Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines

Coronary Artery Disease: Prevention, Treatment and Research
Coronary artery disease (also called coronary heart disease ) is the number-one killer of both men and women in the United States, and it’s the most common type of heart disease. This often preventable disease causes the dangerous thickening and narrowing of the coronary arteries—the vessels that bring blood to the heart—which disrupts the flow of oxygen and nutrients to the heart, causing serious problems.
Without enough blood, coronary artery disease can lead to angina (chest pain). Over time, the heart has to work harder, possibly causing heart failure (when the heart cannot pump efficiently) or arrhythmia (when the heart beats irregularly or too quickly). The damaged arteries may become completely blocked, or become prone to clotting, causing a heart attack.
“Coronary artery disease develops slowly, usually over decades, so the good news is that we have a huge window of opportunity for prevention, through a good lifestyle and healthy habits,” says Seth Martin, M.D., M.H.S. , of the Johns Hopkins Ciccarone Center for the Prevention of Heart Disease.
Preventing coronary artery disease is largely about controlling the risk factors. “Ideally, prevention habits start early, but they remain important all through life,” Bill McEvoy, MBBCh, of the Johns Hopkins Ciccarone Center for the Prevention of Heart Disease says. It’s never too late to effect change, though the earlier in life you do so, the greater the advantage. Smart steps to take:
- Quit smoking—or better yet, never start. Smoking is considered one of the key risk factors for heart attack. Also steer clear of secondhand smoke. If a household member is a smoker, help him or her find ways to quit, such as calling your state’s free 800-QUIT-NOW line, suggests Martin.
- Eat less of the foods that add to heart problems, and more of the foods that protect the heart . Aim for an eating plan that’s low in saturated fats and trans fats, higher in monounsaturated and polyunsaturated the fats found in olive oil and fish, high in fiber (found in plant foods), and low in salt and sugar. Get practical ideas to eat for heart health in Eat Smart .
- Become more active, and stay active, all through life. A good goal is at least 150 minutes (2.5 hours) of moderate exercise each week, or 75 minutes (1.25 hours) of vigorous aerobic exercise each week. Or aim to be active for 30 minutes a day, most days of the week. Check with your doctor before you launch a new workout program if you’ve never worked out before. Learn how implementing an exercise routine helps your heart in Move More .
- Keep your weight within the normal range on a Body Mass Index (BMI) chart. If you’re overweight, losing just 5 percent to 10 percent of your current weight will lower your risk of developing coronary artery disease.
- Find healthy outlets for your stress. Some stress is unavoidable in life. But it tends to push us toward not-so-great habits (overeating, drinking, sitting too much). You’ll be more heart-healthy if you can offload stress in ways you enjoy and that are good for you, such as exercise, meditation and relaxing with friends, says McEvoy. A stress-management program can help.
Diagnosis & Treatment
Because coronary artery disease develops over time, the symptoms depend on the stage of illness. Damage may be present without outward signs. It’s common to first notice shortness of breath or chest pains when you exert yourself physically. Some people have mild episodes of these symptoms. For others, the first experience is more severe chest pain, even heart attack.
To diagnose coronary artery disease, your doctor will look at markers such as blood pressure, cholesterol profile and blood glucose (from a blood test) as well as your health history and family history, says McEvoy. This information can help estimate your 10-year cardiovascular risk—your odds of a heart attack or stroke.
Depending on the symptoms you have, tests that may be given to provide additional information include:
- Coronary calcium testing: A simple CT scan provides images of the heart between beats, showing calcium and plaque buildup. “You can actually see the damage that’s known as hardening of the arteries,” says Martin. This test may be considered in persons without known coronary heart disease in whom the decision to treat with a statin and aspirin is unclear.
- High Sensitivity C-reactive protein blood test: This indicates whether you have higher than average levels of inflammation.
- Electrocardiogram (EKG or ECG): Measurement of the electrical activity of your heartbeat during rest.
- Exercise stress test (“treadmill test”): A test done on a treadmill to measure your heart rate when the heart has to pump harder.
- Echocardiogram : An ultrasound image of your heart.
- Chest X-ray : An image of your heart, lungs and other chest organs.
- Cardiac catheterization : A test in which a thin tube is inserted into an artery to check for blockages in heart arteries.
- Coronary angioplasty : a procedure in which a expandable balloon is used to open up a narrowed artery. Nearly 90% of the time, a stent (metal scaffold) is placed at the site of the narrowing in the artery.
“Treatments work better early on,” says Martin, which is why early identification and intervention are so important. Depending on your health status and goals, there are three key approaches to treating heart disease:
Lifestyle changes. The same steps for preventing coronary artery disease are part of a treatment approach to forestalling further problems—that is, modify the many factors that are in your control, like diet, exercise, de-stressing and not smoking.
Medication. You may be prescribed medications to manage the risk factors for coronary artery disease, such as high blood pressure, high cholesterol, prediabetes and diabetes.
Procedures to help open blood vessels. Several different types of surgeries (usually outpatient) may be done to repair damage to arteries. These include:
- Coronary angioplasty. A “balloon” is inserted into the artery through a catheter (a long, narrow, flexible tube) and then inflated to enlarge the passage through the artery. Typically a stent—a wire mesh tube—is also inserted, which forms a scaffolding around the balloon to keep the artery open.
- Atherectomy. A rotating shaver is used to remove plaque from the artery.
- Coronary artery bypass surgery (or coronary artery bypass graft). In this more serious surgery, an artery or vein from another part of the body, such as the leg, is grafted onto the coronary artery to create a new route around a blocked section. More than one graft may be done at a time.
Living With...
Living in the shadow of a potential heart attack or other heart problems can be unnerving—but it can also be motivating. Here’s what to focus on after a diagnosis.
- Know your numbers. Heart health is in large part a numbers game. The key numbers to know include your HDL and LDL cholesterol, total cholesterol and triglycerides, your blood pressure, your glucose, your BMI and your waist circumference measurement, says McEvoy. Get your measurements and readings as often as recommended, make the recommended lifestyle changes and be sure to take medications as directed. This knowledge can be a powerful incentive.
- Be optimistic. Fear of future cardiac events is common and natural. You may feel anxious, or even depressed. But with good medical care and personal effort, you can still lead a long life of high quality. Small changes really do add up.
Johns Hopkins experts are on the leading edge of research to prevent and treat heart disease. Examples of recent findings include:
Higher levels of physical fitness lower the risk of heart attack. It also cut the risk of death during the time of the study by 75 percent in those who have been diagnosed with coronary artery disease. A Johns Hopkins study found this true whether or not the subjects had a procedure to open blocked arteries (like stenting or bypass surgery).
The traditional formula for assessing LDL cholesterol sometimes underestimates risk. (LDL signals the buildup of plaque in arteries.) Johns Hopkins researchers discovered this risk discrepancy and have devised a more accurate calculation that uses the same basic blood test
Find a Doctor
Specializing In:
- Dyslipidemia and Hypertension
- Dyslipidemia
- Treatment of Bypass Graft Disease with Distal Protection Devices
- Chronic Total Occlusions
- Chronic Total Coronary Occlusion
- Coronary Heart Disease
- Coronary Endothelial Function
- Coronary Artery Disease
- Coronary Artery Bypass Graft Surgery (CABG)
- Coronary Angiography
- Cardiac Disease
- Cardiothoracic Surgery
- Carotid Artery Stenosis
- Cardiovascular Disease
- Intravascular Brachytherapy
- Intravascular Ultrasound (IVUS)
- Ischemic Heart Disease
- Fractional Flow Reserve
- Acute Coronary Care
- Acute Coronary Syndrome (ACS)
- Acute Myocardial Infarction (AMI)
- Laser Atherectomy
- Laser Ablation
Find a Treatment Center
Find Additional Treatment Centers at:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital

Request an Appointment

Fight Inflammation to Help Prevent Heart Disease

The Number One Way to Reduce Heart Risk

Special Heart Risks for Men
Related Topics
- Heart and Vascular
- Patient Care & Health Information
- Diseases & Conditions
- Coronary artery disease
Coronary artery disease (CAD) is a common type of heart disease. It affects the main blood vessels that supply blood to the heart, called the coronary arteries. In CAD, there is reduced blood flow to the heart muscle. A buildup of fats, cholesterol and other substances in and on the artery walls, a condition called atherosclerosis, usually causes coronary artery disease. The buildup, called plaque, makes the arteries narrow.
Coronary artery disease often develops over many years. Symptoms are from the lack of blood flow to the heart. They may include chest pain and shortness of breath. A complete blockage of blood flow can cause a heart attack.
Treatment for coronary artery disease may include medicines and surgery. Eating a nutritious diet, getting regular exercise and not smoking can help prevent coronary artery disease and the conditions that can cause it.
Coronary artery disease also may be called coronary heart disease.
- What is coronary artery disease? A Mayo Clinic cardiologist explains.
Stephen Kopecky, M.D., talks about the risk factors, symptoms and treatment of coronary artery disease (CAD). Learn how lifestyle changes can lower your risk.
{Music playing}
Stephen Kopecky, M.D., Cardiovascular Disease, Mayo Clinic: I'm Dr. Stephen Kopecky, a cardiologist at Mayo Clinic. In this video, we'll cover the basics of coronary artery disease. What is it? Who gets it? The symptoms, diagnosis and treatment. Whether you're looking for answers for yourself or someone you love, we're here to give you the best information available.
Coronary artery disease, also called CAD, is a condition that affects your heart. It is the most common heart disease in the United States. CAD happens when coronary arteries struggle to supply the heart with enough blood, oxygen and nutrients. Cholesterol deposits, or plaques, are almost always to blame. These buildups narrow your arteries, decreasing blood flow to your heart. This can cause chest pain, shortness of breath or even a heart attack. CAD typically takes a long time to develop. So often, patients don't know that they have it until there's a problem. But there are ways to prevent coronary artery disease, and ways to know if you're at risk and ways to treat it.
Who gets it?
Anyone can develop CAD . It begins when fats, cholesterols and other substances gather along the walls of your arteries. This process is called atherosclerosis. It's typically no cause for concern. However, too much buildup can lead to a blockage, obstructing blood flow. There are a number of risk factors, common red flags, that can contribute to this and ultimately lead to coronary artery disease. First, getting older can mean more damaged and narrowed arteries. Second, men are generally at a greater risk. But the risk for women increases after menopause. Existing health conditions matter, too. High blood pressure can thicken your arteries, narrowing your blood flow. High cholesterol levels can increase the rate of plaque buildup. Diabetes is also associated with higher risk, as is being overweight. Your lifestyle plays a large role as well. Physical inactivity, long periods of unrelieved stress in your life, an unhealthy diet and smoking can all increase your risk. And finally, family history. If a close relative was diagnosed at an early age with heart disease, you're at a greater risk. All these factors together can paint a picture of your risk for developing CAD .
What are the symptoms?
When coronary arteries become narrow, the heart doesn't get enough oxygen-rich blood. Remember, unlike most pumps, the heart has to pump its own energy supply. It's working harder with less. And you may begin to notice these signs and symptoms of pressure or tightness in your chest. This pain is called angina. It may feel like somebody is standing on your chest. When your heart can't pump enough blood to meet your body's needs, you might develop shortness of breath or extreme fatigue during activities. And if an artery becomes totally blocked, it leads to a heart attack. Classic signs and symptoms of a heart attack include crushing, substernal chest pain, pain in your shoulders or arms, shortness of breath, and sweating. However, many heart attacks have minimal or no symptoms and are found later during routine testing.
How is it diagnosed?
Diagnosing CAD starts by talking to your doctor. They'll be able to look at your medical history, do a physical exam and order routine blood work. Depending on that, they may suggest one or more of the following tests: an electrocardiogram or ECG, an echocardiogram or soundwave test of the heart, stress test, cardiac catheterization and angiogram, or a cardiac CT scan.
How is it treated?
Treating coronary artery disease usually means making changes to your lifestyle. This might be eating healthier foods, exercising regularly, losing excess weight, reducing stress or quitting smoking. The good news is these changes can do a lot to improve your outlook. Living a healthier life translates to having healthier arteries. When necessary, treatment could involve drugs like aspirin, cholesterol-modifying medications, beta-blockers, or certain medical procedures like angioplasty or coronary artery bypass surgery.
Discovering you have coronary artery disease can be overwhelming. But be encouraged. There are things you can do to manage and live with this condition. Reducing cholesterol, lowering blood pressure, quitting tobacco, eating healthier, exercising and managing your stress can make a world of difference. Better heart health starts by educating yourself. So don't be afraid to seek out information and ask your doctors about coronary artery disease. If you'd like to learn even more about this condition, watch our other related videos or visit Mayoclinic.org. We wish you well.
Symptoms of coronary artery disease happen when the heart doesn't get enough oxygen-rich blood. Coronary artery disease symptoms may include:
- Chest pain, called angina. You may feel squeezing, pressure, heaviness, tightness or pain in the chest. It may feel like somebody is standing on your chest. The chest pain usually affects the middle or left side of the chest. Activity or strong emotions can trigger angina. There are different types of angina. The type depends on the cause and whether rest or medicine makes symptoms better. In some people, especially women, the pain may be brief or sharp and felt in the neck, arm or back.
- Shortness of breath. You may feel like you can't catch your breath.
- Fatigue . If the heart can't pump enough blood to meet your body's needs, you may feel unusually tired.
Symptoms of coronary artery disease may not be noticed at first. Sometimes symptoms only happen when the heart is beating hard, such as during exercise. As the coronary arteries continue to narrow, symptoms can get more severe or frequent.
A completely blocked coronary artery will cause a heart attack. Common heart attack symptoms include:
- Chest pain that may feel like pressure, tightness, squeezing or aching.
- Pain or discomfort that spreads to the shoulder, arm, back, neck, jaw, teeth or sometimes the upper belly.
- Cold sweats.
- Shortness of breath.
- Lightheadedness or sudden dizziness.
Chest pain is usually the most common symptom of heart attack. But for some people, such as women, the elderly and those with diabetes, symptoms may seem unrelated to a heart attack. For example, they may have nausea or a very brief pain in the neck or back. Some people having a heart attack don't notice symptoms.
When to see a doctor
If you think you're having a heart attack, immediately call 911 or your local emergency number. If you don't have access to emergency medical services, have someone drive you to the nearest hospital. Drive yourself only as a last option.
Smoking or having high blood pressure, high cholesterol, diabetes, obesity or a strong family history of heart disease makes you more likely to get coronary artery disease. If you're at high risk of coronary artery disease, talk to your healthcare professional. You may need tests to check for narrowed arteries and coronary artery disease.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
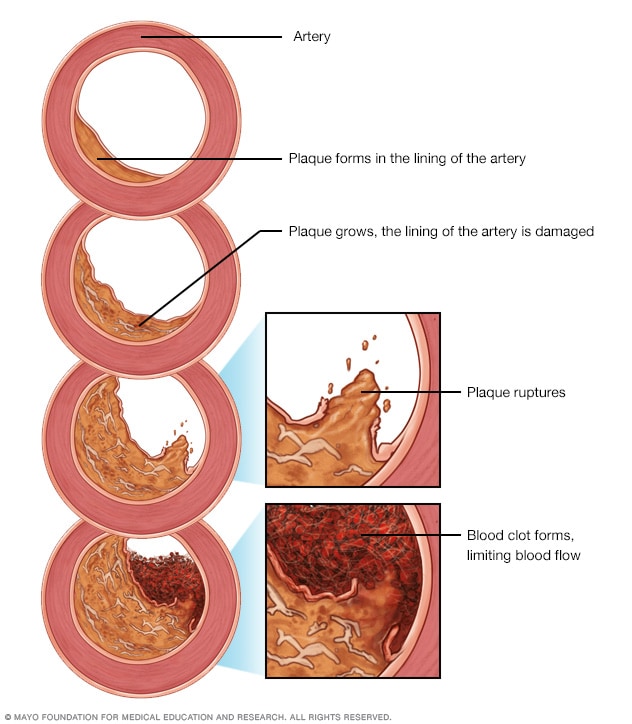
Development of atherosclerosis
If there's too much cholesterol in the blood, the cholesterol and other substances may form deposits called plaque. Plaque can cause an artery to become narrowed or blocked. If a plaque ruptures, a blood clot can form. Plaque and blood clots can reduce blood flow through an artery.
Coronary artery disease is caused by the buildup of fats, cholesterol and other substances in and on the walls of the heart arteries. This condition is called atherosclerosis. The buildup is called plaque. Plaque can cause the arteries to narrow, blocking blood flow. The plaque also can burst, causing a blood clot.
Some causes of atherosclerosis and coronary artery disease are:
- Diabetes or insulin resistance.
- High blood pressure.
- Lack of exercise.
- Smoking or tobacco use.
Risk factors
Coronary artery disease is common.
Coronary artery disease risk factors you can't control include:
- Age. Getting older increases the risk of damaged and narrowed arteries.
- Birth sex. Men are generally at greater risk of coronary artery disease. However, the risk for women increases after menopause.
- Family history. A family history of heart disease makes you more likely to get coronary artery disease. This is especially true if a parent, brother, sister or child got heart disease at an early age. The risk is highest if your father or a brother had heart disease before age 55 or if your mother or a sister developed it before age 65.
Coronary artery disease risk factors you can control are:
- Smoking. If you smoke, quit. Smoking is bad for heart health. People who smoke have a much greater risk of heart disease. Breathing in secondhand smoke also increases the risk.
- High blood pressure. Uncontrolled high blood pressure can make arteries hard and stiff. This can lead to atherosclerosis, which causes coronary artery disease.
- Cholesterol. Too much "bad" cholesterol in the blood can increase the risk of atherosclerosis. "Bad" cholesterol is called low-density lipoprotein (LDL) cholesterol. Not enough "good" cholesterol, called high-density lipoprotein (HDL) cholesterol, also leads to atherosclerosis.
- Diabetes. Diabetes increases the risk of coronary artery disease. Type 2 diabetes and coronary artery disease share some risk factors, such as obesity and high blood pressure.
- Obesity. Too much body fat is bad for overall health. Obesity can lead to type 2 diabetes and high blood pressure. Ask your healthcare team what a healthy weight is for you.
- Chronic kidney disease. Having long-term kidney disease increases the risk of coronary artery disease.
- Not getting enough exercise. Physical activity is important for good health. A lack of exercise is linked to coronary artery disease and some of its risk factors.
- A lot of stress . Emotional stress may damage the arteries and worsen other risk factors for coronary artery disease.
- Unhealthy diet. Eating foods with a lot of saturated fat, trans fat, salt and sugar can increase the risk of coronary artery disease.
- Alcohol use. Heavy alcohol use can lead to heart muscle damage. It also can worsen other risk factors of coronary artery disease.
- Amount of sleep. Too little sleep and too much sleep both have been linked to an increased risk of heart disease.
Risk factors often happen together. One risk factor may trigger another. When grouped together, some risk factors make you even more likely to develop coronary artery disease. For example, metabolic syndrome is a group of conditions that includes high blood pressure, high blood sugar, too much body fat around the waist and high triglyceride levels. Metabolic syndrome increases the risk of coronary artery disease.
Other possible risk factors for coronary artery disease may include:
- Breathing pauses during sleep, called obstructive sleep apnea. This condition causes breathing to stop and start during sleep. It can cause sudden drops in blood oxygen levels. The heart must work harder to pump blood. Blood pressure goes up.
- Increased high-sensitivity C-reactive protein (hs-CRP). This protein appears in higher than usual amounts when there's inflammation somewhere in the body. High hs-CRP levels may be a risk factor for heart disease. It's thought that as coronary arteries narrow, the level of hs-CRP in the blood goes up.
- High triglycerides. This is a type of fat in the blood. High levels may raise the risk of coronary artery disease, especially for women.
- High levels of homocysteine. Homocysteine is a substance that the body uses to make protein and to build and maintain tissue. But high levels of homocysteine may raise the risk of coronary artery disease.
- Preeclampsia. This pregnancy complication causes high blood pressure and increased protein in the urine. It can lead to a higher risk of heart disease later in life.
- Other pregnancy complications. Diabetes or high blood pressure during pregnancy are known risk factors for coronary artery disease.
- Certain autoimmune diseases. People who have conditions such as rheumatoid arthritis and lupus have an increased risk of atherosclerosis.
Complications
Complications of coronary artery disease may include:
- Chest pain, also called angina. This is a symptom of coronary artery disease. But it also can be a complication of worsening CAD. The chest pain happens when arteries narrow and the heart doesn't get enough blood.
- Heart attack. A heart attack can happen if atherosclerosis causes a blood clot. A clot can block blood flow. The lack of blood can damage the heart muscle. The amount of damage depends in part on how quickly you are treated.
- Heart failure. Narrowed arteries in the heart or high blood pressure can slowly make the heart weak or stiff. This can make it harder for the heart to pump blood.
- Irregular heart rhythms, called arrhythmias. If the heart doesn't get enough blood, changes in heart signaling can happen. This can cause irregular heartbeats.
Coronary artery disease care at Mayo Clinic
- Ferri FF. Coronary artery disease. In: Ferri's Clinical Advisor 2022. Elsevier; 2022. https://www.clinicalkey.com. Accessed March 8, 2022.
- Coronary heart disease. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health-topics/coronary-heart-disease. March 8, 2022.
- Usatine RP, et al., eds. Coronary artery disease. In: Color Atlas and Synopsis of Heart Failure. McGraw Hill; 2019.
- Wilson PWF. Overview of the possible risk factors for cardiovascular disease. https://www.uptodate.com/contents/search. Accessed March 8, 2022.
- Masjedi MS, et al. Effects of flaxseed on blood lipids in healthy and dyslipidemic subjects: A systematic review and meta-analysis of randomized controlled trials. Current Problems in Cardiology. 2021; doi:10.1016/j.cpcardiol.2021.100931.
- Riaz H, et al. Association between obesity and cardiovascular outcomes: A systematic review and meta-analysis of mendelian randomization studies. JAMA Network Open. 2018; doi:10.1001/jamanetworkopen.2018.3788.
- Physical Activity Guidelines for Americans. 2nd ed. U.S. Department of Health and Human Services. https://health.gov/our-work/physical-activity/current-guidelines. Accessed March 8, 2022.
- Your guide to lowering your cholesterol with therapeutic lifestyle changes (TLC). National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health-topics/all-publications-and-resources/your-guide-lowering-cholesterol-therapeutic-lifestyle. Accessed March 24, 2022.
- Rethinking drinking. National Institute on Alcohol Abuse and Alcoholism. https://www.rethinkingdrinking.niaaa.nih.gov/. Accessed March 24, 2022.
- 2015-2020 Dietary Guidelines for Americans. U.S. Department of Health and Human Services and U.S. Department of Agriculture. https://health.gov/our-work/food-nutrition/2015-2020-dietary-guidelines/guidelines. Accessed March 24, 2022.
- Omega-3 supplements: In depth. National Center for Complementary and Integrative Health. https://www.nccih.nih.gov/health/omega3-supplements-in-depth. Accessed March 8, 2022.
- Lopez-Jimenez F (expert opinion). Mayo Clinic. May 9, 2024.
- Siscovick DS, et al. Omega-3 polyunsaturated fatty acid (fish oil) supplementation and the prevention of clinical cardiovascular disease: A science advisory from the American Heart Association. Circulation. 2017; doi:10.1161/CIR.0000000000000482.
- Barley. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed March 24, 2022.
- Black psyllium. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed March 24, 2022.
- Nimmagadda R. Allscripts EPSi. Mayo Clinic. April 10, 2024.
- Liao KP. Coronary artery disease in rheumatoid arthritis: Pathogenesis, risk factors, clinical manifestations, and diagnostic implications. https://www.uptodate.com/contents/search. Accessed March 8, 2022.
- What is coronary heart disease? National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health-topics/coronary-heart-disease Accessed March 8, 2022.
- Kannam JP, et al. Chronic coronary syndrome: Overview of care. https://www.uptodate.com/contents/search. Accessed March 8, 2022.
- Arnett DK, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019; doi:10.1161/CIR.0000000000000678.
- Aspirin use to prevent cardiovascular disease: Preventive medication. U.S. Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/uspstf/draft-recommendation/aspirin-use-to-prevent-cardiovascular-disease-preventive-medication. Accessed March 23, 2021.
- Zheng SL, et al. Association of aspirin use for primary prevention with cardiovascular events and bleeding events: A systematic review and meta-analysis. JAMA. 2019; doi:10.1001/jama.2018.20578.
- Cutlip D, et al. Revascularization in patients with stable coronary artery disease: Coronary artery bypass graft surgery versus percutaneous coronary intervention. https://www.uptodate.com/contents/search. Accessed March 24, 2022.
- Hypertension in Adults: Screening. U.S. Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/hypertension-in-adults-screening. Accessed March 24, 2022.
- How and when to have your cholesterol checked. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/cholesterol/checked.htm. Accessed March 24, 2022.
- Blond psyllium. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed March 24, 2022.
- Oats. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed March 24, 2022.
- Garlic. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed March 24, 2022.
- Plant sterols. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed March 24, 2022.
- Ashraf H, et al. Use of flecainide in stable coronary artery disease: An analysis of its safety in both nonobstructive and obstructive coronary artery disease. American Journal of Cardiovascular Drugs. 2021; doi:10.1007/s40256-021-00483-9.
- Ono M, et al. 10-year follow-up after revascularization in elderly patients with complex coronary artery disease. Journal of the American College of Cardiology. 2021; doi:10.1016/j.jacc.2021.04.016.
- Coyle M, et al. A critical review of chronic kidney disease as a risk factor for coronary artery disease. International Journal of Cardiology: Heart & Vasculature. 2021; doi:10.1016/j.ijcha.2021.100822.
- Mankad R (expert opinion). Mayo Clinic. May 9, 2024.
- Scientific Report of the 2020 Dietary Guidelines Advisory Committee. Alcoholic beverages. U.S. Department of Health and Human Services and U.S. Department of Agriculture. https://www.dietaryguidelines.gov/2020-advisory-committee-report. Accessed Feb. 1, 2024.
- Heart disease in women. American Heart Association. https://www.heart.org/en/health-topics/heart-attack/warning-signs-of-a-heart-attack/heart-attack-symptoms-in-women. May 8, 2024.
- Angina treatment: Stents, drugs, lifestyle changes — What's best?
- Coronary artery disease FAQs
- Coronary artery disease: Angioplasty or bypass surgery?
- Coronary artery stent
- Drug-eluting stents
- Four Steps to Heart Health
Associated Procedures
- Cardiac catheterization
- Coronary angiogram
- Coronary angioplasty and stents
- Coronary artery bypass surgery
- Coronary calcium scan
- Echocardiogram
- Electrocardiogram (ECG or EKG)
- Stress test
News from Mayo Clinic
- Mayo Clinic Minute: Signs of coronary artery disease, how to reduce your risk Jan. 24, 2023, 04:15 p.m. CDT
- A History of Cancer, Coronary Artery Disease May Reduce Risk of Dementia Oct. 24, 2022, 02:45 p.m. CDT
Mayo Clinic in Rochester, Minnesota, has been recognized as one of the top Cardiology & Heart Surgery hospitals in the nation for 2024-2025 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Help transform healthcare
Your donation can make a difference in the future of healthcare. Give now to support Mayo Clinic's research.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases & Disorders Education Program
- Publications and Resources
- Clinical Trials
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Ask a Scientist
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- < Back To Home
- Coronary Heart Disease
- What Is Coronary Heart Disease?
- Causes and Risk Factors
- Living With
- Women and Heart Disease
MORE INFORMATION
Coronary Heart Disease What Is Coronary Heart Disease?
Language switcher.

Coronary artery disease affects the larger coronary arteries on the surface of the heart. Another type of heart disease, called coronary microvascular disease, affects the tiny arteries within the heart muscle. Coronary microvascular disease is more common in women .
The cause of coronary heart disease depends on the type. Coronary artery disease is often caused by cholesterol, a waxy substance that builds up inside the lining of the coronary arteries, forming plaque. This plaque buildup can partially or totally block blood flow in the large arteries of the heart. Coronary microvascular disease occurs when there is damage to the inner walls of the heart’s small blood vessels. For most people, coronary heart disease is preventable with a heart-healthy lifestyle and medications.
Symptoms of coronary heart disease may be different from person to person even if they have the same type of coronary heart disease. However, because many people have no symptoms, they do not know they have coronary heart disease until they have chest pain; blood flow to the heart is blocked, causing a heart attack ; or the heart suddenly stops pumping blood, also known as cardiac arrest .
If you have coronary heart disease, you may need heart-healthy lifestyle changes, medicines, surgery, or a combination of these approaches to manage your condition and prevent serious problems .

Know the Difference Fact Sheet
Learn basic facts about coronary heart disease.

Coronary Artery Disease (CAD)
- • Buildup of cholesterol or plaque that causes arteries to stiffen, narrow, and restrict blood flow
- • Symptoms may not be noticeable at first but include fatigue, chest pain, and/or shortness of breath
- • Treatments include heart transplantation, artificial heart implantation, and valve replacements
- • Involves Cardiology
What causes coronary artery disease?
What are the symptoms of coronary artery disease, how is coronary artery disease diagnosed, how is coronary artery disease treated, what surgical procedures does yale medicine offer for the treatment of coronary artery disease, what makes yale medicine’s approach to the treatment of coronary artery disease unique.
There is a lot you can do to prevent coronary artery disease, which causes narrowing of the arteries and increases the risk of heart attack. It's the most common type of heart disease and the leading cause of death for both men and women in the United States.
Eating healthy, exercising, keeping your weight down, controlling your blood pressure and quitting smoking are all essential to preventing this condition.
If you do have risk factors—and they include family history—you should see a good cardiologist. Yale Medicine provides a full spectrum of clinical cardiovascular care, and our specialists have extensive experience with coronary artery disease. If you need surgery, we have renowned surgeons and the most advanced treatments available.
Coronary artery disease is caused by the gradual buildup of cholesterol or plaque, which makes the arteries stiffen and narrow. The result is reduced blood flow to the heart.
Multiple causes of coronary artery disease include:
- Genetics: Having a family history of heart disease
- Lifestyle: Eating unhealthy, high-fat foods and being sedentary
- Medical conditions: Including diabetes, high cholesterol and high blood pressure
Many people with heart disease have more than one of those risk factors.
People with coronary artery disease are at higher risk for a heart attack and other heart conditions that can be debilitating or even fatal. This leads to symptoms such as cardiac angina, the clinical term for shortness of breath and chest pain.
A sudden heart attack may be caused by a blood clot that forms on the surface of the plaque.
In its early stages, coronary artery disease may have no symptoms, though some people experience fatigue, chest pain or shortness of breath.
Doctors screen for heart disease during routine exams, asking questions about your personal and family history, taking blood samples to test cholesterol levels, and measuring your weight and blood pressure.
If a doctor has a reason to suspect you have heart disease, he or she may order additional tests. These can include an electrocardiogram, which measures electrical activity in the heart, or a stress test, which measures how well the heart works when stressed by physical activity.
Most people with coronary artery disease can be helped by one or several of three types of treatment. These are:
- Medication: Prescription drugs can counter the effects of heart disease, helping to keep risk factors including hypertension and cholesterol under control.
- Coronary stent: This is also called a percutaneous coronary intervention. A catheter is sent to the site of the blockage to open up the artery to restore blood flow.
- Heart surgery: A coronary artery bypass graft can reroute blood flow around a blocked artery.
Each of these treatments has advantages and disadvantages for patients. Surgery is generally reserved for patients who do not improve with the help of medication or stents or who can’t be effectively treated with those less-invasive methods.
Yale Medicine offers the full array of modern surgical treatments for all types of coronary artery disease. These include:
- Heart transplants
- Implantation of artificial hearts (called left ventricular assist devices, or LVAD )
- Mitral valve replacemen t and repair, for diseased heart valves
- Transcatheter Aortic Valve Replacement (called TAVR), an innovative treatment for patients with heart disease who are not strong enough for other types of heart surgery
Yale Medicine also offers surgical procedures to treat arrhythmia , hypertrophic cardiomyopathy , complex aortic aneurysm and other related issues.
Yale Medicine offers world-class expertise in treating all types of coronary artery disease with excellent outcomes.
Our doctors place a strong emphasis on multidisciplinary collaboration among cardiologists , interventional cardiologists, and cardiac surgeons .
Treatment planning for every high-risk patient with heart disease includes a formal collaborative discussion to evaluate all treatment options without any bias toward one specialty. This ensures that every patient benefits from input from specialists from several disciplines—a particular advantage for patients with complex heart disease.
Patients with heart disease who come to Yale Medicine for treatment can count on receiving cutting-edge therapies, using the latest, most innovative technologies and instrumentation.
Our cardiac surgeons’ clinical and basic research brings important advantages to patients, who have access to some of the newest technologies for the surgical treatment of heart disease.
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Coronary Heart Disease, Myocardial Infarction, and Stroke — A Public Health Issue

Available for Download [PDF – 3 MB]
Adults are living longer, and diseases of the heart and circulatory vessels are prevalent in this growing population of older adults. 1 Comorbid conditions along with cognition, sleep, physical balance and strength are factors that affect a person’s ability to function well and make disease management for people with coronary heart disease more challenging. 1,2 Maintaining functional abilities is critical for older adults from the perspective of overall health status, heart health, and chronic disease management. 1,2 Physical activity is key to preserving functional capacity and reducing frailty, which occurs more frequently in people with heart disease. 1,2 High blood pressure is an under-recognized contributing factor to premature disability and institutionalization and also key to preserving functional capacity. 3
Physical activity is important for maintaining heart muscle, vessel elasticity, reducing blood pressure levels and improving physical balance and strength. 1 It is foundational to chronic disease management programs and cardiac or stroke rehabilitation plans for improved mobility, fexibility and muscle strengthening. 1, 2
High blood pressure is a risk factor for coronary heart disease, myocardial infarction and stroke and is very common in older adults. 3 It is a leading cause of preventable illness and death. 3 Controlling high blood pressure is shown to reduce the risk of fatal myocardial infarctions and strokes. 3
Lowering blood pressure can be done safely with an established, monitored medication regime, physical activity and reduced sodium/salt intake. 3 Treating high blood pressure in older adults is a challenge due to other comorbid conditions, frailty, cognitive impairment and multiple medication use. 3
Coronary heart disease develops when major blood vessels supplying the heart with blood, oxygen and nutrients become damaged or blocked due to plaque build-up that limits blood flow. 4 Angina, a symptom of coronary heart disease, is chest pain or discomfort that occurs if an area of heart muscle is starved of oxygen-rich blood. 4 A heart attack occurs when the flow of oxygen-rich blood to a section of heart muscle suddenly becomes blocked and the heart can’t get oxygen and may damage heart muscle. 4 A stroke leads to death of brain cells due to lack of oxygen, caused by blockage of blood flow or rupture of a vessel to the brain. 4

Data for Public Health Action
As the older adult population continues to live longer, and diseases of the heart and circulatory vessels continue to increase, public health professionals are challenged to assist middle-aged and older adults in maintaining their functional capacity. Promoting chronic disease self-management through high blood pressure control, maintaining physical activity and a medication regime management is critical to older adult quality of life.

This brief examines the following questions:
- What percentage of adults report having coronary heart disease (CHD), including myocardial infarction and angina?
- What percentage of adults report having a stroke?
- What percentage of adults report being diagnosed with CHD, or a stroke, or both?
- What percentage of adults report being diagnosed with CHD, or a stroke, or both were taking high blood pressure medications?
- What percentage of adults report being diagnosed with CHD, or a stroke, or both were physically inactive, or had not exercised in the past month?
- What percentage of adults report being diagnosed with CHD, or a stroke, or both report good to excellent health or experienced 14 or more unhealthy days?
- What percentage of adults report being diagnosed with CHD, or a stroke, or both report having health care coverage and annual check-up?
- What percentage of adults report being diagnosed with CHD, or a stroke, or both report having two or more chronic diseases?
- What percentage of middle-aged and older adults report being diagnosed with CHD, or a stroke, or both self-report having subjective cognitive decline?
- What percentage of adults diagnosed with CHD, or a stroke, or both report being a caregiver by providing care or assistance to a friend or family member in the past 30 days or for two years or more?
The coronary heart disease and stroke data presented in this brief were collected from community-dwelling adults 45 years of age and older in 2015-2017 through the Behavioral Risk Factor Surveillance System (BRFSS).5 Questions related to coronary heart disease and stroke were administered in 50 states, the District of Columbia and two territories—Puerto Rico and Guam. Additional data reports can be generated and viewed through the CDC Healthy Aging Data Portal .
These data were examined in two age groups, adults 45-64 years and aged 65 years and older, as well as by sex, race and ethnicity, chronic disease status, and other demographic characteristics.
Characteristics of Middle-Aged and Older Adults with Coronary Heart Disease a
Figure 1: Adults Aged 45 years and Older Who Reported Having Coronary Heart Disease

Has a doctor, nurse, or other health professional ever told you that you had any of the following: Ever told you had a heart attack, also called a myocardial infarction? Ever told you had angina or coronary heart disease?

- 7.1% adults aged 45 to 64 years reported having CHD compared with 17.0% of adults aged 65 years and older.
- 13.6% of men reported having CHD compared with 8.4% of women.
- The prevalence of CHD varied among racial/ethnic groups: 11.4% of whites, 10.0% of blacks/African Americans, 8.8% of Hispanics, and 6.3% of Asians and Pacifc Islanders.
- Prevalence of CHD was lower in adults with more years of formal education (10.9% with post high school education) compared with adults with few years of formal education (16.5% with less than a high school diploma).
a Respondents were classified as having coronary heart disease (CHD) if they reported having been told by a provider they had CHD. Respondents were also classified as having CHD if they reported having been told they had a heart attack (i.e., myocardial infarction) or angina.
Characteristics of Middle-Aged and Older Adults with a Stroke b
Figure 2: Adults Aged 45 years and Older Who Reported Having Had a Stroke

Has a doctor, nurse, or other health professional ever told you that you had a stroke?

- 3.7% adults aged 45 to 64 years reported having been told that they had a stroke compared with 7.6% of adults aged 65 years and older.
- 5.3% of men reported having been told that they had a stroke compared with 5.0% of women.
- The prevalence of stroke varied among racial/ethnic groups: 5.1% of whites, 7.5% of blacks/African Americans, 3.7% of Hispanics, and 2.9% of Asians and Pacifc Islanders.
- Prevalence of stroke was lower in adults with more years of formal education (5.1% with post high school education) compared with adults with few years of formal education (8.0% with less than a high school diploma).
b Respondents may also have been told they have CHD (not mutually exclusive).
Characteristics of Middle-Aged and Older Adults with Coronary Heart Disease, a or a Stroke, or Both
Figure 3: Adults Aged 45 years and Older Who Reported Having Had Coronary Heart Disease, or a Stroke, or Both

Has a doctor, nurse, or other health professional ever told you that you had any of the following: Ever told you had a heart attack, also called a myocardial infarction? Ever told you had angina or coronary heart disease? Ever told you had a stroke?

- 9.6% adults aged 45 to 64 years reported being diagnosed with CHD, or a stroke, or both compared with 21.7% of adults aged 65 years and older.
- 16.8% of men reported having CHD, or a stroke, or both compared with 11.8% of women.
- The prevalence of CHD, or a stroke, or both varied among racial/ethnic groups: 14.8% of whites, 14.9% of blacks/African Americans, 11.2% of Hispanics, and 8.2% of Asians and Pacifc Islanders.
- Prevalence of CHD, or a stroke, or both was lower in adults with more years of formal education (11.7% of adults with post high school education) compared with adults with few years of formal education (21.2% of adults with less than a high school education).
- 30.5% of adults with CHD or a stroke, or both report living alone.
Health Status: Taking Medications for High Blood Pressure Among Adults with CHD or a Stroke, or Both
Figure 4: Adults Aged 45 years and Older with CHD, or a Stroke, or Both and Reported Taking High Blood Pressure Medicine

Has a doctor, nurse or other health professional ever told you that you have CHD, or a stroke, and or both and have high blood pressure? Are you currently taking medicine for your high blood pressure?

- 64.2% of adults aged 45 to 64 years diagnosed with CHD, or a stroke, or both reported taking high blood pressure medicine compared with 71.6% of adults aged 65 years and older.
- 68.4% of men with CHD, or a stroke, or both reported taking medications for high blood pressure compared with 68.6% of women with CHD, or a stroke, or both.
- The prevalence of CHD, or a stroke, or both and taking high blood pressure medications varied among racial/ethnic groups: 66.8% of whites, 79.9% of blacks/ African Americans, 66.0% of Hispanics, and 75.0% of Asians and Pacifc Islanders.
- Prevalence of adults with CHD, or a stroke or both and taking high blood pressure medicines was lower in adults with more than high school education (66.7%) compared with adults with less than a high school education (71.1%).
Health Status: Physical Activity
Figure 5: Adults Aged 45 years and Older Diagnosed with Coronary Heart Disease, or a Stroke, or Both Who Reported Participating in Physical Activity for 150 Minutes or More per Week in the Past Month

Being physically inactive can be a risk factor for increased complications for people diagnosed with coronary heart disease, or a stroke or both. Low and moderate levels of physical activity significantly reduce long-term risks for coronary heart disease deaths and assist with lowering high blood pressure. 6 The optimal amount of physical activity is moderate intensity aerobic exercise at least 150 minutes per week or 75 minutes per week of vigorous-intensity aerobic activity, for adults aged 45 years and older. 6
The physical activity measure identifies adults who participated in 150+ minutes (or vigorous equivalent minutes) of physical activity per week in past 30 days.
- 39.2% of adults aged 45-64 years diagnosed with CHD, or a stroke, or both reported participating in 150 minutes or more of physical activity per week compared with 46.3% of adults 65 years of age and older.
- 37.5% of women diagnosed with CHD, or a stroke, or both reported participating in 150 minutes or more of physical activity per week compared with 48.0% of men.
- The prevalence of adults participating in physical activity among adults diagnosed with CHD, or a stroke or both varied among racial/ethnic groups: 45.9% of whites, 32.9% of blacks/African Americans, 35.7% of Hispanics, and 50.7% of Asians and Pacifc Islanders.
- Prevalence of physical activity among adults diagnosed with CHD, or a stroke, or both was higher in adults with post high school education (50.8%) compared with adults with less than a high school education (32.7%).
Health Status: Health Care Coverage and Annual Check-ups
Figure 6: Adults Aged 45 years and Older Diagnosed with Coronary Heart Disease, or a Stroke, or Both, Who Had Health Insurance

Do you have any kind of health care coverage, including health insurance, prepaid plans such as HMOs, or government plans such as Medicare, or Indian Health Service?
- 98.2% of adults aged 65 years and older diagnosed with CHD, or a stroke, or both reported having health care coverage compared with 88.9% of adults aged 45-64 years.
- The prevalence of having some form of health care coverage among persons having CHD or a stroke or both varied among racial/ethnic groups: 95.9% of whites, 90.8% of blacks/African Americans, 87.8% of Hispanics, and 89.8% of Asians and Pacific Islanders.
About how long has it been since you last visited a doctor for a routine check-up? Within the past year versus >12 months or never?
- 87.4% of adults diagnosed with CHD, or a stroke, or both reported having a routine check-up within the past year.
- 91.0% of adults aged 65 years and older diagnosed with CHD, or a stroke, or both reported having a routine check-up compared with 82.4% of adults aged 45-64 years.
Health Status: Excellent to Good Health and Unhealthy Days
Persons who have experienced coronary heart disease, or a stroke, or both may experience physical or mental limitations associated with their condition.
Would you say your health is Excellent, Very Good, Good, Fair or Poor? (Good to Excellent Health are data captured)

- 55.3% of adults diagnosed with CHD, or a stroke, or both aged 65 years and older reported their health as good to excellent compared with 43.6% of adults aged 45-64 years.
- Prevalence of adults with CHD, or a stroke, or both who reported their health as good to excellent was higher in adults with post high school education (59.3%) compared with adults with less than a high school education (33.6%).
Now thinking about your mental health, which includes stress, depression and problems with emotions, for how many days during the past 30 days was your mental health not good?
- 11.6% of adults diagnosed with CHD, or a stroke or both aged 65 years and older reported 14 or more mentally unhealthy days in the past month compared with 27.8% of adults aged 45-64 years.
- Prevalence of adults with CHD, or a stroke, or both experiencing 14 or more mentally unhealthy days was lower in adults with post high school education (14.7%) compared with adults with less than a high school education (25.7%).
Now thinking about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good?
- 28.7% of adults diagnosed with CHD, or a stroke, or both aged 65 years and older reported 14 or more physically unhealthy days in the past month compared with 39.2% of adults aged 45-64 years.
Health Status: Chronic Diseases
Figure 7: Adults Aged 45 years and older with Coronary Heart Disease, or a Stroke, or Both Who Reported Having Two or More Chronic Health Conditions

Has a doctor, nurse or other health professional ever told you that you had one of the following: a heart attack, angina or coronary heart disease, stroke, asthma (still have), cancer (skin, other types of cancer), COPD, arthritis, depressive disorder, kidney disease, diabetes?
Multiple chronic diseases (two or more) have been found to be associated with increased potential for functional diffculties. 1 As the number of chronic diseases increases, the management of these diseases becomes increasingly complex, which may lead to a greater need for assistance. 2
- 58.7% of adults diagnosed with CHD, or a stroke, or both reported having two or more other chronic diseases other than CHD or stroke.
- 57.3% adults aged 45 to 64 years diagnosed with CHD, or a stroke, or both report having at least two or more other chronic diseases compared with 59.7% of adults aged 65 years and older.
- 52.5% of men diagnosed with CHD, or a stroke, or both reported having at least two or more other chronic diseases compared to 66.4% of women.
- The prevalence of having at least two other chronic diseases among adults diagnosed CHD, or a stroke or both varied among racial/ethnic groups: 59.1% of whites, 57.2% of blacks/African Americans, 50.7% of Hispanics, and 47.2% of Asians and Pacifc Islanders.
- Prevalence of having at least two other chronic diseases among adults diagnosed with CHD, or a stroke, or both was lower in adults with post high school education (56.5%) compared with adults with less than a high school education (63.3%).
Health Status: Subjective Cognitive Decline
Figure 8: Percentage of Adults Aged 45 Years and Older with Coronary Heart Disease, or a Stroke, or Both Who had Subjective Cognitive Decline

Coronary heart disease can lead to decreased cognitive function. 8 Subjective cognitive decline is the self-reported experience of worsening or more frequent confusion or memory loss within the past year. 7 Intensive blood pressure control may reduce the risk for cognitive decline.10 Cognitive decline can impact effective chronic disease self-management and successful activities of daily living. 8-10
During the past 12 months, have you experienced confusion or memory loss that is happening more often or is getting worse?
- 27.1% of adults aged 45-64 years diagnosed with CHD, or a stroke, or both reported subjective cognitive decline compared with 18.7% of adults 65 years of age and older.
- The prevalence of subjective cognitive decline among middle aged and older adults diagnosed with CHD, or a stroke, or both varied among racial/ethnic groups: 21.5% of whites, 23.1% of blacks/African Americans, 25.1% of Hispanics, and 7.1% of Asians and Pacifc Islanders.
- Prevalence of subjective cognitive decline among adults diagnosed with CHD, or a stroke, or both was lower in adults with post high school education (20.5%) compared with adults with less than a high school education (25.7%).
Prevalence of Coronary Heart Disease, or a Stroke, or Both Among Adult Caregivers
Figure 9: Adults Aged 45 years and Older with Coronary Heart Disease, or a Stroke, or Both Who Reported Being a Caregiver to Someone in the Past Month

Persons who have experienced a heart attack or a stroke, or who have coronary heart disease (angina) may also be a caregiver for a friend or family member. Limitations associated with their own chronic health conditions can cause their caregiver role to become more challenging. 1, 2, 8-10
During the past 30 days, did you provide regular care or assistance to a friend or family member who has a health problem or disability?

Multiple chronic diseases (two or more) have been found to be associated with increased potential for functional difficulties. 1 As the number of chronic diseases increases, the management of these diseases becomes increasingly complex, which may lead to a greater need for assistance. 2
- 21.8% of adults diagnosed with CHD, or a stroke, or both reported providing care or assistance to friend or family member within the past 30 days.
- 36.9% of adult caregivers diagnosed with CHD, or a stroke, or both provided care for a friend or family member within the past 30 days for 20 or more hours per week.
For how long have you provided care for that person?
- 56.1% of adults diagnosed with CHD, or a stroke, or both reported providing care or assistance to friend or family member during the past two years.
Note: Caregiver and Subjective Cognitive Decline (SCD) estimates are based on data collected in 2015-2017 for states that asked these two modules, compared to other topics using only 2017 data.
Call to Action
Public health professionals can use existing data, such as that presented in this brief, to form action steps to assist the growing older population in maintaining heart health and functional capacity by collaborating with partners engaged in heart health, brain health, physical activity, healthy aging, and chronic disease self-management programs at the national, tribal, state, and local levels.
Key Strategies to improve heart, body, and brain health and reduce functional difficulties include:
- The Million Hearts Program—a national initiative with a network of partners focused on preventing 1 million heart attacks, strokes and other cardiovascular events by 2022. 5
- Engage middle aged and older adults diagnosed with coronary heart disease, myocardial infarction, or a stroke to engage in heart healthy behaviors to reduce and prevent hospitalizations or disability.
- Step it Up—a national initiative of the US Surgeon General’s Call to Action to Promote Walking and Walkable Communities. 11
- Increase messaging that emphasizes both the important role of caregivers and the importance of maintaining caregivers’ health and well-being.
- State Heart Disease and Stroke Prevention Programs—The State Public Health Actions to Prevent and Control Diabetes, Heart Disease and Stroke, a multifaceted initiative to improve heart and stroke health. 5
- American College of Preventive Medicine’s Educating Physicians on Benefts of BP Management to Reduce Cognitive Decline—a continuing education program for physicians.
- Educate health care professionals on the benefts of blood pressure management as a potential mechanism to reduce the future risk of cognitive decline and dementia.
- Encourage caregivers to get regular check-ups, use preventive services, and engage in self-care to maintain health.
- Ensure that persons, including caregivers, with a disability or chronic health conditions have access to self-management programs to maintain their health.
Technical Information
The Behavioral Risk Factor Surveillance System (BRFSS) is the nation’s premier system of health-related telephone surveys that collect state data about U.S. residents regarding their health-related risk behaviors, chronic diseases, and use of preventive services. Established in 1984 with 15 states, BRFSS now collects data in all 50 states as well as the District of Columbia and three U.S. territories. BRFSS completes more than 450,000 adult interviews each year, making it the largest and longest continuously conducted health survey system in the world.
The crucial information gathered through this state-based telephone surveillance system is used by national, state, and local public health agencies to identify populations that might be most at risk and to monitor the need for and the effectiveness of various public health interventions.
Although the BRFSS is a useful tool for assessing coronary heart disease and stroke in adult populations, it has some limitations: it excludes people who do not have telephones or are in institutions such as nursing homes; it may under represent people who are severely impaired because of the functional capacity required to participate in the survey; and responses to BRFSS are self-reported and therefore have not been confirmed by a healthcare provider. Despite these limitations, the BRFSS is a uniquely powerful tool to provide the prevalence of coronary heart disease and stroke and related issues among older community-dwelling U.S. adults, due to its large sample size and proven reliability and validity.
The BRFSS is administered and supported by the Division of Population Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. For more information, please visit https://www.cdc.gov/brfss .
- Forman DE, Arena R, Boxer R, et al. Prioritizing functional capacity as a principal end point for therapies oriented to older adults with cardiovascular disease: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2017;135:e894–e918. doi: 10.1161/CIR.0000000000000483
- Kleipool EE, Hoogendijk EO, Trappenburg MC, et al. frailty in older adults with cardiovascular disease: cause, effect or both?. Aging Dis . 2018;9(3):489-497. doi:10.14336/AD.2017.1125.
- Whelton PK, Carey, RM, Aronow WS, et al. 2017 high blood pressure clinical practice guideline: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol . 2018;17(19). doi: 10.1161/HYP.0000000000000066
- National Heart, Lung, and Blood Institute. Health Topics website. https://www.nhlbi.nih.gov/health-topics . Accessed 16 January 2019.
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System website. https://www.cdc.gov/brfss . Accessed 16 January 2019.
- O’Keefe JH, O’Keefe EL, Lavie CJ. The goldilocks zone for exercise: not too little, not too much. Mo Med. 2018;115 (2):98-105.
- Taylor CA, Bouldin ED, McGuire LC. Subjective cognitive decline among adults aged ≥45 years — United States, 2015–2016. Rep . 2018;67:753–757. doi:10.15585/mmwr.mm6727a1
- Haring B, Leng X, Robinson J, et al. Cardiovascular disease and cognitive decline in postmenopausal women: results from the Women’s Health Initiative Memory Study. J Am Heart Assoc . 2013;2(6):e000369. Published 2013 Dec 19. doi:10.1161/JAHA.113.000369
- Lutski M, Weinstein G, Goldbourt U, Tanne D. Cardiovascular health and cognitive decline 2 decades later in men with preexisting coronary artery disease. Am J Cardiol . 2018;121(4):410–415. doi:10.1016/j.amjcard.2017.11.003
- The SPRINT MIND Investigators for the SPRINT Research Group. Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial. JAMA . 2019;321(6):553–561. doi:10.1001/jama.2018.21442 Note: Caregiver and Subjective Cognitive Decline (SCD) estimates are based on data collected in 2015-2017 for states that asked these two modules, compared to other topics using only 2017 data.
- Centers for Disease Control and Prevention. Step it Up! The Surgeon General’s Call to Action to Promote Walking and Walkable Communities website. https://www.cdc.gov/physicalactivity/walking/call-to-action/?s_cid=bb-dnpao-calltoaction-002
Disclaimer: The mark “CDC” is owned by the U.S. Department of Health and Human Services (HHS) and is used with permission. Use of this logo is not an endorsement by HHS or the Centers for Disease Control and Prevention (CDC) or any particular product, service, or enterprise.
To receive email updates about Alzheimer's Disease and Healthy Aging, enter your email address:
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 12 November 2020
Early and accurate detection and diagnosis of heart disease using intelligent computational model
- Yar Muhammad 1 ,
- Muhammad Tahir 1 ,
- Maqsood Hayat 1 &
- Kil To Chong 2
Scientific Reports volume 10 , Article number: 19747 ( 2020 ) Cite this article
27k Accesses
82 Citations
Metrics details
- Cardiovascular diseases
- Computational biology and bioinformatics
- Health care
- Heart failure
Heart disease is a fatal human disease, rapidly increases globally in both developed and undeveloped countries and consequently, causes death. Normally, in this disease, the heart fails to supply a sufficient amount of blood to other parts of the body in order to accomplish their normal functionalities. Early and on-time diagnosing of this problem is very essential for preventing patients from more damage and saving their lives. Among the conventional invasive-based techniques, angiography is considered to be the most well-known technique for diagnosing heart problems but it has some limitations. On the other hand, the non-invasive based methods, like intelligent learning-based computational techniques are found more upright and effectual for the heart disease diagnosis. Here, an intelligent computational predictive system is introduced for the identification and diagnosis of cardiac disease. In this study, various machine learning classification algorithms are investigated. In order to remove irrelevant and noisy data from extracted feature space, four distinct feature selection algorithms are applied and the results of each feature selection algorithm along with classifiers are analyzed. Several performance metrics namely: accuracy, sensitivity, specificity, AUC, F1-score, MCC, and ROC curve are used to observe the effectiveness and strength of the developed model. The classification rates of the developed system are examined on both full and optimal feature spaces, consequently, the performance of the developed model is boosted in case of high variated optimal feature space. In addition, P-value and Chi-square are also computed for the ET classifier along with each feature selection technique. It is anticipated that the proposed system will be useful and helpful for the physician to diagnose heart disease accurately and effectively.
Similar content being viewed by others

Analyzing the impact of feature selection methods on machine learning algorithms for heart disease prediction

An active learning machine technique based prediction of cardiovascular heart disease from UCI-repository database
Finding the influential clinical traits that impact on the diagnosis of heart disease using statistical and machine-learning techniques
Introduction.
Heart disease is considered one of the most perilous and life snatching chronic diseases all over the world. In heart disease, normally the heart fails to supply sufficient blood to other parts of the body to accomplish their normal functionality 1 . Heart failure occurs due to blockage and narrowing of coronary arteries. Coronary arteries are responsible for the supply of blood to the heart itself 2 . A recent survey reveals that the United States is the most affected country by heart disease where the ratio of heart disease patients is very high 3 . The most common symptoms of heart disease include physical body weakness, shortness of breath, feet swollen, and weariness with associated signs, etc. 4 . The risk of heart disease may be increased by the lifestyle of a person like smoking, unhealthy diet, high cholesterol level, high blood pressure, deficiency of exercise and fitness, etc. 5 . Heart disease has several types in which coronary artery disease (CAD) is the common one that can lead to chest pain, stroke, and heart attack. The other types of heart disease include heart rhythm problems, congestive heart failure, congenital heart disease (birth time heart disease), and cardiovascular disease (CVD). Initially, traditional investigation techniques were used for the identification of heart disease, however, they were found complex 6 . Owing to the non-availability of medical diagnosing tools and medical experts specifically in undeveloped countries, diagnosis and cure of heart disease are very complex 7 . However, the precise and appropriate diagnosis of heart disease is very imperative to prevent the patient from more damage 8 . Heart disease is a fatal disease that rapidly increases in both economically developed and undeveloped countries. According to a report generated by the World Health Organization (WHO), an average of 17.90 million humans died from CVD in 2016. This amount represents approximately 30% of all global deaths. According to a report, 0.2 million people die from heart disease annually in Pakistan. Every year, the number of victimizing people is rapidly increasing. European Society of Cardiology (ESC) has published a report in which 26.5 million adults were identified having heart disease and 3.8 million were identified each year. About 50–55% of heart disease patients die within the initial 1–3 years, and the cost of heart disease treatment is about 4% of the overall healthcare annual budget 9 .
Conventional invasive-based methods used for the diagnosis of heart disease which were based on the medical history of a patient, physical test results, and investigation of related symptoms by the doctors 10 . Among the conventional methods, angiography is considered one of the most precise technique for the identification of heart problems. Conversely, angiography has some drawbacks like high cost, various side effects, and strong technological knowledge 11 . Conventional methods often lead to imprecise diagnosis and take more time due to human mistakes. In addition, it is a very expensive and computational intensive approach for the diagnosis of disease and takes time in assessment 12 .
To overcome the issues in conventional invasive-based methods for the identification of heart disease, researchers attempted to develop different non-invasive smart healthcare systems based on predictive machine learning techniques namely: Support Vector Machine (SVM), K-Nearest Neighbor (KNN), Naïve Bayes (NB), and Decision Tree (DT), etc. 13 . As a result, the death ratio of heart disease patients has been decreased 14 . In literature, the Cleveland heart disease dataset is extensively utilized by the researchers 15 , 16 .
In this regard, Robert et al . 17 have used a logistic regression classification algorithm for heart disease detection and obtained an accuracy of 77.1%. Similarly, Wankhade et al . 18 have used a multi-layer perceptron (MLP) classifier for heart disease diagnosis and attained accuracy of 80%. Likewise, Allahverdi et al . 19 have developed a heart disease classification system in which they integrated neural networks with an artificial neural network and attained an accuracy of 82.4%. In a sequel, Awang et al . 20 have used NB and DT for the diagnosis and prediction of heart disease and achieved reasonable results in terms of accuracy. They achieved an accuracy of 82.7% with NB and 80.4% with DT. Oyedodum and Olaniye 21 have proposed a three-phase system for the prediction of heart disease using ANN. Das and Turkoglu 22 have proposed an ANN ensemble-based predictive model for the prediction of heart disease. Similarly, Paul and Robin 23 have used the adaptive fuzzy ensemble method for the prediction of heart disease. Likewise, Tomov et al. 24 have introduced a deep neural network for heart disease prediction and his proposed model performed well and produced good outcomes. Further, Manogaran and Varatharajan 25 have introduced the concept of a hybrid recommendation system for diagnosing heart disease and their model has given considerable results. Alizadehsani et al . 26 have developed a non-invasive based model for the prediction of coronary artery disease and showed some good results regarding the accuracy and other performance assessment metrics. Amin et al . 27 have proposed a framework of a hybrid system for the identification of cardiac disease, using machine learning, and attained an accuracy of 86.0%. Similarly, Mohan et al . 28 have proposed another intelligent system that integrates RF with a linear model for the prediction of heart disease and achieved the classification accuracy of 88.7%. Likewise, Liaqat et al . 29 have developed an expert system that uses stacked SVM for the prediction of heart disease and obtained 91.11% classification accuracy on selected features.
The contribution of the current work is to introduce an intelligent medical decision system for the diagnosis of heart disease based on contemporary machine learning algorithms. In this study, 10 different nature of machine learning classification algorithms such as Logistic Regression (LR), Decision Tree (DT), Naïve Bayes (NB), Random Forest (RF), Artificial Neural Network (ANN), etc. are implemented in order to select the best model for timely and accurate detection of heart disease at an early stage. Four feature selection algorithms, Fast Correlation-Based Filter Solution (FCBF), minimal redundancy maximal relevance (mRMR), Least Absolute Shrinkage and Selection Operator (LASSO), and Relief have been used for selecting the vital and more correlated features that have truly reflect the motif of the desired target. Our developed system has been trained and tested on the Cleveland (S 1 ) and Hungarian (S 2 ) heart disease datasets which are available online on the UCI machine learning repository. All the processing and computations were performed using Anaconda IDE. Python has been used as a tool for implementing all the classifiers. The main packages and libraries used include pandas, NumPy, matplotlib, sci-kit learn (sklearn), and seaborn. The main contribution of our proposed work is given below:
The performance of all classifiers has been tested on full feature spaces in terms of all performance evaluation matrices specifically accuracy.
The performances of the classifiers are tested on selected feature spaces, selected through various feature selection algorithms mentioned above.
The research study recommends that which feature selection algorithm is feasible with which classification algorithm for developing a high-level intelligence system for the diagnosing of heart disease patients.
The rest of the paper is organized as: “ Results and discussion ” section represents the results and discussion, “ Material and methods ” section describes the material and methods used in this paper. Finally, we conclude our proposed research work in “ Conclusion ” section.
Results and discussion
This section of the paper discusses the experimental results of various contemporary classification algorithms. At first, the performance of all used classification models i.e. K-Nearest Neighbors (KNN), Decision Tree (DT), Extra-Tree Classifier (ETC), Random Forest (RF), Logistic Regression (LR), Naïve Bayes (NB), Artificial Neural Network (ANN), Support Vector Machine (SVM), Adaboost (AB), and Gradient Boosting (GB) along with full feature space is evaluated. After that, four feature selection algorithms (FSA): Fast Correlation-Based Filter (FCBF), Minimal Redundancy Maximal Relevance (mRMR), Least Absolute Shrinkage and Selection Operator (LASSO), and Relief are applied to select the prominent and high variant features from feature space. Furthermore, the selected feature spaces are provided to classification algorithms as input to analyze the significance of feature selection techniques. The cross-validation techniques i.e. k-fold (10-fold) are applied on both the full and selected feature spaces to analyze the generalization power of the proposed model. Various performance evaluation metrics are implemented for measuring the performances of the classification models.
Classifiers’ predictive outcomes on full feature space
The experimental outcomes of the applied classification algorithms on the full feature space of the two benchmark datasets by using 10-fold cross-validation (CV) techniques are shown in Tables 1 and 2 , respectively.
The experimental results demonstrated that the ET classifier performed quite well in terms of all performance evaluation metrics compared to the other classifiers using 10-fold CV. ET achieved 92.09% accuracy, 91.82% sensitivity, 92.38% specificity, 97.92% AUC, 92.84% Precision, 0.92 F1-Score and 0.84 MCC. The specificity indicates that the diagnosed test was negative and the individual doesn't have the disease. While the sensitivity indicates the diagnostic test was positive and the patient has heart disease. In the case of the KNN classification model, multiple experiments were accomplished by considering various values for k i.e. k = 3, 5, 7, 9, 13, and 15, respectively. Consequently, KNN has shown the best performance at value k = 7 and achieved a classification accuracy of 85.55%, 85.93% sensitivity, 85.17% specificity, 95.64% AUC, 86.09% Precision, 0.86 F1-Score, and 0.71 MCC. Similarly, DT classifier has achieved accuracy of 86.82%, 89.73% sensitivity, 83.76% specificity, 91.89% AUC, 85.40% Precision, 0.87 F1-Score, and 0.73 MCC. Likewise, GB classifier has yielded accuracy of 91.34%, 90.32% sensitivity, 91.52% specificity, 96.87% AUC, 92.14% Precision, 0.92 F1-Score, and 0.83 MCC. After empirically evaluating the success rates of all classifiers, it is observed that ET Classifier out-performed among all the used classification algorithms in terms of accuracy, sensitivity, and specificity. Whereas, NB shows the lowest performance in terms of accuracy, sensitivity, and specificity. The ROC curve of all classification algorithms on full feature space is represented in Fig. 1 .
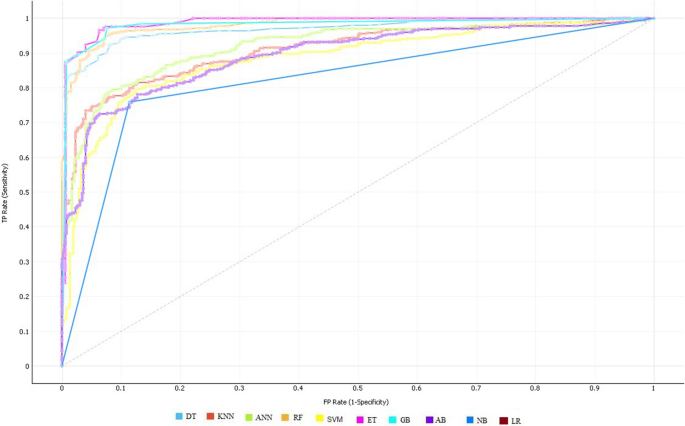
ROC curves of all classifiers on full feature space using 10-fold cross-validation on S 1 .
In the case of dataset S 2 , composed of 1025 total instances in which 525 belong to the positive class and 500 instances of having negative class, again ET has obtained quite well results compared to other classifiers using a 10-fold cross-validation test, which are 96.74% accuracy, 96.36 sensitivity, 97.40% specificity, and 0.93 MCC as shown in Table 2 .
Classifiers’ predictive outcomes on selected feature space
Fcbf feature selection technique.
FCBF feature selection technique is applied to select the best subset of feature space. In this attempt, various length of subspaces is generated and tested. Finally, the best results are achieved by classification algorithms on the subset of feature space (n = 6) using a 10-fold CV. Table 3 shows various performance measures of classifiers executed on the selected features space of FCBF.
Table 3 demonstrates that the ET classifier obtained quite good results including accuracy of 94.14%, 94.29% sensitivity, and specificity of 93.98%. In contrast, NB reported the lowest performance compared to the other classification algorithms. The performance of classification algorithms is also illustrated in Fig. 2 by using ROC curves.
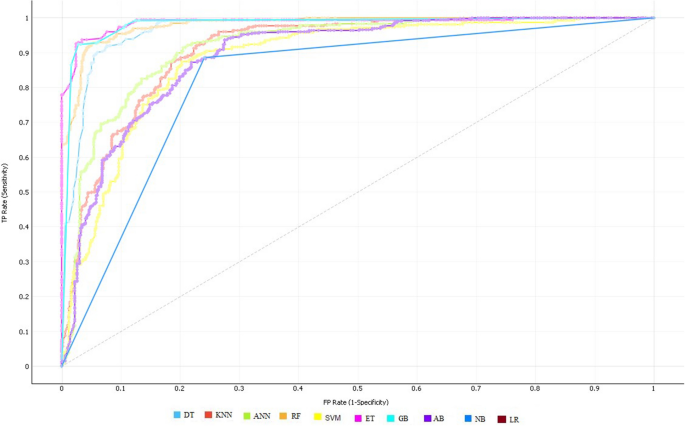
ROC curve of all classifiers on selected features by FCBF feature selection algorithm.
mRMR feature selection technique
mRMR feature selection technique is used in order to select a subset of features that enhance the performance of classifiers. The best results reported on a subset of n = 6 of feature space which is shown in Table 4 .
In the case of mRMR, still, the success rates of the ET classifier are well in terms of all performance evaluation metrics compared to the other classifiers. ET has attained 93.42% accuracy, 93.92% sensitivity, and specificity of 93.88%. In contrast, NB has achieved the lowest outcomes which are 81.84% accuracy. Figure 3 shows the ROC curve of all ten classifiers using the mRMR feature selection algorithm.
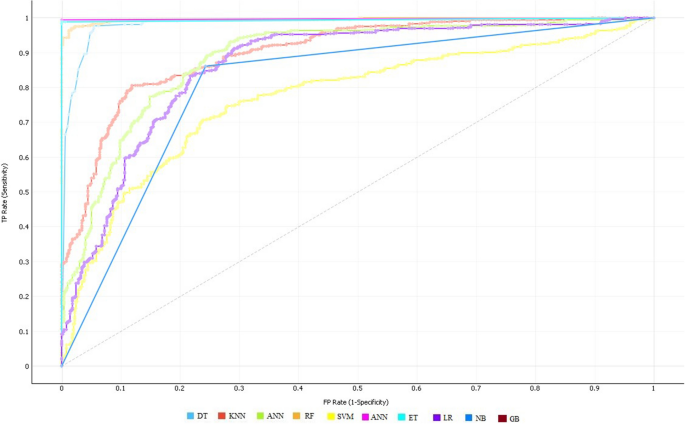
ROC curve of all classifiers on selected features using the mRMR feature selection algorithm.

LASSO feature selection technique
In order to choose the optimal feature space which not only reduces computational cost but also progresses the performance of the classifiers, LASSO feature selection technique is applied. After performing various experiments on different subsets of feature space, the best results are still noted on the subspace of (n = 6). The predicted outcomes of the best-selected feature space are reported in Table 5 using the 10-fold CV.
Table 5 demonstrated that the predicted outcomes of the ET classifier are considerable and better compared to the other classifiers. ET has achieved 89.36% accuracy, 88.21% sensitivity, and specificity of 90.58%. Likewise, GB has yielded the second-best result which is the accuracy of 88.47%, 89.54% sensitivity, and specificity of 87.37%. Whereas, LR has performed worse results and achieved 80.77% accuracy, 83.46% sensitivity, and specificity of 77.95%. ROC curves of the classifiers are shown in Fig. 4 .
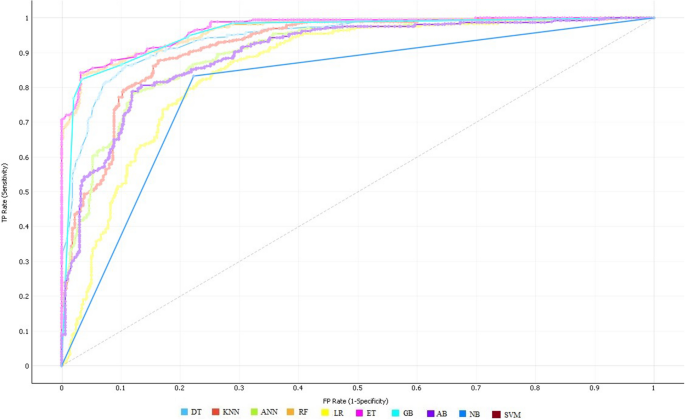
ROC curve of all classifiers on selected feature space using the LASSO feature selection algorithm.
Relief feature selection technique
In a sequel, another feature selection technique Relief is applied to investigate the performance of classifiers on different sub-feature spaces by using the wrapper method. After empirically analyzing the results of the classifiers on a different subset of feature spaces, it is observed that the performance of classifiers is outstanding on the sub-space of length (n = 6). The results of the optimal feature space on the 10-fold CV technique are listed in Table 6 .
Again, the ET classifier performed outstandingly in terms of all performance evaluation metrics as compared to other classifiers. ET has obtained an accuracy of 94.41%, 94.93% sensitivity, and specificity of 94.89%. In contrast, NB has shown the lowest performance and achieved 80.29% accuracy, 81.93% sensitivity, and specificity of 78.55%. The ROC curves of the classifiers are demonstrated in Fig. 5 .
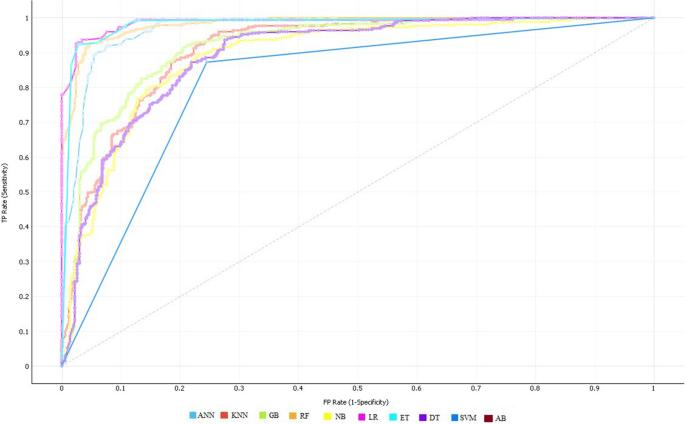
ROC curve of all classifiers on selected features selected by the Relief feature selection algorithm.
After executing classification algorithms along with full and selected feature spaces in order to select the optimal algorithm for the operational engine, the empirical results have revealed that ET performed well not only on all feature space but also on optimal selected feature space among all the used classification algorithms. Furthermore, the ET classifier obtained quite promising accuracy in the case of the Relief feature selection technique which is 94.41%. Overall, the performance of ET is reported better in terms of most of the measures while other classifiers have shown good results in one measure while worse in other measures. In addition, the performance of the ET classifier is also evaluated on a 10-fold CV in combination with different sub-feature spaces of varying length starting from 1 to 12 with a step size of 1 to check the stability and discrimination power of the classifier as described in 30 . Doing so will assist the readers to have a better understanding of the impact, of the number of selected features on the performance of the classifiers. The same process is repeated for another dataset i.e. S 2 (Hungarian heart disease dataset) as well, to know the impact of selected features on the classification performance.
Tables 7 and 8 shows the performance of the ET classifier using 10-fold CV in combination with different feature sub-spaces starting from 1 to 12 with a step size of 1. The experimental results show that the performance of the ET classifier is affected significantly by using the varying length of sub-feature spaces. Finally, it is concluded that all these achievements are ascribed with the best selection of Relief feature selection technique which not only reduces the feature space but also enhances the predictive power of classifiers. In addition, the ET classifier has also played a quite promising role in these achievements because it has clearly and precisely learned the motif of the target class and reflected it truly. In addition, the performance of the ET classifier is also evaluated on 5-fold and 7-fold CV in combination with different sub-spaces of length 5 and 7 to check the stability and discrimination power of the classifier. It is also tested on another dataset S 2 (Hungarian heart disease dataset). The results are shown in supplementary materials .
In Table 9 , P-value and Chi-Square values are also computed for the ET classifier in combination with the optimal feature spaces of different feature selection techniques.
Performance comparison with existing models
Further, a comparative study of the developed system is conducted with other states of the art machine learning approaches discussed in the literature. Table 10 represents, a brief description and classification accuracies of those approaches. The results demonstrate that our proposed model success rate is high compared to existing models in the literature.
Material and methods
The subsections represent the materials and the methods that are used in this paper.
The first and rudimentary step of developing an intelligent computational model is to construct or develop a problem-related dataset that truly and effectively reflects the pattern of the target class. Well organized and problem-related dataset has a high influence on the performance of the computational model. Looking at the significance of the dataset, two datasets i.e. the Cleveland heart disease dataset S 1 and Hungarian heart disease dataset (S 2 ) are used, which are available online at the University of California Irvine (UCI) machine learning repository and UCI Kaggle repository, and various researchers have used it for conducting their research studies 28 , 31 , 32 . The S1 consists of 304 instances, where each instance has distinct 13 attributes along with the target labels and are selected for training. The dataset is composed of two classes, presence or absence of heart disease. The S 2 is composed of 1025 instances in which 525 instances belong to positive class while the rest of 500 instances have negative class. The description of attributes of both the datasets is the same, and both have similar attributes. The complete description and information of the datasets with 13 attributes are given in Table 11 .
Proposed system methodology
The main theme of the developed system is to identify heart problems in human beings. In this study, four distant feature selection techniques namely: FCBF, mRMR, Relief, and LASSO are applied on the provided dataset in order to remove noisy, redundant features and select variant features, consequently may cause of enhancing the performance of the proposed model. Various machine learning classification algorithms are used in this study which include, KNN, DT, ETC, RF, LR, NB, ANN, SVM, AB, and GB. Different evaluation metrics are computed to assess the performance of classification algorithms. The methodology of the proposed system is carried out in five stages which include dataset preprocessing, selection of features, cross-validation technique, classification algorithms, and performance evaluation of classifiers. The framework of the proposed system is illustrated in Fig. 6 .
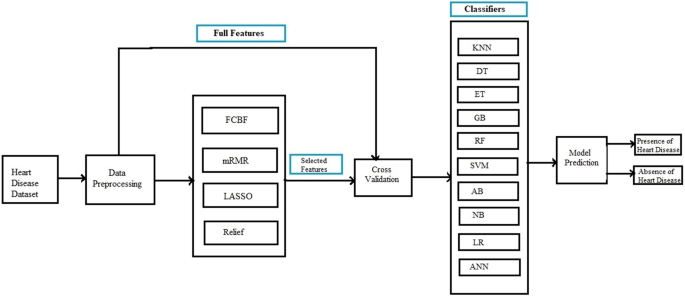
An Intelligent Hybrid Framework for the prediction of heart disease.
Preprocessing of data
Data preprocessing is the process of transforming raw data into meaningful patterns. It is very crucial for a good representation of data. Various preprocessing approaches such as missing values removal, standard scalar, and Min–Max scalar are used on the dataset in order to make it more effective for classification.
Feature selection algorithms
Feature selection technique selects the optimal features sub-space among all the features in a dataset. It is very crucial because sometimes, the classification performance degrades due to irrelevant features in the dataset. The feature selection technique improves the performance of classification algorithms and also reduces their execution time. In this research study, four feature selection techniques are used and are listed below:
Fast correlation-based filter (FCBF): FCBF feature selection algorithm follows a sequential search strategy. It first selects full features and then uses symmetric uncertainty for measuring the dependencies of the features on each other and how they affect the target output label. After this, it selects the most important features using the backward sequential search strategy. FCBF outperforms on high dimensional datasets. Table 12 shows the results of the selected features (n = 6) by using the FCBF feature selection algorithm. Each attribute is given a weight based on its importance. According to the FCBF feature selection technique, the most important features are THA and CPT as shown in Table 12 . The ranking that the FCBF gives to all the features of the dataset is shown in Fig. 7 .
Minimal redundancy maximal relevance (mRMR): mRMR uses the heuristic approach for selecting the most vital features that have minimum redundancy and maximum relevance. It selects those features which are useful and relevant to the target. As it follows a heuristic approach so, it checks one feature at a time and then computes its pairwise redundancy with the other features. The mRMR feature selection algorithm is not suitable for high domain feature problems 33 . The results of selected features by the mRMR feature selection algorithm (n = 6) are listed in Table 13 . In addition, among these attributes, PES and CPT have the highest score. Figure 7 describes the attributes ranking given by the mRMR feature selection algorithm to all attributes in the feature space.
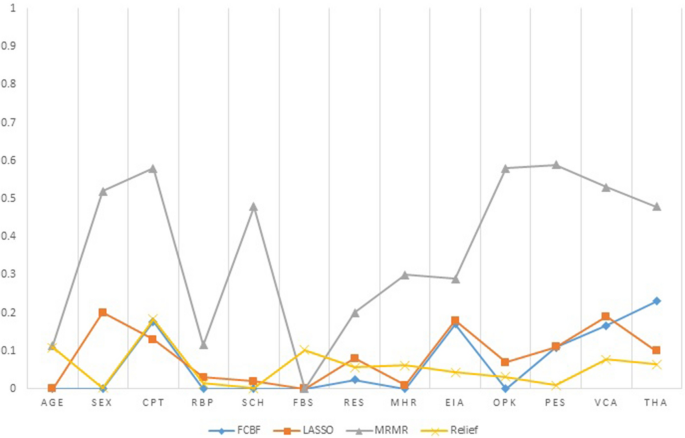
Features ranking by four feature selection algorithms (FCBF, LASSO, mRMR, Relief).
Least absolute shrinkage and selection operator (LASSO) LASSO selects features based on updating the absolute value of the features coefficient. In updating the features coefficient values, zero becoming values are removed from the features subset. LASSO outperforms with low feature coefficient values. The features having high coefficient values will be selected in the subset of features and the rest will be eliminated. Moreover, some irrelevant features with higher coefficient values may be selected and are included in the subset of features 30 . Table 14 represents the six most profound attributes which have a great correlation with the target and their scores selected by the LASSO feature selection algorithm. Figure 7 represents the important features and their scoring values given by the LASSO feature selection algorithm.
Relief feature selection algorithm Relief utilizes the concept of instance-based learning which allocates weight to each attribute based on its significance. The weight of each attribute demonstrates its capability to differentiate among class values. Attributes are rated by weights, and those attributes whose weight is exceeding a user-specified cutoff, are chosen as the final subset 34 . The relief feature selection algorithm selects the most significant attributes which have more effect on the target 35 . The algorithm operates by selecting instances randomly from the training samples. The nearest instance of the same class (nearest hit) and opposite class (nearest miss) is identified for each sampled instance. The weight of an attribute is updated according to how well its values differentiate between the sampled instance and its nearest miss and hit. If an attribute discriminates amongst instances from different classes and has the same value for instances of the same class, it will get a high weight.
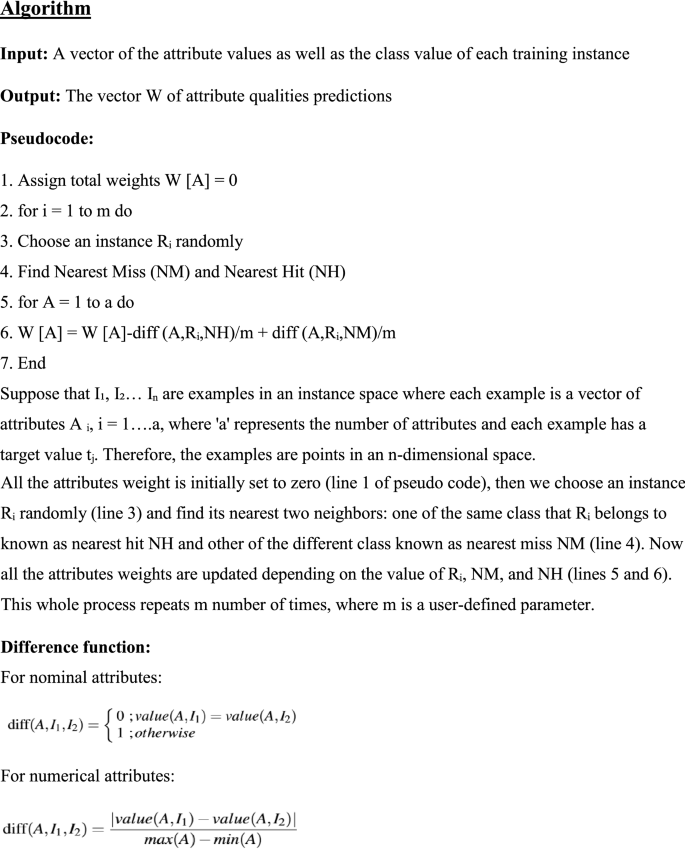
The weight updating of attributes works on a simple idea (line 6). That if instance R i and NH have dissimilar value (i.e. the diff value is large), that means the attribute splits two instances with the same class which is not worthwhile, and thus we reduce the attributes weight. On the other hand, if the instance R i and NM have a distinct value that means the attribute separates the two instances with a different class, which is desirable. The six most important features selected by the Relief algorithm are listed in descending order in Table 15 . Based on weight values the most vital features are CPT and Age. Figure 7 demonstrates the important features and their ranking given by the Relief feature selection algorithm.
Machine learning classification algorithms
Various machine learning classification algorithms are investigated for early detection of heart disease, in this study. Each classification algorithm has its significance and the importance is reported varied from application to application. In this paper, 10 distant nature of classification algorithms namely: KNN, DT, ET, GB, RF, SVM, AB, NB, LR, and ANN are applied to select the best and generalize prediction model.
Classifier validation method
Validation of the prediction model is an essential step in machine learning processes. In this paper, the K-Fold cross-validation method is applied to validating the results of the above-mentioned classification models.
K-fold cross validation (CV)
In K-Fold CV, the whole dataset is split into k equal parts. The (k-1) parts are utilized for training and the rest is used for the testing at each iteration. This process continues for k-iteration. Various researchers have used different values of k for CV. Here k = 10 is used for experimental work because it produces good results. In tenfold CV, 90% of data is utilized for training the model and the remaining 10% of data is used for the testing of the model at each iteration. At last, the mean of the results of each step is taken which is the final result.
Performance evaluation metrics
For measuring the performance of the classification algorithms used in this paper, various evaluation matrices have been implemented including accuracy, sensitivity, specificity, f1-score, recall, Mathew Correlation-coefficient (MCC), AUC-score, and ROC curve. All these measures are calculated from the confusion matrix described in Table 16 .
In confusion matrix True Negative (TN) shows that the patient has not heart disease and the model also predicts the same i.e. a healthy person is correctly classified by the model.
True Positive (TP) represents that the patient has heart disease and the model also predicts the same result i.e. a person having heart disease is correctly classified by the model.
False Positive (FP) demonstrates that the patient has not heart disease but the model predicted that the patient has i.e. a healthy person is incorrectly classified by the model. This is also called a type-1 error.
False Negative (FN) notifies that the patient has heart disease but the model predicted that the patient has not i.e. a person having heart disease is incorrectly classified by the model. This is also called a type-2 error.
Accuracy Accuracy of the classification model shows the overall performance of the model and can be calculated by the formula given below:
Specificity specificity is a ratio of the recently classified healthy people to the total number of healthy people. It means the prediction is negative and the person is healthy. The formula for calculating specificity is given as follows:
Sensitivity Sensitivity is the ratio of recently classified heart patients to the total patients having heart disease. It means the model prediction is positive and the person has heart disease. The formula for calculating sensitivity is given below:
Precision: Precision is the ratio of the actual positive score and the positive score predicted by the classification model/algorithm. Precision can be calculated by the following formula:
F1-score F1 is the weighted measure of both recall precision and sensitivity. Its value ranges between 0 and 1. If its value is one then it means the good performance of the classification algorithm and if its value is 0 then it means the bad performance of the classification algorithm.
MCC It is a correlation coefficient between the actual and predicted results. MCC gives resulting values between − 1 and + 1. Where − 1 represents the completely wrong prediction of the classifier.0 means that the classifier generates random prediction and + 1 represents the ideal prediction of the classification models. The formula for calculating MCC values is given below:
Finally, we will examine the predictability of the machine learning classification algorithms with the help of the receiver optimistic curve (ROC) which represents a graphical demonstration of the performance of ML classifiers. The area under the curve (AUC) describes the ROC of a classifier and the performance of the classification algorithms is directly linked with AUC i.e. larger the value of AUC greater will be the performance of the classification algorithm.
In this study, 10 different machine learning classification algorithms namely: LR, DT, NB, RF, ANN, KNN, GB, SVM, AB, and ET are implemented in order to select the best model for early and accurate detection of heart disease. Four feature selection algorithms such as FCBF, mRMR, LASSO, and Relief have been used to select the most vital and correlated features that truly reflect the motif of the desired target. Our developed intelligent computational model has been trained and tested on two datasets i.e. Cleveland (S1) and Hungarian (S2) heart disease datasets. Python has been used as a tool for implementation and simulating the results of all the utilized classification algorithms.
The performance of all classification models has been tested in terms of various performance metrics on full feature space as well as selected feature spaces, selected through various feature selection algorithms. This research study recommends that which feature selection algorithm is feasible with which classification model for developing a high-level intelligent system for the diagnosis of a patient having heart disease. From simulation results, it is observed that ET is the best classifier while relief is the optimal feature selection algorithm. In addition, P-value and Chi-square are also computed for the ET classifier along with each feature selection algorithm. It is anticipated that the proposed system will be useful and helpful for the doctors and other care-givers to diagnose a patient having heart disease accurately and effectively at the early stages.
Heart disease is one of the most devastating and fatal chronic diseases that rapidly increase in both economically developed and undeveloped countries and causes death. This damage can be reduced considerably if the patient is diagnosed in the early stages and proper treatment is provided to her. In this paper, we developed an intelligent predictive system based on contemporary machine learning algorithms for the prediction and diagnosis of heart disease. The developed system was checked on two datasets i.e. Cleveland (S1) and Hungarian (S2) heart disease datasets. The developed system was trained and tested on full features and optimal features as well. Ten classification algorithms including, KNN, DT, RF, NB, SVM, AB, ET, GB, LR, and ANN, and four feature selection algorithms such as FCBF, mRMR, LASSO, and Relief are used. The feature selection algorithm selects the most significant features from the feature space, which not only reduces the classification errors but also shrink the feature space. To assess the performance of classification algorithms various performance evaluation metrics were used such as accuracy, sensitivity, specificity, AUC, F1-score, MCC, and ROC curve. The classification accuracies of the top two classification algorithms i.e. ET and GB on full features were 92.09% and 91.34% respectively. After applying feature selection algorithms, the classification accuracy of ET with the relief feature selection algorithm increases from 92.09 to 94.41%. The accuracy of GB increases from 91.34 to 93.36% with the FCBF feature selection algorithm. So, the ET classifier with the relief feature selection algorithm performs excellently. P-value and Chi-square are also computed for the ET classifier with each feature selection technique. The future work of this research study is to use more optimization techniques, feature selection algorithms, and classification algorithms to improve the performance of the predictive system for the diagnosis of heart disease.
Bui, A. L., Horwich, T. B. & Fonarow, G. C. Epidemiology and risk profile of heart failure. Nat. Rev. Cardiol. 8 , 30 (2011).
Article PubMed Google Scholar
Polat, K. & Güneş, S. Artificial immune recognition system with fuzzy resource allocation mechanism classifier, principal component analysis, and FFT method based new hybrid automated identification system for classification of EEG signals. Expert Syst. Appl. 34 , 2039–2048 (2010).
Article Google Scholar
Heidenreich, P. A. et al. Forecasting the future of cardiovascular disease in the United States: A policy statement from the American Heart Association. Circulation 123 , 933–944 (2011).
Durairaj, M. & Ramasamy, N. A comparison of the perceptive approaches for preprocessing the data set for predicting fertility success rate. Int. J. Control Theory Appl. 9 , 255–260 (2016).
Google Scholar
Das, R., Turkoglu, I. & Sengur, A. Effective diagnosis of heart disease through neural networks ensembles. Expert Syst. Appl. 36 , 7675–7680 (2012).
Allen, L. A. et al. Decision making in advanced heart failure: A scientific statement from the American Heart Association. Circulation 125 , 1928–1952 (2014).
Yang, H. & Garibaldi, J. M. A hybrid model for automatic identification of risk factors for heart disease. J. Biomed. Inform. 58 , S171–S182 (2015).
Article PubMed PubMed Central Google Scholar
Alizadehsani, R., Hosseini, M. J., Sani, Z. A., Ghandeharioun, A. & Boghrati, R. In 2012 IEEE 12th International Conference on Data Mining Workshops. 9–16 (IEEE, New York).
Arabasadi, Z., Alizadehsani, R., Roshanzamir, M., Moosaei, H. & Yarifard, A. A. Computer aided decision making for heart disease detection using hybrid neural network-Genetic algorithm. Comput. Methods Programs Biomed. 141 , 19–26 (2017).
Samuel, O. W., Asogbon, G. M., Sangaiah, A. K., Fang, P. & Li, G. An integrated decision support system based on ANN and Fuzzy_AHP for heart failure risk prediction. Expert Syst. Appl. 68 , 163–172 (2017).
Patil, S. B. & Kumaraswamy, Y. Intelligent and effective heart attack prediction system using data mining and artificial neural network. Eur. J. Sci. Res. 31 , 642–656 (2009).
Vanisree, K. & Singaraju, J. Decision support system for congenital heart disease diagnosis based on signs and symptoms using neural networks. Int. J. Comput. Appl. 19 , 6–12 (2015).
B. Edmonds. In Proceedings of AISB Symposium on Socially Inspired Computing 1–12 (Hatfield, 2005).
Methaila, A., Kansal, P., Arya, H. & Kumar, P. Early heart disease prediction using data mining techniques. Comput. Sci. Inf. Technol. J. https://doi.org/10.5121/csit.2014.4807 (2014).
Samuel, O. W., Asogbon, G. M., Sangaiah, A. K., Fang, P. & Li, G. An integrated decision support system based on ANN and Fuzzy_AHP for heart failure risk prediction. Expert Syst. Appl. 68 , 163–172 (2018).
Nazir, S., Shahzad, S., Mahfooz, S. & Nazir, M. Fuzzy logic based decision support system for component security evaluation. Int. Arab J. Inf. Technol. 15 , 224–231 (2018).
Detrano, R. et al. International application of a new probability algorithm for the diagnosis of coronary artery disease. Am. J. Cardiol. 64 , 304–310 (2009).
Gudadhe, M., Wankhade, K. & Dongre, S. In 2010 International Conference on Computer and Communication Technology (ICCCT) , 741–745 (IEEE, New York).
Kahramanli, H. & Allahverdi, N. Design of a hybrid system for the diabetes and heart diseases. Expert Syst. Appl. 35 , 82–89 (2013).
Palaniappan, S. & Awang, R. In 2012 IEEE/ACS International Conference on Computer Systems and Applications 108–115 (IEEE, New York).
Olaniyi, E. O., Oyedotun, O. K. & Adnan, K. Heart diseases diagnosis using neural networks arbitration. Int. J. Intel. Syst. Appl. 7 , 72 (2015).
Das, R., Turkoglu, I. & Sengur, A. Effective diagnosis of heart disease through neural networks ensembles. Expert Syst. Appl. 36 , 7675–7680 (2011).
Paul, A. K., Shill, P. C., Rabin, M. R. I. & Murase, K. Adaptive weighted fuzzy rule-based system for the risk level assessment of heart disease. Applied Intelligence 48 , 1739–1756 (2018).
Tomov, N.-S. & Tomov, S. On deep neural networks for detecting heart disease. arXiv:1808.07168 (2018).
Manogaran, G., Varatharajan, R. & Priyan, M. Hybrid recommendation system for heart disease diagnosis based on multiple kernel learning with adaptive neuro-fuzzy inference system. Multimedia Tools Appl. 77 , 4379–4399 (2018).
Alizadehsani, R. et al. Non-invasive detection of coronary artery disease in high-risk patients based on the stenosis prediction of separate coronary arteries. Comput. Methods Programs Biomed. 162 , 119–127 (2018).
Haq, A. U., Li, J. P., Memon, M. H., Nazir, S. & Sun, R. A hybrid intelligent system framework for the prediction of heart disease using machine learning algorithms. Mobile Inf. Syst. 2018 , 3860146. https://doi.org/10.1155/2018/3860146 (2018).
Mohan, S., Thirumalai, C. & Srivastava, G. Effective heart disease prediction using hybrid machine learning techniques. IEEE Access 7 , 81542–81554 (2019).
Ali, L. et al. An optimized stacked support vector machines based expert system for the effective prediction of heart failure. IEEE Access 7 , 54007–54014 (2019).
Peng, H., Long, F. & Ding, C. Feature selection based on mutual information criteria of max-dependency, max-relevance, and min-redundancy. IEEE Trans. Pattern Anal. Mach. Intell. 27 (8), 1226–1238 (2005).
Palaniappan, S. & Awang, R. In 2008 IEEE/ACS International Conference on Computer Systems and Applications 108–115 (IEEE, New York).
Ali, L., Niamat, A., Golilarz, N. A., Ali, A. & Xingzhong, X. An expert system based on optimized stacked support vector machines for effective diagnosis of heart disease. IEEE Access (2019).
Pérez, N. P., López, M. A. G., Silva, A. & Ramos, I. Improving the Mann-Whitney statistical test for feature selection: An approach in breast cancer diagnosis on mammography. Artif. Intell. Med. 63 , 19–31 (2015).
Tibshirani, R. Regression shrinkage and selection via the lasso: A retrospective. J. R. Stat. Soc. Ser. B Stat. Methodol. 73 , 273–282 (2011).
Article MathSciNet Google Scholar
Peng, H., Long, F. & Ding, C. Feature selection based on mutual information criteria of max-dependency, max-relevance, and min-redundancy. IEEE Trans. Pattern Anal. Mach. Intell. 27 , 1226–1238 (2012).
de Silva, A. M. & Leong, P. H. Grammar-Based Feature Generation for Time-Series Prediction (Springer, Berlin, 2015).
Book Google Scholar
Download references
Acknowledgements
This research was supported by the Brain Research Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (No. NRF-2017M3C7A1044815).
Author information
Authors and affiliations.
Department of Computer Science, Abdul Wali Khan University Mardan, Mardan, 23200, KP, Pakistan
Yar Muhammad, Muhammad Tahir & Maqsood Hayat
Department of Electronic and Information Engineering, Jeonbuk National University, Jeonju, 54896, South Korea
Kil To Chong
You can also search for this author in PubMed Google Scholar
Contributions
All authors have equal contributions.
Corresponding authors
Correspondence to Maqsood Hayat or Kil To Chong .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Muhammad, Y., Tahir, M., Hayat, M. et al. Early and accurate detection and diagnosis of heart disease using intelligent computational model. Sci Rep 10 , 19747 (2020). https://doi.org/10.1038/s41598-020-76635-9
Download citation
Received : 03 April 2020
Accepted : 28 October 2020
Published : 12 November 2020
DOI : https://doi.org/10.1038/s41598-020-76635-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Comprehensive evaluation and performance analysis of machine learning in heart disease prediction.
- Halah A. Al-Alshaikh
- Abeer A. AlSanad
Scientific Reports (2024)
Heart Disease Prediction Using Weighted K-Nearest Neighbor Algorithm
- Khalidou Abdoulaye Barry
- Youness Manzali
- Mohamed Elfar
Operations Research Forum (2024)
Future prediction for precautionary measures associated with heart-related issues based on IoT prototype
- Ganesh Keshaorao Yenurkar
- Aniket Pathade
Multimedia Tools and Applications (2024)
An improved machine learning-based prediction framework for early detection of events in heart failure patients using mHealth
- Deepak Kumar
- Keerthiveena Balraj
- Anurag S. Rathore
Health and Technology (2024)
Identification and classification of pneumonia disease using a deep learning-based intelligent computational framework
- Lanying Tang
Neural Computing and Applications (2023)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- JRSM Cardiovasc Dis
- v.6; Jan-Dec 2017
Primary prevention of cardiovascular disease: A review of contemporary guidance and literature
Jack stewart.
1 Department of Cardiology, Ashford & St Peter’s NHS Foundation Trust, London, UK; Institute of Cardiovascular Research, Biological Sciences, University of London, Surrey, UK
Gavin Manmathan
2 Department of Cardiology, Ashford & St Peter’s NHS Foundation Trust, London, UK
Peter Wilkinson
Cardiovascular disease is a significant and ever-growing problem in the United Kingdom, accounting for nearly one-third of all deaths and leading to significant morbidity. It is also of particular and pressing interest as developing countries experience a change in lifestyle which introduces novel risk factors for cardiovascular disease, leading to a boom in cardiovascular disease risk throughout the developing world. The burden of cardiovascular disease can be ameliorated by careful risk reduction and, as such, primary prevention is an important priority for all developers of health policy. Strong consensus exists between international guidelines regarding the necessity of smoking cessation, weight optimisation and the importance of exercise, whilst guidelines vary slightly in their approach to hypertension and considerably regarding their approach to optimal lipid profile which remains a contentious issue. Previously fashionable ideas such as the polypill appear devoid of in-vivo efficacy, but there remain areas of future interest such as the benefit of serum urate reduction and utility of reduction of homocysteine levels.
Introduction
Cardiovascular disease (CVD) is an umbrella term for a number of linked pathologies, commonly defined as coronary heart disease (CHD), cerebrovascular disease, peripheral arterial disease, rheumatic and congenital heart diseases and venous thromboembolism. Globally CVD accounts for 31% of mortality, the majority of this in the form of CHD and cerebrovascular accident. 1
In England CVD accounts for nearly 34% of all deaths, whilst the figure is approximately 40% in the European Union. 2 The rate of CVD worldwide is predicted to increase as the prevalence of risk factors for CVD rises in previously low-risk countries. Currently 80% of CVD mortality occurs in developing nations 3 and CVD is expected to be the major cause of mortality in most developing nations by 2020, overtaking infectious disease. 4 Not only is CVD a leading cause of mortality, but it is the leading cause of loss of disability-adjusted life years globally. 3
The World Health Organisation (WHO) estimate that over 75% of premature CVD is preventable and risk factor amelioration can help reduce the growing CVD burden on both individuals and healthcare providers. 5 Whilst age is a known risk factor for the development of CVD, autopsy evidence suggests that the process of developing CVD in later years is not inevitable, 6 thus risk reduction is crucial.
The INTERHEART study elucidated the effect of CVD risk factors including dyslipidaemia, smoking, hypertension, diabetes, abdominal obesity, whilst it demonstrated the protective effects of consumption of fruits and vegetables, and regular physical activity. These risk factors were consistent throughout all populations and socioeconomic levels studied, helping to establish the viability of uniform approaches to CVD primary prevention worldwide. 7
In this review we look at the main components of primary prevention of CVD as discussed in current best practice guidelines in the United Kingdom, Europe and America and attempt to provide a summary of primary prevention guidelines in CVD for clinicians.
We looked specifically at the current National Institute for Health and Care Excellence (NICE) guidelines. 8 – 10 European Society of Cardiology (ESC) guidelines, 3 , 11 , 12 as well as guidelines from the American Heart Association (AHA) and American College of Cardiologists (ACC) 13 – 15 or, in the case of hypertension, guidelines referred to by the ACC. 16 We highlighted areas targeted by these guidelines and performed a review of current literature. A literature search was performed using the search terms ‘Primary prevention in Cardiovascular Disease’, then a combination of ‘diet’, ‘hypertension’, ‘lipids’, ‘exercise’, ‘smoking’, ‘alcohol’ ‘polypill’, ‘weight’, ‘blood glucose’ and the term ‘cardiovascular disease prevention’. Data, guidelines and their scientific underpinning were extracted from the above and compared.
Here we discuss the main areas targeted for primary prevention of CVD, looking at current guidelines, the data which supports them and any variation in guideline recommendations.
Lifestyle modifications
Exercise is universally recognised as having a positive impact on the majority of health outcomes and its effect on CVD is no different. Mortality and morbidity directly due to exercise remains minimal even up to very intense levels of exercise and in the overwhelming majority the benefits outweigh the risks. 17
NICE recommend 150 minutes of moderate intensity aerobic activity per week, or 75 minutes of vigorous aerobic activity. This can be defined either subjectively or in terms of relative changes in metabolic rate. They also advise muscle strengthening activities on two or more days per week. 8 NICE give only a consensus recommendation regarding the utility of exercise as primary prevention, however guidelines from the AHA and ESC give class 1 A recommendations with almost identical prescriptions, referring to a solid and consensual body of evidence. 11 , 13
The guidelines all state that any form of exercise provides CVD risk reduction, with those newly starting exercise achieving greatest benefit and any subsequent increases providing significant but diminishing returns. Persuading the population to exercise as suggested remains difficult despite the obvious benefits, but the evidence is clear that any increase in physical activity reduces risk of CVD. 18
Diet is thought to play a significant role in CVD risk but the body of evidence regarding its use is not clear, nor are the guidelines overwhelmingly consensual.
The AHA recommend the Dietary Approaches to Stop Hypertension (DASH) diet which is low in sugars and saturated fats, high in vegetables, fruits and whole grains. This has been shown to as a method to lower blood pressure (BP) and low-density lipoprotein cholesterol (LDL-C) which are independent risk factors for CVD, but they do not attempt to show a direct reduction in CVD risk. 13
NICE recommend reducing saturated fat intake, increasing monounsaturated fatty acids and five portions of fruit and vegetables per day. They also suggest a high fibre diet and two portions of fish per week. They do acknowledge that they lack evidence that these changes will impact directly on CVD risk, but rather that they have benefits on other areas of health. Notably, the majority of the studies referenced came from pre-1990s when dietary patterns were substantially different, and almost all their data were underpowered concerning CVD risk. 19
The ESC recommends switching from saturated to polyunsaturated fatty acids, an increase in fibre, fruit, vegetable and fish intake as well as abstinence from alcohol and adherence to a Mediterranean type diet. These have all been shown to offer significant reductions in CVD risk. 11
There is also clear evidence that industrially produced transfats are causally linked to CHD 20 and these are specifically proscribed in ESC and NICE guidelines.
The disparity between the recommendations is multi-factorial. For example, NICE guidelines on fibre intake look only at randomised controlled trials (RCTs) from the 1980s cf. the ESC which refers to meta-analyses of data up to the 2010s.
Regarding the advice on saturated fats, the ESC guidelines use modelling data to extrapolate a CVD risk reduction from reduction in LDL-C rather than epidemiological evidence or RCTs, whilst AHA guidelines do not comment specifically on CVD risk. This is an area where NICE guidelines would benefit from an update of its evidence base and greater use of prospective or epidemiological data to justify its recommendations.
In summary, there does seem to be good evidence for recommending diets high in fibre, fruit and vegetable intake and low in simple sugars and salt. Adherence to a Mediterranean style diet also appears to be cardioprotective.
Smoking has long been known as the major risk factor for CVD. 21 European data indicate that smoking doubles the 10 year CVD mortality rate 3 whilst 30% of US CVD mortality is attributable to smoking. 13 Not only is it deleterious but this effect is dose related with no safe lower limit seen. 22 Passive smoking is similarly harmful as workplace exposure increases CVD risk by 30% and UK public health initiatives including smoking bans are associated with a significant fall in CVD events. 11
Stopping smoking is the single most cost-effective intervention in CVD prevention, and some benefits are seen within months of cessation. 11 , 13 All guidelines recommend cessation, with short and long-term benefits seen irrespective of length or intensity of smoking habit.
Pharmacologically, the use of nicotine replacement therapy (NRT), buproprion (a norepinephrine dopamine reuptake inhibitor) and particularly varenicline (a partial nicotine receptor agonist) are universally recommended. The two former both improve abstinence rates by 50–70%, whilst varenicline doubles abstinence. 23 , 24
Medication choice should be patient led, with a particular note to side-effect profiles. NRT previously held warnings regarding its use in those with CVD but evidence suggests that the benefits of smoking cessation outweigh the risks. 25 Also recommended is physician intervention as a cost-effective method of reducing smoking, 26 notably effective in secondary prevention post myocardial infarction (MI). 15
E-Cigarettes are still controversial with regards to CVD risk. Whilst the reduction in toxic products within cigarette smoke is undoubtedly beneficial, animal models of nicotine exposure still display CVD effects with increased atherosclerotic plaques found in mice models. 27 Long-term data are awaited to determine the effect upon humans.
Having a body mass index (BMI) > 25 is a risk factor for CVD with lowest all-cause mortality seen at BMI 20–25 but, due to increased all-cause mortality with BMI < 20, 28 reductions below this level are not routinely recommended. No guidelines recommend specific intervention regarding weight, but advise maintenance of a healthy weight for reduction of CVD risk. BMI is a good predictor of CVD risk, particularly at higher levels, but there is good evidence that, at all levels of BMI, visceral adiposity and liver fat are significant drivers of risk. 29 This helps to explain the heterogeneity in the CVD risk profile seen in the overweight as it varies depending on the location of adipose deposition. There are moves to suggest that, alongside reduction in BMI, reduction in waist circumference as a proxy for reductions in visceral fat should become an important target for amelioration of CVD risk.
Alcohol consumption is a controversial subject given the known sequelae of regular and excess alcohol use. The difficulty exists as historically the evidence suggested a J-shaped curve when it comes to risk, where abstinence is associated with an increase in CVD compared to light drinkers, with low levels of alcohol consumption associated with a lower level of CHD. 30 Besides the understood physiological effects of alcohol, interfering with platelet aggregation, evidence from the INTERHEART study would appear to substantiate these claims, showing reductions in risk for those with moderate and light use of alcohol. 31 A recent large mendelian analysis by Holmes et al. 32 has, however, shown that within a genetic subset for alcohol dehydrogenase, reductions in alcohol intake are associated with reduction in CVD risk across the spectrum of alcohol intake. This would suggest that reductions in alcohol intake, even for moderate drinkers, are associated with a reduction in CVD risk. It is on this basis that the ESC guidelines recommend no safe level of alcohol intake. 11 NICE guidelines 8 were produced prior to this data being released and continue with advice on moderate intake, advising not more than four units per day for men and three for women, despite these being arbitrary figures. The ACC also advise moderation along the same lines, with one to two drinks per day for men, and one drink per day for women. 33 As yet there does not seem to be a consensus of opinion regarding safe levels, but high levels are evidently deleterious.
Medical treatment
Lipid-lowering therapy.
Interventions to ameliorate lipid levels have long been used in primary prevention and sub-fractions of serum lipids have been studied to differentiate their individual effects on CVD risk profile.
LDL-C is the best understood atherogenic sub-fraction with a strong correlation between LDL-C levels and CVD risk: reducing LDL-C by 1.0 mmol/L causes a corresponding 20–25% risk reduction in CVD mortality and non-fatal MI. 11
It has been hypothesised that raised high-density lipoprotein cholesterol (HDL-C) levels are cardioprotective but the causal link remains unproven. This controversy is borne out by the adverse CVD profile of HDL raising drugs such as torcetrapib, as well as recent mendelian randomisation analysis suggesting no intrinsic benefit from naturally higher levels of HDL-C. 11
Apolipoprotein B (ApoB) seems a similar predictor of CVD risk to LDL, whilst serum triglycerides lack the strength of data of LDL but remain an independent risk factor for CVD. 11
3-Hydroxy-3-methyl-glutaryl-coenzyme A reductase inhibitors, commonly referred to as statins, have been used since the 1980s to reduce LDL-C levels. Their side-effect and risk profile is well recognised, with a reported 5–10% experiencing significant side-effects, commonly in the form of myalgia, arthralgia and temporary gastrointestinal upset. 34
The AHA recommend statins for primary prevention in all patients with a serum LDL-C > 4.9 mmol/L regardless of risk profile, 14 whilst the ESC recommend statins in high-risk patients or those with cholesterol levels raised to > 4.9 mmol/L. 11 They are more circumspect about their general use, but do recommend them as ideal first-line monotherapy without suggesting dosing levels.
QRISK2 is a risk stratifying method which determines 10-year risk profile using multiple physiological and comorbidity data including serum cholesterol ratios. NICE guidelines advise atorvastatin 20 mg to be offered as primary prevention in patients < 85 years with a QRISK2 score of > 10%. It also notes that patients > 85 years are likely to benefit from a similar CVD risk reduction despite a lack of confirmatory data. NICE does not use specific cholesterol levels nor ratios as individual markers of risk, though does suggest specialist referral if total lipid levels > 9 mmol/L or non-HDL > 7.5 mmol/L. Satisfactory lipid levels remain an area of controversy, with no guidelines defining a normal range. 8
Statins are one of the most commonly prescribed medications worldwide, thus the data behind their use is plentiful, with atorvastatin shown to significantly reduce LDL-C and be the most cost-effective throughout all risk profiles. NICE states that treatment remains cost effective for those with a QRISK2 < 10%, but due to the reported side-effect profile NICE suggests 10% risk of CVD as a cut-off for statins as primary prevention. 8
The controversy regarding the above is twofold. Firstly, a 2013 paper by Abramson et al. claimed that their reanalysis of the data showed no reduction in mortality or morbidity in the low-risk population, 35 thus causing iatrogenic harm in the form of intolerable side-effects – reported in 5–10% of patients. Secondly, the corollary of this guideline would be the almost ubiquitous prescription of statins in otherwise well patients. A male aged 65 years would obtain a risk of 10% despite optimal BMI, optimal cholesterol and no comorbidities, the same being true for a 70-year-old female. 36 Given the current side-effect recommendations there is reluctance amongst the medical profession to engage in blanket therapy for a theoretical gain on a population-wide basis. Reanalysis from Collins et al., however, suggested that the side-effect profile is significantly misreported and therefore the risk–benefit ratio shifts back in favour of statins. 37 Their analysis attributes a 1% of risk of diabetes, 1% risk of muscle pain or weakness, 0.1% risk of haemorrhagic stroke and 0.05% risk of myopathy over five years of statin therapy – a significant reduction in side-effect rate.
Whilst controversy remains, the evidence is compelling for use in those with significant CVD risks and may be appropriate in more moderate risk profiles, but prescription requires careful tailoring to individual patients. A summary of guideline recommendations for LDL reduction can be seen in Table 1 .
Guidelines for LDL reduction.
| Guideline | NICE | ACC | ESC |
|---|---|---|---|
| Level at which to attempt LDL reduction | QRISK2 score > 10% if < 85 yrs | >4.9 mmol/L irrespective of risk | >4.9 mmol/L if high risk of CVD |
| Recommended pharmacotherapy | Atorvastatin 20 mg | Statin – no preferred version | Statin – no preferred version |
LDL: low-density lipoprotein; CVD: cardiovascular disease.
Non-statin therapies are also used, commonly in patients whose lipid profiles are not optimised by statin monotherapy. Commonly used drugs include bile acid sequestrants, fibrates and nicotinic acid, but these drugs are not recommended as monotherapy due to side-effects and a lack of reduction in CVD events. 11 Further reductions in serum LDL can be achieved with combination therapies. No guideline recommends specific combinations but they do suggest combination with other lipid-lowering drugs in resistant cases or in those not tolerant of statins.
New therapies are forthcoming, with phase III data from proprotein convertase subtilisin–kexin type 9 (PCSK9) monoclonal antibodies such as alirocumab providing increasingly effective lipid-lowering therapies. They can be used either as monotherapies or as add-ons to statins with a significant impact on CVD events. 38 Both alirocumab and evolocumab have recently been recommended by NICE for CVD prevention in those with primary hypercholesterolaemia, mixed dyslipidaemia or in whom statins are not sufficient to control cholesterol. 39 Their use is likely to become more widespread with further phase III and IV clinical trial data and eventual reduction in cost.
Anti-hypertensive therapies
Hypertension is an independent risk factor for the development of CVD. The effect of increasing BP > 115/75 mmHg is consistent and exponential, where each 20 mmHg increase in systolic blood pressure (SBP) or a 10 mmHg increase in diastolic BP doubles the risk of a cardiovascular event. 40
Previous meta-analyses have shown a reduction in CVD risk over a wider range of BPs suggesting that there is no lower limit to the benefit of BP reduction, and no obvious cut-off at which further reductions become harmful. 41 , 42
Contemporary meta-analyses indicate that the benefits of lowering BP from a baseline < 140 may be equivocal or even detrimental. 43 Combining this evidence would suggest that BP reductions in hypertensives reduce mortality, but for normotensive or pre-hypertensive patients there is little evidence for early treatment.
Given that hypertension acts as an independent risk factor for CVD, and synergistically with other risk factors, it is the consensus opinion that the threshold for treatment of hypertension in those at risk of CVD should be lower. 44
Regarding timing of intervention and precise target ranges there is some variability between guidelines which can be seen broadly in Table 2 .
Guidelines for commencement of anti-hypertensives and target BP.
| Guideline | NICE | ACC recommended guidelines | ESC |
|---|---|---|---|
| Commencement of treatment – no comorbidities | >160/100 mmHg | >150/90 mmHg if ≥60 yrs | >160/100 mmHg – after lifestyle modification attempted |
| >140/90 mmHg if <60 yrs | |||
| Target | <140/90 mmHg if <80 yrs | <150/90 mmHg if ≥60 yrs | <140/90 mmHg if < 60 yrs |
| <150/90 mmHg if >80 yrs | <140/90 mmHg if < 60 yrs | SBP 140–150 mmHg if > 60 yrs | |
| Commencement of treatment if CKD/ DM/ risk of CVD | >140/90 mmHg | >140/90 mmHg | >140/90 mmHg |
| Target | <140/90 mmHg | <140/90 mmHg | <140/90 mmHg |
CKD: chronic kidney disease; DM: diabetes mellitus; CVD: cardiovascular disease.
The ESC and NICE guidelines note that the majority of data showed greatest benefit for those with BP > 160/100 mmHg, and whilst there may be benefit at lower levels 45 the evidence was not yet considered strong enough to give direct recommendations. 12
Strong evidence suggests that the reduction in BP is more important than the individual drug class used, 46 compounded by the fact that the majority of people with hypertension require more than one antihypertensive drug for optimal control. 47
The recommended pharmacotherapy can be seen in Table 3 .
Recommended anti-hypertensive therapy.
| Guideline | NICE | ACC recommended guidelines | ESC |
|---|---|---|---|
| First line anti-hypertensive therapy | If <55 yrs – ACEi/ARB If > 55 yrs/Afrocaribbean descent – CCB or thiazide | ACEI/ARB, thiazide, CCBs If black – thiazide or CCB | ACEi, thiazide, CCB, ARB, beta blocker |
| Additional notes | Use 2 drugs if goal BP not reached within one month |
ACEi: angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blocker; CCB: calcium channel blocker; BP: blood pressure.
NICE justify the changes in treatment for Afro-Caribbean patients due to differences in plasma renin concentrations between ethnic groups and a tendency towards lower cardiac output with increased peripheral resistance in Afro-Caribbean hypertensives. 48 The ACC recommended guidelines note that the ALLHAT trial showed improved outcomes in Afro-Caribbean patients treated with thiazides, whilst calcium channel blocker (CCBs) improved all outcomes other than heart failure. 49
A small discrepancy exists with the ESC guidelines. Their use of beta blockers stems from a meta-analysis suggesting that the class cause an equal reduction in CVD mortality, though the ESC do acknowledge conflicting data which suggests inferiority and an increased side-effect profile. 12
Whilst risk of CVD increases with BP, the majority of population events occur within the upper range of normal, therefore NICE public health guidelines 10 suggest that a population-wide drop in BP would lead to a significant reduction in CVD events. As this group does not receive antihypertensive treatment, they recommend population measures to reduce salt intake. Salt intake is well associated with BP, with a strong causal link between increased intake and rise in BP. The reverse is also true: studies looking at reduction in salt intake show consistent reductions in BP, particularly in hypertensive individuals, 50 and there is evidence of CVD event reduction. 51 Given the above, all three guidelines recommend reduction in salt intake on an individual and population level regardless of BP.
Specific daily targets vary, largely due to the responsibilities of each organisation: AHA 2.4 g, ESC 5–6 g and NICE 6 g reducing to 3 g by 2025. 10 , 11 , 13 NICE also has a greater public health remit than the ESC and AHA and recommends national-level interventions such as population education, pricing changes on higher-salt products, and national legislation if necessary to aid reduction in salt intake (NICE PH25). All agree, however, that lower salt intake leads to BP reduction and concomitant CVD risk reduction. 52
Blood glucose
Glucose control is pertinent in the diabetic populations but is non-significantly associated with CVD risk in non-diabetics. On average diabetes mellitus (DM) risk of CVD, whilst those with impaired fasting glucose (IFG) are known to be at significant risk of CVD as well as progression to DM. 53 In DM serum glucose reduction is shown to reduce CVD, with lowest risk at normal blood sugars. 54 More intense glucose reductions were deleterious, with particular CVD risk from certain thiazolidinediones and dipeptidyl peptidase-4 inhibitors. 55 Recent trials from the sodium/glucose transporter 2 inhibitor class of oral hypoglycaemics such as empagliflozin have been shown to significantly reduce all-cause mortality by 32%, as well as CVD death by 28% and HF by 35% in comparison with standard care. 56 It appears that these effects were not mediated by reduction in glucose, rather cardio-renal haemodynamic effects, but the substantial benefits demonstrated would recommend its early use in diabetic patients. Current guidelines need to be updated with further data on these medications.
Anti-platelet therapy
Anti-platelet therapy is a significant contributor to secondary prevention but should be avoided in primary prevention in those without comorbidities due to increased bleeding risk with no evidence of CVD risk reduction. In patients with DM the advice is conflicting: ESC guidelines maintain that the bleeding risk exceeds the benefits of aspiring therapy, whilst the American College of Chest Physicians recommend aspirin therapy in patients with DM and 10-year CVD event risk of ≥ 10%. 57
Further areas of research
Other areas include the polypill, uric acid and homocysteine. The use of a polypill – a combination pill for CVD risk reduction – has impressive theoretical benefits, but meta-analyses on in-vivo data have not demonstrated significant improvement in CVD risk. 58
Lowering serum uric acid levels may improve CVD risk, as it is known that both patients with gout or hyperuricaemia receiving urate-lowering therapies have improved CVD and all cause-mortality 59 , 60 ; however more research is needed to clarify if these benefits translate to population-wide risk reduction. Homocysteine is a known atherogen, but lowering therapies have not demonstrated a reduced CVD. 61
The objective of CVD prevention is to reduce the occurrence of major cardiovascular events thereby reducing premature disability and morbidity whilst prolonging survival and quality of life.
The American, European and British guidelines demonstrate numerous methods to reduce CVD risk profile with strong consensus regarding smoking and exercise, whilst the fine details may vary slightly for other factors. Pharmaceutical options have developed over the years whilst lifestyle advice remains largely unchanged.
Primary prevention continues to evolve and with greater availability of long-term data comes improved understanding of the means by which we can reduce CVD risk. It is an endeavour that must be continued if we are to reduce the burden of a preventable disease.
Acknowledgements
The authors thank Ms Nicola F Raeside and Ms Katherine A Addy.
Declaration of conflicting interests
The author(s) declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval
Dr Jack Stewart.
Contributorship
The main text was written by Dr. Jack Stewart, draft revision was performed by Dr Gavin Manmathan and the review was supervised and guided by Dr Peter Wilkinson.
VA Rating for CAD (Coronary Artery Disease)
Last Updated
Claire Szewczyk

Table of Contents
Coronary Artery Disease (CAD) is a common condition among veterans, particularly those exposed to Agent Orange during their service. The coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to plaque buildup, leading to chest pain, heart attacks, and other serious heart issues.
The VA recognizes the significant impact of CAD on veterans’ health and offers disability ratings to provide necessary compensation.
How Does the VA Rate CAD?
The VA rates CAD based on the severity of the condition and its impact on the veteran’s ability to work and perform daily activities. Ratings range from 10% to 100%, reflecting the extent of the disability and corresponding compensation levels.
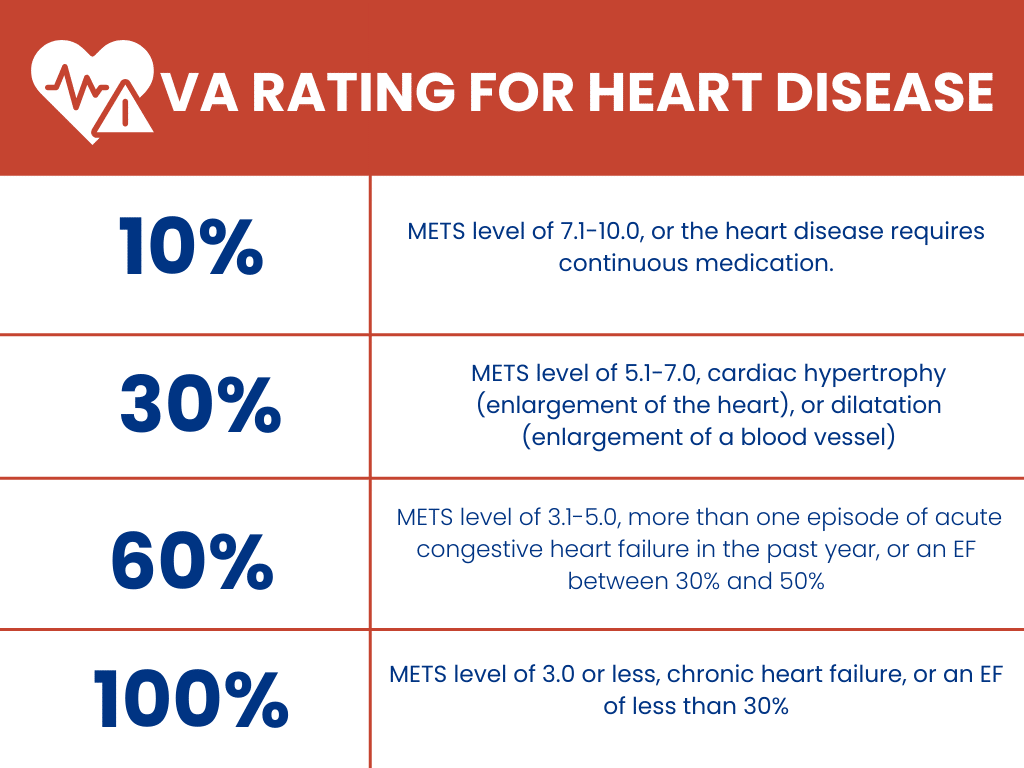
Learn to Prepare (and Win!) Your VA Claim with Our Free Ebook The Road to VA Compensation Benefits
Conditions that Fall Under the Coronary Artery Disease Umbrella
Several conditions are categorized similarly to CAD, including:
- Angina (chest pain)
- Myocardial infarction (heart attack)
- Atherosclerosis (plaque buildup in the arteries)
- Chronic ischemic heart disease
These conditions are interconnected and can significantly affect a veteran’s health and quality of life, warranting varying levels of VA disability compensation.
Is CAD a Presumptive Condition?
Agent Orange, a herbicide used during the Vietnam War , has been linked to numerous health issues, including CAD and other heart conditions. Veterans exposed to Agent Orange are at higher risk for developing them, and the VA recognizes this connection by offering presumptive service connection for ischemic heart disease, which includes CAD.
This means eligible veterans will receive VA disability compensation without needing to prove a direct service connection . For those exposed to Agent Orange, the presumption of service connection simplifies the path to obtaining deserved benefits for CAD and related conditions.
Successful Increase of Noncompensable (0%) Rating
Claim File Referenced Here A veteran initially received a noncompensable (0%) rating for coronary artery disease with arteriosclerosis. However, after presenting new medical evidence that demonstrated the true severity of his condition, the veteran successfully secured a 60% disability rating. Ejection Fraction Findings: On October 19, 2010, a VA echocardiogram revealed that the veteran had an ejection fraction of 45 +/- 5 percent. This crucial finding aligned with the criteria for a 60% disability rating under the VA’s diagnostic code for coronary artery disease, which requires an ejection fraction between 30% and 50%. 2004 CT Scan: The veteran’s post-service medical records initially only showed generalized arteriosclerosis, but no direct evidence of coronary artery disease. This was reflected in an August 2004 VA CT scan, which detected calcification of the aorta without indicating a specific heart condition. December 2010 Nuclear Radiology Consultation: The veteran’s MET level was measured at 4.8 METs, further supporting the case for a higher rating due to the physical limitations caused by his heart condition. January 2012 VA Heart Examination: The veteran underwent a VA heart examination in January 2012, where his METs level was assessed at >3-5, consistent with activities such as light yard work or brisk walking. This examination confirmed ongoing symptoms of dyspnea, dizziness, fatigue, and occasional syncope, which were vital in maintaining the 60% rating. Ultimately, the Board of Veterans’ Appeals recognized the veteran’s worsening condition and granted a 60% disability rating effective from October 19, 2010. This case highlights the importance of thorough medical evaluation and the role of specific diagnostic tests, such as ejection fraction measurements, in securing a higher VA disability rating.
Master the VA Disability Claims Process
Your Free Guide to Getting VA Benefits
Content Reviewed by
Cassandra Crosby
Cassandra, an Accredited Agent and claims advocate for Matthew Hill & Shelly Mark’s teams, reviewed the information provided in this post.
Claire Szewczyk is a Digital Content Coordinator for Hill & Ponton, PA in Florida. She was a former US Airforce civilian employee, who worked at Hill Air Force Base, in Layton, UT as a flight testing administrator. She has also spent several years working with the Department of Veterans Affairs audiology programs in Salt Lake City, UT and Pocatello, ID. She enjoys working with the Veteran population and keeping them up to date with information they need the most.
More Articles
News and advice about the VA, disability ratings and benefits.
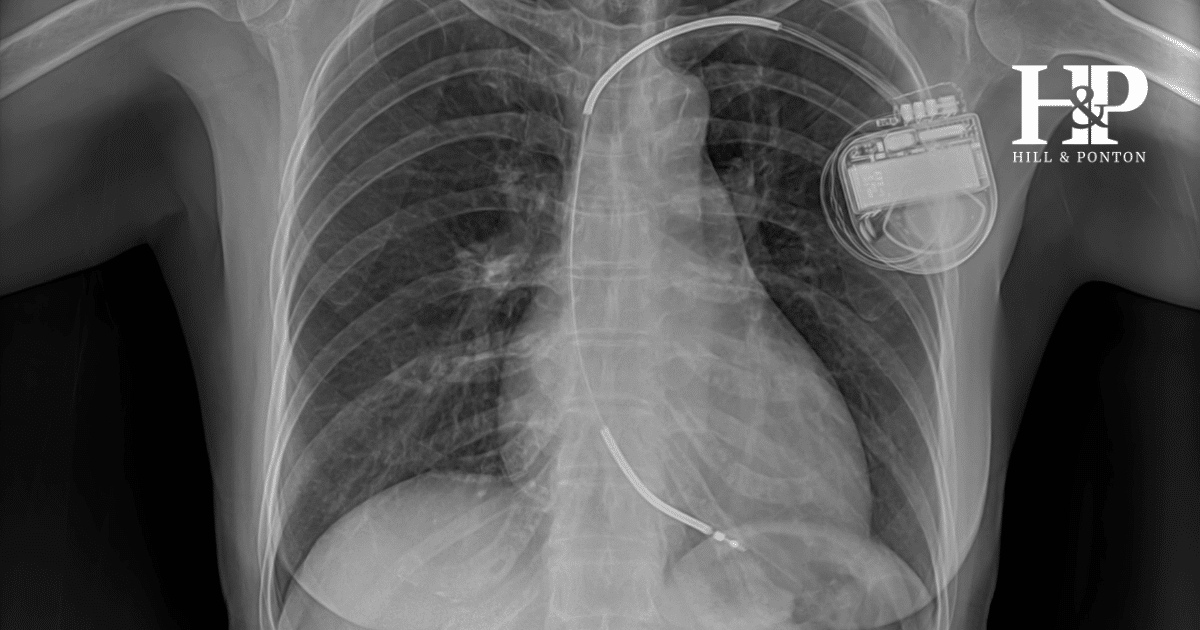
VA Disability Ratings for Pacemakers and Implantable Cardiac Defibrillators

VA Disability Rating for Tachycardia
Heart Arrhythmia VA Disability Rating
Testimonials, supporting veterans nationwide.
Thank you to the firm of Hill & Ponton!! Brian Hill and his staff were able to get my 100% disability with the VA for my exposure to herbicides in Thailand. I have been fighting for this for many years and kept getting denied, after consulting with Hill & Ponton I decided to let them help me and it was the best decision I could have made. I found their professionalism to be outstanding.
– Chip P.
North Carolina
They got my disability rating after I was denied twice. They knew exactly how to format and submit the claim. I was rated 50%, Hill & Ponton weren’t done, they found other medical that related to exposure and submitted additional claims. I could not have received a disability rating without Hill & Ponton. If you need help, choose Hill & Ponton.
– Thomas D.
The service provided by Hill and Ponton was exemplary. The lawyers and staff took care of every aspect with respect and understanding of the clients needs. In my case, as a new widow, they patiently walked me through each step. They kept me informed of the progress. I cannot say enough about the service they provided. Thank you Brian and staff.
– Judith K Zitzewitz
As a Vet you may have filed a disability claim, and if you want to win your claim you need to call Hill and Ponton. I didn’t know what to do about my condition or status until I made the call. At H&P they not only took my case, but made me feel like family. They changed my life and they will change your life too. It’s true! In my opinion you can’t do better and you won’t regret it!
– Paul K

About Hill & Ponton
Learn about the VA disability law firm, champions for veterans since 1986.

IMAGES
COMMENTS
Coronary Heart Disease (CHD) it is also know as Coronary Artery Disease. It happens when the blood vessels delivering to the heart develop blockage or are narrowed by plaque, which reduces the flow of the blood, oxygen and nutrients supplied to the heart. If this happens the person starts to feel chest pain (also known as angina pectoris) and ...
Heart disease, including coronary heart disease, remains the leading cause of death in the United States. However, the rate of heart disease deaths has declined by 70% over the past 50 years, thanks in part to NHLBI-funded research. Many current studies funded by the NHLBI focus on discovering genetic associations and finding new ways to ...
Request an Appointment. 410-955-5000 Maryland. 855-695-4872 Outside of Maryland. +1-410-502-7683 International. Coronary artery disease (also called coronary heart disease) is the number-one killer of both men and women in the United States, and it's the most common type of heart disease.
Symptoms of coronary artery disease happen when the heart doesn't get enough oxygen-rich blood. Coronary artery disease symptoms may include: Chest pain, called angina. You may feel squeezing, pressure, heaviness, tightness or pain in the chest. It may feel like somebody is standing on your chest.
Heart disease is the leading cause of death in the United States. Coronary heart disease is a type of heart disease where the arteries of the heart cannot deliver enough oxygen-rich blood to the heart. It is also sometimes called coronary artery disease or ischemic heart disease. About 20.5 million U.S. adults have coronary artery disease ...
Reference lists of identified papers, relevant reviews and meta-analyses were scrutinized for additional articles. The study period was 2000-2019 and excluding letters, editorials, conference abstracts, reviews, and comments, we used the following key words "Coronary Artery Disease", "Acute Coronary Syndrome", "Coronary Heart ...
The coronary heart disease studies were not restricted during the search by sample size because of the limited number of studies in selected countries. The study reviews the potential risk factors responsible for coronary heart disease globally. ... Duplicate articles and papers with incomplete information, like conference proceedings, were ...
The Heart Protection Study (HPS) showed unambiguous benefit of statin administration in individuals aged 40 to 80 years with total cholesterol >135 mg/dL and at risk because of a previous MI or other coronary or noncoronary artery occlusive disease, diabetes mellitus, or treated hypertension. 19 The Physicians' Health Study (PHS) showed that ...
Coronary artery disease (CAD) continues to pose a health challenge, impacting numerous individuals and placing strain on healthcare systems worldwide. The narrowing and blockage of arteries due to CAD can lead to complications like heart attacks and heart failure. Over time, dedicated efforts from researchers, professionals, and governments ...
These are the blood vessels that supply blood and oxygen to the heart. The condition is also called coronary heart disease (CHD). CAD is usually caused by atherosclerosis. Atherosclerosis is the buildup of cholesterol plaque inside the coronary arteries. These plaques are made up of fatty deposits, inflammatory cells, calcium, and fibrous tissue.
Coronary artery disease (CAD) is the world-wide leading cause of death not only in high-income countries but also increasingly in developing countries. 1 Although death rates from CAD have decreased in most high- and middle-income countries in the past 2 decades, there are worrying signs of a lessening trend in the United States, 2 and the dramatic increases of world-wide obesity 3 and ...
Coronary artery disease is caused by the gradual buildup of cholesterol or plaque, which makes the arteries stiffen and narrow. The result is reduced blood flow to the heart. Multiple causes of coronary artery disease include: Genetics: Having a family history of heart disease. Lifestyle: Eating unhealthy, high-fat foods and being sedentary.
However, coronary heart disease, or CHD, is actually a result of coronary artery disease, or CAD. With CAD, plaque first grows within the walls of the coronary arteries until the blood flow to the heart's muscle is limited, which prevents the heart muscle from receiving enough oxygen. This is also called ischemia.
No disease can have been so extensively studied. The work of recent years has yielded remarkable advances in our understanding, and in diagnostic and interventional cardiology, surgery, and pharmacology—effort well spent for a disease that carries such heavy social and economic costs. The clinical condition of coronary heart disease (CHD) presents as (i) angina, (ii) myocardial infarction ...
Pathophysiology of Coronary Heart Disease: As previously touched upon, Coronary Heart Disease is caused by a build up of fat deposits within the coronary arteries and more than 110,000 people in the UK die each year because of this condition. These fatty deposits or atheroma as they are medically termed are a mixture of cholesterol and other ...
Coronary artery disease is a condition in which there is an inadequate supply of blood and oxygen to the myocardium. It results from occlusion of the coronary arteries and results in a demand-supply mismatch of oxygen. It typically involves the formation of plaques in the lumen of coronary arteries that impede blood flow. It is the major cause of death in the US and worldwide. At the beginning ...
The objective of this series is to provide our readership with a timely, comprehensive selection of important papers that are relevant to the quality and outcomes, and general cardiology audience. ... recommended depression screening in patients with coronary heart disease: data from the Heart and Soul Study. Circ Cardiovasc Qual Outcomes. 2011 ...
High blood pressure is a risk factor for coronary heart disease, myocardial infarction and stroke and is very common in older adults. 3 It is a leading cause of preventable illness and death. 3 Controlling high blood pressure is shown to reduce the risk of fatal myocardial infarctions and strokes. 3. Lowering blood pressure can be done safely ...
There are several kinds of heart disease, including: cardiomyopathy: a heart muscle disease that causes the heart to become abnormally enlarged, thickened, and/or stiffened. congenital heart disease: heart disease or abnormalities in the heart's structure that are present at birth. coronary artery disease: accumulation of cholesterol-filled ...
Cardiovascular disease (CVD) is a collective term designating all types of affliction affecting the blood circulatory system, including the heart and vasculature, which, respectively, displaces and conveys the blood. This multifactorial disorder encompasses numerous congenital and acquired maladies. CVD represents the leading noncommunicable cause of death in Europe (∼50% of all deaths; ∼ ...
Heart disease is a fatal human disease, rapidly increases globally in both developed and undeveloped countries and consequently, causes death. Normally, in this disease, the heart fails to supply ...
Ischemic heart disease (IHD) is the greatest single cause of mortality and loss of disability-adjusted life years worldwide, and a substantial portion of this burden falls on low- and middle-income countries (LMICs). Deaths from IHD and acute coronary syndrome (ACS) occur, on average, at younger ages in LMICs than in high-income countries, often at economically productive ages, and likewise ...
Aim: This paper presents a review of the qualitative literature which examines the experiences of patients with coronary heart disease. The paper also assesses whether the experiences of both female and male patients are reflected in the literature and summarizes key themes. Background: Understanding patients' experiences of their illness is important for coronary heart disease prevention and ...
Cardiovascular disease (CVD) is an umbrella term for a number of linked pathologies, commonly defined as coronary heart disease (CHD), cerebrovascular disease, peripheral arterial disease, rheumatic and congenital heart diseases and venous thromboembolism. Globally CVD accounts for 31% of mortality, the majority of this in the form of CHD and ...
Coronary Artery Disease (CAD) is a common condition among veterans, particularly those exposed to Agent Orange during their service. The coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to plaque buildup, leading to chest pain, heart attacks, and other serious heart issues.