Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals

You are here
- Volume 76, Issue 2
- COVID-19 pandemic and its impact on social relationships and health
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-1512-4471 Emily Long 1 ,
- Susan Patterson 1 ,
- Karen Maxwell 1 ,
- Carolyn Blake 1 ,
- http://orcid.org/0000-0001-7342-4566 Raquel Bosó Pérez 1 ,
- Ruth Lewis 1 ,
- Mark McCann 1 ,
- Julie Riddell 1 ,
- Kathryn Skivington 1 ,
- Rachel Wilson-Lowe 1 ,
- http://orcid.org/0000-0002-4409-6601 Kirstin R Mitchell 2
- 1 MRC/CSO Social and Public Health Sciences Unit , University of Glasgow , Glasgow , UK
- 2 MRC/CSO Social and Public Health Sciences Unit, Institute of Health & Wellbeing , University of Glasgow , Glasgow , UK
- Correspondence to Dr Emily Long, MRC/CSO Social and Public Health Sciences Unit, University of Glasgow, Glasgow G3 7HR, UK; emily.long{at}glasgow.ac.uk
This essay examines key aspects of social relationships that were disrupted by the COVID-19 pandemic. It focuses explicitly on relational mechanisms of health and brings together theory and emerging evidence on the effects of the COVID-19 pandemic to make recommendations for future public health policy and recovery. We first provide an overview of the pandemic in the UK context, outlining the nature of the public health response. We then introduce four distinct domains of social relationships: social networks, social support, social interaction and intimacy, highlighting the mechanisms through which the pandemic and associated public health response drastically altered social interactions in each domain. Throughout the essay, the lens of health inequalities, and perspective of relationships as interconnecting elements in a broader system, is used to explore the varying impact of these disruptions. The essay concludes by providing recommendations for longer term recovery ensuring that the social relational cost of COVID-19 is adequately considered in efforts to rebuild.
- inequalities
Data availability statement
Data sharing not applicable as no data sets generated and/or analysed for this study. Data sharing not applicable as no data sets generated or analysed for this essay.
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/jech-2021-216690
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Infectious disease pandemics, including SARS and COVID-19, demand intrapersonal behaviour change and present highly complex challenges for public health. 1 A pandemic of an airborne infection, spread easily through social contact, assails human relationships by drastically altering the ways through which humans interact. In this essay, we draw on theories of social relationships to examine specific ways in which relational mechanisms key to health and well-being were disrupted by the COVID-19 pandemic. Relational mechanisms refer to the processes between people that lead to change in health outcomes.
At the time of writing, the future surrounding COVID-19 was uncertain. Vaccine programmes were being rolled out in countries that could afford them, but new and more contagious variants of the virus were also being discovered. The recovery journey looked long, with continued disruption to social relationships. The social cost of COVID-19 was only just beginning to emerge, but the mental health impact was already considerable, 2 3 and the inequality of the health burden stark. 4 Knowledge of the epidemiology of COVID-19 accrued rapidly, but evidence of the most effective policy responses remained uncertain.
The initial response to COVID-19 in the UK was reactive and aimed at reducing mortality, with little time to consider the social implications, including for interpersonal and community relationships. The terminology of ‘social distancing’ quickly became entrenched both in public and policy discourse. This equation of physical distance with social distance was regrettable, since only physical proximity causes viral transmission, whereas many forms of social proximity (eg, conversations while walking outdoors) are minimal risk, and are crucial to maintaining relationships supportive of health and well-being.
The aim of this essay is to explore four key relational mechanisms that were impacted by the pandemic and associated restrictions: social networks, social support, social interaction and intimacy. We use relational theories and emerging research on the effects of the COVID-19 pandemic response to make three key recommendations: one regarding public health responses; and two regarding social recovery. Our understanding of these mechanisms stems from a ‘systems’ perspective which casts social relationships as interdependent elements within a connected whole. 5
Social networks
Social networks characterise the individuals and social connections that compose a system (such as a workplace, community or society). Social relationships range from spouses and partners, to coworkers, friends and acquaintances. They vary across many dimensions, including, for example, frequency of contact and emotional closeness. Social networks can be understood both in terms of the individuals and relationships that compose the network, as well as the overall network structure (eg, how many of your friends know each other).
Social networks show a tendency towards homophily, or a phenomenon of associating with individuals who are similar to self. 6 This is particularly true for ‘core’ network ties (eg, close friends), while more distant, sometimes called ‘weak’ ties tend to show more diversity. During the height of COVID-19 restrictions, face-to-face interactions were often reduced to core network members, such as partners, family members or, potentially, live-in roommates; some ‘weak’ ties were lost, and interactions became more limited to those closest. Given that peripheral, weaker social ties provide a diversity of resources, opinions and support, 7 COVID-19 likely resulted in networks that were smaller and more homogenous.
Such changes were not inevitable nor necessarily enduring, since social networks are also adaptive and responsive to change, in that a disruption to usual ways of interacting can be replaced by new ways of engaging (eg, Zoom). Yet, important inequalities exist, wherein networks and individual relationships within networks are not equally able to adapt to such changes. For example, individuals with a large number of newly established relationships (eg, university students) may have struggled to transfer these relationships online, resulting in lost contacts and a heightened risk of social isolation. This is consistent with research suggesting that young adults were the most likely to report a worsening of relationships during COVID-19, whereas older adults were the least likely to report a change. 8
Lastly, social connections give rise to emergent properties of social systems, 9 where a community-level phenomenon develops that cannot be attributed to any one member or portion of the network. For example, local area-based networks emerged due to geographic restrictions (eg, stay-at-home orders), resulting in increases in neighbourly support and local volunteering. 10 In fact, research suggests that relationships with neighbours displayed the largest net gain in ratings of relationship quality compared with a range of relationship types (eg, partner, colleague, friend). 8 Much of this was built from spontaneous individual interactions within local communities, which together contributed to the ‘community spirit’ that many experienced. 11 COVID-19 restrictions thus impacted the personal social networks and the structure of the larger networks within the society.
Social support
Social support, referring to the psychological and material resources provided through social interaction, is a critical mechanism through which social relationships benefit health. In fact, social support has been shown to be one of the most important resilience factors in the aftermath of stressful events. 12 In the context of COVID-19, the usual ways in which individuals interact and obtain social support have been severely disrupted.
One such disruption has been to opportunities for spontaneous social interactions. For example, conversations with colleagues in a break room offer an opportunity for socialising beyond one’s core social network, and these peripheral conversations can provide a form of social support. 13 14 A chance conversation may lead to advice helpful to coping with situations or seeking formal help. Thus, the absence of these spontaneous interactions may mean the reduction of indirect support-seeking opportunities. While direct support-seeking behaviour is more effective at eliciting support, it also requires significantly more effort and may be perceived as forceful and burdensome. 15 The shift to homeworking and closure of community venues reduced the number of opportunities for these spontaneous interactions to occur, and has, second, focused them locally. Consequently, individuals whose core networks are located elsewhere, or who live in communities where spontaneous interaction is less likely, have less opportunity to benefit from spontaneous in-person supportive interactions.
However, alongside this disruption, new opportunities to interact and obtain social support have arisen. The surge in community social support during the initial lockdown mirrored that often seen in response to adverse events (eg, natural disasters 16 ). COVID-19 restrictions that confined individuals to their local area also compelled them to focus their in-person efforts locally. Commentators on the initial lockdown in the UK remarked on extraordinary acts of generosity between individuals who belonged to the same community but were unknown to each other. However, research on adverse events also tells us that such community support is not necessarily maintained in the longer term. 16
Meanwhile, online forms of social support are not bound by geography, thus enabling interactions and social support to be received from a wider network of people. Formal online social support spaces (eg, support groups) existed well before COVID-19, but have vastly increased since. While online interactions can increase perceived social support, it is unclear whether remote communication technologies provide an effective substitute from in-person interaction during periods of social distancing. 17 18 It makes intuitive sense that the usefulness of online social support will vary by the type of support offered, degree of social interaction and ‘online communication skills’ of those taking part. Youth workers, for instance, have struggled to keep vulnerable youth engaged in online youth clubs, 19 despite others finding a positive association between amount of digital technology used by individuals during lockdown and perceived social support. 20 Other research has found that more frequent face-to-face contact and phone/video contact both related to lower levels of depression during the time period of March to August 2020, but the negative effect of a lack of contact was greater for those with higher levels of usual sociability. 21 Relatedly, important inequalities in social support exist, such that individuals who occupy more socially disadvantaged positions in society (eg, low socioeconomic status, older people) tend to have less access to social support, 22 potentially exacerbated by COVID-19.
Social and interactional norms
Interactional norms are key relational mechanisms which build trust, belonging and identity within and across groups in a system. Individuals in groups and societies apply meaning by ‘approving, arranging and redefining’ symbols of interaction. 23 A handshake, for instance, is a powerful symbol of trust and equality. Depending on context, not shaking hands may symbolise a failure to extend friendship, or a failure to reach agreement. The norms governing these symbols represent shared values and identity; and mutual understanding of these symbols enables individuals to achieve orderly interactions, establish supportive relationship accountability and connect socially. 24 25
Physical distancing measures to contain the spread of COVID-19 radically altered these norms of interaction, particularly those used to convey trust, affinity, empathy and respect (eg, hugging, physical comforting). 26 As epidemic waves rose and fell, the work to negotiate these norms required intense cognitive effort; previously taken-for-granted interactions were re-examined, factoring in current restriction levels, own and (assumed) others’ vulnerability and tolerance of risk. This created awkwardness, and uncertainty, for example, around how to bring closure to an in-person interaction or convey warmth. The instability in scripted ways of interacting created particular strain for individuals who already struggled to encode and decode interactions with others (eg, those who are deaf or have autism spectrum disorder); difficulties often intensified by mask wearing. 27
Large social gatherings—for example, weddings, school assemblies, sporting events—also present key opportunities for affirming and assimilating interactional norms, building cohesion and shared identity and facilitating cooperation across social groups. 28 Online ‘equivalents’ do not easily support ‘social-bonding’ activities such as singing and dancing, and rarely enable chance/spontaneous one-on-one conversations with peripheral/weaker network ties (see the Social networks section) which can help strengthen bonds across a larger network. The loss of large gatherings to celebrate rites of passage (eg, bar mitzvah, weddings) has additional relational costs since these events are performed by and for communities to reinforce belonging, and to assist in transitioning to new phases of life. 29 The loss of interaction with diverse others via community and large group gatherings also reduces intergroup contact, which may then tend towards more prejudiced outgroup attitudes. While online interaction can go some way to mimicking these interaction norms, there are key differences. A sense of anonymity, and lack of in-person emotional cues, tends to support norms of polarisation and aggression in expressing differences of opinion online. And while online platforms have potential to provide intergroup contact, the tendency of much social media to form homogeneous ‘echo chambers’ can serve to further reduce intergroup contact. 30 31
Intimacy relates to the feeling of emotional connection and closeness with other human beings. Emotional connection, through romantic, friendship or familial relationships, fulfils a basic human need 32 and strongly benefits health, including reduced stress levels, improved mental health, lowered blood pressure and reduced risk of heart disease. 32 33 Intimacy can be fostered through familiarity, feeling understood and feeling accepted by close others. 34
Intimacy via companionship and closeness is fundamental to mental well-being. Positively, the COVID-19 pandemic has offered opportunities for individuals to (re)connect and (re)strengthen close relationships within their household via quality time together, following closure of many usual external social activities. Research suggests that the first full UK lockdown period led to a net gain in the quality of steady relationships at a population level, 35 but amplified existing inequalities in relationship quality. 35 36 For some in single-person households, the absence of a companion became more conspicuous, leading to feelings of loneliness and lower mental well-being. 37 38 Additional pandemic-related relational strain 39 40 resulted, for some, in the initiation or intensification of domestic abuse. 41 42
Physical touch is another key aspect of intimacy, a fundamental human need crucial in maintaining and developing intimacy within close relationships. 34 Restrictions on social interactions severely restricted the number and range of people with whom physical affection was possible. The reduction in opportunity to give and receive affectionate physical touch was not experienced equally. Many of those living alone found themselves completely without physical contact for extended periods. The deprivation of physical touch is evidenced to take a heavy emotional toll. 43 Even in future, once physical expressions of affection can resume, new levels of anxiety over germs may introduce hesitancy into previously fluent blending of physical and verbal intimate social connections. 44
The pandemic also led to shifts in practices and norms around sexual relationship building and maintenance, as individuals adapted and sought alternative ways of enacting sexual intimacy. This too is important, given that intimate sexual activity has known benefits for health. 45 46 Given that social restrictions hinged on reducing household mixing, possibilities for partnered sexual activity were primarily guided by living arrangements. While those in cohabiting relationships could potentially continue as before, those who were single or in non-cohabiting relationships generally had restricted opportunities to maintain their sexual relationships. Pornography consumption and digital partners were reported to increase since lockdown. 47 However, online interactions are qualitatively different from in-person interactions and do not provide the same opportunities for physical intimacy.
Recommendations and conclusions
In the sections above we have outlined the ways in which COVID-19 has impacted social relationships, showing how relational mechanisms key to health have been undermined. While some of the damage might well self-repair after the pandemic, there are opportunities inherent in deliberative efforts to build back in ways that facilitate greater resilience in social and community relationships. We conclude by making three recommendations: one regarding public health responses to the pandemic; and two regarding social recovery.
Recommendation 1: explicitly count the relational cost of public health policies to control the pandemic
Effective handling of a pandemic recognises that social, economic and health concerns are intricately interwoven. It is clear that future research and policy attention must focus on the social consequences. As described above, policies which restrict physical mixing across households carry heavy and unequal relational costs. These include for individuals (eg, loss of intimate touch), dyads (eg, loss of warmth, comfort), networks (eg, restricted access to support) and communities (eg, loss of cohesion and identity). Such costs—and their unequal impact—should not be ignored in short-term efforts to control an epidemic. Some public health responses—restrictions on international holiday travel and highly efficient test and trace systems—have relatively small relational costs and should be prioritised. At a national level, an earlier move to proportionate restrictions, and investment in effective test and trace systems, may help prevent escalation of spread to the point where a national lockdown or tight restrictions became an inevitability. Where policies with relational costs are unavoidable, close attention should be paid to the unequal relational impact for those whose personal circumstances differ from normative assumptions of two adult families. This includes consideration of whether expectations are fair (eg, for those who live alone), whether restrictions on social events are equitable across age group, religious/ethnic groupings and social class, and also to ensure that the language promoted by such policies (eg, households; families) is not exclusionary. 48 49 Forethought to unequal impacts on social relationships should thus be integral to the work of epidemic preparedness teams.
Recommendation 2: intelligently balance online and offline ways of relating
A key ingredient for well-being is ‘getting together’ in a physical sense. This is fundamental to a human need for intimate touch, physical comfort, reinforcing interactional norms and providing practical support. Emerging evidence suggests that online ways of relating cannot simply replace physical interactions. But online interaction has many benefits and for some it offers connections that did not exist previously. In particular, online platforms provide new forms of support for those unable to access offline services because of mobility issues (eg, older people) or because they are geographically isolated from their support community (eg, lesbian, gay, bisexual, transgender and queer (LGBTQ) youth). Ultimately, multiple forms of online and offline social interactions are required to meet the needs of varying groups of people (eg, LGBTQ, older people). Future research and practice should aim to establish ways of using offline and online support in complementary and even synergistic ways, rather than veering between them as social restrictions expand and contract. Intelligent balancing of online and offline ways of relating also pertains to future policies on home and flexible working. A decision to switch to wholesale or obligatory homeworking should consider the risk to relational ‘group properties’ of the workplace community and their impact on employees’ well-being, focusing in particular on unequal impacts (eg, new vs established employees). Intelligent blending of online and in-person working is required to achieve flexibility while also nurturing supportive networks at work. Intelligent balance also implies strategies to build digital literacy and minimise digital exclusion, as well as coproducing solutions with intended beneficiaries.
Recommendation 3: build stronger and sustainable localised communities
In balancing offline and online ways of interacting, there is opportunity to capitalise on the potential for more localised, coherent communities due to scaled-down travel, homeworking and local focus that will ideally continue after restrictions end. There are potential economic benefits after the pandemic, such as increased trade as home workers use local resources (eg, coffee shops), but also relational benefits from stronger relationships around the orbit of the home and neighbourhood. Experience from previous crises shows that community volunteer efforts generated early on will wane over time in the absence of deliberate work to maintain them. Adequately funded partnerships between local government, third sector and community groups are required to sustain community assets that began as a direct response to the pandemic. Such partnerships could work to secure green spaces and indoor (non-commercial) meeting spaces that promote community interaction. Green spaces in particular provide a triple benefit in encouraging physical activity and mental health, as well as facilitating social bonding. 50 In building local communities, small community networks—that allow for diversity and break down ingroup/outgroup views—may be more helpful than the concept of ‘support bubbles’, which are exclusionary and less sustainable in the longer term. Rigorously designed intervention and evaluation—taking a systems approach—will be crucial in ensuring scale-up and sustainability.
The dramatic change to social interaction necessitated by efforts to control the spread of COVID-19 created stark challenges but also opportunities. Our essay highlights opportunities for learning, both to ensure the equity and humanity of physical restrictions, and to sustain the salutogenic effects of social relationships going forward. The starting point for capitalising on this learning is recognition of the disruption to relational mechanisms as a key part of the socioeconomic and health impact of the pandemic. In recovery planning, a general rule is that what is good for decreasing health inequalities (such as expanding social protection and public services and pursuing green inclusive growth strategies) 4 will also benefit relationships and safeguard relational mechanisms for future generations. Putting this into action will require political will.
Ethics statements
Patient consent for publication.
Not required.
- Office for National Statistics (ONS)
- Ford T , et al
- Riordan R ,
- Ford J , et al
- Glonti K , et al
- McPherson JM ,
- Smith-Lovin L
- Granovetter MS
- Fancourt D et al
- Stadtfeld C
- Office for Civil Society
- Cook J et al
- Rodriguez-Llanes JM ,
- Guha-Sapir D
- Patulny R et al
- Granovetter M
- Winkeler M ,
- Filipp S-H ,
- Kaniasty K ,
- de Terte I ,
- Guilaran J , et al
- Wright KB ,
- Martin J et al
- Gabbiadini A ,
- Baldissarri C ,
- Durante F , et al
- Sommerlad A ,
- Marston L ,
- Huntley J , et al
- Turner RJ ,
- Bicchieri C
- Brennan G et al
- Watson-Jones RE ,
- Amichai-Hamburger Y ,
- McKenna KYA
- Page-Gould E ,
- Aron A , et al
- Pietromonaco PR ,
- Timmerman GM
- Bradbury-Jones C ,
- Mikocka-Walus A ,
- Klas A , et al
- Marshall L ,
- Steptoe A ,
- Stanley SM ,
- Campbell AM
- ↵ (ONS), O.f.N.S., Domestic abuse during the coronavirus (COVID-19) pandemic, England and Wales . Available: https://www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/articles/domesticabuseduringthecoronaviruscovid19pandemicenglandandwales/november2020
- Rosenberg M ,
- Hensel D , et al
- Banerjee D ,
- Bruner DW , et al
- Bavel JJV ,
- Baicker K ,
- Boggio PS , et al
- van Barneveld K ,
- Quinlan M ,
- Kriesler P , et al
- Mitchell R ,
- de Vries S , et al
Twitter @karenmaxSPHSU, @Mark_McCann, @Rwilsonlowe, @KMitchinGlasgow
Contributors EL and KM led on the manuscript conceptualisation, review and editing. SP, KM, CB, RBP, RL, MM, JR, KS and RW-L contributed to drafting and revising the article. All authors assisted in revising the final draft.
Funding The research reported in this publication was supported by the Medical Research Council (MC_UU_00022/1, MC_UU_00022/3) and the Chief Scientist Office (SPHSU11, SPHSU14). EL is also supported by MRC Skills Development Fellowship Award (MR/S015078/1). KS and MM are also supported by a Medical Research Council Strategic Award (MC_PC_13027).
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
/media/video/upload/Opener_rt.mp4)
How Science Beat the Virus
And what it lost in the process

Listen to more stories on audm
This article was published online on December 14, 2020.
In fall of 2019, exactly zero scientists were studying COVID‑19, because no one knew the disease existed. The coronavirus that causes it, SARS‑CoV‑2, had only recently jumped into humans and had been neither identified nor named. But by the end of March 2020, it had spread to more than 170 countries, sickened more than 750,000 people, and triggered the biggest pivot in the history of modern science. Thousands of researchers dropped whatever intellectual puzzles had previously consumed their curiosity and began working on the pandemic instead. In mere months, science became thoroughly COVID-ized.
As of this writing, the biomedical library PubMed lists more than 74,000 COVID-related scientific papers—more than twice as many as there are about polio, measles, cholera, dengue, or other diseases that have plagued humanity for centuries. Only 9,700 Ebola-related papers have been published since its discovery in 1976; last year, at least one journal received more COVID‑19 papers than that for consideration. By September, the prestigious New England Journal of Medicine had received 30,000 submissions—16,000 more than in all of 2019. “All that difference is COVID‑19,” Eric Rubin, NEJM ’s editor in chief, says. Francis Collins, the director of the National Institutes of Health, told me, “The way this has resulted in a shift in scientific priorities has been unprecedented.”
Much like famous initiatives such as the Manhattan Project and the Apollo program, epidemics focus the energies of large groups of scientists. In the U.S., the influenza pandemic of 1918, the threat of malaria in the tropical battlegrounds of World War II, and the rise of polio in the postwar years all triggered large pivots. Recent epidemics of Ebola and Zika each prompted a temporary burst of funding and publications . But “nothing in history was even close to the level of pivoting that’s happening right now,” Madhukar Pai of McGill University told me.
That’s partly because there are just more scientists: From 1960 to 2010, the number of biological or medical researchers in the U.S. increased sevenfold , from just 30,000 to more than 220,000. But SARS-CoV-2 has also spread farther and faster than any new virus in a century. For Western scientists, it wasn’t a faraway threat like Ebola. It threatened to inflame their lungs. It shut down their labs. “It hit us at home,” Pai said.
In a survey of 2,500 researchers in the U.S., Canada, and Europe, Kyle Myers from Harvard and his team found that 32 percent had shifted their focus toward the pandemic. Neuroscientists who study the sense of smell started investigating why COVID‑19 patients tend to lose theirs. Physicists who had previously experienced infectious diseases only by contracting them found themselves creating models to inform policy makers. Michael D. L. Johnson at the University of Arizona normally studies copper’s toxic effects on bacteria. But when he learned that SARS‑CoV‑2 persists for less time on copper surfaces than on other materials, he partially pivoted to see how the virus might be vulnerable to the metal. No other disease has been scrutinized so intensely, by so much combined intellect, in so brief a time.
These efforts have already paid off. New diagnostic tests can detect the virus within minutes. Massive open data sets of viral genomes and COVID‑19 cases have produced the most detailed picture yet of a new disease’s evolution. Vaccines are being developed with record-breaking speed. SARS‑CoV‑2 will be one of the most thoroughly characterized of all pathogens, and the secrets it yields will deepen our understanding of other viruses, leaving the world better prepared to face the next pandemic.
But the COVID‑19 pivot has also revealed the all-too-human frailties of the scientific enterprise . Flawed research made the pandemic more confusing, influencing misguided policies. Clinicians wasted millions of dollars on trials that were so sloppy as to be pointless. Overconfident poseurs published misleading work on topics in which they had no expertise. Racial and gender inequalities in the scientific field widened.
Amid a long winter of sickness , it’s hard not to focus on the political failures that led us to a third surge. But when people look back on this period, decades from now, they will also tell stories, both good and bad, about this extraordinary moment for science. At its best, science is a self-correcting march toward greater knowledge for the betterment of humanity. At its worst, it is a self-interested pursuit of greater prestige at the cost of truth and rigor. The pandemic brought both aspects to the fore. Humanity will benefit from the products of the COVID‑19 pivot. Science itself will too, if it learns from the experience.
In February, Jennifer Doudna, one of America’s most prominent scientists, was still focused on CRISPR—the gene-editing tool that she’d co-discovered and that won her a Nobel Prize in October. But when her son’s high school shut down and UC Berkeley, her university, closed its campus, the severity of the impending pandemic became clear. “In three weeks, I went from thinking we’re still okay to thinking that my whole life is going to change,” she told me. On March 13, she and dozens of colleagues at the Innovative Genomics Institute, which she leads, agreed to pause most of their ongoing projects and redirect their skills to addressing COVID‑19. They worked on CRISPR-based diagnostic tests. Because existing tests were in short supply, they converted lab space into a pop-up testing facility to serve the local community. “We need to make our expertise relevant to whatever is happening right now,” she said.
Scientists who’d already been studying other emerging diseases were even quicker off the mark. Lauren Gardner, an engineering professor at Johns Hopkins University who has studied dengue and Zika, knew that new epidemics are accompanied by a dearth of real-time data. So she and one of her students created an online global dashboard to map and tally all publicly reported COVID‑19 cases and deaths. After one night of work, they released it, on January 22. The dashboard has since been accessed daily by governments, public-health agencies, news organizations, and anxious citizens.
Studying deadly viruses is challenging at the best of times, and was especially so this past year. To handle SARS‑CoV‑2, scientists must work in “biosafety level 3” labs, fitted with special airflow systems and other extreme measures; although the actual number is not known, an estimated 200 such facilities exist in the U.S. Researchers often test new drugs and vaccines on monkeys before proceeding to human trials, but the U.S. is facing a monkey shortage after China stopped exporting the animals, possibly because it needed them for research. And other biomedical research is now more difficult because of physical-distancing requirements. “Usually we had people packed in, but with COVID, we do shift work,” Akiko Iwasaki, a Yale immunologist, told me. “People are coming in at ridiculous hours” to protect themselves from the very virus they are trying to study.
Recommended Reading

What the Chaos in Hospitals Is Doing to Doctors

How the Pandemic Defeated America

This Is No Way to Be Human
Experts on emerging diseases are scarce: These threats go neglected by the public in the lulls between epidemics. “Just a year ago I had to explain to people why I was studying coronaviruses,” says Lisa Gralinski of the University of North Carolina at Chapel Hill. “That’s never going to be a concern again.” Stressed and stretched, she and other emerging-disease researchers were also conscripted into unfamiliar roles. They’re acting as makeshift advisers to businesses, schools, and local governments. They’re barraged by interview requests from journalists. They’re explaining the nuances of the pandemic on Twitter, to huge new follower counts. “It’s often the same person who’s helping the Namibian government to manage malaria outbreaks and is now being pulled into helping Maryland manage COVID‑19,” Gardner told me.
But the newfound global interest in viruses also means “you have a lot more people you can talk through problems with,” Pardis Sabeti, a computational geneticist at the Broad Institute of MIT and Harvard, told me. Indeed, COVID‑19 papers are more likely than typical biomedical studies to have authors who had never published together before, according to a team led by Ying Ding, who works at the University of Texas at Austin.
Fast-forming alliances could work at breakneck speed because many researchers had spent the past few decades transforming science from a plodding, cloistered endeavor into something nimbler and more transparent. Traditionally, a scientist submits her paper to a journal, which sends it to a (surprisingly small) group of peers for (several rounds of usually anonymous) comments; if the paper passes this (typically months-long) peer-review gantlet, it is published (often behind an expensive paywall). Languid and opaque, this system is ill-suited to a fast-moving outbreak. But biomedical scientists can now upload preliminary versions of their papers, or “preprints,” to freely accessible websites, allowing others to immediately dissect and build upon their results. This practice had been slowly gaining popularity before 2020, but proved so vital for sharing information about COVID‑19 that it will likely become a mainstay of modern biomedical research. Preprints accelerate science, and the pandemic accelerated the use of preprints. At the start of the year, one repository, medRxiv (pronounced “med archive”), held about 1,000 preprints. By the end of October, it had more than 12,000.
Open data sets and sophisticated new tools to manipulate them have likewise made today’s researchers more flexible. SARS‑CoV‑2’s genome was decoded and shared by Chinese scientists just 10 days after the first cases were reported. By November, more than 197,000 SARS‑CoV‑2 genomes had been sequenced. About 90 years ago, no one had even seen an individual virus; today, scientists have reconstructed the shape of SARS‑CoV‑2 down to the position of individual atoms. Researchers have begun to uncover how SARS‑CoV‑2 compares with other coronaviruses in wild bats, the likely reservoir; how it infiltrates and co-opts our cells; how the immune system overreacts to it, creating the symptoms of COVID‑19. “We’re learning about this virus faster than we’ve ever learned about any virus in history,” Sabeti said.
By March, the odds of quickly eradicating the new coronavirus looked slim. A vaccine became the likeliest endgame, and the race to create one was a resounding success. The process normally takes years, but as I write this, 54 different vaccines are being tested for safety and efficacy, and 12 have entered Phase 3 clinical trials—the final checkpoint. As of this writing, Pfizer/BioNTech and Moderna have announced that, based on preliminary results from these trials, their respective vaccines are roughly 95 percent effective at preventing COVID‑19. * “We went from a virus whose sequence was only known in January, and now in the fall, we’re finishing— finishing —a Phase 3 trial,” Anthony Fauci, the director of the National Institute of Allergy and Infectious Diseases and a member of the White House’s coronavirus task force, told me. “Holy mackerel.”
Most vaccines comprise dead, weakened, or fragmented pathogens, and must be made from scratch whenever a new threat emerges. But over the past decade, the U.S. and other countries have moved away from this slow “one bug, one drug” approach. Instead, they’ve invested in so-called platform technologies, in which a standard chassis can be easily customized with different payloads that target new viruses. For example, the Pfizer/BioNTech and Moderna vaccines both consist of nanoparticles that contain pieces of SARS‑CoV‑2’s genetic material—its mRNA. When volunteers are injected with these particles, their cells use the mRNA to reconstruct a noninfectious fragment of the virus, allowing their immune system to prepare antibodies that neutralize it. No company has ever brought an mRNA vaccine to market before, but because the basic platform had already been refined, researchers could quickly repurpose it with SARS‑CoV‑2’s mRNA. Moderna got its vaccine into Phase 1 clinical trials on March 16, just 66 days after the new virus’s genome was first uploaded—far faster than any pre-COVID vaccine.
Meanwhile, companies compressed the process of vaccine development by running what would normally be sequential steps in parallel, while still checking for safety and efficacy. The federal government’s Operation Warp Speed, an effort to accelerate vaccine distribution, funded several companies at once—an unusual move. It preordered doses and invested in manufacturing facilities before trials were complete, reducing the risk for pharmaceutical companies looking to participate. Ironically, federal ineptitude at containing SARS‑CoV‑2 helped too. In the U.S., “the fact that the virus is everywhere makes it easier to gauge the performance of a vaccine,” says Natalie Dean of the University of Florida, who studies vaccine trials. “You can’t do a [Phase 3] vaccine trial in South Korea,” because the outbreak there is under control.
Read: How the pandemic will end
Vaccines will not immediately end the pandemic . Millions of doses will have to be manufactured, allocated, and distributed ; large numbers of Americans could refuse the vaccine ; and how long vaccine-induced immunity will last is still unclear. In the rosiest scenario, the Pfizer/BioNTech and Moderna vaccines are approved and smoothly rolled out over the next 12 months. By the end of the year, the U.S. achieves herd immunity, after which the virus struggles to find susceptible hosts. It still circulates, but outbreaks are sporadic and short-lived. Schools and businesses reopen. Families hug tightly and celebrate joyously over Thanksgiving and Christmas.
And the next time a mystery pathogen emerges, scientists hope to quickly slot its genetic material into proven platforms, and move the resulting vaccines through the same speedy pipelines that were developed during this pandemic. “I don’t think the world of vaccine development will ever be the same again,” says Nicole Lurie of the Coalition for Epidemic Preparedness Innovations.
As fast as the vaccine-development process was, it could have been faster. Despite the stakes, some pharmaceutical companies with relevant expertise chose not to enter the race, perhaps dissuaded by intense competition. Instead, from February to May, the sector roughly tripled its efforts to develop drugs to treat COVID‑19, according to Kevin Bryan, an economist at the University of Toronto. The decades-old steroid dexamethasone turned out to reduce death rates among severely ill patients on ventilators by more than 12 percent. Early hints suggest that newer treatments such as the monoclonal-antibody therapy bamlanivimab, which was just approved for emergency use by the FDA, could help newly infected patients who have not yet been hospitalized. But although these wins are significant, they are scarce. Most drugs haven’t been effective. Health-care workers became better at saving hospitalized patients more through improvements in basic medical care than through pharmaceutical panaceas—a predictable outcome, because antiviral drugs tend to offer only modest benefits.
The quest for COVID‑19 treatments was slowed by a torrent of shoddy studies whose results were meaningless at best and misleading at worst. Many of the thousands of clinical trials that were launched were too small to produce statistically solid results. Some lacked a control group—a set of comparable patients who received a placebo, and who provided a baseline against which the effects of a drug could be judged. Other trials needlessly overlapped. At least 227 involved hydroxychloroquine—the antimalarial drug that Donald Trump hyped for months. A few large trials eventually confirmed that hydroxychloroquine does nothing for COVID‑19 patients, but not before hundreds of thousands of people were recruited into pointlessly small studies . More than 100,000 Americans have also received convalescent plasma—another treatment that Trump touted. But because most were not enrolled in rigorous trials, “we still don’t know if it works—and it likely doesn’t,” says Luciana Borio, the former director for medical and biodefense preparedness at the National Security Council. “What a waste of time and resources.”
Read: How we survive the winter
In the heat of a disaster, when emergency rooms are filling and patients are dying, it is hard to set up one careful study, let alone coordinate several across a country. But coordination is not impossible. During World War II , federal agencies unified private companies, universities, the military, and other entities in a carefully orchestrated effort to speed pharmaceutical development from benchtop to battlefield. The results—revolutionary malaria treatments, new ways of mass-producing antibiotics, and at least 10 new or improved vaccines for influenza and other diseases—represented “not a triumph of scientific genius but rather of organizational purpose and efficiency,” Kendall Hoyt of Dartmouth College has written.
Similar triumphs occurred last year—in other countries. In March, taking advantage of the United Kingdom’s nationalized health system, British researchers launched a nationwide study called Recovery, which has since enrolled more than 17,600 COVID‑19 patients across 176 institutions. Recovery offered conclusive answers about dexamethasone and hydroxychloroquine and is set to weigh in on several other treatments. No other study has done more to shape the treatment of COVID‑19. The U.S. is now catching up. In April, the NIH launched a partnership called ACTIV , in which academic and industry scientists prioritized the most promising drugs and coordinated trial plans across the country. Since August, several such trials have started. This model was late, but is likely to outlast the pandemic itself, allowing future researchers to rapidly sort medical wheat from pharmaceutical chaff. “I can’t imagine we’ll go back to doing clinical research in the future the way we did in the past,” the NIH’s Francis Collins said.
Even after the COVID‑19 pandemic, the fruits of the pivot will leave us better equipped for our long and intensifying war against harmful viruses. The last time a virus caused this much devastation—the flu pandemic of 1918—scientists were only just learning about viruses, and spent time looking for a bacterial culprit. This one is different. With so many scientists observing intently as a virus wreaks its horrible work upon millions of bodies, the world is learning lessons that could change the way we think about these pathogens forevermore.
Consider the long-term consequences of viral infections. Years after the original SARS virus hit Hong Kong in 2003, about a quarter of survivors still had myalgic encephalomyelitis—a chronic illness whose symptoms, such as extreme fatigue and brain fogs, can worsen dramatically after mild exertion. ME cases are thought to be linked to viral infections, and clusters sometimes follow big outbreaks. So when SARS‑CoV‑2 started spreading, people with ME were unsurprised to hear that tens of thousands of COVID‑19 “long-haulers” were experiencing incapacitating symptoms that rolled on for months . “Everyone in my community has been thinking about this since the start of the pandemic,” says Jennifer Brea, the executive director of the advocacy group #MEAction.
ME and sister illnesses such as dysautonomia, fibromyalgia, and mast cell activation syndrome have long been neglected, their symptoms dismissed as imaginary or psychiatric. Research is poorly funded, so few scientists study them. Little is known about how to prevent and treat them. This negligence has left COVID‑19 long-haulers with few answers or options, and they initially endured the same dismissal as the larger ME community. But their sheer numbers have forced a degree of recognition. They started researching, cataloging their own symptoms. They gained audiences with the NIH and the World Health Organization. Patients who are themselves experts in infectious disease or public health published their stories in top journals. “Long COVID” is being taken seriously, and Brea hopes it might drag all post-infection illnesses into the spotlight. ME never experienced a pivot. COVID‑19 might inadvertently create one.
Anthony Fauci hopes so. His career was defined by HIV, and in 2019 he said in a paper he co-wrote that “the collateral advantages of” studying HIV “have been profound.” Research into HIV/AIDS revolutionized our understanding of the immune system and how diseases subvert it. It produced techniques for developing antiviral drugs that led to treatments for hepatitis C. Inactivated versions of HIV have been used to treat cancers and genetic disorders. From one disease came a cascade of benefits. COVID‑19 will be no different. Fauci had personally seen cases of prolonged symptoms after other viral infections, but “I didn’t really have a good scientific handle on it,” he told me. Such cases are hard to study, because it’s usually impossible to identify the instigating pathogen. But COVID‑19 has created “the most unusual situation imaginable,” Fauci said—a massive cohort of people with long-haul symptoms that are almost certainly caused by one known virus. “It’s an opportunity we cannot lose,” he said.
Read: The core lesson of the COVID-19 heart debate
COVID‑19 has developed a terrifying mystique because it seems to behave in unusual ways. It causes mild symptoms in some but critical illness in others. It is a respiratory virus and yet seems to attack the heart, brain, kidneys, and other organs. It has reinfected a small number of people who had recently recovered. But many other viruses share similar abilities; they just don’t infect millions of people in a matter of months or grab the attention of the entire scientific community. Thanks to COVID‑19, more researchers are looking for these rarer sides of viral infections, and spotting them.
At least 20 known viruses, including influenza and measles, can trigger myocarditis—inflammation of the heart. Some of these cases resolve on their own, but others cause persistent scarring, and still others rapidly progress into lethal problems. No one knows what proportion of people with viral myocarditis experience the most mild fate, because doctors typically notice only those who seek medical attention. But now researchers are also intently scrutinizing the hearts of people with mild or asymptomatic COVID‑19 infections, including college athletes, given concerns about sudden cardiac arrest during strenuous workouts. The lessons from these efforts could ultimately avert deaths from other infections.
Respiratory viruses, though extremely common, are often neglected. Respiratory syncytial virus, parainfluenza viruses, rhinoviruses, adenoviruses, bocaviruses, a quartet of other human coronaviruses—they mostly cause mild coldlike illnesses, but those can be severe. How often? Why? It’s hard to say, because, influenza aside, such viruses attract little funding or interest. “There’s a perception that they’re just colds and there’s nothing much to learn,” says Emily Martin of the University of Michigan, who has long struggled to get funding to study them. Such reasoning is shortsighted folly. Respiratory viruses are the pathogens most likely to cause pandemics, and those outbreaks could potentially be far worse than COVID‑19’s.
Read: We need to talk about ventilation
Their movements through the air have been poorly studied, too. “There’s this very entrenched idea,” says Linsey Marr at Virginia Tech, that viruses mostly spread through droplets (short-range globs of snot and spit) rather than aerosols (smaller, dustlike flecks that travel farther). That idea dates back to the 1930s, when scientists were upending outdated notions that disease was caused by “bad air,” or miasma. But the evidence that SARS‑CoV‑2 can spread through aerosols “is now overwhelming,” says Marr, one of the few scientists who, before the pandemic, studied how viruses spread through air. “I’ve seen more acceptance in the last six months than over the 12 years I’ve been working on this.”
Another pandemic is inevitable, but it will find a very different community of scientists than COVID‑19 did. They will immediately work to determine whether the pathogen—most likely another respiratory virus—moves through aerosols, and whether it spreads from infected people before causing symptoms. They might call for masks and better ventilation from the earliest moments, not after months of debate. They will anticipate the possibility of an imminent wave of long-haul symptoms, and hopefully discover ways of preventing them. They might set up research groups to prioritize the most promising drugs and coordinate large clinical trials. They might take vaccine platforms that worked best against COVID‑19, slot in the genetic material of the new pathogen, and have a vaccine ready within months.
For all its benefits, the single-minded focus on COVID‑19 will also leave a slew of negative legacies. Science is mostly a zero-sum game, and when one topic monopolizes attention and money, others lose out. Last year, between physical-distancing restrictions, redirected funds, and distracted scientists, many lines of research slowed to a crawl. Long-term studies that monitored bird migrations or the changing climate will forever have holes in their data because field research had to be canceled. Conservationists who worked to protect monkeys and apes kept their distance for fear of passing COVID‑19 to already endangered species. Roughly 80 percent of non-COVID‑19 clinical trials in the U.S.—likely worth billions of dollars—were interrupted or stopped because hospitals were overwhelmed and volunteers were stuck at home. Even research on other infectious diseases was back-burnered. “All the non-COVID work that I was working on before the pandemic started is now piling up and gathering dust,” says Angela Rasmussen of Georgetown University, who normally studies Ebola and MERS. “Those are still problems.”
The COVID‑19 pandemic is a singular disaster, and it is reasonable for society—and scientists—to prioritize it. But the pivot was driven by opportunism as much as altruism. Governments, philanthropies, and universities channeled huge sums toward COVID‑19 research. The NIH alone received nearly $3.6 billion from Congress. The Bill & Melinda Gates Foundation apportioned $350 million for COVID‑19 work. “Whenever there’s a big pot of money, there’s a feeding frenzy,” Madhukar Pai told me. He works on tuberculosis, which causes 1.5 million deaths a year—comparable to COVID‑19’s toll in 2020. Yet tuberculosis research has been mostly paused. None of Pai’s colleagues pivoted when Ebola or Zika struck, but “half of us have now swung to working on COVID‑19,” he said. “It’s a black hole, sucking us all in.”
While the most qualified experts became quickly immersed in the pandemic response, others were stuck at home looking for ways to contribute. Using the same systems that made science faster, they could download data from free databases, run quick analyses with intuitive tools, publish their work on preprint servers, and publicize it on Twitter. Often, they made things worse by swerving out of their scholarly lanes and plowing into unfamiliar territory. Nathan Ballantyne, a philosopher at Fordham University, calls this “ epistemic trespassing .” It can be a good thing: Continental drift was championed by Alfred Wegener, a meteorologist; microbes were first documented by Antonie van Leeuwenhoek, a draper. But more often than not, epistemic trespassing just creates a mess, especially when inexperience couples with overconfidence.
On March 28, a preprint noted that countries that universally use a tuberculosis vaccine called BCG had lower COVID‑19 mortality rates. But such cross-country comparisons are infamously treacherous. For example, countries with higher cigarette-usage rates have longer life expectancies, not because smoking prolongs life but because it is more popular in wealthier nations. This tendency to draw faulty conclusions about individual health using data about large geographical regions is called the ecological fallacy. Epidemiologists know to avoid it. The BCG-preprint authors, who were from an osteopathic college in New York, didn’t seem to . But their paper was covered by more than 70 news outlets, and dozens of inexperienced teams offered similarly specious analyses. “People who don’t know how to spell tuberculosis have told me they can solve the link between BCG and COVID‑19,” Pai said. “Someone told me they can do it in 48 hours with a hackathon.”

Other epistemic trespassers spent their time reinventing the wheel. One new study, published in NEJM , used lasers to show that when people speak, they release aerosols. But as the authors themselves note, the same result—sans lasers—was published in 1946, Marr says. I asked her whether any papers from the 2020 batch had taught her something new. After an uncomfortably long pause, she mentioned just one.
In some cases, bad papers helped shape the public narrative of the pandemic. On March 16, two biogeographers published a preprint arguing that COVID‑19 will “marginally affect the tropics” because it fares poorly in warm, humid conditions. Disease experts quickly noted that techniques like the ones the duo used are meant for modeling the geographic ranges of animal and plant species or vector-borne pathogens, and are ill-suited to simulating the spread of viruses like SARS-CoV-2. But their claim was picked up by more than 50 news outlets and echoed by the United Nations World Food Program. COVID‑19 has since run rampant in many tropical countries, including Brazil, Indonesia, and Colombia—and the preprint’s authors have qualified their conclusions in later versions of the paper. “It takes a certain type of person to think that weeks of reading papers gives them more perspective than someone with a Ph.D. on that subject, and that type of person has gotten a lot of airtime in this pandemic,” says Colin Carlson of Georgetown.
The incentives to trespass are substantial. Academia is a pyramid scheme: Each biomedical professor trains an average of six doctoral students across her career, but only 16 percent of the students get tenure-track positions . Competition is ferocious, and success hinges on getting published—a feat made easier by dramatic results. These factors pull researchers toward speed, short-termism, and hype at the expense of rigor—and the pandemic intensified that pull. With an anxious world crying out for information, any new paper could immediately draw international press coverage—and hundreds of citations.
The tsunami of rushed but dubious work made life harder for actual experts, who struggled to sift the signal from the noise. They also felt obliged to debunk spurious research in long Twitter threads and relentless media interviews—acts of public service that are rarely rewarded in academia. And they were overwhelmed by requests to peer-review new papers. Kristian Andersen, an infectious-disease researcher at Scripps Research, told me that journals used to send him two or three such requests a month. Now “I’m getting three or five a day,” he said in September.
The pandemic’s opportunities also fell inequitably upon the scientific community. In March, Congress awarded $75 million to the National Science Foundation to fast-track studies that could quickly contribute to the pandemic response. “That money just went ,” says Cassidy Sugimoto of Indiana University, who was on rotation at the agency at the time. “It was a first-come, first-served environment. It advantaged people who were aware of the system and could act upon it quickly.” But not all scientists could pivot to COVID‑19, or pivot with equal speed.
Among scientists, as in other fields, women do more child care, domestic work, and teaching than men, and are more often asked for emotional support by their students. These burdens increased as the pandemic took hold, leaving women scientists “less able to commit their time to learning about a new area of study, and less able to start a whole new research project,” says Molly M. King, a sociologist at Santa Clara University. Women’s research hours fell by nine percentage points more than did men’s because of the pressures of COVID‑19. And when COVID‑19 created new opportunities, men grabbed them more quickly. In the spring, the proportion of papers with women as first authors fell almost 44 percent in the preprint repository medRxiv, relative to 2019. And published COVID‑19 papers had 19 percent fewer women as first authors compared with papers from the same journals in the previous year. Men led more than 80 percent of national COVID‑19 task forces in 87 countries . Male scientists were quoted four times as frequently as female scientists in American news stories about the pandemic.
American scientists of color also found it harder to pivot than their white peers, because of unique challenges that sapped their time and energy. Black, Latino, and Indigenous scientists were most likely to have lost loved ones, adding mourning to their list of duties. Many grieved, too, after the killings of Breonna Taylor, George Floyd, Ahmaud Arbery, and others. They often faced questions from relatives who were mistrustful of the medical system, or were experiencing discriminatory care. They were suddenly tasked with helping their predominantly white institutions fight racism. Neil Lewis Jr. at Cornell, who studies racial health disparities, told me that many psychologists had long deemed his work irrelevant. “All of a sudden my inbox is drowning,” he said, while some of his own relatives have become ill and one has died.
Science suffers from the so-called Matthew effect, whereby small successes snowball into ever greater advantages, irrespective of merit. Similarly, early hindrances linger. Young researchers who could not pivot because they were too busy caring or grieving for others might suffer lasting consequences from an unproductive year. COVID‑19 “has really put the clock back in terms of closing the gap for women and underrepresented minorities,” Yale’s Akiko Iwasaki says. “Once we’re over the pandemic, we’ll need to fix it all again.”
COVID-19 has already changed science immensely, but if scientists are savvy, the most profound pivot is still to come—a grand reimagining of what medicine should be. In 1848, the Prussian government sent a young physician named Rudolf Virchow to investigate a typhus epidemic in Upper Silesia. Virchow didn’t know what caused the devastating disease, but he realized its spread was possible because of malnutrition, hazardous working conditions, crowded housing, poor sanitation, and the inattention of civil servants and aristocrats—problems that require social and political reforms. “Medicine is a social science,” Virchow said, “and politics is nothing but medicine in larger scale.”
This viewpoint fell by the wayside after germ theory became mainstream in the late 19th century. When scientists discovered the microbes responsible for tuberculosis, plague, cholera, dysentery, and syphilis, most fixated on these newly identified nemeses. Societal factors were seen as overly political distractions for researchers who sought to “be as ‘objective’ as possible,” says Elaine Hernandez, a medical sociologist at Indiana University. In the U.S., medicine fractured. New departments of sociology and cultural anthropology kept their eye on the societal side of health, while the nation’s first schools of public health focused instead on fights between germs and individuals. This rift widened as improvements in hygiene, living standards, nutrition, and sanitation lengthened life spans: The more social conditions improved, the more readily they could be ignored.
The ideological pivot away from social medicine began to reverse in the second half of the 20th century. The women’s-rights and civil-rights movements, the rise of environmentalism, and anti-war protests created a generation of scholars who questioned “the legitimacy, ideology, and practice of any science … that disregards social and economic inequality,” wrote Nancy Krieger of Harvard . Beginning in the 1980s, this new wave of social epidemiologists once again studied how poverty, privilege, and living conditions affect a person’s health—to a degree even Virchow hadn’t imagined. But as COVID‑19 has shown, the reintegration is not yet complete.
Politicians initially described COVID‑19 as a “great equalizer,” but when states began releasing demographic data, it was immediately clear that the disease was disproportionately infecting and killing people of color . These disparities aren’t biological. They stem from decades of discrimination and segregation that left minority communities in poorer neighborhoods with low-paying jobs, more health problems, and less access to health care—the same kind of problems that Virchow identified more than 170 years ago.
From the September 2020 issue: How the pandemic defeated America
Simple acts like wearing a mask and staying at home, which rely on people tolerating discomfort for the collective good, became society’s main defenses against the virus in the many months without effective drugs or vaccines. These are known as nonpharmaceutical interventions—a name that betrays medicine’s biological bias. For most of 2020, these were the only interventions on offer, but they were nonetheless defined in opposition to the more highly prized drugs and vaccines.
In March, when the U.S. started shutting down, one of the biggest questions on the mind of Whitney Robinson of UNC at Chapel Hill was: Are our kids going to be out of school for two years? While biomedical scientists tend to focus on sickness and recovery, social epidemiologists like her “think about critical periods that can affect the trajectory of your life,” she told me. Disrupting a child’s schooling at the wrong time can affect their entire career, so scientists should have prioritized research to figure out whether and how schools could reopen safely. But most studies on the spread of COVID‑19 in schools were neither large in scope nor well-designed enough to be conclusive. No federal agency funded a large, nationwide study, even though the federal government had months to do so. The NIH received billions for COVID‑19 research , but the National Institute of Child Health and Human Development—one of its 27 constituent institutes and centers—got nothing.
The horrors that Rudolf Virchow saw in Upper Silesia radicalized him, pushing the future “father of modern pathology” to advocate for social reforms. The current pandemic has affected scientists in the same way. Calm researchers became incensed as potentially game-changing innovations like cheap diagnostic tests were squandered by a negligent administration and a muzzled Centers for Disease Control and Prevention. Austere publications like NEJM and Nature published explicitly political editorials castigating the Trump administration for its failures and encouraging voters to hold the president accountable. COVID‑19 could be the catalyst that fully reunifies the social and biological sides of medicine, bridging disciplines that have been separated for too long.
“To study COVID‑19 is not only to study the disease itself as a biological entity,” says Alondra Nelson, the president of the Social Science Research Council. “What looks like a single problem is actually all things, all at once. So what we’re actually studying is literally everything in society, at every scale, from supply chains to individual relationships.”
The scientific community spent the pre-pandemic years designing faster ways of doing experiments, sharing data, and developing vaccines, allowing it to mobilize quickly when COVID‑19 emerged. Its goal now should be to address its many lingering weaknesses. Warped incentives, wasteful practices, overconfidence, inequality, a biomedical bias—COVID‑19 has exposed them all. And in doing so, it offers the world of science a chance to practice one of its most important qualities: self-correction.
* The print version of this article stated that the Moderna and Pfizer/BioNTech vaccines were reported to be 95 percent effective at preventing COVID-19 infections. In fact, the vaccines prevent disease, not infection.
This article appears in the January/February 2021 print edition with the headline “The COVID-19 Manhattan Project.”
About the Author
More Stories
Fatigue Can Shatter a Person
Who’s the Cutest Little Dolphin? Is It You?

Wait Wait...Don't Tell Me
Listen live.

On the Media
While maintaining the civility and fairness that are the hallmarks of public radio, On the Media tackles sticky issues with a frankness and transparency that has built trust with listeners and earned it awards for its body of work.
Coronavirus: The world has come together to flatten the curve. Can we stay united to tackle other crises?
Watching the world come together gives me hope for the future, writes mira patel, a high school junior..

Mira Patel and her sister Veda. (Courtesy of Dee Patel)
Related Content

This 24-year-old entrepreneur is helping Black-owned restaurants survive coronavirus
Black and Mobile is an online delivery service that caters to Black-owned restaurants. The coronavirus shutdown has increased demand for its service.
4 years ago

Home desks won’t replace Philly’s high-rise office towers anytime soon, analysts say
Philadelphia’s office market might fare better post-coronavirus than those of other U.S. cities, CBRE analysts said in a new report.
Before the pandemic, I had often heard adults say that young people would lose the ability to connect in-person with others due to our growing dependence on technology and social media. However, this stay-at-home experience has proven to me that our elders’ worry is unnecessary. Because isolation isn’t in human nature, and no advancement in technology could replace our need to meet in person, especially when it comes to learning.
As the weather gets warmer and we approach summertime, it’s going to be more and more tempting for us teenagers to go out and do what we have always done: hang out and have fun. Even though the decision-makers are adults, everyone has a role to play and we teens can help the world move forward by continuing to self-isolate. It’s incredibly important that in the coming weeks, we respect the government’s effort to contain the spread of the coronavirus.
In the meantime, we can find creative ways to stay connected and continue to do what we love. Personally, I see many 6-feet-apart bike rides and Zoom calls in my future.
If there is anything that this pandemic has made me realize, it’s how connected we all are. At first, the infamous coronavirus seemed to be a problem in China, which is worlds away. But slowly, it steadily made its way through various countries in Europe, and inevitably reached us in America. What was once framed as a foreign virus has now hit home.
Watching the global community come together, gives me hope, as a teenager, that in the future we can use this cooperation to combat climate change and other catastrophes.
As COVID-19 continues to creep its way into each of our communities and impact the way we live and communicate, I find solace in the fact that we face what comes next together, as humanity.
When the day comes that my generation is responsible for dealing with another crisis, I hope we can use this experience to remind us that moving forward requires a joint effort.
Mira Patel is a junior at Strath Haven High School and is an education intern at the Foreign Policy Research Institute in Philadelphia. Follow her on Instagram here.
Becoming a storyteller at WHYY, your local public media station, is easier than you might think. Text STORYTELLER to 267-494-9949 to learn more.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.
Part of the series

Coronavirus Pandemic
You may also like.
Threats and violence suspend high school football games Friday night
Fight breaks out at a game between Pennsauken and Camden High Schools, threats suspend games in Chester and Northampton Counties.
3 years ago

Philly students get vaxxed at the zoo before heading back to school
The event is the first of its kind for the school district, but arrives after months of partnering with CHOP to organize other vaccination clinics around the city.

Montco high school senior reflects on missing experiences because of coronavirus
Grace Honeyman, a senior at Harriton High School, talks with her father about how she’s dealing with missing milestones due to coronavirus.
Want a digest of WHYY’s programs, events & stories? Sign up for our weekly newsletter.
Together we can reach 100% of WHYY’s fiscal year goal
We need your support today
Independent journalism is more important than ever. Vox is here to explain this unprecedented election cycle and help you understand the larger stakes. We will break down where the candidates stand on major issues, from economic policy to immigration, foreign policy, criminal justice, and abortion. We’ll answer your biggest questions, and we’ll explain what matters — and why. This timely and essential task, however, is expensive to produce.
We rely on readers like you to fund our journalism. Will you support our work and become a Vox Member today?
Read these 12 moving essays about life during coronavirus
Artists, novelists, critics, and essayists are writing the first draft of history.
by Alissa Wilkinson

The world is grappling with an invisible, deadly enemy, trying to understand how to live with the threat posed by a virus . For some writers, the only way forward is to put pen to paper, trying to conceptualize and document what it feels like to continue living as countries are under lockdown and regular life seems to have ground to a halt.
So as the coronavirus pandemic has stretched around the world, it’s sparked a crop of diary entries and essays that describe how life has changed. Novelists, critics, artists, and journalists have put words to the feelings many are experiencing. The result is a first draft of how we’ll someday remember this time, filled with uncertainty and pain and fear as well as small moments of hope and humanity.
- The Vox guide to navigating the coronavirus crisis
At the New York Review of Books, Ali Bhutto writes that in Karachi, Pakistan, the government-imposed curfew due to the virus is “eerily reminiscent of past military clampdowns”:
Beneath the quiet calm lies a sense that society has been unhinged and that the usual rules no longer apply. Small groups of pedestrians look on from the shadows, like an audience watching a spectacle slowly unfolding. People pause on street corners and in the shade of trees, under the watchful gaze of the paramilitary forces and the police.
His essay concludes with the sobering note that “in the minds of many, Covid-19 is just another life-threatening hazard in a city that stumbles from one crisis to another.”
Writing from Chattanooga, novelist Jamie Quatro documents the mixed ways her neighbors have been responding to the threat, and the frustration of conflicting direction, or no direction at all, from local, state, and federal leaders:
Whiplash, trying to keep up with who’s ordering what. We’re already experiencing enough chaos without this back-and-forth. Why didn’t the federal government issue a nationwide shelter-in-place at the get-go, the way other countries did? What happens when one state’s shelter-in-place ends, while others continue? Do states still under quarantine close their borders? We are still one nation, not fifty individual countries. Right?
- A syllabus for the end of the world
Award-winning photojournalist Alessio Mamo, quarantined with his partner Marta in Sicily after she tested positive for the virus, accompanies his photographs in the Guardian of their confinement with a reflection on being confined :
The doctors asked me to take a second test, but again I tested negative. Perhaps I’m immune? The days dragged on in my apartment, in black and white, like my photos. Sometimes we tried to smile, imagining that I was asymptomatic, because I was the virus. Our smiles seemed to bring good news. My mother left hospital, but I won’t be able to see her for weeks. Marta started breathing well again, and so did I. I would have liked to photograph my country in the midst of this emergency, the battles that the doctors wage on the frontline, the hospitals pushed to their limits, Italy on its knees fighting an invisible enemy. That enemy, a day in March, knocked on my door instead.
In the New York Times Magazine, deputy editor Jessica Lustig writes with devastating clarity about her family’s life in Brooklyn while her husband battled the virus, weeks before most people began taking the threat seriously:
At the door of the clinic, we stand looking out at two older women chatting outside the doorway, oblivious. Do I wave them away? Call out that they should get far away, go home, wash their hands, stay inside? Instead we just stand there, awkwardly, until they move on. Only then do we step outside to begin the long three-block walk home. I point out the early magnolia, the forsythia. T says he is cold. The untrimmed hairs on his neck, under his beard, are white. The few people walking past us on the sidewalk don’t know that we are visitors from the future. A vision, a premonition, a walking visitation. This will be them: Either T, in the mask, or — if they’re lucky — me, tending to him.
Essayist Leslie Jamison writes in the New York Review of Books about being shut away alone in her New York City apartment with her 2-year-old daughter since she became sick:
The virus. Its sinewy, intimate name. What does it feel like in my body today? Shivering under blankets. A hot itch behind the eyes. Three sweatshirts in the middle of the day. My daughter trying to pull another blanket over my body with her tiny arms. An ache in the muscles that somehow makes it hard to lie still. This loss of taste has become a kind of sensory quarantine. It’s as if the quarantine keeps inching closer and closer to my insides. First I lost the touch of other bodies; then I lost the air; now I’ve lost the taste of bananas. Nothing about any of these losses is particularly unique. I’ve made a schedule so I won’t go insane with the toddler. Five days ago, I wrote Walk/Adventure! on it, next to a cut-out illustration of a tiger—as if we’d see tigers on our walks. It was good to keep possibility alive.
At Literary Hub, novelist Heidi Pitlor writes about the elastic nature of time during her family’s quarantine in Massachusetts:
During a shutdown, the things that mark our days—commuting to work, sending our kids to school, having a drink with friends—vanish and time takes on a flat, seamless quality. Without some self-imposed structure, it’s easy to feel a little untethered. A friend recently posted on Facebook: “For those who have lost track, today is Blursday the fortyteenth of Maprilay.” ... Giving shape to time is especially important now, when the future is so shapeless. We do not know whether the virus will continue to rage for weeks or months or, lord help us, on and off for years. We do not know when we will feel safe again. And so many of us, minus those who are gifted at compartmentalization or denial, remain largely captive to fear. We may stay this way if we do not create at least the illusion of movement in our lives, our long days spent with ourselves or partners or families.
- What day is it today?
Novelist Lauren Groff writes at the New York Review of Books about trying to escape the prison of her fears while sequestered at home in Gainesville, Florida:
Some people have imaginations sparked only by what they can see; I blame this blinkered empiricism for the parks overwhelmed with people, the bars, until a few nights ago, thickly thronged. My imagination is the opposite. I fear everything invisible to me. From the enclosure of my house, I am afraid of the suffering that isn’t present before me, the people running out of money and food or drowning in the fluid in their lungs, the deaths of health-care workers now growing ill while performing their duties. I fear the federal government, which the right wing has so—intentionally—weakened that not only is it insufficient to help its people, it is actively standing in help’s way. I fear we won’t sufficiently punish the right. I fear leaving the house and spreading the disease. I fear what this time of fear is doing to my children, their imaginations, and their souls.
At ArtForum , Berlin-based critic and writer Kristian Vistrup Madsen reflects on martinis, melancholia, and Finnish artist Jaakko Pallasvuo’s 2018 graphic novel Retreat , in which three young people exile themselves in the woods:
In melancholia, the shape of what is ending, and its temporality, is sprawling and incomprehensible. The ambivalence makes it hard to bear. The world of Retreat is rendered in lush pink and purple watercolors, which dissolve into wild and messy abstractions. In apocalypse, the divisions established in genesis bleed back out. My own Corona-retreat is similarly soft, color-field like, each day a blurred succession of quarantinis, YouTube–yoga, and televized press conferences. As restrictions mount, so does abstraction. For now, I’m still rooting for love to save the world.
At the Paris Review , Matt Levin writes about reading Virginia Woolf’s novel The Waves during quarantine:
A retreat, a quarantine, a sickness—they simultaneously distort and clarify, curtail and expand. It is an ideal state in which to read literature with a reputation for difficulty and inaccessibility, those hermetic books shorn of the handholds of conventional plot or characterization or description. A novel like Virginia Woolf’s The Waves is perfect for the state of interiority induced by quarantine—a story of three men and three women, meeting after the death of a mutual friend, told entirely in the overlapping internal monologues of the six, interspersed only with sections of pure, achingly beautiful descriptions of the natural world, a day’s procession and recession of light and waves. The novel is, in my mind’s eye, a perfectly spherical object. It is translucent and shimmering and infinitely fragile, prone to shatter at the slightest disturbance. It is not a book that can be read in snatches on the subway—it demands total absorption. Though it revels in a stark emotional nakedness, the book remains aloof, remote in its own deep self-absorption.
- Vox is starting a book club. Come read with us!
In an essay for the Financial Times, novelist Arundhati Roy writes with anger about Indian Prime Minister Narendra Modi’s anemic response to the threat, but also offers a glimmer of hope for the future:
Historically, pandemics have forced humans to break with the past and imagine their world anew. This one is no different. It is a portal, a gateway between one world and the next. We can choose to walk through it, dragging the carcasses of our prejudice and hatred, our avarice, our data banks and dead ideas, our dead rivers and smoky skies behind us. Or we can walk through lightly, with little luggage, ready to imagine another world. And ready to fight for it.
From Boston, Nora Caplan-Bricker writes in The Point about the strange contraction of space under quarantine, in which a friend in Beirut is as close as the one around the corner in the same city:
It’s a nice illusion—nice to feel like we’re in it together, even if my real world has shrunk to one person, my husband, who sits with his laptop in the other room. It’s nice in the same way as reading those essays that reframe social distancing as solidarity. “We must begin to see the negative space as clearly as the positive, to know what we don’t do is also brilliant and full of love,” the poet Anne Boyer wrote on March 10th, the day that Massachusetts declared a state of emergency. If you squint, you could almost make sense of this quarantine as an effort to flatten, along with the curve, the distinctions we make between our bonds with others. Right now, I care for my neighbor in the same way I demonstrate love for my mother: in all instances, I stay away. And in moments this month, I have loved strangers with an intensity that is new to me. On March 14th, the Saturday night after the end of life as we knew it, I went out with my dog and found the street silent: no lines for restaurants, no children on bicycles, no couples strolling with little cups of ice cream. It had taken the combined will of thousands of people to deliver such a sudden and complete emptiness. I felt so grateful, and so bereft.
And on his own website, musician and artist David Byrne writes about rediscovering the value of working for collective good , saying that “what is happening now is an opportunity to learn how to change our behavior”:
In emergencies, citizens can suddenly cooperate and collaborate. Change can happen. We’re going to need to work together as the effects of climate change ramp up. In order for capitalism to survive in any form, we will have to be a little more socialist. Here is an opportunity for us to see things differently — to see that we really are all connected — and adjust our behavior accordingly. Are we willing to do this? Is this moment an opportunity to see how truly interdependent we all are? To live in a world that is different and better than the one we live in now? We might be too far down the road to test every asymptomatic person, but a change in our mindsets, in how we view our neighbors, could lay the groundwork for the collective action we’ll need to deal with other global crises. The time to see how connected we all are is now.
The portrait these writers paint of a world under quarantine is multifaceted. Our worlds have contracted to the confines of our homes, and yet in some ways we’re more connected than ever to one another. We feel fear and boredom, anger and gratitude, frustration and strange peace. Uncertainty drives us to find metaphors and images that will let us wrap our minds around what is happening.
Yet there’s no single “what” that is happening. Everyone is contending with the pandemic and its effects from different places and in different ways. Reading others’ experiences — even the most frightening ones — can help alleviate the loneliness and dread, a little, and remind us that what we’re going through is both unique and shared by all.
- Recommendations
Most Popular
- The Trump Arlington National Cemetery controversy, explained
- Georgia’s MAGA elections board is laying the groundwork for an actual stolen election
- Your guide to the Brittany Mahomes-Donald Trump drama, such as it is
- Kamala Harris’s big housing plan has a big problem
- What the heck is “corn sweat” and is it making the Midwest more dangerous?
Today, Explained
Understand the world with a daily explainer plus the most compelling stories of the day.
This is the title for the native ad
More in Culture

Why everyone suddenly cares about Brittany Mahomes’s politics.

The second season of the series has huge news for fans of Tom Bombadil.

A newsletter about kids, for everyone.

How the once-maligned retailer quietly became a closet staple — and a stock market giant — once again.

My generation was taught to change the system. That lesson came at a cost.

The pods across the pond feel a lot less toxic.
- Research article
- Open access
- Published: 04 June 2021
Coronavirus disease (COVID-19) pandemic: an overview of systematic reviews
- Israel Júnior Borges do Nascimento 1 , 2 ,
- Dónal P. O’Mathúna 3 , 4 ,
- Thilo Caspar von Groote 5 ,
- Hebatullah Mohamed Abdulazeem 6 ,
- Ishanka Weerasekara 7 , 8 ,
- Ana Marusic 9 ,
- Livia Puljak ORCID: orcid.org/0000-0002-8467-6061 10 ,
- Vinicius Tassoni Civile 11 ,
- Irena Zakarija-Grkovic 9 ,
- Tina Poklepovic Pericic 9 ,
- Alvaro Nagib Atallah 11 ,
- Santino Filoso 12 ,
- Nicola Luigi Bragazzi 13 &
- Milena Soriano Marcolino 1
On behalf of the International Network of Coronavirus Disease 2019 (InterNetCOVID-19)
BMC Infectious Diseases volume 21 , Article number: 525 ( 2021 ) Cite this article
18k Accesses
32 Citations
14 Altmetric
Metrics details
Navigating the rapidly growing body of scientific literature on the SARS-CoV-2 pandemic is challenging, and ongoing critical appraisal of this output is essential. We aimed to summarize and critically appraise systematic reviews of coronavirus disease (COVID-19) in humans that were available at the beginning of the pandemic.
Nine databases (Medline, EMBASE, Cochrane Library, CINAHL, Web of Sciences, PDQ-Evidence, WHO’s Global Research, LILACS, and Epistemonikos) were searched from December 1, 2019, to March 24, 2020. Systematic reviews analyzing primary studies of COVID-19 were included. Two authors independently undertook screening, selection, extraction (data on clinical symptoms, prevalence, pharmacological and non-pharmacological interventions, diagnostic test assessment, laboratory, and radiological findings), and quality assessment (AMSTAR 2). A meta-analysis was performed of the prevalence of clinical outcomes.
Eighteen systematic reviews were included; one was empty (did not identify any relevant study). Using AMSTAR 2, confidence in the results of all 18 reviews was rated as “critically low”. Identified symptoms of COVID-19 were (range values of point estimates): fever (82–95%), cough with or without sputum (58–72%), dyspnea (26–59%), myalgia or muscle fatigue (29–51%), sore throat (10–13%), headache (8–12%) and gastrointestinal complaints (5–9%). Severe symptoms were more common in men. Elevated C-reactive protein and lactate dehydrogenase, and slightly elevated aspartate and alanine aminotransferase, were commonly described. Thrombocytopenia and elevated levels of procalcitonin and cardiac troponin I were associated with severe disease. A frequent finding on chest imaging was uni- or bilateral multilobar ground-glass opacity. A single review investigated the impact of medication (chloroquine) but found no verifiable clinical data. All-cause mortality ranged from 0.3 to 13.9%.
Conclusions
In this overview of systematic reviews, we analyzed evidence from the first 18 systematic reviews that were published after the emergence of COVID-19. However, confidence in the results of all reviews was “critically low”. Thus, systematic reviews that were published early on in the pandemic were of questionable usefulness. Even during public health emergencies, studies and systematic reviews should adhere to established methodological standards.
Peer Review reports
The spread of the “Severe Acute Respiratory Coronavirus 2” (SARS-CoV-2), the causal agent of COVID-19, was characterized as a pandemic by the World Health Organization (WHO) in March 2020 and has triggered an international public health emergency [ 1 ]. The numbers of confirmed cases and deaths due to COVID-19 are rapidly escalating, counting in millions [ 2 ], causing massive economic strain, and escalating healthcare and public health expenses [ 3 , 4 ].
The research community has responded by publishing an impressive number of scientific reports related to COVID-19. The world was alerted to the new disease at the beginning of 2020 [ 1 ], and by mid-March 2020, more than 2000 articles had been published on COVID-19 in scholarly journals, with 25% of them containing original data [ 5 ]. The living map of COVID-19 evidence, curated by the Evidence for Policy and Practice Information and Co-ordinating Centre (EPPI-Centre), contained more than 40,000 records by February 2021 [ 6 ]. More than 100,000 records on PubMed were labeled as “SARS-CoV-2 literature, sequence, and clinical content” by February 2021 [ 7 ].
Due to publication speed, the research community has voiced concerns regarding the quality and reproducibility of evidence produced during the COVID-19 pandemic, warning of the potential damaging approach of “publish first, retract later” [ 8 ]. It appears that these concerns are not unfounded, as it has been reported that COVID-19 articles were overrepresented in the pool of retracted articles in 2020 [ 9 ]. These concerns about inadequate evidence are of major importance because they can lead to poor clinical practice and inappropriate policies [ 10 ].
Systematic reviews are a cornerstone of today’s evidence-informed decision-making. By synthesizing all relevant evidence regarding a particular topic, systematic reviews reflect the current scientific knowledge. Systematic reviews are considered to be at the highest level in the hierarchy of evidence and should be used to make informed decisions. However, with high numbers of systematic reviews of different scope and methodological quality being published, overviews of multiple systematic reviews that assess their methodological quality are essential [ 11 , 12 , 13 ]. An overview of systematic reviews helps identify and organize the literature and highlights areas of priority in decision-making.
In this overview of systematic reviews, we aimed to summarize and critically appraise systematic reviews of coronavirus disease (COVID-19) in humans that were available at the beginning of the pandemic.
Methodology
Research question.
This overview’s primary objective was to summarize and critically appraise systematic reviews that assessed any type of primary clinical data from patients infected with SARS-CoV-2. Our research question was purposefully broad because we wanted to analyze as many systematic reviews as possible that were available early following the COVID-19 outbreak.
Study design
We conducted an overview of systematic reviews. The idea for this overview originated in a protocol for a systematic review submitted to PROSPERO (CRD42020170623), which indicated a plan to conduct an overview.
Overviews of systematic reviews use explicit and systematic methods for searching and identifying multiple systematic reviews addressing related research questions in the same field to extract and analyze evidence across important outcomes. Overviews of systematic reviews are in principle similar to systematic reviews of interventions, but the unit of analysis is a systematic review [ 14 , 15 , 16 ].
We used the overview methodology instead of other evidence synthesis methods to allow us to collate and appraise multiple systematic reviews on this topic, and to extract and analyze their results across relevant topics [ 17 ]. The overview and meta-analysis of systematic reviews allowed us to investigate the methodological quality of included studies, summarize results, and identify specific areas of available or limited evidence, thereby strengthening the current understanding of this novel disease and guiding future research [ 13 ].
A reporting guideline for overviews of reviews is currently under development, i.e., Preferred Reporting Items for Overviews of Reviews (PRIOR) [ 18 ]. As the PRIOR checklist is still not published, this study was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009 statement [ 19 ]. The methodology used in this review was adapted from the Cochrane Handbook for Systematic Reviews of Interventions and also followed established methodological considerations for analyzing existing systematic reviews [ 14 ].
Approval of a research ethics committee was not necessary as the study analyzed only publicly available articles.
Eligibility criteria
Systematic reviews were included if they analyzed primary data from patients infected with SARS-CoV-2 as confirmed by RT-PCR or another pre-specified diagnostic technique. Eligible reviews covered all topics related to COVID-19 including, but not limited to, those that reported clinical symptoms, diagnostic methods, therapeutic interventions, laboratory findings, or radiological results. Both full manuscripts and abbreviated versions, such as letters, were eligible.
No restrictions were imposed on the design of the primary studies included within the systematic reviews, the last search date, whether the review included meta-analyses or language. Reviews related to SARS-CoV-2 and other coronaviruses were eligible, but from those reviews, we analyzed only data related to SARS-CoV-2.
No consensus definition exists for a systematic review [ 20 ], and debates continue about the defining characteristics of a systematic review [ 21 ]. Cochrane’s guidance for overviews of reviews recommends setting pre-established criteria for making decisions around inclusion [ 14 ]. That is supported by a recent scoping review about guidance for overviews of systematic reviews [ 22 ].
Thus, for this study, we defined a systematic review as a research report which searched for primary research studies on a specific topic using an explicit search strategy, had a detailed description of the methods with explicit inclusion criteria provided, and provided a summary of the included studies either in narrative or quantitative format (such as a meta-analysis). Cochrane and non-Cochrane systematic reviews were considered eligible for inclusion, with or without meta-analysis, and regardless of the study design, language restriction and methodology of the included primary studies. To be eligible for inclusion, reviews had to be clearly analyzing data related to SARS-CoV-2 (associated or not with other viruses). We excluded narrative reviews without those characteristics as these are less likely to be replicable and are more prone to bias.
Scoping reviews and rapid reviews were eligible for inclusion in this overview if they met our pre-defined inclusion criteria noted above. We included reviews that addressed SARS-CoV-2 and other coronaviruses if they reported separate data regarding SARS-CoV-2.
Information sources
Nine databases were searched for eligible records published between December 1, 2019, and March 24, 2020: Cochrane Database of Systematic Reviews via Cochrane Library, PubMed, EMBASE, CINAHL (Cumulative Index to Nursing and Allied Health Literature), Web of Sciences, LILACS (Latin American and Caribbean Health Sciences Literature), PDQ-Evidence, WHO’s Global Research on Coronavirus Disease (COVID-19), and Epistemonikos.
The comprehensive search strategy for each database is provided in Additional file 1 and was designed and conducted in collaboration with an information specialist. All retrieved records were primarily processed in EndNote, where duplicates were removed, and records were then imported into the Covidence platform [ 23 ]. In addition to database searches, we screened reference lists of reviews included after screening records retrieved via databases.
Study selection
All searches, screening of titles and abstracts, and record selection, were performed independently by two investigators using the Covidence platform [ 23 ]. Articles deemed potentially eligible were retrieved for full-text screening carried out independently by two investigators. Discrepancies at all stages were resolved by consensus. During the screening, records published in languages other than English were translated by a native/fluent speaker.
Data collection process
We custom designed a data extraction table for this study, which was piloted by two authors independently. Data extraction was performed independently by two authors. Conflicts were resolved by consensus or by consulting a third researcher.
We extracted the following data: article identification data (authors’ name and journal of publication), search period, number of databases searched, population or settings considered, main results and outcomes observed, and number of participants. From Web of Science (Clarivate Analytics, Philadelphia, PA, USA), we extracted journal rank (quartile) and Journal Impact Factor (JIF).
We categorized the following as primary outcomes: all-cause mortality, need for and length of mechanical ventilation, length of hospitalization (in days), admission to intensive care unit (yes/no), and length of stay in the intensive care unit.
The following outcomes were categorized as exploratory: diagnostic methods used for detection of the virus, male to female ratio, clinical symptoms, pharmacological and non-pharmacological interventions, laboratory findings (full blood count, liver enzymes, C-reactive protein, d-dimer, albumin, lipid profile, serum electrolytes, blood vitamin levels, glucose levels, and any other important biomarkers), and radiological findings (using radiography, computed tomography, magnetic resonance imaging or ultrasound).
We also collected data on reporting guidelines and requirements for the publication of systematic reviews and meta-analyses from journal websites where included reviews were published.
Quality assessment in individual reviews
Two researchers independently assessed the reviews’ quality using the “A MeaSurement Tool to Assess Systematic Reviews 2 (AMSTAR 2)”. We acknowledge that the AMSTAR 2 was created as “a critical appraisal tool for systematic reviews that include randomized or non-randomized studies of healthcare interventions, or both” [ 24 ]. However, since AMSTAR 2 was designed for systematic reviews of intervention trials, and we included additional types of systematic reviews, we adjusted some AMSTAR 2 ratings and reported these in Additional file 2 .
Adherence to each item was rated as follows: yes, partial yes, no, or not applicable (such as when a meta-analysis was not conducted). The overall confidence in the results of the review is rated as “critically low”, “low”, “moderate” or “high”, according to the AMSTAR 2 guidance based on seven critical domains, which are items 2, 4, 7, 9, 11, 13, 15 as defined by AMSTAR 2 authors [ 24 ]. We reported our adherence ratings for transparency of our decision with accompanying explanations, for each item, in each included review.
One of the included systematic reviews was conducted by some members of this author team [ 25 ]. This review was initially assessed independently by two authors who were not co-authors of that review to prevent the risk of bias in assessing this study.
Synthesis of results
For data synthesis, we prepared a table summarizing each systematic review. Graphs illustrating the mortality rate and clinical symptoms were created. We then prepared a narrative summary of the methods, findings, study strengths, and limitations.
For analysis of the prevalence of clinical outcomes, we extracted data on the number of events and the total number of patients to perform proportional meta-analysis using RStudio© software, with the “meta” package (version 4.9–6), using the “metaprop” function for reviews that did not perform a meta-analysis, excluding case studies because of the absence of variance. For reviews that did not perform a meta-analysis, we presented pooled results of proportions with their respective confidence intervals (95%) by the inverse variance method with a random-effects model, using the DerSimonian-Laird estimator for τ 2 . We adjusted data using Freeman-Tukey double arcosen transformation. Confidence intervals were calculated using the Clopper-Pearson method for individual studies. We created forest plots using the RStudio© software, with the “metafor” package (version 2.1–0) and “forest” function.
Managing overlapping systematic reviews
Some of the included systematic reviews that address the same or similar research questions may include the same primary studies in overviews. Including such overlapping reviews may introduce bias when outcome data from the same primary study are included in the analyses of an overview multiple times. Thus, in summaries of evidence, multiple-counting of the same outcome data will give data from some primary studies too much influence [ 14 ]. In this overview, we did not exclude overlapping systematic reviews because, according to Cochrane’s guidance, it may be appropriate to include all relevant reviews’ results if the purpose of the overview is to present and describe the current body of evidence on a topic [ 14 ]. To avoid any bias in summary estimates associated with overlapping reviews, we generated forest plots showing data from individual systematic reviews, but the results were not pooled because some primary studies were included in multiple reviews.
Our search retrieved 1063 publications, of which 175 were duplicates. Most publications were excluded after the title and abstract analysis ( n = 860). Among the 28 studies selected for full-text screening, 10 were excluded for the reasons described in Additional file 3 , and 18 were included in the final analysis (Fig. 1 ) [ 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ]. Reference list screening did not retrieve any additional systematic reviews.

PRISMA flow diagram
Characteristics of included reviews
Summary features of 18 systematic reviews are presented in Table 1 . They were published in 14 different journals. Only four of these journals had specific requirements for systematic reviews (with or without meta-analysis): European Journal of Internal Medicine, Journal of Clinical Medicine, Ultrasound in Obstetrics and Gynecology, and Clinical Research in Cardiology . Two journals reported that they published only invited reviews ( Journal of Medical Virology and Clinica Chimica Acta ). Three systematic reviews in our study were published as letters; one was labeled as a scoping review and another as a rapid review (Table 2 ).
All reviews were published in English, in first quartile (Q1) journals, with JIF ranging from 1.692 to 6.062. One review was empty, meaning that its search did not identify any relevant studies; i.e., no primary studies were included [ 36 ]. The remaining 17 reviews included 269 unique studies; the majority ( N = 211; 78%) were included in only a single review included in our study (range: 1 to 12). Primary studies included in the reviews were published between December 2019 and March 18, 2020, and comprised case reports, case series, cohorts, and other observational studies. We found only one review that included randomized clinical trials [ 38 ]. In the included reviews, systematic literature searches were performed from 2019 (entire year) up to March 9, 2020. Ten systematic reviews included meta-analyses. The list of primary studies found in the included systematic reviews is shown in Additional file 4 , as well as the number of reviews in which each primary study was included.
Population and study designs
Most of the reviews analyzed data from patients with COVID-19 who developed pneumonia, acute respiratory distress syndrome (ARDS), or any other correlated complication. One review aimed to evaluate the effectiveness of using surgical masks on preventing transmission of the virus [ 36 ], one review was focused on pediatric patients [ 34 ], and one review investigated COVID-19 in pregnant women [ 37 ]. Most reviews assessed clinical symptoms, laboratory findings, or radiological results.
Systematic review findings
The summary of findings from individual reviews is shown in Table 2 . Overall, all-cause mortality ranged from 0.3 to 13.9% (Fig. 2 ).

A meta-analysis of the prevalence of mortality
Clinical symptoms
Seven reviews described the main clinical manifestations of COVID-19 [ 26 , 28 , 29 , 34 , 35 , 39 , 41 ]. Three of them provided only a narrative discussion of symptoms [ 26 , 34 , 35 ]. In the reviews that performed a statistical analysis of the incidence of different clinical symptoms, symptoms in patients with COVID-19 were (range values of point estimates): fever (82–95%), cough with or without sputum (58–72%), dyspnea (26–59%), myalgia or muscle fatigue (29–51%), sore throat (10–13%), headache (8–12%), gastrointestinal disorders, such as diarrhea, nausea or vomiting (5.0–9.0%), and others (including, in one study only: dizziness 12.1%) (Figs. 3 , 4 , 5 , 6 , 7 , 8 and 9 ). Three reviews assessed cough with and without sputum together; only one review assessed sputum production itself (28.5%).

A meta-analysis of the prevalence of fever

A meta-analysis of the prevalence of cough

A meta-analysis of the prevalence of dyspnea

A meta-analysis of the prevalence of fatigue or myalgia

A meta-analysis of the prevalence of headache

A meta-analysis of the prevalence of gastrointestinal disorders

A meta-analysis of the prevalence of sore throat
Diagnostic aspects
Three reviews described methodologies, protocols, and tools used for establishing the diagnosis of COVID-19 [ 26 , 34 , 38 ]. The use of respiratory swabs (nasal or pharyngeal) or blood specimens to assess the presence of SARS-CoV-2 nucleic acid using RT-PCR assays was the most commonly used diagnostic method mentioned in the included studies. These diagnostic tests have been widely used, but their precise sensitivity and specificity remain unknown. One review included a Chinese study with clinical diagnosis with no confirmation of SARS-CoV-2 infection (patients were diagnosed with COVID-19 if they presented with at least two symptoms suggestive of COVID-19, together with laboratory and chest radiography abnormalities) [ 34 ].
Therapeutic possibilities
Pharmacological and non-pharmacological interventions (supportive therapies) used in treating patients with COVID-19 were reported in five reviews [ 25 , 27 , 34 , 35 , 38 ]. Antivirals used empirically for COVID-19 treatment were reported in seven reviews [ 25 , 27 , 34 , 35 , 37 , 38 , 41 ]; most commonly used were protease inhibitors (lopinavir, ritonavir, darunavir), nucleoside reverse transcriptase inhibitor (tenofovir), nucleotide analogs (remdesivir, galidesivir, ganciclovir), and neuraminidase inhibitors (oseltamivir). Umifenovir, a membrane fusion inhibitor, was investigated in two studies [ 25 , 35 ]. Possible supportive interventions analyzed were different types of oxygen supplementation and breathing support (invasive or non-invasive ventilation) [ 25 ]. The use of antibiotics, both empirically and to treat secondary pneumonia, was reported in six studies [ 25 , 26 , 27 , 34 , 35 , 38 ]. One review specifically assessed evidence on the efficacy and safety of the anti-malaria drug chloroquine [ 27 ]. It identified 23 ongoing trials investigating the potential of chloroquine as a therapeutic option for COVID-19, but no verifiable clinical outcomes data. The use of mesenchymal stem cells, antifungals, and glucocorticoids were described in four reviews [ 25 , 34 , 35 , 38 ].
Laboratory and radiological findings
Of the 18 reviews included in this overview, eight analyzed laboratory parameters in patients with COVID-19 [ 25 , 29 , 30 , 32 , 33 , 34 , 35 , 39 ]; elevated C-reactive protein levels, associated with lymphocytopenia, elevated lactate dehydrogenase, as well as slightly elevated aspartate and alanine aminotransferase (AST, ALT) were commonly described in those eight reviews. Lippi et al. assessed cardiac troponin I (cTnI) [ 25 ], procalcitonin [ 32 ], and platelet count [ 33 ] in COVID-19 patients. Elevated levels of procalcitonin [ 32 ] and cTnI [ 30 ] were more likely to be associated with a severe disease course (requiring intensive care unit admission and intubation). Furthermore, thrombocytopenia was frequently observed in patients with complicated COVID-19 infections [ 33 ].
Chest imaging (chest radiography and/or computed tomography) features were assessed in six reviews, all of which described a frequent pattern of local or bilateral multilobar ground-glass opacity [ 25 , 34 , 35 , 39 , 40 , 41 ]. Those six reviews showed that septal thickening, bronchiectasis, pleural and cardiac effusions, halo signs, and pneumothorax were observed in patients suffering from COVID-19.
Quality of evidence in individual systematic reviews
Table 3 shows the detailed results of the quality assessment of 18 systematic reviews, including the assessment of individual items and summary assessment. A detailed explanation for each decision in each review is available in Additional file 5 .
Using AMSTAR 2 criteria, confidence in the results of all 18 reviews was rated as “critically low” (Table 3 ). Common methodological drawbacks were: omission of prospective protocol submission or publication; use of inappropriate search strategy: lack of independent and dual literature screening and data-extraction (or methodology unclear); absence of an explanation for heterogeneity among the studies included; lack of reasons for study exclusion (or rationale unclear).
Risk of bias assessment, based on a reported methodological tool, and quality of evidence appraisal, in line with the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) method, were reported only in one review [ 25 ]. Five reviews presented a table summarizing bias, using various risk of bias tools [ 25 , 29 , 39 , 40 , 41 ]. One review analyzed “study quality” [ 37 ]. One review mentioned the risk of bias assessment in the methodology but did not provide any related analysis [ 28 ].
This overview of systematic reviews analyzed the first 18 systematic reviews published after the onset of the COVID-19 pandemic, up to March 24, 2020, with primary studies involving more than 60,000 patients. Using AMSTAR-2, we judged that our confidence in all those reviews was “critically low”. Ten reviews included meta-analyses. The reviews presented data on clinical manifestations, laboratory and radiological findings, and interventions. We found no systematic reviews on the utility of diagnostic tests.
Symptoms were reported in seven reviews; most of the patients had a fever, cough, dyspnea, myalgia or muscle fatigue, and gastrointestinal disorders such as diarrhea, nausea, or vomiting. Olfactory dysfunction (anosmia or dysosmia) has been described in patients infected with COVID-19 [ 43 ]; however, this was not reported in any of the reviews included in this overview. During the SARS outbreak in 2002, there were reports of impairment of the sense of smell associated with the disease [ 44 , 45 ].
The reported mortality rates ranged from 0.3 to 14% in the included reviews. Mortality estimates are influenced by the transmissibility rate (basic reproduction number), availability of diagnostic tools, notification policies, asymptomatic presentations of the disease, resources for disease prevention and control, and treatment facilities; variability in the mortality rate fits the pattern of emerging infectious diseases [ 46 ]. Furthermore, the reported cases did not consider asymptomatic cases, mild cases where individuals have not sought medical treatment, and the fact that many countries had limited access to diagnostic tests or have implemented testing policies later than the others. Considering the lack of reviews assessing diagnostic testing (sensitivity, specificity, and predictive values of RT-PCT or immunoglobulin tests), and the preponderance of studies that assessed only symptomatic individuals, considerable imprecision around the calculated mortality rates existed in the early stage of the COVID-19 pandemic.
Few reviews included treatment data. Those reviews described studies considered to be at a very low level of evidence: usually small, retrospective studies with very heterogeneous populations. Seven reviews analyzed laboratory parameters; those reviews could have been useful for clinicians who attend patients suspected of COVID-19 in emergency services worldwide, such as assessing which patients need to be reassessed more frequently.
All systematic reviews scored poorly on the AMSTAR 2 critical appraisal tool for systematic reviews. Most of the original studies included in the reviews were case series and case reports, impacting the quality of evidence. Such evidence has major implications for clinical practice and the use of these reviews in evidence-based practice and policy. Clinicians, patients, and policymakers can only have the highest confidence in systematic review findings if high-quality systematic review methodologies are employed. The urgent need for information during a pandemic does not justify poor quality reporting.
We acknowledge that there are numerous challenges associated with analyzing COVID-19 data during a pandemic [ 47 ]. High-quality evidence syntheses are needed for decision-making, but each type of evidence syntheses is associated with its inherent challenges.
The creation of classic systematic reviews requires considerable time and effort; with massive research output, they quickly become outdated, and preparing updated versions also requires considerable time. A recent study showed that updates of non-Cochrane systematic reviews are published a median of 5 years after the publication of the previous version [ 48 ].
Authors may register a review and then abandon it [ 49 ], but the existence of a public record that is not updated may lead other authors to believe that the review is still ongoing. A quarter of Cochrane review protocols remains unpublished as completed systematic reviews 8 years after protocol publication [ 50 ].
Rapid reviews can be used to summarize the evidence, but they involve methodological sacrifices and simplifications to produce information promptly, with inconsistent methodological approaches [ 51 ]. However, rapid reviews are justified in times of public health emergencies, and even Cochrane has resorted to publishing rapid reviews in response to the COVID-19 crisis [ 52 ]. Rapid reviews were eligible for inclusion in this overview, but only one of the 18 reviews included in this study was labeled as a rapid review.
Ideally, COVID-19 evidence would be continually summarized in a series of high-quality living systematic reviews, types of evidence synthesis defined as “ a systematic review which is continually updated, incorporating relevant new evidence as it becomes available ” [ 53 ]. However, conducting living systematic reviews requires considerable resources, calling into question the sustainability of such evidence synthesis over long periods [ 54 ].
Research reports about COVID-19 will contribute to research waste if they are poorly designed, poorly reported, or simply not necessary. In principle, systematic reviews should help reduce research waste as they usually provide recommendations for further research that is needed or may advise that sufficient evidence exists on a particular topic [ 55 ]. However, systematic reviews can also contribute to growing research waste when they are not needed, or poorly conducted and reported. Our present study clearly shows that most of the systematic reviews that were published early on in the COVID-19 pandemic could be categorized as research waste, as our confidence in their results is critically low.
Our study has some limitations. One is that for AMSTAR 2 assessment we relied on information available in publications; we did not attempt to contact study authors for clarifications or additional data. In three reviews, the methodological quality appraisal was challenging because they were published as letters, or labeled as rapid communications. As a result, various details about their review process were not included, leading to AMSTAR 2 questions being answered as “not reported”, resulting in low confidence scores. Full manuscripts might have provided additional information that could have led to higher confidence in the results. In other words, low scores could reflect incomplete reporting, not necessarily low-quality review methods. To make their review available more rapidly and more concisely, the authors may have omitted methodological details. A general issue during a crisis is that speed and completeness must be balanced. However, maintaining high standards requires proper resourcing and commitment to ensure that the users of systematic reviews can have high confidence in the results.
Furthermore, we used adjusted AMSTAR 2 scoring, as the tool was designed for critical appraisal of reviews of interventions. Some reviews may have received lower scores than actually warranted in spite of these adjustments.
Another limitation of our study may be the inclusion of multiple overlapping reviews, as some included reviews included the same primary studies. According to the Cochrane Handbook, including overlapping reviews may be appropriate when the review’s aim is “ to present and describe the current body of systematic review evidence on a topic ” [ 12 ], which was our aim. To avoid bias with summarizing evidence from overlapping reviews, we presented the forest plots without summary estimates. The forest plots serve to inform readers about the effect sizes for outcomes that were reported in each review.
Several authors from this study have contributed to one of the reviews identified [ 25 ]. To reduce the risk of any bias, two authors who did not co-author the review in question initially assessed its quality and limitations.
Finally, we note that the systematic reviews included in our overview may have had issues that our analysis did not identify because we did not analyze their primary studies to verify the accuracy of the data and information they presented. We give two examples to substantiate this possibility. Lovato et al. wrote a commentary on the review of Sun et al. [ 41 ], in which they criticized the authors’ conclusion that sore throat is rare in COVID-19 patients [ 56 ]. Lovato et al. highlighted that multiple studies included in Sun et al. did not accurately describe participants’ clinical presentations, warning that only three studies clearly reported data on sore throat [ 56 ].
In another example, Leung [ 57 ] warned about the review of Li, L.Q. et al. [ 29 ]: “ it is possible that this statistic was computed using overlapped samples, therefore some patients were double counted ”. Li et al. responded to Leung that it is uncertain whether the data overlapped, as they used data from published articles and did not have access to the original data; they also reported that they requested original data and that they plan to re-do their analyses once they receive them; they also urged readers to treat the data with caution [ 58 ]. This points to the evolving nature of evidence during a crisis.
Our study’s strength is that this overview adds to the current knowledge by providing a comprehensive summary of all the evidence synthesis about COVID-19 available early after the onset of the pandemic. This overview followed strict methodological criteria, including a comprehensive and sensitive search strategy and a standard tool for methodological appraisal of systematic reviews.
In conclusion, in this overview of systematic reviews, we analyzed evidence from the first 18 systematic reviews that were published after the emergence of COVID-19. However, confidence in the results of all the reviews was “critically low”. Thus, systematic reviews that were published early on in the pandemic could be categorized as research waste. Even during public health emergencies, studies and systematic reviews should adhere to established methodological standards to provide patients, clinicians, and decision-makers trustworthy evidence.
Availability of data and materials
All data collected and analyzed within this study are available from the corresponding author on reasonable request.
World Health Organization. Timeline - COVID-19: Available at: https://www.who.int/news/item/29-06-2020-covidtimeline . Accessed 1 June 2021.
COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Available at: https://coronavirus.jhu.edu/map.html . Accessed 1 June 2021.
Anzai A, Kobayashi T, Linton NM, Kinoshita R, Hayashi K, Suzuki A, et al. Assessing the Impact of Reduced Travel on Exportation Dynamics of Novel Coronavirus Infection (COVID-19). J Clin Med. 2020;9(2):601.
Chinazzi M, Davis JT, Ajelli M, Gioannini C, Litvinova M, Merler S, et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368(6489):395–400. https://doi.org/10.1126/science.aba9757 .
Article CAS PubMed PubMed Central Google Scholar
Fidahic M, Nujic D, Runjic R, Civljak M, Markotic F, Lovric Makaric Z, et al. Research methodology and characteristics of journal articles with original data, preprint articles and registered clinical trial protocols about COVID-19. BMC Med Res Methodol. 2020;20(1):161. https://doi.org/10.1186/s12874-020-01047-2 .
EPPI Centre . COVID-19: a living systematic map of the evidence. Available at: http://eppi.ioe.ac.uk/cms/Projects/DepartmentofHealthandSocialCare/Publishedreviews/COVID-19Livingsystematicmapoftheevidence/tabid/3765/Default.aspx . Accessed 1 June 2021.
NCBI SARS-CoV-2 Resources. Available at: https://www.ncbi.nlm.nih.gov/sars-cov-2/ . Accessed 1 June 2021.
Gustot T. Quality and reproducibility during the COVID-19 pandemic. JHEP Rep. 2020;2(4):100141. https://doi.org/10.1016/j.jhepr.2020.100141 .
Article PubMed PubMed Central Google Scholar
Kodvanj, I., et al., Publishing of COVID-19 Preprints in Peer-reviewed Journals, Preprinting Trends, Public Discussion and Quality Issues. Preprint article. bioRxiv 2020.11.23.394577; doi: https://doi.org/10.1101/2020.11.23.394577 .
Dobler CC. Poor quality research and clinical practice during COVID-19. Breathe (Sheff). 2020;16(2):200112. https://doi.org/10.1183/20734735.0112-2020 .
Article Google Scholar
Bastian H, Glasziou P, Chalmers I. Seventy-five trials and eleven systematic reviews a day: how will we ever keep up? PLoS Med. 2010;7(9):e1000326. https://doi.org/10.1371/journal.pmed.1000326 .
Lunny C, Brennan SE, McDonald S, McKenzie JE. Toward a comprehensive evidence map of overview of systematic review methods: paper 1-purpose, eligibility, search and data extraction. Syst Rev. 2017;6(1):231. https://doi.org/10.1186/s13643-017-0617-1 .
Pollock M, Fernandes RM, Becker LA, Pieper D, Hartling L. Chapter V: Overviews of Reviews. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane. 2020. Available from www.training.cochrane.org/handbook .
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions version 6.1 (updated September 2020). Cochrane. 2020; Available from www.training.cochrane.org/handbook .
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. The impact of different inclusion decisions on the comprehensiveness and complexity of overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):18. https://doi.org/10.1186/s13643-018-0914-3 .
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. A decision tool to help researchers make decisions about including systematic reviews in overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):29. https://doi.org/10.1186/s13643-018-0768-8 .
Hunt H, Pollock A, Campbell P, Estcourt L, Brunton G. An introduction to overviews of reviews: planning a relevant research question and objective for an overview. Syst Rev. 2018;7(1):39. https://doi.org/10.1186/s13643-018-0695-8 .
Pollock M, Fernandes RM, Pieper D, Tricco AC, Gates M, Gates A, et al. Preferred reporting items for overviews of reviews (PRIOR): a protocol for development of a reporting guideline for overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):335. https://doi.org/10.1186/s13643-019-1252-9 .
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Open Med. 2009;3(3):e123–30.
Krnic Martinic M, Pieper D, Glatt A, Puljak L. Definition of a systematic review used in overviews of systematic reviews, meta-epidemiological studies and textbooks. BMC Med Res Methodol. 2019;19(1):203. https://doi.org/10.1186/s12874-019-0855-0 .
Puljak L. If there is only one author or only one database was searched, a study should not be called a systematic review. J Clin Epidemiol. 2017;91:4–5. https://doi.org/10.1016/j.jclinepi.2017.08.002 .
Article PubMed Google Scholar
Gates M, Gates A, Guitard S, Pollock M, Hartling L. Guidance for overviews of reviews continues to accumulate, but important challenges remain: a scoping review. Syst Rev. 2020;9(1):254. https://doi.org/10.1186/s13643-020-01509-0 .
Covidence - systematic review software. Available at: https://www.covidence.org/ . Accessed 1 June 2021.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Borges do Nascimento IJ, et al. Novel Coronavirus Infection (COVID-19) in Humans: A Scoping Review and Meta-Analysis. J Clin Med. 2020;9(4):941.
Article PubMed Central Google Scholar
Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX, Wang QZ, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9(1):29. https://doi.org/10.1186/s40249-020-00646-x .
Cortegiani A, Ingoglia G, Ippolito M, Giarratano A, Einav S. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care. 2020;57:279–83. https://doi.org/10.1016/j.jcrc.2020.03.005 .
Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109(5):531–8. https://doi.org/10.1007/s00392-020-01626-9 .
Article CAS PubMed Google Scholar
Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(6):577–83. https://doi.org/10.1002/jmv.25757 .
Lippi G, Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): evidence from a meta-analysis. Prog Cardiovasc Dis. 2020;63(3):390–1. https://doi.org/10.1016/j.pcad.2020.03.001 .
Lippi G, Henry BM. Active smoking is not associated with severity of coronavirus disease 2019 (COVID-19). Eur J Intern Med. 2020;75:107–8. https://doi.org/10.1016/j.ejim.2020.03.014 .
Lippi G, Plebani M. Procalcitonin in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chim Acta. 2020;505:190–1. https://doi.org/10.1016/j.cca.2020.03.004 .
Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta. 2020;506:145–8. https://doi.org/10.1016/j.cca.2020.03.022 .
Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109(6):1088–95. https://doi.org/10.1111/apa.15270 .
Lupia T, Scabini S, Mornese Pinna S, di Perri G, de Rosa FG, Corcione S. 2019 novel coronavirus (2019-nCoV) outbreak: a new challenge. J Glob Antimicrob Resist. 2020;21:22–7. https://doi.org/10.1016/j.jgar.2020.02.021 .
Marasinghe, K.M., A systematic review investigating the effectiveness of face mask use in limiting the spread of COVID-19 among medically not diagnosed individuals: shedding light on current recommendations provided to individuals not medically diagnosed with COVID-19. Research Square. Preprint article. doi : https://doi.org/10.21203/rs.3.rs-16701/v1 . 2020 .
Mullins E, Evans D, Viner RM, O’Brien P, Morris E. Coronavirus in pregnancy and delivery: rapid review. Ultrasound Obstet Gynecol. 2020;55(5):586–92. https://doi.org/10.1002/uog.22014 .
Pang J, Wang MX, Ang IYH, Tan SHX, Lewis RF, Chen JIP, et al. Potential Rapid Diagnostics, Vaccine and Therapeutics for 2019 Novel coronavirus (2019-nCoV): a systematic review. J Clin Med. 2020;9(3):623.
Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623. https://doi.org/10.1016/j.tmaid.2020.101623 .
Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020;215(1):87–93. https://doi.org/10.2214/AJR.20.23034 .
Sun P, Qie S, Liu Z, Ren J, Li K, Xi J. Clinical characteristics of hospitalized patients with SARS-CoV-2 infection: a single arm meta-analysis. J Med Virol. 2020;92(6):612–7. https://doi.org/10.1002/jmv.25735 .
Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–5. https://doi.org/10.1016/j.ijid.2020.03.017 .
Bassetti M, Vena A, Giacobbe DR. The novel Chinese coronavirus (2019-nCoV) infections: challenges for fighting the storm. Eur J Clin Investig. 2020;50(3):e13209. https://doi.org/10.1111/eci.13209 .
Article CAS Google Scholar
Hwang CS. Olfactory neuropathy in severe acute respiratory syndrome: report of a case. Acta Neurol Taiwanica. 2006;15(1):26–8.
Google Scholar
Suzuki M, Saito K, Min WP, Vladau C, Toida K, Itoh H, et al. Identification of viruses in patients with postviral olfactory dysfunction. Laryngoscope. 2007;117(2):272–7. https://doi.org/10.1097/01.mlg.0000249922.37381.1e .
Rajgor DD, Lee MH, Archuleta S, Bagdasarian N, Quek SC. The many estimates of the COVID-19 case fatality rate. Lancet Infect Dis. 2020;20(7):776–7. https://doi.org/10.1016/S1473-3099(20)30244-9 .
Wolkewitz M, Puljak L. Methodological challenges of analysing COVID-19 data during the pandemic. BMC Med Res Methodol. 2020;20(1):81. https://doi.org/10.1186/s12874-020-00972-6 .
Rombey T, Lochner V, Puljak L, Könsgen N, Mathes T, Pieper D. Epidemiology and reporting characteristics of non-Cochrane updates of systematic reviews: a cross-sectional study. Res Synth Methods. 2020;11(3):471–83. https://doi.org/10.1002/jrsm.1409 .
Runjic E, Rombey T, Pieper D, Puljak L. Half of systematic reviews about pain registered in PROSPERO were not published and the majority had inaccurate status. J Clin Epidemiol. 2019;116:114–21. https://doi.org/10.1016/j.jclinepi.2019.08.010 .
Runjic E, Behmen D, Pieper D, Mathes T, Tricco AC, Moher D, et al. Following Cochrane review protocols to completion 10 years later: a retrospective cohort study and author survey. J Clin Epidemiol. 2019;111:41–8. https://doi.org/10.1016/j.jclinepi.2019.03.006 .
Tricco AC, Antony J, Zarin W, Strifler L, Ghassemi M, Ivory J, et al. A scoping review of rapid review methods. BMC Med. 2015;13(1):224. https://doi.org/10.1186/s12916-015-0465-6 .
COVID-19 Rapid Reviews: Cochrane’s response so far. Available at: https://training.cochrane.org/resource/covid-19-rapid-reviews-cochrane-response-so-far . Accessed 1 June 2021.
Cochrane. Living systematic reviews. Available at: https://community.cochrane.org/review-production/production-resources/living-systematic-reviews . Accessed 1 June 2021.
Millard T, Synnot A, Elliott J, Green S, McDonald S, Turner T. Feasibility and acceptability of living systematic reviews: results from a mixed-methods evaluation. Syst Rev. 2019;8(1):325. https://doi.org/10.1186/s13643-019-1248-5 .
Babic A, Poklepovic Pericic T, Pieper D, Puljak L. How to decide whether a systematic review is stable and not in need of updating: analysis of Cochrane reviews. Res Synth Methods. 2020;11(6):884–90. https://doi.org/10.1002/jrsm.1451 .
Lovato A, Rossettini G, de Filippis C. Sore throat in COVID-19: comment on “clinical characteristics of hospitalized patients with SARS-CoV-2 infection: a single arm meta-analysis”. J Med Virol. 2020;92(7):714–5. https://doi.org/10.1002/jmv.25815 .
Leung C. Comment on Li et al: COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(9):1431–2. https://doi.org/10.1002/jmv.25912 .
Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. Response to Char’s comment: comment on Li et al: COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(9):1433. https://doi.org/10.1002/jmv.25924 .
Download references
Acknowledgments
We thank Catherine Henderson DPhil from Swanscoe Communications for pro bono medical writing and editing support. We acknowledge support from the Covidence Team, specifically Anneliese Arno. We thank the whole International Network of Coronavirus Disease 2019 (InterNetCOVID-19) for their commitment and involvement. Members of the InterNetCOVID-19 are listed in Additional file 6 . We thank Pavel Cerny and Roger Crosthwaite for guiding the team supervisor (IJBN) on human resources management.
This research received no external funding.
Author information
Authors and affiliations.
University Hospital and School of Medicine, Universidade Federal de Minas Gerais, Belo Horizonte, Minas Gerais, Brazil
Israel Júnior Borges do Nascimento & Milena Soriano Marcolino
Medical College of Wisconsin, Milwaukee, WI, USA
Israel Júnior Borges do Nascimento
Helene Fuld Health Trust National Institute for Evidence-based Practice in Nursing and Healthcare, College of Nursing, The Ohio State University, Columbus, OH, USA
Dónal P. O’Mathúna
School of Nursing, Psychotherapy and Community Health, Dublin City University, Dublin, Ireland
Department of Anesthesiology, Intensive Care and Pain Medicine, University of Münster, Münster, Germany
Thilo Caspar von Groote
Department of Sport and Health Science, Technische Universität München, Munich, Germany
Hebatullah Mohamed Abdulazeem
School of Health Sciences, Faculty of Health and Medicine, The University of Newcastle, Callaghan, Australia
Ishanka Weerasekara
Department of Physiotherapy, Faculty of Allied Health Sciences, University of Peradeniya, Peradeniya, Sri Lanka
Cochrane Croatia, University of Split, School of Medicine, Split, Croatia
Ana Marusic, Irena Zakarija-Grkovic & Tina Poklepovic Pericic
Center for Evidence-Based Medicine and Health Care, Catholic University of Croatia, Ilica 242, 10000, Zagreb, Croatia
Livia Puljak
Cochrane Brazil, Evidence-Based Health Program, Universidade Federal de São Paulo, São Paulo, Brazil
Vinicius Tassoni Civile & Alvaro Nagib Atallah
Yorkville University, Fredericton, New Brunswick, Canada
Santino Filoso
Laboratory for Industrial and Applied Mathematics (LIAM), Department of Mathematics and Statistics, York University, Toronto, Ontario, Canada
Nicola Luigi Bragazzi
You can also search for this author in PubMed Google Scholar
Contributions
IJBN conceived the research idea and worked as a project coordinator. DPOM, TCVG, HMA, IW, AM, LP, VTC, IZG, TPP, ANA, SF, NLB and MSM were involved in data curation, formal analysis, investigation, methodology, and initial draft writing. All authors revised the manuscript critically for the content. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Livia Puljak .
Ethics declarations
Ethics approval and consent to participate.
Not required as data was based on published studies.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: appendix 1..
Search strategies used in the study.
Additional file 2: Appendix 2.
Adjusted scoring of AMSTAR 2 used in this study for systematic reviews of studies that did not analyze interventions.
Additional file 3: Appendix 3.
List of excluded studies, with reasons.
Additional file 4: Appendix 4.
Table of overlapping studies, containing the list of primary studies included, their visual overlap in individual systematic reviews, and the number in how many reviews each primary study was included.
Additional file 5: Appendix 5.
A detailed explanation of AMSTAR scoring for each item in each review.
Additional file 6: Appendix 6.
List of members and affiliates of International Network of Coronavirus Disease 2019 (InterNetCOVID-19).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Borges do Nascimento, I.J., O’Mathúna, D.P., von Groote, T.C. et al. Coronavirus disease (COVID-19) pandemic: an overview of systematic reviews. BMC Infect Dis 21 , 525 (2021). https://doi.org/10.1186/s12879-021-06214-4
Download citation
Received : 12 April 2020
Accepted : 19 May 2021
Published : 04 June 2021
DOI : https://doi.org/10.1186/s12879-021-06214-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Coronavirus
- Evidence-based medicine
- Infectious diseases
BMC Infectious Diseases
ISSN: 1471-2334
- General enquiries: [email protected]
EDITORIAL article
Editorial: coronavirus disease (covid-19): the impact and role of mass media during the pandemic.

- 1 Department of Social and Organizational Psychology, Iscte-University Institute of Lisbon, CIS-IUL, Lisbon, Portugal
- 2 Department of Psychology and Social Work, Mid Sweden University, Östersund, Sweden
- 3 Department of Psychiatry and Psychotherapy, Medical School and University Hospital, Eberhard Karls University of Tübingen, Tübingen, Germany
Editorial on the Research Topic Coronavirus Disease (COVID-19): The Impact and Role of Mass Media During the Pandemic
The outbreak of the coronavirus disease 2019 (COVID-19) has created a global health crisis that had a deep impact on the way we perceive our world and our everyday lives. Not only has the rate of contagion and patterns of transmission threatened our sense of agency, but the safety measures to contain the spread of the virus also required social and physical distancing, preventing us from finding solace in the company of others. Within this context, we launched our Research Topic on March 27th, 2020, and invited researchers to address the Impact and Role of Mass Media During the Pandemic on our lives at individual and social levels.
Despite all the hardships, disruption, and uncertainty brought by the pandemic, we received diverse and insightful manuscript proposals. Frontiers in Psychology published 15 articles, involving 61 authors from 8 countries, which were included in distinct specialized sections, including Health Psychology, Personality and Social Psychology, Emotion Science, and Organizational Psychology. Despite the diversity of this collective endeavor, the contributions fall into four areas of research: (1) the use of media in public health communication; (2) the diffusion of false information; (3) the compliance with the health recommendations; and (4) how media use relates to mental health and well-being.
A first line of research includes contributions examining the use of media in public health communication. Drawing on media messages used in previous health crises, such as Ebola and Zika, Hauer and Sood describe how health organizations use media. They offer a set of recommendations for COVID-19 related media messages, including the importance of message framing, interactive public forums with up-to-date information, and an honest communication about what is known and unknown about the pandemic and the virus. Following a content analysis approach, Parvin et al. studied the representations of COVID-19 in the opinion section of five Asian e-newspapers. The authors identified eight main issues (health and drugs, preparedness and awareness, social welfare and humanity, governance and institutions, the environment and wildlife, politics, innovation and technology, and the economy) and examined how e-newspapers from these countries attributed different weights to these issues and how this relates to the countries' cultural specificity. Raccanello et al. show how the internet can be a platform to disseminate a public campaign devised to inform adults about coping strategies that could help children and teenagers deal with the challenges of the pandemic. The authors examined the dissemination of the program through the analysis of website traffic, showing that in the 40 days following publication, the website reached 6,090 visits.
A second related line of research that drew the concern of researchers was the diffusion of false information about COVID-19 through the media. Lobato et al. examined the role of distinct individual differences (political orientation, social dominance orientation, traditionalism, conspiracy ideation, attitudes about science) on the willingness to share misinformation about COVID-19 over social media. The misinformation topics varied between the severity and spread of COVID-19, treatment and prevention, conspiracy theories, and miscellaneous unverifiable claims. Their results from 296 adult participants (Mage = 36.23; 117 women) suggest two different profiles. One indicating that those reporting more liberal positions and lower social dominance were less willing to share conspiracy misinformation. The other profile indicated that participants scoring high on social dominance and low in traditionalism were more willing to share both conspiracy and other miscellaneous claims, but less willing to share misinformation about the severity and spread of COVID-19. Their findings can have relevant contributions for the identification of specific individual profiles related to the widespread of distinct types of misinformation. Dhanani and Franz examined a sample of 1,141 adults (Mage = 44.66; 46.9% female, 74.7% White ethnic identity) living in the United States in March 2020. The authors examined how media consumption and information source were related to knowledge about COVID-19, the endorsement of misinformation about COVID-19, and prejudice toward Asian Americans. Higher levels of trust in informational sources such as public health organizations (e.g., Center for Disease Control) was associated with greater knowledge, lower endorsement of misinformation, and less prejudice toward Asian Americans. Media source was associated with distinct levels of knowledge, willingness to endorsement misinformation and prejudice toward American Asians, with social media use (e.g., Twitter, Facebook) being related with a lower knowledge about COVID-19, higher endorsement of misinformation, and stronger prejudice toward Asian Americans.
A third line of research addressed the factors that could contribute to compliance with the health recommendations to avoid the spread of the disease. Vai et al. studied early pre-lockdown risk perceptions about COVID-19 and the trust in media sources among 2,223 Italians (Mage = 36.4, 69.2% female). They found that the perceived usefulness of the containment measures (e.g., social distancing) was related to threat perception and efficacy beliefs. Lower threat perception was associated with less perception of utility of the containment measures. Although most participants considered themselves and others capable of taking preventive measures, they saw the measures as generally ineffective. Participants acknowledged using the internet as their main source of information and considered health organizations' websites as the most trustworthy source. Albeit frequently used, social media was in general considered an unreliable source of information. Tomczyk et al. studied knowledge about preventive behaviors, risk perception, stigmatizing attitudes (support for discrimination and blame), and sociodemographic data (e.g., age, gender, country of origin, education level, region, persons per household) as predictors of compliance with the behavioral recommendations among 157 Germans, (age range: 18–77 years, 80% female). Low compliance was associated with male gender, younger age, and lower public stigma. Regarding stigmatizing attitudes, the authors only found a relation between support for discrimination (i.e., support for compulsory measures) and higher intention to comply with recommendations. Mahmood et al. studied the relation between social media use, risk perception, preventive behaviors, and self-efficacy in a sample of 310 Pakistani adults (54.2% female). The authors found social media use to be positively related to self-efficacy and perceived threat, which were both positively related to preventive behaviors (e.g., hand hygiene, social distancing). Information credibility was also related to compliance with health recommendations. Lep et al. examined the relationship between information source perceived credibility and trust, and participants' levels of self-protective behavior among 1,718 Slovenians (age range: 18–81 years, 81.7% female). The authors found that scientists, general practitioners (family doctors), and the National Institute of Public Health were perceived as the more credible source of information, while social media and government officials received the lowest ratings. Perceived information credibility was found to be associated with lower levels of negative emotional responses (e.g., nervousness, helplessness) and a higher level of observance of self-protective measures (e.g., hand washing). Siebenhaar et al. also studied the link between compliance, distress by information, and information avoidance. They examined the online survey responses of 1,059 adults living in Germany (Mage = 39.53, 79.4% female). Their results suggested that distress by information could lead to higher compliance with preventive measures. Distress by information was also associated with higher information avoidance, which in turn is related to less compliance. Gantiva et al. studied the effectiveness of different messages regarding the intentions toward self-care behaviors, perceived efficacy to motivate self-care behaviors in others, perceived risk, and perceived message strength, in a sample of 319 Colombians (age range: 18–60 years, 69.9% female). Their experiment included the manipulation of message framing (gain vs. loss) and message content (economy vs. health). Participants judged gain-frame health related messages to be stronger and more effective in changing self-behavior, whereas loss-framed health messages resulted in increased perceived risk. Rahn et al. offer a comparative view of compliance and risk perception, examining three hazard types: COVID-19 pandemic, violent acts, and severe weather. With a sample of 403 Germans (age range: 18–89 years, 72% female), they studied how age, gender, previous hazard experience and different components of risk appraisal (perceived severity, anticipated negative emotions, anticipatory worry, and risk perception) were related to the intention to comply with behavioral recommendations. They found that higher age predicted compliance with health recommendations to prevent COVID-19, anticipatory worry predicted compliance with warning messages regarding violent acts, and women complied more often with severe weather recommendations than men.
A fourth line of research examined media use, mental health and well-being during the COVID-19 pandemic. Gabbiadini et al. addressed the use of digital technology (e.g., voice/video calls, online games, watching movies in party mode) to stay connected with others during lockdown. Participants, 465 Italians (age range: 18–73 years, 348 female), reported more perceived social support associated with the use of these digital technologies, which in turn was associated with fewer feelings of loneliness, boredom, anger, and higher sense of belongingness. Muñiz-Velázquez et al. compared the media habits of 249 Spanish adults (Mage = 42.06, 53.8% female) before and during confinement. They compared the type of media consumed (e.g., watching TV series, listening to radio, watching news) and found the increased consumption of TV and social networking sites during confinement to be negatively associated with reported level of happiness. People who reported higher levels of well-being also reported watching less TV and less use of social networking sites. Majeed et al. , on the other hand, examined the relation between problematic social media use, fear of COVID-19, depression, and mindfulness. Their study, involving 267 Pakistani adults (90 female), suggested trait mindfulness had a buffer effect, reducing the impact of problematic media use and fear of COVID-19 on depression.
Taken together, these findings highlight how using different frames for mass media gives a more expansive view of its positive and negative roles, but also showcase the major concerns in the context of a pandemic crisis. As limitations we highlight the use of cross-sectional designs in most studies, not allowing to establish true inferences of causal relationships. The outcome of some studies may also be limited by the unbalanced number of female and male participants, by the non-probability sampling method used, and by the restricted time frame in which the research occurred. Nevertheless, we are confident that all the selected studies in our Research Topic bring important and enduring contributions to the understanding of how media, individual differences, and social factors intertwine to shape our lives, which can also be useful to guide public policies during these challenging times.
Author Contributions
PA: conceptualization, writing the original draft, funding acquisition, writing—review, and editing. FE: conceptualization, writing—review, and editing. MP: writing—review and editing. NP: conceptualization, writing the original draft, writing—review, and editing. All authors approved the submitted version.
PA and NP received partial support to work on this Research Topic through Fundação para a Ciência e Tecnologia (FCT) with reference to the project PTDC/CCI-INF/29234/2017. MP contribution was supported by the German Research Foundation (DFG, PA847/22-1 and PA847/25-1). The authors are independent of the funders.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to express our gratitude to all the authors who proposed their work, all the researchers who reviewed the submissions to this Research Topic, and to Rob Richards for proofreading the Editorial manuscript.
Keywords: COVID-19, coronavirus disease, mass media, health communication, prevention, intervention, social behavioral changes
Citation: Arriaga P, Esteves F, Pavlova MA and Piçarra N (2021) Editorial: Coronavirus Disease (COVID-19): The Impact and Role of Mass Media During the Pandemic. Front. Psychol. 12:729238. doi: 10.3389/fpsyg.2021.729238
Received: 22 June 2021; Accepted: 30 July 2021; Published: 23 August 2021.
Edited and reviewed by: Eduard Brandstätter , Johannes Kepler University of Linz, Austria
Copyright © 2021 Arriaga, Esteves, Pavlova and Piçarra. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Patrícia Arriaga, patricia.arriaga@iscte-iul.pt
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Collection 29 March 2022
2021 Top 25 COVID-19 Articles
The 25 most downloaded Nature Communications articles* on COVID-19 published in 2021 illustrate the collaborative efforts of the international community to combat the ongoing pandemic. These papers highlight valuable research into the biology of coronavirus infection, its detection, treatment as well as into vaccine development and the epidemiology of the disease.
Browse all Top 25 subject area collections here .
*Data obtained from SN Insights (based on Digital Science's Dimensions) and normalised to account for articles published later in the year.
Research highlights
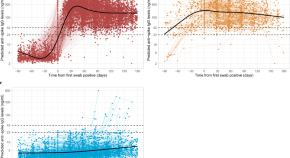
Anti-spike antibody response to natural SARS-CoV-2 infection in the general population
Most people who are infected with SARS-CoV-2 seroconvert within a few weeks, but the determinants and duration of the antibody response are not known. Here, the authors characterise these features of the immune response using data from a large representative community sample of the UK population.
- Philippa C. Matthews
- the COVID-19 Infection Survey team
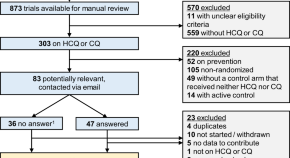
Mortality outcomes with hydroxychloroquine and chloroquine in COVID-19 from an international collaborative meta-analysis of randomized trials
Hydroxychloroquine and chloroquine have been investigated as a potential treatment for Covid-19 in several clinical trials. Here the authors report a meta-analysis of published and unpublished trials, and show that treatment with hydroxychloroquine for patients with Covid-19 was associated with increased mortality, and there was no benefit from chloroquine.
- Cathrine Axfors
- Andreas M. Schmitt
- Lars G. Hemkens
Malignant cerebral infarction after ChAdOx1 nCov-19 vaccination: a catastrophic variant of vaccine-induced immune thrombotic thrombocytopenia
Vaccination is an effective strategy in suppressing COVID-19 pandemic, but rare adverse effects have been reported, including cerebral venous thrombosis. Here the authors report two cases of middle cerebral artery infarct within 9-10 days following ChAdOx1 nCov-19 vaccination that also manifest pulmonary and portal vein thrombosis.
- M. De Michele
- M. Iacobucci
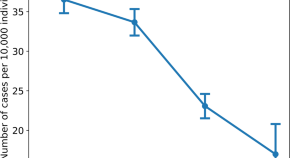
Correlation of SARS-CoV-2-breakthrough infections to time-from-vaccine
The duration of effectiveness of SARS-CoV-2 vaccination is not yet known. Here, the authors present preliminary evidence of BNT162b2 vaccine waning across all age groups above 16, with a higher incidence of infection in people who received their second dose early in 2021 compared to later in the year.
- Barak Mizrahi
- Tal Patalon

COVID-19 mRNA vaccine induced antibody responses against three SARS-CoV-2 variants
Emerging SARS-CoV-2 variants contain mutations in the spike protein that may affect vaccine efficacy. Here, Jalkanen et al . show, using sera from 180 BNT162b2-vaccinated health care workers, that neutralization of SARS-CoV2 variant B.1.1.7 is not affected, while neutralization of B.1.351 variant is five-fold reduced.
- Pinja Jalkanen
- Pekka Kolehmainen
- Ilkka Julkunen

Exposure to SARS-CoV-2 generates T-cell memory in the absence of a detectable viral infection
T cells compose a critical component of the immune response to coronavirus infection with SARS-CoV-2. Here the authors characterise the T cell response to SARS CoV-2 in patients and their close contacts, and show the presence of SARS-CoV-2 specific T cells in the absence of detectable virus infection.
- Zhongfang Wang
- Xiaoyun Yang
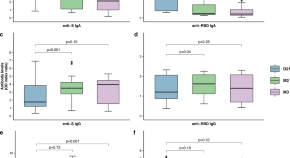
Rapid decline of neutralizing antibodies against SARS-CoV-2 among infected healthcare workers
The humoral immune response to SARS-CoV-2 infection is not yet fully understood. Here, Marot et al. monitor the longitudinal profile and neutralizing activity of IgG, IgA, and IgM among 26 healthcare workers and provide evidence for a short-lasting humoral immune protection due to a decrease of neutralizing antibody titers within 3 months.
- Stéphane Marot
- Isabelle Malet
- Anne-Geneviève Marcelin
Efficacy and tolerability of bevacizumab in patients with severe Covid-19
In this single-arm clinical trial, the authors show that treatment of COVID-19 patients with bevacizumab, an anti-vascular endothelial growth factor drug, can improve PaO 2 /FiO 2 ratios and oxygen-support status. Relative to an external control group, bevacizumab shows clinical efficacy by improving oxygenation.
- Jiaojiao Pang
Evidence for SARS-CoV-2 related coronaviruses circulating in bats and pangolins in Southeast Asia
A bat origin for SARS-CoV-2 has been proposed. Here, by sampling wild Rhinolophus acuminatus bats from Thailand, the authors identified a SARS-CoV-2-related coronavirus (SC2r-CoV), designated as RacCS203, with 91.5% genome similarity to SARS-CoV-2, and show that sera obtained from bats and Malayan pangolin neutralize SARS-CoV-2.
- Supaporn Wacharapluesadee
- Chee Wah Tan
- Lin-Fa Wang
SARS-CoV-2 gene content and COVID-19 mutation impact by comparing 44 Sarbecovirus genomes
The SARS-CoV-2 gene set remains unresolved, hindering dissection of COVID-19 biology. Comparing 44 Sarbecovirus genomes provides a high-confidence protein-coding gene set. The study characterizes protein-level and nucleotide-level evolutionary constraints, and prioritizes functional mutations from the ongoing COVID-19 pandemic.
- Irwin Jungreis
- Rachel Sealfon
- Manolis Kellis
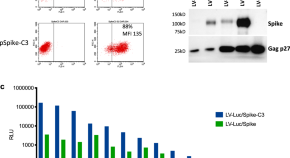
Neutralizing antibody responses to SARS-CoV-2 in symptomatic COVID-19 is persistent and critical for survival
Antibody responses are critical for protection from developing severe COVID-19 following SARS-CoV-2 infection. Here the authors show that antibody responses against SARS-CoV-2 spike protein correlate with neutralizing capacity and protection, are not affected by heterologous boosting of influenza or common cold immunity, and can last up to 8 months.
- Stefania Dispinseri
- Massimiliano Secchi
- Gabriella Scarlatti

New-onset IgG autoantibodies in hospitalized patients with COVID-19
Infection with SARS-CoV2 and the development of Coronavirus disease 2019 (COVID-19) has been linked to induction of autoimmunity and autoantibody production. Here the authors characterise the new-onset IgG autoantibody response in hospitalised patients with COVID-19 which they correlate to the magnitude of the SARS-CoV2 response.
- Sarah Esther Chang
- Paul J. Utz
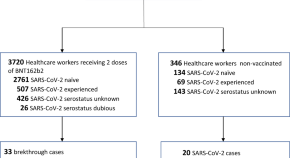
SARS-CoV-2 vaccine breakthrough infections with the alpha variant are asymptomatic or mildly symptomatic among health care workers
Several COVID-19 vaccines have shown good efficacy in clinical trials. Here, the authors provide real world effectiveness data in a group of BNT162b2 vaccinated health care workers and find that breakthrough infections are asymptomatic or mild.
- Francesca Rovida
- Irene Cassaniti
- Fausto Baldanti

Duration and key determinants of infectious virus shedding in hospitalized patients with coronavirus disease-2019 (COVID-19)
Duration of infectious SARS-CoV-2 shedding is an important measure for improved disease control. Here, the authors use virus cultures of respiratory tract samples from COVID-19 patients and observe a median shedding duration of 8 days and a drop below 5% after 15,2 days post onset of symptoms.
- Jeroen J. A. van Kampen
- David A. M. C. van de Vijver
- Annemiek A. van der Eijk
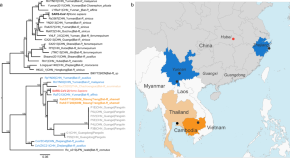
A novel SARS-CoV-2 related coronavirus in bats from Cambodia
In this study, Delaune et al., isolate and characterise a SARS-CoV-2-related coronavirus from two bats sampled in Cambodia. Their findings suggest that the geographic distribution of SARS-CoV-2-related viruses is wider than previously reported.
- Deborah Delaune
- Veasna Duong
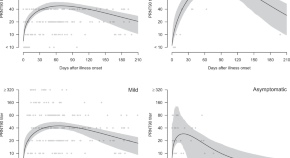
Neutralizing antibody titres in SARS-CoV-2 infections
Here, the authors perform plaque reduction neutralization (PRNT) assays quantitating SARS-CoV-2 specific neutralizing antibodies from 195 patients in different disease states and find that patients with severe disease exhibit higher peaks of neutralizing antibody titres than patients with mild or asymptomatic infections and that serum neutralizing antibody persists for over 6 months in most people.
- Eric H. Y. Lau
- Owen T. Y. Tsang
- Malik Peiris
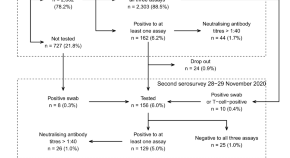
SARS-CoV-2 antibody dynamics and transmission from community-wide serological testing in the Italian municipality of Vo’
Vo’, Italy, is a unique setting for studying SARS-CoV-2 antibody dynamics because mass testing was conducted there early in the pandemic. Here, the authors perform two follow-up serological surveys and estimate seroprevalence, the extent of within-household transmission, and the impact of contact tracing.
- Ilaria Dorigatti
- Enrico Lavezzo
- Andrea Crisanti
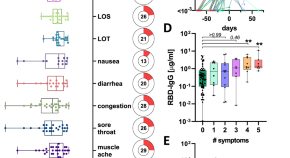
Discrete SARS-CoV-2 antibody titers track with functional humoral stability
The extent of antibody protection against SARS-CoV-2 remains unclear. Here, using a cohort of 120 seroconverted individuals, the authors longitudinally characterize neutralization, Fc-function, and SARS-CoV-2 specific T cell responses, which they show to be prominent only in those subjects that elicited receptor-binding domain (RBD)-specific antibody titers above a certain threshold, suggesting that development of T cell responses to be related to anti-RBD Ab production.
- Yannic C. Bartsch
- Stephanie Fischinger
- Galit Alter
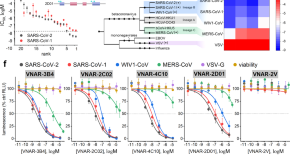
Mechanisms of SARS-CoV-2 neutralization by shark variable new antigen receptors elucidated through X-ray crystallography
Shark antibodies (Variable New Antigen Receptors, VNARs) are the smallest naturally occurring antibody fragments. Here, the authors screen a VNAR phage display library against the SARS-CoV2 receptor binding domain (RBD) and identify VNARs that neutralize the SARSCoV-2 virus and discuss their mechanisms of viral neutralization.
- Obinna C. Ubah
- Eric W. Lake
- Caroline J. Barelle
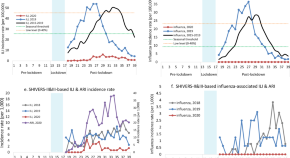
Impact of the COVID-19 nonpharmaceutical interventions on influenza and other respiratory viral infections in New Zealand
New Zealand has been relatively successful in controlling COVID-19 due to implementation of strict non-pharmaceutical interventions. Here, the authors demonstrate a striking decline in reports of influenza and other non-influenza respiratory pathogens over winter months in which the interventions have been in place.
- Q. Sue Huang
- Richard J. Webby
A potent SARS-CoV-2 neutralising nanobody shows therapeutic efficacy in the Syrian golden hamster model of COVID-19
Neutralizing nanobodies (Nb) are of considerable interest as therapeutic agents for COVID-19 treatment. Here, the authors functionally and structurally characterize Nbs that bind with high affinity to the receptor binding domain of the SARS-CoV-2 spike protein and show that an engineered homotrimeric Nb prevents disease progression in a Syrian hamster model of COVID-19 when administered intranasally.
- Jiandong Huo
- Halina Mikolajek
- Raymond J. Owens

Reprogrammed CRISPR-Cas13b suppresses SARS-CoV-2 replication and circumvents its mutational escape through mismatch tolerance
Cas13b can be harnessed to target and degrade RNA transcripts inside a cellular environment. Here the authors reprogram Cas13b to target SARSCoV-2 transcripts in infected mammalian cells and reveal its resilience to variants thanks to single mismatch tolerance.
- Mohamed Fareh
- Joseph A. Trapani
SARS-CoV-2-specific T cell memory is sustained in COVID-19 convalescent patients for 10 months with successful development of stem cell-like memory T cells
T cells are instrumental to protective immune responses against SARS-CoV-2, the pathogen responsible for the COVID-19 pandemic. Here the authors show that, in convalescent COVID-19 patients, memory T cell responses are detectable up to 317 days post-symptom onset, in which the presence of stem cell-like memory T cells further hints long-lasting immunity.
- Jae Hyung Jung
- Min-Seok Rha
- Eui-Cheol Shin
Seven-month kinetics of SARS-CoV-2 antibodies and role of pre-existing antibodies to human coronaviruses
Long-term characterisation of SARS-CoV-2 antibody kinetics is needed to understand the protective role of the immune response. Here the authors describe antibody levels and neutralisation activity in healthcare workers over seven months and investigate the role of immunity to endemic human coronaviruses.
- Natalia Ortega
- Marta Ribes
- Carlota Dobaño

Mechanism of SARS-CoV-2 polymerase stalling by remdesivir
Remdesivir is a nucleoside analog that inhibits the SARS-CoV-2 RNA dependent RNA polymerase (RdRp) and is used as a drug to treat COVID19 patients. Here, the authors provide insights into the mechanism of remdesivir-induced RdRp stalling by determining the cryo-EM structures of SARS-CoV-2 RdRp with bound RNA molecules that contain remdesivir at defined positions and observe that addition of the fourth nucleotide following remdesivir incorporation into the RNA product is impaired by a barrier to further RNA translocation.
- Goran Kokic
- Hauke S. Hillen
- Patrick Cramer
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Fact sheets
- Facts in pictures
Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Observatory
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
There is a current outbreak of Coronavirus (COVID-19) disease Find out more →
- Health topics /
Coronavirus disease (COVID-19) is an infectious disease caused by the SARS-CoV-2 virus.
Most people infected with the virus will experience mild to moderate respiratory illness and recover without requiring special treatment. However, some will become seriously ill and require medical attention. Older people and those with underlying medical conditions like cardiovascular disease, diabetes, chronic respiratory disease, or cancer are more likely to develop serious illness. Anyone can get sick with COVID-19 and become seriously ill or die at any age.
The best way to prevent and slow down transmission is to be well informed about the disease and how the virus spreads. Protect yourself and others from infection by staying at least 1 metre apart from others, wearing a properly fitted mask, and washing your hands or using an alcohol-based rub frequently. Get vaccinated when it’s your turn and follow local guidance.
The virus can spread from an infected person’s mouth or nose in small liquid particles when they cough, sneeze, speak, sing or breathe. These particles range from larger respiratory droplets to smaller aerosols. It is important to practice respiratory etiquette, for example by coughing into a flexed elbow, and to stay home and self-isolate until you recover if you feel unwell.
Stay informed:
- Advice for the public
- Myth busters
- All information on the COVID-19 outbreak
To prevent infection and to slow transmission of COVID-19, do the following:
- Get vaccinated when a vaccine is available to you.
- Stay at least 1 metre apart from others, even if they don’t appear to be sick.
- Wear a properly fitted mask when physical distancing is not possible or when in poorly ventilated settings.
- Choose open, well-ventilated spaces over closed ones. Open a window if indoors.
- Wash your hands regularly with soap and water or clean them with alcohol-based hand rub.
- Cover your mouth and nose when coughing or sneezing.
- If you feel unwell, stay home and self-isolate until you recover.
COVID-19 affects different people in different ways. Most infected people will develop mild to moderate illness and recover without hospitalization.
Most common symptoms:
- loss of taste or smell.
Less common symptoms:
- sore throat
- aches and pains
- a rash on skin, or discolouration of fingers or toes
- red or irritated eyes.
Serious symptoms:
- difficulty breathing or shortness of breath
- loss of speech or mobility, or confusion
- chest pain.
Seek immediate medical attention if you have serious symptoms. Always call before visiting your doctor or health facility.
People with mild symptoms who are otherwise healthy should manage their symptoms at home.
On average it takes 5–6 days from when someone is infected with the virus for symptoms to show, however it can take up to 14 days.
- Q&As on COVID-19 and related health topics
- WHO Coronavirus (COVID-19) Dashboard
- COVID-19 Clinical Care Pathway
- COVID-19 Impact on nutrition analytical framework
- COVID-19 Vaccine delivery toolkit
- Global Clinical Platform for COVID-19
- Coronavirus disease (COVID-19) pandemic
- Access to COVID-19 Tools (ACT) Accelerator
- COVID-19 Technology access pool
- ACT-Accelerator Ethics & Governance Working Group
- Advisory Group on Therapeutics Prioritization for COVID-19
- COVID-19 IHR Emergency Committee
- COVID-19 Infection Prevention and Control Guidance Development Group
- Facilitation Council for the Access to COVID-19 Tools (ACT) Accelerator
- International Travel and Health (ITH) guideline development group (GDG) for COVID-19
- Technical Advisory Group on the COVID-19 Technology Access Pool
- Technical Advisory Group on COVID-19 Vaccine Composition
- Technical Advisory Group on SARS-CoV-2 Virus Evolution
- Working Group on Ethics and COVID-19
- COVID-19 Training
WHO and Switzerland strengthen partnership for global BioHub System
COVID-19 eliminated a decade of progress in global level of life expectancy
Statement on the antigen composition of COVID-19 vaccines
WHO reports widespread overuse of antibiotics in patients hospitalized with COVID-19

WHO SEAR 11th Epidemiological Bulletin 2024
This epidemiological bulletin aims to provide the situation of key infectious diseases in the WHO South-East Asia region to inform risk assessments and...

WHO SEAR 10th Epidemiological Bulletin 2024

WHO SEAR 9th Epidemiological Bulletin 2024

WHO SEAR 8th Epidemiological Bulletin 2024
Who documents.
/epidemic-and-pandemic-preparedness-and-prevention-(epp)/emerging-diseases-and-zoonoses-(ezd)/ceu_170_thumbnail.tmb-144v.png?sfvrsn=6f0c669c_1)
COVID-19 epidemiological update – 13 August 2024
SARS-CoV-2 PCR percent positivity during the four-week reporting period from 24 June to 21 July 2024, as detected in integrated sentinel surveillance as...
/epidemic-and-pandemic-preparedness-and-prevention-(epp)/emerging-diseases-and-zoonoses-(ezd)/ceu_169_thumbnail.tmb-144v.png?sfvrsn=9e49356_1)
COVID-19 epidemiological update – 15 July 2024
SARS-CoV-2 PCR percent positivity during the four-week reporting period from 27 May to 23 June 2024, as detected in integrated sentinel surveillance as...

COVID-19 epidemiological update – 17 June 2024
SARS-CoV-2 PCR percent positivity, as detected in integrated sentinel surveillance as part of the Global Influenza Surveillance and Response System...

COVID-19 epidemiological update – 17 May 2024
Tracking SARS-CoV-2 variants
Promoting a fair and equitable response to the COVID-19 pandemic
Promoting the health of refugees and migrants during COVID-19 pandemic
Preparing and preventing epidemics and pandemics
Donors making a difference for WHO’s work to save lives in Sudan and South Sudan
Development partners making a difference: The European Union supports WHO in eight Asian countries to prepare for the future
Infographics

Diagnostic testing for SARS-CoV-2 infection

Why testing is important?

Pandemic preparedness: Introducing WHO's Investigations and Studies (Unity Studies) approach

Nurses Facing COVID - 2023 Health Emergencies "GRAND PRIX" at the 4th Health for All Film Festival

WHO's Science in 5: Older adults and COVID-19 vaccines - 14 October 2022

WHO’s Science in 5 on COVID-19: Genome Sequencing
INB related interactive dialogues
Webinar program on mental health and post COVID-19 condition
Related links
- Share full article
Advertisement
Supported by
current events
12 Ideas for Writing Through the Pandemic With The New York Times
A dozen writing projects — including journals, poems, comics and more — for students to try at home.

By Natalie Proulx
The coronavirus has transformed life as we know it. Schools are closed, we’re confined to our homes and the future feels very uncertain. Why write at a time like this?
For one, we are living through history. Future historians may look back on the journals, essays and art that ordinary people are creating now to tell the story of life during the coronavirus.
But writing can also be deeply therapeutic. It can be a way to express our fears, hopes and joys. It can help us make sense of the world and our place in it.
Plus, even though school buildings are shuttered, that doesn’t mean learning has stopped. Writing can help us reflect on what’s happening in our lives and form new ideas.
We want to help inspire your writing about the coronavirus while you learn from home. Below, we offer 12 projects for students, all based on pieces from The New York Times, including personal narrative essays, editorials, comic strips and podcasts. Each project features a Times text and prompts to inspire your writing, as well as related resources from The Learning Network to help you develop your craft. Some also offer opportunities to get your work published in The Times, on The Learning Network or elsewhere.
We know this list isn’t nearly complete. If you have ideas for other pandemic-related writing projects, please suggest them in the comments.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
COVID-19 and African Americans
- 1 Department of Internal Medicine, Division of Cardiology, Northwestern University, Feinberg School of Medicine, Chicago, Illinois
- Editorial Health Equity—A New Kind of “Herd Immunity” David R. Williams, PhD, MPH; Lisa A. Cooper, MD, MPH JAMA
- Viewpoint Disparities Research, Disparities Researchers, and Health Equity Mercedes R. Carnethon, PhD; Kiarri N. Kershaw, PhD; Namratha R. Kandula, MD, MPH JAMA
- Viewpoint Mathematical Models Predicting the COVID-19 Pandemic Nicholas P. Jewell, PhD; Joseph A. Lewnard, PhD; Britta L. Jewell, PhD JAMA
- A Piece of My Mind Failing Another National Stress Test on Health Disparities William F. Owen Jr, MD; Richard Carmona, MD, MPH; Claire Pomeroy, MD, MBA JAMA
- Research Letter Variation in COVID-19 Hospitalizations and Deaths Across New York City Boroughs Rishi K. Wadhera, MD, MPP, MPhil; Priya Wadhera, MD, MS; Prakriti Gaba, MD; Jose F. Figueroa, MD, MPH; Karen E. Joynt Maddox, MD, MPH; Robert W. Yeh, MD, MSc; Changyu Shen, PhD JAMA
- Viewpoint COVID-19 and Racial/Ethnic Disparities Monica Webb Hooper, PhD; Anna María Nápoles, PhD, MPH; Eliseo J. Pérez-Stable, MD JAMA
- Viewpoint Responding to COVID-19 With a Structurally Competent Health Care System Jonathan M. Metzl, MD, PhD; Aletha Maybank, MD, MPH; Fernando De Maio, PhD JAMA
- Viewpoint Policy Solutions for Reversing the Color-blind US Public Health Response to COVID-19 Marisa K. Dowling, MD, MPP; Robin L. Kelly, PhD, MA JAMA
- Viewpoint The Moral Determinants of Health Donald M. Berwick, MD, MPP JAMA
- Viewpoint Academic Medicine and Black Lives Matter—Time for Deep Listening Clyde W. Yancy, MD, MSc JAMA
- A Piece of My Mind Ways to Improve Racial Competence Randy A. Vince Jr, MD JAMA
- Medical News & Perspectives Taking a Closer Look at COVID-19, Health Inequities, and Racism Jennifer Abbasi JAMA
- A Piece of My Mind Eliminating Structural Racism Rachel B. Issaka, MD, MAS JAMA
- Medical News & Perspectives Researchers Strive to Recruit Hard-Hit Minorities Into COVID-19 Vaccine Trials Mary Chris Jaklevic, MSJ JAMA
- Research Letter Allocation of COVID-19 Relief Funding to Disproportionately Black Counties Pragya Kakani, AB; Amitabh Chandra, PhD; Sendhil Mullainathan, PhD; Ziad Obermeyer, MD JAMA
- Medical News & Perspectives Surgeon Fills COVID-19 Testing Gap in Philadelphia’s Black Neighborhoods Mary Chris Jaklevic, MSJ JAMA
- Original Investigation Trends in Health Equity in the United States, 1993-2017 Frederick J. Zimmerman, PhD; Nathaniel W. Anderson, BA JAMA Network Open
- Insights Data and Policy Solutions to Address Racial and Ethnic Disparities in the COVID-19 Pandemic Utibe R. Essien, MD, MPH; Atheendar Venkataramani, MD, PhD JAMA Health Forum
- Editor's Comment In Pursuit of a Deeper Understanding of Racial Justice and Health Equity John Z. Ayanian, MD, MPP; Melinda B. Buntin, PhD JAMA Health Forum
- JAMA Forum Health Disparities Among Black Persons in the US and Addressing Racism in the Health Care System Aaron E. Carroll, MD, MS JAMA Health Forum
Much has been published in leading medical journals about the phenomenon of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. The resulting condition, coronavirus disease 2019 (COVID-19), has had a societal effect comparable only to the Spanish flu epidemic of 1918. As the flow of clinical science has better informed the contemporary narratives, more is being learned about which individuals and groups experience the most dire complications. Researchers have emphasized older age, male sex, hypertension, diabetes, obesity, concomitant cardiovascular diseases (including coronary artery disease and heart failure), and myocardial injury as important risk factors associated with worse outcomes; specifically, case-fatality rates vary over 100%. 1 - 3 These data sourced from China and Europe have not been replicated in the US, but the US experience may nevertheless represent similarly distressing outcomes in these highest-risk phenotypes.
The concerns about these observations are appropriate and the published data are indeed actionable; those who fit the highest-risk phenotypes can be advised to assiduously adhere to safe practices including hand hygiene, use of masks in public spaces, and social distancing/physical isolation. 4 These measures not only are flattening the curve but are no doubt saving lives. However, a new concern has arisen: evidence of potentially egregious health care disparities is now apparent. Persons who are African American or black are contracting SARS-CoV-2 at higher rates and are more likely to die. 5 Why is this uniquely important to me? I am an academic cardiologist; I study health care disparities; and I am a black man.
What is currently known about these differences in disease risk and fatality rates? In Chicago, more than 50% of COVID-19 cases and nearly 70% of COVID-19 deaths involve black individuals, although blacks make up only 30% of the population. Moreover, these deaths are concentrated mostly in just 5 neighborhoods on the city’s South Side. 6 In Louisiana, 70.5% of deaths have occurred among black persons, who represent 32.2% of the state’s population. 7 In Michigan, 33% of COVID-19 cases and 40% of deaths have occurred among black individuals, who represent 14% of the population. 5 If New York City has become the epicenter, this disproportionate burden is validated again in underrepresented minorities, especially blacks and now Hispanics, who have accounted for 28% and 34% of deaths, respectively (population representation: 22% and 29%, respectively). 8
The Johns Hopkins University and American Community Survey indicate that to date, of 131 predominantly black counties in the US, the infection rate is 137.5/100 000 and the death rate is 6.3/100 000. 5 This infection rate is more than 3-fold higher than that in predominantly white counties. Moreover, this death rate for predominantly black counties is 6-fold higher than in predominantly white counties. Even though these data are preliminary and further study is warranted, the pattern is irrefutable: underrepresented minorities are developing COVID-19 infection more frequently and dying disproportionately. Do these observations qualify as evident health care disparities?
Yes. The definition of a health care disparity is not simply a difference in health outcomes by race or ethnicity, but a disproportionate difference attributable to variables other than access to care. 9 Given the known risk factors for COVID-19 complications, the confluence of hypertension, diabetes, obesity, and the higher prevalence of cardiovascular disease among black persons may be driving these early signals. Data fully adjusted for comorbidities have not been reported but it is likely that some, if not most, of these differences in disease rates and outcomes will be explained by concomitant comorbidities.
But concerns go beyond these comorbidities. Where and how black individuals live matters. If race per se enters this discussion, it is because in so many communities, race determines home. Once adverse outcomes attributable to known risks for COVID-19 complications are disaggregated from total morbidity and mortality burden due to COVID-19, the pernicious influence of adverse social determinants of health is likely to become apparent. 10 The communities where many black people reside are in poor areas characterized by high housing density, high crime rates, and poor access to healthy foods. Low socioeconomic status alone is a risk factor for total mortality independent of any other risk factors. These social determinants of health must be considered in a complex equation, including known cardiovascular risk factors, which puts underrepresented minorities who live in at-risk communities at greater risk for disease, not just for cardiovascular diseases but now for COVID-19 mortality.
The most effective strategy known to reduce COVID-19 infection is social distancing, but herein lies a vexing challenge. Being able to maintain social distancing while working from home, telecommuting, and accepting a furlough from work but indulging in the plethora of virtual social events are issues of privilege . In certain communities these privileges are simply not accessible. Thus, consider the aggregate of a higher burden of at-risk comorbidities, the pernicious effects of adverse social determinants of health, and the absence of privilege that does not allow a reprieve from work without dire consequences for a person’s sustenance, does not allow safe practices, and does not even allow for 6-foot distancing. The consequent infection and death rates due to COVID-19 complications are no longer surprising; they should have been expected. These observations are rooted in the recalcitrant reality of the deeply entrenched history of health care disparities and may settle as the most painful example yet of the regressive tax of poor health. COVID-19 has become the herald event that now fully exposes the deep and chronic social wounds in US communities.
What makes this particularly egregious is that unlike the known risk factors for which physicians and others can stridently offer clear advice regarding prevention, these concerns—the burden of ill health, limited access to healthy food, housing density, the need to work or else, the inability to practice social distancing—cannot be well-articulated as clear, pithy, and easily actionable items.
What is the action plan? It is less an action plan and more of a commitment. A 6-fold increase in the rate of death for African Americans due to a now ubiquitous virus should be deemed unconscionable. This is a moment of ethical reckoning. The scourge of COVID-19 will end, but health care disparities will persist. Does the US chronicle these poor outcomes due to COVID-19 complications with the higher burden of cardiovascular disease, poorer outcomes for breast cancer, higher amputation rates for peripheral vascular disease, lower kidney transplant rates, and worse rates for maternal mortality, then safely park everything in the health care disparity domain and go back to “normal”? Or will the nation finally hear this familiar refrain, think differently, and as has been done in response to other major diseases, declare that a civil society will no longer accept disproportionate suffering?
Public health is complicated and social reengineering is complex, but change of this magnitude does not happen without a new resolve. The US has needed a trigger to fully address health care disparities; COVID-19 may be that bellwether event. Certainly, within the broad and powerful economic and legislative engines of the US, there is room to definitively address a scourge even worse than COVID-19: health care disparities. It only takes will. It is time to end the refrain.
Corresponding Author : Clyde W. Yancy, MD, MSc, Division of Cardiology, Northwestern University, FSM, 676 N St Clair, Chicago, IL 60611 ( [email protected] ).
Published Online: April 15, 2020. doi:10.1001/jama.2020.6548
Conflict of Interest Disclosures: None reported.
Additional Contributions: I thank Kristin T. Yancy and Nina M. Yancy for their review of the manuscript.
See More About
Yancy CW. COVID-19 and African Americans. JAMA. 2020;323(19):1891–1892. doi:10.1001/jama.2020.6548
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

45,000+ students realised their study abroad dream with us. Take the first step today
Meet top uk universities from the comfort of your home, here’s your new year gift, one app for all your, study abroad needs, start your journey, track your progress, grow with the community and so much more.

Verification Code
An OTP has been sent to your registered mobile no. Please verify

Thanks for your comment !
Our team will review it before it's shown to our readers.

- School Education /
Essay On Covid-19: 100, 200 and 300 Words

- Updated on
- Apr 30, 2024

COVID-19, also known as the Coronavirus, is a global pandemic that has affected people all around the world. It first emerged in a lab in Wuhan, China, in late 2019 and quickly spread to countries around the world. This virus was reportedly caused by SARS-CoV-2. Since then, it has spread rapidly to many countries, causing widespread illness and impacting our lives in numerous ways. This blog talks about the details of this virus and also drafts an essay on COVID-19 in 100, 200 and 300 words for students and professionals.
Table of Contents
- 1 Essay On COVID-19 in English 100 Words
- 2 Essay On COVID-19 in 200 Words
- 3 Essay On COVID-19 in 300 Words
- 4 Short Essay on Covid-19
Essay On COVID-19 in English 100 Words
COVID-19, also known as the coronavirus, is a global pandemic. It started in late 2019 and has affected people all around the world. The virus spreads very quickly through someone’s sneeze and respiratory issues.
COVID-19 has had a significant impact on our lives, with lockdowns, travel restrictions, and changes in daily routines. To prevent the spread of COVID-19, we should wear masks, practice social distancing, and wash our hands frequently.
People should follow social distancing and other safety guidelines and also learn the tricks to be safe stay healthy and work the whole challenging time.
Also Read: National Safe Motherhood Day 2023
Essay On COVID-19 in 200 Words
COVID-19 also known as coronavirus, became a global health crisis in early 2020 and impacted mankind around the world. This virus is said to have originated in Wuhan, China in late 2019. It belongs to the coronavirus family and causes flu-like symptoms. It impacted the healthcare systems, economies and the daily lives of people all over the world.
The most crucial aspect of COVID-19 is its highly spreadable nature. It is a communicable disease that spreads through various means such as coughs from infected persons, sneezes and communication. Due to its easy transmission leading to its outbreaks, there were many measures taken by the government from all over the world such as Lockdowns, Social Distancing, and wearing masks.
There are many changes throughout the economic systems, and also in daily routines. Other measures such as schools opting for Online schooling, Remote work options available and restrictions on travel throughout the country and internationally. Subsequently, to cure and top its outbreak, the government started its vaccine campaigns, and other preventive measures.
In conclusion, COVID-19 tested the patience and resilience of the mankind. This pandemic has taught people the importance of patience, effort and humbleness.
Also Read : Essay on My Best Friend
Essay On COVID-19 in 300 Words
COVID-19, also known as the coronavirus, is a serious and contagious disease that has affected people worldwide. It was first discovered in late 2019 in Cina and then got spread in the whole world. It had a major impact on people’s life, their school, work and daily lives.
COVID-19 is primarily transmitted from person to person through respiratory droplets produced and through sneezes, and coughs of an infected person. It can spread to thousands of people because of its highly contagious nature. To cure the widespread of this virus, there are thousands of steps taken by the people and the government.
Wearing masks is one of the essential precautions to prevent the virus from spreading. Social distancing is another vital practice, which involves maintaining a safe distance from others to minimize close contact.
Very frequent handwashing is also very important to stop the spread of this virus. Proper hand hygiene can help remove any potential virus particles from our hands, reducing the risk of infection.
In conclusion, the Coronavirus has changed people’s perspective on living. It has also changed people’s way of interacting and how to live. To deal with this virus, it is very important to follow the important guidelines such as masks, social distancing and techniques to wash your hands. Getting vaccinated is also very important to go back to normal life and cure this virus completely.
Also Read: Essay on Abortion in English in 650 Words
Short Essay on Covid-19
Please find below a sample of a short essay on Covid-19 for school students:
Also Read: Essay on Women’s Day in 200 and 500 words
to write an essay on COVID-19, understand your word limit and make sure to cover all the stages and symptoms of this disease. You need to highlight all the challenges and impacts of COVID-19. Do not forget to conclude your essay with positive precautionary measures.
Writing an essay on COVID-19 in 200 words requires you to cover all the challenges, impacts and precautions of this disease. You don’t need to describe all of these factors in brief, but make sure to add as many options as your word limit allows.
The full form for COVID-19 is Corona Virus Disease of 2019.
Related Reads
Hence, we hope that this blog has assisted you in comprehending with an essay on COVID-19. For more information on such interesting topics, visit our essay writing page and follow Leverage Edu.
Simran Popli
An avid writer and a creative person. With an experience of 1.5 years content writing, Simran has worked with different areas. From medical to working in a marketing agency with different clients to Ed-tech company, the journey has been diverse. Creative, vivacious and patient are the words that describe her personality.
Leave a Reply Cancel reply
Save my name, email, and website in this browser for the next time I comment.
Contact no. *

Connect With Us
45,000+ students realised their study abroad dream with us. take the first step today..

Resend OTP in

Need help with?
Study abroad.
UK, Canada, US & More
IELTS, GRE, GMAT & More
Scholarship, Loans & Forex
Country Preference
New Zealand
Which English test are you planning to take?
Which academic test are you planning to take.
Not Sure yet
When are you planning to take the exam?
Already booked my exam slot
Within 2 Months
Want to learn about the test
Which Degree do you wish to pursue?
When do you want to start studying abroad.
January 2024
September 2024
What is your budget to study abroad?
How would you describe this article ?
Please rate this article
We would like to hear more.
Have something on your mind?

Make your study abroad dream a reality in January 2022 with
India's Biggest Virtual University Fair

Essex Direct Admission Day
Why attend .

Don't Miss Out
Pandemics Don’t Really End—They Echo
T he public health emergency related to the COVID-19 pandemic officially ended on May 11, 2023. It was a purely administrative step. Viruses do not answer to government decrees. Reported numbers were declining, but then started coming up again during the summer. By August, hospital admissions climbed to more than 10,000 a week. This was nowhere near the 150,000 weekly admissions recorded at the peak of the pandemic in January 2022.
The new variant is more contagious. It is not yet clear whether it is more lethal. Nor is it clear whether the recent rise is a mere uptick or foreshadows a more serious surge. More than 50,000 COVID-19 deaths have been reported in the U.S. in 2023. Somehow, this has come to be seen as almost normal.
Even while health authorities are keeping their eyes on new “variables of concern,” for much of the public COVID has been cancelled. The news media have largely moved on to other calamities. The pandemic is over. Is it?
History shows that pandemics have ragged endings. Some return again and again. The Justinian Plague that swept through the Roman Empire in the 6 th century returned in waves over the next 200 years. The Black Death that killed half the population of Europe between 1347 and 1351 came back more than 40 times over the next 400 years.
Read More: Will the New Vaccine Work Against the Latest Variant?
The effect of the COVID-19 pandemic will be felt long after the last rapid test comes back positive. Millions today are still suffering from “ long COVID ”—a range of medical conditions that can appear long after the initial infection. This concept can be applied to the whole of society.
Pandemics have always frayed the social fabric, disrupted economies, deepened social divides, and intensified prejudices, leaving behind psychological scars—all of which have lasting political repercussions.
Angered by the British crown’s attempt to restore the inequalities of the pre-pandemic feudal system, which had been weakened by the massive depopulation caused by the plague, English peasants marched on London and nearly brought down the king. Repeated waves of cholera in Europe during the 19 th century increased social tensions and contributed to growing class warfare. A sharp increase in labor strife followed the 1918 flu pandemic.
Today, society seems similarly on edge and quick to violence, an observation that was also made about medieval society following the plague. The U.S. homicide rate in 2020 and 2021 increased by nearly 40 percent. It appears to have come down in some cities, but violent crime remains above pre-pandemic levels. Mass shootings have hit an all-time high, while random unprovoked aggression has increased in public spaces. The pandemic is not entirely to blame, but it has likely been a contributing factor.
Many Americans quit their jobs after the pandemic. Others are refusing to give up working from home . The so-called great resignation appears to be ending, but the labor militancy that featured in post-pandemic societies continues.
While the COVID-19 pandemic comes nowhere near the depopulation effects of the plague, it emptied the sidewalks in many major American cities. Office buildings have fewer workers. Restaurants have lost business. It is not uncommon to see rows of boarded up retail shops. COVID does not get all the blame. The rise in crime in many city centers keeps many away. Urban geography may be permanently altered.
As it often did after past pandemics, pessimism pervades the post-pandemic moodscape. Its explanation lies beyond the pathogens. A Biblical host of natural and man-made disasters—pestilence, war, famine, floods, drought, fire, contribute to a sense of foreboding.
The 1918 flu pandemic left a legacy of distrust in institutions and each other, which was passed down to children and grandchildren, COVID may have similar long-term effects.
Americans are a cantankerous lot, increasingly suspicious of malevolent motives behind anything government does. Partisan news outlets look for conflict and stoke outrage. In past pandemics, conspiracy theories flourished, often blaming immigrants and Jews. So too, some COVID conspiracy theories suggest that the virus was designed to kill Whites or Blacks, while sparing Asians and Jews. Nothing changes.
Some believe the government created the pandemic hoax or deliberately misled the public about the seriousness of the situation. They argue that needless lockdown orders and business shutdown ruined the economy; providing financial relief to businesses and families opened the way for massive corruption and left the country with insupportable debt; mask and vaccine mandates were assaults on personal liberty for the benefit of big Pharma profits. Some still claim that the vaccines themselves rivaled the virus in their lethality. Defiance has been elevated to patriotism.
Owing to response measures, improved medications, life-saving procedures for treating critically-ill patients, and the rapid availability of a vaccine, the outbreak did not replicate the death tolls of previous pandemics.
Although it sounds perverse, saving lives ended up contributing to the controversy. Simply put: The pandemic was not deadly enough . The 2 nd century Antonine Plague killed a quarter of the Roman Empire’s population. The 6 th century Justinian plague killed half the population of Europe. According to some historians, the first wave of the plague in the 14 th century again wiped out half of Europe’s inhabitants.
COVID has killed more than a million Americans, roughly a third of one percent—or about the same percentage of the population killed in World War II. As a percentage of the total population, the 1918 flu was twice as deadly.
The demographics of the death toll are important. The 1918 flu killed many younger people—those 25-40 years old accounted for 40% of the fatalities—while COVID killed mainly older Americans, as three-quarters of the dead were 65 or older. Those under 40 accounted for just 2.5% of the fatalities.
Some questioned why the country’s well-being should be jeopardized to save the elderly, many of whom already had other afflictions anyway. Expressed in the cruelest terms, nature was culling the herd. Indeed, some of the same groups that during earlier debates about national health care expressed outrage at the prospect of death panels “pulling the plug on grandma” suggested during the pandemic that the elderly would be willing to die to save the economy.
The COVID pandemic lacked visual impact. Except for those directly affected, COVID’s toll remained abstract. There was no modern equivalent of town criers calling “Bring out your dead” accompanied by carts making the rounds to collect corpses. Had COVID led to bodies piled in the streets, shared dread might have outweighed our differences. As it turned out, we had the science to address the pandemic. What we lacked was the social accord.
Discord continues in the political arena. The tradeoffs between preserving individual rights and protecting the public are legitimate areas to explore, but rather than looking for lessons to be learned, some politicians appear determined to settle scores. Pandemic disputes will almost certainly feature in the 2024 presidential election.
Any future outbreak of disease will likely again see cable news, the internet, and social media play major roles in shaping the information individuals choose in their decision making. This will inevitably make emergency control measures more difficult to impose. COVID’s biggest political casualty may be governability itself.
We are unable to join hands to remember the more than a million Americans that have succumbed to the virus—that are succumbing still. We cannot express a nation’s gratitude to the scientists, public health officials, and heroic frontline health workers, thousands of whom died saving lives during the pandemic. Stuck in the well-worn paths of previous pandemic prejudices and conspiracy theory re-runs, we cannot come together to mourn our losses and celebrate our survival.
There will be no collective thanksgiving, no elegies, no closure. As we have seen time and time again throughout human history, pandemics do not end—they echo.
More Must-Reads from TIME
- Breaking Down the 2024 Election Calendar
- How Nayib Bukele’s ‘Iron Fist’ Has Transformed El Salvador
- What if Ultra-Processed Foods Aren’t as Bad as You Think?
- How Ukraine Beat Russia in the Battle of the Black Sea
- Long COVID Looks Different in Kids
- How Project 2025 Would Jeopardize Americans’ Health
- What a $129 Frying Pan Says About America’s Eating Habits
- The 32 Most Anticipated Books of Fall 2024
Contact us at [email protected]

COVID-19 , flu and RSV shots − an epidemiologist explains why all three matter this fall
Associate Professor of Epidemiology, University of San Francisco
Disclosure statement
Annette Regan receives funding from the National Institutes for Health and the US Centers for Disease Control and Prevention. She has served on a Data Safety Monitoring Board for Moderna Inc.
View all partners
The Food and Drug Administration approved and granted emergency use authorization on Aug. 22, 2024, for the newest, updated version of the COVID-19 vaccine . The Centers for Disease Control and Prevention quickly endorsed the new shot to protect against severe illness.
The 2024 summer wave of COVID-19 cases is a good reminder of why people need to stay up to date with their vaccines.
As the fall and winter seasons approach, the usual seasonal respiratory viruses, including flu and respiratory syncytial virus, or RSV , will also be on the rise. Vaccines are now available to help protect against these viruses.
The Conversation asked epidemiologist Annette Regan to explain why officials recommend that people get these shots over the coming months.
What strain is the new COVID-19 shot based on and why?
The COVID-19 vaccine has been updated several times since the original shot in 2020-21 to keep up with how the SARS-CoV-2 virus is changing.
In September 2023, the CDC recommended that all people get the newly updated vaccine that was designed to protect against XBB.1.5 , the variant that had been dominant in the U.S. that summer, regardless of whether they had received all recommended shots in the past.
Now, in August 2024, the XBB.1.5 variant is no longer around and has been replaced by the KP.2 and KP.3 variants , which make up more than 60% of variants currently detected .
Moderna and Pfizer both made updated formulations of the COVID-19 shot that target this new KP.2 variant. It is a monovalent vaccine, which means it includes only the KP.2 strain.
This strain was selected because it was the most common variant at the time the choice was made. Even when new variants such as KP.3 emerge, we researchers expect the updated vaccine to protect against the newer strains. For example, the 2023-24 vaccine was designed to target the XBB.1.5 strain, and studies showed that it continued to protect against the JN.1 variant that later emerged.
The CDC recommends a single shot for everyone 6 months and older, with some exceptions. Children 6 months to 4 years old who have not received any prior shots of COVID-19 vaccine still need two or three shots of the updated 2024-25 vaccine. Adults 65 and older and children and adults with certain health conditions may require an additional shot as well.
People who recently had a SARS-CoV-2 infection may consider delaying their shot for three months after the illness, since risk of reinfection is thought to be low during the months after infection.
How did the 2023 updated vaccine perform?
Recent studies have shown that people who received the 2023-24 vaccine were 54% less likely to develop symptomatic COVID-19 illness , 39% to 51% less likely to visit an emergency department or urgent care with COVID-19 , and 50% to 53% less likely to be hospitalized with COVID-19 compared with unvaccinated people.
The vaccine was most effective among those who had received their shot more recently.
What is the best timing for the shots?
COVID-19 hospitalizations and deaths have been rising since May 2024, with the highest rates seen in adults 65 and older and infants under 6 months old. Therefore, public health experts are recommending that people get the COVID-19 shot as soon as possible to protect against severe illness.
Because infants younger than 6 months are not old enough to be directly vaccinated, COVID-19 vaccination during pregnancy is the best way to protect these babies .
When it comes to the flu, cases and hospitalizations seem to rise steeply between November and December. Some years, however, such as the 2022-23 flu season , they start as early as October.
It’s important to remember that vaccines do not offer immediate protection. You need about two weeks for your body to generate enough antibodies to offer protection. September or early October is a good time to get the flu shot to ensure you are protected in time. However, if you aren’t able to get the shot before November, it’s important to know that it is still helpful to get the shot as long as flu is around.
Is it OK to get both the COVID-19 and flu shots at the same time?
Getting the COVID-19 and flu shots together can certainly make it easier to get up to date with these recommended vaccinations. Data shows that getting the flu shot and the COVID-19 shot together is safe and effective .
Some vaccine companies are working to develop a combined flu/COVID-19 vaccine to reduce the number of shots needed. This vaccine still needs to be approved by the Food and Drug Administration but could become available soon.
Who should get the RSV shot and when?
RSV is another common respiratory virus that can cause severe illness in young children and older adults. There are two groups of people who should get one of the three currently available RSV vaccines: adults 60 years and older and pregnant people. The CDC recommends a single dose of either GSK’s AREXVY, Moderna’s mRESVIA or Pfizer’s ABRYSVO for all adults 75 years and older and adults between the ages of 60 to 74 who are at increased risk of severe RSV disease.
Unlike the COVID-19 and flu shots, additional RSV doses are not currently recommended, because research suggests that the vaccine offers protection for at least two RSV seasons . These vaccines are relatively new, however, and more data will be needed to see how long this protection really lasts. Additional doses may be recommended in the future.
The CDC recommends only Pfizer’s shot for people in weeks 32 to 36 of pregnancy between September and January. The Pfizer vaccine is the only RSV vaccine that has been licensed and approved for use in pregnancy.
These vaccines are different from the antibodies that can be given to infants at or after birth, called Beyfortus (nirsevimab). The CDC recommends one dose of nirsevimab for infants who are younger than 8 months old born during or shortly before their first RSV season. For some children who are 8 to 19 months old and are at increased risk of severe RSV disease, a dose of nirsevimab may also be recommended during their second RSV season.
Both the RSV vaccine and nirsevimab offer safe and effective options for preventing RSV in young babies.
Pregnant people should get advice from their health care professionals about which option is best for them.
- Centers for Disease Control and Prevention (CDC)
- COVID-19 vaccines
- COVID-19 vaccines and variants
- Centers for Disease Control and Prevention
- Food and Drug Administration (FDA)
- RSV vaccine

Director of STEM

Community member - Training Delivery and Development Committee (Volunteer part-time)

Chief Executive Officer

Finance Business Partner

Head of Evidence to Action
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Effects of COVID-19 pandemic in daily life
Dear Editor,
COVID-19 (Coronavirus) has affected day to day life and is slowing down the global economy. This pandemic has affected thousands of peoples, who are either sick or are being killed due to the spread of this disease. The most common symptoms of this viral infection are fever, cold, cough, bone pain and breathing problems, and ultimately leading to pneumonia. This, being a new viral disease affecting humans for the first time, vaccines are not yet available. Thus, the emphasis is on taking extensive precautions such as extensive hygiene protocol (e.g., regularly washing of hands, avoidance of face to face interaction etc.), social distancing, and wearing of masks, and so on. This virus is spreading exponentially region wise. Countries are banning gatherings of people to the spread and break the exponential curve. 1 , 2 Many countries are locking their population and enforcing strict quarantine to control the spread of the havoc of this highly communicable disease.
COVID-19 has rapidly affected our day to day life, businesses, disrupted the world trade and movements. Identification of the disease at an early stage is vital to control the spread of the virus because it very rapidly spreads from person to person. Most of the countries have slowed down their manufacturing of the products. 3 , 4 The various industries and sectors are affected by the cause of this disease; these include the pharmaceuticals industry, solar power sector, tourism, Information and electronics industry. This virus creates significant knock-on effects on the daily life of citizens, as well as about the global economy.
Presently the impacts of COVID-19 in daily life are extensive and have far reaching consequences. These can be divided into various categories:
- • Challenges in the diagnosis, quarantine and treatment of suspected or confirmed cases
- • High burden of the functioning of the existing medical system
- • Patients with other disease and health problems are getting neglected
- • Overload on doctors and other healthcare professionals, who are at a very high risk
- • Overloading of medical shops
- • Requirement for high protection
- • Disruption of medical supply chain
- • Slowing of the manufacturing of essential goods
- • Disrupt the supply chain of products
- • Losses in national and international business
- • Poor cash flow in the market
- • Significant slowing down in the revenue growth
- • Service sector is not being able to provide their proper service
- • Cancellation or postponement of large-scale sports and tournaments
- • Avoiding the national and international travelling and cancellation of services
- • Disruption of celebration of cultural, religious and festive events
- • Undue stress among the population
- • Social distancing with our peers and family members
- • Closure of the hotels, restaurants and religious places
- • Closure of places for entertainment such as movie and play theatres, sports clubs, gymnasiums, swimming pools, and so on.
- • Postponement of examinations
This COVID-19 has affected the sources of supply and effects the global economy. There are restrictions of travelling from one country to another country. During travelling, numbers of cases are identified positive when tested, especially when they are taking international visits. 5 All governments, health organisations and other authorities are continuously focussing on identifying the cases affected by the COVID-19. Healthcare professional face lot of difficulties in maintaining the quality of healthcare in these days.
Declaration of competing interest
None declared.

- Liberty University
- Jerry Falwell Library
- Special Collections
- < Previous
Home > ETD > Doctoral > 5957
Doctoral Dissertations and Projects
Exploring health science students' perception of the influence of health precaution practices during the covid-19 pandemic.
Marquitta L. Foster , Liberty University Follow
School of Health Sciences
Doctor of Philosophy
The COVID-19 Pandemic, Health Science Students, Health Precautions Practices, During the COVID-19 Pandemic
Disciplines
Health and Physical Education
Recommended Citation
Foster, Marquitta L., "Exploring Health Science Students' Perception of the Influence of Health Precaution Practices During the COVID-19 Pandemic" (2024). Doctoral Dissertations and Projects . 5957. https://digitalcommons.liberty.edu/doctoral/5957
The purpose of this phenomenological study was to address a lack of research on health science students’ perceptions and use of health precautions during the COVID-19 pandemic. Albert Bandura’s Social Cognitive Theory frames this study of bachelor's, master’s and doctoral level students at Liberty University, George Mason University, and Norfolk State University. Data was gathered via surveys, interviews, and observations from 35 students across the three universities, providing a diverse pool of age, gender, and ethnicity. The initial survey gathered demographic data on whether students considered themselves immunocompromised, their view on COVID-19's severity for the immunocompromised, and whether they felt COVID-19 had increased the need for medical check-ups and vaccinations. Follow-up interviews were conducted, transcribed, and coded, identifying themes related to students’ awareness of COVID-19, the influence of students’ knowledge on their behavior, attitudes toward pandemic-era restrictions and contact tracing, and their use of health precautions. Many students reported increased use of health precautions during the pandemic, and those students with experience with vulnerable populations expressed using more health precautions out of concern for others’ well-being both during and after the pandemic. Students at all educational levels mentioned the importance of sharing accurate information. The findings suggest that enhancing students’ understanding of disease transmission, and effective strategies for communicating with lay people, could be productive. Practice communicating with non-scientists should be integrated into health science classes to capitalize on health science students’ care for others and position as trusted resources. Future research could explore the impact of these changes on students’ understanding of disease transmission, communication skills, and self-efficacy.
Since August 29, 2024
Included in
Health and Physical Education Commons
- Collections
- Faculty Expert Gallery
- Theses and Dissertations
- Conferences and Events
- Open Educational Resources (OER)
- Explore Disciplines
Advanced Search
- Notify me via email or RSS .
Faculty Authors
- Submit Research
- Expert Gallery Login
Student Authors
- Undergraduate Submissions
- Graduate Submissions
- Honors Submissions
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
Advertisement
Will mpox become a global pandemic like covid-19?
A new variant of mpox is surging in Central Africa, raising concerns about how quickly it could spread further afield
By Michael Le Page
27 August 2024

An mpox awareness banner at Chennai International Airport in India on 21 August
R.SATISH BABU/AFP via Getty Images
A new mpox variant called clade Ib that emerged in the Democratic Republic of the Congo last year has now spread to several neighbouring countries. Sweden and Thailand have also each detected a case in individuals who travelled from this region. So, how serious a threat is it?
It is clear that mpox clade Ib is nowhere near as transmissible as respiratory viruses such as SARS-CoV-2, and thus it almost certainly won’t cause a pandemic on the scale of covid-19. However, initial…
Sign up to our weekly newsletter
Receive a weekly dose of discovery in your inbox! We'll also keep you up to date with New Scientist events and special offers.
To continue reading, subscribe today with our introductory offers
No commitment, cancel anytime*
Offer ends 10 September 2024.
*Cancel anytime within 14 days of payment to receive a refund on unserved issues.
Inclusive of applicable taxes (VAT)
Existing subscribers
More from New Scientist
Explore the latest news, articles and features

Does mpox cause lingering symptoms like long covid?
Subscriber-only

How deadly is mpox and what treatments are available?

Everything you need to know about the mpox outbreak

Why is mpox a global emergency again so soon?
Popular articles.
Trending New Scientist articles
- Open access
- Published: 26 August 2024
Paramedics’ experiences and observations: work-related emotions and well-being resources during the initial months of the COVID-19 pandemic—a qualitative study
- Henna Myrskykari 1 , 2 &
- Hilla Nordquist 3
BMC Emergency Medicine volume 24 , Article number: 152 ( 2024 ) Cite this article
91 Accesses
1 Altmetric
Metrics details
As first responders, paramedics are an extremely important part of the care chain. COVID-19 significantly impacted their working circumstances. We examined, according to the experiences and observations of paramedics, (1) what kinds of emotions the Emergency Medical Service (EMS) personnel experienced in their new working circumstances, and (2) what work-related factors became resources for the well-being of EMS personnel during the initial months of the COVID-19 pandemic.
This qualitative study utilized reflective essay material written by experienced, advanced-level Finnish paramedics ( n = 30). The essays used in this study were written during the fall of 2020 and reflected the period when Finland had declared a state of emergency (on 17.3.2020) and the Emergency Powers Act was implemented. The data was analyzed using an inductive thematic analysis.
The emotions experienced by the EMS personnel in their new working circumstances formed three themes: (1) New concerns arose that were constantly present; (2) Surviving without proper guidance; and (3) Rapidly approaching breaking point. Three themes were formed from work-related factors that were identified as resources for the well-being of the EMS personnel. These were: (1) A high level of organizational efficiency was achieved; (2) Adaptable EMS operations; and (3) Encouraging atmosphere.
Conclusions
Crisis management practices should be more attentive to personnel needs, ensuring that managerial and psychological support is readily available in crisis situations. Preparedness that ensures effective organizational adaptation also supports personnel well-being during sudden changes in working circumstances.
Peer Review reports
At the onset of the COVID-19 pandemic, healthcare personnel across the globe faced unprecedented challenges. As initial responders in emergency healthcare, paramedics were quickly placed at the front lines of the pandemic, dealing with a range of emergencies in unpredictable conditions [ 1 ]. The pandemic greatly changed the everyday nature of work [ 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 ]. Those working on the front line were suddenly forced to adjust to personal protective equipment (PPE) requirements [ 9 , 10 ] and rapidly changing instructions that caused significant adjustments to their job description [ 11 , 12 ]. For instance, it has been reported that during the initial stages of the COVID-19 pandemic, Emergency Medical Services (EMS) personnel, including paramedics working in prehospital emergency care, experienced a significant increase in stress [ 10 , 13 ] due to several reasons, such as the lack of protection and support, increased demands, lack of personnel, fear of exposure to COVID-19 during missions, concerns of spreading the virus to family members, and frustration over quickly changing work policies [ 11 , 14 , 15 ].
With the unprecedented challenges posed by the COVID-19 pandemic, some research has been directed toward identifying available resources that help in coping with such situations. For example, Sangal et al. [ 15 ] underscored the association between effective communication and reduced work stress and burnout, and emphasized the critical need for two-way communication, consistent messaging, and the strategic consolidation of information prior to its dissemination. In parallel, Dickson et al. [ 16 ] highlight the pivotal role of leadership strategies in fostering a healthful work environment. These strategies include being relationally engaging, visibly present, open, and caring for oneself and others, while embodying core values such as compassion, empathy, courage, and authenticity. Moreover, Awais et al. [ 14 ] identify essential measures to reduce mental distress and support EMS personnel’s overall well-being in pandemic conditions, such as by providing accessible mental health and peer support, ensuring a transparent information flow, and the implementation of clear, best-practice protocols and guidelines. As a lesson learned from COVID-19, Kihlström et al. (2022) add that crisis communication, flexible working conditions, compensation, and allowing for mistakes should be part of crisis management. They also emphasize the importance of psychological support for employees. [ 12 ]
Overall, the COVID-19 pandemic had a multifaceted impact on EMS personnel, highlighting the necessity for comprehensive support and resilience strategies to safeguard their well-being [ 11 , 17 , 18 ] alongside organizational functions [ 12 , 19 ]. For example, in Finland, it has been noted in the aftermath of COVID-19 that the availability and well-being of healthcare workers are key vulnerabilities of the resilience of the Finnish health system [ 12 ]. Effective preparedness planning and organizational resilience benefit from learning from past events and gaining a deeper understanding of observations across different organizational levels [ 12 , 19 , 20 ]. For these reasons, it is important to study how the personnel experienced the changing working circumstances and to recognize the resources, even unexpected ones, that supported their well-being during the initial phase of the COVID-19 pandemic [ 12 , 19 ].
The aim of this study was to examine the emotions experienced and the resources identified as supportive of work well-being during the initial months of the COVID-19 pandemic, from the perspective of the paramedics. Our research questions were: According to the experiences and observations of paramedics, (1) what kinds of emotions did the EMS personnel experience in the new working circumstances, and (2) what work-related factors became resources for the well-being of EMS personnel during the initial months of the COVID-19 pandemic? In this study, emotions are understood as complex responses involving psychological, physiological, and behavioral components, triggered by significant events or situations [ 21 ]. Resources are understood as physical, psychological, social, or organizational aspects of the work that help achieve work goals, reduce demands and associated costs [ 22 ].
Materials and methods
This qualitative study utilized reflective essay material written in the fall of 2020 by experienced, advanced-level paramedics who worked in the Finnish EMS during the early phase of the pandemic, when Finland had declared (March 17, 2020 onward) a state of emergency and implemented the Emergency Powers Act. This allowed for new rules and guidelines from the government to ensure the security of healthcare resources. Some work rules for healthcare personnel changed, and non-urgent services were limited.
Data collection procedures
This study is part of a broader, non-project-based research initiative investigating the work well-being of paramedics from various perspectives, and the data was collected for research purposes from this standpoint. The data collection for this study was conducted at the South-Eastern Finland University of Applied Sciences as part of the Current Issues in EMS Management course. The course participants were experienced, advanced-level Finnish paramedics who were students of the master’s degree program in Development and Management of Emergency Medical Services. A similar data collection method has been utilized in other qualitative studies [for example, 23 , 24 ].
The South-Eastern Finland University of Applied Sciences granted research permission for the data collection on August 20, 2020. The learning platform “Learn” (an adapted version of Moodle [ 25 ]) was used to gather the data. A research notice, privacy statement, and essay writing instructions were published on the platform on August 21, 2020. The paramedics were asked to write about their own experiences and observations regarding how the state of emergency impacted the work well-being of EMS personnel. They were instructed not to use references but only their own reflections. Three guiding questions were asked: “What kind of workloads did EMS personnel experience during the state of emergency?” “How has this workload differed from normal conditions?” and “What effects did this workload have on the well-being of the EMS personnel?”. The assignment did not refer solely to paramedics because the EMS field community may also include individuals with other titles (such as EMS field supervisors or firefighters performing prehospital emergency care); hence the term “EMS personnel” was used.
The essay was part of the mandatory course assignments, but submitting it for research purposes was voluntary. The paramedics were informed that their participation in the study would not affect their course evaluations. They had the freedom to decline, remove parts of, or withdraw the essay before analysis. None of the paramedics exercised these options. They were also informed that the last author removes any identifying details (such as names, places, and organizational descriptions that could reveal their workplace) before sharing the data with other, at the time unnamed, researchers. The last author (female) is a senior researcher specializing in EMS and work well-being topics, a principal lecturer of the respective course, and the head of the respective master’s program, and familiar to all of them through their studies. The paramedics were aware that the essays were graded by the last author on a pass/fail scale as part of the course assessment. However, comprehensive and well-reasoned reflections positively influenced the course grade. The evaluation was not part of this study. The paramedics had the opportunity to ask further questions about the study directly from the last author during and after the essay writing process and the course.
The paramedics wrote the essays between August 23, 2020, and November 30, 2020. Thirty-two paramedics (out of 39) returned their essays using the Learn platform during this timeframe. Thus, seven of the course completions were delayed, and the essays written later were no longer appropriate to include in the data due to the time elapsed since the initial months of the COVID-19 pandemic.
All 32 gave their informed consent for their essays to be included in the study. Essays written by paramedics who had not actively participated in EMS field work during exceptional circumstances were excluded from the material ( n = 2), because they wrote the essay from a different perspective, as they could not reflect on their own experiences and observations. Thus, a total of 30 essays were included in the study. The total material was 106 pages long and comprised 32,621 words in Finnish.
Study participants
Thirty advanced-level paramedics from Finland participated in this study. They all had a bachelor’s degree in emergency care or nursing with additional emergency care specialization. At the time of the study, they were pursuing their master’s studies. Thirteen of them were women, and seventeen were men. The average age of the participants was 33.5 years among women and 35.9 years among men. Women had an average of 8.7 years of work experience, and men had 8.8 years. All the participating paramedics worked in EMS in different areas across Finland (except northern Finland) during their studies and the early phase of the pandemic.
Data analysis
The data was analyzed with a thematic analysis following the process detailed by Braun & Clarke [ 26 ]. First, the two researchers thoroughly familiarized themselves with the data, and the refined aim and research questions of the study were formulated inductively in collaboration based on the content of the data (see [ 26 ], page 84). After this, a thorough coding process was mainly carried out by the first author (female), who holds a master’s degree, is an advanced-level paramedic who worked in EMS during the pandemic, and at the time of the analysis was pursuing her doctoral studies in a different subject area related to EMS. Generating the initial codes involved making notes of interesting features of anything that stood out or seemed relevant to the research question systematically across the entire dataset. During this process, the original paragraphs and sentences were copied from the essay material into a table in Microsoft Word, with each research question in separate documents and each paragraph or sentence in its own row. The content of these data extracts was then coded in the adjacent column, carefully preserving the original content but in a more concise form. Then, the content was analyzed, and codes were combined to identify themes. After that, the authors reviewed the themes together by moving back and forth between the original material, the data in the Word documents, and the potential themes. During this process, the authors worked closely and refined the themes, allowing them to be separated and combined into new themes. For example, emotions depicting frustration and a shift to indifference formed their own theme in this kind of process. Finally, the themes were defined into main, major and minor themes and named. In the results, the main themes form the core in response to the research questions and include the most descriptions from the data. The major themes are significant but not as central as the main themes. Major themes provide additional depth and context to the results. One minor theme was formed as the analysis process progressed, and it provided valuable insights and details that deepened the response to the research question. All the coded data was utilized in the formed themes. The full content of the themes is reported in the Results section.
The emotions experienced by the EMS personnel in their new working circumstances formed three themes: New concerns arose that were constantly present (main theme); Surviving without proper guidance (major theme); and Rapidly approaching breaking point (major theme) (Fig. 1 ). Work-related factors identified as resources for the well-being of EMS personnel formed three themes: A high level of organizational efficiency was achieved (main theme); Adaptable EMS operations (major theme); and Encouraging atmosphere (minor theme) (Fig. 2 ).
Emotions experienced by the EMS personnel in their new working circumstances
Main theme: New concerns arose that were constantly present
The main theme included several kinds of new concerns. In the beginning, the uncertainty about the virus raised concerns about work safety and the means to prevent the spread of the disease. The initial lack of training and routines led to uncertainty. In addition, the decrease in the number of EMS missions raised fears of units being reduced and unilateral decisions by the management to change the EMS personnel’s work responsibilities. The future was also a source of uncertainty in the early stages. For example, the transition to exceptional circumstances, concerns about management and the supervisors’ familiarity with national guidelines and lack of information related to sickness absence procedures, leave, personal career progression, and even the progress of vaccine development, all contributed to this feeling of uncertainty. The initial uncertainty was described as the most challenging phase, but the uncertainty was also described as long-lasting.
Being on the front line with an unknown, potentially dangerous, and easily transmissible virus caused daily concerns about the personnel’s own health, especially when some patients hid their symptoms. The thought of working without proper PPE was frightening. On the other hand, waiting for a patient’s test result was stressful, as it often resulted in many colleagues being quarantined. A constant concern for the health of loved ones and the fear of contracting the virus and unknowingly bringing it home or transmitting it to colleagues led the EMS personnel to change their behavior by limiting contact.
Being part of a high-risk group , I often wondered , in the case of coronavirus , who would protect me and other paramedics from human vanity and selfishness [of those refusing to follow the public health guidelines]? (Participant 25)
The EMS personnel felt a weight of responsibility to act correctly, especially from the perspective of keeping their skills up to date. The proper selection of PPE and aseptic procedures were significant sources of concern, as making mistakes was feared to lead to quarantine and increase their colleagues’ workloads. At the same time, concerns about the adequacy of PPE weighed on the personnel, and they felt pressure on this matter to avoid wastage of PPEs. The variability in the quality of PPE also caused concerns.
Concerns about acting correctly were also tied to ethical considerations and feelings of inadequacy when the personnel were unable to explain to patients why COVID-19 caused restrictions on healthcare services. The presence of students also provoked such ethical concerns. Recognizing patients’ symptoms correctly also felt distressing due to the immense responsibility. This concern was also closely tied to fear and even made some question their career choices. The EMS personnel were also worried about adequate treatment for the patients and sometimes felt that the patients were left alone at home to cope. A reduction in patient numbers in the early stages of the pandemic raised concerns about whether acutely ill individuals were seeking help. At the same time, the time taken to put on PPE stressed the personnel because it increased delays in providing care. In the early phase of the pandemic, the EMS personnel were stressed that patients were not protected from them.
I’m vexed in the workplace. I felt it was immediately necessary to protect patients from us paramedics as well. It wasn’t specifically called for , mostly it felt like everyone had a strong need to protect themselves. (Participant 30)
All these concerns caused a particularly heavy psychological burden on some personnel. They described feeling more fatigued and irritable than usual. They had to familiarize themselves with new guidelines even during their free time, which was exhausting. The situation felt unjust, and there was a looming fear of the entire healthcare system collapsing. COVID-19 was omnipresent. Even at the base station of the EMS services, movement was restricted and social distancing was mandated. Such segregation, even within the professional community, added to the strain and reduced opportunities for peer support. The EMS personnel felt isolated, and thoughts about changing professions increased.
It was inevitable that the segregation of the work community would affect the community spirit , and a less able work community has a significant impact on the individual level. (Participant 8)
Major theme: Surviving without proper guidance
At the onset of the pandemic, the job description of the EMS personnel underwent changes, and employers could suddenly relocate them to other work. There was not always adequate support for familiarizing oneself with the new roles, leading to a feeling of loss of control. The management was described as commanding and restricting the personnel’s actions. As opportunities to influence one’s work diminished, the sense of job satisfaction and motivation decreased.
Some felt that leadership was inadequate and neglectful, especially when the leaders switched to remote work. The management did not take the situation seriously enough, leaving the EMS personnel feeling abandoned. The lack of consistent leadership and failure to listen to the personnel caused dissatisfaction and reduced occupational endurance. In addition, the reduced contact with colleagues and close ones reduced the amount of peer support. The existing models for psychological support were found to be inadequate.
Particularly in the early stages, guidelines were seen as ambiguous and deficient, causing frustration, irritation, and fear. The guidelines also changed constantly, even daily, and it was felt that the information did not flow properly from the management to the personnel. Changes in protection recommendations also led to skepticism about the correctness of the national guidance, and the lack of consistent guidelines perplexed the personnel. Internalizing the guidelines was not supported adequately, but the necessity to grasp new information was described as immense and cognitively demanding.
At times , it felt like the work was a kind of survival in a jungle of changing instructions , one mission at a time. (Participant 11)
Major theme: Rapidly approaching breaking point
Risking one’s own health at work caused contentious feelings while concurrently feeling angry that management could work remotely. The arrogant behavior of people toward COVID-19 left them frustrated, while the EMS personnel had to limit their contacts and lost their annual leave. There were fears about forced labor.
Incomplete and constantly changing guidelines caused irritation and indifference, as the same tasks had to be performed with different levels of PPE within a short time. Some guidelines were difficult to comply with in practice, which was vexing.
Using a protective mask was described as distressing, especially on long and demanding missions. Communication and operation became more difficult. Some described frustration with cleaning PPE meant for single use.
Ensuring the proper implementation of a work pair’s aseptic and equipment maintenance was burdensome, and explaining and repeating guidelines was exhausting. A feeling of indifference was emphasized toward the end of a long shift.
After the initial stage, many began to slip with the PPE guidelines and found the instructions excessive. COVID-19 information transmitted by the emergency center lost its meaning, and instructions were left unheeded, as there was no energy to believe that the patient would have COVID-19, especially if only a few disease cases had been reported in their area.
It was disheartening to hear personnel being labeled as selfish for demanding higher pay during exceptional circumstances. This lack of recognition eroded professionalism and increased thoughts of changing professions.
However , being a doormat and a human toilet , as well as a lack of appreciation , undermines my professionalism and the prolonged situation has led me to seriously consider a different job , where values other than dedication and constant flexibility carry weight. I have heard similar thoughts from other colleagues. None of us do this for money. (Participant 9)
Work-related factors identified as resources for the well-being of EMS personnel
Main theme: A high level of organizational efficiency was achieved
The main theme held several different efficient functions. In the early stages of the pandemic, some felt that the information flow was active. Organizations informed the EMS personnel about the disease, its spread, and its impact on the workplace and emergency care activities.
Some felt that managers were easily accessible during the pandemic, at least remotely. Some managers worked long days to be able to support their personnel.
The response to hate and uncertainty was that one of the supervisors was always present in the morning and evening meetings. Supervisors worked long hours so as to be accessible via remote access. (Participant 26)
The organizations took effective steps to control infections. Quick access to COVID-19 tests, clear guidelines for taking sick leave, and permission to take sick leave with a low threshold were seen as positive things. The consideration of personnel belonging to risk groups by moving them to other work tasks was also perceived as positive. In addition, efforts were made to prevent the emergence of infection chains by isolating EMS personnel in their own social facilities.
Established guidelines, especially on the correct use of protective measures, made it easier to work. Some mentioned that the guidelines were available in ambulances and on phones, allowing the protection guidelines to be checked before going on a mission.
The employers took into account the need for psychological support in a diverse manner. Some organizations provided psychological support such as peer debriefing activities, talking therapy with mental health professionals, actively inquiring about their personnel’s feelings, and training them as support workers. The pandemic situation also caused organizations to create their own standard operating models to decrease mental load.
Fortunately , the problem has now been addressed actively , as a peer-to-peer defusing model was built up at our workplace during the crisis , and group defusing has started , the purpose of which is to lighten the work-related mental load. (Participant 3)
Major theme: Adaptable EMS operations
There were several different resources that clarified mission activities. The amount of protective and cleaning equipment was ramped up, and the treatment equipment was quickly updated to meet the demands brought about by the pandemic and to enable safety distances for the EMS personnel. In addition, various guidelines were amended to reduce exposure. For example, personnel on the dedicated COVID-19 ambulances were separated to work without physical contact with others, and field supervisors joined the EMS missions less often than before. Moreover, people at the scene were contacted by phone in advance to ensure that there would be no exposure risk, which also allowed other occupational safety risks to be identified. New practices resulted from the pandemic, such as cleaning communication equipment during shift changes and regularly using PPE with infected patients. All of these were seen as positive resources for efficient work.
At the end of each shift , all keys , telephones , etc., were cleaned and handed over to the next shift. This practice was not previously established in our area , but this will become a permanent practice in the future and is perceived by everyone in our work community as a positive thing. (Participant 10)
Some stated that access to PPE was sufficient, especially in areas where the number of COVID-19 infections was low. PPE was upgraded to make it easier to wear. Further, organizations acquired a variety of cleaning equipment to speed up the disinfection of ambulances.
Organizations hired more employees to enable leave and the operation of dedicated COVID-19 ambulances. The overall number of ambulances was also increased. Non-urgent missions were handled through enhanced phone services, reducing the unnecessary exposure of EMS personnel to COVID-19.
Five extra holiday substitutes were hired for EMS so that the employer could guarantee the success of agreed leave , even if the Emergency Preparedness Act had given them opportunities to cancel or postpone it. (Participant 12)
Minor theme: Encouraging atmosphere
Peer support from colleagues, a positive, comfortable, pleasant work environment, and open discussion, as well as smooth cooperation with other healthcare employees were felt to be resources for work well-being by reducing the heavy workload experienced. Due to the pandemic, the appreciation of healthcare was felt to increase slightly, which was identified as a resource.
One factor affecting resilience in the healthcare sector is certainly that in exceptional circumstances , visibility and appreciation have somewhat increased. (Participant 23)
This study examined, according to the experiences and observations of paramedics, (1) what kinds of emotions the Emergency Medical Service (EMS) personnel experienced in their new working circumstances, and (2) what work-related factors became resources for the well-being of EMS personnel during the initial months of the COVID-19 pandemic. Each research question was answered with three themes.
Previous studies have shown that the pandemic increased the workload of paramedics, prompting changes in their operating models and the function of EMS to align with new pandemic-related requirements [ 9 , 27 ]. Initially, the paramedics in the current study described facing unclear and deficient guidelines and feeling obligated to follow instructions without adequate support to internalize them. Constantly changing instructions were linked to negative emotions in various ways. Moreover, the overwhelming flood of information was heavily connected to this, although the information flow was also perceived as a resource, especially when it was timely and well-structured. The study by Sangal et al. [ 15 ] has raised similar observations and points out the importance of paying special attention to the personnel working in the frontline, as in EMS, who might be more heavily impacted by too much information and anxiety about it. They also discovered that three factors are crucial for addressing the challenges of information overload and anxiety: consolidating information before distributing it, maintaining consistent communication, and ensuring communication is two-way. McAlearney et al. [ 11 ] found that first responders, including EMS personnel, reported frustration regarding COVID-19 information because of inconsistencies between sources, misinformation on social media, and the impact of politics. A Finnish study also recognized that health systems were not sufficiently prepared for the flood of information in the current media environment [ 12 ]. Based on these previous results and our findings, it can be concluded that proper implementation of crisis communication should be an integral part of organizations’ preparedness in the future, ensuring that communication effectively supports employee actions in real-life situations. Secondly, this topic highlights the need for precise guidelines and their implementation. With better preparedness, similar chaos could be avoided in the future [ 17 ].
Many other factors also caused changes in work. The EMS mission profile changed [ 3 , 4 , 5 , 6 ], where paramedics in this study saw concerns. To prevent infection risk, the number of pre-arrival calls increased [ 7 ], the duration of EMS missions increased [ 8 , 9 ], and the continuous use of PPE and enhanced hygiene standards imposed additional burdens [ 9 , 10 ]. In Finland, there was no preparedness for the levels of PPE usage required in the early stages of the pandemic [ 12 ]. In this study, paramedics described that working with potentially inadequate PPE caused fear and frustration, which was increased by a lack of training, causing them to feel a great deal of responsibility for acting aseptically and caring for patients correctly. Conversely, providing adequate PPE, information and training has been found to increase the willingness to work [ 28 ] and the sense of safety in working in a pandemic situation [ 29 ], meaning that the role of precise training, operating instructions and leadership in the use of PPE is emphasized [ 30 ].
The paramedics in this study described many additional new concerns in their work, affecting their lives comprehensively. It has been similarly described that the pandemic adversely affected the overall well-being of healthcare personnel [ 31 ]. The restrictions implemented also impacted their leisure time [ 32 ], and the virus caused concerns for their own and their families’ health [ 11 , 28 ]. In line with this, the pandemic increased stress, burnout [ 10 , 33 ], and anxiety among EMS personnel and other healthcare personnel working on the frontline [ 11 , 14 , 34 , 35 ]. These kinds of results underscore the need for adequate guidance and support, a lack of which paramedics reported experiencing in the current study.
Personnel play a crucial role in the efficient operation of an organization and comprise the main identified resource in this study. Previous studies and summaries have highlighted that EMS personnel did not receive sufficient support during the COVID-19 pandemic [ 11 , 14 , 17 , 18 ]. Research has also brought to light elements of adequate support related to the pandemic, such as a review by Dickson et al. [ 16 ] that presents six tentative theories for healthful leadership, all of which are intertwined with genuine encounter, preparedness, and information use. In this current study, the results showed numerous factors related to these contexts that were identified as resources, specifically underlined by elements of caring, effective operational change, knowledge-based actions, and present leadership, similarly described in a study by Eaton-Williams & Williams [ 18 ]. Moreover, the paramedics in our study highlighted the importance of encouragement and identified peer support from colleagues as a resource, which is in line with studies in the UK and Finland [ 12 , 23 , 37 ].
In the early stages of the pandemic, it was noted that the EMS personnel lacked adequate training to manage their mental health, and there was a significant shortage of psychosocial support measures [ 14 ], although easy access to support would have been significant [ 18 ]. In the current study, some paramedics felt that mental health support was inadequate and delayed, while others observed an increase in mental health support during the pandemic, seeing it as an incentive for organizations to develop standard operating models for mental support, for example. This awakening was identified as a resource. This is consistent, as providing psychological support to personnel has been highlighted as a core aspect of crisis management in a Finnish study assessing health system resilience related to COVID-19 [ 12 ]. In a comprehensive recommendation commentary, Isakov et al. [ 17 ] suggest developing a national strategy to improve resilience by addressing the mental health consequences of COVID-19 and other occupational stressors for EMS personnel. This concept, applicable beyond the US, supports the view that EMS organizations are becoming increasingly aware of the need to prepare for and invest in this area.
A fundamental factor likely underlying all the described emotions was that changes in the job descriptions of the EMS personnel due to the pandemic were significant and, in part, mandated from above. In this study, paramedics described feelings of concern and frustration related to these many changes and uncertainties. According to Zamoum and Gorpe (2018), efficient crisis management emphasizes the importance of respecting emotions, recognizing rights, and making appropriate decisions. Restoring trust is a significant challenge in a crisis situation, one that cannot be resolved without complete transparency and open communication [ 38 ]. This perspective is crucial to consider in planning for future preparedness. Overall, the perspective of employee rights and obligations in exceptional circumstances has been relatively under-researched, but in Australia, grounding research on this perspective has been conducted with paramedics using various approaches [ 39 , 40 , 41 ]. The researchers conclude that there is a lack of clarity about the concept of professional obligation, specifically regarding its boundaries, and the issue urgently needs to be addressed by developing clear guidelines that outline the obligation to respond, both in normal day-to-day operations and during exceptional circumstances [ 39 ].
Complex adaptive systems (CAS) theory recognizes that in a resilient organization, different levels adapt to changing environments [ 19 , 20 ]. Barasa et al. (2018) note that planned resilience and adaptive resilience are both important [ 19 ]. Kihlström et al. (2022) note that the health system’s resilience was strengthened by a certain expectation of crisis, and they also recognized further study needs on how effectively management is responding to weak signals [ 12 ]. This could be directly related to how personnel can prepare for future changes. The results of this study revealed many negative emotions related to sudden changes, but at the same time, effective organizational adaptation was identified as a resource for the well-being of EMS personnel. Dissecting different elements of system adaptation in a crisis has been recognized as a highly necessary area for further research [ 20 ]. Kihlström et al. (2022) emphasize the importance of ensuring a healthy workforce across the entire health system. These frameworks suggest numerous potential areas for future research, which would also enhance effective preparedness [ 12 ].
Limitations of the study
In this study, we utilized essay material written in the fall of 2020, in which experienced paramedics reflected on the early stages of the COVID-19 pandemic from a work-oriented perspective. The essays were approached inductively, meaning that they were not directly written to answer our research questions, but the aim and the research questions were shaped based on the content [ 26 ]. The essays included extensive descriptions that aligned well with the aim of this study. However, it is important to remember when interpreting the results that asking specifically about this topic, for instance, in an interview, might have yielded different descriptions. It can be assessed that the study achieved a tentative descriptive level, as the detailed examination of complex phenomena such as emotions and resources would require various methods and observations.
Although the essays were mostly profound, well-thought-out, and clearly written, their credibility [ 42 ] may be affected by the fact that several months had passed between the time the essays were written and the events described. Memories may have altered, potentially influencing the content of the writings. Diary-like material from the very onset of the pandemic might have yielded more precise data, and such a data collection method could be considered in future research on exceptional circumstances.
The credibility [ 42 ] could also have been enhanced if the paramedics who wrote the essays had commented on the results and provided additional perspectives on the material and analysis through a multi-phase data collection process. This was not deemed feasible in this study, mainly because there was a 2.5-year gap between data collection and the start of the analysis. However, this also strengthened the overall trustworthiness of the study, as it allowed the first author, who had worked in prehospital emergency care during the initial phase of the pandemic, to maintain a distance from the subject, and enabled a comparison of our own findings with previously published research that investigated the same period in different contexts. The comparison was made when writing the discussion, with the analysis itself being inductive and following the thematic analysis process described by Braun & Clarke [ 26 ].
When evaluating credibility [ 42 ], it should also be noted that the participants who wrote the essays, i.e., the data for the study, were experienced paramedics but also students and one of the researchers was their principal lecturer. This could potentially limit credibility if the students, for some reason, did not want to produce truthful content for their lecturer to read. However, this risk can be considered small because the essays’ topics did not concern the students’ academic progress, the essays’ content was quite consistent, and the results aligned with other studies. As a strength, it can be considered that the students shared their experiences without holding back, as the thoughts were not for workplace use, and they could trust the data privacy statement.
To enhance transferability [ 42 ], the context of the study was described in detail, highlighting the conditions prevailing in Finnish prehospital emergency care during the early stages of the pandemic. Moreover, including a diverse range of perspectives from paramedics working in different regions of Finland (except Northern Finland) contributes to the transferability of the study, indicating that the results may be applicable and relevant to a wider context beyond a single specific region.
Dependability [ 42 ] was reinforced by the close involvement of two researchers from different backgrounds in the analysis of the material, but a limitation is that no separate analyses were conducted. However, the original data was repeatedly revisited during the analysis, which strengthened the dependability. Moreover, the first author kept detailed notes throughout the analysis process, and the last author supervised the progress while also contributing to the analysis and reporting. The research process is also reported in detail.
This study highlighted numerous, mainly negative emotions experienced by EMS personnel during the initial months of the COVID-19 pandemic due to new working circumstances. At the same time, several work-related factors were identified as resources for their well-being. The findings suggest that crisis management practices should be more attentive to personnel needs, ensuring that personnel have the necessary support, both managerial and psychological, readily available in crisis situations. Effective organizational adaptation in a crisis situation also supports personnel well-being, emphasizing the importance of effective preparedness. Future research should particularly focus on considering personnel well-being as part of organizational adaptation during exceptional circumstances and utilize these findings to enhance preparedness.
Data availability
The datasets generated and analyzed during the current study are not publicly available due to the inclusion of sensitive information and the extent of the informed consent provided by the participants.
Abbreviations
Complex Adaptive Systems (theory)
Coronavirus Disease 2019
Emergency Medical Services
Personal Protective Equipment
United Kingdom
Drennan IR, Blanchard IE, Buick JE. Opportunity for change: is it time to redefine the role of paramedics in healthcare? CJEM. 2021;23(2):139–40. https://doi.org/10.1007/s43678-021-00105-y
Boechler L, Cameron C, Smith JC, Ford-Jones P, Suthers P. Impactful approaches to Leadership on the Front lines of the COVID-19 pandemic: lived experiences of Canadian paramedics. Healthc Q. 2021;24(3):42–7. https://doi.org/10.12927/hcq.2021.26620 .
Article PubMed Google Scholar
Lerner EB, Newgard CD, Mann NC. Effect of the Coronavirus Disease 2019 (COVID-19) pandemic on the U.S. Emergency Medical Services System: a preliminary Report. Acad Emerg Med. 2020;27(8):693–9. https://doi.org/10.1111/acem.14051 .
Article PubMed PubMed Central Google Scholar
O’Connor AW, Hannah HA, Burnor EA, Fukutaki KG, Peterson T, Ballard DW, et al. Emergency Medical Service Utilization and response following COVID-19 emergency and stay-at-home policies: an interrupted time-series analysis. Cureus. 2021;21(11). https://doi.org/10.7759/cureus.19794 .
Azbel M, Heinänen M, Lääperi M, Kuisma M. Effects of the COVID-19 pandemic on trauma-related emergency medical service calls: a retrospective cohort study. BMC Emerg Med. 2021;9(1):102. https://doi.org/10.1186/s12873-021-00495-3 .
Article CAS Google Scholar
Lane DJ, Blanchard IE, Buick JE, Shaw M, McRae AD. Changes in presentation, presenting severity and disposition among patients accessing emergency services during the first months of the COVID-19 pandemic in Calgary, Alberta: a descriptive study. CMAJ Open. 2021;9(2):592–601. https://doi.org/10.9778/cmajo.20200313 .
Article Google Scholar
Shukla V, Lau CSM, Towns M, Mayer J, Kalkbrenner K, Beuerlein S, et al. COVID-19 exposure among First Responders in Arizona. J Occup Environ Med. 2020;62(12):981–5. https://doi.org/10.1097/JOM.0000000000002027 .
Article CAS PubMed Google Scholar
Andrew E, Nehme Z, Stephenson M, Walker T, Smith K. The impact of the COVID-19 pandemic on demand for emergency ambulances in Victoria, Australia. Prehosp Emerg Care. 2021;16:1–7. https://doi.org/10.1080/10903127.2021.1944409 .
Eskol JR, Zegers FD, Wittrock D, Lassen AT, Mikkelsen S. Increased ambulance on-scene times but unaffected response times during the first wave of the COVID-19 pandemic in Southern Denmark. BMC Emerg Med. 2022;9(1):61. https://doi.org/10.1186/s12873-022-00623-7 .
Schumann H, Böckelmann I, Thielmann B. Relaxation and strain among emergency medical service personnel and emergency control center dispatchers during the first two waves of the SARS-CoV-2 pandemic. Med Pr. 2023;15(5):353–62. https://doi.org/10.13075/mp.5893.01401 .
McAlearney AS, Gaughan AA, MacEwan SR, Gregory ME, Rush LJ, Volney J, et al. Pandemic experience of first responders: fear, frustration, and stress. Int J Environ Res Public Health. 2022;13(8):4693. https://doi.org/10.3390/ijerph19084693 .
Kihlström L, Huhtakangas M, Karreinen S, Viita-Aho M, Keskimäki I, Tynkkynen LK. Local cooperation has been the cornerstone: facilitators and barriers to resilience in a decentralized health system during COVID-19 in Finland. J Health Organ Manag. 2022. https://doi.org/10.1108/JHOM-02-2022-0069 .
Hendrickson RC, Slevin RA, Hoerster KD, Chang BP, Sano E, McCall CA, et al. The impact of the COVID-19 pandemic on Mental Health, Occupational Functioning, and Professional Retention among Health Care workers and First Responders. J Gen Intern Med. 2022;37(2):397–408. https://doi.org/10.1007/s11606-021-07252-z .
Awais SB, Martins RS, Khan MS. Paramedics in pandemics: protecting the mental wellness of those behind enemy lines. Br J Psychiatry. 2021;218(2):75–6. https://doi.org/10.1192/bjp.2020.193 .
Sangal RB, Bray A, Reid E, Ulrich A, Liebhardt B, Venkatesh AK, et al. Leadership communication, stress, and burnout among frontline emergency department staff amid the COVID-19 pandemic: a mixed methods approach. Healthc (Amst). 2021;9(4):100577. https://doi.org/10.1016/j.hjdsi.2021.100577 .
Dickson CAW, Davies C, McCormack B, Westcott L, Merrell J, Mcilfatrick S, et al. UK nurses’ and midwives’ experiences of healthful leadership practices during the COVID-19 pandemic: a rapid realist review. J Nurs Manag. 2022;30(8):3942–57. https://doi.org/10.1111/jonm.13790 .
Isakov A, Carr M, Munjal KG, Kumar L, Gausche-Hill MEMS. Agenda 2050 meets the COVID-19 pandemic. Health Secur. 2022;20(S1):S97–106. https://doi.org/10.1089/hs.2021.0179 .
Eaton-Williams PJ, Williams J. See us as humans. Speak to us with respect. Listen to us. A qualitative study on UK ambulance staff requirements of leadership while working during the COVID-19 pandemic. BMJ Lead. 2023;7(2):102–7. https://doi.org/10.1136/leader-2022-000622 .
Barasa E, Mbau R, Gilson L. What is resilience and how can it be nurtured? A systematic review of empirical literature on Organizational Resilience. Int J Health Policy Manag. 2018;7(6):491–503. https://doi.org/10.15171/ijhpm.2018.06 .
Coetzee C, Van Niekerk D, Raju E. Disaster resilience and complex adaptive systems theory: finding common grounds for risk reduction. Disaster Prev Manage. 2016;25(2):196–211. https://doi.org/10.1108/DPM-07-2015-0153 .
American Psychological Association. Emotion. APA Dictionary of Psychology. https://dictionary.apa.org/emotion . Accessed on 26.6.2024.
Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands-resources model of burnout. J Appl Psychol. 2001;86(3):499–512.
Ericsson CR, Lindström V, Rudman A, Nordquist H. Paramedics’ perceptions of job demands and resources in Finnish emergency medical services: a qualitative study. BMC Health Serv Res. 2022;22(1):1469. https://doi.org/10.1186/s12913-022-08856-9 .
Rinkinen T, Kinnula M, Nordquist H. Technological development roles and needs in pre-hospital emergency care from the advanced level paramedics’ perspective. Int Emerg Nurs. 2024;73:101406. https://doi.org/10.1016/j.ienj.2024.101406 .
Moodle Pty Ltd. 2020. https://moodle.org/ . Accessed on date 17.6.2024.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:2:77–101. https://doi.org/10.1191/1478088706qp063oa .
Prezant DJ, Lancet EA, Zeig-Owens R, Lai PH, Appel D, Webber MP, et al. System impacts of the COVID-19 pandemic on New York City’s emergency medical services. J Am Coll Emerg Physicians Open. 2020;9(6):1205–13. https://doi.org/10.1002/emp2.12301 .
Alwidyan MT, Oteir AO, Trainor J. Working during pandemic disasters: views and predictors of EMS providers. Disaster Med Public Health Prep. 2022;16(1):116–22. https://doi.org/10.1017/dmp.2020.131 .
Rebmann T, Charney RL, Loux TM, Turner JA, Abbyad YS, Silvestros M. Emergency Medical Services Personnel’s pandemic influenza training received and willingness to work during a future pandemic. Prehosp Emerg Care. 2020;24(5):601–9. https://doi.org/10.1080/10903127.2019.1701158 .
Article CAS PubMed PubMed Central Google Scholar
McCann-Pineo M, Li T, Barbara P, Levinsky B, Berkowitz J. Factors influencing Use of Personal Protective Equipment among Emergency Medical services Responders during the COVID-19 pandemic: a Retrospective Chart Review. West J Emerg Med. 2022;23(3):396–407. https://doi.org/10.5811/westjem.2022.2.55217 .
Vanhaecht K, Seys D, Bruyneel L, Cox B, Kaesemans G, Cloet M, et al. COVID-19 is having a destructive impact on health-care workers’ mental well-being. Int J Qual Health Care. 2021;20(1):mzaa158. https://doi.org/10.1093/intqhc/mzaa158 .
Zolnikov TR, Furio F. First responders and social distancing during the COVID-19 pandemic. J Hum Behav Soc Environ. 2021;31(1–4):244–53. https://doi.org/10.1080/10911359.2020.1811826 .
Spychała A, Piwowarska M, Piekut A. The COVID-19 pandemic as a stress factor in the work of a paramedic. Med Pr. 2023;8(1):9–17. https://doi.org/10.13075/mp.5893.01278 .
Roberts R, Wong A, Jenkins S, Neher A, Sutton C, O’Meara P, et al. Mental health and well-being impacts of COVID-19 on rural paramedics, police, community nurses and child protection workers. Aust J Rural Health. 2021;29(5):753–67. https://doi.org/10.1111/ajr.12804 .
Chang YT, Hu YJ. Burnout and Health issues among Prehospital Personnel in Taiwan Fire Departments during a Sudden Spike in Community COVID-19 cases: a cross-sectional study. Int J Environ Res Public Health. 2022;16(4):2257. https://doi.org/10.3390/ijerph19042257 .
Mausz J, Donnelly EA, Moll S, Harms S, McConnell M. Mental disorder symptoms and the relationship with resilience among paramedics in a single Canadian site. Int J Environ Res Public Health. 2022;17(8):4879. https://doi.org/10.3390/ijerph19084879 .
Phung VH, Sanderson K, Pritchard G, Bell F, Hird K, Wankhade P, et al. The experiences and perceptions of wellbeing provision among English ambulance services staff: a multi-method qualitative study. BMC Health Serv Res. 2022;15(1):1352. https://doi.org/10.1186/s12913-022-08729-1 .
Zamoum K, Gorpe TS. Crisis Management: a historical and conceptual Approach for a better understanding of today’s crises. Crisis Manage - Theory Pract InTech. 2018. https://doi.org/10.5772/intechopen.76198 .
Anderson C, Pooley JA, Mills B, Anderson E, Smith EC. Do paramedics have a Professional Obligation to work during a pandemic? A qualitative exploration of Community Member expectations. Disaster Med Public Health Prep. 2020;14(3):406–12. https://doi.org/10.1017/dmp.2020.212 .
Smith E, Burkle FM, Gebbie K, Ford D, Bensimon C. Acceptable limitations on Paramedic Duty to treat during disaster: a qualitative exploration. Prehosp Disaster Med. 2018;33(5):466–70. https://doi.org/10.1017/S1049023X18000857 .
Smith E, Burkle F, Gebbie K, Ford D, Bensimon C. A qualitative study of paramedic duty to treat during disaster response. Disaster Med Public Health Prep. 2019;13(2):191–6. https://doi.org/10.1017/dmp.2018.15 .
Cypress BS. Rigor or reliability and validity in qualitative research: perspectives, strategies, reconceptualization, and recommendations. Dimens Crit Care Nurs. 2017;36(4):253–63. https://doi.org/10.1097/DCC.0000000000000253 .
TENK. Guidelines for the responsible conduct of research and for handling allegations of misconduct in Finland [Internet]. Helsinki: Finnish National Board on Research Integrity TENK; 2023. https://tenk.fi/sites/default/files/2023-11/RI_Guidelines_2023.pdf . Accessed 13 Jan 2024.
TENK. Ethical review in human sciences [Internet]. Helsinki: Finnish National Board on Research Integrity TENK; 2020. https://tenk.fi/sites/default/files/2021-1/Ethical_review_in_human_sciences_2020.pdf . Accessed 13 Jan 2024.
Download references
Acknowledgements
We want to sincerely thank all the paramedics who participated in this study.
Open access funded by Helsinki University Library.
Open Access funding provided by University of Helsinki (including Helsinki University Central Hospital).
Author information
Authors and affiliations.
Faculty of Medicine, University of Helsinki, Helsinki, Finland
Henna Myrskykari
Emergency Medical Services, University of Turku and Turku University Hospital, Turku, Finland
Department of Healthcare and Emergency Care, South-Eastern Finland University of Applied Sciences, Kotka, Finland
Hilla Nordquist
You can also search for this author in PubMed Google Scholar
Contributions
Study design (HM, HN). Data collection (HN). Methodology (HN). Analysis (HM, HN). Writing (HM, HN). Review and editing (HM, HN). Supervision (HN). Both authors read and approved the final manuscript.
Corresponding author
Correspondence to Henna Myrskykari .
Ethics declarations
Ethics approval and consent to participate.
The study followed the good scientific practice defined by the Finnish National Board on Research Integrity TENK [ 43 ]. The study was conducted in accordance with the Helsinki Declaration and applicable national guidelines. Adhering to the Finnish National Board on Research Integrity (TENK) guidelines on ethical principles of research with human participants and ethical review in the human sciences in Finland, an ethical review statement from a human sciences ethics committee was not required for this type of study. The participants consisted of adult students engaged in regular employment. Their involvement in the research was grounded on informed consent. The study did not involve concerns regarding the participants’ physical integrity, nor were they subjected to exceptionally strong stimuli. The potential for causing mental harm was not beyond what is typically encountered in everyday life, and their participation did not pose any safety risks [ 44 ].
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Myrskykari, H., Nordquist, H. Paramedics’ experiences and observations: work-related emotions and well-being resources during the initial months of the COVID-19 pandemic—a qualitative study. BMC Emerg Med 24 , 152 (2024). https://doi.org/10.1186/s12873-024-01072-0
Download citation
Received : 25 April 2024
Accepted : 13 August 2024
Published : 26 August 2024
DOI : https://doi.org/10.1186/s12873-024-01072-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Emergency medical services
- Health personnel
- Qualitative research
BMC Emergency Medicine
ISSN: 1471-227X
- General enquiries: [email protected]
- Election 2024
- Entertainment
- Newsletters
- Photography
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election results
- Google trends
- AP & Elections
- U.S. Open Tennis
- Paralympic Games
- College football
- Auto Racing
- Movie reviews
- Book reviews
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Zuckerberg says the White House pressured Facebook over some COVID-19 content during the pandemic
Meta CEO Mark Zuckerberg says senior Biden administration officials pressured Facebook to “censor” some COVID-19 content during the pandemic. He vowed that the social media giant would push back if it faced such demands again.
- Copy Link copied
WASHINGTON (AP) — Meta CEO Mark Zuckerberg says senior Biden administration officials pressured Facebook to “censor” some COVID-19 content during the pandemic and vowed that the social media giant would push back if it faced such demands again.
In a letter to Rep. Jim Jordan, the Republican chair of the House Judiciary Committee, Zuckerberg alleges that the officials, including those from the White House, “repeatedly pressured” Facebook for months to take down “certain COVID-19 content including humor and satire.”
The officials “expressed a lot of frustration” when the company didn’t agree, he said in the letter.
“I believe the government pressure was wrong and I regret that we were not more outspoken about it,” Zuckerberg wrote in the letter dated Aug. 26 and posted on the committee’s Facebook page and to its account on X.
The letter is the latest repudiation by Zuckerberg of efforts to target misinformation around the coronavirus pandemic during and after the 2020 presidential election, particularly as allegations have emerged that some posts were deleted or restricted wrongly.
“I also think we made some choices that, with the benefit of hindsight and new information, we wouldn’t make today,” he said, without elaborating. “We’re ready to push back if something like this happens again.”
In response, the White House said in a statement that, “When confronted with a deadly pandemic, this Administration encouraged responsible actions to protect public health and safety. Our position has been clear and consistent: we believe tech companies and other private actors should take into account the effects their actions have on the American people, while making independent choices about the information they present.”
Experts warn this year’s U.S. election could be swamped by misinformation on social media with the proliferation of artificial intelligence and other tools to produce false news stories and content that could mislead voters.
Facebook in early 2021 appended what Zuckerberg called labels with “credible information” to posts about COVID-19 vaccines. That’s after it moved in April 2020 — just as the virus had led to global shutdowns and radical changes in everyday life — to warn users who shared misinformation about COVID-19.
Conservatives have long derided Facebook and other major tech companies as favoring liberal priorities and accused them of censorship.
Zuckerberg has tried to change the company’s perception on the right, going on podcaster Joe Rogan’s show in 2022 and complimenting Republican nominee Donald Trump’s response to an assassination attempt as “badass.” He sent Monday’s letter to the House Judiciary Committee, whose chairman, Jordan, is a longtime Trump ally.
Zuckerberg also said he would no longer donate money to widen election access for voters through the Chan Zuckerberg Initiative, the company that runs the philanthropy for him and his wife, Priscilla Chan.
The couple previously donated $400 million to help local election offices prepare for voters in the 2020 presidential election, with funds used for protective equipment to prevent the spread of the coronavirus at polling sites, drive-thru voting locations and equipment to process mail ballots.
“I know that some people believe this work benefited one party over the other” despite analyses showing otherwise, he said. “My goal is to be neutral and not play a role one way or another - or to even appear to be playing a role. So I don’t plan on making a similar contribution this cycle.”

IMAGES
VIDEO
COMMENTS
Reading time: 3 min (864 words) The COVID-19 pandemic has led to a dramatic loss of human life worldwide and presents an unprecedented challenge to public health, food systems and the world of work. The economic and social disruption caused by the pandemic is devastating: tens of millions of people are at risk of falling into extreme poverty ...
COVID-19 is a worldwide pandemic that puts a stop to economic activity and poses a severe risk to overall wellbeing. The global socio-economic impact of COVID-19 includes higher unemployment and poverty rates, lower oil prices, altered education sectors, changes in the nature of work, lower GDPs and heightened risks to health care workers. ...
1. Introduction. The coronavirus disease 2019 (COVID-19) pandemic has led to unprecedented changes in people's daily lives, with implications for mental health and well-being [1-4], both at the level of a given country's population, and when considering specific vulnerable groups [5-7].In order to mitigate the untoward impact of the pandemic (including lockdown) and support mental health ...
This essay examines key aspects of social relationships that were disrupted by the COVID-19 pandemic. It focuses explicitly on relational mechanisms of health and brings together theory and emerging evidence on the effects of the COVID-19 pandemic to make recommendations for future public health policy and recovery. We first provide an overview of the pandemic in the UK context, outlining the ...
6. COVID-19 has already changed science immensely, but if scientists are savvy, the most profound pivot is still to come—a grand reimagining of what medicine should be. In 1848, the Prussian ...
Alex, a writer and fellow disabled parent, found the freedom to explore a fuller version of herself in the privacy the pandemic provided. "The way I dress, the way I love, and the way I carry ...
Writing About COVID-19 in College Essays. Experts say students should be honest and not limit themselves to merely their experiences with the pandemic. The global impact of COVID-19, the disease ...
The novel coronavirus disease 2019 (COVID-19), caused by the pathogen severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), originated in Wuhan, China, and has now spread internationally with over 4·3 million individuals infected and over 297 000 deaths as of May 14, 2020, according to the Johns Hopkins Coronavirus Resource Center. While COVID-19 has been termed a great equaliser ...
As COVID-19 continues to creep its way into each of our communities and impact the way we live and communicate, I find solace in the fact that we face what comes next together, as humanity. When the day comes that my generation is responsible for dealing with another crisis, I hope we can use this experience to remind us that moving forward ...
Read these 12 moving essays about life during coronavirus. Artists, novelists, critics, and essayists are writing the first draft of history. A woman wearing a face mask in Miami. Alissa Wilkinson ...
The spread of the "Severe Acute Respiratory Coronavirus 2" (SARS-CoV-2), the causal agent of COVID-19, was characterized as a pandemic by the World Health Organization (WHO) in March 2020 and has triggered an international public health emergency [].The numbers of confirmed cases and deaths due to COVID-19 are rapidly escalating, counting in millions [], causing massive economic strain ...
South Korea beat back that potentially catastrophic outbreak, and continued to greatly limit its cases. They had fewer than 1,000 deaths in all of 2020. In the United States, that would translate ...
The Journal of Vocational Behavior has not traditionally published essays, but these are such unusual times, and COVID-19 is so relevant to our collective research on work that I thought it was a good idea. I issued an invitation to the Associate Editors to submit a brief (3000 word) essay on the implications of COVID-19 on work and/or workers ...
The transition to an online education during the coronavirus disease 2019 (COVID-19) pandemic may bring about adverse educational changes and adverse health consequences for children and young adult learners in grade school, middle school, high school, college, and professional schools. The effects may differ by age, maturity, and socioeconomic ...
The outbreak of the coronavirus disease 2019 (COVID-19) has created a global health crisis that had a deep impact on the way we perceive our world and our everyday lives. Not only has the rate of contagion and patterns of transmission threatened our sense of agency, but the safety measures to contain the spread of the virus also required social ...
The 25 most downloaded Nature Communications articles* on COVID-19 published in 2021 illustrate the collaborative efforts of the international community to combat the ongoing pandemic.These papers ...
VOL. 387 NO. 11. The coronavirus disease 2019 (Covid-19) pandemic has claimed an estimated 15 million lives, including more than 1 million lives in the United States alone. The rapid development ...
Coronavirus disease (COVID-19) Coronavirus disease (COVID-19) is an infectious disease caused by the SARS-CoV-2 virus. Most people infected with the virus will experience mild to moderate respiratory illness and recover without requiring special treatment. However, some will become seriously ill and require medical attention.
In a post-Covid-19 world, a new international order will be redrawn by the powerful countries taking into account the lessons learnt in dealing with the current pandemic. The role of international institutions will also be critically reviewed. Developing countries with low GDP growth, high debt and dependence on oil and essential technologies ...
Future historians may look back on the journals, essays and art that ordinary people are creating now to tell the story of life during the coronavirus. But writing can also be deeply therapeutic.
COVID-19 has become the herald event that now fully exposes the deep and chronic social wounds in US communities. What makes this particularly egregious is that unlike the known risk factors for which physicians and others can stridently offer clear advice regarding prevention, these concerns—the burden of ill health, limited access to ...
In conclusion, COVID-19 tested the patience and resilience of the mankind. This pandemic has taught people the importance of patience, effort and humbleness. Also Read: Essay on My Best Friend. Essay On COVID-19 in 300 Words. COVID-19, also known as the coronavirus, is a serious and contagious disease that has affected people worldwide.
T he public health emergency related to the COVID-19 pandemic officially ended on May 11, 2023. It was a purely administrative step. It was a purely administrative step. Viruses do not answer to ...
The COVID-19 pandemic has had a profound impact on individuals, societies, and economies worldwide. Its multifaceted nature presents a wealth of topics suitable for academic exploration. This essay provides guidance on developing engaging and insightful essay topics related to COVID-19, offering a comprehensive range of perspectives to choose from.
COVID-19 is still killing hundreds of Americans every week. What strain is the new COVID-19 shot based on and why? The COVID-19 vaccine has been updated several times since the original shot in ...
Presently the impacts of COVID-19 in daily life are extensive and have far reaching consequences. These can be divided into various categories: Closure of places for entertainment such as movie and play theatres, sports clubs, gymnasiums, swimming pools, and so on. This COVID-19 has affected the sources of supply and effects the global economy.
The purpose of this phenomenological study was to address a lack of research on health science students' perceptions and use of health precautions during the COVID-19 pandemic. Albert Bandura's Social Cognitive Theory frames this study of bachelor's, master's and doctoral level students at Liberty University, George Mason University, and Norfolk State University. Data was gathered via ...
It is clear that mpox clade Ib is nowhere near as transmissible as respiratory viruses such as SARS-CoV-2, and thus it almost certainly won't cause a pandemic on the scale of covid-19. However ...
The essays used in this study were written during the fall of 2020 and reflected the period when Finland had declared a state of emergency (on 17.3.2020) and the Emergency Powers Act was implemented. ... COVID-19 significantly impacted their working circumstances. We examined, according to the experiences and observations of paramedics, (1 ...
WASHINGTON (AP) — Meta CEO Mark Zuckerberg says senior Biden administration officials pressured Facebook to "censor" some COVID-19 content during the pandemic and vowed that the social media giant would push back if it faced such demands again.. In a letter to Rep. Jim Jordan, the Republican chair of the House Judiciary Committee, Zuckerberg alleges that the officials, including those ...