Scholarship. AcknowledgmentsWe would like to thank the participating dairy farmers for sharing their knowledge and perspectives. Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. 1. Hamann, J. Diagnosis of mastitis and indicators of milk quality In: H Wageningen, editor. Mastitis in dairy production: Current knowledge and future solutions . 2nd ed. Netherlands: Wageningen Academic Publishers (2007). 83–90. Google Scholar 2. Sears, PM, and McCarthy, KK. Diagnosis of mastitis for therapy decisions. Vet Clin North Am Food Anim Pract . (2003) 19:93–108. doi: 10.1016/S0749-0720(02)00074-9 Crossref Full Text | Google Scholar 3. Ruegg, PL. Making antibiotic treatment decisions for clinical mastitis. Vet Clin North Am Food Anim Pract . (2018) 34:413–25. doi: 10.1016/j.cvfa.2018.06.002 PubMed Abstract | Crossref Full Text | Google Scholar 4. Krishnamoorthy, P, Suresh, KP, Jayamma, KS, Shome, BR, Patil, SS, and Amachawadi, RG. An understanding of the global status of major bacterial pathogens of milk concerning bovine mastitis: a systematic review and meta-analysis (Scientometrics). Pathogens . (2021) 10:545. doi: 10.3390/pathogens10050545 5. Aghamohammadi, M, Haine, D, Kelton, DF, Barkema, HW, Hogeveen, H, Keefe, GP, et al. Herd-level mastitis-associated costs on Canadian dairy farms. Front Vet Sci . (2018) 5:100. doi: 10.3389/fvets.2018.00100 6. Pereyra, VG, Pol, M, Pastorino, F, and Herrero, A. Quantification of antimicrobial usage in dairy cows and preweaned calves in Argentina. Prev Vet Med . (2015) 122:273–9. doi: 10.1016/j.prevetmed.2015.10.019 7. USDA. Dairy 2014, milk quality, milking procedures, and mastitis on U.S. dairies, 2014. (2016). Available at: https://www.aphis.usda.gov/animal_health/nahms/dairy/downloads/dairy14/Dairy14_dr_Mastitis.pdf (Accessed November 9, 2023). 8. De Jong, E, McCubbin, KD, Uyama, T, Brummelhuis, C, Bodaneze, J, Kelton, DF, et al. Adoption and decision factors regarding selective treatment of clinical mastitis on Canadian dairy farms. J Dairy Sci . (2023) 107:476–88. doi: 10.3168/jds.2023-23608 9. Warder, LM, Heider, LC, Léger, DF, Rizzo, D, McClure, JT, de Jong, E, et al. Quantifying antimicrobial use on Canadian dairy farms using garbage can audits. Front Vet Sci . (2023) 10:1185628. doi: 10.3389/fvets.2023.1185628 10. McCubbin, KD, Anholt, RM, de Jong, E, Ida, JA, Nóbrega, DB, Kastelic, JP, et al. Knowledge gaps in the understanding of antimicrobial resistance in Canada. Front Public Health . (2021) 9:726484. doi: 10.3389/fpubh.2021.726484 11. Belage, E, Dufour, S, Bauman, C, Jones-Bitton, A, and Kelton, DF. The Canadian National Dairy Study 2015 - adoption of milking practices in Canadian dairy herds. J Dairy Sci . (2017) 100:3839–49. doi: 10.3168/jds.2016-12187 12. De Jong, E, McCubbin, KD, Speksnijder, D, Dufour, S, Middleton, JR, Ruegg, PL, et al. Invited review: selective treatment of clinical mastitis in dairy cattle. J Dairy Sci . (2023) 106:3761–78. doi: 10.3168/jds.2022-22826 13. Garforth, C. Livestock keepers' reasons for doing and not doing things which governments, vets and scientists would like them to do. Zoonoses Public Health . (2015) 62:29–38. doi: 10.1111/zph.12189 14. Lhermie, G, Gröhn, YT, and Raboisson, D. Addressing antimicrobial resistance: an overview of priority actions to prevent suboptimal antimicrobial use in food-animal production. Front Microbiol . (2017) 7:2114. doi: 10.3389/fmicb.2016.02114 15. Vaarst, M, Paarup-Laursen, B, Houe, H, Fossing, C, and Andersen, HJ. Farmers’ choice of medical treatment of mastitis in Danish dairy herds based on qualitative research interviews. J Dairy Sci . (2002) 85:992–1001. doi: 10.3168/jds.S0022-0302(02)74159-3 16. Cobo-Angel, C, LeBlanc, SJ, Roche, SM, and Ritter, C. A focus group study of Canadian dairy farmers’ attitudes and social referents on antimicrobial use and antimicrobial resistance. Front Vet Sci . (2021) 8:1–13. doi: 10.3389/fvets.2021.645221 17. Rees, GM, Reyher, KK, Barrett, DC, and Buller, H. ‘It's cheaper than a dead cow’: understanding veterinary medicine use on dairy farms. J Rural Stud . (2021) 86:587–98. doi: 10.1016/j.jrurstud.2021.07.020 18. Casseri, E, Bulut, E, Soto, SL, Wemette, M, Stout, A, Safi, AG, et al. Understanding antibiotic resistance as a perceived threat towards dairy cattle through beliefs and practices: a survey-based study of dairy farmers. Antibiotics . (2022) 11:997. doi: 10.3390/antibiotics11080997 19. Tong, A, Sainsbury, P, and Craig, J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care . (2007) 19:349–57. doi: 10.1093/intqhc/mzm042 20. Heis, JP. A Hausa man makes a decision: a contribution to the anthropological perspective on decision-making. Anthropol Forum . (2018) 28:236–54. doi: 10.1080/00664677.2018.1482737 21. Kim, JS, and Cameron, D. Typology of farm management decision-making research. Int J Agric Manag . (2013) 2:81–90. doi: 10.5836/ijam/2013-02-03 22. Lozier, J, Rayburn, E, and Shaw, J. The decision to finish cattle on pasture: an ethnographic approach. J Sustain Agric . (2006) 28:5–23. doi: 10.1300/J064v28n03_03 23. Garro, LC. On the rationality of decision-making studies: part 1: decision models of treatment choice. Med Anthropol Q . (1998) 12:319–40. doi: 10.1525/maq.1998.12.3.319 24. Braun, V, and Clarke, V. Using thematic analysis in psychology. Qual Res Psychol . (2006) 3:77–101. doi: 10.1191/1478088706qp063oa 25. Braun, V, and Clarke, V. Thematic analysis: A practical guide . London, UK: SAGE Publications Ltd. (2022). 26. Ryan, GW, and Bernard, HR. Techniques to identify themes. Field Methods . (2003) 15:85–109. doi: 10.1177/1525822X02239569 27. Braun, V, and Clarke, V. To saturate or not to saturate? Questioning data saturation as auseful concept for thematic analysis and sample-size rationales. Qual Res Sport Exerc Health . (2019) 13:201–16. doi: 10.1080/2159676X.2019.1704846 28. Malterud, K, Siersma, VD, and Guassora, AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res . (2015) 26:1753–60. doi: 10.1177/1049732315617444 29. Government of Canada. CAN/CGSB-32.310–2020. Organic production systems. General principles and management standards. (2021). Available at: https://publications.gc.ca/collections/collection_2020/ongc-cgsb/P29-32-310-2020-eng.pdf (Accessed July 28, 2024) 30. Evans, SM. Hutterite agriculture in Alberta: the contribution of an ethnic isolate. Agric Hist . (2019) 93:656–81. doi: 10.3098/ah.2019.093.4.656 31. Kayitsinga, J, Schewe, RL, Contreras, GA, and Erskine, RJ. Antimicrobial treatment of clinical mastitis in the eastern United States: the influence of dairy farmers’ mastitis management and treatment behavior and attitudes. J Dairy Sci . (2017) 100:1388–407. doi: 10.3168/jds.2016-11708 32. Wilm, J, Svennesen, L, Østergaard Eriksen, E, Halasa, T, and Krömker, V. Veterinary treatment approach and antibiotic usage for clinical mastitis in Danish dairy herds. Antibiotics . (2021) 10:189. doi: 10.3390/antibiotics10020189 33. Fischer, K, Sjöström, K, Strienström, A, and Emanuelson, U. Dairy farmers’ perspectives on antibiotic use: a qualitative study. J Dairy Sci . (2019) 102:2724–37. doi: 10.3168/jds.2018-15015 34. Bausewein, M, Mansfeld, R, Doherr, MG, Harms, J, and Sorge, US. Survey on dairy farmers management practices for and satisfaction with the detection of clinical mastitis by automatic milking systems in Bavaria, Germany. Milk Sci Int . (2023) 76:28–34. doi: 10.48435/MSI.2023.5 35. Mollenhorst, H, Rijkaart, LJ, and Hogeveen, H. Mastitis alert preferences of farmers milking with automatic milking systems. J Dairy Sci . (2012) 95:2523–30. doi: 10.3168/jds.2011-4993 36. Bausewein, M, Mansfeld, R, Doherr, MG, Harms, J, and Sorge, US. Sensitivity and specificity for the detection of clinical mastitis by automatic milking systems in Bavarian dairy herds. Animals . (2022) 12:2131. doi: 10.3390/ani12162131 37. Deng, Z, Lam, TJGM, Hogeveen, H, Spaninks, M, Heij, N, Postema, M, et al. Antimicrobial use and farmers’ attitude toward mastitis treatment on dairy farms with automatic or conventional milking systems. J Dairy Sci . (2020) 103:7302–14. doi: 10.3168/jds.2019-17960 38. Sepúlveda-Varas, P, Proudfoot, KL, Weary, DM, and von Keyserlingk, MA. Changes in behaviour of dairy cows with clinical mastitis. Appl Anim Behav Sci . (2016) 175:8–13. doi: 10.1016/j.applanim.2014.09.022 39. Siivonen, J, Taponen, S, Hovinen, M, Pastell, M, Lensink, BJ, Pyörälä, S, et al. Impact of acute clinical mastitis on cow behaviour. Appl Anim Behav Sci . (2011) 132:101–6. doi: 10.1016/j.applanim.2011.04.005 40. Medrano-Galarza, C, Gibbons, J, Wagner, S, De Passillé, AM, and Rushen, J. Behavioral changes in dairy cows with mastitis. J Dairy Sci . (2012) 95:6994–7002. doi: 10.3168/jds.2011-5247 41. Oliveira, L, and Ruegg, PL. Treatments of clinical mastitis occurring in cows on 51 large dairy herds in Wisconsin. J Dairy Sci . (2014) 97:5426–36. doi: 10.3168/jds.2013-7756 42. McDougall, S, Abbeloos, E, Piepers, S, Rao, A, Astiz, S, Werven, TV, et al. Addition of Metacam® (meloxicam) to the treatment of clinical mastitis improves subsequent reproductive performance. 61–63. 2015 British Mastitis Conference. (2015) The Dairy Group, Worcester, UK 43. Krömker, V, Schmenger, A, Klocke, D, Mansion-de Vries, EM, Wente, N, Zhang, Y, et al. Non-inferiority trial investigating the efficacy of non-steroidal anti-inflammatory drugs and antimicrobial treatment of mild to moderate clinical mastitis in dairy cows with long-lasting udder diseases. Front Vet Sci . (2021) 8:417. doi: 10.3389/fvets.2021.660804 44. Tenhagen, BA, Köster, G, Wallmann, J, and Heuwieser, W. Prevalence of mastitis pathogens and their resistance against antimicrobial agents in dairy cows in Brandenburg, Germany. J Dairy Sci . (2006) 89:2542–51. doi: 10.3168/jds.s0022-0302(06)72330-x 45. Swinkels, JM, Hilkens, A, Zoche-Golob, V, Krömker, V, Buddiger, M, Jansen, J, et al. Social influences on the duration of antibiotic treatment of clinical mastitis in dairy cows. J Dairy Sci . (2015) 98:2369–80. doi: 10.3168/jds.2014-8488 46. Schukken, YH, Bennett, GJ, Zurakowski, MJ, Sharkey, HL, Rauch, BJ, Thomas, MJ, et al. Randomized clinical trial to evaluate the efficacy of a 5-day ceftiofur hydrochloride intramammary treatment on nonsevere gram-negative clinical mastitis. J Dairy Sci . (2011) 94:6203–15. doi: 10.3168/jds.2011-4290 47. Ruegg, PL. What is success? A narrative review of research evaluating outcomes of antibiotics used for treatment of clinical mastitis. Front Vet Sci . (2021) 8:38. doi: 10.3389/fvets.2021.639641 48. Taylor, DD, Martin, JN, Morley, PS, Belk, KE, White, AE, and Walter, EJ. Survey of production animal veterinarians’ prescription practices, factors influencing antimicrobial drug use, and perceptions of and attitudes toward antimicrobial resistance. J Am Vet Med Assoc . (2020) 257:87–96. doi: 10.2460/javma.257.1.87 49. Friedman, DB, Kanwat, CP, Headrick, ML, Patterson, NJ, Neely, JC, and Smith, LU. Importance of prudent antibiotic use on dairy farms in South Carolina: a pilot project on farmers’ knowledge, attitudes and practices. Zoonoses Public Health . (2007) 54:366–75. doi: 10.1111/j.1863-2378.2007.01077.x 50. McDougall, S, Niethammer, J, and Graham, EM. Antimicrobial usage and risk of retreatment for mild to moderate clinical mastitis cases on dairy farms following on-farm bacterial culture and selective therapy. N Z Vet J . (2018) 66:98–107. doi: 10.1080/00480169.2017.1416692 51. Kahneman, D, and Frederick, S. Representativeness revisited: attribute substitution in intuitive judgment In: Heuristics and biases: The psychology of intuitive judgment . New York: Cambridge University Press (2002). 49–81. 52. Evans, JS. Dual-processing accounts of reasoning, judgment, and social cognition. Ann Rev Psychol . (2008) 59:255–78. doi: 10.1146/annurev.psych.59.103006.093629 53. Phillips, WJ, Fletcher, JM, Marks, AD, and Hine, DW. Thinking styles and decision making: a meta-analysis. Psychol Bull . (2016) 142:260–90. doi: 10.1037/bul0000027 54. Thaler, RH, and Sunstein, SR. Nudge: Improving decisions about health, wealth, and happiness . New Haven: Yale University Press (2008). 55. Schulz-Hardt, S, and Mojzisch, A. How to achieve synergy in group decision making: lessons to be learned from the hidden profile paradigm. Eur Rev Soc Psychol . (2012) 23:305–43. doi: 10.1080/10463283.2012.744440 56. Ritter, C, Adams, CL, Kelton, DF, and Barkema, HW. Factors associated with dairy farmers' satisfaction and preparedness to adopt recommendations after veterinary herd health visits. J Dairy Sci . (2019) 102:4280–93. doi: 10.3168/jds.2018-15825 57. Gröndal, H, Blanco-Penedo, I, Fall, N, and Sternberg-Lewerin, S. Trust, agreements, and occasional breakdowns: Veterinarians' perspectives on farmer-veterinarian relationships and use of antimicrobials for Swedish dairy cattle. J Dairy Sci . (2023) 106:534–46. doi: 10.3168/jds.2022-21834 58. Mesmer-Magnus, JR, and DeChurch, LA. Information sharing and team performance: a meta-analysis. J Appl Psychol . (2009) 94:535–46. doi: 10.1037/a0013773 59. Rowland, P, Lising, D, Sinclair, L, and Baker, GR. Team dynamics within quality improvement teams: a scoping review. Int J Qual Health Care . (2018) 30:416–22. doi: 10.1093/intqhc/mzy045 60. Kolbe, M, and Boos, M. Laborious but elaborate: the benefits of really studying team dynamics. Front Psychol . (2019) 10:1–16. doi: 10.3389/fpsyg.2019.01478 61. Charani, E, Ahmad, R, Rawson, TM, Castro-Sanchèz, E, Tarrant, C, and Holmes, AH. The differences in antibiotic decision-making between acute surgical and acute medical teams: an ethnographic study of culture and team dynamics. Clin Infect Dis . (2019) 69:12–20. doi: 10.1093/cid/ciy844 62. Ida, JA, Wilson, WM, Nydam, DV, Gerlach, SC, Kastelic, JP, Russell, ER, et al. Contextualized understandings of dairy farmers’ perspectives on antimicrobial use and regulation in Alberta, Canada. J Dairy Sci . (2023) 106:547–64. doi: 10.3168/jds.2021-21521 63. Government of Canada. Responsible use of Medically Important Antimicrobials in Animals. (2021). Available at: https://www.canada.ca/en/public-health/services/antibiotic-antimicrobial-resistance/animals/actions/responsible-use-antimicrobials.html (Accessed August 2, 2024). 64. National Farm Animal Care Council. Veterinary oversight of antimicrobial use in animals in Canada. (2024) Available at: https://www.nfacc.ca/codes-of-practice/dairy-cattle/code2023#section5 (Accessed August 2, 2024). 65. Deakin, H, and Wakefield, K. Skype interviewing: reflections of two PhD researchers. Qual Res . (2014) 14:603–16. doi: 10.1177/1468794113488126 Keywords: clinical mastitis, decision-making, antimicrobial use, treatment choice, farmer attitudes Citation: de Jong E, van der Velden I, Smid A-MC, Ida JA, Reyher KK, Kelton DF and Barkema HW (2024) Dairy farmers’ considerations for antimicrobial treatment of clinical mastitis in British Columbia and Alberta, Canada. Front. Vet. Sci . 11:1417958. doi: 10.3389/fvets.2024.1417958 Received: 15 April 2024; Accepted: 31 July 2024; Published: 08 August 2024. Reviewed by: Copyright © 2024 de Jong, van der Velden, Smid, Ida, Reyher, Kelton and Barkema. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. *Correspondence: Herman W. Barkema, [email protected] † Deceased Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.  |
|---|
IMAGES
VIDEO
COMMENTS
Clinical Laboratory Science Personal Statement. Decent Essays. 703 Words. 3 Pages. Open Document. After discovering my passion for science and math, I pursue a career in Clinical Laboratory Science with enthusiasm. My desire to study this subject originates from the exciting and rapidly-moving subject area that is highly relevant to major ...
The medical laboratory science personal statement serves as a window into the unique blend of skills, qualities, and aspirations that an individual brings to this critical field. In this essay , we navigate through the intricacies of crafting a compelling personal statement, addressing key questions and shedding light on the importance of ...
Biomedical Science Personal Statement Example 27. The human body is undoubtedly the earth's most impressive creation - six million years of evolution has resulted in this complex system, with all parts working together to maintain life. Throughout my high school years, I have been interested in the intersection of biology and medicine...
Part 1: Introduction to the medical school personal statement. You probably know someone who achieved a solid GPA and MCAT score, conducted research, shadowed physicians, engaged in meaningful volunteer work, and met all the other medical school requirements, yet still got rejected by every school they applied to.. You may have even heard of someone who was rejected by over 30 medical schools ...
To apply for the BSHS in Medical Laboratory Sciences (Hybrid or 100% Online), you'll need: Completed application; ... Personal statement: Applicants must include a 250-500 word essay describing your reasons for undertaking study at GW, your academic objectives, career goals, and related qualifications including collegiate, professional, and ...
Clinical Lab Sciences There are many pieces to the clinical lab scientist training program application, including your GPA, personal statement, list of experiences, letters of recommendation, and biographical information. Use the navigation below to explore each aspect of preparing for a clinical lab scientist training program.
1) Submit a personal statement (include your research experience and career goals). 2) Letter of intent summarizing your background and outlining your short- and long-term training and research goals in this discipline. 3) In the statement of purpose, briefly explain why you want to pursue an advanced degree.
similar problems in adjacent fields. In addition to educational development in the laboratory, I have also chosen to add a clinical aspect. Through the an initiative that pairs basic science PhD students with a clinical mentor to inform translational research, I have been able to add new perspectives to the way I perform research. By
This is roughly 1.5 pages or 500 words. Going under this length is fine, and a tight 400-word personal statement is far preferable to a 500-word statement filled with digressions, wordiness, and redundancy. If you aren't using the AMCAS form, your personal statement should never go over the stated length limit. Attend to grammar and punctuation.
Please check HERE for detailed guidelines on how to write a personal statement (statement of purpose). I am aspiring to study a BSc (Hons) Biomedical Science Programme at the University of Bedfordshire It will provide knowledge as well as graduate-level analytical and transferable skills to prepare for a wide range of careers or further study.
1) Please type in black neatly. Write a personal goal statement explaining why you would like to be accepted by the Medical Laboratory Sciences Program and what you would like to do with this career. Include any of the following, if applicable to you: a. ability to balance multiple responsibilities such as athletics, employment and voluntary ...
This personal statement is unrated. Life, the universe and everything - areas of eternal human endeavour. My penchant is for the life aspect; specifically medical science and its fundamental role in 21st century life, something I've first-hand experience of, seeing two highly intelligent systems in science and human anatomy come together as one.
Personal Statement Example 6. This Personal Statement comes from a student who got into Graduate Entry Medicine at King's - and also had interviews for Undergraduate Medicine at King's, QMUL and Exeter. Get some inspiration for your Medicine Personal Statement with these successful examples from current Medical School students.
Medical Laboratory Sciences Competency Exploration Core Competencies Community Service Student Organizations Personal Statement Writing ... An applicant's personal statement is one of the most important pieces of your application materials. It is the school and admission's committee first opportunity to hear from you about why you are ...
A quick note about saying you want to go to med school/grad school. That is fine for me as long as it is a field that uses CLS knowledge. If you are going to med school maybe say you want to go be a lab director or something. Basic grammar and communication skills. Please proofread your statement. Grammar and spelling issues are becoming ...
I read an article from Clinical Advances in Haematology and Oncology about immunology and breast cancer. I discovered that many clinical trials of anticancer vaccines and immune checkpoint inhibitors are being conducted. ... From shadowing laboratory technicians in conducting research and studies, I learnt the importance of ancillary staff ...
Your personal statement is an important part of your application to Oxford. It allows you to tell us about your interests, achievements and ambitions in your own words. Although we do not formally score your statement we read it carefully and use the information it contains as part of our short-listing exercise.
Satisfactory Essays. 217 Words. 1 Page. Open Document. I intend to study Medical Laboratory Science at South Dakota State University. My goal is to acquire my bachelor's degree by completing four years in that program to earn a degree that would allow me to find a high paying career. An additional perk to my career path would be the fact that ...
Biomedical Laboratory Sciences (BLS) is a challenging and rewarding health care profession that has great impact on patient care. Working in a variety of settings, laboratory scientists are essential members of the health care team who provide vital information about the status and function of the body and its systems.
"Applying to the Clinical Laboratory Science major was the best decision I have ever made." - Courtney Santos The CLS program will prepare students for entry-level laboratory positions and a future in a constantly growing area of health care. Now is a great time to start a career in the clinical laboratory profession, because there … Read more
This personal statement is unrated. The University of Oxford defines biomedical science as the "focus on how cells, organs and systems function in the human body" but to me, this is a very basic definition of something that means a lot to me. It is the chance to learn more about the subject that I am passionate about, the chance to be able ...
Preparing an Effective Personal Statement. W hen applying to graduate schools, you will be required to submit a personal statement as part of your application packet. Writing a personal statement takes time because it requires taking a deep look at the things that make you special--who you are, your background, your experiences, your abilities ...
Conjugative plasmids promote the dissemination and evolution of antimicrobial resistance in bacterial pathogens. However, plasmid acquisition can produce physiological alterations in the bacterial host, leading to potential fitness costs that determine the clinical success of bacteria-plasmid associations. In this study, we used a transcriptomic approach to characterize the interactions ...
Background: Interindividual variability in neurobiological and clinical characteristics in mental illness is often overlooked by classical group mean case control studies. Studies using normative modelling to infer person specific deviations of grey matter volume have indicated that group means are not representative of most individuals. The extent to which this variability is present in white ...
2.1 Positionality statement. The lead author (EdJ) is female, 29 years old, and holds a PhD in Veterinary Medical Science from the University of Calgary. Her PhD research focused on mastitis-related antimicrobial use on dairy farms, a topic on which she and her colleagues have published several manuscripts.