
Presentations made painless
- Get Premium

124 Healthcare Essay Topic Ideas & Examples
Inside This Article
Healthcare is a diverse and complex field that encompasses a wide range of topics, issues, and challenges. Whether you are studying healthcare as a student, working in the healthcare industry, or simply interested in learning more about this important area, there are countless essay topics that you can explore. To help you get started, here are 124 healthcare essay topic ideas and examples that you can use for inspiration:
- The impact of healthcare disparities on patient outcomes
- Strategies for improving access to healthcare in underserved communities
- The role of technology in transforming healthcare delivery
- The ethics of healthcare rationing
- The importance of diversity and inclusion in healthcare organizations
- The rise of telemedicine and its implications for patient care
- The impact of the opioid epidemic on healthcare systems
- The role of nurses in promoting patient safety
- The challenges of providing mental health care in a primary care setting
- The future of healthcare: personalized medicine and precision healthcare
- The role of healthcare providers in addressing social determinants of health
- The impact of climate change on public health
- The role of public health campaigns in promoting healthy behaviors
- The challenges of healthcare delivery in rural areas
- The impact of healthcare reform on the uninsured population
- The role of healthcare informatics in improving patient outcomes
- The importance of cultural competency in healthcare delivery
- The ethical implications of genetic testing and personalized medicine
- The impact of healthcare costs on patient access to care
- The role of healthcare administrators in shaping the future of healthcare delivery
- The challenges of implementing electronic health records in healthcare settings
- The impact of healthcare privatization on patient care
- The role of healthcare providers in promoting patient autonomy
- The challenges of providing end-of-life care in a healthcare setting
- The impact of healthcare disparities on maternal and child health outcomes
- The role of healthcare providers in addressing the opioid crisis
- The challenges of providing healthcare to undocumented immigrants
- The impact of the COVID-19 pandemic on healthcare systems
- The role of healthcare providers in promoting vaccination uptake
- The challenges of healthcare delivery in conflict zones
- The impact of healthcare disparities on LGBTQ+ populations
- The role of healthcare providers in promoting healthy aging
- The challenges of providing healthcare to homeless populations
- The impact of healthcare disparities on rural communities
- The role of healthcare providers in addressing food insecurity
- The challenges of providing healthcare to refugees and asylum seekers
- The impact of healthcare disparities on people with disabilities
- The role of healthcare providers in promoting mental health awareness
- The challenges of providing healthcare to incarcerated populations
- The impact of healthcare disparities on immigrant populations
- The role of healthcare providers in promoting sexual health education
- The challenges of providing healthcare to indigenous populations
- The impact of healthcare disparities on veterans' health outcomes
- The role of healthcare providers in promoting healthy lifestyles
- The challenges of providing healthcare to low-income populations
- The impact of healthcare disparities on minority populations
- The role of healthcare providers in promoting preventive care
- The challenges of providing healthcare to elderly populations
- The impact of healthcare disparities on women's health outcomes
- The role of healthcare providers in promoting maternal health
- The challenges of providing healthcare to children and adolescents
- The impact of healthcare disparities on mental health outcomes
- The role of healthcare providers in promoting substance abuse treatment
- The challenges of providing healthcare to homeless youth
- The impact of healthcare disparities on LGBTQ+ youth
- The role of healthcare providers in promoting healthy relationships
- The challenges of providing healthcare to LGBTQ+ youth
- The impact of healthcare disparities on transgender populations
- The role of healthcare providers in promoting gender-affirming care
- The challenges of providing healthcare to LGBTQ+ elders
- The impact of healthcare disparities on people of color
- The role of healthcare providers in promoting racial equity
- The challenges of providing healthcare to immigrant populations
- The impact of healthcare disparities on refugee populations
- The role of healthcare providers in promoting cultural competency
- The challenges of providing healthcare to non-English speaking populations
- The role of healthcare providers in promoting disability rights
- The challenges of providing healthcare to people with mental illnesses
- The impact of healthcare disparities on people experiencing homelessness
- The role of healthcare providers in promoting housing stability
- The challenges of providing healthcare to people living in poverty
- The impact of healthcare disparities on incarcerated populations
- The role of healthcare providers in promoting criminal justice reform
- The challenges of providing healthcare to veterans
- The impact of healthcare
Want to research companies faster?
Instantly access industry insights
Let PitchGrade do this for me
Leverage powerful AI research capabilities
We will create your text and designs for you. Sit back and relax while we do the work.
Explore More Content
- Privacy Policy
- Terms of Service
© 2024 Pitchgrade
100+ Health Essay Topics
Table of Contents
A Guide to Health Essay Topics
Essays have always been a cornerstone of the academic world, allowing individuals to delve deep into topics and convey their understanding. In the realm of health, essays play a pivotal role, given the depth and breadth of topics available. But first, what exactly is a health essay?
What is a Health Essay?
A health essay is a piece of written work that explores a particular topic within the health sector. This could range from specific medical conditions, healthcare policies, trends in medicine, or broader societal issues like mental health. The aim is often to shed light on an issue, provide insights, or promote understanding. As with any essay, a health essay requires research, structure, and a keen understanding of the topic at hand.
Choosing a Health Essay Topic: A Brief Guide
When selecting a topic for your health essay, begin by considering your personal interests or concerns in the health field. Combine this with the current relevance or emerging trends to ensure your topic is both interesting and timely. Research is paramount; always ensure there is enough credible data available. Lastly, ensure your topic is neither too broad that it becomes unmanageable nor too narrow that it lacks depth.
Health Essay Topics:
Mental health:.
- The Stigma Around Mental Health and its Societal Impact
- Effects of Social Media on Teenage Mental Health
- Treatment Options for PTSD in War Veterans
- Childhood Trauma and its Long-term Effects on Mental Health
Nutrition and Diet:
- The Ketogenic Diet: Benefits and Risks
- Impact of Veganism on Overall Health
- Childhood Obesity: Causes and Solutions
- The Role of Gut Microbiota in Human Health
Healthcare Policies:
- Universal Healthcare: Pros and Cons
- The Impact of Healthcare Costs on the Middle Class
- The Role of Insurance in Modern Healthcare
- Healthcare Accessibility in Rural Areas
Diseases and Treatments:
- The Rise of Antibiotic Resistance and its Implications
- Modern Treatment Options for Alzheimer’s Disease
- The Global Impact of HIV/AIDS
- Managing Diabetes: Modern Methods and Challenges
Fitness and Exercise:
- Benefits of Yoga on Mental and Physical Health
- High-Intensity Interval Training (HIIT): Pros and Cons
- The Role of Physical Activity in Reducing Heart Disease
- Childhood Sports and Long-term Physical Wellbeing
Alternative Medicine:
- Acupuncture: Science or Placebo?
- The Efficacy of Herbal Supplements
- Mindfulness and Meditation in Modern Medicine
- The Role of Chiropractic Care in Overall Health
Global Health Issues:
- The Impact of Clean Water on Global Health
- Addressing the Spread of Malaria in Sub-Saharan Africa
- The Health Implications of Air Pollution in Urban Areas
- Child Mortality Rates: Causes and Solutions
Public Health:
- The Relationship Between Socioeconomic Status and Health Outcomes
- Public Health Responses to Pandemics
- The Impact of Urbanization on Health
- Role of Vaccination in Community Health
- Tackling the Global Tobacco Epidemic
Sexual Health:
- The Importance of Sex Education in Schools
- Understanding LGBTQ+ Health Needs
- The Evolution of HIV Treatments
- Contraception and Women’s Health
- The Psychological Impacts of Infertility
Technological Advances in Health:
- Telemedicine: Future of Healthcare?
- The Role of AI in Diagnostic Medicine
- Wearable Health Technology and Patient Monitoring
- Genetic Engineering and Personalized Medicine
- The Impact of 3D Printing on Prosthetics
Environmental Health:
- Climate Change and its Effect on Public Health
- Health Implications of Pesticides in Agriculture
- Air Quality and Respiratory Diseases
- The Health Impacts of Deforestation
- Hazardous Waste Management and Community Health
Aging and Geriatric Health:
- Challenges in Elderly Care
- The Rise of Neurodegenerative Diseases
- Mental Health Issues Among the Elderly
- Physiotherapy and Mobility in Aging Populations
- Nutrition Needs in Older Adults
Pediatric Health:
- Vaccination and Child Health Controversies
- Developmental Disorders: Early Detection and Interventions
- Nutrition and Cognitive Development in Children
- Children’s Mental Health and the School System
- Pediatric Care: Modern Challenges and Solutions
Women’s Health:
- Breast Cancer: Prevention and Treatment
- Mental Health During and After Pregnancy
- Endometriosis and Women’s Quality of Life
- Impact of Hormonal Changes on Mental Wellbeing
- The Importance of Regular Health Screenings for Women
Men’s Health:
- Prostate Health and Early Detection
- Mental Health Stigmas in Men
- Testosterone and Aging: Myths and Realities
- The Importance of Cardiovascular Health in Men
- Male Pattern Baldness: Causes and Treatments
Health Systems and Policy:
- The Ethics of Organ Transplantation and Donation
- The Future of Universal Health Coverage
- Comparative Analysis of Health Systems Globally
- The Role of Private Sector in Public Health
- Healthcare Workers’ Rights and Patient Safety
Substance Abuse and Rehabilitation:
- The Opioid Crisis: Origins and Solutions
- Alcoholism: Societal Impacts and Treatments
- Rehabilitation Programs: Efficacy and Approaches
- The Growing Concern of Vaping Among Teens
- Substance Abuse and Mental Health Comorbidity
Neurological Health:
- The Increasing Prevalence of Parkinson’s Disease
- Understanding Migraine: Causes and Treatments
- Epilepsy: Myths, Realities, and Modern Care
- Brain-Computer Interfaces and Rehabilitation
- The Impact of Sleep on Cognitive Function
Cardiovascular Health:
- Hypertension: Prevention and Management
- Cholesterol: The Good, the Bad, and the Misunderstood
- Cardiac Rehabilitation and its Benefits
- Sedentary Lifestyles and Heart Disease
- Innovations in Cardiovascular Surgery
Digital Health and Wellbeing:
- Cyberchondria: Anxiety from Online Health Searches
- Digital Detox: The Need for Disconnection
- Mobile Apps and Mental Health Support
- Online Consultations: Pros, Cons, and the Future
- The Role of Virtual Reality in Pain Management
Holistic and Integrative Health:
- The Benefits and Challenges of Ayurveda
- Integrative Health Approaches for Chronic Pain
- Mind-Body Practices in Modern Healthcare
- Homeopathy: Science or Pseudoscience?
- The Role of Nutrition in Holistic Health
Order Health Essay:
Feeling overwhelmed with your health essay topic? Let our experts at WriteOnDeadline help! Our team of professionals offers top-notch essay-writing services tailored to your needs. Contact us today, and let us guide you to academic success!
Useful References:
- World Health Organization (WHO) Publications
- Harvard T.H. Chan School of Public Health
- Centers for Disease Control and Prevention (CDC) Articles
- National Institutes of Health (NIH) Research

Health Care Comes Home: The Human Factors (2011)
Chapter: 7 conclusions and recommendations.
7 Conclusions and Recommendations
Health care is moving into the home increasingly often and involving a mixture of people, a variety of tasks, and a broad diversity of devices and technologies; it is also occurring in a range of residential environments. The factors driving this migration include the rising costs of providing health care; the growing numbers of older adults; the increasing prevalence of chronic disease; improved survival rates of various diseases, injuries, and other conditions (including those of fragile newborns); large numbers of veterans returning from war with serious injuries; and a wide range of technological innovations. The health care that results varies considerably in its safety, effectiveness, and efficiency, as well as its quality and cost.
The committee was charged with examining this major trend in health care delivery and resulting challenges from only one of many perspectives: the study of human factors. From the outset it was clear that the dramatic and evolving change in health care practice and policies presents a broad array of opportunities and problems. Consequently the committee endeavored to maintain focus specifically on how using the human factors approach can provide solutions that support maximizing the safety and quality of health care delivered in the home while empowering both care recipients and caregivers in the effort.
The conclusions and recommendations presented below reflect the most critical steps that the committee thinks should be taken to improve the state of health care in the home, based on the literature reviewed in this report examined through a human factors lens. They are organized into four areas: (1) health care technologies, including medical devices and health information technologies involved in health care in the home; (2)
caregivers and care recipients; (3) residential environments for health care; and (4) knowledge gaps that require additional research and development. Although many issues related to home health care could not be addressed, applications of human factors principles, knowledge, and research methods in these areas could make home health care safer and more effective and also contribute to reducing costs. The committee chose not to prioritize the recommendations, as they focus on various aspects of health care in the home and are of comparable importance to the different constituencies affected.
HEALTH CARE TECHNOLOGIES
Health care technologies include medical devices that are used in the home as well as information technologies related to home-based health care. The four recommendations in this area concern (1) regulating technologies for health care consumers, (2) developing guidance on the structure and usability of health information technologies, (3) developing guidance and standards for medical device labeling, and (4) improving adverse event reporting systems for medical devices. The adoption of these recommendations would improve the usability and effectiveness of technology systems and devices, support users in understanding and learning to use them, and improve feedback to government and industry that could be used to further improve technology for home care.
Ensuring the safety of emerging technologies is a challenge, in part because it is not always clear which federal agency has regulatory authority and what regulations must be met. Currently, the U.S. Food and Drug Administration (FDA) has responsibility for devices, and the Office of the National Coordinator for Health Information Technology (ONC) has similar authority with respect to health information technology. However, the dividing line between medical devices and health information technology is blurring, and many new systems and applications are being developed that are a combination of the two, although regulatory oversight has remained divided. Because regulatory responsibility for them is unclear, these products may fall into the gap.
The committee did not find a preponderance of evidence that knowledge is lacking for the design of safe and effective devices and technologies for use in the home. Rather than discovering an inadequate evidence base, we were troubled by the insufficient attention directed at the development of devices that account, necessarily and properly, for users who are inadequately trained or not trained at all. Yet these new users often must
rely on equipment without ready knowledge about limitations, maintenance requirements, and problems with adaptation to their particular home settings.
The increased prominence of the use of technology in the health care arena poses predictable challenges for many lay users, especially people with low health literacy, cognitive impairment, or limited technology experience. For example, remote health care management may be more effective when it is supported by technology, and various electronic health care (“e-health”) applications have been developed for this purpose. With the spectrum of caregivers ranging from individuals caring for themselves or other family members to highly experienced professional caregivers, computer-based care management systems could offer varying levels of guidance, reminding, and alerting, depending on the sophistication of the operator and the criticality of the message. However, if these technologies or applications are difficult to understand or use, they may be ignored or misused, with potentially deleterious effects on care recipient health and safety. Applying existing accessibility and usability guidelines and employing user-centered design and validation methods in the development of health technology products designed for use in the home would help ensure that they are safe and effective for their targeted user populations. In this effort, it is important to recognize how the line between medical devices and health information technologies has become blurred while regulatory oversight has remained distinct, and it is not always clear into which domain a product falls.
Recommendation 1. The U.S. Food and Drug Administration and the Office of the National Coordinator for Health Information Technology should collaborate to regulate, certify, and monitor health care applications and systems that integrate medical devices and health information technologies. As part of the certification process, the agencies should require evidence that manufacturers have followed existing accessibility and usability guidelines and have applied user-centered design and validation methods during development of the product.
Guidance and Standards
Developers of information technologies related to home-based health care, as yet, have inadequate or incomplete guidance regarding product content, structure, accessibility, and usability to inform innovation or evolution of personal health records or of care recipient access to information in electronic health records.
The ONC, in the initial announcement of its health information technology certification program, stated that requirements would be forthcom-
ing with respect both to personal health records and to care recipient access to information in electronic health records (e.g., patient portals). Despite the importance of these requirements, there is still no guidance on the content of information that should be provided to patients or minimum standards for accessibility, functionality, and usability of that information in electronic or nonelectronic formats.
Consequently, some portals have been constructed based on the continuity of care record. However, recent research has shown that records and portals based on this model are neither understandable nor interpretable by laypersons, even by those with a college education. The lack of guidance in this area makes it difficult for developers of personal health records and patient portals to design systems that fully address the needs of consumers.
Recommendation 2. The Office of the National Coordinator for Health Information Technology, in collaboration with the National Institute of Standards and Technology and the Agency for Healthcare Research and Quality, should establish design guidelines and standards, based on existing accessibility and usability guidelines, for content, accessibility, functionality, and usability of consumer health information technologies related to home-based health care.
The committee found a serious lack of adequate standards and guidance for the labeling of medical devices. Furthermore, we found that the approval processes of the FDA for changing these materials are burdensome and inflexible.
Just as many medical devices currently in use by laypersons in the home were originally designed and approved for use only by professionals in formal health care facilities, the instructions for use and training materials were not designed for lay users, either. The committee recognizes that lack of instructional materials for lay users adds to the level of risk involved when devices are used by populations for whom they were not intended.
Ironically, the FDA’s current premarket review and approval processes inadvertently discourage manufacturers from selectively revising or developing supplemental instructional and training materials, when they become aware that instructional and training materials need to be developed or revised for lay users of devices already approved and marketed. Changing the instructions for use (which were approved with the device) requires manufacturers to submit the device along with revised instructions to the FDA for another 510(k) premarket notification review. Since manufacturers can find these reviews complicated, time-consuming, and expensive, this requirement serves as a disincentive to appropriate revisions of instructional or training materials.
Furthermore, little guidance is currently available on design of user
training methods and materials for medical devices. Even the recently released human factors standard on medical device design (Association for the Advancement of Medical Instrumentation, 2009), while reasonably comprehensive, does not cover the topic of training or training materials. Both FDA guidance and existing standards that do specifically address the design of labeling and ensuing instructions for use fail to account for up-to-date findings from research on instructional systems design. In addition, despite recognition that requirements for user training, training materials, and instructions for use are different for lay and professional users of medical equipment, these differences are not reflected in current standards.
Recommendation 3. The U.S. Food and Drug Administration (FDA) should promote development (by standards development organizations, such as the International Electrotechnical Commission, the International Organization for Standardization, the American National Standards Institute, and the Association for the Advancement of Medical Instrumentation) of new standards based on the most recent human factors research for the labeling of and ensuing instructional materials for medical devices designed for home use by lay users. The FDA should also tailor and streamline its approval processes to facilitate and encourage regular improvements of these materials by manufacturers.
Adverse Event Reporting Systems
The committee notes that the FDA’s adverse event reporting systems, used to report problems with medical devices, are not user-friendly, especially for lay users, who generally are not aware of the systems, unaware that they can use them to report problems, and uneducated about how to do so. In order to promote safe use of medical devices in the home and rectify design problems that put care recipients at risk, it is necessary that the FDA conduct more effective postmarket surveillance of medical devices to complement its premarket approval process. The most important elements of their primarily passive surveillance system are the current adverse event reporting mechanisms, including Maude and MedSun. Entry of incident data by health care providers and consumers is not straightforward, and the system does not elicit data that could be useful to designers as they develop updated versions of products or new ones that are similar to existing devices. The reporting systems and their importance need to be widely promoted to a broad range of users, especially lay users.
Recommendation 4. The U.S. Food and Drug Administration should improve its adverse event reporting systems to be easier to use, to collect data that are more useful for identifying the root causes of events
related to interactions with the device operator, and to develop and promote a more convenient way for lay users as well as professionals to report problems with medical devices.
CAREGIVERS IN THE HOME
Health care is provided in the home by formal caregivers (health care professionals), informal caregivers (family and friends), and individuals who self-administer care; each type of caregiver faces unique issues. Properly preparing individuals to provide care at home depends on targeting efforts appropriately to the background, experience, and knowledge of the caregivers. To date, however, home health care services suffer from being organized primarily around regulations and payments designed for inpatient or outpatient acute care settings. Little attention has been given to how different the roles are for formal caregivers when delivering services in the home or to the specific types of training necessary for appropriate, high-quality practice in this environment.
Health care administration in the home commonly involves interaction among formal caregivers and informal caregivers who share daily responsibility for a person receiving care. But few formal caregivers are given adequate training on how to work with informal caregivers and involve them effectively in health decision making, use of medical or adaptive technologies, or best practices to be used for evaluating and supporting the needs of caregivers.
It is also important to recognize that the majority of long-term care provided to older adults and individuals with disabilities relies on family members, friends, or the individual alone. Many informal caregivers take on these responsibilities without necessary education or support. These individuals may be poorly prepared and emotionally overwhelmed and, as a result, experience stress and burden that can lead to their own morbidity. The committee is aware that informational and training materials and tested programs already exist to assist informal caregivers in understanding the many details of providing health care in the home and to ease their burden and enhance the quality of life of both caregiver and care recipient. However, tested materials and education, support, and skill enhancement programs have not been adequately disseminated or integrated into standard care practices.
Recommendation 5. Relevant professional practice and advocacy groups should develop appropriate certification, credentialing, and/or training standards that will prepare formal caregivers to provide care in the home, develop appropriate informational and training materials
for informal caregivers, and provide guidance for all caregivers to work effectively with other people involved.
RESIDENTIAL ENVIRONMENTS FOR HEALTH CARE
Health care is administered in a variety of nonclinical environments, but the most common one, particularly for individuals who need the greatest level and intensity of health care services, is the home. The two recommendations in this area encourage (1) modifications to existing housing and (2) accessible and universal design of new housing. The implementation of these recommendations would be a good start on an effort to improve the safety and ease of practicing health care in the home. It could improve the health and safety of many care recipients and their caregivers and could facilitate adherence to good health maintenance and treatment practices. Ideally, improvements to housing design would take place in the context of communities that provide transportation, social networking and exercise opportunities, and access to health care and other services.
Safety and Modification of Existing Housing
The committee found poor appreciation of the importance of modifying homes to remove health hazards and barriers to self-management and health care practice and, furthermore, that financial support from federal assistance agencies for home modifications is very limited. The general connection between housing characteristics and health is well established. For example, improving housing conditions to enhance basic sanitation has long been part of a public health response to acute illness. But the characteristics of the home can present significant barriers to autonomy or self-care management and present risk factors for poor health, injury, compromised well-being, and greater dependence on others. Conversely, physical characteristics of homes can enhance resident safety and ability to participate in daily self-care and to utilize effectively health care technologies that are designed to enhance health and well-being.
Home modifications based on professional home assessments can increase functioning, contribute to reducing accidents such as falls, assist caregivers, and enable chronically ill persons and people with disabilities to stay in the community. Such changes are also associated with facilitating hospital discharges, decreasing readmissions, reducing hazards in the home, and improving care coordination. Familiar modifications include installation of such items as grab bars, handrails, stair lifts, increased lighting, and health monitoring equipment as well as reduction of such hazards as broken fixtures and others caused by insufficient home maintenance.
Deciding on which home modifications have highest priority in a given
setting depends on an appropriate assessment of circumstances and the environment. A number of home assessment instruments and programs have been validated and proven to be effective to meet this need. But even if needed modifications are properly identified and prioritized, inadequate funding, gaps in services, and lack of coordination between the health and housing service sectors have resulted in a poorly integrated system that is difficult to access. Even when accessed, progress in making home modifications available has been hampered by this lack of coordination and inadequate reimbursement or financial mechanisms, especially for those who cannot afford them.
Recommendation 6. Federal agencies, including the U.S. Department of Health and Human Services and the Centers for Medicare & Medicaid Services, along with the U.S. Department of Housing and Urban Development and the U.S. Department of Energy, should collaborate to facilitate adequate and appropriate access to health- and safety-related home modifications, especially for those who cannot afford them. The goal should be to enable persons whose homes contain obstacles, hazards, or features that pose a home safety concern, limit self-care management, or hinder the delivery of needed services to obtain home assessments, home modifications, and training in their use.
Accessibility and Universal Design of New Housing
Almost all existing housing in the United States presents problems for conducting health-related activities because physical features limit independent functioning, impede caregiving, and contribute to such accidents as falls. In spite of the fact that a large and growing number of persons, including children, adults, veterans, and older adults, have disabilities and chronic conditions, new housing continues to be built that does not account for their needs (current or future). Although existing homes can be modified to some extent to address some of the limitations, a proactive, preventive, and effective approach would be to plan to address potential problems in the design phase of new and renovated housing, before construction.
Some housing is already required to be built with basic accessibility features that facilitate practice of health care in the home as a result of the Fair Housing Act Amendments of 1998. And 17 states and 30 cities have passed what are called “visitability” codes, which currently apply to 30,000 homes. Some localities offer tax credits, such as Pittsburgh through an ordinance, to encourage installing visitability features in new and renovated housing. The policy in Pittsburgh was impetus for the Pennsylvania Residential VisitAbility Design Tax Credit Act signed into law on October 28, 2006, which offers property owners a tax credit for new construction
and rehabilitation. The Act paves the way for municipalities to provide tax credits to citizens by requiring that such governing bodies administer the tax credit (Self-Determination Housing Project of Pennsylvania, Inc., n.d.).
Visitability, rather than full accessibility, is characterized by such limited features as an accessible entry into the home, appropriately wide doorways and one accessible bathroom. Both the International Code Council, which focuses on building codes, and the American National Standards Institute, which establishes technical standards, including ones associated with accessibility, have endorsed voluntary accessibility standards. These standards facilitate more jurisdictions to pass such visitability codes and encourage legislative consistency throughout the country. To date, however, the federal government has not taken leadership to promote compliance with such standards in housing construction, even for housing for which it provides financial support.
Universal design, a broader and more comprehensive approach than visitability, is intended to suit the needs of persons of all ages, sizes, and abilities, including individuals with a wide range of health conditions and activity limitations. Steps toward universal design in renovation could include such features as anti-scald faucet valve devices, nonslip flooring, lever handles on doors, and a bedroom on the main floor. Such features can help persons and their caregivers carry out everyday tasks and reduce the incidence of serious and costly accidents (e.g., falls, burns). In the long run, implementing universal design in more homes will result in housing that suits the long-term needs of more residents, provides more housing choices for persons with chronic conditions and disabilities, and causes less forced relocation of residents to more costly settings, such as nursing homes.
Issues related to housing accessibility have been acknowledged at the federal level. For example, visitability and universal design are in accord with the objectives of the Safety of Seniors Act (Public Law No. 110-202, passed in 2008). In addition, implementation of the Olmstead decision (in which the U.S. Supreme Court ruled that the Americans with Disabilities Act may require states to provide community-based services rather than institutional placements for individuals with disabilities) requires affordable and accessible housing in the community.
Visitability, accessibility, and universal design of housing all are important to support the practice of health care in the home, but they are not broadly implemented and incentives for doing so are few.
Recommendation 7. Federal agencies, such as the U.S. Department of Housing and Urban Development, the U.S. Department of Veterans Affairs, and the Federal Housing Administration, should take a lead role, along with states and local municipalities, to develop strategies that promote and facilitate increased housing visitability, accessibil-
ity, and universal design in all segments of the market. This might include tax and other financial incentives, local zoning ordinances, model building codes, new products and designs, and related policies that are developed as appropriate with standards-setting organizations (e.g., the International Code Council, the International Electrotechnical Commission, the International Organization for Standardization, and the American National Standards Institute).
RESEARCH AND DEVELOPMENT
In our review of the research literature, the committee learned that there is ample foundational knowledge to apply a human factors lens to home health care, particularly as improvements are considered to make health care safe and effective in the home. However, much of what is known is not being translated effectively into practice, neither in design of equipment and information technology or in the effective targeting and provision of services to all those in need. Consequently, the four recommendations that follow support research and development to address knowledge and communication gaps and facilitate provision of high-quality health care in the home. Specifically, the committee recommends (1) research to enhance coordination among all the people who play a role in health care practice in the home, (2) development of a database of medical devices in order to facilitate device prescription, (3) improved surveys of the people involved in health care in the home and their residential environments, and (4) development of tools for assessing the tasks associated with home-based health care.
Health Care Teamwork and Coordination
Frail elders, adults with disabilities, disabled veterans, and children with special health care needs all require coordination of the care services that they receive in the home. Home-based health care often involves a large number of elements, including multiple care providers, support services, agencies, and complex and dynamic benefit regulations, which are rarely coordinated. However, coordinating those elements has a positive effect on care recipient outcomes and costs of care. When successful, care coordination connects caregivers, improves communication among caregivers and care recipients and ensures that receivers of care obtain appropriate services and resources.
To ensure safe, effective, and efficient care, everyone involved must collaborate as a team with shared objectives. Well-trained primary health care teams that execute customized plans of care are a key element of coordinated care; teamwork and communication among all actors are also
essential to successful care coordination and the delivery of high-quality care. Key factors that influence the smooth functioning of a team include a shared understanding of goals, common information (such as a shared medication list), knowledge of available resources, and allocation and coordination of tasks conducted by each team member.
Barriers to coordination include insufficient resources available to (a) help people who need health care at home to identify and establish connections to appropriate sources of care, (b) facilitate communication and coordination among caregivers involved in home-based health care, and (c) facilitate communication among the people receiving and the people providing health care in the home.
The application of systems analysis techniques, such as task analysis, can help identify problems in care coordination systems and identify potential intervention strategies. Human factors research in the areas of communication, cognitive aiding and decision support, high-fidelity simulation training techniques, and the integration of telehealth technologies could also inform improvements in care coordination.
Recommendation 8 . The Agency for Healthcare Research and Quality should support human factors–based research on the identified barriers to coordination of health care services delivered in the home and support user-centered development and evaluation of programs that may overcome these barriers.
Medical Device Database
It is the responsibility of physicians to prescribe medical devices, but in many cases little information is readily available to guide them in determining the best match between the devices available and a particular care recipient. No resource exists for medical devices, in contrast to the analogous situation in the area of assistive and rehabilitation technologies, for which annotated databases (such as AbleData) are available to assist the provider in determining the most appropriate one of several candidate devices for a given care recipient. Although specialists are apt to receive information about devices specific to the area of their practice, this is much less likely in the case of family and general practitioners, who often are responsible for selecting, recommending, or prescribing the most appropriate device for use at home.
Recommendation 9. The U.S. Food and Drug Administration, in collaboration with device manufacturers, should establish a medical device database for physicians and other providers, including pharmacists, to use when selecting appropriate devices to prescribe or recommend
for people receiving or self-administering health care in the home. Using task analysis and other human factors approaches to populate the medical device database will ensure that it contains information on characteristics of the devices and implications for appropriate care recipient and device operator populations.
Characterizing Caregivers, Care Recipients, and Home Environments
As delivery of health care in the home becomes more common, more coherent strategies and effective policies are needed to support the workforce of individuals who provide this care. Developing these will require a comprehensive understanding of the number and attributes of individuals engaged in health care in the home as well as the context in which care is delivered. Data and data analysis are lacking to accomplish this objective.
National data regarding the numbers of individuals engaged in health care delivery in the home—that is, both formal and informal caregivers—are sparse, and the estimates that do exist vary widely. Although the Bureau of Labor Statistics publishes estimates of the number of workers employed in the home setting for some health care classifications, they do not include all relevant health care workers. For example, data on workers employed directly by care recipients and their families are notably absent. Likewise, national estimates of the number of informal caregivers are obtained from surveys that use different methodological approaches and return significantly different results.
Although numerous national surveys have been designed to answer a broad range of questions regarding health care delivery in the home, with rare exceptions such surveys reflect the relatively limited perspective of the sponsoring agency. For example,
- The Medicare Current Beneficiary Survey (administered by the Centers for Medicare & Medicaid Services) and the Health and Retirement Survey (administered by the National Institute on Aging) are primarily geared toward understanding the health, health services use, and/or economic well-being of older adults and provide no information regarding working-age adults or children or information about home or neighborhood environments.
- The Behavioral Risk Factors Surveillance Survey (administered by the Centers for Disease Control and Prevention, CDC), the National Health Interview Survey (administered by the CDC), and the National Children’s Study (administered by the U.S. Department of Health and Human Services and the U.S. Environmental Protection Agency) all collect information on health characteristics, with limited or no information about the housing context.
- The American Housing Survey (administered by the U.S. Department of Housing and Urban Development) collects detailed information regarding housing, but it does not include questions regarding the health status of residents and does not collect adequate information about home modifications and features on an ongoing basis.
Consequently, although multiple federal agencies collect data on the sociodemographic and health characteristics of populations and on the nation’s housing stock, none of these surveys collects data necessary to link the home, its residents, and the presence of any caregivers, thus limiting understanding of health care delivered in the home. Furthermore, information is altogether lacking about health and functioning of populations linked to the physical, social, and cultural environments in which they live. Finally, in regard to individuals providing care, information is lacking regarding their education, training, competencies, and credentialing, as well as appropriate knowledge about their working conditions in the home.
Better coordination across government agencies that sponsor such surveys and more attention to information about health care that occurs in the home could greatly improve the utility of survey findings for understanding the prevalence and nature of health care delivery in the home.
Recommendation 10. Federal health agencies should coordinate data collection efforts to capture comprehensive information on elements relevant to health care in the home, either in a single survey or through effective use of common elements across surveys. The surveys should collect data on the sociodemographic and health characteristics of individuals receiving care in the home, the sociodemographic attributes of formal and informal caregivers and the nature of the caregiving they provide, and the attributes of the residential settings in which the care recipients live.
Tools for Assessing Home Health Care Tasks and Operators
Persons caring for themselves or others at home as well as formal caregivers vary considerably in their skills, abilities, attitudes, experience, and other characteristics, such as age, culture/ethnicity, and health literacy. In turn, designers of health-related devices and technology systems used in the home are often naïve about the diversity of the user population. They need high-quality information and guidance to better understand user capabilities relative to the task demands of the health-related device or technology that they are developing.
In this environment, valid and reliable tools are needed to match users with tasks and technologies. At this time, health care providers lack the
tools needed to assess whether particular individuals would be able to perform specific health care tasks at home, and medical device and system designers lack information on the demands associated with health-related tasks performed at home and the human capabilities needed to perform them successfully.
Whether used to assess the characteristics of formal or informal caregivers or persons engaged in self-care, task analysis can be used to develop point-of-care tools for use by consumers and caregivers alike in locations where such tasks are encouraged or prescribed. The tools could facilitate identification of potential mismatches between the characteristics, abilities, experiences, and attitudes that an individual brings to a task and the demands associated with the task. Used in ambulatory care settings, at hospital discharge or other transitions of care, and in the home by caregivers or individuals and family members themselves, these tools could enable assessment of prospective task performer’s capabilities in relation to the demands of the task. The tools might range in complexity from brief screening checklists for clinicians to comprehensive assessment batteries that permit nuanced study and tracking of home-based health care tasks by administrators and researchers. The results are likely to help identify types of needed interventions and support aids that would enhance the abilities of individuals to perform health care tasks in home settings safely, effectively, and efficiently.
Recommendation 11. The Agency for Healthcare Research and Quality should collaborate, as necessary, with the National Institute for Disability and Rehabilitation Research, the National Institutes of Health, the U.S. Department of Veterans Affairs, the National Science Foundation, the U.S. Department of Defense, and the Centers for Medicare & Medicaid Services to support development of assessment tools customized for home-based health care, designed to analyze the demands of tasks associated with home-based health care, the operator capabilities required to carry them out, and the relevant capabilities of specific individuals.
Association for the Advancement of Medical Instrumentation. (2009). ANSI/AAMI HE75:2009: Human factors engineering: Design of medical devices. Available: http://www.aami.org/publications/standards/HE75_Ch16_Access_Board.pdf [April 2011].
Self-Determination Housing Project of Pennsylvania, Inc. (n.d.) Promoting visitability in Pennsylvania. Available: http://www.sdhp.org/promoting_visitability_in_pennsy.htm [March 30, 2011].
In the United States, health care devices, technologies, and practices are rapidly moving into the home. The factors driving this migration include the costs of health care, the growing numbers of older adults, the increasing prevalence of chronic conditions and diseases and improved survival rates for people with those conditions and diseases, and a wide range of technological innovations. The health care that results varies considerably in its safety, effectiveness, and efficiency, as well as in its quality and cost.
Health Care Comes Home reviews the state of current knowledge and practice about many aspects of health care in residential settings and explores the short- and long-term effects of emerging trends and technologies. By evaluating existing systems, the book identifies design problems and imbalances between technological system demands and the capabilities of users. Health Care Comes Home recommends critical steps to improve health care in the home. The book's recommendations cover the regulation of health care technologies, proper training and preparation for people who provide in-home care, and how existing housing can be modified and new accessible housing can be better designed for residential health care. The book also identifies knowledge gaps in the field and how these can be addressed through research and development initiatives.
Health Care Comes Home lays the foundation for the integration of human health factors with the design and implementation of home health care devices, technologies, and practices. The book describes ways in which the Agency for Healthcare Research and Quality (AHRQ), the U.S. Food and Drug Administration (FDA), and federal housing agencies can collaborate to improve the quality of health care at home. It is also a valuable resource for residential health care providers and caregivers.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
- Skip to primary navigation
- Skip to main content
- Skip to primary sidebar
UPSC Coaching, Study Materials, and Mock Exams
Enroll in ClearIAS UPSC Coaching Join Now Log In
Call us: +91-9605741000
Health Sector in India
Last updated on August 18, 2024 by ClearIAS Team

What is the current Scenario of the Health Care Sector of India? What are the major concerns? How to use India’s huge potential in the health sector to rectify the problems? Read further to learn more about the Health Sector in India.
The Constitution considers the “Right to Life” to be essential, and the government is required to protect everyone’s “ Right to Health .”
The healthcare industry in India includes hospitals, medical tourism, health insurance, medical equipment, telemedicine, outsourcing, clinical trials, and medical gadgets.
The public and private sectors make up the two main components of India’s healthcare delivery system.
Table of Contents
The Scenario of the Health Sector in India
Let us look at an overview of the current healthcare sector in India
Health Infrastructure
The government, or public healthcare system, concentrates on establishing primary healthcare centres (PHCs) in rural areas while maintaining a small number of secondary and tertiary care facilities in major cities. The majority of secondary, tertiary, and quaternary care facilities are run by the private sector.
UPSC CSE 2025: Study Plan ⇓
(1) ⇒ UPSC 2025: Prelims cum Mains
(2) ⇒ UPSC 2025: Prelims Test Series
(3) ⇒ UPSC 2025: CSAT
Note: To know more about ClearIAS Courses (Online/Offline) and the most effective study plan, you can call ClearIAS Mentors at +91-9605741000, +91-9656621000, or +91-9656731000.
India has 1.3 beds per 1,000 people, 0.5 pharmacists per 1,000 people, and 0.8 physicians per 1,000 people, which are all less than half the global average.
Quality of Health Care Services
India is ranked 145 th out of 180 nations in terms of the accessibility and quality of healthcare, according to the Economic Survey (Global Burden of Disease Study 2016)
To achieve an ideal doctor-to-population ratio of 1:1000 by 2030, India will require an additional 2 million doctors.
Disease Burden
Despite having 17% of the world’s population, India bears a disproportionately large portion of the global disease burden (20%).
India’s public healthcare spending was 2.1% of GDP in 2021–2022, up from 1.8% in 2020–2021, according to the Economic Survey of 2022 .
Challenges in Health Sector
Although India’s health sector has made significant progress in terms of health indicators, it still has some serious flaws in service delivery due to inadequate healthcare infrastructure.
Inadequate Accessibility
Insufficient access to basic healthcare services to all, due to a shortage of medical professionals, a lack of quality assurance, and insufficient health spending.
Insufficient Funding
One of the major concerns is the administration’s lack of financial resources and insufficient funding for research and development.
India’s government will only spend 2.1% of its GDP on healthcare in 2021–22, compared to 10% for Japan, Canada, and France.
No focus on Preventive Care
Despite being shown to be quite beneficial in alleviating a variety of difficulties for patients in terms of unhappiness and financial losses, preventive care is undervalued in India.
Shortage of Medical Workforce
Doctors, nurses, and other healthcare professionals are in short supply in India. According to a minister’s study presented in Parliament, India is short 600,000 doctors.
Lack of Infrastructure
Private hospitals are expensive, whereas Government hospitals are either inadequate or lacking in basic facilities for the Indian population.
Optimal Insurance
The concept of health insurance is still unclear in India, and the market is underdeveloped.
Policymaking
Policymaking is undeniably important in providing effective and efficient healthcare services. The problem in India is one of supply rather than demand, and policy can help.
Potential in Health Care Sector in India
Despite the challenges, there were opportunities. The Indian healthcare system has a unique opportunity to advance while taking stock of the past and getting ready for the future while keeping the welfare of its people in mind.
Strong Demand
According to Aspire Circle, the Indian healthcare sector is expected to reach $744 billion by 2030, driven by greater access to insurance, better health awareness, lifestyle diseases, and rising income.
Innovative Technologies
As part of the National Digital Health Mission ( NDHM ), the digital Health ID will be introduced, which will save patient data. It would aid in effective policymaking, and private firms would benefit from a competitive advantage in the market introduction of innovative technology.
With the advent of information technology and big data, it would be simple for private players to spend strategically.
Rising Manpower
The abundance of highly qualified medical personnel in India is a competitive advantage. With 4.7 million workers as of 2021, the Indian healthcare industry is one of the country’s largest employers.
From 0.83 million in 2010 to 1.3 million in November 2021, the number of allopathic doctors with recognised medical qualifications (under the I.M.C Act) registered with state medical councils/national medical council
Cost Competent
India’s costs are competitive with those of its countries in Asia and the West. Surgery in India costs roughly a tenth of what it does in the US or Western Europe.
Attractive Opportunities
Two vaccines Bharat Biotech’s Covaxin and Oxford-Covishield, AstraZeneca’s both made by SII were critical in protecting the Indian population from COVID-19.
India has emerged as a hub for R&D activities for international players due to its relatively low cost of clinical research.
With the help of the government and private stakeholders, a climate conducive to start-ups and entrepreneurship can be created in this field.
Hub of Medical Tourism
India is already one of the world’s most popular medical tourism destinations, and this industry has significant potential in the coming years.
The low cost of medical services has resulted in a rise in the country’s medical tourism, attracting patients from across the world.
India possesses all the necessary factors for this industry to grow rapidly, including a sizable population, a strong pharmaceutical and medical supply chain, more than 750 million smartphone users, the third-largest global start-up pool with simple access to Venture Capital funding, and innovative tech entrepreneurs looking to address global healthcare issues.
Measures Required in the Health Sector
These are the following major measures for improving the health sector in India:
- Strengthening the Infrastructure: Because of India’s large population, there is an urgent need to improve the infrastructure of public hospitals, which are overburdened.
- Encourage Private Hospitals: The government should support private hospitals because they contribute significantly to the Indian Health sector. The challenges are severe and cannot be addressed solely by the government, the private sector must also participate with Government for the public good.
- Increased efficiency: More medical personnel must be hired in order to improve the sector’s capabilities and efficiency.
- Utilization of Technology: Technology must be used to connect the dots in the health system. Medical devices in hospitals and clinics, mobile health apps, wearables, and sensors are just a few examples of technology that should be considered.
- Improving Mental Health Care Services: Increasing financing for mental health services, educating healthcare professionals on how to effectively treat mental health issues, and lowering the stigma attached to mental illness are all part of improving mental health services.
- Addressing the Root Causes of Health Disparities: To address the social determinants of health and reduce overall health inequities, the healthcare system should collaborate with other sectors, such as education, housing, and sanitation.
- Sustainable Health governance: To promote more effective and efficient healthcare services, sustainable health governance may involve implementing better management systems, bolstering healthcare regulatory organisations, and developing independent oversight mechanisms.
- Make Public Awareness: People should be made aware of the value of early detection and prevention. It would also help them save money on out-of-pocket expenses.
- One Health Approach: The need for communal health programmes that address a healthy environment, healthy animals, and healthy people is urgent. This is known as the “one health approach,” and it aims to address these connections between human and animal health.
Also read: Medical Device Sector in India
Major Steps Taken by the Government
Despite the fact that health is a state issue, the Central Government assists state governments in providing health services through a variety of primary, secondary, and tertiary care systems.
In the Union Budget 2023-24:
- Rs. 89,155 crore was allocated to the health sector, an increase of over 13% from the previous budget.
- Allocated Rs. 6835 crore for establishing 22 new All India Institute of Medical Sciences (AIIMS).
- Additionally, the National Health Mission’s budget allocation increased from Rs. 28,974 crore in the preceding years to Rs. 29,085 crore in the current 2023–24 budget.
- Budgetary support for the National Digital Health Mission increased from the previous year’s Rs. 140 crore to the current Rs. 341 crore.
- The funds allotted for autonomous bodies were also scaled up, going from Rs. 10,348 crore in the previous budgeted allocation to Rs. 17,322 crore at the moment.
In order to promote medical tourism in the country, the government of India is extending the e-medical visa facility to the citizens of 156 countries.
Prime Minister Mr. Narendra Modi introduced the Ayushman Bharat Digital Mission in September 2021. The endeavour will link the digital health solutions of hospitals across the country. Every citizen will now have access to a digital health ID, and their medical records will be safeguarded online.
In July 2021, the Ministry of Tourism established the ‘National Medical & Wellness Tourism Board’ to promote medical and wellness tourism in India.
In July 2021, the Union Cabinet approved the continuation of the National Ayush Mission , responsible for the development of traditional medicines in India, as a centrally sponsored scheme until 2026.
In July 2021, the Union Cabinet approved the MoU between India and Denmark on cooperation in health and medicine . The agreement will focus on joint initiatives and technology development in the health sector, with the aim of improving public health status of the population of both countries.
India is a land full of opportunities for Health Care and Services. Along with being one of the top places for high-end diagnostic services, the nation has made significant capital investments in advanced diagnostic facilities to serve a larger proportion of the population.
Future demand for healthcare services is anticipated to increase due to factors such as advancing income levels, an ageing population, rising health awareness, and shifting attitudes toward preventative healthcare.
A comprehensive strategy is required to address issues in India’s healthcare industry. This necessitates active collaboration between all stakeholders, including the public, private, and individual sectors.
In 2023, India’s approach to social determinants of health (SDH) could be consolidated and expanded. As a major economic pillar, India must now maintain its existing interest in strategic health policy.
- Climate Resilient Health Systems
- Violence against healthcare workers (VAHCW) in India
Article written by: Aryadevi E S

Top 10 Best-Selling ClearIAS Courses
Upsc prelims cum mains (pcm) gs course: unbeatable batch 2025 (online), rs.75000 rs.29000, upsc prelims marks booster + 2025 (online), rs.19999 rs.14999, upsc prelims test series (pts) 2025 (online), rs.9999 rs.4999, csat course 2025 (online), current affairs course 2025 (online), ncert foundation course (online), essay writing course for upsc cse (online), ethics course for upsc cse (online), upsc interview marks booster course (online), rs.9999 rs.4999.
About ClearIAS Team
ClearIAS is one of the most trusted learning platforms in India for UPSC preparation. Around 1 million aspirants learn from the ClearIAS every month.
Our courses and training methods are different from traditional coaching. We give special emphasis on smart work and personal mentorship. Many UPSC toppers thank ClearIAS for our role in their success.
Download the ClearIAS mobile apps now to supplement your self-study efforts with ClearIAS smart-study training.
Reader Interactions
Leave a reply cancel reply.
Your email address will not be published. Required fields are marked *

Don’t lose out without playing the right game!
Follow the ClearIAS Prelims cum Mains (PCM) Integrated Approach.
Join ClearIAS PCM Course Now
UPSC Online Preparation
- Union Public Service Commission (UPSC)
- Indian Administrative Service (IAS)
- Indian Police Service (IPS)
- IAS Exam Eligibility
- UPSC Free Study Materials
- UPSC Exam Guidance
- UPSC Prelims Test Series
- UPSC Syllabus
- UPSC Online
- UPSC Prelims
- UPSC Interview
- UPSC Toppers
- UPSC Previous Year Qns
- UPSC Age Calculator
- UPSC Calendar 2024
- About ClearIAS
- ClearIAS Programs
- ClearIAS Fee Structure
- IAS Coaching
- UPSC Coaching
- UPSC Online Coaching
- ClearIAS Blog
- Important Updates
- Announcements
- Book Review
- ClearIAS App
- Work with us
- Advertise with us
- Privacy Policy
- Terms and Conditions
- Talk to Your Mentor
Featured on

and many more...
ClearIAS Programs: Admissions Open
Thank You 🙌
UPSC CSE 2025: Study Plan
Subscribe ClearIAS YouTube Channel

Get free study materials. Don’t miss ClearIAS updates.
Subscribe Now
IAS/IPS/IFS Online Coaching: Target CSE 2025
Cover the entire syllabus of UPSC CSE Prelims and Mains systematically.
Essays in the Economics of Health and Medical Care
More from nber.
In addition to working papers , the NBER disseminates affiliates’ latest findings through a range of free periodicals — the NBER Reporter , the NBER Digest , the Bulletin on Retirement and Disability , the Bulletin on Health , and the Bulletin on Entrepreneurship — as well as online conference reports , video lectures , and interviews .
Health Sector Policy Essays
Operating in structure: health sector policy and governance, popular essay topics.
- American Dream
- Artificial Intelligence
- Black Lives Matter
- Bullying Essay
- Career Goals Essay
- Causes of the Civil War
- Child Abusing
- Civil Rights Movement
- Community Service
- Cultural Identity
- Cyber Bullying
- Death Penalty
- Depression Essay
- Domestic Violence
- Freedom of Speech
- Global Warming
- Gun Control
- Human Trafficking
- I Believe Essay
- Immigration
- Importance of Education
- Israel and Palestine Conflict
- Leadership Essay
- Legalizing Marijuanas
- Mental Health
- National Honor Society
- Police Brutality
- Pollution Essay
- Racism Essay
- Romeo and Juliet
- Same Sex Marriages
- Social Media
- The Great Gatsby
- The Yellow Wallpaper
- Time Management
- To Kill a Mockingbird
- Violent Video Games
- What Makes You Unique
- Why I Want to Be a Nurse
- Send us an e-mail

- Classroom Programme
- Interview Guidance
- Online Programme
- Drishti Store
- My Bookmarks
- My Progress
- Change Password
- From The Editor's Desk
- How To Use The New Website
- Help Centre
Achievers Corner
- Topper's Interview
- About Civil Services
- UPSC Prelims Syllabus
- GS Prelims Strategy
- Prelims Analysis
- GS Paper-I (Year Wise)
- GS Paper-I (Subject Wise)
- CSAT Strategy
- Previous Years Papers
- Practice Quiz
- Weekly Revision MCQs
- 60 Steps To Prelims
- Prelims Refresher Programme 2020
Mains & Interview
- Mains GS Syllabus
- Mains GS Strategy
- Mains Answer Writing Practice
- Essay Strategy
- Fodder For Essay
- Model Essays
- Drishti Essay Competition
- Ethics Strategy
- Ethics Case Studies
- Ethics Discussion
- Ethics Previous Years Q&As
- Papers By Years
- Papers By Subject
- Be MAINS Ready
- Awake Mains Examination 2020
- Interview Strategy
- Interview Guidance Programme
Current Affairs
- Daily News & Editorial
- Daily CA MCQs
- Sansad TV Discussions
- Monthly CA Consolidation
- Monthly Editorial Consolidation
- Monthly MCQ Consolidation
Drishti Specials
- To The Point
- Important Institutions
- Learning Through Maps
- PRS Capsule
- Summary Of Reports
- Gist Of Economic Survey
Study Material
- NCERT Books
- NIOS Study Material
- IGNOU Study Material
- Yojana & Kurukshetra
- Chhatisgarh
- Uttar Pradesh
- Madhya Pradesh
Test Series
- UPSC Prelims Test Series
- UPSC Mains Test Series
- UPPCS Prelims Test Series
- UPPCS Mains Test Series
- BPSC Prelims Test Series
- RAS/RTS Prelims Test Series
- Daily Editorial Analysis
- YouTube PDF Downloads
- Strategy By Toppers
- Ethics - Definition & Concepts
- Mastering Mains Answer Writing
- Places in News
- UPSC Mock Interview
- PCS Mock Interview
- Interview Insights
- Prelims 2019
- Product Promos
- Daily Updates
Indian Economy
Make Your Note
Healthcare Sector in India
- 08 Sep 2022
- GS Paper - 2
- Government Policies & Interventions
- GS Paper - 3
- Government Budgeting
For Prelims: Government Policies & Interventions, Healthcare Sector in India and related Initiatives.
For Mains : Healthcare Sector in India, Challenges and Potential.
Why in News?
Healthcare has become more focused on innovation and technology over the past two years and 80% of healthcare systems are aiming to increase their investment in digital healthcare tools in the coming five years.
What is the Scenario of the Healthcare Sector in India?
- Healthcare industry comprises hospitals, medical devices, clinical trials, outsourcing, telemedicine, medical tourism, health insurance and medical equipment.
- The government (public healthcare system), comprises limited secondary and tertiary care institutions in key cities and focuses on providing basic healthcare facilities in the form of Primary Healthcare Centres (PHCs) in rural areas.
- The private sector provides a majority of secondary, tertiary, and quaternary care institutions with major concentration in metros, tier-I and tier-II cities.
- The Indian healthcare sector is expected to record a three-fold rise, growing at a CAGR (Compound Annual Growth Rate) of 22% between 2016–22 to reach USD 372 billion in 2022 from USD 110 billion in 2016.
- In the Economic Survey of 2022, India’s public expenditure on healthcare stood at 2.1% of GDP in 2021-22 against 1.8% in 2020-21 and 1.3% in 2019-20.
- In FY21, gross direct premium income underwritten by health insurance companies grew 13.3% YoY to Rs. 58,572.46 crore (USD 7.9 billion).
- The Indian medical tourism market was valued at USD 2.89 billion in 2020 and is expected to reach USD 13.42 billion by 2026.
- Telemedicine is also expected to reach USD 5.5 billion by 2025.
What are the Challenges with the Health Sector?
- Inadequate access to basic healthcare services such as shortage of medical professionals, a lack of quality assurance, insufficient health spending, and, most significantly, insufficient research funding.
- One of the major concerns is the administrations' insufficient financial allocation.
- Even neighbouring countries like Bangladesh and Pakistan have over 3% of their GDP going towards the public healthcare system.
- Preventive care is undervalued in India, despite the fact that it has been shown to be quite beneficial in alleviating a variety of difficulties for patients in terms of unhappiness and financial losses.
- In India, R&D and cutting-edge technology-led new projects receive little attention.
- Policymaking is undoubtedly crucial in providing effective and efficient healthcare services. In India, the issue is one of supply rather than demand, and policymaking can help.
- In India, there is a shortage of doctors, nurses, and other healthcare professionals.
- According to a study presented in Parliament by a minister, India is short 600,000 doctors.
- Doctors work in extreme conditions ranging from overcrowded out-patient departments, inadequate staff, medicines and infrastructure.
What is the Potential of the Indian Health Sector?
- India's competitive advantage lies in its large pool of well-trained medical professionals . India is also cost competitive compared to its peers in Asia and western countries. The cost of surgery in India is about one-tenth of that in the US or Western Europe.
- India has all the essential ingredients for the exponential growth in this sector, including a large population, a robust pharma and medical supply chain, 750 million plus smartphone users, 3 rd largest start-up pool globally with easy access to VC (Venture Capital Fund) funding and innovative tech entrepreneurs looking to solve global healthcare problems.
- India will have about 50 clusters for faster clinical testing of medical devices to boost product development and innovation.
- The sector will be driven by life expectancy, shift in disease burden, changes in preferences, growing middle class, increase in health insurance, medical support, infrastructure development and policy support and incentives.
- As of 2021, the Indian healthcare sector is one of India’s largest employers as it employs a total of 4.7 million people. The sector has generated 2.7 million additional jobs in India between 2017-22 -- over 500,000 new jobs per year
What are the Initiatives for the Health Care Sector?
- National Health Mission
- Ayushman Bharat.
- Pradhan Mantri Jan Arogya Yojana (AB-PMJAY) .
- National Medical Commission
- PM National Dialysis Programme.
- Janani Shishu Suraksha Karyakram (JSSK).
- Rashtriya Bal Swasthya Karyakram (RBSK).
Way Forward
- There is an urgent need to improve the infrastructure of public hospitals, which are overburdened as a result of India's large population.
- The government should encourage private hospitals because they make a significant contribution.
- Because the difficulties are severe and cannot be tackled just by the government, the private sector must also engage.
- To improve the sector's capabilities and efficiency, more medical personnel must be inducted.
- Medical gadgets in hospitals and clinics, mobile health apps, wearables, and sensors are only a few examples of technology that should be included in this area.
UPSC Civil Services Examination, Previous Year Questions (PYQs)
Q. Which of the following are the objectives of ‘National Nutrition Mission’? (2017)
- To create awareness relating to malnutrition among pregnant women and lactating mothers.
- To reduce the incidence of anaemia among young children, adolescent girls and women.
- To promote the consumption of millets, coarse cereals and unpolished rice.
- To promote the consumption of poultry eggs.
Select the correct answer using the code given below:
(a) 1 and 2 only (b) 1, 2 and 3 only (c) 1, 2 and 4 only (d) 3 and 4 only
- National Nutrition Mission (POSHAN Abhiyaan) is a flagship programme of the Ministry of Women and Child Development, GoI, which ensures convergence with various programmes like Anganwadi services, National Health Mission, Pradhan Mantri Matru Vandana Yojana, Swachh-Bharat Mission, etc.
- The goals of National Nutrition Mission (NNM) are to achieve improvement in nutritional status of children from 0-6 years, adolescent girls, pregnant women and lactating mothers in a time bound manner during the next three years beginning 2017- 18. Hence, 1 is correct.
- NNM targets to reduce stunting, under-nutrition, anaemia (among young children, women and adolescent girls) and reduce low birth weight of babies. Hence, 2 is correct.
- There is no such provision relating to consumption of millets, unpolished rice, coarse cereals and eggs under NNM. Hence, 3 and 4 are not correct.
- Therefore, option (a) is the correct answer.
Q. “Besides being a moral imperative of a Welfare State, primary health structure is a necessary precondition for sustainable development.” Analyse. (2021)
Source: PIB


Essay on Healthcare in India
Students are often asked to write an essay on Healthcare in India in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Healthcare in India
Introduction.
Healthcare in India is a critical sector. It includes public and private hospitals, clinics, and other medical facilities.
Public Healthcare
The government provides public healthcare. It’s often free or low-cost, making it accessible to many people.
Private Healthcare
Private healthcare, on the other hand, is usually more expensive. However, it tends to have better facilities and shorter wait times.
India faces challenges in healthcare, like inadequate facilities in rural areas and a shortage of trained medical professionals.
250 Words Essay on Healthcare in India
Healthcare in India is a multifaceted system, encompassing public and private sectors, traditional and modern medicine, and urban and rural disparities. This essay explores the current state of healthcare in India, its challenges, and potential solutions.
Current State of Healthcare
India’s healthcare sector has made significant strides, with increased life expectancy and decreased infant mortality. However, it is riddled with disparities. While urban areas enjoy better healthcare facilities, rural regions grapple with inadequate infrastructure and lack of trained medical personnel.
The challenges are manifold. Accessibility and affordability remain major concerns. A large portion of the population lacks access to quality healthcare, while high out-of-pocket expenses push many into poverty. Furthermore, there is a significant shortage of healthcare professionals, particularly in rural areas.
Public-Private Partnership
A public-private partnership (PPP) is seen as a viable solution. The private sector’s resources and efficiency can supplement the public sector’s reach and affordability. However, the implementation of PPPs requires stringent regulations to prevent exploitation.
Role of Technology
Technology can bridge the urban-rural divide. Telemedicine, AI, and mobile health technologies can facilitate remote consultations, predictive diagnostics, and health monitoring, making healthcare more accessible and affordable.
500 Words Essay on Healthcare in India
India’s healthcare sector is a study in contrasts, presenting a complex tapestry of cutting-edge advancements and systemic challenges. With an expansive population and diverse health needs, the healthcare system in India is a critical component of the nation’s development agenda.
The Landscape of Indian Healthcare
India’s healthcare infrastructure is a mix of public and private providers. The public system, under the aegis of the Ministry of Health and Family Welfare, provides primary, secondary, and tertiary care. However, it suffers from inadequate funding, lack of infrastructure, and a dearth of healthcare professionals. The private sector, on the other hand, is burgeoning. It is technologically advanced, offers high-quality services, but is often criticized for being expensive and inaccessible to the poor.
Healthcare Accessibility and Affordability
Government initiatives.
Recognizing these challenges, the Indian government has launched various initiatives. The National Health Mission aims to improve health outcomes, particularly for the rural population. The Ayushman Bharat scheme, launched in 2018, provides health insurance coverage to the underprivileged, aiming to make healthcare more affordable. These initiatives, while commendable, need effective implementation and monitoring to ensure their success.
Technological Innovations
Technological innovations have the potential to revolutionize India’s healthcare landscape. Telemedicine, artificial intelligence, and digital health records can address the issues of accessibility and affordability. Telemedicine can bridge the urban-rural divide by providing remote consultations. AI can assist in disease prediction and management, while digital health records can streamline patient data, improving efficiency and patient care.
Challenges and Future Prospects
The future of healthcare in India lies in adopting a holistic approach. This includes increasing public health expenditure, strengthening primary healthcare, improving health literacy, and leveraging technology.
India’s healthcare sector, while fraught with challenges, is teeming with potential. With the right mix of policy interventions, technology adoption, and a focus on equitable access, India can transform its healthcare landscape, ensuring a healthier future for its citizens. The journey is long and arduous, but with concerted efforts, a robust and inclusive healthcare system is achievable.
That’s it! I hope the essay helped you.
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
- Share full article
Advertisement
Supported by
Guest Essay
Kamala Harris Had a Great Health Care Idea in 2019. She Should Embrace It.

By Jacob S. Hacker
Mr. Hacker is a political science professor at Yale who has researched and written extensively about health care.
From the moment Kamala Harris became the presumptive Democratic nominee, Republicans have sought to paint her as a far-left California liberal. After all, they argue, she supported getting rid of private health insurance in her 2019 presidential campaign.
But Ms. Harris didn’t seek to eliminate private insurance in 2019. The core of her previous campaign’s health plan was an intelligently designed and politically astute public option — a more robust version of the Democratic approach embraced that year by Joe Biden (but one he never pursued after he took office). Essentially, she wanted to encourage Americans to buy into a revamped Medicare program that would give people the choice of public or private coverage.
As the so-called father of the public option , I feel confident in saying that Ms. Harris’s 2019 plan for a public option was — and remains — the strongest ever put forth by a presidential candidate. She shouldn’t run away from it. She should embrace it as a central part of her 2024 campaign both because it is smart policy and because it is smart politics.
Health care is “unbelievably complex,” as President Donald Trump remarked in 2017, as his party’s drive to repeal and replace the Affordable Care Act headed for defeat. Americans hate a lot about the current semi-system — its high prices, its insecure coverage, its rapacious financial practices (and until 2017, they seemed fairly ambivalent about the A.C.A., too).
The G.O.P.’s repeal rout made clear that a majority of Americans don’t want to go back to a time before the Affordable Care Act. It also reinvigorated the Democratic Party. No issue has unified the party or dominated its messaging like health care. It’s where abortion, child and maternal health, the rural health crisis, paid medical and family leave, the health risks of climate change, the continuing threat of Covid and the economic security of working families all come together.
Still, the party does not quite agree on what the big health care policy goal should be. Progressives advocate a universal Medicare program financed by higher taxes, which is to say Medicare for all. Moderates call for upgrading the A.C.A. by adding a public option (which was stripped from the original legislation before its passage in 2010).
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
Multi-Sector Partnerships: Key To Catalyzing Climate, Education And Health Impact In Asia

- Share to Facebook
- Share to Twitter
- Share to Linkedin
Asia’s philanthropy sector can accelerate and scale its impact by partnering with key stakeholders in the public and private sectors to unlock capital and catalyze solutions tackling our greatest challenges.
The "Partnerships for Impact: A Roadmap on Collaboration to Catalyse Climate, Education, and Health Action in Asia" report captures key learnings, innovative solutions, case studies, and actionable takeaways from the Philanthropy Asia Summit (PAS) 2024.
Solving the global climate challenge involves solving for Asia, which accounts for over half of the world’s population and emissions. The region is disproportionately impacted by climate change vis-à-vis the rest of the world. The time to act is now.
“For philanthropy to be transformative, collaboration with government is essential,” said The Rt Hon Tony Blair, Executive Chairman of the Tony Blair Institute for Global Change and former Prime Minister of Great Britain and Northern Ireland, at the Philanthropy Asia Summit in Singapore this April. Governments have the resources, authority and reach to drive significant impact and build sustainable programs.
Blair emphasized the importance of philanthropists in mobilizing private sector investment and government intervention to drive climate, education and health action in Asia.
“The capital required to achieve philanthropic objectives, particularly in addressing climate change, exceeds the resources of the philanthropic sector, let alone individual families or foundations,” says Desmond Kuek, Executive Director and CEO of Temasek Trust. “While the philanthropic sector can provide catalytic capital to crowd in funding from the public and private sectors, it is particularly vital for the private sector to step up.”
Developing economies need US$2 trillion in climate investments every year until 2030, yet only 1.6% of the US$811 billion in philanthropic giving in 2022 was focused on climate change mitigation. This gap exists partly because of a lack of evidence and data-driven approaches to measure impact, which are essential in unlocking both government action and private sector capital.
The Rt Hon Tony Blair, Executive Chairman of the Tony Blair Institute for Global Change and former Prime Minister of Great Britain and Northern Ireland, spoke at a fireside chat at PAS 2024.
Private-Public-Philanthropic Partnerships (PPPPs) Vital To Tackle Interconnected Challenges
Interconnected challenges in climate, education, and health often transcend borders, demanding systems thinking and a holistic approach, supported by multi-sector collaboration and innovation.
To narrow the gap in climate funding, philanthropists can embark on blended finance approaches for green infrastructure projects. Philanthropic capital, being more flexible and long-term with a greater tolerance for risk, can derisk projects and crowd in capital from the public and private sectors. Philanthropists can also support governments in designing their infrastructure plans or pool projects into diversified funds to attract private sector participation.
Empowering and building the capabilities of local communities are essential for the sustained success of philanthropic interventions. Co-creating interventions with local communities ensures that they are culturally relevant and supported by those they aim to help. For example, in Fiji and Indonesia, the Revitalising Informal Settlements and their Environments (RISE) initiative partners with governments to address the disproportionate impact of climate-induced water quality deterioration and flooding on people living in informal settlements. Funding is provided for wastewater treatment and improved sewage systems, which are co-designed with local communities.
Opportunities for collaboration also exist in education. Asia is home to 3 in 5 of the world’s illiterate adults, so intervention must focus on providing education in the early years for children in rural and economically disadvantaged settings. Prudence Foundation, the philanthropic arm of Prudential PLC, has partnered with UNICEF to provide caregiving support to families across Thailand and Indonesia and educate parents on the importance of early learning opportunities to help children develop their full potential.
In public health, significant capital is required to address challenges such as infectious disease outbreaks. For example, there are over 100 million cases of dengue each year, with South and Southeast Asia being major hotspots. The introduction of the Wolbachia bacteria—which reduces the ability of mosquitoes to transmit viruses to people—into mosquito populations is a novel approach that has dramatically reduced dengue incidence in communities. Meanwhile, viable vaccines have been developed in recent years and are waiting for wider rollouts. Scaling such interventions requires PPPPs to provide the necessary funding and infrastructure.
At a PAS 2024 partner session anchored by Wellcome Trust and supported by the Bill & Melinda Gates Foundation and Novo Nordisk Foundation, panelists explored ways to better monitor, control, manage, and treat widespread and epidemic diseases globally, with a focus on Asia.
In such a collaboration model, philanthropists go beyond the role of funders to become change agents who build local capabilities and facilitate collective action to create sustainable impact.
Priming Asia As A Force For Good
Asia’s vibrant philanthropic landscape is evolving in response to increasingly complex and urgent societal and environmental challenges. Bold, evidence-based philanthropic innovation and multi-sector collaboration are vital to catalyze and scale transformative impact, making a more sustainable tomorrow possible.
“A key benefit of philanthropy is the unique opportunity it provides to take big bets and drive social innovation, particularly when pursued through robust and impactful partnerships,” says Lim Seok Hui, CEO of Philanthropy Asia Alliance. “By convening like-minded partners to cross-pollinate best practices between Asia and the world, discover shared interests and explore new models of collaboration, we aim to collectively advance Asian solutions for global challenges.”
These insights were from the Philanthropy Asia Summit 2024, which took place from April 15 to 18 in Singapore. Access the full insights report, titled “ Partnerships for Impact: A Roadmap on Collaboration to Catalyse Climate, Education, and Health Action in Asia .”

- Editorial Standards
- Reprints & Permissions

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
HHS Assistant Secretary for Health ADM Rachel Levine Statement Marking the 2-year Anniversary of the Inflation Reduction Act and its Benefits to the Climate and Health Sector
Today marks the two-year anniversary of the signing of the Inflation Reduction Act, a landmark investment in climate protection. The Inflation Reduction Act is accelerating our progress toward President Biden and Vice President Harris' ambitious climate goals, which include building resiliency and reducing emissions in our health sector.
Climate change poses a threat not just to our health, but to our health systems. Climate change is the most significant threat to human health in the 21st century, according to more than 200 medical journals. It creates both acute and chronic risks, particularly to vulnerable populations, and already costs the American economy billions of dollars a year, significantly burdening the nation’s healthcare system. The health care sector also contributes to the problem itself, accounting for 8.5 percent of the country’s carbon emissions.
The Inflation Reduction Act provides billions of dollars for energy efficiency, renewable energy, and resilience investments that can strengthen our health care organizations, particularly safety net health care organizations. These opportunities support the core mission of health care providers by improving emergency preparedness and lowering operating expenses. Inflation Reduction Act funding opportunities help providers make investments that allow them to stay open before, during, and after emergencies and reduce their own pollution levels.
- For example, Boston Medical Center is using the Investment Tax Credit to help finance the Clean Power Prescription, a first-of-its-kind pilot program that provides solar energy credits to patients who report difficulty affording household utility payments. The credits are generated by a 356 kilowatt (kW) solar array on the campus of Boston Medical Center. Patients enrolled in the pilot receive a monthly credit on their electric bills, totaling $600 over the course of twelve months.
- Valley Children’s Healthcare is using the same tax credit to finance a new microgrid. The new microgrid will ensure that the hospital remains open during power outages and will meet 80 percent of the hospital’s peak time energy needs. The microgrid is also expected to cut carbon emissions by more than 50 percent from Valley Children’s 2021 baseline.
- AdventHealth is using the Investment Tax Credit to install a 3-megawatt solar photovoltaic system that will become one of the largest privately owned solar projects in Florida. The solar canopy is expected to produce 4,200 megawatt hours per year, or the equivalent of annual electricity use for more than 550 U.S. homes. AdventHealth will also be installing 31 dual-port electric vehicle charging stations across the campus for team members and guests.
- OhioHealth is using the Alternative Fuel Vehicle Refueling Property Credit to finance electric vehicle charging stations that charge OhioHealth’s fleet overnight and are free for its rural community to use during the day.
The Office of Climate Change and Health Equity shares the stories of these providers, and information for providers hoping to start making investments in energy efficiency, renewable energy, and resilience, through its Catalytic Program on Utilizing the Inflation Reduction Act . The Program targets outreach to safety net providers and aims to connect the health sector to opportunities that will help them save money and better serve their communities.
We know that climate solutions are health solutions. The Inflation Reduction Act helps the health sector play its part in achieving health equity for all.
Sign Up for Email Updates
Receive the latest updates from the Secretary, Blogs, and News Releases
Subscribe to RSS
Receive latest updates

Related News Releases
Hhs marks farmworker appreciation day; expands language access and increases support for workplace evaluations, clinician education, and more, biden-harris administration announces more than $68 million to improve access to hiv care for women, infants, children and youth, hhs secretary xavier becerra statement on supreme court decision in food and drug administration v. alliance for hippocratic medicine, related blog posts.

Change Story: Director Reginald Mebane

Honoring Lyme Disease Awareness Month with a Multi-Year Plan to Change the Lyme Disease Status Quo
The u.s. department of health and human services is taking action to strengthen primary care, media inquiries.
For general media inquiries, please contact [email protected] .
Disclaimer Policy: Links with this icon ( ) mean that you are leaving the HHS website.
- The Department of Health and Human Services (HHS) cannot guarantee the accuracy of a non-federal website.
- Linking to a non-federal website does not mean that HHS or its employees endorse the sponsors, information, or products presented on the website. HHS links outside of itself to provide you with further information.
- You will be bound by the destination website's privacy policy and/or terms of service when you follow the link.
- HHS is not responsible for Section 508 compliance (accessibility) on private websites.
For more information on HHS's web notification policies, see Website Disclaimers .

Speaking Up About Mental Health Essay Contest Winners Announced
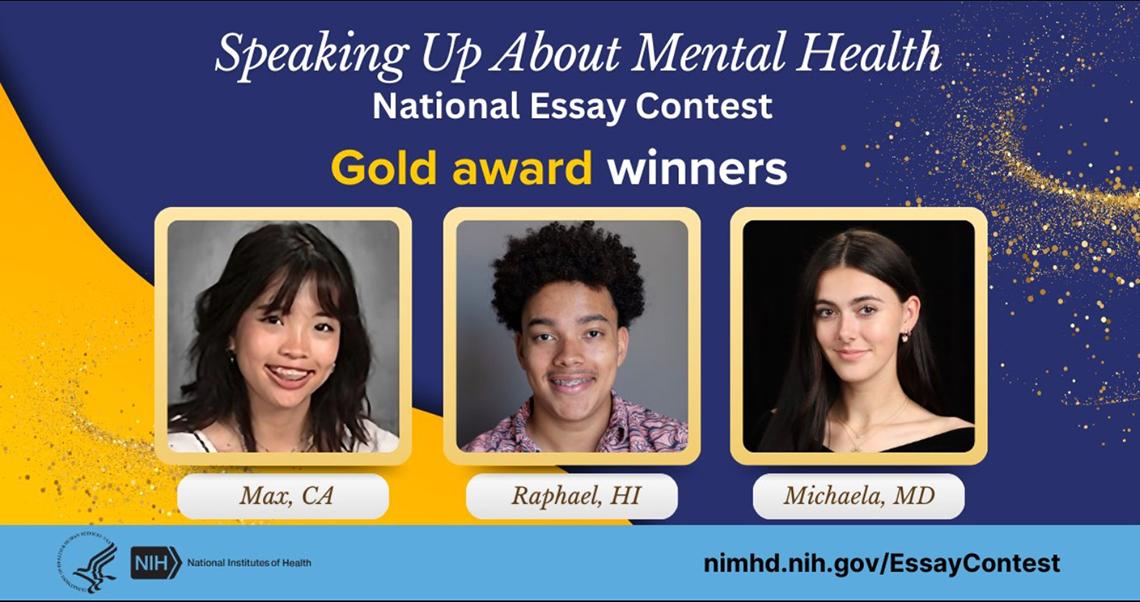
Congratulations to the 18 winners and six honorable mentions for the 2024 Speaking Up About Mental Health Essay Contest.
The contest challenges high school students ages 16-18 to raise awareness of mental health. It gives students a platform to share ways to eliminate and/or reduce mental health stigma faced by young people, especially in diverse communities. More than 370 teens from 33 states submitted essays.
The National Institute of Mental Health, the National Institute on Minority Health and Health Disparities and the Eunice Kennedy Shriver National Institute of Child Health and Human Development co-sponsored the contest. It’s part of a Health and Human Services–wide initiative to tackle the nation’s mental health crisis.
Read the award-winning essays at https://go.nih.gov/eQCZ1X5 . NIH recognizes these talented essay winners for their thoughtfulness and creativity in addressing youth mental health.
The essays are written in the students’ own words and are unedited.
The NIH Record
The NIH Record , founded in 1949, is the biweekly newsletter for employees of the National Institutes of Health.
Published 25 times each year, it comes out on payday Fridays.
Associate Editor: Dana Talesnik [email protected] (link sends e-mail)
Assistant Editor: Eric Bock [email protected] (link sends e-mail)
Staff Writer: Amber Snyder [email protected] (link sends e-mail)
- NIH Record Home
- Current Issue
- Past Issues
- Submission Deadlines
- Privacy Policy
- Disclaimers
- Accessibility
- Freedom of Information Act
- No Fear Act
- HHS Vulnerability Disclosure
- Office of Inspector General
- '' Subscribe
NIH…Turning Discovery Into Health ®
National Institutes of Health 9000 Rockville Pike
U.S. Department of Health and Human Services (link is external)

CT News Junkie
Connecticut News from your locally owned & operated news source at the state Capitol since 2005.
Connecticut Reached New Private-Sector Employment Peak In July

Share this:

Overall, employers added 700 jobs in July, bringing the number of people employed in the state to 1,714,400. The increase in jobs brought the state’s unemployment rate down to 3.6%. The unemployment rate remained flat when compared to a year ago. Connecticut’s rate is significantly lower than the national rate, which stood at 4.3%.
“Jobs have increased every month so far in 2024, and private sector employment is at a new all-time high,” said Patrick Flaherty, Director of the Office of Research at the Connecticut Department of Labor. “While there are monthly fluctuations in particular industries, the overall trend points to steady job growth and low unemployment.”
Of the six Labor Market Areas (LMAs) in the state, three lost jobs while two gained employees. The Hartford-West Hartford-East Hartford, Danbury and Bridgeport-Stamford-Norwalk LMAs all showed job losses, while New Haven and Waterbury saw gains. The Norwich-New London-Westerly LMA was unchanged.
“With an increase of 700 jobs, Connecticut continues its positive economic momentum,” he said in a statement. “We have now seen seven consecutive months of job growth, with private-sector employment reaching an all-time high. On top of that, private sector wages are up 4.5% year-over-year — a sign that employers are doing all they can to provide opportunities and attract and retain Connecticut’s skilled workforce.”
DiPentima announced that the CBIA Foundation has commissioned a report, scheduled to be released next month, that will feature strategic, long-term recommendations for growing the state’s economy and expanding opportunities for all residents.
Jamil Ragland
Jamil Ragland writes and lives in Hartford. You can read more of his writing at www.nutmeggerdaily.com.
The views, opinions, positions, or strategies expressed by the author are theirs alone, and do not necessarily reflect the views, opinions, or positions of CTNewsJunkie.com or any of the author's other employers.
Impact of Technology on Healthcare Services Analytical Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Introduction
Technology and the cost of health care, growth and development in the health care sector, sustainability of health technology, counter arguments, reference list.
This is a position paper based on the given topic. It contains the author’s opinion on the impact of technology on healthcare services. The paper also discusses how technology has changed the education and labor requirements for the healthcare sector.
Health care is among the sectors that lack sufficiency pertaining to adoption of technology and its utility. The turbulent healthcare market has been inundated by increased patient demands, declining margins, constant revisions of the current laws and restrictive laws.
The healthcare sector is increasingly viewing IT as a basic asset in the provision of decision support and health related services, as well as managing the increasing costs of health care. Advancement in technology has influenced the manufacture, distribution, and even administration of healthcare equipments and medicine.
The medical world is now full of machines and bioengineered equipments that require a certain degree of technological proficiency to operate. Moreover, technology has also empowered customers to seek and access their healthcare rights and information. Customers can now use current technology to assess the credentials of medical practitioners.
Negligence and errors in medical treatment that were witnessed before the inception of modern technology have reduced. With this hint in mind, there is a need for research on the impact that technological advancement has had on healthcare. Besides, there is a call for further research on how such technological changes have altered healthcare education and labor requirements in the health sector.
The paper therefore provides a framework/plan for a case study final paper on this subject with four chapters each providing a detailed scrutiny of the issue under study. Primary sources such as statistical findings on the subject will be used in the research. Archival documents such as reports, government publications, responses, and reflections on the subject from different stakeholders will also be used.
Technology has enabled healthcare professionals to treat critical diseases but at the same time the cost of such treatments has increased, making it out of reach for most of the patients. The concerned departments do provide subsidy for the costly technology but that too is for a limited period and only for select technologies.
The first chapter will involve a literature search on the impact of technological changes on the cost of health care. Owing to the adoption of new technological methods of treatment, the cost of healthcare has also risen in the past few years. In this chapter, the impact of technology on the healthcare financing will be evaluated using relevant literature, detailing the same.
Medical technology is expensive and hence today the cost of medicine and medical services has risen. Modern technology has also been credited with the current increased level of accuracy in medical treatment. Cannon (2000), in his literary work, provides details of the various ways that technology has aided in the compliance to medication for mental health patients.
Nagykaldi and Mold (2007) evaluated the role of health information technology on the translation of research into practice, and managed to capture some of the limitations, with cost being a major factor. Teich et al. (2000) also duplicated the findings, with their study showing that cost limits the adoption of basic medical technologies. According to Galas and Hood (2009), medical schools and other health institutions also find it expensive to adapt to new technologies.
This chapter will highlight some of the important milestones in the health sector in relation to health technology. Cannon and Allen (2000) state its usefulness in the medication compliance. However, with the increased medical technology development, the government has to do higher spending in the health sector (Bardhan & Thouin, 2012, 443).
The benefits of the spending will be weighed against the efficacy of the technology in this chapter. Chaudhry et al. (2006) evaluated the benefits over a ten-year period, with benefits being weighed against the costs of technology in healthcare.
The growth in the industry will be evaluated in terms of mechanization and in the solid facilities housing the machines. According to Haddad (2012), these have also seen significant developments. The study by Nagykaldi and Mold (2007) will be important in this chapter to highlight technological developments.
Impacts of the current technology on health education and labor requirements
Information technology can have a great impact on the variety of jobs and their necessity. As is understood, new technology needs appropriate knowledge. The healthcare employees who can adapt to the change will continue and those who can’t will be eliminated. New technology has even changed the approach of the patients. Patients now prefer to contact the doctors via emails.
This has reduced the regular visits by patients to healthcare centers. Obviously, this aspect has reduced the need of more healthcare employees. Cannon and Allen (2000) detail some of the changes in the industry, especially in the dispensing of drugs.
This chapter will deal with the relevance of technological advances in the health sector to the labor requirements and in health education. Modern technology and medical informatics are quickly taking over some of the traditional roles that were played by medical practitioners (Korzep, 2010, p. 354).
Despite the developments in the health technology, the medical practitioners remain the primary healthcare providers. Machines will not replace them any time soon. However, mechanization has led to the reduction in the number of personnel required to perform certain procedures as evidenced in some of the literary works to be reviewed (Nagykaldi & Mold, 2007; Haddad, 2012).
This will be discussed in this chapter in relation to the labor laws. Well-documented health records on computers are quickly replacing the period of bad handwriting of doctors (Dhillon, 2011, 397).
There have been ongoing discussions on whether the investment done by healthcare centers on new technology is necessary and whether the new technology will be able to sustain itself. It is understood that initially, such new technologies might receive subsidies from charity organizations or the government. Sustenance in healthcare means that with time any particular machinery becomes self sufficient (doesn’t need any external aid or grant).
In this chapter, an evaluation of the sustainability of the existing health technology will be evaluated. Over time, smaller, better, and more sophisticated machines have always replaced most of the technological innovations in different fields. The health industry is no exception. Researchers are always looking for better interventions (Chaudhry et al., 2006).
In this section, a review of the likely changes will be done. Some of these are available in the recommendations of the researches that will be reviewed (Cannon and Allen, 2000; Haddad, 2012). In their research, Nagykaldi and Mold (2007) state that technology is dynamic and will change in line with the prevailing innovations. The sustainability of such changes and the existing technological milestones will therefore be reviewed in this section.
It may be argued that while adoption of new technology has improved medical treatment, it has also increased the cost. Another drawback of new technology is the reduction in the job opportunities. The new technology also needs adequate training that again involves cost and time. Specialized personnel are required to handle such technology. A small mistake in handling such technology might be disastrous. So there are both pros and cons of technology.
Bardhan, Indranil, and Mark Thouin.”Health information technology and its impact on the quality and cost of healthcare delivery.” Decision Support Systems 55, no. 2 (May 2013): 438-449.
Cannon, Dale and Allen Steveb. “Comparison of the effects of computer and manual reminders on compliance with a mental health clinical practice guideline.” Journal of the American Medical Informatics Association 7, no. 2 (May 2000):196-203.
Chaudhry, Basit, Wang Jerome, Wu Shinyi, Maglione Margaret, Mojica Walter, Roth Elizabeth, Morton Sally, and Shekelle Paul. “Systematic review: impact of health information technology on quality, efficiency and cost of medical care.” Annals of Internal Medicine 12, no.144 (June 2006): 742-753.
Dhillon, Sigh. “Medical Equipment Reliability: a review, analysis methods and improvement strategies.” International Journal of Reliability, Quality & Safety Engineering 18, no. 4 (June 2011): 391-403.
Galas, David, and Leroy Hood. “Systems Biology and Emerging Technologies Will Catalyze the Transition from Reactive Medicine to Predictive, Personalized, Preventive and Participatory (P4) Medicine.” Interdisciplinary Bio Central 1, no. 1 (March 2009): 1-4.
Haddad, Tamer. “The Applicability of Total Productive Maintenance for Healthcare Facilities: an Implementation Methodology.” International Journal of Business, Humanities and Technology 2, no. 2 (March 2012): 148.
Korzep, Karen. “The future of technology and the effect it may have on replacing human jobs.” Technology & Health Care 18, no. 4/5 (August 2010): 353-358.
Nagykaldi, Zsolt, and Mold James. “The role of health information technology in the translation of research into practice: An Oklahoma Physicians Resource/Research Network (OKPRN) study.” Journal of the American Board of Family Medicine 2, no. 2 (June 2007): 188-195.
Teich, Jonathan, Merchia Pankaj, Schmiz Jennifer, Kuperman Gilad, Spurr Cynthia, and Bates, David. “Effect of computerized physician order entry on prescribing practices.” Archives of Internal Medicine 1, no. 160 (June 2000): 2741-2747.
- IT Infrastructure Prioritization
- Health IT Vendors and Communities Cooperation
- Christian Ethics: Working With Experience and Working With Reason
- Marketing Plan: Johnson & Johnson Inc
- Cancel Culture Meaning and Role in Modern Society
- Technological Development in the Healthcare Industry
- Implementing Telemedicine Solutions: Grand Hospital
- Wireless Technology in Health Monitoring
- Investigative Report on Health IT
- How Technology Is Changing the Health Care Field
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2019, July 9). Impact of Technology on Healthcare Services. https://ivypanda.com/essays/impact-of-technology-on-healthcare-services/
"Impact of Technology on Healthcare Services." IvyPanda , 9 July 2019, ivypanda.com/essays/impact-of-technology-on-healthcare-services/.
IvyPanda . (2019) 'Impact of Technology on Healthcare Services'. 9 July.
IvyPanda . 2019. "Impact of Technology on Healthcare Services." July 9, 2019. https://ivypanda.com/essays/impact-of-technology-on-healthcare-services/.
1. IvyPanda . "Impact of Technology on Healthcare Services." July 9, 2019. https://ivypanda.com/essays/impact-of-technology-on-healthcare-services/.
Bibliography
IvyPanda . "Impact of Technology on Healthcare Services." July 9, 2019. https://ivypanda.com/essays/impact-of-technology-on-healthcare-services/.

COMMENTS
Health benefits aside, increasing investment in primary prevention presents a strong economic imperative. For example, obesity contributes to the treatment costs of many other diseases: 70% of diabetes costs, 23% for CVD and 9% for cancers. Economic losses further extend to absenteeism and decreased productivity.
Pages: 2 Words: 635. Health Sector: Through the Department of Health and other health agencies, the government plays an important role in the development of the health sector. This is through the intensification of health systems and the production of human, financial and other necessary resources. Consequently, the government's involvement in ...
124 Healthcare Essay Topic Ideas & Examples. Healthcare is a diverse and complex field that encompasses a wide range of topics, issues, and challenges. Whether you are studying healthcare as a student, working in the healthcare industry, or simply interested in learning more about this important area, there are countless essay topics that you ...
View our collection of healthcare essays. Find inspiration for topics, titles, outlines, & craft impactful healthcare papers. Read our healthcare papers today! Homework Help; ... Holmas, T.H. & Kaarboe, O. 2011, Monitoring prioritization in the public health-care sector by use of medical guidelines, The case of Norway, Health economics, Vol. 20 ...
This chapter will highlight some of the important milestones in the health sector in relation to health technology. The benefits of the spending will be weighed against the efficacy of the technology in this chapter. This essay discusses health policies, the determinants of health, and the connections between the two.
The purpose of this paper is to define the ways of the reform's further development as well as to define the role of nursing in such a process. Health Care Reform Recommendations From Experts. First, to improve the quality of healthcare and reduce costs, the government should invest in health information technology.
A health essay is a piece of written work that explores a particular topic within the health sector. This could range from specific medical conditions, healthcare policies, trends in medicine, or broader societal issues like mental health. The aim is often to shed light on an issue, provide insights, or promote understanding. As with any essay ...
United States Health Sector Essays. National Healthcare Quality and Disparities Report. Since its birth in 2003, the National Healthcare Quality and Disparities Report has continuously provided an overview of health and health status in the United States. This has been a strong basis under which the transformation of the United States health ...
Health sector reform is a sustained process of fundamental change in policies and institutional arrangements of the health sector1, usually guided by the government. The process lays down a set of policy measures covering the four main core functions of the health system, viz., governance, provision, financing and resource generation.
Many of these are reviewed in more detail in the papers which follow. 3. Health sector reform and sustainable development Health improvement and health sector reform both contribute positively to sustainable development, in different but complementary ways. Health improve- ment directly increases human well-being and augments the potential for ...
Steer, Not Row Concept of Healthcare Policy. This ideology refuses to recognize the role of the clearly societal factors on people's continual ability to enjoy the 'fruits of civilization' while proposing that the task of ensuring the continuation of socio-economic progress is […] Health Care Policy: HPV Vaccination.
1. There's a new appreciation of the importance of health. Late last year, Dr. Tedros Ghebreyesus, Director-General of the World Health Organization (WHO), said: "The time has come for a new narrative that sees health not as a cost, but an investment that is the foundation of productive, resilient and stable economies.". That is exactly ...
Healthcare Management (discussion Questions) Healthcare Management: Compliance and egulation Various regulatory and compliance issues that dictate how health care professionals conduct themselves standardize the healthcare industry. According to Goodman and Norbeck (2013), the healthcare sector is turning into an industry focused on regulatory compliance, as opposed to patient care.
Health Care Comes Home lays the foundation for the integration of human health factors with the design and implementation of home health care devices, technologies, and practices. The book describes ways in which the Agency for Healthcare Research and Quality (AHRQ), the U.S. Food and Drug Administration (FDA), and federal housing agencies can ...
Health Sector Essays. Healthcare Sector Policy. Introduction Health sector involvement in health policy and the law greatly impacts how public health is delivered, how people act and reason, where they live, and the organization itself. This enhances general public health (Wilensky & Teitelbaum, 2019). ...
The healthcare industry in India includes hospitals, medical tourism, health insurance, medical equipment, telemedicine, outsourcing, clinical trials, and medical gadgets. The public and private sectors make up the two main components of India's healthcare delivery system. The Scenario of the Health Care Sector in India.
Chapter 9: An Econometric Analysis of Spatial Variations in Mortality Rates by Race and Sex. Author (s): (p. 161-227) In addition to working papers, the NBER disseminates affiliates' latest findings through a range of free periodicals — the NBER Reporter, the NBER Digest, the Bulletin on Retirement and Disability, the Bulletin on Health ...
Health Sector Policy Essays. Operating in Structure: Health Sector Policy and Governance. A social contract has been defined as an agreement between the members of an organized society such that the rulers define the responsibilities and rights of the community while the others voluntarily exchange these freedoms and liberties for protection ...
Pages: 1 (353 words) Sources: 3 Document Type: Essay Document #: 94252025. Fraud and abuse present significant problems for the health sector, leading to both financial losses and reduced quality of care. The outcomes of fraud and abuse are similar; but fraud and abuse are … of care.
The sector will be driven by life expectancy, shift in disease burden, changes in preferences, growing middle class, increase in health insurance, medical support, infrastructure development and policy support and incentives. As of 2021, the Indian healthcare sector is one of India's largest employers as it employs a total of 4.7 million people.
500 Words Essay on Healthcare in India Introduction. India's healthcare sector is a study in contrasts, presenting a complex tapestry of cutting-edge advancements and systemic challenges. With an expansive population and diverse health needs, the healthcare system in India is a critical component of the nation's development agenda.
Over the past three decades, routine immunizations have prevented 1.1 million deaths and saved the United States $540 billion, the C.D.C. estimated.
This essay discusses health policies, the determinants of health, and the connections between the two. The determinants of health are individual and environmental factors that affect people's physical and mental well-being and the ability to […] Food & Beverage Choices and Health Impacts.
Health care is "unbelievably complex," as President Donald Trump remarked in 2017, as his party's drive to repeal and replace the Affordable Care Act headed for defeat. Americans hate a lot ...
Interconnected challenges in climate, education, and health often transcend borders, demanding systems thinking and a holistic approach, supported by multi-sector collaboration and innovation.
The Program targets outreach to safety net providers and aims to connect the health sector to opportunities that will help them save money and better serve their communities. We know that climate solutions are health solutions. The Inflation Reduction Act helps the health sector play its part in achieving health equity for all. ###
Congratulations to the 18 winners and six honorable mentions for the 2024 Speaking Up About Mental Health Essay Contest. The contest challenges high school students ages 16-18 to raise awareness of mental health. It gives students a platform to share ways to eliminate and/or reduce mental health stigma faced by young people, especially in diverse communities. More than 370 teens from 33 states ...
A previous mpox public health emergency, declared in 2022, was caused by the relatively mild Clade 2. However, this time it is the far more deadly Clade 1 - which has killed up to 10% of those ...
The private sector has now recovered 106.1% of pre-Covid lockdown employment. On the other side, the government supersector lost 1,200 jobs in July. Government employment sits at 97.5% of pre ...
This is a position paper based on the given topic. It contains the author's opinion on the impact of technology on healthcare services. The paper also discusses how technology has changed the education and labor requirements for the healthcare sector. Get a custom critical writing on Impact of Technology on Healthcare Services. 193 writers ...