Exploring Medical Tourism Opportunities in India (With Special Reference to Delhi/ NCRZ)
Proceedings of 10th International Conference on Digital Strategies for Organizational Success
7 Pages Posted: 23 Jan 2019

Avinash Chandra
Bundelkhand University
Date Written: January 6, 2019
Medical Tourism is the fastest growing sector of healthcare throughout the world. We can say during the last decade medical tourism is continuously gaining popularity, patients are more educated than ever and are going online to research information and are travelling to where they can get the best quality care at an affordable price. India, has great number of advantages with regard to medical tourism such as many private and government hospitals, availability of internationally trained medical staff, availability of international airports at all major medical tourism destination and plethora of historical and touristic attractions but despite of all these facilities our medical tourism segment is not fully utilized and it has an insignificant market share and limited available services. The Government of India has taken various initiatives like National Health Policy in 2002, Creating a department of Ayush for the complementary and alternative medicines and treatments, initiating the marketing development schemes for travel agents to promote medical tourism through proper marketing and also encouraging public – private partnership and medical visa (M-Visa) up to one year, which can be extended further up to one year. In spite of all these steps taken by Indian government the Indian tourism market is concentrated to only some major cities such as MUMBAI, CHENNAI, KERALA AND BANGLORE. Since the growth potential of medical tourism seems to be promising more destinations are needed to be developed to meet the need of medical tourism markets. Delhi is being capital of India and having number of reputed government and private hospital of world class standard has great potential of becoming medical hub of world. The current study aims to project the strength and challenges of medical tourism scenario in India with Special Reference to Delhi and NCR. I choose this topic for research work with objectives to investigate the new trends in medical field, to find out the potential of Delhi-NCR as medical tourism destination, to investigate factors that are responsible for choosing Delhi as health care destination by tourist. My research work will help in identifying different challenges and opportunities in DELHI-NCR for medical treatment. I am optimistic that the findings of the research work will help in promoting DELHI-NCR as medical hub of not only India but the world.
Keywords: Medical, Tourism, Health Policy
Suggested Citation: Suggested Citation
Avinash Chandra (Contact Author)
Bundelkhand university ( email ).
NH- 25 Jhansi, Uttar Pradesh India
Do you have a job opening that you would like to promote on SSRN?
Paper statistics, related ejournals, global health ejournal.
Subscribe to this fee journal for more curated articles on this topic
Transportation, Economy & Society eJournal
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Philos Ethics Humanit Med

Medical tourism in india: perceptions of physicians in tertiary care hospitals
Imrana qadeer.
1 Center of Social Medicine and Community Health, School of Social Sciences, Jawaharlal Nehru University, New Delhi 110067, India
Sunita Reddy
Associated data.
Senior physicians of modern medicine in India play a key role in shaping policies and public opinion and institutional management. This paper explores their perceptions of medical tourism (MT) within India which is a complex process involving international demands and policy shifts from service to commercialisation of health care for trade, gross domestic profit, and foreign exchange. Through interviews of 91 physicians in tertiary care hospitals in three cities of India, this paper explores four areas of concern: their understanding of MT, their views of the hospitals they work in, perceptions of the value and place of MT in their hospital and their views on the implications of MT for medical care in the country. An overwhelming majority (90%) of physicians in the private tertiary sector and 74.3 percent in the public tertiary sector see huge scope for MT in the private tertiary sector in India. The private tertiary sector physicians were concerned about their patients alone and felt that health of the poor was the responsibility of the state. The public tertiary sector physicians’ however, were sensitive to the problems of the common man and felt responsible. Even though the glamour of hi-tech associated with MT dazzled them, only 35.8 percent wanted MT in their hospitals and a total of 56 percent of them said MT cannot be a public sector priority. 10 percent in the private sector expressed reservations towards MT while the rest demanded state subsidies for MT. The disconnect between their concern for the common man and professionals views on MT was due to the lack of appreciation of the continuum between commercialisation, the denial of resources to public hospitals and shift of subsidies to the private sector. The paper highlights the differences and similarities in the perceptions and context of the two sets of physicians, presents evidence, that questions the support for MT and finally analyzes some key implications of MT on Indian health services, ethical issues emerging out of that and the need for understanding the linkages between public and private sectors for a more effective intervention for an equitable medical care policy.
Biographic sketch
Imrana qadeer.
Imrana Qadeer’s areas of research interests are organization of health services, Primary Health Care, Political Economy of Health, Epidemiology, Health Policy Analysis, Research Methods, Systems Research, Women’s Health and Nutrition. She has published her research in national and international journals and books. Her forthcoming book is Health of the Dalit Women in India.
As a Professor at the Centre of Social medicine and Community Health, School of Social Science, Jawaharlal Nehru University, New Delhi she taught and guided research in public health for 34 years. Over 2008-2010, she was offered the prestigious J P Naik Senior fellowship by the Centre for Women's Development Studies, New Delhi. An MD in Pediatrics and a clinical registrar at the All India Institute of Medical Science, New Delhi she moved into public health to develop a critique of the bio-medical approach to public health in India. She worked with several formal institutions such as, the Planning Commission, the Population commission, and the monitoring Committee of the National Rural Health Mission. She was a member of the Standing Committee, currently a visiting Prof. at Council for Social Development of the University Grants Commission on Women’s Studies Centres in Indian Universities and is also associated with several grass root organizations working on health issues.
Dr. Sunita Reddy is an Anthropologist, specialized in medical anthropology, currently teaching in the ‘Center of Social Medicine and Community Health’, School of Social Sciences, Jawaharlal Nehru University. Dr. Reddy has been teaching and researching on Public Health issues. Her areas of research are women and children’s health, public private partnership in health services, Disaster studies and Medical Tourism. She has done a longitudinal research on Rehabilitation Post Tsunami in Andaman and Nicobar Islands and published a book ‘Clash of Waves’ by Indos Publishers, New Delhi (2013). She has published research papers widely in peer reviewed journals and has presented papers in many national and International conferences. She has been delivering lectures for Academic Staff colleges, for Indian Foreign Service probationers and other institutions. She is a Core group member, in formulation of guidelines on psycho-social health, widows and children in disasters, for National Disaster Management Authority (NDMA) and also member in expert group for “CBRN Disaster Management: A Step Towards Capacity Building & Resilience in Industries” throughout the country.
Introduction
Medical Tourism in Asia is estimated as worth $ 4 billion by the year 2012 [ 1 ]. The critical factors that led to cross border travel to seek superior medical care are the rising cost of care in the developed world and presence of uninsured or underinsured people there. Patients from developed world are now seeking care in countries where hi-tech is available and inexpensive. Huge cost differentials (Asian countries charging 20% of the cost of US and UK), cheaper airfare, ‘world class’ hi-tech medical care today offers business opportunities for corporate hospitals in Asian countries.
Medical Tourism (MT) in India can be traced to the increasing numbers of corporate hospitals in the metropolitan cities. With increasing liberalization since the 80s, tertiary care in India’s health sector was opened to private sector provisioning and public institutions permitted to accept private investments in the hope of enhancing revenues [ 2 ]. The Tenth and Eleventh Plans [ 2 , 3 ] welcomed MT, commercialisation of the public sector and a hi-tech tertiary sector market as a part of reforms. The drafts of the National Health Bill [ 4 ] and the 12 th Five year Plan of India emphasised the role of private sector in medical care [ 5 ]. This privatization and commercialization that transformed medical care from a service to a commodity was a conscious policy decision accompanied by a range of subsidies including land, equipment and drug imports etc. [ 2 , 3 , 6 ]. It also attracted medical experts from the public hospitals who had received state supported medical education [ 7 ]. Like any other business in welfare services in India, medical industry also started attracting clients through capturing the high-tech services. The health services were transformed from a national medical priority based network of institutions to one that offered the services- elective (could be planned in advance) and tuned to the needs of the global patients.
Thus, the emergence of medical tourism within India’s policy frame at the turn of the century cannot be seen as an outcome of international influences alone. The ideological underpinnings of the Indian State itself are reflected in the policy shifts towards commercialisation and growth of MT that transforms health services into a source of trade, gross domestic profit, and foreign xchange [ 8 ]. The government policy of merging medical expansion and tourism was announced by Finance minister in his 2003 annual budget speech, where he called for ‘India becoming a global health destination’ [ 9 ]. Thus chains of such institutions and medi-cities got underway. India’s XIth Plan mentions a list of corporate hospitals, which provide high-end health care services through business process outsourcing [ 3 ], p.275 and the XII Plan depends heavily on the public private partnerships in financing of tertiary care as a way to handle the financial challenge [ 5 ]. Confederation of Indian Industry (CII) and Indian Health Care Federation (IHCF) wants to establish an Indian health care brand synonymous with ‘safety, trust, and excellence’ [ 10 ]. The good public sector tertiary hospitals too are being geared to practice MT. The assumption behind these policies is that the revenue thus, generated will add to the economic growth that is the basis of welfare. The fast growth of private tertiary sector hospitals and their use indicates profit maximisation for medical business and need satisfaction for the upper middle classes, but what of the physicians among them trained in the science of medicine and public health? Are they satisfied and aware of emerging ethical contradictions? These are issues this paper helps us answer.
The paper focuses on the perceptions of MT among senior physicians around four areas of concern: their understanding of MT, their perceptions and views on the hospitals they work in, the value and place of MT in their hospitals and the implications of MT for medical care in the country. The validity of their perceptions is then examined against available literature on the subject. By contrasting these views of public and corporate tertiary care physicians the paper also highlights their contrasting ethics of medical care.
This study focuses on the perceptions of MT among senior physicians from selected public and corporate tertiary hospitals. Though based on a relatively small sample of 91 physicians, it is critical as these physicians influence the health policies through their influence on public opinion specially the middle class, their advisory and consultancy roles in health planning at the Ministry of Health and Family Welfare of the Centre and State Governments, and micromanagement of their departments and institutions. The study is based on in-depth interviews as its main tool along with observations, hospital records and secondary literature. Open-ended interview schedules shown in Additional file 1 and probes in Additional file 2 , wherever necessary were used. The interviews on an average took one hour and the responses were noted verbatim.
Two reputed public and two well known corporate hospitals in each of these three cities were selected purposively. Till 2010, there was no Ethics Review Board constituted for social science research either at the School of Social Sciences or at the Jawaharlal Nehru University Level. Following the general ethical guidelines practiced in academics the authors took written consent from the hospital authorities and verbal consent from the physicians to interview and publish their views. Anonymity of both- the physicians and the hospitals is maintained. Physicians from four public and six corporate tertiary hospitals from three metropolitan cities - Delhi, Chennai and Hyderabad - were selected. In Chennai, public hospitals refused permission due to some problems with the media just before the fieldwork in 2006-2007. The departments of cardiology, orthopaedics, surgery, and paediatrics with high focus on MT, other departments with or without MT and medical administrators were also chosen for interviews. The selection of physicians was thus purposive depending on their willingness for the interview. While writing, the method of paraphrasing multiple quotes was used both for bringing out commonalities and differences between the physicians of public and corporate tertiary sectors.
Table 1 gives the distribution of physicians in the study sample. The interviews from the corporate hospitals in three cities covered 52 physicians and from public sector hospitals in two cities covered 39 physicians.
Distribution of physicians interviewed across type of tertiary care hospitals in three cities
| Physicians | Public | Corporate | Public | Corporate | Public | Corporate |
| MT Centred Specialities* | 16 | 12 | 7 | 6 | - | 19 |
| Specialities with or without MT** | 9 | 1 | 2 | 2 | - | 7 |
| Administration | 3 | 2 | 2 | 3 | - | |
| Total | 28 | 15 | 11 | 11 | - | 26 |
*Specialities from Cardiology, Orthopaedics, Surgery and Paediatrics.
**Specialists from General Medicine, urology, neurology, gastroenterology, oncology Geriatrics and Preventive and Social Medicine.
Understanding of medical tourism
Physicians in the public and corporate sectors viewed MT as ‘ attracting business through marketing ’. It was ‘ travel from home to another country for treatment where the host country derives financial benefit from their travels ’. The difference was in their attitude towards competition and benefits.
The corporate sector physicians emphasised three main reasons for the popularity of MT: ‘ providing opportunities to overseas patients to avail the hi - tech medical facilities in India at a low cost , through skilled physicians who can compete with physicians in the USA and the UK ’; ‘ quality services are cheaper in India ’ with ‘ culturally similar conditions for neighbouring countries ’; and ‘ due to post - 11 September visa restrictions to the USA , the Arabs and Africans prefer India ’. Some also opined that ‘ aspects like arrival , pick up , transport , and reception at airports ensure patient satisfaction and help standardise price structure ’. Others went to the extent of proclaiming: ‘ We deliver caring services ’; ‘ India is known for its hospitality and there are no racial differences here ’; ‘ Indians are by nature compassionate and brainy , so we can tap this potential ’; ‘ We are proud of our medical expertise ’; and ‘ We have state of the art equipment comparable with the best in the world ’.
Public sector physicians were more detached with a “not-for-us” attitude with lesser involvement in the competition around MT. While they all felt, ‘O verseas patients come to public hospital for simpler treatment due to lack of good quality tertiary care in their own country or long queues ’, only those in one Delhi hospital with greater exposure to foreign clients felt, ‘ Medical tourism is a new term for an old phenomenon as our hospital has been treating foreign patients for long ’; ‘ The volume of overseas patients is not high and they pay like the private patient ’. Use of the term tourism with clinical work made these physicians uncomfortable. ‘ Tourism is always pleasure related , whereas MT is not ’; ‘ only traditional healing centres could be identified for promoting health tourism ’. Thus, the majority underplayed the commercial underpinning of the word ‘tourism’, where the notion of profit from service was critical as they saw them as reinvestments!
Professional perceptions on work load and conditions in tertiary public and corporate care hospitals
Long queues for OPDs in public hospitals without a place even to stand, beds occupied by more than one patient in three out of four hospitals, stood in contrast to the decorated spaces and low patient load of the corporate hospitals. Public hospital OPDs had 1,500- 8,000 patients every day as compared to 100 to 1,200 per day in corporate hospitals. The bed strength of the former ranged between 1,500- 2,500, while the beds in corporate hospitals varied from 130 to 300.
In public hospitals, inadequacy of funds, political interference in recruitment and promotion leading to mistrust, and undermining the autonomy of institutions were a constant refrain. The internal problems reported were: unhealthy work culture, inefficiency of staff, trade unions without a strong sense of responsibility. A self-critical reputed senior doctor said, ‘ Physicians lack spirit of academic pursuits , transparency and autonomy in research in a disturbed work culture , therefore , quality of care gets affected and outputs are often irrelevant to our health needs. There is also a disjunction between what we do and what our national priorities are ’. Others agreed that these problems affected medical care for the poor negatively. ‘ Patients from other states , especially from rural areas , live on roads or Dharamshalas ( inns ), paying Rs20 - Rs100 per day. CGHS patients wait for surgical treatment despite doctor ’ s orders for admission , for lack of beds. The wait is on an average 6 months - sometimes patients die. There is paucity of blood and Social Welfare Fund schemes are often misused by administration and politicians as few people know of these ’.
Dissatisfaction was expressed by public sector physicians in many ways, ‘ We don ’ t have adequate medical facilities for the poor in India ; without subsidy or insurance 70 % of the population cannot afford super specialty treatment . ‘ Physicians are mostly overburdened ’, ‘ We have to first meet proper standards of bed and nurse availability ’. ‘ The working conditions are so poor that , at the end of the day , it is the love for one ’ s work which sustains one in such an environment and individuals focus only on what they can do , forgetting the macro picture ’. ‘ Public sector has reached a point where a deliberate policy to improve it is unavoidable if standards have to rise ’. A self critical perspective was, ‘ the patient has no rights , at times we are arrogant , so do not seek active participation from the patient in choosing from the options available to him ’.
In contrast, the corporate sector physicians were satisfied with their working conditions. They emphasised the need to work in a technically equipped work place where they get job satisfaction and are able to practice scientific medicine. They pointed out that their institutions offered differential packages for different income groups. Another advantage they saw was in using their skill to the maximum by taking up consultancies in more than one hospital.
Public sector doctor’s perception of Mt
Out of the 39 interviews of public sector physicians, three sets of opinions emerged on the promotion of MT in public hospitals discussed below. The majority, i.e. 29, were very positive about the scope of MT in India. 14 of these (35.8%) thought it should be promoted even in the public sector while 15 (38.4%) felt public sector was in no position to compete and only the private sector could take advantage of it. Only eight physicians (20.5%) were critical of MT as a strategy. Two (5.1%) did not comment.
Against MT in principle
The eight physicians against MT in principle, considered MT as, ‘ a crime against the ordinary Indians , an undemocratic policy ’, ‘ practiced without any consensus or meeting of all parties ’. ‘ There is a need to look at our own health needs against which the idea of MT in public hospitals – that were not meant for making profits – makes no sense .’ ‘ Have we treated all Indians that we want to invite patients from abroad ?’ ‘ The poor do not get any benefits from the Foreign Exchange .’ ‘ The promotion of MT will not improve the country ’ s health when we are not able to provide basic services to the people ’. They added, ‘ Our hospital focuses on education , research , and services and will resist money making policies like MT ’. They believed that, ‘ Medicine is for services and not for business. MT is against the oath of Hippocrates and therefore unethical ’; ‘ it undermines the ‘ very basis of faith between physicians and patients ’, ‘ our institution has the capacity and quality to promote MT , but the institution is not meant for private service … If we spend so much time and energy on few patients it will deviate from the norm / protocol of the institution ’. Proud of the public sector’s ability to provide hi-tech 24 hour care without profit, they said, ‘ Nobody has the time to provide ancillary services , when key services have to be ensured !’ Facilities like deluxe rooms and personal security, required by medical tourists, were inconceivable for them.
‘ Resource mobilization by the State ’, ‘ political will , appropriate priorities , regionalisation and internal tourism ’ was their answer to inequity, reflecting an acceptance of some degree of the commercialisation which they criticised otherwise. Despite their frustration with state policies, and their view that, ‘ MT takes advantage of lack of proper regulatory authority or effective laws and implementing agencies and makes malpractice possible , both in the use of technology and pricing ’, they barely contested the State support to MT in the private sector, or pointed towards its international business connections.
They wanted cross border medical treatment for humanitarian reasons and to promote international relations and not MT. For them the issue was not competing for patients in the medical market, but their inability to fully provide for their own patients and the patients’ inability to afford payments. ‘ The Ministry and the government want us to generate our own revenue but we are not getting into the market ’. This moralistic admonition of commercialisation was reflected by a doctor’s outburst, ‘ Our ethics are bad , we let Indian physicians go abroad and invite patients from abroad when we ourselves have surplus patients ’.
Thus 35.8 percent of the public hospital physicians felt they could use MT to the benefit of patients and professional while 38.4 percent felt that in the present form public hospitals were ill suited for MT and would further deprive the general patients, 20.5 percent were in principle against MT in public hospitals.
MT in corporate hospitals alone
Fifteen public hospital physicians considered MT a legitimate function of the corporate hospitals (with their ‘spare capacity’). Public hospitals were seen as ‘ ill equipped ’, ‘ already over burdened ’, and ‘ ill suited ’ for it. The objections were two. Firstly: ‘ MT is going to create a divide by diverting resources from the poor who will suffer more , it will enhance the burden of the poor patients unless the government separates the two sets of institutions ’; ‘ The onus of care for the poor lies with the public sector and it should look after the interests of the general public ’. Secondly, they argued that: ‘ Given the present level of investments in public hospitals it is out of the question to achieve the standards needed for MT ’; ‘ The importance given to medical tourism will certainly affect general health care and public hospital is for all and not for some specific people ’. A doctor said, most physicians expressed their anguish at the state of Public health services, and emphasised the inadequacies, which need to be catered to before embarking on MT. They were clear that, ‘ MT can be encouraged and promoted in corporate and private tertiary hospitals and it would help the economy and the growth of hi - tech in India ’.
MT both in public and corporate institutions
Nine specialists argued that India has the best low cost medical expertise in South Asia for treating the overseas patients and generating high revenues. They saw a tremendous scope for MT especially in plastic surgery, orthopaedics, and other non-invasive techniques. ‘ Wherever these departments are well established and of international standards , they can be opened for MT .’ In Hyderabad, one of the public hospitals was planning to open a 7 th floor for foreign patients to promote MT - especially for NRIs. The remaining five specialists felt that primary and secondary health care should be under the public sector, while tertiary care should be through private sector and the pay clinics of government medical colleges and teaching institutions which should provide subsidised/free care for the poor.
The inter-state movement of patients from less developed states and towns to the metropolitan cities was viewed as yet another possibility for internal MT and an opportunity to improve hospital infrastructure, services, and research facilities within the public sector tertiary institutions. Some also argued that, ‘ A government doctor works from 9 a.m. to 4 p.m. and rest of the time many physicians do not have anything to do but are not allowed to practice privately. Why does the government not utilise the idle hours of the physicians who want to work extra time by opening ‘ pay clinics ’ in the evenings ? Pay clinics can be operated in the same hospital by developing good infrastructure. In this way , the government will get substantial amount of revenue. This can be utilised for development of existing departments. Otherwise , the government is losing a good hand ’. The contention was that, ‘ In the government hospitals , there is a need to have more incentives ’. Others disagreed and argued that, ‘ Physicians in public hospitals work approximately 12 hours a day and to promote MT we need to invest in new infrastructure and manpower as the same set of people cannot meet the additional load ’. This was critical so that, ‘ we do not bleed existing resources , both human and mechanical ’. It was also claimed that, ‘ This would not be because of any lack of professionalism in the public sector but due to their poor infrastructure and support systems. The public hospital environment is too dirty to attract foreigners , in fact , it prevents people from coming ’.
They also wanted to have hi-tech facilities like telemedicine which they considered necessary - ‘ if patients have to be managed at a distance ’, ‘ be able to compete with corporate sector physicians ’, and ‘ see different types of patients ’. Further, ‘ quality of care may improve because of the need to meet western standards ’. This set of experts wanted to simplify laws of organ transplant and make donors easily accessible. They felt that people come to public sector hospitals because of the doctor’s name; for MT, the entire infrastructure has to improve along with ‘ quality of care , values and ethics ’.
They argued that the public hospitals too can generate revenue through MT by overcoming some infrastructural deficiencies. Holistic healing and preventive care should be given priority under MT and they suggested package deals of ‘ services with free accommodation ’ to Medical Tourists. The notion of ‘ generating money ’ for the public hospitals through MT was generally accepted.
Interestingly, those who supported adoption of MT and welcomed markets in public sector medical care did accept that the public sector hospital is the only recourse for the poor. They argued that improving infrastructure will help the poor as well, since the profits would be ploughed back into their care if it could be ‘ ensured that no discrimination happens between patients ’. The main arguments for promotion of MT in public hospitals were that: a) it would lead to healthy competition and inter-state tourism; b) equipment and infrastructure would be updated and new technology could be brought in for all; c) a learning opportunity for physicians; d) improved quality of care for all; f) revenue generation for the government; g) arrest brain drain from public hospitals; h) a cure for poor administration and inadequate working conditions.
Perception of physicians in corporate hospitals
90.4% (47) physicians of the corporate hospitals saw a huge potential for MT. None talked about the public sector, which they said, ‘ is the responsibility of the State and is not our concern ’. A minority of 9.6% i.e. five physicians were critical of MT and were upset with its promotion, they reflected, ‘g iven the poor medical facilities in many parts of the country , the first important thing to do is to indulge in some soul searching before inviting people from abroad ’; ‘w e need to serve our own people ’, or that, ‘ MT is like selling India in its naked poverty ’. One specialist said, ‘ International insurance companies will really benefit from the idea by saving costs and time of the insurance cover , they will look for cheaper options ’. Two of these experts, in a missionary tertiary care hospital, added, ‘ we are trying for ISC ( International Standards Certification ) to promote MT … for private hospitals what matters is money !’ Their views were however overshadowed by the MT enthusiasts who felt, ‘ An excellent concept that can put India at the top by focusing on specialty treatment ’. The range of concerns expressed by them was the following:
Finding clients
‘ If Thailand can attract 2 million medical tourists per year , India should attract 20 million ’, said the Chairman of a leading corporate hospital. Another vision was to see India as, ‘ the health care hub of the east ’. The logic, ‘ India has human capital , is human friendly , and has an infrastructure which can be expanded. India needs to progressively exploit this potential ’. Another opined, ‘ MT has picked up in Mumbai , and Delhi is not far behind ’, and that, ‘ it would be beneficial for the country ’. An invitee to a consultation on Britain’s National Health Service by the NHS, UK, he had recommended that NHS should send patients to India for cheaper treatment. He said, ‘ It will be the underprivileged population in UK that would be sent to India for medical treatment. It ’ s a win - win situation forprivate hospitals to attract patients , earn money , be competitive , enhance their standards of care , and generate employment ’. In the process the bigger medical corporations might wipe out the smaller less competitive institutions he added. However, estimating the vast potential of MT, another doctor opined ‘ In Britain alone , there are 10 million patients who are in the waiting list in NHS , out of which only 11 % are British and rest are ethnic people with 80 % having private insurance. This is the group which we need to cover - ethnic and privately insured ’. Others proposed targeting the uninsured overseas clients and holding health festivals in client countries like Oman and Maldives.
Benefits of MT
These experts saw innumerable benefits of promoting MT, specially, in areas such as dentistry, cardiology, orthopaedics, cosmetic surgery, and paediatrics. The most obvious benefit was, ‘ earning foreign exchange ’ or ‘ more the patients , more the income , which will eventually lead to growth of business .’ Many felt, ‘ With up - gradation of facilities , health service standards will go up automatically ’. MT was also ‘ an opportunity to treat different sets of patients having different clinical problems to acquire knowledge and hone our skills ’. It was ‘ a boon to learn new techniques and handle more complicated and as yet incurable diseases ’, with the incoming technologies. They argued that,’ 60 % of employment is generated through service sector all over the world , so , by making our institutions globally competitive , we can generate employment and retain competent physicians ’. MT, they said, would also create a ‘ friendly international atmosphere ’: its commercial value required that its growth be ‘ exponential ’!
Other ways suggested to promote MT were: by standardizing and getting accreditation, direct flights to the cities, improving roads, easy money transfers, medical visas and systematic and planned scaling by the state as is being practiced already.
Physicians view of implications of Mt for medical care in India
Most experts in corporate institutions saw their own sector as the most critical in medical care and earnestly believed that, ‘ by selling Indian health industry abroad , and by marketing health care , one can increase the earnings and utilise that money in improving the existing infrastructure ’. ‘ This would force the inefficient public sector to compete and thereby raise its standards and improve job opportunities ’. This set obviously had no consideration about where the public sector resources and their own subsidies came from. Only a minority of five accepted that, ‘ by getting patients from abroad , dollars will get priority and the less privileged Indian patients will take a backseat ’ but they did not talk of implications for public sector.
Among those for MT, the perceived implications were positive as discussed earlier. Some even argued, ‘ MT may actually be stopping the brain drain of physicians going to work abroad by opening avenues in private sector ’. Others felt, ‘ Infrastructural improvement will improve services for all ’.
Experts against introduction of MT in public sector pointed out the negative implications of MT, such as: reduced medical care for the poor due to diversion of manpower to the care of overseas patients within the institution, as well as ‘ probable rise in malpractice by corporate hospitals by not fulfilling the condition of 25 % free admissions to patients and thereby increasing the load on public hospitals ’. Thirdly, in MT, ‘ the preventive component of medicine is left behind ’.
Yet another concern was brain drain out of the public hospitals. Even though it was said, ‘ We cannot stop them as there is a difference in salaries ’ or , ‘ As such there is no mass exodus ’, Others reaffirmed ‘ an internal brain drain ’; ‘ a lot of our expert staff , physicians and paramedics leave public hospitals for the private sector ’. ‘ Most of the physicians working in XXXX , a XXXX are from government hospitals ’. ‘ Our hospital gets some of the best junior residents from all over the country , and it is used like a nursery for training before they join the private sector ’. Other than money, the reason for leaving the public sector was said to be ‘ eagerness to learn more and use sophisticated technology like robotic surgery and not getting stagnated ’. These views matched the finding of the study as more than fifty percent of physicians working in corporate hospitals had earlier served in public hospitals. In Chennai, 13 out of 23 physicians (3 did not respond); in Hyderabad, 5 out of 11; and in Delhi, 10 out of 15 had served in public hospitals.
Among opponents of MT there were some who did not think it would have any impact as their institution was capable of fairly handling its patients. Others said, ‘ If it is only in private hospitals then , that being a separate sector , there is no implication for general patients ’. According to them, promotion of MT in private sector may, in fact, help the poor as the growth of private sector diverts the middle and upper middle class patients away from public hospitals, which can then exclusively cater to the poor. ‘ Rather than the poor , the rich will be affected by MT , as many times , preference is given to foreign patients who have higher paying capacity rather than rich Indian patients ’.
These views were no doubt contradictory among the physicians for and against MT across the two sectors. Even among the opponents of MT in the public sector, the articulation of the significance of shifts of state subsidies and policy of commercialisation was muted. They saw their challenge as one of ethical practice, getting State resources and problems of micro-management.
Historically, the middle class – especially physicians and bureaucrats, tend to play a key role in the evolution of policy for medical care [ 11 ]. Our study reveals certain trends in the perceptions of selected senior medical physicians that are critical: as pointed out earlier this group of physicians contributes to the formation of public opinion, national policy and programs and shapes institutional traditions and organisation.
Doctor’s Perceptions: differences and similarities & ethical underpinnings
An overwhelming majority (90%) of physicians in the private sector held the State responsible for the care of the larger population. In contrast, the public sector physicians’ daily challenge of saving lives within the constraints of their patients’ economic status and the meagre facilities available, made them sensitive to the problems of the common man. The glamour of hi-tech associated with MT however dazzled most physicians of both sectors. All physicians of the public hospitals under study felt responsible for the poor, 59 percent (23) acknowledged the irrelevance of MT for common patients and potential problems with MT in public tertiary hospitals, while 36 percent (14) thought it would improve overall patient care due to added revenues 5.1 percent (2) remained non-commital.
The economic and political linkages and dynamics between public and private sectors were largely missing from the doctor’s perceptions which was primarily limited to micro management of institutions. The disconnect between their concern for the common man and their views on MT was due to the lack of appreciation of the continuum between commercialisation and MT, and the link between denial of resources to public hospitals and shift of subsidies to the private sector [ 12 ]. The profit motive behind MT was recognised, hence, those who did not favour MT did it mostly on moral and ethical grounds.
Interestingly, only the private sector physicians, and those public sector physicians who supported MT in their institutions, talked frankly about the existing and possible links with the international market and its potentials for earning revenues, the need to consolidate the medical industry and of State subsidies to push MT without acknowledging the negative impact of the shift of state subsidies and of the logic of market forces which undermines epidemiological priorities. In contrast those in the public sector opposing MT in principle, underlined the importance of policy changes to mobilise resources for the public sector and rebuild the culture of service.
Private sector physicians were very articulate about their views on the role of the State. They demanded State support to promote MT and believed that the “competition” thus offered would force the public sector to improve! This contorted logic completely ignores the fact that the public sector was set up with State subsidies to be able to run services that are non-competitive and based on epidemiological needs, and that costs were standardised by the State to achieve equity in access. Without State subsidies it would collapse, as commercial competition shifts the emphasis to services like Obstetrics, Orthopaedics, Cardio-thoracic surgery transplants, and Urology etc. and their required manpower that distort priorities within public hospitals and health system as such [ 8 , 13 , 14 ]. The public sector experts, though wary of perpetual shortages, accepted the State’s indifference and had little to say about its constraints though, a few of them talked of reforming the medical care system.
Unaware of the massive indirect shifts of resources that are being proposed [ 12 ], the physicians in this study saw public and private sectors as discrete entities. Almost all (94.7%) opposing MT in public institutions granted corporate sector, the right to use MT to generate revenues as they believed, ‘ It adds to India ’ s economic growth ’. They did not ask how inclusive is this strategy for economic growth except for one who believed, MT operates outside the public system , the Foreign Exchange earned stays in the private sector , and the country ’ s poor do not ever benefit ’. The others did not raise the issue of declining resources due to state support to private sector. These views illustrate that the physicians were not familiar with the shifting overall pattern of state financing of health services and it’s links with private sector, so well known to analysts of the health service system [ 7 , 15 ]. Most of them in one voice spoke of the huge potential of MT in India as a vehicle for economic growth while only 10 percent in the private and 20.5 percent in the public sector expressed discomfort with the very strategy of MT in their institutions.
Seen in the framework of domains of micro ethics (relationship with, care, autonomy and choice of patient) and macro ethics (issues of equity, justice, resource allocation, care of the vulnerable and maximum benefit for largest number) provided by Nancy M. Baum [ 16 ] and Calman and Downie [ 17 ], our findings indicate that private tertiary sector doctor’s concerns are largely limited to the micro ethical domain related to standards of care and management, regulations, doctor patient relations, beneficence etc. Only 10 percent of them referred to some macro ethical issues of MT as part of public health-such as needs of the majority and concern for the poor. It was primarily the public sector physicians who at all mentioned macro-ethical issues covering financial constraints, equity for the most vulnerable sections, priorities in technological choices for provisioning of services in public institutions of tertiary care and need for primary health care. Even among them 38.4 percent who wanted the state of the art technology and MT to mobilise revenues for the general patients- like 90 percent of their counterparts in the private sector had no problem with medical care becoming commodity and a part of the market. This however was under the impression that MT can mobilise resources for general patients. Thus, they saw no conflict in macro ethical issues and MT.
Implications for state policy
A weak professional resistance to MT among senior physicians gives the state a better chance to push forward its neoliberal policies and MT, a logical outcome of the market principle, now extends the boundaries of tertiary health care market. The projected Rs.8,50,000 crores contribution to the GDP by 2020, if the Government supported it, prompted the Union budget for 2003-2004 to give infrastructure status to tourism, paving the way for long term State subsidies [ 18 ]. MT is thus a beneficiary of this support while the allocations for health have remained below 1.2% of the GDP over the National Five Year Plan periods.
The State itself promoted establishment of corporations of corporate hospitals to manage MT, as in Maharashtra and Gujarat. The Gujarat government announced its Medical Tourism Policy in December 2006, linking its profits with those of the insurance system and professing an annual increase of 33% in MT growth. To promote this ‘business’ it proposed a focus on medical education, manpower development (as of physiotherapists, optometrists, pharmacists and nurses), state of the art diagnostics, blood banks, alternate systems and medi-cities. It set up a high level business council under the Chief Minister to plan the promotion of MT [ 19 ]. Thus, MT also became an official reason for supporting medi-cities as in Gurgaon (State of Haryana), Kolkata, and Bangalore and professional attraction towards hi-tech helped the state in this expansion.
Evidence negating perception of advantages of Mt
The corporate hospital consultants saw increase in GDP, business, employment, professional advancement, competitive spirit, international standard of care with advanced technology, and improved infrastructure as advantages. All of this matched the State’s vision, and the satisfaction of the Indian elite with economic growth rates and its world class medical care is seen as evidence of success. However, debates on the destructive impact of the corporatisation of medicine, the emergence of MT, and social responsibility/irresponsibility of the corporate sector [ 20 ] show the other side of reality. But an understanding of the roots of MT and its larger implications evaded the majority of our respondents. Several serious implications have been recognised in the literature:
– i. Direct and indirect shift of subsidies for corporate sector. The former itself is calculated to be Rs.57,000 crores [ 14 ].
– ii. MT is overshadowing the poor state of Indian public hospitals as the 11 th Plan focused on the former and glamorised the institutions catering to MT [ 3 ].
– iii. Rise in prices of medical services is making it even less accessible and more inequitable. The logic of price rise is the need for profit maximisation to break even the initial investment of around Rs.100 crores for a 200 bed corporate hospital. It takes some 4-5 years to break even and some 7-8 years to make reasonable profits. Investment in hospitals is characterised by low returns – the profit rates are around 13% lower than that in IT, finance, or retail [ 21 ].
– iv. Rising numbers of establishments of profitable super specialisation and focus on life style surgeries, assisted reproduction, orthopaedic, eyes and cardiac services are distorting priorities as epidemiological reality becomes irrelevant for investors [ 22 ].
– v. Overemphasis on tertiary care is leading to shortage of skilled work force in primary care and distorted manpower planning [ 23 ].
– vi. Brain drain both external and internal [ 24 ].
– vii. Hi-tech institutions act as a push factor for insurance businesses which keep the poor out in India yet, the potential for earning revenues through MT will become an important argument for private hospitals demanding more subsidies from the government in the long run and further undermining services for the poor [ 25 ]. Yet there is evidence to show lack of transparency and unethical practices in these hi-tech institutions in India [ 6 ].
These facts however, did not constitute the basis of perceptions of even the 27.5 percent of those who were in principle against MT in public sector tertiary hospitals or the 9.6 percent of the private sector physicians who felt it did not help the poor. Both rejected MT on ethical and experiential grounds, the former more openly than the latter.
Despite the fact that patients from the developed world seek MT to save costs in elective treatment (plastic surgery, cosmetic, dental and wellness treatment) or if they are under and uninsured, MT may not be a solution forever. If the efforts of developed nations to restrict losses they incur by cross-border patient travel, by creating their own security systems, succeed, then the profitability of MT may decline. Developed nations are changing insurance laws for those who use MT [ 10 ], and developing collective mechanisms of cross border treatment at regulated prices as in the European Union [ 26 ] or introducing health Reforms as in the US [ 27 ] to handle the crisis of health services. What will then happen to the huge five star high-tech hospitals in India, once their clientele falls? Already many of them survive on heavy State subsidy and by converting hospitals into restaurants, pastry, gift and glossy book shops. Even when it contributes to the growth-oriented economy, its benefits exclude the majority. Is it then an impending disaster, the costs of which will be shifted on to the State and the exchequer as in the case of the Commonwealth Games [ 28 ]?
Under these rather alarming circumstances, where India’s health service system is responding to the needs of an elite international and national community, the role of physicians committed to the majority of Indian patients acquires great significance. Their silence and indifference can harm the common patients. Therefore, an over-arching understanding of MT and its implications for the public health system is crucial. It helps one to realise that MT is for cross-border trade in medical care, transfer of technology, manpower, and knowledge that favours the elite and not necessarily the ordinary users of public sector tertiary hospitals. This realisation then provides a more objective basis to their demand for essential policy changes.
a All identifying information has been removed and replace with XXXX to ensure anonymity.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Both the authors IQ and SR have contributed equally to the study, from conceptualising the problem, review of literature and designing research and formulating the tools. Under the guidance of IQ, SR along with the research team conducted the field work. Both the authors have analysed and written the paper. Both the authors have read and approved the final manuscript.
Supplementary Material
Interview schedule for senior physicians in public and corporate hospitals.
Acknowledgements
We are grateful to the School of Social Sciences, JNU and MHSP project (Monitoring shifts in health sector policies in South Asia) for the financial assistance to make this research possible. We would also like to thank researchers Francis Adaikalam, Sutanya Mahapatra, Srilaxmi Divakar and Ashima Jena for helping us in data collection.
- CII-McKinsey. Health Care in India: The Road Ahead. CII. New Delhi: McKinsey and Company and Indian Healthcare Federation; 2002. [ Google Scholar ]
- Planning Commission. Tenth Five Year Plan, 2002-2007. Volume 2. New Delhi: Chapter on Health, Government of India; 2002. [ Google Scholar ]
- Planning Commission. Eleventh Five Year Plan, 2007-2012. Volume 2. New Delhi: Chapter on Health, Government of India; 2008. [ Google Scholar ]
- Government of India. Ministry of health and family welfare, draft national health bill. 2009.
- Planning Commission. Twelfth Five Year Plan, 2012-2017. Volume 3. New Delhi: Chapter on Health, Government of India; 2013. [ Google Scholar ]
- Qadeer I, Reddy S. Medical care in the shadow of public private partnership. Social Scientist. 2006; 8 (9–10):4–20. [ Google Scholar ]
- Baru RV. Privatisation of health services: a south asian perspective. Econ Pol Wkly. 2003; 8 (42):4433–4437. [ Google Scholar ]
- Chanda R. Trade in Health Services. 2010. http://www.who.int/trade/en/THpart1chap3.pdf webcite. [ PMC free article ] [ PubMed ]
- Budget 2003- 2004: speech of Jaswant Singh, minister of finance and company affairs, Feb. 28 2003. 2013. http://indiabudget.nic.in/bspeech/bs200304.pdf Webcite.
- CII. Great Advantage in India Medical Tourism: CII August 2004. 2013. http://www.medicaltourindia.com/medical-tourism-news.asp Webcite. Accessed on 5th May 2013.
- Banerji D. In: Public Health and the Poverty of Reforms. Qadeer I, Sen K, Nayar KR, editor. New Delhi: Sage Publication; 2001. Landmarks in the development of health services in India. [ Google Scholar ]
- Reddy S, Qadeer I. Medical tourism in India: progress or predicament? Econ Pol Wkly. 2010; 8 (20):69–75. [ Google Scholar ]
- Whittaker A. Pleasure and pain: medical travel in Asia. Global Public Health. 2008; 8 (3):271–290. doi: 10.1080/17441690701463936. [ CrossRef ] [ Google Scholar ]
- Chanda R. Trade in health services. Bull World Health Organisation. 2002; 8 (2):158–163. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sengupta A, Nundy S. The private health sector in India. BMJ. 2005; 8 :1157–1158. doi: 10.1136/bmj.331.7526.1157. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Baum NM, Sarah EG, Susan DG, Peter DJ. American Society for Bioethics and the Humanities Annual Meeting: Connecting and Collaborating 10 (19) Washington, DC; 2007. Ethical issues facing public health practitioners; p. 7. [ Google Scholar ]
- Calman KC, Downie RS. In: Oxford Text Book of Public Health. Roger D, Robert B, Mary AL, Martin G, editor. London: Oxford University Press; 2011. Ethical principles and ethical issues in public health. [ Google Scholar ]
- Medical tourism policy. 2010. http://www.indiacore.com/tourism.html webcite.
- Gujarat medical tourism policy: draft. 2010. http://www.discoveredindia.com/gujarat/tourism-sectors-in-gujarat/medical-tourism-in-gujarat.htm webcite.
- Sengupta A. Medical tourism in India: winners and losers. Indian J Med Ethics. 2008; 8 (1):4–5. [ PubMed ] [ Google Scholar ]
- Kumar P, Simi TB. Barriers to movement of healthcare professionals a case study of India. 2010. http://www.cuts-citee.org/pdf/RREPORT07-03.pdf Webcite.
- Venkata K, Prasad CB. Medical Tourism Industry - Advantage India. 2010. http://dspace.iimk.ac.in/bitstream/2259/483/1/255-260.pdf Webcite.
- Hazarika I. Medical tourism: Its potential impact on the health workforce and health systems in India. J Health Plann Policy. 2010; 8 (3):248–251. doi: 10.1093/heapol/czp050. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hopper CR. Adding insult to injury: the healthcare brain drain. J Med Ethics. 2008; 8 (9):684–7. doi: 10.1136/jme.2007.023143. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gupta SA. Medical Tourism in India: winners and loosers. Indian Journal of Medical Ethics. 2008; 8 (1):4–5. [ PubMed ] [ Google Scholar ]
- Bertinato L, Busse R, Fahy N, Quigley HL, McKee M, Palm W, Passarani I, Ronfini F. Policy brief cross border health care in Europe. 2010. http://www.euro.who.int/__data/assets/pdf_file/0006/108960/E87922.pdf Webcite.
- Health care reforms to impact medical tourism. 2010. http://www.imtjonline.com/news/?EntryId82=129713 Webcite.
- Chotani S, Sultana S. Common Wealth Games in Delhi: How much does national prestige cost? A report; 2007. New Delhi: Monograph of The Hazards Centre; 2007. [ Google Scholar ]
Advertisement
An Assessment of Competitiveness of Medical Tourism Industry in India: A Case of Delhi NCR
- Original Research
- Published: 01 August 2022
- Volume 17 , pages 215–228, ( 2022 )
Cite this article

- Neha Malhotra ORCID: orcid.org/0000-0002-8380-8739 1 &
- Kartik Dave ORCID: orcid.org/0000-0001-6581-8979 1
5191 Accesses
19 Citations
7 Altmetric
Explore all metrics
India has emerged as a prominent medical tourism hub, yet the dynamic forces in the regional and global landscape are creating a complex balance of opportunities and risks for the Indian stakeholders. The outbreak of Corona virus pandemic in 2019 has further complicated the market dynamics for the medical tourism industry. This study aims to analyse the key driving factors for the medical tourism industry in India and the issues that Indian stakeholders should address in crafting a winning strategy. A qualitative research design was adopted, and data were collected through semi structured in-depth interviews with practitioners and senior representatives of the hospital management. The study adopted abduction logic and analysed data by means of constant comparison method. The study presents the assessment of the medical tourism industry in India and the scope of opportunity for Indian players.
Similar content being viewed by others
Framework for Promotion of Medical Tourism: A Case of India

Medical Tourism: The Islamic Perspective

Developing Medical Tourism in Bangladesh: Issues, Challenges and Policies
Explore related subjects.
- Artificial Intelligence
Avoid common mistakes on your manuscript.
Introduction
Catalysed by emerging technologies, varying economic and demographic trends and a new age of healthcare consumerism; the worldwide scenario of healthcare is rapidly evolving. Additionally, a growing ageing population, and a swelling burden of diseases is rising the demand and cost of medical services. This evolution in healthcare is driving cross-country and cross-industry convergence (Deloitte Global, 2021 ), resulting in an upsurge in the worldwide medical tourism market. As this trend towards the healthcare is enduring around the world, more and more countries are extending their health systems to access care, not just for their natives but also gaining strength as leading service providers for international patients. While much of the initial focus was on the developed world, the epicentre is now shifting towards the emerging countries. Governments of these developing countries are working towards prioritising their health systems; enhancing productivity, boosting avenues for innovation and entrepreneurship, generating employment opportunities, increasing foreign exchange earnings, and hence driving GDP growth (Rahman, 2019 ).
India has been having its own unprecedented progress in this sector. To counter the emergent health issues, the health system in India has metamorphosed rapidly since the 90 s and has become the focal point of development. With the presence of clinical and technical expertise, international standards and highly competitive prices; India has emerged as a leading contender in the medical tourism industry (Bagga et al., 2020 ). Yet the accelerating shift in the regional and global landscape is making it challenging for the stakeholders to balance opportunities with risks. The industry is showing ramification of rapid disruption and intensified competition. Service providers are facing new playing fields. Recognizing this change alone isn’t enough. Government and entrepreneurs need to become adept at dealing with disruption and adapt the operating models, in a holistic way, to mitigate the outcomes of the shifting paradigm. It is imperative to introspect and identify the capabilities and resources that stakeholders need to realise. This is critical to endure the sophistication and competence of the medical tourism industry in India.
The outbreak of Corona virus pandemic in 2019 has further complicated the market dynamics for the medical tourism industry. Uncertainty over travel restrictions, changing quarantine measures across the world and the overall unprecedentedness of the situation, have made the entire ecosystem of medical tourism industry more precarious. With cross-border travel restrictions and the need to redirect hospital resources to treat COVID-19 patients, healthcare providers have to manage a dual burden of economic and health crises (Stackpole et al., 2021 ). The challenges posed by this pandemic have further demonstrated how crucial it has become for medical tourism industry in India to review their competitive positioning, access deeper competencies and build resilience.
A review of extant literature indicates very little empirical research has been done to done to examine factors of competitiveness of a medical tourism destination (Abubakar & Ilkan, 2016 ; Heung et al., 2010 ; Thayarnsin & Douglas, 2016 ; Yeoh et al., 2013 ). Theoretical understanding around the phenomena requires further academic attention (Chuang et al., 2014 ), specifically with regards to the perspective of medical tourism providers (Taheri et al., 2021 ). Virani et al. ( 2020 ) have also directed our attention to the neglect of policy-relevant research on medical tourism. This study aims to address this gap. By considering the perspective of medical practitioners and senior representatives of hospital management, this study identifies and analyses the key factors driving success in medical tourism industry and the issues that Indian healthcare providers and policymakers should address in crafting a winning strategy. Taking Delhi NCR as the context, this outlook propounds insightful research into the existing state of medical tourism industry in India, explores the dimensions and factors that can help India shape an effective ecosystem for this sector and suggests considerations for an optimum future of medical tourism industry in India.
Literature Review
The literature review encompasses a succinct discussion on the medical tourism industry, its global trends and the current state of Asian and Indian medical tourism industry, along with the key dimensions of medical tourism as highlighted in the literature.
Medical Tourism
Globalisation is restructuring the industries worldwide. Medical tourism is one such manifestation of globalisation in the healthcare industry (Connell, 2013 ; Ganguli & Ebrahim, 2017 ). Broadly it refers to travelling internationally for healthcare. Since its rapid development in 1990s, medical tourism has received a major reflection from both academia and industry. Though the growing interest to study this industry is well evident, there is still no international consent on the definition or measure of this sector. The existing literature addresses the terms health tourism and medical tourism in a loose and disorganised manner. Terms frequently used, and often synonymously, in this regard are ‘ medical tourism ’, ‘health tourism’, ‘medical travel’, ‘health travel’ and ‘cross-border healthcare’. While some researchers have used “medical travel” and “health travel” synonymously (Gola, 2016 ) others refer to health tourism as a wider field with medical tourism as its subset (Carrera & Bridges, 2006 ; Smith & Puczko, 2009 ). In agreement with Smith and Puczko ( 2009 ), this study represents medical tourism distinctly from other subsets of health tourism. The word ‘medical’ here refers to illness, disorder or injuries. As put forth by Jagyasi ( 2008 ), medical tourism is “the set of activities in which a person travels often long distance or across the border, to avail medical services with direct or indirect engagement in leisure, business or other purposes”. Contrarily, health tourism is a wide-ranging phenomenon where travel can be undertaken for a variety of reasons from preventive and health-conductive treatment to rehabilitation and curative forms of travel (Dunets, et al., 2020 ). Other than medical tourism, health tourism encompasses other related fields like—wellness tourism (involving relaxation and exercises) and sports/adventure tourism (involving outdoor recreation) (Hall, 2011 ). Medical tourism itself has sub branches like ‘reproductive tourism’ and ‘dental tourism’. Another emerging term is “domestic tourism” which refers to the act of travelling within one’s own country for medical purposes (Hudson & Li, 2012 ; Reddy, 2010 ). This study focuses primarily on medical tourism and identifies this practice as travelling internationally to receive medical treatment.
Global Medical Tourism Trends
Lack of specific data, novelty of the concept, and the fragmented and unstructured nature of this industry makes it challenging to review this industry and give an estimate of its size (Chambers & McIntosh, 2008 ; de la Hoz-Correa et al., 2018 ). Prominent market research databases have reported global medical tourism market to be worth USD 104.7 billion in 2019, and have projected it to grow at a CAGR of 12.8%, to reach USD 273.7 billion by 2027 (Chhabra et al., 2021 ; Taheri et al., 2021 ).
Even though there is no fixed estimate of this industry, medical tourism is well-considered amongst the most dynamically growing industries today. Trade economists have documented a strong impact of this phenomenon on the global economy (Bookman & Bookman, 2007 ) especially the emerging countries of the world (Lee & Hung, 2010 ; Pafford, 2009 ). It not only adds to their foreign exchange, but also boosts investments in the medical and tourism sector streamlining their services (Ramirez de Arellano, 2007 ). Asia has been specifically considered as a hub for medical tourism (Connell, 2006 ). Countries like Singapore, India, Thailand, Brunei, Cuba, Hong Kong, Hungary, Israel, Jordan, Lithuania, Malaysia, the Philippines, and the United Arab Emirates have emerged as major providers for healthcare services to international patients (Heung, et al., 2010 ). Several other countries like Mexico, Turkey, Brazil, Costa Rica, Argentina and Bolivia are also working toward establishing themselves as major healthcare destinations (Singh, 2008 ).
The global demand and expenditure for healthcare services is on a rise due to factors such as growing and ageing populations, changing disease patterns and rapid transformations in costly digital technologies. With the rising disparity in healthcare costs, governments, corporations and individuals are looking at outsourcing healthcare facilities to emerging markets (Turner, 2007 ), especially those with advance and cost-effective healthcare facilities, and a proximity to developed countries. Medical tourism is also a viable and economical option for uninsured or underinsured patients. On the other hand, there is a substantial disparity in the quality of healthcare services. Patients from countries with limited government spending on healthcare and under developed private sector are forced to look at options beyond their borders. (KPMG, 2014 ).
Medical Tourism Industry in Asia
Last decade has seen Asia as an emerging leader of the medical tourism industry. This growth is fuelled by the availability of a variety of high quality and cost-effective medical procedures in Asia, improved connectivity and infrastructure and along with the presence of attractive locations to explore. The availability of advanced treatments in fields such as cardiology, neurology, orthopaedic, spine, ophthalmology along with aesthetics and alternative treatments like Ayurveda, Unani, Herbal and Yoga, makes Asia a sought-after destination. With private sector as the primary driver of medical tourism in this region, Asia has seen a faster growth of this industry vis-a-vis any other region globally. Many prominent healthcare providers in Asia are internationally accredited and have positioned themselves as distinguished service providers to patients from both within the region and far beyond. A market research on medical tourism industry anticipates the medical tourism market in Asia to cross USD 14 Billion by 2022 (iGATE Research, 2017 ). The research reports that Thailand, Singapore and India account for maximum proportion of international medical tourists in this region, followed by South Korea and Malaysia. Philippines and Taiwan are amongst other fast emerging markets in this sector. International patients contribute to a one-third or more of revenue in these private hospitals, and hence several private hospitals in this region are targeting this global world medical travellers’ market and have also gained a strong position for themselves in the industry (Mooter, 2017 ). An increased focus from government, foreign investment inflows and emerging startups are fueling up the competition not just between countries, but players as well. With the competition becoming stiffer, these countries and players are becoming more proactive in building their unique identifiers. Price is no longer the only factor of differentiation, countries are now looking at founding their proposition on parameters like diverse offerings, niche market, customized offering and even luxury (KPMG, 2014 ).
Medical Tourism Industry in India
Healthcare is amongst the largest and most complex sectors in India and is poised to touch USD 133.44 billion by 2020 (Outlook India, 2019 ). Healthcare in India is becoming one of biggest industries in terms of revenue generation and employment as well. Giving further impetus to this industry is the medical tourism sector which is bolstering the level of enhancements of care services in India. Table A1, as given in Supplementary Appendix file, states some basic facts related to the medical tourism industry in India. With its key differentiating factors of extremely competitive pricing, highly trained doctors, high quality care and availability of a range of treatments, India has realized the potential of medical tourism and positioned itself as one of the largest service providers in this region (Connell, 2013 ; KPMG, 2014 ; Medhekar et al., 2019 ). A study by KPMG India and Google, has pegged the medical travel industry in India at USD 4.8 Billion in 2017 (KPMG India & Google, 2018 ). The pre-Covid estimations expected the Indian medical tourism market to reach USD 13 billion by 2020 (KPMG India & Google, 2018 ). Despite the deliberative effects of Covid-19 on Travel and hospitality industry, the Indian medical tourism was estimated between USD 5–6 billion in 2021 (Financial Express, 2022 ). A right combination of cost efficiency and quality has driven the growth of this sector in India. Table A2, as given in supplementary appendix file, gives a comparative cost chart, for some common procedures, between India and other major medical tourism destination. Further the presence of a robust private sector, with international accreditations, has reinforced India’s standing. India offers a range of treatments from cardiology, neuro, paediatrics, ortho, ophthalmology, urology, gynaecology, general surgery, dental, cosmetics along with traditional healing options (Qadeer & Reddy, 2013 ). As per a report by Ministry of Tourism, Government of India, around 4,95,000 medical tourists travelled to India in 2017, with Bangladesh, Afghanistan, Iraq, Maldives being the top 5 source countries followed by Oman, Yemen, Uzbekistan, Kenya, Nigeria and Tanzania (Ministry of Tourism, 2018 ). In the following years larger share of travel is expected from Africa and GEC countries (KPMG India & Google, 2018 ).Realizing the opportunity, Government of India has taken a few initiatives to promote and encourage the growth of medical travel to the country. These include Government of India’s health tourism policy; setting up a ‘National Medical & Wellness Tourism Promotion Board’ for regulatory, accreditation and marketing issues; accreditation of hospitals under the National Accreditation Board for Hospitals; dedicated website to promote medical and wellness tourism; promotions at international platforms such as World Travel Mart London, ITB Berlin, ATM, etc.; coverage under Ministry of Tourism's ‘Incredible India Campaign’; introducing separate category of medical visas—‘M Visas’; a proposal for setting up tourism circuits, along with a medical circuit which will connect modern medicine centres and Ayurveda; providing fiscal support and other benefits under Market Development Assistance Scheme (MDA); and lowering import duties on medical technology, equipment and machinery (KPMG, 2014 ; Medhekar et al., 2019 ; Ministry of Tourism, 2018 ).
Key Dimensions of Medical Tourism Industry
This section presents the factors, as highlighted in the literature, that impact the development of medical tourism in a region. Cost and quality are considered amongst the most important dimensions of medical tourism industry (Aziz et al., 2015 ; Bagga et al., 2020 ; Cortez, 2008 ). Affordability and service quality of hospitality and tourism have also been considered as important attributes for a medical tourism destination (Chuang et al., 2014 ; Fetscherin & Stephano, 2016 ; Olya & Nia, 2021 ).
Several studies, e.g. Ghosh and Mandal ( 2019 ) and Fetscherin and Stephano ( 2016 ), have highlighted the importance of the type of treatments offered, medical facilities, practitioner competence, service quality and standards of medical care offered by the service providers (Kamassi et al., 2020 ). Technological upgradation and medical innovation are other important factors linked to the success in this sector (Cortez, 2008 ; Velasco et al., 2013 ). Literature also points towards the importance of trust, credibility, perception and hence the need for certification, international standards and accreditation (Debata et al., 2015 ; Hall, 2011 ; Seow et al., 2017 ).
Beladi et al. ( 2019 ) and Ebrahim and Ganguli ( 2019 ) have explored the role of human resource development and administrative efficiency. Infrastructure and facilities with regards to accommodation, transportation, communication are other important dimensions recognized for medical tourism (Heung & Kucukusta, 2013 ; Kamassi et al., 2020 ).
Country specific factors and attributes such as country knowledge, culture, language, accessibility, safety and security, have also been analysed (Bagga et al., 2020 ; Cham et al., 2021 ; Olya & Nia, 2021 ). Crouch and Ritchie ( 2005 ) in their study have highlighted the importance of socio-cultural and political environment of the destination country. Tourism-specific factors of the destination country, such as weather, attractions, culture and exoticness, have also been considered while studying the attractiveness of a medical tourism destination (Fetscherin & Stephano, 2016 ; Lovelock et al., 2018 ).
Medical tourism destination marketing, destination branding and tourism destination image have also been considered important with respect to the development of medical tourism in any region (Hoz-Correa & Muñoz-Leiva, 2019 ).
Studies have also observed public and private coordination and collaboration of the medical tourism stakeholders, to enhance the development of medical tourism sector (Beladi et al., 2019 ; Ebrahim & Ganguli, 2019 ). Government support and a favourable policy framework have been considered as important factors for this industry (Hall, 2011 ; Wang, 2012 ). Snyder et al. ( 2015 ) and Omay and Cengiz ( 2013 ) have specifically advocated the need for a regulatory framework and policy intervention to improve the efficiency coordination, uniformity and standardisation in this sector and promote the medical tourism industry (Momeni et al., 2018 ).
Methodology
Considering the emerging nature of this industry, qualitative approach was exercised to truly analyse the value proposition of India as a medical tourism destination. A qualitative framework encourages both theoretical and applied knowledge and aids in the development of novel and alternate theories (Bygrave, 1989 ; Creswell, 2013 ). Case study method was adopted to classify and analyse the dimensions that can position India as a prominent healthcare service provider for overseas patients. Merriam ( 2002 ) describes case study as a comprehensive description and examination of a phenomenon or a social unit of study. The case being studied becomes the boundary of the research, and by focussing on a single context this approach seeks to offer an extensive enquiry and meaning of the phenomenon under study (Creswell, 2007 ; Miles & Huberman, 1994 ; Yin, 2011 ). For the present research, context was bounded geographically and the problem at hand was thoroughly explored in the Delhi-NCR region. As also suggested by Stake ( 1995 ), a holistic analysis of medical tourism industry in Delhi NCR allowed for an instrumental way to investigate the phenomenon at a broader level in India.
The Case Study Context: Delhi NCR
This study was conducted in Delhi NCR, i.e. National Capital Region of India. It includes Delhi, officially the NCT, National Capital Territory in India and several other regions neighbouring it; Gurugram, NOIDA and Faridabad being the prominent ones. Delhi NCR has witnessed an unprecedented growth in both, the healthcare infrastructure and as well as services in this last decade. The presence of corporate majors like Fortis, Max, Apollo; high-end hospitals like Medanta, Artemis; day care surgery centres and specialised centres, such as for IVF, eye care, birthing centres; has enabled Delhi NCR to emerge as a healthcare hub (Kachhap, 2012 ). Increased activity from the new corporate players have also spurred the existing older players like BLK, Gangaram and Moolchand to revive and widen their portfolio. These healthcare brands are consistently working towards building a strong medical tourism sector. With its robust medical infrastructure, advanced medical specialities, competitive pricing and highly trained doctors, Delhi NCR is amongst the most prominent healthcare destinations in India for international patients. These hospitals provide valuable services to medical tourists, ranging from special wards and lounges for international patients and their companions, translator services, international cuisines, accommodation services and the like. Moreover, its connectivity, location and rich cultural heritage and presence of international standards of hospitality make Delhi NCR a prime tourist destination. These factors make Delhi NCR an important context for exploring the medical tourism industry in India as a whole.
Data Collection
The qualitative approach and exploratory nature of this study maintains that the researcher becomes an agency for data collection. This enables the researcher to get close to the social phenomenon being studied and enable a deeper understanding of the social reality (Bryman, 1988 ; Marshall & Rossman, 1995 ). This also gives researcher the flexibility to delve into the issues that emerge during the study. The qualitative data for this study was collected by the researchers through semi structured in-depth interviews with senior practitioners, and senior members of hospital management. Conducting interviews allowed the researchers to apprehend wide-ranging perspectives and experiences of respondents with regards to medical tourism.
Potential participants for interviews were identified through purposive sampling, to ensure appropriateness, purpose and rich information. Participants were selected from multi-speciality hospitals, offering healthcare services to medical tourists, and through ongoing referrals from interview participants. Table A3, as given in supplementary appendix file, gives a brief profile of the respondents of this study. As a wide-ranging guideline for qualitative design, the study did not look for an increasing number of cases but aimed to collect an extensive detail from each case under study (Creswell, 2007 ). For this research the number of participant cases to be studied was not predetermined. Instead, taking reference from Maykut and Morehouse ( 1994 ), as the study progressed and data was analysed, additional cases required were determined by the extent to which each additional case would contribute to the understanding of the research problem. Data collection was concluded when it was realised that the emerging issues and themes were getting “saturated” and no new data was being found (Creswell, 2007 ; Glaser & Strauss, 1967 ; Strauss & Corbin, 1990 , 1998 ). For this study data saturation occurred within 20 samples. Having a smaller sample size allowed the research to spend an extensive time with each case and encouraged that the understanding, of Delhi-NCR’s competitiveness as a medical tourism destination, which emerged was representative of the practitioners’ perspective (Shaw, 1999 ).
The interviews were conducted in the respondents’ hospitals. The interviews lasted for about 45 min. These were conducted face to face, were audio recorded, after checking with the participants, and later transcribed verbatim. Vital areas of concern were recognised after a thorough literature review on medical tourism and an appraisal of the dimensions of competitiveness of a medical tourism destination, identified by (Malhotra & Dave, 2022 ). These served as the guide for conducting interviews.
Data Analysis
Data was analysed by means of constant comparison method as outlined by Glaser and Strauss ( 1967 ), Strauss and Corbin ( 1990 , 1998 ) and Creswell ( 2007 ). Accordingly, data collection and data analysis were done simultaneously. This allowed the researcher to make necessary adjustment to the research process, such as, sample selection, and testing the emerging themes or concepts with subsequent data (Merriam, 2002 ). This study has adopted the ‘abduction’ logic for data analysis. An abductive analysis approach emphasizes that instead of keeping all predefined theoretical concepts aside, a researcher should enter the field with a broad theoretical understanding and during the research process develop and build upon their theoretical repertoires (Timmermans & Tavory, 2012 ). As also proposed by Lichy et al. ( 2020 ), since the data set for this study was modest in size, coding was conducted manually.
The theoretical background referred to in this paper is a study, by the same authors, on the dimensions and drivers of medical tourism industry. (Malhotra & Dave, 2022 ) previously developed this paper based on a systematic review of empirical studies on the medical tourism industry globally. The purpose of the study was to identify and analyse the factors and dimensions that influence the competitiveness of a country as a medical tourism destination. Figure 1 outlines the dimensions identified by their study. These are structured around the domains of medical tourism opportunity and a country’s positioning, infrastructure and health human resource competence, care delivery, governance and regulatory framework.
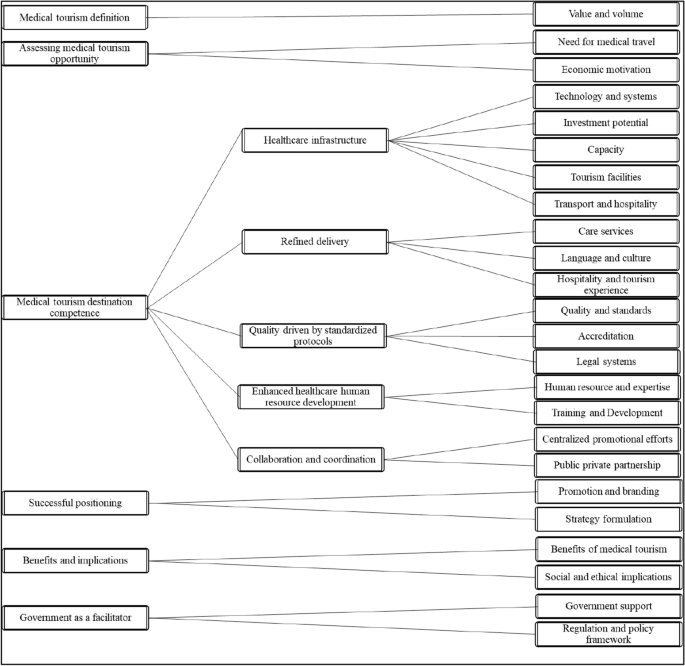
Source: Malhotra & Dave ( 2022 )
Factors influencing a country’s medical tourism industry.
This study uses the extant structure to systemize its findings from research work in Delhi NCR that pursues an understanding on how the value proposition of medical tourism industry can be redefined here. This helps us explore the wider relevance of the proposed dimensions in the study by (Malhotra & Dave, 2022 ) and its implications in a specific context. By analysing the experiences of the practitioners from Delhi NCR, the study has able been able to identify an additional dimension that impact a medical tourism destinations’ competitiveness. This dimension is the role of medical facilitators and it has been included in the existing domain of Refined Delivery. Taken together, this has helped to emerge a more comprehensive range of dimensions that are relevant for the development of an advanced medical tourism destination.
This section organises the fieldwork findings around the dimensions outlined in the (Malhotra & Dave, 2022 ) study to identify any contrast and facilitate discussion on Delhi-NCR’s proposition as a medical tourism destination. These dimensions are: assessing a country’s competence as a medical tourism destination, successful positioning and government as a facilitator. While each of these dimensions have been considered independently, for analytical purpose, the apparent correlation between these three domains should be acknowledged. Along with this the discussion also includes respondents’ views on the opportunity assessment of medical tourism for India, its benefits and social implications.

Assessing Medical Tourism as an Opportunity
The ambiguity in the size or figures of the medical tourism market, as highlighted in the literature review, was also reported in the fieldwork of this study. Participants emphasised the concern regarding lack of data on the volume of value of this industry or the market shares. Almost all respondents saw medical tourism as an opportunity for India. They reflected that the market is increasing on a year-to-year basis and that there is a huge potential for the coming 5 to 10 years as well. The major reasons reported for India’s exponential growth in this segment is its clinical expertise, major cost competitiveness over other countries, conducive and friendly environment.
“Reason for the growth is that India has the advantage of being clinically excellent. Technology if not the best is at par with most other countries, our clinicians are trained abroad and they are returning back to practice in India. So clinical excellence has built up” (Respondent 9) “Indian hospitals are clinically sound, environment is conducive, we have a price point advantage over many other countries, then we speak a language that is understood, or getting people who speak their language is easier and cost effective” (Respondent 11)
Some of the respondents also highlighted the evolution in the medical tourism industry, with destination countries getting matured and looking to invest in their own healthcare infrastructure, new medical tourist hubs coming up and a growing impetus of value driven services.
“Very soon you’ll see, facilities there will be developed, clinicians from here will go and train their people. They will still carry back procedures, which cannot be done there, because of the environment, or which require critical post-op care.” (Respondent 14)
Assessing a Country’s Competence as a Medical Tourist Destination
A well-crafted strategy can lay the foundation for a competitive destination for medical tourism and creating an environment of holistic care for medical tourists. The study shows a consensus on the competence of India and specifically Delhi NCR as a healthcare provider.
Healthcare Infrastructure
In the last decade, Delhi NCR has seen the emergence of a robust private healthcare system. Most respondents agreed that Delhi-NCR’s healthcare infrastructure, if not superior, is at par with most other destinations. And that it is one of prominent drivers of medical tourism industry here.
“In purely technical terms of medical infrastructure, I think we are at par with both Singapore and Thailand, or any other country for that matters, where they have an edge over us?? I think it’s in terms of their overall infrastructure…their ethos of cleanliness for example. It takes us an effort to do that, whereas in a place like Singapore it’s given, so that’s the challenge for us Indians” (Respondent 9)
Refined Delivery
Respondents indicate a lack of streamlined and standardised care delivery. This includes not just healthcare services, but service touch points of travel, tourism, airport and hospitality. While Delhi NCR has an appeal over factors such as accommodation, cultural adaptability, language interpreters and general conduciveness, it still has a long way to go.
“Facilities and infrastructure in hospitals are no less than anywhere else, but I think the degree of professionalism can improve a lot. Our systems and processes are not as smooth as how they should be... like the whole process starts when a patient needs medical care in a certain country, so he gets in touch with a local hospital or agent in the source country who in turn gets in tough with the hospital here, that interface could be smoother.” (Respondent 11) “It’s not about their lack of trust on India’s healthcare system, its generally the perception of India as a country and safety of their travel. Say for e.g., patient addressal mechanism could be stronger.” (Respondent 6)
The ‘role of medical facilitators’ was not highlighted in (Malhotra & Dave, 2022 ) original framework. The research work in this study in the Delhi-NCR region, however, raised a number of critical systems impacts and policy implications regarding the role of medical facilitators or middlemen in the Indian medical tourism market. Participants demonstrated a consistent view regarding the prominent role of the facilitators in the medical value chain, in channelizing the international patients towards a particular country and subsequently a healthcare service provider. There was also a prevalent concern regarding the lack of transparency and regulation in the way these middlemen operate, quality of service delivered, corruption or any unethical practices, and most of all a lack of credibility. Participants expressed an apprehension on the way these facilitators impact the quality of care delivery or the overall experience of overseas patients.
“There are these middlemen, also known as facilitators, they form a very important but also the weakest link in this chain. There is no accountability, no regulation… all this can severely impact the service delivery and in turn our name, our credibility goes down” (Respondent 8)
Quality Driven by Standardized Protocols
Most respondents have recognised the importance of accreditation. Issue of safety and quality is a primary concern for the medical tourists. Delhi-NCR hospitals are accredited with both Indian standard of—National Accreditation Board for Hospitals and Healthcare Providers (NABH) and more importantly Joint Commission International (JCI).
“NABH is a recent Indian government initiative to get some sort of quality standardisation in the healthcare industry, it’s not as stringent as JCI, but at least some initiation has been done.” (Respondent 4) “We had our first international accreditation done in 2006 and now second one around 2011–12. The Indian NABH is comparable, but it’s fairly new and not recognised well in international market. Say JCI is well recognised internationally, so we have to get that done if we want to get recognition in the international healthcare industry. Though sometime one is not able to justify the cost incurred on these international accreditations, but still they are very important.” (Respondent 15)
Enhanced Healthcare Human Resource Development
Though Delhi-NCR’s hospitals are clinically competent, lack of skill at the paramedic level was felt by several; respondents. Most respondents reflected the need for superior training programmes for paramedics, and not just in specialities but also in general category and front staff. Only then will service quality standards be met. Respondents expressed the problem of lack of retention of trained paramedics and healthcare workforce.
“Areas of improvement for us would be paramedics. We don’t have training institutes; we need to have a much more vibrant infrastructure for skilling people. Skill development is not there. One excuse given here is the numbers we deal with makes it impossible to work on trainings…” (Respondent 8) “Doctors travel to enhance their skills, where is the exposure for paramedics? On the job training is never enough to improve their service standards.” (Respondent 2)
Coordination and Collaboration for a Superior Care Delivery
Most respondents highlighted a lack of coordination or participation at an industry level. Though several forums like FICCI, CII and the like have been recognised to have some level of representation, however these collaborations and partnerships are still at an early stage. An important reason highlighted was the clash of opinions between players. The industry is still at a fragmented state, where each hospital is strategizing to increase its share in the pie.
Successful Positioning
Most respondents spoke about the individual efforts and strategies, at the group hospital level. Each corporate is trying to position in the international market, in its own capacity. There are some efforts by the government as well in this regard.
“Yes, these corporate groups and other private players are strategizing for capturing medical tourism market, it is a big agenda for them.” (Respondent 5 )
By far, Delhi NCR has been able to position itself as a clinically competent and a cost-effective player. It also scores over other players in terms of its cultural adaptability and soft service skills. Indian doctors are considered more approachable.
“On the price that we are charging, the service that we are giving is very good. We have a patient from Canada, he tells us that our service quality, the kind of attention we give is far better than what they get in west. Because, here we give personal attention, people talk to you, they are ready to go out of their way to help you…” (Respondent 3)
Government as a Facilitator
There was a mixed opinion regarding the role of government as a facilitator. A majority of the respondents felt that government should stay out of the medical tourism sector and the system. They strongly felt that any kind of intervention or regulation by the government would hamper the growth of this industry in India.
“Thankfully govt doesn’t interfere, else the business would go down. As in case of many other sectors... the fact that govt has stayed away from this business like in case of IT sector, has helped the business to come to a certain level... the moment govt steps in, and starts the process of licencing, permits, accreditation. the whole system will come down… let this run as a free market interaction, cause that will bring the best quality at the lowest price… leave the market to its business...” (Respondent 7)
The other opinion recognises the government’s efforts in a positive state. They feel the government has stepped in whenever it needs to, for visa facilitation, rationalisation of visa costs as the like. Initiatives from government and regulatory bodies are required to make the system cleaner and more transparent.
“Regulation is like a double edge sword, it helps you in certain things, it harms you in certain ways. So as long as the regulations are crafted carefully, taking in to the considerations the infrastructure of the institutions…” (Respondent 15)
Social Implications and Benefits of Medical Tourism
The widely shared outlook demonstrated the positive impact of medical tourism on a country’s healthcare and tourism industry. Participants expressed a consistent vision of an overall upgradation of both healthcare and basic infrastructure in the country as a result of the fast-growing competition in the medical tourism market. The participants typically did not express a concern on the social implication of medical tourism industry on the domestic healthcare industry of India, however suggested a holistic outlook to the entire proposition.
“We should not ague on how encouraging medical tourism in India can have a negative impact in our own healthcare burden... If you see we have come a long way, our healthcare system, our medical expertise, technology, has progressed immensely… competition is good for any industry.” (Respondent 12) “If we talk about the impact of medical tourism on Indian healthcare industry, I should say it’s been a positive one… this proposition has added value, credibility and given us a global visibility. One can see a long-term benefit to the domestic industry, not just healthcare but other sectors as well, tourism, logistics, hospitality… Our overall standards of service and hospitality is increasing.” (Respondent 12)
Research aimed at exploring the sources of competitiveness, in a particular industry, for firms competing in international or regional markets (e.g., Momaya, 2019 ; Moon et al., 2015 ; Thompson et al., 2013 ) have emphasised the role of abilities, proprietary knowledge, innovation capability, sustainable business and economic model, technological innovation, pace of internationalisation, quality, business excellence and human resources. Based on our research and taking these factors into consideration, India’s capability as a medical tourism destination is assessed below and gap areas identified. Table 1 provides a synthesis of the growth drivers for India’s medical tourism industry and the opportunity scope.
With increasing significance of quality and outcomes of the service (Mishra & Sharma, 2021 ), ‘value’ has become the watchword for the healthcare industry. The term to be used here is then medical ‘value’ travel. The addressable market is huge and several countries are strategizing to tap into this opportunity. India’s needs to build a value proposition around the right combinations of cost and quality efficiency.
Clinical expertise and cost are primarily the two important drivers of medical tourism market in India (Ebrahim & Ganguli, 2019 ). It has an edge over other countries with respect to its cost competitiveness. With several prominent super speciality brand names, Delhi NCR has become a hub for medical tourism. The emergence of a robust private sector has significantly enhanced the quality and standards of healthcare. With the presence of clinical and technical expertise, and international standards, Delhi’s credibility as a medical destination is on a rise. Delhi also scores high on the parameters like cultural adaptability and soft skills. The surge in emerging unconventional formats of healthcare delivery and technological revolutions are further fuelling the growth of this industry in India.
Delhi’s holistic appeal as a medical travel destination is hampered by a significantly poor perception on factors such as safety, travel infrastructure, tourism experience and streamlined systems. There have been few initiatives from the government, however much work needs to be done. Regulatory initiatives are specifically required in the areas of transparent accreditation to prevent false claims and substandard care deliveries. Most of all there needs to be a streamlined effort to bring the industry together and work on common grounds of promotion, streamlined systems and travel infrastructure. The medical facilitators play a prominent role in the medical tourism value chain. However, there is an urgent need to define and regularise their position. The channel needs to be streamlined to promote transparency in the process and curtail any unethical and unfair practice that can impact the service outcome and in turn the overall credibility.
Delhi NCR, being the capital and focal point of major developments in the country, has significant scope for improvements in airport and travel infrastructure. As in case of the hospitality industry, service delivery standards need to get streamlined in healthcare industry as well. This would mean investing in training and retaining of paramedics, not just with specialities, but general nurses and staff well.
Industry to focus on brand building initiatives, driven by digital marketing solutions and user specific marketing campaigns. Industry can leverage from collaborative efforts of the stakeholders and public private partnerships to extend potentials of enhancing expertise, efficiency and investment. Most of all it is critical to focus on factors like safety, pollution, drinking water quality, sanitation and corruption to promote a strong positive image of the country that can positively impact medical tourism industry.
As the market is getting matured, industry dynamics are changing. ‘Value’ and ‘Sustainability’ have become the operative words around the world. India and specifically Delhi NCR can look at streamlining the medical value chain by adding and generating value at each touch point, both for India and the source country. With countries which are ready to step up their healthcare facilities, India can explore the option of ‘reverse medical travel’, where in Indian doctors can help set up facilities in the source countries and train their health resources. The complicated and serious procedures will still have to refered back to India, due to the nature of procedure or the critical post-op are required. Such initiatives have already started taking place, but at a minuscule scale. Indian healthcare system needs to take a giant leap towards leveraging the unconventional operating models and technological revolutions, building an ecosystem that encourages and supports innovation. Tapping the international market in a big way will further power this growth.
Limitations and Avenues for Future Research
Case study research has an inherent limitation of generalisability. This research is limited to redefining the value proposition of the medical tourism industry in the Delhi-NCR region only. However, to get an overall perspective of India as a destination, such a study needs to get extended to other major medical tourism hubs as well, such as Chennai, Hyderabad, Kolkata, Mumbai. Also, this study is limited to the surgical aspect of the medical tourism market. Further research could also focus on another growing segment of wellness tourism. Domestic tourism is also an important but a relatively unexplored area. Other micro-niche areas can be super-specialities such as cardiac, ortho, dental, or reproductive services. Facilitators for an important but a very weak link in the medical travel value chain. Further research could focus to either remove or to strengthen this link.
India’s evolution, as amongst the world’s most preferred medical tourist destinations, is expected to sustain a steady growth. This growth is driven by five major factors: cost competitiveness, medical expertise, quality of healthcare services, robust private sector and cultural adaptability. Even as these factors propel India forward, there are some major gaps to bridge. The most pressing concerns in front of the Indian medical tourism industry are paucity of an amenable policy framework, inadequate tourism and logistic infrastructure, unstandardized service quality standards, and India’s poor perception on macroeconomic factors such as corruption, environment quality, safety. To successfully build a future of envisioned growth, India must place a premium on a collaborative effort from all the stakeholders, to address these issues; a commitment to innovation and sustained inclusive growth.
As for the healthcare systems around the world, COVID-19 pandemic has shaken the foundations of Indian healthcare industry as well. With business and health restrictions, medical tourism industry also suffered the initial setback (Ayittey, 2020 ). Government, tourism companies and healthcare providers are struggling to remodel their business to adjust to current realities, withstand the pandemic and accelerate recovery. As the trajectory of the COVID-19 pandemic is not clear, the future remains uncertain. This pandemic and uncertainty around it have further intensified the need for the industry players to direct their focus on realignment and revaluation of their business models and work towards enhancing resilience and agility.
The purpose of this research is to analyse the factors that are crucial for India to identify, create and finally deliver a distinctive value proposition as medical tourism destination. Following a literature review and a qualitative study with Delhi NCR as a case, this research advances the medical tourism body of knowledge. The paper discusses the research process and the methodology adopted for the study in detail. Finally, the report analyses India’s, and specifically Delhi-NCR’s, competence as a medical tourist destination and synthesises the key growth drivers and opportunities for this industry.
Key Questions Reflecting Applicability in Real Life
What are the critical success factors in medical tourism industry?
What are the dimensions and factors that can help India increase its competitiveness as a medical tourism destination?
How can service providers ensure a steady growth of the medical tourism ecosystem, to ensure sustainability and competitiveness?
What role can policy support play for the medical tourism ecosystem in India and its competitiveness?
How has the Covid-19 Pandemic affected the medical tourism ecosystem? Which segment of the industry can rebound stronger in which cities?
Data Availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Code Availability
Code sharing is not applicable to this study as no new code was created or analysed in this study.
Abubakar, A. M., & Ilkan, M. (2016). Impact of online WOM on destination trust and intention to travel: A medical tourism perspective. Journal of Destination Marketing & Management, 5 (3), 192–201. https://doi.org/10.1016/j.jdmm.2015.12.005
Article Google Scholar
Ayittey, F. K., Ayittey, M. K., Chiwero, N. B., Kamasah, J. S., & Dzuvor, C. (2020). Economic impacts of Wuhan 2019-nCoV on China and the world. Journal of Medical VIrology, 92 (5), 473. https://doi.org/10.1002/jmv.25706
Aziz, A., Yusof, R. M., Ayob, M., & Bakar, N. T. A. (2015). Measuring tourist behavioural intention through quality in Malaysian medical tourism industry. Procedia Economics and Finance, 31 , 280–285. https://doi.org/10.1016/S2212-5671(15)01179-X
Bagga, T., Vishnoi, S. K., Jain, S., & Sharma, R. (2020). Medical tourism: Treatment, therapy and tourism. International Journal of Scientific and Technology Research, 9 (3), 4447–4453.
Google Scholar
Beladi, H., Chao, C. C., Ee, M. S., & Hollas, D. (2019). Does medical tourism promote economic growth? A cross-country analysis. Journal of Travel Research, 58 (1), 121–135. https://doi.org/10.1177/0047287517735909
Bookman, M., & Bookman, K. (2007). Medical tourism in developing countries . Palgrave Macmillan.
Book Google Scholar
Bryman, A. (1988). Doing Research in Organisations . Routledge.
Bygrave, W. (1989). The entrepreneurship paradigm (I): A philosophical look at its research methodologies. Entrepreneurship Theory and Practice, 14 (1), 7–26.
Carrera, P., & Bridges, J. (2006). Globalization and healthcare: Understanding health and medical tourism. Expert Review of Pharmacoeconomics and Outcomes Research . https://doi.org/10.1586/14737167.6.4.447
Cham, T. H., Lim, Y. M., Sia, B. C., Cheah, J. H., & Ting, H. (2021). Medical tourism destination image and its relationship with the intention to revisit: A study of Chinese medical tourists in Malaysia. Journal of China Tourism Research, 17 (2), 163–191. https://doi.org/10.1080/19388160.2020.1734514
Chambers, D., & McIntosh, B. (2008). Using authenticity to achieve competitive advantage in medical tourism in the English-speaking Caribbean. Third World Quarterly, 29 , 919–937. https://doi.org/10.1080/01436590802106056
Chhabra, A., Munjal, M., Mishra, P. C., Singh, K., Das, D., Kuhar, N., & Vats, M. (2021). Medical tourism in the Covid-19 era: Opportunities, challenges and the way ahead. Worldwide Hospitality and Tourism Themes . https://doi.org/10.1108/WHATT-05-2021-0078
Chuang, T. C., Liu, J. S., Lu, L. Y., & Lee, Y. (2014). The main paths of medical tourism: From transplantation to beautification. Tourism Management, 45 , 49–58. https://doi.org/10.1016/j.tourman.2014.03.016
Connell, J. (2006). Medical tourism: Sea, sun, sand and… surgery. Tourism Management, 27 (6), 1093–1100. https://doi.org/10.1016/j.tourman.2005.11.005
Connell, J. (2013). Contemporary medical tourism: Conceptualisation, culture and commodification. Tourism Management, 34 , 1–13. https://doi.org/10.1016/j.tourman.2012.05.009
Cortez, N. (2008). Patients without borders: The emerging global market for patients and the evolution of modern health care. Indiana Law Journal, 83 , 1–24.
Creswell, J. W. (2007). Qualitative inquiry and research design: Choosing among five approaches (2nd ed.). Sage Publications Inc.
Creswell, J. (2013). Qualitative Inquiry & Research Design Choosing among Five Approaches . CA Sage: Thousand Oaks.
Crouch, G. I., & Ritchie, J. B. (2005). Application of the analytic hierarchy process to tourism choice and decision making: A review and illustration applied to destination competitiveness. Tourism Analysis, 10 (1), 17–25. https://doi.org/10.3727/1083542054547930
De La Hoz-Correa, A., & Muñoz-Leiva, F. (2019). The role of information sources and image on the intention to visit a medical tourism destination: A cross-cultural analysis. Journal of Travel & Tourism Marketing, 36 (2), 204–219. https://doi.org/10.1080/10548408.2018.1507865
De la Hoz-Correa, A., Muñoz-Leiva, F., & Bakucz, M. (2018). Past themes and future trends in medical tourism research: A co-word analysis. Tourism Management, 65 , 200–211. https://doi.org/10.1016/j.tourman.2017.10.001
Debata, B. R., Patnaik, B., Mahapatra, S. S., & Sree, K. (2015). Interrelations of service quality and service loyalty dimensions in medical tourism: A structural equation modelling approach. Benchmarking: an International Journal, 22 (1), 18–55. https://doi.org/10.1108/BIJ-04-2013-0036
Deloitte Global. (2021). Digital transformation and health care delivery model convergence. Retrieved from https://www2.deloitte.com/content/dam/Deloitte/global/Documents/Life-Sciences-Health-Care/gx-digital-transformation.pdf
Dunets, A. N., Yankovskaya, V., Plisova, A. B., Mikhailova, M. V., Vakhrushev, I. B., & Aleshko, R. A. (2020). Health tourism in low mountains: A case study. Entrepreneurship and Sustainability Issues, 7 (3), 2213. https://doi.org/10.9770/jesi.2020.7.3(50)
Ebrahim, A. H., & Ganguli, S. (2019). A comparative analysis of medical tourism competitiveness of India, Thailand and Singapore. Tourism: an International Interdisciplinary Journal, 67 (2), 102–115.
Fetscherin, M., & Stephano, R. M. (2016). The medical tourism index: Scale development and validation. Tourism Management, 52 , 539–556. https://doi.org/10.1016/j.tourman.2015.08.010
Financial Express. (2022, March). Medical value tourism in India: What makes the country a leading Medical Tourism Destination. Financial Express.
Ganguli, S., & Ebrahim, A. (2017). A qualitative analysis of Singapore’s medical tourism competitiveness. Tourism Management Perspectives . https://doi.org/10.1016/j.tmp.2016.12.002
Ghosh, T., & Mandal, S. (2019). Medical tourism experience: Conceptualization, scale development, and validation. Journal of Travel Research, 58 (8), 1288–1301. https://doi.org/10.1177/0047287518813469
Glaser, B., & Strauss, A. (1967). The Discovery of Grounded Theory Strategies for Qualitative Research . CA Sociology Press.
Gola, S. (2016). Medical tourism in India – in whose interest? Journal of International Trade Law and Policy, 15 (2/3), 115–133. https://doi.org/10.1108/JITLP-01-2016-0005
Hall, C. M. (2011). Health and medical tourism: A kill or cure for global public health? Tourism Review, 66 (1/2), 4–15. https://doi.org/10.1108/16605371111127198
Heung, V. C., & Kucukusta, D. (2013). Wellness tourism in China: Resources, development and marketing. International Journal of Tourism Research, 15 (4), 346–359. https://doi.org/10.1002/jtr.1880
Heung, V., Kucukusta, D., & Song, H. (2010). A conceptual model of medical tourism: implications for future research. Journal of Travel and Tourism Marketing, 27 (3), 236–251. https://doi.org/10.1080/10548401003744677
Hudson, S., & Li, Z. (2012). Domestic Medical Tourism: A Neglected Dimension of Medical Tourism Research. Journal of Hospitality Marketing & Management, 21 (3), 227–246. https://doi.org/10.1080/19368623.2011.615018
iGATE Research. (2017). Asia Medical Tourism Market and Forecast To 2022.
Jagyasi, P. (2008). Defining medical tourism - Another approach. Medical Tourism Magazine, 6 , 9–11.
Kachhap, M. (2012). Developing Delhi - Express Healthcare. Retrieved from www.expresshealthcare.in : https://www.expresshealthcare.in/archive/developing-delhi/563/
Kamassi, A., Abd Manaf, N. H., & Omar, A. (2020). The identity and role of stakeholders in the medical tourism industry: State of the art. Tourism Review . https://doi.org/10.1108/TR-01-2019-0031
KPMG. (2014). Medical value travel in India. FICCI Heal Conference. KPMG India.
KPMG India, & Google. (2018). Indian brands going global, A USD39 billion opportunity.
Lee, C., & Hung, W. (2010). Tourism, health and income in Singapore. International Journal of Tourism Research, 12 (4), 355–359. https://doi.org/10.1002/jtr.755
Lichy, J., Farquhar, J. D., & Kachour, M. (2020). Entrepreneurship via social networks–“connected woman” in Lebanon. Qualitative Market Research: An International Journal. https://doi.org/10.1108/QMR-01-2020-0004
Lovelock, B., Lovelock, K., & Lyons, K. (2018). The impact of outbound medical (dental) tourism on the generating region: New Zealand dental professionals’ perspectives. Tourism Management, 67 , 399–410. https://doi.org/10.1016/j.tourman.2018.02.001
Malhotra N. & Dave K. (2022). Dimensions and Drivers of Medical Tourism Industry: A Systematic Review of Qualitative Evidence. International Journal of Business and Globalisation . https://doi.org/10.1504/IJBG.2022.10042738 (in press).
Marshall, C., & Rossman, G. (1995). Designing Qualitative Research (2nd ed.). Sage.
Maykut, P., & Morehouse, R. (1994). Beginning Qualitative Research: A Philosophical and Practical Guide . The free press.
Medhekar, A., Wong, H. Y., & Hall, J. E. (2019). Factors influencing inbound medical travel to India. Journal of Health Organization and Management . https://doi.org/10.1108/JHOM-08-2018-0234
Merriam, S. B. (2002). Introduction to qualitative research. In S. B. Merriam (Ed.), Qualitative research in practice: Examples for discussion and analysis (pp. 1–33). San Francisco: Jossey-Bass
Miles, M. B., & Huberman, A. M. (1994). Qualitative data analysis (2nd ed.). Sage Publications.
Ministry of Tourism. (2018). India Tourism Statistics 2018. Ministry of Tourism, Government of India.
Mishra, V., & Sharma, M. G. (2021). Framework for promotion of medical tourism: A case of India. International Journal of Global Business and Competitiveness, 16 (1), 103–111. https://doi.org/10.1007/s42943-021-00027-7
Momaya K. S. (2019). The past and the future of competitiveness research: A review in an emerging context of innovation and EMNEs. International Journal of Global Business and Competitiveness, 14 (1), 1–10. https://doi.org/10.1007/s42943-019-00002-3
Momeni, K., Janati, A., Imani, A., & Khodayari-Zarnaq, R. (2018). Barriers to the development of medical tourism in East Azerbaijan province, Iran: A qualitative study. Tourism Management, 69 , 307–316. https://doi.org/10.1016/j.tourman.2018.05.007
Moon, H. C., Lee, Y. W., & Yin, W. (2015). A new approach to analysing the growth strategy of business groups in developing countries: The case study of India’s Tata Group. International Journal of Global Business and Competitiveness, 10 (1), 1–15.
Mooter, B. V. (2017, Nov). Medical Tourism in Asia-Pacific Growing Rapidly. BRINK, The Edge of Risk.
Olya, H., & Nia, T. H. (2021). The medical tourism index and behavioral responses of medical travelers: A mixed-method study. Journal of Travel Research, 60 (4), 779–798. https://doi.org/10.1177/0047287520915278
Omay, E. G. G., & Cengiz, E. (2013). Health tourism in Turkey: Opportunities and threats. Mediterranean Journal of Social Sciences, 4 (10), 424–424. https://doi.org/10.5901/mjss.2013.v4n10p424
Outlook India. (2019, July). Heath is Priceless Live Healthy. Outlook.
Pafford, B. (2009). The third wave–Medical tourism in the 21st century. Southern Medical Journal, 102 (8), 810–813. https://doi.org/10.1097/smj.0b013e3181aa8ce4
Qadeer, I., & Reddy, S. (2013). Medical tourism in india: Perceptions of physicians in tertiary care hospitals. Philosophy, Ethics, and Humanities in Medicine. https://doi.org/10.1186/1747-5341-8-20
Rahman, R. (2019). The privatisation of healthcare system in Bangladesh. International Journal of Health Care Quality Assurance . https://doi.org/10.1108/IJHCQA-11-2017-0217
Ramirez de Arellano, A. (2007). Patients without borders: The emergence of medical tourism. International Journal of Health Services, 37 (1), 193–198. https://doi.org/10.2190/4857-468G-2325-47UU
Reddy, G. R. (2010). Travel for treatment: Students’ perspective on medical tourism. International Journal of Tourism Research, 12 , 510–522. https://doi.org/10.1002/jtr.769
Seow, A. N., Choong, Y. O., Moorthy, K., & Chan, L. M. (2017). Intention to visit Malaysia for medical tourism using the antecedents of Theory of Planned Behaviour: A predictive model. International Journal of Tourism Research, 19 (3), 383–393. https://doi.org/10.1002/jtr.2120
Shaw, E. (1999). A guide to the qualitative research process. Qualitative Market Research: An International Journal, 2 (2), 59–70. https://doi.org/10.1108/13522759910269973
Singh, P. K. (2008). Medical tourism . Kanishka Publishers.
Smith, M., & Puczko, L. (2009). Health and wellness tourism . Elsevier.
Stackpole, I., Ziemba, E., & Johnson, T. (2021). Looking around the corner: COVID-19 shocks and market dynamics in US medical tourism. The International Journal of Health Planning and Management, 36 (5), 1407–1416. https://doi.org/10.1002/hpm.3259
Stake, R. E. (1995). The art of case study research . Sage Publications.
Strauss, A., & Corbin, J. M. (1990). Basics of qualitative research: Grounded theory procedures and techniques . Sage Publications Inc.
Strauss, A., & Corbin, J. M. (1998). Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory . Sage Publications Inc.
Snyder, J., Byambaa, T., Johnston, R., Crooks, V. A., Janes, C., & Ewan, M. (2015). Outbound medical tourism from Mongolia: A qualitative examination of proposed domestic health system and policy responses to this trend. BMC Health Services Research, 15 (1), 1–8. https://doi.org/10.1186/s12913-015-0849-5
Taheri, B., Chalmers, D., Wilson, J., & Arshed, N. (2021). Would you really recommend it? Antecedents of word-of-mouth in medical tourism. Tourism Management, 83 , 104209. https://doi.org/10.1016/j.tourman.2020.104209
Thayarnsin, S. L., & Douglas, A. C. (2016). A Systematic Review of Challenges in Medical Tourism Destination Management . Travel and tourism research association: Advancing tourism research globally
Thompson, A., Peteraf, M., Gamble, J., Strickland, A. J., III., & Jain, A. K. (2013). Crafting & executing strategy 19/e: The quest for competitive advantage: Concepts and cases . McGraw-Hill Education.
Timmermans, S., & Tavory, I. (2012). Theory construction in qualitative research: from grounded theory to abductive analysis. Sociological Theory, 30 (3), 167–186. https://doi.org/10.1177/0735275112457914
Turner, L. (2007). First world health care at third world prices’: Globalization, bioethics and medical tourism. BioSocieties, 2007 , 303–325. https://doi.org/10.1017/S1745855207005765
Velasco, R. P., Myint, C. Y., Khampang, R., Tantivess, S., & Teerawattananon, Y. (2013). Advanced health biotechnologies in Thailand: Redefining policy directions. Journal of Translational Medicine, 11 (1), 1. https://doi.org/10.1186/1479-5876-11-1
Virani, A., Wellstead, A. M., & Howlett, M. (2020). Where is the policy? A bibliometric analysis of the state of policy research on medical tourism. Global Health Research and Policy, 5 (1), 1–16. https://doi.org/10.1186/s41256-020-00147-2
Wang, H. Y. (2012). Value as a medical tourism driver. Managing Service Quality: An International Journal, 22 (5), 465–491. https://doi.org/10.1108/09604521211281387
Yeoh, E., Othman, K., & Ahmad, H. (2013). Understanding medical tourists: Word-of-mouth and viral marketing as potent marketing tools. Tourism Management, 34 , 196–201. https://doi.org/10.1016/j.tourman.2012.04.010
Yin, R. K. (2011). Applications of Case Study Research . Sage.
Download references
Acknowledgements
The authors extend their special thanks to all the respondents of this study, who despite their busy schedules and heavy engagements, took time to give us their insights and critical inputs to improve the quality of this research. Besides, the authors wish to acknowledge all the reviewers including the members on the Editorial Board of this journal, whose constructive critique helped in improving the quality of the paper to a great extent.
The authors declare that there was no funding from any agency or institution for conducting this study.
Author information
Authors and affiliations.
Ambedkar University, Delhi, India
Neha Malhotra & Kartik Dave
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by NM and KD. The first draft of the manuscript was written by NM and all authors read and approved the final manuscript.
Corresponding author
Correspondence to Neha Malhotra .
Ethics declarations
Conflict of interest.
On behalf of all authors, the corresponding author states that there is no conflict of interest. The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (PDF 533 KB)
Rights and permissions.
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Malhotra, N., Dave, K. An Assessment of Competitiveness of Medical Tourism Industry in India: A Case of Delhi NCR. JGBC 17 , 215–228 (2022). https://doi.org/10.1007/s42943-022-00060-0
Download citation
Received : 25 March 2022
Accepted : 05 July 2022
Published : 01 August 2022
Issue Date : December 2022
DOI : https://doi.org/10.1007/s42943-022-00060-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical tourism
- Emerging countries
- Destination competitiveness
- Destination marketing
- Opportunities
- Find a journal
- Publish with us
- Track your research
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Factors Influencing Medical Tourism in India: A Critical Review

2019, Samvad
With the ascend of scientific and technical progression by developing economies of the world, transcontinental healthcare services have become a reality. Medical tourism attempts to entice tourists by intentionally promoting its healthcare services and facilities, in addition to its regular tourist comforts. The aim of the present study is to develop a conceptual model of factors influencing medical tourism and inclusive growth in India based on the evidence from past. The study is approached from the theoretical perspective, comprehensively assesses and analyzes the previous literature to discuss the role of medical tourism as a boon for inclusive growth. The present study develops a conceptual model on factors influencing medical tourism and discusses how the antecedents of medical tourism including individual-related and provider-related creates the value for a destination. The dimensions of medical tourism are basic resources which are indispensable for attaining inclusive growth. An apparent limitation of the present study was the non-existence of the contributions based on the empirical data.
Related Papers
Empirical Economics Letters
Suresh C H A N D R A ch , parashuramulu bongani
Favourable support from Government of India and presence of dominating pharma sector supported by advanced medical facilities has combinedly supported for the growth of Medical Tourism in India. Though the present share of total tourism is less than ten percent, yet the medical tourism sector has been prospering well. The rising tourist arrivals rate for medical tourism has shown positive signs of development. In this paper, a critical examination is made on development of medical tourism in terms of comparison of medical procedures, segment wise analysis on foreign tourist arrivals and role of government for the development of medical tourism. The study is a descriptive research oriented. The analysis is made on the basis of reports extracted from Ministry of Tourism, Government of India.
International Journal of Global Business and Competitiveness
Vinaytosh Mishra
IAEME Publication
We have all grown up hearing “Health is Wealth” but today the same preaching holds good as the Health Industry in India witnesses enormous growth and has become a big revenue generator thus attempting to create wealth for the nation especially during the times when the dollar is overpowering the rupee. The cost effectiveness of medical treatments in India without a compromise on the quality & standards has led to the growth of Medical or Health Tourism industry in the Country. India has long been known all over the world for the best medical and healing solutions, this has contributed to large inflow of foreign medical tourists to India to explore the fast and convenient Health Tourism services. It has been a tradition in India to consider guests as incarnations of God (atithi devo bhava) and are given prime importance, so the treatment offered to such tourists is definitely par excellence. Indian Medical Tourism aims to help tourists who visit India for any kind of medical treatment, be it organ transplant, dental treatment, implants, joint replacements or surgeries by organizing hassle free health travel and health treatment for them. India has always had well qualified, competent doctors in each and every specialization, and this fact has now been realized world over. India’s world class Medical Facilities with most competitive charges for treatments, has made India a very lucrative destination for people wanting to undergo treatment for any ailment. This Paper attempts to study the factors that have initiated the growth of Medical Tourism in India and what needs to be done to over come the obstacles faced by this Industry in order to keep this industry growing in the years to come so as to make Health a contributor to Wealth in India
Dr. Ramachandran Manickam , Bhavna R Sharma
Patil chetan Vitthal [2] Amrutkar Rupesh subhash [3] Bhavna R Sharma [4] M. Ramachandran [1][2][3] Abstract Medical tourism is a rapidly-growing practice of travelling across international borders to obtain health care. It encompasses primarily and predominantly biomedical procedures, combined with travel and tourism. The term medical tourism has been coined by travel agencies and the mass media to describe the rapidly growing practice of travelling across international borders to obtain hi-tech medical care. The key competitive advantages of India in medical tourism stem from the following: low cost advantage, strong reputation in the advanced healthcare segment and the diversity of tourist destinations available in the country. Medical tourism or health care tourism is fast growing multibillion-dollar industry around the world. It is an economic activity that entails trade in services and represents the mixing of two of the largest world industries: medicine and tourism. The paper identifies the strengths of India's medical tourism service providers and points at a number of problems that may reduce the growth opportunity of this industry. This paper focuses on the key issues and opportunities possessed by Indian medical tourism sector that enable it to overcome domestic and international barriers on upgrading its medical services. Finally, this paper analyses and concludes the main reasons why the developing country like India attracts foreign tourists for the medical treatment. It is a basket of services to patient-tourists who want their medical treatments done in foreign countries. Medical tourism can be defined as provision of 'cost effective' personal health care/private medical care in association with the tourism industry for patients needing surgical healthcare and other forms of dedicated & specialized treatment.
Sky Institute
India has an additional requirement of 0.8 million doctors and 1.7 million nurses, apart from facing a significant shortage of paramedics. 45% of the population travels more than 100 Kms to access tertiary level of medical care. Poor accessibility, accountability, affordability, and availability of healthcare services are key constraints that make the idea of 'Health for all' a seemingly impossible accomplishment. Besides, the sector is largely dominated by unorganized private players, mostly comprising of clinics and nursing homes. These facilities offer limited range of services and operate with minimal standards of quality. Moreover, the public sector focus is mainly on primary care with a program based approach. Other issues restricting growth of the sector are of high capital expenditure, high dependence on imported medical equipments, long gestation period for the business to turn profitable, archaic norms for medical education, and absence of any central governing authority for paramedical education.
Dr Madhuri Sawant
Ministry of Tourism, Government of India has taken several steps to promote India as a medical tourism destination. This paper presents a critical analysis of the concept of medical tourism, the present status of medical tourism in India and its socio-economic aspects. The paper concludes with ethical concerns in the practice of medical tourism.
SUmanth Reddy
Journal of International Trade Law and Policy
Purpose The present paper aims to analyse who actually benefits from the policies to promote international trade in healthcare services through medical tourism in India. It also assesses the implications of unfettered and unchecked medical tourism for public health policy-making. Design/methodology/approach The research methodology adopted in this paper is inter-disciplinary (socioeconomic and legal) and includes a mix of doctrinal and empirical qualitative research. Findings The present paper argues that in the absence of any baseline data in the public domain on inbound traffic of tourists visiting India on medical tourism, it is difficult to assess and evaluate the private sector claims and that the absence of any format for data collection, management and analysis results in questionable accountability and institutional fragmentation and non-coordination. Furthermore, it results in asymmetrical policy-making in areas like international trade, which may have unintended negative e...
Ahasanul Haque
Publisher ijmra.us UGC Approved , Dr. Shreya Bhargav
Tourism is a kind of economic bonanza which significantly contribute to the growth of a state as well as a country. The rate of success of this industry is dependent upon a range of activities ranging from transportation to accommodation. These activities are: 1) Travel and transport facilities, 2) Accommodation, 3) Food and drink, 4) Entertainment/recreation, 5) Information and assistance and 6) Souvenirs. Medical tourism is a novel form of niche tourism gradually becoming popular in the present world and India has emerged as a popular destination for providing Global standards of health care at affordable costs. It mixes leisure, fun and relaxation together with wellness and healthcare. Within Asia, India, Thailand and Singapore are the three countries that receive maximum medical tourists owing to low cost of treatment, quality healthcare infrastructure, and availability of highly skilled doctors.More recently there has been a spatial shift in medical travel especially to Asian countries from advanced economies. Presently Indian health care sector is considered one of the largest tourism sector in terms of both revenue and workforce employment. Indian medical tourism industry is expected to reach $6 billion by 2018, with number of people arriving in the country for health treatment set to twice over next four year.
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
International Journal of Leisure and Tourism Marketing
Babu George
International Journal in Management and Social Science
Dr Mohammad Amiri
Iranian journal of public health
Md Abdul Momen
Economic and Political Weekly
imrana qadeer
B Suresh Lal, PhD
Muthukrishnaveni R Anand
Case Centre
Alka Maurya
Mohnish Singh
Interal Res journa Managt Sci Tech
Journal of Medical and Scientific Research
s180994 P.Vasavi SKLM
Ansuman Samal
International Journal of Environmental Research and Public Health
Viktoriia Vovk
Philosophy, Ethics, and Humanities in Medicine
Sunita Reddy
IOSR Journals
Kamal Rathore
SUJAY PATHAK
Verina D'Souza, and Prakash Pinto, ATNA Journal of Tourism Studies,18(1),2023, 1-26
Prakash Pinto
Enlightening Tourism: A Pathmaking Journal
Parikshat Singh Manhas
International journal of health sciences
Studies in Indian Place Names
Dr. Anirban Sarkar
Scholar Science Journals
IJRASET Publication
seema zagade
Dr Indu Grewal
Bulletin of Geography: Socio-Economic Series (in press)
Gijsbert Hoogendoorn
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Medical tourism in India: perceptions of physicians in tertiary care hospitals
Affiliation.
- 1 Center of Social Medicine and Community Health, School of Social Sciences, Jawaharlal Nehru University, New Delhi 110067, India. [email protected].
- PMID: 24345280
- PMCID: PMC3901785
- DOI: 10.1186/1747-5341-8-20
Senior physicians of modern medicine in India play a key role in shaping policies and public opinion and institutional management. This paper explores their perceptions of medical tourism (MT) within India which is a complex process involving international demands and policy shifts from service to commercialisation of health care for trade, gross domestic profit, and foreign exchange. Through interviews of 91 physicians in tertiary care hospitals in three cities of India, this paper explores four areas of concern: their understanding of MT, their views of the hospitals they work in, perceptions of the value and place of MT in their hospital and their views on the implications of MT for medical care in the country. An overwhelming majority (90%) of physicians in the private tertiary sector and 74.3 percent in the public tertiary sector see huge scope for MT in the private tertiary sector in India. The private tertiary sector physicians were concerned about their patients alone and felt that health of the poor was the responsibility of the state. The public tertiary sector physicians' however, were sensitive to the problems of the common man and felt responsible. Even though the glamour of hi-tech associated with MT dazzled them, only 35.8 percent wanted MT in their hospitals and a total of 56 percent of them said MT cannot be a public sector priority. 10 percent in the private sector expressed reservations towards MT while the rest demanded state subsidies for MT. The disconnect between their concern for the common man and professionals views on MT was due to the lack of appreciation of the continuum between commercialisation, the denial of resources to public hospitals and shift of subsidies to the private sector. The paper highlights the differences and similarities in the perceptions and context of the two sets of physicians, presents evidence, that questions the support for MT and finally analyzes some key implications of MT on Indian health services, ethical issues emerging out of that and the need for understanding the linkages between public and private sectors for a more effective intervention for an equitable medical care policy.
PubMed Disclaimer
Similar articles
- Do Legal Issues Deserve Space in Specialty Medical Journals ? Nagpal N. Nagpal N. J Assoc Physicians India. 2016 Feb;64(2):86-87. J Assoc Physicians India. 2016. PMID: 27730795
- Medical leadership competencies: A comparative study of physicians in public and private sector hospitals in India. Gulati K, Madhukar V, Verma V, Singh AR, Gupta SK, Sarkar C. Gulati K, et al. Int J Health Plann Manage. 2019 Jan;34(1):e947-e963. doi: 10.1002/hpm.2709. Epub 2018 Nov 27. Int J Health Plann Manage. 2019. PMID: 30480333
- Regulating the private health care sector: the case of the Indian Consumer Protection Act. Bhat R. Bhat R. Health Policy Plan. 1996 Sep;11(3):265-79. doi: 10.1093/heapol/11.3.265. Health Policy Plan. 1996. PMID: 10160372
- Synergies between veterinarians and para-professionals in the public and private sectors: organisational and institutional relationships that facilitate the process of privatising animal health services in developing countries. Woodford JD. Woodford JD. Rev Sci Tech. 2004 Apr;23(1):115-35; discussion 391-401. doi: 10.20506/rst.23.1.1472. Rev Sci Tech. 2004. PMID: 15200091 Review.
- Evidence Brief: The Quality of Care Provided by Advanced Practice Nurses [Internet]. McCleery E, Christensen V, Peterson K, Humphrey L, Helfand M. McCleery E, et al. Washington (DC): Department of Veterans Affairs (US); 2014 Sep. Washington (DC): Department of Veterans Affairs (US); 2014 Sep. PMID: 27606392 Free Books & Documents. Review.
- Medical, Health and Wellness Tourism Research-A Review of the Literature (1970-2020) and Research Agenda. Zhong L, Deng B, Morrison AM, Coca-Stefaniak JA, Yang L. Zhong L, et al. Int J Environ Res Public Health. 2021 Oct 16;18(20):10875. doi: 10.3390/ijerph182010875. Int J Environ Res Public Health. 2021. PMID: 34682622 Free PMC article. Review.
- The social paradoxes of commercial surrogacy in developing countries: India before the new law of 2018. Rozée V, Unisa S, de La Rochebrochard E. Rozée V, et al. BMC Womens Health. 2020 Oct 15;20(1):234. doi: 10.1186/s12905-020-01087-2. BMC Womens Health. 2020. PMID: 33059640 Free PMC article.
- The north-south policy divide in transnational healthcare: a comparative review of policy research on medical tourism in source and destination countries. Virani A, Wellstead AM, Howlett M. Virani A, et al. Global Health. 2020 Apr 22;16(1):37. doi: 10.1186/s12992-020-00566-3. Global Health. 2020. PMID: 32321561 Free PMC article. Review.
- "Medical tourism will…obligate physicians to elevate their level so that they can compete": a qualitative exploration of the anticipated impacts of inbound medical tourism on health human resources in Guatemala. Crooks VA, Labonté R, Ceron A, Johnston R, Snyder J, Snyder M. Crooks VA, et al. Hum Resour Health. 2019 Jul 12;17(1):53. doi: 10.1186/s12960-019-0395-z. Hum Resour Health. 2019. PMID: 31299994 Free PMC article.
- Socialization, legitimation and the transfer of biomedical knowledge to low- and middle-income countries: analyzing the case of emergency medicine in India. Sriram V, George A, Baru R, Bennett S. Sriram V, et al. Int J Equity Health. 2018 Sep 24;17(1):142. doi: 10.1186/s12939-018-0824-y. Int J Equity Health. 2018. PMID: 30244680 Free PMC article.
- CII-McKinsey. Health Care in India: The Road Ahead. CII. New Delhi: McKinsey and Company and Indian Healthcare Federation; 2002.
- Planning Commission. Tenth Five Year Plan, 2002-2007. Volume 2. New Delhi: Chapter on Health, Government of India; 2002.
- Planning Commission. Eleventh Five Year Plan, 2007-2012. Volume 2. New Delhi: Chapter on Health, Government of India; 2008.
- Government of India. Ministry of health and family welfare, draft national health bill. 2009.
- Planning Commission. Twelfth Five Year Plan, 2012-2017. Volume 3. New Delhi: Chapter on Health, Government of India; 2013.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- BioMed Central
- Europe PubMed Central
- PubMed Central
Other Literature Sources
- scite Smart Citations

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Market News
- My Portfolio
- My Watchlist
- International Markets
- Mutual Fund
Bangladesh Crisis Impacts India's Medical Tourism: Report
By Rediff Money Desk , Mumbai Aug 14, 2024 19:38

You May Like To Read

Bangladesh Businesses Hit by Cash Crunch Amidst Political... Aug 12, 2024 11:55

Air India Express Launches Direct Flights to Dhaka from... Jul 31, 2024 16:00
India Hospitality Sector to Boom: Thomas Cook Aug 01, 2024 15:20

New Portal for Chinese Technicians in India's PLI Sector Aug 07, 2024 14:21

Budget 2024: Hospitality Sector Disappointed by Lack of... Jul 23, 2024 17:29

Lupin Gets USFDA Approval for Generic Seizure Medication Jul 12, 2024 17:31

Gadkari Urges GST Withdrawal on Life & Medical Insurance... Jul 31, 2024 13:33

QMS Medical Acquires 51% Stake in Saarathi Healthcare Jul 05, 2024 15:44

American Airlines Flight Diverted to London Due to... Jul 15, 2024 18:13
TODAY'S MOST TRADED COMPANIES
- Company Name
- GTL Infrastructure
- 2.74 (+ 2.62)
- Srestha Finvest
- 2.24 (+ 4.67)
- Ola Electric Mobilit
- 132.76 (+ 19.99)
- Suzlon Energy Ltd.
- 79.93 (+ 4.10)
- IFL Enterprises
- 1.22 (+ 4.27)
More »

Foxconn, the Taiwanese electronics giant, plans to establish a battery energy storage...
Taiwanese electronics giant Foxconn is planning to establish a Battery Energy Storage...

FSSAI launches project to assess microplastic contamination in food products and...
Moneywiz Live!
Stocks | Mutual Funds | Investment tracking | |||
| Gainers - | | Losers - | | | | | | | | ||
- India Today
- Business Today
- Harper's Bazaar
- Brides Today
- Cosmopolitan
- India Today Hindi
- Reader’s Digest
- Aaj Tak Campus
Download App

Kolkata trainee doctor's legs were 90 degrees apart, no clothes: Family's ordeal
The family of the kolkata trainee doctor, who was raped and murdered, said they were told that their daughter had died by suicide and were made to wait outside the hospital for three hours..
Listen to Story

- Family initially told victim died by suicide, made to wait 3 hours to see body
- Father says he knew something had happened to his daughter when hospital called
- Calcutta High Court transfers probe to CBI
The family members of the 31-year-old trainee doctor, who was raped and murdered at Kolkata's RG Kar Medical College and Hospital , revealed their harrowing ordeal after they were informed about the incident. The family said they were told that their daughter had died by suicide and were made to wait outside the hospital for three hours before they could see her body.
Lallantop, India Today TV's sister channel, spoke to the parents and relatives of the victim. The father of the trainee doctor said when he got a call from the hospital, he knew something had happened to his daughter.
"She (pointing at his wife) started crying. They (hospital authorities) said our daughter has died by suicide and we must come immediately," he said.
"We ask everyone (who is coming to meet us)... give us justice. Our daughter cannot be returned to us, but we can at least seek justice for her," he added.
Sources told India Today TV that the Assistant Superintendent of RG Kar Hospital's Chest Medicine Wing was the first to inform the victim's family about the incident. The Assistant Superintendent told them that she died by suicide inside the hospital premises , sources said.
One of the relatives, who lives in the neighbourhood and went with the parents to the hospital, said the victim's mother was inconsolable after learning about her daughter.
"I heard her (mother) cry aloud. When I went there, she hugged me and cried that everything is over. She told me her daughter has died by suicide as told by the hospital," the relative said.
The relative said when they reached the hospital, they were made to wait outside for three hours.
"The parents pleaded before them (hospital authorities) to show them their daughter's face. But still they were made to wait for three hours," the relative said.
The relative recounted the horrific condition in which the trainee doctor's body was found.
"After three hours, they allowed the father to go inside and see her body. He was only allowed to click a picture, which he showed us when he came outside. She had no clothes on her body. Her legs were 90 degrees apart... this cannot happen unless the pelvic girdle breaks, which means she was torn apart," the relative said.
WHAT DID THE AUTOPSY REVEAL?
The four-page postmortem report of the trainee doctor revealed that she was throttled to death. Her thyroid cartilage was broken due to strangling and injuries were found on her belly, lips, fingers, and left leg.
The report also mentioned that the woman was bleeding from both eyes, mouth and private parts. The report said the wounds in her private parts were caused by "perverted sexuality" and "genital torture".
However, the reason for her eye wound has not been determined yet.
IN THIS STORY

COMMENTS
The paper discusses the research process and the methodology adopted for the study in detail. Finally, the report analyses India's, and specifically Delhi-NCR's, competence as a medical tourist destination and synthesises the key growth drivers and opportunities for this industry. ... Qadeer I, Reddy S. Medical tourism in india: Perceptions ...
The findings of the reviewed literature are listed in the introduction section of this paper. The first step included using the finding of the literature review and input from the focus group to propose a framework for the development of medical tourism in a region. ... Bakucz M. Past themes and future trends in medical tourism research: A co ...
Medical tourism is quickly growing in developing countries. The healthcare players have recognized it as a potential area for economic diversification. The major factors affecting medical tourism in a country are cost, quality, language, and ease of travel. The healthcare services in India cost significantly lower than in western countries and the middle east. That is one of the reasons behind ...
Abstract. Medical tourism has been a rising service industry across the world for the last two decades. This paper outlines the theoretical perspective that governs the study of medical tourism, analyses the development of the sector in India and puts forth suggestions on how to promote further growth of medical tourism in the country.
The paper identifies the strengths of India's medical tourism service providers and points at a number of problems that may reduce the growth opportunity of this industry.
Medical Tourism in India: Progress or Predicament? SUNITA REDDY, IMRANA QADEER It is estimated that the size of the medical tourism market in the country will be Rs 1,95,000 crore in 2012. Based on a literature review of healthcare business media, policy documents and a few academic papers, this essay looks at the scope for medical tourism in India
Abstract. Medical Tourism is the fastest growing sector of healthcare throughout the world. We can say during the last decade medical tourism is continuously gaining popularity, patients are more educated than ever and are going online to research information and are travelling to where they can get the best quality care at an affordable price.
Senior physicians of modern medicine in India play a key role in shaping policies and public opinion and institutional management. This paper explores their perceptions of medical tourism (MT) within India which is a complex process involving international demands and policy shifts from service to commercialisation of health care for trade, gross domestic profit, and foreign exchange.
Another regarding medical tourism in India, found that it is common for medical tourists to incorporate travel plans during their medical procedure trip [44]. And, a study on expectation ...
IJNRD2306562 International Journal of Novel Research and Development (www.ijnrd.org) f631 Wellness and Rejuvenation. Alternate Therapies aimed at wellness, rejuvenation and better lifestyle. ... Medical Tourism in India was estimated to be worth USD 5-6 Billion in 2019. The segment is expected to grow to USD 13 Billion by 2022-23.
The medical tourism in Indi a will touch the $8 billion. mark by the end of 2020, the infl ux of the population that. experiences a saving of close to 50 to 70 percent on medical. tourism industr ...
The study presents the assessment of the medical tourism industry in India and the scope of opportunity for Indian players. ... The paper discusses the research process and the methodology adopted for the study in detail. Finally, the report analyses India's, and specifically Delhi-NCR's, competence as a medical tourist destination and ...
Design/methodology/approach The research methodology adopted in this paper is inter-disciplinary (socioeconomic and legal) and includes a mix of doctrinal and empirical qualitative research. ... Medical tourism in India accounted to be U.S. $ 3 billion market by 2015 and was estimated to touch U.S. $ 7-8 billion by 2020 (FICCI Heal, 2008 ...
International Science Congress Association. This paper presents an exploratory study involving qualitative research. The scope of the study is restricted to international medical tourism alone. Content analysis technique has been employed to identify research issues pertaining to medical tourism in India.
The Indian medical tourism will reach USD 10 to 15 billion, with four times the growth in the IT market. This research paper aims to understand the reasons for the growth of medical tourism in India, the government, and corporate hospitals in promoting Medical tourism. Research throws light on
medical tourism in India with the help of data analysis. Key Words: Ayurvedic Treatment, Globalization, Health care services, Medical Tourism I. INTRODUCTION In today's era Medical Tourism is expanding worldwide, sometimes medical tourism can be said as health tourism and wellness tourism, in this customer from different parts of the
ISSN (Online) : 2348- 5329. Factors Influencing Medical Tou rism in India: A. Critical Review. Sumit Oberoi. and Pooja Kansra. 1 Research Scholar, Mittal School of Business, Lovely Professional ...
Senior physicians of modern medicine in India play a key role in shaping policies and public opinion and institutional management. This paper explores their perceptions of medical tourism (MT) within India which is a complex process involving international demands and policy shifts from service to commercialisation of health care for trade, gross domestic profit, and foreign exchange.
IJCRT2306013 International Journal of aCreative Research Thoughts (IJCRT) www.ijcrt.org 106 development drivers in the service sector. India is not only known for its tourism attractions, but also for its ... The India medical tourism market was valued at USD 2.89 billion in 2020 and is expected to reach USD 13.42 billion by 2026 3.2.2.3 Middle ...
An Overview of Medical and Wellness Tourism in India International Business Research Conference, 2018 69 |Page several Asian destinations like Singapore, Malaysia and Thailand that are offering medical care facilities and promoting medical tourism. India excels among them for the following reasons:- State of the Art medical facilities
in 2009 rose to 8.5 lakhs in 2011 and is likely to touch 32 lakhs by 2015) 315. Medical tourists in India basically come from Middle East, Iran, Pakistan, Bangladesh, Afghanistan, Turkey, Europe ...
India ranks among the top 10 countries for medical tourism globally and is especially preferred amongst South-Asian, African and Middle East countries. Bangladesh stands out as the leading contributor to medical tourism among neighbouring countries, surpassing the Middle East, Myanmar, Maldives, Sri Lanka, and Pakistan.
In India, medical tourism is becoming more popular. Medical tourism industry of India is expected to be worth $5-6 billion by mid2020. ... The analysis is based on secondary data such as Ph. D ...
Junior doctors protest against the rape and killing of a trainee doctor at RG Kar Medical College and Hospital in Kolkata. (Photo: PTI) India Today News Desk. New Delhi, UPDATED: Aug 14, 2024 13:15 IST. ... Lallantop, India Today TV's sister channel, spoke to the parents and relatives of the victim. The father of the trainee doctor said when he ...
medical tourism in India, was opined by 82% foreign tourist patients. In the opinion of 72% patients, due. to government initiation in aggressive promotion o f medical tourism, there is a growth ...