- Applying For Scholarships

Why I Deserve This Scholarship Essay Examples 2023
Jennifer Finetti Aug 3, 2022
Get our best scholarship practices, insights & tips delivered to your inbox
Thank you for subscribing!
One of the most popular scholarship essay questions is “Why do you deserve this scholarship?” Answering such a question can be difficult because you don’t want to sound too needy or greedy. Your essay must stand out from the competition while still being humble and appreciative. Check out these essay writing tips, along with a scholarship essay sample about why I deserve the scholarship.
Tips for writing a “Why do you deserve this scholarship?” essay
Your essay will be unique to your experiences, but there are some general guidelines you should follow. Here are tips for writing a “why I’m deserving scholarship” essay:
- Explain how the scholarship money would contribute to your long-term goals. You’re asking the scholarship committee to invest in your future. They want to ensure their investment goes to a worthy cause. Explain how your education will play a role in your career and overall goals after graduation.
- Focus on the purpose of the scholarship. While writing your essay, keep in mind what the scholarship is for and where it comes from. Tailor your response to the scholarship so it resonates with the review committee.
- Don’t be afraid to promote yourself. This may be your only chance to tell the committee about your achievements. Showing your past success will instill confidence about your future success.
- Use a thesis statement, just like you would with any other essay. You should refer back to the thesis throughout the essay and tie it into the conclusion. If you have trouble creating the thesis at the beginning, write the rest of the essay first. Read through, see what stands out the most, and then write an intro with a cohesive thesis.
- When explaining obstacles in your life, focus on how you overcame them. Show that you’re a problem solver, able to persevere through any situation. You can mention difficulties from your past, but turn the attention to what you did as a result of them.
- Avoid generalizations. Generic statements like “I deserve this because I am a hard worker” aren’t enough. Every applicant is a hard worker, has ‘good grades,’ etc. What makes you different, special and memorable? That should be the topic of your scholarship essay.
- Support your statements with examples. Instead of saying, “I’m a hard worker,” say, “I upheld two jobs while I was in high school to support my family, and I still maintained a 3.75 GPA.” This is no longer a generalization. It is an achievement specific to your life and upbringing.
- Use positive language. Phrases like ‘well-prepared,’ ‘qualified candidate’ and ‘specialized training’ showcase achievements in a positive light. Even in a negative situation, show the positive way you got through it.
- Avoid words like ‘very’ and ‘really.’ You can typically find a one-word substitute that sounds more professional. Very hard turns into difficult. Very good becomes exceptional. Here is an excellent guide for modifiers that replace very .
- Take a one-day break before you edit. Once you have a solid draft written, do not jump straight into editing. Wait a day before looking over your essay. This will let you read the essay with fresh eyes so you can catch inconsistencies, grammar mistakes, and more.

Example 1: Why I deserve this scholarship essay (100 words)
With a 100 word scholarship essay, you need to jump into the thesis as quickly as possible. There is not enough space for a lengthy introduction. Use concise language, and showcase your biggest achievements/goals. You should have enough sentences to break into two small paragraphs, though one may only be two to three sentences.
The fastest path to earning scholarships
Simplify and focus your application process with the one-stop platform for vetted scholarships.
I believe I deserve this scholarship because I am an innovative problem solver. As the student council president, I helped re-organize my school library to better accommodate students’ needs. I worked with staff to categorize books to better reflect current school subjects. I will use the same leadership mindset to obtain my business degree with a focus on project management. My goal is to work in construction management to increase efficiency in low-income housing development. With this scholarship and the need-based grants I will receive, I can complete my education and continue to solve problems within my community.
Word Count: 98
Example 2: Why I deserve this scholarship essay (250 words)
A 250-word scholarship essay usually consists of 4-5 paragraphs. The introduction can have a short lead-in, but it should arrive at the thesis quickly. The body paragraphs should support the assertion made in the first paragraph (the reason you deserve the scholarship). The conclusion should summarize the essay collectively, and it may include a statement of appreciation.
One of the most debated topics in America is how to provide affordable healthcare to the masses. I believe the answer lies in accessible healthcare providers. Nurse practitioners often go unappreciated and unrecognized for their versatility and value in the medical profession. With this scholarship, I could continue my training to become a nurse practitioner and provide attainable medical services to underserved communities. Growing up in a small Montana farming town, the closest hospital was 45 minutes away. The only local family doctor charged whatever he wanted because he was the sole provider. My parents relied on home remedies to treat any ailment my brother and I developed. This is when my passion for medicine first took form. Minimal medical care was not a concern until my father went to the hospital for severe stomach problems. These were the result of Crohn’s disease, a condition that can be managed with treatment. Because my father had not been to the doctor in years, the flare up was highly aggressive. It took months to get it under control and get him on preventative medication. I decided to go to college to help people like my father. As a nurse practitioner I can practice medicine without charging a fortune for my services. I plan to serve in rural communities where hospitals and doctors are limited or non-existent. I am grateful to be considered for this scholarship opportunity, and should I be selected, I will use it to advance my medical education.
Word Count: 248

Example 3: Why I deserve this scholarship essay (500 words)
With a 500-word scholarship essay, you have room to tell your story and create an experience for the reader. Use several introductory sentences to lead into your thesis and set the tone for the essay. The body paragraph should flow in a logical manner, most often chronologically. Then the conclusion should re-emphasize the thesis and leave the scholarship committee with something to remember.
Winston Churchill once said, “Success consists of going from failure to failure without loss of enthusiasm.” And while I never define my obstacles as ‘failures,’ I mark my success by my repeated perseverance through adversity. I have faced several challenges over the years, from dyslexia to homelessness; yet I continued to earn exemplary grades and graduate at the top of my class. I deserve this scholarship because I have the strength and determination to achieve my goals, no matter what hurdles I have to overcome. I was not born a gifted student. Testing and assignments were always difficult for me, whether I studied or not. In second grade, my parents had me tested for learning disabilities. The psychologist said that I had a hyperactivity disorder and prescribed medication to suppress my energy. After two years abiding by that treatment, I was re-evaluated and diagnosed with dyslexia. This helped me get the treatment I needed, and I finally made progress in school. Shortly after I learned how to study with dyslexia, my father lost his job. He was the sole breadwinner for the household, and I was soon on the street with my mother and two younger siblings. I got a job in newspaper delivery, one of the few fields that will hire a 12-year-old. My father found odd jobs to bring money to the family, and together we were eventually able to pay for a two-bedroom apartment to live in. I was valedictorian that school year, and I maintained a perfect attendance record. Like my father, I knew I had to do whatever was necessary to succeed and thrive. In high school, I developed an interest for psychology. I noticed patterns in behaviors, both in myself and in the people around me. I asked my child therapist, the one who officially diagnosed me with dyslexia, if I could work at his clinic over the summers. He allowed me to intern at his counseling center my junior and senior year, and I gained valuable insight into the business side of psychology. I am now entering the second year of my psychology degree. I plan to complete my bachelor’s degree and earn a Doctorate of Neuropsychology in the years that follow. My focus is on psychological testing, specifically for children with autism or learning disabilities. I spent years struggling in school because of a preventable misdiagnosis. I want to ensure that other children do not face the same struggles in their future. Why do I deserve this scholarship? Because I have the passion and determination to become a trusted member of the psychological community. With my education, I can help children get the treatment they need at an early age, giving the best chance at finding their own success. You’re not just helping me get through college. You’re improving the quality of life for countless families to come. I appreciate your consideration, and I look forward to building a lasting relationship with your organization.
Word Count: 492
You Should Also Read…
How to Write a Scholarship Motivation Letter
Why Are You Applying to This Scholarship Essay (with Example)
How to Write a Scholarship Essay Introduction (With Example)
How to End a Scholarship Essay
How to Write a Great 250-Word Essay
How to Write a Great 500 Word Essay
5 People Who Should Review Your Scholarship Essays
- Scholarship Essay

Jennifer Finetti
As a parent who recently helped her own kids embark on their college journeys, Jennifer approaches the transition from high school to college from a unique perspective. She truly enjoys engaging with students – helping them to build the confidence, knowledge, and insight needed to pursue their educational and career goals, while also empowering them with the strategies and skills needed to access scholarships and financial aid that can help limit college costs. She understands the importance of ensuring access to the edtech tools and resources that can make this process easier and more equitable - this drive to support underserved populations is what drew her to ScholarshipOwl. Jennifer has coached students from around the world, as well as in-person with local students in her own community. Her areas of focus include career exploration, major selection, college search and selection, college application assistance, financial aid and scholarship consultation, essay review and feedback, and more. She works with students who are at the top of their class, as well as those who are struggling. She firmly believes that all students, regardless of their circumstances, can succeed if they stay focused and work hard in school. Jennifer earned her MA in Counseling Psychology from National University, and her BA in Psychology from University of California, Santa Cruz.
Related Stories View All

Computer Science Scholarships

College Baseball Scholarships

Foot Locker Scholarship
Get started with scholarshipowl.
Simplify and focus your application process with the one-stop platform for vetted scholarships
10 Successful Medical School Essays
Sponsored by.

-- Accepted to: Harvard Medical School GPA: 4.0 MCAT: 522
Sponsored by A ccepted.com : Great stats don’t assure acceptance to elite medical schools. The personal statement, most meaningful activities, activity descriptions, secondaries and interviews can determine acceptance or rejection. Since 1994, Accepted.com has guided medical applicants just like you to present compelling medical school applications. Get Accepted !
I started writing in 8th grade when a friend showed me her poetry about self-discovery and finding a voice. I was captivated by the way she used language to bring her experiences to life. We began writing together in our free time, trying to better understand ourselves by putting a pen to paper and attempting to paint a picture with words. I felt my style shift over time as I grappled with challenges that seemed to defy language. My poems became unstructured narratives, where I would use stories of events happening around me to convey my thoughts and emotions. In one of my earliest pieces, I wrote about a local boy’s suicide to try to better understand my visceral response. I discussed my frustration with the teenage social hierarchy, reflecting upon my social interactions while exploring the harms of peer pressure.
In college, as I continued to experiment with this narrative form, I discovered medical narratives. I have read everything from Manheimer’s Bellevue to Gawande’s Checklist and from Nuland’s observations about the way we die, to Kalanithi’s struggle with his own decline. I even experimented with this approach recently, writing a piece about my grandfather’s emphysema. Writing allowed me to move beyond the content of our relationship and attempt to investigate the ways time and youth distort our memories of the ones we love. I have augmented these narrative excursions with a clinical bioethics internship. In working with an interdisciplinary team of ethics consultants, I have learned by doing by participating in care team meetings, synthesizing discussions and paths forward in patient charts, and contributing to an ongoing legislative debate addressing the challenges of end of life care. I have also seen the ways ineffective intra-team communication and inter-personal conflicts of beliefs can compromise patient care.
Writing allowed me to move beyond the content of our relationship and attempt to investigate the ways time and youth distort our memories of the ones we love.
By assessing these difficult situations from all relevant perspectives and working to integrate the knowledge I’ve gained from exploring narratives, I have begun to reflect upon the impact the humanities can have on medical care. In a world that has become increasingly data driven, where patients can so easily devolve into lists of numbers and be forced into algorithmic boxes in search of an exact diagnosis, my synergistic narrative and bioethical backgrounds have taught me the importance of considering the many dimensions of the human condition. I am driven to become a physician who deeply considers a patient’s goal of care and goals of life. I want to learn to build and lead patient care teams that are oriented toward fulfilling these goals, creating an environment where family and clinician conflict can be addressed efficiently and respectfully. Above all, I look forward to using these approaches to keep the person beneath my patients in focus at each stage of my medical training, as I begin the task of translating complex basic science into excellent clinical care.
In her essay for medical school, Morgan pitches herself as a future physician with an interdisciplinary approach, given her appreciation of how the humanities can enable her to better understand her patients. Her narrative takes the form of an origin story, showing how a childhood interest in poetry grew into a larger mindset to keep a patient’s humanity at the center of her approach to clinical care.
This narrative distinguishes Morgan as a candidate for medical school effectively, as she provides specific examples of how her passions intersect with medicine. She first discusses how she used poetry to process her emotional response to a local boy’s suicide and ties in concern about teenage mental health. Then, she discusses more philosophical questions she encountered through reading medical narratives, which demonstrates her direct interest in applying writing and the humanities to medicine. By making the connection from this larger theme to her own reflections on her grandfather, Morgan provides a personal insight that will give an admissions officer a window into her character. This demonstrates her empathy for her future patients and commitment to their care.
Her narrative takes the form of an origin story, showing how a childhood interest in poetry grew into a larger mindset to keep a patient's humanity at the center of her approach to clinical care.
Furthermore, it is important to note that Morgan’s essay does not repeat anything in-depth that would otherwise be on her resume. She makes a reference to her work in care team meetings through a clinical bioethics internship, but does not focus on this because there are other places on her application where this internship can be discussed. Instead, she offers a more reflection-based perspective on the internship that goes more in-depth than a resume or CV could. This enables her to explain the reasons for interdisciplinary approach to medicine with tangible examples that range from personal to professional experiences — an approach that presents her as a well-rounded candidate for medical school.
Disclaimer: With exception of the removal of identifying details, essays are reproduced as originally submitted in applications; any errors in submissions are maintained to preserve the integrity of the piece. The Crimson's news and opinion teams—including writers, editors, photographers, and designers—were not involved in the production of this article.
-- Accepted To: A medical school in New Jersey with a 3% acceptance rate. GPA: 3.80 MCAT: 502 and 504
Sponsored by E fiie Consulting Group : “ EFIIE ” boasts 100% match rate for all premedical and predental registered students. Not all students are accepted unto their pre-health student roster. Considered the most elite in the industry and assists from start to end – premed to residency. EFIIE is a one-stop-full-service education firm.
"To know even one life has breathed easier because you have lived. This is to have succeeded." – Ralph Waldo Emerson.
The tribulations I've overcome in my life have manifested in the compassion, curiosity, and courage that is embedded in my personality. Even a horrific mishap in my life has not changed my core beliefs and has only added fuel to my intense desire to become a doctor. My extensive service at an animal hospital, a harrowing personal experience, and volunteering as an EMT have increased my appreciation and admiration for the medical field.
At thirteen, I accompanied my father to the Park Home Animal Hospital with our eleven-year-old dog, Brendan. He was experiencing severe pain due to an osteosarcoma, which ultimately led to the difficult decision to put him to sleep. That experience brought to light many questions regarding the idea of what constitutes a "quality of life" for an animal and what importance "dignity" plays to an animal and how that differs from owner to owner and pet to pet. Noting my curiosity and my relative maturity in the matter, the owner of the animal hospital invited me to shadow the professional staff. Ten years later, I am still part of the team, having made the transition from volunteer to veterinarian technician. Saving a life, relieving pain, sharing in the euphoria of animal and owner reuniting after a procedure, to understanding the emotions of losing a loved one – my life was forever altered from the moment I stepped into that animal hospital.
As my appreciation for medical professionals continued to grow, a horrible accident created an indelible moment in my life. It was a warm summer day as I jumped onto a small boat captained by my grandfather. He was on his way to refill the boat's gas tank at the local marina, and as he pulled into the dock, I proceeded to make a dire mistake. As the line was thrown from the dock, I attempted to cleat the bowline prematurely, and some of the most intense pain I've ever felt in my life ensued.
Saving a life, relieving pain, sharing in the euphoria of animal and owner reuniting after a procedure, to understanding the emotions of losing a loved one – my life was forever altered from the moment I stepped into that animal hospital.
"Call 911!" I screamed, half-dazed as I witnessed blood gushing out of my open wounds, splashing onto the white fiberglass deck of the boat, forming a small puddle beneath my feet. I was instructed to raise my hand to reduce the bleeding, while someone wrapped an icy towel around the wound. The EMTs arrived shortly after and quickly drove me to an open field a short distance away, where a helicopter seemed to instantaneously appear.
The medevac landed on the roof of Stony Brook Hospital before I was expeditiously wheeled into the operating room for a seven-hour surgery to reattach my severed fingers. The distal phalanges of my 3rd and 4th fingers on my left hand had been torn off by the rope tightening on the cleat. I distinctly remember the chill from the cold metal table, the bright lights of the OR, and multiple doctors and nurses scurrying around. The skill and knowledge required to execute multiple skin graft surgeries were impressive and eye-opening. My shortened fingers often raise questions by others; however, they do not impair my self-confidence or physical abilities. The positive outcome of this trial was the realization of my intense desire to become a medical professional.
Despite being the patient, I was extremely impressed with the dedication, competence, and cohesiveness of the medical team. I felt proud to be a critical member of such a skilled group. To this day, I still cannot explain the dichotomy of experiencing being the patient, and concurrently one on the professional team, committed to saving the patient. Certainly, this experience was a defining part of my life and one of the key contributors to why I became an EMT and a volunteer member of the Sample Volunteer Ambulance Corps. The startling ring of the pager, whether it is to respond to an inebriated alcoholic who is emotionally distraught or to help bring breath to a pulseless person who has been pulled from the family swimming pool, I am committed to EMS. All of these events engender the same call to action and must be reacted to with the same seriousness, intensity, and magnanimity. It may be some routine matter or a dire emergency; this is a role filled with uncertainty and ambiguity, but that is how I choose to spend my days. My motives to become a physician are deeply seeded. They permeate my personality and emanate from my desire to respond to the needs of others. Through a traumatic personal event and my experiences as both a professional and volunteer, I have witnessed firsthand the power to heal the wounded and offer hope. Each person defines success in different ways. To know even one life has been improved by my actions affords me immense gratification and meaning. That is success to me and why I want to be a doctor.
This review is provided by EFIIE Consulting Group’s Pre-Health Senior Consultant Jude Chan
This student was a joy to work with — she was also the lowest MCAT profile I ever accepted onto my roster. At 504 on the second attempt (502 on her first) it would seem impossible and unlikely to most that she would be accepted into an allopathic medical school. Even for an osteopathic medical school this score could be too low. Additionally, the student’s GPA was considered competitive at 3.80, but it was from a lower ranked, less known college, so naturally most advisors would tell this student to go on and complete a master’s or postbaccalaureate program to show that she could manage upper level science classes. Further, she needed to retake the MCAT a third time.
However, I saw many other facets to this student’s history and life that spoke volumes about the type of student she was, and this was the positioning strategy I used for her file. Students who read her personal statement should know that acceptance is contingent on so much more than just an essay and MCAT score or GPA. Although many students have greater MCAT scores than 504 and higher GPAs than 3.80, I have helped students with lower scores and still maintained our 100% match rate. You are competing with thousands of candidates. Not every student out there requires our services and we are actually grateful that we can focus on a limited amount out of the tens of thousands that do. We are also here for the students who wish to focus on learning well the organic chemistry courses and physics courses and who want to focus on their research and shadowing opportunities rather than waste time deciphering the next step in this complex process. We tailor a pathway for each student dependent on their health care career goals, and our partnerships with non-profit organizations, hospitals, physicians and research labs allow our students to focus on what matters most — the building up of their basic science knowledge and their exposure to patients and patient care.
Students who read her personal statement should know that acceptance is contingent on so much more than just an essay and MCAT score or GPA.
Even students who believe that their struggle somehow disqualifies them from their dream career in health care can be redeemed if they are willing to work for it, just like this student with 502 and 504 MCAT scores. After our first consult, I saw a way to position her to still be accepted into an MD school in the US — I would not have recommended she register to our roster if I did not believe we could make a difference. Our rosters have a waitlist each semester, and it is in our best interest to be transparent with our students and protect our 100% record — something I consider a win-win. It is unethical to ever guarantee acceptance in admissions as we simply do not control these decisions. However, we respect it, play by the rules, and help our students stay one step ahead by creating an applicant profile that would be hard for the schools to ignore.
This may be the doctor I go to one day. Or the nurse or dentist my children or my grandchildren goes to one day. That is why it is much more than gaining acceptance — it is about properly matching the student to the best options for their education. Gaining an acceptance and being incapable of getting through the next 4 or 8 years (for my MD/PhD-MSTP students) is nonsensical.
-- Accepted To: Imperial College London UCAT Score: 2740 BMAT Score: 3.9, 5.4, 3.5A
My motivation to study Medicine stems from wishing to be a cog in the remarkable machine that is universal healthcare: a system which I saw first-hand when observing surgery in both the UK and Sri Lanka. Despite the differences in sanitation and technology, the universality of compassion became evident. When volunteering at OSCE training days, I spoke to many medical students, who emphasised the importance of a genuine interest in the sciences when studying Medicine. As such, I have kept myself informed of promising developments, such as the use of monoclonal antibodies in cancer therapy. After learning about the role of HeLa cells in the development of the polio vaccine in Biology, I read 'The Immortal Life of Henrietta Lacks' to find out more. Furthermore, I read that surface protein CD4 can be added to HeLa cells, allowing them to be infected with HIV, opening the possibility of these cells being used in HIV research to produce more life-changing drugs, such as pre-exposure prophylaxis (PreP). Following my BioGrad laboratory experience in HIV testing, and time collating data for research into inflammatory markers in lung cancer, I am also interested in pursuing a career in medical research. However, during a consultation between an ENT surgeon and a thyroid cancer patient, I learnt that practising medicine needs more than a scientific aptitude. As the surgeon explained that the cancer had metastasised to her liver, I watched him empathetically tailor his language for the patient - he avoided medical jargon and instead gave her time to come to terms with this. I have been developing my communication skills by volunteering weekly at care homes for 3 years, which has improved my ability to read body language and structure conversations to engage with the residents, most of whom have dementia.
However, during a consultation between an ENT surgeon and a thyroid cancer patient, I learnt that practising medicine needs more than a scientific aptitude.
Jude’s essay provides a very matter-of-fact account of their experience as a pre-medical student. However, they deepen this narrative by merging two distinct cultures through some common ground: a universality of compassion. Using clear, concise language and a logical succession of events — much like a doctor must follow when speaking to patients — Jude shows their motivation to go into the medical field.
From their OSCE training days to their school’s Science society, Jude connects their analytical perspective — learning about HeLa cells — to something that is relatable and human, such as a poor farmer’s notable contribution to science. This approach provides a gateway into their moral compass without having to explicitly state it, highlighting their fervent desire to learn how to interact and communicate with others when in a position of authority.
Using clear, concise language and a logical succession of events — much like a doctor must follow when speaking to patients — Jude shows their motivation to go into the medical field.
Jude’s closing paragraph reminds the reader of the similarities between two countries like the UK and Sri Lanka, and the importance of having a universal healthcare system that centers around the just and “world-class” treatment of patients. Overall, this essay showcases Jude’s personal initiative to continue to learn more and do better for the people they serve.
While the essay could have benefited from better transitions to weave Jude’s experiences into a personal story, its strong grounding in Jude’s motivation makes for a compelling application essay.
-- Accepted to: Weill Cornell Medical College GPA: 3.98 MCAT: 521
Sponsored by E fie Consulting Group : “ EFIIE ” boasts 100% match rate for all premedical and predental registered students. Not all students are accepted unto their pre-health student roster. Considered the most elite in the industry and assists from start to end – premed to residency. EFIIE is a one-stop-full-service education firm.
Following the physician’s unexpected request, we waited outside, anxiously waiting to hear the latest update on my father’s condition. It was early on in my father’s cancer progression – a change that had shaken our entire way of life overnight. During those 18 months, while my mother spent countless nights at the hospital, I took on the responsibility of caring for my brother. My social life became of minimal concern, and the majority of my studying for upcoming 12th- grade exams was done at the hospital. We were allowed back into the room as the physician walked out, and my parents updated us on the situation. Though we were a tight-knit family and my father wanted us to be present throughout his treatment, what this physician did was give my father a choice. Without making assumptions about who my father wanted in the room, he empowered him to make that choice independently in private. It was this respect directed towards my father, the subsequent efforts at caring for him, and the personal relationship of understanding they formed, that made the largest impact on him. Though my decision to pursue medicine came more than a year later, I deeply valued what these physicians were doing for my father, and I aspired to make a similar impact on people in the future.
It was during this period that I became curious about the human body, as we began to learn physiology in more depth at school. In previous years, the problem-based approach I could take while learning math and chemistry were primarily what sparked my interest. However, I became intrigued by how molecular interactions translated into large-scale organ function, and how these organ systems integrated together to generate the extraordinary physiological functions we tend to under-appreciate. I began my undergraduate studies with the goal of pursuing these interests, whilst leaning towards a career in medicine. While I was surprised to find that there were upwards of 40 programs within the life sciences that I could pursue, it broadened my perspective and challenged me to explore my options within science and healthcare. I chose to study pathobiology and explore my interests through hospital volunteering and research at the end of my first year.
Though my decision to pursue medicine came more than a year later, I deeply valued what these physicians were doing for my father, and I aspired to make a similar impact on people in the future.
While conducting research at St. Michael’s Hospital, I began to understand methods of data collection and analysis, and the thought process of scientific inquiry. I became acquainted with the scientific literature, and the experience transformed how I thought about the concepts I was learning in lecture. However, what stood out to me that summer was the time spent shadowing my supervisor in the neurosurgery clinic. It was where I began to fully understand what life would be like as a physician, and where the career began to truly appeal to me. What appealed to me most was the patient-oriented collaboration and discussions between my supervisor and his fellow; the physician-patient relationship that went far beyond diagnoses and treatments; and the problem solving that I experienced first-hand while being questioned on disease cases.
The day spent shadowing in the clinic was also the first time I developed a relationship with a patient. We were instructed to administer the Montreal cognitive assessment (MoCA) test to patients as they awaited the neurosurgeon. My task was to convey the instructions as clearly as possible and score each section. I did this as best I could, adapting my explanation to each patient, and paying close attention to their responses to ensure I was understood. The last patient was a challenging case, given a language barrier combined with his severe hydrocephalus. It was an emotional time for his family, seeing their father/husband struggle to complete simple tasks and subsequently give up. I encouraged him to continue trying. But I also knew my words would not remedy the condition underlying his struggles. All I could do was make attempts at lightening the atmosphere as I got to know him and his family better. Hours later, as I saw his remarkable improvement following a lumbar puncture, and the joy on his and his family’s faces at his renewed ability to walk independently, I got a glimpse of how rewarding it would be to have the ability and privilege to care for such patients. By this point, I knew I wanted to commit to a life in medicine. Two years of weekly hospital volunteering have allowed me to make a small difference in patients’ lives by keeping them company through difficult times, and listening to their concerns while striving to help in the limited way that I could. I want to have the ability to provide care and treatment on a daily basis as a physician. Moreover, my hope is that the breadth of medicine will provide me with the opportunity to make an impact on a larger scale. Whilst attending conferences on neuroscience and surgical technology, I became aware of the potential to make a difference through healthcare, and I look forward to developing the skills necessary to do so through a Master’s in Global Health. Whether through research, health innovation, or public health, I hope not only to care for patients with the same compassion with which physicians cared for my father, but to add to the daily impact I can have by tackling large-scale issues in health.
Taylor’s essay offers both a straightforward, in-depth narrative and a deep analysis of his experiences, which effectively reveals his passion and willingness to learn in the medical field. The anecdote of Taylor’s father gives the reader insight into an original instance of learning through experience and clearly articulates Taylor’s motivations for becoming a compassionate and respectful physician.
Taylor strikes an impeccable balance between discussing his accomplishments and his character. All of his life experiences — and the difficult challenges he overcame — introduce the reader to an important aspect of Taylor’s personality: his compassion, care for his family, and power of observation in reflecting on the decisions his father’s doctor makes. His description of his time volunteering at St. Michael’s Hospital is indicative of Taylor’s curiosity about medical research, but also of his recognition of the importance of the patient-physician relationship. Moreover, he shows how his volunteer work enabled him to see how medicine goes “beyond diagnoses and treatments” — an observation that also speaks to his compassion.
His description of his time volunteering at St. Michael's Hospital is indicative of Taylor's curiosity about medical research, but also of his recognition of the importance of the patient-physician relationship.
Finally, Taylor also tells the reader about his ambition and purpose, which is important when thinking about applying to medical school. He discusses his hope of tackling larger scale problems through any means possible in medicine. This notion of using self interest to better the world is imperative to a successful college essay, and it is nicely done here.
-- Accepted to: Washington University
Sponsored by A dmitRx : We are a group of Chicago-based medical students who realize how challenging medical school admissions can be, so we want to provide our future classmates with resources we wish we had. Our mission at AdmitRx is to provide pre-medical students with affordable, personalized, high-quality guidance towards becoming an admitted medical student.
Running has always been one of my greatest passions whether it be with friends or alone with my thoughts. My dad has always been my biggest role model and was the first to introduce me to the world of running. We entered races around the country, and one day he invited me on a run that changed my life forever. The St. Jude Run is an annual event that raises millions of dollars for St. Jude Children’s Research Hospital. My dad has led or our local team for as long as I can remember, and I had the privilege to join when I was 16. From the first step I knew this was the environment for me – people from all walks of life united with one goal of ending childhood cancer. I had an interest in medicine before the run, and with these experiences I began to consider oncology as a career. When this came up in conversations, I would invariably be faced with the question “Do you really think you could get used to working with dying kids?” My 16-year-old self responded with something noble but naïve like “It’s important work, so I’ll have to handle it”. I was 16 years young with my plan to become an oncologist at St. Jude.
As I transitioned into college my plans for oncology were alive and well. I began working in a biochemistry lab researching new anti-cancer drugs. It was a small start, but I was overjoyed to be a part of the process. I applied to work at a number of places for the summer, but the Pediatric Oncology Education program (POE) at St. Jude was my goal. One afternoon, I had just returned from class and there it was: an email listed as ‘POE Offer’. I was ecstatic and accepted the offer immediately. Finally, I could get a glimpse at what my future holds. My future PI, Dr. Q, specialized in solid tumor translational research and I couldn’t wait to get started.
I was 16 years young with my plan to become an oncologist at St. Jude.
Summer finally came, I moved to Memphis, and I was welcomed by the X lab. I loved translational research because the results are just around the corner from helping patients. We began a pre-clinical trial of a new chemotherapy regimen and the results were looking terrific. I was also able to accompany Dr. Q whenever she saw patients in the solid tumor division. Things started simple with rounds each morning before focusing on the higher risk cases. I was fortunate enough to get to know some of the patients quite well, and I could sometimes help them pass the time with a game or two on a slow afternoon between treatments. These experiences shined a very human light on a field I had previously seen only through a microscope in a lab.
I arrived one morning as usual, but Dr. Q pulled me aside before rounds. She said one of the patients we had been seeing passed away in the night. I held my composure in the moment, but I felt as though an anvil was crushing down on me. It was tragic but I knew loss was part of the job, so I told myself to push forward. A few days later, I had mostly come to terms with what happened, but then the anvil came crashing back down with the passing of another patient. I could scarcely hold back the tears this time. That moment, it didn’t matter how many miraculous successes were happening a few doors down. Nothing overshadowed the loss, and there was no way I could ‘get used to it’ as my younger self had hoped.
I was still carrying the weight of what had happened and it was showing, so I asked Dr. Q for help. How do you keep smiling each day? How do you get used to it? The questions in my head went on. What I heard next changed my perspective forever. She said you keep smiling because no matter what happened, you’re still hope for the next patient. It’s not about getting used to it. You never get used to it and you shouldn’t. Beating cancer takes lifetimes, and you can’t look passed a life’s worth of hardships. I realized that moving passed the loss of patients would never suffice, but I need to move forward with them. Through the successes and shortcomings, we constantly make progress. I like to imagine that in all our future endeavors, it is the hands of those who have gone before us that guide the way. That is why I want to attend medical school and become a physician. We may never end the sting of loss, but physicians are the bridge between the past and the future. No where else is there the chance to learn from tragedy and use that to shape a better future. If I can learn something from one loss, keep moving forward, and use that knowledge to help even a single person – save one life, bring a moment of joy, avoid a moment of pain—then that is how I want to spend my life.
The change wasn’t overnight. The next loss still brought pain, but I took solace in moving forward so that we might learn something to give hope to a future patient. I returned to campus in a new lab doing cancer research, and my passion for medicine continues to flourish. I still think about all the people I encountered at St. Jude, especially those we lost. It might be a stretch, but during the long hours at the lab bench I still picture their hands moving through mine each step of the way. I could never have foreseen where the first steps of the St. Jude Run would bring me. I’m not sure where the road to becoming a physician may lead, but with helping hands guiding the way, I won’t be running it alone.
This essay, a description of the applicant’s intellectual challenges, displays the hardships of tending to cancer patients as a milestone of experience and realization of what it takes to be a physician. The writer explores deeper ideas beyond medicine, such as dealing with patient deaths in a way to progress and improve as a professional. In this way, the applicant gives the reader some insight into the applicant’s mindset, and their ability to think beyond the surface for ways to become better at what they do.
However, the essay fails to zero in on the applicant’s character, instead elaborating on life events that weakly illustrate the applicant’s growth as a physician. The writer’s mantra (“keep moving forward”) is feebly projected, and seems unoriginal due to the lack of a personalized connection between the experience at St. Jude and how that led to the applicant’s growth and mindset changes.
The writer explores deeper ideas beyond medicine, such as dealing with patient deaths in a way to progress and improve as a professional.
The writer, by only focusing on grief brought from patient deaths at St. Jude, misses out on the opportunity to further describe his or her experience at the hospital and portray an original, well-rounded image of his or her strengths, weaknesses, and work ethic.
The applicant ends the essay by attempting to highlight the things they learned at St. Jude, but fails to organize the ideas into a cohesive, comprehensible section. These ideas are also too abstract, and are vague indicators of the applicant’s character that are difficult to grasp.
-- Accepted to: New York University School of Medicine
Sponsored by MedEdits : MedEdits Medical Admissions has been helping applicants get into medical schools like Harvard for more than ten years. Structured like an academic medical department, MedEdits has experts in admissions, writing, editing, medicine, and interview prep working with you collaboratively so you can earn the best admissions results possible.
“Is this the movie you were talking about Alice?” I said as I showed her the movie poster on my iPhone. “Oh my God, I haven’t seen that poster in over 70 years,” she said with her arms trembling in front of her. Immediately, I sat up straight and started to question further. We were talking for about 40 minutes, and the most exciting thing she brought up in that time was the new flavor of pudding she had for lunch. All of sudden, she’s back in 1940 talking about what it was like to see this movie after school for only 5¢ a ticket! After an engaging discussion about life in the 40’s, I knew I had to indulge her. Armed with a plethora of movie streaming sights, I went to work scouring the web. No luck. The movie, “My Son My Son,” was apparently not in high demand amongst torrenting teens. I had to entreat my older brother for his Amazon Prime account to get a working stream. However, breaking up the monotony and isolation felt at the nursing home with a simple movie was worth the pandering.
While I was glad to help a resident have some fun, I was partly motivated by how much Alice reminded me of my own grandfather. In accordance with custom, my grandfather was to stay in our house once my grandmother passed away. More specifically, he stayed in my room and my bed. Just like grandma’s passing, my sudden roommate was a rough transition. In 8th grade at the time, I considered myself to be a generally good guy. Maybe even good enough to be a doctor one day. I volunteered at the hospital, shadowed regularly, and had a genuine interest for science. However, my interest in medicine was mostly restricted to academia. To be honest, I never had a sustained exposure to the palliative side of medicine until the arrival of my new roommate.
The two years I slept on that creaky wooden bed with him was the first time my metal was tested. Sharing that room, I was the one to take care of him. I was the one to rub ointment on his back, to feed him when I came back from school, and to empty out his spittoon when it got full. It was far from glamorous, and frustrating most of the time. With 75 years separating us, and senile dementia setting in, he would often forget who I was or where he was. Having to remind him that I was his grandson threatened to erode at my resolve. Assured by my Syrian Orthodox faith, I even prayed about it; asking God for comfort and firmness on my end. Over time, I grew slow to speak and eager to listen as he started to ramble more and more about bits and pieces of the past. If I was lucky, I would be able to stich together a narrative that may or may have not been true. In any case, my patience started to bud beyond my age group.
Having to remind him that I was his grandson threatened to erode at my resolve.
Although I grew more patient with his disease, my curiosity never really quelled. Conversely, it developed further alongside my rapidly growing interest in the clinical side of medicine. Naturally, I became drawn to a neurology lab in college where I got to study pathologies ranging from atrophy associated with schizophrenia, and necrotic lesions post stroke. However, unlike my intro biology courses, my work at the neurology lab was rooted beyond the academics. Instead, I found myself driven by real people who could potentially benefit from our research. In particular, my shadowing experience with Dr. Dominger in the Veteran’s home made the patient more relevant in our research as I got to encounter geriatric patients with age related diseases, such as Alzhimer’s and Parkinson’s. Furthermore, I had the privilege of of talking to the families of a few of these patients to get an idea of the impact that these diseases had on the family structure. For me, the scut work in the lab meant a lot more with these families in mind than the tritium tracer we were using in the lab.
Despite my achievements in the lab and the classroom, my time with my grandfather still holds a special place in my life story. The more I think about him, the more confident I am in my decision to pursue a career where caring for people is just as important, if not more important, than excelling at academics. Although it was a lot of work, the years spent with him was critical in expanding my horizons both in my personal life and in the context of medicine. While I grew to be more patient around others, I also grew to appreciate medicine beyond the science. This more holistic understanding of medicine had a synergistic effect in my work as I gained a purpose behind the extra hours in the lab, sleepless nights in the library, and longer hours volunteering. I had a reason for what I was doing that may one day help me have long conversations with my own grandchildren about the price of popcorn in the 2000’s.
The most important thing to highlight in Avery’s essay is how he is able to create a duality between his interest in not only the clinical, more academic-based side of medicine, but also the field’s personal side.
He draws personal connections between working with Alice — a patient in a hospital or nursing home — and caring intensely for his grandfather. These two experiences build up the “synergistic” relationship between caring for people and studying the science behind medicine. In this way, he is able to clearly state his passions for medicine and explain his exact motives for entering the field. Furthermore, in his discussion of her grandfather, he effectively employs imagery (“rub ointment on his back,” “feed him when I came back from school,” etc.) to describe the actual work that he does, calling it initially as “far from glamorous, and frustrating most of the time.” By first mentioning his initial impression, then transitioning into how he grew to appreciate the experience, Avery is able to demonstrate a strength of character, sense of enormous responsibility and capability, and open-minded attitude.
He draws personal connections between working with Alice — a patient in a hospital or nursing home — and caring intensely for his grandfather.
Later in the essay, Avery is also able to relate his time caring for his grandfather to his work with Alzheimer’s and Parkinson’s patients, showcasing the social impact of his work, as the reader is likely already familiar with the biological impact of the work. This takes Avery’s essay full circle, bringing it back to how a discussion with an elderly patient about the movies reminds him of why he chose to pursue medicine.
That said, the essay does feel rushed near the end, as the writer was likely trying to remain within the word count. There could be a more developed transition before Avery introduces the last sentence about “conversations with my own grandchildren,” especially as a strong essay ending is always recommended.
-- Accepted To: Saint Louis University Medical School Direct Admission Medical Program
Sponsored by Atlas Admissions : Atlas Admissions provides expert medical school admissions consulting and test preparation services. Their experienced, physician-driven team consistently delivers top results by designing comprehensive, personalized strategies to optimize applications. Atlas Admissions is based in Boston, MA and is trusted by clients worldwide.
The tension in the office was tangible. The entire team sat silently sifting through papers as Dr. L introduced Adam, a 60-year-old morbidly obese man recently admitted for a large open wound along his chest. As Dr. L reviewed the details of the case, his prognosis became even bleaker: hypertension, diabetes, chronic kidney disease, cardiomyopathy, hyperlipidemia; the list went on and on. As the humdrum of the side-conversations came to a halt, and the shuffle of papers softened, the reality of Adam’s situation became apparent. Adam had a few months to live at best, a few days at worst. To make matters worse, Adam’s insurance would not cover his treatment costs. With no job, family, or friends, he was dying poor and alone.
I followed Dr. L out of the conference room, unsure what would happen next. “Well,” she muttered hesitantly, “We need to make sure that Adam is on the same page as us.” It’s one thing to hear bad news, and another to hear it utterly alone. Dr. L frantically reviewed all of Adam’s paperwork desperately looking for someone to console him, someone to be at his side. As she began to make calls, I saw that being a physician calls for more than good grades and an aptitude for science: it requires maturity, sacrifice, and most of all, empathy. That empathy is exactly what I saw in Dr. L as she went out of her way to comfort a patient she met hardly 20 minutes prior.
Since high school, I’ve been fascinated by technology’s potential to improve healthcare. As a volunteer in [the] Student Ambassador program, I was fortunate enough to watch an open-heart surgery. Intrigued by the confluence of technology and medicine, I chose to study biomedical engineering. At [school], I wanted to help expand this interface, so I became involved with research through Dr. P’s lab by studying the applications of electrospun scaffolds for dermal wound healing. While still in the preliminary stages of research, I learned about the Disability Service Club (DSC) and decided to try something new by volunteering at a bowling outing.
As she began to make calls, I saw that being a physician calls for more than good grades and an aptitude for science: it requires maturity, sacrifice, and most of all, empathy.
The DSC promotes awareness of cognitive disabilities in the community and seeks to alleviate difficulties for the disabled. During one outing, I collaborated with Arc, a local organization with a similar mission. Walking in, I was told that my role was to support the participants by providing encouragement. I decided to help a relatively quiet group of individuals assisted by only one volunteer, Mary. Mary informed me that many individuals with whom I was working were diagnosed with ASD. Suddenly, she started cheering, as one of the members of the group bowled a strike. The group went wild. Everyone was dancing, singing, and rejoicing. Then I noticed one gentleman sitting at our table, solemn-faced. I tried to start a conversation with him, but he remained unresponsive. I sat with him for the rest of the game, trying my hardest to think of questions that would elicit more than a monosyllabic response, but to no avail. As the game ended, I stood up to say bye when he mumbled, “Thanks for talking.” Then he quickly turned his head away. I walked away beaming. Although I was unable to draw out a smile or even sustain a conversation, at the end of the day, the fact that this gentleman appreciated my mere effort completely overshadowed the awkwardness of our time together. Later that day, I realized that as much as I enjoyed the thrill of research and its applications, helping other people was what I was most passionate about.
When it finally came time to tell Adam about his deteriorating condition, I was not sure how he would react. Dr. L gently greeted him and slowly let reality take its toll. He stoically turned towards Dr. L and groaned, “I don’t really care. Just leave me alone.” Dr. L gave him a concerned nod and gradually left the room. We walked to the next room where we met with a pastor from Adam’s church.
“Adam’s always been like that,” remarked the pastor, “he’s never been one to express emotion.” We sat with his pastor for over an hour discussing how we could console Adam. It turned out that Adam was part of a motorcycle club, but recently quit because of his health. So, Dr. L arranged for motorcycle pictures and other small bike trinkets to be brought to his room as a reminder of better times.
Dr. L’s simple gesture reminded me of why I want to pursue medicine. There is something sacred, empowering, about providing support when people need it the most; whether it be simple as starting a conversation, or providing support during the most trying of times. My time spent conducting research kindled my interest in the science of medicine, and my service as a volunteer allowed me to realize how much I valued human interaction. Science and technology form the foundation of medicine, but to me, empathy is the essence. It is my combined interest in science and service that inspires me to pursue medicine. It is that combined interest that makes me aspire to be a physician.
Parker’s essay focuses on one central narrative with a governing theme of compassionate and attentive care for patients, which is the key motivator for her application to medical school. Parker’s story focuses on her volunteer experience shadowing of Dr. L who went the extra mile for Adam, which sets Dr. L up as a role model for Parker as she enters the medical field. This effectively demonstrates to the reader what kind of doctor Parker wants to be in the future.
Parker’s narrative has a clear beginning, middle, and end, making it easy for the reader to follow. She intersperses the main narrative about Adam with experiences she has with other patients and reflects upon her values as she contemplates pursuing medicine as a career. Her anecdote about bowling with the patients diagnosed with ASD is another instance where she uses a story to tell the reader why she values helping people through medicine and attentive patient care, especially as she focuses on the impact her work made on one man at the event.
Parker's story focuses on her volunteer experience shadowing of Dr. L who went the extra mile for Adam, which sets Dr. L up as a role model for Parker as she enters the medical field.
All throughout the essay, the writing is engaging and Parker incorporates excellent imagery, which goes well with her varied sentence structure. The essay is also strong because it comes back full circle at its conclusion, tying the overall narrative back to the story of Dr. L and Adam, which speaks to Parker’s motives for going to medical school.
-- Accepted To: Emory School of Medicine
Growing up, I enjoyed visiting my grandparents. My grandfather was an established doctor, helping the sick and elderly in rural Taiwan until two weeks before he died at 91 years old. His clinic was located on the first floor of the residency with an exam room, treatment room, X-ray room, and small pharmacy. Curious about his work, I would follow him to see his patients. Grandpa often asked me if I want to be a doctor just like him. I always smiled, but was more interested in how to beat the latest Pokémon game. I was in 8th grade when my grandfather passed away. I flew back to Taiwan to attend his funeral. It was a gloomy day and the only street in the small village became a mourning place for the villagers. Flowers filled the streets and people came to pay their respects. An old man told me a story: 60 years ago, a village woman was in a difficult labor. My grandfather rushed into the house and delivered a baby boy. That boy was the old man and he was forever grateful. Stories of grandpa saving lives and bringing happiness to families were told during the ceremony. At that moment, I realized why my grandfather worked so tirelessly up until his death as a physician. He did it for the reward of knowing that he kept a family together and saved a life. The ability for a doctor to heal and bring happiness is the reason why I want to study medicine. Medical school is the first step on a lifelong journey of learning, but I feel that my journey leading up to now has taught me some things of what it means to be an effective physician.
With a newfound purpose, I began volunteering and shadowing at my local hospital. One situation stood out when I was a volunteer in the cardiac stress lab. As I attached EKG leads onto a patient, suddenly the patient collapsed and started gasping for air. His face turned pale, then slightly blue. The charge nurse triggered “Code Blue” and started CPR. A team of doctors and nurses came, rushing in with a defibrillator to treat and stabilize the patient. What I noticed was that medicine was not only about one individual acting as a superhero to save a life, but that it takes a team of individuals with an effective leader, working together to deliver the best care. I want to be a leader as well as part of a team that can make a difference in a person’s life. I have refined these lessons about teamwork and leadership to my activities. In high school I was an 8 time varsity letter winner for swimming and tennis and captain of both of those teams. In college I have participated in many activities, but notably serving as assistant principle cellist in my school symphony as well as being a co-founding member of a quartet. From both my athletic experiences and my music experiences I learned what it was like to not only assert my position as a leader and to effectively communicate my views, but equally as important I learned how to compromise and listen to the opinions of others. Many physicians that I have observed show a unique blend of confidence and humility.
What I noticed was that medicine was not only about one individual acting as a superhero to save a life, but that it takes a team of individuals with an effective leader, working together to deliver the best care.
College opened me up to new perspectives on what makes a complete physician. A concept that was preached in the Guaranteed Professional Program Admissions in Medicine (GPPA) was that medicine is both an art and a science. The art of medicine deals with a variety of aspects including patient relationships as well as ethics. Besides my strong affinity for the sciences and mathematics, I always have had interest in history. I took courses in both German literature and history, which influenced me to take a class focusing on Nazi neuroscientists. It was the ideology of seeing the disabled and different races as test subjects rather than people that led to devastating lapses in medical ethics. The most surprising fact for me was that doctors who were respected and leaders in their field disregarded the humanity of patient and rather focused on getting results from their research. Speaking with Dr. Zeidman, the professor for this course, influenced me to start my research which deals with the ethical qualms of using data derived from unethical Nazi experimentation such as the brains derived from the adult and child euthanasia programs. Today, science is so result driven, it is important to keep in mind the ethics behind research and clinical practice. Also the development of personalized genomic medicine brings into question about potential privacy violations and on the extreme end discrimination. The study of ethics no matter the time period is paramount in the medical field. The end goal should always be to put the patient first.
Teaching experiences in college inspired me to become a physician educator if I become a doctor. Post-MCAT, I was offered a job by Next Step Test Prep as a tutor to help students one on one for the MCAT. I had a student who stated he was doing well during practice, but couldn’t get the correct answer during practice tests. Working with the student, I pointed out his lack of understanding concepts and this realization helped him and improves his MCAT score. Having the ability to educate the next generation of doctors is not only necessary, but also a rewarding experience.
My experiences volunteering and shadowing doctors in the hospital as well as my understanding of what it means to be a complete physician will make me a good candidate as a medical school student. It is my goal to provide the best care to patients and to put a smile on a family’s face just as my grandfather once had. Achieving this goal does not take a special miracle, but rather hard work, dedication, and an understanding of what it means to be an effective physician.
Through reflecting on various stages of life, Quinn expresses how they found purpose in pursuing medicine. Starting as a child more interested in Pokemon than their grandfather’s patients, Quinn exhibits personal growth through recognizing the importance of their grandfather’s work saving lives and eventually gaining the maturity to work towards this goal as part of a team.
This essay opens with abundant imagery — of the grandfather’s clinic, flowers filling the streets, and the village woman’s difficult labor — which grounds Quinn’s story in their family roots. Yet, the transition from shadowing in hospitals to pursuing leadership positions in high schools is jarring, and the list of athletic and musical accomplishments reads like a laundry list of accomplishments until Quinn neatly wraps them up as evidence of leadership and teamwork skills. Similarly, the section about tutoring, while intended to demonstrate Quinn’s desire to educate future physicians, lacks the emotional resonance necessary to elevate it from another line lifted from their resume.
This essay opens with abundant imagery — of the grandfather's clinic, flowers filling the streets, and the village woman's difficult labor — which grounds Quinn's story in their family roots.
The strongest point of Quinn’s essay is the focus on their unique arts and humanities background. This equips them with a unique perspective necessary to consider issues in medicine in a new light. Through detailing how history and literature coursework informed their unique research, Quinn sets their application apart from the multitude of STEM-focused narratives. Closing the essay with the desire to help others just as their grandfather had, Quinn ties the narrative back to their personal roots.
-- Accepted To: Edinburgh University UCAT Score: 2810 BMAT Score: 4.6, 4.2, 3.5A
Exposure to the medical career from an early age by my father, who would explain diseases of the human body, sparked my interest for Medicine and drove me to seek out work experience. I witnessed the contrast between use of bone saws and drills to gain access to the brain, with subsequent use of delicate instruments and microscopes in neurosurgery. The surgeon's care to remove the tumour, ensuring minimal damage to surrounding healthy brain and his commitment to achieve the best outcome for the patient was inspiring. The chance to have such a positive impact on a patient has motivated me to seek out a career in Medicine.
Whilst shadowing a surgical team in Texas, carrying out laparoscopic bariatric procedures, I appreciated the surgeon's dedication to continual professional development and research. I was inspired to carry out an Extended Project Qualification on whether bariatric surgery should be funded by the NHS. By researching current literature beyond my school curriculum, I learnt to assess papers for bias and use reliable sources to make a conclusion on a difficult ethical situation. I know that doctors are required to carry out research and make ethical decisions and so, I want to continue developing these skills during my time at medical school.
The chance to have such a positive impact on a patient has motivated me to seek out a career in Medicine.
Attending an Oncology multi-disciplinary team meeting showed me the importance of teamwork in medicine. I saw each team member, with specific areas of expertise, contributing to the discussion and actively listening, and together they formed a holistic plan of action for patients. During my Young Enterprise Award, I facilitated a brainstorm where everyone pitched a product idea. Each member offered a different perspective on the idea and then voted on a product to carry forward in the competition. As a result, we came runners up in the Regional Finals. Furthermore, I started developing my leadership skills, which I improved by doing Duke of Edinburgh Silver and attending a St. John Ambulance Leadership course. In one workshop, similar to the bariatric surgeon I shadowed, I communicated instructions and delegated roles to my team to successfully solve a puzzle. These experiences highlighted the crucial need for teamwork and leadership as a doctor.
Observing a GP, I identified the importance of compassion and empathy. During a consultation with a severely depressed patient, the GP came to the patient's eye level and used a calm, non-judgmental tone of voice, easing her anxieties and allowing her to disclose more information. While volunteering at a care home weekly for two years, I adapted my communication for a resident suffering with dementia who was disconnected from others. I would take her to a quiet environment, speak slowly and in a non-threatening manner, as such, she became talkative, engaged and happier. I recognised that communication and compassion allows doctors to build rapport, gain patients' trust and improve compliance. For two weeks, I shadowed a surgeon performing multiple craniotomies a day. I appreciated the challenges facing doctors including time and stress management needed to deliver high quality care. Organisation, by prioritising patients based on urgency and creating a timetable on the ward round, was key to running the theatre effectively. Similarly, I create to-do-lists and prioritise my academics and extra-curricular activities to maintain a good work-life balance: I am currently preparing for my Grade 8 in Singing, alongside my A-level exams. I also play tennis for the 1st team to relax and enable me to refocus. I wish to continue my hobbies at university, as ways to manage stress.
Through my work experiences and voluntary work, I have gained a realistic understanding of Medicine and its challenges. I have begun to display the necessary skills that I witnessed, such as empathy, leadership and teamwork. The combination of these skills with my fascination for the human body drives me to pursue a place at medical school and a career as a doctor.
This essay traces Alex's personal exploration of medicine through different stages of life, taking a fairly traditional path to the medical school application essay. From witnessing medical procedures to eventually pursuing leadership positions, this tale of personal progress argues that Alex's life has prepared him to become a doctor.
Alex details how experiences conducting research and working with medical teams have confirmed his interest in medicine. Although the breadth of experiences speaks to the applicant’s interest in medicine, the essay verges on being a regurgitation of the Alex's resume, which does not provide the admissions officer with any new insights or information and ultimately takes away from the essay as a whole. As such, the writing’s lack of voice or unique perspective puts the applicant at risk of sounding middle-of-the-road.
From witnessing medical procedures to eventually pursuing leadership positions, this tale of personal progress argues that Alex's life has prepared him to become a doctor.
The essay’s organization, however, is one of its strengths — each paragraph provides an example of personal growth through a new experience in medicine. Further, Alex demonstrates his compassion and diligence through detailed stories, which give a reader a glimpse into his values. Through recognizing important skills necessary to be a doctor, Alex demonstrates that he has the mature perspective necessary to embark upon this journey.
What this essay lacks in a unique voice, it makes up for in professionalism and organization. Alex's earnest desire to attend medical school is what makes this essay shine.
-- Accepted To: University of Toronto MCAT Scores: Chemical and Physical Foundations of Biological Systems - 128, Critical Analysis and Reading Skills - 127, Biological and Biochemical Foundations of Living Systems - 127, Psychological, Social, and Biological Foundations of Behavior - 130, Total - 512
Moment of brilliance.
Revelation.
These are all words one would use to describe their motivation by a higher calling to achieve something great. Such an experience is often cited as the reason for students to become physicians; I was not one of these students. Instead of waiting for an event like this, I chose to get involved in the activities that I found most invigorating. Slowly but surely, my interests, hobbies, and experiences inspired me to pursue medicine.
As a medical student, one must possess a solid academic foundation to facilitate an understanding of physical health and illness. Since high school, I found science courses the most appealing and tended to devote most of my time to their exploration. I also enjoyed learning about the music, food, literature, and language of other cultures through Latin and French class. I chose the Medical Sciences program because it allowed for flexibility in course selection. I have studied several scientific disciplines in depth like physiology and pathology while taking classes in sociology, psychology, and classical studies. Such a diverse academic portfolio has strengthened my ability to consider multiple viewpoints and attack problems from several angles. I hope to relate to patients from all walks of life as a physician and offer them personalized treatment.
I was motivated to travel as much as possible by learning about other cultures in school. Exposing myself to different environments offered me perspective on universal traits that render us human. I want to pursue medicine because I believe that this principle of commonality relates to medical practice in providing objective and compassionate care for all. Combined with my love for travel, this realization took me to Nepal with Volunteer Abroad (VA) to build a school for a local orphanage (4). The project’s demands required a group of us to work closely as a team to accomplish the task. Rooted in different backgrounds, we often had conflicting perspectives; even a simple task such as bricklaying could stir up an argument because each person had their own approach. However, we discussed why we came to Nepal and reached the conclusion that all we wanted was to build a place of education for the children. Our unifying goal allowed us to reach compromises and truly appreciate the value of teamwork. These skills are vital in a clinical setting, where physicians and other health care professionals need to collaborate as a multidisciplinary team to tackle patients’ physical, emotional, social, and psychological problems.
I hope to relate to patients from all walks of life as a physician and offer them personalized treatment.
The insight I gained from my Nepal excursion encouraged me to undertake and develop the role of VA campus representative (4). Unfortunately, many students are not equipped with the resources to volunteer abroad; I raised awareness about local initiatives so everyone had a chance to do their part. I tried to avoid pushing solely for international volunteerism for this reason and also because it can undermine the work of local skilled workers and foster dependency. Nevertheless, I took on this position with VA because I felt that the potential benefits were more significant than the disadvantages. Likewise, doctors must constantly weigh out the pros and cons of a situation to help a patient make the best choice. I tried to dispel fears of traveling abroad by sharing first-hand experiences so that students could make an informed decision. When people approached me regarding unfamiliar placements, I researched their questions and provided them with both answers and a sense of security. I found great fulfillment in addressing the concerns of individuals, and I believe that similar processes could prove invaluable in the practice of medicine.
As part of the Sickkids Summer Research Program, I began to appreciate the value of experimental investigation and evidence-based medicine (23). Responsible for initiating an infant nutrition study at a downtown clinic, I was required to explain the project’s implications and daily protocol to physicians, nurses and phlebotomists. I took anthropometric measurements and blood pressure of children aged 1-10 and asked parents about their and their child’s diet, television habits, physical exercise regimen, and sunlight exposure. On a few occasions, I analyzed and presented a small set of data to my superiors through oral presentations and written documents.
With continuous medical developments, physicians must participate in lifelong learning. More importantly, they can engage in research to further improve the lives of their patients. I encountered a young mother one day at the clinic struggling to complete the study’s questionnaires. After I asked her some questions, she began to open up to me as her anxiety subsided; she then told me that her child suffered from low iron. By talking with the physician and reading a few articles, I recommended a few supplements and iron-rich foods to help her child. This experience in particular helped me realize that I enjoy clinical research and strive to address the concerns of people with whom I interact.
Research is often impeded by a lack of government and private funding. My clinical placement motivated me to become more adept in budgeting, culminating in my role as founding Co-President of the UWO Commerce Club (ICCC) (9). Together, fellow club executives and I worked diligently to get the club ratified, a process that made me aware of the bureaucratic challenges facing new organizations. Although we had a small budget, we found ways of minimizing expenditure on advertising so that we were able to host more speakers who lectured about entrepreneurship and overcoming challenges. Considering the limited space available in hospitals and the rising cost of health care, physicians, too, are often forced to prioritize and manage the needs of their patients.
No one needs a grand revelation to pursue medicine. Although passion is vital, it is irrelevant whether this comes suddenly from a life-altering event or builds up progressively through experience. I enjoyed working in Nepal, managing resources, and being a part of clinical and research teams; medicine will allow me to combine all of these aspects into one wholesome career.
I know with certainty that this is the profession for me.
Jimmy opens this essay hinting that his essay will follow a well-worn path, describing the “big moment” that made him realize why he needed to become a physician. But Jimmy quickly turns the reader’s expectation on its head by stating that he did not have one of those moments. By doing this, Jimmy commands attention and has the reader waiting for an explanation. He soon provides the explanation that doubles as the “thesis” of his essay: Jimmy thinks passion can be built progressively, and Jimmy’s life progression has led him to the medical field.
Jimmy did not make the decision to pursue a career in medicine lightly. Instead he displays through anecdotes that his separate passions — helping others, exploring different walks of life, personal responsibility, and learning constantly, among others — helped Jimmy realize that being a physician was the career for him. By talking readers through his thought process, it is made clear that Jimmy is a critical thinker who can balance multiple different perspectives simultaneously. The ability to evaluate multiple options and make an informed, well-reasoned decision is one that bodes well for Jimmy’s medical career.
While in some cases this essay does a lot of “telling,” the comprehensive and decisive walkthrough indicates what Jimmy’s idea of a doctor is. To him, a doctor is someone who is genuinely interested in his work, someone who can empathize and related to his patients, someone who can make important decisions with a clear head, and someone who is always trying to learn more. Just like his decision to work at the VA, Jimmy has broken down the “problem” (what his career should be) and reached a sound conclusion.
By talking readers through his thought process, it is made clear that Jimmy is a critical thinker who can balance multiple different perspectives simultaneously.
Additionally, this essay communicates Jimmy’s care for others. While it is not always advisable to list one’s volunteer efforts, each activity Jimmy lists has a direct application to his essay. Further, the sheer amount of philanthropic work that Jimmy does speaks for itself: Jimmy would not have worked at VA, spent a summer with Sickkids, or founded the UWO finance club if he were not passionate about helping others through medicine. Like the VA story, the details of Jimmy’s participation in Sickkids and the UWO continue to show how he has thought about and embodied the principles that a physician needs to be successful.
Jimmy’s essay both breaks common tropes and lives up to them. By framing his “list” of activities with his passion-happens-slowly mindset, Jimmy injects purpose and interest into what could have been a boring and braggadocious essay if it were written differently. Overall, this essay lets the reader know that Jimmy is seriously dedicated to becoming a physician, and both his thoughts and his actions inspire confidence that he will give medical school his all.
The Crimson's news and opinion teams—including writers, editors, photographers, and designers—were not involved in the production of this content.
Raising Funds for Medical Expenses Sample Letter
Today, I’m here to share my insights and provide a step-by-step guide to help you create compelling fundraising letters for medical expenses.
Key Takeaways:
- Understand the Purpose : Learn the significance of personalization in fundraising letters.
- Know Your Audience : Tailor your message to resonate with the potential donors.
- Craft a Compelling Story : Use real-life examples to illustrate the impact of donations.
- Be Clear and Concise : Ensure your letter is easy to understand and to the point.
- Provide a Call to Action : Guide readers on how they can contribute.
- Express Gratitude : Always thank your audience, regardless of their decision to donate.
Step 1: Understand Your Audience
Before penning down your letter, it’s crucial to understand who your audience is. Are they family members, friends, or strangers? Their relationship with the patient will influence how you frame your message.
Step 2: Start with a Personal Touch
Begin your letter with a personal greeting. A “Dear [Name]” is warmer and more engaging than a generic salutation.
Step 3: Share the Patient’s Story
Narrate the patient’s journey, focusing on the human aspect rather than just the medical details. This helps in creating a connection with the reader.
Example : “John, a loving father and a devoted husband, was recently diagnosed with…”
Step 4: Explain the Need for Funds
Trending now: find out why.
Be transparent about the financial situation. Detail the medical expenses and any insurance shortcomings, ensuring the reader understands the urgency and necessity of their support.
Step 5: Make a Specific Ask
Rather than a vague request for help, specify the amount needed or suggest donation tiers. This provides clarity for potential donors.
Table : Suggested Donation Tiers
| Tier | Amount | Impact |
|---|---|---|
| 1 | $50 | Covers medication for a week |
| 2 | $100 | Pays for a consultation |
| 3 | $500 | Supports a minor procedure |
Step 6: Provide a Clear Call to Action
Guide the reader on how to donate. Include detailed instructions or links to a donation page, making the process as straightforward as possible.
Step 7: Express Gratitude
Always conclude with a heartfelt thank you. Acknowledge the reader’s time and consideration, regardless of their decision to donate.
Step 8: Include Your Contact Information
Provide a way for donors to reach out if they have questions or require more information.
Tips from Personal Experience:
- Authenticity Resonates : Be genuine in your storytelling. Authenticity builds trust and connection.
- Update Your Donors : Consider sending updates to those who contributed, sharing how their donations have made a difference.
- Proofread : Ensure your letter is free of errors. A well-written letter reflects your seriousness and respect for the reader.
Raising Funds for Medical Expenses Letter Template:
Dear [Name],
I hope this message finds you well. I’m reaching out to share [Patient’s Name]’s story, a [Relation/Description of the Person], who is currently facing a challenging medical situation.
[Describe the patient’s condition, the required treatments, and the emotional and financial toll it’s taking on the patient/family.]
We are aiming to raise [Amount] to cover [Specific Expenses]. Any contribution, big or small, will significantly impact [Patient’s Name]’s life and our family’s well-being.
To donate, please [Instructions on How to Donate]. If you have any questions or need further information, feel free to contact me at [Contact Information].
Thank you so much for considering our request and for your support during this difficult time. Your generosity is not just a donation but a beacon of hope for our family.
Warm regards,
[Your Name]
I’d love to hear your thoughts and experiences with raising funds for medical expenses. Have you written or received a letter that touched your heart? Do you have additional tips to share? Please leave a comment below to join the conversation.
Frequently Asked Questions (FAQs)

Q: What Should I Include in the Opening of My Medical Fundraising Letter?
Answer: In my experience, the opening should be heartfelt and personal. Start by introducing yourself and your situation briefly. Mention your child’s name, their condition, and the reason for writing. A sincere and direct opening sets the tone for the rest of the letter.
Q: How Detailed Should the Description of Medical Expenses Be?
Answer: From what I’ve learned, it’s important to be clear but not overwhelming. List the major expenses like treatment costs, travel for treatment, and any lost income due to care responsibilities. Provide enough detail to be transparent about the financial need without overloading the reader with information.
Q: Is It Appropriate to Share Emotional Struggles in the Letter?
Answer: Absolutely. Sharing your emotional journey adds a human element to your letter. When I wrote about our fears, hopes, and determination, it helped in forming a deeper connection with the readers. Be genuine about your feelings; it can resonate powerfully with potential donors.
Q: How Specific Should My Fundraising Goal Be?
Answer: It’s crucial to be specific. State your fundraising goal clearly and explain how the funds will be used. In my case, specifying the amount needed for each aspect of my child’s care made our needs tangible and helped donors understand exactly how their contributions would help.
Q: Should I Include Personal Contact Information in the Letter?
Answer: Yes, providing contact information is essential. It offers a direct way for donors to reach out or ask questions. I included my email and phone number, which not only facilitated donations but also opened the door for emotional support from the community.
Q: How Can I Effectively Conclude the Letter?
Answer: End with a note of gratitude and a gentle reminder of the request. I always thank the reader for their time and consideration, restate the fundraising goal, and include a final, heartfelt appeal for support. This reinforces your message and leaves the reader with a clear call to action.
Related Articles
Financial aid request letter sample: free & customizable, sample letter requesting financial assistance for education: free & easy, sample letter asking for financial assistance for education: free & effective, 3 proven letters for education aid: secure funding now, leave a comment cancel reply.
Your email address will not be published. Required fields are marked *
Have a language expert improve your writing
Check your paper for plagiarism in 10 minutes, generate your apa citations for free.
- Knowledge Base
- College essay
- How to Write a Scholarship Essay | Template & Example
How to Write a Scholarship Essay | Template & Example
Published on October 11, 2021 by Kirsten Courault . Revised on May 31, 2023.
A good scholarship essay demonstrates the scholarship organization’s values while directly addressing the prompt. If you plan ahead , you can save time by writing one essay for multiple prompts with similar questions.
Table of contents
Apply for a wide variety of scholarships, make a scholarship tracker spreadsheet, tailor your essay to the organization and the prompt, write a focused and relevant personal story, scholarship essay example, other interesting articles, frequently asked questions about college application essays.
Scholarships are a type of student financial aid that don’t require repayment. They are awarded based on various factors, including academic merit, financial need, intended major, personal background, or activities and interests.
Like college applications, scholarship applications often require students to submit their grades, standardized test scores, letters of recommendation, and an essay.
A scholarship essay shares your values and qualities in the context of a specific question, such as “How does technology affect your daily life?” or “Who has had the greatest impact on your life?”
Be wary of scholarship scams
While some applications may not require an essay, be wary of scholarship scams that do the following:
- Guarantee you scholarship money for a fee
- Claim scholarship information is exclusive to their company
- Ask for your bank or credit card information to hold the scholarship
Some legitimate companies do charge for releasing comprehensive scholarship lists or creating a tailored list of scholarship opportunities based on your profile.
However, you can always discover scholarship opportunities for free through your school counselor, community network, or an online search.
Many students focus on well-known, large scholarship opportunities, which are usually very competitive. To maximize your chance of success, invest time in applying for a wide variety of scholarships: national and local, as well as big and small award amounts. There are also scholarships for international students .
In addition to charitable foundation and corporate scholarships, you should consider applying for institutional scholarships at your prospective universities, which can award money based on your application’s strength, your financial situation, and your demonstrated interest in the school.
Check with your guidance counselor, local organizations, community network, or prospective schools’ financial aid offices for scholarship opportunities. It’s a good idea to start applying as early as your junior year and continue throughout your senior year.
Choose the right scholarships for you
Choose scholarships with missions and essay topics that match your background, experiences, and interests. If the scholarship topic is meaningful to you, it will be easier for you to write an authentic and compelling essay.
Don’t shy away from applying for local scholarships with small dollar amounts. Even a few hundred dollars can help you pay for books.
Local scholarships may be more tailored to your community, background, and activities, so they’re likely more relevant to you. Fewer students apply for these scholarships, so you have less competition and a higher chance of success.
Some places to look for local scholarships include
- Civic organizations, such as the Rotary Club, Lions Club, etc.
- Your church, mosque, synagogue, or place of worship
- Community groups, such as the YMCA
- Ethnicity-based organizations
- Your local library or local small businesses
- Organizations related to your intended major
- Your city or town
- Your school district
- Unions, such as SEIU, the Teamsters, CWA, etc.
- Your employer or your parents’ employers
- Banks, credit unions, and local financial institutions
Prevent plagiarism. Run a free check.
While researching scholarship opportunities, create a scholarship tracker spreadsheet to keep track of the following:
- Scholarship amounts
- Required application materials
You can use our free Google Sheets template to track your scholarship applications.
Scholarship application tracker template
You can also include scholarship essay prompts in your college essay tracker sheet . By grouping or color-code overlapping essay prompts, you can plan to write a single essay for multiple scholarships. Sometimes, you can also reuse or adapt your main college essay .
Even if you’re adapting another essay, it’s important to make sure your essay directly addresses the prompt, stays within the word count limit , and demonstrates the organization’s values. The scholarship committee will be able to tell if you reuse an essay that doesn’t quite respond to the prompt, so be sure to tailor it to the questions asked.
Research each organization
Before writing, research the scholarship organization’s mission and reason for awarding the scholarship. Learning more about the organization can help you select an appropriate topic and relevant story.
While you should tailor your essay to the organization’s values, maintain your authentic voice. Never use false or exaggerated stories. If the organization’s values don’t align with yours or you can’t brainstorm a relevant story for the scholarship, continue searching for other scholarship opportunities to find a more appropriate one for you.
After researching the organization, identify a specific personal experience that embodies its values and exemplifies why you will be a successful student.
Choose a story with the following criteria:
- Responds to the prompt
- Demonstrates the organization’s values
- Includes an authentic story
- Focuses on you and your experience, not someone else’s
A good scholarship essay is not
- A resume of your achievements
- A lengthy opinion piece about the essay topic
- An essay featuring a negative tone that puts down others
If appropriate, you can briefly address how the scholarship money will help you achieve your educational goals. You should also end with a brief thank-you.
Take a look at the full essay example below. Hover over the underlined parts to read explanations of why they work.
Prompt: Describe how working for Chelsea’s Chicken restaurant has developed leadership skills that will help you succeed in college. Give specific examples of leadership characteristics that you have exhibited during your employment with us.
As a nervous 16-year-old, I walked into Chelsea’s Chicken for my first day of work determined to make enough money to put gas in my car and buy pizza on the weekends. My only previous job was mowing my neighbors’ lawns when they were on vacation, so I had no idea what to expect. I was a bit intimidated by my new responsibilities, especially handling money and helping disgruntled customers.
However, it didn’t take me long to learn my way around the cash register and successfully address customer complaints. One day, Roger, the store manager, asked me if I wanted to join Chelsea’s Chicken Leadership Training Initiative. He said he saw leadership potential in me because of my attitude with the customers and my enthusiasm for learning new job responsibilities. It surprised me because I had never thought of myself as a leader, but I quickly agreed, and Roger handed me a three-ring binder that was thicker than my math and science textbooks put together! He told me to take it home and read over it during the following week.
In that binder, I discovered that being a leader means taking the initiative, especially when the job is undesirable. One week later, I got to practice that idea when a little kid threw up in the bathroom and missed the toilet. It smelled terrible, but I stepped forward and told Roger that I would clean it up. My coworkers thought I was crazy, but I started to believe in my leadership potential.
That night as we closed the store, Roger pulled me aside in the parking lot and told me that he could tell that I had been studying the manual. He wanted to give me more responsibility, along with a dollar-per-hour pay raise. I was surprised because I had been working there for only a couple of months, but his encouragement helped me make a connection: good leadership helps other people, and it often is rewarded. I was determined to experience more of both.
Within a month, I was ready to take the Team Leader exam, which mattered because I would receive a promotion and a much bigger raise if I passed. But, when I got to work, two of the scheduled team members had called in sick. We were noticeably short-handed, and our customers weren’t happy about it.
I walked back to the lockers, put on my vest and hat, and took my place behind an open register. Customers immediately moved into my line to place their orders. Roger looked at me with surprise and asked, “Did you forget that you’re testing tonight?” I responded, “No, sir—but what’s the use of taking a leadership test if you aren’t going to lead in real life?” Roger smiled at me and nodded.
He stayed late that night after we closed so that I could leave early and still take the test. I noticed that Roger was always staying late, helping employees learn new skills. His example taught me that leaders take the initiative to develop other leaders. He gave me a clear picture of what shared leadership looks like, making room for others to grow and excel. When I asked him where he learned to do that, he said, “From the same leadership manual I gave you!”
Chelsea’s Chicken has offered me so much more than a paycheck. Because of Roger’s example, I have learned to take the initiative to care for my family and friends, such as being the first to do the dishes without my mom asking or volunteering to pick up my friend for our SAT prep course. Now, as I prepare to enter college, I have confidence in my leadership ability. I know I’m signing up for a challenging major—Biology, Pre-Med—yet I also know that Chelsea’s Chicken has helped me to develop the perseverance required to complete my studies successfully.
If you want to know more about academic writing , effective communication , or parts of speech , make sure to check out some of our other articles with explanations and examples.
Academic writing
- Writing process
- Transition words
- Passive voice
- Paraphrasing
Communication
- How to end an email
- Ms, mrs, miss
- How to start an email
- I hope this email finds you well
- Hope you are doing well
Parts of speech
- Personal pronouns
- Conjunctions
A scholarship essay requires you to demonstrate your values and qualities while answering the prompt’s specific question.
After researching the scholarship organization, identify a personal experience that embodies its values and exemplifies how you will be a successful student.
Invest time in applying for various scholarships , especially local ones with small dollar amounts, which are likely easier to win and more reflective of your background and interests. It will be easier for you to write an authentic and compelling essay if the scholarship topic is meaningful to you.
You can find scholarships through your school counselor, community network, or an internet search.
You can start applying for scholarships as early as your junior year. Continue applying throughout your senior year.
Yes, but make sure your essay directly addresses the prompt, respects the word count , and demonstrates the organization’s values.
If you plan ahead, you can save time by writing one scholarship essay for multiple prompts with similar questions. In a scholarship tracker spreadsheet, you can group or color-code overlapping essay prompts; then, write a single essay for multiple scholarships. Sometimes, you can even reuse or adapt your main college essay .
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
Courault, K. (2023, May 31). How to Write a Scholarship Essay | Template & Example. Scribbr. Retrieved August 12, 2024, from https://www.scribbr.com/college-essay/scholarship-essay/
Is this article helpful?

Kirsten Courault
Other students also liked, how to apply for college | timeline, templates & checklist, how to research and write a "why this college" essay, us college essay tips for international students, "i thought ai proofreading was useless but..".
I've been using Scribbr for years now and I know it's a service that won't disappoint. It does a good job spotting mistakes”

- Fundraising Ideas
- Fundraising Letters
- Fundraising Checklists
- Corporate Giving and Matching Gifts
- Learn About Fundraising
- Sample Fundraising Letter for Medical Expenses
Following is a sample fundraising letter to be used for raising funds for medical expenses. You can use this appeal for direct or email requests, but also for any of the online fundraising sites. (See most popular fundraising sites and services here .)
Feel free to copy, modify and paste as needed. For any other use please contact us.
Also read Maintaining Respect and Compassion When Raising Funds for an Individual .
… or click here for more fundraising letters .
Dear Friends,
We’re reaching out to let you know that we are kicking off a campaign to help Coach Amy and her family, and we need your help!
You may have heard that Coach Amy’s youngest daughter, Clara, was diagnosed with a rare form of cancer last year. Three different specialists have recommended a new treatment that is now routine in France and Germany, but insurance will not pay. They claim it is still too experimental. It will cost the family more than $50,000 to travel to Europe and pay the doctor bills at a private clinic.
We all love Coach Amy because she has a fierce spirit and inspires so many children and others in our community to be their best. She often stays overtime at the basketball court to help a teammate, too, sacrificing precious time she could be spending with her own family.
The effects of this illness are devastating her family, however. The prognosis, with the medicine, is a 55 percent survival rate, with a full recovery. The other options, which insurance will cover, include painful chemotherapy treatments. They only have a 25 percent survival rate and low chances for full remission.
The family has appealed the insurance company, but with no luck. The local bank has agreed to give them a high risk loan, for which they have to mortgage their home for a second time. The payments will be over $1,800 a month for 3 years, meaning that Amy or her husband will have to get a second job.
We can’t cure Clara, but we can help ease the financial burden and resultant stress that the family is facing. Our goal is to raise the entire $50,000 for them, to pay back the bank by the end of the year.
You can help in the following ways:
- Give a gift today on our giving page [link here]. For a gift over $500, local restaurant Beechies will thank you with a free dinner for 4!
- Think about pledging a monthly gift toward the loan payments, which we hope to pay with donations as we raise the rest. [link here]
- Help us fundraise with your own fundraiser! If you can’t afford to give yourself, please think about pledging to fundraise from your own friends and family on her behalf. If you can attract 10 donations of $25, it would have a great impact.
- Help us collect donations for our silent auction, which will be held at the school in 2 months. We can use anything of value, though our theme is going to be basketball in honor of the Coach. ( Follow our Pinterest board for Basket Ideas for Fundraisers here .)
If you have other ideas, we are happy to hear them as well. Otherwise, please consider making as generous a gift as you can today, or pledging to do so in the coming months toward our $50,0000 fundraising goal.
Parent Association
P.S.: Please take a minute right now and make a donation. Coach Amy, who has given so much to us and our families over the years, truly needs our help!
Subscribe to our newsletter
And receive fundraising ideas, how-to articles, and tips for a successful campaign.
Enter your email address below and follow the confirmation prompts. You will be able to unsubscribe at any time through a link in any emails.
- Link to facebook
- Link to linkedin
- Link to twitter
- Link to youtube
- Writing Tips
How to Write a Scholarship Essay (With Examples)
6-minute read
- 22nd August 2022
Writing a scholarship essay can seem like a daunting task. For many students , higher education isn’t possible without financial aid, and scholarships are especially valuable because the money awarded doesn’t have to be paid back.
Even though the stakes are high, there are a few manageable steps you can take to ensure you write a great essay to submit with your scholarship applications. We have a few top tips to help you get started, along with writing examples to demonstrate some key points. Check out our guide below to learn more.
A scholarship essay is a great opportunity to present yourself and your accomplishments in an impactful way. It is, therefore, essential to be aware of each scholarship deadline so you can allow sufficient time for the writing process, which typically includes the following:
· Read the essay prompt and brainstorm ideas.
· Create an outline covering the key points you want to address.
· Write a draft and seek feedback from trusted teachers, family, or friends.
· Make any necessary revisions and proofread before submitting your final draft.
Scholarship review committees will be able to tell if you rushed through your essay, so give yourself the best chance of winning an award by staying organized and on schedule!
Who and What?
Researching the scholarship provider and diligently reviewing the essay prompts can help you write an essay that makes you stand out as a top candidate.
1. Who are you writing to?
Learn more about the organization offering the scholarship and why the scholarship fund was created.
For instance, a scholarship may honor its organization’s founder, and the founder’s qualities (e.g., integrity, good citizenship, and leadership) might be the same values guiding the scholarship program as a way to continue the founder’s legacy.
If you identify with any of the same qualities, you can incorporate those keywords into your essay to demonstrate your shared values. Remember to remain authentic, though!
2. What are you writing about?
You must read the essay prompt carefully to identify precisely what you need to accomplish with your essay.
Some prompts ask about your career goals and how you plan to achieve them or your achievements and the challenges you overcame to reach them.
You’ll write about common topics across multiple scholarship applications – some may even be similar to your college admission essay – so you can repurpose your essays as long as you’re diligent about tailoring each one to its prompt.
Your application will likely require other items such as transcripts and test scores, but the essay is your chance to offer something entirely unique. Write about key experiences that highlight who you are and what you’ve accomplished, or you could mention something you’re passionate about.
Remember to follow any specific instructions regarding length and formatting, and be sure to answer all questions listed in the prompt. It can hurt your chances if you’re unable to show the committee that you’re detail-oriented and can follow directions.
Structuring Your Essay
Your essay should follow a standard format that includes a clear beginning, middle, and end. Typically, you should:
· Establish your main idea in the introduction.
· Include a separate body paragraph for each key point that supports your main idea.
· Draw it all together and revisit your main idea in the conclusion.
Scholarship committees read thousands of essays each year. And often, there are hundreds of applicants for an award that can only go to a select few candidates. Writing a powerful introduction and conclusion gives you a chance to make a lasting impression.
1. Introduction
Write an introduction that hooks the reader and encourages them to stay engaged till the end of your essay. Don’t be afraid to add personal, tangible details and an anecdote .
Find this useful?
Subscribe to our newsletter and get writing tips from our editors straight to your inbox.
For example, if you’re writing about your career goals, demonstrate why you’ve chosen that career:
It was the biggest game of the season, and the stands were packed despite the bitter cold. My heart was beating louder than all of the cheers, and I was filled with the anticipation that one more run into the end zone would give us the championship. Everything went silent during that run when the tackle shattered both my leg and my dreams.
My world has always revolved around being an athlete – until one day it couldn’t. I spent many frustrating months rehabilitating, but I got through it because of my dedicated physical therapist, who helped me recover both physically and mentally after a devastating loss. And it was that profound experience that led me to pursue a career in the exercise sciences.
2. Conclusion
The conclusion is the last thing your reader will see, so it’s another opportunity for you to make your essay memorable.
Rather than summarizing with a general statement such as “this is why you should award me a scholarship,” perhaps explain what the financial assistance will help you achieve:
My parents never had the opportunity to go to college, and neither did their parents. I watched them work hard every day just to make ends meet, and I often questioned whether I could achieve anything more. Nevertheless, I spent four years working as hard as I saw my parents work, and I beat the odds by getting accepted to college. A scholarship could be invaluable for me, as it would allow me to attend and be successful without having to worry about finances.
Persuasive Writing
While you don’t want your scholarship essay to be overly informal, you’re certainly allowed to add some creativity and personal details to help persuade your readers.
One of the best ways to do so is by writing with the modes of persuasion ; that is, ethos, pathos, and logos.
Demonstrate your credibility. Use your real-life experiences and interesting details to establish, for example, how you’ve contributed to your community:
I saw how much bullying was impacting so many students at my school, so I founded my high school’s first anti-bullying club and organized campaigns to bring attention to the harm that people can cause one another.
Evoke an emotional response. The “show, don’t tell ” writing technique, which involves using descriptive words when discussing actions and emotions, can be especially useful here:
During one of our first awareness assemblies, the theater was completely silent as I read aloud anonymous stories from students about the scars bullying had left on their lives. Tears were stinging in my eyes as I described the struggles my classmates were facing, but I persevered to give a voice to those who didn’t have one.
Convey your point with reason and facts. Use statistics to demonstrate what you’ve accomplished:
In the first year alone, our club improved students’ feelings of safety and acceptance at our school by 53%.
Proofreading and Editing
Don’t forget the importance of proofreading your essay, as spelling and grammar mistakes can leave a bad impression on your reader. Our expert editors can help ensure your writing is clear, concise, and error-free. Give yourself a better chance at impressing scholarship committees by submitting a free trial document today!
Share this article:
Post A New Comment
Got content that needs a quick turnaround? Let us polish your work. Explore our editorial business services.
5-minute read
Free Email Newsletter Template (2024)
Promoting a brand means sharing valuable insights to connect more deeply with your audience, and...
How to Write a Nonprofit Grant Proposal
If you’re seeking funding to support your charitable endeavors as a nonprofit organization, you’ll need...
9-minute read
How to Use Infographics to Boost Your Presentation
Is your content getting noticed? Capturing and maintaining an audience’s attention is a challenge when...
8-minute read
Why Interactive PDFs Are Better for Engagement
Are you looking to enhance engagement and captivate your audience through your professional documents? Interactive...
7-minute read
Seven Key Strategies for Voice Search Optimization
Voice search optimization is rapidly shaping the digital landscape, requiring content professionals to adapt their...
4-minute read
Five Creative Ways to Showcase Your Digital Portfolio
Are you a creative freelancer looking to make a lasting impression on potential clients or...

Make sure your writing is the best it can be with our expert English proofreading and editing.
Top 10 scholarship essay prompts and how to answer them (with infographic)
Checking each scholarship application’s questions and essays can be time-consuming. But what if you could find out what the most common essay topics were – and then reuse those same scholarship essays across multiple applications?
Well, Going Merry can help you do just that. We took a random sample of about 700 scholarship applications on our scholarship platform and categorized the prompts for any essays requiring 250 or more words. Finally, we ran the numbers to find out what the top 10 most common scholarship essay prompts are.
These 10 topics represented a whopping 90% of all scholarship essay prompts. So that means if you had these 10 essays ready to go, you could apply to the vast majority of scholarships with very little additional work, especially when you use Going Merry’s auto-filled application forms .
Here’s our list of the Top 10 Most Common Scholarship Essay Prompts.
- Here’s an excerpt of the winning scholarship essay from John Flowers Jr.:
2. How have you contributed to your community?
3. tell us about yourself., 4. tell us about a time you failed and what you learned from it., 5. what are your academic and/or career goals, 6. what impact has sports had on your life.
- And here’s a winning essay on this scholarship topic from Jesús Adrian Arroyo-Ramirez:
Here’s an example of a winning scholarship essay from Gabby DeMott in which a student developed a new understanding of herself and others.
Here’s a winning going merry scholarship essay from daniel gill on what makes him unique (hint: he brings puppetry and education together with expressive arts):, 10. why do you want to study/pursue [x], download the top 10 scholarship essay prompts, more resources related to writing for college, ready to start writing some of these top scholarship essay prompts.

1. How will this scholarship help you?
You should answer this scholarship essay prompt by explaining how the award money will help you in at least one of the following ways: financially , professionally, and/or academically.
Financially, you can share family hardships or goals on how you plan to use the money to help pay for portions of college – for textbooks, tuition, a laptop, or other school supplies.
Professionally, the scholarship might help you pursue a degree in a field you’re interested in. If you’re a first-generation student, you can highlight that this would help you pursue both academic and career dreams as the first in your family.
For example, John Flowers Jr., a Going Merry scholarship winner , described in his scholarship essay that the award would help him be able to pay for his books.
“Winning this scholarship will make a difference to me because it will allow me to cover college financial issues that may hold me back from reaching my career. Being less stressed about worrying about college fees will allow me to focus more of my attention in class to earn the credits, and not worry about how I’m going to pay for the class.”
Here’s an excerpt of the winning scholarship essay from John Flowers Jr. :
My parents were never given a shot at having an education beyond high school. They were never given a shot to show their full potential and make a difference in the world […] Being young and seeing my parents struggle is hard for me. It’s challenging seeing the people you love go through a hard time and you can’t do anything about it. […] But then I realized I can do something about it. I can get good grades in school. I can take college level courses throughout high school. I can attend a 4-year university and earn my bachelor’s degree in Business Entrepreneurship. That was my thought process as a Freshman. Now being a Senior I turned those “I cans” into “I did.” I DID get good grades all through school. I DID take college level courses. I will be walking straight out of high school with 17 college credit hours. […] I DID get into a 4-year university; and 4 years from now I want to be able to say I DID earn my bachelor’s degree in Business Entrepreneurship. Nothing would make me happier than to be able to take care of my parents the way they have been taking care of my all my life; and nothing would make me better as a person than to be able to say I did this. […] Winning this scholarship will make a difference to me because it will allow me to cover college financial issues that may hold me back from reaching my career. Being less stressed about worrying about college fees will allow me to focus more of my attention in class to earn the credits, and not worry about how I’m going to pay for the class. Even book fees will add up over time due to how many different classes there are. Being able to use this scholarship to pay for books that are required for a certain class will be a big help, especially for a student who has lots of classes that have to be taken.
This is a common essay prompt for community service scholarships . In this essay, describe your experience in community service, explain how you’ve given back, or share volunteer opportunities you’ve participated in. For example, if you’ve organized a community donation box and taken the donations to a nonprofit organization, share how you got involved in that and how it helped the community.
Two more things to mention–even when they’re not explicitly asked:
- How have you learned or grown due to your community service? Scholarship committees want to know how this work has contributed to your character.
- How do you plan to continue to support your community in the future? Bonus points if your college plans (which they’d be partially funding!) help you further contribute. Sometimes this is easy because your intended career path is service-oriented (for example, if you want to be a nurse, doctor, teacher, or social worker), but other times you may wish to give back on the side (for instance, by doing pro-bono work if you want to be a lawyer).
You have a lot of creative freedom with this scholarship prompt! But don’t get too crazy. Generally, this kind of “open-ended” prompt is a bit of a trick. In the end, the scholarship committee still wants to know:
- What motivates you to do (study or pursue a career in) what you plan to do? Remember, they’re funding your future, so they want to know about your plans and why you’re passionate about them.
- What kind of (good) characteristics do you have? They’re ultimately choosing people to invest in, so they want you to be a good person. Characteristics you might want to show are empathy, service, leadership, perseverance, or determination.
- What kind of successes have you had in the past? This is your chance to brag about what you’ve accomplished so far.
This essay topic is quite similar to writing a college personal statement , except that with this one, you want to more explicitly tie things back to your future plans.

Scholarship providers understand that no student is perfect, and they want to know how you learned from a failure – this can be an academic, professional, or personal failure. Break down how you failed, why you failed, and how it made you better. You can also reveal something you learned from that failure, such as what you would do differently in the future, so you don’t run into that situation again, or how that moment changed your life and how you picked yourself up. This is a moment to show how you can learn and persevere.
If the essay is very short (say, 100-300 words), be clear and concise. Explain what you want to study, and then what kind of career you want to lead afterwards. Be sure to save room for 1-2 sentences explaining why you’re motivated to pursue that path.
If you have a longer essay (for example, 500-1000 words), take the time to describe what inspired you to pursue certain academic and/or career goals. For example: One of your parents has always owned his or her own business and now you’re inspired to be an entrepreneur, to pursue a degree in business. Describe that moment of realization when you decided that would be your career goal. Maybe a conversation with that parent sparked inspiration to pursue that, or maybe it was simply watching them work as you grew up. Looking to the future, how do you plan to pursue that career goal? How will the scholarship award help you pursue it? Tell a story; paint a picture. Get creative with it!
Check out these blog posts for additional information on writing an essay about your academic goals and/or career goals .
This essay prompt is generally for scholarships supporting student-athletes.
So if you played sports throughout high school, share how it’s affected your life, You can reflect on experiences with teammates (if it’s a team sport), what you learned (or gained) from practices or meets/competitions, any injuries you had to overcome, how you balanced athletics and academics, how it affected your schedule (early-morning wake-ups, anyone?), and time with your coach(es) or sports mentors.
You’ll also want to look forwards and not just backwards. How will you take your sports experiences with you, into college and beyond? Maybe there’s a direct connection: being on a team inspired you to one day pursue a career in sports and eventually coach. Or the effects can be more indirect: You’ve learned time management skills that will help you in college, or you’ve learned teamwork skills that will help you when you begin working.
7. Why do you deserve this scholarship?
Scholarship providers are basically asking, “Why should it be you?” with this scholarship essay prompt. Paint a picture of why you’re the most deserving student for this scholarship award.
You’ll want to establish at least these two things:
- You’ve proven yourself as high-achieving (in the past). Discuss accomplishments you’re proud of or any accolades (honors, awards, or simply verbal compliments) you’ve received.
- You’re driven to succeed (in the future). Show that you’ve got clear future plans and the gusto to make them happen.
In addition to that, a strong essay will show at least one of these additional traits:
- You’re passionate. If you’ve got a good story to explain your motivation for your studies or future career plans, now’s the time to tell that tale. Here’s the moment to wow the scholarship committee with why you care more than anyone else, and why.
- You’re unique. Scholarship committees love finding someone who’s just different and stands out from the rest. If you’ve had an unusual upbringing or an uncommon interest, lean into that. (For instance, scholarship winner Daniel Gill wrote about his passion for using puppetry to help autistic children — now that’s cool and unique!)
- You’ve got a particular financial need . For need-based scholarships, this essay question may in part be asking you why your financial need is greater than other applicants’.
Want more tips? We have a whole separate post dedicated to answering this scholarship essay prompt.
And here’s a winning essay on this scholarship topic from Jesús Adrian Arroyo-Ramirez :
I always knew I was different than my friends in some way. Growing up, I struggled to speak English while everyone else had little to no problems. I needed extra help in school while my friends coasted by with ease. My friends would hop on planes and travel all around the world while I had to stay at home. At the age of 13 all of my friends started driving while I still couldn’t. I built up the courage and asked my mother why I did not have access to the simple liberties everyone else did. My name Is Jesús Adrian Arroyo-Ramirez, and I was illegally brought to this country when I was just six years old. At the time I had no clue that I was breaking any laws, and I did not realize the fact that my life was going to change forever. Growing up with a different citizenship situation than my peers was and still is the biggest challenge I have to face in my life. Looking back there is not a single thing that I would change. Knowing that I had to work harder than everyone else led me to be the person that I am today. I took that fire inside of me, pushed myself, graduated first in my class with a cumulative 4.0 GPA, became a Kansas Scholar, and graduated High School with a semester’s worth of college credit. In November of 2016, everything began to look up for me. I received a work permit and a social security card all thanks to the DACA program. I was finally able to get my license, get a job, and most importantly attend college. I plan to continue my success in the classroom and do everything to the best of my ability as I know that under my current circumstances it can all be ripped away from me at any moment. Growing up with my situation has taught me to not take advantage of a single opportunity. There has been continued support around me past and current and I know there are people out there rooting for my success. I will strive to be the first generation in my family to graduate from an American University and I will set a stepping stone for my future family so they will not have to struggle as I did. My citizenship is not a setback, it is a mere obstacle that I will always learn to work around if it means giving my future children a better life, just like my mother did for me.

8. Tell us about a time when you had a belief or idea challenged.
Have you studied abroad? Visited a foreign country on a family trip? Had a thought-provoking discussion with a teacher, religious leader, or friend? Think about an experience or a moment that challenged – or even changed – one of your beliefs or ideas. Explain what your original understanding of the idea was, when that idea was challenged, and how you felt about it afterward. Scholarship providers are interested in seeing reflection and growth, so expanding on every detail, including where you were, who you were with, and what you were feeling, can help tell your story in your essay.
There were only a few minutes to go and our eyes were glued to screen. On the edge of our seats, clutching whoever happened to be next to us, we watched as the referee blew his whistle and the German players took their free kick. The ball was hit with precision and skill; it flew up over the Swedish players, past their goalie, and was caught safely in the back of the opposing team’s net. We all jumped up and screamed, a mixture of German and English, of excitement and relief, of pride and anticipation. We stood, enraptured, for the last several minutes of the game as Germany kept its 2-1 lead over Sweden. The horde of us, Germans and Americans alike, hugged and cheered and made our way out onto the balcony, where we chanted “Deutschland! Deutschland! Deutschland!” for the whole village, the whole country, the whole world to hear. Never have I felt so accepted while being an outsider, so proud of a country that isn’t even mine, so part of something I didn’t really belong to. My German friends didn’t care that we were from different countries; they didn’t care that we would only be staying for three weeks. They accepted us into their homes and their daily lives, their traditions and their celebrations. In watching that World Cup game, it didn’t matter that we were from different places; we were all cheering for the same team. The acceptance I felt in Germany extended beyond that living room. I came to the country on a three week exchange with ten other students from my school. We each stayed with host families and attended the Wildermuth Gymnasium, which was surprisingly accommodating to a gaggle of loud American teenagers. The teachers were friendly and welcoming, the students treated us like ordinary peers, and even the people I interacted with in public were understanding. Before coming to Germany I feared judgment based on my level of the language (which is nowhere near as good as the German students’ English) and American politics. It was intimidating to be in a country with limited knowledge of the language and the customs, even though everyone was welcoming. People did ask myself and the other students about the US’s political climate, but no one blamed us for it. They recognized that we were outsiders, that the place we came from had flaws, and they accepted us anyway. Since that trip, I’ve found myself trying to provide that acceptance to people in my own country. For example, I work at a canoe livery and we receive a lot of visitors with limited English. Some of my coworkers will avoid such customers because they don’t want to take the time to explain things, to exercise patience with someone who may not understand them. If people had done this to me in Germany, my time there would have been much less enjoyable; in fact, I would have been offended. So now when someone walks up to me at the livery and asks a question in English that isn’t perfect, I smile and welcome them. I take my time to make sure they understand, that they can have a good time, and that they feel accepted. It’s a small action, but I know firsthand that it can make a big impact, at my place of work and in the world.
9. How are you unique? (Discuss your background, identity, interest, or talent)
Everyone has a trait, a quirk, an activity that makes them unique, whether it’s sports, their upbringing, their hobbies, or interests. Go into as much detail as you feel comfortable to answer this scholarship essay prompt.
Share a story about your family culture, how you were raised, moments that shaped you into being who you are today. If sports is your thing, for example, share how playing sports at a young age taught you about teamwork, working with a coach, discipline and structure. If you couldn’t play sports due to an injury or a disability, explain how you felt when you learned that you had to find other ways to thrive and how it affected your actions.
Sometimes we think that a topic has been written about so many times that it doesn’t matter, but what makes you unique – your story, your history – is your story to tell.
As an Expressive Arts specialist, I use puppet play and the arts (with three to five-year-olds) to teach sharing, identifying and working with feelings, making friends, mindfulness, and asking for what you need in peaceful ways. Additionally, I perform developmentally appropriate puppet shows in classrooms about fairness, valuing difference (including differences in gender expression and skin tone), and peaceful conflict resolution. By teaching diversity, equity, and inclusion through puppetry, I feel that I am making a difference. In this work, I have noticed an unexplained phenomenon. Educational puppetry is particularly effective in helping children with ASD develop social and communication skills. One girl with ASD in my school refused to follow the daily routine until a parrot puppet helped guide her through the transitions. Through puppet play, a boy with impulse control challenges learned to manage his feelings and stop hitting other children. One boy with Autism showed remarkable progress with puppet play. Now in Kindergarten, his ability to communicate and make friends makes his academic success possible. Teachers value this work; it reinforces the social and emotional teaching they practice daily. One teacher told me, “What you do with puppets and our kids is amazing. You need to share this work beyond our preschool.” Application Questions and Answers My goal is to support young children with Autism in public school settings develop the social-emotional skills they need for academic and personal success. I aim to accomplish this by creating and implementing evidence-based strategies that use puppets as intervention tools. A Masters and Credential in ECSE, and the Autism Spectrum Graduate Certificate program I will complete, are essential to broadening my impact. The program will provide me with the theoretical foundation, the student teaching experiences, the credentials, and the academic community required to work with children and families in public school settings. For example, as part of the ECSE Program Masters and Credential Roadmap, I am taking the Seminar in Educational Research course. I am learning how to conduct scholarly research, a fundamental skill in creating innovative approaches that work. I am eager to apply the knowledge and skills I learn at SFSU toward helping more children open doors to connection. Additionally, I am learning leadership skills by volunteering for SFSU’s Early Childhood Special Education Conference. Most conference attendees are undergraduate students, interested in working with young children at-risk and with disabilities. As Co-Chair of the Presenter Committee, I am recruiting dynamic and engaging speakers who will lead workshops. I am eager to apply all of the knowledge and skills I learn at SFSU toward helping more children open doors to connection. I am at a critical juncture in my path. Helping children who experience social disconnection integrate into their classrooms, is my passion. This scholarship will help me work toward a world where every child has access to education and all children know they belong.
Reflect on what inspires you to want to pursue a certain field of study. If you’re interested in studying psychology and pursuing a career as a psychologist, for example, explain how you enjoy understanding how and why people make certain decisions, how you became fascinated by the science behind it.
Another example: Let’s say you’re interested in pursuing a career in communications. This might seem like a broader category, but you can highlight your love for writing, your ability to pick up on details in and out of school, and presenting this in a way that makes sense to the people around you. Just be careful not to get stuck in broad generalities. For this essay prompt in particular, many applicants will often have the same basic answer as you. So you’ll want to use specific anecdotes to make your essay stand out.

Check out these blog posts to continue researching how to answer scholarship essay prompts:
- How to write an essay about yourself
- Writing about your career goals
- How to write the best personal statement
- Write a winning scholarship essay about your academic goals
- Scholarship essay format and structure
Now that you have a better understanding of how to answer these scholarship essay prompts, it’s time to put your knowledge in motion with your scholarship applications. Sign up for a free Going Merry profile where you can upload your scholarship essays. You’ll enter your information once – such as your expected graduation year, what you plan to study in college, and your location – and then we’ll match you with thousands of scholarships. You can even sort scholarships by competitiveness, location, amount, and deadline!
- Recent Posts
- Scholarships for Students in Pennsylvania for 2024 - November 11, 2020
- Counselor Starter Guide: How to Use Going Merry’s Scholarship Platform - September 9, 2020
- How to write a financial need statement for your scholarship application (with examples!) - August 13, 2020
Ready to find scholarships that are a match for you?
- Research article
- Open access
- Published: 09 November 2020
Medical crowdfunding in a healthcare system with universal coverage: an exploratory study
- Ágnes Lublóy ORCID: orcid.org/0000-0002-3701-1876 1 , 2
BMC Public Health volume 20 , Article number: 1672 ( 2020 ) Cite this article
12k Accesses
23 Citations
6 Altmetric
Metrics details
In recent years, crowdfunding for medical expenses has gained popularity, especially in countries without universal health coverage. Nevertheless, universal coverage does not imply covering all medical costs for everyone. In countries with universal coverage unmet health care needs typically emerge due to financial reasons: the inability to pay the patient co-payments, and additional and experimental therapies not financed by the health insurance fund. This study aims at mapping unmet health care needs manifested in medical crowdfunding campaigns in a country with universal health coverage.
In this exploratory study we assess unmet health care needs in Germany by investigating 380 medical crowdfunding campaigns launched on Leetchi.com . We combine manual data extraction with text mining tools to identify the most common conditions, diseases and disorders which prompted individuals to launch medical crowdfunding campaigns in Germany. We also assess the type and size of health-related expenses that individuals aim to finance from donations.
We find that several conditions frequently listed in crowdfunding campaigns overlap with the most disabling conditions: cancer, mental disorders, musculoskeletal disorders, and neurological disorders. Nevertheless, there is no strong association between the disease burden and the condition which prompted individuals to ask for donations. Although oral health, lipoedema, and genetic disorders and rare diseases are not listed among leading causes of disability worldwide, these conditions frequently prompted individuals to turn to crowdfunding. Unmet needs are the highest for various therapies not financed by the health insurance fund; additional, complementary, and animal-assisted therapies are high on the wish list. Numerous people sought funds to cover the cost of scientifically poorly supported or unsupported therapies. In line with the social drift hypothesis, disability and bad health status being associated with poor socioeconomic status, affected individuals frequently collected donations for their living expenses.
Conclusions
In universal healthcare systems, medical crowdfunding is a viable option to finance alternative, complementary, experimental and scientifically poorly supported therapies not financed by the health insurance fund. Further analysis of the most common diseases and disorders listed in crowdfunding campaigns might provide guidance for national health insurance funds in extending their list of funded medical interventions. The fact of numerous individuals launching crowdfunding campaigns with the same diseases and disorders signals high unmet needs for available but not yet financed treatment. One prominent example of such treatment is liposuction for patients suffering from lipoedema; these treatments were frequently listed in crowdfunding campaigns and might soon be available for patients at the expense of statutory health insurance in Germany.
Peer Review reports
Crowdfunding is the practice of funding a project or enterprise by collecting small amounts of money from numerous people, typically via online platforms. In the past two decades the market of crowdfunding has been growing quickly; crowdfunding has become a new way to finance, for example, start-up companies, projects in the visual arts and music, technological innovation, scientific research, and community projects.
In the last decade, crowdfunding for medical expenses has gained popularity as well, especially in the United States. Bassani et al. [ 1 ] report that 76 medical crowdfunding platforms operating worldwide had raised over $132 million as of October 2017; and that the number of health-related crowdfunding campaigns reached 13,633. In the United States, medical crowdfunding is considered to be a symptom of an inadequate healthcare system; in 2007, 62% of individual bankruptcy filings were related to medical costs due to injury and severe illness [ 2 ]. Crowdfunding not only provides relief for a large number of sick people but also helps them to avoid medical bankruptcy [ 3 , 4 ]. Nevertheless, crowdfunding is a typical tool for obtaining one-off financing; and one-off funding is inadequate to finance chronic diseases and other life-long health problems.
In Europe, medical crowdfunding might be regarded as marginal when compared to the USA. In Europe, as a result of universal health coverage, residents can benefit from adequate, effective and accessible health services and are financially protected. Although the management of health systems varies greatly across Europe, they all provide universal or nearly universal health coverage for their residents [ 5 ]. Universal coverage does not imply covering all medical costs for each individual. Typically, not every resident and not all medical procedures are covered. In the healthcare sector, demand for higher quality care is increasing constantly while the healthcare budget is limited. Nowadays, new medications and innovative medical interventions are appearing on the market quicker than ever. Unmet needs for health care emerge as these new medications and innovative medical procedures are typically not financed by national health insurance funds, due either to insufficient information about their efficacy or the required time-consuming legislative changes [ 6 , 7 , 8 , 9 , 10 , 11 ]. Long waiting times (and thus the incentive to use private health care providers instead of public ones) and patient co-payment [ 12 ] might also motivate individuals to turn to medical crowdfunding.
This study aims at mapping unmet health care needs manifested in medical crowdfunding campaigns in a healthcare system with universal health coverage. In particular, we explore the most common condition, disease or disorder which prompted individuals to turn to crowdfunding in Germany, where universal coverage is provided through statutory and private health insurance. In addition, we reveal the type and size of health-related expenses that individuals aim to finance via crowdfunding. This study is exploratory in nature; it allows a glimpse into the unmet health care needs of residents in a healthcare system with universal health coverage.
The German healthcare system
In Germany, health insurance is mandatory for all; residents may choose between statutory health insurance and substitutive private health insurance [ 13 ]. In Germany, the share of GDP allocated to health spending was 11.7% in 2019 in comparison with an OECD average of 8.8% [ 14 ]. Germany spent the equivalent of USD 6646 per person on health in 2019, compared with an OECD average of USD 4224 [ 14 ]. In 2019, public sources accounted for 85% of overall health spending, the third highest among the (Organisation for Economic Co-operation and Development) OECD countries [ 14 ]. In 2018, Germany was ranked 12th among 35 European countries when measuring the consumer friendliness of the health system by the Euro Health Consumer Index [ 15 ].
German statutory health insurance offers comprehensive health care coverage to 90% of the population (73 million people) [ 16 ]. Residents earning less than 62.550 euros per year are automatically enrolled in the statutory health insurance system [ 17 ]. Only individuals earning more than 62.550 euros per year, self-employed and civil servants can choose which type of health insurance they prefer [ 18 ].
In 2020, the statutory health insurance system is administered by 105 non-profit organisations known as Krankenkasssen (sickness funds) [ 19 ]. These sickness funds are obliged to provide the same minimum level of care and they are not allowed to refuse anyone as a member [ 20 ]. In 2020, all sickness funds charge a basic rate of 14.6% of an employee’s gross salary with a monthly ceiling of 4687.50 euros in 2020 [ 21 ]. Statutory health insurance covers treatment such as hospital treatment, visits to general practitioners and specialists, rehabilitation (home care and physiotherapy), health checks from the age of 35, cancer screening, medicines, therapies and aids (hearing aids and wheelchairs, dental check-ups, dentures and crowns, orthodontic treatment up to age 18 [ 18 ]). In order to avoid overusing the system and to cover some costs of the statutory healthcare system, co-payment charges apply. Most importantly, patients are expected to cover 10% of prescription costs (minimum 5 euros and maximum 10 euros), 10 euros per day for hospital stays (up to a maximum of 28 days per year), 10% of home help costs (minimum 5 euros and maximum 10 euros per day) and 10% of travel costs (minimum 5 euros and maximum 10 euros per journey) [ 22 ].
Depending on the provider, individuals may also be charged an additional contribution of up to 1.1%, on average [ 21 ]. This additional contribution may entitle individuals to extra treatment not covered by statutory health insurance, such as additional dental care (professional tooth cleaning or dentures), flu and travel vaccinations, cancer screening under 30, osteopathy, homoeopathy, in vitro fertilisation, contraception [ 18 ]. Individuals can easily compare the coverage and extra treatments offered by sickness funds by visiting the website of Krankenkassen Deutschland or Tarifcheck [ 23 , 24 ].
Moreover, individuals may purchase additional private insurance from health insurance providers to supplement the care they receive under statutory insurance [ 25 ]. These supplementary services, depending on the provider, might cover travel health insurance, additional sickness benefits, additional long-term care benefits, better hospital treatment (private hospital rooms, higher fees), additional dental care and alternative medication [ 18 ].
Unmet medical needs
According to the subjective method, unmet medical needs are present if individuals perceive that they have not received the care they needed [ 26 ]. According to the objective approach, unmet medical needs are present if it is clinically proven that individuals did not receive the necessary care [ 27 ]. In this research, we follow the subjective method and assess both unmet medical needs (e.g., medication, surgery, rehabilitation, treatment-related travel costs) and unmet health-related needs (e.g., difficulties in covering living expenses, given poor health status) self-reported in medical crowdfunding campaigns. In 2012, 3.4% of the EU population reported unmet medical needs according to information extracted from the European Union Statistics of Income and Living Conditions [ 28 ].
In the literature, unmet medical needs are explained by two factors: the characteristics of the healthcare system and the attributes of individuals seeking care [ 29 ]. The former factor, among others, includes availability of health care services, waiting times before being scheduled for a procedure, referral patterns, and the booking system [ 29 , 30 ]. Patient co-payments might also create barriers to health care access and thus generate unmet needs, especially given the rising co-payments for pharmaceuticals and outpatient care in several European countries [ 28 , 30 ]. Fjær et al. [ 30 ], using data from the European Social Survey, report that two-thirds of unmet needs for health care can be explained by two factors: waiting lists and appointment availability [ 30 ].
The association between unmet medical needs and the characteristics of individuals seeking care is widely researched. In general, studies report that young people, women, individuals with low socio-economic status (e.g., unemployed, homeless, drug users), those with low income and financial constraints, individuals with secondary and tertiary education, and individuals in poor health have a higher likelihood of reporting unmet medical needs [ 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 ]. Several studies assess unmet medical needs in specific subpopulations, for example, among young adults [ 41 ], the unemployed [ 31 ], homeless women with children [ 42 ], or the elderly [ 36 ]. Some other studies map the unmet needs of particular patient groups such as individuals with disabilities [ 43 ], patients suffering from cancer [ 44 , 45 ], people with multiple sclerosis [ 46 ] or dementia [ 47 ].
Empirical evidence shows that the prevalence of self-reported unmet medical needs varies greatly in Europe [ 34 , 48 , 49 , 50 ]. Using data from the 2008 European Social Survey, Cylus and Papanicolas [ 48 ] show that respondents from Germany report similar levels of perceived barriers to care as respondents from Denmark, France, Poland and Slovenia. Data from the European Union Statistics on Income and Living Conditions (EU - SILC) 2009 survey show that the rate of unmet medical needs in Germany is comparable to that of Denmark, Finland, Italy, and Iceland [ 34 ]. Another study using data from six different EU-SILC surveys (2008–2013) documents that the percentage of the population reporting foregone medical care in Germany is similar to that of France, Norway, Slovakia and Sweden [ 49 ]. The level of unmet needs in Germany is relatively low when compared to the rest of Europe [ 34 , 48 , 49 ]. For Germany, a study among the elderly also finds that the prevalence of self-reported unmet medical needs for health care is low overall [ 36 ].
Crowdfunding for unmet medical needs
Renwick and Mossialos [ 51 ] provide a useful typology for crowdfunded health projects. They classify health-related crowdfunding campaigns into four types according to the project’s purpose and the funding method. In their typology, crowdfunding projects might finance health expenses, health initiatives, research, or commercial health innovation. Crowdfunding projects in the first category aim at financing a patient’s out-of-pocket expenses for medical services and products, while health initiatives in the second category provide benefit to the wider public or a specific group of people and raise funds, for example, for patient education programmes and disease awareness.
While unmet medical needs are evident when individuals aim at covering their health expenses from donations, all other types of crowdfunding campaigns are related to unmet medical or health-related needs of specific patient populations. Education and awareness-related health initiatives are indications of unmet need for knowledge among patients with a specific disease or disorder, while crowdfunded health projects typically focus on unmet medical needs of patients where treatment is not yet available. Finally, commercial health innovations aim at meeting the drug and therapy (innovative, complementary or alternative) needs of individuals with disposable income.
The market for crowdfunded health projects is large and growing exponentially. Given the decentralized nature of the crowdfunding market, estimating the size of the market is challenging. Bassani et al. [ 1 ] estimate that by October 2017 health care campaigns raised over $132 million. In contrast, medical crowdfunding campaigns launched on GoFundMe suggest a much larger market size. By 2018, GoFundMe hosted more than 250,000 medical campaigns per year worldwide; these campaigns raised more than $650 million in total [ 52 , 53 ].
A few studies assess the unmet medical needs of specific patient groups as revealed in crowdfunding campaigns. Studies cover, for example, the unmet needs of patients suffering from cancer [ 54 , 55 ], patients undergoing orthopaedic surgery [ 56 ] or abortion [ 57 , 58 ], individuals undergoing organ transplants [ 59 , 60 ] or desiring gender change [ 61 ].
Two very recent studies map the health-related needs of a diverse population using crowdfunding; these studies are the closest to the present study. These recent exploratory studies download selected campaigns from GoFundMe for UK and for British Columbia, Canada, respectively [ 62 , 63 ]. For the UK, the authors analyse 400 campaigns drawn from a non-representative sample (campaigns with larger fundraising target and raising more funds are overrepresented) and point to the barriers in treatment access: limited access to novel therapies in cancer treatment and long waiting times [ 62 ]. For Canada, the authors investigate 423 campaigns from British Columbia and show that individuals frequently sought financial support due to gaps in the wider social system: lost wages because of illness and travel-related costs to access care [ 63 ]. The authors argue that the commonly perceived limitations of the Canadian health system, such as long waiting times for care and limited access to specialist services did not frequently motivate individuals to seek help from the crowd [ 63 ].
Crowdfunded health projects reflect only a small fraction of unmet medical and medical-related needs. In general, younger adults with higher digital literacy launch crowdfunding campaigns. Berliner and Kenworthy [ 3 ] report that crowdfunding campaigns are typically launched by individuals who have better reading and writing skills, and who have mastered good medical, social media and technical literacy. Snyder et al. [ 64 ] also argue that crowdfunding is used by relatively privileged members of society, those being digitally literate and having large social networks. Indeed, large social networks play an important role in reaching the fundraising target; sharing campaigns online through social media sites such as Twitter or Facebook increases the probability of success [ 56 , 65 , 66 , 67 ]. At the same time, membership of marginalized race and gender groups decreases the probability of reaching the fundraising target; the average donation amount is lower among these marginalized groups [ 68 ].
Perhaps the most important critique of crowdfunding is that the less privileged are squeezed out of the crowdfunding market; they not only launch proportionately fewer campaigns, but they also receive less by way of donations per campaign [ 54 , 61 , 64 , 68 ]. Fundraising campaigns for medical care reveal and reinforce health and social inequalities [ 54 , 61 , 64 , 68 ]. The unmet medical needs of the most needy remain unmet even after launching crowdfunding campaigns. In this way crowdfunding creates an unequal and biased marketplace, thus fuelling health inequities and widens the gap in society [ 54 , 64 , 68 ].
Donation-based crowdfunding platforms are screened in Germany, the most highly populated country in Europe [ 69 ]. On the one hand, the more populated a country is, the higher the chance that individuals search for financing of additional health needs. On the other hand, Germany has a universal healthcare system, the target system of this research. As argued before, the vast majority of residents are enrolled in mandatory state health insurance, which covers a wide array of health care services. Nevertheless, some medical costs are not covered (e.g., patient co-payments, several alternative and complementary therapies, medical interventions with a low expected success rate, experimental therapies) which might motivate individuals to turn to crowdfunding.
In Germany, as of May 2018, three large donation-based crowdfunding platforms offered individuals the opportunity to launch crowdfunding campaigns to cover their medical expenses: Leetchi, Betterplace, and Gynny [ 70 ]. On Leetchi, as of 4 May 2018, the time of screening crowdfunding platforms for eligibility, 560 projects were listed in the category of Medicine ( Medizin ) [ 71 ]. On Betterplace 629 crowdfunding campaigns were launched in the category of Health ( Gesundheit ) in Europe [ 72 ]. As compared to Leetchi, Betterplace maintains a strong focus on campaigns launched by non-profit organizations, such as municipalities, hospitals, and foundations; the number of crowdfunding campaigns launched by individuals was rather exceptional. On Gynny 2372 projects were listed covering a wide array of categories [ 73 ]. Although Gynny is listed as a crowdfunding platform on Crowdfunding.de, the platform is designed very differently from typical donation-based crowdfunding platforms. On Gynny individuals can donate through online shopping at partner shops without paying extra charges; they simply need to insert the code of the crowdfunding campaign they wish to support. In this research, crowdfunding campaigns were downloaded from Leetchi; typically, individuals launch campaigns there and its design is similar to many other donation-based crowdfunding platforms.
From the 560 campaigns listed on Leetchi in the category of medicine [ 71 ] we excluded those which were unrelated to health. The excluded campaigns were identified through text mining. We built a vocabulary of 505 health-related German words; the vocabulary included words such as diagnose, sick, medicine, medication, doctor, therapy, pain, cancer, treatment, cure, care, and operation and all related compound words. From the 560 crowdfunding campaigns, 164 did not meet this inclusion criterion; the text of these campaigns did not include any of the 505 health-related words defined in the vocabulary.
In addition, from campaigns containing at least one word from the vocabulary, the following were excluded: 1) duplicates; 2) campaigns written in a language other than German; 3) campaigns without any text; 4) campaigns covering non-health related needs of refugees, the homeless or hungry; 5) campaigns involving medical care for animals. Campaigns entitled “Illness of Kunz Walter” or “Medical help” are typical examples of campaigns excluded due to empty campaign descriptions [ 74 , 75 ]. The campaign entitled “Humanitarian aid for refugees in Europe” is a prototype of a campaign excluded due to non-health related needs [ 76 ]. As a result of these additional exclusion criteria, 16 crowdfunding campaigns were excluded. The final sample thus included 380 crowdfunding campaigns.
Text mining
In this exploratory research, in order to develop categories for which kind of condition, disease or disorder people asked for donations, we screened the titles of the campaigns. During this screening, we developed a vocabulary with keywords (e.g., cancer, mobility, mental disorder) which allowed us to identify the health problem. When developing the vocabulary, we acknowledged that in German it is very common to form compound words—words which assemble several words at the same time to form one word. The number of associated words is unlimited; and sometimes the new word has a completely different meaning. Thus, we first extracted all words which included the keyword, and then we screened the list of the extracted compound words and excluded the irrelevant ones (i.e., changed meaning). We added the relevant compound words to the vocabulary of keywords. Using the text mining package tm in R we identified those campaigns which included any of the words in the extended vocabulary. In order to do so, first we ran some basic text transformation and text cleaning functions and then we built a term-document matrix including all the words in the vocabulary. Finally, we screened the text of the unclassified campaigns and added new health-related keywords to the vocabulary, and repeated the procedure specified above.
In addition to the condition-specific vocabulary, we also developed a vocabulary which allowed us to identify the health-related expenses that individuals aimed at covering from donations. The vocabulary was developed in the same way as specified above, albeit with different key words (e.g., medication, cost of therapy, travel, accommodation, cost of living, holidays).
Finally, by extracting part of a text string based on position in the text string we extracted funding needs as stated in the textual description of the crowdfunding campaigns.
Manual data extraction
Once the health-related campaigns were identified, we extracted three kinds of information manually from the textual descriptions. First, we read each campaign text carefully and validated the condition, disease or disorder which motivated individuals to seek additional funding. In the case of misspecification, we assigned a new motive for crowdfunding (manual validation). In total, we validated 35 health problems listed at least twice and 18 health problems listed only once. Footnote 1 Second, we extracted the costs type that individuals aimed at covering from donations. The most important cost types identified were as follows: medication, surgery, therapy, medical equipment, treatment-related travel and accommodation, living expenses, holidays, medical research and patient education. Third, we identified whether individuals sought funding for treatment abroad or for non-residents.
From the 560 crowdfunding campaigns, in total, 180 did not meet one of the inclusion criteria. As a result, the final sample included 380 crowdfunding campaigns.
The health problem
In several crowdfunding campaigns we identified more than one condition, disease or disorder which prompted individuals to ask for donations. Individuals listed one to six conditions per crowdfunding campaign. In 18 campaigns, although the campaign was evidently health-related and the cost to be covered from the donations could be identified, the condition was not specified. In the majority (62.63%) of campaigns (238 out of 380), individuals listed one specific reason. In 25% of campaigns (95 out of 380), individuals specified two conditions. In 20 campaigns (5.26%) three conditions, in seven campaigns (1.84%) four conditions, and in one campaign five conditions were listed. As a maximum, individuals mentioned six different conditions ( n = 1).
The most frequent conditions, diseases or disorders which motivated individuals to ask for donations are shown in Table 1 ; the last column of the table provides information about the cost to be covered. As shown in Table 1 , the most frequent health problems include cancer, mental disorder, disability, accident, lipoedema, genetic disorders and rare diseases, elderly and dementia, sclerosis, and oral health.
Around one fourth of crowdfunding campaigns (101 out of 380; 26.58%) were related to cancer/tumour . Table 2 shows the cancer type by body location or system; this information could be extracted only for around half of the campaigns (51 out of 101); no details were provided in the remaining campaigns. Malignancies of the brain, breast, gastrointestinal tract and leukaemia were the leading cancer indications for crowdfunding. Most commonly individuals asked for donations for various therapies not financed by the health insurance fund ( n = 42), including alternative therapies, scientifically poorly supported therapies and innovative therapies such as therapies with new substances, micro-immune therapy, Methadon-therapy, and stem cell infusion. Immunotherapy and rehabilitation after surgery were also requested several times. The second most common cost element individuals aimed at covering from the donations were living expenses ( n = 26). Cancer is a chronic condition [ 77 ] which puts a significant financial burden on families due both to patient co-payment (medication, immune strengthener) and lost income.
The second most frequent health problem listed in around one-tenth of crowdfunding campaigns was mental disorder , typically depression ( n = 34, 8.94%). Those suffering from mental disorder most frequently sought additional funding for animal-assisted therapies or living expenses. Funding for various therapies such as psychotherapy or infusion therapy was also often requested.
Disability was the third most frequent motive for crowdfunding; individuals with a wide array of disabilities and their families were in financial need ( n = 26, 6.84%). The 26 disability-related campaigns shown in Table 1 can be explained by reasons other than genetic disorder and rare disease ( n = 20), autism spectrum disorder ( n = 8), paresis ( n = 5), cerebral palsy ( n = 2) and cases where animal-assisted therapy was requested ( n = 26); these severe disabilities are listed separately and excluded from this category. In this category disability covered, for example, brain damage, severe asthma, severe epilepsy, cancer-related disability, and spinal cord or back injury. In the majority of the campaigns, individuals requested funding to facilitate their mobility (electric wheelchairs, wheelchair-accessible vehicles, handicapped-accessible homes).
Accident was ranked as the 4th most frequent cause for medical crowdfunding ( n = 23, 6.05%); these campaigns were posted to provide relief from the severe consequences of a past accident. From the donations individuals aimed to cover a wide array of expenses, such as handicapped-accessible cars, living expenses and various therapies, for example, physiotherapy, rehabilitation, and Adeli-therapy.
The 5th most frequent medical condition mentioned was lipoedema ( n = 22, 5.79%). Lipoedema is a disorder with symptoms of swelling and enlargement of the lower limbs; an abnormal amount of subcutaneous fat is deposited under the skin [ 78 ]. Genetic and hormonal factors contribute to the risk of developing lipoedema [ 78 ]. As of now no effective treatment for lipoedema exists; only symptoms can be alleviated. In crowdfunding campaigns individuals almost exclusively requested funding for surgery to remove fat tissues, arguing that the health insurance fund does not cover the cost of the desired intervention.
Genetic disorders and rare diseases were mentioned in 20 out of 380 campaigns (5.26%) and ranked in the top six. Down syndrome was listed in three campaigns, and Rett syndrome in two campaigns. Other genetic disorders and rare diseases were mentioned only once. These covered a wide array of conditions, such as Ehlers-Danlos Syndrome, Hodgkin’s Syndrome, Lesch-Nyhan Syndrome, and Li-Fraumeni Syndrome. Those suffering from genetic disorders and rare diseases requested funding for diverse activities. Various therapies, such as physiotherapy, therapy with animals, innovative and scientifically poorly supported therapies were high on the wish list, followed by living expenses, and medical aids to increase mobility.
The 7th most frequent medical condition mentioned in crowdfunding campaigns was dementia and elderly care ( n = 19, 5.00%). Dementia and old age in general are associated with poorer health status and several symptoms; symptoms might be so severe that they interfere with daily life. Crowdfunding campaigns were initiated with diverse purposes, among others to support an existing elderly care institution and to cover living expenses.
Both sclerosis and oral health urged individuals to launch crowdfunding campaigns in 15 cases (3.95%). Lateral sclerosis (the death of neurons controlling voluntary muscles) and multiple sclerosis ( damaged insulating covers of nerve cells in the brain and spinal cord) may develop into severe and disabling disease; patients’ muscles become uncoordinated and weak and they might lose their ability to walk [ 79 , 80 ]. This lifelong condition puts a heavy burden on the patients and their families; individuals most frequently asked for financial support to cover their daily expenses. Funding was also frequently requested for research. Regarding oral health, donations were requested from the crowd for dental or orthodontal treatment not covered by health insurance. In several cases, although health insurance covered some previous treatments, the requested treatment was no longer covered.
Table 3 lists the 10-19th most frequent condition, disease or disorder which prompted individuals to ask for donations from the crowd. The table also provides information about the costs to be covered from donations. Table 4 shows those health problems for which individuals requested funding only in a few campaigns (five or less).
Costs to cover
Table 5 shows the 15 most frequent health-related costs for which individuals requested funding on Leetchi. The last column of Table 5 provides some additional information on the cost element. As shown in Table 5 , the most frequent medical expense individuals aimed to cover from the donations was related to therapy ; financial support for therapy was requested in almost one-fourth of the campaigns ( n = 90; 23.68%). The second most frequent cost type for which individuals asked for donations were living expenses ( n = 77, 20.26%). Living expenses might manifest in various forms, such as paying bills or a rental fee, obtaining a driving licence, house renovation, car costs for going to the doctor or work, removing mould professionally, and leisure activities. Typically, the underlying health problem put such a heavy burden on families, partly due to lost income, partly due to financing additional medications and therapies, that they turned to the crowd to ease their financial burden.
In one-tenth of the campaigns, individuals requested financial support for an institution ( n = 39, 10.26%). Almost as popular were requests for donations to facilitate patients’ mobility ( n = 37; 9.74%). Families also often asked for donations for medication ( n = 30, 7.89%), arguing that drug costs put heavy burden on their budget in addition to the burden of the disease, disorder or condition.
Treatment for foreigners and treatment abroad
Regarding geographic coverage , the huge majority of crowdfunding campaigns did not list any country, city or nationality in the campaign description ( n = 304, 80%). These projects were typically posted by residents to fund health care services delivered in their neighbourhood in Germany. In total, almost 13% of crowdfunding projects ( n = 49, 12.89%) involved a foreign country for reasons other than holidays; funding was requested either for patients residing abroad and thus not covered by the German health insurance fund ( n = 31), or for a health initiative in a developing country ( n = 18). Developing countries were involved in 35 out of the 49 projects; countries within the European Economic Area (EU, Norway and Switzerland) were mentioned in five crowdfunding projects; other European countries, e.g. Bosnia and Herzegovina, Russia, and Turkey were mentioned in eight crowdfunding campaigns. High-income countries outside Europe were mentioned in only one crowdfunding campaign; an individual sought funding for medical intervention offered in the USA only. Although the underlying conditions varied greatly, for non-resident patients the three most frequent conditions included cancer ( n = 12), transplants ( n = 5) and accidents ( n = 4).
Donations were asked for treatment abroad in 27 out of 380 cases (7.11%). Typically, individuals asked for donations to finance therapy not available in Germany ( n = 12), such as Adeli-therapy offered in Slovakia, new innovative therapies only offered in the US, or stem cell infusion therapy. Animal-assisted therapies involving dolphins were high on the wish list ( n = 10). Surgery outside Germany was requested only in three cases. Although the underlying conditions varied greatly, three conditions were frequently mentioned: disability ( n = 10) with a comorbidity of epilepsy in half of the cases, cancer ( n = 5) and brain damage ( n = 3). Other disorders, diseases or conditions included cerebral palsy, paresis, genetic disorder, autism, prosthesis, orthopaedic intervention, accident, and mental disorder.
Funding need
Funding need was stated only in 197 out of 380 crowdfunding campaigns (51.84%). In the remaining cases ( n = 183, 48.16%) campaign holders typically wrote that donors could give as much as they want. Table 6 shows the descriptive statistics of funding needs, while Fig. 1 plots the histogram of funding needs for campaigns with a target sum. The mean funding need was €14,166 after excluding two outliers with a target sum of €1 and €6 million. (The former campaign aimed to ease the life of patients with hyperhidrosis and bromhidrosis through surgery, innovative medical intervention and financial support, while the latter asked for donations for a researcher without any publications on Google Scholar.) Campaigns with lower funding needs were more popular; the funding need was €6000 or lower in more than half of cases (102 out of 198). Nevertheless, there were a few campaigns with large funding needs: 18 campaigns aimed at collecting more than €30,000.
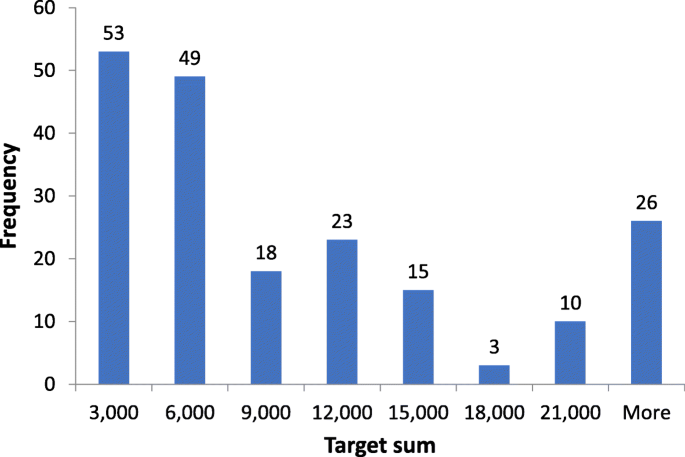
Histogram of funding need
Funding needs were the highest, on average, in the category of elderly and dementia (€40,208, n = 12), followed by transplants (€35,840, n = 5), cancer (€18,859, n = 40), sclerosis (€16,350, n = 6), and lipoedema (€15,317, n = 15). For the 14 most frequent conditions the full list is shown in Table 7 , ordered by average funding need in decreasing order.
Unmet needs due to financial strains
On Leetchi, all four types of crowdfunded health projects classified by Renwick and Mossialos [ 51 ] were present. The huge majority of campaigns aimed at financing expenses for medical services. Not-for-profit health initiatives served as a motive for crowdfunding in around 15% of campaigns in the form of fundraising for medical institutions or charitable organizations, and patient education and disease awareness campaigns. Donations were requested for research less frequently. Commercial health innovation was listed in only one fraudulent campaign [ 83 ] discussed in subsection 4.4 in more detail.
Although the expenses that individuals aimed to finance via crowdfunding varied greatly, unmet medical needs due to financial strains were listed in almost 80% of crowdfunding campaigns (Table 5 ). Footnote 2 Across all conditions, donations were most frequently requested for therapies, typically additional or complementary therapy not financed by the health insurance fund. Animal-assisted therapies were also high on the wish list; although these therapies are not always covered by statutory health insurance, they are expected to ease the emotional and physical burden of affected individuals and families. A similar argument can be made for equipment to facilitate mobility.
The medical condition that individuals were suffering from resulted in significant unmet non-medical needs as well. Individuals could not pay the bill they received, and they could not go on holidays they desired; their (or their children’s) poor health status typically did not allow them to earn sufficient income. Living expenses was the second most frequently listed cost type in accordance with the financial strain that several disorders and diseases exert on families. This finding is in line with the empirical evidence showing that poor health status may be associated with poor socioeconomic conditions, labelled as social drift or selection in the literature [ 84 ]. If affected families enjoyed better socioeconomic status, they could finance these expenses without any difficulty.
Crowdfunding motives, causes of death, and disease burden
There is a weak association between the most frequent causes of death and the condition which motivated individuals to ask for donations. According to the WHO, in upper-middle income countries the top ten causes of death are as follows: ischaemic heart disease; stroke; chronic obstructive pulmonary disease, trachea, bronchus and lung cancer; Alzheimer’s disease and other dementias; lower respiratory infections; diabetes mellitus; road injury; liver cancer, stomach cancer [ 85 ]. From the most frequent causes of death only three overlap with the most frequently mentioned motives in medical crowdfunding campaigns: cancer (the most frequent motive for crowdfunding); accident (the 4th most frequent motive for crowdfunding), and elderly and dementia (the 7th most frequent motive for crowdfunding). Regarding cancer, when cancer is screened by type, lung cancer and cancer affecting the gastrointestinal or digestive system amount to more than 30% of cases (Table 2). As a result, these two cancer types alone assure that cancer is among the top ten motives for medical crowdfunding.
There is also no strong association between the disease burden measured by disability-adjusted life years and the condition which motivated individuals to ask for donations. In the remaining part of this subsection that association is discussed. First, we show signs of a strong positive association and then we elaborate on those conditions where no association can be found.
Cancer is the most frequent motive for crowdfunding, it is named in more than one-fourth of campaigns. According to the Global Burden of Disease (GBD) Study 2017 cancer is the second leading cause of disability worldwide and it exerts enormous emotional, physical and financial strain on patients, families and health systems [ 86 ]. Given the high severity of health loss and the related financial burden, it is no surprise that even insured cancer sufferers ask for donations, most frequently for alternative and highly innovative therapies not financed by the health insurance fund. At the same time, in 12 campaigns donations were also asked for uninsured non-residents reflecting the fact that health systems in low- and middle-income countries typically lack resources to manage cancer. In crowdfunding campaigns, the most frequently listed cancer type by body location or system only partly overlaps with the most common types of cancer as listed by the WHO [ 87 ]. For example, while lung, breast, and stomach cancer were high on the list in both cases, brain tumour and leukaemia were frequently mentioned in crowdfunding campaigns (Table 2), but not listed as the most common types of cancer by the WHO [ 87 ].
The second most frequent medical condition appearing in around one-tenth of crowdfunding campaigns was mental disorder , typically depression. WHO lists depression as the leading cause of disability worldwide and as a major contributor to the overall global burden of disease [ 88 ]. In Europe, mental disorder is ranked fifth when measuring the overall disease burden with the number of years lost due to ill-health, disability or early death [ 89 ]. In a health system with universal coverage those suffering from mental disorder asked for donations most frequently for animal-assisted therapies to improve their mental health and for living expenses to compensate for lost income.
In Europe, musculoskeletal disorders are ranked as the third most disabling condition when measured by disability-adjusted life years [ 89 ]. Musculoskeletal disorders affect human body movement or musculoskeletal system; these are injuries and disorders characterised by limited mobility, dexterity, and functional ability [ 90 ]. Musculoskeletal condition-related disabilities and accidents resulting in injuries were among the most frequent conditions prompting individuals to turn to crowdfunding in Germany, reflecting how burdensome and severely disabling these conditions are. Donations were the most frequently requested for easing mobility, for example, wheelchair-accessible vehicles and handicapped-accessible homes. Similarly, therapeutic fees were also repeatedly mentioned for both musculoskeletal condition-related disabilities and accidents: typically, additional or innovative therapies not financed by the health insurance fund.
In Europe, neurological disorders are ranked as the fourth most disabling condition when measured by disability-adjusted life years [ 89 ]. Among others, these disorders include epilepsy, Alzheimer’s disease and other dementias, Parkinson’s disease, multiple sclerosis, and cerebrovascular diseases. Elderly and dementia, sclerosis, and epilepsy were among the most frequent conditions prompting medical crowdfunding. In addition to living expenses, donations were asked for elderly care institutions, for research about sclerosis, and for watch dogs and additional and innovative therapies for patients with epilepsy.
At the same time, neither cardiovascular diseases, having the highest overall disease burden, nor several other diseases characterized by the highest number of years lost due to ill-health, disability or early death (chronic respiratory diseases, diabetes, kidney and digestive diseases, substance use disorders, skin and subcutaneous diseases, sense organ diseases) featured among the most frequent motives for crowdfunding [ 89 ]. One possible explanation for this mismatch could be that for these diseases efficient treatments are available for insured individuals, despite the high disease burden.
Moreover, oral health, lipoedema, genetic disorders and rare diseases, not listed among leading causes of disability worldwide [ 89 ], prompted individuals to turn to crowdfunding relatively frequently. For oral health, individuals typically requested donations from the crowd when treatments were available but not covered by the health insurance fund. For lipoedema, no effective treatment exists: only the symptoms can be alleviated by removing fat (liposuction). In the past, the statutory health insurance typically did not cover the cost of these liposuction procedures, which prompted desperate patients to ask for donations. Very recently, however, the highest decision-making body of the joint self-government of health insurance funds in Germany, the Gemeinsame Bundesausschus defined a patient group eligible for liposuction at the expense of statutory health insurance [ 82 ]. Children suffering from genetic disorders and rare diseases exert enormous emotional and financial strain on families; families typically live only on one income and ask for donations for therapies not covered by the health insurance fund, either due to their additional or innovative nature. Donations for research activities were also relatively frequently mentioned with the hope that the disorder might soon be cured.
Statutory financing versus crowdfunding
Medical crowdfunding might be a viable option for those scientifically proven treatments which are not financed by the German statutory health insurance system for some reason. When funding is requested for a non-resident, a safety gap exists in a system other than the German statutory healthcare system. When funding is requested for an insured individual, then there is a safety gap: the desired medical intervention is not covered at all or it is not covered by the insurance scheme without additional contributions. Frequently requested scientifically proven treatments include, among others, rehabilitation after injury or cancer, surgery, dental or orthodontal treatments, animal-assisted therapies (excluding dolphin therapy), and therapy with medication. Scientifically proven treatments requested only a couple of times include, for example, microimmuno-therapy for cancer patients ( n = 2) [ 91 ], stem cell transplant for a patient with autoimmune disease [ 92 , 93 ], antibody-drug conjugate (Adcetris with the active substance of brentuximab vendotin) medication again for a cancer patient [ 94 , 95 ], and MiraDry therapy for treating excessive underarm sweating [ 96 , 97 ]. Medical equipment to facilitate mobility might be also listed in this category; although their efficacy is proven they are not financed for some reason.
Policy makers responsible for setting the coverage of the statutory health insurance scheme might consider addressing some of the above-listed safety gaps among insured individuals. In a systematic analysis, the prevalence of medical conditions might be compared with their popularity in medical crowdfunding campaigns. Such a comparison might reveal striking mismatches in the rankings which should act as a warning signal for potential safety gaps. Policy makers should analyse those cases in detail where the condition or desired treatment is mentioned in crowdfunding platforms more often than would be justified on the basis of prevalence rates. One prominent example for such a mismatch is related to lipoedema. As argued above, this mismatch has recently been recognized by the decision-making body of the joint self-government of health insurance funds in Germany, and liposuction is now covered by statutory health insurance for more patients [ 82 ]. Given the limited healthcare budget, several safety gaps are acknowledged by the statutory health insurance fund and purposely left with the individual to cover. Prominent examples of such cases include therapies with a low expected success rate (e.g., in-vitro fertilization for women with severe endometriosis) or much higher costs (e.g., orthodontic treatment beyond age 18). Both situations regularly prompted individuals to turn to crowdfunding; as long as the state budget does not allow coverage of such expenses crowdfunding might be a viable option for health financing in these cases.
Medical crowdfunding should be considered as a viable option for experimental therapies; without sufficient evidence, statutory health insurance does not cover such therapies. Donations for experimental therapies were requested in four crowdfunding campaigns. Two patients suffering from cancer aimed to finance innovative cancer treatments: chemotherapy combined with a therapy using exosomes (pumping them in the spinal metastasis) [ 8 ], and chemotherapy where methadone, an analgesic against cancer pain, is used as a chemosensitizer [ 9 , 98 ]. Two patients, one suffering from a rare form of Leukaemia [ 10 ], the other suffering from a rare genetic disorder (Limb-girdle muscular dystrophy) were collecting donations for taking part in a research programme [ 11 ]. The first patient wanted to visit the Children’s Hospital in Seattle and take part in a study for a Car-T-Cell therapy, while the second aimed at participating in a research programmes on cell and gene therapy development for muscular dystrophy at the Experimental and Clinical Research Centre in Berlin.
Medical crowdfunding might also be considered as a viable option for poorly supported therapies. Treatments funded from donations might increase the evidence base and thus provide sufficient scientific evidence for their efficacy, which in turn might enable the statutory health insurance scheme to add the therapy to the list and cover the cost in the future. Prominent examples of such therapies include Adeli-therapy, Doman-therapy and NeuroScan Balance therapy. Adeli-therapy was requested in four crowdfunding campaigns; the published evidence on this therapy is scant and involves a small number of participants [ 99 , 100 , 101 ]. Doman-therapy was requested in one campaign [ 102 ]. This is a therapy offered for children with special needs in Philadelphia [ 103 ]. An early study concluded that data so far available are insufficient to justify the system of treatment [ 104 ]; no similar study has yet been published afterwards. Similarly, although NeuroScan Balance is offered in several clinics in Germany [ 105 ] and was requested by one individual [ 106 ], there is no published evidence on Google Scholar.
Alternative and complementary therapies can also be considered good candidates for medical crowdfunding. Such therapies include, among others, acupuncture, homeopathy, naturopathy, Chinese and oriental medicine, body movement therapy, music and dance therapy [ 107 ]. Alternative and complementary therapies might give comfort and increase the well-being of patients and their families. In the sample, donations were relatively frequently requested for traditional alternative therapies (n = 11), while less frequently for dance therapy, typically against Alzheimer’s and other dementias (n = 3). Although such therapies are justified from the point of view that it allows patients to feel better and cope better with their medical condition, the budget of the statutory health insurance fund is limited, and thus does not allow it to cover all costs, including the costs of several alternative and complementary therapies. With an unlimited budget, such therapies should be financed. Crowdfunding is a means to attract additional funding to the budget available for healthcare and thus might work as a complementary tool for health care financing.
Medical crowdfunding might also be considered as a viable option for those medical interventions which increase the well-being of individuals but cannot be considered as traditional, alternative, or complementary therapies. Such interventions include, for example, plastic surgery improving the appearance of a body part, gender change, and dolphin therapy. Regarding the latter, empirical evidence shows that dolphin-assisted therapies most probably only improve the mood of a child and its family while on vacation [ 108 ]. Therapies increasing the well-being of individuals were frequently listed as motives in crowdfunding campaigns: cosmetic surgery was mentioned in nine, gender change in four, while dolphin therapy in ten campaigns. Financing such therapies is evidently beyond the scope of universal coverage. Should such therapies be financed by donations from the crowd? We may let the crowd decide on this one.
Scientifically unsupported and dangerous treatments should be neither supported by the statutory health insurance fund nor allowed to be launched on crowdfunding websites. Crowdfunding activity for five such treatments is investigated by Vox et al. [ 109 ]: homeopathy or naturopathy for cancer, hyperbaric oxygen therapy for brain injury, stem-cell therapy for brain injury and spinal cord injury, and long-term antibiotic therapy for chronic Lyme disease. Some of these treatments are ineffective (homeopathy for cancer and hyperbaric oxygen therapy for brain injury), while others may result in serious adverse effects (stem-cell therapy for central nervous system injury and long-term antibiotic therapy for chronic Lyme disease) [ 109 , 110 , 111 ]. Individuals launched four medical crowdfunding campaigns for such treatments on Leetchi, in particular, for naturopathy to cure cancer. As medical crowdfunding platforms provide a forum for spreading inaccurate information about treatment [ 110 ], it would be important to develop patient education initiatives and health policies targeted at potential users of scientifically unsupported and dangerous treatments [ 111 ]. Otherwise, false hopes will be raised, there will be longer delays in appropriate care, and the survival rate will decrease.
Deficiencies in the health care system
In one-fourth of the crowdfunding campaigns ( n = 96, 25.26%) individuals blamed the sickness fund and referred to gaps in service provision. Those gaps were almost exclusively related to the range of services provided by the sickness funds. Prominent examples of such gaps include additional, alternative and complementary therapies, rehabilitation after injury or cancer, and equipment to facilitate mobility. Accessing alternative, complementary, and novel therapies is highly important for patients with poor life prognosis and those with strong disabilities. In a low number of cases individuals expressed their desire to get access to specific treatment methods which was rejected by the sickness fund. Prominent examples of such rejection include dental and orthodontal care, liposuction intervention and in-vitro fertilization with low expected success rate.
Not all medical needs described in the campaign texts should be considered as a health system gap. Scientifically unsupported and dangerous treatments, and medical interventions increasing the well-being of individuals but not being considered as traditional, alternative and complementary therapies (e.g., cosmetic surgeries, gender change) fall well outside the scope of the statutory health insurance scheme.
A small number of residents sought funds for treatment abroad ( n = 27, 7.11%). These campaigns were all related to accessing care not available in Germany. Special rehabilitation therapies not available in Germany ( n = 12, 3.16%) and dolphin-therapies most probably only improving the mood of the child and the family being on vacation ( n = 10, 2.63%) are prominent examples for such care [ 108 ]. Surgeries outside Germany were requested only in three cases (0.79%). No individuals believed that they would have access to better care elsewhere; nobody desired to be treated abroad when the treatment was available in Germany.
In the textual description of the campaigns, individuals complained about long waiting times only in a few cases ( n = 5, 1.32%). In spite of the complaints and the desire to shorten the waiting times, individuals did not consider the possibility of bypassing the waiting list, for example, by undergoing the medical procedure in a private clinic. Only one fundraiser expressed fears that her health condition would deteriorate further by the time the statutory health insurance takes care of her. Deteriorating health condition was rather mentioned as an argument to raise funds for an alternative treatment which might help improving the health status.
Fraud and ethical considerations
Out of the 380 campaigns, two were evidently fraudulent campaigns. One researcher, claimed to be the discoverer of mitochondrial intelligence, asked for €6 million in donations to save the lives of millions [ 83 ]. This target sum is by far the highest on Leetchi in the category of health; it is twice as high as the target sum of all other medical crowdfunding campaigns in aggregate. In his project description Dorian Treitz claims to be the discoverer of mitochondrial intelligence, a discovery not yet published, which has dramatic consequences for all of us [ 83 ]. Nevertheless, the campaign holder had no publications on Google Scholar.
In another campaign, donations were asked for special therapy weeks for blind children for letting them experience seeing without eyes [ 112 ]. The organizer, Axel Kimmel, claims that with their innovative technique blind people can visually recognize the world again. According to current knowledge in medicine, although it is possible to sense light without sight as humans may have light-detecting molecules outside of the eyes [ 113 ], humans cannot see without eyes; they cannot detect the wavelengths of the electromagnetic spectrum and turn it into visual images. It is also worth noting that this crowdfunding campaign has been described as a magic trick by former trainer Reinhard Hofstetter pointing out that it is all about motivation, beliefs and positive attitudes towards life [ 114 ].
In general, the functioning of crowdfunding platforms is conditional upon trust in their legitimacy; this trust is a precondition for donors to participate. As a result, to enhance platform legitimacy, crowdfunding platforms should take a larger role in detecting and punishing fraudulent behaviour. Those campaigns where fraud is evident should not be published on crowdfunding platforms. For published campaigns, easy-to-use tools should be available for individuals to report suspected fraud; such campaigns should then be investigated and removed if indeed deemed fraudulent.
In addition to misusing funds, crowdfunding raises several important ethical concerns. Among others, medical crowdfunding may undermine privacy; to establish credibility, individuals launching a medical crowdfunding campaign must disclose personal health information [ 65 , 115 , 116 ]. Although campaign holders are typically aware of losing their privacy, they are not overwhelmingly concerned; the financial need outweighed the discomfort of publishing personal health information online [ 116 ]. In health systems with universal coverage, crowdfunding might introduce market norms that could commodify health care [ 117 ]. In countries without universal health coverage, medical crowdfunding might widen health inequities as it benefits relatively wealthy members of society, those being digitally literate and having large social networks [ 64 ]. These people rely on medical crowdfunding which will undermine systemic health reforms by delaying or impeding those reforms through alleviating a need that is or should fall on the system to meet [ 54 , 61 , 64 , 68 ]. Another ethical concern is using medical crowdfunding for scientifically unsupported or potentially dangerous treatments [ 109 , 118 ]. Vox et al. [ 109 ] report that over 1000 medical crowdfunding campaigns raised money for five different treatments that are unsupported by evidence or are potentially unsafe—more than $6.7 million in total.
Limitations
This exploratory study suffers from several limitations when mapping unmet health care need. Most importantly, many affected individuals may not consider crowdfunding as a viable option for financing their medical expenses and do not launch any crowdfunding campaigns. Thus, unmet health care needs are only mapped for a subpopulation of patients; namely, for those who have mastered better medical, social media and technical literacies and have better reading and writing skills [ 3 , 64 ]. As a result, children and young adults are overrepresented, while the middle-aged and elderly are underrepresented in the sample when compared to the age distribution of the population in Germany [ 69 ], given the higher digital literacy of young adults (as parents of children). Medical conditions and expenses identified in this study should thus be considered as a non-representative snapshot of unmet health care needs.
As a second limitation, the funding need estimates of this study are only indicative of unmet health care and health-related needs. Although unmet needs are evidently present, estimating related funding needs presents a challenge. Affected individuals may not consider crowdfunding as a viable option for financing their medical expenses, and half of those launching a crowdfunding campaign do not state any target sum, merely that donors should give as much as they want.
Third, we mapped unmet health care needs based on crowdfunding campaigns from one platform from one country. Had we extracted information from other crowdfunding platforms and from other countries, we might have identified partly different medical conditions and expenses due to variations in platform settings and expenses universally covered. Nevertheless, the typology proposed in this study should be valid to some extent for all countries with universal health coverage. Finally, we could only filter out evident misuse of funds raised via crowdfunding. We could not control for other forms of fraud such as lying about medical conditions, creating fake campaigns for sick acquaintances, and using donations for purposes other than those indicated in the campaign description [ 65 ].
In this exploratory study we mapped the unmet medical and health-related needs of residents in Germany, in a healthcare system with universal health coverage., We identified the most common conditions, diseases and disorders which prompted individuals to turn to crowdfunding. The nine most common conditions covered almost two-thirds of campaigns. We found that some of these conditions overlap with the most disabling conditions when measured by disability-adjusted life years. Cancer, mental, musculoskeletal and neurological disorders were frequently listed conditions in crowdfunding campaigns while being leading causes of disability worldwide. Nevertheless, there is no strong association between the disease burden and the condition which prompted individuals to ask for donations. Although oral health, lipoedema, and genetic disorders and rare diseases were not listed among the leading causes of disability worldwide, these conditions frequently prompted individuals to turn to crowdfunding.
In Germany, where statutory health insurance provides wide coverage, medical crowdfunding might be considered as a viable option for financing experimental and poorly supported therapies lacking an evidence base, alternative and complementary therapies giving comfort and increasing the well-being of patients and their families, therapies with a low expected success rate (e.g., in-vitro fertilization for women with severe endometriosis) or much higher costs (e.g., orthodontic treatment beyond age 18), and interventions which increase the well-being of individuals but cannot be considered as traditional, alternative and complementary therapies (e.g., cosmetic surgery, gender change, dolphin therapy). Scientifically unsupported and dangerous treatments, such as homeopathy for cancer, should be neither supported by the statutory health insurance fund nor allowed to be launched on crowdfunding websites.
The medical condition that individuals were suffering from resulted in significant unmet non-medical needs as well. This exploratory study revealed that in more than one-fifth of crowdfunding campaigns, individuals sought financial support to cover their daily expenses. Due to their or a family member’s poor health status individuals could not earn sufficient income and thus turned to crowdfunding to address the financial burden caused by poor health beyond medical needs. This finding is in line with the social drift hypothesis − disabled and bad health status is associated with poor socioeconomic status. These campaigns thus were motivated by gaps in the wider social system. Asking donations for daily expenses show that unmet non-medical needs should also be part of the discussion on the burden of ill health and gaps in the social security system.
This study provided a first glimpse into using the textual descriptions of medical crowdfunding campaigns as a supplementary source of information for the statutory health insurance scheme. It offered an innovative insight into the unmet medical and social needs of a non-representative patient population. Although it is too early to formulate relevant policy recommendations based on this exploratory study, further analysis of the most common diseases and disorders listed in crowdfunding campaigns might provide guidance to national health insurance funds in extending their list of funded medical interventions in countries with universal health coverage. Individuals in desperate need launching crowdfunding campaigns with those diseases signal high unmet needs for available but as yet unfinanced treatment. One prominent example of such treatment is liposuction for patients suffering from lipoedema; these treatments were frequently listed in crowdfunding campaigns and might soon be available for patients at the expense of the statutory health insurance in Germany.
Given the exploratory nature of this study, there is a clear need for additional research. Future studies should address the implications of medical crowdfunding for the health status of individuals; the possibility to access a larger pool of alternative, complementary and experimental therapies; the non-desired consequence of assessing scientifically unproven and dangerous treatments; the implications for equity; and the potential gaps in the health care and social security system. In addition, fraud in medical crowdfunding should be kept to a minimum, there is a need for policy recommendations to avoid such fraud.
Availability of data and materials
All the data analysed during the current study can be downloaded from leetichi.com ( https://www.leetchi.com/en/money-pots/medical ). For this study, the data was downloaded on 4 May 2018. The dataset and the vocabulary of 505 health-related German words used in this study are available from the corresponding author on reasonable request.
The health problems listed at least twice were as follows: Accident, AIDS, alcohol dependence, allergy, autism spectrum disorder, autoimmune diseases, brain damage, cancer, cerebral palsy, diabetes, disability, elderly and dementia, epilepsy, eye problems/blind, gastrointestinal problems, gender change, genetic disorders and rare diseases, heart attack, heart problem, hunger, in vitro fertility treatments, inflammatory lung diseases, kidney problems, lipoedema, lung problems other than inflammatory lung diseases, mental disorder, oral health, orthopaedics, paresis, plastic surgery, prosthesis & orthosis, sclerosis, stroke, transplants, weight/obesity.
An unmet need was considered as medical if funding was requested for direct or indirect medical expenses: therapy, including animal assisted therapy; equipment to facilitate mobility; medication; surgery, including excess fat/skin removal; dental or orthodontal treatment; medical aids and devices; treatment-related travel and accommodation costs.
Abbreviations
Acquired Immunodeficiency Syndrome
Global Burden of Disease Study
European Union
European Union Statistics on Income and Living Conditions
National Health System
Organisation for Economic Co-operation and Development
United States
World Health Organization
Bassani G, Marinelli N, Vismara S. Crowdfunding in healthcare. J Technol Transf. 2019;44(4):1290–310 https://doi.org/10.1007/s10961-018-9663-7 .
Article Google Scholar
Himmelstein D, Thorne D, Warren E, Woolhandler S. Medical bankruptcy in the United States, 2007: results of a national study. Am J Med. 2009;122(8):741–6 https://doi.org/10.1016/j.amjmed.2009.04.012 .
Article PubMed Google Scholar
Berliner LS, Kenworthy NJ. Producing a worthy illness: personal crowdfunding amidst financial crisis. Soc Sci Med. 2007;187:233–42 https://doi.org/10.1016/j.socscimed.2017.02.008 .
Burtch G, Chan J. Reducing medical bankruptcy through crowdfunding: evidence from Giveforward . Proceedings of the international conference on information systems. 2014. https://aisel.aisnet.org/icis2014/proceedings/ISHealthcare/35/ .
Google Scholar
European Union. The management of health systems in the EU member states - the role of local and regional authorities: European Union. European Committee of the Regions; 2012. https://doi.org/10.2863/83500 .
Directive 2001/83/EC of the European Parliament and of the Council of 6 November 2001 on the Community code relating to medicinal products for human use. Official Journal of the European Communities, L311/67, 28/11/2001. p. 67–128. https://eur-lex.europa.eu/eli/dir/2001/83/oj . Accessed 27 July 2020.
Regulation (EC) No 1394/2007 of the European Parliament and of the Council of 13 November 2007 on advanced therapy medicinal products and amending Directive 2001/83/EC and Regulation (EC) No 726/2004. Official Journal of the European Union L324/121, 10/12/2007. p. 121–137. https://eur-lex.europa.eu/eli/reg/2007/1394/oj . Accessed 27 July 2020.
Leetchi: Hoffnung für Petra https://www.leetchi.com/c/soziales-von-petra-28583605 . Accessed 3 Aug 2020.
Leetchi: Echium braucht Hilfe. https://www.leetchi.com/c/soziales-von-echium . Accessed 3 Aug 2020.
Leetchi: Hoffnung für Daniel https://www.leetchi.com/c/hoffnung-fuer-daniel . Accessed 3 Aug 2020.
Leetchi: Muskeldystrophie - neue Hoffnung für Olivers Zukunft https://www.leetchi.com/c/soziales-von-oliver-23269319 . Accessed 3 Aug 2020.
Thomson S, Evetovits T, Cylus J, Jakab M. Monitoring financial protection to assess progress towards universal health coverage in Europe. Public Health Panor. 2016;2(03):357–66.
Busse R, Blümel M. Germany. Health system review. Health Syst Transit. 2014;16(2):1–296.
PubMed Google Scholar
OECD. OECD.Stat. Health expenditure and financing. https://stats.oecd.org/Index.aspx?DataSetCode=SHA Accessed 7 July 2020.
Björnberg A, Phang AY. Euro health consumer index 2018 report. Health consumer powerhouse. Brussels: Health Consumer Powerhouse AB; 2019.
GKV-Spitzenverband (National Association of Statutory Health Insurance Funds). Responsibility for healthcare. The national association of the health and long-term care insurance funds. https://www.gkv-spitzenverband.de/english/statutory_health_insurance/statutory_health_insurance.jsp . Accessed 27 July 2020.
Bundesministerium für Arbeit und Soziales. Referentenentwurf zur Sozialversicherungs-Rechengrößenverordnung. 2020. https://www.bmas.de/DE/Presse/Meldungen/2019/referentenentwurf-zur-sozialversicherungs-rechengroessenverordnung.html. Accessed 27 July 2020.
Statutory health insurance in Germany (Gesetzliche Krankenversicherung). https://www.iamexpat.de/expat-info/german-health-insurance/statutory-health-insurance-germany . Accessed 27 July 2020.
GKV-Spitzenverband (National Association of Statutory Health Insurance Funds). Die gesetzlichen Krankenkassen. https://www.gkv-spitzenverband.de/krankenversicherung/kv_grundprinzipien/alle_gesetzlichen_krankenkassen/alle_gesetzlichen_krankenkassen.jsp . Accessed 27 July 2020.
Gesetzliche Krankenversicherung (GKV). Bundesministerium für Gesundheit. https://www.bundesgesundheitsministerium.de/gkv.html . Accessed 27 July 2020.
Beiträge und Tarife. Bundesministerium für Gesundheit. https://www.bundesgesundheitsministerium.de/beitraege-und-tarife.html . Accessed 27 July 2020.
Zuzahlungsregelungen der gesetzlichen Krankenversicherung. Informationsblatt Nr. 223–06. Stand: 2018. https://www.bundesgesundheitsministerium.de/zuzahlung-krankenversicherung.html . Accessed 27 July 2020.
Krankenkassen Deutschland. https://www.krankenkassen.de/krankenkassen-vergleich/tarife-und-beitraege/ . Accessed 27 July 2020.
Tarifcheck. https://www.tarifcheck.de/private-krankenversicherung/ . Accessed 27 July 2020.
Wahltarife, Bonusprogramme und Zusatzleistungen. Bundesministerium für Gesundheit. https://www.bundesgesundheitsministerium.de/wahltarife-bonusprogramme-und-zusatzleistungen.html#c4857 . Accessed 27 July 2020.
Allin S, Grignon M, Le Grand J. Subjective unmet need and utilization of health care services in Canada: what are the equity implications? Soc Sci Med. 2010;70(3):465–72 https://doi.org/10.1016/j.socscimed.2009.10.027 .
Carr W, Wolfe S. Unmet needs as sociomedical indicators. Int J Health Serv. 1976;6(3):417–30 https://doi.org/10.2190/MCG0-UH8D-0AG8-VFNU .
Article CAS PubMed Google Scholar
Reeves A, McKee M, Stuckler D. The attack on universal health coverage in Europe: recession, austerity and unmet needs. Eur J Pub Health. 2015;25(3):364–5 https://doi.org/10.1093/eurpub/ckv040 .
Fiorillo D. Reasons for unmet needs for health care: the role of social capital and social support in some Western EU countries. Int J Health Econ Manag. 2020;20(1):79–98 https://doi.org/10.1007/s10754-019-09271-0 .
Fjær EL, Stornes P, Borisova LV, McNamara CL, Eikemo TA. Subjective perceptions of unmet need for health care in Europe among social groups: findings from the European social survey (2014) special module on the social determinants of health. Eur J Pub Health. 2017;27(suppl_1):82–9 https://doi.org/10.1093/eurpub/ckw219 .
Åhs AM, Westerling R. Health care utilization among persons who are unemployed or outside the labour force. Health policy. 2006;78(2–3):178–93 https://doi.org/10.1016/j.healthpol.2005.10.010 .
Allin S, Masseria C. Unmet need as an indicator of health care access. Eurohealth. 2009;15(3):7.
Bryant T, Leaver C, Dunn J. Unmet healthcare need, gender, and health inequalities in Canada. Health Policy. 2009;91(1):24–32 https://doi.org/10.1016/j.healthpol.2008.11.002 .
Chaupain-Guillot S, Guillot O. Health system characteristics and unmet care needs in Europe: an analysis based on EU-SILC data. Eur J Health Econ. 2015;16(7):781–96 https://doi.org/10.1007/s10198-014-0629-x .
Connolly S, Wren MA. Unmet healthcare needs in Ireland: analysis using the EU-SILC survey. Health Policy. 2017;121(4):434–41 https://doi.org/10.1016/j.healthpol.2017.02.009 .
Hoebel J, Rommel A, Schröder SL, Fuchs J, Nowossadeck E, Lampert T. Socioeconomic inequalities in health and perceived unmet needs for healthcare among the elderly in Germany. Int J Env Res Pub He. 2017;14(10):1127 https://doi.org/10.3390/ijerph14101127 .
Lee SY, Kim CW, Kang JH, Seo NK. Unmet healthcare needs depending on employment status. Health Policy. 2015;119(7):899–906 https://doi.org/10.1016/j.healthpol.2014.09.007 .
Litaker D, Love TE. Health care resource allocation and individuals’ health care needs: examining the degree of fit. Health Policy. 2005;73(2):183–93 https://doi.org/10.1016/j.healthpol.2004.11.010 .
Thammatacharee N, Tisayaticom K, Suphanchaimat R, Limwattananon S, Putthasri W, Netsaengtip R, Tangcharoensathien V. Prevalence and profiles of unmet healthcare need in Thailand. BMC Public Health. 2012;12(1):923 https://doi.org/10.1186/1471-2458-12-923 .
Article PubMed PubMed Central Google Scholar
Zavras D, Zavras AI, Kyriopoulos II, Kyriopoulos J. Economic crisis, austerity and unmet healthcare needs: the case of Greece. BMC Health Serv Res. 2016;16(1):309 https://doi.org/10.1186/s12913-016-1557-5 .
Marshall EG. Do young adults have unmet healthcare needs? J Adolesc Health. 2011;49(5):490–7 https://doi.org/10.1016/j.jadohealth.2011.03.005 .
Vuillermoz C, Vandentorren S, Brondeel R, Chauvin P. Unmet healthcare needs in homeless women with children in the greater Paris area in France. PLoS One. 2017;12(9):e0184138 https://doi.org/10.1371/journal.pone.0184138 .
Article PubMed PubMed Central CAS Google Scholar
Sakellariou D, Rotarou ES. Access to healthcare for men and women with disabilities in the UK: secondary analysis of cross-sectional data. BMJ Open. 2017;7(8) https://doi.org/10.1136/bmjopen-2017-016614 .
Sanson‐Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P, Supportive Care Review Group. The unmet supportive care needs of patients with cancer. Cancer. 2000;88(1):226–37 https://doi.org/10.1002/(SICI)1097-0142(20000101)88:1<226::AID-CNCR30>3.0.CO;2-P .
Hudis CA, Gianni L. Triple-negative breast cancer: an unmet medical need. Oncologist. 2011;S1(16):1–11 https://doi.org/10.1634/theoncologist.2011-S1-0 .
Ponzio M, Tacchino A, Zaratin P, Vaccaro C, Battaglia MA. Unmet care needs of people with a neurological chronic disease: a cross-sectional study in Italy on multiple sclerosis. Eur J Pub Health. 2015;25(5):775–80 https://doi.org/10.1093/eurpub/ckv065 .
Gaugler JE, Kane RL, Kane RA, Newcomer R. Unmet care needs and key outcomes in dementia. J Am Geriatr Soc. 2005;53(12):2098–105 https://doi.org/10.1111/j.1532-5415.2005.00495.x .
Cylus J, Papanicolas I. An analysis of perceived access to health care in Europe: how universal is universal coverage? Health Policy. 2015;119(9):1133–44 https://doi.org/10.1016/j.healthpol.2015.07.004 .
Elstad JI. Income inequality and foregone medical care in Europe during the great recession: multilevel analyses of EU-SILC surveys 2008–2013. Int J Equity Health. 2016;15:101 https://doi.org/10.1186/s12939-016-0389-6 .
Detollenaere J, Hanssens L, Vyncke V, De Maeseneer J, Willems S. Do we reap what we sow? Exploring the association between the strength of European primary healthcare systems and inequity in unmet need. PLoS One. 2017;e0169274:12 https://doi.org/10.1371/journal.pone.0169274 .
Renwick MJ, Mossialos E. Crowdfunding our health: economic risks and benefits. Soc Sci Med. 2017;191:48–56 https://doi.org/10.1016/j.socscimed.2017.08.035 .
GoFundMe. Get help with medical Fundraising. https://www.GoFundMe.com/start/medical-fundraising . Accessed 3 Aug 2019.
Kittelsen SK, Fukuda-Parr S, Storeng KT. The political determinants of health inequities and universal health coverage. Glob Health. 2019;15(S1):73 https://doi.org/10.1186/s12992-019-0514-6 .
van Duynhoven A, Lee A, Michel R, Snyder J, Crooks V, Chow-White P, Schuurman N. Spatially exploring the intersection of socioeconomic status and Canadian cancer-related medical crowdfunding campaigns. BMJ Open. 2019;9(6):e026365 https://doi.org/10.1136/bmjopen-2018-026365 .
Cohen AJ, Brody H, Patino G, Ndoye M, Liaw A, Butler C, Breyer BN. Use of an online crowdfunding platform for unmet financial obligations in cancer care. JAMA Intern Med. 2019;179(12):1717–20 https://doi.org/10.1001/jamainternmed.2019.3330 .
Article PubMed Central PubMed Google Scholar
Durand WM, Johnson JR, Eltorai AE, Daniels AH. Medical crowdfunding for patients undergoing orthopedic surgery. Orthopedics. 2018;41(1):e58–63 https://doi.org/10.3928/01477447-20171114-04 .
Solotke MT, Faria NB, Karim H, Roy S, Ross JS, Cron J. Exploring crowdfunding campaigns for abortion services. Contraception. 2020;102(1):18–22 https://doi.org/10.1016/j.contraception.2020.02.008 .
Zenone MA, Snyder J. Crowdfunding abortion: an exploratory thematic analysis of fundraising for a stigmatized medical procedure. BMC Womens Health. 2020;20:90 https://doi.org/10.1186/s12905-020-00938-2 .
Durand WM, Peters JL, Eltorai AE, Kalagara S, Osband AJ, Daniels AH. Medical crowdfunding for organ transplantation. Clin Transpl. 2018;32(6):e13267 https://doi.org/10.1111/ctr.13267 .
Pol SJ, Snyder J, Anthony SJ. “Tremendous financial burden”: Crowdfunding for organ transplantation costs in Canada. PLoS One. 2019;14(12):e0226686 https://doi.org/10.1371/journal.pone.0226686 .
Article CAS PubMed PubMed Central Google Scholar
Barcelos CA. Go fund inequality: the politics of crowdfunding transgender medical care. Crit Public Health. 2020;30(3):330–9 https://doi.org/10.1080/09581596.2019.1575947 .
Coutrot IP, Smith R, Cornelsen L. Is the rise of crowdfunding for medical expenses in the UK symptomatic of systemic gaps in health and social care? J Health Serv Res Po. 2020;1355819619897949 https://doi.org/10.1177/1355819619897949 .
Snyder J, Zenone M, Crooks V, Schuurman N. What medical crowdfunding campaigns can tell us about local health system gaps and deficiencies: exploratory analysis of British Columbia, Canada. J Med Internet Res. 2020;22(5):e16982 https://doi.org/10.2196/16982 .
Snyder J, Chow-White P, Crooks VA, Mathers A. Widening the gap: additional concerns with crowdfunding in health care. Lancet Oncol. 2017;18(5):e240 https://doi.org/10.1016/S1470-2045(17)30259-0 .
Snyder J, Mathers A, Crooks VA. Fund my treatment!: a call for ethics-focused social science research into the use of crowdfunding for medical care. Soc Sci Med. 2016;169(11):27–30 https://doi.org/10.1016/j.socscimed.2016.09.024 .
Byrnes JE, Ranganathan J, Walker BL, Faulkes Z. To crowdfund research, scientists must build an audience for their work. PLoS One. 2014;9(12):e110329 https://doi.org/10.1371/journal.pone.0110329 .
Ortiz RA, Witte S, Gouw A, Sanfilippo A, Tsai R, Fumagalli D, Yu C, Lant K, Lipintz N, Shepphird J, Alvina FB. Engaging a community for rare genetic disease: best practices and education from individual crowdfunding campaigns. Interact J Med Res. 2018;7(1):e3 https://doi.org/10.2196/ijmr.7176 .
Kenworthy N, Dong Z, Montgomery A, Fuller E, Berliner L. A cross-sectional study of social inequities in medical crowdfunding campaigns in the United States. PLoS One. 2020;15(3):e0229760 https://doi.org/10.1371/journal.pone.0229760 .
Eurostat. Population on 1 January 2020 - persons. Code: tps00001. https://ec.europa.eu/eurostat/tgm/refreshTableAction.do?tab=table&plugin=1&pcode=tps00001&language=en Accessed 2 Aug 2020.
Crowdfunding.de: Crowdfunding Plattformen. Übersicht und Links zu deutschen und internationalen Crowdfunding Plattformen. Platftform-Liste. https://www.crowdfunding.de/plattformen/#spenden . Accessed 12 Mar 2018.
Leetchi: Projects and causes. Health. https://www.leetchi.com/en/money-pots/medical . Accessed 4 Mar 2018.
Betterplace: Projekte Entdecken. Gesundheit. https://www.betterplace.org/de/discover-projects?categoryId=4 . Accessed 4 Mar 2018.
Gynny: Projekte. http://www.gynny.de/home#collapse4 . Accessed 4 Mar 2018.
Leetchi: Krankheit von Kunz Walter. https://www.leetchi.com/c/krankheit-von-kunz-walter . Accessed 4 Mar 2018.
Leetchi: Medizinhilfe. https://www.leetchi.com/c/medizinhilfe . Accessed 4 Mar 2018.
Leetchi: Humanitäre Hilfe für Geflüchtete in Europa. https://www.leetchi.com/c/organisationen-von-balkanbus . Accessed 3 Aug 2020.
Phillips JL, Currow DC. Cancer as a chronic disease. Collegian. 2010;17(2):47–50 https://doi.org/10.1016/j.colegn.2010.04.007 .
Child AH, Gordon KD, Sharpe P, Brice G, Ostergaard P, Jeffery S, Mortimer PS. Lipedema: an inherited condition. Am J Med Genet A. 2010;152(4):970–6 https://doi.org/10.1002/ajmg.a.33313 .
NHS: Motor neuron disease. https://www.nhs.uk/conditions/motor-neurone-disease/ . Accessed 18 Apr 2019.
NHS: Multiple sclerosis. https://www.nhs.uk/conditions/multiple-sclerosis/symptoms/ . Accessed 18 Apr 2019.
NHS: Lipoedema. https://www.nhs.uk/conditions/lipoedema/ . Accessed 23 July 2019.
Ärzteblatt: Liposuktion kann ab Stadium 3 künftig Kassenleistung sein, 19 September 2019. https://www.aerzteblatt.de/nachrichten/106125/Liposuktion-kann-ab-Stadium-3-kuenftig-Kassenleistung-sein . .
Leetchi: Beinahe vergaster Wissenschaftler bittet um Mithilfe. Organised for: Dorian Antonius Luzius Swetovit Treitz. https://www.leetchi.com/c/dorian-treitz . Accessed 10 Nov 2019.
Adler NE, Ostrove JM. Socioeconomic status and health: what we know and what we don't. Ann N Y Acad Sci. 1999;896(1):3–15.
World Health Organization: The top 10 causes of death. https://www.who.int/en/news-room/fact-sheets/detail/the-top-10-causes-of-death . Accessed 4 Aug 2020.
James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1789–858 https://doi.org/10.1016/S0140-6736(18)32279-7 .
World Health Organization: Cancer. Key facts. https://www.who.int/news-room/fact-sheets/detail/cancer . Accessed 12 Nov 2019.
World Health Organization: Depression. Key facts. https://www.who.int/news-room/fact-sheets/detail/depression . Accessed 13 Nov 2019.
European Union. EU burden from non-communicable diseases and key risk factors. Health Promotion and Disease Prevention Knowledge Gateaway, Societal Impacts. https://ec.europa.eu/jrc/en/health-knowledge-gateway/societal-impacts/burden . Accessed 13 Nov 2019.
World Health Organization: Musculoskeletal conditions. Key facts. https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions . Accessed 14 Nov 2019.
Huang P, Wang X, Liang X, Yang J, Zhang C, Kong D, Wang W. Nano-, micro-, and macroscale drug delivery systems for cancer immunotherapy. Acta Biomater. 2019;85:1–26 https://doi.org/10.1016/j.actbio.2018.12.028 .
Leetchi: Meine Tochter soll leben. https://www.leetchi.com/c/meine-tochter-soll-leben-31416995 . Accessed 3 Aug 2020.
Marmont AM. Will hematopoietic stem cell transplantation cure human autoimmune diseases? J Autoimmun. 2008;30(3):145–50 https://doi.org/10.1016/j.jaut.2007.12.009 .
Leetchi: Krebshilfe für Valentina. https://www.leetchi.com/c/soziales-von-valentina-tshahova . Accessed 3 Aug 2020.
European Medicines Agency. Adcetris. Brentuximab vedotin. https://www.ema.europa.eu/en/medicines/human/EPAR/adcetris . Accessed 3 Aug 2020.
Leetchi: Hyperhidrose und Bromhidrose (Übermässiges Schwitzen). https://www.leetchi.com/c/organisationen-von-julia-koenig Accessed 3 Aug 2020.
International Hyperhidrosis Society. miraDry® https://www.sweathelp.org/hyperhidrosis-treatments/miradry.html Accessed 3 Aug 2020.
Michalska M, Katzenwadel A, Wolf P. Methadone as a “tumor theralgesic” against cancer. Front Pharmacol. 2017;8:733 https://doi.org/10.3389/fphar.2017.00733 .
Mahani MK, Karimloo M, Amirsalari S. Effects of modified Adeli suit therapy on improvement of gross motor function in children with cerebral palsy. Hong Kong J Occup Th. 2011;21(1):9–14 https://doi.org/10.1016/j.hkjot.2011.05.001 .
Turner AE. The efficacy of Adeli suit treatment in children with cerebral palsy. Dev Med Child Neurol. 2006;48(5):324 https://doi.org/10.1017/S0012162206000715 .
Lee BH. Clinical usefulness of Adeli suit therapy for improving gait function in children with spastic cerebral palsy: a case study. J Phys Ther Sci. 2016;28(6):1949–52 https://doi.org/10.1589/jpts.28.1949 .
Leetchi: Doman-Therapie für Tammi, https://www.leetchi.com/c/soziales-von-tammi . Accessed 3 Aug 2020.
Doman International: What is the Doman Method? https://www.domaninternational.org/blog/what-is-the-doman-method-by-spencer-doman Accessed 3 Aug 2020.
Cohen HJ, Birch HG, Taft LT. Some considerations for evaluating the Doman-Delacato “patterning” method. Pediatrics. 1970;45(2):302–14.
CAS PubMed Google Scholar
NeuroScanBalance®. https://www.neuroscanbalance.de/ . Accessed 3 Aug 2020.
Leetchi: Oskar der Kämpfer NeuroScanBalance Methode. https://www.leetchi.com/c/oskar-herzfehler . Accessed 3 Aug 2020.
Types of Complementary and Alternative Medicine. What are the different types of CAM? https://www.hopkinsmedicine.org/health/wellness-and-prevention/types-of-complementary-and-alternative-medicine . Accessed 4 Aug 2020.
Marino L, Lilienfeld SO. Dolphin-assisted therapy: more flawed data and more flawed conclusions. Anthrozoos. 2007;20(3):239–49 https://doi.org/10.2752/089279307X224782 .
Vox F, Folkers KM, Turi A, Caplan AL. Medical crowdfunding for scientifically unsupported or potentially dangerous treatments. JAMA. 2018;320(16):1705–6 https://doi.org/10.1001/jama.2018.10264 .
Snyder J, Turner L, Crooks VA. Crowdfunding for unproven stem cell–based interventions. JAMA. 2018;319(18):1935–6 https://doi.org/10.1001/jama.2018.3057 .
Snyder J, Turner L. Crowdfunding for stem cell-based interventions to treat neurologic diseases and injuries. Neurology. 2019;93(6):252–8 https://doi.org/10.1212/WNL.0000000000007838 .
Leetchi: Hilf blinden Kindern wieder zu sehen. Organised for: Sehen ohne Augen-Team. https://www.leetchi.com/c/hilf-blinden-kinder-wieder-zu-sehen. Accessed 10 Nov 2019.
Van Gelder RN. Non-visual photoreception: sensing light without sight. Curr Biol. 2008;18(1):R38–9 https://doi.org/10.1016/j.cub.2007.11.027 .
Article PubMed CAS Google Scholar
Hofstetter Reinhard, Sehen-ohne-Augen??? Sorry nur ein Zaubertrick: http://www.reinhard-hofstetter.at/EGP/Menuefuerung/egpfr10.htm Accessed 20 Nov 2019.
Snyder J. Crowdfunding for medical care: ethical issues in an emerging health care funding practice. Hast Cent Rep. 2016;46(6):36–42 https://doi.org/10.1002/hast.645 .
Gonzales AL, Kwon EY, Lynch T, Fritz N. “Better everyone should know our business than we lose our house”: costs and benefits of medical crowdfunding for support, privacy, and identity. New Media Soc. 2018;20(2):641–58 https://doi.org/10.1177/1461444816667723 .
Dressler G, Kelly SA. Ethical implications of medical crowdfunding: the case of Charlie Gard. J Med Ethics. 2018;44(7):453–7 https://doi.org/10.1136/medethics-2017-104717 .
Snyder J, Cohen IG. Medical crowdfunding for unproven medical treatments: should Gofundme become a gatekeeper? Hast Cent Rep. 2019;49(6):32–8 https://doi.org/10.1002/hast.1066 .
Download references
Acknowledgements
I thank the editorial team at BMC Public Health for sending out this manuscript to five reviewers. I am grateful to the reviewers for carefully reviewing the manuscript and raising valid points on how the manuscript can be improved.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Finance and Accounting, Stockholm School of Economics in Riga, Strēlnieku iela 4a, Rīga, LV-1010, Latvia
Ágnes Lublóy
Department of Finance, Corvinus University of Budapest, Fővám tér 8, Budapest, 1093, Hungary
You can also search for this author in PubMed Google Scholar
Contributions
ÁL conceived and designed the study, downloaded the data from the public domain, developed the methodology, analysed the data, interpreted the results, and wrote the manuscript. The author read and approved the final manuscript.
Corresponding author
Correspondence to Ágnes Lublóy .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The author declares that she has no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lublóy, Á. Medical crowdfunding in a healthcare system with universal coverage: an exploratory study. BMC Public Health 20 , 1672 (2020). https://doi.org/10.1186/s12889-020-09693-3
Download citation
Received : 04 June 2020
Accepted : 14 October 2020
Published : 09 November 2020
DOI : https://doi.org/10.1186/s12889-020-09693-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical crowdfunding
- Universal health coverage
- Unmet health care need
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
How to Write a Medical Expenses Fund-Raising Letter
M.t. wroblewski, 29 sep 2017.

Soliciting people for money is never an easy task, especially against the backdrop of a poor economy. But when the cause is worthwhile, people often rally and try to do whatever they can to help. Such is often the case when someone is facing huge medical expenses. You can write a successful fund-raising letter–and watch those donations come streaming in–if you can write a compelling narrative explaining the person’s predicament and be sure to welcome donations of any monetary value.
Acknowledge that “times are tough” for many people right now–people who have lost their jobs and their homes and people who are underemployed. Make the point that times may be especially difficult for people who have encountered poor health (or a debilitating medical condition or whatever the specific case may be).
Request, right in the first paragraph of your fund-raising letter, that you are seeking donations to help defray the medical expenses of the subject of your letter. Be sure to note any common association or relationship the people may share, such as being neighbors in the same community, members of the same church, or patrons of the same civic group.
Tell the story of your subject’s medical predicament, being specific and descriptive, but not melodramatic and theatrical. (Chances are, the story is dramatic enough.) Include quotes from the subject’s family and physicians, if appropriate.
With specificity, explain what the subject has endured and his' or hers' prognosis. Invoke clear, simple English; if you must use high-brow medical terms (jargon), be sure to explain what they mean.
Conclude this “emotional appeal” section with the total amount of the medical expenses the subject is facing and how much of that total (if any) is covered by insurance.
Repeat your request for a monetary donation, imbuing a subtle sense of urgency that the money be donated as soon as possible. “Subtle sense of urgency” does not have to be a contradiction in terms if you say, for example: “Why not make your donation today, and rest assured that (the subject of the letter) will reap the benefits of your generosity immediately?”
Write a closing paragraph that thanks the recipient in advance for his or her donation – and even simply for considering it.

Write a post-script (a P.S.), as research has shown repeatedly that many people often scan a letter first for the correct spelling of their names (at the top) and then for the final thoughts (at the bottom). You may repeat your request for a financial donation, but be sure to phrase it in such a way that is different than in the body of the letter. A P.S. inherently “allows” you to be more personable and friendly, but don’t go overboard, either.
About the Author
With education, health care and small business marketing as her core interests, M.T. Wroblewski has penned pieces for Woman's Day, Family Circle, Ladies Home Journal and many newspapers and magazines. She holds a master's degree in journalism from Northern Illinois University.
Related Articles

How to Express Gratitude to Someone Who Gave You a...

How to Write an Amazing Letter of Appreciation

What to Say on an Appreciation Plaque

How to Write an Effective Conclusion Paragraph for...

How to Express Words of Sympathy

Top Things Kids Should Know When Writing a Paragraph

How to Write a Letter of Recommendation for Nursing

How to Communicate Your Hurt Feelings Effectively

What to Write in a Thank You Sympathy Card to Church...

How to Write an Essay in 150 Words


What to Say in Silent Auction Thank You Cards

How to Write a Request for a Waiver for the Military

How to Write a Thank You Letter to a Mayor

How to Write Character Letters About Siblings to Judges

How to Write an Informative Letter

How to Resign an Army Officer Commission

How to Use Contractions in a College Essay

How to Write a Letter to Local Compaines Asking for...

Fundraising Slogan Ideas

How to Write a Sponsorship Letter for National American...
Regardless of how old we are, we never stop learning. Classroom is the educational resource for people of all ages. Whether you’re studying times tables or applying to college, Classroom has the answers.
- Accessibility
- Terms of Use
- Privacy Policy
- Copyright Policy
- Manage Preferences
© 2020 Leaf Group Ltd. / Leaf Group Media, All Rights Reserved. Based on the Word Net lexical database for the English Language. See disclaimer .
Royal Medical Benevolent Fund
- You are here:
Essay competitions, awards and prizes
If you have a flair for essay writing, then look out for competitions run by the Royal Colleges and many other professional medical associations, usually to encourage interest in their specialty. Closing dates for submission fall throughout the year so keep your eyes open!
Some organisations that run competitions include:
British Association of Dermatologists
- British Association of Forensic Medicine
- General Medical Council
- Medical Women’s Federation
- Pain Relief Foundation
- Royal College of Obstetricians and Gynaecologists
- Royal College of Ophthalmologists
- Royal College of Pathologists
- Royal College of General Practitioners
- Royal College of Radiologists
- Royal Society of Medicine (for members only, costs £25 a year to join)
- Institute of Medical Ethics (for F1 & F2 UK doctors)
Project Funding
Some organisations and Trusts offer funding for research projects, vacation research work experience and intercalated degree year research. We’ve compiled a list of these, again it isn’t exhaustive so we do encourage further research.
Some of these applications may require a supporting statement from a member of academic staff. Check criteria carefully before applying.
The Biochemical Society
Grants are available for stipends of £200 per week for 6 – 8 weeks, and up to £1,600 in total, to support a summer placement in a lab for an undergraduate student. Applications must be made on behalf of and in association with a named student.
Website: www.biochemistry.org Email: [email protected]
The British Association of Dermatologists offer a range of awards between £250 and £3,000 towards fees and living expenses for an intercalated year project related to dermatology and skin biology. It also offers £500 undergraduate project grants.
Website: www.bad.org.uk Email: [email protected]
Association for the Study of Medical Education
The Association for the Study of Medical Education offers awards related to the development of excellent medical education. Applications are welcomed from anyone on the continuum of medical education (UG, PG or qualified and studying professional development) and will be assessed against their criteria. They also have a number of other essay prizes available and awards so it is worth researching their website.
Tel: 0131 225 9111 Website: www.asme.org.uk Email: [email protected]
The Genetics Society
The Genetics Society Summer Studentship scheme offers grants of up to £3,000 for undergraduate students interested in gaining research experience in any area of genetics by carrying out a research project over the long vacation ( more information ). They also have a range of competitions and awards that you can look into on their website.
Website: https://genetics.org.uk/grants/summer-studentships/ Email: [email protected]
The Institute of Medical Ethics
The Institute of Medical Ethics (IME) offers grants, student elective bursaries, and scholarships (covering the next academic year) for students wishing to do an intercalated degree in medical ethics or an allied subject.
Website: https://ime-uk.org/grants-and-competitions/
The Physiological Society
Vacation Studentships offer undergraduates the opportunity to undertake a research project on an area of physiology over their summer break. Working under an academic supervisor, they can get to experience day-to-day life in the laboratory first-hand. Funding of £150 a week, to cover living costs, is on offer for up to eight weeks.
Website: www.physoc.org Email: [email protected]
The Pathological Society
Funding for students wanting to intercalate a BSc in Pathology but who do not have LEA or other government support. Also offer awards to fund electives and vacation studies in pathology.
Website: www.pathsoc.org
The Paget’s Association
The Paget’s Association awards Student Research Bursaries of up to £6,000 to promising UK medical or science students (MRes, MSc, BSc or equivalent higher degree) to pursue research into any aspects of Paget’s Disease of Bone.
Tel: 0161 799 4646 Website
Other resources
The list above is not exhaustive so we do encourage further research.
A good place to start is RD Learning , a database of health-related research funding opportunities.
Please contact us if you notice any broken links, of any other funding opportunities or if any options are no longer running.
IELTS Writing Task 2 Sample Answer Essay: Medical Research (Real Past IELTS Exam)
by Dave | Real Past Tests | 0 Comment
This is an IELTS writing task 2 sample answer essay on the topic of whether governments should direct more funding towards medical or environmental research.
It’s a good topic to practice with because it focuses on two common IELTS topics: medicine and the environment.
Be sure to sign up for on Patreon.com/HowtodoIELTS for my exclusive Ebooks and other materials!
IELTS Writing Task 2 Sample Answer Essay: Medical Research
Governments should spend more money on medical research and less on researching the environment. To what extent do you agree or disagree?
Many believe governments today should prioritise funding for medicine over environmental studies. In my opinion, learning more about the environment is one way to inform policy regarding climate change but more money should be directed towards medical research.
Those advocating for increased focus on the environment are eager to understand and counter the effects of climate change. There is arguably no greater threat facing the future of human civilisation than a degrading natural world. At the moment, billions are being poured into studies to understand how fast the polar ice caps are melting, what the impact will be, the damage to ecosystems, the interrelation between humans and these delicate ecosystems as well as the role of fossil fuels in aggravating climate change. There are wildly different theories about all these areas and some think the best utilisation of research grants is to give scientists free rein to study and collaborate in the hope of coming to a stronger consensus, which can then shape international accords and domestic policy decisions.
Despite the force of the above argument, I believe health is a more tangible and pressing concern. There is constant disagreement from climate scientists and it is unclear if increased funding would be a remedy or injury. Health research is unequivocally positive. Some of the many advances in health from the last several decades include increased understanding of mental illness, less invasive procedures for surgery, better vaccines, and countless new iterations of advanced medical equipment. These are all put into practice immediately and save or better lives in every country around the world. More money for research now would open up possibilities for new medical innovations that could involve experimentation with genetic modification and greater understanding of disease prevention.
In conclusion, making sense of climate change is important but nothing is more essential than one’s health. Governments ought to find ways to balance these competing interests but also be mindful of what most benefits their present citizenry.
1. Many believe governments today should prioritise funding for medicine over environmental studies. 2. In my opinion, learning more about the environment is one way to inform policy regarding climate change but more money should be directed towards medical research.
- Paraphrase the overall topic for the whole essay.
- Write a clear opinion.
1. Those advocating for increased focus on the environment are eager to understand and counter the effects of climate change. 2. There is arguably no greater threat facing the future of human civilisation than a degrading natural world. 3. At the moment, billions are being poured into studies to understand how fast the polar ice caps are melting, what the impact will be, the damage to ecosystems, the interrelation between humans and these delicate ecosystems as well as the role of fossil fuels in aggravating climate change. 4. There are wildly different theories about all these areas and some think the best utilisation of research grants is to give them free rein to study and collaborate in the hope of coming to a stronger consensus, which can then shape international accords and domestic policy decisions.
- Write a clear topic sentence with your main idea at the end of it.
- Explain/develop the idea.
- Make your support as specific and clear as possible.
- State the results and the reasons to support your original main idea.
1. Despite the force of the above argument, I believe health is a more tangible and pressing concern. 2. There is constant disagreement from climate scientists and it is unclear if increased funding would be a remedy or injury. 3. Health research is unequivocally positive. 4. Some of the many advances in health from the last several decades include increased understanding of mental illness, less invasive procedures for surgery, better vaccines, and countless new iterations of advanced medical equipment. 5. These are all put into practice immediately and save or better lives in every country around the world. 6. More money for research now would open up possibilities for new medical innovations that could involve experimentation with genetic modification and greater understanding of disease prevention.
- Write a new topic sentence with a main idea at the end.
- Here I start with a counter-example to make it clear why this is my opinion.
- I transition to why health is important.
- I inclue a lot of specific detail related to health advances.
- Then I state why these advances are so important.
- Conclude your paragraph with more support – no need for summary.
1. In conclusion, making sense of climate change is important but nothing is more essential than one’s health. 2. Governments ought to find ways to balance these competing interests but also be mindful of what most benefits their present citizenry.
- Repeat your opinion.
- Include a final thought/detail for full marks from the examiner.
What do the words in bold below mean?
Many believe governments today should prioritise funding for medicine over environmental studies . In my opinion, learning more about the environment is one way to inform policy regarding climate change but more money should be directed towards medical research.
Those advocating for increased focus on the environment are eager to understand and counter the effects of climate change. There is arguably no greater threat facing the future of human civilisation than a degrading natural world . At the moment, billions are being poured into studies to understand how fast the polar ice caps are melting , what the impact will be, the damage to ecosystems , the interrelation between humans and these delicate ecosystems as well as the role of fossil fuels in aggravating climate change . There are wildly different theories about all these areas and some think the best utilisation of research grants is to give researchers free rein to study and collaborate in the hope of coming to a stronger consensus , which can then shape international accords and domestic policy decisions .
Despite the force of the above argument , I believe health is a more tangible and pressing concern . There is constant disagreement among climate scientists and it is unclear if increased funding would be a remedy or injury . Health research is unequivocally positive . Some of the many advances in health from the last several decades include increased understanding of mental illness , less invasive procedures for surgery , better vaccines , and countless new iterations of advanced medical equipment. These are all put into practice immediately and save or better lives in every country around the world. More money for research now would open up possibilities for new medical innovations that could involve experimentation with genetic modification and greater understanding of disease prevention .
In conclusion, making sense of climate change is important but nothing is more essential than one’s health. Governments ought to find ways to balance these competing interests but also be mindful of what most benefits their present citizenry .
prioritise make more important
medicine health related study
environmental studies learning about the natural world
inform policy regarding climate change help shape/make better decisions about global warming
directed towards focused on
advocating in favour of
increased focus more emphasis
eager excited for
counter argue against
arguably no greater threat facing probably nothing more pressing
degrading natural world hurting the environment
poured put into
how fast the polar ice caps are melting the speed with which icebergs are disappearing
damage injury
ecosystems plants and animals interacting with their environment
interrelation interaction
delicate ecosystems fragile environments
role part to play in
fossil fuels oil, gas
aggravating climate change making the environment worse
wildly different theories many different ideas
utilisation use
research grants money to study
give researchers free rein allow them to study whatever they want
collaborate work together
in the hope of with the goal of
coming to a stronger consensus agreeing on
shape international accords influence international agreements
domestic policy decisions a country’s laws
Despite the force of the above argument nonetheless
tangible real impact
pressing concern important problem
constant disagreement never agree on
climate scientists researchers looking into global warming
unclear equivocal
increased funding more money for
injury hurt
unequivocally positive definitely good
last several decades 30 or so years
increased understanding of mental illness more knowledge on mental disorders
less invasive procedures for surgery not have to cut into a person as much
vaccines shot to make you immune to a disease
countless new iterations many new versions
put into practice immediately used right away
open up possibilities allow for
new medical innovations new ideas in health
experimentation trying out ideas
genetic modification changing your genes/biology
disease prevention stopping illnesses
making sense of understanding
nothing is more essential than the most important thing is
balance equality
competing interests forces in conflict
mindful aware of
what most benefits their present citizenry the biggest advantage for all people of a country
Pronunciation
Listen and repeat:
praɪˈɒrɪˌtaɪz ˈmɛdsɪn ɪnˌvaɪərənˈmɛntl ˈstʌdiz ɪnˈfɔːm ˈpɒlɪsi rɪˈgɑːdɪŋ ˈklaɪmɪt ʧeɪnʤ dɪˈrɛktɪd təˈwɔːdz ˈædvəkeɪtɪŋ ɪnˈkriːst ˈfəʊkəs ˈiːgə ˈkaʊntə ˈɑːgjʊəbli nəʊ ˈgreɪtə θrɛt ˈfeɪsɪŋ dɪˈgreɪdɪŋ ˈnæʧrəl wɜːld pɔːd haʊ fɑːst ðə ˈpəʊlər aɪs ˈkæps ɑː ˈmɛltɪŋ ˈdæmɪʤ ˈiːkəʊˌsɪstəmz ˌɪntə(ː)rɪˈleɪʃən ˈdɛlɪkɪt ˈiːkəʊˌsɪstəmz rəʊl ˈfɒsl fjʊəlz ˈægrəveɪtɪŋ ˈklaɪmɪt ʧeɪnʤ ˈwaɪldli ˈdɪfrənt ˈθɪəriz ˌjuːtɪlaɪˈzeɪʃən rɪˈsɜːʧ grɑːnts gɪv rɪˈsɜːʧəz friː reɪn kəˈlæbəreɪt ɪn ðə həʊp ɒv ˈkʌmɪŋ tuː ə ˈstrɒŋgə kənˈsɛnsəs ʃeɪp ˌɪntə(ː)ˈnæʃənl əˈkɔːdz dəʊˈmɛstɪk ˈpɒlɪsi dɪˈsɪʒənz dɪsˈpaɪt ðə fɔːs ɒv ði əˈbʌv ˈɑːgjʊmənt ˈtænʤəbl ˈprɛsɪŋ kənˈsɜːn ˈkɒnstənt ˌdɪsəˈgriːmənt ˈklaɪmɪt ˈsaɪəntɪsts ʌnˈklɪə ɪnˈkriːst ˈfʌndɪŋ ˈrɛmɪdi ˈɪnʤəri ˌʌnɪˈkwɪvəkəli ˈpɒzətɪv lɑːst ˈsɛvrəl ˈdɛkeɪdz ɪnˈkriːst ˌʌndəˈstændɪŋ ɒv ˈmɛntl ˈɪlnɪs lɛs ɪnˈveɪsɪv prəˈsiːʤəz fɔː ˈsɜːʤəri ˈvæksiːnz ˈkaʊntlɪs njuː ˌɪtəˈreɪʃənz pʊt ˈɪntuː ˈpræktɪs ɪˈmiːdiətli ˈəʊpən ʌp ˌpɒsəˈbɪlɪtiz njuː ˈmɛdɪkəl ˌɪnəʊˈveɪʃənz ɛksˌpɛrɪmɛnˈteɪʃən ʤɪˈnɛtɪk ˌmɒdɪfɪˈkeɪʃən dɪˈziːz prɪˈvɛnʃən ˈmeɪkɪŋ sɛns ɒv ˈnʌθɪŋ ɪz mɔːr ɪˈsɛnʃəl ðæn ˈbæləns kəmˈpiːtɪŋ ˈɪntrɪsts ˈmaɪndfʊl wɒt məʊst ˈbɛnɪfɪts ðeə ˈprɛznt ˈsɪtɪznri
Vocabulary Practice
Remember and fill in the blanks:
Many believe governments today should p_____________e funding for m_____________e over e_________________________s . In my opinion, learning more about the environment is one way to i____________________________________e but more money should be d________________________s medical research.
Those a___________________g for i_______________________s on the environment are e______________r to understand and c_____________r the effects of climate change. There is a_______________________________g the future of human civilisation than a d__________________________d . At the moment, billions are being p__________________d into studies to understand h_____________________________________g , what the impact will be, the d____________e to e________________s , the i______________________n between humans and these d_____________________s as well as the r________e of f___________________s in a____________________________e . There are w________________________s about all these areas and some think the best u__________________n of r_____________________s is to g_____________________________n to study and c_______________e i_______________f c_______________________s , which can then s__________________________s and d________________________s .
D_______________________________________t , I believe health is a more t____________e and p______________________n . There is c___________________________t among c_____________________s and it is u_____________r if i____________________g would be a r_____________y or i__________y . Health research is u_______________________e . Some of the many advances in health from the l________________________s include i__________________________________s , l_______________________________y , better v____________s , and c_______________________s of advanced medical equipment. These are all p____________________________________y and save or better lives in every country around the world. More money for research now would o_______________________s for n___________________________s that could involve e_____________________n with g_________________________n and greater understanding of d_______________________n .
In conclusion, m________________________f climate change is important but n_________________________n one’s health. Governments ought to find ways to b_____________e these c_____________________s but also be m___________l of w______________________________________________y .
Listen and check:
Listening Practice
Learn about some real-life medical researchers at Mass General:
Reading Practice
Read about genetic engineering here:
https://www.wired.com/story/scientists-take-a-harder-look-at-genetic-engineering-of-human-embryos/
Speaking Practice
Talk about the health-related topic of walking below from the real IELTS speaking exam :
Do you go places on foot a lot? Did you walk more when you were younger? Why do some people prefer walking to driving a car? Do people in your country walk a lot? Real Past IELTS Exam
Writing Practice
Write about the following topic related to the environment and then check with my sample answer:
The increase in the production of consumer goods results in damage to the natural environment. What are the causes of this? What can be done to solve this problem? Real Past IELTS Exam
IELTS Writing Task 2 Sample Answer Essay: Demand for Consumer Goods
Recommended For You
Latest IELTS Writing Task 1 2024 (Graphs, Charts, Maps, Processes)
by Dave | Sample Answers | 147 Comments
These are the most recent/latest IELTS Writing Task 1 Task topics and questions starting in 2019, 2020, 2021, 2022, 2023, and continuing into 2024. ...
Recent IELTS Writing Topics and Questions 2024
by Dave | Sample Answers | 342 Comments
Read here all the newest IELTS questions and topics from 2024 and previous years with sample answers/essays. Be sure to check out my ...
Find my Newest IELTS Post Here – Updated Daily!
by Dave | IELTS FAQ | 18 Comments

IELTS Writing Task 2 Sample Answer: Medical Testing (Real Test)
by Dave | Real Past Tests | 4 Comments
This is an IELTS Writing Task 2 Sample Answer on the topic of medical testing on animals. Here is the question: Some ...
IELTS Writing Task 2 Sample Answer Essay: The Internet & School (Real Past IELTS Exam/Test)
by Dave | Real Past Tests | 9 Comments
This is an IELTS writing task 2 sample answer essay from the real exam on the topic of the internet and schools. Education ...
IELTS Writing Task 2 Sample Answer Essay: Zoos and Rare Animals
by Dave | Real Past Tests | 2 Comments
This is an IELTS writing task 2 sample answer essay on whether zoos are cruel and exploitive or helpful for rare animals from the real IELTS ...
Submit a Comment Cancel reply
You must be logged in to post a comment.
Exclusive Ebooks, PDFs and more from me!
Sign up for patreon.
Don't miss out!
"The highest quality materials anywhere on the internet! Dave improved my writing and vocabulary so much. Really affordable options you don't want to miss out on!"
Minh, Vietnam
Hi, I’m Dave! Welcome to my IELTS exclusive resources! Before you commit I want to explain very clearly why there’s no one better to help you learn about IELTS and improve your English at the same time... Read more
Patreon Exclusive Ebooks Available Now!
- Open access
- Published: 26 May 2022
Structural changes in the Russian health care system: do they match European trends?
- Sergey Shishkin ORCID: orcid.org/0000-0002-0807-3277 1 ,
- Igor Sheiman ORCID: orcid.org/0000-0002-5238-4187 2 ,
- Vasily Vlassov ORCID: orcid.org/0000-0001-5203-549X 2 ,
- Elena Potapchik ORCID: orcid.org/0000-0001-7004-3100 1 &
- Svetlana Sazhina ORCID: orcid.org/0000-0002-2023-3384 1
Health Economics Review volume 12 , Article number: 29 ( 2022 ) Cite this article
7934 Accesses
4 Citations
4 Altmetric
Metrics details
In the last two decades, health care systems (HCS) in the European countries have faced global challenges and have undergone structural changes with the focus on early disease prevention, strengthening primary care, changing the role of hospitals, etc. Russia has inherited the Semashko model from the USSR with dominance of inpatient care, and has been looking for the ways to improve the structure of service delivery. This paper compares the complex of structural changes in the Russian and the European HCS.
We address major developments in four main areas of medical care delivery: preventive activities, primary care, inpatient care, long-term care. Our focus is on the changes in the organizational structure and activities of health care providers, and in their interaction to improve service delivery. To describe the ongoing changes, we use both qualitative characteristics and quantitative indicators. We extracted the relevant data from the national and international databases and reports and calculated secondary estimates. We also used data from our survey of physicians and interviews with top managers in medical care system.
The main trends of structural changes in Russia HCS are similar to the changes in most EU countries. The prevention and the early detection of diseases have developed intensively. The reduction in hospital bed capacity and inpatient care utilization has been accompanied by a decrease in the average length of hospital stay. Russia has followed the European trend of service delivery concentration in hospital-physician complexes, while the increase in the average size of hospitals is even more substantial. However, distinctions in health care delivery organization in Russia are still significant. Changes in primary care are much less pronounced, the system remains hospital centered. Russia lags behind the European leaders in terms of horizontal ties between providers. The reasons for inadequate structural changes are rooted in the governance of service delivery.
The structural transformations must be intensified with the focus on strengthening primary care, further integration of care, and development of new organizational structures that mitigate the dependence on inpatient care.
In the last two decades, health care systems in the European Union countries have faced global challenges, including aging populations, a substantial rise in chronic and multiple diseases, the emergence of new medical and information technologies, and a growing citizen awareness of the role of a healthy lifestyle in disease prevention [ 1 ]. The responses of health systems to these challenges included structural changes in their organization with a focus on the promotion of healthy lifestyles and disease prevention, the growing scale of screening for early disease detection, strengthening primary care, changing the role of the hospitals, the development of chronic disease management programs, etc. [ 2 , 3 ]
Studies of these trends address mostly Western countries. Much less attention has been paid to the post-Soviet countries. In this paper, we study structural changes in the health care in Russia. Russian health care has inherited the Semashko model of health care organization. Its main distinction is state-centered financing, regulation, and provision of health care. The model has specific forms of provider organization, for example, outpatient clinics (polyclinics) with a large number of various specialists, the separation of care for adults and children, and large highly-specialized hospitals [ 4 ].
The Soviet and post-Soviet health systems have been underfunded. Public health funding in the 1990s dropped almost by one third in real terms [ 5 ]. The organization of medical care in the 1990s has not changed significantly relative to Soviet times, and the system has adapted through the reduction in the volume of services and increased payments by patients, frequently informal [ 6 ]. The surge in oil prices after 2000 allowed health funding to increase and while encouraged noticeable changes in service delivery.
The changes in the Russian health system have been discussed in the literature mostly focusing on specific sectors and health finance reforms [ 5 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 ]. But these changes in different sectors were not analyzed together, from a single methodological position, as changes in the structural characteristics of the Russian health care system, i.e. the changes in the ratio of different types of medical care, in the structure of medical service providers, in functionalities and modes of their interaction.
The objective of this paper is to explore the entire complex of structural changes over the past two decades in comparison with European trends. What were the structural changes in European health care systems, what were they like in Russia, and how can their differences be explained?
Study design
We followed a six-step methodological framework. The first stage involved designation of the types of medical care and the types of structural changes for identification and comparison. We considered four main areas of medical care delivery: preventive activities, primary care, inpatient care, long-term care. We focused on three different dimensions of structural changes: i) changes in the organizational structure of medical service providers; ii) changes in the structure of their activities (in its types and in their coverage of the population / patients); iii) changes in the organization of interaction between different service providers.
The second stage consisted of identifying for each type of medical care the changes in these three dimensions in the last twenty years before the COVID-19 pandemic. We described the changes that met two criteria: 1) these changes are assessed in the OECD, WHO, and World Bank reviews, and other review publications on this topic as the most noteworthy characteristics of the development of European health care systems, and 2) they have spread in a large number of European countries.
The changes identified according to the formulated criteria cover not all dimensions of structural changes for each type of medical care. For preventive activities, there are changes in the types of activities and in their coverage of the population. In primary and inpatient care, there are changes in the organizational structure of service providers, in the structure of their activities, and in the organization of interaction with other providers. In long-term care, there are changes in the structure of developed activities and their coverage of the population.
To describe the ongoing changes, we use both qualitative characteristics and, if possible, quantitative indicators that highlight them to the greatest extent.
The third stage involved detection of structural changes in four main areas of medical care delivery in Russia. We used the results of our previous studies and conducted an additional search for data characterizing structural changes in health care, using new statistical data, evidence derived from our survey of physicians and interviews with top managers in medical care system.
On the fourth stage we compared the identified structural changes in European health care systems (HCS) with the changes taking place in Russian health care. We identified the presence or absence of similar types of structural changes and the differences between them. The fifth stage was the consideration of the driving forces of structural changes in the Russian health care system. The sixth stage included discussion of the reasons for the distinctions with European developments.
Data sources
To identify the main structural changes in medical care delivery during last twenty years we searched the literature addressing both European HCS and Russia in the all aspects of changes of health care system indicators, better classified by MeSH term “health care reform”. We searched MEDLINE using the query: (russia OR europ* OR “european union” OR semashko) AND health care reform [mh] AND 2000:2021[dp]). All 788 findings were checked manually and 86 were relevant. We also used sources snowballed from these reports and the grey literature related to Russian health care, including those in limited circulation, unpublished documents, memorandums, and presentations from our personal collections covering more than twenty years.
We also used data from an online survey of 999 primary care physicians (further – survey) conducted by the authors in April–May 2019. The respondents representing 82 out of 85 regions of the Russian Federation were asked about implementation of the national prophylactic medical examination program. We also interviewed four leading specialists of the national Ministry of Health on the criteria for the inclusion of the components into the program.
To identify the driving forces of structural changes in the Russian health care system, we used materials from 10 interviews on the issues of implementing state health care programs that we conducted in 2019 with current and former top-managers in the federal government and in five regional governments. We also used the grey literature as well as published reports.
We used statistical data from the international databases of OECD [ 18 ], WHO [ 19 ], World Bank [ 20 ], as well as the Russian sources — the Federal State Statistics Service [ 21 ] and the Russian Research Instuitute of Health [ 22 ]. The data was analyzed for the period from 2000 to the latest date with available data for both EU member states and Russia. To ensure the comparability of the composition of countries in different years, the analysis of the dynamics of some indicators was limited to EU 19 members, i.e. excluding Cyprus, Greece, Croatia, Bulgaria, Luxemburg, Malta, Netherland, Poland, and Romania. The averages for EU 19 estimates are based on population size-weighted averages. If the studied publications and databases did not contain the necessary indicators, we made our own estimates.
Each section of the paper contains a brief description of the main trends in the European countries, and then provides a comparative analysis of the corresponding changes in Russian health care. The comparison is followed by a discussion of the driving forces and the limitations of structural changes in Russia compared to the main European trends. We limited our analysis to the pre – COVID-19 pandemic years.
The development of preventive activities
European hcs.
Most of them have implemented health check-ups, and population and opportunistic screenings for the early detection of diseases. These activities are viewed as a way to improve outcomes by ensuring that health services can focus on diagnosing and treating disease earlier [ 23 ]. The population covered by screenings is high and growing. In Germany 81% of population between 50 and 74 years in 2014 had been tested for colorectal cancer at least once, in Austria 78%, France 60%, Great Britain 48% [ 24 ].
The impact of these activities on health outcomes depends on the selection of preventive services, as well as on their implementation in specific national contexts. The selection of preventive services is increasingly based on research into their potential impact on mortality and other health indicators, as well as their cost effectiveness, with some services being declined because of their inadequate input into health gains [ 25 ]. It is particularly important that screenings are focused on socially disadvantaged groups with the highest probability of disease identification and the expected benefits of their management. Therefore, screening programs are based on the evaluation of local needs. Physicians have discretion in the choice of patients for screenings, depending on their importance for specific groups of the population, and individual risks and preferences.
It is increasingly common for a screening program to include follow-up management of any detected illnesses, with the implication that policy makers design such programs as a set of interrelated preventive and curative activities [ 26 ].
The original Semashko model and the current legislation prioritize preventive activities, while their implementation has been limited by the chronic underfunding of the health system. In the 2000s, the priority of prevention campaigns was revitalized in the form of a national prophylactic medical examination program (Prophylactic Program, called Dispanserization) that is a set of health check-ups and screenings. The major expectation from this Prophylactic Program is the same as in European HCS [ 27 ].
To supplement the analysis of the Prophylactic Program, we analyzed the evidence base for the components of the program and interviewed leading specialists of the federal Ministry of Health on the criteria for the inclusion of the components into the program. We found that some screenings were not evidence based and effect on the population health and/or health of participants is small [ 28 ]. The screening package of the dispanserization was expanded and reduced couple of times, but still number of ineffective screenings are included in the package (electrocardiography (ECG) screening of healthy subjects, prostate specific antigen (PSA) screening of middle age and adult men, urinalysis and routine blood tests, mammography from age 40 etc.).
Primary care physicians play a major role in conducting screenings and check-ups as well as subsequent interventions. There are also public health units responsible exclusively for these preventive activities in big polyclinics. Polled in 2019, primary care physicians responded that in 11% of polyclinics check-ups are carried out in these departments only, and in 24% of primary care organizations the check-ups are conducted by district physicians as well as by staff of these preventive units.
Under the current Prophylactic Program, people over 40 are supposed to have a set of check-ups annually; those 18–39 every three years. Most children go through physicals only. The official estimates of the coverage of the eligible population in the Prophylactic Program are around 100% [ 29 ], while service providers are less optimistic. According to the survey, more than half of the respondents reported that this share was less than 60%, while 17.4% reported less than 20% [ 27 ].
An important shortcoming of the Prophylactic Program design and implementation is the gap between its major objective and the capacity of primary care. The shortage of primary care physicians does not allow the target groups to be provided with all preventive services. Physicians have to distort the service to their registered population and to underprovide the follow-up care of detected cases. The lack of a systematic approach, less focus on local conditions, and the lack of a professional autonomy of providers are the major distinctions between Russian prevention campaigns and similar activities in Europe.
The Prophylactic Program is built on the presumption that preventive activities should include the follow-up management of any detected conditions. There is some evidence, however, that this is not taking place: according to our survey, a half of primary care physicians are unaware of the results of check-ups and screenings. The reported coverage and quality of the follow-up management of identified cases are low: a half of the respondents indicate that less than 60% of patients with identified diseases become objects of the follow-up disease management. Only 7.7% of respondents indicate that a set of disease management services corresponds to a pattern of dispensary surveillance issued by the federal Ministry of Health. The majority reports that these requirements are met only for some patients or are not met at all.
Disease management of newly identified chronic and multiple cases is focused on process rather than outcome indicators. The information on the latter is very fragmented. According to our survey, a decrease in the number of disability days of chronic patients is reported by only 14% of physicians. More than a half of respondents are unaware of the number of emergency care visits and hospital admissions of their chronic patients.
Strengthening primary care
There is a trend of multi-disciplinary primary care practices or networks development and promotion of teamwork and providers coordination in response to the growing complexity of patients. In Spain, France, and the UK it is increasingly common for large general practices to serve more than 20,000 people and provide a wider spectrum of services than in traditional solo and group practices. These emerging extended practices include pharmacists, mental care professionals, dieticians, and sometimes 2–3 specialists [ 30 , 31 ]. The role of nurses is also expanding. Most advanced nurses independently see patients, provide immunizations, health promotion, routine checks for chronically ill patients in all EU member states [ 32 ]. Related to these extended practices is the growing concentration of primary care providers via mergers and reconfigurations that increase the size of the units. The major benefits are economies of scale and scope through staff sharing and better integrated care.
There is also a general trend to strengthen the links with the local community, social care and hospitals [ 32 ]. Primary care providers are increasingly involved in chronic disease management programs together with other professionals in and out of general practices. Links with hospitals are developing beyond simple referral systems [ 33 ].
The trend of multidisciplinary practices development has greatly affected Russian health care. However, this trend in Russia differs significantly from the European HCS. It began in the 1980s, when large numbers of specialists were employed by polyclinics, which are the major providers of both primary care and outpatient specialty care. Today, large urban polyclinics employ 15–20 categories of specialists, and polyclinics in small towns 3–5 categories. The generalist who serves for the catchment area (district doctors) is limited in the scope of services they provide. Multidisciplinary practices are built through employing new specialists, while in European countries mainly through nurses and other categories of staff. Specialists in Russian polyclinics do not supplement, but essentially replace district doctors: they accounted for 66% of visits in 2019. Footnote 1
The scope of district doctors’ services is limited: at least 30–40% of initial visits end with referrals to a specialist or to a hospital, while in Europe only 5–15% [ 35 , 36 ]. Gatekeeping is promoted, but district doctors are overloaded and not interested in expanding the scope of their services. Specialists in polyclinics have insufficient training and poorly equipped, e.g. urologists do not do ureteroscopy and ophthalmologists do not practice surgery.
Since the 1990s, some regions started replacing district doctors and pediatricians with general practitioners. But this initiative has not been supported by the federal Ministry of Health, therefore the institution of a general practitioner is not accepted throughout the country. Currently, the share of general practitioners in the total number of generalists serving a catchment area is only 15% (Fig. 1 ). The model of general practice is used only in some regions. The main part of the primary care in the country is provided by district doctors and pediatricians, whose task profile remains narrower than that of general practitioners. The division of primary care for children and adults is preserved. The family is not a whole object of medical care. This division is actively defended by Russian pediatricians with references to specific methods of managing child diseases.
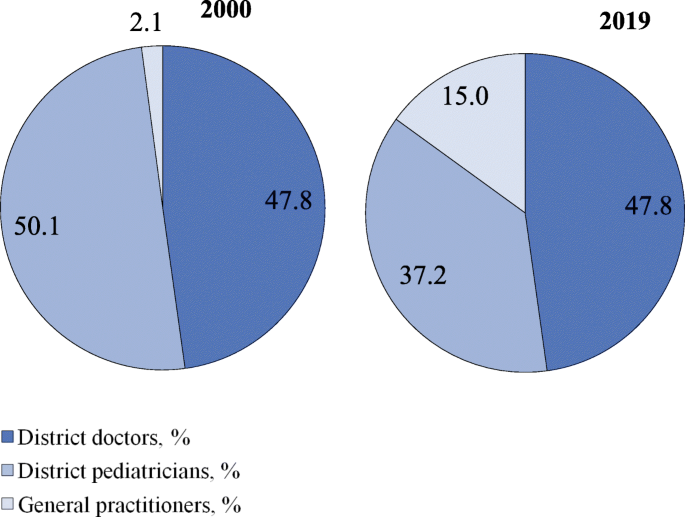
Distribution of generalists in Russia by categories in 2000, 2019. Source: Calculated from RRIH [ 22 , 37 ]
The prevailing trend in all European HCS is to increase the role of nurses. In Russia, the participation of nurses in medical care is limited to fulfilling doctors’ prescriptions and performing ancillary functions.
The transformation of inpatient care
Due to increased costs, technological advances in diagnosis and treatment, there were changes in patterns of diseases and patients treated in hospitals. A substantial amount of inpatient care has been moved to outpatient settings with a respective decrease in bed capacity. This is an almost universal trend in European HCS [ 19 ].
Hospitals continue to be centers of high-tech care, which concentrate most difficult cases and intensify inpatient care with a corresponding decrease in the average length of stay. These changes have been promoted by the move to diagnostic related groups based payment systems and a growing integration with other sectors of service delivery.
In many European countries, most hospitals no longer act as discrete entities and have become units of hospital-physician systems which are multi-level complex adaptive structures [ 3 ]. A new function of hospital specialists is their involvement in chronic disease management in close collaboration with general practitioners, outpatient specialists, and rehabilitative and community care providers [ 38 ].
Over the past two decades the treatment of relatively simple cases and preoperative testing have gradually moved to day care wards and polyclinics. In annual health funding, the federal government sets decreasing targets of inpatient care which are obligatory and which regions use to plan their inpatient care. However, inpatient care discharges per 100 people have been almost stable (21.9 in 2000 and 22.4 in 2018) in contrast to the EU 19 members Footnote 2 (18.4 in 2000 and 16.9 in 2018) [ 18 ]. The pressure of decreasing targets resulted in a drop in the average length of hospital stays (Fig. 2 ) and the total bed-days per person (Fig. 3 ). These indicators, along with bed supply (Fig. 4 ), decreased even faster than in the EU.
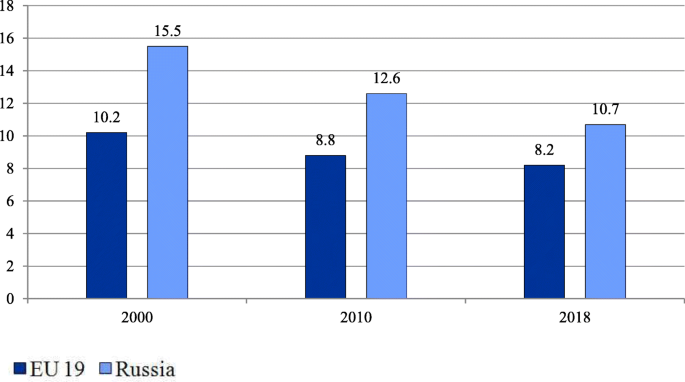
Average length of stay in hospital in EU members and Russia (days). Note: Calculated for EU 19 member states (see Methods). The EU 19 average length of hospital stay estimates are calculated as the sum of the products of inpatient care discharges by the average length of stay for each country, weighted average by the total inpatient care discharges. Source: OECD Health Statistics [ 18 ]
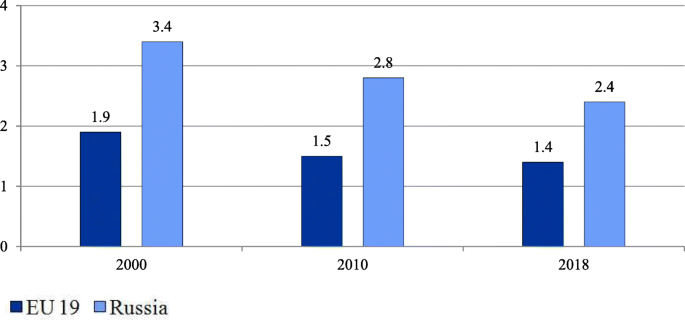
Number of bed-days per person in the EU and Russia. Note: Calculated for EU 19 member states (see Methods). EU 19 estimates are calculated as the sum of the products of inpatient care discharges by the average length of stay for each country weighted by the total population. Source: OECD Health Statistics [ 18 ]

Hospital beds per 1000 people in the EU and Russia. Note: Calculated as the average for all EU 28 members weighted by the total population. Source: World Bank [ 20 ]
At the same time, the intensity of medical care processes in hospitals in Russia remains significantly lower than in European countries. An indicator of this is the gap in the number of hospital employees per 1000 discharged (Table 1 ).
Over the past 20 years, significant efforts have been made to deploy day wards, both in hospitals and polyclinics, to reduce the burden on hospitals. As a result, the proportion of patients treated in day wards in the total number of patients treated in hospitals increased from 7.6% in 2000 to 20.8% in 2016 [ 21 ]. However, there is fragmentary evidence that this figure is still noticeably lower than in Europe. The share of cataract surgery carried out as ambulatory cases varies in most European countries between 80 to 99% [ 24 ] but is negligible in Russia.
Despite these positive trends, the health system remains hospital centered. The number of bed-days per person remains nearly twice as high as the EU average (Fig. 3 ).
An important trend is the increasing concentration of hospitals. The number of hospitals halved between 2000 and 2018, mostly due to mergers, but also due to the closures of inadequately equipped hospitals. This process has led to an increase in the average size of hospitals from 156 beds in 2000 to 223 beds in 2018 [ 21 ]. This figure is higher today than in Western countries with large territories. The average hospital size in France was 130 beds in 2018 and in Germany 215 beds in 2017 [ 18 ]. In Russia, with its very low population density, the reduction in the number of small rural hospitals resulted in some accessibility problems.
At the same time, the incorporation of previously independent polyclinics into hospitals is under way. The proportion of independent polyclinics in the total number of polyclinics has decreased from 35% in 2000 to 19% in 2014 [ 36 ].
The development of long-term care
Over the last 20 years, most European countries have increasingly developed the public provision of long-term care. The number of nursing and elderly home beds per 100,000 people in the EU increased from 581.7 in 2000 to 748.3 in 2014 [ 19 ], although the pace of changes, the coverage of citizens in need of long-term care, and its organization and funding differ substantially across countries [ 39 ]. Many countries control costs by keeping people in their homes longer and shifting the responsibility for non-institutional forms of care to communities [ 40 ]. An expected outcome of investment in long-term care is the reduction of informal care utilization.
Compared to European HCS, long-term care is underdeveloped in Russia. The number of nursing care beds declined from 14.7 per 100,000 people in 2011 to 10.6 in 2019 [ 22 ]. The share of citizens over working age and people with disabilities receiving outpatient and inpatient care within the long-term care system in the total number of citizens over working age and people with disabilities in need of long-term care, was only 2.9% in 2019 [ 41 ].
In contrast to the European HCS, Russia has not built a strong long-term care sector with the capacity to reduce the workload of acute inpatient care settings. Hospitals have to keep some patients longer resulting in a relatively higher length of stay. Palliative care as another sector of the long-term care which started to develop only a few years ago.
Driving forces and tools of structural changes in the Russian health care system
These changes have been driven by the federal and regional governments. They use two main tools to manage structural changes: 1) setting health care targets for the entire country and for regions, and 2) implementing vertical health care programs.
Since 1998, the federal government has annually approved a program of benefit packages for health (the Program). It sets targets for the utilization of medical care for each sector of service delivery, as well as unit cost targets. The Program is designed to balance the volumes of care with the amount of public funding. The annual versions of the Program gradually reduced the targets for inpatient care to encourage a shift to outpatient care. The federal targets are used in regional health planning. In the first decade of using the Program, the changes in the actual volume of medical care were small, but in the second decade, pressure from the federal center on the regions increased, and the gap between the federal targets and the actual utilization of care has noticeably narrowed (Table 2 ).
The development of the legislation on the delimitation of responsibility between levels of government, carried out in the last two decades, has consistently strengthened the regional governments role in restructuring medical care delivery. In 2012, almost all resources of health care governance were transferred from the municipal to the regional level (including the governance of primary health care. During the period 2000–2019 the number of public hospitals has decreased by 2.2 times, the number of hospital beds by 1.5 times, polyclinics 1.3 times, feldsher-obstetric posts 1.3 times. Footnote 3
When oil prices increased, the federal government poured additional resources into vertical programs. They are administered by the federal Ministry of Health and regional governments. The major programs: the ‘Priority national health project’ (2004–2012), the Prophylactic Program (2008 – ongoing), and regional programs for the modernization of health care (2011–2013). All additional and some basic resources are earmarked in an attempt to develop the highest priority activities: preventive care, obstetric care, cardiovascular surgery, oncology, etc.
The role of the centralized administration of these priority programs is controversial. The federal government initiated them, provided regions with additional funding, and made the program’s targets a priority of health policy. According to interviews with federal and regional officials, the implementation of programs is heavily controlled by the federal government: practically all decisions on specific activities, target indicators and resource allocation are approved on the federal level. The Russian regions have low flexibility to respond to local needs such as variation in disease incidence, the capacity of health care, or vulnerable population groups.
Structural changes in the provision of inpatient care were prompted by the introduction of a diagnostic related groups based payment system in the early 2010s. This was initiated by the federal government and implemented with the participation of the World Bank experts. It makes more profitable for hospitals to reduce the duration of hospitalizations and to complicate the structure of inpatient treatment [ 44 ].
We found that despite significant differences in health care organization, some structural changes in Russia have followed the general European trends. A similar rise in the coverage of the population with screenings is underway in Russia. There is a clear tendency to replace some inpatient care with day care. The volume of inpatient care is reducing —mostly due to a significant decrease in the length of stays, while the rate of hospital admission remains relatively stable. As in the most European HCS, the concentration of medical organizations and the formation of large outpatient and inpatient complexes is developing.
However, there are some substantial differences: the development of prevention programs is relatively less focused on the most vulnerable target groups and on local needs; primary care specialization is much stronger than in European HCS; the role of first contact generalists is waning; the worldwide tendency of increasing the role of nurses is almost invisible in Russia; long-term care is starting to develop but is still at a very low level and palliative care is in its infancy; integration in the health system are much less pronounced—both at the level of individual medical organizations and between health sectors.
The reasons for these differences are rooted in the specific features of health governance in Russia.
The Semashko model, by virtue of its genesis, reproduces the state administration patterns of a planned economy. The main driving force of changes is the bureaucracy. Its managerial activities are guided by the mechanism described by J. Kornai: ‘postponement, putting out the fire, postponement’ [ 45 ]. The governance focuses on mobilizing and distributing available resources to solve or mitigate the most pressing problems - ‘fire fighting’. This is what determines the fragmentation of structural changes in Russian health care compared to structural changes in European countries.
Materials of interviews with heads of federal and regional health authorities suggest that in the existing governance system each of its levels must demonstrate the success of its activity exclusively to the higher levels of management. It is easier to achieve success when solving problems of optimizing the volume of medical care and the organizational structure of medical institutions, and much more difficult when solving problems of improving the efficiency of all elements of medical care system, which requires changes in their functionality and ways of interaction. It requires more financial resources and better management at all levels of health governance.
A number of deeply rooted limitations for carrying out structural transformations in Russian health care can be highlighted.
Firstly, the low capacity of primary care providers and to some extent the unwillingness of patients to replace inpatient care with outpatient treatment prevents a shift of patients from hospitals to polyclinics.
Secondly, a feature of the Russian health care system is the weak development of horizontal links between medical organizations related to different levels of medical care, and between medical workers within medical organizations working in different departments [ 36 , 46 , 47 ]. The interaction of different providers is carried out mostly through vertical channels. This is a serious obstacle to the development of horizontal integration [ 36 ].
Thirdly, democratic institutions for the development of health care are historically underdeveloped in Russia and this influences the choice of health policy priorities. According to interviews with heads of regional health authorities, the role of local communities is negligible, and the role of the medical community is marginal. Professional organizations are rarely involved in decision-making on health issues. The input of public councils to government bodies is largely imitative. Information about the activities of the system as a whole and of individual medical organizations is restricted for public use. This enables health authorities to focus on achievements in their reports, while hiding shortcomings. Feedback from patients, and society as a whole, is poorly expressed.
Conclusions
Russian health care, whose genetic basis was the Soviet Semashko model, after a difficult ‘survival’ period in the 1990s, underwent significant structural changes over the next two decades. To a large extent, the directions of these changes have coincided with European trends. The prevention and the early detection of diseases have developed intensively. The reduction in hospital bed capacity and inpatient care was accompanied by an intensification of inpatient treatment and a decrease in the average length of stay. Russia has followed the European trend of service delivery concentration in hospital-physician complexes, while the increase in the average size of hospitals is even more substantial. Structural changes in primary care are much less pronounced. The resources and competences of providers and the governance of primary care are still not enough to abolish the hospital-centered model of service delivery. Russia has intensively implemented vertical health care programs to develop the priority activities, but still significantly lags in the level of development of horizontal ties among services providers.
Specific structural changes in Russia are rooted in the organization and governance of service delivery. The interests of federal and regional bureaucracies, which act as the main drivers of changes, are pushing them to prioritize the changes in volumes of medical care and organizational structure of health care providers and not spend a lot of effort on improving their functionality and modes of interaction between providers of medical care. An important role is also played by the low capacity of primary care units to provide quality care.
To respond effectively to modern global challenges, reduce mortality, and improve the health of the population, structural transformations in Russian health care must be intensified with the focus on strengthening primary care, the further integration of care, and an accelerated development of new structures that mitigate the dependence on inpatient care.
Availability of data and materials
The data used and analysed during the current study are publicly available.
Calculated using data from [ 34 ].
See Methods.
Calculated using data from [ 21 ].
Abbreviations
European Union
Health Care System
Organization for Economic Co-operation and Development
World Health Organization
World Health Organization. Better Health for Europe: more equitable and sustainable. Copenhagen: WHO; 2019. https://apps.who.int/iris/bitstream/handle/10665/327427/9789289054225-eng.pdf . Accessed 9 Mar 2021.
Kringos D, Boerma W, Bourgueil Y, et al. The strength of primary care in Europe: an international comparative study. Br J Gen Pract. 2013;63(616):e742–50. https://doi.org/10.3399/bjgp13X674422 .
Article PubMed PubMed Central Google Scholar
McKee M, Merkur S, Edwards N, Nolte E, eds. The changing role of the Hospital in European Health Systems. European Observatory on Health Systems and Policies. Cambrige University Press; 2020. https://www.euro.who.int/__data/assets/pdf_file/0010/448048/Changing-role-of-hospitals-eng.pdf . Accessed 11 Feb 2021.
Davis C. Priority and the shortage model: the medical system in the socialist economy. In: Davis C, Charemza W, editors. Models of disequilibrium and shortage in centrally planned economies. London: Chapman and Hall; 1989. p. 427–59.
Chapter Google Scholar
Shishkin S. Russia’s health care system: difficult path of reform. In: Alexeev M, Weber S, editors. The Oxford handbook of the Russian economy. Oxford: Oxford University Press; 2013. p. 748–74.
Google Scholar
Shishkin SV, Vlassov VV. Russia's healthcare system: in need of modernisation. BMJ. 2009;338:b2132. https://doi.org/10.1136/bmj.b2132 .
Rese A, Balabanova D, Danishevski K, McKee M, Sheaff R. Implementing general practice in Russia: getting beyond the first steps. BMJ. 2005;331(7510):204–7. https://doi.org/10.1136/bmj.331.7510.204 .
Human Rights in Patient Care. Stockholm Region Office in St.Petersburg. Russian Healthcare System Overview. St. Petersburg, 2010. 2010. https://health-rights.org/index.php/cop/item/russian-healthcare-system-overview . Accessed 29 Nov 2020.
Gordeev VS, Pavlova M, Groot W. Two decades of reforms. Appraisal of the financial reforms in the Russian public healthcare sector. Health Policy. 2011;102(2-3):270–7. https://doi.org/10.1016/j.healthpol.2010.08.009 .
Popovich L, Potapchik E, Shishkin S, Richardson E, Vacroux A, Mathivet B. Russian Federation: health system review. Health Syst Transit. 2011;13(7):1-190, xiii-xiv.
PubMed Google Scholar
Bochkareva VK. Health-care reform and ensuring equal access to free medical services. Probl Econ Transit. 2013;55(12);12-31. https://doi.org/10.2753/PET1061-1991551203 .
Sheiman I, Shevski V. Evaluation of health care delivery integration: the case of the Russian Federation. Health Policy. 2014. https://doi.org/10.1016/j.healthpol.2013.12.011 .
Kontsevaya A, Sabgaida T, Ivanova A, Leon DA, McKee M. How has the management of acute coronary syndrome changed in the Russian Federation during the last 10 years? Health Policy. 2017;121(12):1274-9. https://doi.org/10.1016/j.healthpol.2017.09.018 .
Tagaeva TO, Kazantseva LK. Public health and health Care in Russia. Probl Econ Transit. 2017;59(11-12):973-90. https://doi.org/10.1080/10611991.2017.1431488 .
Belova N. Health Care in Rural Areas. Sociol Res. 2018;57(2):123-35. https://doi.org/10.1080/10610154.2018.1577621 .
Sheiman I, Shishkin S, Shevsky V. The evolving Semashko model of primary health care: the case of the Russian Federation. Risk Manag Healthc Policy. 2018;11:209-20. https://doi.org/10.2147/RMHP.S168399 .
Somanathan A, Sheiman I, Salakhutdinova S, Buisman L. Universal health coverage in Russia: extending coverage for the poor in the post-soviet era. Universal health coverage study series. Washington, DC: Universal Health Coverage Study Series The World Bank Group; 2018. p. 37. https://openknowledge.worldbank.org/handle/10986/30026 . Accessed 10 Mar 2021.
OECD. Health Statistics. OECD; 2020. https://stats.oecd.org/Index.aspx?ThemeTreeId=9 . Accessed 01 Dec 2020.
World Health Organization (WHO). European Health for All database (HFA-DB). WHO; 2020. https://gateway.euro.who.int/ru/datasets/european-health-for-all-database/ . Accessed 29 Nov 2020.
World Bank. World Bank Open Data. The World Bank Group, 2020. https://data.worldbank.org/ .
Federal State Statistics Service website (Rosstat). Health care in Russia. Moscow: 2020. https://rosstat.gov.ru/folder/210/document/13218 . Accessed 02 Dec 2020.
Russian Research Institute for Health (RRIH). Health statistics. Moscow: 2020. https://mednet.ru/napravleniya/mediczinskaya-statistika . Accessed 29 Nov 2020.
International Agency for Research on Cancer. Cancer Screening in the European Union. Report on the implementation of the Council Recommendation on cancer screening. Lyon: European Commission; 2017. https://ec.europa.eu/health/sites/default/files/major_chronic_diseases/docs/2017_cancerscreening_2ndreportimplementation_en.pdf . Accessed 19 Dec 2020.
OECD. Health at a Glance 2019: OECD Indicators. Paris: OECD Publishing; 2019.
Book Google Scholar
McKee M, Rechel B. Screening. In: Rechel B and McKee M eds. Facets of public health in Europe. WHO Observatory for health systems and health reforms. Berkshire: Open University Press; 2014. https://www.euro.who.int/__data/assets/pdf_file/0003/271074/Facets-of-Public-Health-in-Europe.pdf . Accessed 21 Mar 2021.
Sagan A, McDaid D, Rajan S, Farrington J, McKee M. Screening: When is it appropriate and how can we get it right? European Observatory on health systems and health reforms. European Observatory Policy Brief. 35. Copenhagen, 2020. https://apps.who.int/iris/bitstream/handle/10665/330810/Policy-brief-35-1997-8073-eng.pdf . Accessed 20 Apr 2021.
Sheiman IM, Shishkin SV, Shevsky VI, Sazhina SV, Ponkratova OF. Regular medical check-ups in Russia: expectations and reality. Mir Rossii. 2021;30(4):6-29. https://doi.org/10.17323/1811-038X-2021-30-4-6-29 .
Rebrova OI, Fedyaeva VK, Omel'ianovskiĭ VV, Ilyin MA. Stage 1 screenings of periodical health check: a systematic review of long-term efficiency. Profilakticheskaya Meditsina. 2017;20(3):55-59. https://doi.org/10.17116/profmed201720355-59 .
Federal Fund of Mandatory Health Insurance. Report about the mandatory health insurance system activity in the Russian Federation in 2019. Mandatory Med Insur Russian Federat. 2020;4:22.
Dedeu T, Marti T. Multiprofile primary health care teams in Catalonia, Spain: a population-based effective model of service delivery. WHO; 2018. https://www.euro.who.int/__data/assets/pdf_file/0009/366498/HSS-NCDs-Policy-brief-cat.pdf . Accessed 15 Feb 2020.
Kumpunen S, Curry N, Farnworth M, Rosen R. Collaboration in general practice: surveys of GP practice and clinical commissioning groups. Nuffield trust, Royal College of General Practitioners; 2017. https://www.nuffieldtrust.org.uk/files/2017-10/collaboration-in-general-practice-2017-final.pdf . Accessed 20 Dec. 2020.
OECD. Realizing the full potential of primary care. Policy Brief. OECD; 2019. https://www.oecd.org/health/health-systems/OECD-Policy-Brief-Primary-Health-Care-May-2019.pdf . Accessed 11 Dec 2020.
Damiani G, Pascucci D, Sindoni A, et al. The bigger, the better? A systematic review on the impact of mergers on primary care organizations. Eur J Pub Health. 2021;31(2):244-52. https://doi.org/10.1093/eurpub/ckaa248 .
The Ministry of Health of the Russian Federation. The accounting form No. 30 of the Federal Statistical Surveillance for 2019 (raw data) (not in the public domain).
Kringos DE, WGW B, Hutchinson A, Saltman R. Building primary Care in a Changing Europe. Eur Observ Health Syst Health. Observatory Studies Series. 2015;38;172.
Sheiman I, Shevsky V. Concentration of health care providers: does it contribute to integration of service delivery? Risk Manag Healthc Policy. 2019;12:153-66. https://doi.org/10.2147/RMHP.S205905 .
Rugol LV, Son IM, Starodubov VI, Pogonin AV. Some results of healthcare reforming. Soc Aspects Popul. Health. 2021;67(1):4. https://doi.org/10.21045/2071-5021-2018-64-6-1 .
Article Google Scholar
Urbanski D, Reichert A, Amelung V. Discharge and Transition Management in Integrated Care. In: Amelung V, Stein V, Goodwin N, Balicer R, Nolte E, Suter E, editors. Handbook Integrated Care; 2017. p. 97–111.
Hernández-Quevedo C, Maresso A, Merkur S, Quentin W, Richardson E, Ginneken E. 20 years of health system reforms in Europe: what’s new? Eurohealth. 2018;24(2):23–8.
Spasova S, Baeten R, Vanhercke B. Challenges in long-term care in Europe. Eurohealth. 2018;24(4):7–12.
The presidium of the presidential Council for the Strategic Development and Priority Projects. The Federal Project ‘the senior generation’. Protocol No 16 dated December 24, 2018. The Ministry of Labour and Social Protection; 2018. https://mintrud.gov.ru/ministry/programms/demography/3 . Accessed 15 Nov 2020.
Government of the Russian Federation. Resolutions of the government of the Russian Federation ‘on the program of the state guarantees of free provision of medical care to Citizens’ 1998–2018. The Federal Compulsory Medical Insurance Fund. 2018. https://www.ffoms.gov.ru/system-oms/about-fund/questions-oms/programm-gos-guarantee/ . Accessed 11 Sept 2021.
The Ministry of Health of the Russian Federation. Reports on the implementation of the program of the state guarantees of free provision of medical care to Citizens, 1999–2019. Moscow: The Ministry of Health of the Russian Federation, 2000-2019.
Avxentyeva MV, Omelyanovskiy VV, Petrovskiy AV, et al. New approaches to the development of diagnostic related groups for Cancer pharmacotherapy in Russian Federation. Med Technol Assess Choice. 2018;2(32):8–22.
Kornai J. Economics of shortage. Amsterdam: Elsevier Science. 1980.
Kuhlmann E, Shishkin S, Richardson E, et al. Understanding the role of physicians within the managerial structure of Russian hospitals. Health Policy. 2019;123(8):773-81. https://doi.org/10.1016/j.healthpol.2019.05.020 .
Sazhina SV, Shevsky VI, Sheiman IM, Shishkin SV. Interaction of health care providers: physicians' survey outcomes. Soc Aspects Popul Health. 2021;67(1):4 http://vestnik.mdnet.ru/content/view/1230/30/lang,ru/ .
Download references
Acknowledgements
Authors’ information (optional).
Sergey Shishkin – DSc in Economics, Director, Centre for Health Policy, HSE University.
Igor Sheiman – PhD in Economics, Professor, Health Economics and Management Department, HSE University.
Vasily Vlassov – DSc in Internal Diseases, Professor, Health Economics and Management Department, HSE University.
Elena Potapchik – PhD in Economics, Leading Research Fellow, Centre for Health Policy, HSE University.
Svetlana Sazhina – MPA, Leading Analyst, Centre for Health Policy, HSE University.
The study was funded by the grant provided by the Ministry of Science and Higher Education of the Russian Federation (Grant Agreement No. 075–15–2020-928).
Author information
Authors and affiliations.
Centre for Health Policy, National Research University Higher School of Economics, 4 Slavyanskaya Ploshchad, Building 2, Moscow, Russia, 109074
Sergey Shishkin, Elena Potapchik & Svetlana Sazhina
Department of Health Care Administration and Economics, School of Politics and Governance, Faculty of Social Sciences, National Research University Higher School of Economics, 20 Myasnitskaya Ulitsa, Moscow, Russia, 101000
Igor Sheiman & Vasily Vlassov
You can also search for this author in PubMed Google Scholar
Contributions
Sergey Shishkin conceptualized, designed the study and supervised the work. All authors collected, analyzed and interpreted the data. Elena Potapchik, Svetlana Sazhina made statistical analysis. Sergey Shishkin, Igor Sheiman and Vasily Vlassov wrote a first draft of the manuscript. All authors critically reviewed the draft. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Sergey Shishkin .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Shishkin, S., Sheiman, I., Vlassov, V. et al. Structural changes in the Russian health care system: do they match European trends?. Health Econ Rev 12 , 29 (2022). https://doi.org/10.1186/s13561-022-00373-z
Download citation
Received : 19 January 2022
Accepted : 05 May 2022
Published : 26 May 2022
DOI : https://doi.org/10.1186/s13561-022-00373-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health care system
- Health service provision
- Primary care
- Inpatient care
- Structural changes
- Semashko model
Health Economics Review
ISSN: 2191-1991
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Analysis of the Financing of Russian Health Care over the Past 100 Years
Vladimir reshetnikov.
1 Department of Public Health and Healthcare, First Moscow State Medical University of the Ministry of Health of the Russian Federation (Sechenov University), 119991 Moscow, Russia; moc.liamg@22negvesra
Evgeny Arsentyev
Sergey bolevich.
2 Department of Human Pathology, First Moscow State Medical University of the Ministry of Health of the Russian Federation (Sechenov University), 119991 Moscow, Russia; ur.xednay@1102hcivelob
Yuriy Timofeyev
3 Faculty of Business and Management, National Research University Higher Schools of Economics, 101000 Moscow, Russia; [email protected]
Mihajlo Jakovljević
4 Department of Global Health Economics and Policy, Faculty of Medical Sciences, University of Kragujevac, 34000 Kragujevac, Serbia; moc.liamg@amahtogatradis
5 Division of Health Economics, Lund University, SE 220 07 Lund, Sweden
The evolution of epidemiological burden in Imperial Russia and, consecutively, the Union of Soviet Socialist Republics (USSR), took place mostly over the duration of the past century. It is very important since dozens of Eastern European and Asian nations, with similarities in life style, regardless of dominant Orthodox Christian, Sunni-Shia Islamic, or Shamanic ethno-religious patterns, share this old statehood tradition. This profound change reflected in gradual movement from communicable, infectious diseases, traumatism, and early childhood and maternal mortality towards chronic non-communicable diseases [ 1 ]. To some extent, these changes were accelerated by two world wars and the deep regulatory reforms of social and pension systems, together with health care provision and financing mechanisms imposed, as a result of the Bolshevik, October Revolution in 1917. This long-term evolution, particularly in the post-World War II decades, was ultimately associated with the occurrence of population aging throughout entire Northern Hemisphere [ 2 ]. It got worse in the East due to the deep Russian recession reaching the bottom in 1998 and effectively dragging all mutually dependent formerly centrally-planned economies [ 3 ]. Compared to their Western European counterparts, Russian and other Eastern European ethnicities mostly remain in a slightly earlier stage of population ageing, which is yet tangible by serious policies [ 4 ]. Since the beginning of the 21st century, bold economic recovery and growth took place, ultimately leading to successful fertility policies. The boost in total fertility levels, which was raised from 1.3 to 1.7 children per woman of reproductive age, was the highest net achievement of its kind by any European country during the second decade of the 21st century [ 5 ]. All of these complex historical changes following the business cycles [ 6 ] in the capitalist free-market economies had heavily reflected the ability of the Russian Federation and its predecessor states to increase investment in healthcare and provide equitable and affordable medical care to its citizens [ 7 ]. Therefore, this paper attempts to look at the inner legislative evolution of health financing in Russia over the last 100 years.
At the beginning of the 20th century, a progressive form of medical care for the population—Zemstvo district medicine—was embodied in the Russian Empire. However, a significant drawback of rural medicine was its extremely high cost. At the end of the 19th and the beginning of the 20th century, most Zemstvos spent between 25% and 40% of their budget on healthcare [ 8 ]. For example, in 1887, the Cheboksary Zemstvo district spent 40.6% of its budget on medicine. The cost of Zemstvo district medicine in 1912 in 40 Zemstvo provinces accounted for 26% of the total Zemstvo district budget [ 9 ].
After the October Revolution of 1917, the Bolshevik government made a decision about concentrating the entire healthcare management of the country in a single, competent body that would be under their full control. In addition, in 1918, in the Russian Soviet Federative Socialist Republic (RSFSR), the first nationwide medical delivery system was created [ 10 ]. The People’s Commissariat of Health was established and was a state body responsible for all the country’s health care. The first Commissar of Health was Nikolay Andreyevich Semashko [ 11 ].
Figure 1 shows government spending on the health care system as a percentage of the country’s total budget for the RSFSR in 1918–1921 and for the USSR in 1922–1989.

Government expenditure on health from the Russian Soviet Federative Socialist Republic (RSFSR) to the Union of Soviet Socialist Republics (USSR).
After the legalization of the central health authority of the republic, the government began the construction of a unified state system of health care financing. Until 1919, there were two main sources of health care financing in the country: the state-governed one and, superior to it, an insurance-based system, which was funded by employers’ tax contributions. Thus, for the final implementation of a single, Soviet, medicine, it was necessary to eliminate “insurance medicine”. Despite the resistance of insurance companies, in February 1919, the Council of People’s Commissars approved the document “On the transfer of the entire medical part of the former health insurance funds to the People’s Commissar of Health”, and liquidated health insurance companies.
Nevertheless, even after the acquisition of insurance resources, the funds for health care were still not sufficient. Moreover, during the period of the new economic policy, the Bolshevik government decided to revive the elements of insurance-based medical care, but within the framework of the social insurance system. In 1921–1923, the employers’ insurance premiums were determined for certain types of social insurance, including the medical insurance premium of 5.5%–7% of the wage fund. The exact values of these premiums were dependent on the type of occupational hazards [ 11 ].
However, insurance medicine was already an integral part of the unified health care system, which made it possible to accumulate additional funds to finance health care (through insurance funds formed from employers’ contributions). The contributions to the All-Union Fund were transferred from the central social insurance authorities directly to the People’s Commissariat of Health [ 12 , 13 ].
During this period, the state insurance model of the organization of health care actually operated. Nevertheless, there was still not enough money for health care.
Since 1928, after the start of the implementation of the five-year plans for the development of the national economy of the USSR, social policy faded into the background: the health care system was financed according to the residual principle. Due to the economic growth after the beginning of the first five-year plan, under the conditions of a shortage of resources, there was an increasing gap between the economic and social aspects of development. With a significant increase of investment in the industrial sector, the portion of expenditures allocated toward the social sphere and health care in particular decreased. Most of the medical institutions were transferred from the state to the local budget, which was not sufficient everywhere. This circumstance led to the shutdown of a number of medical institutions and the introduction of paid medical services. However, soon the 3rd All-Russian Congress of Health Departments proclaimed the inviolability of the basic principles of health care: namely, its state-funded and free-of-charge basis. This important change ultimately led to the Semashko system, delivering the first-ever universal health coverage nationwide, to all of its citizens, regardless of their household income, at the basic medical technology level of that time. This contribution is recognized in health economics literature [ 7 ].
In the 1930s, the residual principle of health care financing remained in the republic: allocations for health care were decreasing. However, in 1934, elements of insurance medicine were completely abolished, and allocations for medical assistance to the insured were included into the general health budget. Financing of medical care was carried out exclusively at the expense of state budget funds. This model of healthcare financing existed until 1989 [ 14 ].
It is fair to say that “free” health care in the USSR (like other social funds) was provided by direct underpayments for labor and deductions from wages in the form of taxes. Thus, the state acted as a mediator, performing the functions of redistribution, transferring of funds from employment income to those citizens who could not provide themselves with a subsistence minimum [ 15 ].
After the outbreak of World War II, allocations for health care steadily declined due to the need to develop the military industry. A particularly sharp decline in the financing of health care occurred in 1941, after the USSR entered World War II. In 1941, healthcare accounted for only 3.6% of the total budget of the USSR. Only by 1948, it became possible to achieve pre-war levels of spending on healthcare: 5.3% of the total budget.
However, since 1950, due to the rearmament of the army, as well as the indirect participation of the USSR in the Korean War, healthcare expenditure again decreased, reaching 4.6% of the total budget in 1953.
In the period of the Khrushchev’s “ thaw ” in the USSR, the amount of government expenditure directed toward health care began to grow. By the early 1960s, healthcare expenditure reached 6%–6.5% of the total budget of the USSR.
Between 1965 and 1980, the real level of healthcare spending increased. Low inflation led to a substantial increase in real spending. However, this real growth did not keep pace with the general growth of the economy and social spending. The portion of health care in the state budget fell from 6.5% in 1965 to 4.5% by 1985. This circumstance indicated both a worsening of the economic situation and a decreased priority role of healthcare in the government’s agenda.
In the 1960s, approximately 6%–6.5% of GDP was allocated for health care, and in the last years of the USSR’s existence the level dropped to 3%–3.5%, which was significantly lower than in the countries of the Organization for Economic Cooperation and Development (OECD). (For comparison, in 1985, this rate was 6.5% and 12.9% in the United Kingdom and the United States, respectively) [ 16 ].
During the “ perestroika ” period (period of transformation), the Soviet government significantly increased total health expenditure in nominal terms, but during these years the inflation rate exceeded the increase in spending. The portion of the state budget allocated toward health care grew, reaching a value of 5.6% in 1990 (not more than 3% of GDP) [ 17 ].
Thus, since 1985, the actual level of expenditure on healthcare again steadily declined, reaching 2.6% of GDP by 1995. The situation was particularly aggravated by the difficult economic situation in the country associated with the collapse of the USSR.
Figure 2 demonstrates public healthcare expenditure in the Russian Federation. The reform of the Russian health care financing began in 1991 due to the inability of the state to provide the formerly guaranteed volume of free medical services. The German model of health care, based on the principles of medical insurance, was chosen as a guideline. This model was considered to be the most optimal for Russia, since it provided for the preservation of state control in financing (and, therefore, control of the health care system) [ 18 ].

Expenditures of the budget system of the Russian Federation on the health care system (consolidated budget of the Russian Federation and budgets of state extra-budgetary funds). Note: Since 2005, data on the consolidated budget of the Russian Federation are provided taking into account the budgets of state extra-budgetary funds. From 1995 to 2010, the cost of physical culture is taken into account. Since 2011, only expenditure on healthcare has been presented. Budgets of state extra-budgetary funds include compulsory health insurance. Thus, the compulsory insurance contributions of all Russian employers are also included in the official statistical report of public expenditure on health.
However, the transition to the budget-insurance model of health financing did not allow for more than 3.1% of GDP to be allocated to healthcare. Only since 2005, after an increase in budget allocations, spending on healthcare reached 3.7% of GDP. Despite a certain positive trend (an increase in spending on health care to 4.3% of GDP in 2009), in 2013–2014, health financing fell again to 3.2% of GDP. In 2016, this rate was 3.6% of GDP. Thus, in the history of Russian healthcare, expenditure on healthcare never exceeded the Soviet level of 6–6.5%. The health system input–output ratio can be roughly observed through the relationship between total health spending and core efficiency indicators, such as life expectancy at birth. According to recent research, the Russian Federation and the surrounding countries of the Commonwealth of Independent States (CIS) are achieving bold progress, although are still lagging against Western Europe [ 19 ]. Current health system vulnerabilities also present room for improvements and hidden opportunities in the form of net gains in human longevity and improvements in other morbidity- and mortality-related outcomes to be achieved by increased investment in healthcare [ 20 ]. This fact presents a window of opportunity for the Russian Federation’s future healthcare planning strategies during the 2020s.
Author Contributions
Conceptualization, V.R., E.A. and S.B.; methodology, V.R.; validation, V.R., Y.T. and M.J.; formal analysis, E.A.; investigation, E.A.; resources, V.R.; data curation, E.A.; writing—original draft preparation, E.A.; writing—review and editing, Y.T.; visualization, Y.T.; supervision, V.R.; project administration, M.J.
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Joseph Brodsky papers
- PDF Finding Aid
- Ask a Question
- Collection Overview
- Finding Aid View
- Digital Materials
- Container List
Scope and Contents
The Joseph Brodsky Papers document the life and work of Russian-born poet, essayist and Nobel Laureate Joseph Brodsky. The papers consist of correspondence, writings, personal papers (including legal, medical and financial records), audiovisual material, teaching material, student papers, newspaper clippings and printed ephemera, spanning the years 1890-2004, with the bulk of the material dating from the period 1972-1996. The papers document all aspects of Brodsky's professional life, including writings, appearances, readings, lectures, advocacy and relations with other literary figures. The research interest of the papers encompasses Russian-language poetry, the Soviet emigre experience, and poetry translation. Researchers interested in Brodsky's creative process will find much relevant material, including multiple drafts (many corrected) of poems and essays (including translations by Brodsky and others). Teaching material is present in small quantities and provides only sporadic documentation of Brodsky's career as an educator. Personal papers are also present and chiefly document immigration and other legal affairs. Brodsky's work, while rarely political, reflects broad historical and political themes that defined his era: empire, emigration, and the relationship of the individual to the state. The trajectory of Brodsky's publishing and teaching is inextricable from the emigre experience, as his early works were censored in the Soviet Union and promoted by publishers and scholars in the United States. After the fall of the Soviet Union, the Russian literary public was able to "reclaim" Brodsky openly and his works (including Russian translations of his essays) were published there. Brodsky's bilingual emigre identity is elucidated in his writings. A significant proportion of Brodsky's poetry was translated from Russian to English, often by multiple translators, and some poems exist in alternate versions. Brodsky's prose was also oft-translated: his early essays were written in Russian and translated into English, though most of his prose was written in English. While Brodsky's notes and corrections indicate engagement with the translation of his prose, it is evident that his commitment to and involvement in the translation of his poetry was profound. Brodsky's personal papers document his bitter struggle with American and Soviet bureaucracies as he tried first to have his parents visit him in the United States and then to attend his father's funeral. After emigration, as evidenced particularly in his letters to editors, Brodsky lent his international acclaim to the cause of politically persecuted literary figures in the Soviet Union and elsewhere. Brodsky's literary milieu, like his life and work, was transnational and multilingual. Correspondence, writings and audiovisual recordings document his close relationships with fellow Nobel Laureates Seamus Heaney, Czes?aw Mi?osz and Derek Walcott and with English-language poets Anthony Hecht and Mark Strand, among others. Many of these poets translated Brodsky's poetry or dedicated poems to Brodsky in memorium. Hundreds of aspiring and accomplished Russian-language poets also sent him manuscripts, as evidenced in Writings of Others.
- circa 1890-2004
- Majority of material found within 1972 - 1996
- Brodsky, Joseph, 1940-1996
Language of Materials
In Russian and English.
Conditions Governing Access
The materials are open for research. Access to some material is restricted, as detailed in the following paragraphs. Consult the appropriate curator for more information. Letters of Recommendation (Boxes 21-22), Student Papers (Boxes 127-131) and Restricted Papers (Boxes 214-217) are restricted until 2071. The notebooks in Box 40 are partially restricted until 2071. Access to the original notebooks is restricted. A microfilm of unrestricted pages is available. Boxes 168-169, 171-176, 220-225, and 232 (audiovisual material): Restricted fragile material. Reference copies may be requested. Consult Access Services for further information. Boxes 218-219, 226 and 233-241: Restricted fragile material. Reference copies are available for electronic documents. Consult Access Services for further information. For other materials, reference surrogates have been substituted in the main files. For further information consult the appropriate curator.
Existence and Location of Copies
Portions of the collection are available on microfilm.
Conditions Governing Use
The Joseph Brodsky Papers is the physical property of the Beinecke Rare Book and Manuscript Library, Yale University. Literary rights, including copyright, belong to the authors or their legal heirs and assigns. For further information, consult the appropriate curator.
Immediate Source of Acquisition
Purchased on the Edwin J. Beinecke Book Fund from Lame Duck Books in 2004. One box was donated by the Estate of Joseph Brodsky in 2005. According to a letter in her correspondence (April 1996), Ann Kjellberg (Joseph Brodsky's assistant and, after his death, literary executor) began to assemble an archive of Brodsky's papers in 1991. This effort continued after his death in 1996. Friends and associates of Brodsky (George Kline, Carl Proffer, Masha Vorobiov and others) sent Kjellberg originals and photocopies of papers to be included in the archive. Provenance of individual items can sometimes be traced by Kjellberg's or others' notes on the material.
Arrangement
Organized into eleven series: I. Correspondence, 1964-2004. II. Writings, 1959-2000. III. Interviews and Speeches, 1974-1996. IV. Teaching Material and Student Papers, 1973-1995. V. Personal Papers, 1961-2000. VI. Photographs, 1890-2001. VII. Audiovisual Material, 1953-2002. VIII. Clippings, 1964-2002. IX. Printed Material, 1920-2003. X. Artwork, 1972-1986. XI. Papers of Others, 1912-2000.
Associated Materials
Printed material received with the collection was removed for separate cataloging and can be accessed by searching the library's online catalog.
115.28 Linear Feet ((228 boxes) + 3 broadside)
Catalog Record
A record for this collection is available in Orbis, the Yale University Library catalog
Persistent URL
https://hdl.handle.net/10079/fa/beinecke.brodsky
Additional Description
The Joseph Brodsky Papers document the life and work of Russian-born poet, essayist and Nobel Laureate Joseph Brodsky, with a particular emphasis on the time period of his residence in the United States (1972-1996). The papers consist of correspondence, writings, personal papers (including legal, medical and financial records), audiovisual material, teaching material, student papers, newspaper clippings and printed ephemera, spanning the years 1890-2004, with the bulk of the material dating from the period 1972-1996.
Joseph Brodsky, 1940-1996
Joseph Brodsky, Russian-born poet, essayist and Nobel Laureate, was born in Leningrad on May 24, 1940 to Aleksandr Ivanovich Brodskii and Mariia Moiseevna Brodskaia (nee Vol'pert). His birth was just one year before the start of the Leningrad Blockade; thus his early years were ones of extreme hardship. The Brodsky family's Jewish heritage exposed them to the anti-Semitic atmosphere of the post-war Soviet Union, causing Aleksandr Ivanovich to lose his rank in the Army and preventing Joseph from entering into the submarine academy. The communal apartment where Brodsky lived with his parents (and where his parents lived until their deaths) was memorialized in his essay "A room and a half." Joseph Brodsky ended his formal schooling by walking out of his public school classroom at age fifteen and worked in a variety of places, including a factory, a morgue, and on geological expiditions. He began to write poetry in his teens and soon demonstrated a keen interest in translation. He taught himself Polish and English in order to translate poetry, including that of Czes?aw Mi?osz and John Donne. Brodsky's Russian literary influences included Anna Akhmatova, Osip Mandelshtam, Boris Pasternak and Marina Tsvetaeva. His early writings in Russia were circulated in samizdat (self-published) collections, the most complete one compiled by Vladimir Maramzin. Brodsky was arrested several times starting in 1961, tried in 1964 as a "social parasite" ( tuneiadets ), and sentenced to five years of labor in Norenskaia (a village in the Arkhangelsk Province of northern Russia). Brodsky lived in Norenskaia from March of 1964 to October of 1965 and wrote prolificly there. Brodsky's trial and sentence brought him increasing international attention when Frida Vigdorova's transcript was publicized in the Western media. It was also around this time that his poetry began to be compiled and published in the United States. Stikhotvoreniia i Poemy (Washington, D.C. & New York: Inter-Language Literary Associates) was published in in 1965, followed by Ostanovka v pustyne (New York: Izdatel'stvo imeni Chekhova) in 1970. Even after his release from Norenskaia, Brodsky continued to be at constant risk of arrest. In 1972 he was forced to emigrate when he was suddenly granted a visa (for which he had not applied) to emigrate to Israel. He had to leave Russia within a matter of weeks. Brodsky traveled to Austria, where he stayed with W.H. Auden for several weeks, and to England before coming to the United Sates. He accepted a position as Poet in Residence at the University of Michigan (a post that Carl Proffer, founder of Ardis Publishing, was instrumental in securing). Brodsky taught at Michigan until 1981, when he accepted a permanent position on the faculty of Mount Holyoke College. He then divided his time between New York City and South Hadley, Massachusetts. He became a United States citizen in 1977. Brodsky never returned to Russia after emigrating, though later in his life political circumstances would have allowed it and his Russian readers clamored for it. Among Brodsky's many awards and honors are a John Simon Guggenheim Memorial Foundation Fellowship (1977), a John D. and Catherine T. MacArthur Foundation award (1981), a National Book Critics Circle award (1986), the Nobel Prize in Literature (1987), France's Order of the Legion of Honor (1991), and honorary degrees from Yale University (1978), Dartmouth College (1989), and Oxford University (1991). He was Poet Laureate of the United States from 1991 to 1992. Brodsky suffered from heart disease throughout his adult life and he had several open-heart surgeries. He died of heart failure on January 28, 1996. During his lifetime, much of Brodsky's collected poetry and prose was published by Ardis in Ann Arbor, Michigan (Russian-language poetry) and Farrar, Straus and Giroux in New York (English-language poetry, English translations and prose collections). Brodsky's major publications from 1977 to 2000 include:
- Chast' rechi: Stikhotvoreniia 1972-76 (Ardis, 1977)
- Konets prekrasnoi epokhi: Stikhotvoreniia 1964-71 (Ardis, 1977)
- V Anglii (Ardis, 1977)
- A Part of Speech (Farrar, Straus and Giroux, 1980)
- Rimskie elegii (New York: Russica, 1982)
- Novye stansy k Avguste: Stikhi k M.B., 1962-1982 (Ardis, 1983)
- Less Than One: Selected Essays (Farrar, Straus & Giroux, 1986)
- Uraniia (Ardis, 1987)
- To Urania: Selected Poems 1965-1985 (Farrar, Straus & Giroux, 1988)
- Watermark (Farrar, Straus & Giroux, 1992)
- On Grief and Reason: Essays (Farrar, Straus & Giroux, 1995)
- Peizazh s navodneniem (Dana Point, California: Ardis, 1996)
- So Forth: Poems (Farrar, Straus & Giroux, 1996)
- Collected Poems in English, 1972-1999 (Farrar, Straus & Giroux, 2000)
Processing Information
The collection was formerly classed as Uncat.MSS 649, Uncat.MSS 766, Uncat.MSS 876 and Uncat.MSS 926. The Library of Congress system is used to transliterate Russian, but diacritics are not used. Illustrative examples are: Iuz Aleshkovskii and Efim Etkind. Names of Russian emigres are spelled in accordance with the individual's usage or record of publication. Therefore these spellings do not necessarily conform to standard Library of Congress transliteration. For example, the spelling Joseph Brodsky is used throughout the finding aid, while Brodsky's parents are referred to as Aleksandr Brodskii and Mariia Brodskaia. Electronic files were refreshed into the Yale University Library Rescue Repository. Technical specifications are filed with the media in Restricted Fragile. Boxes 227-231 and folders 3767-3822 and 4710-4758 are unused. Original videocassettes are now housed in boxes 171-176. Restricted fragile material. Boxes 161-167 and folders 3645-3723, 3725-3736, 3747-3756, 3758-3766 are unused. Original audiocassettes and reel-to-reel audiotapes are now housed in boxes 220-225 and 232. Restricted fragile material.
- American literature -- 20th century
- Ardis (Firm)
- Auden, W. H. (Wystan Hugh), 1907-1973
- Audiocassettes
- Audiovisual materials
- Authors, American -- 20th Century -- Archives
- Authors, Russian -- 20th Century -- Archives
- Barańczak, Stanisław, 1946-2014
- Berlin, Isaiah, 1909-1997
- Born digital
- Brodski, Mariia
- Brodskiĭ, Aleksandr
- Clippings (information artifacts)
- Dovlatov, Sergeĭ, 1941-1990
- Electronic documents
- Emigration and immigration
- Essays -- 20th Century
- Essays -- Translations into English
- Essays -- Translations into Russian
- Farrar, Straus, and Giroux
- Golyshev, Viktor, 1937-
- Hecht, Anthony, 1923-2004
- Jangfeldt, Bengt, 1948-
- Katilius, Elmira
- Katilius, Ramunas, 1935-2014
- Kjellberg, Ann
- Kline, George L. (George Louis), 1921-2014
- Mandelʹshtam, Nadezhda, 1899-1980
- Mandelʹshtam, Osip, 1891-1938
- Maramzin, Vladimir, 1934-
- Miłosz, Czesław, 1911-2004
- Nobel Prize winners
- Nobel lectures, including presentation speeches and laureates' biographies
- Photographs
- Picken, Margo
- Poetry -- 20th Century
- Poetry -- Translations into English
- Poetry -- Translations into Russian
- Poetry International (Festival)
- Poets, American -- 20th century
- Poets, Russian -- 20th Century
- Proffer, Carl R.
- Proffer, Ellendea, 1944-
- Russia -- Emigration and immigration
- Russian literature -- 20th Century
- Samizdat -- Russia
- Schiltz, Véronique, 1942-
- Shults, Sergei
- Solzhenit͡syn, Aleksandr Isaevich, 1918-2008
- Spender, Stephen, 1909-1995
- Sumerkin, Alexander, 1943-2006
- Translators
- Ufli︠a︡nd, Vladimir, 1937-
- Underground literature -- Soviet Union
- United States -- Emigration and immigration
- Verheul, Kees, 1940-
- Viereck, Peter, 1916-2006
- Vorobiov, Masha
- Walcott, Derek, 1930-2017
- Weissbort, Daniel, 1935-2013
- Wilbur, Richard, 1921-2017
- Ėtkind, E. G. (Efim Grigorʹevich), 1918-1999
Finding Aid & Administrative Information
Repository details.
Part of the Beinecke Rare Book and Manuscript Library Repository
121 Wall Street New Haven, CT 06511
Opening Hours
Access information.
The Beinecke Library is open to all Yale University students and faculty, and visiting researchers whose work requires use of its special collections. You will need to bring appropriate photo ID the first time you register. Beinecke is a non-circulating, closed stack library. Paging is done by library staff during business hours. You can request collection material online at least two business days in advance of your visit, using the request links in Archives at Yale. For more information, please see Planning Your Research Visit and consult the Reading Room Policies prior to visiting the library.
Navigate the collection
Joseph Brodsky Papers. Beinecke Rare Book and Manuscript Library, Yale University.
Cite Item Description
Joseph Brodsky Papers. Beinecke Rare Book and Manuscript Library, Yale University. https://archives.yale.edu/repositories/11/resources/784 Accessed August 18, 2024.
What happened in the Kolkata rape case that triggered doctors’ protests?
Activists and doctors in India demand better safeguarding of women and medical professionals after a trainee medic was raped and murdered in Kolkata.

Activists and doctors across India continued to protest on Wednesday to demand justice for a female doctor, who was raped and murdered while on duty in a hospital in the eastern city of Kolkata.
Feminist groups rallied on the streets in protests titled “Reclaim the Night” in Kolkata overnight on Wednesday – on the eve of India’s independence day – in solidarity with the victim, demanding the principal of RG Kar Medical College resign. Some feminist protesters also marched well beyond Kolkata, including in the capital Delhi.
Keep reading
Doctors across india protest rape and murder of medic in kolkata, india supreme court to monitor investigations into manipur sexual violence, goals not guns: how a girls football team in india’s manipur beats violence, four arrested after spanish blogger on india motorcycle tour gangraped.
While the protests were largely peaceful, a small mob of men stormed the medical college and vandalised property. This group was dispersed by the police.
This comes after two days of nationwide protests by doctors following the incident at RG Kar Medical College in West Bengal’s capital city. “Sit-in demonstrations and agitation in the hospital campus will continue,” one of the protesting doctors, identified as Dr Mridul, told Al Jazeera.
Services in some medical centres were halted indefinitely, and marches and vigils shed light on issues of sexual violence, as well as doctors’ safety in the world’s most populous nation.
What happened to the doctor in Kolkata?
A 31-year-old trainee doctor’s dead body, bearing multiple injuries, was found on August 9 in a government teaching hospital in Kolkata.
The parents of the victim were initially told “by hospital authorities that their daughter had committed suicide,” lawyer and women’s rights activist Vrinda Grover told Al Jazeera. But an autopsy confirmed that the victim was raped and killed.
Grover has appeared for victims in sexual violence cases in India in the past, including Bilkis Bano , a Muslim woman who was gang-raped during the 2002 Gujarat riots, and Soni Sori, a tribal activist based in Chhattisgarh state.
Thousands of doctors marched in Kolkata on Monday, demanding better security measures and justice for the victim.
On Tuesday, the Kolkata High Court transferred the case to the Central Bureau of Investigation (CBI).
The Federation of Resident Doctors Association (FORDA) called for a nationwide halting of elective services in hospitals starting on Monday. Elective services are medical treatments that can be deferred or are not deemed medically necessary.

On Tuesday, FORDA announced on its X account that it is calling off the strike after Health Minister Jagat Prakash Nadda accepted protest demands.
One of these demands was solidifying the Central Protection Act, intended to be a central law to protect medical professionals from violence, which was proposed in the parliament’s lower house in 2022, but has not yet been enacted.
FORDA said that the ministry would begin working on the Act within 15 days of the news release, and that a written statement from the ministry was expected to be released soon.
Press release regarding call off of strike. In our fight for the sad incident at R G Kar, the demands raised by us have been met in full by the @OfficeofJPNadda , with concrete steps in place, and not just verbal assurances. Central Healthcare Protection Act ratification… pic.twitter.com/OXdSZgM1Jc — FORDA INDIA (@FordaIndia) August 13, 2024
Why are some Indian doctors continuing to protest?
However, other doctors’ federations and hospitals have said they will not back down on the strike until a concrete solution is found, including a central law to curb attacks on doctors.
Those continuing to strike included the Federation of All India Medical Associations (FAIMA), Delhi-based All India Institute Of Medical Sciences (AIIMS) and Indira Gandhi Hospital, local media reported.
Ragunandan Dixit, the general secretary of the AIIMS Resident Doctors’ Association, said that the indefinite strike will continue until their demands are met, including a written guarantee of the implementation of the Central Protection Act.
Medical professionals in India want a central law that makes violence against doctors a non-bailable, punishable offence, in hopes that it deters such violent crimes against doctors in the future.
Those continuing to protest also call for the dismissal of the principal of the college, who was transferred. “We’re demanding his termination, not just transfer,” Dr Abdul Waqim Khan, a protesting doctor told ANI news agency. “We’re also demanding a death penalty for the criminal,” he added.
“Calling off the strike now would mean that female resident doctors might never receive justice,” Dr Dhruv Chauhan, member of the National Council of the Indian Medical Association’s Junior Doctors’ Network told local news agency Press Trust of India (PTI).
Which states in India saw doctors’ protests?
While the protests started in West Bengal’s Kolkata on Monday, they spread across the country on Tuesday.
The capital New Delhi, union territory Chandigarh, Uttar Pradesh capital Lucknow and city Prayagraj, Bihar capital Patna and southern state Goa also saw doctors’ protests.

Who is the suspect in the Kolkata rape case?
Local media reported that the police arrested suspect Sanjoy Roy, a civic volunteer who would visit the hospital often. He has unrestricted access to the ward and the police found compelling evidence against him.
The parents of the victim told the court that they suspect that it was a case of gang rape, local media reported.
Why is sexual violence on the rise in India?
Sexual violence is rampant in India, where 90 rapes were reported on average every day in 2022.
Laws against sexual violence were made stricter following a rape case in 2012, when a 22-year-old physiotherapy intern was brutally gang-raped and murdered on a bus in Delhi. Four men were hanged for the gang rape, which had triggered a nationwide protests.
But despite new laws in place, “the graph of sexual violence in India continues to spiral unabated,” said Grover.
She added that in her experience at most workplaces, scant attention is paid to diligent and rigorous enforcement of the laws.
“It is regrettable that government and institutions respond only after the woman has already suffered sexual assault and often succumbed to death in the incident,” she added, saying preventive measures are not taken.
In many rape cases in India, perpetrators have not been held accountable. In 2002, Bano was raped by 11 men, who were sentenced to life imprisonment. In 2022, the government of Prime Minister Narendra Modi authorised the release of the men, who were greeted with applause and garlands upon their release.
However, their remission was overruled and the Supreme Court sent the rapists back to jail after public outcry.
Grover believes that the death penalty will not deter rapists until India addresses the deeply entrenched problem of sexual violence. “For any change, India as a society will have to confront and challenge, patriarchy, discrimination and inequality that is embedded in our homes, families, cultural practices, social norms and religious traditions”.
What makes this case particularly prominent is that it happened in Kolkata, Sandip Roy, a freelance contributor to NPR, told Al Jazeera. “Kolkata actually prided itself for a long time on being really low in the case of violence against women and being relatively safe for women.”
A National Crime Records Bureau (NCRB) report said that Kolkata had the lowest number of rape cases in 2021 among 19 metropolitan cities, with 11 cases in the whole year. In comparison, New Delhi was reported to have recorded 1, 226 cases that year.
Prime Minister Modi’s governing Bharatiya Janata Party (BJP) has called for dismissing the government in West Bengal, where Kolkata is located, led by Mamata Banerjee of All India Trinamool Congress (AITC). Banerjee’s party is part of the opposition alliance.
Rahul Gandhi, the leader of the opposition in parliament, also called for justice for the victim.
“The attempt to save the accused instead of providing justice to the victim raises serious questions on the hospital and the local administration,” he posted on X on Wednesday.
Roy spoke about the politicisation of the case since an opposition party governs West Bengal. “The local government’s opposition will try to make this an issue of women’s safety in the state,” he said.
Have doctors in India protested before?
Roy explained to Al Jazeera that this case is an overlap of two kinds of violence, the violence against a woman, as well as violence against “an overworked medical professional”.
Doctors in India do not have sufficient workplace security, and attacks on doctors have started protests in India before.
In 2019, two junior doctors were physically assaulted in Kolkata’s Nil Ratan Sircar Medical College and Hospital (NRSMCH) by a mob of people after a 75-year-old patient passed away in the hospital.
Those attacks set off doctors’ protests in Kolkata, and senior doctors in West Bengal offered to resign from their positions to express solidarity with the junior doctors who were attacked.
More than 75 percent of Indian doctors have faced some form of violence, according to a survey by the Indian Medical Association in 2015.
What happens next?
The case will now be handled by the CBI, which sent a team to the hospital premises to inspect the crime scene on Wednesday morning, local media reported.
According to Indian law, the investigation into a case of rape or gang rape is to be completed within two months from the date of lodging of the First Information Report (police complaint), according to Grover, the lawyer.
The highest court in West Bengal, which transferred the case from the local police to the CBI on Tuesday, has directed the central investigating agency to file periodic status reports regarding the progress of the investigation.
The FIR was filed on August 9, which means the investigation is expected to be completed by October 9.
Bengal women will create history with a night long protest in various major locations in the state for at 11.55pm on 14th of August’24,the night that’ll mark our 78th year as an independent country. The campaign, 'Women, Reclaim the Night: The Night is Ours', is aimed at seeking… pic.twitter.com/Si9fd6YGNb — purpleready (@epicnephrin_e) August 13, 2024
Shawnee Mission Northwest student dies after medical emergency during workout
SHAWNEE, Kan. (KCTV) - A 15-year-old student at Shawnee Mission Northwest High School has died just days after the academic year started.
A sophomore student was taken to the hospital after requiring medical attention during an off-season conditioning practice. Johnson County MED-ACT confirmed that emergency services were called Wednesday afternoon to Shawnee Mission Northwest High School, and they took a 15-year-old student in critical condition to the hospital.
The school district learned Friday that the student had passed away.
The district shared the news in an email sent to families.
Gruman mentioned that there are many things that are not yet known about Ovet’s death. The incident has had a district-wide impact.
“This is shocking news to all of us. It’s not supposed to happen. Young people aren’t supposed to die,” Shawnee Mission School District spokesperson David Smith said. “All of us are just trying to come to terms with that and process it and to feel the grief that’s associated with this. This is not what is supposed to happen.”
Smith also said Ovet will be missed by many.
“From the reactions that I’ve heard from teachers and other staff that this was a great kid and there is really going to be a loss at Northwest.”
The school has staff available to talk with anyone who is struggling to handle the emotional situation. The district said Ovet was a beloved member of the Shawnee Mission Northwest Community.
“This was shocking news to all of us. It’s not supposed to happen. Young people aren’t supposed to die,” Shawnee Mission School District chief communications officer David Smith said. “All of us are just trying to come to terms with that, process it, and feel the grief that’s associated with this. This is not what is supposed to happen.”
Ovet’s family is asking for privacy during the devastating time.
Read the full email from Shawnee Mission Northwest High School below:

Copyright 2024 KCTV. All rights reserved.

Johnson County Museum closes after visitors damage exhibit

Former teacher pleads guilty after students reveal illegal relationships

Blue Springs Police: Mass shooting linked to ‘violent’ motorcycle gang

Cheerleader dies after parents allegedly treat life-threatening injuries with smoothies, vitamins instead of medical care

3 family members killed in crash while on the way to teenager’s college move-in day

Restaurant in Kansas City’s 18th and Vine District announces plans to close

Woman charged with burglary after shooting deaths of father, son in Freeman
Latest news.

Community mourns loss of sophomore during off-season practice

Fatal shooting reported near Kansas City park, one in stable condition

Hundreds gather to honor life of Shawnee Mission Northwest football player

Argument with stranger leads to murder charges for Independence man

Attempt to scam $10K off Missouri resident lands one man behind bars

Overland Park man injured when SUV flips after rear-end collision on Highway 71

Driver injured after bird causes motorcycle to swerve into oncoming traffic
- Things To Do
- Advertise with Us
- Newsletters
- Connect With Us
- For Subscribers
- Contributor Content
- Home & Garden Ideas

GoFundMe launched to help WAPL-FM's Rick McNeal as he faces new challenges in his recovery
APPLETON- As longtime WAPL-FM morning show co-host Rick McNeal continues to recover from medical issues amid new challenges, a GoFundMe has been established to help get him back on his feet.
McNeal has been absent from “The Rick and Cutter Show” since mid-March after falling in his apartment and developing cellulitis, a painful bacterial infection, and a blood clot in his left leg. He spent nine days in the hospital before being moved to a rehabilitation facility.
In an update to listeners on the show’s Facebook page in mid-April, McNeal reported that he had been able to stand on his infected leg for the first time without assistance, but there have since been setbacks and financial hurdles.
In the GoFundMe launched Wednesday by friend Amy Sterken, she writes:
“He was on the road to recovery and able to walk a few feet when an antibiotic he was on caused kidney failure. While recovering from that, the muscle mass in his legs that enabled him to walk, degenerated. This put him back at square one.
“It has been a struggle to start standing again, and I hope that he will be walking again before too long. However, the insurance company and Medicare have deemed his progress too slow and discontinued coverage. He is now on the hook for $7,500 out of pocket before the end of the week and another $11,000 before the end of the month. At this rate, another $11,000 at the end of next month.
Without this continued therapy, he is likely to never walk again.”
More than $11,000 of the $45,000 goal had been raised by Thursday morning.
More: 95.9 KISS-FM announces date for Katie Schurk and Nick Vitrano's return to air with Otis Day
More: 'I'm taking a new road': WBAY bids farewell to Kathryn Bracho after 21 years, as she moves on from TV news
In a post on “The Rick and Cutter Show’s” Facebook page on Wednesday, co-host Cutter asked listeners of the classic rock station to help out however they can.
“I just talked to Rick and it’s time for all of us to come together and help the man who’s helped us time and time again,” he wrote. “He’s done more for this community than he probably knows, now it’s time for this community to support him. Even if it’s just a little bit, I’m begging let’s do this for Rick.”
McNeal and his sense of humor have been a fixture at WAPL for nearly 40 years, including more than 30 with former co-host Len Nelson. There has been a flood of support for him over the last three months.
"People love Rick, and even if you don't love him, you still kind of love him," Cutter told the Green Bay Press-Gazette. "He has a way of words. He's one of the best writers I've ever met in my life. But people miss him, and I miss him. I think at the end of the day, this isn't about telling jokes on a radio station, this is about his life, and people want to help. It's awesome to see the outpouring of love for him."
When the idea of a GoFundMe was first proposed, McNeal said he worried people might think he was "some kind of beggar," but then he thought of the countless times he has been a part of fundraisers and benefits on air at WAPL for people in need. He never viewed those people that way.
"It's so gratifying, looking down the list of people who have already donated and seeing the names of friends, old and new, as well as listeners to whom I've become acquainted over the years," McNeal said in a message to the Press-Gazette. "It's perhaps even more gratifying to see name after name that I don't recognize of people I've never met who felt strongly enough to donate money to help the disembodied voice on the radio."
Earlier this month, McNeal shared a photo of himself with a smile on the radio show's Facebook page with the caption: "Proof of life photo. Contrary to what may have heard or hoped I am still alive if not kicking."
Kendra Meinert is an entertainment and feature writer at the Green Bay Press-Gazette. Contact her at 920-431-8347 or [email protected] . Follow her on X @KendraMeinert .
- Share full article
Advertisement
Supported by
Leonard Hayflick, Who Discovered Why No One Lives Forever, Dies at 96
A biomedical researcher, he found that normal cells can divide only a certain number of times before they age — which, he said, explained aging on a cellular level.

By Clay Risen
Leonard Hayflick, a biomedical researcher who discovered that normal cells can divide only a certain number of times — setting a limit on the human life span and frustrating would-be-immortalists everywhere — died on Aug. 1 at his home in Sea Ranch, Calif. He was 96.
His son, Joel Hayflick, said the cause was pancreatic cancer.
Like many great scientific findings, Dr. Hayflick’s came somewhat by accident. As a young scientist in the early 1960s at the Wistar Institute, a research organization at the University of Pennsylvania, he was trying to develop healthy embryonic cell lines in order to study whether viruses can cause certain types of cancer.
He and a colleague, Paul Moorhead, soon noticed that somatic — that is, nonreproductive — cells went through a phase of division, splitting between 40 and 60 times, before lapsing into what he called senescence.
As senescent cells accumulate, he posited, the body itself begins to age and decline. The only cells that do not go into senescence, he added, are cancer cells.
As a result of this cellular clock, he said, no amount of diet or exercise or genetic tweaking will push the human species past a life span of about 125 years.
This finding, which the Nobel-winning virologist Macfarlane Burnet later called the Hayflick limit, ran counter to everything scientists believed about cells and aging — especially the thesis that cells themselves are immortal, and that aging is a result of external causes, like disease, diet and solar radiation.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
- Nation & World
- Environment
- Coronavirus
Road rage driver faces murder charge after Columbus teen dies from fatal gunshot
A teenage boy died Tuesday at a United Dairy Farmers store in a road rage shooting on the city's Southwest Side, according to Columbus police.
Police received a report at 8:11 p.m. of a shooting at the UDF store at 3535 Clime Road near Demorest Road, according to city police 911 dispatchers. Responding officers found the teen, identified by police as Gage Anderson, 17, suffering from a gunshot wound and unresponsive.
Medics took Anderson to OhioHealth Grant Medical Center, Downtown, where he was pronounced dead at 8:40 p.m., according to police dispatchers.
Police took Skyler Burley, 30, into custody following a chase that ended in the 3800 block of Lynward Road, just over a mile away from the shooting, police said.
Officers said Burley and Anderson did not know each other and the shooting stemmed from a road rage dispute. Burley was charged with murder and booked into the Franklin County jail.
Witnesses described a vehicle leaving the scene, and a police helicopter crew identified it. Officers stopped it near the intersection of Lynward Road and Maurine Drive.
According to court records, Burley was charged with aggravated menacing in November 2018. The charges were dismissed at the prosecutor’s request. Aggravated menacing is a first degree misdemeanor in Ohio in which the defendant alleges to cause someone serious physical harm.
Details of the previous arrest were not immediately available.
Anyone with information on the shooting can contact Detective Stevens at 614-645-3750, the homicide unit at 614-645-4730, or Central Ohio Crime Stoppers at 614-461-8477.
@ShahidMeighan
Ukraine war latest: Ukraine blows hole in another Russian bridge; Kursk offensive puts 'new constraints' on Putin's war plans
Ukraine has attacked a second Russian bridge in the Kursk region in a week as it continues its offensive across the border. Analysts say the incursion has put pressure on Russian forces across the frontline and forced Vladimir Putin to decide how to defend the border long-term.
Sunday 18 August 2024 12:09, UK
- Ukraine blows hole in second Russian bridge
- Kursk offensive puts new pressures on entire Russian frontline, analysts say
- Safety 'deteriorating' at Ukrainian nuclear power plant
- Ukrainian drone sparks fire at Russian oil depot
- Russia launches third ballistic missile attack on Ukrainian capital this month
- 'We could lose': Russian state TV commentators gloomy over Kursk
- Sean Bell: Humiliated Putin will respond ruthlessly to Ukrainian masterstroke
- Michael Clarke : Pokrovsk in real trouble as Russian troops advance
- Listen to the Daily above and tap here to follow wherever you get your podcasts
- Live reporting by Brad Young
We've had more details from Belarusian President Alexander Lukashenko on his movement of troops to the Ukrainian border.
Minsk has deployed nearly a third of its armed forces along the entire border, the Belta state news agency reported.
The exact number of soldiers was not specified, but Belarus' professional army consists of 48,000 and around 12,000 state border troops, according to the 2022 International Institute for Strategic Studies' Military Balance.
The president claimed Ukraine had stationed more than 120,000 troops at its border with Belarus.
"Seeing their aggressive policy, we have introduced there and placed in certain points - in case of war, they would be defence - our military along the entire border," Belta cited Mr Lukashenko as saying in an interview with Russian state television.
Yesterday, Kyiv said it had seen no signs of a Belarusian troop build-up at the border.
Belarusian defence minister Viktor Khrenin said on Friday there was a high probability of an armed provocation from Ukraine and that the situation at their shared border "remains tense".
Western leaders have left "handcuffs" on Ukrainians using their donated weapons because they fear playing to Vladimir Putin's agenda, military analyst Sean Bell says.
While the UK gave Ukraine free reign over its donated Storm Shadow missiles, so long as they hit military targets, the British government wants consensus with the US before they are used inside Russia - and "the US is rather cautious still".
Bell explains the argument made in the West - especially the US - is that they do not want to lend any credence to Putin's claims that Russia is fighting NATO or the West, rather than Ukraine.
" The risk is it plays to that agenda and Putin starts saying 'I'm actually in a war against the West' and therefore starts to respond accordingly."
Bell said: "But these handcuffs on the Ukrainians led to President Zelenskyy last night, in his nightly address, praising the West, particularly singling out the UK, for providing great weapons but also urging that the limitations are freed."
Belarusian President Alexander Lukashenko says Ukraine has stationed more than 120,000 troops at its border with Belarus.
Minsk has sent military formations along its entire border in response, Russia's RIA state news agency said.
Mr Lukashenko, one of Vladimir Putin's closest international allies, said the border is mined "as never before" and that Ukrainian troops would incur huge losses if they tried to cross it.
More detail now on Russia's overnight missile attack on Kyiv, which Ukraine says were "most likely" North Korean weapons.
Serhiy Popko, the head of the Kyiv military administration, said: "According to preliminary information, the Russians again, for the third time in a row, most likely used North Korean ballistic missiles."
South Korea, Ukraine and the United States have accused North Korea of supplying artillery and missiles to Russia, which both states have denied.
Meanwhile, North Korea condemned Ukraine's incursion into Russia and said it would always stand with Russia, state media reported.
The dictatorship blamed the US for the attack, adding it was pushing the situation to the brink of World War Three, KCNA news agency said.
"We strongly condemn the armed attack against the Russian territory by the Zelenskyy puppet regime under the control and support of the United States and the West as an unforgivable act of aggression and terror," North Korea's foreign ministry said.
North Korea has dramatically upgraded its ties with Russia in the past year with two summit meetings by their leaders who pledged closer cooperation in all areas.
In June, North Korean leader Kim Jong Un and Russian President Vladimir Putin signed a pact in Pyongyang on "comprehensive strategic partnership" that included a mutual defence agreement.
The Ukrainian air force says it has attacked a second bridge in Russia's Kursk region.
Footage posted on a commander's Telegram channel shows an attack on a bridge in Zvannoe, Kursk over the Seym river.
This is the same river over which another bridge was destroyed earlier this week.
Ukraine's destruction of infrastructure in the area is believed to be an attempt to hamper Russian supply lines or reinforcements.
Air force commander Lieutenant General Mykola Oleshchuk wrote: "Minus one more bridge! The aviation of the air force continues to deprive the enemy of its logistical capabilities with accurate air strikes, which significantly affects the course of hostilities."
Ukraine's offensive in Kursk has generated frontline-wide pressures on Russian forces, according to the Institute for the Study of War.
Vladimir Putin is almost certain to attempt to retake the Russian territory, which will require more manpower and equipment from elsewhere in the theatre, the US-based think tank said.
Long-term, Putin will be forced to make a decision about committing more resource Russia's long international border with Ukraine, imposing "constraints" on theatre-wide planning that "Russia previously did not face".
"The Ukrainian incursion in Kursk Oblast and the heightened Russian priority of maintaining the tempo of offensive operations in Donetsk Oblast will likely place greater strain on Russia's remaining operational reserves and likely begin to impact Russia's ability to sustain consistent offensive operations throughout the theatre," the ISW said.
"Further Russian redeployments to Kursk Oblast would also further weaken Russia's ability to sustain offensive operations in northeastern and eastern Ukraine."
The Russian military has already redeployed 11 battalions from within Kursk Oblast and four Russian force groupings from elsewhere.
This may be at odds with Putin's strategy of grinding attrition and indefinite, incremental territorial gains, but "persisting Ukrainian occupation of Russian territory would be a strategic blow to Putin's decades-long effort to cement a legacy of Russian stability, security, and geopolitical resurgence".
Russia has launched its third ballistic missile attack on Kyiv this month.
A witness heard blasts that sounded like air defence systems early this morning, before fresh air raid alerts sounded over the threat of more missiles heading towards the city.
Preliminary data showed all missiles were destroyed on their approach to the city, the military administration of the Ukrainian capital said.
"This is already the third ballistic strike on the capital in August, with exact intervals of six days between each attack," said Serhiy Popko, the head of the Kyiv military administration.
He added that Ukraine's air defence units also destroyed a number of drones launched by Russia.
There were no immediate reports of casualties or damage.
Ukraine's air force chief said its forces destroyed eight Russian attack drones and five out of eight missiles launched overnight towards the Kyiv, Sumy and Poltava regions.
A Ukrainian drone attack has caused a fire at a Russian oil reservoir, according to reports.
More than 70 firefighters rushed to tackle the blaze that covered 5,000 square metres in the Azov district of the Rostov-on-Don region, according to the Russian emergencies ministry.
Baza, a Telegram channel close to Russian law enforcement, said an oil depot was damaged in Rostov, while Russia's SHOT channel posted a video showing dark smoke rising from what it said was an oil depot.
Regional governor Vasily Golubev said debris from a destroyed Ukrainian drone sparked a diesel fuel fire at an "industrial warehouse".
Russia's air defence units destroyed five drones that Ukraine launched overnight targeting the Kursk, Belgorod and Rostov regions, Russia's defence ministry said.
Russia rarely admits direct hits by Ukrainian drones.
Welcome back to our live coverage of the war, as we continue to track Ukraine's surprise incursion into the Kursk region of Russia.
Kyiv has been calling for permission to use more Western weapons in Russia, as it seeks to improve Ukraine's future negotiating position and threaten the stability of Vladimir Putin's.
We'll be bringing you live updates and analysis throughout the day, but before we begin, here is a recap of the key developments over the last 24 hours.
Bridge attack: Russia's foreign ministry claimed Ukraine used Western rockets to destroy a bridge over the Seym river in the Kursk region.
Kursk: Volodymyr Zelenskyy heralded the achievements of his forces in Kursk, encouraging them to inflict "maximum damage on all Russian positions".
Ukraine's offensive in the region showed that escalating attacks against Russia was "nothing to be afraid of", a former foreign policy adviser to Mr Zelenskyy said.
Meanwhile, military analyst Sean Bell forecast that Vladimir Putin will not accept any negotiations involving the occupied Kursk territory, despite Ukrainian ambitions, and will instead deal with it "ruthlessly".
Western weapons: Washington appeared to be effectively blocking the UK from permitting Kyiv to fire Storm Shadow missiles inside Russia. The UK has been waiting for US approval for more than a month, a government source told The Times.
'Insane' propaganda: Kyiv dismissed "insane Russian propaganda" alleging Ukraine planned to carry out nuclear attacks. Moscow had accused Ukraine - without providing any evidence - of gearing up to attack the Kursk nuclear power plant and developing a "dirty bomb"; an explosive used to scatter radioactive waste.
Threat to nuclear safety: Safety at Ukraine's occupied Zaporizhzhia Nuclear Power Plant was deteriorating after a drone strike on a nearby road, the International Atomic Energy Agency said.
Ukrainian President Volodymyr Zelenskyy has praised the UK's "true leadership" in its support of Ukraine - but warned "the situation has slowed down recently" as it pushes into Russian territory.
In his nightly video address, he stressed it is "crucial that our partners remove barriers that hinder us from weakening Russian positions in the way this war demands".
He promised to "intensify our diplomatic efforts" amid the Kursk incursion, naming the UK, US, and France as key targets.
It comes amid speculation Germany is planning to halve its Ukrainian aid budget next year.
Mr Zelenskyy finished his X post by saying: "Throughout this war, we've seen the UK demonstrate true leadership—in arms, politics, and support for Ukrainian society.
"This has saved thousands of lives, reflecting the strength of the UK."
But he added: "Unfortunately, the situation has slowed down recently.
"We will discuss how to fix this because long-range capabilities are vital for us. The whole world sees how effective Ukrainians are—how our entire nation defends its independence."
In a Sunday Express interview, Defence Secretary John Healey endorsed Ukraine using British weapons inside Russia - as long as it keeps within international law.
Be the first to get Breaking News
Install the Sky News app for free


COMMENTS
Here are tips for writing a "why I'm deserving scholarship" essay: Explain how the scholarship money would contribute to your long-term goals. You're asking the scholarship committee to invest in your future. They want to ensure their investment goes to a worthy cause. Explain how your education will play a role in your career and ...
The essay is your chance to show how you are the ideal representative. Submit an essay that is neat and readable. Make sure your essay is neatly typed, and that there is a lot of 'white space' on the page. Double-space the essay, and provide adequate margins (1″-1 1/2″) on all sides. Make sure your essay is well written.
ESSAY. Exposure to the medical career from an early age by my father, who would explain diseases of the human body, sparked my interest for Medicine and drove me to seek out work experience. I ...
Scholarship Essay Example #1. Kang Foundation Scholarship ($1000), Kingdom Dreamer Scholarship Fund Scholarship through Sarang Church ($2000), and the national contest from the Lamber Goodnow legal team ($1000) by Peter Kang. Prompt: Open topic.
I always thank the reader for their time and consideration, restate the fundraising goal, and include a final, heartfelt appeal for support. This reinforces your message and leaves the reader with a clear call to action. Learn from a parent's personal experience on writing an effective fundraising letter for medical expenses.
Yes, but make sure your essay directly addresses the prompt, respects the word count, and demonstrates the organization's values. If you plan ahead, you can save time by writing one scholarship essay for multiple prompts with similar questions. In a scholarship tracker spreadsheet, you can group or color-code overlapping essay prompts; then, write a single essay for multiple scholarships.
Why This Scholarship Essay Example Worked: 3. Life Happens Scholarship by Emily Trader. Why This Scholarship Essay Example Worked: 4. Going Merry Scholarship Success Story by Jesus Adrian Arroyo-Ramirez. Why This Scholarship Essay Example Worked: 5. Why College Is Important to Me by Nicole Kuznetsov.
Following is a sample fundraising letter to be used for raising funds for medical expenses. You can use this appeal for direct or email requests, but also for any of the online fundraising sites. (See most popular fundraising sites and services here .) Feel free to copy, modify and paste as needed. For any other use please contact us.
Rachel Rudeen, former admissions coordinator for the University of Minnesota Medical School, says personal statements help medical schools determine whether applicants have the character necessary ...
Structuring Your Essay. Your essay should follow a standard format that includes a clear beginning, middle, and end. Typically, you should: · Establish your main idea in the introduction. · Include a separate body paragraph for each key point that supports your main idea. · Draw it all together and revisit your main idea in the conclusion.
4. Tell us about a time you failed and what you learned from it. Scholarship providers understand that no student is perfect, and they want to know how you learned from a failure - this can be an academic, professional, or personal failure. Break down how you failed, why you failed, and how it made you better.
In recent years, crowdfunding for medical expenses has gained popularity, especially in countries without universal health coverage. Nevertheless, universal coverage does not imply covering all medical costs for everyone. In countries with universal coverage unmet health care needs typically emerge due to financial reasons: the inability to pay the patient co-payments, and additional and ...
Part 1: Introduction to the medical school personal statement. You probably know someone who achieved a solid GPA and MCAT score, conducted research, shadowed physicians, engaged in meaningful volunteer work, and met all the other medical school requirements, yet still got rejected by every school they applied to.. You may have even heard of someone who was rejected by over 30 medical schools ...
Such is often the case when someone is facing huge medical expenses. You can write a successful fund-raising letter-and watch those donations come streaming in-if you can write a compelling narrative explaining the person's predicament and be sure to welcome donations of any monetary value. Acknowledge that "times are tough" for many ...
perspective is critical, and now aspire to explore medical entrepreneurship as a doctor who bridges clinical, technical, and commercial viewpoints. I want to push the frontier of patient care by developing technological innovations and ensuring that they are effectively delivered to patients. I grew up repairing items and relationships at home.
The Paget's Association. The Paget's Association awards Student Research Bursaries of up to £6,000 to promising UK medical or science students (MRes, MSc, BSc or equivalent higher degree) to pursue research into any aspects of Paget's Disease of Bone. Tel: 0161 799 4646. Website.
The 4 categories of successful factors that are actors in medical crowdfunding interact with each other [ 7, 49, 50 ]. First, raisers register in the platforms to initiate campaigns to raise money for medical expenses with illness narratives, which include fundraising goals, fundraising time, and fundraising events.
It is indisputably important for researchers to develop new medical treatments in the battle against poor health and disease. 2. In my opinion, this research should be funded primarily by governments and well-regulated private companies. Paraphrase the overall topic for the essay. Write your opinion - directly answer the question. 1.
Write a clear topic sentence with your main idea at the end of it. Explain/develop the idea. Make your support as specific and clear as possible. State the results and the reasons to support your original main idea. 1. Despite the force of the above argument, I believe health is a more tangible and pressing concern. 2.
Ambulance car-based GAZelle is the most common type of ambulance in Russia. Healthcare in Russia is provided by the state through the Federal Compulsory Medical Insurance Fund, and regulated through the Ministry of Health. [1] The Constitution of the Russian Federation has provided all citizens the right to free healthcare since 1993. In 2008, 621,000 doctors and 1.3 million nurses were ...
In the last two decades, health care systems in the European Union countries have faced global challenges, including aging populations, a substantial rise in chronic and multiple diseases, the emergence of new medical and information technologies, and a growing citizen awareness of the role of a healthy lifestyle in disease prevention [].The responses of health systems to these challenges ...
Financing of medical care was carried out exclusively at the expense of state budget funds. This model of healthcare financing existed until 1989 [ 14 ]. It is fair to say that "free" health care in the USSR (like other social funds) was provided by direct underpayments for labor and deductions from wages in the form of taxes.
The Joseph Brodsky Papers document the life and work of Russian-born poet, essayist and Nobel Laureate Joseph Brodsky. The papers consist of correspondence, writings, personal papers (including legal, medical and financial records), audiovisual material, teaching material, student papers, newspaper clippings and printed ephemera, spanning the years 1890-2004, with the bulk of the material ...
In 2019, two junior doctors were physically assaulted in Kolkata's Nil Ratan Sircar Medical College and Hospital (NRSMCH) by a mob of people after a 75-year-old patient passed away in the hospital.
Read the full email from Shawnee Mission Northwest High School below: August 16, 2024. Dear Shawnee Mission Northwest Staff and Families, I am writing to share some difficult news with you.
(Medical Insurance). • You can join a separate Medicare drug plan to get Medicare drug coverage (Part D). • You can use any doctor or hospital that takes Medicare, anywhere in the U.S. • To help pay your out-of-pocket costs in Original Medicare (like your 20% coinsurance), you can also shop for and buy supplemental coverage. Part A
APPLETON- As longtime WAPL-FM morning show co-host Rick McNeal continues to recover from medical issues amid new challenges, a GoFundMe has been established to help get him back on his feet. ...
There was a wrinkle, though. The National Institutes of Health had funded the research on his WI-38 cell line but declined to fund its distribution, even as other researchers clamored for samples. Dr.
A teenage boy died Tuesday at a United Dairy Farmers store in a road rage shooting on the city's Southwest Side, according to Columbus police. Police received a report at 8:11 p.m. of a shooting ...
Ukraine's foreign ministry describes "Russian propaganda" that its forces are planning to use dirty bombs or attack nuclear power plants in the Kursk region are "crazy". Russia's defence ministry ...