- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- New advances in type 1...
New advances in type 1 diabetes
- Related content
- Peer review
This article has a correction. Please see:
- New advances in type 1 diabetes - June 03, 2024
- Savitha Subramanian , professor of medicine ,
- Farah Khan , clinical associate professor of medicine ,
- Irl B Hirsch , professor of medicine
- University of Washington Diabetes Institute, Division of Metabolism, Endocrinology and Nutrition, University of Washington, Seattle, WA, USA
- Correspondence to: I B Hirsch ihirsch{at}uw.edu
Type 1 diabetes is an autoimmune condition resulting in insulin deficiency and eventual loss of pancreatic β cell function requiring lifelong insulin therapy. Since the discovery of insulin more than 100 years ago, vast advances in treatments have improved care for many people with type 1 diabetes. Ongoing research on the genetics and immunology of type 1 diabetes and on interventions to modify disease course and preserve β cell function have expanded our broad understanding of this condition. Biomarkers of type 1 diabetes are detectable months to years before development of overt disease, and three stages of diabetes are now recognized. The advent of continuous glucose monitoring and the newer automated insulin delivery systems have changed the landscape of type 1 diabetes management and are associated with improved glycated hemoglobin and decreased hypoglycemia. Adjunctive therapies such as sodium glucose cotransporter-1 inhibitors and glucagon-like peptide 1 receptor agonists may find use in management in the future. Despite these rapid advances in the field, people living in under-resourced parts of the world struggle to obtain necessities such as insulin, syringes, and blood glucose monitoring essential for managing this condition. This review covers recent developments in diagnosis and treatment and future directions in the broad field of type 1 diabetes.
Introduction
Type 1 diabetes is an autoimmune condition that occurs as a result of destruction of the insulin producing β cells of the pancreatic islets, usually leading to severe endogenous insulin deficiency. 1 Without treatment, diabetic ketoacidosis will develop and eventually death will follow; thus, lifelong insulin therapy is needed for survival. Type 1 diabetes represents 5-10% of all diabetes, and diagnosis classically occurs in children but can also occur in adulthood. The burden of type 1 diabetes is expansive; it can result in long term complications, decreased life expectancy, and reduced quality of life and can add significant financial burden. Despite vast improvements in insulin, insulin delivery, and glucose monitoring technology, a large proportion of people with type 1 diabetes do not achieve glycemic goals. The massive burden of type 1 diabetes for patients and their families needs to be appreciated. The calculation and timing of prandial insulin dosing, often from food with unknown carbohydrate content, appropriate food and insulin dosing when exercising, and cost of therapy are all major challenges. The psychological realities of both acute management and the prospect of chronic complications add to the burden. Education programs and consistent surveillance for “diabetes burnout” are ideally available to everyone with type 1 diabetes.
In this review, we discuss recent developments in the rapidly changing landscape of type 1 diabetes and highlight aspects of current epidemiology and advances in diagnosis, technology, and management. We do not cover the breadth of complications of diabetes or certain unique scenarios including psychosocial aspects of type 1 diabetes management, management aspects specific to older adults, and β cell replacement therapies. Our review is intended for the clinical reader, including general internists, family practitioners, and endocrinologists, but we acknowledge the critical role that people living with type 1 diabetes and their families play in the ongoing efforts to understand this lifelong condition.
Sources and selection criteria
We did individual searches for studies on PubMed by using terms relevant to the specific topics covered in this review pertaining to type 1 diabetes. Search terms used included “type 1 diabetes” and each individual topic—diagnosis, autoantibodies, adjuvant therapies, continuous glucose monitoring, automated insulin delivery, immunotherapies, diabetic ketoacidosis, hypoglycemia, and under-resourced settings. We considered all studies published in the English language between 1 January 2001 and 31 January 2023. We selected publications outside of this timeline on the basis of relevance to each topic. We also supplemented our search strategy by a hand search of the references of key articles. We prioritized studies on each highlighted topic according to the level of evidence (randomized controlled trials (RCTs), systematic reviews and meta-analyses, consensus statements, and high quality observational studies), study size (we prioritized studies with at least 50 participants when available), and time of publication (we prioritized studies published since 2003 except for the landmark Diabetes Control and Complications Trial and a historical paper by Tuomi on diabetes autoantibodies, both from 1993). For topics on which evidence from RCTs was unavailable, we included other study types of the highest level of evidence available. To cover all important clinical aspects of the broad array of topics covered in this review, we included additional publications such as clinical reviews as appropriate on the basis of clinical relevance to both patients and clinicians in our opinion.
Epidemiology
The incidence of type 1 diabetes is rising worldwide, possibly owing to epigenetic and environmental factors. Globally in 2020 an estimated 8.7 million people were living with type 1 diabetes, of whom approximately 1.5 million were under 20 years of age. 2 This number is expected to rise to more than 17 million by 2040 ( https://www.t1dindex.org/#global ). The International Diabetes Federation estimates the global prevalence of type 1 diabetes at 0.1%, and this is likely an underestimation as diagnoses of type 1 diabetes in adults are often not accounted for. The incidence of adult onset type 1 diabetes is higher in Europe, especially in Nordic countries, and lowest in Asian countries. 3 Adult onset type 1 diabetes is also more prevalent in men than in women. An increase in prevalence in people under 20 years of age has been observed in several western cohorts including the US, 4 5 Netherlands, 6 Canada, 7 Hungary, 8 and Germany. 9
Classically, type 1 diabetes presents over the course of days or weeks in children and adolescents with polyuria, polydipsia, and weight loss due to glycosuria. The diagnosis is usually straightforward, with profound hyperglycemia (often >300 mg/dL) usually with ketonuria with or without ketoacidemia. Usually, more than one autoantibody is present at diagnosis ( table 1 ). 10 The number of islet autoantibodies combined with parameters of glucose tolerance now forms the basis of risk prediction for type 1 diabetes, with stage 3 being clinical disease ( fig 1 ). 11 The originally discovered autoantibody, islet cell antibody, is no longer used clinically owing to variability of the assay despite standardisation. 12
Autoantibody characteristics associated with increased risk of type 1 diabetes 10
- View inline

Natural history of type 1 diabetes. Adapted with permission from Insel RA, et al. Diabetes Care 2015;38:1964-74 11
- Download figure
- Open in new tab
- Download powerpoint
Half of all new cases of type 1 diabetes are now recognized as occurring in adults. 13 Misclassification due to misdiagnosis (commonly as type 2 diabetes) occurs in nearly 40% of people. 14 As opposed to typical childhood onset type 1 diabetes, progression to severe insulin deficiency, and therefore its clinical presentation in adults, is variable. The term latent autoimmune diabetes of adults (LADA) was introduced 30 years ago to identify adults who developed immune mediated diabetes. 15 An international consensus defined the diagnostic criteria for LADA as age >30 years, lack of need for insulin use for at least six months, and presence of islet cell autoantibodies. 16 However, debate as to whether the term LADA should even be used as a diagnostic term persists. The American Diabetes Association (ADA) Standards of Care note that for the purpose of classification, all forms of diabetes mediated by autoimmune β cell destruction are included in the classification of type 1 diabetes. 17 Nevertheless, they note that use of the term LADA is acceptable owing to the practical effect of heightening awareness of adults likely to have progressive autoimmune β cell destruction and thereby accelerating insulin initiation by clinicians to prevent diabetic ketoacidosis.
The investigation of adults with suspected type 1 diabetes is not always straightforward ( fig 2 ). 18 Islet cell autoantibodies such as glutamic acid decarboxylase antibody (GADA), tyrosine phosphatase IA2 antibody, and zinc transporter isoform 8 autoantibody act as markers of immune activity and can be detected in the blood with standardized assays ( table 1 ). The presence of one or more antibodies in adults with diabetes could mark the progression to severe insulin deficiency; these individuals should be considered to have type 1 diabetes. 1 Autoantibodies, especially GADA, should be measured only in people with clinically suspected type 1 diabetes, as low concentrations of GADA can be seen in type 2 diabetes and thus false positive measurements are a concern. 19 That 5-10% of cases of type 1 diabetes may occur without diabetes autoantibodies is also now clear, 20 and that the diabetes autoantibodies disappear over time is also well appreciated. 21

Flowchart for investigation of suspected type 1 diabetes in adults, based on data from white European populations. No single clinical feature in isolation confirms type 1 diabetes. The most discriminative feature is younger age at diagnosis (<35 years), with lower body mass index (<25), unintentional weight loss, ketoacidosis, and glucose >360 mg/dL at presentation. Adapted with permission from Holt RIG, et al. Diabetes Care 2021;44:2589-625 1
Genetic risk scoring (GRS) for type 1 diabetes has received attention to differentiate people whose classification is unclear. 22 23 24 Developed in 2019, the T1D-GRS2 uses 67 single nucleotide polymorphisms from known autoimmune loci and can predict type 1 diabetes in children of European and African ancestry. Although GRS is not available for routine clinical use, it may allow prediction of future cases of type 1 diabetes to allow prevention strategies with immune intervention (see below).
A major change in the type 1 diabetes phenotype has occurred over the past few decades, with an increase in obesity; the reasons for this are complex. In the general population, including people with type 1 diabetes, an epidemic of sedentary lifestyles and the “westernized diet” consisting of increased processed foods, refined sugars, and saturated fat is occurring. In people with type 1 diabetes, the overall improvement in glycemic control since the report of the Diabetes Control and Complications Trial (DCCT) in 1993 (when one or two insulin injections a day was standard therapy) has resulted in less glycosuria so that the typical patient with lower body weight is uncommon in high income countries. In the US T1D Exchange, more than two thirds of the adult population were overweight or obese. 25
Similarly, obesity in young people with type 1 diabetes has also increased over the decades. 26 The combination of autoimmune insulin deficiency with obesity and insulin resistance has received several descriptive names over the years, with this phenotype being described as double diabetes and hybrid diabetes, among others, 26 27 but no formal nomenclature in the diabetes classification exists. Many of these patients have family members with type 2 diabetes, and some patients probably do have both types of diabetes. Clinically, minimal research has been done into how this specific population responds to certain antihyperglycemic oral agents, such as glucagon-like peptide 1 (GLP-1) receptor agonists, given the glycemic, weight loss, and cardiovascular benefits seen with these agents. 28 These patients are common in most adult diabetes practices, and weight management in the presence of insulin resistance and insulin deficiency remains unclear.
Advances in monitoring
The introduction of home blood glucose monitoring (BGM) more than 45 years ago was met with much skepticism until the report of the DCCT. 29 Since then, home BGM has improved in accuracy, precision, and ease of use. 30 Today, in many parts of the world, home BGM, a static measurement of blood glucose, has been replaced by continuous glucose monitoring (CGM), a dynamic view of glycemia. CGM is superior to home BGM for glycemic control, as confirmed in a meta-analysis of 21 studies and 2149 participants with type 1 diabetes in which CGM use significantly decreased glycated hemoglobin (HbA 1c ) concentrations compared with BGM (mean difference −0.23%, 95% confidence interval −3.83 to −1.08; P<0.001), with a greater benefit if baseline HbA 1c was >8% (mean difference −0.43%, −6.04 to −3.30; P<0.001). 31 This newer technology has also evolved into a critical component of automated insulin delivery. 32
CGM is the standard for glucose monitoring for most adults with type 1 diabetes. 1 This technology uses interstitial fluid glucose concentrations to estimate blood glucose. Two types of CGM are available. The first type, called “real time CGM”, provides a continuous stream of glucose data to a receiver, mobile application, smartwatch, or pump. The second type, “intermittently scanned CGM,” needs to be scanned by a reader device or smartphone. Both of these technologies have shown improvements in HbA 1c and amount of time spent in the hypoglycemic range compared with home BGM when used in conjunction with multiple daily injections or “open loop” insulin pump therapy. 33 34 Real time CGM has also been shown to reduce hypoglycemic burden in older adults with type 1 diabetes ( table 2 ). 36 Alerts that predict or alarm with both hypoglycemia and hyperglycemia can be customized for the patient’s situation (for example, a person with unawareness of hypoglycemia would have an alert at a higher glucose concentration). Family members can also remotely monitor glycemia and be alerted when appropriate. The accuracy of these devices has improved since their introduction in 2006, so that currently available sensors can be used without a confirmation glucose concentration to make a treatment decision with insulin. However, some situations require home BGM, especially when concerns exist that the CGM does not match symptoms of hypoglycemia.
Summary of trials for each topic covered
Analysis of CGM reports retrospectively can assist therapeutic decision making both for the provider and the patient. Importantly, assessing the retrospective reports and watching the CGM in real time together offer insight to the patient with regard to insulin dosing, food choices, and exercise. Patients should be encouraged to assess their data on a regular basis to better understand their diabetes self-management. Table 3 shows standard metrics and targets for CGM data. 52 Figure 3 shows an ambulatory glucose profile.
Standardized continuous glucose monitoring metrics for adults with diabetes 52

Example of ambulatory glucose profile of 52 year old woman with type 1 diabetes and fear of hypoglycemia. CGM=continuous glucose monitoring; GMI=glucose management indicator
Improvements in technology and evidence for CGM resulting in international recommendations for its widespread use have resulted in greater uptake by people with type 1 diabetes across the globe where available and accessible. Despite this, not everyone wishes to use it; some people find wearing any device too intrusive, and for many the cost is prohibitive. These people need at the very least before meal and bedtime home BGM.
A next generation implantable CGM device (Sensionics), with an improved calibration algorithm that lasts 180 days after insertion by a healthcare professional, is available in both the EU and US. Although fingerstick glucose calibration is needed, the accuracy is comparable to that of other available devices. 53
Advances in treatments
The discovery of insulin in 1921, resulting in a Nobel Prize, was considered one of the greatest scientific achievements of the 20th century. The development of purified animal insulins in the late 1970s, followed by human insulin in the early 1980s, resulted in dramatic reductions in allergic reactions and lipoatrophy. Introduction of the first generation of insulin analogs, insulin lispro in the mid-1990s followed by insulin glargine in the early 2000s, was an important advance for the treatment of type 1 diabetes. 54 We review the next generation of insulin analogs here. Table 4 provides details on available insulins.
Pharmacokinetics of commonly used insulin preparations
Ultra-long acting basal insulins
Insulin degludec was developed with the intention of improving the duration of action and achieving a flatter profile compared with the original long acting insulin analogs, insulin glargine and insulin detemir. Its duration of action of 42 hours at steady state means that the profile is generally flat without significant day-to-day variability, resulting in less hypoglycemia compared with U-100 glargine. 39 55
When U-100 insulin glargine is concentrated threefold, its action is prolonged. 56 U-300 glargine has a different kinetic profile and is delivered in one third of the volume of U-100 glargine, with longer and flatter effects. The smaller volume of U-300 glargine results in slower and more gradual release of insulin monomers owing to reduced surface area in the subcutaneous space. 57 U-300 glargine also results in lesser hypoglycemia compared with U-100 glargine. 58
Ultra-rapid acting prandial insulins
Rapid acting insulin analogs include insulin lispro, aspart, and glulisine. With availability of insulin lispro, the hope was for a prandial insulin that better matched food absorption. However, these newer insulins are too slow to control the glucose spike seen with ingestion of a high carbohydrate load, leading to the development of insulins with even faster onset of action.
The first available ultra-rapid prandial insulin was fast acting insulin aspart. This insulin has an onset of appearance approximately twice as fast (~5 min earlier) as insulin aspart, whereas dose-concentration and dose-response relations are comparable between the two insulins ( table 4 ). 59 In adults with type 1 diabetes, mealtime and post-meal fast acting aspart led to non-inferior glycemic control compared with mealtime aspart, in combination with basal insulin. 60 Mean HbA 1c was 7.3%, 7.3%, and 7.4% in the mealtime faster aspart, mealtime aspart, and post‐meal faster aspart arms, respectively (P<0.001 for non-inferiority).
Insulin lispro-aabc is the second ultra-rapid prandial insulin. In early kinetic studies, insulin lispro-aabc appeared in the serum five minutes faster with 6.4-fold greater exposure in the first 15 minutes compared with insulin lispro. 61 The duration of exposure of the insulin concentrations in this study was 51 minutes faster with lispro-aabc. Overall insulin exposure was similar between the two groups. Clinically, lispro-aabc is non-inferior to insulin lispro, but postprandial hyperglycemia is lower with the faster acting analog. 62 Lispro-aabc given at mealtime resulted in greater improvement in post-prandial glucose (two hour post-prandial glucose −31.1 mg/dL, 95% confidence interval −41.0 to −21.2; P<0.001).
Both ultra-rapid acting insulins can be used in insulin pumps. Lispro-aabc tends to have more insertion site reactions than insulin lispro. 63 A meta-analysis including nine studies and 1156 participants reported increased infusion set changes on rapid acting insulin analogs (odds ratio 1.60, 95% confidence interval 1.26 to 2.03). 64
Pulmonary inhaled insulin
The quickest acting insulin is pulmonary inhaled insulin, with an onset of action of 12 minutes and a duration of 1.5-3 hours. 65 When used with postprandial supplemental dosing, glucose control is improved without an increase in hypoglycemia. 66
Insulin delivery systems
Approved automated insulin delivery systems.
CGM systems and insulin pumps have shown improvement in glycemic control and decreased risk of severe hypoglycemia compared with use of self-monitoring of blood glucose and multiple daily insulin injections in type 1 diabetes. 67 68 69 Using CGM and insulin pump together (referred to as sensor augmented pump therapy) only modestly improves HbA 1c in patients who have high sensor wear time, 70 71 but the management burden of diabetes does not decrease as frequent user input is necessary. Thus emerged the concept of glucose responsive automated insulin delivery (AID), in which data from CGM can inform and allow adjustment of insulin delivery.
In the past decade, exponential improvements in CGM technologies and refined insulin dosing pump algorithms have led to the development of AID systems that allow for minimization of insulin delivery burden. The early AID systems reduced hypoglycemia risk by automatically suspending insulin delivery when glucose concentrations dropped to below a pre-specified threshold but did not account for high glucose concentrations. More complex algorithms adjusting insulin delivery up and down automatically in response to real time sensor glucose concentrations now allow close replication of normal endocrine pancreatic physiology.
AID systems (also called closed loop or artificial pancreas systems) include three components—an insulin pump that continuously delivers rapid acting insulin, a continuous glucose sensor that measures interstitial fluid glucose at frequent intervals, and a control algorithm that continuously adjusts insulin delivery that resides in the insulin pump or a smartphone application or handheld device ( fig 4 ). All AID systems that are available today are referred to as “hybrid” closed loop (HCL) systems, as users are required to manually enter prandial insulin boluses and signal exercise, but insulin delivery is automated at night time and between meals. AID systems, regardless of the type used, have shown benefit in glycemic control and cost effectiveness, improve quality of life by improving sleep quality, and decrease anxiety and diabetes burden in adults and children. 72 73 74 Limitations to today’s HCL systems are primarily related to pharmacokinetics and pharmacodynamics of available analog insulins and accuracy of CGM in extremes of blood glucose values. The iLet bionic pancreas, cleared by the US Food and Drug Administration (FDA) in May 2023, is an AID system that determines all therapeutic insulin doses for an individual on the basis of body weight, eliminating the need for calculation of basal rates, insulin to carbohydrate ratios, blood glucose corrections, and bolus dose. The control algorithms adapt continuously and autonomously to the individual’s insulin needs. 38 Table 5 lists available AID systems.

Schematic of closed loop insulin pump technology. The continuous glucose monitor senses interstitial glucose concentrations and sends the information via Bluetooth to a control algorithm hosted on an insulin pump (or smartphone). The algorithm calculates the amount of insulin required, and the insulin pump delivers rapid acting insulin subcutaneously
Comparison of commercially available hybrid closed loop systems 75
Unapproved systems
Do-it-yourself (DIY) closed loop systems—DIY open artificial pancreas systems—have been developed by people with type 1 diabetes with the goal of self-adjusting insulin by modifying their individually owned devices. 76 These systems are built by the individual using an open source code widely available to anyone with compatible medical devices who is willing and able to build their own system. DIY systems are used by several thousand people across the globe but are not approved by regulatory bodies; they are patient-driven and considered “off-label” use of technology with the patient assuming full responsibility for their use. Clinicians caring for these patients should ensure basic diabetes skills, including pump site maintenance, a knowledge of how the chosen system works, and knowing when to switch to “manual mode” for patients using an artificial pancreas system of any kind. 76 The small body of studies on DIY looping suggests improvement in HbA 1c , increased time in range, decreased hypoglycemia and glucose variability, improvement in night time blood glucose concentrations, and reduced mental burden of diabetes management. 77 78 79 Although actively prescribing or initiating these options is not recommended, these patients should be supported by clinical teams; insulin prescription should not be withheld, and, if initiated by the patient, unregulated DIY options should be openly discussed to ensure open and transparent relationships. 78
In January 2023, the US FDA cleared the Tidepool Loop app, a DIY AID system. This software will connect the CGM, insulin pump, and Loop algorithm, but no RCTs using this method are available.
β cell replacement therapies
For patients with type 1 diabetes who meet specific clinical criteria, β cell replacement therapy using whole pancreas or pancreatic islet transplantation can be considered. Benefits of transplantation include immediate cessation of insulin therapy, attainment of euglycemia, and avoidance of hypoglycemia. Additional benefits include improved quality of life and stabilization of complications. 80 Chronic immunosuppression is needed to prevent graft rejection after transplantation.
Pancreas transplantation
Whole pancreas transplantation, first performed in 1966, involves complex abdominal surgery and lifelong immunosuppressive therapy and is limited by organ donor availability. Today, pancreas transplants are usually performed simultaneously using two organs from the same donor (simultaneous pancreas-kidney transplant (SPKT)), sequentially if the candidate has a living donor for renal transplantation (pancreas after kidney transplant (PAKT)) or on its own (pancreas transplantation alone). Most whole pancreas transplants are performed with kidney transplantation for end stage diabetic kidney disease. Pancreas graft survival at five years after SPKT is 80% and is superior to that with pancreas transplants alone (62%) or PAKT (67%). 81 Studies from large centers where SPKT is performed show that recipients can expect metabolic improvements including amelioration of problematic hypoglycemia for at least five years. 81 The number of pancreas transplantations has steadily decreased in the past two decades.
Islet transplantation
Islet transplantation can be pursued in selected patients with type 1 diabetes marked by unawareness of hypoglycemia and severe hypoglycemic episodes, to help restore the α cell response critical for responding to hypoglycemia. 82 83 Islet transplantation involves donor pancreas procurement with subsequent steps to isolate, purify, culture, and infuse the islets. Multiple donors are needed to provide enough islet cells to overcome islet cell loss during transplantation. Survival of the islet grafts, limited donor supply, and lifelong need for immunosuppressant therapy remain some of the biggest challenges. 84 Islet transplantation remains experimental in the US and is offered in a few specialized centers in North America, some parts of Europe, and Australia. 85
Disease modifying treatments for β cell preservation
Therapies targeting T cells, B cells, and cytokines that find use in a variety of autoimmune diseases have also been applied to type 1 diabetes. The overarching goal of immune therapies in type 1 diabetes is to prevent or delay the loss of functional β cell mass. Studies thus far in early type 1 diabetes have not yet successfully shown reversal of loss of C peptide or maintenance of concentrations after diagnosis, although some have shown preservation or slowing of loss of β cells. This suggests that a critical time window of opportunity exists for starting treatment depending on the stage of type 1 diabetes ( fig 1 ).
Teplizumab is a humanized monoclonal antibody against the CD3 molecule on T cells; it is thought to modify CD8 positive T lymphocytes, key effector cells that mediate β cell death and preserves regulatory T cells. 86 Teplizumab, when administered to patients with new onset of type 1 diabetes, was unable to restore glycemia despite C peptide preservation. 87 However, in its phase II prevention study of early intervention in susceptible individuals (at least two positive autoantibodies and an abnormal oral glucose tolerance test at trial entry), a single course of teplizumab delayed progression to clinical type 1 diabetes by about two years ( table 2 ). 43 On the basis of these results, teplizumab received approval in the US for people at high risk of type 1 diabetes in November 2022. 88 A phase III trial (PROTECT; NCT03875729 ) to evaluate the efficacy and safety of teplizumab versus placebo in children and adolescents with new diagnosis of type 1 diabetes (within six weeks) is ongoing. 89
Thus far, targeting various components of the immune response has been attempted in early type 1 diabetes without any long term beneficial effects on C peptide preservation. Co-stimulation blockade using CTLA4-Ig abatacept, a fusion protein that interferes with co-stimulation needed in the early phases of T cell activation that occurs in type 1 diabetes, is being tested for efficacy in prevention of type 1 diabetes ( NCT01773707 ). 90 Similarly, several cytokine directed anti-inflammatory targets (interleukin 6 receptor, interleukin 1β, tumor necrosis factor ɑ) have not shown any benefit.
Non-immunomodulatory adjunctive therapies
Adjunctive therapies for type 1 diabetes have been long entertained owing to problems surrounding insulin delivery, adequacy of glycemic management, and side effects associated with insulin, especially weight gain and hypoglycemia. At least 50% of adults with type 1 diabetes are overweight or obese, presenting an unmet need for weight management in these people. Increased cardiovascular risk in these people despite good glycemic management presents additional challenges. Thus, use of adjuvant therapies may tackle these problems.
Metformin, by decreasing hepatic glucose production, could potentially decrease fasting glucose concentrations. 91 It has shown benefit in reducing insulin doses and possibly improving metabolic control in obese/overweight people with type 1 diabetes. A meta-analysis of 19 RCTs suggests short term improvement in HbA 1c that is not sustained after three months and is associated with higher incidence of gastrointestinal side effects. 92 No evidence shows that metformin decreases cardiovascular morbidity in type 1 diabetes. Therefore, owing to lack of conclusive benefit, addition of metformin to treatment regimens is not recommended in consensus guidelines.
Glucagon-like peptide receptor agonists
Endogenous GLP-1 is an incretin hormone secreted from intestinal L cells in response to nutrient ingestion and enhances glucose induced insulin secretion, suppresses glucagon secretion, delays gastric emptying, and induces satiety. 93 GLP-1 promotes β cell proliferation and inhibits apoptosis, leading to expansion of β cell mass. GLP-1 secretion in patients with type 1 diabetes is similar to that seen in people without diabetes. Early RCTs of liraglutide in type 1 diabetes resulted in weight loss and modest lowering of HbA 1c ( table 2 ). 49 50 Liraglutide 1.8 mg in people with type 1 diabetes and higher body mass index decreased HbA 1c , weight, and insulin requirements with no increased hypoglycemia risk. 94 However, on the basis of results from a study of weekly exenatide that showed similar results, these effects may not be sustained. 51 A meta-analysis of 24 studies including 3377 participants showed that the average HbA 1c decrease from GLP-1 receptor agonists compared with placebo was highest for liraglutide 1.8 mg daily (−0.28%, 95% confidence interval −0.38% to−0.19%) and exenatide (−0.17%, −0.28% to 0.02%). The estimated weight loss from GLP-1 receptor agonists compared with placebo was −4.89 (−5.33 to−4.45) kg for liraglutide 1.8 mg and −4.06 (−5.33 to−2.79) kg for exenatide. 95 No increase in severe hypoglycemia was seen (odds ratio 0.67, 0.43 to 1.04) but therapy was associated with higher levels of nausea. GLP-1 receptor agonist use may be beneficial for weight loss and reducing insulin doses in a subset of patients with type 1 diabetes. GLP-1 receptor agonists are not a recommended treatment option in type 1 diabetes. Semaglutide is being studied in type 1 diabetes in two clinical trials ( NCT05819138 ; NCT05822609 ).
Sodium-glucose cotransporter inhibitors
Sodium-glucose cotransporter 2 (SGLT-2), a protein expressed in the proximal convoluted tubule of the kidney, reabsorbs filtered glucose; its inhibition prevents glucose reabsorption in the tubule and increases glucose excretion by the kidney. Notably, the action of these agents is independent of insulin, so this class of drugs has potential as adjunctive therapy for type 1 diabetes. Clinical trials have shown significant benefit in cardiovascular and renal outcomes in type 2 diabetes; therefore, significant interest exists for use in type 1 diabetes. Several available SGLT-2 inhibitors have been studied in type 1 diabetes and have shown promising results with evidence of decreased total daily insulin dosage, improvement in HbA 1c , lower rates of hypoglycemia, and decrease in body weight; however, these effects do not seem to be sustained at one year in clinical trials and seem to wane with time. Despite beneficial effects, increased incidence of diabetic ketoacidosis has been observed in all trials, is a major concern, and is persistent despite educational efforts. 96 97 98 Low dose empagliflozin (2.5 mg) has shown lower rates of diabetic ketoacidosis in clinical trials ( table 2 ). 47 Favorable risk profiles have been noted in Japan, the only market where SGLT-2 inhibitors are approved for adjunctive use in type 1 diabetes. 99 In the US, SGLT-2 inhibitors are approved for use in type 2 diabetes only. In Europe, although dapagliflozin was approved for use as adjunct therapy to insulin in adults with type 1 diabetes, the manufacturer voluntarily withdrew the indication for the drug in 2021. 100 Sotagliflozin is a dual SGLT-1 and SGLT-2 inhibitor that decreases renal glucose reabsorption through systemic inhibition of SGLT-2 and decreases glucose absorption in the proximal intestine by SGLT-1 inhibition, blunting and delaying postprandial hyperglycemia. 101 Studies of sotagliflozin in type 1 diabetes have shown sustained HbA 1c reduction, weight loss, lower insulin requirements, lesser hypoglycemia, and more diabetic ketoacidosis relative to placebo. 102 103 104 The drug received authorization in the EU for use in type 1 diabetes, but it is not marketed there. Although SGLT inhibitors are efficacious in type 1 diabetes management, the risk of diabetic ketoacidosis is a major limitation to widespread use of these agents.
Updates in acute complications of type 1 diabetes
Diabetic ketoacidosis.
Diabetic ketoacidosis is a serious and potentially fatal hyperglycemic emergency accompanied by significant rates of mortality and morbidity as well as high financial burden for healthcare systems and societies. In the past decade, increasing rates of diabetic ketoacidosis in adults have been observed in the US and Europe. 105 106 This may be related to changes in the definition of diabetic ketoacidosis, use of medications associated with higher risk, and admission of patients at lower risk. 107 In a US report of hospital admissions with diabetic ketoacidosis, 53% of those admitted were between the ages of 18 and 44, with higher rates in men than in women. 108 Overall, although mortality from diabetic ketoacidosis in developed countries remains low, rates have risen in people aged >60 and in those with coexisting life threatening illnesses. 109 110 Recurrent diabetic ketoacidosis is associated with a substantial mortality rate. 111 Frequency of diabetic ketoacidosis increases with higher HbA 1c concentrations and with lower socioeconomic status. 112 Common precipitating factors include newly diagnosed type 1 diabetes, infection, poor adherence to insulin, and an acute cardiovascular event. 109
Euglycemic diabetic ketoacidosis refers to the clinical picture of an increased anion gap metabolic acidosis, ketonemia, or significant ketonuria in a person with diabetes without significant glucose elevation. This can be seen with concomitant use of SGLT-2 inhibitors (currently not indicated in type 1 diabetes), heavy alcohol use, cocaine use, pancreatitis, sepsis, and chronic liver disease and in pregnancy 113 Treatment is similar to that for hyperglycemic diabetic ketoacidosis but can require earlier use and greater concentrations of a dextrose containing fluid for the insulin infusion in addition to 0.9% normal saline resuscitation fluid. 114
The diagnosis of diabetic ketoacidosis has evolved from a gluco-centric diagnosis to one requiring hyperketonemia. By definition, independent of blood glucose, a β-hydroxybutyrate concentration >3 mmol/L is required for diagnosis. 115 However, the use of this ketone for assessment of the severity of the diabetic ketoacidosis is controversial. 116 Bedside β-hydroxybutyrate testing during treatment is standard of care in many parts of the world (such as the UK) but not others (such as the US). Concerns have been raised about accuracy of bedside β-hydroxybutyrate meters, but this is related to concentrations above the threshold for diabetic ketoacidosis. 116
Goals for management of diabetic ketoacidosis include restoration of circulatory volume, correction of electrolyte imbalances, and treatment of hyperglycemia. Intravenous regular insulin infusion is the standard of care for treatment worldwide owing to rapidity of onset of action and rapid resolution of ketonemia and hyperglycemia. As hypoglycemia and hypokalemia are more common during treatment, insulin doses are now recommended to be reduced from 0.1 u/kg/h to 0.05 u/kg/h when glucose concentrations drop below 250 mg/dL or 14 mM. 115 Subcutaneous rapid acting insulin protocols have emerged as alternative treatments for mild to moderate diabetic ketoacidosis. 117 Such regimens seem to be safe and have the advantages of not requiring admission to intensive care, having lower rates of complications related to intravenous therapy, and requiring fewer resources. 117 118 Ketonemia and acidosis resolve within 24 hours in most people. 115 To prevent rebound hyperglycemia, the transition off an intravenous insulin drip must overlap subcutaneous insulin by at least two to four hours. 115
Hypoglycemia
Hypoglycemia, a common occurrence in people with type 1 diabetes, is a well appreciated effect of insulin treatment and occurs when blood glucose falls below the normal range. Increased susceptibility to hypoglycemia from exogenous insulin use in people with type 1 diabetes results from multiple factors, including imperfect subcutaneous insulin delivery tools, loss of glucagon within a few years of diagnosis, progressive impairment of the sympatho-adrenal response with repeated hypoglycemic episodes, and eventual development of impaired awareness. In 2017 the International Hypoglycemia Study Group developed guidance for definitions of hypoglycemia; on the basis of this, a glucose concentration of 3.0-3.9 mmol/L (54-70 mg/dL) was designated as level 1 hypoglycemia, signifying impending development of level 2 hypoglycemia—a glucose concentration <3 mmol/L (54 mg/dL). 119 120 At approximately 54 mg/dL, neuroglycopenic hypoglycemia symptoms, including vision and behavior changes, seizures, and loss of consciousness, begin to occur as a result of glucose deprivation of neurons in the central nervous system. This can eventually lead to cerebral dysfunction at concentrations <50 mg/dL. 121 Severe hypoglycemia (level 3), denoting severe cognitive and/or physical impairment and needing external assistance for recovery, is a common reason for emergency department visits and is more likely to occur in people with lower socioeconomic status and with the longest duration of diabetes. 112 Prevalence of self-reported severe hypoglycemia is very high according to a global population study that included more than 8000 people with type 1 diabetes. 122 Severe hypoglycemia occurred commonly in younger people with suboptimal glycemia according to a large electronic health record database study in the US. 123 Self- reported severe hypoglycemia is associated with a 3.4-fold increase in mortality. 124 125
Acute consequences of hypoglycemia include impaired cognitive function, temporary focal deficits including stroke-like symptoms, and memory deficits. 126 Cardiovascular effects including tachycardia, arrhythmias, QT prolongation, and bradycardia can occur. 127 Hypoglycemia can impair many activities of daily living, including motor vehicle safety. 128 In a survey of adults with type 1 diabetes who drive a vehicle at least once a week, 72% of respondents reported having hypoglycemia while driving, with around 5% reporting a motor vehicle accident due to hypoglycemia in the previous two years. 129 This contributes to the stress and fear that many patients face while grappling with the difficulties of ongoing hypoglycemia. 130
Glucagon is highly efficacious for the primary treatment of severe hypoglycemia when a patient is unable to ingest carbohydrate safely, but it is unfortunately under-prescribed and underused. 131 132 Availability of nasal, ready to inject, and shelf-stable liquid glucagon formulations have superseded the need for reconstituting older injectable glucagon preparations before administration and are now preferred. 133 134 Real time CGM studies have shown a decreased hypoglycemic exposure in people with impaired awareness without a change in HbA 1c . 34 135 136 137 138 CGM has shown benefit in decreasing hypoglycemia across the lifespan, including in teens, young adults, and older people. 36 139 Although CGM reduces the burden of hypoglycemia including severe hypoglycemia, it does not eliminate it; overall, such severe level 3 hypoglycemia rates in clinical trials are very low and hard to decipher in the real world. HCL insulin delivery systems integrated with CGM have been shown to decrease hypoglycemia. Among available rapid acting insulins, ultra-rapid acting lispro (lispro-aabc) seems to be associated with less frequent hypoglycemia in type 1 diabetes. 140 141
As prevention of hypoglycemia is a crucial aspect of diabetes management, formal training programs to increase awareness and education on avoidance of hypoglycemia, such as the UK’s Dose Adjustment for Normal Eating (DAFNE), have been developed. 142 143 This program has shown fewer severe hypoglycemia (mean 1.7 (standard deviation 8.5) episodes per person per year before training to 0.6 (3.7) episodes one year after training) and restoration of recognition of hypoglycemia in 43% of people reporting unawareness. Clinically relevant anxiety and depression fell from 24.4% to 18.0% and from 20.9% to 15.5%, respectively. A structured education program with cognitive and psychotherapeutic aspects for changing hypoglycemia related behaviors, called the Hypoglycemia Awareness Restoration Program despite optimized self-care (HARPdoc), showed a positive effect on changing unhelpful beliefs around hypoglycemia and improved diabetes related and general distress and anxiety scores. 144
Management in under-resourced settings
According to a recent estimate from the International Diabetes Federation, 1.8 million people with type 1 diabetes live in low and middle income countries (LMICs). 2 In many LMICs, the actual burden of type 1 diabetes remains unknown and material resources needed to manage type 1 diabetes are lacking. 145 146 Health systems in these settings are underequipped to tackle the complex chronic disease that is type 1 diabetes. Few diabetes and endocrinology specialist physicians are available owing to lack of specific postgraduate training programs in many LMICs; general practitioners with little to no clinical experience in managing type 1 diabetes care for these patients. 146 This, along with poor availability and affordability of insulin and lack of access to technology, results in high mortality rates. 147 148 149 In developed nations, low socioeconomic status is associated with higher levels of mortality and morbidity for adults with type 1 diabetes despite access to a universal healthcare system. 150 Although global governments have committed to universal health coverage and therefore widespread availability of insulin, it remains very far from realization in most LMICs. 151
Access to technology is patchy and varies globally. In the UST1DX, CGM use was least in the lowest fifth of socioeconomic status. 152 Even where technology is available, successful engagement does not always occur. 153 In a US cohort, lower CGM use was seen in non-Hispanic Black children owing to lower rates of device initiation and higher rates of discontinuation. 154 In many LMICs, blood glucose testing strips are not readily available and cost more than insulin. 151 In resource limited settings, where even diagnosis, basic treatments including insulin, syringes, and diabetes education are limited, use of CGM adds additional burden to patients. Need for support services and the time/resources needed to download and interpret data are limiting factors from a clinician’s perspective. Current rates of CGM use in many LMICs are unknown.
Inequities in the availability of and access to certain insulin formulations continue to plague diabetes care. 155 In developed countries such as the US, rising costs have led to insulin rationing by around 25% of people with type 1 diabetes. 156 LMICs have similar trends while also remaining burdened by disproportionate mortality and complications from type 1 diabetes. 155 157 With the inclusion of long acting insulin analogs in the World Health Organization’s Model List of Essential Medicines in 2021, hope has arisen that these will be included as standard of care across the world. 158 In the past, the pricing of long acting analogs has limited their use in resource poor settings 159 ; however, their inclusion in WHO’s list was a major step in improving their affordability. 158 With the introduction of lower cost long acting insulin biosimilars, improved access to these worldwide in the future can be anticipated. 160
Making insulin available is not enough on its own to improve the prognosis for patients with diabetes in resource poor settings. 161 Improved healthcare infrastructure, better availability of diabetes supplies, and trained personnel are all critical to improving type 1 diabetes care in LMICs. 161 Despite awareness of limitations and barriers, a clear understanding of how to implement management strategies in these settings is still lacking. The Global Diabetes Compact was launched in 2021 with the goal of increasing access to treatment and improving outcomes for people with diabetes across the globe. 162
Emerging technologies and treatments
Monitoring systems.
The ability to measure urinary or more recently blood ketone concentrations is an integral part of self-management of type 1 diabetes, especially during acute illness, intermittent fasting, and religious fasts to prevent diabetic ketoacidosis. 163 Many people with type 1 diabetes do not adhere to urine or blood ketone testing, which likely results in unnecessary episodes of diabetic ketoacidosis. 164 Noting that blood and urine ketone testing is not widely available in all countries and settings is important. 1 Regular assessment of patients’ access to ketone testing (blood or urine) is critical for all clinicians. Euglycemic diabetic ketoacidosis in type 1 diabetes is a particular problem with concomitant use of SGLT-2 inhibitors; for this reason, these agents are not approved for use in these patients. For sick day management (and possibly for the future use of SGLT-2 inhibitors in people with type 1 diabetes), it is hoped that continuous ketone monitoring (CKM) can mitigate the risks of diabetic ketoacidosis. 165 Like CGM, the initial CKM device measures interstitial fluid β-hydroxybutyrate instead of glucose. CKM use becomes important in conjunction with a hybrid closed loop insulin pump system and added SGLT-2 inhibitor therapy, where insulin interruptions are common and hyperketonemia is frequent. 166
Perhaps the greatest technological challenge to date has been the development of non-invasive glucose monitoring. Numerous attempts have been made using strategies including optics, microwave, and electrochemistry. 167 Lack of success to date has resulted in healthy skepticism from the medical community. 168 However, active interest in the development of non-invasive technology with either interstitial or blood glucose remains.
Insulin and delivery systems
In the immediate future, two weekly basal insulins, insulin icodec and basal insulin Fc, may become available. 169 Studies of insulin icodec in type 1 diabetes are ongoing (ONWARDS 6; NCT04848480 ). How these insulins will be incorporated in management of type 1 diabetes is not yet clear.
Currently available AID systems use only a single hormone, insulin. Dual hormone AID systems incorporating glucagon are in development. 170 171 Barriers to the use of dual hormone systems include the need for a second chamber in the pump, a lack of stable glucagon formulations approved for long term subcutaneous delivery, lack of demonstrated long term safety, and gastrointestinal side effects from glucagon use. 74 Similarly, co-formulations of insulin and amylin (a hormone co-secreted with insulin and deficient in people with type 1 diabetes) are in development. 172
Immunotherapy for type 1 diabetes
As our understanding of the immunology of type 1 diabetes expands, development of the next generation of immunotherapies is under active pursuit. Antigen specific therapies, peptide immunotherapy, immune tolerance using DNA vaccination, and regulatory T cell based adoptive transfer targeting β cell senescence are all future opportunities for drug development. Combining immunotherapies with metabolic therapies such as GLP-1 receptor agonists to help to improve β cell mass is being actively investigated.
The quest for β cell replacement methods is ongoing. Transplantation of stem cell derived islets offers promise for personalized regenerative therapies as a potentially curative method that does away with the need for donor tissue. Since the first in vivo model of glucose responsive β cells derived from human embryonic stem cells, 173 different approaches have been attempted. Mesenchymal stromal cell treatment and autologous hematopoietic stem cells in newly diagnosed type 1 diabetes may preserve β cell function without any safety signals. 174 175 176 Stem cell transplantation for type 1 diabetes remains investigational. Encapsulation, in which β cells are protected using a physical barrier to prevent immune attack and avoid lifelong immunosuppression, and gene therapy techniques using CRISPR technology also remain in early stages of investigation.
Until recently, no specific guidelines for management of type 1 diabetes existed and management guidance was combined with consensus statements developed for type 2 diabetes. Table 6 summarizes available guidance and statements from various societies. A consensus report for management of type 1 diabetes in adults by the ADA and European Association for the Study of Diabetes became available in 2021; it covers several topics of diagnosis and management of type 1 diabetes, including glucose monitoring, insulin therapy, and acute complications. Similarly, the National Institute for Health and Care Excellence also offers guidance on management of various aspects of type 1 diabetes. Consensus statements for use of CGM, insulin pump, and AID systems are also available.
Guidelines in type 1 diabetes
Conclusions
Type 1 diabetes is a complex chronic condition with increasing worldwide prevalence affecting several million people. Several successes in management of type 1 diabetes have occurred over the years from the serendipitous discovery of insulin in 1921 to blood glucose monitoring, insulin pumps, transplantation, and immunomodulation. The past two decades have seen advancements in diagnosis, treatment, and technology including development of analog insulins, CGM, and advanced insulin delivery systems. Although we have gained a broad understanding on many important aspects of type 1 diabetes, gaps still exist. Pivotal research continues targeting immune targets to prevent or delay onset of type 1 diabetes. Although insulin is likely the oldest of existing modern drugs, no low priced generic supply of insulin exists anywhere in the world. Management of type 1 diabetes in under resourced areas continues to be a multifaceted problem with social, cultural, and political barriers.
Glossary of abbreviations
ADA—American Diabetes Association
AID—automated insulin delivery
BGM—blood glucose monitoring
CGM—continuous glucose monitoring
CKM—continuous ketone monitoring
DCCT—Diabetes Control and Complications Trial
DIY—do-it-yourself
FDA—Food and Drug Administration
GADA—glutamic acid decarboxylase antibody
GLP-1—glucagon-like peptide 1
GRS—genetic risk scoring
HbA1c—glycated hemoglobin
HCL—hybrid closed loop
LADA—latent autoimmune diabetes of adults
LMIC—low and middle income country
PAKT—pancreas after kidney transplant
RCT—randomized controlled trial
SGLT-2—sodium-glucose cotransporter 2
SPKT—simultaneous pancreas-kidney transplant
Questions for future research
What future new technologies can be helpful in management of type 1 diabetes?
How can newer insulin delivery methods benefit people with type 1 diabetes?
What is the role of disease modifying treatments in prevention and delay of type 1 diabetes?
Is there a role for sodium-glucose co-transporter inhibitors or glucagon-like peptide 1 receptor angonists in the management of type 1 diabetes?
As the population with type 1 diabetes ages, how should management of these people be tailored?
How can we better serve people with type 1 diabetes who live in under-resourced settings with limited access to medications and technology?
How patients were involved in the creation of this manuscript
A person with lived experience of type 1 diabetes reviewed a draft of the manuscript and offered input on important aspects of their experience that should be included. This person is involved in large scale education and activism around type 1 diabetes. They offered their views on various aspects of type 1 diabetes, especially the use of adjuvant therapies and the burden of living with diabetes. This person also raised the importance of education of general practitioners on the various stages of type 1 diabetes and the management aspects. On the basis of this feedback, we have highlighted the burden of living with diabetes on a daily basis.
Series explanation: State of the Art Reviews are commissioned on the basis of their relevance to academics and specialists in the US and internationally. For this reason they are written predominantly by US authors
Contributors: SS and IBH contributed to the planning, drafting, and critical review of this manuscript. FNK contributed to the drafting of portions of the manuscript. All three authors are responsible for the overall content as guarantors.
Competing interests: We have read and understood the BMJ policy on declaration of interests and declare the following interests: SS has received an honorarium from Abbott Diabetes Care; IBH has received honorariums from Abbott Diabetes Care, Lifescan, embecta, and Hagar and research support from Dexcom and Insulet.
Provenance and peer review: Commissioned; externally peer reviewed.
- DeVries JH ,
- Hess-Fischl A ,
- Gregory GA ,
- Robinson TIG ,
- Linklater SE ,
- International Diabetes Federation Diabetes Atlas Type 1 Diabetes in Adults Special Interest Group
- Harding JL ,
- Wander PL ,
- Dabelea D ,
- Mayer-Davis EJ ,
- SEARCH for Diabetes in Youth Study
- Lawrence JM ,
- SEARCH for Diabetes in Youth Study Group
- Fazeli Farsani S ,
- Souverein PC ,
- van der Vorst MM ,
- Sutherland J ,
- Rokszin G ,
- Stahl-Pehe A ,
- Kamrath C ,
- Atkinson MA ,
- Bingley PJ ,
- Bonifacio E ,
- Leslie RD ,
- Evans-Molina C ,
- Freund-Brown J ,
- Thomas NJ ,
- Zimmet PZ ,
- Rowley MJ ,
- Knowles W ,
- Fourlanos S ,
- Greenbaum CJ ,
- ElSayed NA ,
- American Diabetes Association
- Miller RG ,
- Secrest AM ,
- Sharma RK ,
- Songer TJ ,
- McDonald T ,
- Greenfield JR
- Tridgell DM ,
- Spiekerman C ,
- Greenbaum CJ
- Glessner J ,
- Foster NC ,
- Miller KM ,
- Becker DJ ,
- Khawandanah J
- Pedrosa MR ,
- Franco DR ,
- Gieremek HW ,
- Nathan DM ,
- Diabetes Control and Complications Trial Research Group
- Klonoff DC ,
- Parkes JL ,
- Kovatchev BP ,
- Raghinaru D ,
- iDCL Trial Research Group
- Riddlesworth T ,
- DIAMOND Study Group
- Leelarathna L ,
- Neupane S ,
- FLASH-UK Trial Study Group
- Polonsky W ,
- Hirsch IB ,
- Pratley RE ,
- Kanapka LG ,
- Rickels MR ,
- Wireless Innovation for Seniors With Diabetes Mellitus (WISDM) Study Group
- Tauschmann M ,
- APCam11 Consortium
- Russell SJ ,
- Damiano ER ,
- Bionic Pancreas Research Group
- Bailey TS ,
- Group Information ,
- Bergenstal RM ,
- Dellva MA ,
- Mathieu C ,
- Herold KC ,
- Type 1 Diabetes TrialNet Study Group
- Libman IM ,
- DiMeglio LA ,
- T1D Exchange Clinic Network Metformin RCT Study Group
- Petrie JR ,
- Chaturvedi N ,
- REMOVAL Study Group
- Dandona P ,
- Phillip M ,
- DEPICT-1 Investigators
- Rosenstock J ,
- Marquard J ,
- Laffel LM ,
- Hemmingsson JU ,
- ADJUNCT ONE Investigators
- Pieber TR ,
- ADJUNCT TWO Investigators
- Reynolds J ,
- Battelino T ,
- Liljenquist D ,
- Becker RH ,
- Bergmann K ,
- Lehmann A ,
- Cheng AYY ,
- Stender-Petersen K ,
- Hövelmann U ,
- Carlson AL ,
- Komatsu M ,
- Coutant DE ,
- Stamati A ,
- Karagiannis T ,
- Christoforidis A
- Heinemann L ,
- Baughman R ,
- Akturk HK ,
- Snell-Bergeon JK ,
- Prabhu JN ,
- Seyed Ahmadi S ,
- Westman K ,
- Pivodic A ,
- Hermann JM ,
- Freiberg C ,
- DPV Initiative
- Dicembrini I ,
- Cosentino C ,
- Mannucci E ,
- Abelseth J ,
- Karageorgiou V ,
- Papaioannou TG ,
- Weisman A ,
- Cardinez M ,
- Kramer CK ,
- Asarani NAM ,
- Reynolds AN ,
- Elbalshy M ,
- Jennings P ,
- Burnside MJ ,
- Williman JA ,
- Fridell JA ,
- Stratta RJ ,
- Gruessner AC
- Robertson RP
- Shapiro AM ,
- Pepper AR ,
- Shapiro AMJ
- Walker JT ,
- Saunders DC ,
- Brissova M ,
- Gitelman SE ,
- Bluestone JA
- Hagopian W ,
- Ferry RJ Jr . ,
- Protégé Trial Investigators
- von Scholten BJ ,
- Kreiner FF ,
- Gough SCL ,
- von Herrath M
- Type 1 Diabetes TrialNet Abatacept Study Group
- Hardie DG ,
- Dejgaard TF ,
- Christiansen E ,
- ADJUNCT ONE and ADJUNCT TWO Investigators
- Yunasan E ,
- Peters AL ,
- Palanca A ,
- van Nes F ,
- Ampudia Blasco FJ ,
- Dobbins RL ,
- Greenway FL ,
- Zambrowicz BP ,
- Brodovicz K ,
- Soleymanlou N ,
- Wissinger E ,
- Juhaeri J ,
- Mayer-Davis EJ
- Dhatariya KK ,
- Glaser NS ,
- Umpierrez GE
- Ramphul K ,
- Umpierrez G ,
- Korytkowski M
- Weinstock RS ,
- T1D Exchange Clinic Network
- Eshkoli T ,
- Brandstaetter E ,
- Jotkowitz A
- Dhatariya KK
- Joint British Diabetes Societies for Inpatient Care
- Kilpatrick ES ,
- Butler AE ,
- Ostlundh L ,
- Koufakis T ,
- Agiostratidou G ,
- International Hypoglycaemia Study Group
- van de Ven KC ,
- Heerschap A ,
- van der Graaf M ,
- de Galan BE
- Alsifri S ,
- Aronson R ,
- HAT Investigator Group
- Pettus JH ,
- Shepherd L ,
- Van Houten HK ,
- Ziegenfuss JY ,
- Wermers RA ,
- Schernthaner G ,
- Anderson J ,
- Saunders AL ,
- Snell-Bergeon J ,
- Forlenza GP ,
- Bispham J ,
- Gabbay RA ,
- Pontiroli AE ,
- Tagliabue E
- T1D Exchange Intranasal Glucagon Investigators
- Freckmann G ,
- Ehrmann D ,
- El Laboudi A ,
- Spanudakis E ,
- Anantharaja S ,
- Peleckis AJ ,
- Dalton-Bakes C ,
- van Beers CA ,
- Kleijer SJ ,
- CGM Intervention in Teens and Young Adults with T1D (CITY) Study Group ,
- Piras de Oliveira C ,
- Ribeiro A ,
- Chigutsa F ,
- Malecki MT ,
- Hopkins D ,
- Lawrence I ,
- Mansell P ,
- Stanton-Fay SH ,
- Hamilton K ,
- Chadwick PM ,
- DAFNEplus study group
- Goldsmith K ,
- Yudkin JS ,
- Buntinx F ,
- Mapatano MA ,
- De Clerck M ,
- Truyers C ,
- Chambers D ,
- O’Cathain A
- Klatman EL ,
- Auzanneau M ,
- Tanenbaum ML ,
- Iturralde E ,
- Lipman TH ,
- Bhutta ZA ,
- Pfiester E ,
- Thieffry A ,
- Ballhausen H ,
- Gajewska KA ,
- O’Donnell S
- Wareham NJ ,
- Joosse HJ ,
- Raposo JF ,
- de Courten M
- Hemmingsen B ,
- Abouhassan T ,
- Albanese-O’Neill A ,
- Jacobsen L ,
- Haller MJ ,
- Castorino K ,
- Lovblom LE ,
- Cardinez N ,
- Nguyen KT ,
- Andersen G ,
- Meiffren G ,
- Famulla S ,
- Castellanos LE ,
- Balliro CA ,
- Sherwood JS ,
- Tsoukas MA ,
- Bernier-Twardy S ,
- Martinson LA ,
- Carlsson PO ,
- Schwarcz E ,
- Korsgren O ,
- Oliveira MC ,
- Stracieri AB ,
- Buzzetti R ,
- Mauricio D ,
- McGibbon A ,
- Ingersoll K ,
- Tugwell B ,
- Diabetes Canada Clinical Practice Guidelines Expert Committee
- Fleming GA ,
- McCall AL ,
- Gianchandani R ,
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Entire Site
- Research & Funding
- Health Information
- About NIDDK
- Research Programs & Contacts
Clinical Research in Type 1 Diabetes
Determinants, etiology, progression, prevention, and treatment of Type 1 Diabetes in children and adults.
The Clinical Research in Type 1 Diabetes program includes studies across the lifespan that address the etiology, pathogenesis, prevention and treatment (medical- and self-management) of type 1 diabetes in youth and adults. The program also supports research on hypoglycemia in T1D, including clinical studies and basic research using healthy individuals to understand the physiologic mechanisms of hypoglycemia. The program includes investigator-initiated clinical or behavioral studies, large, multi-center clinical trials that are conducted under cooperative agreements or contracts, and secondary analyses of ongoing clinical trials in diabetes and endocrinology.
NIDDK Program Staff
- Beena Akolkar, Ph.D. Clinical research in the prevention and immunopathogenesis of Type 1 Diabetes and the genetics and genomics of Type 1 and Type 2 Diabetes
- Guillermo A. Arreaza-Rubín, M.D. Diabetes and endocrine disease bioengineering and glucose sensing
- Miranda Broadney, M.D., M.P.H. Pediatrics, Pediatric Endocrinology, Clinical Management of Diabetes Mellitus, Insulin Resistance, Pediatric Obesity
- Maureen Monaghan Center, Ph.D., CDCES Health Psychology, Behavioral Science, Clinical Management of Diabetes
- Ellen Leschek, M.D. Type 1 and type 2 diabetes clinical research
- Hanyu Liang, M.D., Ph.D. Hepatic Metabolism; Insulin Resistance; Type 2 Diabetes; Obesity; Bariatric Surgery
- Lisa M. Spain, Ph.D. Disease-modifying clinical trials in type 1 diabetes, etiology and pathogenesis of type 1 diabetes
- Theresa Teslovich Woo, Ph.D. Human behavior, developmental cognitive neuroscience, and brain-based mechanisms involved in obesity and diabetes
Recent Funding Opportunities
Research resource for human organs and tissues (u42 clinical trial not allowed), notice of special interest (nosi): analysis of existing linked datasets to understand the relationship between housing program participation and risk for chronic diseases and other conditions (r01-clinical trial not allowed), limited competition for the continuation of type 1 diabetes in acute pancreatitis consortium - clinical centers (t1dapc-ccs) (u01 clinical trial optional), single source for the continuation of the type 1 diabetes in acute pancreatitis consortium - data coordinating center (t1dapc-dcc) (u01 clinical trial optional), notice of special interest (nosi): heal initiative: development and translation of diagnostic and therapeutic devices via blueprint medtech, related links.
View related clinical trials from ClinicalTrials.gov.
Study sections conduct initial peer review of applications in a designated scientific area. Visit the NIH’s Center for Scientific Review website to search for study sections.
Research Resources
NIDDK makes publicly supported resources, data sets, and studies available to researchers to accelerate the rate and lower the cost of new discoveries.
- Ancillary Studies to Major Ongoing Clinical Studies to extend our knowledge of the diseases being studied by the parent study investigators under a defined protocol or to study diseases and conditions not within the original scope of the parent study but within the mission of the NIDDK.
- NIDDK Central Repository for access to clinical resources including data and biospecimens from NIDDK-funded studies.
- NIDDK Information Network (dkNET) for simultaneous search of digital resources, including multiple datasets and biomedical resources relevant to the mission of the NIDDK.
Additional Research Programs
Research training.
NIDDK supports the training and career development of medical and graduate students, postdoctoral fellows, and physician scientists through institutional and individual grants.
Diversity Programs
The NIDDK offers and participates in a variety of opportunities for trainees and researchers from communities underrepresented in the biomedical research enterprise. These opportunities include travel and scholarship awards, research supplements, small clinical grants, high school and undergraduate programs, and a network of minority health research investigators.
Small Business
Small business programs.
NIDDK participates in the Small Business Innovation Research (SBIR) and Small Business Technology Transfer (STTR) programs. These programs support innovative research conducted by small businesses that has the potential for commercialization.
Human Subjects Research
NIDDK provides funding for pivotal clinical research, from preliminary clinical feasibility to large multi-center studies.
Translational Research
NIDDK provides funding opportunities and resources to encourage translation of basic discoveries into novel therapeutics.
Meetings & Workshops

Oct. 24 - 25, 2024 Miami, FL

Supports researchers with tools to enhance scientific rigor, reproducibility, and transparency, and provides a big data knowledge base for genomic and pathway hypothesis generation.

Providing education and training for the next generation of biomedical and behavioral scientist

Learn about current projects and view funding opportunities sponsored by the NIH Common Fund .
Registration is required at eRA Commons and grants.gov and can take 4 weeks.
- Biochemistry and Molecular Biology
- Biostatistics
- Environmental Health and Engineering
- Epidemiology
- Health Policy and Management
- Health, Behavior and Society
- International Health
- Mental Health
- Molecular Microbiology and Immunology
- Population, Family and Reproductive Health
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Research Gaps Around Type 1 Diabetes
A large body of research on Type 2 diabetes has helped to develop guidance, informing how patients are diagnosed, treated, and manage their lifestyle. In contrast, Type 1 diabetes, often mistakenly associated only with childhood, has received less attention.
In this Q&A, adapted from the April 17 episode of Public Health On Call , Stephanie Desmon speaks to Johns Hopkins epidemiologists Elizabeth Selvin , PhD '04, MPH, and Michael Fang , PhD, professor and assistant professor, respectively, in the Department of Epidemiology, about recent findings that challenge common beliefs about type 1 diabetes. Their conversation touches on the misconception that it’s solely a childhood condition, the rise of adult-onset cases linked to obesity, and the necessity for tailored approaches to diagnosis and care. They also discuss insulin prices and why further research is needed on medications like Ozempic in treating Type 1 diabetes.
I want to hear about some of your research that challenges what we have long understood about Type 1 diabetes, which is no longer called childhood diabetes.
MF: Type 1 diabetes was called juvenile diabetes for the longest time, and it was thought to be a disease that had a childhood onset. When diabetes occurred in adulthood it would be type 2 diabetes. But it turns out that approximately half of the cases of Type 1 diabetes may occur during adulthood right past the age of 20 or past the age of 30.
The limitations of these initial studies are that they've been in small clinics or one health system. So, it's unclear whether it's just that particular clinic or whether it applies to the general population more broadly.
We were fortunate because the CDC has collected new data that explores Type 1 diabetes in the U.S. Some of the questions they included in their national data were, “Do you have diabetes? If you do, do you have Type 1 or Type 2? And, at what age were you diagnosed?”
With these pieces of information, we were able to characterize how the age of diagnosis of Type 1 diabetes differs in the entire U.S. population.
Are Type 1 and Type 2 diabetes different diseases?
ES: They are very different diseases and have a very different burden. My whole career I have been a Type 2 diabetes epidemiologist, and I’ve been very excited to expand work with Type 1 diabetes.
There are about 1.5 million adults with Type 1 diabetes in the U.S., compared to 21 million adults with Type 2 diabetes. In terms of the total cases of diabetes, only 5 to 10 percent have Type 1 diabetes. Even in our largest epidemiologic cohorts, only a small percentage of people have Type 1 diabetes. So, we just don't have the same national data, the same epidemiologic evidence for Type 1 diabetes that we have for Type 2. The focus of our research has been trying to understand and characterize the general epidemiology and the population burden of Type 1 diabetes.
What is it about Type 1 that makes it so hard to diagnose?
MF: The presentation of symptoms varies by age of diagnosis. When it occurs in children, it tends to have a very acute presentation and the diagnosis is easier to make. When it happens in adulthood, the symptoms are often milder and it’s often misconstrued as Type 2 diabetes.
Some studies have suggested that when Type 1 diabetes occurs in adulthood, about 40% of those cases are misdiagnosed initially as Type 2 cases. Understanding how often people get diagnosed later in life is important to correctly diagnose and treat patients.
Can you talk about the different treatments?
MF: Patients with Type 1 diabetes are going to require insulin. Type 2 diabetes patients can require insulin, but that often occurs later in the disease, as oral medications become less and less effective.
ES: Because of the epidemic of overweight and obese in the general population, we’re seeing a lot of people with Type 1 diabetes who are overweight and have obesity. This can contribute to issues around misdiagnosis because people with Type 1 diabetes will have signs and will present similarly to Type 2 diabetes. They'll have insulin resistance potentially as a result of weight gain metabolic syndrome. Some people call it double diabetes—I don't like that term—but it’s this idea that if you have Type 1 diabetes, you can also have characteristics of Type 2 diabetes as well.
I understand that Type 1 used to be considered a thin person's disease, but that’s not the case anymore. MF: In a separate paper, we also explored the issue of overweight and obesity in persons with Type 1 diabetes. We found that approximately 62% of adults with Type 1 diabetes were either overweight or obese, which is comparable to the general U.S. population.
But an important disclaimer is that weight management in this population [with Type 1 diabetes] is very different. They can't just decide to go on a diet, start jogging, or engage in rigorous exercise. It can be a very, very dangerous thing to do.
Everybody's talking about Ozempic and Mounjaro—the GLP-1 drugs—for diabetes or people who are overweight to lose weight and to solve their diabetes. Where does that fit in with this population?
ES: These medications are used to treat Type 2 diabetes in the setting of obesity. Ozempic and Mounjaro are incretin hormones. They mediate satiation, reduce appetite, slow gastric emptying, and lower energy intake. They're really powerful drugs that may be helpful in Type 1 diabetes, but they're not approved for the management of obesity and Type 1 diabetes. At the moment, there aren't data to help guide their use in people with Type 1 diabetes, but I suspect they're going to be increasingly used in people with Type 1 diabetes.
MF: The other piece of managing weight—and it's thought to be foundational for Type 1 or Type 2—is dieting and exercising. However, there isn’t good guidance on how to do this in persons with Type 1 diabetes, whereas there are large and rigorous trials in Type 2 patients. We’re really just starting to figure out how to safely and effectively manage weight with lifestyle changes for Type 1 diabetics, and I think that's an important area of research that should continue moving forward.
ES: Weight management in Type 1 diabetes is complicated by insulin use and the risk of hypoglycemia, or your glucose going too low, which can be an acute complication of exercise. In people with Type 2 diabetes, we have a strong evidence base for what works. We know modest weight loss can help prevent the progression and development of Type 2 diabetes, as well as weight gain. In Type 1, we just don't have that evidence base.
Is there a concern about misdiagnosis and mistreatment? Is it possible to think a patient has Type 2 but they actually have Type 1?
MF: I think so. Insulin is the overriding concern. In the obesity paper, we looked at the percentage of people who said their doctors recommended engaging in more exercise and dieting. We found that people with Type 1 diabetes were less likely to receive the same guidance from their doctor. I think providers may be hesitant to say, “Look, just go engage in an active lifestyle.”
This is why it's important to have those studies and have that guidance so that patients and providers can be comfortable in improving lifestyle management.
Where is this research going next?
ES: What's clear from these studies is that the burden of overweight and obesity is substantial in people with Type 1 diabetes and it's not adequately managed. Going forward, I think we're going to need clinical trials, clear clinical guidelines, and patient education that addresses how best to tackle obesity in the setting of Type 1 diabetes.
It must be confusing for people with Type 1 diabetes who are hearing about people losing all this weight on these drugs, but they go to their doctor who says, “Yeah, but that's not for you.”
ES: I hope it's being handled more sensitively. These drugs are being used by all sorts of people for whom they are not indicated, and I'm sure that people with Type 1 diabetes are accessing these drugs. I think the question is, are there real safety issues? We need thoughtful discussion about this and some real evidence to make sure that we're doing more good than harm.
MF: Dr. Selvin’s group has published a paper, estimating that about 15% of people with Type 1 diabetes are on a GLP-1. But we don't have great data on what potentially can happen to individuals.
The other big part of diabetes that we hear a lot about is insulin and its price. Can you talk about your research on this topic?
MF: There was a survey that asked, “Has there been a point during the year when you were not using insulin because you couldn’t afford it?” About 20% of adults under the age of 65 said that at some point during the year, they couldn't afford their insulin and that they did engage in what sometimes is called “cost-saving rationing” [of insulin].
Medicare is now covering cheaper insulin for those over 65, but there are a lot of people for whom affordability is an issue. Can you talk more about that?
MF: The fight is not over. Just because there are national and state policies, and now manufacturers have been implementing price caps, doesn't necessarily mean that the people who need insulin the most are now able to afford it.
A recent study in the Annals of Internal Medicine looked at states that adopted or implemented out-of-pocket cost caps for insulin versus those that didn't and how that affected insulin use over time. They found that people were paying less for insulin, but the use of insulin didn't change over time. The $35 cap is an improvement, but we need to do more.
ES: There are still a lot of formulations of insulin that are very expensive. $35 a month is not cheap for someone who is on insulin for the rest of their lives.
RELATED:
- Overweight and Obesity in People With Type 1 Diabetes Nearly Same as General Population
- The Impacts of COVID-19 on Diabetes and Insulin
- Why Eli Lilly’s Insulin Price Cap Announcement Matters
Related Content

The Current and Future Outlook for Primary Health Care in South Asia

New Report Highlights U.S. 2022 Gun-Related Deaths: Firearms Remain Leading Cause of Death for Children and Teens, and Disproportionately Affect People of Color

What is Public Mental Health?

Study Estimates Home Blood Pressure Devices Don’t Fit Properly for More than 17 Million U.S. Adults
A ‘Critical Pathogen’: The Rise of Drug-Resistant Fungal Diseases
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
September 18, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Bacterial infections could be trigger for type 1 diabetes, new research suggests
by Cardiff University

For the first time, scientists have found that proteins from bacteria can trigger the immune system to attack insulin-producing cells, leading to the development of type 1 diabetes.
The new research showed that killer T-cells—a type of white blood cell that's involved in tackling bacterial infections—can cause type 1 diabetes when activated by bacteria. The researchers showed that proteins from bacterial species known to infect humans could generate killer T-cells that could kill insulin-producing cells.
This research, led by Professor Andrew Sewell at Cardiff University's School of Medicine, expands on their previous studies, which demonstrated that killer T-cells play a major role in initiating type 1 diabetes by killing insulin-producing cells .
Professor Sewell said, "Type 1 diabetes is an autoimmune disease that usually affects children and young adults , where the cells that produce insulin are attacked by the patient's own immune system. This leads to a lack of insulin, meaning that people living with type 1 diabetes need to inject insulin multiple times a day to control their blood sugar levels.
"There is currently no cure for type 1 diabetes and patients require life-long treatment. People living with type 1 diabetes may also develop medical complications later in life, so there is an urgent need to understand the underlying causes of the condition to help us find better treatments."
In laboratory experiments, the researchers introduced bacterial proteins into cell lines from healthy donors and monitored the reaction of killer T-cells from these donors. They found that strong interaction with the bacterial proteins triggered killer T-cells to attack cells that make insulin.
The clinical lead for this study, Dr. Lucy Jones, said, "We observed this in relation to a specific HLA— human leukocyte antigen —a gene that codes for proteins that help the immune system differentiate between our own cells and invading cells.
"The specific HLA associated with the bacterial infection that triggers diabetes is only present in around 3% of the population in the UK. So the bacterial pathogens that can generate anti-insulin T-cells are caused by a rare infection in a small minority of people."
Professor Sewell added, "Killer T-cells are able to target and attack body cells that produce a specific protein . We found that after encountering proteins from some infectious bacteria, killer T-cells could mistakenly also kill cells producing the insulin protein. We found activated T-cells with this same 'cross-reactivity' in the blood of patients with type 1 diabetes suggesting that what we saw in laboratory experiments could have triggered the disease."
The research, published in the Journal of Clinical Investigation , provides the first evidence of how proteins from bacterial germs can trigger the type of killer T-cells seen in patients with type 1 diabetes. The team hopes that knowing more about this process, will allow new ways to diagnose, prevent, or even halt the development of type 1 diabetes.
"We hope that understanding how T-cells trigger diseases like type 1 diabetes will allow us to diagnose and treat disease before the onset of symptoms. Early treatment is known to result in a better prognosis as the healthy pancreatic beta cells that are being attacked can be protected before they are destroyed," said Garry Dolton, the study's first author.
Dr. Lucy Jones said, "Thanks to patients and health care staff being research active, this strong research collaboration between Cwm Taf Morgannwg University health board and Cardiff University has improved our understanding of diabetes."
Explore further
Feedback to editors

Clinical trial demonstrates success in treating rare blood disorder

Long-term outcomes good for face transplant recipients, study finds

Study shows political leanings influence happiness, meaning, and psychological richness

Some diabetes drugs tied to lower risk of dementia, Parkinson's disease
2 hours ago

The MIND diet may lower the risk of memory problems later in life, study shows

New research finds higher levels of leptin indicate brain protection against late-life dementia
3 hours ago

Researchers identify role of Parkinson's-related protein in cancer and T cell activation

Ground squirrel study points to potential development of a cataract drug
4 hours ago

Tailoring radiation therapy for brain cancer treatment: A personal investigation

Changes in chromosomes of cancer cells may increase their sensitivity to anti-cancer drugs
Related stories.

Psoriasis drug shows promise for treating childhood diabetes
Jul 30, 2024

What is type 1.5 diabetes? It's a bit like type 1 and a bit like type 2—but it's often misdiagnosed
Aug 27, 2024

Stem cell therapy could be breakthrough against type 1 diabetes
Jun 25, 2024

Examining the protein that protects insulin-producing cells
Mar 21, 2024

Small protein protects pancreatic cells in model of type 1 diabetes
Aug 16, 2021

Research provides further evidence that epigenetic changes can cause type 2 diabetes
Dec 13, 2023
Recommended for you

Antiviral-resistant variants of SARS-CoV-2 can emerge in immunocompromised people
5 hours ago

Lowering cancer drug dose could open tumors to immunotherapy
6 hours ago

Scientists discover proteins in meat, milk and other foods suppress gut tumors
7 hours ago


Team develops next-generation wearable continuous glucose monitoring system for diabetes management

Study shows widely used test for gestational diabetes misses 70% of cases
8 hours ago
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
- Frontiers in Endocrinology
- Clinical Diabetes
- Research Topics
Physical Activity and Type 1 Diabetes
Total Downloads
Total Views and Downloads
About this Research Topic
Type 1 diabetes is a challenging condition to manage since it includes many facets such as treatment with insulin, technical devices, physiological and behavioral factors. Regular exercise is a cornerstone in diabetes treatment, but management of different forms of physical activity could be difficult for ...
Keywords : Diabetes, Physical Activity, Glucose Monitoring, Hypoglycemia, Performance
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines.
Submission closed.
Participating Journals
Total views.
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Diabetes articles from across Nature Portfolio
Diabetes describes a group of metabolic diseases characterized by high blood sugar levels. Diabetes can be caused by the pancreas not producing insulin (type 1 diabetes) or by insulin resistance (cells do not respond to insulin; type 2 diabetes).
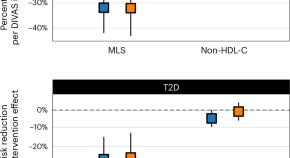
Blood lipid profiling indicates that dietary fat quality is associated with cardiometabolic risk
Dietary guidelines advise substituting saturated fats with unsaturated fats. We used detailed blood fat composition profiling in diet trials and population studies to confirm that a moderate high-fat diet from plant oils is better for metabolism and heart health than a diet with similar fat levels from animal sources.
New insights into the regulation of GIPR signalling
Two recent studies have unravelled novel modes of glucose-dependent insulinotropic polypeptide receptor (GIPR) signalling regulation. Kizilkaya et al. characterized the effect of changes in β-arrestin 2 coupling with naturally occurring GIPR coding variants, whereas Regmi et al. investigated GIPR expression profiles and functional regulation in adipocytes.
- Yusman Manchanda
- Alejandra Tomas
Related Subjects
- Diabetes complications
- Diabetes insipidus
- Gestational diabetes
- Type 1 diabetes
- Type 2 diabetes
Latest Research and Reviews

Exploring the unexplored: identifying knowledge gaps in novel pharmacological treatments for diabetic retinopathy
- Amin Sharifan
- Sobha Sivaprasad
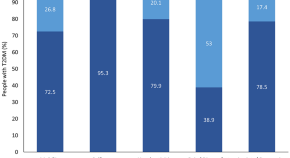
Impairment of health-related quality of life among people with type 2 diabetes and advanced liver fibrosis
- Maurice Michel
- Jesús Funuyet-Salas
- Jörn M. Schattenberg

A drug mix and dose decision algorithm for individualized type 2 diabetes management
- Mila Nambiar
- Yong Mong Bee
- Pavitra Krishnaswamy
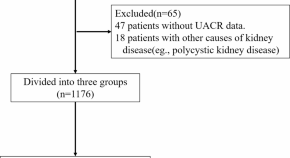
Association of different obesity indexes with diabetic kidney disease in patients with type 2 diabetes mellitus: a cross-sectional study
- Pingping Zhao
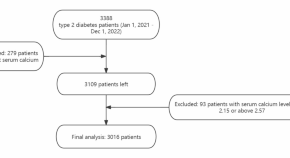
Association of serum calcium levels with diabetic kidney disease in normocalcemic type 2 diabetes patients: a cross-sectional study
- Nailong Yang
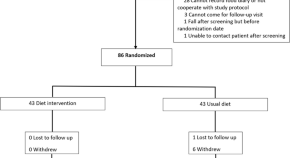
Impact of diet intervention on visceral adipose tissue and hepatic fat in patients with obesity or type 2 diabetes: a randomized trial
- Rungroj Krittayaphong
- Witcha Treesuwan
- Apichart Vanavichit
News and Comment

Brain goop that traps hunger neurons drives obesity
A mechanism for metabolic disease is traced to a defective cellular scaffolding that holds together the brain’s hunger cells.

40 million deaths by 2050: toll of drug-resistant infections to rise by 70%
By 2050, around 2 million people — the majority aged over 70 — could die from drug-resistant infections each year.
- Miryam Naddaf
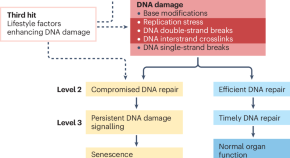
The role of DNA damage in diabetic complications
Mechanistic and clinical data indicate that DNA damage contributes to the pathogenesis and progression of diabetic complications. Thus, DNA damage and its signalling are entering the field of diabetology.
- Varun Kumar
- Ali Önder Yildirim
- Peter P. Nawroth

Prenatal exposure to famine affects lifelong health
Analysis of data related to the Ukraine famine of 1932–1933 shows that in utero exposure to famine increases the risk of adult type 2 diabetes by more than twofold.
- Karen O’Leary
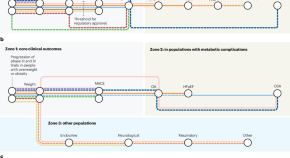
GLP1 agonists: current and future landscape of clinical trials for patients with metabolic dysfunction
Guidelines currently recommend organ-specific management of obesity-related complications. Agents that agonize glucagon-like peptide 1 receptors, including those that co-agonize other anorexigenic hormone receptors, lead to substantial weight loss and benefits in people with varying obesity-related complications, with further trials underway. These medications enable cause-specific management of obesity complications.
- Jonathan Goldney
- Melanie J. Davies

How rival weight-loss drugs fare at treating obesity, diabetes and more
Wegovy, Zepbound and similar medications all lead to metabolic improvements, but scientists are starting to unpick the differences between them.
- Mariana Lenharo
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

T1D Research T2D Research Diabetes in Pregnancy Publications
T1D Programs T2D Programs Diabetes in Pregnancy Clinical Care
Meet Our Team Board of Trustees Careers Financials Annual Report Contact Us Ways to Give
Temporary Location 5425 Hollister Ave, Suite 230 Santa Barbara, CA 93111
Phone: 805-682-7638 Fax: 805-456-0334 Patient Care: 805-682-4793
Tax ID # 95-1684086
With a $2.7 million grant from the National Institutes of Health, researchers from the Keck School of Medicine of USC will lead a multi-site study to understand and optimize brain development in children with type 1 diabetes. (Photo/Adobe Stock
USC launches large-scale nationwide study of type 1 diabetes and brain development
A new large-scale longitudinal study, led by the Keck School of Medicine of USC, will unite 12 research centers across the United States to explore how type 1 diabetes affects children during a window of time known to be critical for healthy brain development.
Ultimately, the findings could help refine clinical guidelines for managing type 1 diabetes, including what glucose levels are safest in terms of healthy brain development. The study could also aid in the creation of targeted treatments for the condition, including changes to sleep, diet, and physical activity that can help specific patients.
The five-year study is supported by a grant of more than $2.7 million from the National Institutes of Health.
To read the full story, click here .
Share This Story, Choose Your Platform!
- Recent News
- News Archive
- For the Media
- Issue Archive
Recent Post
- USC launches large-scale nationwide study of type 1 diabetes and brain development September 18, 2024
- Keck Hospital of USC named a 2024 top performer by Vizient, Inc. September 18, 2024
- USC COMPASS undergraduate program prepares juniors and seniors for stem cell careers September 17, 2024
- Exposure to air pollution during pregnancy increases postpartum depression risk September 16, 2024
- Generous gift from Jerre and Mary Joy Stead boosts neurosurgery at USC September 12, 2024
- The Keck School of Medicine of USC names 11 endowed faculty members September 11, 2024
- USC Roski Eye Institute celebrates new Glendale location September 10, 2024
- New multidisciplinary program aims to help breakers prevent and manage injuries September 10, 2024
- Study shows cells get involved in unhealthy relationships after acute kidney injury September 9, 2024
- Papadopoulos elected Fellow by Royal Society of Canada for 2024 September 6, 2024
- Researchers receive funding to develop next generation of intelligent biocomputers September 6, 2024
- Keck Medicine of USC physicians featured in Pasadena Magazine’s ‘Top Doctors’ September 4, 2024
WHAT ARE YOU LOOKING FOR?
Key searches, usc launches large-scale nationwide study of type 1 diabetes and brain development.
With a $2.7 million grant from the National Institutes of Health, researchers from the Keck School of Medicine of USC will lead a multi-site study to understand and optimize brain development in children with type 1 diabetes.
About half of adults with type 1 diabetes face significant cognitive impairment, including problems with working memory and executive function that affect day-to-day thinking. But less is known about how the condition affects children during a window of time known to be critical for healthy brain development.
A new large-scale longitudinal study, led by the Keck School of Medicine of USC, will unite 12 research centers across the United States to explore that important question. Researchers will collaborate to recruit a large, diverse group of children newly diagnosed with diabetes, taking a sweeping look at the environmental, lifestyle, social, and clinical factors that affect the way the brain develops. The five-year study is supported by a grant of more than $2.7 million from the National Institutes of Health.
“What we really want to know is: In children newly diagnosed with type 1 diabetes, what are factors that may either accelerate or mitigate the risk of developing brain-related complications?” said Kathleen Alanna Page, MD , an associate professor of medicine at the Keck School of Medicine and one of the project’s principal investigators.
With a target sample size of more than 1,000 children, the study is one of the first large-scale efforts to look at the neurocognitive effects of type 1 diabetes in this age group. The study is also unusual in its commitment to recruiting a racially, ethnically and income-diverse group of participants. Most past research on type 1 diabetes has looked primarily at white children.
“We want to translate these insights into real-world opportunities that can help the greatest number of children with diabetes,” Page said.
Ultimately, the findings could help refine clinical guidelines for managing type 1 diabetes, including what glucose levels are safest in terms of healthy brain development. The study could also aid in the creation of targeted treatments for the condition, including changes to sleep, diet, and physical activity that can help specific patients.
“All of that is going to be critically important in improving outcomes in children with diabetes and putting them on the trajectory for better health in the long term,” Page said.
Technological breakthroughs
Advanced tools, including insulin pumps and continuous glucose monitors, have revolutionized the way type 1 diabetes is monitored and treated. Page and her team will now leverage these devices to conduct research in a new way.
Continuous glucose monitors provide detailed reports on glucose levels in real time, including information about how glucose fluctuates throughout the day and the amount of time spent in “high-glucose” and “low-glucose” states.
“Comparing that data to information about brain health can help us refine our clinical guidelines and targets for how tight we want those glucose levels to be, and really help with the clinical management of type 1 diabetes,” Page said.
For example: Is it harmful to have multiple episodes of low glucose or high glucose, and how tight does the range of glucose levels need to be to keep the brain healthy? Do these factors differ between children and adults, or in type 1 versus type 2 diabetes?
The researchers will also use functional magnetic resonance imaging (fMRI) to look noninvasively at the structure, function and development of patients’ brains.
“We not only have more sophisticated ways of monitoring and treating type 1 diabetes, but we also have powerful ways to study the brain that we’ve never had before,” Page said.
A critical window
Studying the brain during childhood can offer valuable insights about long-term health. The brain develops rapidly during this timeframe and is particularly vulnerable to external harms, including changes in glucose that may influence how the brain functions.
To track and measure brain development, the researchers will collect data on academic performance, memory and attention, and neurobehavioral outcomes such as anxiety and behavioral health.
Researchers from each of the 10 study sites will soon convene to create a detailed study protocol, then begin recruiting participants. Page will lead the study from the Southern California hub, alongside co-principal investigators Jennifer Raymond, MD, an associate professor of pediatric endocrinology at Children’s Hospital Los Angeles, and Anny H. Xiang, PhD, director of the division of biostatistics research at Kaiser Permanente Southern California.
“This is somewhere that the Keck School can really shine, because we have all of the resources and the team to approach this question, as well as a diverse population that we serve,” Page said.
About this research
In addition to USC, the consortiums’ other study sites are the University of Minnesota; Washington University in St. Louis; the University of North Carolina at Chapel Hill; Indiana University-Purdue University Indianapolis; the University of Florida; New York University School of Medicine; the University of California, Davis; Vanderbilt University Medical Center; Joslin Diabetes Center; Nemours Children’s Clinic; and the University of Colorado Denver.
This work is supported by the National Institutes of Health [1U01DK140786].
Related Posts

- Press Release
- Department of Medicine
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Type 1 diabetes.
Jessica Lucier ; Scott C. Dulebohn .
Last Update: March 3, 2023 .
- Continuing Education Activity
Type 1 diabetes mellitus (T1D) is an autoimmune disease that leads to the destruction of insulin-producing pancreatic beta cells. Individuals with T1D require life-long insulin replacement with multiple daily insulin injections daily, insulin pump therapy, or the use of an automated insulin delivery system. Without insulin, diabetic ketoacidosis (DKA) develops and is life-threatening. In addition to insulin therapy, glucose monitoring with (preferably) a continuous glucose monitor (CGM) and a blood glucose monitor if CGM is unavailable is recommended. Self-management education and support should include training on monitoring, insulin administration, ketone testing when indicated, nutrition including carbohydrate estimates, physical activity, ways of avoiding and treating hypoglycemia, and use of sick day rules. Psychosocial issues also need to be recognized and addressed. This activity reviews the evaluation and management of T1D. It highlights the importance of a multidisciplinary approach to enhance outcomes.
- Describe the pathophysiology of type 1 diabetes mellitus.
- Explain the management of type 1 diabetes mellitus.
- Review other conditions for which patients with type 1 diabetes mellitus are at increased risk of developing.
- Explain the importance of improving coordination amongst the interprofessional team to enhance care for patients affected by type 1 diabetes mellitus.
- Introduction
Type 1 diabetes mellitus (T1D) is an autoimmune disease that leads to the destruction of insulin-producing pancreatic beta cells. There is heterogeneity in the metabolic, genetic, and immunogenetic characteristics of T1D and age-related differences, requiring a personalized approach for each individual. Loss of insulin secretion can occur quickly or gradually. Residual insulin production (detectable/higher c-peptide) is more common in adult-onset compared to youth-onset T1D, whereas diabetic ketoacidosis is more common in youth with T1D. [1] Detectable c-peptide is associated with better glycemic control. [2] The presence of other autoimmune conditions, obesity, comorbidities, and the development of diabetes-related complications is also variable. [3]
Successful management of T1D requires multiple daily insulin injections (MDI), insulin pump therapy, or the use of an automated insulin delivery system, as well as glucose monitoring, preferably with a continuous glucose monitor (CGM). All people with T1D should be able to perform capillary blood glucose monitoring (BGM) if CGM is unavailable. Self-management education, training, and support, as well as addressing psychosocial issues, help to optimize outcomes. A collaborative multidisciplinary approach, utilizing medical providers, nurse and dietitian educators, pharmacists, community resources, and specialists as needed (including podiatrists, mental health professionals, social workers, ophthalmologists, cardiologists, and others), is recommended. [4]
In T1D, there is autoimmune destruction of the beta cells in the pancreatic islets over months or years, causing an absolute deficiency of insulin. Although the exact etiology of T1D is still unknown, researchers believe there is a genetic predisposition with a strong link with specific HLA (DR and DQ) alleles. This association is more pronounced in youth-onset T1D compared to adult-onset T1D. [5] Multiple other genes contribute to heritability as well. [6]
In those at risk, it is generally believed that viruses, environmental including dietary factors, and/or other stressors can trigger autoimmune beta-cell destruction. Some studies have found an increased risk of development of T1D related to infection with Coxsackie virus, enteroviruses, cytomegalovirus, rubella virus, influenza B, mumps virus, and more recently, SARS-CoV-2 (COVID-19). [7] [8] [9] In The Environmental Determinants of Diabetes in the Young (TEDDY) study, breastfeeding was not associated with the risk of islet autoimmunity in children genetically at increased risk. However, a systematic review and meta-analysis concluded that breastfeeding and the later introduction of gluten, fruit, and cow’s milk were associated with a lower risk of developing T1D. [10] Research to better understand the etiology of T1D is ongoing.
The presence of circulating pancreatic islet autoantibodies suggests that the individual is at risk for or has developed T1D. These antibodies include islet cell cytoplasmic antibodies (ICA), antibodies to insulin (IAA), glutamic acid decarboxylase isoform 65 (GAD65), insulinoma antigen 2/islet tyrosine phosphatase 2 (IA-2) and zinc transporter isoform 8 (ZnT8). IAAs are primarily detected in children. [11] GAD65 is the most common autoantibody detected in adults [3] . ICA is no longer routinely recommended, as it is an imprecise assay. The greater the number of detectable antibodies and the higher their titers, the greater the risk of developing T1D.
- Epidemiology
T1D is one of the most frequent chronic diseases in children but can have its onset at any age. In adults, new-onset type 1 diabetes may be misdiagnosed as type 2 diabetes and is more common than youth-onset T1D. [3] [ [5] There has been a steady increase in the incidence and prevalence of T1D, representing approximately 5% to 10% of people with diabetes. A systematic review and meta-analysis reported that the worldwide prevalence of T1D was 9.5%, with an incidence of 15 per 100,000 people. [12] Worldwide, there is also a considerable geographic variation in incidence. The highest reported incidences are in Finland and other Northern European nations, with rates approximately 400 times greater than those seen in China and Venezuela, where there is the lowest reported incidence.
- Pathophysiology
The development of T1D occurs in 3 stages. Stage 1 is asymptomatic and characterized by normal fasting glucose, normal glucose tolerance, and the presence of ≥2 pancreatic autoantibodies. Stage 2 diagnostic criteria include the presence of pancreatic autoantibodies (usually multiple) and dysglycemia: impaired fasting glucose (fasting glucose 100 to 125 mg/dL) or impaired glucose tolerance (2-hour post-75 gm glucose load glucose 140 to 199 mg/dL) or an HbA1c 5.7% to 6.4%. Individuals remain asymptomatic. In stage 3, there is diabetes, defined by hyperglycemia (random glucose ≥200 mg/dL) with clinical symptoms, fasting glucose ≥126 mg/dL, glucose ≥200 mg/dL two hours after ingesting 75 g of glucose during an oral glucose tolerance test and/or HbA1c ≥6.5%. If the individual lacks classic symptoms of hyperglycemia or hyperglycemic crisis, it is recommended that two tests be performed (simultaneously or at different times) to confirm the diagnosis. If there is an acute onset of symptoms with hyperglycemia, as more often occurs in youth-onset T1D, HbA1c may be misleading at the time of diagnosis, and glucose criteria should be used. [4]
T1D, especially in children, classically presents with hyperglycemic symptoms, which can be sudden, and include polydipsia, polyuria, polyphagia, nocturnal enuresis, blurred vision, unintentional weight loss, fatigue, and weakness. If not evaluated and treated promptly, it can become a medical emergency. In addition to hyperglycemia, electrolyte abnormalities may be present. If these individuals are not treated, DKA can develop, requiring hospitalization and treatment with intravenous fluids, insulin, potassium, and careful monitoring. Almost one-third of youth present with DKA. [13]
In adult-onset diabetes, the onset of symptoms is more variable than in youth, and DKA is less common. It can be difficult to distinguish T1D and type 2 diabetes. GAD65 should be the initial antibody tested when diagnosing T1D in adults is suspected. If negative and/or if available, IA2 and/or ZNT8 should be measured as well. C-peptide levels can be used when there is a question about which type of diabetes is present. A random C-peptide should be drawn with concurrent serum glucose. If the duration of diabetes exceeds three years, c-peptide >600 pmol/L strongly suggests type 2 diabetes. A low (<200 pmol/L) or undetectable c-peptide confirms the diagnosis of T1D. [3]
- History and Physical
At the initial outpatient visit, obtaining a complete medical, surgical, psychosocial, and family history, including pregnancy and contraception history, is essential. History of prior diabetes education, monitoring of BG and ketones, use of CGM, administration of insulin, recognition/treatment of hypoglycemia, use of glucagon, diet, physical activity, smoking and alcohol use, understanding of sick-day rules, ability to problem solve and immunization history, should also be obtained. Particular attention should be paid to the date of diagnosis, prior treatment, current medications, presence of hypoglycemia unawareness, and history of acute complications (hypoglycemia including severe episodes and episodes of DKA) and chronic complications (skin disorders, dental problems, retinopathy, macular edema, neuropathy, kidney disease, cardiovascular disease, peripheral arterial disease, stroke, foot ulcers, amputations, hearing loss, sleep disorders). Since people with type 1 diabetes are at increased risk of other autoimmune disorders, including autoimmune thyroid disease and celiac disease, the history should also focus on these conditions. [3]
Clinicians should measure height, weight, and blood pressure. The skin should be examined, especially at insulin injection or infusion sites. If lipodystrophy is evident, they should be educated on the importance of varying insulin injection/infusion sites. The thyroid, heart, chest, and abdomen should also be examined. A foot exam is performed to examine pedal pulses and detect foot deformities, pre-ulcerative lesions, ulcerations, calluses, and onychomycosis. It is also important to test vibratory and protective sensations; abnormal testing with a 10-g monofilament exam suggests an increased risk of ulceration.
When screening for psychosocial issues, a number of measures are available such as the Patient Health Questionnaire (PHQ-2/PHQ-9) for Depression and Generalized Anxiety Disorder (GAD-7). Diabetes distress and social determinants of health should be assessed. Since eating disorders are more common in type 1 diabetes, particularly in young women, evaluation should be considered clinically indicated. Early cognitive decline is also common, so cognitive testing should be considered when impairment is suspected. [3]
Data from CGMs, blood glucose meters, insulin pumps, and automated insulin delivery systems should be downloaded, examined, and discussed at each visit and between visits when needed to adjust treatment regimens to achieve glycemic goals.
CGMs are devices that measure glucose in interstitial fluid and are extremely useful tools for people with T1D. Sensors are inserted into the subcutaneous tissue and transmit glucose readings every 5 minutes to a receiver where they can be displayed in real-time. One can examine trends and use low and high glucose alarms to prevent serious hypoglycemia and hyperglycemia episodes. Alarms can also alert to a rapid change in glucose value. Readings from certain CGM sensors can be transmitted to smartphones and can be shared with relatives, friends, or caregivers. A less expensive CGM option uses a “reader” (a device the user scans over the site of sensor placement) or a smartphone to visualize recent glucose readings and trends. All these devices make it easier to monitor glucose values throughout the day and night. Users examine trends and are provided with important information to guide insulin therapy and food intake to help avoid wide glycemic excursions and hypoglycemia.
Data from CGMs can be uploaded and stored in cloud-based systems. These data include percent: Time in range TIR, usually 70 to 180 mg/dL; TIR targets are lower during pregnancy and higher in those who are frail and/or with complex comorbidities or limited life expectancy), time below range (TBR; <70 mg/dL; level 1 hypoglycemia is 54-69 mg/dL and level 2 hypoglycemia is <54 mg/dL); time above range (TAR; usually >180 mg/dL; level 1 hyperglycemia is 181 to 250 mg/dL and level 2 hyperglycemia is >250 mg/dL); and glycemic variability (% CV; coefficient of variation). These data should be reviewed with the goal of understanding factors contributing to hypoglycemia and hyperglycemia and to help guide insulin dosing, diet, and physical activity to achieve goals. A primary goal should be minimizing hypoglycemia. A higher percent TIR is associated with decreased diabetes-related complications. [14] [15] HbA1c, TIR, and TBR improve when MDI or pump therapy is augmented with CGM use. The glucose management indicator (GMI) is calculated using average sensor readings over a 14-day period and correlates with the estimated HbA1c. [16]
When CGM data are unavailable, examination of BG data fasting, pre-meal, 1 to 3 hours postprandial (when adjusting prandial dosing), bedtime, when hypoglycemia is suspected, and occasionally in the middle of the night, should be used to direct insulin dosing. Insulin dosing data from connected insulin pens and pumps should also be discussed.
HbA1c is recommended every 3 to 6 months. The HbA1c reflects glycemic control over the previous 2 to 3 months. A typical goal HbA1c is <7.0%, with higher goals in people with frailty, cardiovascular disease/multiple comorbidities, history of severe hypoglycemia, and/or hypoglycemia unawareness. Lower goals are used when they can be achieved safely (without an increase in hypoglycemia).
Other laboratory tests include a yearly lipid profile, serum creatinine, eGFR, and urine albumin to creatinine ratio. Serum potassium should be monitored if taking an ACE-I, ARB, or diuretic, and AST, ALT, TSH, celiac screen, vitamin B12, and vitamin D at least once and as indicated clinically. These tests could be repeated more frequently if the previous results were abnormal. Since people with T1D are at an increased risk of developing other autoimmune diseases, such as autoimmune thyroid disease, celiac disease, primary adrenal insufficiency, and rheumatoid arthritis, screening for autoimmune disorders should be considered when clinically appropriate. [17] [4]
- Treatment / Management
People with T1D require insulin therapy, glucose monitoring (preferably CGM), and diabetes self-management education and support. Multiple daily insulin injections (MDI) using basal (preferably a long-acting insulin) and bolus (preferably rapid-acting insulin for meals and correction)insulins, continuous subcutaneous insulin infusion (rapid-acting insulin) through an insulin pump, or use of automated insulin delivery (hybrid closed loop) systems with rapid-acting insulin, are available. Automated insulin delivery is associated with greater time in the target range and less hypoglycemia. When initiating a treatment plan, use shared decision-making, considering individualized realistic and attainable goals, risk of hypoglycemia, lifestyle, and the availability and affordability of different regimens. [4]
Hypoglycemia is the most frequent adverse effect of insulin therapy. It is important to educate people with diabetes and their partners about the signs and symptoms of hypoglycemia, which include diaphoresis, tachycardia, lightheadedness, confusion, hunger, visual changes, and tremors. With a long duration of T1D, hypoglycemia unawareness becomes more common. Generally, 15 to 20 g of glucose should be given orally for blood glucose below 70 mg/dL. [17] Glucose readings should be rechecked 15 minutes later, with additional carbohydrates given if needed.d Once the glucose reading has normalized, if glucose readings again begin to fall, a snack should be given to prevent a recurrence. Glucagon should be prescribed for emergency use for severe hypoglycemia (when there is an inability to consume carbohydrates by mouth). People with T1D should also receive sick day instructions, including how to manage hyperglycemia and ketone testing. When initiating insulin therapy in an adult, the person’s weight in kilograms is multiplied by 0.2 to 0.6 units to calculate the initial total daily insulin dose (TDD). Generally, basal requirements are 40% to 50% of the TDD, and the rest approximates the daily rapid-acting insulin that must be given before or with meals. Dosing is modified based on many factors, including diet, physical activity, and CGM and/or BGM results.
When possible, people with T1D should meet with a dietitian, be taught carbohydrate counting, and be instructed to use an insulin-to-carbohydrate ratio (grams of carbohydrate covered by one unit of insulin) for mealtime dosing. If carbohydrate counting is not possible, a carbohydrate-consistent diet is helpful. Estimating the fall in glucose resulting from 1 unit of rapid-acting insulin, called a correction or insulin sensitivity factor, is also recommended when treating hyperglycemia. The correction factor can be initially estimated using the formula 1800 divided by the TDD. This number will need to be adjusted per subsequent glucose monitoring results. When using correction doses, the individual needs to be careful not to take injections too close together (“stacking”) to avoid overdosing (insulin administered when there is still active insulin from previous doses causing overlapping insulin doses) and hypoglycemia.
It is important to note that insulin requirements vary across the lifespan and under specific circumstances. For example, larger insulin doses are typically required during puberty, pregnancy, when steroids are given, and with the development of obesity. Individuals need less insulin when they are engaged in aerobic exercise and during the “honeymoon period.” The honeymoon period occurs soon after diagnosis when there can be a temporary recovery of beta-cell function.
Multiple types of insulin can be used for insulin injection therapy. [18] Rapid-acting insulin (lispro, aspart, glulisine) will generally have onset in 12 to 30 minutes, peak in 1 to 3 hours, and have a duration of action of 3-6 hours. Ultra-rapid-acting lispro or aspart have a slightly quicker onset of action and somewhat shorter duration of action. . Short-acting insulin (regular insulin) has an onset in 30 minutes to 1 hour and peak in 2 to 4 hours with a duration of 5 to 8 hours.
For basal insulin injection therapy, long-acting insulin is preferred, often given once a day (U-100 and U-300 glargine, degludec) or 1 to 2 times daily (detemir and U-100 glargine). Glargine does not have a pronounced peak and lasts approximately 20 to 24 hours. U-300 glargine lasts more than 24 hours, and degludec has a longer duration of action, up to 42 hours. Intermediate insulin (NPH, NPL) is the least expensive basal insulin, but it is associated with more hypoglycemia. It has onset in 1 to 2 hours, peak action at 2 to 8 hours, duration of 12 to 24 hours, and is usually given before breakfast and bedtime. When MDI is used, the individual will ideally use rapid-acting insulin with each meal for hyperglycemia correction and a daily long-acting basal insulin.
Insulin pumps deliver insulin every 5 minutes to provide basal needs and deliver boluses of insulin to control mealtime excursions and correct hyperglycemia. Only rapid-acting insulin is used in insulin pumps/automated insulin delivery systems. Some pumps use external tubing to infuse insulin from the pump to the infusion site in the subcutaneous tissue, while another pump uses a “pod” that contains insulin, which is directly applied to the skin and is controlled via a wireless connection to a controller or smartphone. Insulin pumps are programmed with adjustable basal rates, insulin-to-carbohydrate ratios, correction factors, and target glucose ranges.
Some insulin pumps communicate with CGMs and have threshold/predictive low-glucose suspend features. With these devices, insulin delivery is suspended when hypoglycemia occurs or is predicted to occur. In the newer hybrid closed-loop automated insulin delivery systems, the CGM sends glucose data to an insulin pump with a control algorithm. Basal insulin delivery is automated based on the CGM readings received every 5 minutes and the target glucose. Advanced systems deliver automated correction boluses as well. Mealtime bolus insulin is still required to be delivered under the direction of the user.
Several clinical trials are currently underway, testing “closed-loop” fully automated insulin delivery systems, as well as a closed-loop system that delivers insulin and glucagon. The hope is that these closed-loop automated insulin systems will lead to better glucose management, with minimal risk of hypoglycemia and reduced burden for people with T1D.
Physical activity is recommended for people with T1D. Exercise increases insulin sensitivity, improves cardiovascular health, improves lipid profiles, decreases microvascular complications, reduces the risk of osteoporosis, and decreases mortality. Glycemic control can be more difficult during times of activity related to the intensity and duration of the activity, amount of circulating insulin, glucose level before exercise, and dietary intake. Individuals should be taught the effect of different types of activity (aerobic vs. anaerobic) on glucose levels, how to balance carbohydrate intake and insulin doses when active, and how to avoid hypoglycemia and wide glycemic excursions with exercise.
In addition to insulin therapy, diet, and physical activity, individuals with T1D should generally have an annual eye exam by an eye care specialist and an annual foot exam. Those with foot deformities, neuropathy, a history of foot ulcers, or peripheral arterial disease should have their feet examined at each visit, be educated in proper foot care/footwear, and, if available, see a podiatrist and be evaluated for orthotics if indicated. Other specialists, such as nephrologists, ophthalmologists, and cardiologists, as well as referrals to community resources, social workers, and mental health professionals, may be needed. The use of statins and other anti-hyperlipidemic therapy, smoking cessation, and anti-hypertension therapy to reduce cardiovascular risk and risk of nephropathy and retinopathy are important and discussed later in this article. Pancreatic and islet cell transplantation are two treatment options that can restore normoglycemia.
A pancreatic transplant is usually performed simultaneously with a kidney transplant (SPK transplant). These transplants are considered when end-stage renal disease is present, in relatively younger individuals (<50 years old without coronary artery disease), and when usual treatment options have been unsuccessful in preventing large variability and severe hypoglycemia. Individuals who receive a pancreatic transplant or an islet-cell transplantation require immunosuppressive therapy. Encapsulated islets could obviate the need for immunosuppressive therapy and are a promising future therapy. These and other research initiatives give hope to the increasing number of people with T1D that a cure is in their future. [4]
- Differential Diagnosis
- Diabetes mellitus type 2
- Pancreatic diabetes
- Steroid-induced diabetes
- Diabetes insipidus
- Factitious illness
- Psychogenic polydipsia
- Renal glycosuria
With better glucose, blood pressure, lipid control, and better foot care, there has been a reduction in the morbidity and mortality associated with T1D. Rates of serious diabetes-related complications are lower; if present, their onset has been delayed for many. Although people with T1D have 2 to 5-fold higher mortality than those without diabetes, mortality rates have declined. This is discussed further in other sections. [19]
- Complications
The major acute complications of diabetes are hypoglycemia and serious hyperglycemia, including diabetic ketoacidosis. The major chronic complications are listed below:
- Nephropathy
- Neuropathy: peripheral and autonomic
- Retinopathy/macular edema
- Heart disease, including coronary artery disease, heart failure, cardiomyopathy
- Peripheral arterial disease
- Cerebrovascular disease, including stroke and TIA
- Hearing loss
- Diabetic foot diseases, including foot ulcers and amputations
- Deterrence and Patient Education
Patient medication compliance and follow-up with specialists and educators are critical factors in preventing complications. At every patient encounter, the pharmacist, nurse, and clinicians should emphasize the importance of blood glucose control, long-term complications, and management goals. The patient should be encouraged to modify their lifestyle to reduce the risk of complications. In addition, all patients with diabetes should be made aware of the signs and symptoms of hypoglycemia and ways of managing it. Patients should be educated about available resources and the benefits of joining support groups. A dietitian should educate the patient about foods that can be consumed, and the nurse should educate the patient on blood glucose monitoring at home.
- Enhancing Healthcare Team Outcomes
Self-management of T1D includes administering insulin multiple times daily with glucose monitoring and attention to food intake and physical activity every day, which is a considerable burden. Whereas newer technologies have helped people improve their glycemic control, they are costly, complex, and require education and training. Many people with diabetes fear hypoglycemia, hyperglycemia, and the development of complications, and depression, anxiety, and eating disorders can develop. The medical, education, training, psychological, and social challenges faced by people with T1D daily are best addressed by an interprofessional team that includes clinicians (MDs, DOs, NPs, and PAs), nurses (including diabetes nurse educators), pharmacists, dieticians, mental health professionals, social workers, podiatrists, and the use of community resources. Individualized treatment approaches, which can reduce the burden and further improve outcomes, are needed, and the interprofessional care model will yield the best possible patient outcomes. [3]
It is imperative for all interprofessional team members to coordinate their activities and interventions with the rest of the team and utilize open communication channels to ensure everyone involved in patient care, as well as the patient themselves, has access to the same accurate, updated patient information. Nurses are often crucial in coordinating activities between various professionals on the case and play a role in patient evaluation, education, and monitoring. Pharmacists should work directly with diabetes educators to ensure proper insulin dosing and participate in patient medication education and reconciliation. These examples of interprofessional care will help drive improved patient outcomes. [Level 5]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Jessica Lucier declares no relevant financial relationships with ineligible companies.
Disclosure: Scott Dulebohn declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Lucier J, Dulebohn SC. Type 1 Diabetes. [Updated 2023 Mar 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Diabetes technology and treatments in the paediatric age group. [Int J Clin Pract Suppl. 2011] Review Diabetes technology and treatments in the paediatric age group. Shalitin S, Peter Chase H. Int J Clin Pract Suppl. 2011 Feb; (170):76-82.
- Continuous Subcutaneous Insulin Infusion (CSII) Pumps for Type 1 and Type 2 Adult Diabetic Populations: An Evidence-Based Analysis. [Ont Health Technol Assess Ser....] Continuous Subcutaneous Insulin Infusion (CSII) Pumps for Type 1 and Type 2 Adult Diabetic Populations: An Evidence-Based Analysis. Medical Advisory Secretariat. Ont Health Technol Assess Ser. 2009; 9(20):1-58. Epub 2009 Oct 1.
- The effectiveness of continuous subcutaneous insulin pumps with continuous glucose monitoring in outpatient adolescents with type 1 diabetes: A systematic review. [JBI Libr Syst Rev. 2012] The effectiveness of continuous subcutaneous insulin pumps with continuous glucose monitoring in outpatient adolescents with type 1 diabetes: A systematic review. Matsuda E, Brennan P. JBI Libr Syst Rev. 2012; 10(42 Suppl):1-10.
- Glycemic Control in Relation to Technology Use in a Single-Center Cohort of Children with Type 1 Diabetes. [Diabetes Technol Ther. 2022] Glycemic Control in Relation to Technology Use in a Single-Center Cohort of Children with Type 1 Diabetes. Sawyer A, Sobczak M, Forlenza GP, Alonso GT. Diabetes Technol Ther. 2022 Jun; 24(6):409-415. Epub 2022 Feb 16.
- Review Continuous glucose monitoring systems for type 1 diabetes mellitus. [Cochrane Database Syst Rev. 2012] Review Continuous glucose monitoring systems for type 1 diabetes mellitus. Langendam M, Luijf YM, Hooft L, Devries JH, Mudde AH, Scholten RJ. Cochrane Database Syst Rev. 2012 Jan 18; 1(1):CD008101. Epub 2012 Jan 18.
Recent Activity
- Type 1 Diabetes - StatPearls Type 1 Diabetes - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Informatics
- Molecular Dx
- Patient Care
- Precision Medicine
- Translational Research
- Browse Issues
- Molecular Diagnostics
- Oncology/Therapeutics
- Healthcare Informatics
- Get Inside Precision Medicine Magazine
- Get Inside Precision Medicine eNewsletters
- Learning Labs
- Inside Precision Medicine Live

Breakthrough 10-Year Study: Immune Therapy Transforms Survival for Advanced Melanoma Patients
Bringing radioimmunotherapy to solid tumors, sophia presents multimodal ai-driven research on patient stratification in lung cancer, msk researchers discover new type of sclc, breast, ovarian cancer risks of rad51c variants assessed systematically, usc launches study on how type 1 diabetes affects childhood brain development.

The Keck School of Medicine of USC has announced the launch of a nationwide longitudinal study aimed at understanding how type 1 diabetes impacts brain development in children. Funded by a $2.7 million grant from the National Institutes of Health, this multi-site study will involve collaboration among 12 research centers across the United States.
Type 1 diabetes has been linked to cognitive impairments in adults, particularly in areas such as working memory and executive function. However, the effects on children during critical developmental periods remain largely unexplored. This study seeks to fill that gap by recruiting more than 1,000 children recently diagnosed with the condition.
“What we really want to know is: In children newly diagnosed with type 1 diabetes, what are factors that may either accelerate or mitigate the risk of developing brain-related complications?” said Kathleen Alanna Page, MD, an associate professor of medicine at USC and one of the principal investigators for the project.
The study’s design aims to include participants from a range of racial, ethnic, and socioeconomic backgrounds, which is a departure from past type 1 diabetes research that has largely focused on white children.
“We want to translate these insights into real-world opportunities that can help the greatest number of children with diabetes,” Page emphasized.
The researchers believe this study could refine clinical guidelines for managing type 1 diabetes, particularly determining what glucose levels are best for healthy brain development. It could also suggest other therapeutic approaches such as adjustments in sleep, diet, and physical activity designed for individual patients.
“All of that is going to be critically important in improving outcomes in children with diabetes and putting them on the trajectory for better health in the long term,” Page noted.
Advanced tools such as insulin pumps and continuous glucose monitors, which have significantly changed the treatment landscape for type 1 diabetes, will play an important role in the research. Continuous glucose monitors, for instance can provide important data detailing how glucose levels fluctuate during the day to detail the amount of time a person spends in “high-glucose” and “low-glucose” state.
Page said that being able to compare information about brain health could help refine clinical guidelines for type 1 diabetes and to help determine, more precisely how tight the range of glucose levels should be for appropriate clinical management.
The study will also employ functional magnetic resonance imaging (fMRI) to non-invasively examine the structure and function of the children’s brains, offering insights that were previously difficult to obtain.
Childhood is a period of rapid brain development, and the researchers believe this study can provide insight into the long-term health effects of type 1 diabetes. In addition to the brain imaging, the study will also collect data relating to academic performance, memory and attention, as well as neurobehavioral data such as anxiety and behavioral health.
As the project progresses, researchers from each of the study sites will gather to finalize a detailed study protocol before recruitment begins. Leading the study from the Southern California hub, Page will be joined by co-principal investigators Jennifer Raymond, MD, a pediatric endocrinologist at the Children’s Hospital Los Angeles, and Anny H. Xiang, PhD, director of biostatistics research at Kaiser Permanente Southern California.
Other sites participating in the study are the University of Minnesota; Washington University in St. Louis; the University of North Carolina at Chapel Hill; Indiana University-Purdue University Indianapolis; the University of Florida; New York University School of Medicine; the University of California, Davis; Vanderbilt University Medical Center; Joslin Diabetes Center; Nemours Children’s Clinic; and the University of Colorado Denver.
- News & Features
Related Content

Wearable Sensor Allows Accurate Eye Tracking to Predict Brain Disorders

HRT Reduces Insulin Resistance after Menopause According to Meta-Analysis

Study Identifies Key Factors for Long-Term Weight Loss with GLP-1 Medications

AFib Three Times More Common than Thought
- Terms of Service
- Cookie Policy
Immunotherapy and Cancer: Harnessing the Power of Diagnostic Assays
Rise of genomics in clinical trials, conquering cml: the breakthrough paradigm change of treatment-free remission.
Talk to us about diabetes
0345 123 2399
customer support
Research spotlight - what causes Type 1 diabetes?
Our immune system normally protects us against infection and illness. but in type 1 diabetes, the immune system attacks the cells in the pancreas that make insulin – the hormone responsible for regulating levels of glucose in the blood., scientists are working hard to find out what causes this to happen..
Find out about the research we're funding below. We've also linked up with Steve Morgan Foundation and JDRF to accelerate the development of new treatments and a a cure for type 1 diabetes. Find out more about the Type 1 Diabetes Grand Challenge .
The genetics of Type 1 diabetes isn’t simple. There’s no single gene that, if inherited from your parents, means you’re going to develop Type 1 diabetes.
In fact, there are a number of genes involved in Type 1 diabetes. These genes don’t ‘give’ you Type 1 diabetes, but increase the chances of you developing it. The more high risk genes you have, the more likely you are to develop Type 1 diabetes.
But having several high risk genes doesn’t mean you will definitely develop Type 1. Take genetically identical twins as an example. There are pairs of identical twins where one twin develops Type 1 diabetes, and the other doesn’t. This means that our risk of Type 1 diabetes isn’t solely linked to our genetic make-up.
The number of people being diagnosed with Type 1 diabetes is on the rise. And this number is rising too quickly for Type 1 diabetes to be down to genes alone – our genes can’t change that quickly. Something else is contributing to this increase in Type 1 diabetes.
Scientists believe that our environment plays a role in the development of Type 1 diabetes, in combination with these high risk genes.
| , and what . |
Viral infection

Several viruses have been associated with Type 1 diabetes, but one type of virus, called Human Enteroviruses (HEVs), have the strongest body of evidence. HEVs are a large family of viruses that enter the gut and are spread through poor hygiene or sanitation. One of the most famous HEVs is the polio virus, but most HEVs aren’t as serious as polio and can appear as a common flu-like infection that the immune system will clear on its own.
Small studies have found traces of HEVs in pancreas samples from people newly diagnosed with Type 1 diabetes, and from people who have lived with Type 1 for a long time. Some research has suggested that a baby’s risk of Type 1 diabetes is higher if their mother picks up a HEV during pregnancy. But the evidence is mixed, and no conclusions can be drawn yet. We know that our immune system responds to viruses, but we don’t yet know if or how a HEV infection could lead to Type 1 diabetes. There are several possible theories:
- HEVs might look similar to parts of insulinproducing cells in the pancreas, causing the immune system to mistakenly attack the cells.
- HEV infections might expose insulinproducing cells to the immune system in an unusual way, leading to an attack.
- HEV infections might change how insulinproducing cells work, making them appear as a threat to the immune system.
| to understand how and why some insulin-producing cells lose their ability to fight off viral infections during the development of Type 1 diabetes. is one of the biggest studies trying to uncover the environmental triggers of Type 1 diabetes. It’s investigating many factors, including viral infections and nutrition. |
Gut microbiome
The ‘microbiome’ describes all of the different bacteria and other microorganisms living inside us. Most of these are found in our gut. They can influence our health in different ways, including how our immune system works and how we break down sugar.
There are a number of factors that could affect the gut microbiome, such as whether a baby is born via caesarean delivery, our diets during early childhood and the use of antibiotics. All of these are intertwined with how the gut microbiome develops and how diverse it is, which appears to be important in the development of Type 1 diabetes.
Studies have shown that the gut microbiome in children with Type 1 diabetes is different compared to children without Type 1. There is even evidence to suggest that there are fewer types of bacteria in children who show early signs of Type 1 diabetes but haven’t been diagnosed yet.
| is also studying the importance of the gut microbiome by collecting and analysing stool samples, and keeping dietary records of the participants. |
Scientists have questioned whether our diet during childhood could influence our risk of Type 1 diabetes. Cows’ milk, gluten, cereals, omega-3, vitamin D and breast-feeding are all being studied. But the evidence is often contradictory, making it hard to pinpoint which factors could be the most important, both in protecting people from developing Type 1 or increasing the risk.
Also under the spotlight...
Hygiene, pollutants, vaccines, maternal age, psychological stress and seasonal variation have all been put forward as possible environmental factors involved in Type 1 diabetes. It’s a lot to take in, and we don’t have any definitive answers yet, but there’s no shortage of research going on.
What’s the answer?
The take home message: the full picture is still unclear. We still don’t fully understand whether one, or a combination, of these factors causes someone at high risk of Type 1 diabetes to actually develop the condition.
It’s even possible that the timing of the environmental trigger plays a role in this risk. And the way each environmental trigger might lead to Type 1 could also be different. Taken together, this might help to explain why there has been conflicting evidence so far.
Hands up, it’s complicated. But scientists across the world are working hard to understand just how important each suspected trigger could be, and who they could affect in the future. Piecing together this puzzle this will lead us to ways of preventing, delaying or even curing Type 1 diabetes in the future.
Is there a cure for diabetes?
Share this Page
© The British Diabetic Association operating as Diabetes UK, a charity registered in England and Wales (no. 215199) and in Scotland (no. SC039136). A company limited by guarantee registered in England and Wales with (no.00339181) and registered office at Wells Lawrence House, 126 Back Church Lane London E1 1FH


IMAGES
VIDEO
COMMENTS
Type 1 diabetes (also known as diabetes mellitus) is an autoimmune disease in which immune cells attack and destroy the insulin-producing cells of the pancreas. ... Research Highlights 02 Aug 2024 ...
The burden of type 1 diabetes remains substantial, and more research is needed to improve the lives of people with type 1 diabetes and to find a cure. To this end, ADA-funded research continues to drive progress by funding research projects topics spanning technology, islet transplantation, immunology, improving transition to self-management ...
The study by Gong et al. examines the increases in the incidence, prevalence, and burden trends of type 1 diabetes (T1D) in adolescents and young adults over a 30-year span (1990 - 2019) by age ...
The topic has been extensively reviewed in the past . Briefly, inspired by successes with vaccination against, for example, peanut allergy, tolerisation of T effector cells has been attempted using administration of whole antigens, such as oral insulin, or of peptides. ... Although research into type 1 diabetes prevention and disease ...
Abstract. Type 1 diabetes (T1D) is an autoimmune disorder, and insulin deficiency is the result of β-cell dysfunction. Treatment of type 1 diabetes requires constant parenteral insulin administration, which can be very burdensome for the patient. Meticulous use of insulin therapy does not protect the patient against complications.
Type 1 diabetes is an autoimmune condition resulting in insulin deficiency and eventual loss of pancreatic β cell function requiring lifelong insulin therapy. Since the discovery of insulin more than 100 years ago, vast advances in treatments have improved care for many people with type 1 diabetes. Ongoing research on the genetics and immunology of type 1 diabetes and on interventions to ...
I. Introduction. Diabetes mellitus, a metabolic disease defined by elevated fasting blood glucose levels due to insufficient insulin production, has reached epidemic proportions worldwide (World Health Organization, 2020).Type 1 and type 2 diabetes (T1D and T2D, respectively) make up the majority of diabetes cases with T1D characterized by autoimmune destruction of the insulin-producing ...
Type 1 Research Highlights. While the Association's priority is to improve the lives of all people affected by diabetes, type 1 diabetes is a critical focus of the organization. In fact, in 2016, 37 percent of our research budget was dedicated to projects relevant to type 1 diabetes. Read more about the critical research made possible by the ...
Journal of Diabetes Research is an open access journal that publishes articles related to type 1 and type 2 diabetes. Topics include etiology, pathogenesis, management, and prevention of diabetes, as well as associated complications such as nephropathy. As part of Wiley's Forward Series, this journal offers a streamlined, faster publication ...
Hypoglycaemia is a common occurrence in people with type 1 diabetes mellitus, and can have serious consequences. This Review defines hypoglycaemia in type 1 diabetes mellitus, and also outlines ...
Prediction and Prevention of Type 1 Diabetes. Type 1 Diabetes (T1D) is one of the most common chronic autoimmune diseases in children. The disease is characterized by the destruction of beta cells, leading to hyperglycemia, and to a lifelong insulin-dependent state. Although several studies in the last decades have added relevant insights, the ...
TOPICS. AI in Medicine; Climate Crisis and Health; ... Also the parents of children with type 1 diabetes need psychological support, Acta Paediatrica, ... Research; Reviews; Clinical Cases ...
Type 1 diabetes is caused by an autoimmune attack of insulin-producing beta-cells. While genetics and the environment are known to play important roles, the underlying factors explaining why the immune system mistakenly recognize beta-cells as foreign is not known. Now, Dr. Delong has discovered a potential explanation.
Beena Akolkar, Ph.D. Clinical research in the prevention and immunopathogenesis of Type 1 Diabetes and the genetics and genomics of Type 1 and Type 2 Diabetes. Guillermo A. Arreaza-Rubín, M.D. Diabetes and endocrine disease bioengineering and glucose sensing. Miranda Broadney, M.D., M.P.H. Pediatrics, Pediatric Endocrinology, Clinical ...
There are about 1.5 million adults with Type 1 diabetes in the U.S., compared to 21 million adults with Type 2 diabetes. In terms of the total cases of diabetes, only 5 to 10 percent have Type 1 diabetes. Even in our largest epidemiologic cohorts, only a small percentage of people have Type 1 diabetes. So, we just don't have the same national ...
The new research showed that killer T-cells—a type of white blood cell that's involved in tackling bacterial infections—can cause type 1 diabetes when activated by bacteria. The researchers ...
Type 1 diabetes is a challenging condition to manage since it includes many facets such as treatment with insulin, technical devices, physiological and behavioral factors. Regular exercise is a cornerstone in diabetes treatment, but management of different forms of physical activity could be difficult for both the individual with type 1 diabetes as well as the health-care provider. People with ...
Type 1 diabetes mellitus affects 8.5 million people globally and is characterized by autoimmune destruction of pancreatic β cells. This Review discusses cell replacement therapies for T1DM and ...
SDRI is on the cutting edge of research for those living with type 1 diabetes. Our focus on improving glucose control and decreasing the need for insulin remains at the forefront of our mission. 1.84 million Americans have type 1 diabetes, which is expected to increase to 5 million people by 2050. Today, 200,000 people under the age of 20 have ...
A new large-scale longitudinal study, led by the Keck School of Medicine of USC, will unite 12 research centers across the United States to explore how type 1 diabetes affects children during a window of time known to be critical for healthy brain development. Ultimately, the findings could help refine clinical guidelines for managing type
The study is also unusual in its commitment to recruiting a racially, ethnically and income-diverse group of participants. Most past research on type 1 diabetes has looked primarily at white children. "We want to translate these insights into real-world opportunities that can help the greatest number of children with diabetes," Page said.
Type 1 diabetes mellitus (T1D) is an autoimmune disease that leads to the destruction of insulin-producing pancreatic beta cells. There is heterogeneity in the metabolic, genetic, and immunogenetic characteristics of T1D and age-related differences, requiring a personalized approach for each individual. Loss of insulin secretion can occur quickly or gradually. Residual insulin production ...
Current Research. Diabetes Action is committed to funding promising and innovative research to prevent, treat, and cure type 1 and type 2 diabetes and their complications. The following studies are currently being funded by Diabetes Action.
The Keck School of Medicine of USC has announced the launch of a nationwide longitudinal study aimed at understanding how type 1 diabetes impacts brain development in children. Funded by a $2.7 million grant from the National Institutes of Health, this multi-site study will involve collaboration among 12 research centers across the United States.
The ADA is committed to innovation and breakthrough research that will improve the lives of all people living with diabetes. ADA Research: Science. Progress. Hope. ADA research provides critical funding for diabetes research. With 100% of donations directed to research, our goal is to ensure adequate financial resources to support innovative ...
Our immune system normally protects us against infection and illness. But in Type 1 diabetes, the immune system attacks the cells in the pancreas that make insulin - the hormone responsible for regulating levels of glucose in the blood. Scientists are working hard to find out what causes this to happen. Find out about the research we're funding below. We've also linked up with Steve Morgan ...